CHN-32-NORMAL DIETATY REQUIREMENT-SYNP-PHC
⚡📏 Energy (Calories) & Measurement of Body Mass Index (BMI)
📘 Important for GNM/BSc Nursing, NHM, AIIMS, NORCET, GPSC & Community Health Nursing Exams
🔰 Part 1: Energy (Calories)
✅ Definition of Energy:
- Energy is the capacity to do work, which is required by the body for metabolism, growth, physical activity, maintaining body temperature, and repair of tissues.
✅ Unit of Measurement:
- Calorie: Amount of heat energy required to raise the temperature of 1 gram of water by 1°C.
- Kilocalorie (kcal): Commonly used in nutrition; 1 kcal = 1000 calories.
- Joule (SI Unit): 1 kcal = 4.184 kilojoules (kJ).
✅ Energy Yield of Nutrients:
| Nutrient | Energy Provided per Gram |
|---|---|
| Carbohydrates | 4 kcal |
| Proteins | 4 kcal |
| Fats | 9 kcal |
| Alcohol | 7 kcal |
✅ Daily Energy Requirements:
| Age/Group | Average Requirement (kcal/day) |
|---|---|
| Adult Male | 2400–3000 kcal |
| Adult Female | 1800–2200 kcal |
| Pregnant Women | +300 kcal extra |
| Lactating Women | +500 kcal extra |
| Children (1–3 yrs) | 1000–1200 kcal |
| Adolescents | 2200–2800 kcal |
🔰 Part 2: Measurement of Body Mass Index (BMI)
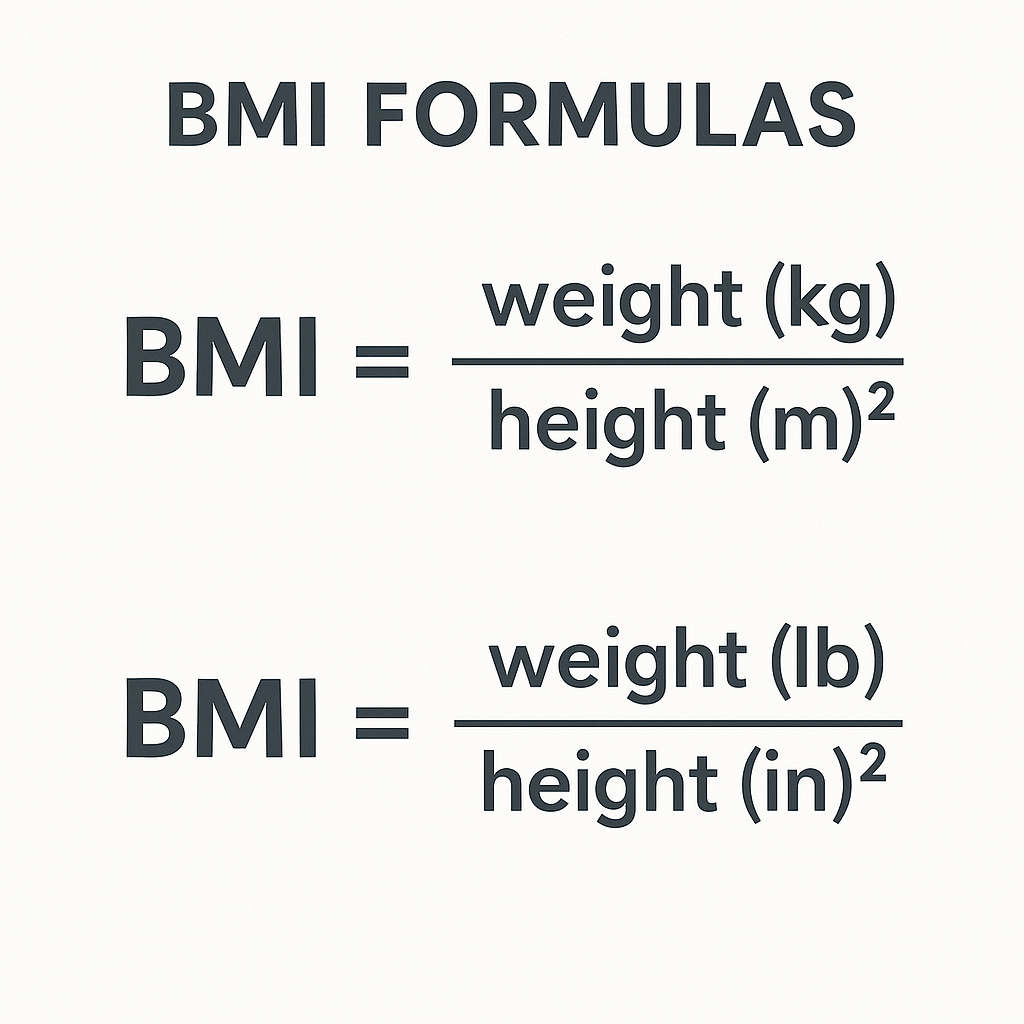
✅ Definition of BMI:
BMI is a simple tool to assess body fat and nutritional status, calculated based on a person’s height and weight.
✅ BMI Formula:
This BMI falls within the Normal range.
✅ BMI Classification (WHO):
| Category | BMI (kg/m²) |
|---|---|
| Underweight | Less than 18.5 |
| Normal Weight | 18.5 – 24.9 |
| Overweight | 25 – 29.9 |
| Obesity Class I | 30 – 34.9 |
| Obesity Class II | 35 – 39.9 |
| Obesity Class III | 40 and above |
✅ Limitations of BMI:
- It does not differentiate between muscle mass and fat mass.
- Not suitable for assessing athletes, pregnant women, and elderly individuals.
👩⚕️ Nurse’s Role in Nutritional Assessment:
- Educate about maintaining a balanced calorie intake according to activity level.
- Monitor and record BMI during health check-ups.
- Provide counseling for weight management based on BMI results.
