BSC SEM 4 UNIT 2 ADULT HEALTH NURSING 2
UNIT 2 Nursing management of patient with disorder of eye
👁️ Anatomy & Physiology of the Eye
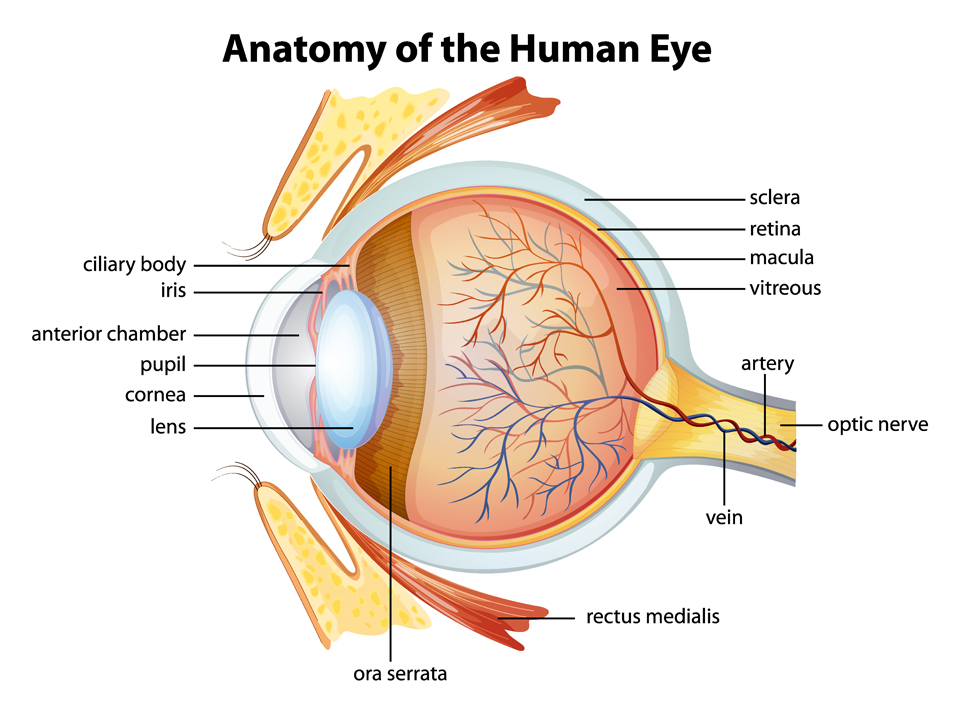
🔹 I. Introduction:
The human eye is a special sensory organ responsible for vision. It works like a camera: gathering light, focusing it, converting it into electrical signals, and sending it to the brain for interpretation.
🟢 II. External Structures of the Eye:
| 🔸Structure | 🔍 Function |
|---|---|
| 👁️ Eyelids | Protect the eye from injury, light, and dehydration |
| 👁️ Eyelashes | Trap dust and particles |
| 👁️ Eyebrows | Prevent sweat and debris from entering the eye |
| 💧 Lacrimal Glands | Produce tears to moisten, lubricate, and protect the eye |
| 👓 Conjunctiva | Transparent membrane covering the sclera and inner eyelid; prevents microbes from entering |
🟡 III. Layers of the Eyeball (Three Tunics):
🔸 1. Fibrous Tunic (Outer Layer):
- 🟤 Sclera: White, opaque outer layer — gives shape & protects internal parts
- 🔵 Cornea: Transparent anterior portion — refracts (bends) light toward the lens
🔸 2. Vascular Tunic / Uvea (Middle Layer):
- 🟣 Choroid: Rich in blood vessels and melanin — absorbs excess light & nourishes retina
- 🌀 Ciliary Body:
- Contains ciliary muscles — control lens shape for focusing (accommodation)
- Secretes aqueous humor
- 🌈 Iris: Colored part; controls pupil size & regulates amount of light entering
- ⚫ Pupil: Adjustable opening; constricts or dilates based on light intensity
🔸 3. Retina (Innermost Layer):
- Contains photoreceptor cells:
- 🔹 Rods: Detect dim light (night vision), black & white
- 🔸 Cones: Detect bright light and color (RGB)
- 📍 Macula lutea: Central vision area
- 🔘 Fovea centralis: Sharpest vision; densely packed cones
- 🚫 Optic Disc (Blind Spot): No photoreceptors; where optic nerve exits
🔵 IV. Internal Structures:
🧿 Lens:
- Transparent, flexible, biconvex structure
- Focuses light rays onto retina
- Controlled by ciliary muscles for near/far focus (accommodation)
💧 V. Chambers of the Eye & Fluids:
| 💠 Chamber | 🧪 Fluid | 💡 Function |
|---|---|---|
| 🔹 Anterior Chamber (between cornea & iris) | Aqueous humor | Nourishes cornea & lens; maintains intraocular pressure |
| 🔸 Posterior Chamber (between iris & lens) | Aqueous humor | Same as above |
| 🔵 Vitreous Chamber (between lens & retina) | Vitreous humor (gel) | Maintains eyeball shape; keeps retina in place |
🧠 VI. Nervous Connections:
- 🧬 Optic Nerve (CN II): Transmits visual signals from retina to brain
- 🧠 Visual Cortex (Occipital Lobe): Processes images sent by the optic nerve
- 🔁 Optic Chiasma: Crosses some nerve fibers to allow binocular vision
⚙️ VII. Physiology of Vision – Step-by-Step:
- 🌟 Light enters through the cornea → aqueous humor → pupil → lens
- 🔍 Lens focuses the light onto the retina
- 📸 Photoreceptors (rods/cones) convert light into electrical signals
- 🔌 Bipolar and ganglion cells transmit impulses
- 📡 Optic nerve carries signal to the visual cortex
- 🧠 Brain interprets the signal into images
✅ Key Functions of Eye Parts (Quick Recap):
| 👁️ Part | 📌 Function |
|---|---|
| Cornea | Refraction (bends light) |
| Lens | Fine focus of light |
| Retina | Photoreception & transduction |
| Iris | Regulates light entry |
| Aqueous humor | Nourishment & pressure maintenance |
| Vitreous humor | Shape maintenance & retina support |
| Optic Nerve | Signal transmission to brain |
👁️🗨️ History-Related Management of a Patient with Eye Disorders
Understanding the patient’s history is the foundation for diagnosing and managing any eye disorder effectively. Below is a detailed guide to collecting history and using it for clinical management.
📋 I. Comprehensive History-Taking – Key Elements:
🔹 1. Chief Complaint (CC):
- What brought the patient to the clinic?
- Examples:
🔸 Blurred vision
🔸 Eye pain
🔸 Redness
🔸 Watering/discharge
🔸 Double vision (diplopia)
🔸 Vision loss
- Examples:
🔹 2. History of Present Illness (HPI):
Ask about the onset, duration, progression, and pattern of symptoms:
- 🕐 When did it start? Sudden or gradual?
- 📈 Is it getting better, worse, or stable?
- 🔄 Any triggers or relieving factors?
- 👁️ One eye or both?
- ⏳ Intermittent or continuous?
- 🔥 Associated symptoms like photophobia, pain, discharge, itching?
🔹 3. Past Ocular History:
- 👓 Use of glasses or contact lenses?
- 👁️ Previous eye surgeries or trauma?
- 🔍 History of any eye infections (e.g., conjunctivitis, keratitis)?
- 🧬 Any history of glaucoma, cataract, macular degeneration?
🔹 4. Medical History:
- 🩺 Systemic illnesses that may affect the eye:
- Diabetes mellitus (→ diabetic retinopathy)
- Hypertension (→ hypertensive retinopathy)
- Thyroid disease (→ proptosis)
- Autoimmune disorders (e.g., rheumatoid arthritis → uveitis)
🔹 5. Medication History:
- 💊 Any current or past medication?
- Long-term steroid use (→ risk of glaucoma/cataract)
- Antimalarials (e.g., hydroxychloroquine → macular toxicity)
- Antihistamines, antidepressants (→ dry eye)
🔹 6. Family History:
- 👨👩👧👦 History of genetic eye disorders?
- E.g., Glaucoma, Retinitis Pigmentosa, Color blindness, Myopia
🔹 7. Occupational and Lifestyle History:
- 🧑🏭 Exposure to dust, chemicals, welding light?
- 💻 Hours of screen time (→ computer vision syndrome)
- 🌞 Outdoor work? (UV light exposure → pterygium)
- 🧴 Use of eye makeup or poor hygiene?
🔹 8. Allergy & Immunization History:
- 🧪 Allergies to eye drops or preservatives?
- 💉 Tetanus and other relevant vaccinations?
⚕️ II. Nursing & Clinical Management Based on History:
✅ 1. Assessment Planning:
- Perform relevant eye exams based on symptoms:
- Visual acuity test
- Pupil reaction
- Slit-lamp examination
- Tonometry (IOP check)
- Fundoscopy
✅ 2. Diagnosis:
- Use the detailed history to differentiate between conditions:
- Red eye + discharge + itching → likely allergic conjunctivitis
- Sudden vision loss + pain → acute angle-closure glaucoma
- Gradual vision loss → cataract or macular degeneration
✅ 3. Intervention & Management:
- 🧴 Start specific topical or systemic medications as indicated
- 🩹 Provide eye hygiene instructions
- 🧊 Apply cool compress for inflammation
- 🕶️ Recommend sunglasses or protective eyewear
- 🛌 Advise rest and reduced screen exposure if applicable
🧠 III. Patient Education Based on History:
| 💡 History Factor | 📘 Education Strategy |
|---|---|
| Contact lens use | Teach about hygiene, lens care, avoid overnight use |
| Diabetes/HTN | Emphasize regular eye check-ups |
| Prolonged screen time | Recommend 20-20-20 rule, anti-glare screen |
| UV exposure | Recommend protective sunglasses |
| Allergy history | Avoid allergens, use prescribed antihistamines |
| Family history | Early screening, genetic counseling if necessary |
📌 Conclusion / Key Points:
🔹 Always begin management with thorough history-taking
🔹 History guides clinical reasoning and appropriate intervention
🔹 History helps in early detection of systemic causes of eye disorders
🔹 Guides preventive care, lifestyle modification, and referral if needed
👁️🗨️ Physical Assessment.
🔍 I. Purpose of Physical Eye Assessment:
✅ To evaluate visual function and eye health
✅ To detect abnormalities or injuries
✅ To assist in diagnosis and nursing care planning
✅ To monitor progress during treatment
🧑⚕️ II. General Preparation for Eye Assessment:
🔹 Ensure adequate lighting in the room
🔹 Use clean gloves and sanitized equipment
🔹 Gain patient consent and explain the procedure
🔹 Ensure the patient is seated comfortably at eye level
🔬 III. Physical Examination Steps (Head-to-Toe Order):
🔸 1. Inspection:
Observe both eyes visually and symmetrically
| Area | What to Observe |
|---|---|
| 👁️ Eyelids | Swelling, redness, ptosis (drooping) |
| 👁️ Eyelashes | Inward turning (entropion), outward turning (ectropion) |
| 👀 Conjunctiva | Redness, discharge, pallor, hemorrhage |
| 👁️ Sclera | White (normal), yellow (jaundice), blue (osteogenesis imperfecta) |
| 👁️ Cornea | Clarity, opacity, ulceration, foreign body |
| 🌈 Iris & Pupil | Shape, symmetry, color, response to light |
🔸 2. Palpation:
- Gently palpate around the eye for:
- Swelling
- Tenderness
- Displacement
- Lacrimal gland enlargement
🔸 3. Pupil Assessment (PERRLA):
PERRLA = Pupils Equal, Round, Reactive to Light and Accommodation
✅ Direct & consensual light reflex
✅ Check pupil size and shape
✅ Assess for accommodation (pupils constrict as object moves close)
🔸 4. Visual Acuity Test (Snellen Chart):
- Performed one eye at a time (cover the other)
- Patient reads from 20 feet
- Record as a fraction (e.g., 20/20 = normal vision)
🔸 5. Extraocular Movements (EOMs):
- Use the “H-pattern” test
- Ask the patient to follow your finger with only their eyes
- Assesses function of 6 eye muscles and cranial nerves III, IV, VI
🔸 6. Visual Fields by Confrontation:
- Stand in front of patient, cover one eye on both sides
- Move fingers in periphery — patient signals when seen
- Tests for peripheral vision loss (e.g., in glaucoma)
🔸 7. Ophthalmoscopic Examination:
Used to examine internal structures:
- Retina
- Optic disc
- Macula
- Blood vessels
- Look for: hemorrhages, exudates, papilledema, retinal detachment
⚕️ IV. Management Based on Assessment Findings:
| Finding | Probable Condition | Immediate Management |
|---|---|---|
| Redness + discharge | Conjunctivitis | Warm compress, antibiotic drops |
| Visual field loss | Glaucoma | Refer for tonometry, eye drops to reduce IOP |
| Cloudy lens | Cataract | Pre-surgical referral, educate on surgery |
| Papilledema | ↑ Intracranial pressure | Neurology referral |
| Ptosis + fatigue | Myasthenia gravis | Neurology consult, eye protection |
| Yellow sclera | Jaundice | Evaluate liver function |
| Unequal pupils | Neurological emergency | Immediate medical attention |
📘 V. Nursing Responsibilities During Eye Disorder Care:
🔹 Perform routine eye assessments and document changes
🔹 Administer prescribed medications (eye drops/ointments)
🔹 Educate about hand hygiene and eye care
🔹 Ensure eye protection with patches/shields if needed
🔹 Position patient in well-lit area to reduce falls
🔹 Refer for specialist care if critical signs noted
🧠 VI. Summary (Key Points):
✅ Physical assessment is essential in diagnosing and managing eye problems
✅ Use systematic inspection, palpation, and functional testing
✅ Abnormal findings direct appropriate interventions, referrals, and education
✅ Nurses play a crucial role in monitoring and supporting patient vision care
👁️🗨️ Diagnostic Tests.
