BSC SEM 4 UNIT 5 PATHOLOGY 2 & GENETICS.
UNIT 5 Services related to genetics
INTRODUCTION.
Services related to genetics in nursing are increasingly important in modern healthcare due to advancements in genetic science, personalized medicine, and preventive care. In nursing, genetic services involve the understanding, identification, education, and support of patients and families affected by or at risk for genetic conditions.
🔬 Genetics-Related Services in Nursing
1. Genetic Assessment and Risk Identification
- Taking a detailed family history (three-generation pedigree).
- Identifying individuals at risk for inherited disorders.
- Recognizing patterns suggestive of genetic conditions (e.g., early-onset cancers, congenital anomalies).
2. Genetic Counseling Support
- Providing pre- and post-test education.
- Referring patients to certified genetic counselors or specialists.
- Assisting patients in understanding inheritance patterns, test implications, and possible outcomes.
3. Genetic Testing and Interpretation Assistance
- Supporting patients in decision-making about genetic testing (e.g., BRCA1/BRCA2, prenatal screening).
- Educating about types of genetic tests (diagnostic, predictive, carrier, prenatal).
- Interpreting and communicating test results under physician or genetic counselor guidance.
4. Patient and Family Education
- Explaining basic genetic concepts in understandable language.
- Discussing lifestyle modifications and preventive strategies based on genetic risks.
- Helping families understand disease progression, recurrence risks, and reproductive options.
5. Ethical, Legal, and Psychosocial Support
- Supporting informed consent and confidentiality in genetic testing.
- Addressing emotional responses like anxiety, guilt, or fear.
- Advocating for patient autonomy and rights regarding genetic information.
6. Care Planning and Coordination
- Incorporating genetic risk factors into nursing care plans.
- Coordinating with multidisciplinary teams for long-term management (e.g., oncology, pediatrics, cardiology).
- Monitoring and supporting patients during interventions or surveillance programs.
7. Prenatal and Reproductive Services
- Supporting prenatal screening (e.g., Down syndrome, thalassemia).
- Counseling in high-risk pregnancies (e.g., maternal age, family history of disorders).
- Referral to reproductive specialists for genetic disorders.
8. Pediatric Genetic Services
- Early identification of developmental or metabolic disorders.
- Coordinating newborn screening programs.
- Educating parents on inherited childhood disorders (e.g., cystic fibrosis, hemophilia).
9. Chronic Disease and Cancer Genetic Services
- Managing genetic aspects of chronic conditions like diabetes, hypertension, or Alzheimer’s.
- Participating in oncology care involving hereditary cancers (e.g., colon, breast).
- Promoting lifestyle modifications in genetically predisposed individuals.
10. Community and Preventive Services
- Educating the community about common genetic conditions.
- Promoting genetic screening in high-risk populations (e.g., consanguineous marriages).
- Advocating for public health initiatives related to genetics.
🧠 Examples of Genetic Conditions in Nursing Practice
- Sickle Cell Anemia
- Thalassemia
- Cystic Fibrosis
- Huntington’s Disease
- Familial Hypercholesterolemia
- BRCA-related breast/ovarian cancers
- Down Syndrome
- Tay-Sachs disease
🧬 Role of the Nurse in Genomics (Competencies)
- Knowledge: Understand genetics and genomics principles.
- Skills: Collect genetic histories, support decision-making.
- Attitudes: Respect cultural, ethical, and emotional aspects of genetic issues.
🧬 Genetic Testing in Nursing:
🌟 1. Definition of Genetic Testing
Genetic testing is a medical test that identifies changes in chromosomes, genes, or proteins to detect genetic disorders, assess risk of disease, or guide treatment.
