CHN-FAMILY PLANNING-SYNOPSIS-8-PHC
📘 TERMS USED IN FAMILY PLANNING
🧠 For Nursing Competitive Exams – NORCET, AIIMS, RRB, NHM, ESIC, NCLEX
🔰 1. Family Planning
🔹 The practice of controlling the number and spacing of children in a family using various contraceptive methods.
🧠 Goal: Improve health, prevent unwanted pregnancies, and promote informed reproductive choices.
🔰 2. Contraception
🔹 Methods or devices used to prevent pregnancy.
✳️ Includes barrier, hormonal, intrauterine, surgical, and natural methods.
🔰 3. Spacing Methods
🔹 Temporary contraceptives used to delay or space childbirth.
📌 Examples: Condoms, oral pills, IUCD, injectables
🔰 4. Permanent Methods
🔹 Sterilization procedures for males and females to permanently prevent conception.
📌 Female: Tubectomy | Male: Vasectomy
🔰 5. Total Fertility Rate (TFR)
🔹 The average number of children a woman would have during her reproductive years.
📌 Replacement level: 2.1
🔰 6. Eligible Couple
🔹 A currently married couple where the wife is in the reproductive age group (15–49 years).
🔰 Unmet Need for Contraception
🔹 When a woman wants to avoid pregnancy but is not using any contraceptive method.
🔰 Birth Control
🔹 General term for methods that prevent conception and unwanted births.
🔰 Sterilization
🔹 A permanent method of contraception.
✅ Male: Vasectomy
✅ Female: Tubectomy
🔰 IUCD (Intrauterine Contraceptive Device)
🔹 A device inserted into the uterus to prevent pregnancy.
📌 Example: Cu-T 380A – provides protection for 10 years.
🔰 Centchroman (Chhaya)
🔹 A non-hormonal oral contraceptive pill taken weekly.
✅ Free under national program
🔰 Antara
🔹 A DMPA injectable contraceptive, given every 3 months, provided under government program.
🔰 Lactational Amenorrhea Method (LAM)
🔹 A natural contraceptive method effective for 6 months postpartum if exclusively breastfeeding.
🔰 MTP (Medical Termination of Pregnancy)
🔹 A legally approved method to terminate pregnancy safely under the MTP Act in India.
🔰 Barrier Methods
🔹 Prevent sperm from reaching the egg.
📌 Example: Male/Female condoms
🔰 Oral Contraceptive Pills (OCPs)
🔹 Pills containing estrogen + progesterone, taken daily to prevent ovulation.
📌 Govt brands: Mala-D, Mala-N
📦 Government-Supplied Contraceptives & Their Names
| 🩺 Method | 📌 Brand Name |
|---|---|
| Male Condom | Nirodh |
| Oral Pills | Mala-N / Mala-D |
| Weekly Pill | Chhaya |
| Injectable (DMPA) | Antara |
| IUCD | Cu-T 380A |
🧠 Top MCQs to Remember
✅ Q1. Who is considered an eligible couple?
🅰️ Married woman aged 15–49 years
✅ Q2. What is the full form of IUCD?
🅰️ Intrauterine Contraceptive Device
✅ Q3. What is the duration of protection by Cu-T 380A?
🅰️ 10 years
✅ Q4. What is Centchroman used for?
🅰️ Non-hormonal weekly oral contraceptive (Chhaya)
✅ Q5. What is the replacement level of fertility?
🅰️ TFR = 2.1
👨👩👧👦 FAMILY PLANNING
🧠 Essential for Nursing Competitive Exams – NORCET, AIIMS, RRB, NHM, ESIC, NCLEX
🔰 Definition
Family Planning is the practice of controlling the number and spacing of children in a family through the use of contraceptive methods, sexual education, and fertility regulation.
It promotes maternal-child health, women’s empowerment, and sustainable population growth.
🎯 Objectives of Family Planning
✅ Prevent unwanted pregnancies
✅ Promote planned births and healthy spacing
✅ Improve maternal and child health
✅ Control population growth
✅ Reduce infant and maternal mortality
📜 Family Planning in India – Key Milestones
| 📅 Year | 🏛️ Development |
|---|---|
| 1952 | India became the 1st country to launch an official Family Planning Program |
| 1977 | Shift from “population control” → “family welfare” |
| 2000 | Included in National Population Policy |
| Current | Part of Reproductive and Child Health (RCH-II) and Mission Parivar Vikas |
🧰 Family Planning Methods
🔹 1. Temporary Methods (Spacing Methods)
| 🩺 Method | 🧠 Description |
|---|---|
| Condoms (Male/Female) | Barrier method; also prevents STIs |
| Oral Pills (COCs) | Combined estrogen + progesterone pills |
| POP (Mini Pills) | Progesterone-only pills (for lactating) |
| IUCD (Copper-T / LNG-IUS) | Inserted into uterus; long-term protection |
| Injectables (DMPA) | Given every 3 months IM |
| Emergency Contraception | Within 72 hrs of unprotected sex |
🔹 2. Permanent Methods (Sterilization)
| ⚙️ Method | 📌 Key Point |
|---|---|
| Tubectomy (Female) | Fallopian tubes are cut/blocked |
| Vasectomy (Male) | Vas deferens is cut/blocked (less invasive) |
🔹 3. Natural Methods
- Rhythm Method (Calendar)
- Withdrawal Method
- Lactational Amenorrhea Method (LAM) – effective up to 6 months if exclusively breastfeeding
👩⚕️ Nursing Responsibilities in Family Planning
✔️ Educate couples about available contraceptives
✔️ Maintain privacy and confidentiality
✔️ Provide free government-supplied contraceptives (e.g., condoms, IUCD)
✔️ Encourage male involvement
✔️ Monitor for side effects and follow-up
✔️ Refer for sterilization procedures or complications
📦 Free Contraceptives Provided Under National Program
| 🆓 Method | 💡 Name/Brand |
|---|---|
| Condoms | Nirodh |
| Oral Pills | Mala-N / Mala-D |
| IUCD | Cu-T 380A |
| Injectable | Antara |
| Centchroman (Non-hormonal) | Chhaya (weekly pill) |
🧠 High-Yield MCQs
✅ Q1. Which country launched the first national family planning program?
🅰️ India (1952)
✅ Q2. What is the duration of protection by Cu-T 380A?
🅰️ 10 years
✅ Q3. What is the government-supplied oral contraceptive brand?
🅰️ Mala-D / Mala-N
✅ Q4. Which contraceptive is safe during lactation?
🅰️ Progesterone-only pill (POP) or LAM
✅ Q5. What is the injectable contraceptive provided by Govt of India?
