ENG💯General Nursing & PAPERMidwifery (Second Year) GNM-S.Y-MSN-II-30/01/2024 (UPLOAD PAPER NO.7)
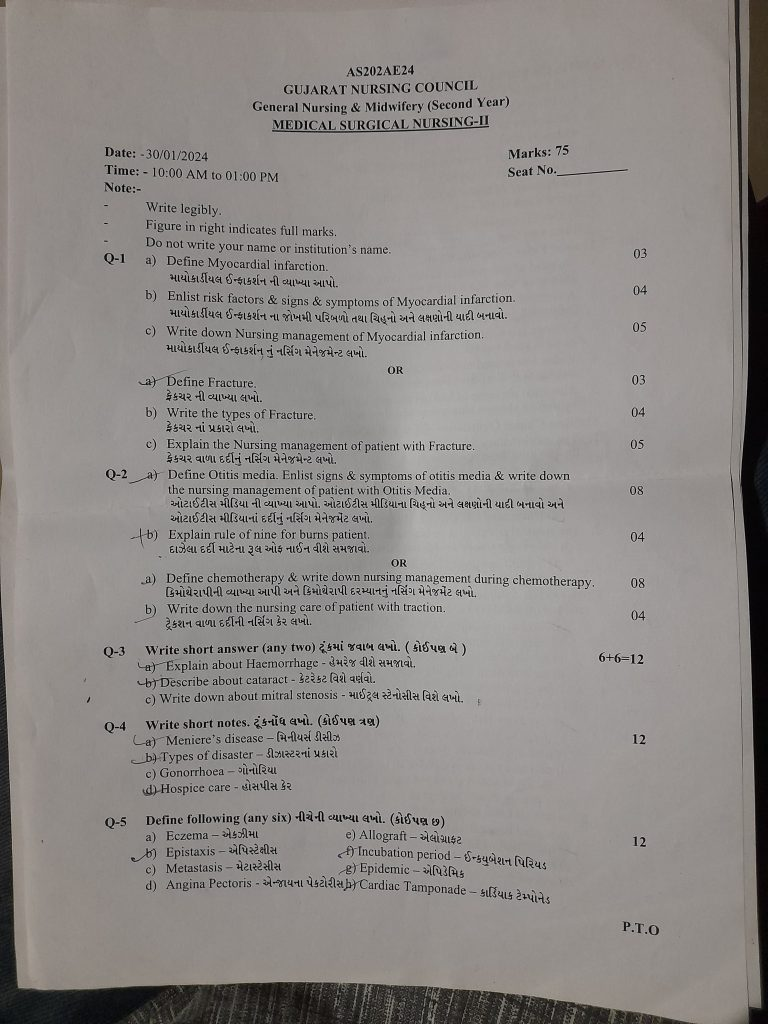
GNM-GNC-S.Y-MSN-II-Date: -30/01/2024
⏩Q-1 🔸a) Define Myocardial infarction. (03)
Myocardial infarction, commonly known as a heart attack, is a serious medical emergency characterized by the interruption of blood flow to the heart muscles. This blockage typically occurs due to the sudden formation of a blood clot or plaque buildup in the coronary arteries, which supply oxygen-rich blood to the heart.
During a myocardial infarction, the affected coronary artery becomes blocked, leading to a lack of oxygen and nutrients reaching a portion of the heart muscle. As a result, the affected heart muscle tissue can suffer irreversible damage and undergo necrosis (death of tissue cells). The severity of myocardial infarction can vary from mild to severe, depending on the extent of blockage and the duration before treatment is initiated.
Immediate medical intervention is crucial to restore blood flow to the affected heart muscle and minimize damage. Treatment typically involves medications to dissolve the clot (thrombolytics), procedures such as angioplasty to reopen the blocked artery, and lifestyle changes to reduce the risk of future heart attacks.
Myocardial infarction is a leading cause of death worldwide and requires prompt recognition and intervention to improve outcomes and prevent complications.
🔸b) Enlist risk factors & signs & symptoms of Myocardial infarction.
Risk Factors:
✓ Non-modifiable Risk Factors:
- Age
- Gender (men are 3 times more prone than women)
- Family history
- Race (African Americans have higher incidence of heart disease)
✓ Modifiable Risk Factors:
- Smoking
- High blood pressure
- High cholesterol level
- Diabetes
- Obesity
- Physical inactivity
- Unhealthy diet
- Stress
- Type A personality
- Lack of estrogen in women
- Elevated serum homocysteine
Signs & Symptoms:
- Chest pain or discomfort
- Pain may radiate to arm, jaw, neck, shoulder, or back
- Pain is substernal, severe, and diffuse
- Feeling of heaviness, squeezing in the chest
- Pain is not relieved by rest and medication
- Shortness of breath
- Diaphoresis (excessive sweating)
- Cool, clammy, and moist skin
- Decreased cardiac contractility
- Decreased cardiac output
- Nausea and vomiting
- Restlessness
- Dizziness
- Lightheadedness
- Fainting
- Confusion
- Disorientation
- Fever
Myocardial infarction (heart attack) is a critical condition requiring immediate medical attention. Recognizing these signs and symptoms and understanding the associated risk factors is crucial for timely intervention and improving outcomes.
🔸c ) Write down Nursing management of Myocardial infarction. (05)
Acute Pain Management Related to Myocardial Infarction:
- Assess pain level, location, duration, intensity, and timing.
- Identify factors triggering and relieving pain.
- Provide Fowler’s or semi-Fowler’s position to facilitate lung expansion.
- Provide distraction therapy to divert attention from pain.
- Provide relaxation therapy.
- Administer prescribed medication.
- Monitor medication side effects and effectiveness.
- Maintain accurate records and reports.
Decrease cardiac output related to decrease cardiac contractility / reduced preload afterload contractility / decrease coronary blood flow as evidence by increase heart rate
Decreased Cardiac Output Management Related to Myocardial Infarction:
- Assess patient’s condition.
- Monitor vital signs.
- Monitor cardiovascular status.
- Monitor ECG patterns.
- Auscultate heart sounds and rhythms.
- Assess peripheral pulses.
- Monitor hemodynamic parameters.
- Maintain intake-output chart.
- Monitor urine output hourly.
- Provide Fowler’s or high-Fowler’s position.
- Administer IV fluids as prescribed.
- Administer prescribed medications.
- Monitor medication side effects and effectiveness.
- Maintain records and reports.
Ineffective Tissue Perfusion Management Related to Myocardial Infarction:
- Assess patient’s condition.
- Monitor vital signs.
- Assess skin for cool, moist signs.
- Assess fluid volume status.
- Check skin temperature, peripheral pulses, capillary refill.
- Assess need for bed rest.
- Administer oxygen therapy.
- Provide mechanical ventilation if necessary.
- Provide fluid resuscitation as prescribed.
- Administer prescribed medications.
