ENGLISH ANATOMY URINARY SYSTEM
URINARY SYSTEM
KEY TERMS
1) Renal cortex (renal cortex) := the outermost layer (part) of the kidney.
2) Bowman’s capsule: = nephron (Nephron which is the basic functional unit of the kidney) Bowman’s capsule is the cup-shaped mouth-like part of the nephron.
3) Nephron: It is the basic functional unit of kidney. It is the microscopic structural unit of the kidney and the biologically functional unit of the kidney.
4) Renal medulla: This is the innermost layer of the kidney.
5) Glomerulus:= This glomerulus is a bundle of very thin capillaries. Which is located inside Bowman’s capsule.
6) Osmolarity: The osmotic pressure of any solution (liquid) is expressed in osmolarity. On which number of moles are present in kilogram of water.
7) ureters:= This is a type of tubular structure. The tube that connects the kidney to the urinary bladder. It allows urine to pass from the kidney to the bladder.
8)urethra:= This is a type of tubular structure that connects the urinary bladder to the external environment of the body. Urine is excreted from the body through its external opening.
9) Bifurcation:= Bifurcation means dividing any branch into two parts.
10) Diuresis: = Excessive production of urine.
11) Renal artery (Renal artery):= This is a blood vessel that is in the kidney. Delivers oxygenated blood supply.
12) Excretion (Excretion): = Whatever waste product (urine) of this body is taken out of the body.
13) Renal vein := These blood vessels carry the filtered blood (deoxygenated blood) to the return circulation. It brings blood back from the kidneys.
14) Renin := This hormone alters the systemic blood pressure. This is a hormone secreted by the kidneys.
15) Sphincter := These are ring-like muscle fibers that have the ability to contract.
- Introduction of urinary system
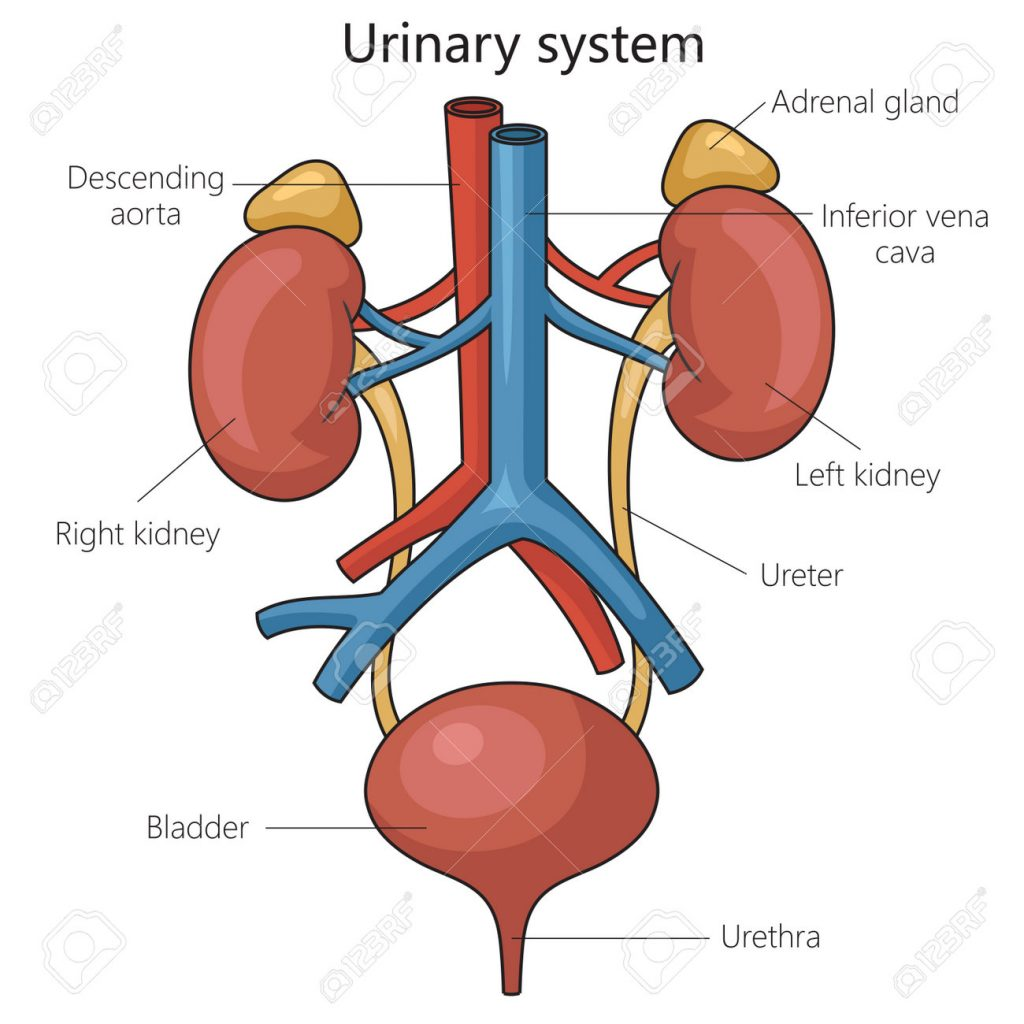
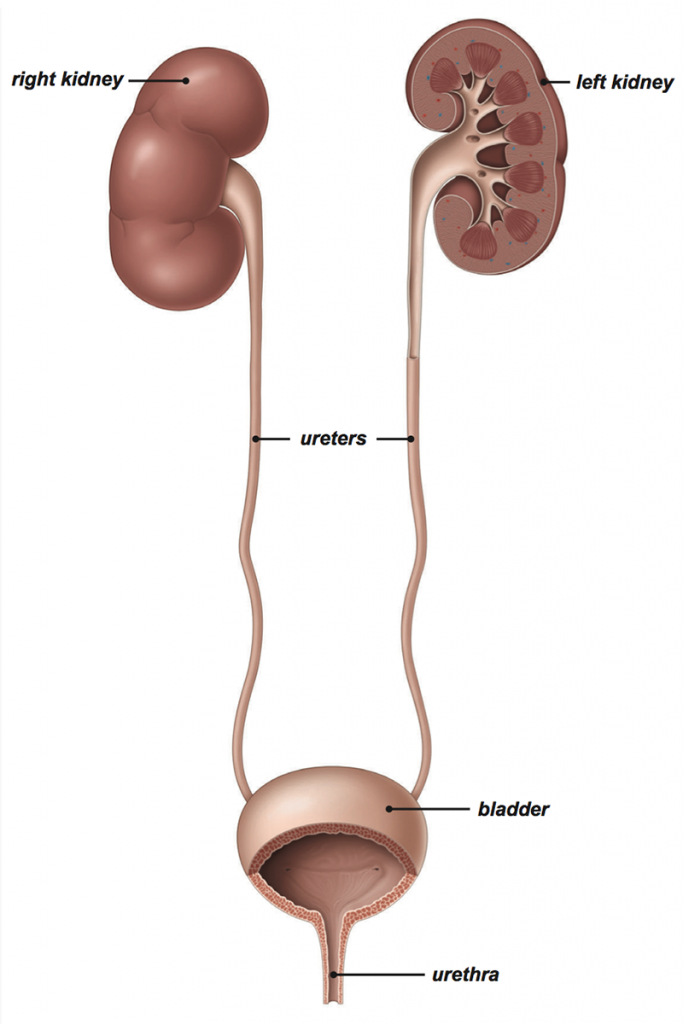