In nursing, genetic testing plays a vital role in:
- Preventive care
- Diagnosis
- Family planning
- Personalized treatment strategies
🔍 2. Types of Genetic Testing
| Type | Purpose | Example |
|---|---|---|
| Diagnostic Testing | Confirms a suspected genetic condition | Testing for Huntington’s disease |
| Predictive/Presymptomatic Testing | Detects risk of developing a genetic disorder before symptoms appear | BRCA1/BRCA2 testing for breast cancer |
| Carrier Testing | Identifies individuals who carry one copy of a gene mutation | Carrier status for thalassemia |
| Prenatal Testing | Detects genetic conditions in a fetus | Amniocentesis for Down syndrome |
| Newborn Screening | Detects genetic/metabolic disorders early in life | Phenylketonuria (PKU), hypothyroidism |
| Pharmacogenomic Testing | Determines how genes affect drug response | CYP450 gene variants for drug metabolism |
| Preimplantation Genetic Diagnosis (PGD) | Testing embryos during IVF | Screening for cystic fibrosis |
| Whole Genome/Exome Sequencing | Analyzes entire genetic code | Rare or undiagnosed conditions |
🎯 3. Purposes of Genetic Testing in Nursing
- Early detection of inherited diseases
- Risk assessment for individuals and families
- Personalized treatment planning
- Support for reproductive decision-making
- Prevention and health promotion strategies
- Counseling and psychosocial support
👩⚕️ 4. Nursing Roles in Genetic Testing
A. Pre-Test Responsibilities
- Take a detailed family history (3-generation pedigree)
- Identify high-risk individuals for testing
- Provide education about:
- Purpose and types of testing
- Benefits and risks
- Possible outcomes
- Support informed consent process
- Prepare the patient emotionally
B. During Testing
- Collect and label samples (blood, saliva, tissue)
- Maintain privacy and confidentiality
- Monitor for any reactions (if invasive sampling)
C. Post-Test Responsibilities
- Help interpret results (with counselor/physician)
- Educate on implications (positive, negative, uncertain)
- Support emotionally distressed patients
- Refer to genetic counselors, psychologists, or specialists
- Involve in long-term care planning based on results
⚖️ 5. Ethical, Legal, and Social Issues (ELSI)
- Informed consent before testing
- Right to refuse testing
- Confidentiality of genetic information
- Genetic discrimination risks (insurance, employment)
- Psychological impact (guilt, anxiety, stigma)
- Family communication: implications for relatives
📘 6. Nursing Competencies in Genetic Testing (As per AACN and ANA)
- Understand basic genomic principles
- Take accurate family histories
- Identify red flags for genetic conditions
- Communicate test results in layman’s terms
- Make appropriate referrals
- Apply genetic info in care planning
- Advocate for ethical practices
🧠 7. Examples of Common Conditions Requiring Genetic Testing
- Cancer: BRCA1/2 (breast/ovarian), Lynch syndrome (colon)
- Blood disorders: Thalassemia, Sickle cell anemia
- Neurological disorders: Huntington’s, Alzheimer’s
- Metabolic diseases: PKU, Tay-Sachs
- Prenatal screening: Trisomy 21 (Down syndrome)
- Congenital anomalies: Cleft palate, heart defects
💡 8. Genetic Testing in Public Health and Community Nursing
- Organizing community awareness campaigns
- Promoting screening in high-risk populations (e.g., consanguineous marriages)
- Educating on preventive lifestyle modifications
- Involvement in national programs (like Rashtriya Bal Swasthya Karyakram)
🧬 Gene Therapy:
🌟 1. Definition of Gene Therapy
Gene therapy is a technique that involves modifying or manipulating genes within a person’s cells to treat or prevent disease. It introduces, removes, or alters genetic material to correct defective genes responsible for disease development.
🔬 2. Types of Gene Therapy
| Type | Description | Example |
|---|---|---|
| Somatic Gene Therapy | Targets non-reproductive cells; effects are not passed to offspring | Used in cancer or blood disorders |
| Germline Gene Therapy | Targets reproductive (sperm/egg) cells; changes are heritable | Currently banned in humans in most countries |
| In vivo Gene Therapy | Genes are delivered directly into the patient’s body | Used in genetic eye diseases |
| Ex vivo Gene Therapy | Cells are taken from the body, modified in the lab, and reintroduced | Used in CAR-T cell therapy for leukemia |
🧪 3. Techniques of Gene Therapy
- Gene Addition – A healthy gene is added to compensate for a faulty one.
- Gene Editing (CRISPR-Cas9) – Specific DNA sequences are modified.
- Gene Silencing (RNAi) – Faulty gene expression is turned off.
- Suicide Gene Therapy – Inserts genes into cancer cells to make them self-destruct.