- Monitor medication side effects and effectiveness.
- Maintain records and reports.
Impaired Gas Exchange Management Related to Myocardial Infarction:
- Assess patient’s condition.
- Monitor vital signs.
- Monitor respiratory rate, rhythm, arterial blood gases, tidal volume, peak inspiratory pressure, extubation parameters.
- Assess skin, mucous membranes, nail beds for signs.
- Auscultate breath sounds.
- Provide semi-Fowler’s or Fowler’s position.
- Provide bed rest.
- Administer supplemental oxygen.
- Administer prescribed medications.
- Monitor medication side effects and effectiveness.
- Maintain records and reports.
Anxiety Management Related to Myocardial Infarction:
- Assess patient’s condition.
- Assess signs of anxiety such as restlessness, sleeplessness.
- Focus on the patient’s psychological needs and listen attentively to their concerns.
- Provide psychological support and actively listen to patient’s feelings and discomfort.
- Educate patient about their condition and treatment to alleviate anxiety and build confidence.
- Provide psychological support.
- Administer anti-anxiety agents as prescribed.
- Resolve all doubts and queries of patient.
- Provide mental diversion therapy and recreational therapy.
- Provide knowledge about their condition and treatment to alleviate anxiety and build patient confidence.
- Provide psychological support to the patient.
- Offer Mind Diversional Therapy and recreational therapy.
- Antianxiety agent administer
Activity Intolerance Management Related to Myocardial Infarction:
- Inhas Activity Level
- (Increasing Activity Level)
- Assess the patient’s condition.
- Check the patient’s activity level.
- Provide bed rest initially to the patient.
- Gradually encourage a range of motion exercises for the patient.
- Assist the patient with their activity.
- Provide rest between two activities.
- Check for any breathing difficulty or palpitations during activity.
- If present, stop the patient’s activity and provide rest.
- Avoid heavy lifting for the patient.
- Avoid tasks that could strain the heart.
🔸 OR 🔸
🔸a) Define Fracture.
Fracture means the continuity break of a bone.
Fracture is recognized as a breakdown within the continuity of a bone, involving the bone itself, its tissue, bone marrow, and periosteum.
🔸b) Write the types of Fracture.
1) Complete Fracture: In this type, the bone breaks completely across its cross-section. Complete fracture divides the bone into two parts.
2) Incomplete Fracture: In this type, the bone does not break completely. There is a crack in the bone but it does not completely break down.
3) Closed Fracture: Also known as a “simple fracture,” in which the bone breaks but remains inside the skin, meaning the skin is intact and does not show the fracture site. Closed fractures are associated with minimal risk of infection.
4) Open Fracture: An open fracture, also termed a “compound fracture,” is where the bone breaks through the skin and is visible externally. The fracture site is exposed to external contaminants, and bacteria can enter through the open wound, potentially causing infection.
5) Displaced Fracture: In this type of fracture, the ends of the broken bone separate and are not aligned properly. Displaced fractures often require surgical intervention.
6) Comminuted Fracture: This fracture type involves the fragmentation of bone into multiple pieces. Comminuted fractures are more common in elderly people due to increased bone fragility.
🔸Classification by Fracture Pattern:
1) Linear Fracture: In this type, the fracture line of the bone is parallel to its long axis and usually occurs due to direct force on the bone.
2) Transverse Fracture: In this type, the fracture is seen at a right angle (90 degrees).
3) Oblique Fracture: Here, the fracture line is at an angle of 45 degrees, typically due to twisting forces.
4) Spiral Fracture: Also known as a “torsion fracture,” it occurs due to twisting forces.
5) Depressed Fracture: This type involves the bone being pressed inward, such as in skull bones and facial bones.
6) Longitudinal Fracture: This is a fracture that occurs along the long axis of the bone.
🔸Classification by Type of Fracture:
1) Avulsion Fracture: In this type, the bone segment is detached from its ligament and tendon.
2) Compression Fracture: Also known as a “crush fracture,” it occurs due to compression on the bone. The bone is compressed in this type.
3) Greenstick Fracture: In this type, the bone breaks on one side and bends on the other. Greenstick fractures are more common in children.
4) Impacted Fracture: In impacted fractures, there is a loss of continuity of the bone due to compression.
5) Pathological Fracture: This type of fracture occurs due to a pre-existing disease, such as osteoporosis or cancer.
6) Stress Fracture: This is a small crack in the bone caused by repetitive loading on the bone. Stress fractures are common in athletes.
✓ Classification by Eponym :
1) Colles Fracture:
- Definition: Colles fracture is commonly referred to as a “broken wrist.” It occurs when the radius bone fractures within one centimeter of its articulation with the wrist surface.
- Location: The fracture typically involves the distal end of the radius bone, specifically the area near its articulation with the wrist.
2) Pott’s Fracture:
- Definition: Pott’s fracture primarily involves the medial malleolus of the tibia and the fibula.
- Location: This fracture is characterized by the involvement of the medial malleolus (which is part of the tibia) and the fibula.
🔸Classification by Anatomic Location:
1) Articular Fracture: In this type, the fracture occurs in the joint’s articular surface. It often involves damage to the articular cartilage and may damage the subchondral bone.
2) Extra-articular Fracture: In this type, the fracture occurs near the joint but does not involve the joint capsule’s involvement. This type of fracture is common in the hip.
3) Intra-capsular Fracture: This type of fracture occurs within the joint capsule. It does not involve the joint capsule’s involvement and is more common in the neck of the femur.
🔸c) Explain the Nursing management of patient with Fracture. (05)
Certainly! Here’s the nursing management for a patient with a fracture:
1. Monitor Vital Signs:
– Regularly monitor the patient’s vital signs including temperature, pulse, respiration rate, and blood pressure to detect any signs of complications such as infection or shock.
2. Assess Neurovascular Status:
– Perform neurovascular assessments to evaluate circulation, sensation, and movement in the affected limb(s). Check for signs of impaired circulation or nerve function.
3. Pain Management:
– Use pain scales to assess and monitor the patient’s pain level. Administer prescribed analgesics as per the doctor’s orders to alleviate pain and ensure patient comfort.
4. Maintain Intake and Output Chart:
– Record and monitor the patient’s fluid intake and output to ensure adequate hydration and detect any fluid imbalance.
5. Check for Edema or Swelling:
– Assess for any signs of swelling or edema in the affected limb(s). Elevate the affected extremity to reduce swelling if present.
6. Assess Cast Tightness:
– Regularly check the tightness and fit of the cast or splint to ensure it is not too tight, which could impair circulation or cause discomfort.
7. Monitor for Signs of Infection:
– Watch for any signs of infection such as increased pain, redness, swelling, or discharge at the injury site. Report any abnormalities to the medical team promptly.
8. Provide Comfortable Positioning:
– Assist the patient in finding a comfortable position that helps alleviate pain and promotes healing of the fracture.