🧪 I. Importance of Diagnostic Tests in Eye Care:
✔️ Confirm clinical diagnosis
✔️ Assess severity and progression of eye disease
✔️ Guide medical, surgical, and nursing management
✔️ Monitor treatment outcomes and complications
🔬 II. Common Diagnostic Tests for Eye Disorders:
🔹 1. Visual Acuity Test (Snellen Chart):
- Purpose: Checks sharpness of vision
- Procedure: Patient reads letters from a chart at 20 feet
- Use: Diagnose refractive errors (myopia, hyperopia)
➡️ Management:
- Prescription of glasses/contact lenses
- Referral to ophthalmologist if uncorrected vision remains poor
🔹 2. Tonometry:
- Purpose: Measures intraocular pressure (IOP)
- Use: Detect glaucoma
➡️ Management:
- If IOP is high → Initiate anti-glaucoma medications (e.g., timolol, latanoprost)
- Educate on medication compliance
- Regular follow-ups to prevent optic nerve damage
🔹 3. Slit Lamp Examination:
- Purpose: Detailed view of anterior structures (cornea, lens, iris)
- Use: Diagnose conjunctivitis, cataract, corneal ulcer, uveitis
➡️ Management:
- Targeted treatment:
- Antibiotics/antivirals for infections
- Anti-inflammatory drops for uveitis
- Cataract → surgical referral
🔹 4. Ophthalmoscopy (Fundoscopy):
- Purpose: Visualizes retina, macula, optic disc, blood vessels
- Use: Detects:
- Diabetic retinopathy
- Retinal detachment
- Hypertensive changes
- Papilledema
➡️ Management:
- Retinopathy → Tight control of diabetes/hypertension, retinal laser therapy
- Detachment → Immediate ophthalmic surgery
- Papilledema → Neuro referral for brain imaging
🔹 5. Refraction Test:
- Purpose: Measures refractive error
- Use: Prescribe corrective lenses
➡️ Management:
- Glasses or contact lens fitting
- LASIK consultation if desired
🔹 6. Fluorescein Dye Test:
- Purpose: Detects corneal abrasions, ulcers, foreign bodies
- Use: Dye stains damaged corneal areas under blue light
➡️ Management:
- Prescribe antibiotic drops/ointment
- Instruct on eye protection
- Daily review if ulcer present
🔹 7. Visual Field Test (Perimetry):
- Purpose: Checks peripheral vision
- Use: Diagnose glaucoma, optic nerve damage, brain tumors
➡️ Management:
- Identify field loss pattern
- Continue glaucoma therapy or neurology referral
🔹 8. Color Vision Test (Ishihara Plates):
- Purpose: Assess ability to distinguish colors
- Use: Detect color blindness, especially in children or drivers
➡️ Management:
- Education and career counseling
- No medical treatment, but supportive measures can be given
🔹 9. A-Scan and B-Scan Ultrasonography:
- Purpose: Measure eye length or view internal eye structures
- Use: Pre-cataract surgery, retinal detachment, intraocular tumors
➡️ Management:
- Surgical planning (e.g., cataract lens selection)
- Surgical referral for detachment or tumor
🔹 10. OCT (Optical Coherence Tomography):
- Purpose: Cross-sectional imaging of retina and optic nerve
- Use: Macular degeneration, diabetic retinopathy, glaucoma
➡️ Management:
- Laser therapy, anti-VEGF injections (e.g., ranibizumab)
- Disease monitoring over time
⚕️ III. Nursing Responsibilities in Diagnostic Testing:
🩺 Before Test:
- Explain the procedure to reduce anxiety
- Check for allergies (e.g., fluorescein dye)
- Obtain informed consent
🩺 During Test:
- Assist patient positioning
- Ensure infection control
- Monitor for adverse reactions
🩺 After Test:
- Document findings
- Monitor for discomfort, allergic reaction
- Reinforce follow-up and medication instructions
📘 IV. Conclusion / Key Takeaways:
✔️ Eye diagnostic tests are critical tools for confirming diagnosis
✔️ Results guide the treatment plan, including medical or surgical steps
✔️ Nurses play an essential role in preparing, assisting, and educating the patient
✔️ Prompt testing ensures better outcomes and vision preservation
👓 Refractive Errors of the Eye
📘 Definition:
Refractive errors are vision problems that occur when the eye fails to focus light properly on the retina, resulting in blurred or distorted vision.
🔹 Normally, light rays entering the eye should be focused directly on the retina (the light-sensitive layer at the back of the eye) to form a clear image.
🔹 In refractive errors, the shape or structure of the eye prevents proper focusing, leading to blurry vision, either at near, far, or both distances.
⚠️ Causes of Refractive Errors:
🔸 1. Abnormal Shape of the Eyeball
- Too long eyeball → Myopia (nearsightedness)
- Too short eyeball → Hyperopia (farsightedness)
🔸 2. Irregular Curvature of the Cornea or Lens
- Uneven or asymmetrical curve → Astigmatism
🔸 3. Age-related Changes in the Lens
- Loss of lens elasticity with age → Presbyopia
🔍 Other Contributing Factors:
| 🔹 Factor | 🔎 Description |
|---|---|
| 🧬 Genetics | Family history of myopia or hyperopia |
| 📚 Prolonged Near Work | Reading, screen time in childhood → may lead to myopia |
| 💡 Poor Lighting Conditions | During visual tasks |
| ⚙️ Uncorrected Vision Strain | May worsen refractive conditions over time |
| 📈 Aging Process | Natural hardening of the lens (presbyopia begins ~40 years) |
👁️🗨️ Types of Refractive Errors
Refractive errors occur when light rays are not properly focused on the retina due to abnormalities in the shape or structure of the eye.
🔹 1. Myopia (Nearsightedness) –
📘 Definition:
A condition where near objects are seen clearly, but distant objects appear blurry.
🔍 Cause:
- The eyeball is too long, or
- The cornea is too curved
➡️ Light focuses in front of the retina.
👁️🗨️ Visual Experience:
- Clear vision for reading
- Blurry vision while watching TV or driving
🔸 2. Hyperopia (Farsightedness) –
📘 Definition:
A condition where distant objects are seen clearly, but near objects appear blurry.
🔍 Cause:
- The eyeball is too short, or
- The cornea is too flat
➡️ Light focuses behind the retina.
👁️🗨️ Visual Experience:
- Clear distance vision
- Strain while reading or doing close work
🔹 3. Astigmatism –
📘 Definition:
A refractive error caused by an irregular curvature of the cornea or lens, leading to blurred or distorted vision at all distances.
🔍 Cause:
- The cornea or lens is shaped like a football, not a sphere
- Causes multiple focal points instead of one
👁️🗨️ Visual Experience:
- Wavy, blurred, or double vision
- Eye strain, headaches
🔸 4. Presbyopia –
📘 Definition:
An age-related loss of the eye’s ability to focus on near objects, usually occurring after age 40.
🔍 Cause:
- Loss of elasticity in the natural lens
- Decreased ability to accommodate near objects
👁️🗨️ Visual Experience:
- Difficulty reading small print
- Holding books at arm’s length
- Eye fatigue with close work
📊 Comparison Table of Refractive Errors:
| 🧠 Type | 🔍 Focal Point | 👁️ Distance Vision | 📚 Near Vision | 🧬 Common Cause |
|---|---|---|---|---|
| Myopia | In front of retina | ❌ Blurred | ✅ Clear | Long eyeball |
| Hyperopia | Behind the retina | ✅ Clear | ❌ Blurred | Short eyeball |
| Astigmatism | Multiple points | ❌ Distorted | ❌ Distorted | Irregular cornea |
| Presbyopia | Behind retina (age-related) | ❌ Blurred | ❌ Blurred | Aging lens |
🔬 Pathophysiology of Refractive Errors
Refractive errors occur when the eye is unable to properly bend (refract) and focus light rays onto the retina. The retina is the innermost, light-sensitive layer of the eye responsible for transmitting visual signals to the brain.
Normal vision requires that light rays be perfectly focused on the retina. In refractive errors, the light rays fall in front of, behind, or scatter away from the retina.
🔹 1. Myopia (Nearsightedness)
🧠 Pathophysiology:
- In myopia, the axial length of the eyeball is longer than normal, or the cornea is too curved.
- This causes incoming parallel light rays to converge and focus in front of the retina, rather than directly on it.
- As a result, distant objects appear blurry, while near objects can be seen clearly.
🧪 Summary:
- 🔁 Light focuses in front of retina
- 📏 Eyeball too long (axial myopia)
- 🔄 Corneal curvature too steep (refractive myopia)
🔸 2. Hyperopia (Farsightedness)
🧠 Pathophysiology:
- In hyperopia, the eyeball is shorter than normal, or the cornea is too flat.
- Light rays entering the eye are focused behind the retina when looking at near objects.
- The eye may initially compensate by accommodating the lens, but this leads to eye strain and blurry near vision.
🧪 Summary:
- 🔁 Light focuses behind the retina
- 📏 Eyeball too short (axial hyperopia)
- 🔄 Corneal curvature too flat (refractive hyperopia)
🔹 3. Astigmatism
🧠 Pathophysiology:
- In astigmatism, the cornea or lens has an irregular curvature, often shaped more like a football than a basketball.
- Because of this asymmetry, light rays entering the eye are refracted unequally, resulting in multiple focal points, either in front of or behind the retina.
- The result is distorted or blurred vision at all distances.
🧪 Summary:
- 🔁 Light rays do not meet at a single focal point
- ⚙️ Cornea/lens has uneven curvature
- 🌀 Causes scattered or blurred image on the retina
🔸 4. Presbyopia
🧠 Pathophysiology:
- Presbyopia is an age-related condition caused by the gradual loss of flexibility in the crystalline lens and weakening of ciliary muscles.
- The lens becomes less elastic and unable to accommodate (change shape) for near vision.
- This results in difficulty focusing on close objects, especially during reading or detailed work.
🧪 Summary:
- 🧓 Age-related degeneration of lens elasticity
- ❌ Accommodation failure due to lens hardening
- 🔁 Light focuses behind the retina during near tasks
✅ Combined Overview Table – Pathophysiology at a Glance
| Refractive Error | Focal Point | Structural Cause | Key Pathophysiology |
|---|---|---|---|
| Myopia | In front of retina | Long eyeball or steep cornea | Excessive refraction or axial elongation |
| Hyperopia | Behind the retina | Short eyeball or flat cornea | Inadequate refraction or reduced axial length |
| Astigmatism | Multiple points | Irregular corneal/lens shape | Unequal light refraction across meridians |
| Presbyopia | Behind retina (during near focus) | Aging lens + weak ciliary muscles | Loss of accommodation due to rigid lens |
👁️🗨️ Refractive Errors: Signs, Symptoms & Diagnosis
🔹 I. Signs & Symptoms of Refractive Errors
✅ Common Symptoms (All Types):
- 🔸 Blurred vision (near, far, or both – depending on type)
- 🔸 Eye strain or discomfort
- 🔸 Headache, especially after reading or screen use
- 🔸 Squinting or narrowing the eyes to see clearly
- 🔸 Difficulty seeing at night or in low light
- 🔸 Frequent rubbing of eyes
- 🔸 Double vision (in some cases of astigmatism)
- 🔸 Dryness or watery eyes
- 🔸 Difficulty reading or focusing on small objects
🔹 Type-Specific Symptoms:
| 🧠 Type of Refractive Error | 🔎 Signs & Symptoms |
|---|---|
| Myopia (Nearsightedness) | 👀 Clear near vision, 👓 Blurred distance vision, ❌ Trouble seeing road signs, 🎯 Eye strain during outdoor activities |
| Hyperopia (Farsightedness) | 📚 Blurred near vision, 🧠 Headaches after close work, 😵 Fatigue while reading, 👀 Squinting |
| Astigmatism | 🔁 Blurred/distorted vision at all distances, 📏 Difficulty with fine detail, 💢 Eye discomfort, 😵 Headaches |
| Presbyopia | 👓 Difficulty reading small print, 📖 Holding objects farther away to see, 📚 Eye fatigue, 🧓 Appears after age 40 |
🧪 II. Diagnostic Methods for Refractive Errors
🔬 1. Visual Acuity Test (Snellen Chart)
- 🔹 Measures clarity of vision at 20 feet
- 📊 Result like 20/20 (normal), 20/60 (vision is blurry at 20 ft what normal sees at 60 ft)
🧪 2. Retinoscopy
- A light is shined into the eye, and the reflection from the retina is analyzed with lenses
- Helps estimate the degree and type of refractive error
🧪 3. Refraction Test (Subjective Refraction)
- Patient looks through a phoropter or lens device and reports which lens gives clearer vision
- Used to determine exact lens power for glasses or contact lenses
🧪 4. Autorefractor Testing
- A computerized instrument automatically calculates refractive error by analyzing how light changes as it enters the eye
- Quick and useful for children or uncooperative patients
🧪 5. Keratometry
- Measures the curvature of the cornea
- Essential in diagnosing astigmatism
🧪 6. Cycloplegic Refraction (in children)
- Eye drops are used to paralyze accommodation temporarily, allowing more accurate measurement of refractive error, especially in children or suspected hyperopia
✅ Summary Table: Signs, Symptoms, and Diagnosis
| 🔍 Type | ⚠️ Key Symptoms | 🔬 Diagnostic Tests |
|---|---|---|
| Myopia | Blurred distant vision, eye strain | Snellen chart, Retinoscopy, Autorefractor |
| Hyperopia | Blurred near vision, headaches | Snellen chart, Cycloplegic refraction |
| Astigmatism | Blurred/distorted vision at all distances | Keratometry, Retinoscopy, Refraction test |
| Presbyopia | Difficulty reading near, holding books at a distance | Refraction test, Near vision chart |
👁️🗨️ Refractive Errors – Medical and Surgical Management
🧴 I. Medical Management of Refractive Errors
Medical (non-surgical) treatment focuses on correcting the focus of light rays onto the retina using external aids or supportive measures.
