ENGLISH Bacterial infection of skin disease(juhi) PART 5 INTE
Bacterial infection of skin
Bacterial skin infection is known as pyoderma.
Pyoderma means ‘pus in the skin’.
Cutaneous infections caused by pus forming bacteria are known as pyoderma. This feature is not always visible to the naked eye.
This infection can be primary or secondary.
Primary skin infection occurs due to a break in skin integrity and direct contact with an organism.
While secondary skin infection is seen due to primary skin infection or due to trauma, injury or surgery on the screen.
Bacterial skin infections are mainly caused by gram positive staphylococcus aureus and beta hemolytic streptococci bacteria.
Write a Factors associated with bacterial skin disease
Moisture, Perspiration, Friction
Obesity
Poor hygiene and poor nutrition
Systemic diseases such as diabetes
Immunosuppression
Pathophysiology of bacterial skin infection
Bacteria enter the body through a cut in the skin, hair follicle or other opening.
|
When bacteria get a favorable environment, they multiply and increase in number
|
Due to which primary (localized) infection is seen.
|
If the primary infection is not treated, it can reach the deep tissues and blood.
|
Due to which systemic infection or secondary infection is seen.
Explain Sign & symptoms seen in bacterial skin disease
Papule and pustule
Nodule and bump
Erythema
Redness
Swelling
Abscess
Pain
Tenderness
Etching
Fever
Chills
Malaise
Diagnosis of bacterial skin infection
History collection (to ascertain whether any systemic disease or immunosuppression therapy is ongoing)
Physical examination (to know the characteristic of lesion and wound)
Complete blood count (especially white blood cell counts)
Culture and sensitivity test (to know the type of infection and which medicine is more effective)
Ultrasonography (to determine if an abscess is present in the soft tissue)
Medical management of bacterial skin infection
Applying a topical antibiotic to the lesion or wound.
Systemic antibiotic penicillin, cloxacillin, dicloxacillin, erythromycin and cephalosporin drugs are used to treat bacterial infections.
Apply warm moist compression.
Clean the wound thoroughly with antistaphylococcal soap.
Use of antipyretic drug to reduce fever.
Use of analgesic medicine to relieve pain. Surgical management of bacterial skin infection
An incision and drainage procedure is used to remove a skin abscess.
Nursing management of bacterial skin infection
To assess vital signs.
Note the color, type of lesion.
Explain to the patient the importance of hygiene and hand washing.
Advise patient to clean wound with antistaphylococcal soap and antiseptic solution.
Regular dressing on the wound.
Explain wound care to the patient.
Advise the patient not to touch the wound frequently.
Advise patient’s family members that each member should use separate towel and wash cloth.
Using gloves when dealing with a wound or lesion.
Advise the patient to use an electric razor while shaving. Apply lotion on the area after shaving.
Change the patient’s position every two hours to prevent bedsores.
Explain the procedure to the patient before the procedure.
Administering medicine prescribed by a doctor.
To maintain records and reports.
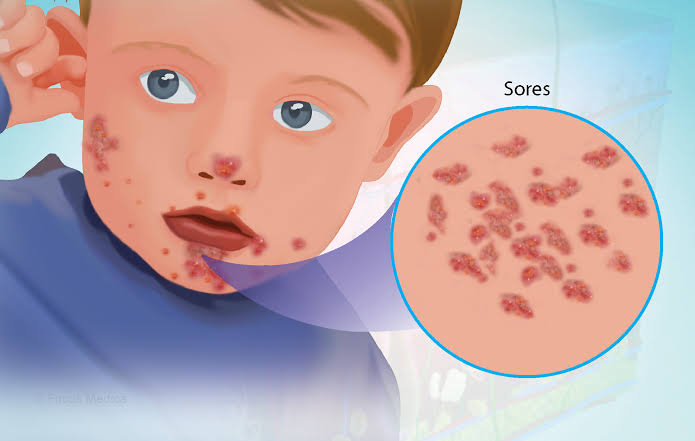
Impetigo (Define Impetigo)
Impetigo is also known as ‘school sore’. Because impetigo is more common in children and spreads among themselves as well as sores.
