ENGLISH-29/07/2024 (UPLOAD)-PAPER SOLUTION NO.09
29/07/2024 -PAPER SOLUTION NO.09
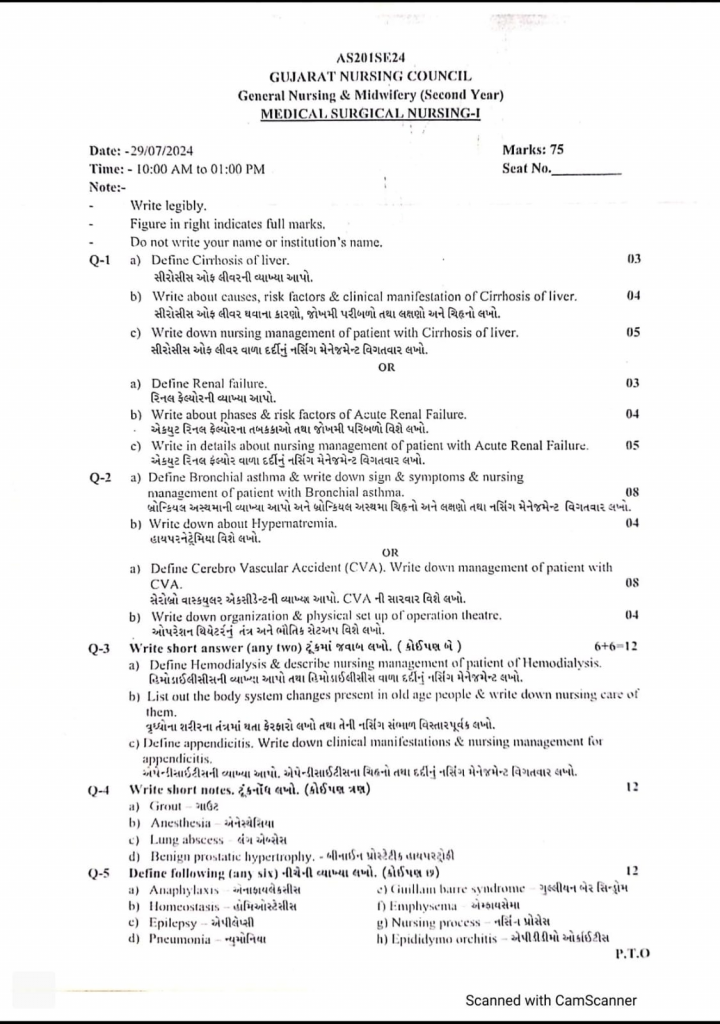
Q-1 a) Define Cirrhosis of liver.
Cirrhosis of the liver is a chronic, degenerative disease in which the normal cells of the liver are damaged and fibrous scar tissues form in the liver. Scar tissues form instead of healthy liver tissues and due to this, blood flow to the liver is blocked and the liver does not function properly, which leads to liver failure. The liver becomes distorted, hardened and lumpy.
Classification of liver cirrhosis:
Classification of hepatic cirrhosis:
1) Alcoholic cirrhosis
2) Post necrotic cirrhosis
3) Biliary cirrhosis
1) Alcoholic cirrhosis:
Alcoholic cirrhosis is also called Laennec’s cirrhosis and is the most common type of cirrhosis.
This cirrhosis is mainly caused by hepatitis C and chronic alcohol use.
In this, the liver is damaged mainly due to malnutrition and chronic alcohol consumption.
In this type of cirrhosis, fibrous tissues form around the portal area and central veins.
2) Post necrotic cirrhosis:
Post necrotic cirrhosis is mainly seen due to any toxic agent and viral hepatitis.
Due to this, liver cell damage is called post necrotic cirrhosis.
Post necrotic cirrhosis is seen in 10-30% of patients.
3) Biliary cirrhosis:
Biliary cirrhosis is a chronic disease. Which is mainly seen due to inflammation and damage to the bile duct in the liver.
In biliary cirrhosis, fibrous tissue and scar formation occurs around the bile duct of the liver. Due to this, chronic obstruction occurs in the bile duct.
b) Write about causes, risk factors & clinical manifestation of Cirrhosis of liver.
Etiology (causes) and risk factors of liver/hepatic cirrhosis:
Due to long-term alcohol consumption.
Due to chronic hepatitis.
Due to obesity.
Due to Wilson’s disease.
Due to cystic fibrosis.
Due to blockage of bile duct.
Due to autoimmune hepatitis.
Due to toxic hepatitis.
Due to chronic congestive heart failure.
Due to non-alcoholic fatty liver disease.
Due to biliary atresia.
Due to surgery in the gallbladder.
Due to glycogen storage disease.
Due to alpha 1 antitrypsin deficiency.
Due to galactosemia.
Clinical manifestation/sign and symptoms of hepatic cirrhosis:
Early stage:
Weight loss,
Fatigue,
Liver enlargement,
Nausea,
Vomiting,
Vascular spider (vascular spider: superficial capillaries are dilated with red dots)
Palmer erythema.
In the ankle.
Intense itching.
Late stage:
Symptoms: abnormal collection of fluid in the abdominal cavity.
Jaundice,
Light colored stool,
Yellowish bright colored urine,
Bruising and bleeding,
Distended veins in the abdomen
Later stage:
Brain function is lost.
The liver cannot remove toxic materials from the blood.
Mental disturbances.
Poor concentration.
Slurred speech.
Atrexis: Flapping and hand tremors are seen.
Motor control is lost in some parts of the body.
Involuntary flapping movements of the hands are seen.
c) Write down nursing management of patient with Cirrhosis of liver.
1) Oedema or Fluid Overload:-
Fluid should be given to the patient in limited quantities
Intake and output of the patient should be maintained
Diuretics should be given as per the doctor’s order
Sodium intake should be reduced in the diet
The patient’s weight and abdominal circumference should be checked daily and recorded
2) Relieve anxiety :-
IPR should be maintained with the patient
The patient should be called by name with respect
The patient’s questions should be answered truthfully and positively.
If possible, a relative or friend should be allowed to stay with the patient
- Fluid electrolyte imbalance:-
Dehydration or overhydration should be checked in the patient
The patient should be encouraged to take sufficient amount of liquid food.
If the patient cannot take it orally, then fluid should be given through I.V. line.
Maintain the patient’s intake-output chart
- Rest and Sleep :-
While giving the medicine to the patient, one should take care of rest and the patient should not be disturbed unnecessarily
The patient should be given a wrinkle free bed
Medicines like those that disturb sleep should be given on time
Drugs:- Lasix should be given in the morning,
Evening medicines should be given before going to bed
- Prevent complication:-
Regular observation of the patient should be done, including checking vital signs, including checking TPR, B.P and recording it
The patient’s intake and output chart should be maintained
If any complication is found, the doctor should be informed immediately.
Emergency medicine tray should always be kept ready and kept in a place where all patients are as close as possible.
OR
a) Define Renal failure.
Renal failure:
Renal failure is also known as kidney failure. Renal failure is a condition in which the kidneys lose their ability to remove waste products from the body and perform filtration. This condition causes toxic materials to accumulate in the body and electrolyte imbalances in the body. Renal failure is a condition in which the kidneys fail to function adequately.
There are two types of renal failure.
