ENGLISH-CHILD HEALTH NURSING (GNM 2ND YEAR) 12/12/2024(Done)-UPLOAD

CHILD HEALTH NURSING (GNM 2ND YEAR) 12/12/2024
Q-1 a) What is diarrhea? What are the causes of diarrhea in children? 03 What is diarrhea? Explain the causes of diarrhea in children.03
Diarrhea is a condition in which liquid, loose and watery stools are passed more than three times a day (in 24 hours). And the frequency of these loose, watery stools is also high. Due to diarrhea, excessive amounts of fluid and electrolytes are lost from the body, which leads to the condition of dehydration.
{Diarrhea is a disease in which passage of loose, liquid or watery stool more than three times per day}.
types of the Diarrhea:
There are four main types of diarrhea.
1) Acute Diarrhea
2) Chronic Diarrhea
3) Persistent Diarrhea
4) Dysentery
1) Acute Diarrhea: Acute diarrhea is a condition in which the onset of diarrhea is sudden and of short duration and lasts for two It lasts for less than a week. Acute diarrhea is mainly caused by any infection.
2) Chronic Diarrhea: Chronic diarrhea is a condition in which loose watery stools are present for more than 3 weeks, it is called chronic diarrhea. Chronic diarrhea is due to any organic disease.
3) Persistent Diarrhea: Persistent diarrhea is a condition in which attacks of acute diarrhea are seen for more than two weeks and that diarrhea is caused by infection.
4) Dysentery
1) Acute Diarrhea: Acute diarrhea is a condition in which the onset of diarrhea is sudden and of short duration and lasts for less than two weeks. Acute diarrhea is mainly caused by any infection.
2) Chronic Diarrhea: Chronic diarrhea is a condition in which loose watery stools persist for more than 3 weeks and is called chronic diarrhea. Chronic diarrhea is caused by any organic disease.
3) Persistent Diarrhea: Persistent diarrhea is a condition in which attacks of acute diarrhea are observed for more than two weeks and that diarrhea is caused by an infection.
4) Dysentery: Dysentery is a condition in which blood, mucus and pus are present in the stool and it is accompanied by abdominal colic, fever, and tenesmus (this is a condition in which there is a need to pass stool even though the bowel is already empty.).
Etiology/ cause of the Diarrhea. (Causes of diarrhea):
Due to unhygienic conditions.
Due to infection.
Viral infection:
- Rota virus,
- Enterovirus,
- Due to adenovirus,
- Due to measles virus.
- Due to influenza virus.
Bacterial infection:
- E coli,
- Shigella bacteria Due to,
- Salmonella bacteria.
- Staphylococcus bacteria.
- Vibrio cholerae.
Parasitic infections:
- Entamoeba histolytica,
- Giardia lamblia,
- Cryptosporidium,
- P. falciparum, P. vivax, P. ovale and P. malariae.
Fungal infection:
- Caused by Candida albicans,
- Infectious Condition
- Upper Respiratory Tract Infection,
- Otitis Media,
- Tonsillitis,
- Pneumonia,
Urinary Tract Infection.
Dietic and nutritional factors:
- Overfeeding,
- Due to starvation,
- Due to food allergies and food poisoning.
- Due to other predisposing conditions
such as,
Age,
Season,
Artificial feeding
b) Write clinical manifestations & stages of dehydration in children. 04
Introduction:
Dehydration is a pathophysiological condition in which the loss of fluid and electrolytes from the patient’s body results in a fluid volume deficit. The most common causes in child patients may be acute diarrhea, vomiting, fever, or excessive perspiration due to heat. Dehydration can be life-threatening if proper medical intervention is not done.
Clinical Manifestations of Dehydration in Children:
The severity of dehydration in a child patient depends on the patient’s age, the amount of internal fluid loss, and electrolyte imbalance. The following symptoms are commonly seen:
1. Dry Mucous Membranes
2. Sunken Eyes
3. Decreased Skin Turgor and Positive Late Test
4. Absence of Tears
5. Patient’s Urine Output Decreased Urine Output or Oliguria
6. Increased Pulse Rate and Weak Pulse
7. Increased Capillary Refill Time
8. Patient appears lethargic or irritable
9. Palpation of the fontanel in a pediatric patient may cause depression
10. Skin feels dry and cold
Stages of Dehydration:
Dehydration is classified into three stages according to severity:
1. Mild Dehydration:
Fluid loss is about 3 to 5 percent of body weight. The patient is usually alert. The mouth may be dry and slightly thirsty.
2. Moderate Dehydration:
6 to 9 percent body weight loss Patient is tired and irritable Eyes go inward Skin turgor is delayed Conjunctiva feels dry Urine output decreases Pulse feels rapid and weak
3. Severe Dehydration:
Body weight loss ≥ 10 percent Patient is lethargic or semiconscious with alteration in level of consciousness Both the eyes and fontanelles may be deeply depressed, the pulse may be weak and fast, the blood pressure may be low, the skin may be cold, clammy and tinted, the capillary refill time may be ≥ 3 seconds, and a state of shock may develop.
In children, prompt assessment and stage-specific treatment of dehydration is essential. It is essential to identify the symptoms and provide appropriate rehydration therapy according to the stage so that the patient’s health can be stabilized. Special attention should be paid to young children because they lose fluid rapidly and can quickly lead to severe dehydration.
c) Explain nursing management of diarrhea. Explain nursing management of diarrhea. 05
- Provide rehydration therapy to the child.
- Provide oral rehydration solution (ORS) to maintain the child’s hydration status.