Urinary system is one type of excretory system of the body. It removes the waste products of the body out of the body. Any body substances that are not used in the body (metabolic waste) are removed from the body. It includes the following organs.
2 kidneys := which does the formation of urine. They are right and left 2.
2 ureters:= which carry urine from kidney to urinary bladder. They are right and left 2.
1urinary bladder := This is the organ in which urine is collected. It is in the number of 1.
1 Urethra:= through which the urine accumulated in the urinary bladder is excreted outside the body.
- Gross Structure Of Kidney
There are 2 kidneys in the human body. They are located in the right and left abdominal cavities on either side of the vertebral column on the posterior side of the body.
Kidney is a bean shaped organ. It lies from the level of the 12th thoracic vertebra to the level of the 3rd lumbar vertebra.
Kidney is 11 cm long by 5 to 6 cm wide. Its weight is approximately 150 grams. The right kidney is positioned slightly lower than the left kidney because the liver occupies a larger portion on the right side.
Veins around the kidney.
The kidney is an organ located in the abdominal cavity. One is located on both the right and left sides. Abdominal cavity organs like liver, small intestine, adrenal glands, stomach, spleen, pancreas etc. are located around both kidneys.
Structure of the Kidney..
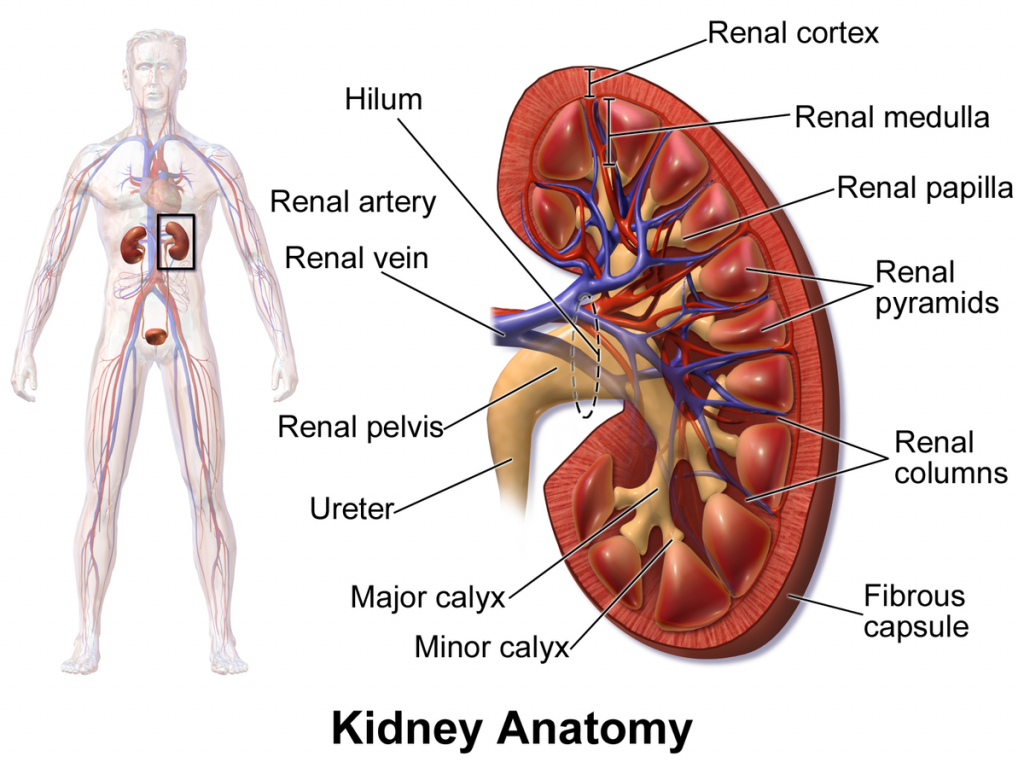
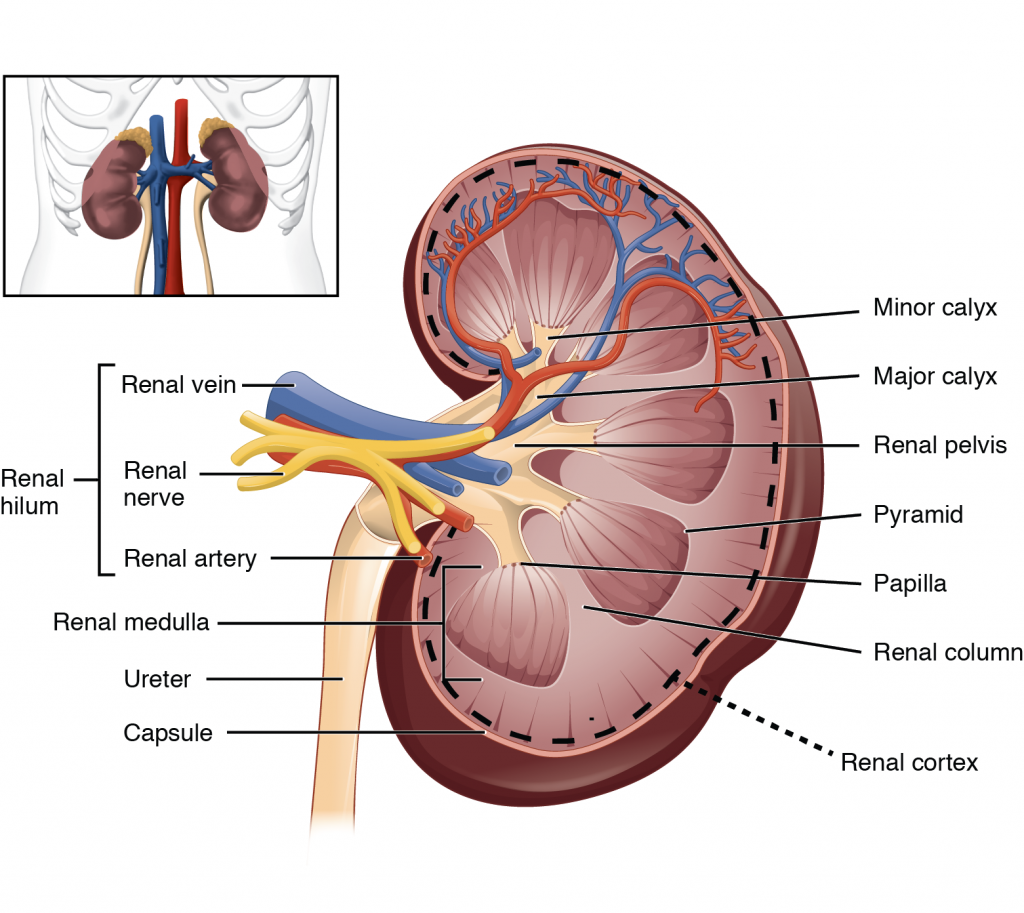
Kidney is a shapeless organ. A groove in the middle is called hilum or renal hilum. Through which the structure of renal artery, renal vein, nerves, lymph vessels and ureter enters and exits.