9. Encourage Gradual Active Range of Motion Exercises:
– Instruct and assist the patient in performing gentle active range of motion exercises as prescribed to prevent stiffness and promote joint mobility.
10. Instruct Deep Breathing Exercises:
– Encourage the patient to perform deep breathing exercises to prevent respiratory complications such as pneumonia, especially if mobility is limited.
11. Teach Relaxation Techniques:
– Teach relaxation techniques such as deep breathing, guided imagery, or progressive muscle relaxation to help manage pain and reduce anxiety.
12. Elevate Affected Limb(s) Above Heart Level:
– Position the affected limb(s) above heart level when resting to reduce swelling and improve venous return, which aids in reducing edema.
13. Use Aseptic Technique During Dressing Changes:
– Follow strict aseptic technique protocols during dressing changes to prevent infection and promote wound healing.
14. Instruct Range of Motion Exercises in the Affected Extremity:
– Teach and encourage the patient to perform range of motion exercises in the affected extremity to prevent muscle atrophy and promote circulation.
15. Provide Education on Early Ambulation and Its Benefits:
– Educate the patient about the benefits of early ambulation as prescribed by the doctor, emphasizing its role in preventing complications and promoting recovery.
16. Ensure Adequate Protein and Calcium-Rich Diet:
– Provide dietary education focusing on foods rich in protein and calcium to support bone healing and overall recovery.
17. Educate on Assistive Devices (e.g., crutches, walkers, slings):
– Provide instructions and education on the proper use of assistive devices to aid mobility and promote independence during recovery.
18. Change Position Every Two Hours:
– Regularly change the patient’s position every two hours to prevent pressure ulcers and promote comfort.
19. Provide Reassurance:
– Offer emotional support and reassurance to the patient and family members throughout the recovery process.
20. Administer Prescribed Antibiotics, Analgesics, Calcium Supplements:
– Ensure timely administration of prescribed medications such as antibiotics for infection prevention, analgesics for pain management, and calcium supplements for bone healing.
21. Maintain Records and Reports:
– Keep accurate records of assessments, interventions, and the patient’s progress. Report any significant findings or changes in condition to the healthcare team.
Implementing comprehensive nursing management ensures optimal care for patients with fractures, promoting healing and minimizing complications.
⏩Q-2 🔸a) Define Otitis media. Enlist signs & symptoms of otitis media & write down the nursing management of patient with Otitis Media ( 08 )
Otitis media is an infection and inflammation of the middle ear. Here are the signs and symptoms associated with otitis media:
Earache (Otalgia):
- Dizziness and severe pain in the ear are common symptoms of otitis media.
Hearing Loss:
- Partial or complete loss of hearing due to fluid buildup and inflammation in the middle ear.
Tinnitus Sensation:
- Perception of ringing or buzzing sounds in the ear without any external source.
Ear Fullness:
- Sensation of fullness or pressure in the ear due to fluid accumulation.
Fluid Drainage:
- Pus or fluid draining from the ear, which may indicate a perforated eardrum in severe cases.
Balance Problems:
- Issues with balance and coordination, often accompanied by dizziness or vertigo.
Irritability:
- Restlessness or irritability, especially in infants and young children experiencing ear pain.
Fever:
- Elevated body temperature, which can occur as the body responds to the infection.
Headache:
- Pain or discomfort in the head, often associated with the pressure buildup in the ear.
Vomiting:
- Nausea and vomiting, particularly in younger children who may have difficulty expressing their discomfort.
Sleeping Difficulty:
- Trouble sleeping or frequent waking due to pain or discomfort in the ear.
Here is the nursing management plan for otitis media, addressing various aspects of patient care:
Acute Pain related to inflammation and pressure on tympanic membrane
: Relieve Pain
Assess Patient Condition:
- Evaluate the location, duration, and intensity of pain.
Positioning:
- Provide a comfortable position that can help alleviate discomfort.
Hot Water Bag Application:
- Apply a hot water bag to the affected ear site to alleviate discomfort.
Provide Knowledge on Mind Diversions:
- Educate the patient about activities or techniques to distract from pain.
Relaxation Techniques:
- Encourage the patient to use relaxation techniques.
Administer Prescribed Medications:
- Administer medications prescribed by the doctor.
Maintain Records and Reports:
- Document the intervention and the patient’s response.
Impaired Verbal Communication related to hearing deficit
: Improve Hearing and Communication
Assess Patient Condition:
- Evaluate the patient’s condition and level of hearing impairment.
Audiogram or Tympanogram Assistance:
- Assist in assessing hearing acuity using audiograms or tympanograms.
Check Hearing Acuity:
- Conduct a hearing acuity check.
Use Simple Language:
- Use simple language when communicating with the patient.
Use Short Sentences:
- Use short sentences during communication.
Use Non-verbal Communication Methods:
- Use non-verbal communication methods when necessary.
Administer Prescribed Medicine and Ear Drops:
- Administer medications and ear drops as prescribed by the doctor.
Maintain Records and Reports:
- Document all assessments, interventions, and patient responses.
Risk for Infection related to eustachian tube dysfunction
Prevent Infection
Assess Patient Condition:
- Evaluate the patient’s condition.
Monitor Vital Signs:
- Monitor vital signs regularly.
Check Signs of Infection:
- Check for signs of infection such as restlessness or fever.
Monitor Blood Reports:
- Monitor blood reports as necessary.
Provide Isolation:
- Provide isolation to prevent the spread of infection.
Use Aseptic Techniques:
- Use aseptic techniques during patient care.
Administer Prescribed Medicine:
- Administer medications as prescribed by the doctor.
Maintain Records and Reports:
- Document all assessments, interventions, and patient responses.
Anxiety related to disease condition
Reduce Anxiety
Assess Patient Condition:
- Evaluate the patient’s condition.
Assess Anxiety Signs:
- Assess signs of anxiety such as restlessness or sleeplessness.
Provide Psychological Support:
- Offer psychological support and listen to the patient’s concerns.
Encourage Expression of Feelings and Discomfort:
- Encourage the patient to express feelings and discomfort.
Provide Knowledge on Condition and Treatment:
- Educate the patient about their condition and treatment to increase confidence.
Provide Psychological Support:
Offer psychological support.
Administer Anti-Anxiety Agents:
- Administer anti-anxiety agents as prescribed.
Maintain Records and Reports:
- Document all interventions and patient responses.
🔸b) Explain rule of nine for burns patient ( 04)
The Rule of Nines is a method used to estimate the total body surface area (TBSA) affected by burns in adults. It divides the body into regions, each representing approximately 9% or multiples of 9% of the TBSA, allowing for a quick assessment and initial management of burns:
Rule of Nines:
- Head: 9%
- Right Arm: 9%
- Left Arm: 9%
- Right Leg: 18% (front) + 18% (back) = Total 36%
- Left Leg: 18% (front) + 18% (back) = Total 36%
- Chest: 18%
- Back: 18%
- Genital Area: 1%
Application:
- Head: The head is assigned 9% of the total body surface area.