- Oral rehydration therapy is considered an effective treatment for mild to moderate dehydration.
- Provide intravenous fluid therapy to the child.
- If the child has a condition of dehydration and ORS therapy is not properly effective, provide intravenous fluid therapy to the child.
- Provide proper feeding to the child along with intravenous therapy to prevent malnutrition.
- Provide easily digestible food to the child who can take food by mouth.
- Ex: Toast, rice, blanched food.
- Maintain adequate fluid and electrolyte levels of the child.
- If the child has diarrheal disease due to any bacterial infection, provide antibiotic medicine.
- Provide antidiarrheal medicine to the child, such as,
Loperamide,
Bismuth Subsalysilate. - Properly assess the child.
- Assess the severity of the diarrheal disease.
- Assess the frequency, volume and consistency of diarrhea.
- Assess the child for any symptoms of dehydration.
- Maintain proper fluid and electrolyte levels of the child.
- Provide oral rehydration solution to maintain the child’s hydration status.
- Provide intravenous fluid therapy if the child is severely dehydrated.
- Provide proper nutritional support to the child.
- Provide continuous breast feeding to the child.
- If the child can take food by mouth, provide easily digestible food to the child.
- Provide proper medication to the child.
- If the child has diarrhea due to any bacterial infection, provide antibiotic medication.
- If the child has any parasitic infection, provide antiparasitic medicine.
- Advise the child to practice proper hand hygiene techniques to prevent any kind of infection.
- Continuously monitor the child.
- Provide education to the child’s parents or handle safe water and food to prevent the condition of diarrhea.
- Advise the child’s parents to provide regular medication to the child.
- Prevention care of the Diarrhea:
- Advise the parents to provide adequate breast feeding to the child.
- Advise the child’s parents to maintain proper hand hygiene.
- Advise the child’s parents to properly prepare safe water and food in a hygienic manner.
- Provide proper hygienic bottle fitting to the child.
- Advise the child’s parents not to use any kind of pacifier.
- Advise the child’s parents to maintain strict personal hygiene.
- Advise the child to keep the child’s nails short and advise the child to keep the child’s hands and toys clean at all times.
- Provide adequate fluids to the child.
- Provide education to the parents to provide easily digestible food such as rice, dal, soup, coconut water to the child.
- Advise parents to provide homemade ORS solution to the child if necessary.
- Advise parents to provide regular medication to the child.
OR
a) What is meningitis? What is meningitis? 03
Meninges: The meninges are the protective membranes that cover the brain and spinal cord. These meninges are made up of three layers. 1) Duramater
(Outermost layer) 2) Arachnoid mater (Intermediate layer) 3) Pia mater (Innermost layer)So, there are three layers of meninges that cover and protect the brain and spinal cord.
Meningitis: When there is infection and inflammation in the meninges layer surrounding the brain and spinal cord, the condition is called meningitis. This infection can be caused by bacteria, viruses, and microorganisms.
b) Write down clinical manifestations of meningitis. 04
Headache,
Very high fever,
Maintenance status altered. Confusion.
Altered consciousness.
Vomiting.
Photophobia (an inability to tolerate light).
Irritability.
Drowsiness.
Confusion Occur.
Altered consciousness.
Vomiting.
Sign of meningeal irritation.
Knuckle rigidity (neck stiffness).
Headache.
Altered mental status To be.
To be surprised.
To have joint pain.
To have muscles.
Positive Brudzinski sign:
In Brudzinski sign, when the child is provided with a supine position and his neck is flexed towards the chest, his hip and ankle automatically flex, which is called Brudzinski sign. is.
Kerning sign:
In the Kerning sign, when the patient is provided with a supine position, after which the knee and hip of the patient are flexed, if the patient feels pain when the knee is extended again, it is called Kerning sign.
K:= Knee,
E:= Extention
R:= Resistense That is, the patient feels pain when the knee is directly extended.
e) Explain the nursing management of meningitis. Explain the nursing management of meningitis.05
Properly assess the child.
Continuously monitor the child’s vital signs.
Properly assess the child’s hydration status.
Maintain the child’s proper fluid and electrolyte levels.
Provide analgesic medicine if the child is in pain. To do.
Properly assess the child’s neurological status.
Provide anticonvulsant medicine if the child is having seizures.
Provide proper nutritional support to the child.
Provide proper psychological support to the child.
Educate the child about the disease, its causes, and its symptoms and Provide proper education about the signs.
Continuously monitor the child’s intake output.
Continuously monitor the child’s vital signs and neurological status.
Continuously monitor the child’s level of consciousness.
Advise the child to take medicine regularly.
Advise the child to follow up regularly.
Provide proper psychological support to the child.
Q-2 a)What is exclusive breast feeding? Explain physiology of lactation. What is exclusive breast feeding? Explain Physiology of Lactation 08
Exclusive Breast Feeding:
Exclusive Breast Feeding is a process in which a patient feeds her newborn infant only breast milk from birth to six months of age and during this period no formula, water, juice, solid food or other liquids are given — except when medically indicated, such as oral rehydration solution (ORS), medicines or essential vitamins.
This practice is very important for the immunity, nutrition, and organ development of the infant and also reduces the risk of uterine recovery and breast or ovarian cancer in the patient.
According to WHO and UNICEF, exclusive breastfeeding is recommended for at least 6 months from birth.
Lactation is the process of milk production. After the birth of the child, the mother provides complete nutrition to the child through breastfeeding. The physiology of lactation can be described as follows.
The mother’s breast tissue is made up of lobes and lobules. The lobules contain tiny alveoli and ducts. These tiny alveoli are connected to the lactiferous ducts, which open into the areola.