- Guide in planning calorie-appropriate diets.
📚 Golden One-Liners for Quick Revision:
- 1 gram of fat provides 9 kcal – highest among nutrients.
- Normal BMI range is 18.5 to 24.9 kg/m².
- BMI helps in assessing nutritional status and obesity risk.
- Calories are the unit to measure energy intake and expenditure.
✅ Top 5 MCQs for Practice:
Q1. Which nutrient provides the highest energy per gram?
🅰️ Carbohydrates
🅱️ Proteins
✅ 🅲️ Fats
🅳️ Vitamins
Q2. What is the formula for calculating BMI?
🅰️ Weight (kg) × Height (m)
✅ 🅱️ Weight (kg) ÷ Height (m²)
🅲️ Height (m) ÷ Weight (kg)
🅳️ Weight (kg) ÷ Height (m)
Q3. A BMI of 28 kg/m² falls under which category?
🅰️ Normal
✅ 🅱️ Overweight
🅲️ Underweight
🅳️ Obesity Class I
Q4. Which age group has the highest daily energy requirement?
🅰️ Adult Female
🅱️ Pregnant Women
✅ 🅲️ Lactating Women
🅳️ Children
Q5. BMI is not suitable for which of the following groups?
🅰️ Children
🅱️ General adult population
✅ 🅲️ Athletes and pregnant women
🅳️ Healthy adults
📚🔥 Basal Metabolic Rate (BMR) – Determination and Factors Affecting It
📘 Important for GNM/BSc Nursing, NHM, AIIMS, NORCET, GPSC & Community Health Nursing Exams
✅ Definition of BMR:
Basal Metabolic Rate (BMR) is the amount of energy (calories) expended by the body at complete rest to maintain vital body functions such as breathing, blood circulation, body temperature regulation, and cellular metabolism.
✅ “BMR represents the minimum energy required to sustain life in a resting individual.”
✅ Normal BMR Values:
| Category | BMR Range (kcal/day) |
|---|---|
| Adult Male | 1500 – 1800 kcal |
| Adult Female | 1200 – 1400 kcal |
🔬 Determination of BMR:
📌 Methods:
- Direct Calorimetry:
- Measures the total heat produced by the body in a special calorimeter chamber.
- Accurate but expensive and complex.
- Indirect Calorimetry:
- Measures oxygen consumption and carbon dioxide production.
- Based on the fact that oxygen is required for energy production.
- Commonly used and more practical.
- Harris-Benedict Formula (Estimation Method):
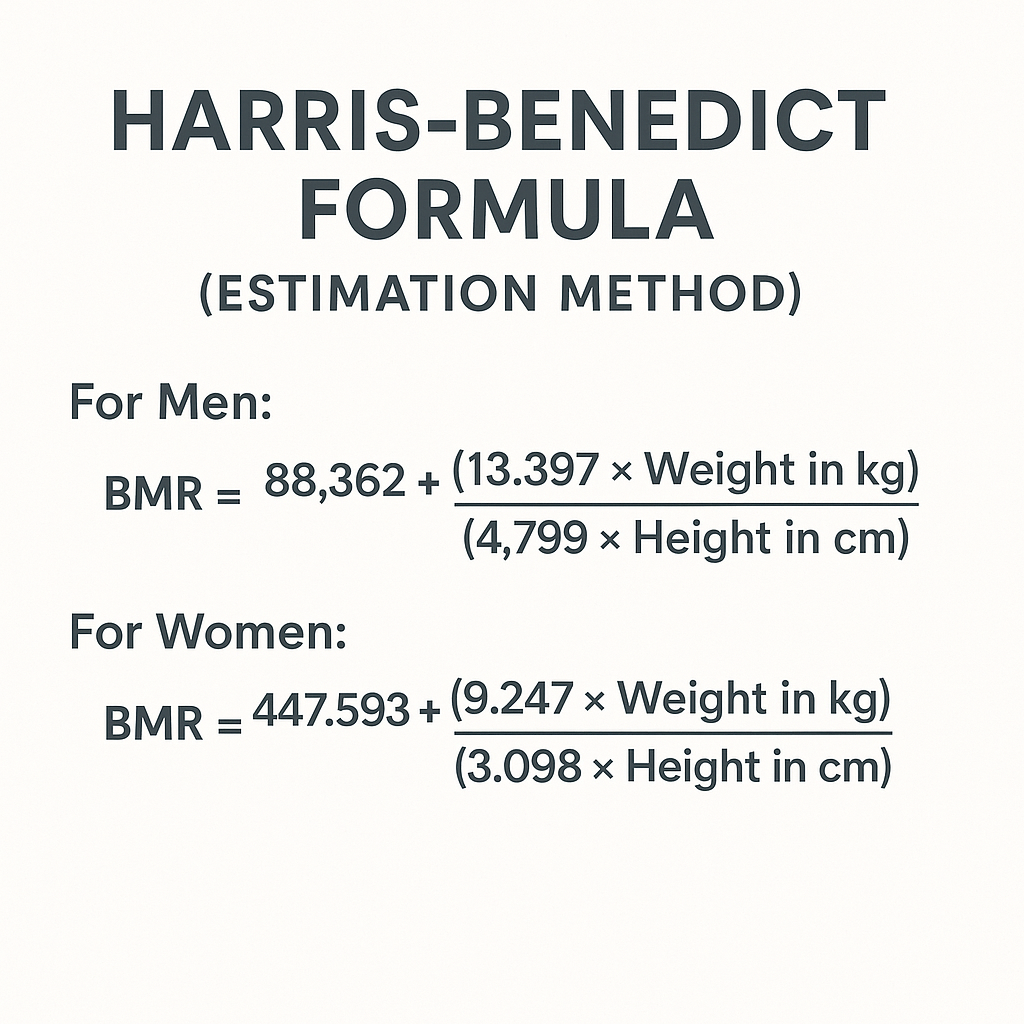
🎯 Factors Affecting BMR:
🟩 1. Age:
- BMR is highest in infants and children due to active growth.