- Acute renal failure
Acute renal failure is also known as acute kidney injury (AKI). In which kidney function declines suddenly and rapidly. Acute kidney failure is a condition in which the functional ability of the kidneys is suddenly impaired, due to which the kidneys cannot filter properly and urine output also decreases. (less than 1ml/ kg/ hr) and cannot maintain electrolyte balance and fluid balance in the body. Acute kidney failure occurs within 7 to 90 days. In acute kidney failure, mainly the glomerular filtration rate (GFR) decreases, the concentration of blood urea nitrogen increases, the amount of creatinine increases, urine output is less than 400ml throughout the day, the condition of hyperkalemia arises and sodium retention is seen in the body.
- Chronic Renal Failure
This is an irreversible renal disease. In which there is a progressive loss of renal function. Which is seen due to some other disease. In this condition, when acute renal disease is not treated on time, it is a chronic condition seen due to the gradual decrease in kidney function. In which the kidneys fail to filter the blood and waste products accumulate in the blood.
b) Write about phases & risk factors of Acute Renal Failure.
Acute Renal Failure (ARF) Phases:
1.(Initiation Phase)
Features:
This phase begins immediately after injury and usually lasts for hours to days. It can be caused by ischemia, toxins, or sepsis.
Urine output is normal or slightly decreased.
Blood Urea Nitrogen and Creatinine levels are slightly elevated.
Kidney damage can also be reversed with appropriate treatment.
- Oliguric Phase
Features:
This phase usually lasts for 1 to 2 weeks. Urine output is less than 400 mL/day.
Glomerular Filtration Rate decreases.
Fluid overload, electrolyte disturbances such as hyperkalemia, and metabolic acidosis occur.
The patient may experience muscle tension, sleep disturbances, nausea, vomiting, and high blood pressure.
Life-threatening emergency states may also develop during this phase.
3.Diuretic Phase
Features:
This phase marks the beginning of recovery.
There is a significant increase in urine output (in some cases up to 3 to 5 liters/day).
Filtration now increases, but tubular function is not yet completely recovered.
Conditions such as dehydration, hypokalemia, and hypotension may arise.
Careful fluid and electrolyte management of the patient is required.
4.Recovery Phase
Features:
Duration: This phase can last from a week to months.
Normal urine output and BUN and creatinine levels return to normal.
Most patients recover completely, although some patients are at risk of developing chronic kidney disease.
Summary:
Acute renal failure is a severe condition in which kidney function is immediately reduced. It has four phases:
1.Initiation Phase: The onset and injury
2.Oliguric Phase: Urine output decreases and electrolyte disturbances occur
3.Diuretic Phase: Urine output increases but irregularly
4.Recovery Phase: The kidneys gradually recover.
Causes and Risk Factors of the Acute Renal failure:
1) Pre Renal cause
Due to impaired blood supply to the kidney. Due to dehydration.
Diarrhea.
Vomiting.
Hemorrhage.
Burn.
Due to excessive use of diuretic medicine.
Due to decreased cardiac output.
Due to congestive heart failure.
Due to cardiogenic shock.
Due to acute pulmonary embolism.
Due to constriction of blood vessels supplying blood to the kidney.
Due to dilation of blood vessels supplying blood to the kidney.
2) Intrarenal:
Intrarenal failure is mainly seen due to structural damage in glomeruli, kidney tubules, nephrons. Due to prolonged renal ischemia.
Due to blood clot, cholesterol deposition around veins and arteries.
Due to infection.
Due to hemolytic uremic syndrome.
Due to severe transfusion reaction.
Due to exposure to any nephrotoxic agent.
Like:
NSAID Drug,
ACE inhibitor,
Aminoglycoside Lupus,
Multiple myeloma,
3) Postrenal:
Due to obstruction of urine flow.
Due to enlargement of the prostate gland.
Due to kidney stones.
Due to cancer of the urinary tract organs.
Due to certain types of medications.
Due to bladder stones.
Due to enlargement of the prostate gland.
Due to bladder cancer.
Due to neurological disorders.
c) Write in details about nursing management of patient with Acute Renal Failure.
a) Pain:
Analgesics should be given to the patient as per the doctor’s orders.
The patient should be positioned properly.
Other antibiotics should also be given to the patient at the right time.
In case of severe pain, the doctor should be informed immediately and if there is an order, opioids should be given.
b) Fever:
The patient’s body temperature should be checked regularly.
If there is high fever, the patient should be given antipyretics.
If the patient is feeling cold, an extra blanket should be given.
A wet cloth should be kept on the patient’s head.
c) Anxiety:
The patient should be treated with courtesy.
The patient and his relatives should be informed about the hospital and ward setup.
If possible, a relative should be allowed to stay with the patient at all times
Answer all the patient’s questions calmly and positively
D) Body fluid overload or electrolyte imbalance :-
Antiemetics should be given for vomiting
The patient should be checked for overhydration and edema and the severity of edema should be monitored.
Give diuretic drugs to the patient as per the doctor’s order
The patient should be encouraged to take small amounts of fluids
The patient’s daily body weight should be checked and recorded
The level of pitting edema in the patient should be recorded
The patient’s intake and output chart should be maintained.
E) Altered Nutrition less than body requirement :-
Based on the patient’s age, weight and blood glucose level as well as the nutritional needs should be calculated and encouraged to take a diet accordingly.
The patient’s blood glucose level should be checked regularly
The patient should be given a diet as follows:
High calorie
Low protein
Low salt or no salt
Low fluid
The patient should be given vitamins and iron supplements.
F) Prevent complication:-
Regular observation of the patient should be done.
The patient’s TPR and BP chart should be maintained
The patient’s problem should be listened to carefully and signs of complications should be noted.
If any type of complication is found in the patient, the doctor should be informed immediately.
An emergency medicine tray should always be kept ready with the patient
G) Restlessness:-
The patient should be given a comfortable position.
If the patient has difficulty breathing, then oxygen therapy should be given
Diuretic medicines should be given to the patient only in the morning and afternoon. It should not be given in the evening and at night, due to which the patient experiences nocturia, due to which the patient cannot sleep.
If the patient has a catheter, it should be kept in the right position and the insertion site should be kept clean.
H) Unhygienic conditions:-
If necessary, the patient should also be given diapers
The patient should be helped to maintain personal hygiene.
Suitable water should be provided for bathing according to the season.
If the patient is unable to do mouth care himself, then mouth care should be done
If necessary, bed bath should also be given
Q-2 a) Define Bronchial asthma & write down sign & symptoms & nursing management of patient with Bronchial asthma.08
Bronchial asthma:
Bronchial asthma is a chronic inflammatory respiratory disorder. In which the airways (respiratory track) become hyperresponsive to certain stimuli, due to which the airways become inflamed and narrowed, and due to mucus production, the airways become constricted and obstruction is seen in them. Asthma is reversible.
Some types of etiological factors cause airway hyperresponsiveness.
Due to this, inflammation is seen in the airways. Due to which hypersecretion of mucus, contraction of airway muscles and swelling of bronchial membranes are seen, due to which airways become narrowed. Due to this, cough, chest tightness, shortness of breath and wheezing sound are seen.
