ENGLISH-COMMUNITY HEALTHA NURSING -18/04/2023 (done-only shs-modify pending)-PAPER NO.SIX-UPLOAD
ENGLISH-COMMUNITY HEALTHA NURSING -18/04/2023 PAPER NO.6
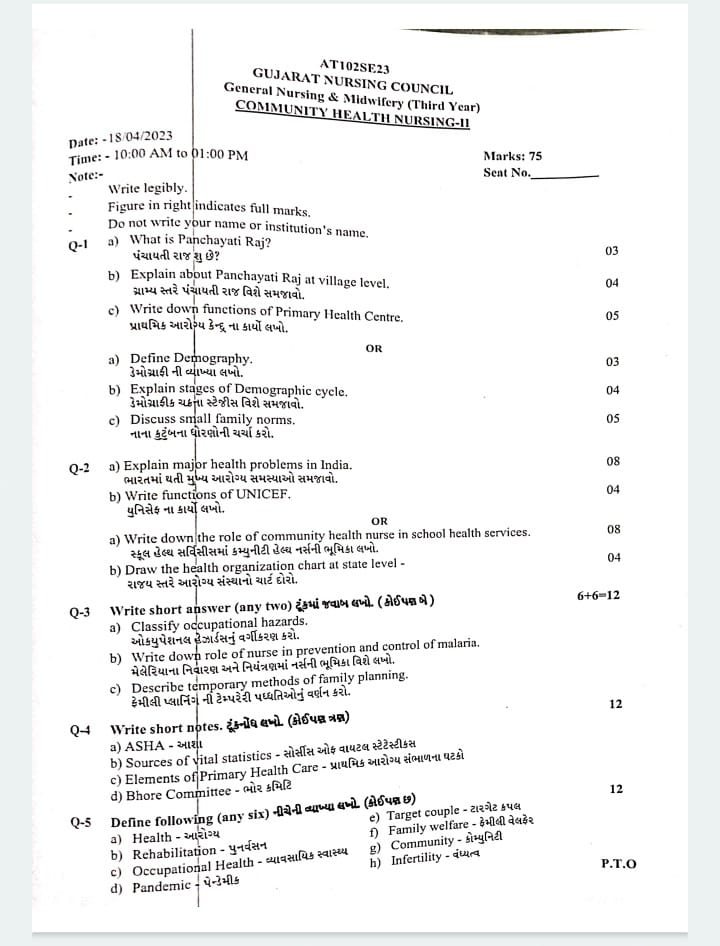
Q-1 a) What is Panchayati Raj? પંચાયતી રાજ શુ છે?
What is Panchayati Raj?
The Panchayati Raj System was introduced in 1957.
This system connects the villages with the districts, so that people’s partitions increase and the administration is strengthened at the basic level.
The Panchayati Raj System includes three -level structures of Rural Self Government to invest in various levels.
1 Panchayat at Village Level
2 Panchayat Committee at Block Level
3 District Council At District Level
The Panchayati Raj Samiti is the unique welfare agencies of our Democratic Pattan in which the Public Welfare Plan and Development Program can be run at the grass route level.
b) Explain about Panchayati Raj at village level. ગ્રામ્ય સ્તરે પંચાયતી રાજ વિશે સમજાવો.
Explain about Panchayati Raj at the village level
The Panchayat Raj Village Level includes the following three institutions.
1 gram assembly
2 Gram Panchayat
3 Justice Panchayat
- Gram Meeting
The Gram Sabha is a meeting of all adults from Village, which is the registered voters of the village.
They meet at least twice a year and discount on imported issues.
It discusses health related developmental aspects. The Gram Sabha elections a member of the Gram Panchayat - Gram Panchayat
The Gram Panchayat consists of 15 to 30 elected members, known as the Punch. The Gram Panchayat covers more than 5000 or 15,000 populations.
Gram Panchayat
The function of the Gram Panchayat is very widespread and it covers the Antire Field of the Civil Administration The function is as follows
Sanitation
Public health
Socio Economic Development of Village
Planning and organizing a health activity in Village
3.New panchayat
It includes five members of the panchayat
It gives a solution with mutual consent in disputes between two parties or groups of the village or the persons of the village
It resolves the problem of going into a formal judicial system and creates Harmony & Peace Full Environment in Members and Village.
c) Write down functions of Primary Health Centre. પ્રાથમિક આરોગ્ય કેન્દુ ના કાર્યો લખો.
Works of Primary Health Center:
The Establishment of the Primary Health Center (PHC) was made by the Bhor Committee to provide health services in the Rural Area, which is a PHC of 30,000 in the Plain area, while in the Hilly, Tribal, and the PHC of the PHC of 20,000 in the backyard area.
The functions of the Primary Health Center (PHC) are as follows:
1) Medical Care
2) MCH Services Including Family Planning.
3) Safe water supply and basic sanitation.
4) Prevention and Control of Lokley Endemic Disease
5) Collection and Reporting of Vital Statistics.
6) Education About Health.
7) National Health Program Establishment and Awareness
8) Referral Services
9) Training of Health Guide, Health Worker, Local Dai and Health Assistant.
10) Basic Laboratory Services.
Description:
•> 1) Medical Care:
Primary Health Center provides basic medical care to treat acute and chronic health condition. It also provides outstanding patients with through diagnosis, treatment and miner ilens and injury.
PHC Medical Care is an Essential for Meeting Community Immediate Health Need.
Medical care patients are provided with tablets, injections, dressing, and other treatment as per their decisions.
2) MCH (Maternal and Child Health) Services Including Family Planning:
Comprehensive Maternal and Child Health Care is provided in the Primary Health Center, including prenatal care,
Antinatal checkup,
Safe Delivery Services,
Post Nettle Care,
Immunization is also provided for the child.
In order to support Family Planning Initiatives,
Family Planning,
Counseling,
Contraceptive,
And a reproductive health service is provided.
It also includes RCH in Maternal and Child Health, which takes up the care up to Adoltsant in the reproductive child health of the mother.
This is explained about antinetal care, nutrition, hygiene, immunization, and laboratory examinations, etc.
Regular checkups, observations, as well as education about family planning are provided in the post nettle period.
3) Safe Water Supply and Basic Sanitation:
The Primary Health Center works to improve the health of the public in the community by providing the facility of safe drinking water and sanitation in the community.
Primary Health Center is proved to promote hygienic practice, as well as promoting clean water source, and education for promoting the overall health of the community, as well as to promote clean water sources.
Steps are taken to maintain environment cleanliness in which people are educated about basic sanitation, excreta disposal, and cleanliness of kitchen, garden.
In addition, there should be drinking water wells and taps for safe water supply which should be chlorination.
4) Prevention and Control of Lokley Endemic Disease:
The Primary Health Center plays a crucial role to control the prevention, survey, and locally endemic diseases.
It contains masters to prevent diseases, including vaccination, providing endemic diseases treatment, and its trains are monitored to prevent out -of -breaking diseases.
5) Collection and Reporting of Vital Statistics:
The Primary Health Center works for collecting and reporting if there is an insidion of any disease in the Vital Statistic such as birth rate, death rate, and perticular community. This collected data is required for health planning, for allocation of resources, to improve health out cums, and to monitor health trends to give priorities to health interviews.
6) Education About Health:
The Primary Health Center provides education about the person and the community about Preventive Health Practices, Nutrition, Hygiene, Sanitation and Disease Prevention Strategies.
The Primary Health Center organizes Health Education Session, Workshop and Seminar to bring improvement to health conditions.
7) National Health Program Establishment and Awareness:
The Primary Health Center implements the National Health Program and Companing, which Main Aime A,
Specific Health Issues contains, including the immunization drive,
Campaigns on Disease Moors Afts, Nutrition Supplementation, and Health Awareness are launched.
They spread awareness about National Health Priorities and encrape the partship of the community in Health Initiatives.
Each National Health Program has important operations. The clinic provides the services related to the National Health Program, such as,
Anemia Control Program,
Refer to the Mother of Mother in Enormal Condition during Malaria, Deria, Leprosy, Immunization, TB Control Program, Supplementary Program Labor for additional services, referring it to Female Health Worker, Oxillary and Nurse Mid Wife or Medical Officer.
8) Referral Services:
When the patient needs any Specialist Medical Treatment or requires any special diagnosis, and if its facilities are not available in the Primary Health Center, the Primary Health Center also works to refer to the patient.
The Primary Health Center provides Immidal Referral Services as per the requirement of the patient, which can bring improvement in the health condition of the patient and prevent complication.
9) Training of Health Guide Health Workers, Local Day, and Health Assistant.