- It declines with age as muscle mass decreases and metabolic activity slows.
🟨 2. Gender:
- Males generally have a higher BMR than females because of greater muscle mass.
- Females have relatively more body fat, which has lower metabolic activity.
🟧 3. Body Surface Area and Weight:
- Larger body size and greater surface area lead to higher BMR.
- Lean body mass (muscles) increases BMR, while fat mass does not.
🟥 4. Hormonal Factors:
- Thyroxine (Thyroid Hormone): Increases BMR.
- Hyperthyroidism → Increased BMR
- Hypothyroidism → Decreased BMR
- Adrenaline also temporarily raises BMR.
🟦 5. Climate and Temperature:
- BMR increases in cold climates to generate heat for body temperature regulation.
- Exposure to extreme temperatures increases energy expenditure.
🟪 6. Physiological Conditions:
- Pregnancy and Lactation: BMR increases to meet additional metabolic demands.
- Fever and Illness: Infections, burns, trauma increase BMR significantly.
🟫 7. Sleep and Rest:
- BMR decreases during deep sleep and complete rest.
📖 Additional Influencing Factors:
- Emotional states like stress and anxiety increase BMR.
- Regular physical activity raises BMR over time by increasing muscle mass.
- Certain drugs (e.g., caffeine, nicotine) temporarily increase BMR.
👩⚕️ Nurse’s Role:
- Assess patient’s nutritional needs based on BMR and activity level.
- Educate about the importance of maintaining healthy metabolism.
- Monitor conditions affecting BMR, such as thyroid disorders, fever, or malnutrition.
📚 Golden One-Liners for Quick Revision:
🟨 BMR is the minimum energy required at rest for vital functions.
🟨 BMR is measured using calorimetry or estimation formulas.
🟨 Factors like age, gender, hormones, and body size affect BMR.
🟨 Thyroid hormones are key regulators of metabolic rate.
✅ Top 5 MCQs for Practice:
Q1. Which hormone increases BMR?
🅰️ Insulin
🅱️ Estrogen
✅ 🅲️ Thyroxine
🅳️ Oxytocin
Q2. BMR is highest in which age group?
🅰️ Elderly
🅱️ Adults
✅ 🅲️ Infants and Children
🅳️ Teenagers
Q3. Which method is most commonly used to calculate BMR?
🅰️ Direct Calorimetry
✅ 🅱️ Indirect Calorimetry
🅲️ Blood Test
🅳️ Skinfold Measurement
Q4. BMR decreases during which of the following conditions?
🅰️ Fever
🅱️ Hyperthyroidism
✅ 🅲️ Hypothyroidism
🅳️ Pregnancy
Q5. Which of the following will increase BMR?
🅰️ Fasting
🅱️ Deep Sleep
✅ 🅲️ Physical Activity
🅳️ Old Age
🥗📏 Balanced Diet – Calculation for Different Categories of People & Normal Food Requirements
📘 Important for GNM/BSc Nursing, NHM, AIIMS, NORCET, GPSC & Community Health Nursing Exams
✅ 1. Calculation of Calorie (Energy) Requirement:
Energy requirements depend on age, sex, physiological condition, and physical activity level.
📖 General Formula for Daily Caloric Requirement:

📚 Activity Factors:
| Activity Level | Factor |
|---|---|
| Sedentary | 1.2 |
| Moderate Activity | 1.5 |
| Heavy Activity | 1.9 |
📚 Caloric Requirement as per ICMR (Indian Council of Medical Research):
| Category | Calorie Requirement (kcal/day) | Protein (g/day) |
|---|---|---|
| Adult Male (Sedentary) | 2400 | 60 |
| Adult Male (Moderate) | 2800 | 60 |
| Adult Male (Heavy) | 3500 | 60 |
| Adult Female (Sedentary) | 1900 | 55 |
| Adult Female (Moderate) | 2200 | 55 |
| Adult Female (Heavy) | 2900 | 55 |
| Pregnant Women | +300 kcal extra | 65 |
| Lactating Women | +500 kcal extra | 75 |
| Children (1–3 years) | 1000–1200 | 16 |
| Adolescents (Boys) | 2500–2800 | 70 |
| Adolescents (Girls) | 2100–2400 | 65 |
✅ 2. Normal Food Requirement Calculation (Food Groups):
| Food Group | Adult Male (g/day) | Adult Female (g/day) |
|---|---|---|
| Cereals & Millets | 400 – 450 | 350 – 400 |
| Pulses (Legumes) | 60 – 70 | 50 – 60 |
| Green Leafy Vegetables | 100 | 100 |
| Other Vegetables | 200 | 200 |
| Roots & Tubers | 100 | 100 |
| Fruits | 100 | 100 |
| Milk & Dairy Products | 300 ml | 300 ml |
| Fats & Oils | 25 – 30 | 20 – 25 |
| Sugar & Jaggery | 20 – 30 | 20 – 25 |
| Eggs/Meat/Fish | Optional (50–100) | Optional (50–100) |
| Water | 2 – 3 liters | 2 – 3 liters |
📖 Example Calculation for an Adult Male (Moderate Activity):
- Total Calories Needed: 2800 kcal/day
- Distribution of Calories:
- Carbohydrates: 55–60% → ~1540 kcal (385 g)
- Proteins: 15% → ~420 kcal (105 g)
- Fats: 25–30% → ~700 kcal (78 g)
🎯 Balanced Diet for Special Groups:
✅ Pregnant Women:
- Additional 300 kcal/day.
- Increase in iron, calcium, folic acid, and protein.
- Example: Add extra milk, fruits, pulses, and green leafy vegetables.
✅ Lactating Women:
- Additional 500 kcal/day.
- Increase in protein, calcium, and vitamin A.