Clinical manifestation/Sign and symptoms of the Bronchial asthma:
Dyspnea,
Wheezing,
Coughing with or without expectoration of sputum,
Chronic cough,
Shortness of breath,
Tight feeling in chest,
Increase respiratory rate,
Child is pale, irritable, blurred vision,
Chest pain,
Breath sound is diminished,
Headache,
Muscle twitching,
Confusion,
Coma.
nursing management of patient with Bronchial asthma. Nursing Management of Bronchial Asthma
Impaired gas exchange related to altered oxygen supply, obstruction of airway
Improve gas exchange
Monitor vital signs.
Assess respiratory rate, rhythm and breathing pattern.
Assess breath sounds and chest movement.
Monitor pulse oximetry and arterial blood gas values.
Provide the patient with a Fowler position and restrict his/her activity.
Explain and encourage deep breathing and cuffing exercises to the patient.
Provide knowledge to the patient about pursed lip breathing and diaphragmatic breathing.
If secretions are present, encourage the patient to expectorate.
If SpO2 level is low, provide oxygen therapy.
Provide nebulization to the patient.
Administer prescribed medicine (bronchodilator) by the doctor.
Maintain records and reports.
Ineffective airway clearance related to obstruction from narrowed lumen Maintain patent airway (maintain airway patent)
Monitor vital signs.
Assess respiratory rate, rhythm, and breathing pattern.
Assess breath sounds and chest movement.
Monitor pulse oximetry and arterial blood gas values.
Provide the patient with a Fowler position and restrict his/her activity.
Explain and encourage the patient about deep breathing and cuffing exercises.
Provide knowledge about pursed lip breathing and diaphragmatic breathing to the patient.
Encourage the patient to expectorate phlegm if secretions are present.
Provide oxygen therapy if SpO2 level is low.
Provide nebulization to the patient.
Administer prescribed medicine (bronchodilator) by the doctor.
Maintain records and reports.
Ineffective breathing pattern related to bronchospasm Improving breathing pattern (Improving breathing pattern)
Monitor vital signs.
Assess respiratory rate, rhythm and breathing pattern.
Assess breath sounds and chest movement.
Monitor pulse oximetry and arterial blood gas values.
Provide the patient with a Fowler position and restrict his/her activity.
Explain and encourage deep breathing and cuffing exercises to the patient.
Provide knowledge about pursed lip breathing and diaphragmatic breathing to the patient.
Encourage the patient to expectorate phlegm if secretions are present.
Provide oxygen therapy if SpO2 levels are low.
Provide nebulization to the patient.
Administer prescribed medicine (bronchodilator) by the doctor.
Maintain records and reports.
Anxiety related to disease condition, hospitalization Reduce anxiety
Assess the patient’s condition.
Pay attention to the patient’s psychological needs and listen carefully to the patient.
Encourage the patient to express his feelings, discomfort and anxiety.
Solve all the doubts and queries of the patient.
Provide the patient with knowledge about his condition and treatment so that his anxiety is removed and the patient becomes confident.
Provide psychological support to the patient.
Provide mind diversion therapy and recreational therapy to the patient.
Activity intolerance related to fatigue, dyspnea Increase activity level
Assess the patient’s condition.
Check the patient’s activity level.
Provide bed rest to the patient initially.
Then gradually encourage the patient to do range of motion exercises.
Assist the patient with his/her activity.
Provide rest to the patient between 2 activities.
Check whether the patient has any breathing difficulty during the activity.
If breathing difficulty is observed, stop the patient’s activity and provide rest.
b) Write down about Hypernatremia.
Sodium excess/ hypernatremia:
Hypernatremia is an electrolyte imbalance in which the amount of sodium in the blood increases. When the amount of fluid in our body is less and if the salt is more and if the renal function is impaired, then the amount of sodium in the body increases and the condition of hypernatremia arises.
The normal level of sodium in the body is 135 to 145 meq/liter.
If the value of sodium in the body increases more than the normal value, it is called hypernatremia.
(The normal level of sodium in hypernatremia is >145 meq/liter).
Etiology/cause of hypernatremia:
Loss of fluid from the body,
Vomiting,
Diarrhea,
Sweating,
High fever,
Dehydration,
Not drinking enough water,
Some medications such as steroids, licorice and certain blood pressure lowering drugs,
Some endocrine diseases such as diabetes and aldosteronism,
Excessive salt intake.
Excessive use of sodium bicarbonate.
Uncontrolled diabetes.
Exercising heavily.
Renal dysfunction.
Osmotic diuretics.
Clinical manifestation/sign and symptoms of Hypernatremia:
Increase thirst.
Dry and sticky mucous membranes.
Restlessness and agitation.
Decrease urine output.
Decrease weight.
Weakness.
Tissue firming.
Disorientation.
Tachycardia.
Confusion and personality change.
Decrease consciousness level.
Loss of appetite.
Nausea.
Vomiting.
Fluid and Electrolyte imbalance.
Pulmonary Edema.
Pitting Edema.
Abnormal Skin turgur.
Postural hypotension.
Difficulty in breathing.
Diagnostic evaluation of hypernatremia:
History taking,
Physical examination,
Serum electrolyte: serum sodium level >145meq/liter.
High serum osmolarity.
Increased urine specific gravity.
Management of hypernatremia:
Administer hypotonic electrolyte solution intravenously to the patient.
Instruct the patient to drink adequate amounts of water.
Provide the patient with diuretic medicine.
Maintain the patient’s intake output chart.
Monitor fluid loss or gain in patients at risk of increased sodium levels.
Maintain and assess the patient’s intake output chart.
Instruct the patient to consume a low sodium diet.
Notice how thirsty the patient is.
Check the patient’s body temperature for elevations.
Check the patient’s vital signs for changes.
Check the patient’s level of consciousness.
Check the patient for headache, nausea, vomiting, and any changes in the patient’s vital signs.
Monitor the patient’s intake output chart and assess the sodium level.
If the patient is having seizures, lower the bed and raise the side rails on the bed.
If the patient has diabetes insipidus, ask him to drink plenty of water.
Tell the patient to avoid salty foods, salt tablets, salty liquids, and soft drinks.
Educate the patient to consume plenty of water during exercise.
Tell the patient to consume adequate amounts of water when taking diuretic medications.
Assess whether the patient’s sodium level is increasing or decreasing.
Maintain aseptic technique when providing intravenous fluids.
Monitor the patient carefully if he or she has a fever or is vomiting uncontrollably.
Admit a patient who is vomiting profusely to the hospital immediately to prevent dehydration.
Check that the patient is oriented to time, place, and person.
Provide reassurance to the patient.
OR
a) Define Cerebro Vascular Accident (CVA). Write down management of patient with 08
CVA it’s called Verebrovascular Accident (Cerebro Vascular Accident):
Cerebro vascular accident is also called stroke. Stroke is also often called Brain Attack (“Brain Attack”). Cerebro vascular accident is a condition in which the brain cells, tissues and any particular brain part are not supplied with sufficient amount of oxygen due to insufficient amount of blood supply. Due to this, the brain cells, tissues and parts of the brain are not supplied with sufficient amount of oxygen, due to which the brain part is infraction (Death of the brain tissues) occurs, so that part of the brain cannot function properly and the body function that is done by that part of the brain is also impaired.
Classification of the Cerebro vascular Accident:
1) Ischemic stroke:
This type of stroke occurs due to interruption of blood supply to the brain.