🔹 1. Corrective Lenses:
👓 Eyeglasses:
- Most common and safest method
- Prescribed based on type and degree of refractive error
- Special lenses:
- Concave lenses for Myopia
- Convex lenses for Hyperopia
- Cylindrical lenses for Astigmatism
- Bifocal/Progressive lenses for Presbyopia
🟠 Benefits:
- Non-invasive
- Easily adjustable
- Affordable
🔹 2. Contact Lenses:
- Placed directly on the cornea
- Available as soft, rigid gas permeable, or toric lenses
- Types:
- Spherical lenses – for myopia/hyperopia
- Toric lenses – for astigmatism
- Multifocal lenses – for presbyopia
🟠 Benefits:
- Wider field of vision
- Better for sports and aesthetics
⚠️ Considerations:
- Require strict hygiene
- Risk of infection, dryness
🔹 3. Orthokeratology (Ortho-K):
- Special rigid contact lenses worn overnight
- Temporarily reshape the cornea to improve daytime vision
- Mostly used in mild to moderate myopia
🔹 4. Low Vision Aids (in extreme cases):
- For patients with high uncorrectable refractive errors
- Includes magnifiers, reading telescopes, or electronic devices
🔧 II. Surgical Management of Refractive Errors
Surgical treatment is recommended for permanent correction, especially when patients want to avoid lifelong glasses/contact use.
🔸 1. LASIK (Laser-Assisted In Situ Keratomileusis):
- Most common laser refractive surgery
- A flap is created on the cornea, then reshaped using excimer laser
- Corrects myopia, hyperopia, and astigmatism
✅ Benefits:
- Quick recovery
- Minimal pain
- Rapid vision improvement
🔸 2. PRK (Photorefractive Keratectomy):
- Surface layer of the cornea is removed and reshaped with laser
- Suitable for patients with thin corneas where LASIK is contraindicated
✅ Benefits:
- Similar results to LASIK
- No flap-related complications
🔸 3. LASEK (Laser Sub-Epithelial Keratomileusis):
- Combines features of LASIK and PRK
- The epithelial layer is preserved and repositioned after laser reshaping
🔸 4. SMILE (Small Incision Lenticule Extraction):
- Minimally invasive, flapless laser surgery
- Used mainly for myopia and astigmatism
🔸 5. Phakic Intraocular Lenses (IOLs):
- Implantation of a lens inside the eye, without removing the natural lens
- For patients with very high myopia or hyperopia not suitable for laser
🔸 6. Refractive Lens Exchange (RLE):
- Similar to cataract surgery
- Natural lens is removed and replaced with an artificial intraocular lens (IOL)
- Preferred in severe hyperopia or presbyopia, especially in older adults
🧑⚕️ Post-Surgical Care:
- Use of antibiotic and steroid eye drops
- Avoid rubbing eyes
- Regular follow-up with ophthalmologist
- Protective eyewear to prevent trauma or infection
- Monitor for complications: infection, glare, dry eyes, halo
📌 Summary Table: Management at a Glance
| 🔧 Type | 🧴 Medical Options | 🔪 Surgical Options |
|---|---|---|
| Myopia | Glasses, contact lenses, Ortho-K | LASIK, PRK, SMILE, Phakic IOL |
| Hyperopia | Convex lenses, contacts | LASIK, PRK, RLE |
| Astigmatism | Cylindrical lenses, toric contacts | LASIK, PRK, LASEK |
| Presbyopia | Reading glasses, multifocal lenses | RLE, Multifocal IOLs, Monovision LASIK |
🧑⚕️👁️ Nursing Management of Refractive Errors
🎯 Objectives of Nursing Management:
✔️ Assist in accurate assessment and identification of vision problems
✔️ Provide education and support regarding corrective options
✔️ Promote eye health and hygiene
✔️ Ensure safety and improve quality of life
✔️ Support patients through pre- and post-operative care (if surgical)
📋 I. Assessment Phase
🔍 Collect a detailed nursing history:
- Blurred vision, eye strain, headaches, squinting
- Onset, duration, and effect on daily life
- Use of glasses or contact lenses
- Compliance with treatment or follow-up visits
🔬 Perform/assist with basic eye assessments:
- Visual acuity test (Snellen chart)
- Observation for squinting, rubbing eyes, or misalignment
- Check pupil reactions, symmetry, and eyelid position
💊 II. Nursing Interventions
🔹 A. Non-Surgical Management (Eyeglasses or Contact Lenses)
✅ Provide Education:
- Importance of wearing prescribed lenses regularly
- Care and maintenance of contact lenses
- Avoid sharing lenses
- Clean spectacles and store lenses properly
✅ Monitor for complications:
- Redness, watering, itching → may indicate allergy or infection
- Signs of poor lens hygiene (especially in children or teens)
✅ Assist with referrals:
- Refer to optometrist/ophthalmologist if visual changes occur
🔹 B. Pre-Operative Nursing Care (for LASIK/PRK/Other Eye Surgeries)
✔️ Educate about the procedure, recovery time, and expectations
✔️ Instruct to stop contact lens use before surgery (as advised)
✔️ Ensure pre-op eye drops are administered correctly
✔️ Provide emotional support, especially in anxious patients
✔️ Confirm informed consent is obtained
🔹 C. Post-Operative Nursing Care
✅ Monitor for complications:
- Infection: redness, discharge, pain
- Vision disturbances: glare, halos, or worsening vision
- Dryness, burning, foreign body sensation
✅ Administer eye drops as prescribed:
- Antibiotic (e.g., moxifloxacin)
- Steroid (e.g., prednisolone)
- Lubricating drops for dry eyes
✅ Educate on post-op precautions:
- Do not rub eyes
- Avoid water/soap entering eyes
- Use eye shield while sleeping
- Avoid makeup, dust exposure for a few weeks
- Limit screen time initially
✅ Schedule and encourage follow-up visits to track healing
📘 III. Health Education & Lifestyle Advice
| 🧠 Topic | 📌 Key Advice |
|---|---|
| Regular Eye Check-ups | Especially for children, elderly, or patients with diabetes |
| Eye Hygiene | Hand hygiene before touching eyes or lenses |
| Proper Lighting | Avoid eye strain by reading in well-lit areas |
| Screen Time | Follow 20-20-20 rule (every 20 min, look 20 ft away for 20 seconds) |
| Nutrition | Encourage intake of Vitamin A, lutein, and omega-3s |
| Protective Eyewear | Use sunglasses or safety glasses as needed |
🧑⚕️ IV. Nursing Diagnosis (Examples):
🩺 1. Disturbed Sensory Perception (Visual)
🩺 2. Knowledge Deficit related to eye care and lens use
🩺 3. Risk for Injury related to poor visual acuity
🩺 4. Anxiety related to impaired vision or surgery
🩺 5. Non-compliance with vision correction regimen
✅ Conclusion / Key Points:
🔹 Nursing care plays a vital role in early detection, patient education, and rehabilitation
🔹 Proper post-op care and instructions are essential for successful outcomes in surgical correction
🔹 Nurses must promote compliance, hygiene, and lifestyle modifications to support long-term vision health.
👁️🗨️ Refractive Errors – Nutritional Consideration, Complications, and Key Points
🥦 I. Nutritional Considerations in Refractive Errors
While refractive errors are mostly structural or functional, good nutrition supports overall eye health, prevents associated problems, and may slow progression in some cases.
✅ Important Nutrients for Eye Health:
| 🧪 Nutrient | 💡 Role in Vision | 🥗 Sources |
|---|---|---|
| Vitamin A | Maintains corneal clarity, essential for night vision | Carrots, spinach, sweet potatoes, liver |
| Vitamin C | Antioxidant, protects against lens degeneration | Citrus fruits, bell peppers, broccoli |
| Vitamin E | Protects eye cells from free radical damage | Almonds, sunflower seeds, avocado |
| Lutein & Zeaxanthin | Found in retina, filters harmful light rays | Kale, spinach, corn, eggs |
| Zinc | Helps Vitamin A function in the retina | Pumpkin seeds, meat, legumes |
| Omega-3 fatty acids | Supports tear production, reduces dry eye | Flaxseed, fish (salmon, mackerel), walnuts |
🧑⚕️ Dietary Advice for Refractive Error Patients:
- Include colorful vegetables & fruits (leafy greens, carrots)
- Encourage hydration for healthy tear production
- Avoid junk foods, excess sugar, and processed fats
- Encourage frequent small meals rich in nutrients for screen-exposed individuals
⚠️ II. Complications of Refractive Errors
If left uncorrected or poorly managed, refractive errors can lead to various functional and health complications:
🔹 1. Eye Strain (Asthenopia):
- Constant squinting or focusing → fatigue, headaches, discomfort
🔹 2. Chronic Headaches:
- From prolonged visual effort or incorrect lenses
🔹 3. Amblyopia (Lazy Eye):
- Common in children with untreated refractive errors
- One eye becomes weaker due to suppressed visual input
🔹 4. Strabismus (Squint):
- May develop in children with uncorrected hyperopia
🔹 5. Social and Educational Impact:
- In children: affects reading, concentration, learning
- In adults: driving, safety hazards, reduced productivity
🔹 6. Contact Lens-related Infections:
- Improper hygiene may lead to keratitis, conjunctivitis, or corneal ulcers
🔹 7. Post-Surgical Complications (if LASIK or PRK):
- Dry eyes
- Light sensitivity
- Glare/halos at night
- Rarely: under-correction or over-correction
📌 III. Key Points (Summary for Quick Revision)
✅ Refractive errors are optical defects due to improper focusing of light on the retina.
✅ Major types include:
- Myopia (near objects clear, far blurry)
- Hyperopia (far objects clear, near blurry)
- Astigmatism (blurred/distorted vision at all distances)
- Presbyopia (age-related near vision loss)
✅ Managed primarily through:
- Eyeglasses or contact lenses
- Laser surgeries (e.g., LASIK, PRK)
- Lens replacement (RLE) for severe or aging-related errors
✅ Nurses play a key role in:
- Assessment, education, and post-surgical care
✅ Nutrition (Vitamin A, C, E, lutein, omega-3) is supportive, especially for overall eye health
✅ Early correction prevents amblyopia, strabismus, and academic or occupational limitations
✅ Regular eye check-ups are essential, especially for:
- 👶 Children (every 6–12 months)
- 👵 Adults over 40 (presbyopia, cataract screening)
👁️🗨️ Eyelid Infection.
📘 Definition:
Eyelid infections refer to inflammatory or infectious conditions affecting the eyelid margins, skin, or glands. These infections can be bacterial, viral, fungal, or parasitic, and often result in redness, swelling, pain, and sometimes discharge or crusting.
🦠 It may involve:
- The outer eyelid skin
- The eyelash follicles
- The oil (meibomian) glands
- The tear-producing structures
⚠️ Causes of Eyelid Infections:
| 🔹 Cause Type | 🧬 Specific Causes |
|---|---|
| Bacterial | Staphylococcus aureus, Streptococcus species – most common |
| Viral | Herpes simplex virus (HSV), Varicella-zoster virus (VZV) |
| Fungal | Rare, but can include Candida or Aspergillus in immunocompromised |
| Parasitic | Demodex mites on eyelash follicles |
| Non-infectious triggers | Poor hygiene, eye makeup contamination, blepharitis, contact lens use |
🔁 Often associated with:
- Touching eyes with unclean hands
- Cosmetic contamination
- Allergies or chronic inflammation
- Coexisting conditions (diabetes, skin conditions)
🔍 Types of Eyelid Infections:
🔸 1. Blepharitis
📘 Definition: Chronic inflammation of the eyelid margins, often caused by bacteria, dandruff-like skin flakes, or oil gland dysfunction.