The Primary Health Center conducts training program, which provides a training program to improve their skills and knowledge to Community Health Worker, Traditional Birth Attendance, Health Assistant, Health Assistant, and other Health Care Persons.
Promotion of this training Main MA Health, Prevention of Disease, Maternal and Child Health, and Improving Health Care Persons Skills in Basic Medical Care.
10) Basic Laboratory Services:
The Primary Health Center conducts a basic laboratory services that are tested such as diagnostic tests, blood tests, microscopic tests, urine tests, etc.
All of these functions provided by the Primary Health Center provides the prevention, promotive, curative care of the community, which can cause overall health condition improvement of the people of the community and its walbing can remain maintenance.
OR
a) Define Demography. ડેમોગ્રાફી ની વ્યાખ્યા લખો.
Demography Definition:
Demos Means People
Graphin Means The Record.
Demographic Human Population and its elements ie size, composition and scientific study of distribution are called demography. Demography is a scientific study of population.
Concept of Demography Demography is a branch of science that has studied about Human Population, only three elements are specially provided.
3) Geographical distribution based on state or territory.
1) If any changes occur in the size of the population, that is, the size is the increases or decrees.
2) Structure of Population (Basic of Edge and Size).
b) Explain stages of Demographic cycle. ડેમોગ્રાફીક ચક્રના સ્ટેજીસ વિશે સમજાવો.
The mainly 5 stage of the demographic falls.
1) First Stage = High Stasner Stage,
2) Second Stage = Early Expanding,
3) Third stage = late expanding,
4) Fourth Stage = Low Stationery,
5) Fifth Stage = Declain Stage
1) First Stage = High Stasner Stage:
There are no changing in the size and composition of the population in the high stationary stage.
Birth Rate: ^ High
Death Rate: ^ High
Because of them, the high birth rate and the high death rate, both canceling each other, and that the Population is stationary.
Until the mid -17th century, the world’s population was in this stage and India was in this stage until 1920.
Ex: India in 1920
2) Second Stage = Early Expanding:
Death rate is decreed in the second stage Early Excendting Stage because there is an improvement in the health condition and the birth rate remains unchanged.
Birth Rate: ^ Unchang
Death Rate: ↓ Declain
The berth rate does not change in the Early Expanding stage, but the deerlet is reduced, which causes a slight increase in the size of the population.
The world’s population was in this stage from the 17th century middle to the middle of the 19th century. India was in this stage from 1921 to 1950
Ex: South Asia, Africa
3) Third Stage = Late Expanding:
The death rate in the third stage late expanding stage is a little more Declain and Berth Date is a little dicline.
Birth Rate: ↓ Slide (a little) decline
Death Rate: ↓ Farfar Declain
Birth date in the late expanding stage is a bit decline while the death rate is a little more decline but the birth date is a little higher than the death rate is seen.
Ex: China, Singapore and India
4) Fourth Stage = Low Stationery:
Birth date is taken in the Fourth Stage Law Stationary Stage and a debt rate is also caused by a stable stationary (stable).
Birth Rate: ↓ Take
Death Rate: ↓ Take
Due to the low birth and death proportion in this stage, the stability of the population is seen and this is usually the mainly in the developed and industrialized country.
Zero population growth is noted in Australia during 1980-1985.Ex: = Australia in 1980-1985.
5) Fifth Stage = Declain Stage:
Birth date in the Fifth Stage Decline Stage is a Further Law when the date remains unchecked, causing a decrease in population.
Birth rate: ↓ Take Farter
Death Rate: ↓ Unchanged
Thus, due to the decline in this decline stage, the decline in populations is seen due to the decline and when the dethrate is, which is usually found in Germany and Hungary.
Ex: = germany and hungary.
Demographic bicycles help explain how populations are developed and transitioned by various stages of development, affectionate from Sosio-Economic Factor, Technological Advancement and Cultural Changes.
c) Discuss small family norms. નાના કુટુંબના ધોરણોની ચર્ચા કરો.
Small Family Norms is a set of social and cultural rules and beliefs that anchorage the number of children in the family, especially for having one or two children. This normus involves ideas and habits that gives the family priority to keep the family in small size, so that the health, education and economic condition of the family members can be better and can develop in the society. The concept also covers medical terms such as Population Control, Maternal and Child Health, and Family Planning, which has the purpose of reducing the risk of a more childbirth for the health of the female. Therefore, the main purpose of Small Family Normas is to build Healthy, Social and Affordable and Sustainable Family.
Q-2 a) Explain major health problems in India. ભારતમાં થતી મુખ્ય આરોગ્ય સમસ્યાઓ સમજાવો.
A health problem is a condition in which a person is unable to function normally.
Some of the major health problems include:
1) Communicable diseases,
2) Non-communicable diseases,
3) Nutritional problems,
4) Environmental problems,
5) Medical care problems,
6) Population problems
•>1) Communicable diseases:
Communicable diseases are diseases that are transmitted from one person to another by infectious agents or their toxic products. This transmission can mainly occur directly or indirectly.
Its transmission can occur through contact with body fluids, through respiratory droplets, and through contact with contaminated surfaces.
Communicable diseases are a major health problem in India and 54% of deaths in India are due to communicable diseases.
Communicable diseases such as malaria, tuberculosis, diarrhea,
Acute respiratory diseases,
Filariasis,
HIV/AIDS,
Sexually transmitted diseases(STD)/Sexually transmitted infections(STI).
These communicable diseases are considered a major health problem in India.
a) Malaria:
Malaria is a major health problem in India.
Malaria is caused by the Plasmodium parasite which is transmitted through the bite of mosquitoes. There are four types of malarial parasites:
1) Plasmodium vivax,
2) Plasmodium ovale,
3) Plasmodium malariae
4) Plasmodium falciparum.
Malaria continues to be a major health problem in India. Although the total number of cases has decreased compared to previous years, the incidence of Plasmodium falciparum has increased.
According to WHO, malaria affects 36% of the world’s population, with India contributing more than 70% of the 2.5 million cases reported in South East Asia, while 2/3 of the Indian population lives in malaria zones, with the highest incidence of malaria cases in the states of Madhya Pradesh, Chhattisgarh, Jharkhand, Odisha, Andhra Pradesh, Maharashtra, West Bengal and the North Eastern states.
During 2015, 1.13 million malaria cases were reported, of which 67% were due to P. falciparum, while 287 deaths were reported.
b) Tuberculosis:
Tuberculosis is a bacterial disease caused by Mycobacterium tuberculosis. The tuberculosis bacteria infect the lungs and are spread by sneezing, coughing.
India is the country with the highest TB burden. It remains a major health problem. One-fifth of the world’s incidence of tuberculosis disease is found in India alone.
Every year, about 2.2 million people develop tuberculosis disease, of which 0.62 million are new smear-positive highly infectious cases and 0.24 million people die of tuberculosis disease every year.
According to WHO 2010, the incidence of tuberculosis in India was estimated at 249 per 100,000 population and the mortality rate due to tuberculosis disease was 23 per 100,000 population.
( C ) Leprosy:
Leprosy is another major health problem in India.
It is a bacterial disease caused by the bacteria Mycobacterium Leprae. It is transmitted through close contact with an infected person. This disease affects the skin, mucous membranes, and nervous system. It causes skin discoloration and nerve damage.
Leprosy is a major health problem in India. According to the World Health Organization (WHO), 65% of new cases of leprosy occur in India. During 2013-14, about 1.27 lakh cases were detected. Out of which 9.49% were in children under 15 years of age and deformity grade II.
Of these, 51.48% of the cases were estimated to be multibacillary. All states and union territories report cases of leprosy. However, there is significant variation not only between one state and another but also between one district and another.
India is home to 54% of the world’s leprosy.
(d) Diarrhoea:
Diarrhoea is caused by bacteria, viruses and other disease conditions.
Diarrhoeal diseases are considered a major cause of morbidity and mortality in children under five years of age.
There are about 11.67 million cases of diarrhoeal diseases in India, which are caused by poor environmental conditions.
In 2013, more than 100,000 children under the age of 11 months died of diarrhoea.
After pneumonia, diarrhoea is the second leading killer of young children worldwide.
India has the highest incidence of diarrhoeal diseases. Diarrhoea is a preventable and treatable disease.
It is also the leading cause of malnutrition in children under five years of age.
More than 2.3 million children die every year, of which 334,000 children die due to diarrhoeal diseases.
(e) Acute Respiratory Diseases:
Acute respiratory diseases are a major cause of morbidity and mortality in children under five years of age in India.
During 2014, 34.81 million episodes of acute respiratory disease were reported with 2,932 deaths.