🅰️ Antara (DMPA)
👨👩👧👦 FAMILY PLANNING PROGRAMS IN INDIA
🧠 For Nursing Competitive Exams – NORCET, AIIMS, RRB, NHM, ESIC, NCLEX
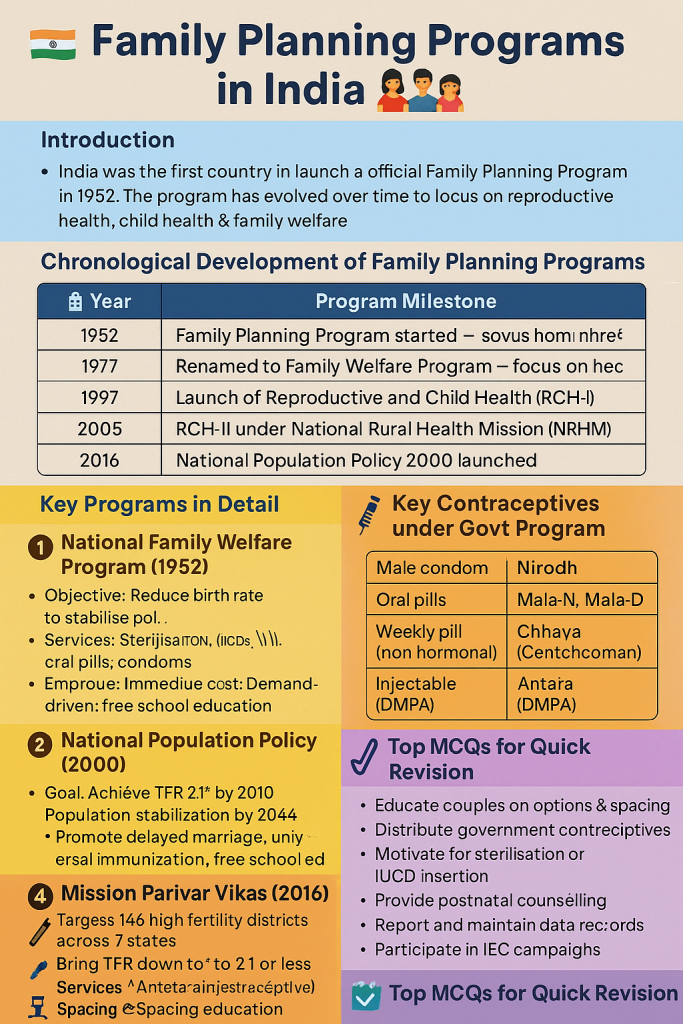
🔰 Introduction
India was the first country in the world to launch an official Family Planning Program in 1952. The program has evolved over time to focus on reproductive health, child health, and family welfare, not just population control.
🧭 Chronological Development of Family Planning Programs
| 📅 Year | 🏛️ Program Milestone |
|---|---|
| 1952 | Family Planning Program started – world’s first government-led population control effort |
| 1977 | Renamed to Family Welfare Program – focus on health and voluntary choice |
| 1997 | Launch of Reproductive and Child Health (RCH-I) program |
| 2005 | RCH-II under National Rural Health Mission (NRHM) |
| 2000 | National Population Policy 2000 launched |
| 2016 | Mission Parivar Vikas launched for high-fertility districts |
📘 Key Programs in Detail
1️⃣ National Family Welfare Program (1952)
🔹 Objective: Reduce birth rate to stabilize population
🔹 Services: Sterilization, IUCDs, oral pills, condoms
🔹 Approach: Initially target-based (now demand-driven)
2️⃣ National Population Policy (2000)
🎯 Goal: Achieve replacement level fertility (TFR 2.1) by 2010
🎯 Ultimate Aim: Population stabilization by 2045
🔹 Immediate focus on contraceptive services, maternal health, child survival
🔹 Promote delayed marriage, universal immunization, free school education
3️⃣ Reproductive and Child Health (RCH) Programme
| 🧩 RCH-I (1997) | RCH-II (2005 onwards) |
|---|---|
| Integrates FP, MCH, and immunization | Focuses on quality of care, skilled birth attendance |
| Includes RTI/STI management | Includes Janani Suraksha Yojana (JSY) and safe abortion services |
4️⃣ Mission Parivar Vikas (2016)
📍 Target: 146 high fertility districts across 7 states (UP, Bihar, MP, Chhattisgarh, Assam, Jharkhand, Rajasthan)
🎯 Aim: Bring TFR down to 2.1 or less
🧰 Services include:
✔️ Antara (injectable contraceptive)
✔️ Chhaya (Centchroman pill – weekly)
✔️ IUCDs, sterilization, spacing education
📦 Key Contraceptives under Govt Program
| 🆓 Method | 💡 Brand Name |
|---|---|
| Male Condom | Nirodh |
| Oral Pills | Mala-N, Mala-D |
| Weekly Pill (non-hormonal) | Chhaya (Centchroman) |
| Injectable | Antara (DMPA) |
| IUCD | CuT 380A (10 years) |
👩⚕️ Role of Nurse in Family Planning Program
✔️ Educate couples on options & spacing
✔️ Distribute government contraceptives
✔️ Motivate for sterilization or IUCD insertion
✔️ Provide postnatal counseling
✔️ Report and maintain data records
✔️ Participate in IEC campaigns
🧠 Top MCQs for Quick Revision
✅ Q1. In which year did India launch its first family planning program?
🅰️ 1952
✅ Q2. What is the goal TFR under National Population Policy 2000?
🅰️ 2.1
✅ Q3. Mission Parivar Vikas targets which type of districts?
🅰️ High fertility districts
✅ Q4. Which injectable contraceptive is provided under national program?
🅰️ Antara
✅ Q5. Which is the non-hormonal weekly pill promoted in India?
🅰️ Chhaya (Centchroman)
🌿 NATURAL METHODS OF FAMILY PLANNING
🧠 For Nursing Competitive Exams – NORCET, AIIMS, NHM, RRB, ESIC, NCLEX
🔰 Definition
Natural methods of family planning are techniques used to prevent pregnancy without using any devices, drugs, or surgery. These methods are based on awareness of the fertile period in a woman’s menstrual cycle.
🌱 Advantages of Natural Methods
✅ No side effects
✅ Cost-free
✅ Culturally acceptable
✅ Promotes body awareness and partner communication
🚫 Limitations
❌ Less reliable (80–85% effective)
❌ Requires discipline & accurate tracking
❌ Not suitable for irregular cycles
❌ No protection from STIs/HIV
📘 Types of Natural Family Planning Methods
1️⃣ 📆 Calendar Method (Rhythm Method)
🔹 Avoid intercourse during the fertile period (Day 10–17 in a 28-day cycle)
🔹 First fertile day = Shortest cycle – 18
🔹 Last fertile day = Longest cycle – 11
🔹 Requires 6 months of cycle tracking
2️⃣ 🌡️ Basal Body Temperature (BBT) Method
🔹 Track body temperature daily before getting out of bed
🔹 After ovulation, temperature rises by 0.5°F to 1°F
🔹 Avoid intercourse 2–3 days before and after rise in BBT
3️⃣ 💧 Cervical Mucus Method (Billings Method)
🔹 Observe changes in vaginal mucus:
✅ Sticky/dry = infertile
✅ Clear, stretchy, egg-white mucus = fertile
🔹 Avoid intercourse during fertile mucus days
4️⃣ 🔄 Symptothermal Method
🔹 Combination of:
✔️ Calendar method
✔️ BBT
✔️ Cervical mucus
✔️ Breast tenderness, ovulation pain
🔹 Most accurate of natural methods
5️⃣ 👶 Lactational Amenorrhea Method (LAM)
🔹 Used during first 6 months postpartum
🔹 Effective if:
✔️ Exclusively breastfeeding
✔️ No menses resumed
✔️ Baby < 6 months
🔸 98% effective if all conditions met
🧠 Nursing Responsibilities
👩⚕️ Educate couples on:
✔️ Correct method usage
✔️ Cycle tracking and fertile period
✔️ Limitations of each method
✔️ Importance of motivation & regularity
✔️ Counseling for switching to other methods if needed
📌 Quick MCQs for Revision
✅ Q1. Which method is based on cervical mucus observation?