The inner border or hilum of the kidney is found on the side of the vertebral column.Its outer border is convex. The kidney is a hanging organ on both sides of the abdominal cavity. To hold it in position, it is surrounded by a network of fatty tissue and fibroelastic connective tissue called the renal fascia. With the help of this kidney can maintain its position and it also gets protection.
When the kidney is viewed in a longitudinal section, it is seen to be distributed into three kidney structures.
- Fibrous capsule.
It is part of the fibrous tissue that surrounds the kidney. This membrane is arranged around the kidney. Which acts as a layer to protect and maintain the shape of the kidney.
- Cortex.
It is redis brown in color made up of tissue. Which is located under the kidney capsule.
- Medulla.
In the kidney, the inner part from the cortex is called the medulla. It also has redish brown color. The triangular shaped pyramidal structures are called renal pyramids. The base part of this renal pyramid is towards the cortex and the pointed part of the pyramid i.e. the part of the renal papilla is arranged inwards towards the hilum.
The renal papilla forms an anterior cup-like structure called the calyx. The part with larger space is called major calyx and the part with smaller space is called minor calyx. The minor calyx opens into the major calyx. Beyond this calyx is the wide funnel-shaped portion called the renal pelvis.
The urine filtered by the kidney falls into the wide funnel-shaped part of the calyx, i.e. the renal pelvis. Here the urine collects and then exits the kidney through a narrow structure called the ureter from the renal pelvis anteriorly and reaches the urinary bladder.
Urine filtered by the kidney passes from the minor calyx to the major calyx and from the major calyx to the renal pelvis. It then reaches the urinary bladder through the ureter. This action is not controlled by any kind of nervous system. In the wall of the renal pelvis there are special muscles and pacemaker cells due to the contraction of which this urine flows forward.