✅ Children:
- High-energy, protein-rich diet for growth.
- Include milk, eggs, cereals, fruits, and vegetables.
✅ Elderly People:
- Require fewer calories but more calcium, fiber, and vitamins.
- Reduce fat and sugar intake to avoid lifestyle diseases.
👩⚕️ Nurse’s Role in Calculating and Planning Diets:
- Assess nutritional status and energy requirements based on age, activity, and health condition.
- Plan and suggest balanced diet charts accordingly.
- Provide nutrition counseling to special groups like pregnant women, lactating mothers, children, and the elderly.
📚 Golden One-Liners for Quick Revision:
- Balanced diet provides adequate calories, proteins, fats, vitamins, minerals, and water.
- Caloric requirement increases during pregnancy, lactation, and heavy physical work.
- Nurses play a vital role in diet counseling and nutritional assessment.
✅ Top 5 MCQs for Practice:
Q1. How many extra calories are needed during pregnancy?
🅰️ 200 kcal
🅱️ 400 kcal
✅ 🅲️ 300 kcal
🅳️ 500 kcal
Q2. The recommended daily protein intake for an adult female is:
🅰️ 45 grams
🅱️ 50 grams
✅ 🅲️ 55 grams
🅳️ 65 grams
Q3. How much cereal is recommended for an adult male per day?
🅰️ 200 grams
🅱️ 300 grams
✅ 🅲️ 400–450 grams
🅳️ 600 grams
Q4. Which group requires the highest caloric intake?
🅰️ Children
🅱️ Pregnant Women
✅ 🅲️ Lactating Women
🅳️ Elderly
Q5. What percentage of total daily calories should ideally come from carbohydrates?
🅰️ 20–30%
🅱️ 35–45%
✅ 🅲️ 55–60%
🅳️ 70–80%
📚🥗 Menu Planning and Food Combinations Affecting or Enhancing Nutritive Value of the Diet
📘 Important for GNM/BSc Nursing, NHM, AIIMS, NORCET, GPSC & Community Health Nursing Exams
✅ Definition of Menu Planning:
Menu planning is the process of selecting and organizing meals to ensure that they meet the nutritional requirements, health needs, preferences, and budget of individuals or groups.
✅ “A well-planned menu ensures a balanced, appealing, and nutritious diet for good health and disease prevention.”
🎯 Objectives of Menu Planning:
- Ensure balanced nutrition covering all food groups.
- Cater to age, health status, and activity levels.
- Include economical and locally available foods.
- Provide variety to avoid monotony in meals.
- Consider special requirements for pregnancy, lactation, children, elderly, and patients.
✅ Balanced Menu Example for a Day (Adult Male – Moderate Activity):
| Meal | Items | Nutritional Contribution |
|---|---|---|
| Morning | Warm Lemon Water + Soaked Almonds | Detoxification, Healthy Fats |
| Breakfast | Vegetable Upma + Boiled Egg + Milk | Carbohydrates, Proteins, Calcium |
| Mid-Morning | Seasonal Fruit (Banana/Guava) | Vitamins, Minerals, Fiber |
| Lunch | Chapati + Rice + Dal + Mixed Veg Curry + Curd + Salad | Balanced Macronutrients, Probiotics |
| Evening | Roasted Chana or Sprouts + Herbal Tea | Protein, Fiber, Antioxidants |
| Dinner | Chapati + Green Leafy Vegetable Sabji + Dal + Buttermilk | Vitamins, Proteins, Digestion Aid |
📖 Food Combinations Affecting and Enhancing Nutritive Value:
🟩 1. Enhancing Nutrient Bioavailability:
- ✅ Vitamin C + Iron-Rich Foods:
- Example: Lemon juice with green leafy vegetables or sprouts.
- Effect: Vitamin C enhances iron absorption (prevents anemia).
- ✅ Protein Combination (Complementary Proteins):
- Example: Cereals (wheat, rice) + Pulses (dal, legumes) = Complete Protein.
- Effect: Improves protein quality by providing all essential amino acids.
- ✅ Fat-Soluble Vitamins with Fats:
- Example: Carrot or Spinach cooked with oil or ghee.
- Effect: Enhances absorption of Vitamins A, D, E, K.
- ✅ Probiotics and Prebiotics Together:
- Example: Curd (probiotic) with fiber-rich foods like salads.
- Effect: Improves gut health and digestion.
🟨 2. Combinations Reducing Nutrient Absorption (Negative Interactions):
- ❌ Tea/Coffee with Iron-Rich Foods:
- Effect: Tannins in tea and coffee reduce iron absorption.
- ❌ Calcium with Iron Supplements:
- Effect: Both compete for absorption, reducing bioavailability.
- ❌ High-Fiber Foods with Micronutrients:
- Effect: Excessive fiber can bind with minerals like zinc, iron, and calcium, reducing their absorption.
📚 Golden One-Liners for Quick Revision:
🟨 Vitamin C-rich foods enhance iron absorption.
🟨 Cereals and pulses together provide complete proteins.
🟨 Avoid tea/coffee immediately after iron-rich meals to prevent iron malabsorption.
🟨 Healthy menu planning ensures balanced nutrient intake and improved health outcomes.
✅ Top 5 MCQs for Practice:
Q1. Which of the following food combinations improves iron absorption?
🅰️ Rice + Curd
🅱️ Chapati + Tea
✅ 🅲️ Spinach + Lemon Juice
🅳️ Milk + Pulses
Q2. Which vitamin enhances calcium absorption?
🅰️ Vitamin C
✅ 🅱️ Vitamin D
🅲️ Vitamin E
🅳️ Vitamin K
Q3. What is an example of a complementary protein combination?
🅰️ Rice + Pulses
🅱️ Milk + Fruits
🅲️ Tea + Snacks
🅳️ Coffee + Biscuits
Q4. Which food should be avoided immediately after meals to enhance iron absorption?