(f) Filariasis:
Filariasis is endemic in about 255 districts of 16 states and five union territories in India. About 630 million population is at risk. To achieve elimination of LF (Lymphatic Filariasis), GOI (Government of India) has initiated nationwide annual Mass Drug Administration (MDA) with annual single recommended dose of diethylcarbamazine citrate tablets, besides increasing home-based foot care and hydrocele operations.
The National Filariasis Control Programme was launched in 1955.
( G )HIV/AIDS:
HIV( Human Immunodeficiency Virus)/AIDS( Acquired Immunodeficiency Syndrome.
AIDS( Acquired Immunodeficiency Syndrome) is caused by exposure to infected blood semen(vaginal fluid).
The Indian Ministry of Health and Family Welfare estimated that the prevalence of HIV among adults (15-49 years) in 2011 was 0.27%, while the number of people living with HIV was 420,88,642, the number of new HIV infections in adults was 1,16,456 and the annual number is .
( h)STD/ STI:
More than 1 million people get sexually transmitted infections every day. Every year, about 550 million people get STIs- chlamydia, gonorrhea, syphilis and Get sick from trichomoniasis.
More than 530 million people have genital herpes. More than 290 million women have human papillomavirus infection. Most STI infections present without symptoms. These sexually transmitted infections can be transmitted from mother to child through the placenta or during delivery of the baby.
2) Noncommunicable Diseases:
Noncommunicable diseases are diseases that are not spread by infection or other people, but are usually caused by unhealthy behavior. They are the leading cause of death worldwide and pose a major threat to health and development, especially in low- and middle-income countries.
Noncommunicable diseases include
Cardiovascular disease,
Hypertension,
Cancer,
Diabetes Diseases like diabetes mellitus,
mental disorders,
tobacco consumption,
alcoholism,
accidents,
chronic lung disease,
cataracts,
and
stroke are involved.
( a ) Cardiovascular Disease:
Ischemic heart disease is a major cause of death which is generally increasing rapidly in economically developed countries and developing countries and is estimated to be the single most important cause of death in India by the year 2015.
According to WHO, an estimated 17 million people died from heart-related diseases in 2005, which was compared to 30% of global deaths. And about 80% of these deaths occurred in low and middle-income countries like India. According to the World Health Federation, 35% of cardiovascular diseases in India are 35-64 years old. It happens in the middle of the year.
( b ) Cancer:
Cancer has become an important health problem in India.
Every year, about 7-9 lakh cases are estimated to occur. It is estimated that there are 25 lakh cases of cancer in the country. Out of this, half of the total cancer cases are related to tobacco consumption in males and 20% of tobacco related cases are in females.
Every year, about 1 million tobacco related deaths occur.
Approximately 50% of deaths in developing countries are due to cancer. Breast cancer-20.01, cervical cancer-14.42 and ovarian cancer-5.6 were recorded in women.
Currently, India has the highest number of oral cancer cases in the world due to tobacco chewing in its rural areas.
(c) Diabetes Mellitus:
India is often referred to as the “diabetes capital of the world” due to the high prevalence of diabetes, especially type 2 diabetes. The rate of diabetes is increasing due to genetic predisposition, urbanization and dietary changes.
In 2011, it was estimated that 62.4 million people were affected by diabetes mellitus, an increase of about 2 million in just 1 year.
In India, 77.2 million people are estimated to have pre-diabetes.
About 4.4 million Indians in their most productive years, between the ages of 20 and 79, are unaware that they have diabetes. Diabetes killed about 1 million people in India in 2011.
India’s rural population is more affected by diabetes (34 million), while the urban population (28 million) is affected by diabetes mellitus. India ranks second after China.
( d ) Mental Disorders:
Mental disorders contribute to 13% of the global disease burden. According to the National Institute of Mental Health (NIMH), the prevalence rate of schizophrenia in India is 1.1% of the total population, while the overall lifetime prevalence of mental disorders in the total population is 10-12%.
( e ) Tobacco Consumption:
According to the National Family Health Survey-3, the prevalence of smoking among males and females in the age group of 15-49 years was 32.7% and 1.4% respectively.
Among the youth, 40% of males and 5% of females use tobacco.
19% of males smoke cigarettes or bidis and 30% use paan rasala, gutkha or other tobacco.
Tobacco use in any form is a major cause of cancer, especially oral cancer in people who chew tobacco.
( f ) Alcoholism:
The pattern of alcohol intake in India varies with geographical area. Punjab, Andhra Pradesh, Goa and the North-Eastern states have the highest incidence where alcohol intake is higher among males than the rest of the country. Female alcohol intake is higher in Arunachal Pradesh, Assam and Sikkim. The estimated alcohol consumers in 2005 were 62.5 million and out of these, 10.6 million are alcohol addicts in India.
( G ) Accidents:
According to WHO, road accidents in India have increased from 1.32 lakh (in 2010) to 1.43 lakh (in 2011).
During 1990-2000, the number of deaths due to accidents was 47%, of which 93% were due to unnatural causes and 7% due to natural causes.
The mortality rate due to accidents in the age group below 14 years was 8.2%; 15-44 years was 62%, 45-59 years was 20% and the age group above 60 years was 9.2%.
( h) Chronic Lung Disease:
Chronic lung diseases include conditions like chronic obstructive pulmonary disease (COPD) and asthma, which are aggravated by air pollution and tobacco use.
(I) Cataract:
In India, more than 12 million people are blind. Refractive error accounts for 19.70% of cases. Cataract surgery with intraocular lens (IOL) implantation has increased significantly from less than 5% in 1994 to 95% in 2011-12.
(j) Strokes:
In India, the increase in coronary heart disease and stroke is mainly observed in urban communities than in rural communities. Cardiovascular diseases are the main cause of death in 17.5 million people, mainly heart disease and stroke.
After heart disease, stroke is the second leading cause of death with 5.8 million fatal cases every year, of which 40% are in people under 70 years of age. About 12% of strokes occur in the population under 40 years of age. The number of stroke cases in India has increased by 17.5% in the last few decades.
3) Nutritional Problems:
The major nutritional problems seen in India include,
PEM (Protein Energy Malnutrition),
Nutritional Anemia,
Low Birth Weight Babies,
Xerophthalmia (Nutritional Blindness),
Iodine Deficiency Disorder,
Latherism,
Fluorosis.
a)PEM (Protein Energy Malnutrition):
Protein Energy Malnutrition is a problem seen due to deficiency of protein and calories and it is seen due to low consumption of food.
Protein Energy Malnutrition is generally of two types.
1) Kwasiorkor which is seen due to deficiency of protein.
2) Marasmus is seen due to calorie deficiency.
Thus, due to protein and calorie deficiency, the weight of the child is seen less than its age.
Protein energy mal nutrition is caused by insufficient food or food gap.
This problem is seen in every state of India.
But nutritional marasmus is seen more than kwashiorkor.
(b) Nutritional anemia:
Nutritional anemia is usually seen due to inadequate nutritious diet.
Usually due to vitamin B12 deficiency, 60 to 80% of women have anemia condition.
Adult girls are seen more.
( c) Low birth weight babies:
Low birth weight babies are generally seen in developing countries where the baby weighs less than 2.5 kg at birth and its main cause is maternal malnutrition or anemia.
(d) Xerophthalmia:
Xerophthalmia means dry eye. This is a medical condition in which there is no production of tears in the eye. This condition is usually seen due to deficiency of Vitamin A (Av) and mainly this condition is seen in children below 1 to 3 years of age.
(e) Iodine Deficiency Disorders:
Iodine deficiency causes goiter in which there is enlargement of the thyroid gland which is located in the neck. 71 million people in India are affected by goiter.
( f ) Lathyrus:
Lathyrus is caused by a particular type of lentil. This type of problem is especially seen with the saffron lentil (Lathyrus sativus). In which weakness, muscular spasm, weakness and paraplegia are seen. In India, this problem is especially seen in states like Madhya Pradesh, Jharkhand and Bihar.
( h ) Fluorosis:
Fluorosis is caused due to excessive fluoride content in drinking water. Fluorosis is also a major health problem in India. It is seen in Tamil Nadu, Andhra Pradesh, Punjab, Bihar, Rajasthan, Kerala and Jharkhand.
4) Environmental Problem:
Environmental problem is mainly seen due to two reasons.
( I ) Lack of safe drinking water,
( II ) Improper sanitation method for excreta disposal
These two reasons mainly cause soil pollution and water pollution.
Currently, safe water is available in 95% of urban areas and 79% in rural areas.
And facilities for excreta disposal are available in 61% of urban areas and only 15% in rural areas, which leads to soil pollution.
Apart from this, environmental pollution is also seen in urban areas due to improper disposal of waste products from vehicles and factories, which affects the health of the people.