🅰️ Billings method
✅ Q2. What is the fertile period in a 28-day cycle?
🅰️ Day 10 to 17
✅ Q3. LAM is effective for how long?
🅰️ First 6 months postpartum if exclusively breastfeeding
✅ Q4. Which natural method is most accurate?
🅰️ Symptothermal method
✅ Q5. What happens to BBT after ovulation?
🅰️ It rises by 0.5°F to 1°F
🧤👩⚕️ MALE CONDOM & FEMALE DIAPHRAGM
🧠 Complete Overview for Nursing Competitive Exams – NORCET, AIIMS, NHM, RRB, ESIC
🧤 1️⃣ MALE CONDOM
🔰 Definition
A male condom is a flexible, sheath-like barrier (usually latex or polyurethane) worn over the penis during intercourse to prevent sperm from entering the vagina.
⚙️ Mechanism of Action
✔️ Mechanical barrier
✔️ Prevents sperm from reaching the egg
✔️ Also prevents STIs including HIV
📉 Failure Rates
| 🧪 Type of Use | 📊 Failure Rate (per 100 women/year) |
|---|---|
| Typical Use | 13% (due to breakage, slippage, incorrect use) |
| Perfect Use | 2% or less |
📦 Key Features
| 🔹 Parameter | 🔍 Detail |
|---|---|
| Material | Latex, polyurethane, or lambskin |
| Protection against STIs | ✅ Yes (except lambskin) |
| Duration | Single use per intercourse |
| Available from Govt. | Nirodh (free supply) |
| Disposal | Wrap & discard in closed bin (not flushable) |
✅ Advantages
✔️ Widely available (OTC)
✔️ Cheap and effective
✔️ Prevents both pregnancy + infections
✔️ No systemic side effects
❌ Disadvantages
❌ May break or slip
❌ Requires compliance with every act
❌ Some may experience latex allergy
👩⚕️ Nursing Responsibilities
- Teach correct use with demonstration (banana model)
- Check expiry date and storage conditions
- Encourage dual protection (with OCP or injectable)
- Educate against using oil-based lubricants with latex condoms
👩⚕️ 2️⃣ FEMALE DIAPHRAGM
🔰 Definition
A female diaphragm is a flexible rubber or silicone cup inserted into the vagina before intercourse to cover the cervix, preventing sperm from entering the uterus.
⚙️ Mechanism of Action
✔️ Cervical barrier
✔️ Used with spermicidal gel to immobilize sperm
✔️ Does not protect from STIs
📉 Failure Rates
| 🧪 Type of Use | 📊 Failure Rate (per 100 women/year) |
|---|---|
| Typical Use | 17–20% |
| Perfect Use | 6%–10% |
⚠️ Higher failure rate if not used with spermicide
📦 Key Features
| 🔹 Parameter | 🔍 Detail |
|---|---|
| Material | Latex or silicone rubber |
| Reusability | Yes (up to 1–2 years with care) |
| Insertion Time | Up to 6 hours before sex |
| Removal Time | Leave in for at least 6 hours after sex, max 24 hours |
| Fitting Requirement | ✅ Must be fitted by a trained provider |
✅ Advantages
✔️ Female-controlled method
✔️ No hormonal side effects
✔️ Reusable and cost-effective over time
❌ Disadvantages
❌ Requires insertion skill
❌ No protection from STIs/HIV
❌ May cause UTI or vaginal irritation
❌ Not suitable for women with cervical prolapse or recurrent UTI
👩⚕️ Nursing Responsibilities
- Teach insertion and removal technique
- Explain use with spermicidal jelly
- Educate on cleaning, drying, and storing
- Ensure refitting after childbirth or major weight change
- Counsel on emergency contraception if diaphragm dislodges
🧠 Golden MCQs for Practice
✅ Q1. Failure rate of male condom with typical use is—
🅰️ 13%
✅ Q2. Does the diaphragm protect against HIV?
🅰️ ❌ No
✅ Q3. What is the name of the free male condom brand in India?
🅰️ Nirodh
✅ Q4. How long must diaphragm be kept after sex?
🅰️ Minimum 6 hours
✅ Q5. What is the key requirement for diaphragm effectiveness?
🅰️ Use with spermicide
🧫🧬 INTRAUTERINE CONTRACEPTIVE DEVICES (IUCDs)
🧠 Complete Overview for NORCET, AIIMS, NHM, RRB, ESIC, NCLEX
🔰 Definition
Intrauterine Contraceptive Devices (IUCDs) are long-acting, reversible contraceptives (LARCs) inserted into the uterus to prevent pregnancy.
They are safe, effective, and widely used in national family planning programs.