🅰️ Buttermilk
🅱️ Warm Water
✅ 🅲️ Tea/Coffee
🅳️ Fruit Juice
Q5. The addition of oil in carrot curry enhances the absorption of which vitamin?
🅰️ Vitamin C
✅ 🅱️ Vitamin A
🅲️ Vitamin B12
🅳️ Vitamin B6
📚💰 Budgeting for Food, Low-Cost Meals, and Food Substitutes
📘 Important for GNM/BSc Nursing, NHM, AIIMS, NORCET, GPSC & Community Health Nursing Exams
✅ 1. Budgeting for Food
📖 Definition:
Budgeting for food means planning the purchase and consumption of nutritious food within a fixed financial limit, ensuring that the family’s nutritional needs are met economically.
🎯 Objectives of Food Budgeting:
- Ensure a balanced diet within available income.
- Avoid unnecessary food wastage.
- Promote the use of locally available and seasonal foods.
- Provide adequate calories, proteins, vitamins, and minerals at minimum cost.
📚 Steps in Food Budgeting:
- Assess the family’s monthly income.
- Determine the nutritional needs based on age, gender, and health status.
- Allocate appropriate funds for essential food groups (cereals, pulses, milk, fruits, vegetables).
- Plan to buy seasonal and locally available foods which are cheaper and fresher.
- Avoid buying processed, junk, and packaged foods.
- Store food properly to prevent spoilage and waste.
✅ 2. Low-Cost Nutritious Meals
📚 Principles of Planning Low-Cost Meals:
- Use low-cost, nutrient-dense local foods.
- Combine foods to improve protein quality (e.g., cereals + pulses).
- Use green leafy vegetables for vitamins and minerals.
- Prepare meals using economical cooking methods (boiling, steaming instead of frying).
- Utilize kitchen waste efficiently (e.g., using vegetable peels for soups).
📚 Examples of Low-Cost Meals:
- Breakfast: Vegetable Poha/Upma with Lemon + Boiled Egg (Optional)
- Lunch: Rice/Chapati + Dal + Seasonal Vegetables + Curd/Buttermilk
- Evening Snack: Roasted Groundnuts or Sprouts + Herbal Tea
- Dinner: Chapati + Green Leafy Vegetable Sabji + Dal + Buttermilk
✅ 3. Food Substitutes (Low-Cost Alternatives)
| Nutrient Required | Expensive Food | Low-Cost Substitute |
|---|---|---|
| Protein | Meat, Fish, Eggs | Pulses, Soya Beans, Groundnuts, Sprouts |
| Calcium | Milk, Cheese | Ragi (Finger Millet), Green Leafy Vegetables, Sesame Seeds |
| Iron | Red Meat | Spinach, Amaranth, Jaggery, Pulses |
| Vitamin C | Oranges, Kiwi | Amla (Gooseberry), Lemon, Guava |
| Fats | Butter, Ghee | Groundnut Oil, Sunflower Oil, Mustard Oil |
| Energy | Cakes, Biscuits | Bananas, Jaggery, Roasted Chana |
📖 Note:
- Sprouting pulses increases their nutritional value and digestibility.
- Ragi is a rich and cheap source of calcium, excellent for children and elderly.
👩⚕️ Nurse’s Role in Food Budgeting and Nutrition Counseling:
- Teach families about low-cost, high-nutrient foods.
- Promote the use of seasonal and locally available foods.
- Educate about reducing food wastage and economical meal preparation.
- Guide families in making wise food purchasing decisions.
📚 Golden One-Liners for Quick Revision:
- Low-cost meals should be nutritious and culturally acceptable.
- Cereals and pulses together improve protein quality.
- Green leafy vegetables are low-cost and rich in iron and calcium.
- Nurses play a key role in promoting economical and balanced diets.
✅ Top 5 MCQs for Practice:
Q1. Which is a low-cost, high-protein food substitute?
🅰️ Chicken
🅱️ Cheese
✅ 🅲️ Soya Beans
🅳️ Ice Cream
Q2. Which is a cheap source of calcium?
🅰️ Milk
🅱️ Cheese
✅ 🅲️ Ragi
🅳️ Chicken
Q3. Food budgeting helps in:
🅰️ Increasing food waste
🅱️ Buying expensive processed foods
✅ 🅲️ Ensuring nutrition within financial limits
🅳️ Reducing food variety
Q4. Amla is a low-cost source of which vitamin?
🅰️ Vitamin A
🅱️ Vitamin D
✅ 🅲️ Vitamin C
🅳️ Vitamin K
Q5. What is the role of a nurse in food budgeting?
🅰️ Promote only expensive foods
🅱️ Ignore family income while planning diets
✅ 🅲️ Educate about low-cost nutritious alternatives
🅳️ Encourage waste of food
📚⚠️ Diseases and Disorders Caused by Imbalance of Nutrients
📘 Essential for GNM/BSc Nursing, NHM, AIIMS, NORCET, GPSC & Community Health Nursing Exams
✅ Introduction:
Imbalance of nutrients occurs when the body receives either an excess or deficiency of essential nutrients, leading to malnutrition. This can cause various deficiency disorders and lifestyle-related diseases.
🎯 Types of Nutritional Imbalance:
- Under-Nutrition:
- Insufficient intake of calories and nutrients.
- Leads to deficiency diseases.
- Over-Nutrition:
- Excessive intake of calories, fats, and sugars.
- Leads to lifestyle diseases and obesity.