Thrombotic Stroke:
This type of stroke occurs due to the formation of a blood clot in one or more blood vessels of the brain, the condition of thrombotic stroke arises.
Embolic Stroke:
In this stroke, a blood clot forms in any blood vessel of the body and that blood clot travels to the blood vessels of the brain and then the blood clot that has traveled gets stuck in the vessels of the brain, then an embolic stroke occurs.
2) Heamorraagic Strock:
Hemorrhagic stroke is when any cerebral vessels rupture due to any reason, bleeding occurs in the brain and due to this, the condition of hemorrhagic stroke arises.
medical management of the patient with the Cerebro Vascular Accident.
1) provide Thrombolytic Agent to the patient.
Thrombolytic agent breaks down the blood clots formed in the blood vessels and provides space for blood flow to the particular part. Thrombolytic agent is to provide tissue plasminogen agent (TPA) to the patient.
2) provide Anticoagulant drug to the patient.
Anticoagulant drugs prevent the formation of blood clots and play a role in maintaining blood supply.
Ex:= Heparin,Warfarin.
3) Provide Antiplatelet drug to the patient.
This medicine prevents the aggregation of platelets due to which blood clot formation does not occur.
4) Provide Diuretics medication to the patient.
If there is accumulation of fluid, then provide diuretic medicine to the patient to remove it and decrease intracranial pressure.
5) Continuously monitor the patient’s vital signs.
6) Provide supplementary oxygen to the patient.
7) If the patient is having severe headache, then provide analgesic medication to the patient.
8) Advise the patient to make lifestyle modifications.
Surgical management of patients with the Cerebro Vascular Accident.
Surgery is mainly performed to repair the ruptured blood vessels and to remove the blood clots that have formed in the blood vessels.
Nursing management of patients with the Cerebro Vascular Accident.
1) Ineffective Cerebral tissues percussion related to interruption of blood supply.
2) Impaired physical mobility related to Neuromuscular Impairment.
3)Impaired Verbal communication related to loss of facial muscles tone.
4) Knowledge deficit related to Disease condition and treatment.
Nursing management:
Assess the neurological status of the patient.
Advise the patient to take proper rest.
Provide oxygen to the patient properly.
Monitor the patient’s vital signs properly.
Change the patient’s position frequently.
Advise the patient to speak slowly.
Advise the patient to limit activity.
Advise the patient to take medication properly.
Maintain the patient’s hydration status properly.
Maintain the patient’s nutritional status properly.
Advise the patient to do daily routine activities in small amounts.
Provide analgesic medicine if the patient is in pain.
Collaborate properly with other health care personnel for the proper care of the patient.
Provide occupational therapy, physical therapy, speech therapy to the patient.
Advise the patient to avoid fatty foods.
Advise the patient to avoid smoking and alcohol.
Advise the patient to exercise regularly.
Advise the patient to maintain his blood cholesterol level in the normal range.
Assess the patient’s proper glass go com scale.
Advise the patient to exercise properly.
Advise the patient to speak in small amounts.
Advise the patient to reduce weight if he is obese.
Advise the patient to take proper medication.
Advise the patient to follow up properly.
b) Write down organization & physical set up of operation theatre. . 04
Operation theater style should be
The room environment should be comfortable
There should be a system for infection control
Modern equipment should be used
The operation theater should be separate from other rooms in the hospital
There should be separate arrangements for different operations
There should be an arrangement for artificial ventilation to maintain the temperature of the operation theater
There should be a system for 24 hours electricity supply
Each door of the operation theater should have a hydraulic system
There should be a mobile X-ray system
The operation theater should have all the rooms as per the requirement
The operation theater should be connected to the hospital by a road.
The light fitting and sewer line of the operation theater should be underground
The ground flooring of the operation theater should be made of marble or cobblestone.
The windows and doors of the OT should be of one-way glass and should be covered with curtains.
The floors, walls and furniture of the OT should be washable.
After entering the OT, there should be an arrangement so that the patient cannot easily see other patients, the operation or the staff members.
There should also be a mobile light and shadowless light.
The staff and servants working in the OT should be well trained.
The following units should be present in the Idle Operation Theater. To prevent infection, there should be a facility so that the patient enters from one side and exits from the other side.
Reception room:-
When the patient enters the operation theater, there should be a separate room to receive him.
The patient area should be comfortable. The walls of this room should be colorful and posters should be posted.
There should be a reception room for adults and children. And the room should have a telephone system. This room should be away from the operation theater room. Nursing staff should be on duty in this room.
Changing room:-
This room should be away from the operation theater room. In this room, every staff wears OT dress.
Anesthesia room:-
This room should be attached to the main operation room. This room should have a bed, anesthesia trolley and related equipment. This room should have a cupboard to keep anesthetic equipment. This room should have oxygen, suction machine, B. P. Apparatus, anesthetic drugs, and emergency drugs in sufficient quantities in trays. This room should be in such a way that the patient cannot see it
Scrub room:-
The surgeon and staff scrub in this room. For this, necessary things like antiseptic liquid, soap, towel, mirror should be arranged and there should be a large size sink and a handle tap for hand washing procedure and there should be a provision for 24 hours water supply and this room should have sterilized apron and gloves
Main operation room:-
It is the main part of the OT where the operation is done. This room should be air conditioned. This room should have all the modern equipment like suction machine, mobile light, mobile X-ray, cautery machine, oxygen, anesthesia trolley, emergency injection tray, ventilator etc.
There should be tables according to the operation to give the position. And there should be shadowless light on the operation table.
Preparation room :-
There should be separate arrangement of tubs and ranks for making sets and drums according to different operations
Sterile supply room :-
This room should be arranged for keeping sterilized items and for their supply
Central sterilization supply unit :-
This room should be away from the operation room where all the items are sterilized. For this, there should be an autoclave machine. This room should have proper ventilation.
Minor operating room :-
This separate room should be arranged for minor procedures
Utility room :-
This room should be arranged for cleaning and separating the instruments, linen, gloves etc. used and damaged during the operation
Infectious disease operating room:-
If there is a patient with infectious diseases, then a separate room should be arranged for them to operate so that it should be separate from the main operation room so that the spread of infection can be prevented and timely Regular fumigation should be done
Recovery room :-
The main purpose of the recovery room is to provide total nursing care to the operated patient. The staff working in this room should have knowledge of post-operative and post-anesthetic complications.
This room should have resuscitation equipment, suction machine, emergency drugs, as well as oxygen. There should be a modern bed arrangement for the patient so that the patient can be given the right position and there should be necessary equipment in post-operative.
Q-3 Write short answer (any two)6+6-12
a) Define Hemodialysis & describe nursing management of patient of Hemodialysis.
Definition:-
Hemodialysis is a method of removing excess waste (metabolic waste products) from the body in cases of renal failure, in which excess waste is removed from the blood.
After removing harmful substances, the purified blood is returned to the patient’s body.
Purpose :-
To remove excess waste from the patient’s body.
To make the body’s buffer system positive
To remove excess fluid from the body
To reduce water retention
To maintain the level of electrolytes in the body
To prevent other complications
Indications:-
Acute renal failure
Chronic renal failure
Uremia
Renal encephalopathy
Severe edema
Metabolic acidosis
Procedure :-
In hemodialysis, there is a machine (dialyzer) for purifying the blood. In which impure arterial blood is taken from the patient’s body and sent to it. The useless waste in the blood is filtered and then becomes pure blood, which is injected into the patient through a vein.