⚙️ Mechanism of Action
- 🧬 Copper IUCD: Releases copper ions that are toxic to sperm, preventing fertilization
- 💊 Hormonal IUCD (LNG-IUS): Releases Levonorgestrel, thickens cervical mucus & suppresses endometrium
- 🌡️ Alters uterine environment, preventing implantation
📚 Types of IUCDs
| 🧪 Generation | 🔍 Type | 🧠 Examples | ⏳ Duration |
|---|---|---|---|
| 1st Gen | Inert | Lippes Loop | ❌ Obsolete |
| 2nd Gen | Copper-bearing | Cu-T 200B, Cu-T 380A, PPIUCD | Cu-T 380A = 10 years |
| 3rd Gen | Hormone-releasing | LNG-IUS (Mirena), Progestasert | 3–5 years (Mirena = 5 yrs) |
🔷 Common IUCDs Used in India
1️⃣ Cu-T 380A
🔹 Copper IUCD with 380 mm² copper surface
🔹 Effective for up to 10 years
🔹 Provided free under Government of India’s Family Planning Program
2️⃣ PPIUCD (Postpartum IUCD)
🔹 Specially designed Cu-T 380A inserted within 10 minutes to 48 hours after delivery
🔹 Offered to postpartum women during institutional delivery
🔹 Reduces chances of unintended pregnancy in early postpartum period
🔹 Strings are longer to facilitate later identification
3️⃣ LNG-IUS (Levonorgestrel-Releasing IUCD – e.g., Mirena)
🔹 Releases 20 mcg of levonorgestrel per day
🔹 Effective for 5 years
🔹 Also used to treat heavy menstrual bleeding & endometriosis
📉 Failure Rates
| 📊 Use Type | 🧫 Copper IUCD | 💊 Hormonal IUCD |
|---|---|---|
| Typical Use | ~0.6–0.8% | ~0.1–0.2% |
| Perfect Use | ~0.1% | ~0.1% |
✅ Advantages
✔️ Highly effective & reversible
✔️ Long duration (up to 10 years)
✔️ No need for daily action
✔️ Immediate return of fertility on removal
✔️ Safe during breastfeeding (esp. Cu-T)
✔️ Hormonal IUDs reduce menstrual bleeding and cramps
❌ Disadvantages / Side Effects
❌ Heavier, prolonged periods (copper IUD)
❌ Spotting or irregular bleeding (hormonal IUD)
❌ Risk of expulsion (2–10%), especially in postpartum insertions
❌ Rare risk of perforation if improperly inserted
❌ No protection from STIs/HIV
🛑 Contraindications
🔺 Pregnancy
🔺 Pelvic inflammatory disease (PID)
🔺 Current STI (gonorrhea, chlamydia)
🔺 Unexplained vaginal bleeding
🔺 Cervical/uterine cancer
🔺 Allergy to copper (for copper IUCD)
🧠 ‘PAINS’ Mnemonic – Danger Signs to Report
🔸 P: Period late (possible pregnancy)
🔸 A: Abdominal/pelvic pain
🔸 I: Infection signs (discharge, fever)
🔸 N: Not feeling well (systemic symptoms)
🔸 S: Strings missing or longer/shorter
👩⚕️ Nursing Responsibilities
✔️ Educate about mechanism, duration, and warning signs
✔️ Ensure screening for STIs before insertion
✔️ Maintain aseptic technique
✔️ Explain string check monthly by the user
✔️ Provide follow-up after 6 weeks and annually
✔️ Document and report any adverse events
📘 IUCD Services in National Program (India)
| 🩺 Service | 🧠 Details |
|---|---|
| Free IUCD | Cu-T 380A in PHCs/CHCs/SCs |
| Postpartum IUCD | Offered at institutional deliveries |
| Trained personnel | Doctors, nurses (after skill training) |
| Brands used | Cu-T 380A (Copper) / LNG-IUS (private setup) |
🧠 Top MCQs
✅ Q1. What is the duration of action of Cu-T 380A?
🅰️ 10 years
✅ Q2. When is a PPIUCD inserted?
🅰️ Within 10 minutes to 48 hours after delivery
✅ Q3. Hormonal IUCD used in India is—
🅰️ LNG-IUS (Mirena)
✅ Q4. What is the key danger sign post IUCD insertion?
🅰️ PAINS symptoms (Period late, Abdominal pain, etc.)
✅ Q5. Which IUCD is preferred in postpartum mothers?
🅰️ PPIUCD (Cu-T 380A, specially designed)
💊👩⚕️ ORAL CONTRACEPTIVE PILLS (OCPs)
🧠 Must-know for Nursing Competitive Exams – NORCET, AIIMS, NHM, RRB, ESIC, NCLEX
🔰 Definition
Oral contraceptive pills (OCPs) are hormonal medications taken by mouth to prevent pregnancy by inhibiting ovulation, altering cervical mucus, and modifying the endometrium.
📚 Types of Oral Contraceptive Pills
| 💊 Type | 🧠 Components | 👩⚕️ Who can use |
|---|---|---|
| 1. Combined Oral Pills (COCs) | Estrogen + Progestin | Most women with regular cycles |
| 2. Progestin-only Pills (POPs) | Progestin only | Breastfeeding women, those intolerant to estrogen |
| 3. Emergency Contraceptive Pills | High-dose hormones (Levonorgestrel) | Within 72 hours of unprotected sex |
📘 Examples of Pills Used in India
| 💊 Type | 📦 Brand Name | 🆓 Provided Under Govt. Program |
|---|---|---|
| Combined OCPs | Mala-N, Mala-D | ✅ Yes |
| Progestin-Only | Mini Pill, Cerazette | ❌ Private setup mostly |
| Non-hormonal Weekly | Centchroman (Chhaya) | ✅ Yes |
| Emergency Pill | iPill, Ezy Pill | ❌ (Available OTC) |
🎯 Mechanism of Action
🔹 Combined OCPs
✔️ Inhibit ovulation
✔️ Thicken cervical mucus
✔️ Alter endometrial lining
🔹 POPs (Mini Pills)
✔️ Thicken mucus
✔️ Reduce sperm motility
✔️ Suppress ovulation (not always)
📉 Effectiveness
| 📊 Type | ✅ Perfect Use | ❌ Typical Use |
|---|---|---|
| Combined Pills | ~99.7% | ~91% |
| POPs (Mini Pills) | ~99% | ~90% |
✅ Advantages
✔️ Highly effective when taken correctly
✔️ Regulates periods
✔️ Reduces cramps, acne, and PMS
✔️ POPs safe during lactation
✔️ Protects against ovarian and endometrial cancer
❌ Disadvantages & Side Effects
❌ Must be taken daily at the same time
❌ Nausea, breast tenderness, mood changes
❌ Spotting, weight gain (in some)
❌ No protection from STIs/HIV
❌ Risk of DVT (in smokers >35 years using COCs)
🛑 Contraindications
🔺 History of thromboembolism
🔺 Breast cancer or liver disease
🔺 Migraine with aura
🔺 Smokers >35 years (COCs)
🔺 Pregnancy
🧠 Key Instructions to Women
✔️ Start within 5 days of period
✔️ Take at same time daily
✔️ If missed 1 pill → take immediately + continue
✔️ Missed ≥2 pills → use backup method (condom)
✔️ Return for follow-up and side-effect monitoring
🧪 Non-Hormonal Oral Contraceptive (Centchroman)
🔹 Brand: Chhaya
🔹 Dose: One pill twice a week for 3 months, then once weekly
🔹 Mechanism: Delays ovum transport, prevents implantation
🔹 Advantage: No hormonal side effects, ideal for rural and adolescent use
🧠 Golden MCQs for Practice
✅ Q1. Which OCPs are provided by Govt. of India?
🅰️ Mala-N, Mala-D
✅ Q2. What is the active component of emergency pills?
🅰️ Levonorgestrel
✅ Q3. Which OCP is safe in breastfeeding?
🅰️ Progestin-only pill (POP)
✅ Q4. Centchroman is taken how often?
🅰️ Once weekly (after initial biweekly for 3 months)
✅ Q5. What is a major contraindication of COCs?
🅰️ History of thromboembolism
💉 INJECTABLE CONTRACEPTION
🧠 Must-Know for Nursing Competitive Exams – NORCET, AIIMS, NHM, RRB, ESIC, NCLEX
🔰 Definition
Injectable contraceptives are long-acting hormonal contraceptives given via intramuscular or subcutaneous injection to prevent pregnancy by inhibiting ovulation, altering cervical mucus, and modifying the endometrium.