- Arms: Each arm is allocated 9%.
- Legs: Each leg is typically assigned 18% (front and back combined).
- Trunk: Both the front (chest) and the back (back) of the trunk are allocated 18% each.
- Genital Area: The genital area is a smaller percentage (1%) due to its size relative to the rest of the body.
Usage:
- Emergency Assessment: Medical professionals use the Rule of Nines during the initial assessment of burn victims to quickly estimate the extent of burn injuries.
- Treatment Planning: It helps in determining the need for fluid resuscitation, wound management, and other critical care interventions based on the percentage of TBSA affected.
Limitations:
- Children and Infants: This method is not applicable for children and infants because their body proportions differ significantly from adults. Instead, pediatric-specific methods like the Lund and Browder chart are used, which provide a more accurate estimation of TBSA based on age-adjusted body proportions.
Conclusion:
The Rule of Nines is a valuable tool in the initial assessment and management of burn injuries in adults. It provides a systematic approach to quickly estimate the extent of burns, facilitating prompt and appropriate medical intervention to improve patient outcomes. For pediatric cases, alternative methods tailored to their unique body proportions should be employed for accurate assessment and treatment planning.
🔸OR 🔸
🔸a) Define chemotherapy & write down nursing management during chemotherapy. (08)
Definition of Chemotherapy:
Chemotherapy refers to a treatment modality involving the use of chemical agents (anticancer drugs) to destroy or slow down the growth of cancer cells. These drugs work by disrupting the cell division process, thereby targeting and killing rapidly dividing cancer cells.
Nursing Management During Chemotherapy:
Monitoring Vital Signs:
- Regularly monitor the patient’s vital signs to detect any immediate adverse reactions or changes in condition.
Isolation Precautions:
- Maintain isolation precautions to minimize the risk of infection, especially if the patient’s immune system is compromised due to chemotherapy.
Personal Hygiene Maintenance:
- Emphasize the importance of personal hygiene to reduce the risk of infections. Educate patients on proper handwashing techniques.
Advice on Well-Balanced Diet:
- Provide dietary advice emphasizing a well-balanced diet that is calorie-rich, high in protein, high in fiber, and includes adequate amounts of vitamin C and other essential nutrients.
Assessment of Skin Integrity and Sensitivity:
- Regularly assess the patient’s skin for any signs of irritation or breakdown. Use Vitamin E and D-based lubricants to maintain skin integrity.
Monitoring Bleeding Time, Clotting Time, and Platelet Count:
- Monitor bleeding and clotting times, as well as platelet counts, to assess the patient’s risk of bleeding.
Preventing Any Type of Injury:
- Take precautions to prevent any type of injury, especially during intravenous administration or catheterization.
Avoiding Alcohol and Smoking:
- Advise patients to avoid alcohol and smoking during chemotherapy as they can interfere with the treatment’s efficacy and increase side effects.
Monitoring for Any Type of Vomiting:
- Administer antiemetic drugs to prevent vomiting and manage nausea effectively, which are common side effects of chemotherapy.
Assessing Hair Loss:
- Monitor the patient’s emotional response to hair loss and provide support as needed. Offer resources for coping with changes in appearance.
Trimming Nails and Lubricating Scalp:
- Encourage patients to trim their nails short and keep the scalp moisturized with Vitamin E and D-based products to minimize discomfort.
Promoting Exercise and Emotional Expression:
- Encourage light exercise and activities that promote emotional expression to help patients cope with stress and maintain mental well-being.
Providing Psychological Support:
- Offer psychological support and counseling to help patients and their families cope with the emotional challenges of chemotherapy.
Monitoring Fluid and Electrolyte Levels:
- Regularly monitor fluid intake and output, as well as electrolyte levels, to prevent dehydration and maintain balance.
Clearing All Doubts of Patients and Relatives:
- Address any concerns or doubts that patients or their relatives may have regarding chemotherapy, its side effects, and the overall treatment plan.
Effective nursing management during chemotherapy plays a crucial role in enhancing patient outcomes by ensuring proper monitoring, supportive care, and patient education throughout the treatment process.
🔸b) Write down the nursing care of patient with traction. (04)
1) Minimizing the Effect of Immobility:
- Monitor the patient’s vital signs regularly.
- Assess the traction site for any issues.
- Check for burning sensation at the site where traction is applied.
- Encourage regular exercises to maintain joint strength and function.
- Ensure adequate fluid intake for the patient.
- Advocate for a high-fiber diet.
- Provide stool softeners and enemas as needed.
2) Prevention of Infection:
- Continuously monitor the patient’s vital signs.
- Assess for any pressure sores at prominent bony sites.
- Evaluate for any skin irritation.
- Check for burning sensation at the site where traction is applied.
- Assess if there are signs present for infection.
- Use aseptic techniques when dealing with the patient.
- Administer antibiotic medicine if required.
- Maintain records and reports.
3) Promoting Tissue Perfusion:
- Assess the patient’s skin condition.
- Check skin temperature, color, and hydration level.
- Monitor the patient’s vital signs.
- Assess the patient’s motor sensory function.
- Evaluate the sensation level of the patient.
- Assess the patient’s neurovascular status.
- Encourage oral fluid intake for the patient.
- Apply petroleum jelly on the skin as needed.
- Change the patient’s position every two hours.
- Use comfort and protective devices to prevent pressure ulcers.
- Administer medications prescribed by the doctor.
General care of a patient with traction:
- Assess the patient’s neurovascular status.
- Monitor vital signs of the patient.
- Regularly assess the site where traction is applied for any abnormalities.
- Check for pain sensation, skin color, numbness, and coolness.
- Encourage the patient to perform regular exercises, deep breathing exercises, and wear elastic stockings if prescribed.
- Regularly assess the site where traction is applied for any abnormalities.
- Keep the patient in a neutral position.
- Provide a calm and comfortable position for the patient.
⏩Q-3 Write short answer (any two) (6+6=12)
🔸a) Explain about Haemorrhage –
🔸 Haemorrhage –
Definition:
Haemorrhage, also known as bleeding, occurs when blood escapes from damaged blood vessels, either within the body or externally.
Types of Haemorrhage:
1. **External Haemorrhage:
– In external haemorrhage, bleeding occurs from a visible wound, abrasion, or injury site on the body’s surface.
2. **Internal Haemorrhage:**
– Internal haemorrhage involves bleeding within the body, which may not be immediately visible. Examples include intracranial haemorrhage, gastrointestinal haemorrhage, and pulmonary haemorrhage.
Classification based on Blood Vessel Type:
– Arterial Haemorrhage: Recognized by bright red blood due to higher arterial pressure, which poses severe and life-threatening risks.
– Venous Haemorrhage:Identified by dark red blood, usually less severe compared to arterial bleeding.