🔹 Symptoms:
- Red, itchy eyelids
- Crusting or dandruff-like debris
- Burning sensation
- Gritty or foreign body feeling
🔹 Types:
- Anterior blepharitis – affects base of eyelashes
- Posterior blepharitis – affects meibomian glands (oil glands)
🔸 2. Hordeolum (Stye)
📘 Definition: Acute, painful, bacterial infection (usually Staphylococcus aureus) of an oil gland or eyelash follicle.
🔹 Symptoms:
- Painful red bump
- Localized swelling
- Tenderness
- Pus formation (may drain spontaneously)
🔹 Types:
- External stye – on outer lid margin (Zeis/Moll gland)
- Internal stye – deeper, affects meibomian glands
🔸 3. Chalazion
📘 Definition: A sterile (non-infectious) inflammation of a blocked meibomian gland leading to a painless lump in the eyelid.
🔹 Symptoms:
- Firm, painless nodule
- May cause heaviness or pressure
- Can lead to secondary infection if untreated
🔹 🔁 Can follow untreated or recurrent stye
🔸 4. Herpes Zoster Ophthalmicus
📘 Definition: Reactivation of varicella-zoster virus (shingles) affecting the ophthalmic branch of the trigeminal nerve.
🔹 Symptoms:
- Painful vesicular rash on eyelids
- Swelling, burning, tingling
- Risk of corneal damage and vision loss
🔸 5. Herpes Simplex Blepharitis
📘 Definition: Eyelid infection caused by Herpes Simplex Virus (HSV).
🔹 Symptoms:
- Clear fluid-filled vesicles on eyelid
- Pain, redness, crusting
- May recur with stress or illness
🔬 I. Pathophysiology of Eyelid Infections
Eyelid infections typically begin when microorganisms (mostly bacteria) enter through:
✅ Hair follicles of eyelashes
✅ Meibomian (oil) glands
✅ Small skin breaks, cuts, or blocked ducts
🔁 Sequence of Events:
- Invasion by pathogen (commonly Staphylococcus aureus)
- Inflammatory response triggered at infection site
- Accumulation of pus, fluid, and immune cells leads to redness, swelling, and pain
- In some cases (e.g., chalazion), blockage without active infection causes cyst formation
🧠 Specific Examples:
- Stye (Hordeolum): Acute infection → suppuration (pus) in a gland → painful red lump
- Blepharitis: Chronic inflammation from oil gland dysfunction or microbial colonization → flaking and redness of eyelids
- Chalazion: Chronic lipogranulomatous inflammation due to blocked meibomian gland, not infectious
- Herpetic eyelid infection: Viral invasion (HSV/VZV) → damage to skin cells → vesicle formation and pain
⚠️ II. Signs & Symptoms of Eyelid Infections
| 🧪 Type | ⚠️ Key Signs & Symptoms |
|---|---|
| Blepharitis | Red, itchy eyelids, crusting at eyelash base, burning, gritty sensation, tearing |
| Hordeolum (Stye) | Painful, red swollen lump near eyelash, pus point, tenderness, localized warmth |
| Chalazion | Firm, painless nodule on eyelid (can become painful if secondarily infected), heaviness |
| Herpes Simplex Blepharitis | Vesicles on eyelid, tingling, redness, crusting, recurrent outbreaks |
| Herpes Zoster Ophthalmicus | Painful rash with fluid-filled blisters, tingling, swelling, often unilateral, fever, eye pain |
🔸 General Symptoms (all types) may include:
- Eyelid swelling
- Redness
- Discomfort or pain
- Tearing
- Sensitivity to light
- Visual disturbance (if lesion obstructs vision or involves cornea)
🧪 III. Diagnosis of Eyelid Infections
🔹 1. Clinical Examination:
- Inspection of eyelid margin, lashes, and eye using visual observation
- Palpation of eyelid for tenderness, nodules
- Fluorescein staining if corneal involvement suspected
🔹 2. History Taking:
- Onset, duration, recurrence
- Presence of pain, discharge, crusts
- Any previous eye surgeries or trauma
- Contact lens use or eye makeup habits
- Systemic history (e.g., diabetes, immune suppression)
🔹 3. Swab Culture and Sensitivity (if severe or recurrent):
- From eyelid margin or discharge
- Identifies the infectious organism (bacterial, viral, fungal)
- Helps guide antibiotic therapy
🔹 4. Slit Lamp Examination:
- Magnified view of eyelid, meibomian glands, and conjunctiva
- Detects extent of inflammation, gland blockage, or damage
🔹 5. Viral Tests:
- Tzanck smear or PCR testing in suspected herpes
- Confirms HSV or VZV infection
🔹 6. Biopsy (rare):
- In persistent, non-healing chalazion or suspicious lesions → to rule out malignancy
✅ Summary Table
| 🔍 Feature | ✏️ Blepharitis | ✏️ Hordeolum | ✏️ Chalazion | ✏️ HSV | ✏️ HZV |
|---|---|---|---|---|---|
| Onset | Chronic | Acute | Gradual | Recurrent | Acute |
| Pain | Mild | Yes | No (unless infected) | Burning | Severe |
| Swelling | Mild/moderate | Localized | Firm lump | Mild | Extensive |
| Discharge | Crusting | Possible pus | No | Clear fluid | Vesicles |
| Cause | Bacteria/skin | Bacteria | Blocked gland | HSV | Varicella-zoster |
| Diagnosis | Clinical, slit lamp | Clinical | Clinical | Tzanck smear | PCR, clinical |
💊 I. Medical Management
Management depends on the type of eyelid infection, severity, and recurrence. Most are managed medically unless complications arise.
🔸 1. Blepharitis (Chronic Inflammation of Lid Margins)
🔹 Treatment:
- Warm compresses 2–4 times/day to soften crusts and improve gland function
- Lid hygiene: Cleaning eyelid margins with diluted baby shampoo or commercial lid scrubs
- Topical antibiotics:
- Erythromycin or Bacitracin ointment
- Used along lash line at night
- Artificial tears: For dry eyes or irritation
- Oral antibiotics (for severe or meibomian gland dysfunction):
- Doxycycline, Tetracycline (for 2–6 weeks)
🔸 2. Hordeolum (Stye – Acute Bacterial Infection)
🔹 Treatment:
- Warm compresses (10–15 min, 3–4 times/day) to promote drainage
- Topical antibiotics:
- Moxifloxacin, Ciprofloxacin, or Erythromycin eye ointment
- Systemic antibiotics (if cellulitis or recurrent):
- Amoxicillin-clavulanate or Cephalexin
- Pain relief: NSAIDs like ibuprofen or paracetamol
🔸 3. Chalazion (Sterile Meibomian Cyst)
🔹 Treatment:
- Warm compresses + gentle massage
- No antibiotics usually unless infected secondarily
- Steroid injection (Triamcinolone) – for non-resolving or inflamed lesions
🔸 4. Herpes Simplex Blepharitis
🔹 Treatment:
- Topical antiviral: Acyclovir ointment
- Oral antiviral (for extensive disease):
- Acyclovir or Valacyclovir
- Avoid steroid drops unless prescribed under ophthalmic supervision
🔸 5. Herpes Zoster Ophthalmicus (Shingles of the Eye)
🔹 Treatment:
- Oral antivirals:
- Acyclovir 800 mg 5×/day
- Or Valacyclovir 1000 mg TID for 7–10 days
- Pain control: NSAIDs or neuropathic pain meds (e.g., Gabapentin)
- Antibiotic eye drops if secondary infection suspected
- Lubricating drops to prevent corneal dryness
🔪 II. Surgical Management
Surgical intervention is required when:
🔹 Medical treatment fails
🔹 The lesion is large, persistent, or cosmetically concerning
🔹 Abscess formation occurs
🔸 1. Incision and Drainage (I&D)
✅ Indication:
- Painful hordeolum that doesn’t resolve in 1–2 weeks
- Chalazion >1 month not responding to conservative therapy
✅ Procedure:
- Local anesthesia
- Small incision on inner eyelid
- Drainage of pus or cyst contents
- Apply topical antibiotics post-procedure
🔸 2. Chalazion Excision
✅ Indication:
- Large, persistent, or recurrent chalazion
- Cosmetic or vision interference
✅ Procedure:
- Performed under local anesthesia
- Curettage of the meibomian gland
- Pressure patch applied for 24 hours post-op
🔸 3. Biopsy (Excisional or Incisional)
✅ Indication:
- Recurrent chalazion in elderly (rule out sebaceous gland carcinoma)
- Suspicious or non-healing lesions
🧠 Post-Surgical Care:
- Apply antibiotic ointment (e.g., erythromycin)
- Use cold compresses for swelling
- Educate on hand hygiene and eye protection
- Schedule follow-up visits
- Avoid eye makeup or contact lenses temporarily
✅ Summary Table
| Condition | Medical Management | Surgical Management |
|---|---|---|
| Blepharitis | Lid hygiene, antibiotics, warm compresses | Rarely needed |
| Hordeolum | Warm compress, topical/systemic antibiotics | I&D if not resolved |
| Chalazion | Warm compress, steroid injection | Excision if persistent |
| Herpes Simplex | Antiviral ointment/tablets | Not usually required |
| Herpes Zoster | Systemic antivirals, pain control | Only for complications or biopsy |
👩⚕️👁️ Nursing Management of Eyelid Infections
🎯 Objectives of Nursing Management:
✔️ Alleviate discomfort and inflammation
✔️ Promote healing and prevent recurrence
✔️ Educate patient on proper eyelid hygiene
✔️ Monitor for complications and provide supportive care
✔️ Encourage compliance with medical/surgical treatments
📋 I. Assessment
🔍 Subjective Data:
- Patient’s complaints of pain, itching, swelling, blurry vision
- History of similar episodes or recurrent infections
- Contact lens use or eye makeup habits
- Allergies or systemic diseases (e.g., diabetes, skin disorders)
🔬 Objective Data:
- Inspect for:
- Redness, swelling, crusting, vesicles on eyelids
- Tender nodules or pus formation
- Tearing or discharge
- Visual changes or eye movement discomfort
💊 II. Nursing Interventions
🔸 1. Relieve Symptoms & Promote Healing
- Apply warm compresses (10–15 minutes, 3–4 times/day) to reduce inflammation and promote drainage
- Instruct patient not to squeeze or touch the lesion
- Gently clean eyelid margins using sterile cotton swab with diluted baby shampoo or prescribed lid wipes
🔸 2. Administer Medications as Prescribed
- Apply antibiotic ointments or drops to affected area (e.g., erythromycin, ciprofloxacin)
- Monitor for allergic reactions or side effects (burning, redness)
- Administer oral antibiotics or antivirals if prescribed (e.g., doxycycline, acyclovir)
- Ensure compliance with analgesics or anti-inflammatory medications for pain relief
🔸 3. Post-Operative Care (If Surgical Drainage or Excision Done)
- Monitor surgical site for:
- Redness, warmth, purulent discharge, or bleeding
- Apply cold compress first 24 hours, followed by warm compress after 48 hours if advised
- Teach patient to:
- Avoid eye makeup and contact lenses until fully healed
- Use prescribed topical medications correctly
- Report any vision changes or signs of infection
🧠 III. Patient Education
| 📘 Topic | 🧾 Teaching Instructions |
|---|---|
| Lid Hygiene | Wash hands before touching eyes; clean lids daily if chronic blepharitis present |
| Warm Compress | Instruct on proper temperature, frequency, and gentle massage technique |
| Medication Use | Apply eye drops or ointments without contaminating tip; complete full course of treatment |
| Avoidance | Discourage eye rubbing, sharing towels or cosmetics |
| Contact Lenses | Avoid during active infection; clean thoroughly before reuse |
| Makeup | Avoid during infection; discard old/contaminated products |
| Follow-up | Emphasize importance of review appointments to monitor recovery or prevent recurrence |
📌 IV. Nursing Diagnoses (Examples):
- Acute Pain related to inflammation or swelling of eyelid
- Risk for Infection (Spread) related to bacterial invasion
- Disturbed Sensory Perception (Visual) due to swelling or discharge
- Deficient Knowledge related to hygiene, medication use, or recurrence prevention
- Risk for Injury related to impaired vision or photophobia
✅ V. Evaluation Criteria:
- Patient reports relief of pain and discomfort
- Swelling, redness, and discharge have reduced or resolved
- Patient demonstrates correct application of medications and compresses
- Verbalizes understanding of hygiene and recurrence prevention
- No complications or spread of infection observed
🥗 I. Nutritional Considerations
While eyelid infections are typically infectious or inflammatory, nutrition plays a supportive role in promoting healing, boosting immunity, and reducing recurrence.