Care Problem:
Medical care is seen to be developed in urban areas than in village areas.
In urban areas, due to overcrowding in hospitals, inadequate staff and drugs and medicines not being available in adequate amounts, it also affects the health of the people.
While in rural areas, 80% of the population believes in the indigenous system of medicine, along with inadequate health resources, it affects the health of the people.
The lack of proper distribution of health care services in urban and rural areas also affects the health of the people.
Due to lack of sufficient manpower, material, money, and inadequate health services in villages, health problems are created due to which morbidity and mortality are seen.
6) Population Problem:
Thus, the following health problems are seen in the nation
Population problem is one of the biggest health problems of India which affects many aspects of development including, employment, education, housing, health care sanitation and environment.
India comes second in population after China.
People migrate from rural to urban areas to get more facilities due to which population density increases in urban areas.
b) Write functions of UNICEF. યુનિસેફ ના કાર્યો લખો.
1.child health
UNICEF provides support for vaccine production in many countries
UNICEF helps in environmental sanitation programs to improve the quality of life of people living in villages to ensure that they have access to safe drinking water and safe water for household use.
Currently, the focus is on ensuring that mothers and children have access to primary health care. This includes immunization in the fund and young children’s health care, family planning, safe water and sanitation.
Child nutrition
UNICEF gives high priority to improving nutrition. The old SAF first helped in nutrition by supplementing child diets with the development of low-cost protein-rich food mixtures in the 1950s.
In collaboration with FAO, UNICEF began supporting the Apply Nutritional Programme through channels such as community development, agricultural extension, schools and health services, to encourage and support rural areas to grow and consume the foods needed for better child nutrition.
UNICEF also provides equipment for modern dairy farming in various parts of India
Family and Child Welfare
UNICEF’s main objective is to improve the care of children inside and outside the home through Parent Education Day Care Centres, Child Welfare and Youth Agencies and Women’s Clubs
This programme is being implemented as part of the expansion of Health, Nutrition Education and Home Economics
Education UNICEF, in collaboration with UNESCO, funds the training of all persons including health and sanitation workers and teachers. It emphasizes the motto that universal immunization is the best prevention. UNICEF also provides technical supplies, equipment, paper for tax books, medicine for health clinics and pipes for clean water supply in villages.
It helps the government to plan, develop and expand community-based services in the areas of maternal and child health, nutrition, clean water and sanitation
It It helps mothers and children in natural disasters and epidemic diseases. It works to prevent TB, malaria, eye diseases and other diseases. UNICEF supports and helps implement various works for children and the Convention on the Rights of the Child. UNICEF covers programs that help children survive, protect and develop, such as immunization, nutritional habits, growth monitoring, home best management, drinking water, environment, fitting practices, sanitation and education of girls, etc.
OR
a) Write down the role of community health nurse in school health services. સ્કૂલ હેલ્થ સર્વિસીસમાં કમ્યુનીટી હેલ્થ નર્સની ભૂમિકા લખો.
Health nurses play an important role in the school health program. They are responsible for the health services and welfare of school students. Their main responsibilities are as follows:
Health screening and monitoring:
School nurses monitor the health of students, such as length, weight, vision and hearing system, and provide treatment as needed
Disease and prevention:
Nurses educate about health problems and conduct health education sessions, such as hygiene, current illnesses, and prevention of diseases
Emergency treatment:
Provide immediate treatment to students in case of injuries or urgent health problems.
Mental Health:
Nurses assess the mental health of students and help with related problems such as depression, anxiety, and other problems.
Guidance:
Guiding students on health-related questions and issues and providing information about the services available to them.. Community Health Program: Nurses work to develop health groups for their schools, such as school screening, nutrition, and best practices.
In this way, community health nurses provide a very important service for physical, mental, and social health in schools.
Community health nurses play a broader and more important role in school health programs. They provide health services to students, teachers, and families and promote health.
Health Education and Promotion for Students:
Nurses educate students on physical health, nutrition, hygiene, precautions, and daily lifestyle.
Provides guidance on how to prevent diseases and epidemics, such as hygiene, healthy eating, exercise, and psychological well-being.
Provides guidance on issues such as addiction.
Physical Observation and Medical Monitoring:
Nurses conduct regular health screenings in schools, such as scans for eye, ear and mouth problems
Monitor depression and mental health problems, and provide necessary social and vocational guidance.
Microplanning and Public Health:
Plans health programs in schools and plans for disease resistance
Trains teachers and parents to help in health care so that they can monitor the health of the child
4.Primary Health Care and Emergency Treatment
Nurses provide initial treatment in the event of any immediate medical emergency in schools, such as accidental injury, severe bleeding, primary diagnosis of cancer, etc.
Nurses are active in referring injured students to appropriate medical institutions.
Recording and Reporting
Nurses maintain health records, which contain primary health data, disease history and treatment records of students.
This data is important for facilitating health services.
Health Promotion and Health-Related Projects:
Nurses inspire schools to run health-related programs, such as “Activities for Healthy Living”, “Sanitation and Safety Campaign”, “Campaigns for Nutrition”, etc.
They make students health conscious and instill concerns and arrangements for them to live healthily in their environment
Thus, the work of a community health nurse in a school health program is very important for the physical, mental, and social well-being of the student.
b) Draw the health organization chart at state level – રાજય સ્તરે આરોગ્ય સંસ્થાનો ચાર્ટ દોરો.
In the state, the State Minister of Health is the head of the Health and Family Welfare Department and the Health Secretary and the Commission of Health and various directors work under him. He has his own political vision and accordingly the Health Secretary and a large number of administrative staff work accordingly.
State Health Director
This is a technical wing of the State level Health and Family Welfare Department in which the Director of Health and Family Welfare is its head. Under him, the work of Public Health and Health and Family Welfare Services as well as Family Planning Services etc. comes. There is also a Deputy Director to help him and in a state like Gujarat, there is also a Regional Deputy Director. The main work of the old one is for Family Planning Services and Health Education.
At State Level
⬇️
State Ministry of Health State Health Director
State Ministry of Health
⬇️ Headed by
Minister of Health and Family Welfare
⬇️
Deputy Minister of Health and Family Welfare
⬇️
Health Secretary
⬇️
Deputy Secretary
⬇️
Large Administrative Staff
➡️ State Health Director
⬇️
Headed by
⬇️
Director of Health and Family Welfare
⬇️
Deputy Director
⬇️
Assistant Director of Health
⬇️
Regional Activities Public Health *FunctionalActivity
MCh
Nutrition
TB
Family Planning
Leprosy
Health Education
Q-3 Write short answer (any two)
a) Classify occupational hazards. ઓકયુપેશનલ હેઝાર્ડસનું વર્ગીકરણ કરો.
Hazards:
Occupational hazards involve a wide range of risks that workers may experience depending on their specific job role and environment.
Occupational hazards are potential risks or dangers that health care workers are exposed to in their
workplace environment.
These hazards arise from various aspects of the workplace, such as physical conditions, chemical materials, biological agents, psychological factors, and mechanical hazards, etc. These factors pose a risk to the health, safety, and well-being of workers and can lead to injuries, illnesses, or even death if proper precautions and safety measures are not taken.
Occupational hazards that workers may be exposed to include:
1) Physical hazards,
2) Chemical hazards,
3) Biological hazards,
4) Mechanical hazards,
5) Psychological hazards.
1) Physical hazards:
Physical hazards are caused by exposure to heat and cold. Workers are exposed to direct exposure to high temperatures of the sun such as farmers, builders, laborers etc.
There are also high temperatures inside the valley such as the Kotar Gold Valley in Mysore, some industries will have local ‘hot spots’ such as ovens and furnaces that radiate heat such as bakeries, metal works, asbestos factory engine rooms etc.
The effects of high temperatures include extreme heat, heat allergies, heat exhaustion, and muscle cramps.
Many workers are exposed to low temperatures such as in ice factories, high altitudes, cold storage, cold laboratories, etc. These workers may develop chills (pain, itching, and swelling in the hands and feet due to poor blood supply due to excessive exposure to cold), erythrocyanosis, and respiratory difficulties.
High Humidity: High humidity, along with exposure to extreme temperatures in industries such as textile, paper, and ice factories, increases the effects of heat and cold.
Noise: Loud noise is produced in steel, oil, textile, and automobile factories. Loud noise is harmful to health. Its effects depend on the intensity and duration of exposure to loud noise. Loud noise can cause fatigue, nervousness, irritation and partial or complete hearing loss.
Light: Workers may come into contact with poor or glaring and bright light. Poor light causes strain and pain in the eyes, eye strain, headaches. Blurring and bright light causes discomfort, blurring of vision, irritation and visual fatigue.