Each nipple has approximately 20 lactiferous duct openings.
During the second and third trimesters of the mother’s pregnancy, these alveoli secrete the milk colostrum.
After the baby is delivered, the placenta is removed and the levels of estrogen and progesterone decrease. Along with this, the levels of the prolactin hormone increase. These changes start the process of lactation. Which is responsible for the secretion of milk from the breast tissue.
In addition, the main basis of the secretion of milk from the breast is the mechanical stimulation caused by the baby sucking the mother’s breast.
In the process of milk secretion, two reflexes are mainly important, which are as follows.
- Milk producing reflex.
When the baby feeds on the mother’s breast, he shakes and due to this shaking action, the nerve endings in the areola of the mother’s breast are stimulated and it gives impulses to the hypothalamus. These impulses from the hypothalamus reach the anterior pituitary gland and the anterior pituitary gland increases the secretion of prolactin hormone in the blood. Thus, due to the increase in the secretion of prolactin hormone, more milk is produced by the breast tissue. As the baby sucks more, more prolactin hormone is produced and more milk is secreted. - Milk ejection reflex.
This is also called the let-down reflex.
When the baby sucks, the nerve endings in the breast stimulate the posterior pituitary gland through the hypothalamus, which secretes more oxytocin hormone. This oxytocin hormone contracts the myoepithelial cells surrounding the alveoli inside the breast and compresses the alveoli. Due to which the milk comes through the lactiferous duct and reaches the areola of the nipple. In this way, milk is ejected from the duct. Both the above reflexes are stimulated by the baby sucking the mother’s breast and the process of lactation is maintained…
b) Write down advantages of play in children. 04
Introduction:
Play is not just a means of passing time for children, but it is a natural therapeutic medium for physical, mental, social and emotional growth. Different types of games, depending on the child’s developmental stage, help develop physical health, brain stimulation, communication skills, and cognitive functions. Play is extremely important for medical, psychological and neurological health.
Main Advantages of Play in Children:
Physical Development:
During play, a child’s gross motor skills such as running, jumping, climbing, etc. become stronger. The musculoskeletal system is strengthened and coordination and balance are developed.
Sensory Development:
Various games simulate the patient’s human senses such as visual, auditory, tactile, etc., due to which perception and sensory integration improve.
Cognitive Development:
During play, the patient develops observation, memory, focus, problem-solving and decision-making skills. Creative thinking and imagination also become more active.
Social Development:
Interpersonal skills such as cooperation, harmony, sharing and fair play develop in the patient through group play. Social role playing helps the patient to understand social structures.
Emotional Development:
Play helps the patient to express their emotions, release frustrations, and reduce stress. This increases emotional resilience and self-esteem.
Language Development:
During play, patients learn new words, practice verbal communication, and develop language fluency.
Personality Development:
Play helps patients develop self-expression and leadership skills. Personal skills such as leadership, confidence, and adjustment ability develop.
Health Maintenance:
Physical activity provides protection against non-communicable diseases like obesity and diabetes in patients. Play also boosts cardiovascular health.
Behavioral Modulation:
Play develops discipline, rule-following, and frustration tolerance in the patient, which is also helpful in later life.
Therapeutic Value:
Other patients such as autism, ADHD (Attention Deficit Hyperactivity Disorder), and developmental Play acts as an effective therapy for patients with developmental delays.
Play is not just entertainment for a child, but also a source of all-round development. Play Therapy in Pediatric Nursing is an indispensable component for the positive health of the patient. Through play, the child becomes physically, mentally and emotionally well-equipped and his life can become healthier and happier.
OR
a) What is hydrocephalus? Write down nursing management of hydrocephalus. What is hydrocephalus? Write down nursing management of hydrocephalus. 08
Hydrocephalus is a Greek word derived from hydro meaning “water” and cephalus meaning “head” . Hydrocephalus is an abnormal condition in which there is an abnormal accumulation of cerebrospinal fluid in the ventricular system and subarachnoid space. This causes an increase in pressure inside the skull.
The condition of hydrocephalus is usually caused by an imbalance in the production and absorption of cerebrospinal fluid due to obstruction in the CSF pathway. This results in dilation of the cerebral ventricles, enlargement of the head, cognitive impairment, seizures and other neurological problems.
Preoperative Nursing Management
- Properly and continuously assess the child, including assessing baseline health status, vital signs, neurological status and hydration status of the child.
- Continuously monitor the child’s intracranial pressure To do.
- Continuously measure the child’s head circumference.
- Palpate the child’s fontanelles to assess for any increased intracranial pressure.
- Assess the child’s pupillary response and level of consciousness.
- Continuously monitor the child’s vital signs.
- Provide the child with proper care and a quiet environment.
- Maintain aseptic technique while handling the child to prevent nosocomial infections.
- Continuously change the child’s position.
- Properly maintain the child’s nutritional status.
- Properly provide intravenous fluids to the child. To do.
- Keep the child on Nil Per Oral.
- Continuously monitor the child’s intake output chart.
- Properly collaborate with other health care personnel for proper care of the child.
- Surgery is a stressful condition for the child and his family members, so provide proper education about it to the child’s parents and provide them with psychological support. To do.
- Provide proper assurance and emotional support to the child’s parents.
Post-operative Management
- Continuously and closely monitor the child after surgery.
- Frequently monitor the child’s vital signs every fifteen to twenty minutes.
- Properly monitor the child’s neurological status.
- Frequently monitor the child’s body temperature if there is an alteration.