✅ Nutrients Essential for Eye and Skin Health:
| 🧪 Nutrient | 🔍 Role | 🥗 Sources |
|---|---|---|
| Vitamin A | Supports skin and mucous membrane integrity; boosts immune response | Carrots, spinach, pumpkin, liver |
| Vitamin C | Antioxidant, aids in wound healing and immunity | Citrus fruits, guava, bell peppers |
| Vitamin E | Protects cells from oxidative stress | Almonds, sunflower seeds, green leafy vegetables |
| Zinc | Essential for immune function and tissue healing | Pumpkin seeds, beans, meat |
| Omega-3 fatty acids | Reduce inflammation and support meibomian gland health | Fish, flaxseeds, walnuts |
| Probiotics | Improve immunity and reduce recurrent infections | Yogurt, kefir, fermented foods |
🧑⚕️ Dietary Advice for Patients:
- Stay well hydrated (💧 water helps flush toxins and maintain tear production)
- Avoid junk foods, deep-fried or overly processed meals
- Eat colorful fruits and vegetables for antioxidant support
- Maintain a balanced diet rich in whole grains, lean proteins, and healthy fats
- Consider vitamin supplements in case of dietary deficiencies (especially in elderly or immunocompromised)
⚠️ II. Complications of Eyelid Infections
Untreated or recurrent eyelid infections may lead to:
🔹 1. Preseptal or Orbital Cellulitis
- Infection spreading to deeper tissues around the eye
- Requires urgent systemic antibiotics or hospitalization
🔹 2. Chronic Blepharitis
- Long-standing inflammation with frequent flare-ups
- May lead to eyelash loss, scarring, or thickened lid margins
🔹 3. Corneal Involvement
- Especially in viral infections like HSV or HZV
- Can lead to keratitis, corneal ulcer, and vision loss
🔹 4. Chalazion Recurrence
- Recurrent meibomian gland blockage
- May require surgical excision or biopsy to rule out malignancy (e.g., sebaceous gland carcinoma)
🔹 5. Cosmetic Deformity or Eyelid Droop (Ptosis)
- From chronic swelling, scarring, or post-surgical outcomes
📌 III. Key Points (Quick Recap for Exams & Practice)
✔️ Eyelid infections are commonly caused by bacterial (Staphylococcus), viral (HSV, HZV), or blockage/inflammation of glands
✔️ Most common types include:
- Blepharitis – chronic lid margin inflammation
- Hordeolum (stye) – acute painful infection of lash follicle or gland
- Chalazion – non-infectious, blocked meibomian gland
- Herpetic infections – viral origin causing blisters or crusting
✔️ Warm compresses and lid hygiene are the cornerstones of nursing care
✔️ Topical and oral antibiotics/antivirals are used based on the type of infection
✔️ Surgery (I&D or excision) is indicated if lesions do not resolve or recur
✔️ Good nutrition supports recovery and boosts immune function
✔️ Nursing role includes assessment, medication administration, post-op care, patient education, and hygiene reinforcement
✔️ Follow-up and prevention are essential to avoid complications like cellulitis, corneal ulcers, or chronic eyelid disease
👁️🗨️ Eyelid Deformities
📘 Definition:
Eyelid deformities are congenital or acquired structural abnormalities of the eyelid that alter its position, shape, or function, affecting protection, lubrication, and visual function of the eye.
They can be cosmetic or vision-threatening, depending on severity.
🔍 Causes of Eyelid Deformities:
| 🔸 Cause Type | 🔍 Examples |
|---|---|
| Congenital (present at birth) | Coloboma, congenital ptosis, epiblepharon |
| Acquired (due to injury or disease) | Trauma, burns, tumors, nerve palsy, infection |
| Age-related | Weakening of muscles or connective tissue (e.g., involutional ptosis, ectropion) |
| Paralysis or Neuromuscular Disorders | Bell’s palsy, myasthenia gravis |
| Scarring or Fibrosis | Due to surgery, trauma, Stevens-Johnson syndrome |
🔢 Types of Eyelid Deformities:
🔹 1. Ptosis
➡️ Drooping of the upper eyelid due to levator muscle dysfunction
🔹 2. Entropion
➡️ Inward turning of the eyelid margin, causing lashes to rub against the eyeball
🔹 3. Ectropion
➡️ Outward turning of the eyelid margin, exposing inner conjunctiva
🔹 4. Coloboma
➡️ Congenital or acquired notch/defect in the eyelid structure
🔹 5. Epicanthus
➡️ Fold of skin covering the inner corner of the eye (often normal in infants)
🔹 6. Lagophthalmos
➡️ Incomplete closure of eyelids during blinking or sleep
🔹 7. Dermatochalasis
➡️ Excess skin on upper eyelids due to aging or loss of elasticity
🔹 8. Blepharophimosis Syndrome
➡️ Rare congenital condition with narrow eye openings and severe ptosis
🔬 Pathophysiology (General Overview):
Eyelid deformities arise from defects in muscles, nerves, tendons, connective tissue, or skin of the eyelid:
🔹 Ptosis: Dysfunction of the levator palpebrae superioris or Müller’s muscle, or innervating nerves (cranial nerve III or sympathetic fibers)
🔹 Entropion: Caused by overaction of orbicularis oculi muscle, scar contraction, or loose lower lid retractors
🔹 Ectropion: Results from horizontal lid laxity, scarring, or orbicularis muscle weakness, leading to eversion
🔹 Lagophthalmos: Caused by facial nerve palsy or eyelid scarring, preventing full closure of eyelids
⚠️ Signs & Symptoms (Depending on Type):
| 👁️ Deformity | ⚠️ Symptoms |
|---|---|
| Ptosis | Drooping lid, blocked vision, raised eyebrows to compensate |
| Entropion | Eye redness, irritation, tearing, corneal abrasion from lashes |
| Ectropion | Dryness, excessive tearing, visible inner lid, conjunctivitis |
| Coloboma | Notch in eyelid, exposure of eye, dryness, risk of ulceration |
| Lagophthalmos | Eye exposure, dryness, corneal damage during sleep |
| Dermatochalasis | Visual field obstruction, tired appearance |
| Blepharophimosis | Small palpebral fissures, severe ptosis, lazy eye (amblyopia) |
🧪 Diagnosis:
🔍 Clinical Evaluation:
- Inspection of eyelid position, closure, movement
- Measurement of:
- MRD1 (Margin Reflex Distance 1)
- Palpebral fissure height
- Levator function
🔬 Slit-lamp Examination:
- Check corneal integrity and signs of irritation, ulcers
📸 Imaging (if needed):
- CT/MRI if underlying tumor, trauma, or nerve involvement is suspected
👁️ Vision Testing:
- Visual acuity and field tests (especially in ptosis/dermatochalasis)
💊 Medical Management:
✅ Used for mild cases, early stages, or patients unfit for surgery:
| 🧴 Treatment | 🎯 Indication |
|---|---|
| Lubricating eye drops/gel | Lagophthalmos, ectropion, exposure keratopathy |
| Antibiotic ointment | In case of corneal exposure or infection risk |
| Taping the eye closed during sleep | Lagophthalmos, Bell’s palsy |
| Botulinum toxin injections | Temporary correction of entropion or spastic ptosis |
| Patching/occlusion therapy | In children with ptosis to prevent amblyopia |
🔪 Surgical Management:
✂️ 1. Ptosis Surgery:
- Levator resection – strengthens levator muscle
- Frontalis sling – suspends lid to forehead muscle (used in poor levator function)
✂️ 2. Entropion Surgery:
- Everting sutures
- Lid retractors reattachment or lower lid rotation procedures
✂️ 3. Ectropion Surgery:
- Lateral tarsal strip procedure
- Medial canthoplasty
- Skin graft in cicatricial (scar-related) ectropion
✂️ 4. Coloboma Repair:
- Full-thickness eyelid reconstruction using local flaps or grafts
✂️ 5. Lagophthalmos:
- Gold weight implant in upper eyelid
- Tarsorrhaphy – partial closure of eyelids surgically
✂️ 6. Dermatochalasis:
- Blepharoplasty – surgical removal of excess skin for cosmetic or visual reasons
📌 Summary of Key Points:
✔️ Eyelid deformities affect eyelid function, appearance, and ocular health
✔️ May be congenital, acquired, or age-related
✔️ Symptoms vary by type – from irritation to vision obstruction
✔️ Diagnosis involves eyelid measurements, visual exam, and slit-lamp
✔️ Management includes:
- Medical: Lubricants, antibiotics, eye protection
- Surgical: Ptosis correction, entropion/ectropion repair, blepharoplasty
✔️ Early treatment is crucial to prevent corneal damage or vision loss
👩⚕️👁️ Nursing Management of Eyelid Deformities
🎯 Objectives of Nursing Management:
✅ Maintain eye protection and moisture
✅ Prevent complications like corneal injury and infection
✅ Assist in pre- and post-operative care
✅ Educate patients and caregivers about hygiene, eye care, and follow-up
✅ Promote emotional and psychological support for visible deformities
📋 I. Assessment Phase
🔍 History Collection:
- Onset and duration of eyelid droop, eversion/inversion, or incomplete closure
- Visual disturbances (e.g., blurred vision, glare, eye strain)
- Previous eye surgeries, trauma, or family history
- Symptoms of dryness, irritation, tearing, or photophobia
🔬 Physical Observation:
- Eyelid position and movement
- Corneal exposure or signs of keratitis
- Eye discharge or signs of infection
- Use of compensatory mechanisms (e.g., tilting head back in ptosis)
💊 II. Nursing Interventions
🔹 1. Eye Protection & Comfort Measures
- Apply lubricating eye drops or ointments to prevent dryness (especially in lagophthalmos and ectropion)
- Use cool compresses for irritation or inflammation
- For incomplete closure (e.g., facial palsy):
- Gently tape eyelids shut during sleep
- Use moisture chambers or eye shields
- Encourage blinking exercises
🔹 2. Skin & Eyelid Hygiene
- Cleanse eyelids daily with sterile cotton and warm saline or prescribed eyelid scrub
- Maintain lash hygiene to prevent infection or blepharitis
- Prevent rubbing or touching of eyes with unclean hands
🔹 3. Pre-Operative Nursing Care
- Prepare the patient physically and psychologically for surgery
- Educate about the procedure, expected outcomes, and recovery period
- Obtain informed consent
- Ensure pre-op lab investigations and ophthalmic measurements are completed
- Administer prescribed pre-op antibiotics or lubricants
🔹 4. Post-Operative Nursing Care
- Monitor for signs of bleeding, infection, swelling, or discharge
- Apply cold compresses in the first 24 hours to reduce swelling
- Administer prescribed antibiotic and anti-inflammatory eye drops
- Instruct on:
- Avoiding eye rubbing
- Avoiding makeup or contact lenses
- Elevating the head during sleep to reduce edema
- Reinforce importance of follow-up visits for suture removal or monitoring recovery
🧠 III. Patient Education
| 📘 Topic | 🧾 Instructions |
|---|---|
| Hygiene | Clean eyelids gently, avoid harsh rubbing |
| Eye protection | Wear sunglasses outdoors to reduce dryness and exposure |
| Medication | Use prescribed eye drops/ointments correctly without contaminating the tip |
| Infection prevention | Hand hygiene, avoid sharing towels or makeup |
| Diet | Encourage vitamin A and omega-3 rich foods to support healing |
| Psychosocial support | Address body image concerns or emotional impact of deformities |
🧾 IV. Sample Nursing Diagnoses
- Risk for injury related to impaired eyelid function or exposure keratopathy
- Disturbed body image related to visible eyelid deformity
- Deficient knowledge regarding treatment plan and eyelid care
- Impaired comfort related to eye irritation or dryness
- Risk for infection related to altered protective mechanisms of the eyelid
✅ V. Evaluation Criteria
- Patient reports improved comfort and symptom relief
- No signs of infection, ulceration, or corneal dryness
- Patient correctly demonstrates hygiene and medication techniques
- Post-surgical wounds healing without complications
- Patient verbalizes understanding of condition, management, and follow-up needs
🥗 I. Nutritional Considerations
While eyelid deformities are primarily structural or functional, nutrition plays a supportive role in promoting eye surface health, wound healing, and prevention of infection or inflammation, especially post-surgery or in patients with exposure keratopathy.