Microscopic Structure of Kidney. or
Structure Of Nephron
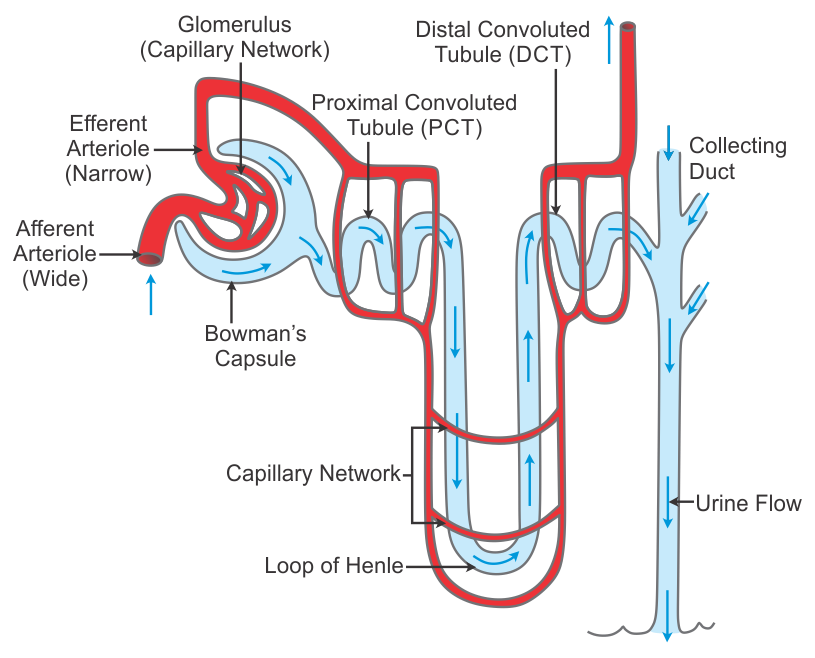
Many compositions are seen when looking at the microscopic structure of the kidney. In which, looking at the kidney under a microscope, a microscopic functional structure i.e. nephron is seen which is the main functional unit of the kidney. There are millions of nephrons in the kidney.
The microscopic structure of nephron includes the following structures.
- Bauman’s Capsule..
Anterior to the nephron is a cup-shaped opening called Bauman’s capsule. The wall of this capsule contains a special type of epithelial cells called podocytes. Both the parietal and visceral layers of the Bowman’s capsule are seen.
A network of arterial capillaries is located between the cup-shaped portion of Bauman’s capsule called the glomerulus. Podocyte cells present here help in the filtration process. The three centimeter long portion anterior to Bowman’s capsule is called the tubular portion.This tubular part can be divided into following parts.
- Proximal convoluted tubule..
The initial tubular portion anterior to Bauman’s capsule is known as the proximal convoluted tubule. It is part of the opening of the tubules of the nephron. Epithelium cells are located in its wall. This part is located in the cortex of the kidney.
- Loop of Henle..
The sharp U turn after the proximal convoluted tubule is called the loop of Henle. It is also called medullary loop. The loop of Henle has a sharp bend between the ascending and descending loops that forms a U-shaped segment. Part of the loop of Henle lies in the medulla of a kidney.
- Distal convoluted tubules.
The tube-shaped portion of the nephron after the loop of Henle is called the distal convoluted tubule. This tube-shaped part forms the trailing limb. Which joins with the collecting duct going forward.
- Collecting Duct ..
The collecting duct is a straight tube. which connects the distal convoluted tubule portion of several nephrons. This tube is known as the large duct. These collecting tubes open into the minor calyx at the junction of the renal pyramids.
When the renal artery enters the kidney through the hilum, it then divides into many smaller arterioles. When these arterioles enter the Bowman’s capsule, the arterioles are called afferent arterioles. The glomerular capsule is divided into a network of capillaries called glomerulus. The arterioles of this capillary network that exit Baumann’s capsule are called efferent arterioles.
The diameter of the efferent arterioles is smaller than the diameter of the afferent arterioles due to which pressure is created on the glomerular membrane and the process of filtration is accelerated and the action of urine formation starts.
Efferent arterioles again divide into smaller capillaries and absorb nutrients and water and mix with the blood circulation.These tiny vessels drain the blood out of the kidney through the renal vein.
Functions of the Kidney..
Kidney is mainly responsible for urine formation.
Kidneys filter the blood and remove the waste products through urine.
The function of the kidney is to maintain the normal balance of electrolytes.
It works to maintain blood pH.
The body functions to remove waste products accumulated at the end of metabolism from the body.
Kidneys secrete a hormone called erythropoietin which plays a very important role in the production of RBCs.
Kidneys secrete a hormone called renin which plays a very important role in maintaining blood pressure.
Kidneys are responsible for maintaining water balance in the body.
- Stages Of Urine Formation (stages of urine formation).
The main function of the kidney is to excrete waste products from the body through urine. Urine produced by the kidneys is collected in the urinary bladder. Then the body exits the head through the urethra. At the bottom of this urine formation
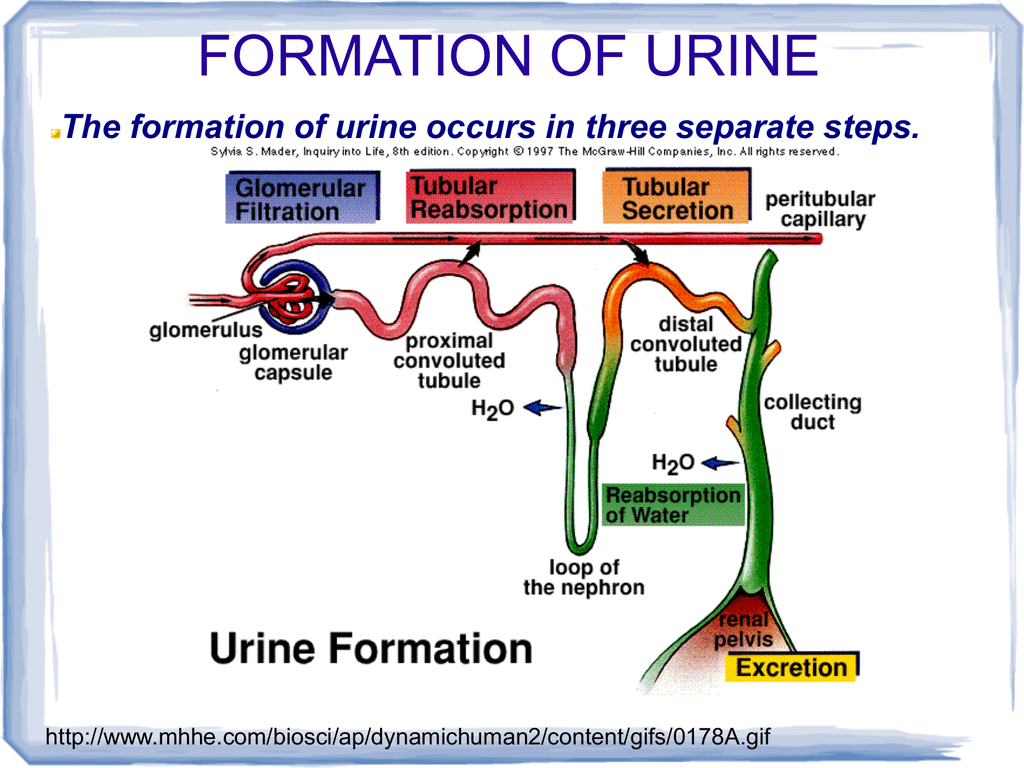
Simple filtration.