🎯 4. Purposes of Gene Therapy
- Correct genetic defects
- Treat acquired diseases (e.g., cancer, HIV)
- Enhance drug response (pharmacogenomics)
- Improve organ regeneration
- Reduce need for repeated treatments (e.g., hemophilia)
🧑⚕️ 5. Role of Nurses in Gene Therapy
A. Before Gene Therapy
- Assess patient history and eligibility
- Provide education on gene therapy purpose, process, risks
- Support informed consent
- Coordinate with geneticists, counselors, and other professionals
B. During Gene Therapy
- Monitor for immediate reactions (fever, immune response)
- Ensure sterile techniques if ex vivo therapy is used
- Assist in sample handling and safe administration of vectors (viral/non-viral)
C. After Gene Therapy
- Monitor for delayed effects, such as inflammation or abnormal immune reactions
- Assess for therapeutic response
- Provide psychosocial support to reduce anxiety or unrealistic expectations
- Educate patient on follow-up care, signs of complications
💉 6. Vectors Used in Gene Therapy
| Vector Type | Description | Examples |
|---|---|---|
| Viral Vectors | Engineered viruses deliver genes | Adenovirus, Lentivirus, AAV |
| Non-Viral Vectors | Safer; lower efficiency | Liposomes, nanoparticles |
| Physical Methods | Use physical force to introduce genes | Electroporation, microinjection |
⚖️ 7. Ethical, Legal, and Social Issues in Gene Therapy
- Informed consent complexities (due to technical nature)
- Long-term risks are not fully known
- Germline therapy concerns about altering human evolution
- Cost and accessibility issues
- Potential for misuse in “gene enhancement”
- Equity in access to advanced treatments
🧠 8. Common Diseases Targeted by Gene Therapy
| Disease | Gene Therapy Approach |
|---|---|
| Hemophilia | Add gene for clotting factor |
| Cystic Fibrosis | Add functioning CFTR gene |
| Spinal Muscular Atrophy (SMA) | Replace SMN1 gene (Zolgensma) |
| Leukemia (ALL) | CAR-T cell gene therapy |
| Inherited Blindness | AAV-based therapy for RPE65 gene defect |
| Thalassemia | Gene addition to correct beta-globin |
📘 9. FDA-Approved Gene Therapies (Examples)
- Zolgensma: For spinal muscular atrophy (SMA)
- Luxturna: For inherited retinal disease
- CAR-T Cell Therapies: For leukemia, lymphoma
🧬 10. Gene Therapy vs. Genetic Testing
| Aspect | Gene Therapy | Genetic Testing |
|---|---|---|
| Purpose | To treat or cure disease | To detect or assess risk |
| Action | Modifies gene expression | Does not alter genes |
| Invasiveness | Invasive (cell manipulation) | Mostly non-invasive |
| Outcome | Therapeutic | Diagnostic/Preventive |
📌 Key Points for Nursing Education
- Nurses must understand basic genetics and gene therapy principles
- Stay updated on current research and clinical trials
- Maintain ethical standards
- Collaborate with interdisciplinary teams
- Educate and empower patients through counseling and support
🧬 Genetic Counseling:
🌟 1. Definition of Genetic Counseling
Genetic counseling is a communication process that helps individuals and families understand and adapt to the medical, psychological, and familial implications of genetic contributions to disease.
It involves:
- Interpretation of family and medical histories
- Risk assessment
- Education about inheritance, testing, management, prevention
- Support for decision-making and coping
🎯 2. Goals of Genetic Counseling
- Educate patients about genetic conditions
- Assess risk of inherited disorders
- Discuss options for genetic testing
- Support decision-making regarding family planning or treatment
- Help cope with diagnosis or risk of genetic disorders
- Promote informed choices and autonomy
🔬 3. Types of Genetic Counseling
| Type | Focus Area | Examples |
|---|---|---|
| Prenatal Counseling | Counseling during pregnancy | Down syndrome, neural tube defects |
| Pediatric Counseling | For children with congenital or developmental disorders | Cystic fibrosis, muscular dystrophy |
| Adult/Presymptomatic Counseling | For adults at risk of late-onset conditions | Huntington’s, BRCA1/BRCA2 cancers |
| Carrier Counseling | For individuals with carrier status | Thalassemia, Tay-Sachs |
| Pharmacogenetic Counseling | Medication response based on genes | Warfarin, antidepressants |
| Cancer Genetic Counseling | For familial or inherited cancer syndromes | Hereditary breast/colon cancer |
🧭 4. Process of Genetic Counseling
Step 1: Referral/Intake
- Patient is referred based on family history or diagnosis.
- Nurse gathers initial data.
Step 2: Family History Collection
- Construct a three-generation pedigree.
- Identify patterns suggestive of inheritance.