✅ Nutrient Deficiency Disorders:
| Nutrient Deficient | Disease/Disorder | Key Symptoms |
|---|---|---|
| Protein-Energy | Kwashiorkor (Protein Deficiency) | Edema, enlarged belly, hair changes |
| Marasmus (Protein & Calorie Deficiency) | Severe weight loss, muscle wasting | |
| Iron | Iron Deficiency Anemia | Fatigue, pallor, breathlessness |
| Iodine | Goiter | Neck swelling, hypothyroidism |
| Cretinism (in infants) | Mental retardation, dwarfism | |
| Vitamin A | Night Blindness, Xerophthalmia | Poor night vision, dry eyes |
| Vitamin D | Rickets (Children), Osteomalacia (Adults) | Bone deformities, weak bones |
| Vitamin C | Scurvy | Bleeding gums, delayed wound healing |
| Vitamin B1 (Thiamine) | Beriberi | Muscle weakness, nerve damage |
| Vitamin B3 (Niacin) | Pellagra | 3 D’s: Dermatitis, Diarrhea, Dementia |
| Calcium | Osteoporosis, Rickets | Weak bones, fractures |
| Zinc | Growth retardation, Delayed healing | Poor immune function, skin lesions |
✅ Nutrient Excess Disorders (Over-Nutrition):
| Excess Nutrient | Disease/Disorder | Key Effects |
|---|---|---|
| Calories (Fats & Sugars) | Obesity | Increased body fat, lethargy |
| Fats (Saturated) | Atherosclerosis, Heart Disease | Blocked arteries, heart attack risk |
| Sugars | Type 2 Diabetes Mellitus | High blood sugar, insulin resistance |
| Sodium (Salt) | Hypertension | High blood pressure, stroke risk |
| Cholesterol | Hyperlipidemia | High LDL, cardiovascular disease |
✅ Mixed Nutritional Deficiency Diseases:
- Protein Energy Malnutrition (PEM):
- Common in children under 5 years.
- Includes Kwashiorkor and Marasmus.
- Multiple Micronutrient Deficiencies:
- Common in underprivileged communities.
- Involves simultaneous deficiencies of iron, iodine, vitamin A, and zinc.
👩⚕️ Nurse’s Role in Prevention:
- Educate on importance of a balanced diet.
- Promote consumption of locally available nutritious foods.
- Identify early signs of malnutrition and refer for medical care.
- Implement and promote nutritional supplementation programs (e.g., Vitamin A prophylaxis, Iron & Folic Acid supplementation).
📚 Golden One-Liners for Quick Revision:
- Vitamin A deficiency causes night blindness.
- Vitamin C deficiency leads to scurvy.
- Protein deficiency causes Kwashiorkor, and calorie deficiency causes Marasmus.
- Overnutrition leads to obesity, hypertension, and diabetes.
✅ Top 5 MCQs for Practice:
Q1. Which disease is caused by vitamin D deficiency in children?
🅰️ Scurvy
🅱️ Pellagra
✅ 🅲️ Rickets
🅳️ Beriberi
Q2. Excess intake of sodium in the diet may lead to:
🅰️ Anemia
🅱️ Osteoporosis
✅ 🅲️ Hypertension
🅳️ Kwashiorkor
Q3. Pellagra is caused due to the deficiency of:
🅰️ Vitamin B1
✅ 🅱️ Niacin (Vitamin B3)
🅲️ Vitamin C
🅳️ Vitamin D
Q4. Which of the following is a protein-energy malnutrition disease?
🅰️ Scurvy
🅱️ Night Blindness
✅ 🅲️ Marasmus
🅳️ Goiter
Q5. Overnutrition is commonly associated with which disease?
🅰️ Kwashiorkor
🅱️ Night Blindness
✅ 🅲️ Type 2 Diabetes Mellitus
🅳️ Beriberi
📚⚠️ Diseases and Disorders Caused by Imbalance of Nutrients
📘 Essential for GNM/BSc Nursing, NHM, AIIMS, NORCET, GPSC & Community Health Nursing Exams
✅ Introduction:
Imbalance of nutrients occurs when the body receives either an excess or deficiency of essential nutrients, leading to malnutrition. This can cause various deficiency disorders and lifestyle-related diseases.
🎯 Types of Nutritional Imbalance:
- Under-Nutrition:
- Insufficient intake of calories and nutrients.
- Leads to deficiency diseases.
- Over-Nutrition:
- Excessive intake of calories, fats, and sugars.
- Leads to lifestyle diseases and obesity.
✅ Nutrient Deficiency Disorders:
| Nutrient Deficient | Disease/Disorder | Key Symptoms |
|---|---|---|
| Protein-Energy | Kwashiorkor (Protein Deficiency) | Edema, enlarged belly, hair changes |
| Marasmus (Protein & Calorie Deficiency) | Severe weight loss, muscle wasting | |
| Iron | Iron Deficiency Anemia | Fatigue, pallor, breathlessness |
| Iodine | Goiter | Neck swelling, hypothyroidism |
| Cretinism (in infants) | Mental retardation, dwarfism | |
| Vitamin A | Night Blindness, Xerophthalmia | Poor night vision, dry eyes |
| Vitamin D | Rickets (Children), Osteomalacia (Adults) | Bone deformities, weak bones |
| Vitamin C | Scurvy | Bleeding gums, delayed wound healing |
| Vitamin B1 (Thiamine) | Beriberi | Muscle weakness, nerve damage |
| Vitamin B3 (Niacin) | Pellagra | 3 D’s: Dermatitis, Diarrhea, Dementia |
| Calcium | Osteoporosis, Rickets | Weak bones, fractures |
| Zinc | Growth retardation, Delayed healing | Poor immune function, skin lesions |
✅ Nutrient Excess Disorders (Over-Nutrition):
| Excess Nutrient | Disease/Disorder | Key Effects |
|---|---|---|
| Calories (Fats & Sugars) | Obesity | Increased body fat, lethargy |
| Fats (Saturated) | Atherosclerosis, Heart Disease | Blocked arteries, heart attack risk |
| Sugars | Type 2 Diabetes Mellitus | High blood sugar, insulin resistance |
| Sodium (Salt) | Hypertension | High blood pressure, stroke risk |
| Cholesterol | Hyperlipidemia | High LDL, cardiovascular disease |
✅ Mixed Nutritional Deficiency Diseases:
- Protein Energy Malnutrition (PEM):
- Common in children under 5 years.