The function of filtration in kidney is done by nephron. The afferent arteriole enters within the Bauman’s capsule within the structure of this nephron and is larger in diameter than the efferent arteriole. This network of arteries is called glomerulus.
Pressure is created on this glomerular membrane due to the difference in diameter of the arterioles. Due to which the filtration process is accelerated.
As the glomerulus membrane and the blood capillary membrane are both semi-permeable, the pressure from the blood towards the Bauman’s capsule increases and urea, uric acid, creatinine and many other substances in the blood are filtered in the Bauman’s capsule. Large molecules and proteins in the blood plasma proteins are not filtered due to which blood capillary pressure is high.
The amount of urine filtered through the glomerular membrane in one minute is called the glomerular filtration rate (GFR). Which is normally around 120ml.
Tubular secretion..
Because the blood does not stay in the blood capillaries for a long time on the glomerular membrane, some substances that cannot be filtered are secreted directly into the tubules from the peritubular capillaries surrounding the convoluted tubule.
From the peritubular capillaries, some drugs, some toxic substances, some extra electrolytes and other extra substances present in the blood are secreted into the tubular area and mixed with urine. This phase is called the phase of tubular secretion
Tubular reabsorption..
Urine filtered by the glomerulus enters Bauman’s capsule.Approximately 120 ml of urine is filtered every minute and comes into the capsule. In 24 hours, 150 to 200 liters of urine is filtered through the blood and enters Bauman’s capsule. But not everything is excreted through urine. This fluid is mainly reabsorbed in the tubular portion and during the day approximately one to one and a half liters is excreted from the body in the form of urine.
Reabsorption mainly occurs in the proximal convoluted tubules. Glucose, sodium chloride, water etc. are absorbed through the tubular portion through the membrane of this tube.
Any substances and water in the body are not excreted by filtration if they are in normal proportions. But fluid and substance in excess of the normal amount in the body is filtered by filtration and enters the tubular portion. This tubular portion reabsorbs water and different substances as required by the body.
The aldosterone hormone in the blood plays a very important role in reabsorption of sodium and excretion of potassium.
Anti-diabetic hormone plays an important role in reabsorption of water.
After passing through all the above stages, the fluid that reaches the collecting duct is called urine.
From this collecting duct, urine reaches the minor calyx and thence to the major calyx and then reaches the renal pelvis. From there, the ureters reach the urinary bladder and the urine is excreted from the body through the urethra.
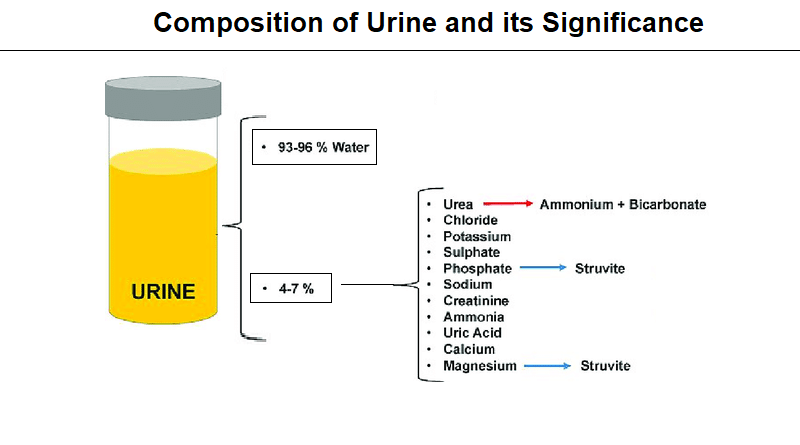
- Composition of Urine..