Impetigo is a contagious superficial skin infection caused by Gram positive Staphylococcus aureus and Group A beta hemolytic Streptococcus and other bacteria.
Impetigo can occur at any age but is more common in children (two to five years).
Impetigo is most often seen on the face, hands, neck and extremities.
write Types of impetigo (Types of impetigo)
There are three types of impetigo based on clinical presentation.
i) Non bullous impetigo
Non bullous impetigo is the most common form of impetigo. In which redis itchy sore is seen around the mouth and nose. Brownish yellow color crust is seen in this sore breakdown.
ii) Bullous impetigo
In bullous impetigo, a large fluid-filled blister develops from the original vesicle. These blisters are painless. As these blisters break down, a raw and red area is seen.
iii) Ecthyma
Ecthyma is a more severe form of impetigo. Ecthyma occurs when impetigo is not treated. In which painful blisters are seen deep in the skin. This blister turns into a pus filled shore and crust.
Write Sign & symptoms seen in impetigo
Small and red color macule is seen in starting.
It then turns into a thin-walled vesicle.
These vesicles are painless.
When this vesicle ruptures, a honey yellow color crust is seen.
Removing this crust reveals a smooth red colored moist surface.
If left untreated, these blisters become painful and a pus-filled sore appears.
Diagnosis of impetigo
History Collection
Physical Examination
Complete blood count
Culture and sensitivity test
Write Medical management of impetigo (Medical management of impetigo)
Provide systemic antibiotics.
Providing benzathine penicillin in non-bullous impetigo.
Use of cloxacillin and dicloxacillin in bullous impetigo.
Using erythromycin medicine for people who are allergic to penicillin.
Topical antibiotic – mupirocin ointment applied two to three times a day.
Wash the lesion thoroughly with an antiseptic solution or soap and remove the crust.
Write Nursing management of impetigo (Nursing management of impetigo)
To note the location and type of skin lesion.
To assess vital signs.
Advise the patient to maintain personal hygiene.
Advise the patient to bathe with antistaphylococcal soap and thoroughly clean the lesion with an antiseptic solution.
Explain wound care to the patient.
Applying topical medicine to the sore.
Advise the patient not to touch the lesion frequently and to wash hands before touching.
Advise the family members of the patient that each member should use a separate towel and wash cloth.
Avoiding the use of items used by the patient and avoiding contact with others.
Administering medicine prescribed by a doctor.
To maintain records and reports.

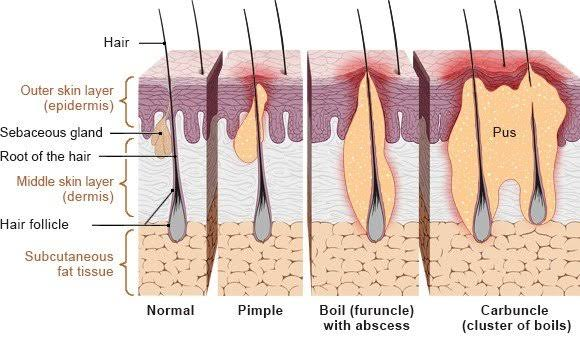
2.Folliculitis
Follicle stands for hair follicle and ITS stands for inflammation
Infection and inflammation of the hair follicle is known as folliculitis.
The infection starts at the opening of the hair follicle and extends down into the follicle.
A bacteria called Staphylococcus aureus is responsible for causing folliculitis.
Folliculitis is more common in areas where excessive friction, moisture and rubbing are present.
Folliculitis occurs mainly in the beard area of the mane where it accumulates, but is also more common in the armpit, groin, buttock and trunk areas.