- Provide the child with a non-operative position to prevent pressure on the shunt.
- Provide the child with a flat position on the bed for 24 hours after surgery.
- Assess the child’s photos and notify immediately if depressed.
- Provide analgesic medication to relieve pain if the child is in pain.
- The child Assess for any complications after surgery.
- Provide the child with proper fluids and maintain their hydration status. Continuously monitor the child’s intake output chart. And continuously maintain the electrolyte level of the child.
- Provide dressing to the child by maintaining proper aseptic technique on the surgical side.
- Provide proper support and education to the child and his family members.
b) Describe about prevention of child labour. Explain about prevention of child labour. 04
Introduction:
Child Labour is a situation in which children below the age of 14 are employed in physically or mentally harmful work. This has a serious impact on their physical development, mental health and education. Comprehensive efforts are required at various levels to eliminate this problem.
1. Promotion and Accessibility of Education:
Education is the most powerful tool for the prevention of child labour. Providing quality education can keep children out of the labor market. It is necessary to enroll children in schools and ensure their attendance through government schemes such as Sarva Shiksha Abhiyan and Mid-Day Meal Scheme.
2.Legal Enforcement and Implementation:
In India, it is a legal offence to employ children below the age of 14 in any hazardous work as per the Child Labour Prohibition and Regulation Act. Child labour can be prevented through strict implementation of this law and effective enforcement of its provisions.
3. Economic Assistance and Support for Families:
In many cases, the economic backwardness of the family is the main reason for putting a child to work. For this, the government and NGOs can help families by providing financial assistance, nutritional support and employment opportunities, so that they do not employ children.
4. Public Awareness Campaigns:
It is important to create awareness among the people in the society that child labor is not only a violation of social justice, but also has a bad effect on the physical and mental health of children. For this, the cooperation of medical professionals, teachers and social workers is essential.
5. Family Guidance and Counseling:
Many parents employ their children without understanding their future. In such a situation, if they are educated about counseling, parental education and life values, they can also stay away from child labor.
Child labor is not only a hindrance to education, but also has a serious impact on the overall health of children. To prevent it, organized efforts are required at the social, economic and medical levels. Every child has the right to – health, education. Therefore, every section of society is obliged to play a serious role in this direction.
Q-3 Write short answer (any two) Write a short answer. (Any two ) 6+6-12
a) Write nursing management of convulsion. Write the nursing management of convulsions in children.
Heading: Nursing Care of the Patient During and After Convulsion
Introduction:
A Convulsion is an uncontrolled and sudden muscle contraction caused by a disorder of the nervous system. This condition is especially seen in epilepsy, febrile seizures caused by fever, trauma, hypoglycemia, etc. Immediate and proper nursing care of a patient with convulsions can save him from a life-threatening condition.
1. Emergency Response and Safety Measures:
Immediately place the patient in a flat position and remove harmful objects from the area.
Turn the patient on his side so that saliva or vomitus from the mouth can drain and aspiration does not occur.
Avoid putting anything in the patient’s mouth — try not to put anything between the teeth while trying to prevent a tongue bite.
Provide a comfortable and safe environment for the patient.
2. Airway Management:
Lateral position is essential to keep the patient’s airway open.
Remove phlegm or secretions with oral suction.
Give oxygen therapy if the patient has cyanosis.
3. Vital Signs Monitoring:
Regularly check pulse, blood pressure, respiratory rate, and temperature.
Keep a note of how long the seizure lasts — prolonged seizure indicates status epilepticus.
4. Medication Management:
Administer anticonvulsants such as Lorazepam, Diazepam or Phenytoin as ordered by the doctor.
Adhere to the correct dose and route of administration (Oral/IV/IM).
Closely observe for drug side effects and allergic reactions.
5. Neurological Assessment:
Assess the patient’s level of consciousness such as GCS score (Glasgow Coma Scale).
Check the pupil response.
Observe the post-ictal state – the patient may appear tired, confused or sleepy.
6. Hydration and Nutrition Management Management):
If the patient’s oral intake is low, administer IV fluids.
After stabilization, help the patient eat soft and nutritious foods.
7. Monitoring for Recurrence:
Watch for recurrence of seizures.
Avoid trigger factors such as stress, sinus infection, fever, etc.
8. Psychosocial Support and Education:
Counseling the patient and family members that convulsions do not always mean epilepsy but may have other causes as well.
Home Care Provide guidance on management, regular medication and follow-up maintenance.
Train patients and parents on first aid for seizures.
9. Documentation:
Write down in detail in the Nurses Note how long the seizure lasted, how the patient behaved, what medication was given, etc.
Also record the patient’s response and side effects.
Convulsion can be a serious medical condition that can be effectively managed with systematic nursing care. Patient safety, timely medication, neurological and vital monitoring, and psychosocial support are key elements. A properly prepared nursing team can improve the patient’s quality of life and prevent recurrence.
b) Write short note on IMNCI.
IMNCI (Integrated Management of Neonatal and Childhood Illness):
IMNCI (Integrated Management of Neonatal and Childhood Illness) — Integrated Management of Neonatal and Childhood Illness
Introduction:
IMNCI (Integrated Management of Neonatal and Childhood Illness) is a comprehensive guideline developed by the World Health Organization (WHO) and UNICEF, whose main objective is to ensure timely diagnosis, appropriate treatment and reduction of mortality of major diseases seen in patients aged 0 to 5 years. The Government of India has incorporated this approach into its health policy and has made it operational across the country by training nurses, ANMs (Auxiliary Nurse Midwives), and frontline health workers.