– Capillary Haemorrhage: Involves small blood vessels, causing minor bleeding like in cuts and abrasions.
Causes of Haemorrhage:
– Trauma or Injury (accidents, falls, violence)
– Medical Conditions (hemophilia, blood clotting disorders, liver disease)
– Medication (blood thinners like warfarin, aspirin)
– Surgery
– Aneurysm
– High Blood Pressure
– Cancer
– Ulcer
– Childbirth Complications
Signs and Symptoms:
– External Haemorrhage:
– Bleeding from an open wound
– Visible blood
– Bruising
– Skin discoloration
– Swelling around the affected area
– Internal Haemorrhage:
– Intracranial Haemorrhage:
– Severe headache
– Confusion or altered mental status
– Vision problems
– Seizures
– Weakness or numbness on one side of the body
– Gastrointestinal Haemorrhage:
– Blood in vomit
– Blood in stool
– Abdominal pain and swelling
– Pulmonary Haemorrhage:
– Coughing up blood
– Chest pain
– Difficulty breathing
– General Symptoms:
– Rapid and shallow breathing
– Rapid pulse
– Hypotension (low blood pressure)
– Pale or clammy skin
– Weakness
– Dizziness
– Lightheadedness
Diagnostic Evaluation:
– History Collection
– Physical Examination
– Complete Blood Count (CBC)
– Coagulation Studies
– Ultrasound
– CT Scan
– MRI
– Angiography
– Endoscopy
Management of Haemorrhage:
– Immediate First Aid Care:
– Apply pressure using clean cloth or bandage to control bleeding.
– Elevate the affected area to reduce blood flow.
– Immobilize the area to prevent further damage.
– Medical Management:
– Minor Haemorrhage:
– Apply topical hemostatic agents to control bleeding.
– Use sutures or staples for small cuts and lacerations.
– Major Haemorrhage:
– Apply a tourniquet in cases of severe limb bleeding.
– Perform blood transfusion if necessary.
– Administer intravenous fluids to maintain blood pressure and organ perfusion.
– Medication such as tranexamic acid may be given to control bleeding.
– Surgical Intervention:
– Ligating or clamping of bleeding vessels.
– Repair of injured tissues or organs.
– Monitoring and Support:
– Monitor vital signs closely (blood pressure, pulse, respiratory rate, oxygen levels).
– Critical care support in severe cases, such as placement in an Intensive Care Unit (ICU) for continuous monitoring and advanced intervention.
Haemorrhage management requires prompt assessment, appropriate intervention, and continuous monitoring to prevent complications and ensure patient recovery.
🔸b) Describe about cataract –
Define cataract A cataract is an ocular condition where clouding and opacity develop in the clear crystalline lens of the eye, leading to blurred vision.
Causes of cataract include:
- Age (Hereditary/genetic factors)
- Exposure to UV light
- Exposure to heat
- Smoking
- Obesity
- Diabetes
- Eye injury
- Previous eye surgery
- Intraocular disorders
- Use of medications (corticosteroids, oral contraceptives)
Write classification of cataract
Classification of cataract includes:
- Age-related (Senile) Cataract: Most common type due to changes in the lens related to aging.
- Congenital Cataract: Present at birth, often due to genetic factors.
- Secondary Cataract: Develops as a result of eye conditions or systemic conditions such as diabetes, trauma, or inflammation.
- Traumatic Cataract: Occurs due to penetrating or blunt trauma to the eye.
- Radiation Cataract: Result of exposure to ionizing radiation.
- Electrical Cataract: Caused by electrical injury or high-voltage electric current contact.
- Toxic Cataract: Result of exposure to toxic chemicals or medications.
- Metabolic Cataract: Develops due to metabolic disorders such as galactosemia or Wilson’s disease.
Classification of cataract according to lens location:
- Nuclear Cataract: In nuclear cataract, clouding occurs in the central part of the lens nucleus.
- Subcapsular Cataract: This type affects the back part of the lens, specifically the subcapsular region.
- Cortical Cataract: Cortical cataracts affect the outer edges (cortex) of the lens, causing spoke-like opacities that start at the periphery and work their way to the center.
- Capsular Cataract: In capsular cataracts, the opacity affects the lens capsule, the thin outer covering of the lens.
- Posterior Subcapsular Cataract: This type involves the posterior part of the lens capsule, just beneath the posterior capsule.
These classifications help in understanding the specific location within the lens where the cataractous changes occur, aiding in diagnosis and treatment planning.
Sure, here are the clinical manifestations, diagnostic evaluation, and management of cataract:
Clinical Manifestations of Cataract:
1. Clouded, blurred, and dim vision: Patients experience progressively worsening vision as the cataract causes the lens to become cloudy, resulting in blurred and dim sight.
2. Trouble seeing at night (night blindness): Difficulty seeing clearly in low-light conditions is common due to reduced light transmission through the clouded lens.
3. Poor vision at night: Vision deteriorates particularly in low-light conditions, impacting activities like driving at night.
4. Double vision in one eye: Cataracts can cause double vision (diplopia) in one eye due to the light scattering unevenly through the lens.
5. Halos around lights: Patients may see circles or halos around lights, making it challenging to see clearly in bright environments.
6. Leukocoria or white pupil: In advanced stages, the pupil may appear white instead of black due to light reflecting off the cataract.
7. Photophobia: Increased sensitivity to light can occur, causing discomfort in brightly lit environments.
8. Reduced light transmission: The cataract reduces the amount of light that reaches the retina, leading to decreased visual acuity.
9. Decreased color perception: Colors may appear faded or less vibrant due to the opacity of the cataract.
Diagnostic Evaluation of Cataract:
1. History collection: Detailed history regarding symptoms, duration, progression, and medical history.
2. Physical examination: Including visual acuity testing and examination of the eye using a slit lamp.
3. Visual acuity test: Measurement of how well the patient sees at various distances.
4. Slit lamp examination: Detailed examination of the eye’s structures using a slit lamp microscope to visualize the extent and type of cataract.
5. Tonometry: Measurement of intraocular pressure to rule out glaucoma or assess its coexistence with cataract.
6. Ultrasound: Used to evaluate the density and location of cataracts, especially in cases where the view is obstructed due to dense cataracts.
Management of Cataract:
1. Phacoemulsification: This modern method involves breaking up the cloudy lens using ultrasound energy and removing it through a small incision. An intraocular lens (IOL) is then implanted to replace the natural lens.
2. Intraocular lens implantation (IOL): After removing the cataract, an artificial lens is placed in the eye (intraocularly) to restore vision.
3. Extracapsular cataract extraction (ECCE): In cases where phacoemulsification is not suitable, the lens and a portion of the lens capsule are removed, leaving the posterior capsule intact.
4. Intracapsular cataract extraction (ICCE): The entire lens and lens capsule are removed. This method is less commonly used now due to the higher risk of complications.