Folliculitis is more common in people who have poor hygiene and wear tight heavy fabric clothes.
write short notes on type of folliculitis
There are following types of folliculitis:
i) Bacterial folliculitis
Bacterial folliculitis is caused by bacteria called Staphylococcus aureus hence bacterial folliculitis is also called ‘Staphylococcus aureus folliculitis’. Bacterial folliculitis is an infection of the hair follicle. In which a small red and white pus filled pimple is seen around the hair follicle.
ii) Hot tube folliculitis
Hot tube folliculitis is caused by a bacteria called Pseudomonas aeruginosa. This bacteria is found in hot tubes, hit pools and water slides. Hence, a round itchy bump is seen on the skin within one to four days after bathing in such a place.
iii) Pseudofolliculitis barbae
Pseudofolliculitis barbae is also known as ‘razor bump’. Pseudo means virtual. In pseudofolliculitis there is no infection of the hair follicle but signs of infection are present. Pseudofolliculitis barbae mainly occurs in the bearded area. In which irritation is seen in that area after saving with a razor. Pseudofolliculitis Barbe is more common in people with curly hair and dark complexion.
iv) Sycosis barbae
Sycosis Barbe is a severe type of folliculitis caused by saving related folliculitis. In sycosis barbe, the entire hair follicle is infected due to which a large red colored pustule is seen.
v) Pityrosporum folliculitis
Pterosporum folliculitis is also known as ‘Malassezia folliculitis’. Pterosporum folliculitis is caused by a yeast infection. Due to which itchy pus filled bumps are seen. Which is mostly seen in upper chest and back.
vi) Eosinophilic folliculitis
Eosinophilic folliculitis occurs in patients with immunosuppression such as those with human immunodeficiency virus (HIV). In which there is an itching pustule bump in the neck, upper arm, solder, fore head.
vii) Gram negative folliculitis
Gram-negative folliculitis occurs as a result of prolonged use of antibiotics used to treat one. Overuse of this medicine causes bacteria to become resistant to it and these resistant bacteria grow and multiply thus creating the condition of folliculitis. In which pus-filled bumps are seen around the nose and mouth.
viii) Furuncle (boil) & Carbuncle
Furuncles and carbuncles are infections caused by Staphylococcus aureus bacteria deep into the hair follicle. A painful inflamed bump is seen in a furuncle. When a carbuncle is found as a cluster of boils.
Sign & symptoms seen in folliculitis
One or more papules and pustules are seen near the hair follicle.
Erythema is seen around the hair follicle.
There is itching and irritation at the site of the infected hair follicle along with a slight burning sensation.
Tenderness is also seen with it.
Diagnosis of folliculitis
History Collection
Physical Examination
Blood culture
Culture and sensitivity test
Potassium Hydroxide Testing
Medical management of folliculitis
Using topical antibiotics clindamycin and bactroban.
Use of antistaphylococcal soap while bathing.
Providing warm moist compression on the affected area.
Prevention of folliculitis
Wash the skin daily.
Maintaining proper hygiene.
Using a clean towel and washcloth.
Avoiding friction and pressure on the skin.
Avoid wearing tight heavy fabric clothes.
Avoid shaving if possible.
Use another method to remove hair.
Using an electric shaving laser and taking utmost care while shaving.
Apply lotion to that area after saving.
Using clean hot tubes and heat pools.

3.Furuncle
A furuncle is also known as a ‘boil’.
One or more hair follicles are infected in the furuncle and these hair follicles are infected deep and the infection extends to the dermis layer.
That is, furuncle is deep folliculitis.
A bacteria called Staphylococcus aureus is responsible for causing furuncles.
Furuncles are most often found in the neck, axilla, armpits, buttocks and perineum area.
Multiple and recurrent seen
The lesions are known as furunculosis.
Sign & symptoms seen in furuncle
Initially a painful pimple of deep, hard, pink or red color is seen.
Its diameter is one to five centimeters.
After a few days, this pimple increases in size and forms a cystic nodule. In which pus collection is seen i.e. formation of abscess.
Tenderness is also seen around the affected area.