📚 Types of Injectable Contraceptives
| 💉 Type | 💊 Drug Used | ⏳ Duration |
|---|---|---|
| Progestin-only (most common) | DMPA – Depot Medroxyprogesterone Acetate | 12 weeks (3 months) |
| Combined Injectable | Estrogen + Progestin (e.g., Cyclofem) | 1 month |
💉 DMPA (Depot Medroxyprogesterone Acetate)
- 📌 Brand (India – Govt.): Antara
- 📌 Dose: 150 mg IM injection every 12 weeks
- 📌 Route: Intramuscular (deltoid or gluteal)
⚙️ Mechanism of Action
✔️ Suppresses ovulation
✔️ Thickens cervical mucus to block sperm
✔️ Alters endometrial lining to prevent implantation
📉 Effectiveness
| 📊 Use Type | 📈 Pregnancy Rate per Year |
|---|---|
| Perfect Use | ~0.2% |
| Typical Use | ~6% |
✅ Highly effective when taken on schedule
✅ Advantages
✔️ Long-term protection (3 months)
✔️ No daily action required
✔️ Safe for breastfeeding mothers
✔️ Useful for women who can’t use estrogen
✔️ May reduce menstrual cramps, anemia, endometriosis
❌ Disadvantages / Side Effects
❌ Irregular bleeding or amenorrhea
❌ Delayed return of fertility (6–9 months)
❌ Weight gain, headache, mood changes
❌ Bone mineral density loss with long-term use
❌ No STI/HIV protection
🛑 Contraindications
🔺 Pregnancy
🔺 Breast cancer
🔺 Unexplained vaginal bleeding
🔺 Severe liver disease
🔺 Osteoporosis or risk factors for low bone density
🧠 Instructions for Use
🗓️ First dose: Within first 5 days of menstrual cycle
📆 Repeat every 12 weeks (3 months)
❗ If dose is late by >2 weeks: Use backup method (e.g., condom)
📋 Check weight, BP, menstrual history at each visit
👩⚕️ Nursing Responsibilities
✔️ Confirm no pregnancy before starting
✔️ Educate on timing and schedule of injections
✔️ Discuss side effects and delayed fertility
✔️ Encourage calcium + vitamin D intake (bone health)
✔️ Ensure client consent and follow-up charting
📘 Government of India Injectable Program
| 🔹 Drug | 💉 Name | 🏥 Where Available |
|---|---|---|
| DMPA 150 mg IM | Antara | PHCs, CHCs, District Hospitals |
| Centchroman | Chhaya (non-injectable) | Free under family welfare schemes |
🧠 MCQs for Revision
✅ Q1. Antara is the brand name of which contraceptive?
🅰️ DMPA injectable (Depot Medroxyprogesterone Acetate)
✅ Q2. What is the dose and schedule of DMPA?
🅰️ 150 mg IM every 3 months
✅ Q3. Can DMPA be given to lactating mothers?
🅰️ Yes, it is safe
✅ Q4. What is a long-term side effect of injectable DMPA?
🅰️ Decreased bone mineral density
✅ Q5. What backup method is advised if DMPA is missed beyond 12 weeks?
🅰️ Use a barrier method like condom
⚠️💊 EMERGENCY CONTRACEPTIVE (EC) PILLS
🧠 Essential for Nursing Competitive Exams – NORCET, AIIMS, NHM, RRB, ESIC, NCLEX
🔰 Definition
Emergency contraceptives are methods used to prevent pregnancy after unprotected intercourse, contraceptive failure, or sexual assault.
🕒 Must be used within a specific time frame (up to 72–120 hours) to be effective.
📚 Types of Emergency Contraception
| 💊 Method | 🧠 Drug/Device | ⏳ Time Limit |
|---|---|---|
| 1. Pills (Hormonal) | Levonorgestrel 1.5 mg (single dose) | Within 72 hours (best < 24h) |
| Ulipristal Acetate 30 mg | Up to 120 hours (5 days) | |
| 2. IUCD (Copper-T 380A) | Copper IUCD inserted by doctor | Within 5 days of sex |
⚙️ Mechanism of Action
✔️ Inhibits or delays ovulation
✔️ Alters endometrial lining, preventing implantation
✔️ May inhibit fertilization by affecting sperm movement
❌ Does NOT work if implantation has already occurred
🩺 Common Brands in India
| 🏷️ Brand | 💊 Drug | 🏪 Availability |
|---|---|---|
| i-Pill, Ezy Pill | Levonorgestrel 1.5 mg | Over-the-counter (OTC) |
| EllaOne | Ulipristal acetate 30 mg | Prescription (Private) |
| Copper IUCD | Cu-T 380A | Govt health centers (on doctor order) |
📉 Effectiveness
| 💊 Type | ✅ Effectiveness |
|---|---|
| Levonorgestrel pill | ~85–89% (best < 24h) |
| Ulipristal acetate | ~95% |
| Copper IUCD | >99% (most effective) |
🧠 Indications for Use
🔹 Unprotected sex
🔹 Missed oral contraceptive pills
🔹 Condom rupture/slip
🔹 Sexual assault
🔹 Failed contraception (forgot injection/IUCD displacement)
❌ Contraindications
🔺 Known or suspected pregnancy
🔺 Severe liver dysfunction
🔺 Allergy to active drug
🔺 For IUCD: active pelvic infection, distorted uterus
⚠️ Side Effects
| 🧬 Side Effect | 💡 Notes |
|---|---|
| Nausea, vomiting | Common – take with food or antiemetic |
| Headache, dizziness | Mild and temporary |
| Menstrual changes | Early or delayed period possible |
| Breast tenderness | Occasionally seen |
📋 Nursing Responsibilities
👩⚕️ Counseling & Education:
✔️ Must be taken as early as possible
✔️ Not to be used as regular contraception
✔️ Encourage to start long-term contraception
✔️ Check for pregnancy if period is delayed >1 week
✔️ For IUCD – Ensure aseptic insertion and follow-up
🧠 Golden MCQs
✅ Q1. Levonorgestrel emergency pill should be taken within —
🅰️ 72 hours (best efficacy < 24 hours)
✅ Q2. Most effective emergency contraceptive method is —
🅰️ Copper-T IUCD (within 5 days)
✅ Q3. What is the dose of Levonorgestrel EC pill?
🅰️ 1.5 mg single dose
✅ Q4. Is emergency contraceptive effective if implantation has occurred?
🅰️ ❌ No
✅ Q5. Common side effect of EC pill is —
🅰️ Nausea and menstrual irregularity
💊🌼 CHHAYA – Non-Hormonal Weekly Oral Contraceptive
🧠 High-Yield Topic for Nursing Competitive Exams – NORCET, AIIMS, NHM, RRB, ESIC
🔰 What is Chhaya?
Chhaya is a non-hormonal, once-a-week oral contraceptive pill containing Centchroman.
It is provided free of cost under the Government of India’s Family Planning Program.