✅ Essential Nutrients for Eyelid & Ocular Health:
| 🧪 Nutrient | 📌 Function | 🥗 Sources |
|---|---|---|
| Vitamin A | Maintains healthy skin, prevents dryness & supports mucosal immunity | Carrots, spinach, sweet potatoes, liver |
| Vitamin C | Enhances tissue repair and immune defense | Citrus fruits, guava, bell peppers |
| Vitamin E | Antioxidant; protects against oxidative damage in healing tissues | Almonds, sunflower seeds, avocado |
| Zinc | Aids in wound healing and epithelial regeneration | Pumpkin seeds, legumes, lean meats |
| Omega-3 Fatty Acids | Reduces inflammation; supports tear production | Fish (salmon, sardines), flaxseeds, walnuts |
| Protein | Essential for tissue repair and immune defense | Eggs, lean meat, dairy, legumes |
🧑⚕️ Dietary Advice:
- Encourage hydration to maintain tear film and tissue moisture
- Consume anti-inflammatory foods (turmeric, ginger, green leafy vegetables)
- Avoid processed, fried, or sugary foods that may impair healing
- Promote frequent small, balanced meals during post-operative recovery
⚠️ II. Complications of Eyelid Deformities
Untreated or improperly managed eyelid deformities can lead to serious ocular and systemic complications:
🔹 1. Exposure Keratitis
- Due to incomplete eyelid closure (e.g., lagophthalmos, ectropion)
- Leads to dry cornea, ulceration, and infection
🔹 2. Corneal Abrasions or Ulcers
- Common in entropion, where eyelashes rub against the cornea
- Can lead to scarring or vision loss
🔹 3. Chronic Conjunctivitis
- Persistent irritation, redness, and discharge due to poor eyelid closure or malposition
🔹 4. Vision Impairment or Amblyopia
- Especially in congenital ptosis or blepharophimosis in children
- Visual development may be hindered if untreated early
🔹 5. Cosmetic Disfigurement
- Affects self-esteem and mental well-being
- May lead to social withdrawal or depression in some patients
🔹 6. Infection or Scarring
- Post-operative or secondary to trauma
- Improper wound care may lead to delayed healing or lid fibrosis
📌 III. Key Points (Quick Revision)
✅ Eyelid deformities are structural abnormalities that impair the normal function and appearance of the eyelids
✅ They can be congenital (e.g., ptosis, coloboma) or acquired (e.g., due to age, trauma, or disease)
✅ Common types include:
- Ptosis (drooping lid)
- Entropion (inward turning)
- Ectropion (outward turning)
- Lagophthalmos (incomplete closure)
✅ Nursing care focuses on:
- Preventing corneal exposure & infection
- Ensuring lubrication & protection of the eye
- Providing pre- and post-operative support
- Educating patients on hygiene and follow-up
✅ Nutritional support enhances healing, immune response, and reduces post-operative complications
✅ Early detection and treatment are essential to prevent vision-threatening complications
✅ Most eyelid deformities are correctable with surgery and proper rehabilitation.
👁️🗨️ Conjunctival Inflammation.
📘 Definition:
Conjunctival inflammation, medically known as conjunctivitis, is the inflammation of the conjunctiva — the thin, transparent membrane that covers the white part of the eye (sclera) and inner surface of the eyelids.
This condition leads to redness, swelling, irritation, discharge, and sometimes watering or crusting, commonly known as “pink eye.”
🔍 Causes of Conjunctival Inflammation:
Conjunctivitis can result from infectious or non-infectious causes:
🔹 1. Infectious Causes:
| 🔸 Agent Type | 🔍 Examples |
|---|---|
| Bacterial | Staphylococcus aureus, Streptococcus pneumoniae, Haemophilus influenzae, Chlamydia trachomatis |
| Viral | Adenovirus (most common), Herpes simplex virus, Varicella-zoster virus |
| Fungal (rare) | Candida, Aspergillus, Fusarium (usually in immunocompromised or post-surgery) |
| Parasitic (rare) | Acanthamoeba (associated with contaminated contact lenses) |
🔹 2. Non-Infectious Causes:
| 🔸 Type | 🔍 Examples |
|---|---|
| Allergic | Pollen, dust mites, pet dander, cosmetics, eye drops |
| Chemical / Irritant | Smoke, chlorine, foreign body, pollutants, acid/alkali exposure |
| Autoimmune-related | Stevens-Johnson Syndrome, Ocular cicatricial pemphigoid |
| Mechanical trauma | Rubbing eyes, contact lens overuse, foreign body |
🔢 Types of Conjunctivitis:
🔸 1. Bacterial Conjunctivitis:
- Often unilateral at onset but may spread to both eyes
- Thick yellow or green discharge, lid crusting
- Redness, gritty feeling, mild discomfort
🔸 2. Viral Conjunctivitis:
- Commonly bilateral, starts in one eye
- Watery discharge, redness, and burning
- Often associated with cold, sore throat, or fever
- Highly contagious (e.g., adenoviral conjunctivitis)
🔸 3. Allergic Conjunctivitis:
- Itching is dominant symptom
- Watery discharge, swelling (chemosis), red eyes
- Usually bilateral
- Often seasonal (hay fever), or triggered by allergens
🔸 4. Chemical/Irritant Conjunctivitis:
- Caused by exposure to irritants (e.g., smoke, chlorine, acid/alkali)
- Immediate burning, tearing, redness, and pain
- Emergency care may be needed for corrosive chemicals
🔸 5. Neonatal Conjunctivitis (Ophthalmia Neonatorum):
- Occurs in newborns within 1st month of life
- Causes: Chlamydia, Neisseria gonorrhoeae, or herpes
- May cause severe eye damage if not treated promptly
🔬 I. Pathophysiology of Conjunctivitis
The conjunctiva is a thin, transparent mucous membrane that lines the inner surface of the eyelids and covers the sclera (white of the eye). In conjunctivitis, this membrane becomes inflamed due to infection, allergen, irritant, or immune-mediated causes.
🧠 Basic Mechanism:
- Trigger/Pathogen Exposure (e.g., bacteria, virus, allergen, chemical)
- ➡️ Irritation/Injury to conjunctival epithelium
- ➡️ Inflammatory response is initiated:
- Dilation of conjunctival blood vessels → Redness (hyperemia)
- Infiltration of immune cells (neutrophils, eosinophils, lymphocytes)
- Increased capillary permeability → Tearing, swelling (chemosis)
- Glandular stimulation → Mucous or purulent discharge
- ➡️ In allergic conjunctivitis, histamine release from mast cells causes intense itching and swelling
🦠 Pathogen-specific Notes:
- Bacteria → Neutrophilic response → thick, purulent discharge
- Viruses → Lymphocytic response → watery discharge, follicular reaction
- Allergens → Eosinophilic response → itching, watery eyes
⚠️ II. Signs & Symptoms of Conjunctivitis
Signs and symptoms vary depending on the type and cause of conjunctivitis:
| 🔍 Type | ⚠️ Signs & Symptoms |
|---|---|
| Bacterial | 💧 Mucopurulent or yellow-green discharge, 👁️ redness, 👀 eyelid swelling, 💢 gritty sensation, 🟨 crusting of lashes |
| Viral | 💦 Watery discharge, 🔴 red eyes, 💢 burning, ⬆️ preauricular lymphadenopathy (in some cases), 😷 often associated with cold/flu |
| Allergic | 😣 Intense itching, 💧 watery/mucoid discharge, 🌬️ sneezing, 👁️ swollen eyelids (chemosis), usually bilateral |
| Chemical/Irritant | 🔥 Burning pain, 💧 excessive tearing, 🔴 redness, 👁️ blurred vision after exposure |
| Neonatal | 👶 Swelling of eyelids, ⏱️ early onset (within 1st month), 💧 discharge, redness, 🦠 risk of corneal damage |
🧪 III. Diagnosis of Conjunctivitis
🧑⚕️ 1. Clinical Diagnosis:
- Diagnosis is primarily clinical, based on history and physical examination
🔍 Key aspects:
- Type of discharge (watery, purulent, mucous)
- Presence of itching, burning, pain
- Laterality (one eye or both)
- Associated systemic symptoms (fever, cold, allergy)
- History of exposure (contact lens, irritants, viral illness, cosmetics)
🔬 2. Slit-Lamp Examination:
- Provides magnified view of:
- Conjunctival vessels
- Corneal clarity
- Follicles or papillae
- Foreign bodies or trauma signs
🧪 3. Laboratory Tests (in severe, recurrent, or neonatal cases):
| 🔬 Test | 💡 Purpose |
|---|---|
| Conjunctival swab & culture | Identify bacterial, viral, or chlamydial pathogens |
| Gram stain | Classify bacteria |
| Giemsa stain | Detect chlamydia or inclusion bodies (viral) |
| PCR testing | For specific viral causes like HSV or adenovirus |
| Allergy testing | For patients with chronic allergic conjunctivitis |
🧒 4. Special Tests for Neonates:
- Immediate gram stain and culture to rule out Neisseria gonorrhoeae (sight-threatening)
- Conjunctival scraping in suspected chlamydia or herpes infection
💊 I. Medical Management
Management of conjunctivitis depends on the underlying cause — bacterial, viral, allergic, or irritant/chemical.
🔹 1. Bacterial Conjunctivitis
✅ Treatment:
- Topical antibiotic eye drops or ointments:
- Erythromycin ointment
- Tobramycin or Gentamicin drops
- Moxifloxacin or Ofloxacin (broad-spectrum fluoroquinolones)
- Lubricating eye drops (artificial tears) for comfort
💡 Special Notes:
- Treat both eyes if infected
- Instruct patient on proper eye hygiene
- Contagious for ~24–48 hours after antibiotics are started
🔹 2. Viral Conjunctivitis
✅ Treatment:
- Supportive care – since it is self-limiting (7–14 days)
- Cold compresses for relief
- Artificial tears for lubrication
- Topical antihistamines for itching
- Antiviral therapy (e.g., Acyclovir) only if HSV is confirmed
⚠️ Precautions:
- Extremely contagious
- Advise strict hand hygiene, no sharing towels, avoid touching eyes
🔹 3. Allergic Conjunctivitis
✅ Treatment:
- Oral or topical antihistamines:
- Olopatadine, Ketotifen eye drops
- Mast cell stabilizers:
- Cromolyn sodium, Nedocromil
- NSAID drops: For inflammation relief
- Avoid known allergens
- Cold compresses to reduce itching and swelling
🔹 4. Chemical/Irritant Conjunctivitis
✅ Treatment:
- Immediate irrigation with sterile saline or water (especially in chemical exposure)
- Remove irritant if present
- Lubricating eye drops
- Topical antibiotics if corneal damage or abrasion is suspected
- Pain relief with NSAIDs or anesthetic drops
🔹 5. Neonatal Conjunctivitis (Ophthalmia Neonatorum)
✅ Treatment:
- Saline irrigation
- Topical and systemic antibiotics:
- Erythromycin ointment
- Ceftriaxone for gonococcal infection
- Azithromycin for chlamydial infection
- Urgent pediatric and ophthalmic referral required
🔪 II. Surgical Management
Surgery is rarely required in conjunctivitis but may be needed in chronic, severe, or complication-associated cases.