Vibration: Vibration occurs while working on machines like grinding, cutting, drilling boring machines etc. Vibration can cause fatigue, nervousness and local effects such as hand and joint injuries etc.
Radiations:
Exposing yourself to radiation from X-rays and radioactive isotopes can cause skin and blood cancer, which can result in genetic changes, malformations, sterility etc. People working in radiology departments, watch factories, ammunition factories come into contact with ionizing radiation. Ultraviolet (UV) radiations such as during welding cause conjunctivitis and keratitis. Ultraviolet radiation can cause sunburn. Roadbuilders, sailors, shepherds and farmers can be affected by ultraviolet radiation.
2) Chemical Hazards: Factories use some or the other chemicals. Chemicals work in 3 ways.
1) Local action Some chemicals can cause conditions like dermatitis and eczema (itching).
2) Inhalation Inhalation of gases and vapors can cause respiratory diseases.
3) Ingestion Mercury, lead, arsenic, zinc, chromium and cadmium, phosphorus etc. cause various diseases.
Types of which are hazardous Gases like carbon monoxide, ozone, carbon dioxide, hydrogen and cyanide etc.
Fumes and vapors from various types of acids, vapors of mercurial etc.
•Mist (Mist)
Mist from the electroplating industry.
•Dust: Small particles formed by crushing and grinding rocks, ores, metals, wood, etc.
Chemical agents that are harmful to the skin, respiratory system and gastrointestinal interstitial system.
Skin problems include dermatitis, eczema, urticaria, ulcers and cancer etc.
•Respiratory problems include various types of pneumoconiosis. Silicosis due to quartz dust,
Anthracosis due to coal dust,
Byssinosis due to cotton dust,
Asbestosis due to asbestos dust,
•Respiratory distress due to carbon monoxide, hydrogen sulfide and hydrogen
•Various pungent gases like cyanide chlorine, ozone, nitrogen oxide, sulfur dioxide can cause throat irritation. Lung cancer can be caused by asbestos, beryllium, coal tar, mineral oil.
Biological hazards are caused by infectious and parasitic agents such as viruses, rickettsia, bacteria. This can also lead to hookworm infestation in farmers. Leptospirosis can occur in workers working in mines.
Tanning factories, veterinary hospitals and dispensaries, zoos, circuses, agricultural workers, butcher shops, etc. can cause various zoonotic diseases such as brucellosis, mycotic infections, parasitic infections and anthrax.
Health workers working in hospitals/dispensaries may come into contact with patients infected with diseases such as tuberculosis, hepatitis, HIV and serum hepatitis etc.
4) Mechanical Hazards: Unprotected machines and their protruding and moving parts and machines with low safety can cause various accidents and injuries, which can lead to partial and permanent disability.
5) Psychological Hazards:
Thus, to prevent such hazards from occurring in workers, it is important to identify them early and properly and take measures to prevent them.
Due to various types of maladjustment problems such as lack of proper job satisfaction, insecurity, frustration and environmental tension, a person cannot adjust properly. This condition can cause physical health problems such as increased blood pressure, indigestion, insomnia, loss of appetite, and conditions like heartburn.
b) Write down role of nurse in prevention and control of malaria. મેલેરિયાના નિવારણ અને નિયંત્રણમાં નર્સની ભૂમિકા વિશે લખો.
B) Role of CHN in prevention and control of malaria
The role of CHN for prevention of malaria is as follows,
To collect blood smear of ANC, PNC and infant of their area and send them for testing.
To provide preservative treatment to the family of their area.
To give radical treatment to positive test.
To refer necessary cases to PHC or CHC.
To provide health education, especially,
To provide information about the agent
host
environment
.
To explain about host protection.
To explain about household measures to reduce mosquito infestation. To explain to people to prevent mosquitoes from entering the house.
To explain to people about the use of mosquito net.
To explain to people about spraying.
Promotion of health
To do serious and complicated disease management
To try to reduce mortality rate. Thus, nurse has an important role in the prevention and control of malaria.
A) Spraying
In areas with two or more cases, DDT is sprayed until vector control is achieved.
If the 1st spraying round is not effective, 3 rounds of spraying are recommended and if it is still not effective, synthetic pyrethroid wiring is sprayed for a duration of 6 weeks, through which the effect of malaria is largely stopped.
B) Surveillance
Active and passive surveillance is continued in certain types of specific areas
Survey is done once every 75 years.
Modified plan operation. Key aliment is blood smear and exam is done through survey.
C) Entomological assessment
Entomological key is its direct assessment.
Testing of suspected cases in the area is done and proper medicine for insecticide in that area is determined.
D) Treatment
In this, preservative and radical treatment are especially given.
Radical treatment is given to effective cases.
e)Follow up
After completion of medical treatment, blood smear is taken again.
In positive case, monthly blood smear is taken regularly within one year.
F) Health education
To create awareness among people about malaria control activities and to get people’s co-operation, health education is given through different methods.
G) Reporting system
Every two weeks, a report of malaria related activities has to be submitted to CHC.
Such information is provided by the M.O. of the area.
The report sent by CHC is sent to the district health quarter.
All the above activities are done through modified plan operation.
c) Describe temporary methods of family planning. ફેમીલી પ્લાનિંગ ની ટેમ્પરેરી પધ્ધતિઓનું વર્ણન કરો.
1.Barrier method
a.Physical method
Male condom:- It is a sheath made of thin latex and plastic which is placed on the penis before sexual intercourse. After ejaculation, it is carefully withdrawn and disposed of in a way that does not cause semen leakage. The condom acts as a barrier that prevents semen from coming into contact with the vagina.
Female condom:- It is made of polyurethane. It has two rings, the external ring covers the cervix and the internal ring covers the vagina. It is prelubricated with silicone.
Diaphragm:- It is a synthetic rubber and plastic material, which has a diameter of 5 to 10 cm. It is used by females. It contains a permicidal jelly and is worn by females before intercourse.
Vaginal sponge:- It is a small device made of polyurethane. It is less effective than diaphragm and has a higher failure rate.
b. Chemical method
Chemical contraception is placed in the vagina. It contains chemicals that destroy sperm.
There are a total of four categories of chemical devices;
-Tablet foam, foam aerosol
-Cream, jelly, paste
-suppositories
-soluble films
c.Combined method
In which chemical contraception is also used along with condom, it is called combined device. Which gives double protection against pregnancy.
2.IUCD – IUCD
Introduction
Intrauterine device is a small and flexible T-shaped device that is inserted into the uterine cavity to prevent pregnancy.
Intrauterine devices (IUCDs) are a popular method of long-term contraceptive which is involved in family welfare programs due to their effectiveness.
Grafenberg Ring was used in Germany in 1929 by Grafenberg, after which many different types of devices were invented which are mainly divided into two parts.
In which,
1) Copper IUCD
Description: Made of plastic and copper. Copper acts as a spermicide, and prevents fertilization.
Duration is effective for 5–10 years depending on the specific type.
Examples: Copper T 380A, Multiload 375.2) Dominal IUCD (LNG-IUD)
Description: Made of plastic and releases levonorgestrel, which thickens cervical mucus, prevents sperm and thins the uterine lining.
Duration is effective for 3–5 years.
Examples: Mirena, Skyla, Liletta, Kyleena.
Intrauterine contraceptive devices involve the following contraceptive devices.
1)lippes loop
2) CUT 200 в
3)CuT 380 A,
4) Multiload Cu 250,
5) Multiload 375,
6)progesttasert,
7) Levonorgestrel IUCD.
1)lippes loop:
Lippes loop is a first generation intrauterine device. Lipes loop is formed from polyethylene.
And it is of double S (S) shape and a nylon thread is attached to it which remains in the vagina, which helps in removing the loop from the intrauterine cavity. It is available in four sizes namely, A, B, C and D.
Lipis loop is nontoxic, reliable and stable. It can also perforate the uterine wall. It contains a small amount of barium5 which makes it visible on X-ray but is not used at present.
2) CU T 200 В:
CU T 200 B is a widely used medicated device. In which a copper wire with a surface area of 215 sq mm is wrapped around the vertical stem of the device.
The stem of the T-shaped device is made of a polyethylene frame. It has a polyethylene monofilament attached to the end of the vertical stem.
This device is removed after 4 years.
Cut 200 B has 200 sq mm surface wire containing 120 mg copper and is removed after 3 years 3)CuT 380 A:
CUT 380 A is a government supplied CUT 380 A. It has a T shape device with two solid copper slim transverse arms and copper wire on the vertical stem.
The total surface area of copper is 380 Sq mm of which 314 mm is on the wire and 33 sq mm on each copper sleeve. It has a monofilament white thread.