Diagnosis of furuncle
History Collection
Physical Examination
Blood count
Culture and sensitivity test
Medical management of furuncle
Using systemic antibiotics to treat bacterial infections.
Applying a topical antibiotic to the affected area.
Providing warm compresses on the affected area.
Clean the lesion or wound with an antistaphylococcal soap.
Surgical management of furuncle
Using an incision and drainage procedure to remove the abscess.
Nursing management of furuncle
To note the size and color of the skin nodule.
To assess vital signs.
Advise the patient not to prick boils and pimples.
Advise the patient to clean the wound thoroughly with antistaphylococcal soap and antiseptic solution.
Explain wound care to the patient.
Applying topical medicine to the wound.
Explain home care to the patient.
Educate the patient about hand wash and hygiene.
Administer the medicine prescribed by the doctor.
To maintain records and reports.

4.Carbuncle
A cluster of boils is known as a carbuncle.
In a carbuncle, multiple hair follicles are infected simultaneously and this infection extends to the surrounding skin and subcutaneous tissue and abscess formation is seen.
Carbuncles are caused by Staphylococcus aureus bacteria.
Carbuncles are mainly found in thick and inelastic areas.
Carbuncle is mostly found in neck, upper arm, buttock, lateral.
Carbuncles and furuncles are more common in people with immunosuppression, diabetes and systemic diseases.
Sign & symptoms seen in carbuncle
A red colored painful pus filled bump is seen in the affected area.
These bumps range in size from a pea to a golf ball.
Due to the collection of pus, the central part is white or yellow in color.
In addition, leukocytosis, fever, chills and fatigue are seen.
Scar formation is seen.
Diagnosis of carbuncle
History Collection
Physical Examination
Complete blood count
Culture and sensitivity test
Ultra sonography
Medical management of carbuncle
Applying a topical antibiotic to the affected area.
Using the systemic antibiotic dicloxacillin or cloxacillin.
Taking analgesic medicine to relieve pain.
Use of antipyretic drugs to reduce fever. Surgical management of carbuncle
Incision and drainage to drain the abscess.
Regular dressing of the incision and drained area.
Home care of carbuncle
Apply a clean, warm, moist cloth to the affected area.
Clean the affected area with antibacterial soap.
Regular dressing changes.
Wash hands before touching the affected area.
Maintaining proper hygiene.
Taking regular medicine and getting checkup done.

- Cellulitis
Cellulitis is a common and serious bacterial infection.
Cellulitis is a secondary skin infection.
In which infection is seen in skin and subcutaneous tissue.
Bacteria called Staphylococcus and Streptococci are responsible for causing cellulitis.
Cellulitis is most often seen in the lower leg. Apart from this, it is also seen in the face, arm and other areas.
If cellulitis is not treated, the infection can spread to the blood and lymph nodes and a life-threatening condition occurs. Sign & symptoms seen in Cellulitis
Signs and symptoms occur on any side of the body.
Redness and swelling are seen in the affected area.
The infected area is found hot and tender.
Spots and blisters are seen in the infected area.
Swelling is seen in the lymph nodes.
Fever, chills and fatigue are also seen. Diagnosis of Cellulitis
History Collection
Physical Examination
Blood count
Culture and sensitivity test
C-reactive protein Medical management of Cellulitis
Using systemic antibiotics to treat bacterial infections.
Apply topical medicine on the affected area.
Providing warm moist compression.
Clean the infected area with an antiseptic solution.
Provide analgesic medicine to relieve pain.
Administer antipyretic drug to remove fever. Nursing management of Cellulitis
Perform vital sign assessments.
Checking the infected area for tenderness and swelling.
Keep the skin dry and clean.
Immobilize and elevate the part with cellulitis.
Changing the patient’s position every two hours.
Clean the infected area with antiseptic solution and then apply topical medicine.
Advising the patient to maintain proper hygiene.
Administer the medicine prescribed by the doctor.
To maintain records and reports.