In hemodialysis, a fistula (connection between an artery and a vein) is made. From where impure blood is removed and pure blood is introduced.
This fistula can be made on wrist, arm and neck.
Complication:-
Dehydration
Hypovolemia
Hypotension
Hypovolemic shock
Septicemia
Death
Care during hemodialysis:-
Check the patient’s weight and record it.
Written consent is obtained from the patient for dialysis.
Explain the dialysis procedure to reduce their anxiety
Provide the patient with a comfortable position
Ask the patient to stop antihypertensive and vasodilator medications before dialysis, if any, as dialysis can cause hypotension
Check and monitor vital signs
If there is any problem during dialysis, the patient should be asked about it and if necessary, the doctor should be informed immediately.
Check the patient’s fistula site regularly because due to the use of heparin during the procedure, the clotting process slows down and the possibility of bleeding increases.
All emergency medications should be kept ready with the patient
The patient should be given the necessary medications.
After the completion of hemodialysis, the patient’s weight should be checked again
The patient should be given the necessary medications after hemodialysis.
b) List out the body system changes present in old age people & write down nursing care of them.
List of the body system changes present in old age people :
- Nervous System:
Changes:
In old age, the size of the brain decreases and neurons gradually degenerate. Due to which symptoms like memory loss, slow reaction and dementia are seen. Both sensory and motor function are affected.
- Cardiovascular System:
Changes:
Heart rate slows down and elasticity of veins and arteries decreases. Atherosclerosis increases, which increases the risk of heart attack and high blood pressure.
3.Respiratory System:
Changes:
The elasticity of the lungs decreases, and the ability of the alveoli to expand decreases. Due to the decrease in oxygen uptake, fatigue, low energy, and low stamina are observed.
4.Digestive System:
Changes:
The secretion of digestive juices slows down, due to which the stool becomes hard and constipation occurs. The function of the pancreas and liver also gradually decreases.
- Urinary System:
Changes:
The filtering function of the kidneys decreases. Blood urea nitrogen and creatinine levels may increase. Urinary incontinence occurs, which reduces the ability to hold urine.
- Endocrine System:
Changes:
The levels of major hormones such as insulin, thyroid and adrenal hormones decrease. The risk of diabetes increases due to the slowing of insulin response.
- Reproductive System:
Changes:
After menopause in women, estrogen levels decrease. Testosterone gradually decreases in men. Both affect reproductive ability and sexual function.
- Musculoskeletal System:
Changes:
Bone density decreases (Osteoporosis). Cartilage decreases, which causes osteoarthritis. Tissues become thin, which is called muscle atrophy.
- Integumentary System:
Changes:
The skin becomes thin, dry and less elastic. Collagen and elastin decrease. Hair turns white and hair also decreases due to the decrease in the number of follicles.
- Immune System:
Changes:
The activity of T-cells and B-cells decreases, due to which the body does not get protection from viruses and bacteria. Transmission of diseases increases and feedback on vaccination is also less.
In old age, gradual changes occur in every system of the human body, which is a part of the normal aging process. However, the effects of these changes can be minimized with proper diet, physical activity, regular medical checkups and a healthy lifestyle.
nursing care of old age people:
1) Promotion of Self Respect and Dignity:-
Some institutes or groups usually have some restrictions on personal choices and independence.
The feelings and emotions of the elderly should be respected.
While the staff makes positive efforts to develop good relationships with the patients and gain their personal respect and friendship.
By developing good relationships, the group can be controlled and difficult situations can also be made easier.
2) Promotion of Comfort:
Relaxation is necessary for physical and mental comfort. There are many factors that contribute to the comfort of the elderly such as skin care, care of bone structure, maintenance of temperature and fluid balance.
3) Safety:-
Provide unpolished floors, good lighting, proper bed height, proper walking aids
4) Daily Living Activities:-
Encourage the patient to do as much daily activity as possible so that complications like dehydration, thrombosis, pressure sores, contractures, etc. can be avoided.
5) Promotion of independence:-
Encourage the patient to take self-care as much as possible and ask him to make his own decisions.
6) Encourage mobility and movement
7) Ask him to take necessary medicines and provide sufficient knowledge about those medicines such as side effects of the medicine, its use.
8) If the patient is in pain, do rehabilitation according to his condition.
Additional Information:-
Skin care:-
Use mild soap
Bath once or twice a week
Hair care and brushing every day
Use moisturizers
Keep nails short
Use sunscreen, hat, long-sleeved clothes
Stay away from things like hot water bottles.
Pay enough attention to footwear so that sores do not occur
Avoid sun stroke
Supporting Changes in Bones and Joints:-
Do light exercise
Take precautions to avoid falls
Precautions
Give a balanced diet including calcium and vitamin D supplements
Monitor the patient for pain and treat as needed
Give the patient more time as it may take them longer to function.
Supporting Changes in Vision:-
Proper lighting should be provided to the patient
If necessary, help the patient in choosing clothes
Use natural tear products.
Contact the patient directly.
Supporting Changes to Hearing:-
Keep the volume down while talking.
Put yourself in the patient’s shoes so that you can understand the patient’s needs
Make sure that the person’s attention is on you before speaking.
Get checked by a doctor and if necessary, get the wax (mail) removed
Arrange a hearing assessment and if necessary, provide hearing aid.
5.Supporting Changes in Smell and Taste:-
Attractive meals should be prepared in which food with good smell should be prepared.
Spoiled food should not be given to eat
6.Supporting Changes in the Cardiovascular System:-
People get tired more easily due to cardiovascular changes, so they should be given more rest.
Regular blood pressure monitoring should be done as per the advice of healthcare professionals
If the person is unable to move on his own, he should be made to change positions frequently
Ask him to take adequate fluids and if dehydration is noticed in the patient, seek immediate medical help.
7.Supporting Changes in the Respiratory System:-
Short-term activities should be planned
More time is needed for rest.
If the person is unable to move on his own, then he should be made to change positions frequently
If the person has persistent cough during or after meals, then ask him to consult a doctor
Keep the body alignment and position proper
Stay away from polluted air
Give oxygen therapy if necessary
8.Digestive Care:-
Maintain oral hygiene
Take appropriate treatment if there is tooth damage
Provide a comfortable environment for eating
High fiber, high protein food with different tastes and textures should be given.
Advise to drink more fluids
Give calcium and vitamin D supplements to prevent osteoporosis
9.Supporting Changes in Elimination:–
Maintain daily activities
Plan for the bathroom when going out
Reduce caffeine intake
Increase fiber intake
Do light exercise
Provide emotional support.
Everything should be given as needed.
- Urinary Care:-
Increase fluid intake
Drink less fluid before bedtime
Wear clothes that can be easily removed
Use absorbent pads
- Elderly care at home:-
If there is a wound, take care of it and get it dressed regularly
Monitor vital signs and give medicine on time.
Manage any pain or discomfort the patient may experience
Help with daily hygiene needs.
c) Define appendicitis. Write down clinical manifestations & nursing management for appendicitis
Appendicitis:
(Appendix: The appendix is a small finger-like structure located near the beginning of the large intestine)
Appendicitis is the infection and inflammation of the vermiform appendix.