5. Preoperative care: Identifying the patient and confirming the doctor’s order to operate the cataract.
Identify the Patient and Verify the Doctor’s Order for Cataract Surgery:
- Confirm the patient’s identity and ensure that the doctor’s order for cataract surgery is correctly documented in the patient’s file.
Collect Appropriate History:
- Gather detailed medical history related to the cataract and any other relevant health conditions.
Perform Physical Examination:
- Conduct a thorough physical examination, focusing on the eyes and general health assessment.
Monitor Patient’s Vital Signs:
- Monitor vital signs such as blood pressure, pulse rate, and temperature to ensure stability before surgery.
Perform Necessary Blood Tests for Surgery:
- These may include a complete blood count (CBC), HIV screening, hepatitis B surface antigen (HBsAg) test, cross-matching for blood transfusion if required, and an ECG (electrocardiogram) to assess heart function.
Explain the Procedure to the Patient:
- Provide a detailed explanation of the surgical procedure, its indications, and contraindications. Address any fears and anxieties the patient may have regarding the surgery.
Consultation with the Patient and Their Family Members:
- Discuss the surgical plan and post-operative care with the patient and their family members to ensure understanding and cooperation.
Prepare the Patient for Facial Wash:
- Advise the patient to wash their face on the morning of surgery, and instruct them to avoid applying any makeup or lotion around the eyes.
Ensure Nil by Mouth (NBM) for 4 to 8 Hours Before Surgery:
- Instruct the patient not to eat or drink anything for a specific period before the surgery, typically 4 to 8 hours, depending on institutional protocols.
Administer Mydriatic and Cycloplegic Eyedrops Before Surgery:
- These eyedrops dilate and paralyze the pupil, facilitating intraoperative maneuvers and reducing the risk of complications.
Administer Antibiotic and Antiemetic Drugs:
- Give antibiotics to prevent infection and antiemetics to prevent nausea and vomiting after surgery.
Post-Operative Care:
- Monitor the patient closely in the recovery area.
- Ensure adequate pain relief and comfort.
- Educate the patient and family on post-operative care instructions.
- Schedule follow-up visits as necessary.
Post-Operative Care After Cataract Surgery:
Monitor Patient’s Vital Signs:
- After completion of surgery, monitor the patient’s vital signs closely to ensure stability.
Check for Any Operating Room Symptoms:
- Assess if the patient experiences any symptoms related to the surgery, such as pain or discomfort, and address them promptly.
Avoid Applying Pressure on the Operated Eye:
- Instruct the patient to avoid touching or rubbing the operated eye to prevent any undue pressure.
Avoid Pressure on the Opposite Side of the Operating Eye:
- Advise the patient to be cautious about applying pressure on the opposite side of the operated eye to prevent discomfort.
Demonstrate Eye Drop Installation Technique:
- Demonstrate and explain the correct technique for instilling eye drops to the patient to ensure proper administration for healing.
Recommend Eye Shield Wear:
- Encourage the patient to wear an eye shield to protect the eye and prevent accidental injury during the initial recovery period.
Advise Against Sneezing, Coughing, and Straining:
- Instruct the patient to avoid sneezing, coughing forcefully, or straining as these actions can increase intraocular pressure and potentially affect the surgical outcome.
Avoid Heavy Lifting:
- Advise the patient to avoid heavy lifting and strenuous activities that could strain the eyes during the recovery period.
Discharge Instructions:
- Provide written and verbal instructions on post-operative care, including medication schedules and follow-up appointments.
- Ensure the patient understands the importance of adherence to prescribed eye drops and medications.
- Schedule a follow-up visit to assess the healing progress and remove any sutures if necessary.
- Emergency contact information: Provide contact details for any urgent queries or concerns post-discharge.
🔸c) Write down about mitral stenosis –
Mitral Stenosis Overview:
Definition: Mitral stenosis is a form of valvular heart disease where the opening (or orifice) of the mitral valve becomes narrowed, restricting blood flow from the left atrium to the left ventricle. This narrowing causes blood to back up into the left atrium.
Causes of Mitral Stenosis:
- Rheumatic Fever: A complication of untreated streptococcal throat infection.
- Congenital Heart Defect: Birth defects affecting the structure of the mitral valve.
- Infective Endocarditis: Infection of the inner lining of the heart.
- Autoimmune Diseases (e.g., SLE): Conditions where the immune system attacks healthy tissues.
- Age-related Degeneration: Wear and tear over time causing calcification of the mitral valve.
Signs and Symptoms of Mitral Stenosis:
- Shortness of Breath: Especially after exertion or at night (orthopnea).
- Orthopnea: Difficulty breathing when lying flat.
- Fatigue and Weakness: Due to reduced cardiac output.
- Heart Palpitations: Sensation of irregular heartbeats.
- Irregular Heartbeat: Arrhythmias such as atrial fibrillation.
- Chest Pain: Typically on exertion (angina).
- Swelling in Ankles and Feet: Due to fluid retention (edema).
- Cough: Often associated with respiratory infections.
- Loud, rumbling heart murmur: Heard during physical examination.
Diagnostic Evaluation of Mitral Stenosis:
- History Collection: Detailed medical history to identify risk factors and symptoms.
- Physical Examination: Including listening for heart murmurs and signs of heart failure.
- Echocardiogram (Echo): Ultrasound imaging to assess the structure and function of the heart.
- Electrocardiogram (ECG): Measures the electrical activity of the heart.
- Cardiac Catheterization: Invasive procedure to measure pressure and obtain imaging of the heart.
- Chest X-ray, MRI, and CT Scan: Imaging modalities to assess heart and lung status.
Medical Management of Mitral Stenosis:
- Diuretics: To reduce pulmonary congestion and fluid overload.
- Beta-Blockers / Calcium Channel Blockers: Control heart rate and relieve symptoms like dyspnea and palpitations.
- Anticoagulants: Prevent blood clots and thromboembolism.
- Antiarrhythmic Medications: Manage irregular heart rhythms.
Surgical Management of Mitral Stenosis:
- Valve Repair: Surgical techniques such as commissurotomy to separate fused valve leaflets.
- Balloon Valvuloplasty: Minimally invasive procedure using a catheter with an inflated balloon to widen the narrowed valve opening.
- Valve Replacement: Surgical removal of the damaged valve and replacement with a mechanical or bioprosthetic valve.
Mitral stenosis requires careful management to alleviate symptoms, prevent complications, and improve quality of life. Treatment options depend on the severity of the condition and individual patient factors. Regular follow-up and adherence to treatment plans are crucial for long-term management.
⏩Q-4 Write short notes.
🔸a) Meniere’s disease –
Meniere’s disease is an inner ear disorder that affects the auditory system (hearing) and vestibular system (balance). It is characterized by sudden and recurrent episodes of vertigo, hearing loss, and tinnitus.