📛 Generic Name:
🔹 Centchroman (also called Ormeloxifene)
🧬 Type of Contraceptive
🔹 Non-hormonal oral contraceptive
🔹 Selective Estrogen Receptor Modulator (SERM)
⚙️ Mechanism of Action
✔️ Delays ovum transport in fallopian tubes
✔️ Alters endometrial receptivity, preventing implantation
✔️ Does not inhibit ovulation
✔️ No hormonal side effects like nausea or weight gain
📦 Dosage Schedule
| 📅 Duration | 💊 Dosage |
|---|---|
| First 3 months | 1 tablet twice a week (e.g., Sunday & Wednesday) |
| After 3 months | 1 tablet once a week (same day each week) |
📌 Start on 1st day of menstrual cycle
📉 Effectiveness
✔️ ~98% effective with correct use
❗ Lower if taken irregularly
✅ Advantages
✔️ Non-hormonal – No estrogen or progesterone
✔️ No effect on lactation – safe during breastfeeding
✔️ Minimal side effects
✔️ Easy weekly dosing
✔️ Provided free in public health centers
✔️ Reversible with rapid return of fertility
❌ Disadvantages / Side Effects
❌ Irregular periods (in first few months)
❌ Not effective if doses are missed
❌ No STI/HIV protection
❌ Requires strict adherence to weekly schedule
🛑 Contraindications
🔺 Known/suspected pregnancy
🔺 History of menstrual irregularity
🔺 Hypersensitivity to Centchroman
🔺 Severe liver disease
👩⚕️ Nursing Responsibilities
✔️ Educate on correct schedule (2/week for 3 months → then weekly)
✔️ Emphasize importance of regular timing
✔️ Check LMP to rule out pregnancy before starting
✔️ Encourage compliance and explain side effects (if any)
✔️ Offer follow-up & switch to another method if periods are persistently irregular
📘 Chhaya vs Mala-D
| 🧪 Aspect | 🌼 Chhaya | 💊 Mala-D (COC) |
|---|---|---|
| Type | Non-hormonal (Centchroman) | Hormonal (Estrogen + Progestin) |
| Dose frequency | Weekly | Daily |
| Breastfeeding safe? | ✅ Yes | ❌ Not recommended |
| Menstrual cycle | May be irregular | Regularizes cycle |
| Government supply | ✅ Free | ✅ Free |
🧠 MCQs for Quick Review
✅ Q1. What is the active drug in Chhaya pill?
🅰️ Centchroman
✅ Q2. How often is Chhaya taken after 3 months?
🅰️ Once a week
✅ Q3. Chhaya is safe for lactating mothers – True/False?
🅰️ ✅ True
✅ Q4. Is Chhaya hormonal?
🅰️ ❌ No (non-hormonal)
✅ Q5. Chhaya is supplied free under which program?
🅰️ National Family Welfare Program (India)
🩹💊 HORMONAL CONTRACEPTIVE PATCH
🧠 High-Yield for Nursing Competitive Exams – NORCET, AIIMS, NHM, RRB, ESIC, NCLEX
🔰 Definition
The hormonal contraceptive patch is a transdermal patch that delivers estrogen and progestin hormones through the skin into the bloodstream to prevent pregnancy.
📛 Brand Names
- 🌟 Evra® Patch
- 🌟 Xulane®
💊 Contents
- Ethinyl estradiol (Estrogen)
- Norelgestromin (Progestin)
⚙️ Mechanism of Action
✔️ Inhibits ovulation
✔️ Thickens cervical mucus → prevents sperm entry
✔️ Alters endometrial lining → prevents implantation
📅 Usage Schedule
| ⏱️ Application | 📋 Instructions |
|---|---|
| One patch/week | Apply on clean, dry, intact skin |
| 3 patches in 3 weeks | Week 1–3: New patch each week |
| Week 4 (Patch-free) | Menstruation occurs during this time |
🔁 Cycle repeats every 28 days
💯 Effectiveness
| 🧪 Use Type | 📊 Pregnancy Rate/year |
|---|---|
| Perfect use | ~99.7% |
| Typical use | ~91% |
✅ Advantages
✔️ Weekly use (No daily pill)
✔️ Highly effective
✔️ Predictable menstrual cycle
✔️ Improves acne and PMS symptoms
✔️ Easy to apply and non-invasive
❌ Disadvantages / Side Effects
❌ Skin irritation at patch site
❌ Breast tenderness, nausea
❌ Spotting between periods
❌ Risk of venous thromboembolism (VTE)
❌ No STI/HIV protection
🛑 Contraindications
🔺 Pregnancy
🔺 History of thrombosis/DVT/PE
🔺 Smoker over 35 years
🔺 Liver disease
🔺 Breast cancer
🔺 Uncontrolled hypertension or migraine with aura
👩⚕️ Nursing Responsibilities
👩⚕️ Educate on:
- Correct patch placement: upper arm, buttock, abdomen, or back
- Avoid applying on breasts or irritated skin
- Replace on the same day each week
- Check for detachment or skin rash
- Counsel on backup contraception if patch falls off for >24 hours
📌 Common Patch Sites
- Upper outer arm
- Abdomen (below waist)
- Buttock
- Upper back
🧠 High-Yield MCQs
✅ Q1. How often is the hormonal patch changed?
🅰️ Once a week for 3 weeks, 1 patch-free week
✅ Q2. What hormones are in contraceptive patches?
🅰️ Ethinyl estradiol + Norelgestromin
✅ Q3. Can a woman with DVT history use the patch?
🅰️ ❌ No (contraindicated)
✅ Q4. Is the patch safe in lactating mothers?
🅰️ ❌ No (contains estrogen)
✅ Q5. What to do if patch falls off for >24 hours?
🅰️ Use backup contraception and apply a new patch
♀️✂️ FEMALE STERILIZATION (TUBAL LIGATION)
🧠 Essential for Nursing Competitive Exams – NORCET, AIIMS, NHM, RRB, ESIC, NCLEX
🔰 Definition
Female sterilization is a permanent method of contraception in which the fallopian tubes are blocked, tied, or cut to prevent the egg from reaching the uterus for fertilization.
Also called Tubectomy or Tubal Ligation.