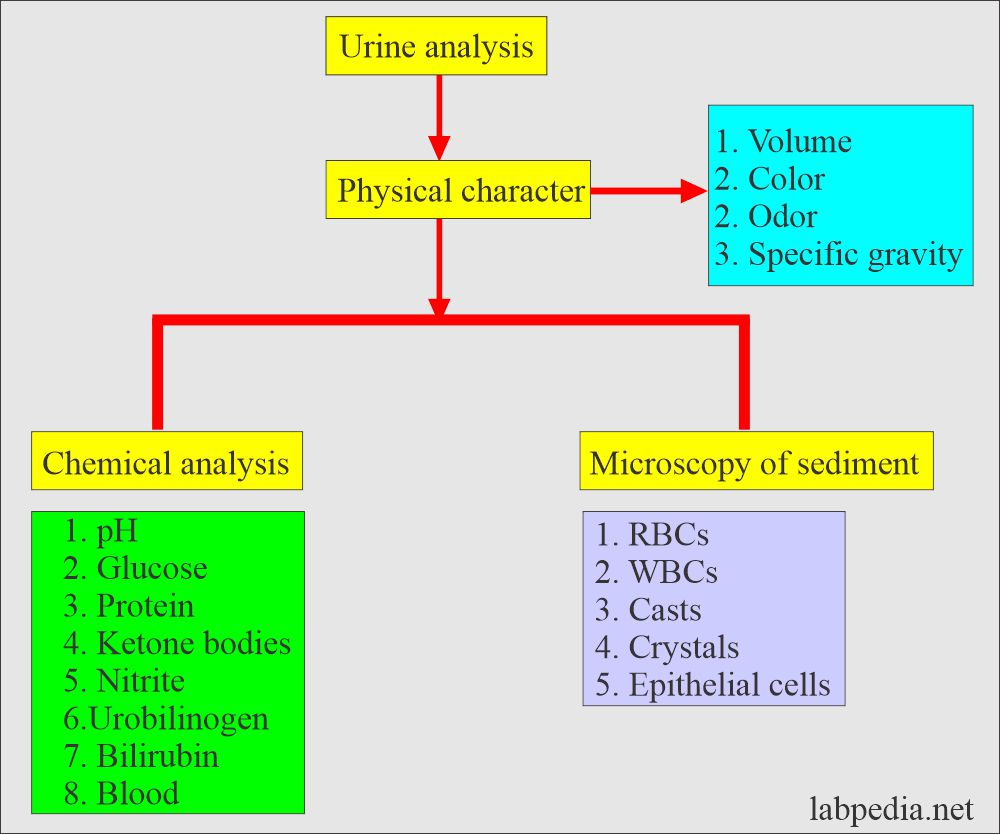
The last 2% of urine contains creatinine, sodium, potassium, chloride, uric acid, sulfate and other waste products.
The specific gravity of urine ranges from 1.0 10 to 1.025.
The pH of urine is slightly acidic ie 4.5 to 8
- RAAS SYSTEM (RENIN ANGIOTENSIN ALDOSTERONE SYSTEM):=
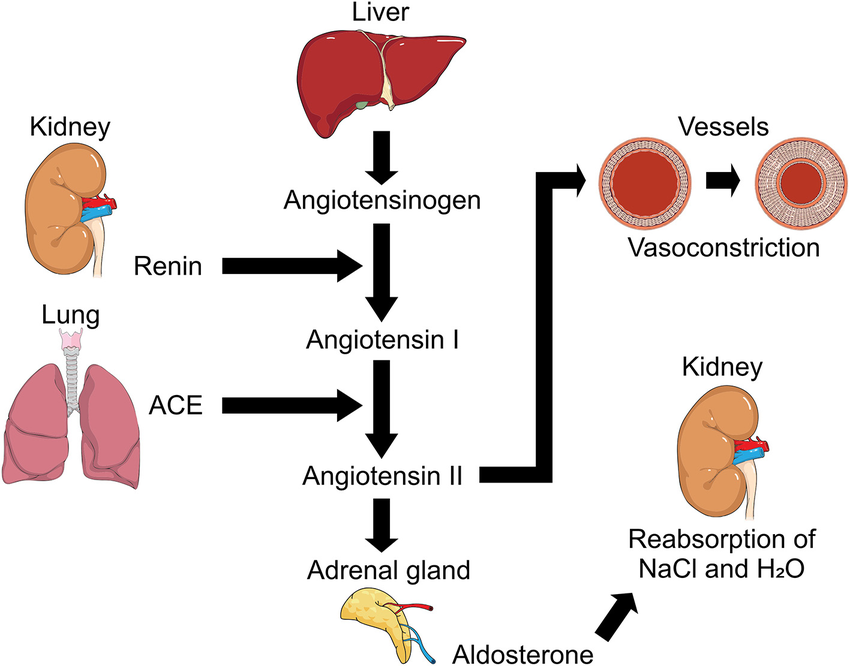
This system is used to increase blood pressure or blood volume in our body when it is low.
When blood volume or blood pressure decreases, the juxtaglomerular cells that lie in the glomerulus of Bauman’s capsule secrete the hormone renin.
When the angiotensinogen hormone is secreted from the liver, the renin hormone converts the angiotensinogen to angiotensin 1.
Angiotensin converting enzyme (ACE) is secreted from lungs which converts angiotensin 1 to angiotensin 2.
Angiotensin 2 acts as a vasoconstrictor. Due to this, blood vessels constrict and blood pressure increases.
Angiotensin 2 activates the adrenal gland and releases the hormone aldosterone from it. This hormone reabsorption of sodium. Due to this, the level of water also increases. Due to this, the blood volume also increases and the blood pressure also increases.
Thus the RAAS system plays an important role in increasing blood pressure in the body when it is low.
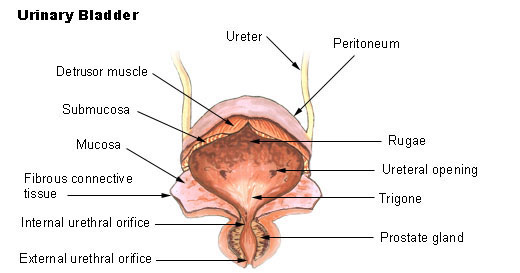
- Ureters
It is a tube-like structure that extends from the kidney to the urinary bladder. Major role of ureter is to transport urine from kidney to bladder.
The ureters are two ducts or tubes. which is attached to the kidney and passes from the kidney to the bladder. It is left and right in number of 2
size
25-30cm or 10-12 inches in length. It has a diameter of 0.6cm (6mm).
Location
The distal part of the renal pelvis of the kidney is narrowed called the hilum. The hilum forms the beginning of the ureter. The ureter passes downward and behind the peritoneum. From the posterior part of the bladder laterally means the opening of the ureter in the bladder from both sides.
Structure
- Mucosa :-(Mucosa)
It is the innermost layer, which is made up of mucus membrane. whose lining consists of transitional epithelium,
- Muscularish or muscle layer
It is the middle layer, which has an inner layer of longitudinal and an outer circular layer of smooth muscle fibers.