Main components of IMNCI:
1. Assessment of the patient:
The patient is observed for symptoms of major diseases — such as breathing difficulty, fever, diarrhea, malnutrition, measles, pneumonia, etc. — and then classified according to severity using a collar coded classification. Giving.
2. Standard Treatment:
Giving treatment as per World Health Organization guidelines for each classification — which includes Oral Rehydration Therapy (ORS Therapy), Zinc, Antibiotics, Antimalarials, etc.
3. Counseling & Home Care Guidelines:
Educating the patient’s parents about nutrition, breastfeeding, medical Follow-up, explaining about danger signs.
4. Referral System:
If the patient’s disease is serious and not possible at the primary level, then refer him to a higher center in a timely manner.
Special features of IMNCI:
- IMNCI has been adapted to the Indian context as per the guidelines of ICMR (Indian Council of Medical Research).
- IMNCI also includes 0-7 days old newborn patients, which makes it more comprehensive than the GOBI-FFF model.
- In IMNCI, apart from treatment, importance has also been given to prevention, parental education and nutritional support.
- This can also be done at the community level by the Village Health Nurse (Health Worker). The implementation of the process has been made possible.
Main diseases covered under IMNCI:
1. Pneumonia:
2. Acute Diarrheal Disease
3. Malaria
4. Measles
5.Under Nutrition
6.Neonatal Sepsis
7.Hypothermia
8.Hypoglycemia
Benefits of IMNCI Program:
- Timely treatment of the patient.
- Child Mortality Rate and Morbidity are reduced.
- Capacity and skills of health workers are developed.
- Health services reach the community level.
- Parents can identify the symptoms of the patient and take immediate treatment.
IMNCI Structure and Classification System:
IMNCI classifies patients through three color codes:
1.Yellow: Patient is treated in general treatment and OPD.
2.Green: Patient requires home care and follow-up.
3.Red: Patient requires immediate referral and hospital admission Necessary.
IMNCI (Integrated Management of Neonatal and Childhood Illness) is a highly effective, integrated and scientific approach for pediatric patients. In a densely populated and resource-poor place like India, IMNCI plays a vital role in improving patient health, reducing infant mortality and empowering health workers. IMNCI is not just a treatment but a complete pediatric public health model.
c) Explain nursing management of handicapped child. Explain the nursing management of a handicapped child.
Introduction:
A handicapped child is a patient who has some kind of long-term limitation in physical, mental, sensory, behavioral or developmental abilities. The complete nursing management of this patient should be based on physical health, psychological support, educational rehabilitation and family involvement. Conditions like Cerebral Palsy, Down Syndrome, Spina Bifida, Autism, and Hearing Impairment are seen in handicap patients.
1. Holistic Approach:
Provide nursing care considering the physical, mental, emotional and social needs of the handicapped patient. Prepare a care plan according to the capacity of each patient.
2. Physical Care & Rehabilitation:
Assist the patient in daily activities — such as dressing, feeding, bathing, etc.
Improve muscle tone and mobility through massage, passive and active exercise. (Mobility) Increase.
Guide for regular sessions of Physiotherapy and Occupational Therapy.
3.Nutritional Management:
Make a diet plan according to the metabolic needs of the patient.
If oral feeding is not possible, provide nutrition through Nasogastric Feeding or Gastrostomy.
Giving special instructions to avoid nutritional deficiency.
4. Communication & Learning Support
If the patient has speech difficulties, then provide assistance through speech therapy.
Making learning easier through audiovisual aids and special education programs.
Alternative communication methods for the patient such as picture cards Use of.
5. Pain and Infection Management
Regular assessment of the patient’s pain level and administration of analgesics as prescribed by the doctor.
Regular position changes and hygiene should be maintained to prevent common complications such as bedsores and urinary tract infections (UTI).
6. Psychological Support & Motivation Motivation)
Use positive reinforcement to increase the patient’s confidence, self-esteem, and self-esteem.
Seek counseling or psychologist’s help for depression, loneliness, and anxiety.
7. Parental Education & Family Involvement
Parents should be involved in the patient’s daily care, rehabilitation, treatment, and Provide training on communication methods.
Create a family support system so that the patient gets a homely and positive environment.
Manage guilt, stress and expectations among parents.
8. Social Interactive Activities
Involve the patient in activities such as group therapy, recreational activities to interact with other children.
Encourage the patient towards a normal life through school and community involvement.
9.Regular Follow-up & Documentation
Maintain regular documentation of the patient’s health status, therapy progress and response.
Keep the patient’s medical records and prescriptions up to date.
Analysis of the effects of each therapy and change To do.
Nursing care for a handicapped child is not just about treatment but also an emotional, professional and continuous supportive process. The main objective of the nurse is to motivate the patient to live to their best potential. For this, health goals can be achieved through individual care plans, parental support, therapy assistance and community involvement.
Q-4 Write short notes. (Any three)
a) Difference between pathological jaundice & physiological jaundice. Difference between pathological jaundice and physiological jaundice
Introduction:
Jaundice is a condition caused by an increase in the level of bilirubin in the patient’s blood, in which the skin and sclera appear yellow. Jaundice is especially common in newborn patients. It
There are two types — Physiological Jaundice and Pathological Jaundice. The differences between the two are very important for the diagnosis and treatment of the patient.
1. Definition:
Physiological Jaundice:
This is a common type of newborn jaundice, which is caused by incomplete development of the liver. It is not associated with any underlying disease and is usually not dangerous.
Pathological Jaundice:
This is a type of jaundice that appears in newborns within the first 24 hours of birth and is indicative of a more severe pathological condition. This can be harmful to the patient and requires immediate treatment.