Appendicitis is an emergency condition. Appendicitis requires immediate abdominal surgery.
Appendicitis causes signs and symptoms such as abdominal pain, vomiting, discomfort, nausea, and fever.
Etiology/cause of the Appendicitis:
Obstruction in the lumen of the appendix.
Bacterial infection.
Parasitic infection.
Inflammatory bowel disease.
Crohn’s disease.
Ulcerative colitis.
Trauma to the abdomen.
Fungal infection.
Environmental factors.
Genetic factors.
Trauma.
Clinical manifestation/sign and symptoms of the Appendicitis.
Right lower quadrant abdominal pain.
Pain in the periumbilical region.
Low grade fever.
Severe abdominal pain.
Decreased appetite.
Nausea.
Vomiting.
Pain at McBurney’s point.
Local tenderness.
Rebound tenderness present.
Abdominal swelling.
Pain while passing urine.
Early signs of Appendicitis:
Guarding sign:
Abdominal muscles tense and tighten when a health care professional palpates the lower abdominal area.
Rebound tenderness:
When a healthcare professional palpates the abdominal area with his hand and then releases the hand, the patient still experiences abdominal pain and tenderness, this is called rebound tenderness.
Rowsing sign:
In the Rowsing sign, when a healthcare professional palpates the left lower abdominal side of the patient with his hand and releases the pressure of the hand and the patient feels pain in the right lower abdominal site, it indicates the presence of the Rowsing sign.
Saus sign:
Saus muscles are located near the appendix in the pelvic cavity. These sausage muscles create abdominal pain when there is infection and inflammation in the appendix. In Saus sign, the patient is asked to lie on the left side. Then the hip of the patient’s right foot is extended to the right hand side. If the patient feels pain, then it indicates Saus sign.
Obturator sign:
In this test, the patient is made to lie down in the supine position. Then internal rotation of the right hip joint is done and if the patient feels pain on the right iliac fossa, then it indicates obturator sign.
Aaron’s Sign:
In Aaron’s sign, when firm pressure is applied to the continuous Mc Burney’s point, if pain is felt in the epigastric region, it indicates the condition of chronic appendicitis.
Blumberg’s Sign:
In Blumberg’s Sign, pressure is applied slowly on the abdominal wall, then the pressure is released rapidly and if the patient feels pain while releasing the pressure, it indicates a positive Blumberg’s sign.
Nursing management:
Nursing assessment
Assess the patient for signs and symptoms of abdominal tenderness, anorexia, nausea, vomiting, temperature increase.
Assess the patient for rebound tenderness sign or not.
Assess the patient for signs of roving.
Assess the patient for any other complications.
Nursing diagnosis:
1)Acute pain related to disease condition.
2)imbalance nutritional status less than body requirement related to nausea and vomiting.
3)Impaired skin integrity related to fluid and electrolyte imbalance.
4)Risk for fluid volume deficit related to excessive amount of fluid loss from the body.
5)Risk for infection related to the disease condition.
Nursing interventions:
1)Reliving pain of the patient.
2)maintain nutritional status of the patient.
3)maintain skin integrity of the patient.
4)preventing fluid volume deficit.
5)Reduce the risk of infection .
Preoperative and Postoperative Nursing Management:
Preoperative Nursing Management:
Take the consent of the patient and his family members before performing the surgery.
Keep the patient on an empty stomach and do not provide anything by mouth.
Maintain the patient’s hydration status by administering intravenous fluids.
Administer antibiotic medicine to prevent infection.
Monitor the patient’s bowel sounds.
Assess the patient’s pain level.
Provide analgesic medicine to relieve the patient’s pain.
To perform proper laboratory investigations of the patient such as,
Blood investigation,
Complete blood count,
Abdominal ultrasonography,
Urinalysis,
Abdominal x ray,
Abdominal ct scan etc. to perform tests.
To properly prepare the area of the surgical site.
Maintain the patient’s fluid and electrolyte balance.
Post operative nursing management:
To receive the patient comfortably in the recovery room.
To monitor the patient’s vital signs properly.
To monitor the patient’s operative site properly.
To assess the patient for any bleeding and suturing on the operative side.
To monitor the patient’s intake output chart.
To advise the patient on deep breathing techniques.
To auscultate the patient’s bowel sounds.
To provide analgesic medicine to the patient.
To provide antibiotic medicine to the patient.
To provide antiemetic medicine to the patient.
Provide intravenous fluids to the patient
Provide the patient with a side lying position after the operation to prevent aspiration of secretions.
Place the patient on an oral feeding tube after the operation.
Provide feeding through a nasogastric tube to the patient.
Provide oxygen to the patient until the anesthesia wears off.
Dress the patient’s operative side using proper sterile technique.
Provide skin care to the patient.
Advise the patient to walk moderately.
Assess the patient for any signs and symptoms of infection.
Involve the patient in daily routine activities.
Advise the patient to maintain personal hygiene.
Provide psychological support to the patient.
Advise the patient to take medication regularly.
Advise the patient to have regular follow-up.
Q-4 Write short notes. 12
a) Gout
Gout :-
Definition:–
Gout is a recurrent attack of inflammatory arthritis. In which the joints are red, swollen, hot. Which is seen due to the increase in uric acid in the blood. Uric acid crystals are deposited in the joints, tendons and surrounding tissues.
Etiology:-
Genetic causes of medullary cystic kidney disease
After surgery
Diabetes mellitus
Hyperlipidemia
Metabolic syndrome
Hemolytic anemia
Hypertension
Chemotherapeutic drugs
Taking immunosuppressive drugs
Renal disease
Use of diuretic drugs
Clinical Manifestation:-
Inflammatory arthritis in which the part is red, swollen, hot is seen mainly on the big toe, in which it is seen in the metatarsal phalangeal
Joint pain is accompanied by fatigue and fever
Tophy is seen
Hyperuricemia
Diagnostic test:-
In blood test. Uric acid is found above 6mg/dl
X-ray joint
E. SR
Kidney function test
Electrolyte
Blood count
Treatment:- acute gout
NSAIDS along with calcitriol & steroids are given.
Dental:- Ibuprofen.
Drugs like allopurinol and febuxostate are given to reduce uric acid levels
Steroids are given in the joint for swelling.
- Manage pain of patient.:
Elevate the affected joint and give it a comfortable position
Give medicines as per doctor’s order
Immobilize the affected joint
Use a bed cradle or footboard to prevent the weight of the bedclothes
Keep checking the patient’s activity and disability
- Explain to the patient about diet precautions, including taking 2-3 liters of fluid per day
- Explain to the patient to stay away from alcohol
- Give the patient necessary instructions for a healthy lifestyle
- Explain to take a proper balanced diet
- Explain the importance of rest and exercise
b) Anesthesia
Anesthesia is a group of chemical agents that cause partial or complete loss of sensation.
Purpose of Anaesthesia:-
To obtain patient cooperation.
To reduce or eliminate pain.
To keep the muscles of the body relaxed.
To perform the surgical procedure comfortably.
To remove sensation
To stop movement
There are three types of anesthesia.