- Adventitia or fibrous layer
It is the outer layer, which is composed of areolar connective tissue. which contains blood vessels, lymphatic vessels and nerves.
Function :-
The ureter acts as a passageway for the passage of urine from the kidney to the bladder.
Due to peristaltic contraction of the smooth muscle layer of the ureter, urine is pushed from the kidney to the bladder.
This contraction passes from the renal pelvis to the bladder.
The rate of contractions is one to five per minute depending on how quickly urine is formed.
The reason why urine does not flow back from the bladder to the ureter is because when the bladder fills with urine, the pressure inside the bladder increases, causing pressure on the opening, which consists of folds of the bladder mucosa as a small valve, which covers the opening of the ureter. Due to this, urine does not go back into the ureter.
Blood supply :-
Blood is supplied by branches of renal artery, abdominal aorta, gonadal artery, internal iliac artery, common iliac artery.
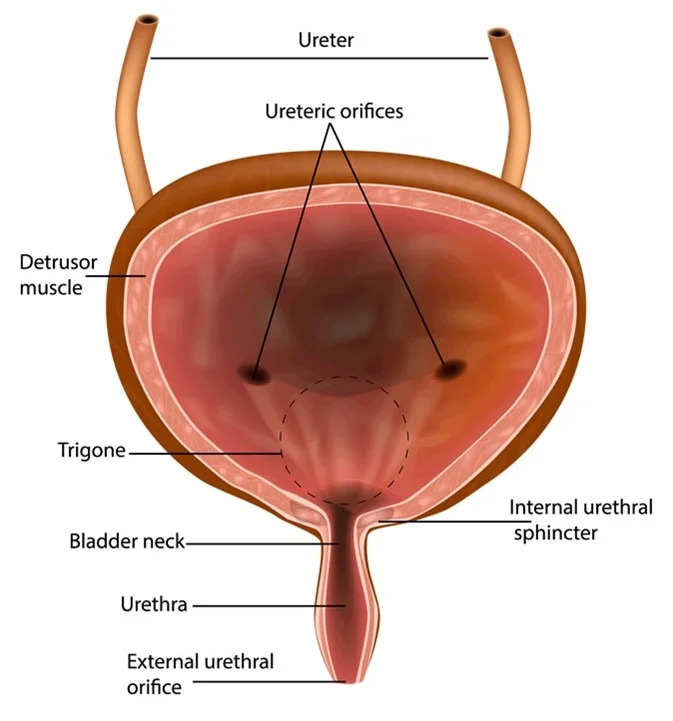
- Urinary bladder
The bladder is a hollow, muscular organ. Its function is as a collector of urine, which receives and stores urine from the kidney and disposes of it after a short period of time.
It stores temporary urine.
Bladder is roughly pear shaped. But when it is filled with urine, it becomes more of an oval shape.
Position
The size, shape and position of the urinary bladder is different for everyone depending on the amount of urine and the age of the person.
In adults, the empty bladder is in the true pelvis. When the bladder fills with urine, it drains into the abdominal cavity.
The bladder in the newborn is in the abdominal cavity.
Capacity
300 to 700 cc. The urge to pass urine begins when the bladder holds 300 to 400 ml of urine.
Structure
Urinary bladder is made up of three layers.
- Mucosa
It is the inner layer. which consists of transitional epithelium tissue. It forms a fold, called a rugai. These folds and the ability of the transitional epithelium to expand cause the bladder to distend.
- Muscular or muscle layer
This is the middle layer. which contains three muscle fibers.
Inner layer contains longitudinal, middle layer circular and outer layer longitudinal muscle fibers.
These muscles are called detrusor muscles. The bladder wall is made up of three layers of smooth muscles. It is called detrozer muscles.
- Adventitia or fibrous layer
It is the outer layer. Which is made up of loose connective tissue. Which contains blood vessels, lymphatic vessels and nerves.
Trigon
There are three orifices or openings in the trigon or triangle bladder wall. which forms a triangle or trigon. The upper two orifices are due to the opening of two ureters in the posterior bladder wall and the lower orifice is due to the opening of the urethra.
sphincter
- External sphincter :-
- Internal sphincter :-
The internal urethral sphincter is not in our control (In Voluntary Control), while the external sphincter is in our control (Voluntary Control).
Functions
Bladder is a collection of urine when the urine has not left the body.
It helps to expel urine from the body with the help of urethra.
The detrusor muscles and transitional epithelium are responsible for storing urine in the bladder.
Blood supply
Blood supplies the internal iliac artery and drains the internal iliac vein.