2. Onset Time:
Physiological Jaundice:
Usually occurs between 24 and 72 hours after birth.
Pathological Jaundice:
Appears within the first 24 hours of birth.
3. Bilirubin Level:
Physiological Jaundice:
Bilirubin levels are usually ≤ 12 mg/dl.
Pathological Jaundice:
Bilirubin levels can be ≥ 15 mg/dl or increase rapidly ≥ 0.5 mg/dl per hour.
4. Causes:
Physiological Jaundice:
Liver immaturity, excessive red blood cell hemolysis, slow bilirubin metabolism.
Pathological Jaundice:
Rh incompatibility, ABO incompatibility, Neonatal sepsis, Hemolytic anemia, G6PD deficiency, Congenital infections.
5.Symptoms:
Physiological Jaundice:
Mild skin pigmentation, patient is generally healthy.
Pathological Jaundice:
Symptoms such as continuous redness, inability to eat, increased sleepiness, stupor and sometimes seizures.
6. Complications:
Physiological Jaundice:
Complications are not usually seen, the risk of Kernicterus is very low.
Pathological Jaundice:
Serious complications such as Kernicterus, Brain damage, Hearing loss, Developmental delay are possible.
7. Treatment:
Physiological Jaundice: Observation, increase breastfeeding. No special intervention is required.
Pathological Jaundice:
Immediate phototherapy, exchange transfusion, intensive medical care are required.
8. Duration:
Physiological Jaundice:
Recovers on its own in approximately 5 to 7 days.
Pathological Jaundice:
Can persist for a longer period and the patient’s condition may worsen if proper treatment is not given.
9. Difference in Clinical Management:
Conclusion:
Physiological Jaundice is a common, self-limiting and less complicated condition, while Pathological Jaundice is a severe and high-risk condition that requires timely recognition and immediate medical intervention. As a nursing professional, it is very important to closely monitor the patient, record symptoms, and provide appropriate management in collaboration with the doctor.
b) Care of child in phototherapy
When a child has jaundice, the liver is not able to metabolize bilirubin in the body. Phototherapy is used to treat this condition.
Phototherapy is a non-invasive, low-cost treatment that uses equipment to convert unconjugated bilirubin into water-soluble nontoxic bilirubin, which is easily excreted from the body through urine and stool.
This therapy should be started in a child with hyperbilirubinemia when the serum bilirubin level is 15 mg/dl. This therapy can be started even before that.
If the condition is severe, then exchange blood transfusion is also done along with this therapy.
If phototherapy is started in the early stages when the serum bilirubin level in the child is increasing, then a very good effect is seen.
Phototherapy can be given to the child continuously or intermittently. It depends on the condition of the child. Fluorescence or halogen light is used in this therapy.
Compact fluorescent lamps or light emitting diodes are also currently used for effective phototherapy.
Blue light is used more in phototherapy. Its wavelength is 420 to 600 nanometers. Which helps in good absorption of bilirubin.
The baby is placed in a warmer in the newborn care unit for phototherapy. 6 to 8 such light sources are fitted on it. During this time, the child’s clothes are removed and only the eye area and private parts are covered to prevent damage to the retina and genital area.
Phototherapy can be given as a single surface or double surface i.e. from both sides. The distance between the child and the light source is kept at 45 cm. This distance can be less depending on the type of light and the severity of the child’s condition.
During phototherapy, it is necessary to change the position of the child every few hours. It is also necessary to feed the child. During this time, the baby’s vital signs should be continuously monitored.
Continuous breast feeding or intravenous or nasogastric feeding is continued to prevent dehydration of the baby during phototherapy.
It is necessary to monitor the baby’s weight and continuously monitor input and output during phototherapy.
The baby’s serum bilirubin level should also be monitored periodically.
Phototherapy can be discontinued after the baby’s serum bilirubin level decreases and comes within the normal range.
Complications of phototherapy.
Generally, phototherapy is a safe Despite the treatment, some side effects may occur, which are as follows.
Dehydration
Hypothermia or hyperthermia
Change in stool frequency
Bronze baby syndrome
Skin rashes
Electric shock
Disturbances in electrolytes
Although the above side effects and complications are rare, it is necessary to take preventive precautions in this regard.
c) UNICEF – UNICEF
UNICEF (United Nations International Children’s Emergency Fund) is a global organization dedicated to advocating for and protecting the rights of children.
Founded in 1946, UNICEF works to improve the lives of children and their families in more than 190 countries and territories. It focuses on the most vulnerable and marginalized populations. Its efforts span a variety of areas, including health, education, nutrition, child protection and emergency relief.
Key Areas of UNICEF
Health and Nutrition:
Ensure access to essential health care services and nutrition, including immunization, maternal and newborn care, and treatment of malnutrition. Emphasize issues such as HIV/AIDS, water sanitation, and hygiene.
Education:
Take measures to ensure that all children, especially girls, and in crisis-affected areas, have access to quality education. Early Childhood Development Providing support and improving educational infrastructure and resources.
Child protection:
Providing protection to children from violence, exploitation and abuse. Address issues such as child labor, trafficking, and child marriage. Support legal and social systems to protect children’s rights.
Emergency Response:
Provide life-saving assistance during emergencies, including natural disasters, conflicts, and epidemics.
Ensure that children and families have access to shelter, food, clean water, medical care, and psychological support in all locations during emergencies.
Advocacy and Policy policy):
Advocate for policies and practices that promote children’s rights and well-being at the local, national and international levels. Partner with governments, NGOs and other stakeholders to influence policy changes and secure funding for child-focused programmes.