🎯 Purpose
✔️ Prevents pregnancy permanently
✔️ Suitable for women who have completed their family
📦 Methods of Female Sterilization
| 🧪 Method | 📝 Details |
|---|---|
| Mini-laparotomy (Mini-lap) | Small abdominal incision to access and block fallopian tubes |
| Laparoscopic sterilization | Uses a laparoscope to apply clips/rings/cautery |
| Postpartum sterilization (PPS) | Done within 48 hours after delivery |
| Interval sterilization | Done 6 weeks after delivery or during non-pregnant phase |
🔍 Procedure Details
🔹 Done under local or general anesthesia
🔹 Usually performed in PHCs, CHCs, and hospitals
🔹 Takes around 15–30 minutes
🔹 Patient is discharged same day or after 24 hours
📉 Effectiveness
💯 >99.5% effective
📌 Failure rate: 0.5–1 per 100 women over 10 years
✅ Advantages
✔️ Permanent method — no daily/weekly use
✔️ Cost-effective in the long term
✔️ No hormonal side effects
✔️ Can be done immediately after childbirth (PPS)
✔️ Does not affect sexual drive or menstruation
❌ Disadvantages / Complications
❌ Permanent (reversal is difficult and costly)
❌ Surgical risks: bleeding, infection, anesthesia-related issues
❌ Possible regret, especially in younger women
❌ Ectopic pregnancy if failure occurs
❌ No STI/HIV protection
🛑 Contraindications
🔺 Current pregnancy
🔺 Severe pelvic infection
🔺 Recent postpartum complications
🔺 Uncontrolled medical disorders
🔺 Lack of informed consent
📋 Government of India Guidelines
| 🔹 Parameter | 📘 Details |
|---|---|
| Minimum age | ✅ 22 years |
| Consent | ✅ Written informed consent mandatory |
| Number of living children | ✅ Preferably 1 or more |
| Incentives | ✅ Monetary incentive under Family Welfare Scheme |
👩⚕️ Nursing Responsibilities
👩⚕️ Pre-procedure:
✔️ Take detailed history & physical exam
✔️ Ensure counseling & informed consent
✔️ Verify non-pregnant status
✔️ NPO (nil by mouth) before surgery
👩⚕️ Post-procedure:
✔️ Monitor vitals, bleeding, pain
✔️ Educate on wound care, signs of infection
✔️ Advise rest for 1–2 days
✔️ Schedule follow-up visit
🧠 MCQs for Quick Revision
✅ Q1. What is the ideal timing for postpartum sterilization?
🅰️ Within 48 hours after delivery
✅ Q2. Is female sterilization reversible?
🅰️ Technically possible, but not reliably — considered permanent
✅ Q3. Does female sterilization affect sexual function?
🅰️ ❌ No
✅ Q4. What is the failure rate of tubal ligation?
🅰️ 0.5–1%
✅ Q5. Which method uses laparoscope and clips?
🅰️ Laparoscopic sterilization
♂️✂️ MALE STERILIZATION (VAS DEFERENS LIGATION / VASECTOMY)
🧠 High-Yield Topic for NORCET, AIIMS, NHM, RRB, ESIC, NCLEX
🔰 Definition
Male sterilization is a permanent method of contraception in which the vas deferens (sperm-carrying tubes) are cut, tied, or sealed, preventing sperm from mixing with semen.
Also called Vasectomy.
🎯 Purpose
✔️ Prevents sperm from reaching the egg
✔️ Simple, safe, and permanent solution for men who have completed their family
📦 Types of Vasectomy
| 💉 Type | 📘 Description |
|---|---|
| Conventional Vasectomy | Small scrotal incision, cutting and tying both vas deferens |
| No-Scalpel Vasectomy (NSV) | A needle-free, minimally invasive method with a special instrument |
| 🔹 NSV is the preferred method in national programs due to less pain, faster recovery, and fewer complications |
⚙️ Mechanism of Action
✔️ Blocks vas deferens, so sperm cannot enter the semen
✔️ Man continues to ejaculate, but without sperm
❗ Effectiveness begins only after 3 months
📉 Effectiveness
💯 >99.85% effective after sperm clearance
📌 Failure rate: <0.15%
✅ Advantages
✔️ Permanent and highly effective
✔️ No effect on libido, erection, or ejaculation
✔️ OPD procedure – no hospitalization needed
✔️ Safer, quicker, and simpler than female sterilization
✔️ Minimal side effects
❌ Disadvantages / Complications
❌ Permanent – requires strong decision
❌ Requires condom use for 3 months until semen is sperm-free
❌ Swelling, pain, bruising (rare)
❌ No STI/HIV protection
❌ Regret in young men or those with unstable relationships
🛑 Contraindications
🔺 Acute scrotal or genital infections
🔺 Bleeding disorders
🔺 Lack of informed consent
🔺 Reluctance to undergo permanent method
📋 Government of India Guidelines
| 📌 Parameter | 🧾 Details |
|---|---|
| Age criteria | ✅ Minimum 22 years |
| Consent | ✅ Mandatory written informed consent |
| Provided at | ✅ PHCs, CHCs, District Hospitals |
| Method promoted | ✅ No-Scalpel Vasectomy (NSV) |
| Incentive | ✅ Monetary incentives available under national program |
👨⚕️ Pre- & Post-Procedure Care (Nurse’s Role)
👨⚕️ Before Vasectomy:
✔️ Take consent & explain irreversibility
✔️ Rule out infections
✔️ Perform basic examination
✔️ Educate about backup contraception for 3 months
👨⚕️ After Vasectomy:
✔️ Apply scrotal support
✔️ Advise rest for 1–2 days
✔️ Watch for bleeding, infection
✔️ Educate on sperm testing after 3 months to confirm azoospermia
📘 Myths vs Facts
| ❌ Myth | ✅ Fact |
|---|---|
| Vasectomy affects sexual performance | ❌ No effect on sex drive or ability |
| It’s immediately effective | ❌ Takes ~3 months for sperm to clear |
| It causes weakness | ❌ No weakness or hormonal changes |
🧠 MCQs for Quick Revision
✅ Q1. What is the name of the surgical method for male sterilization?
🅰️ Vasectomy
✅ Q2. When is vasectomy considered effective?
🅰️ After 3 months / confirmed azoospermia
✅ Q3. Does vasectomy affect sexual function?
🅰️ ❌ No
✅ Q4. Preferred technique under national program is —
🅰️ No-Scalpel Vasectomy (NSV)
✅ Q5. What must be used until semen is sperm-free?
🅰️ Backup contraception (e.g., condom)
FAMILY PLANNING PROGRAMME: Implementation & Incentives
🧠 Important for NORCET, AIIMS, NHM, RRB, ESIC, NCLEX
🔰 Introduction
India was the first country in the world to launch an official National Family Planning Programme in 1952, aiming to control population growth and promote maternal-child health.
🧩 Objectives of the Programme
✔️ Reduce birth rate
✔️ Ensure spacing between births
✔️ Improve maternal and child health
✔️ Promote small family norm
✔️ Empower women through reproductive choices
🏛️ Implementing Bodies
| 🏢 Level | 👥 Responsible Personnel |
|---|---|
| Central Govt | Ministry of Health & Family Welfare (MoHFW) |
| State/District Level | State Health Department, RCH Officers |
| Block/PHC/SC Level | ANMs, ASHAs, Health Workers, Medical Officers |
⚙️ Key Components of Family Planning Services
1️⃣ Spacing Methods
- Oral pills (Mala-N, Chhaya)
- Condoms (Nirodh)
- IUCD (Cu-T 380A, PPIUCD)
- Injectable contraceptives (Antara)
2️⃣ Permanent Methods
- Female Sterilization (Tubectomy)
- Male Sterilization (Vasectomy/NSV)
3️⃣ Emergency Contraception
- Levonorgestrel 1.5 mg pill
- Copper-T IUCD within 5 days
4️⃣ Adolescent and postpartum counseling
📦 Service Delivery Points
✔️ Sub-Centres (SC)
✔️ Primary Health Centres (PHC)
✔️ Community Health Centres (CHC)
✔️ District Hospitals
✔️ Accredited Private Facilities under PPP
💰 Incentives Under the National Family Planning Program
🔹 For Acceptors (Beneficiaries)
| 🧬 Method | 💵 Cash Incentive (Approx.) |
|---|---|
| Female Sterilization | ₹1,000 – ₹1,400 (depending on state category) |
| Male Sterilization (NSV) | ₹1,500 – ₹2,000 (higher to encourage male participation) |
| PPIUCD / Interval IUCD | ₹300 |
| Antara Injectable | ₹100 per dose |
| Chhaya (Centchroman) | Free tablets + counseling |
🔹 For Providers (ASHA/Health Staff)
| 👩⚕️ Role | 💰 Incentive |
|---|---|
| ASHA for motivating sterilization | ₹200 – ₹300 |
| ASHA for IUCD motivation | ₹150 |
| ANM for IUCD insertion | ₹100 |
| ASHA for Antara motivation | ₹100 |
✅ ASHAs and ANMs are vital in mobilization, counseling, and follow-up.