Step 3: Risk Assessment
- Assess genetic risk based on inheritance patterns and test results.
Step 4: Education and Discussion
- Explain condition, inheritance, testing, treatment options.
- Discuss emotional and social impacts.
Step 5: Genetic Testing (if required)
- Explain testing procedures, limitations, implications.
- Arrange informed consent and coordinate testing.
Step 6: Results Interpretation and Support
- Help patient/family understand test results.
- Provide psychological support and referrals as needed.
Step 7: Follow-up and Decision Support
- Offer ongoing support and guide decisions on management or family planning.
👩⚕️ 5. Role of Nurses in Genetic Counseling
✅ Before Counseling
- Collect complete medical and family history
- Identify individuals needing counseling (e.g., family history of birth defects, cancer)
- Educate about the purpose and benefits of genetic counseling
✅ During Counseling
- Support emotional well-being during sessions
- Ensure cultural sensitivity and clear communication
- Advocate for patient rights and informed decisions
✅ After Counseling
- Assist with follow-up care or testing
- Provide education materials
- Support patient/family through decision-making process
- Refer to support groups or specialists if needed
⚖️ 6. Ethical and Legal Considerations
- Informed consent before genetic testing
- Confidentiality of genetic information
- Right not to know (some may choose not to receive results)
- Psychological effects (e.g., anxiety, guilt, fear)
- Discrimination risks (e.g., insurance, jobs)
- Respect cultural and religious values in decision-making
🧠 7. Common Conditions Requiring Genetic Counseling
| Condition | Why Counseling is Needed |
|---|---|
| Thalassemia | For carrier detection in couples |
| Breast cancer (BRCA1/2) | To assess familial cancer risk |
| Cystic fibrosis | For family planning and carrier testing |
| Down syndrome | Prenatal risk and testing |
| Huntington’s disease | Presymptomatic counseling |
| Hemophilia | Inherited bleeding disorder, male transmission |
📘 8. Importance of Genetic Counseling in Nursing Practice
- Nurses often serve as the first point of contact for families
- Play a key role in recognizing risk factors
- Provide education and empathy
- Act as a liaison between patient and genetic counselor
- Assist in genetic literacy and decision-making
💬 Real-Life Example Scenario (Nursing Perspective)
A 28-year-old woman is referred for counseling after her brother is diagnosed with muscular dystrophy. The nurse collects her family history, helps her understand inheritance risks, discusses carrier testing, and supports her emotionally during decision-making.
⚖️🧬 Legal and Ethical Issues Related to Genetics in Nursing:
As genetic science advances rapidly, nurses are often on the frontline of applying genetic knowledge. However, this brings up many legal, ethical, and social challenges. Nurses must be aware of these issues to protect patients’ rights, uphold ethical standards, and maintain legal compliance.
🌟 1. Importance of Legal and Ethical Awareness in Genetic Nursing
- Protects patient autonomy and dignity
- Prevents discrimination and misuse of information
- Promotes informed decision-making
- Builds trust and credibility in the healthcare system
- Ensures compliance with national and international laws
⚖️ 2. Legal Issues in Genetics Nursing
🔹 A. Informed Consent
- Patients must voluntarily agree to genetic testing or therapy after receiving clear, accurate, and complete information.
- Nurses must ensure:
- The patient understands the purpose, procedure, risks, benefits, and alternatives.
- Consent is documented before testing.
- The right to refuse testing is respected.
🔹 B. Confidentiality and Privacy
- Genetic information is highly sensitive and must be kept confidential.
- Nurses must safeguard:
- Genetic test results
- Family history
- Counseling sessions
- Unauthorized disclosure can result in legal liability under laws like:
- Health Insurance Portability and Accountability Act (HIPAA – USA)
- Information Technology Act (India) for data protection
🔹 C. Genetic Discrimination
- Individuals may face discrimination based on their genetic status in:
- Employment
- Health insurance
- Social stigma
- Nurses must advocate against such discrimination and be aware of:
- GINA (Genetic Information Nondiscrimination Act – USA)
- Indian laws are evolving in this area; protection is limited.
🔹 D. Testing in Children and Vulnerable Populations
- Special legal protection is required for:
- Minors
- Individuals with intellectual disabilities
- Pregnant women
- Nurses must ensure that parents or guardians provide legal consent and understand long-term consequences.
🔹 E. Duty to Warn vs. Confidentiality
- Legal dilemma: Should a nurse or healthcare provider warn family members of a genetic risk if the patient refuses to disclose it?