UNICEF’s Guiding Principles:
UNICEF’s work is guided by the principles of the Convention on the Rights of the Child (CRC). It outlines the fundamental rights of all children, including the rights to survival, development, protection and participation. The organization works on the belief that every child, regardless of their background and circumstances, should have a fair chance in life.
How UNICEF Operates Fundraising and Donations:
UNICEF is funded entirely by voluntary contributions from governments, private donors and fundraising initiatives.
Partnerships:
Collaborates with governments, non-governmental organizations (NGOs), civil society, the private sector, and communities to implement programs and reach children in need.
Field Offices:
Operates field offices around the world to directly implement and monitor projects, ensuring that resources reach children and their families.
Key Programs and Initiatives:
Gavi, Vaccine Alliance:
Works with partners to increase access to immunization in low-income countries.
UNICEF-School in a Box:
Provides portable learning supplies to children in emergency and conflict situations.
Impact:
UNICEF has made significant progress in improving the lives of children globally.
It has contributed to reduced child mortality rates, increased school attendance, better nutrition and stronger child protection.
UNICEF continues to be a vital force in global efforts to create a world where every child is healthy, educated, protected and respected.
D) Internationally excepted rights of children.
Internationally recognized children’s rights
The United Nations declared the rights of children on 20 November 1959. They were made with the aim of fulfilling the special needs of the child in mind.
These rights are as follows.
- No right to free education.
- No right to name and nationality.
- The right to receive special care if the child is handicapped. The right to receive affection, love and good understanding.
- The right to receive adequate quality nutrition. The right to receive first aid or relief in times of distress or distress.
- The right to receive good medical care. The right to play well and have recreational facilities.
- The right to develop one’s abilities and become a useful member of society. The right to be brought up in a peaceful and fraternal environment.
- All the above rights are also the right of children to exercise all rights equally without discrimination of religion, caste, creed, sex, color, etc.
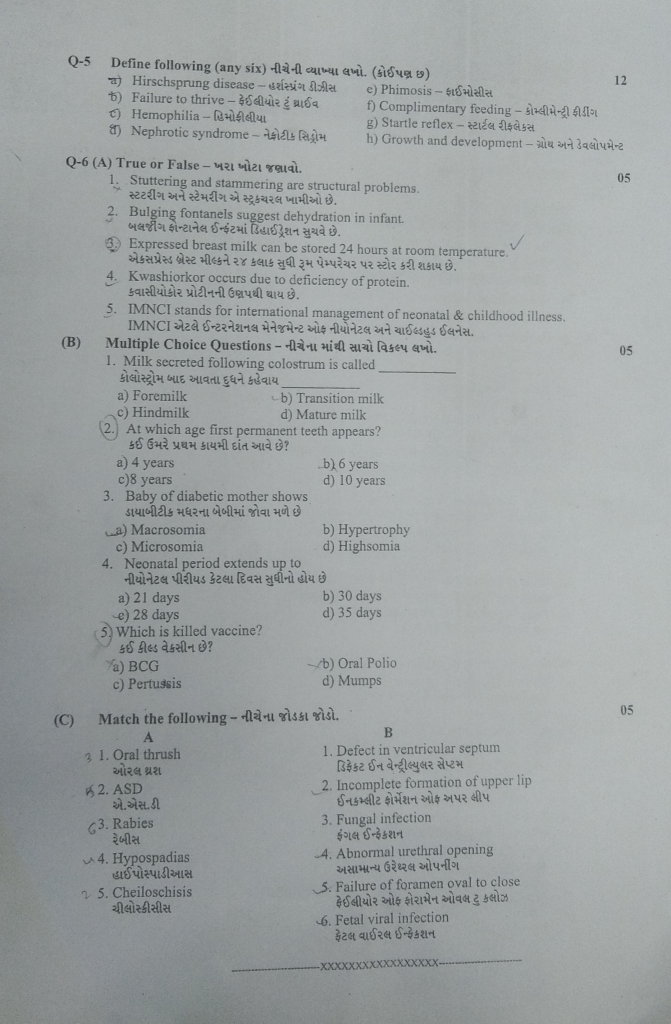
Q-5 Define the following (any six) Write the following definition. (Any six) 12
a ) Hirschsprung disease
Hirschsprung Disease is a congenital neurogenic disease of the intestine, in which ganglion cells (nerve cells) are not present in a certain part of the large intestine, due to which that part cannot perform peristaltic movement and stool does not move forward, resulting in obstruction. This disease mainly affects the rectum and sigmoid colon and presents in newborns with symptoms such as delayed passage of meconium, abdominal distension, and constipation. Rectal biopsy, manometry, and barium enema are used for diagnosis, and surgery is used to remove the affected intestine.
b) Failure to thrive – Failure to thrive
Failure to thrive is a chronic, potentially life-threatening disorder of infants and young children in which infants and children do not gain weight adequately for their age and such children lose weight. In a child who has the condition of Failure to Thrive, the expected growth of the child does not occur and the child’s well-being also becomes impaired. And it indicates psychosomatic growth failure.
Failure to thrive means that in any infant and young child, the child has not gained the weight that the child should have gained at the age (age) and if the child weighs less than that, this condition is called failure to thrive.
c) Hemophilia
Hemophilia is a It is an inherited bleeding disorder that is usually caused by a deficiency of plasma coagulation factors (factors 8, 9, and 11). It is usually found in high amounts in males. In which excessive bleeding occurs and blood clotting is poor.