Etiology of Meniere’s disease
The exact cause of Meniere’s disease is unknown, but it is believed to involve abnormalities in the endolymphatic system (endolymphatic fluid) within the inner ear.
- Here are the terms translated from Gujarati to English:
- Fluid imbalance
- Improper fluid drainage
- Genetic factor
- Immune system disorder
- Head injury
- Viral infection
- Anatomical abnormality
Clinical manifestations of Meniere’s disease
- Vertigo
- Hearing loss
- Tinnitus
- Fullness of ear
- Nausea
- Vomiting
- Headache
- Nystagmus
Diagnostic evaluation of Meniere’s disease
- History collection
- Physical examination
- Audiometry
- Electronystagmography
- Posturography
- MRI
Medical management of Meniere’s disease
There is no cure for Meniere’s disease, but medications are provided to relieve symptoms:
- Antihistamines
- Antiemetics
- Diuretics
- Corticosteroids
- Sedatives
Surgical management of Meniere’s disease
1) Endolymphatic sac decompression
2) Labyrinthectomy
3) Vestibular neurectomy
4) Cryosurgical method
🔸b) Types of disaster –
1.Natural disaster (નેચરલ ડિઝાસ્ટર)
Natural disasters are recognized as natural calamities that cause significant damage, loss of life, and disruption due to weather or environmental events.
- Earthquake (અર્થકવેક): Ground shaking and violent movement due to tectonic plate movement. Causes building collapse, infrastructure damage, landslides.
- Volcanic eruption (વોલકેનિક ઇરપ્શન): Explosion or effusive magma, ash, and gas release from volcanoes. Results in lava flow, ash clouds, air travel disruption, health hazards.
- Tsunami (ત્સુનામી): Series of large waves caused by undersea disturbances. Leads to coastal flooding, infrastructure disruption, significant loss of life.
- Flood (પુર): Overflow of water on dry land, covering it. Causes water damage, property destruction, contamination of water supply.
- Cyclone (સાયકલોન), Typhoon, Hurricane (વાવાઝોડું): Powerful tropical storms characterized by high winds and heavy rainfall.
- Tornado (ટોર્નેડો): Violently rotating column of air in contact with the surface and associated with cumulonimbus clouds.
- Drought (ડ્રોટ): Extended period without rainfall leading to water shortages. Causes crop failure, water scarcity, and wildfires.
- Landslide and Mudslide (ભૂસ્ખલન): Downhill movement of rock, soil, and debris identified as landslides. Causes property damage, road blockages, fatalities, and injuries.
- Wildfires (વાઇલ્ડફાયરસ): Uncontrolled fires in forests. Leads to forest destruction, property loss, air quality degradation, loss of life.
- Blizzard and Snowstorm (હિમવર્ષા): Severe snowstorm with high winds and low visibility. Causes transportation disruptions, hypothermia, infrastructure damage.
- Heatwave (હિટવેવ): Prolonged excessive heat over a period of time. Identified as a heatwave. Results in heatstroke, agricultural damage.
- Dust storm (ડસ્ટ સ્ટ્રોમ): Large amount of dust in the air due to strong winds. Causes reduced visibility, respiratory health issues.
🔸 Man-made Disaster (મેન મેડ ડિઝાસ્ટર)
Man-made disasters are identified as anthropogenic disasters, which are events caused by human actions and negligence. These events have significant impacts on human health, infrastructure, and the environment.
- Industrial Accident (ઇન્ડસ્ટ્રીયલ એક્સિડન્ટ): Accidents such as chemical spills, explosions, toxic releases resulting in significant impact on human life. Examples include the Bhopal Gas Tragedy (1984).
- Nuclear Accident (ન્યુક્લિયર એક્સિડન્ટ): Release of radioactive material due to nuclear power plant failures. Example: Chernobyl Disaster – Ukraine.
- Environmental Pollution (એનવાયરમેન્ટલ પોલ્યુશન): Long-term environmental degradation due to deforestation, improper waste disposal, air, and water pollution.
- Transportation Accident (ટ્રાન્સપોર્ટેશન એક્સિડન્ટ): Major accidents involving vehicles, trains, ships, and airplanes causing significant casualties and property damage.
- Structural Failure (સ્ટ્રકચરલ ફેલિયર): Collapse of buildings, bridges, and other structures due to design flaws, maintenance failures, or poor construction. Example: Morbi Bridge Collapse.
- Conflict and Terrorism (કોન્ફ્લિક્ટ એન્ડ ટેરિરીઝમ): Wars, terrorist acts leading to significant disruption, displacement, and loss of life. Example: Syrian Civil War, 9/11 Attacks in the United States (2001).
🔸c) Gonorrhoea –
- Gonorrhea is a sexually transmitted infection caused by the bacterium Neisseria gonorrhoeae.
- It primarily affects the genital, rectal, and throat areas.
- Gonorrhea spreads through sexual contact with an infected person.
Causes and risk factors of gonorrhea:
Gonorrhea is caused by the bacterium Neisseria gonorrhoeae.
It spreads through sexual contact or perinatal transmission.
- Unprotected sex
- Multiple sexual partners
- Previous or existing sexually transmitted diseases
- Pregnant mothers (can pass gonorrhea to their babies)
- Young age
Signs and symptoms of gonorrhea in men:
- Painful urination
- Pus-like discharge from the tip of the penis
- Swelling or pain in the testicles
- Persistent sore throat
Signs and symptoms of gonorrhea in women:
- Increased vaginal discharge
- Painful urination
- Vaginal bleeding
- Abdominal and pelvic pain
- Pain during intercourse
- Persistent sore throat
- Rectal infection
Diagnostic evaluation of gonorrhea:
- History collection
- Physical examination
- Nucleic acid amplification test (NAAT)
- Culture test
Medical management of gonorrhea:
First-line treatment:
Ceftriaxone: 500 mg intramuscular – single dose
Azithromycin: 1 gm orally – single dose
Alternative treatment for patients allergic to cephalosporins:
- Gentamicin: 240 mg intramuscular
- Azithromycin: 2 gm orally – single dose
- Nursing management of gonorrhea:
- Collect proper patient history.
- Conduct serum examination for syphilis.
- Provide education on personal hygiene.
- Educate the patient about the disease condition and how to solve all doubts and queries.
- Advise the patient to avoid multiple sexual partners.
- Provide education on contraceptive methods and barrier methods.
- Provide psychological support.
- Provide antibiotic medicine to prevent infection.
- Advise substance practice.
- Advise good personal hygiene maintenance.
🔸d) Hospice care
Hospice care is a type of healthcare that provides comfort and support to individuals with terminal illness (those expected to live less than six months). The primary goal of hospice care is to improve the quality of life of patients in their final stage of illness, focusing on managing pain and other symptoms.
Key aspects:
Patient-centered care: Hospice care prioritizes providing care based on the needs and wishes of the patient.