✂️ 1. Membranous Conjunctivitis (Severe bacterial or viral):
- Debridement (removal of pseudomembrane) under anesthesia
- Prevents symblepharon (adhesion) formation between lid and conjunctiva
✂️ 2. Chronic Allergic Conjunctivitis with Giant Papillae:
- Surgical excision of giant papillae on inner eyelid (for severe vernal keratoconjunctivitis)
✂️ 3. Conjunctival Biopsy:
- Performed when:
- Chronic conjunctivitis with unknown cause
- Suspected autoimmune disease (e.g., ocular cicatricial pemphigoid)
- Rule out conjunctival tumors or granulomas
✂️ 4. For Complications:
- Punctal occlusion or tarsorrhaphy may be done in severe exposure keratopathy or chronic dry eye after recurrent conjunctivitis
📌 Post-Treatment Advice (All Types):
- Strict eye hygiene (do not touch/rub eyes)
- Frequent handwashing
- No eye makeup or contact lenses until fully healed
- Complete the course of antibiotics or antivirals
- Use separate towels and bedding to prevent spread
- Avoid allergens or known irritants
👩⚕️👁️ Nursing Management of Conjunctivitis
🎯 Nursing Objectives:
✅ Relieve symptoms such as discomfort, redness, and itching
✅ Prevent the spread of infection (especially viral/bacterial types)
✅ Ensure proper medication administration
✅ Educate the patient and family about hygiene and precautions
✅ Monitor for complications (e.g., corneal involvement)
📋 I. Assessment Phase
🔍 Subjective Assessment:
- Ask about onset, duration, and type of discharge (watery, purulent, mucoid)
- Check for itching, pain, foreign body sensation, or photophobia
- Assess for history of recent flu, allergies, or contact lens use
🔬 Objective Assessment:
- Inspect eyes for:
- Redness, conjunctival swelling, discharge, crusting
- Unilateral or bilateral involvement
- Observe for:
- Lid edema or difficulty in opening eyes
- Lymph node swelling (preauricular nodes in viral cases)
💊 II. Nursing Interventions
🔹 1. Infection Control Measures
- Emphasize hand hygiene before and after touching the eyes
- Advise not to share towels, linens, eye drops, or cosmetics
- Discard old eye makeup and contact lenses
- Keep fingernails short and discourage eye rubbing
🔹 2. Medication Administration
- Administer prescribed eye drops/ointments:
- Antibiotics (for bacterial)
- Antivirals (for HSV)
- Antihistamines (for allergic)
- Teach correct eye drop technique:
- Pull down lower eyelid
- Instill drop without touching bottle to eye
- Close eyes gently; apply light pressure to inner canthus to prevent systemic absorption
🔹 3. Symptom Relief Measures
- Apply cold compresses (viral/allergic) or warm compresses (bacterial)
- Use lubricating eye drops to soothe dryness and irritation
- Ensure cleaning of crusts/discharge with sterile cotton and warm water
- Provide dark sunglasses if photophobia is present
🔹 4. Environmental and Patient Education
| 🧠 Topic | 📘 Teaching Tips |
|---|---|
| Contagion risk | Stay home from school/work during active infection (especially in viral) |
| Avoid contact lenses | Until symptoms fully resolve |
| Follow-up care | Keep appointments to ensure resolution |
| Recognizing complications | Report any vision changes, intense pain, corneal haze, or worsening symptoms |
🧾 III. Nursing Diagnoses (Examples):
- Risk for infection transmission related to contagious eye secretions
- Acute pain/discomfort related to inflammation and irritation of conjunctiva
- Deficient knowledge regarding eye hygiene and treatment compliance
- Impaired comfort related to photophobia, discharge, or itching
- Risk for visual disturbance if inflammation spreads to the cornea
✅ IV. Evaluation Criteria:
- Patient reports relief of discomfort, reduced redness, and discharge
- Eye appears clean and less inflamed
- No signs of infection spread to others or to the cornea
- Patient demonstrates correct use of medications and hygiene measures
- Patient verbalizes understanding of prevention, care, and when to seek help
🥗 I. Nutritional Considerations
While conjunctivitis is often infectious or allergic, proper nutrition plays a supportive role in:
✅ Enhancing immune response
✅ Promoting faster healing
✅ Preventing recurrence of infections
✅ Maintaining ocular surface health
✅ Essential Nutrients for Eye & Immune Health:
| 🧪 Nutrient | 🎯 Role | 🥗 Sources |
|---|---|---|
| Vitamin A | Maintains healthy conjunctival and corneal epithelium | Carrots, sweet potatoes, spinach, liver |
| Vitamin C | Enhances wound healing and immunity | Citrus fruits, guava, strawberries, bell peppers |
| Vitamin E | Protects cells from oxidative stress | Almonds, sunflower seeds, avocado |
| Zinc | Boosts immune function; helps with epithelial repair | Pumpkin seeds, legumes, whole grains |
| Omega-3 Fatty Acids | Reduces inflammation, supports tear production | Fish (salmon), flaxseeds, walnuts |
| Probiotics | Supports immune regulation and reduces allergic responses | Yogurt, kefir, fermented foods |
🧑⚕️ Dietary Advice for Patients:
- Eat balanced meals rich in antioxidants and anti-inflammatory foods
- Stay hydrated (water supports tear film and mucosal defense)
- Limit refined sugars and processed foods that may impair immunity
- For allergic conjunctivitis: identify and avoid dietary allergens if known
⚠️ II. Complications of Conjunctivitis
If untreated or poorly managed, conjunctivitis may lead to:
🔹 1. Corneal Involvement
- Keratitis or corneal ulcer (especially in viral/herpetic cases)
- Can lead to scarring and permanent vision loss
🔹 2. Chronic Conjunctivitis
- Long-standing irritation, inflammation, and discharge
- Seen in neglected allergic or bacterial cases
🔹 3. Conjunctival Scarring
- Especially in severe allergic conjunctivitis or chemical injuries
- May cause symblepharon (adhesion between eyelid and eyeball)
🔹 4. Vision Disturbance
- Blurring due to corneal edema or persistent inflammation
🔹 5. Spread of Infection
- From one eye to the other
- From patient to family or community (especially in viral/bacterial types)
🔹 6. Neonatal Complications
- Risk of blindness in ophthalmia neonatorum if untreated
📌 III. Key Points (Quick Revision)
✅ Conjunctivitis is inflammation of the conjunctiva, caused by bacteria, viruses, allergens, or irritants
✅ Common types include:
- Bacterial (purulent discharge, crusting)
- Viral (watery discharge, highly contagious)
- Allergic (itching, watery eyes, swelling)
- Chemical (pain, redness after exposure)
✅ Diagnosis is mainly clinical, supported by history, slit-lamp exam, and lab tests if needed
✅ Treatment depends on type:
- Antibiotics for bacterial
- Supportive care or antivirals for viral
- Antihistamines/mast cell stabilizers for allergic
- Irrigation and eye protection for chemical
✅ Nursing care includes:
- Hygiene education
- Medication administration
- Cold/warm compresses
- Infection control practices
✅ Nutrition supports healing and immune response — especially Vitamins A, C, E, Zinc, and Omega-3s
✅ Prevention involves:
- Hand hygiene
- Avoiding eye rubbing
- Not sharing personal items
- Proper contact lens hygiene
👁️🩸 Conjunctival Bleeding (Subconjunctival Hemorrhage)
📘 Definition:
Conjunctival bleeding, also called subconjunctival hemorrhage, refers to a localized bleeding beneath the conjunctiva — the transparent membrane covering the sclera (white part of the eye).
🔴 It appears as a bright red patch on the white of the eye, typically painless and non-threatening, but may indicate underlying systemic conditions in some cases.
🔍 Causes of Conjunctival Bleeding:
| ⚠️ Cause Type | 🔎 Examples |
|---|---|
| Traumatic | Eye rubbing, minor injury, foreign body, contact lens misuse |
| Spontaneous (Non-traumatic) | Sudden cough, sneeze, vomiting, heavy lifting |
| Medical Conditions | Hypertension, diabetes, blood clotting disorders, leukemia |
| Medications | Anticoagulants (e.g., warfarin), antiplatelets (aspirin, clopidogrel) |
| Infections or Inflammation | Conjunctivitis, uveitis, scleritis (rarely) |
| Surgical/Procedural | Post eye surgery, local anesthesia injection |
| Neonatal causes | Birth trauma during vaginal delivery |
🔢 Types of Conjunctival Bleeding:
| Type | Description |
|---|---|
| Spontaneous subconjunctival hemorrhage | Most common; unrelated to trauma |
| Traumatic hemorrhage | Due to direct impact or foreign object |
| Recurrent hemorrhage | Suggests systemic causes like hypertension or bleeding disorders |
| Massive hemorrhage | Rare; may cause chemosis or proptosis (orbital involvement) |
🔬 Pathophysiology:
- Conjunctiva has many fragile blood vessels (capillaries) overlying the sclera.
- A sudden increase in venous pressure (from coughing, sneezing, etc.) or trauma can cause one or more of these vessels to rupture.
- Blood leaks into the subconjunctival space.
- Since the conjunctiva is transparent, this blood becomes visible as a well-defined red patch.
- It is not absorbed by tears and thus remains until gradually reabsorbed over 1–2 weeks.
🧠 In systemic disorders (e.g., hypertension, coagulopathy), vessel fragility is increased, making spontaneous rupture more likely.
⚠️ Signs and Symptoms:
| 🔍 Symptom | Description |
|---|---|
| Painless red patch on white of eye | Most common feature; well demarcated, not raised |
| No vision change | Vision is typically normal |
| No discharge or itching | Unlike conjunctivitis |
| Mild irritation or foreign body sensation | Occasionally present |
| In recurrent cases | May be accompanied by systemic symptoms (bruising, bleeding elsewhere) |
🧪 Diagnosis:
🧑⚕️ 1. Clinical Examination:
- Inspection of the eye using torchlight or slit-lamp
- No conjunctival discharge, pupil changes, or corneal opacity
📋 2. History-Taking:
- Recent trauma, straining, lifting, sneezing
- Use of blood thinners
- History of hypertension, diabetes, bleeding disorders
🧪 3. Investigations (if recurrent or severe):
| Test | Purpose |
|---|---|
| Blood Pressure | Check for hypertension |
| CBC | Rule out anemia, thrombocytopenia, leukemia |
| PT/INR, aPTT | Assess clotting function if on anticoagulants |
| Blood sugar | Screen for diabetes |
| Liver function tests | Liver disease may impair clotting |
💊 Medical Management:
In most cases, no specific treatment is required, as the condition is self-limiting.
✅ General Approach:
- Reassurance: It looks alarming but is harmless in most cases
- Cold compress in the first 24 hours for comfort (if recent trauma)
- Lubricating eye drops (artificial tears) if there is irritation
- Avoid rubbing eyes or straining
- Monitor blood pressure and sugar levels
- Review medications (especially anticoagulants)
📋 Treat Underlying Conditions:
- Control hypertension or diabetes
- Adjust blood thinners if INR is high (under doctor’s guidance)
- Treat any underlying infection if present (e.g., conjunctivitis)
🔪 Surgical Management:
Surgical intervention is very rarely needed in subconjunctival hemorrhage. It may be considered only when:
| Indication | Procedure |
|---|---|
| Massive bleeding with chemosis | Drainage may be required |
| Recurrent hemorrhages with systemic cause | Surgery not for the eye, but systemic referral (hematology, cardiology) |
| Associated trauma with globe rupture | Requires emergency ophthalmic surgery |
✅ Summary of Key Points:
🔹 Conjunctival bleeding is often benign and self-limiting
🔹 Appears as a painless red patch on the white of the eye
🔹 Most cases resolve without treatment in 1–2 weeks
🔹 Recurrent cases need systemic evaluation
🔹 Management includes:
- Observation and reassurance
- Control of systemic risk factors
- Lubrication for comfort
🔹 Surgery is rarely indicated
👩⚕️👁️🩸 Nursing Management of Conjunctival Bleeding
🎯 Objectives of Nursing Care:
✔️ Provide comfort and psychological reassurance
✔️ Prevent complications such as recurrence or infection
✔️ Assist in identifying underlying systemic causes
✔️ Educate the patient on eye care and prevention
✔️ Monitor for signs of systemic bleeding or progression
📋 I. Assessment Phase
🔍 History Collection:
- Onset and duration of red patch
- Associated symptoms: discomfort, vision change, trauma, sneezing, coughing, heavy lifting
- Current medications: anticoagulants, antiplatelets
- Past medical history: hypertension, diabetes, bleeding disorders
- Contact lens use or eye rubbing
🧪 Physical Examination:
- Observe size, location, and extent of hemorrhage
- Check for:
- Swelling of eyelids or conjunctiva
- Presence of discharge
- Visual acuity (if affected)
- Measure blood pressure and blood glucose levels
💊 II. Nursing Interventions
🔹 1. Symptom Management and Support
- Provide psychological reassurance: “It looks worse than it is – usually harmless and self-healing”
- Apply cold compress (within 24 hours) to reduce any irritation
- Apply lubricating eye drops (prescribed) to ease mild irritation or dryness
🔹 2. Monitoring and Documentation
- Monitor for:
- Increase in size of hemorrhage
- Visual disturbances, pain, or photophobia
- Signs of recurrence or systemic bleeding (e.g., bruising, gum bleeding, nosebleeds)
- Record:
- Vital signs, especially blood pressure and pulse
- Any changes in the appearance of the affected eye
- Patient complaints or discomfort
🔹 3. Education and Prevention
| 📘 Topic | 💡 Patient Teaching Tips |
|---|---|
| Eye care | Avoid eye rubbing, no pressure or trauma to eyes |
| Activities | Avoid heavy lifting, straining, or vigorous sneezing |
| Medication review | Take anticoagulants/aspirin only under supervision; report excessive bleeding |
| Follow-up care | Advise follow-up if bleeding recurs or lasts more than 2 weeks |
| Blood pressure control | Importance of checking and maintaining BP regularly |
🔹 4. Referral and Interdisciplinary Collaboration
- Refer to:
- Physician or ophthalmologist if symptoms persist or worsen
- Hematologist in case of suspected bleeding disorders
- Internist/Cardiologist for blood pressure, diabetes, or medication adjustment
🧾 III. Nursing Diagnoses (Examples):
- Risk for injury related to fragile conjunctival blood vessels
- Deficient knowledge regarding eye care and recurrence prevention
- Anxiety related to sudden appearance of subconjunctival hemorrhage
- Risk for bleeding related to anticoagulant therapy or systemic disease
✅ IV. Evaluation Criteria:
- Hemorrhage resolves within 1–2 weeks without complication
- Patient verbalizes understanding of the condition and preventive measures
- No recurrence or progression of symptoms
- Vital signs (BP, glucose) remain within normal limits
- No additional signs of systemic bleeding
🥗 I. Nutritional Considerations
Though conjunctival bleeding is usually not caused by diet, nutrition supports vascular health, healing, and prevention of recurrence, especially in individuals with hypertension, diabetes, or fragile blood vessels.
✅ Important Nutrients:
| 🧪 Nutrient | 🎯 Role | 🥗 Sources |
|---|---|---|
| Vitamin C | Strengthens blood vessel walls; antioxidant | Citrus fruits, bell peppers, guava, broccoli |
| Vitamin K | Aids in blood clotting | Green leafy vegetables, broccoli, fish |
| Bioflavonoids | Enhance capillary strength and reduce fragility | Citrus peel, berries, grapes |
| Zinc | Supports tissue healing and immune health | Pumpkin seeds, legumes, meat |
| Iron & Folate | Prevent anemia and support oxygenation | Spinach, lentils, fortified cereals |
| Omega-3 Fatty Acids | Reduce inflammation and support cardiovascular health | Fish, flaxseeds, walnuts |
| Hydration (Water) | Keeps tissues moist and helps clear metabolic waste | Fluids, fruits, soups |
🧑⚕️ Dietary Advice:
- Avoid excessive alcohol, caffeine, and salty foods (may raise blood pressure)
- Reduce sugar and saturated fats in diabetic or hypertensive patients
- Encourage balanced meals with fruits, vegetables, whole grains, and lean protein
- For patients on anticoagulants, maintain consistent vitamin K intake
⚠️ II. Complications
Most conjunctival bleeds are harmless and self-limiting, but certain cases may lead to complications or indicate systemic problems.