- Laws vary, but generally:
- Patient confidentiality is prioritized
- Nurses should encourage patients to share information with relatives
🤝 3. Ethical Issues in Genetics Nursing
🔸 A. Autonomy
- Patients have the right to:
- Make informed choices about testing or therapy
- Decline genetic knowledge
- Nurses must respect these rights even if the decision conflicts with medical advice.
🔸 B. Beneficence and Non-Maleficence
- Nurses should:
- Do good (beneficence) by offering support and education
- Avoid harm (non-maleficence) by preventing emotional, psychological, or social distress due to genetic information
🔸 C. Justice and Equity
- Genetic services must be:
- Fairly distributed across populations
- Accessible to marginalized groups (rural poor, disabled, etc.)
- Nurses must advocate for equity in access to testing and treatment.
🔸 D. Psychological Impact and Counseling
- Patients may experience:
- Anxiety
- Guilt
- Fear
- Nurses must provide empathetic counseling and refer to psychologists when necessary.
🔸 E. Ethical Use of Genetic Technologies
- Issues arise with:
- Gene editing (CRISPR) – altering the human genome
- Designer babies – selecting traits like intelligence or appearance
- Nurses must engage in ethical discussions and discourage misuse.
🧑⚕️ 4. Role of the Nurse in Managing Legal & Ethical Issues
| Responsibility | Explanation |
|---|---|
| Advocate | Protect patient rights and promote fair treatment |
| Educator | Provide accurate information on risks, benefits, and laws |
| Communicator | Facilitate discussions between patients, families, and teams |
| Ethical Decision Support | Assist in making ethically sound healthcare choices |
| Policy Follower | Stay updated with national and institutional policies |
📌 5. Real-Life Scenarios
| Scenario | Legal/Ethical Concern |
|---|---|
| A nurse learns that a patient tested positive for Huntington’s disease but refuses to tell family members. | Conflict between confidentiality and duty to warn |
| A woman wants BRCA testing, but her husband refuses to give permission. | Issue of autonomy and gender rights |
| A hospital denies insurance to a child with a thalassemia gene. | Genetic discrimination |
| A prenatal test reveals a chromosomal disorder. Parents request termination. | Ethical concerns around selective abortion |
📘 6. Indian Context: Legal Status
- No specific law yet dedicated solely to genetic testing or counseling.
- Related laws:
- Pre-Conception and Pre-Natal Diagnostic Techniques (PCPNDT) Act, 1994 – prohibits sex determination
- Information Technology Act, 2000 – for data privacy
- Rights of Persons with Disabilities Act, 2016 – against discrimination
- Future legal reforms are needed for genetic protection.
👩⚕️🧬 Role of Nurse in Genetic Services and Counseling
Nurses play a vital role in integrating genetic science into healthcare by providing genetic services and counseling support. They serve as educators, advocates, coordinators, and caregivers, helping patients and families understand and cope with genetic conditions.
🌟 1. Health History Collection and Risk Assessment
- Take a detailed family history (3-generation pedigree).
- Identify patterns of inherited disorders or genetic risks.
- Recognize red flags (e.g., early-onset disease, multiple affected family members).
🌟 2. Education and Information Sharing
- Provide clear, simple explanations of:
- Basic genetic concepts (genes, inheritance, mutations)
- The purpose, procedure, and implications of genetic testing
- Differences between carrier, affected, and at-risk individuals
- Clarify testing options, limitations, and benefits.
🌟 3. Emotional and Psychosocial Support
- Address patient and family fears, guilt, anxiety, or stress related to:
- Genetic diagnosis
- Family implications
- Risk to children
- Offer empathy, reassurance, and counseling support.
- Refer to psychologists or support groups if needed.
🌟 4. Coordination of Genetic Testing and Services
- Arrange and assist with sample collection (blood, saliva).
- Ensure informed consent is obtained and documented.
- Collaborate with:
- Genetic counselors
- Physicians
- Laboratories
- Ethics committees, if needed
🌟 5. Interpretation Support and Follow-up
- Help patients understand test results (positive, negative, variant of uncertain significance).
- Explain what the results mean for:
- Their health
- Family planning
- Treatment and lifestyle
- Guide them through next steps (screening, preventive care, therapy).
🌟 6. Advocacy and Ethical Responsibility
- Protect patient confidentiality and privacy of genetic information.