Symptom management: It involves managing the patient’s symptoms while providing care. This includes pain relief, management of nausea and shortness of breath, and emotional and spiritual support.
Interdisciplinary team: Hospice care is provided by a team comprising doctors, nurses, social workers, spiritual advisors, and volunteers. All team members work together to support the patient and their family.
Family support: Hospice care also supports the patient’s family. They offer counseling, provide respite care (relief) during caregiving, offer emotional support during end-of-life care, and assist in managing challenges that arise during care.
Settings: Hospice care can be provided in various settings such as home, hospice centers, hospitals, and nursing homes.
Bereavement (grief): After the patient’s death, hospice care provides grief support to family members.
Hospice care is designed to ensure that patients with terminal illnesses receive compassionate and comprehensive care that respects their dignity and focuses on enhancing their quality of life during their final days.
⏩Q-5 Define following (any six) (12)
🔸a) Eczema –
Eczema is a chronic inflammatory skin condition, also known as atopic dermatitis, characterized by itchy, red, and dry skin.
🔸b) Epistaxis –
Epistaxis means nosebleed or nasal hemorrhage.
It occurs when vessels in any area of the mucous membrane lining the nostrils or nasal cavity rupture and bleed, which is identified as epistaxis.
🔸c) Metastasis –
Metastasis refers to the spread of cancer cells from the primary site to other areas of the body. A cancerous tumor may spread to a secondary site (another area) from its primary site, which is recognized as metastasis.
- Localized Metastasis: Cancer spreads to nearby tissues, lymph nodes, or organs from where it started.
- Regional Metastasis: Cancer spreads to nearby lymph nodes, tissues, or organs.
- Distant Metastasis: Cancer spreads to distant areas of the body beyond nearby tissues or organs.
Metastasis is a critical aspect in cancer progression and staging, influencing treatment decisions and prognosis.
🔸d) Angina Pectoris –
Angina pectoris is recognized as “ischemic chest pain.”
Angina pectoris is a medical term used to describe “chest pain” or “discomfort” due to coronary heart disease.
Angina is not a disease itself but rather a symptom seen in coronary artery disease.
Due to the buildup of plaque deposits in the coronary arteries, they become narrowed, which restricts the full delivery of blood and oxygen to the heart muscles, leading to chest pain.
🔸e) Allograft –
An allograft is a type of tissue graft collected from a donor of the same species (genetically non-identical) and transplanted into a recipient of the same species.
Allografts involve the transplantation of tissue collected from one organism to another within the same species, typically from a donor to a recipient who is not genetically identical. This procedure is commonly used in medical treatments such as skin grafts or organ transplants.
🔸f) Incubation period –
The incubation period refers to the time interval between exposure to an infectious agent (bacteria, virus) and the appearance of the first signs and symptoms. It is identified as the time during which the infection silently develops within the body before symptoms become apparent. For example:
- Influenza: 1-4 days
- COVID-19: 2-14 days
- Chickenpox: 10-21 days
🔸g) Epidemic –
An epidemic refers to the rapid spread of a disease within a short period, affecting a particular region or group of people significantly. It typically affects a large portion of the population within that area. For example, the outbreak of pneumonic plague in Surat.
Epidemics are characterized by the sudden increase in cases of a disease beyond what is normally expected in that population during that time period. They often require coordinated public health responses to contain and manage the spread of the disease.
🔸h) Cardiac Tamponade?
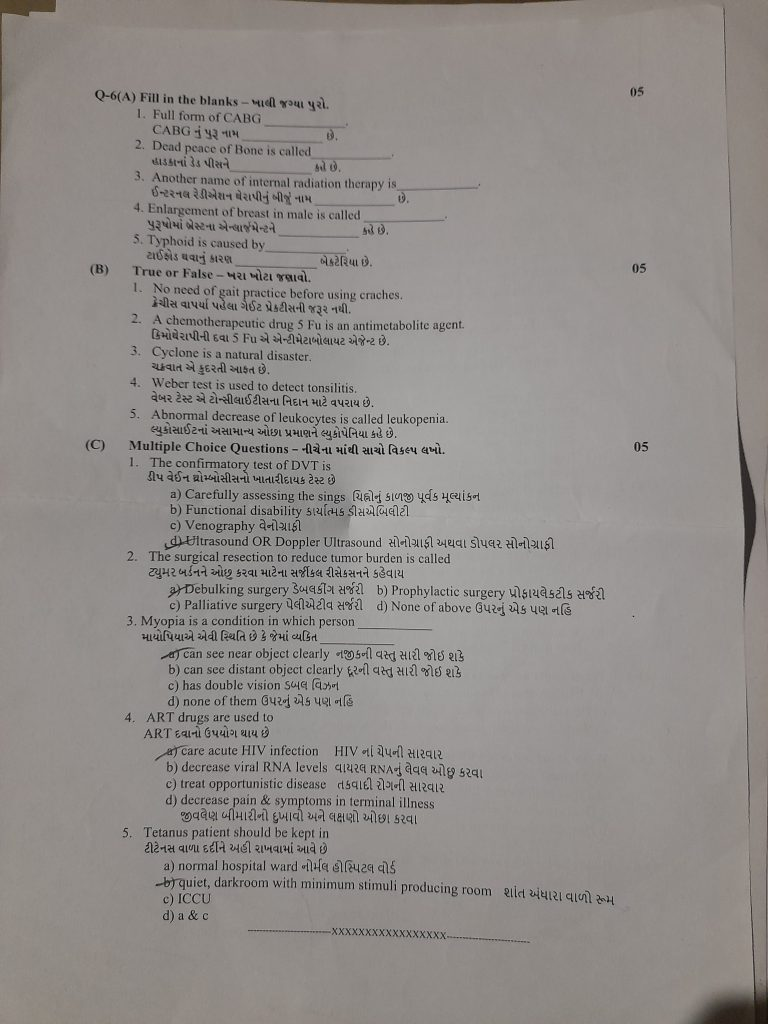
⏩Q-6(A) Fill in the blanks .(05)
1.) Full form of CABG———— Coronary artery bypass graft
2.) Dead peace of Bone is called——— Sequestrum
3.) Another name of internal radiation therapy is——— Brachytherapy
4.) Enlargement of breast in male is called————— Gynecomastia
5.) Typhoid is caused by———— bacterium Salmonella Typhi
⏩(B) ટાઈોક થવાનું કારણ True or False
1.)No need of gait practice before using craches. (FALSE
2.) A chemotherapeutic drug 5 Fu is an antimetabolite agent. (TRUE
3.) Cyclone is a natural disaster. (TRUE
4.)Weber test is used to detect tonsilitis. (FALSE-
5.)Abnormal decrease of leukocytes is called leukopenia. (TRUE
💪 💥☺☺ALL THE BEST ☺☺💥💪
Note: Clicking on “અ” will change the language to English and display the paper solution.