- Includes Kwashiorkor and Marasmus.
- Multiple Micronutrient Deficiencies:
- Common in underprivileged communities.
- Involves simultaneous deficiencies of iron, iodine, vitamin A, and zinc.
👩⚕️ Nurse’s Role in Prevention:
- Educate on importance of a balanced diet.
- Promote consumption of locally available nutritious foods.
- Identify early signs of malnutrition and refer for medical care.
- Implement and promote nutritional supplementation programs (e.g., Vitamin A prophylaxis, Iron & Folic Acid supplementation).
📚 Golden One-Liners for Quick Revision:
- Vitamin A deficiency causes night blindness.
- Vitamin C deficiency leads to scurvy.
- Protein deficiency causes Kwashiorkor, and calorie deficiency causes Marasmus.
- Overnutrition leads to obesity, hypertension, and diabetes.
✅ Top 5 MCQs for Practice:
Q1. Which disease is caused by vitamin D deficiency in children?
🅰️ Scurvy
🅱️ Pellagra
✅ 🅲️ Rickets
🅳️ Beriberi
Q2. Excess intake of sodium in the diet may lead to:
🅰️ Anemia
🅱️ Osteoporosis
✅ 🅲️ Hypertension
🅳️ Kwashiorkor
Q3. Pellagra is caused due to the deficiency of:
🅰️ Vitamin B1
✅ 🅱️ Niacin (Vitamin B3)
🅲️ Vitamin C
🅳️ Vitamin D
Q4. Which of the following is a protein-energy malnutrition disease?
🅰️ Scurvy
🅱️ Night Blindness
✅ 🅲️ Marasmus
🅳️ Goiter
Q5. Overnutrition is commonly associated with which disease?
🅰️ Kwashiorkor
🅱️ Night Blindness
✅ 🅲️ Type 2 Diabetes Mellitus
🅳️ Beriberi
📚🚫 Food Allergy – Causes, Types, and Diet Modifications
📘 Essential for GNM/BSc Nursing, NHM, AIIMS, NORCET, GPSC & Community Health Nursing Exams
✅ Definition of Food Allergy:
A food allergy is an abnormal immune response triggered by certain foods, where the body mistakenly identifies specific proteins as harmful, leading to allergic reactions.
✅ “Food allergy involves an immune-mediated hypersensitivity to specific food proteins.”
🎯 Causes of Food Allergy:
- Genetic Predisposition: Family history of allergies or asthma.
- Immature Digestive System: Common in infants and young children.
- Leaky Gut Syndrome: Increased gut permeability allowing allergens into circulation.
- Exposure to Allergenic Foods Early in Life.
- Environmental Factors and Pollutants.
📖 Common Allergenic Foods:
- Milk and dairy products (Lactose intolerance)
- Wheat and gluten-containing foods (Gluten intolerance/Celiac disease)
- Eggs
- Peanuts and tree nuts
- Soy
- Seafood and shellfish
- Chocolate
✅ Types of Food Intolerance and Allergies:
🟩 1. Gluten Intolerance (Celiac Disease):
- 📌 Cause: Autoimmune reaction to gluten, a protein found in wheat, barley, and rye.
- 📌 Symptoms:
- Diarrhea, abdominal bloating, malabsorption, weight loss, anemia, fatigue.
- 📌 Diet Modification:
- Follow a strict Gluten-Free Diet.
- ❌ Avoid: Wheat, barley, rye, semolina, and all bakery products containing gluten.
- ✅ Allowed: Rice, corn, millet, quinoa, gluten-free flours.
🟨 2. Lactose Intolerance:
- 📌 Cause: Deficiency of lactase enzyme, leading to inability to digest lactose (milk sugar).
- 📌 Symptoms:
- Bloating, flatulence, abdominal cramps, diarrhea after consuming milk or dairy.
- 📌 Diet Modification:
- ❌ Avoid: Milk, cream, paneer, ice cream, and other dairy products.
- ✅ Allowed: Lactose-free milk, yogurt (better tolerated), plant-based milks (soy, almond, coconut), calcium-fortified foods.
🟧 3. Protein Intolerance (Cow’s Milk Protein Allergy):
- 📌 Cause: Immune system reacts to casein or whey proteins in cow’s milk.
- 📌 Symptoms:
- Vomiting, diarrhea, skin rashes (eczema), colic in infants, respiratory problems.
- 📌 Diet Modification:
- ❌ Avoid: Cow’s milk and all milk products.
- ✅ Allowed: Plant-based formulas (soy-based, rice-based), hypoallergenic infant formulas, goat milk (if tolerated under medical advice).
📚 General Management of Food Allergies:
- Identify and Eliminate the Allergen:
- Use elimination diets and allergy testing.
- Read Food Labels Carefully:
- Avoid hidden sources of allergens in processed foods.
- Substitute with Safe and Nutritious Alternatives.
- Emergency Management:
- Severe reactions (anaphylaxis) require immediate treatment with epinephrine injection (EpiPen).
👩⚕️ Nurse’s Role in Managing Food Allergies:
- Educate patients and caregivers about food label reading and allergen avoidance.
- Plan and provide guidance on nutritionally adequate allergen-free diets.
- Recognize early signs of allergic reactions and provide emergency care if needed.
- Refer to a dietician or allergist for specialized management.
📚 Golden One-Liners for Quick Revision:
- Gluten intolerance requires a strict gluten-free diet.
- Lactose intolerance results from lactase enzyme deficiency.
- Cow’s milk protein allergy is common in infants and young children.
- Severe allergic reactions may lead to anaphylaxis requiring emergency care.
✅ Top 5 MCQs for Practice:
Q1. Which food must be avoided in gluten intolerance?
🅰️ Rice
🅱️ Corn
✅ 🅲️ Wheat
🅳️ Millets
Q2. Lactose intolerance is caused by deficiency of which enzyme?