- Advocate for non-discriminatory access to genetic care.
- Ensure patients make autonomous, informed choices.
- Uphold ethical principles like:
- Do no harm
- Justice
- Respect for autonomy
🌟 7. Community Education and Awareness
- Educate the public about:
- Common genetic disorders (e.g., thalassemia, sickle cell, Down syndrome)
- Benefits of early screening and carrier detection
- Consanguineous marriage risks
- Promote genetic literacy in schools, maternal health centers, and rural areas.
🌟 8. Integration into Care Planning
- Incorporate genetic findings into nursing care plans.
- Modify care based on genetic risk or diagnosis (e.g., special precautions, follow-ups).
- Work with multidisciplinary teams for long-term management.
📌 Real-Life Examples of Nurse Involvement
- Supporting a mother with a child diagnosed with cystic fibrosis
- Educating a couple before prenatal testing for Down syndrome
- Coordinating testing for a family with hereditary cancer
- Guiding a teenager who is a carrier of sickle cell gene
✅ In Summary: Nurses Provide…
| Function | Details |
|---|---|
| Assessment | Family history, risk identification |
| Education | Genetic concepts, testing process |
| Support | Emotional, ethical, psychosocial |
| Coordination | Testing, referrals, multidisciplinary care |
| Follow-up | Interpreting results, future planning |
| Advocacy | Protecting rights and autonomy |
| Community Involvement | Awareness, prevention, screening programs |
🧬 Pathological Changes in Gastric Cancer
(Detailed academic explanation in a structured narrative with clinical relevance)
Gastric cancer, also known as stomach cancer, is a malignant neoplasm originating primarily from the gastric mucosa. It is the fifth most common cancer worldwide and the third leading cause of cancer-related deaths. The most frequent type is adenocarcinoma, but others include lymphomas, GISTs (gastrointestinal stromal tumors), and neuroendocrine tumors.
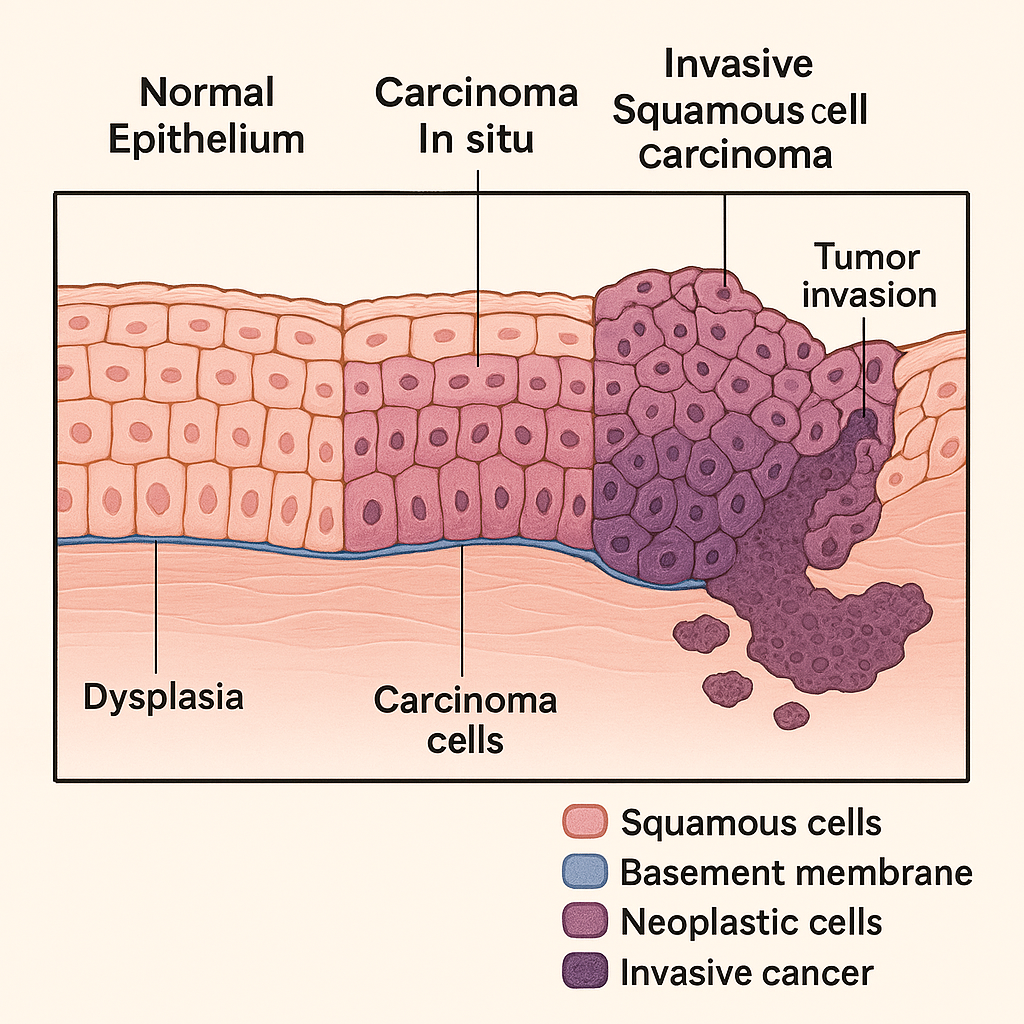
Let’s explore the sequential pathological changes, from normal gastric mucosa to invasive cancer, with a focus on adenocarcinoma.