🧠 Innovative Initiatives
- Mission Parivar Vikas – High-focus districts with TFR > 3
- Scheme for Home Delivery of Contraceptives by ASHAs
- Family Planning Logistic Management Information System (FP-LMIS)
- Ensuring Spacing at Birth (ESB) Scheme
📘 Monitoring & Evaluation
✔️ Monthly reporting through HMIS
✔️ Audits for sterilization quality
✔️ Family planning registers at SC/PHC level
✔️ Performance-based monitoring of ASHA & health workers
🧠 Important MCQs
✅ Q1. Which country launched the first National Family Planning Program?
🅰️ India (in 1952)
✅ Q2. Which injectable contraceptive is provided free in India?
🅰️ DMPA (Antara)
✅ Q3. Who receives higher incentive – male or female sterilization?
🅰️ Male sterilization (to encourage uptake)
✅ Q4. Under Mission Parivar Vikas, what is the TFR focus?
🅰️ Districts with TFR > 3
✅ Q5. Name the oral non-hormonal contraceptive promoted by the Govt.
🅰️ Chhaya (Centchroman)
👨👩👧👦 SMALL FAMILY NORMS
🧠 Important for NORCET, AIIMS, NHM, RRB, ESIC, NCLEX
🔰 Definition
Small Family Norm refers to the idea of limiting family size to two children in order to ensure better health, education, economic stability, and quality of life for all family members.
🎯 Objectives
✔️ Control population growth
✔️ Improve maternal and child health
✔️ Promote responsible parenthood
✔️ Ensure sustainable resource use
✔️ Enhance family welfare and economy
📘 Key Slogan
🗣️ “We two, ours one or two”
(Hum do, hamare do)
✅ Advantages of Small Family Norms
| 🔹 Aspect | ✅ Benefits |
|---|---|
| 👶 Child Health | Better nutrition, timely immunization, good care |
| 👩👧 Maternal Health | Reduced physical burden and complications |
| 📚 Education | More focus and investment per child |
| 💰 Financial Stability | Less financial strain, improved standard of living |
| 🏡 Family Welfare | Better housing, healthcare, and social opportunities |
| 🌍 Population Control | Helps maintain balance between population and resources |
🛠️ Implementation Strategies
1️⃣ Health and family planning counseling by ANMs, ASHAs, health workers
2️⃣ Mass media campaigns: Posters, slogans, TV, radio, social media
3️⃣ Incentives under family welfare program
4️⃣ Promotion of spacing and permanent methods
5️⃣ Inclusion in school health and adult education programs
6️⃣ Mission Parivar Vikas in high-fertility districts
👩⚕️ Nursing & Community Health Role
✔️ Educate eligible couples on family size impact
✔️ Provide information on contraception options
✔️ Encourage spacing between births
✔️ Motivate for permanent methods after 2 children
✔️ Promote maternal & child health services
✔️ Conduct community awareness campaigns
🧠 Common MCQs
✅ Q1. What is the ideal number of children as per small family norm?
🅰️ One or two
✅ Q2. What is the national slogan promoting small family norm?
🅰️ Hum do, hamare do
✅ Q3. Which government mission promotes small family norm in high-fertility areas?
🅰️ Mission Parivar Vikas
✅ Q4. Who is responsible for promoting small family norm at community level?
🅰️ ANM, ASHA, Health Workers
🌐 National Family Welfare Programme (NFWP) – India 🇮🇳
📌 Introduction
🔹 Launched: 1952
🔹 India became the first country in the world to launch an official family planning program.
🔹 Goal: To reduce birth rate and promote population stabilization.
🎯 Objectives of NFWP
✅ Control population growth
✅ Promote maternal and child health
✅ Reduce infant and maternal mortality
✅ Encourage responsible parenthood
✅ Promote contraceptive use
🏥 Key Services Provided
| 🧩 Component | 💡 Details |
|---|---|
| 🍼 Maternal Health | Antenatal, Intranatal, Postnatal care |
| 👶 Child Health | Immunization, Nutrition, ORT |
| 🔄 Family Planning | Spacing & permanent methods (IUCDs, condoms, sterilization) |
| 👩⚕️ RTI/STI Services | Diagnosis and treatment |
| 📢 IEC Activities | Communication to promote awareness |
| 🧪 Infertility Management | Diagnostic and treatment support |
🧪 Important Interventions/Programs under NFWP
| 🗓️ Program | 🔍 Focus Area |
|---|---|
| Reproductive & Child Health (RCH) | Integrated MCH + Family planning |
| Janani Suraksha Yojana (JSY) | Financial aid for institutional delivery |
| Janani Shishu Suraksha Karyakram (JSSK) | Free delivery, transport, drugs for pregnant mothers & infants |
| Mission Parivar Vikas (2016) | Family planning in high-focus states |
| Prerna Strategy | Delaying marriage & first childbirth |
| Home Delivery of Contraceptives (HDC) | By ASHAs at doorstep |
🧷 Contraceptive Methods under NFWP
🔹 Spacing Methods
- Condoms (Nirodh)
- Oral pills (Mala-D)
- IUCD (Copper-T, CuT-380A)
- Injectable contraceptives (Antara)
🔹 Permanent Methods
- Tubectomy (Female sterilization)
- Vasectomy (Male sterilization)
👩⚕️ Role of Nurse in NFWP
🟢 Educate couples on family planning
🟢 Distribute contraceptives
🟢 Refer for sterilization procedures
🟢 Antenatal/postnatal care
🟢 Monitor RTI/STI symptoms
🟢 Community health education
📉 Target/Indicators Monitored
🔸 Crude Birth Rate
🔸 Total Fertility Rate (TFR)
🔸 Couple Protection Rate (CPR)
🔸 Unmet need for contraception
📚 Golden One-Liner for Exams
🟨 India was the first country to launch a government-sponsored family planning program in 1952.
✅ High-Yield MCQ
Q. Which year was the National Family Welfare Programme launched in India?
A. 1947
B. 1950
✅ C. 1952
D. 1965
📝 Rationale: The NFWP was initiated in 1952, making India a global pioneer in state-supported family planning efforts.