1) Local anesthesia:-
This affects a limited area of the body (local part). It usually affects only the part of the body on which surgery is to be performed, which part needs to be numbed.
The following chemicals are used in local anesthesia.
Xylocaine Hydrochloride
Lignocaine Hydrochloride
Amethocaine Hydrochloride
Procaine Hydrochloride
2) Spinal Anesthesia :-
There are two types of this-
1)Epidural Anesthesia:- When the anesthesia is injected into the epidural part of the spinal cord, it is called epidural anesthesia.
2)Spinal Anesthesia:- When the anesthesia is injected into the subarachnoid space of the spinal cord, it is called spinal anesthesia.
Use of Spinal Anesthesia:-
Orchidectomy
Caesarean
Hernia Surgery
Hydrocele Surgery
Penis Surgery
Prostate Surgery etc..
Complication:-
Urinary Retention
Meningitis
CSF Leakage
Hypotension
Paralysis
Allergies, Headaches etc. …
3) General Anesthesia:- When there is a need to lose sensation in the whole body, the person is made unconscious. It is called General Anesthesia. General Anesthesia can be given as follows-
- Intravenously
- By Inhalation
By Intravenous:-
By I.V. Injection The following drugs are used in General Anesthesia.
Thiopental Sodium 2.5%
Hexabarbitone 10%
Methohexytal Sodium 1%
Propofol
Midazolam
Fentanyl
Ketamine Hydrochloride
Droperidol
Inhalation Anesthetics:-
This anesthesia is given through inhalation, which makes the patient unconscious.
Before administering this anesthesia, the patient is given some sedatives, then an endotracheal tube is inserted into the airway, and then it is given through inhalation.
The following drugs are used in this.
Sevoflurane
Nitrous oxide
Ether
Cyclopropane
Methoxyflurane
Enflurane
Penthrene
Responsibility of Nurse :-
The work of administering anesthesia is done by the anesthesiologist or anesthetist, but the nurse helps in it and the responsibility of the nurse is as follows.
First of all, the patient to be given anesthesia should be identified by asking the name
Take written consent.
The questions asked by the patient about anesthesia should be answered by the nurse properly so that the patient’s anxiety can be reduced.
Prepare the necessary equipment.
The nurse prepares the patient for anesthesia and provides gown, shoe cover, cap, etc.
Clean the area where anesthesia is given using aseptic technique.
Keep the necessary drugs for anesthesia in the right place.
Continuous observation of the patient during anesthesia.
Checking the patient’s vital signs.
Checking the patient’s level of consciousness.
The nurse should observe for complications due to anesthesia.
Preparing for surgery after administering anesthesia.
Maintaining records and reports.
Cleaning the anesthesia machine after administering anesthesia.
c) Lung abscess
Lung abscess:
In lung abscess, a pus-filled cavity is found in the lung parenchyma and inflammation and necrosis of the surrounding tissue is observed.
Etiology /causes of lung abscess:
Bacterial infection
Lung abscess is mostly seen due to bacterial infection. Streptococcus pneumoniae, Klebsiella pneumoniae, Staphylococcus aureus are seen due to bacteria.
Foreign body inhalation
Foreign body aspiration
Trauma
Tuberculosis
Chronic lung disease
Clinical manifestations/ Signs and symptoms of lung abscess:
Persistent cough
Blood in sputum
Foul smelling in sputum
Chest pain
Dyspnea
Shortness of breath
Fever
Chills
Weakness
Diaphoresis
Cynosis
Diagnostic evaluation of lung abscess:
History collection collection)
Physical examination
X ray
CT scan
M. R. I.
Sputum culture
Complete blood count
C-reactive protein
Erythrocyte sedimentation rate
Biopsy
Medical management of lung abscess:
Antibiotic therapy
Use broad-spectrum antibiotics (amoxicillin, clindamycin) to treat bacterial infections.
Oxygen therapy
Provide supplemental oxygen if needed.
Percutaneous drainage
If the abscess is large and antibiotics fail to treat it, drainage is necessary. Percutaneous drainage is done under CT scan.
Supportive care
Supportive care includes pain management, oxygen therapy, hydration levels, etc.
Treat underlying conditions
Treat underlying conditions associated with lung abscess.
Surgery
Pulmonary resection (lobectomy) in severe cases.
Nursing management of lung abscess:
Provide antibiotic medication to the patient as treatment.
Provide adequate nutritional support to the patient so that his immune system can be improved and weight can be gained.
Provide education and counseling to the patient about the condition. Explain infection control measures to the patient and his/her family members.
Provide proper antipyretic medication to maintain the patient’s body temperature and if the patient has a fever.
Provide antibiotic drugs to treat bacterial infections.
Provide expectorant drugs to help expel phlegm.
Provide nasal decongestants to relieve congestion.
Provide adequate rest and plenty of fluid intake.
Avoid contact with irritants.
Conduct proper and complete assessment of the patient.
Properly assess the patient’s respiratory status.
Completely assess the patient’s vital signs.
Properly assess the patient’s oxygen saturation.
Continuously monitor the patient’s respiratory status and oxygen saturation to properly assess the patient’s condition.
Continuously monitor the patient’s body temperature.
Advise the patient to maintain hydration status and continuous fluid intake to thin mucus.
Provide the patient with a properly comfortable position.
Provide adequate oxygen to maintain the patient’s body oxygen saturation and provide respiratory support.
Provide the patient with properly prescribed medication.
Provide complete education to the patient and his/her family members about the patient’s condition, its causes, its symptoms and signs, and its treatment.
Provide the patient with proper care and a comfortable environment.
d) Benign prostatic hypertrophy.
1.Definition
Benign Prostatic Hypertrophy (BPH) is a non-cancerous condition in which the prostate gland increases in size. This condition is mainly seen in old age and is common in men.
2.Causes
Age-related hormonal changes
Androgen-Estrogen Imbalance
Excessive production of dihydrotestosterone from testosterone
Family History
3.Symptoms
Frequent Urination
Nocturia – getting up frequently at night to urinate
Urine Hesitancy
Weak Urine Stream Stream
Incomplete Bladder Emptying
Urinary Retention
- Complications
Recurrent Urinary Tract Infections
Bladder Stones
Acute Urinary Retention
Kidney Damage if left untreated for a long time
- Diagnosis
Digital Rectal Exam
PSA Level Test Tests
Urine Flow Study
Ultrasound
Cystoscopy if necessary
6.Treatment
A. Medical Treatment
Alpha Blockers – such as Tamsulosin
5-alpha Reductase Inhibitors – such as Finasteride
B. Surgical Treatment
TURP (Transurethral Resection of Prostate) – most Common Procedures
Laser Therapy
Prostatectomy – When there is a large prostate
- Lifestyle Modifications
Avoid drinking too much fluid at night.
Avoid caffeine and alcohol.
Do not hold urine.
Urinate regularly.
Increase physical activity.
- Pathophysiology
In BPH, the size of the prostate gland gradually increases. It presses on the urethra, which reduces urine flow. The bladder forces urine with increased pressure and over time, the bladder muscles also weaken, resulting in a decrease in the ability to hold and release urine.
Benign Prostatic Hypertrophy (BPH) is a very common condition in older men, but can become serious if not treated properly. It can be successfully treated with timely diagnosis, appropriate medication, and surgery if needed.