🔄 1. Histogenesis of Gastric Adenocarcinoma (Correa’s Cascade)
The development of gastric adenocarcinoma typically follows a multistep process, especially in intestinal-type carcinoma, often described by the Correa pathway:
🔹 A. Normal Gastric Mucosa
- Comprised of columnar epithelial cells with specialized gastric glands (chief, parietal, mucous, G cells).
- Maintains tight cell junctions, polarity, and low mitotic activity.
🔹 B. Chronic Gastritis
- Persistent H. pylori infection, autoimmunity, or dietary carcinogens (e.g., nitrosamines) cause:
- Mucosal inflammation
- Neutrophil infiltration
- Lymphoid follicles
- Glandular atrophy may develop over time.
🔹 C. Intestinal Metaplasia
- Native gastric epithelium transforms into intestinal-type epithelium (goblet cells, absorptive cells, Paneth cells).
- Seen as a defensive adaptation but is premalignant.
🔹 D. Dysplasia (Intraepithelial Neoplasia)
- Low-grade dysplasia: Architectural distortion, mild nuclear atypia.
- High-grade dysplasia: Loss of polarity, marked pleomorphism, hyperchromasia, frequent mitoses.
- The basement membrane remains intact.
🔹 E. Invasive Gastric Adenocarcinoma
- Malignant epithelial cells invade beyond the basement membrane into:
- Lamina propria
- Muscularis mucosae
- Submucosa
- Muscularis propria
- Histological types:
- Intestinal type: Gland-forming, better differentiated, solid mass.
- Diffuse type: Poorly differentiated, signet ring cells, infiltrative, rigid stomach wall (linitis plastica).
🧫 2. Microscopic Features by Histological Type
📘 Intestinal Type Adenocarcinoma
- Forms gland-like structures
- Associated with H. pylori, chronic gastritis, and atrophy
- Nuclear atypia, hyperchromasia, glandular crowding
📘 Diffuse Type Adenocarcinoma
- No gland formation
- Signet ring cells with mucin pushing nuclei to periphery
- Loss of E-cadherin expression
- Thickened gastric wall, “leather bottle” appearance
👁️ 3. Macroscopic (Gross) Types of Gastric Cancer
(Borrmann Classification for Advanced Gastric Cancer)
| Type | Appearance |
|---|---|
| Type I | Polypoid/fungating mass |
| Type II | Ulcerated lesion with raised edges |
| Type III | Ulcerated and infiltrative |
| Type IV | Diffusely infiltrative (linitis plastica) |
🧬 4. Molecular and Genetic Alterations
- H. pylori → inflammation → DNA damage
- p53 mutations, APC, KRAS, E-cadherin (CDH1) loss in diffuse type
- Microsatellite instability (MSI) and Epstein-Barr virus (EBV) linked to specific subtypes
📊 Summary of Pathological Changes in Gastric Cancer
| Stage | Changes |
|---|---|
| Normal Gastric Epithelium | Intact glandular epithelium |
| Chronic Gastritis | Inflammatory infiltrate, gland loss |
| Intestinal Metaplasia | Goblet cells replace gastric epithelium |
| Dysplasia | Nuclear atypia, architectural distortion |
| Carcinoma In Situ | Severe dysplasia with intact basement membrane |
| Invasive Carcinoma | Malignant cells invade mucosa and deeper layers |