Classification of the Hemophillia
There are a total of 3 classifications of hemophilia.
1) Hemophilia A,
2) Hemophilia B,
3) Hemophilia C.
1) Hemophilia A
Hemophilia A is caused by a deficiency of factor VII(8). is.
2) Hemophilia B,
Hemophilia B is usually caused by a deficiency of factor IX(9).
3) Hemophilia C.
Hemophilia C is caused by a deficiency of factor Xi(11).
d) Nephrotic syndrome – Nephrotic syndrome
This is a disease of the urinary system. Which commonly causes hospitalization in children.
This syndrome is characterized by signs and symptoms of more than one condition. The main symptoms of nephrotic syndrome are severe edema (swelling), hypoalbuminemia, albuminuria, and hyperlipidemia, i.e. hypercholesterolemia.
Nephrotic syndrome is a kidney disorder in which glomerular permeability increases, which filters proteins in blood plasma. Due to which the amount of protein increases in the urine and the amount of protein in the blood decreases.
Due to the decrease in the amount of protein in the blood, the fluid in the blood is transferred from the capillaries to the surrounding tissues and cells. So edema i.e. swelling is seen.
Thus nephrotic syndrome is a very complex and common pediatric problem in children.
e) Phimosis – Phimosis
Phimosis is a condition in which the foreskin on the penis tightens and does not retract properly and it tightens on the glans penis. This condition is called phimosis. This condition is mainly congenital but it can also be seen due to any infection. Phimosis Disease Condition Pain and discomfort are seen during sexual activity.
f) Complimentary feeding -कॉल्मिन्ट्री फीडिंग
Complementary Feeding is the process in which after the age of 6 months, additional food i.e. complementary food is started in addition to breast milk. The growing nutritional needs of the child cannot be fulfilled by breast milk alone, therefore, various nutritious foods such as pulses, rice, vegetables etc. (stage-appropriate food) are added to soft and easily digestible foods made with the help of a machine. Breastfeeding should be continued even while continuing complementary feeding. This process is very essential for the growth and nutrition of the child and if it is not done at the right time and in the right way, the child is likely to suffer from problems like Growth failure, Malnutrition and Infection.
g) Startle reflex – Startle reflex
Startle reflex, also known as Moro reflex, is a natural neurological response that is present in newborn infants from birth. When a baby is startled by a sudden noise, sudden movement, or loss of support, the infant will suddenly spread and then retract his arms and legs and often start crying – this process is called the startle reflex. This reflex is usually an indicator of healthy brain development in the infant and usually disappears on its own within 4 to 6 months. If this reflex persists for a long time, it may be a sign of Neurodevelopmental Delay or Neurological Disorder, so observation by a Pediatrician is necessary.
h) Growth and development- Growth and development
Growth- Growth
Growth is a physical maturation in which the number and size of the body’s tissues increase and the size or number of the body’s organs increase. In which the increase in growth is due to cell division and an increase in the components inside the cell Growth occurs due to the body. Changes in the body due to growth are measured in inches/centimeters and pounds/kilograms. Growth is progressive and measurable, with an increase in height and weight. Proper growth with good nutrition is seen with age, so eating good food leads to good growth.
OR
Growth is the physical maturation in which the size and shape of the various organs of the body increase. This is due to the multiplication of cells and the increase in intracellular substance. The change in growth can be measured in centimeters and kilograms.
Development ::
Development is the process in which the body matures functionally and physiologically. Development involves an increase in skills and the capacity to perform functions. Psychological, emotional and social changes occur. Measuring development is difficult but it can be measured.
Q-6 (A) True or False – Tell True or False 05
1.Stuttering and stammering are structural problems. Stuttering and stammering are structural defects:❌
✅Stuttering and stammering are speech fluency disorders, not due to structural damage.
2.Bulging fontanels suggest dehydration in infant. Bulging fontanel suggests dehydration in the infant: ❌
Bulging fontanel suggests raised intracranial pressure, not dehydration.
3.Expressed breast milk can be stored 24 hours at room temperature, Kwashiorkor is caused by protein deficiency. ✅This condition is directly linked to protein malnutrition.
5.IMNCI stands for international management of neonatal & childhood illness. IMNCI stands for International Management of Neonatal and Childhood Illness : ❌
full form of IMNCI = Integrated Management of Neonatal and Childhood Illness.
B) Multiple Choice Questions Which of the following is the correct option? 05
1.Milk secreted following colostrum is called
b) Transition milk
c) Hindmilk
d) Mature milk
(2.) At which age first permanent teeth appear? At what age do the first permanent teeth appear?
a) 4 years
b) 6 years
c)8 years
d) 10 years
3.Baby of diabetic mother shows Diabetic mother’s baby shows –>
a) Macrosomia
b) Hypertrophy
c) Microsomia
d) Highsomia
4.Neonatal period extends up to How many days does the neonatal period last?
a) 21 days
b) 30 days
c) 28 days
d) 35 days
5) Which is killed vaccine? What is a killed vaccine?
a) BCG
b) Oral Polio
c) Pertussis
d) Mumps
(C) Match the following Attach.
1.Oral thrush 1.Defect in ventricular septum
2.ASD 2.Incomplete formation of upper lip
3.Rabies Rabies 3.Fungal infection Fungal infection
4.Hypospadias Hypospadias 4. Abnormal urethral opening
5.Cheiloschisis 5. Failure of foramen oval to close
6.Fetal viral infection
✅ Final Matching Order:
- 1 → 3
- 2 → 5
- 3 → 6
- 4 → 4
- 5 → 2