It remains effective for about 10 years.
4) Multiload Cu 250:
The device is available in a sterile packet with an applicator. It does not have an introducer or plunger available.
The device releases 60–100 μg of copper per day over a period of one year. The device has to be replaced after 3 years.
5) Multiload 375: It has a surface area of 375 mm² of copper wire around its vertical stem. Replacement is every 5 years
6) progesttasert: A bioactive core containing microcrystals of progesterone (38 Mg) is enclosed within a plastic wall that releases approximately 65 μg of progesterone per day into the uterine cavity. The release from the depot continues for only one year. Thus, it has to be replaced after one year.
7) Levonorgestrel IUCD: This is a T-shaped device.
A polydimethylsiloxane membrane around the stem acts as a reservoir of the steroid. The total dose of levonorgestrel is 52mg, which is released at a rate of 20 μg/day. This device is replaced every 5 years.
Mechanism of Action
1) Hormonal IUD releases copper ions, creating an environment impermeable to sperm. Prevents fertilization of eggs by sperm. If fertilization occurs, implantation may be prevented.
2) Hormonal IUD
Releases levonorgestrel to thicken cervical mucus, preventing sperm from entering the uterus. Suppresses endometrial growth, making the lining of the uterine cavity unsuitable for implantation. Partially suppresses ovulation in some females.
Benefits
Effective: More than 99% effective in preventing pregnancy.
Long Lasting: Works as a contraceptive for many years.
Reversible: Fertility returns quickly after removal. Convenience: Requires little maintenance after insertion.
Cost-effective: Economical.
Insertion and Removal
Insertion: Is performed by trained health care personnel.
Usually can be removed during the menstrual period or at any time during pregnancy.
The procedure involves inserting the IUD into the uterine cavity through the cervix.
Removal can be performed at any time by a healthcare provider.
Fertility usually returns immediately after removal.
Common Side Effects: Cramping pain during and after insertion.
Irregular erections and ejaculation, especially during the first month.
Heavy menstrual bleeding.
With hormonal IUD, periods may be reduced or missed.
3.Hormonal method
A.Oral pills
Combined pills
-Mala N, i.e. Norethisterone acetate + ethinyl estradiol
-Mala D, i.e. D norgestrol + ethinyl estradiol
Mini pills
They contain only progestin.i.e.norethisterone + levonorgestrol
Combined pills
They are started from the fifth day of the menstrual cycle and are continued for 21 days. They are taken regularly.
Q4 Write short notes. ટૂંકનોંધ લખો. (કોઈપણ ત્રણ)
a) ASHA – આશા
ASHA (Accredited Social Health Activist)
ASHA stands for Accredited Social Health Activist
It is one of the major initiatives under the National Rural Health Mission (NRHM) of India, which is now a sub-programme under the National Health Mission (NHM), which aims to improve community health outcomes, especially in rural and underserved areas.
One ASHA is for 1000 population.
Here is some detailed information about ASHA:
Selection of ASHA:
ASHA is selected from the same community.
ASHA can be married/divorced/and widowed.
She should be between the ages of 25 to 45 years.
Her minimum education should be up to 8th standard.
She should have good knowledge of communication and leadership.
ASHA is a volunteer worker. She is not paid any salary
She is given Traveling Allowance (TA), Dearness Allowance (DA), Rewards and Non-monetary Incentives.
Role and Responsibility of ASHA:
1) Health Education and Promotion:
ASHA provides education to the people of the community on various health related issues like,
Maternal and Child Health,
Family Planning,
Nutrition,
Sanitation,
And provides education on preventive health care practices.
ASHA organizes awareness sessions, demonstrations and health camps to promote health-seeking behavior and disease prevention.
2) Identification and Referral:
ASHA identifies individuals in need of health care services such as pregnant women,
new born and children under five years of age.
ASHA provides antenatal care, immunization, and treatment for common illnesses and referral services during emergencies.
3) Support for Maternal and Child Health:
ASHA encourages institutional delivery and encourages pregnant women to avail maternal health services under government schemes such as Janani Suraksha Yojana (JSY).
They provide support and guidance to mothers on breastfeeding, child nutrition, and immunization schedules.
4) Facilitation of Access to Health Services:
ASHA helps community members access government-provided health care services, which involve immunization programs, health checkups, and distribution of essential medications.
5) Data Collection and Reporting:
ASHA maintains records of community health-related information, which involves birth rates, deaths, immunizations, and pregnancy rates.
This collected data provides reports to health officials to monitor health indicators and plan health interventions effectively.
6) Community Mobilization and Empowerment:
ASHAs mobilize community participation in health initiatives,
Encourage people in the community to participate in health programs and take ownership of their health.
They provide information and services to empower women to make informed decisions about their health and family planning.
7) Incentives and Support:
ASHAs receive performance-based incentives for delivering health services and achieving targets related to maternal and child health outcomes.
They receive training and continuous support from the government to enhance their skills and knowledge in the health care delivery system.
8) Other Responsibilities:
Impact and Significance: ASHA plays a crucial role in improving maternal and child health outcomes, increasing institutional deliveries, and bringing health awareness in rural and marginalized communities. It contributes to reducing maternal and child mortality rates by providing timely health care services and promoting healthy behaviors. ASHA works as a bridge between the community and health care services by encouraging the people of the community to avail health care services as per the needs of the community.
ASHA helps create awareness in the community by providing instruction on health, nutrition, personal hygiene and sanitation.
It provides counselling to women on safe pregnancy, delivery, best fitting, and complementary feeding, immunization and measures to control infection (especially reproductive tract infections).
ASHA workers provide counselling to women to adopt small family names.
It is a depot holder for essential medicines like ORS, iron and folic acid tablets, chloroquine tablets, oral pills, condoms and disposable delivery kits.
It mobilizes the community to get health services at sub-centres and primary health centres.
It advises pregnant women to seek health care services if they need treatment.
It provides primary medical care for minor ailments like fever, diarrhoea and first aid treatment for minor injuries.
ASHA also provides DOTS (Directly Observed Treatment Short Course) treatment under the National Tuberculosis Control Programme.
It informs sub-centres and primary health centres about births and deaths in the village and about any disease outbreaks.
Training: They undergo comprehensive training to equip them with knowledge and skills related to maternal and child health, family planning, nutrition, hygiene and other aspects of primary health care. The training also includes communication skills, record keeping and understanding of government health programs and policies.
b) Sources of vital statistics – સોર્સીસ ઓફ વાયટલ સ્ટેટેસ્ટીકસ
Sources of Vital Statistics:
1.Civil Registration System (CRS):
Civil Registration System is a continuous, permanent and compulsory recording of the occurrence and characteristics of vital events (birth, death, marriage etc.).
Authority: Administered by the Registrar General of India under the Ministry of Health.
Importance:
Provides primary data for birth and death rates, which are crucial for planning and policy making.
2) Sample Registration System (SRS):
Conducts large-scale demographic surveys for reliable annual estimation of birth rate, death rate and other fertility and mortality indicators.
Authority: Conducted by the Office of the Registrar General of India and the Census Commissioner.
Significance: Supplements the CRS (Sample Registration Systems) data and provides more accurate and timely estimates.
- Census of India:
Conducted every ten years, the Census of India collects comprehensive data on the population. It collects information on age, caste and marital status.
Authority: Conducted by the Office of the Registrar General of India and the Census Commissioner.
Significance: Provides detailed demographic information that supports various statistical analyses and socio-economic planning.
- National Family Health Survey (NFHS):
A large-scale, multi-round survey of households across India.
Authority: Conducted by the Ministry of Health and Family Welfare in coordination with the International Institute for Population Sciences (IIPS).
Significance: Provides data on population, health and nutrition, as well as fertility rates, maternal and child health.
- Health Management Information System (HMIS):
An online portal that collects data from health facilities across India.
Authority: Managed by the Ministry of Health and Family Welfare.
Significance: Provides data on health indicators, service delivery and performance of health programmes.
6) Annual Health Survey (AHS):
Provides district-level estimates of key indicators, such as fertility and mortality rates.
Authority: Conducted by the Office of the Registrar General and Census Commissioner of India.
Importance: Helps in evaluating the impact of health programmes and policies at a more localized level.
7) Demography and Health Survey (DHS):
Conducted periodically to collect data on population, health and nutrition.
Authority: Coordinated by various institutions and often in partnership with international agencies.
Importance: Provides internationally comparable data for monitoring and evaluation.
8) Medical Certification of Cause of Death (MCCD)
A system of recording the cause of death by medical practitioners using a standardized format.
Authority: Managed by the Office of the Registrar General of India.