Q-5 Define following (any six) 12
a) Anaphylaxis
When the human body is exposed to any antigen, an immediate allergic reaction starts in the human body and it provides a hyperactive immune response and within a minute the allergic reaction starts and signs and symptoms are seen in the body, which is called anaphylaxis.
C)Guillain-Barré Syndrome
Guillain-Barré Syndrome (GBS) is a rare autoimmune neurological disorder in which the body’s immune system attacks its own peripheral nervous system. As a result, the myelin sheath of the nerves is damaged, which slows or obstructs nerve signal transmission. The condition begins suddenly and progresses rapidly. It begins with weakness and loss of sensation in the legs and can spread to the arms, face, or breathing. Guillain-Barré Syndrome often occurs after a viral or bacterial infection and can also cause temporary paralysis. However, in most cases, with appropriate medical intervention, the patient gradually recovers.
b) Homeostasis
Homeostasis is a physiological process in which the body keeps its internal environment stable and balanced. This process is controlled by the nervous system and the endocrine system, which use receptors, control centers, and effectors to maintain parameters such as temperature, blood pressure, pH level, and glucose level. When these parameters change, the body responds by producing a homeostatic response to maintain normal physiological functions.
d) Pneumonia
Pneumonia is an infection and inflammation of the lung parenchyma (alveoli) caused by bacterial, viral or fungal infection. In this, the air sacs fill with fluid or pus and become solid. The alveoli normally function to exchange gases, but in the condition of pneumonia, due to infection and inflammation and accumulation of pus, gas exchange is interfered with.
E) Epilepsy
If the patient experiences repeated episodes of seizures, the condition converts to epilepsy. Epilepsy is a mental abnormality in which the electrical impulses of neurons in a person’s brain are severely disturbed, due to which abnormal electrical activity is seen in the neurons and the condition of epilepsy occurs, due to which jerking movements arise in the body.
g) Nursing process
Nursing process was introduced by HALL in 1955. This is a systemic decision making process. In which the problem is solved through the steps of assessment, nursing diagnosis, planning implementation, evaluation. This is a continuous process. The health status and health problem of the patient are assessed from time to time. And the nursing care is modified based on the feedback or evaluation received from it. Thus, the nursing process is a continuous cycle. The steps shown above are interrelated and interdependent with each other.
h) Epididymo orchitis
Epididymo Orchitis is an inflammatory condition affecting the male reproductive system, in which the epididymis and testis simultaneously become inflamed. This condition is usually caused by a bacterial infection or viral infection and is characterized by pain, swelling, redness, and scrotal tenderness. Conditions such as urinary tract infections or sexually transmitted infections can also be responsible for this inflammation.
F) Emphysema
Emphysema is a Greek word meaning ‘inflation’. Emphysema is a chronic lung disease. In which there is over-distension and over-inflation of the air sacs (alveoli) of the terminal bronchioles in the lungs and the air sacs are gradually damaged. Due to which shortness of breath is seen. Emphysema is also known as ‘Pink puffer’.
Due to some reason, hyperinflation occurs in the alveoli. Due to which destruction is seen in the wall of the alveolar capillary. Due to this, the elasticity of the alveoli is lost. In addition, the gas exchange capacity of the alveoli is lost. Air is trapped in the alveoli. The condition of emphysema is seen.
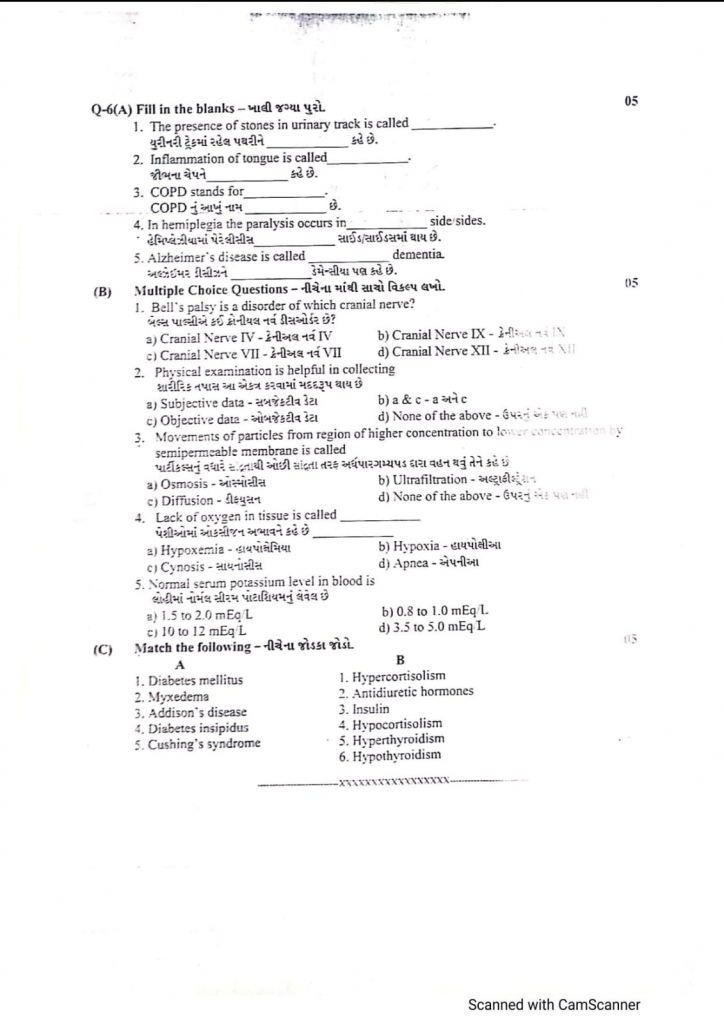
Q-6(A) Fill in the blanks .05
1.The presence of stones in urinary track is called ………(Urolithiasis)
2.Inflammation of tongue is called………. (Glossitis)
3.COPD stands for……… Chronic Obstructive Pulmonary Disease
4.In hemiplegia the paralysis occurs in………. side sides. (Single Side)
5.Alzheimer’s disease is called………. dementia (Senile Dementia)
(B) Multiple Choice Questions- 05
1.Bell’s palsy is a disorder of which cranial nerve? Bell’s palsy is a disorder of which cranial nerve?
a) Cranial Nerve IV
b) Cranial Nerve IX
c) Cranial Nerve VII
d) Cranial Nerve XII
2.Physical examination is helpful in collecting
aj Subjective data
b) a&c
c) Objective data
d) None of the above
3.Movements of particles from region of higher concentration to lower concentration by semipermeable membrane is called
a) Osmosis
b) Ultrafiltration
c) Diffusion
d) None of the above
4.Lack of oxygen in tissue is called Oxygen deficiency is called
а) Нурохеміа-
b) Hypoxia –
c) Cynosis –
d) Apnea –
5.Normal serum potassium level in blood is
a) 1.5 to 2.0 mEq/L
b) 0.8 to 1.0 mEq/L.
c) 10 to 12 mEq L
d) 3.5 to 5.0 mEq L
(C) Match the following – 05
- Diabetes mellitus–1.Hypercortisolism
- Myxedema–2. Antidiuretic hormones
- Addison’s disease–3.Insulin
- Diabetes insipidus– 4.Hypocortisolism
- Cushing’s syndrome–5.Hyperthyroidism