- Urethra
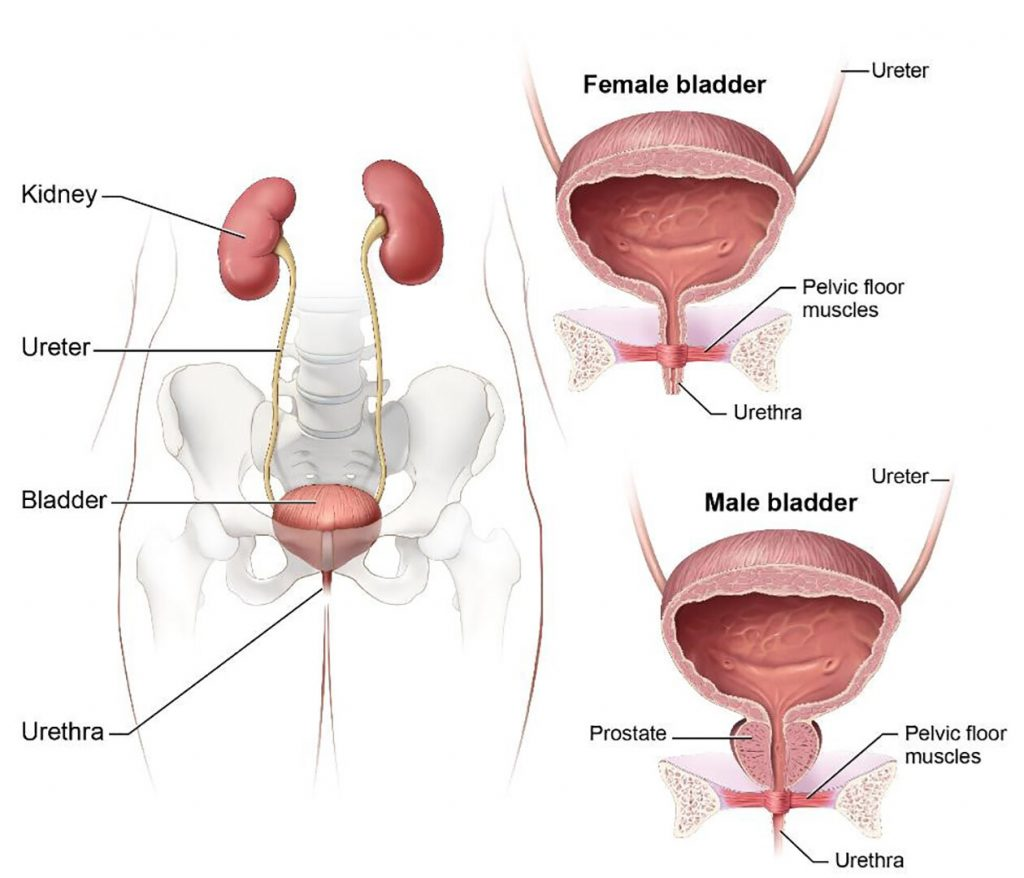
The urethra is a thin-walled tube. which carries urine from the bladder to the outside of the body by peristalsis movement. Urine is discharged from the urinary bladder through this tube.
The urethra extends from the neck of the bladder to the external urethral orifice.
Female urethra
It is 3 to 4 centimeters long. Its external orifice lies anteriorly superior to the vaginal opening and is posterior to the symphysis pubis.
The urethral and vaginal openings are separate.
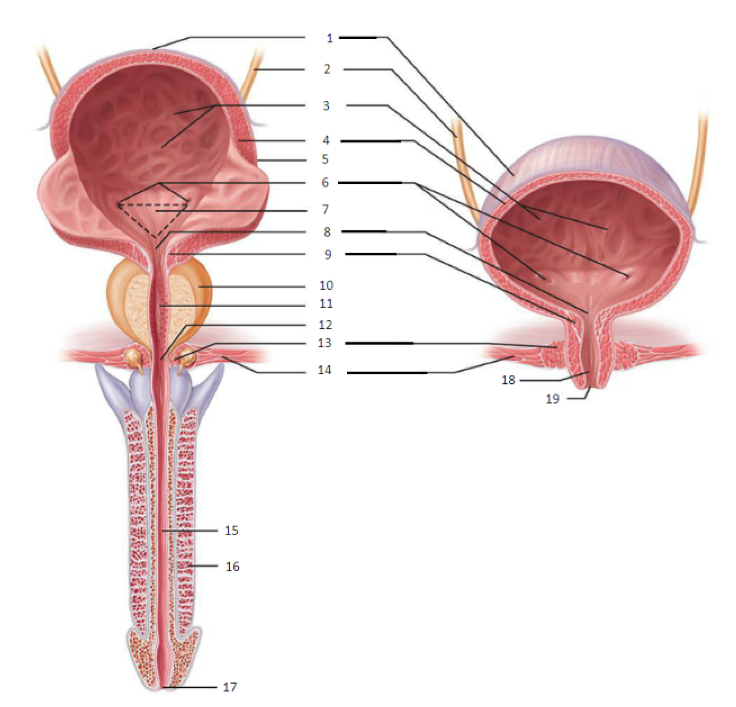
Male urethra
It is 18 to 20 cm long. It has three parts. Prostatic part, membranous part, spongy or penile part.
It opens at the tip of the penis. The male urethra forms part of the urinary system and the reproductive system.
structure
- Mucosa
Mucosa is the inner layer. which has the same layer as the urinary bladder, but its distal end is composed of stratified squamous epithelium tissue.
- Sub mucosa
It is a spongy layer. which contains blood vessels and nerves.
- Muscularis or muscles layer
It is also located in the same layer as the urinary bladder.
Sphincter
- Internal urethral sphincter :-
It is located in the neck of the bladder. It contains elastic tissue and smooth muscle fibers. Which is under the control of the autonomous nervous system (In Voluntary).
The urethral sphincter remains closed due to continuous and slow contractions.
The internal sphincter is voluntary.
2.External sphincter
Surrounding it are skeletal muscles which are supplied by the pudendal nerve. It is voluntary control.
- Micturation
Micturation is a process in which when the bladder is filled with urine, the process of emptying the bladder i.e. passing urine is called micturation.
Process of Micturation
Accumulation
The bladder collects continuous urine until the urine fills up to 200 ml.
Activation
Bladder filling with urine causes stretching of the bladder wall due to which the stretch receptors in the bladder are stimulated.
Transmission
Impulses are transmitted from the bladder by nerves that travel from the sacral portion of the spinal cord to the spinal center (S2-3) and back to the bladder for a stimulatory response, causing contraction of the detrusor muscles.
passage
Due to the strong contraction of the bladder, urine is forced to pass through the internal urethral sphincter. Here the involuntary relaxation of the internal urethral sphincter takes place and the urine reaches the upper part of the urethra.
External sphincter
Due to the presence of skeletal muscles in the external sphincter and due to voluntary control, we can choose to keep the sphincter closed so that urine can be held or by relaxing the sphincter we can expel the urine out of the body, which is called micturition.