Importance: Provides accurate data on mortality patterns and causes of death, which is essential for public health planning.
9) Health Survey and Research
Various surveys and research studies are conducted by government agencies, academic institutions and international organizations.
Examples:
National Sample Survey (NSS), India Human Development Survey etc.
Importance:
These surveys provide additional data on various health and demographic parameters, which helps in comprehensive analysis and policy formulation.
Vital statistics in India are collected from multiple sources, playing a crucial role in providing accurate and comprehensive data on the health and demographic characteristics of each population.
These statistics
c) Elements of Primary Health Care – પ્રાથમિક આરોગ્ય સંભાળના ઘટકો
Elements of Primary Health Care:
Primary Health Care
Primary health care is an essential health care that is universally designed to be accessible to everyone and acceptable to everyone through full participation in it and primary health care should be affordable to the community and the country.
There are 8 essential elements of primary health care which are as follows:
ELEMENTS:
1) E: Ensure safe water supply,
2) L: Locally endemic disease control
3) E: Education
4) M: Maternal and child health (immunization against infectious diseases)
5) E: Environmental sanitation
6) N: Nutrition
7) T: Treatment of minor ailments
8) S: School health services.
•>1) E: Ensure safe water supply:
Adequate supply of safe drinking water and sanitation are essential for good health and are an important factor of the environment.
Access to safe drinking water is essential for preventing waterborne diseases and promoting overall health.
Primary health care involves efforts to ensure that communities have access to clean and safe water sources, which are fundamental for disease prevention and health promotion.
2) L: Locally Endemic Disease Control:
The main focus of primary health care is to control any endemic disease in a particular region or community.
It involves surveillance, preventive measures (such as vaccination and vector control), and early detection and treatment of locally prevalent diseases.
Prevention and control of local and endemic diseases to reduce morbidity rates.
3) E: Education:
Health education is a key component of primary health care.
Its aim is to empower individuals and communities with the knowledge and skills to make informed decisions about their health.
Education covers a wide range of topics including hygiene practices, nutrition, family planning, sexual health, and prevention of disease.
To provide education to the people about health and current health problems. It formulates certain measures to control and prevent these health problems and makes people aware of the health services available to them so that they can use them when needed.
4) M: Maternal and Child Health (Immunization Against Infectious Diseases):
Mothers and children are the most vulnerable groups to health problems and account for a large percentage of the population. Primary health care places significant emphasis on maternal and child health services.
This involves prenatal care,
safe child birth,
proper postnatal care,
newborn care, immunization,
growth monitoring and nutrition to ensure healthy development during critical stages of life.
Protecting mothers and children from illness and other risks ensures good health of families and communities.
Immunization against infectious diseases:
Provide proper immunization to the child to protect them from major infectious diseases. Such as,
Poliomyelitis,
Diphtheria,
Tetanus,
Measles,
Tuberculosis,
Hepatitis B.
etc. Provide proper immunization to the child to prevent infectious conditions.
5) E: Environmental Sanitation:
Environmental sanitation is essential to prevent diseases caused by poor hygiene and environmental conditions.
Primary health care should improve sanitation, properly dispose of waste materials, and provide education on hygienic practices to reduce the risk of communicable diseases in the community.
6) N:Nutrition:
Good nutrition is essential for health and for the growth and development of children.
People should be encouraged to pay attention to a balanced diet.
Nutrition is the foundation of primary health care, which identifies both malnutrition and overnutrition as issues.
It involves promotion of balanced diet, micronutrients, supplementation, support breastfeeding, and nutritional counseling to improve health outcomes and prevent nutritional deficiencies.
It is necessary to provide knowledge on food preparation and preserving nutrients present in the diet.
7) T : Treatment of Minor Alignment:
Primary health care provides accessible and timely treatment for common health conditions and minor alignment. Primary health care is provided by trained health care personnel to manage illnesses (such as respiratory infections, diarrhea, skin conditions, and minor injuries). And there should be easy availability of drugs.
8) S: School Health Services:
School health services are integrated with primary health care to improve the health and well-being of school-age children.
These services include screening, immunization, health education sessions, counseling, and referral for further evaluation and treatment when needed.
Thus, a total of 8 elements are involved in primary health care.
d) Bhore Committee – ભોર કમિટિ
Introduction:
The Bhor Committee was appointed by the British Government of India in 1943 to survey the present health conditions and health organization in India and to make recommendations for its future development. Sir Joseph Bhor was its chairman. The committee had members who were pioneers of public health. They met regularly for two years and submitted their report in 1946.
The Bhor Committee was established in “1946”. Its founder was “Sir Joseph Bhor”, hence it is called the Bhor Committee.
The Bhor Committee is known as the “Health Survey and Development Committee”.
Recommendation: The committee forwarded a comprehensive proposal for the development of the National Programme of Health Services for the first time.
The important recommendations of the Bhor Committee were:
Integration of preventive and curative services at all administrative levels.
Development of Primary Health Centres in two stages:
1) Short Term Measures
2) Long Term Measures
1) Short Term Measures: Provide Primary Health Centre (PHC) covering a population of 40,000 in every rural area.
Primary Health Centre (PHC) will be manned by,
Doctors: 2,
Public Health Nurse: 4,
Nurse: 1,
Midwife: 4,
Trainee Midwife: 4,
Sanitary Inspector: 2,
Health Assistant: 2,
Pharmacist: 2,
Class IV Employees: 15.
A Secondary Health Centre has also been envisaged to provide support to the Primary Health Centre (PHC) and to coordinate and supervise its functions.
2) Long Term Measures:
A Rs 3 million plan is also being proposed to set up a PHC with 75-bed hospitals for every 10,000 and 20,000 population.
To prepare a 650-bed hospital as a secondary health unit and to set up a 2500-bed hospital at the district level.
Major changes should be made in medical education, including providing three months of training in preventive and social medicine to prepare social physicians.
To establish a Village Health Committee for better coordination and support in development programs.
A District Health Board will be established with representation from the public and district health officials.
Q-5 Define following (any six) નીચેની વ્યાખ્યા લખો. (કોઈપણ છ)
a) Health – આરોગ્ય
In 1948, the World Health Organization (WHO) defined health as follows: “Health is a state of complete physical, mental, social and spiritual well-being and not merely an absence of disease or infirmity.”
b) Rehabilitation – પુનવસન
Rehabilitation in community health nursing means bringing a person, family or community back to their level of good physical, mental, social and economic functioning after any accident or incapacity. This process is done by bringing the person back to his normal lifestyle with medical, psychological and social support.
c) Occupational Health – વ્યાવસાયિક સ્વાસ્થ્ય
Occupational health is a branch of public health concerned with the identification, evaluation and control of workplace-related health risks, including physical, chemical, biological, ergonomic and psychological factors. Its aim is to promote and maintain the highest degree of physical, mental and social well-being of all occupational workers by preventing occupational diseases, injuries and accidents.
The general aim of occupational health is to promote and maintain the highest degree of physical, mental and social well-being of workers in all occupations,
to protect workers from risks arising from factors adverse to health in their employment, and to place workers in an occupational environment which meets their physical and psychological needs.
d) Pandemic – પેન્ડેમીક
Pandemic means a disease that is spread all over the world in which a large number of people are infected with that disease and the disease spreads quickly among the people. It is called a mix. Ex. Covid 19 disease
e) Target couple – ટારગેટ કપલ
Target Couple Target couple means a couple who have 2 to 3 live children and need to be highly motivated about family planning. They are called target couples.
f) Family welfare -ફેમીલી વેલફેર
Family welfare means that programs are included to improve the physical, mental, social and economic facilities of the family members, keeping in mind their total facilities. These programs are intended to improve the living standard of the people, education and economic protection.
g) Community – કોમ્યુનિટી
A community is a group of people who share a common geographic area, social structure, culture, or interest and interact with each other. In the health sector, a community is the entire population, including patients, that collectively affects their health, living conditions, lifestyle, and access to health services. Community health is essential to improving the health status of this group, including components such as promotion, prevention, care, and rehabilitation.
h) Infertility વંધ્યત્વ
Infertility is a medical condition in which
the inability to conceive a pregnancy despite having regular and unprotected intercourse for 1 year or more is called infertility.
It affects about 10–15% of couples worldwide. Infertility can be due to various factors affecting the male, female, or both, and can be temporary or permanent.
Types of Infertility
There are generally two types of infertility.
1) Primary infertility,
2) Secondary infertility
1) Primary infertility: It refers to patients who have not been able to conceive a pregnancy even once.
2) Secondary infertility: This indicates that a previous pregnancy was conceived but subsequent pregnancy fails to conceive, which is called secondary infertility.