🅰️ Amylase
🅱️ Lipase
✅ 🅲️ Lactase
🅳️ Protease
Q3. Which is a suitable alternative for cow’s milk protein allergy?
🅰️ Paneer
✅ 🅱️ Soy-based formula
🅲️ Butter
🅳️ Yogurt
Q4. A severe, life-threatening allergic reaction is called:
🅰️ Eczema
🅱️ Asthma
✅ 🅲️ Anaphylaxis
🅳️ Dermatitis
Q5. Which nutrient deficiency should be monitored in lactose intolerance?
🅰️ Iron
🅱️ Vitamin A
✅ 🅲️ Calcium
🅳️ Vitamin C
📚⚠️ Food Intolerance and Inborn Errors of Metabolism
📘 Essential for GNM/BSc Nursing, NHM, AIIMS, NORCET, GPSC & Community Health Nursing Exams
✅ Definition of Food Intolerance:
Food intolerance is the inability to properly digest or metabolize certain foods due to enzyme deficiencies or metabolic defects. It is non-immune mediated and usually leads to digestive discomfort rather than allergic reactions.
✅ “Food intolerance involves a metabolic inability to process certain nutrients, leading to digestive and systemic symptoms.”
✅ Common Causes of Food Intolerance:
- Enzyme Deficiencies (e.g., lactase deficiency in lactose intolerance).
- Inborn Errors of Metabolism (genetic defects affecting metabolism).
- Chemical Sensitivities (e.g., to additives like MSG or sulfites).
🎯 Inborn Errors of Metabolism (IEM):
📖 Definition:
Inborn Errors of Metabolism are genetic disorders where the body lacks specific enzymes required to metabolize certain nutrients, leading to the accumulation of toxic substances or deficiency of essential products.
✅ “IEM are hereditary disorders caused by enzyme defects affecting metabolism of proteins, carbohydrates, or fats.”
📚 Common Inborn Errors of Metabolism:
🟩 1. Phenylketonuria (PKU):
- 📌 Cause: Deficiency of phenylalanine hydroxylase enzyme.
- 📌 Result: Accumulation of phenylalanine causing brain damage and mental retardation.
- 📌 Symptoms:
- Intellectual disability, seizures, delayed milestones, musty odor in urine.
- 📌 Diet Modification:
- ❌ Strictly avoid high-protein foods: Meat, eggs, dairy, pulses.
- ✅ Use special low-phenylalanine formulas and cereals.
🟨 2. Galactosemia:
- 📌 Cause: Deficiency of galactose-1-phosphate uridyl transferase enzyme.
- 📌 Result: Inability to metabolize galactose (a sugar from lactose), leading to liver and kidney damage.
- 📌 Symptoms:
- Vomiting after milk feeding, jaundice, enlarged liver, failure to thrive, cataracts.
- 📌 Diet Modification:
- ❌ Avoid all milk and dairy products.
- ✅ Use lactose-free and galactose-free formulas.
🟧 3. Maple Syrup Urine Disease (MSUD):
- 📌 Cause: Deficiency of enzymes needed to break down branched-chain amino acids (Leucine, Isoleucine, Valine).
- 📌 Symptoms:
- Sweet-smelling urine (like maple syrup), vomiting, poor feeding, lethargy, seizures.
- 📌 Diet Modification:
- ❌ Restrict intake of branched-chain amino acids.
- ✅ Use special medical formulas.
🟥 4. Lactose Intolerance (Common Metabolic Intolerance):
- 📌 Cause: Deficiency of lactase enzyme in the small intestine.
- 📌 Symptoms:
- Bloating, diarrhea, flatulence, abdominal pain after consuming milk.
- 📌 Diet Modification:
- ❌ Avoid milk and lactose-containing foods.
- ✅ Use lactose-free milk and plant-based milk (soy, almond).
📚 General Management of IEM and Food Intolerance:
- Early Diagnosis: Through newborn screening programs (Heel-prick test).
- Strict Dietary Management: Avoid specific nutrients that cannot be metabolized.
- Lifelong Monitoring: Regular health check-ups to prevent complications.
- Use of Special Medical Formulas: For infants and children with IEM.
👩⚕️ Nurse’s Role:
- Educate parents and caregivers about early signs and dietary restrictions.
- Ensure adherence to specialized diets and prevent accidental exposure.
- Provide emotional support to families coping with lifelong dietary management.
- Collaborate with dietitians for meal planning.
📚 Golden One-Liners for Quick Revision:
- Phenylketonuria requires restriction of phenylalanine-rich foods.
- Galactosemia requires a complete dairy-free diet.
- MSUD causes sweet-smelling urine and neurological symptoms.
- Lactose intolerance is managed with lactose-free diets.
- Early detection of IEM is done through newborn screening programs.
✅ Top 5 MCQs for Practice:
Q1. Phenylketonuria is caused by the deficiency of which enzyme?
🅰️ Lactase
🅱️ Galactose-1-phosphate transferase
✅ 🅲️ Phenylalanine hydroxylase
🅳️ Amylase
Q2. In Galactosemia, which food should be strictly avoided?
🅰️ Rice
🅱️ Eggs
✅ 🅲️ Milk and Milk Products
🅳️ Vegetables
Q3. Maple Syrup Urine Disease is associated with the metabolism of:
🅰️ Fatty acids
✅ 🅱️ Branched-chain amino acids
🅲️ Simple sugars
🅳️ Nucleic acids
Q4. Which of the following is a common symptom of lactose intolerance?
🅰️ Fever
🅱️ Constipation
✅ 🅲️ Diarrhea and Bloating
🅳️ Rash
Q5. The most effective method for early detection of Inborn Errors of Metabolism is:
🅰️ Urine test after 1 year
✅ 🅱️ Newborn screening (heel-prick test)
🅲️ Chest X-ray
🅳️ MRI