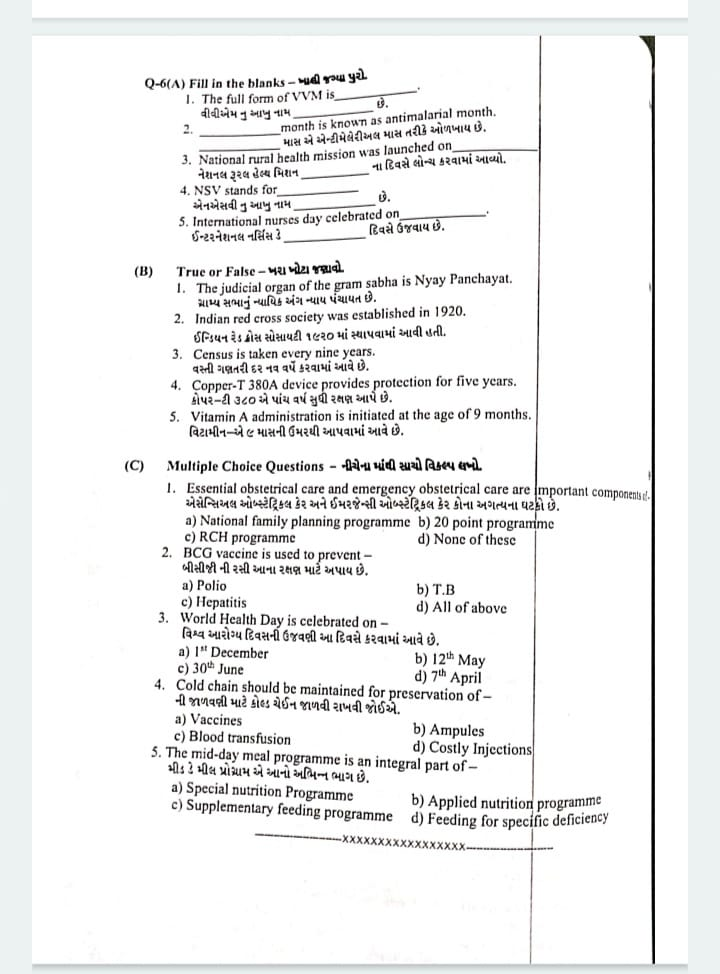
Q-6(A) Fill in the blanks- ખાલી જગ્યા પુરો.
1.The full form of VVM is…… Vaccine Vial Monitor
2…….,..month is known as antimalarial month. June
3.National rural health mission was launched on……… 12th April 2005
4.NSV stands for……. Non-Scalpel Vasectomy
5.International nurses day celebrated on………… 12th May
(B) True or False – ખશ ખોટા જણાવો. ❌✅
1.The judicial organ of the gram sabha is Nyay Panchayat.
ગ્રામ્ય સભાનું ન્યાયિક અંગ ન્યાય પંચાયત છે. ✅ કારણ: Nyay Panchayat is the judicial organ of the Gram Sabha, responsible for resolving minor disputes at the village level.-ગ્રામ્ય સભાનું ન્યાયિક અંગ ન્યાય પંચાયત છે, જે ગામના સ્તરે નાની-મોટી વિવાદો ઉકેલવા માટે જવાબદાર છે.
2.Indian red cross society was established in 1920. ઈન્ડિયન રેડ ક્રોસ સોસાયટી ૧૯૨૦ માં સ્થાપવામાં આવી હતી. ✅ કારણ: The Indian Red Cross Society was established in 1920 under the Indian Red Cross Society Act to provide humanitarian services.-ઈન્ડિયન રેડ ક્રોસ સોસાયટી 1920માં સ્થાપિત થઈ હતી અને તે માનવતાવાદી સેવાઓ પૂરી પાડે છે.
3.Census is taken every nine years. વસ્તી ગણતરી દર નવ વર્ષે કરવામાં આવે છે.❌ કારણ: The census in India is conducted every ten years to collect demographic and other statistical data.-ભારતમાં વસ્તી ગણતરી દર દસ વર્ષે કરવામાં આવે છે, જે લોકસાંખ્યિક અને અન્ય આંકડાકીય ડેટા એકત્રિત કરે છે.
4.380A device provides protection Copper-T for five years.
કોપર-ટી ૩૮૦ એ પાંચ વર્ષ સુધી રક્ષણ આપે છે.❌કારણ: The Copper-T 380A device provides protection for up to 10 years, making it a long-term contraceptive method.–કોપર-ટી 380A ઉપકરણ 10 વર્ષ સુધી રક્ષણ આપે છે, જે લાંબા ગાળાનું ગર્ભનિરોધક સાધન છે.
5.Vitamin A administration is initiated at the age of 9 months.
વિટામીન-એ ૯ માસની ઉંમરથી આપવામાં આવે છે.✅કારણ: The first dose of Vitamin A is given at 9 months along with the measles vaccine to prevent Vitamin A deficiency and associated complications.-વિટામિન Aની પહેલી ડોઝ 9 મહિનાની ઉંમરે મિસલ રસી સાથે આપવામાં આવે છે જે વિટામિન Aની ઊણપ અને સંબંધિત સમસ્યાઓને ટાળે છે.
(C) Multiple Choice Questions – નીચેના માંથી સચો વિકલ્પ લખો.
1.Essential obstetrical care and emergency obstetrical care are mportant components એસેન્સિઅલ ઓબ્સ્ટેટ્રિકલ કેર અને ઈમરજેન્સી ઓબ્સ્ટેટ્રિકલ કેર કોના અગત્યના ઘટકો છે.
a) National family planning programme
b) 20 point programme
c) RCH programme RCH પ્રોગ્રામ
કારણ: Essential and emergency obstetrical care are critical components of the Reproductive and Child Health (RCH) programme, aimed at improving maternal and child health outcomes.-પ્રજનન અને બાળ આરોગ્ય કાર્યક્રમ (RCH) માં માતાના અને બાળકોના આરોગ્યમાં સુધાર માટે અત્યાવશ્યક અને તાત્કાલિક ઓબ્સ્ટેટ્રિકલ કેર સામેલ છે.
d) None of these
2.BCG vaccine is used to prevent – બીસીજી ની રસી આના રક્ષણ માટે અપાય છે.
a) Polio
b) T.B –ટી.બી.
કારણ: The Bacillus Calmette-Guerin (BCG) vaccine is specifically used to protect against tuberculosis (T.B), particularly in children. બેસિલસ કેલમેટે-ગ્યુરિન (BCG) રસી ખાસ કરીને ટી.બી. સામે રક્ષણ માટે ઉપયોગમાં લેવામાં આવે છે, ખાસ કરીને બાળકોમાં.
c) Hepatitis
d) All of above
3.World Health Day is celebrated on – વિશ્વ આરોગ્ય દિવસની ઉજવણી આ દિવસે કરવામાં આવે છે.
a) 1″ December
b) 12th May
c) 30th June
d) 7th April –7 એપ્રિલ
કારણ: World Health Day is celebrated annually on 7th April to mark the founding of the World Health Organization (WHO) in 1948.-વિશ્વ આરોગ્ય સંગઠન (WHO)**ની 1948 માં સ્થાપના યાદ કરવા માટે 7 એપ્રિલે વિશ્વ આરોગ્ય દિવસની ઉજવણી કરવામાં આવે છે.
4.Cold chain should be maintained for preservation of- ની જાળવણી માટે કોલ્ડ ચેઈન જાળવી રાખવી જોઈએ.
a) Vaccines – રસી
કારણ: Cold chain systems are essential for maintaining the potency of vaccines by keeping them at the recommended temperatures from production to administration.- રસીના પોટન્સી જાળવવા માટે ઠંડકની જાળવણી સિસ્ટમ આવશ્યક છે, જેથી ઉત્પાદનથી લઈને વપરાશ સુધી યોગ્ય તાપમાને રાખી શકાય.
c) Blood transfusion
b) Ampules
d) Costly Injections
5.The mid-day meal programme is an integral part of- મીડ ડે મીલ પ્રોગ્રામ એ આનો અભિન્ન ભાગ છે.
a) Special nutrition Programme
b) Applied nutrition programme –એપ્લાઈડ ન્યુટ્રિશન પ્રોગ્રામ
કારણ: The mid-day meal programme, aimed at improving the nutritional status of school children, is part of the Applied Nutrition Programme.-મિડ-ડે મીલ પ્રોગ્રામ, જે શાળા બાળકોના પોષણ સ્થિતિમાં સુધાર માટે છે, તે એપ્લાઈડ ન્યુટ્રિશન પ્રોગ્રામનો ભાગ છે.
c) Supplementary feeding programme
d) Feeding for specific deficiency