🩺 Possible Complications:
- Recurrent Hemorrhage
- May signal uncontrolled hypertension, bleeding disorders, or over-anticoagulation
- Underlying Systemic Disease
- Could indicate diabetes, clotting defects, leukemia, or liver disease
- Corneal or Orbital Involvement (Rare)
- In cases of trauma with deeper injuries
- Vision Threat (Only in associated trauma or deeper globe injury)
- Not typical for simple subconjunctival hemorrhage
- Anxiety/Distress
- Sudden redness may cause alarm, especially in elderly or children
📌 III. Key Points (Quick Revision)
✔️ Conjunctival bleeding is typically due to rupture of small blood vessels in the conjunctiva — often spontaneous or caused by trauma, sneezing, straining, or hypertension.
✔️ Appears as a painless, bright red patch on the white of the eye and is usually self-limiting.
✔️ Medical evaluation is needed if:
- Bleeding is recurrent
- Involves other bleeding sites
- Patient is on anticoagulants
- Accompanied by systemic symptoms (bruises, dizziness, prolonged bleeding)
✔️ Management is conservative:
- Cold compress in early phase
- Artificial tears for comfort
- Control of BP, sugar, and review of blood thinners
✔️ Nutrition supports vascular integrity, healing, and prevention, especially in high-risk groups
✔️ Nursing care includes:
- Reassurance
- Monitoring for systemic signs
- Education on eye protection, hygiene, and medication compliance
👁️🦠 Corneal Inflammation and Infection (Keratitis)
📘 Definition:
Keratitis refers to the inflammation of the cornea, the clear, dome-shaped front layer of the eye that covers the iris and pupil.
It may be infectious or non-infectious and can lead to pain, redness, blurred vision, photophobia, and vision loss if not treated promptly.
🦠 When the cause is infectious, it is termed infective keratitis, which includes bacterial, viral, fungal, or parasitic origins.
🔍 Causes of Corneal Inflammation and Infection:
🔹 1. Infectious Causes:
| Type | Causative Organisms |
|---|---|
| Bacterial | Staphylococcus aureus, Pseudomonas aeruginosa, Streptococcus pneumoniae, Moraxella |
| Viral | Herpes Simplex Virus (HSV), Varicella-Zoster Virus (VZV), Adenovirus |
| Fungal | Fusarium, Aspergillus, Candida — especially after trauma with plant material |
| Parasitic | Acanthamoeba — associated with contact lens misuse and contaminated water |
🔹 2. Non-Infectious Causes:
| Type | Trigger/Condition |
|---|---|
| Traumatic | Corneal abrasion, foreign body, surgery, chemical exposure |
| Allergic/Autoimmune | Vernal keratoconjunctivitis, Sjögren’s syndrome, rheumatoid arthritis |
| Nutritional | Vitamin A deficiency → xerophthalmia and keratitis |
| Neurotrophic | Loss of corneal sensation (e.g., after herpes infection, diabetes, trigeminal nerve damage) |
🔹 Risk Factors:
- Contact lens misuse (e.g., overnight wear, poor hygiene)
- Ocular trauma (e.g., fingernail scratch, plant injury)
- Immunocompromised state (HIV, corticosteroid use)
- Dry eye syndrome
- Corneal surgery (e.g., LASIK)
🔢 Types of Keratitis:
🔸 1. Infective Keratitis
➡️ Caused by microbial pathogens
🧪 May produce corneal ulcers, stromal infiltration, hypopyon
Types include:
- Bacterial keratitis – acute, painful, with purulent discharge
- Viral keratitis – typically from HSV (dendritic ulcers), or VZV
- Fungal keratitis – slow onset, feathery borders, often after trauma
- Parasitic keratitis – Acanthamoeba, very painful, often in contact lens users
🔸 2. Non-infective Keratitis
➡️ Resulting from injury, immune response, or systemic condition
Types include:
- Photokeratitis – UV exposure (e.g., welding without protection, snow blindness)
- Exposure keratitis – due to incomplete eyelid closure (lagophthalmos)
- Neurotrophic keratitis – poor corneal healing due to sensory nerve damage
- Mooren’s ulcer – rare, idiopathic, progressive peripheral corneal ulceration
🔬 I. Pathophysiology of Keratitis
The cornea is an avascular, transparent tissue that plays a vital role in vision by refracting light into the eye.
When exposed to pathogens, trauma, or irritants, the corneal epithelium may be breached, allowing entry of microorganisms or triggering an inflammatory response.
🔁 Mechanism:
- Epithelial Damage or Compromise
- Caused by trauma, contact lenses, dryness, UV rays, or surgery
- ➡️ Entry of Pathogen or Irritant
- Bacteria, viruses, fungi, or parasites penetrate the corneal surface
- ➡️ Inflammatory Response
- Activation of immune cells (macrophages, neutrophils)
- Release of cytokines and inflammatory mediators
- ➡️ Corneal Edema and Cellular Infiltration
- Stromal inflammation, neovascularization, ulceration
- ➡️ Loss of Corneal Transparency and Vision Disturbance
- Scarring or necrosis in severe or untreated cases
🦠 Pathogen-Specific Notes:
- Bacterial keratitis: Rapid tissue destruction and ulceration
- Viral (HSV): Latent virus reactivates → dendritic ulcer
- Fungal: Deep, dry, feathery lesions; often slower but more destructive
- Acanthamoeba: Perineural spread, intense pain with minimal signs
⚠️ II. Signs & Symptoms of Keratitis
| 🚨 Symptom | 🔍 Description |
|---|---|
| Eye pain | Often sudden and severe (especially in bacterial and acanthamoeba keratitis) |
| Redness | Due to ciliary injection (perilimbal hyperemia) |
| Photophobia | Sensitivity to light |
| Tearing or watery discharge | Seen in viral or non-infectious keratitis |
| Purulent discharge | Common in bacterial keratitis |
| Foreign body sensation | Common early symptom |
| Blurred vision | Due to corneal edema or opacity |
| Corneal opacity/ulceration | Visible grayish or white spot on cornea |
| Eyelid swelling | Especially in severe or advanced infections |
| Hypopyon (in bacterial) | Accumulation of pus in anterior chamber |
🧪 III. Diagnosis of Keratitis
Diagnosis is clinical and laboratory-based, especially for infectious types.
🔍 1. Clinical History & Visual Inspection:
- Onset, duration, trauma, contact lens use, systemic illness
- Slit-lamp exam: corneal ulcer, epithelial defects, stromal infiltrates
- Fluorescein staining: Highlights epithelial defects (e.g., dendritic ulcers in HSV)
🔬 2. Slit Lamp Biomicroscopy:
- Assesses:
- Corneal clarity, thickness
- Presence of infiltrates, ulcers, hypopyon, keratic precipitates
🧪 3. Microbiological Investigations:
| Test | Purpose |
|---|---|
| Corneal scraping for Gram stain & culture | Identifies bacterial or fungal organisms |
| KOH mount | Detects fungal filaments |
| Giemsa stain | Identifies Acanthamoeba or viral inclusion bodies |
| PCR or viral culture | For HSV or VZV if suspected |
| Confocal microscopy | Useful in detecting Acanthamoeba cysts in vivo |
👁️ 4. Other Evaluations:
- Visual acuity testing – to monitor impairment
- Intraocular pressure – may rise due to secondary inflammation
- Systemic screening – if associated with autoimmune or infectious disease
💊 I. Medical Management
Medical treatment for keratitis focuses on eliminating the cause, reducing inflammation, preventing complications like ulceration or scarring, and preserving vision.
🔹 1. Bacterial Keratitis
✅ First-Line Treatment:
- Topical broad-spectrum antibiotics:
- Fluoroquinolones (e.g., Moxifloxacin, Ciprofloxacin)
- Fortified antibiotics (e.g., Cefazolin + Tobramycin)
- Instilled hourly initially, then tapered
✅ Supportive:
- Cycloplegic agents (e.g., Atropine 1%) to reduce pain and prevent synechiae
- Lubricating eye drops to support healing
- Oral antibiotics (e.g., Doxycycline) in severe or systemic involvement
🔹 2. Viral Keratitis (Herpes Simplex Virus – HSV)
✅ Treatment:
- Topical antiviral: Acyclovir 3% ointment, 5×/day
- Oral antiviral: Acyclovir 400–800 mg 5×/day for 10–14 days
- Avoid corticosteroids in epithelial keratitis
- For stromal keratitis (immune-mediated):
- May require topical steroids under ophthalmologist supervision + antiviral cover
🔹 3. Fungal Keratitis
✅ Treatment:
- Topical antifungal agents:
- Natamycin 5% (first-line for filamentous fungi)
- Amphotericin B 0.15% (for Candida)
- Oral antifungals: Ketoconazole or Voriconazole
- Treatment is prolonged (4–6 weeks) and may require combination therapy
🔹 4. Acanthamoeba Keratitis
✅ Treatment:
- Topical anti-amoebic agents:
- Polyhexamethylene biguanide (PHMB)
- Chlorhexidine 0.02%
- Oral antifungals or antibiotics may be added
- Pain management and close follow-up are essential
- Often resistant and slow to resolve
🔹 5. Non-infective Keratitis
| Cause | Treatment |
|---|---|
| Photokeratitis | Lubricants, cold compresses, cycloplegics, rest from light exposure |
| Exposure keratitis | Artificial tears, eyelid taping during sleep, moisture chambers |
| Neurotrophic keratitis | Lubrication, punctal plugs, sometimes topical nerve growth factors |
| Autoimmune-related keratitis | Systemic immunosuppressants (under rheumatologist guidance), corticosteroids cautiously used |
🔪 II. Surgical Management
Surgery is considered when medical therapy fails or complications arise (e.g., corneal perforation, non-healing ulcer, or scarring).
✂️ 1. Corneal Debridement
- Removes infected epithelium
- Improves penetration of topical medications
- Performed under slit lamp or minor OT setup
✂️ 2. Tissue Adhesive with Bandage Contact Lens
- For small corneal perforations (<2 mm)
- Prevents aqueous leakage and supports healing
✂️ 3. Therapeutic Penetrating Keratoplasty (TPK)
- Full-thickness corneal transplant
- Indicated in:
- Large, non-healing ulcers
- Imminent/perforated cornea
- Dense scars threatening vision
✂️ 4. Amniotic Membrane Transplantation (AMT)
- Promotes epithelial healing and reduces inflammation
- Used in neurotrophic, chemical, or autoimmune keratitis
✂️ 5. Conjunctival Flap Surgery
- A portion of conjunctiva is rotated over the ulcer site
- Provides vascular support to facilitate healing in non-healing ulcers
✂️ 6. Enucleation or Evisceration (Last resort)
- For severe, painful blind eye due to infection
- Rarely required if infection spreads to the globe or causes panophthalmitis
✅ Summary Table – Management at a Glance
| Type of Keratitis | Medical Management | Surgical Options |
|---|---|---|
| Bacterial | Topical & oral antibiotics | TPK, debridement if needed |
| Viral (HSV) | Topical + oral antivirals | Rarely required |
| Fungal | Topical antifungals | TPK, AMT |
| Parasitic | Anti-amoebic agents | TPK (often resistant) |
| Autoimmune/Exposure | Lubricants, steroids, systemic therapy | AMT, conjunctival flap |
👩⚕️👁️🦠 Nursing Management of Keratitis (Corneal Inflammation and Infection)
🎯 Objectives of Nursing Care:
✅ Relieve symptoms (pain, photophobia, redness)
✅ Prevent complications such as corneal perforation or vision loss
✅ Ensure adherence to medical therapy
✅ Provide patient education on hygiene, eye care, and follow-up
✅ Support emotional and psychological comfort
📋 I. Nursing Assessment
🔍 Subjective Data:
- Complaint of eye pain, burning, foreign body sensation
- History of contact lens use, trauma, exposure to UV, recent infection
- Symptoms of photophobia, blurred vision, or discharge
- Previous history of ocular surgery, herpes infection, or autoimmune disease
🔬 Objective Data:
- Redness of the eye (especially ciliary injection)
- Watering or purulent discharge
- Corneal opacity or visible ulcer (may be noted under slit-lamp or torch)
- Eyelid swelling, hypopyon (pus in anterior chamber – if visible)
- Check visual acuity (if feasible and safe)
💊 II. Nursing Interventions
🔹 1. Symptom Relief & Eye Protection
- Cold compresses for discomfort in non-infective keratitis
- Dark sunglasses or dim lighting to relieve photophobia
- Administer lubricating drops as prescribed (especially in dry or exposure keratitis)
- Encourage rest in a dark, quiet room
🔹 2. Medication Administration
- Instill prescribed eye drops/ointments strictly on schedule:
- Antibacterial, antiviral, antifungal, or anti-amoebic agents
- Cycloplegics (e.g., atropine) to relieve ciliary spasm
- Maintain aseptic technique while instilling drops
- Avoid touching the dropper tip to the eye or eyelids
- Space eye drops 5–10 minutes apart if multiple prescribed
🔹 3. Infection Control Measures
- Perform hand hygiene before and after eye care
- Use gloves when applying ointments or irrigating eyes
- Instruct the patient not to touch or rub eyes
- Discourage sharing of towels, eye drops, or cosmetics
- For infectious keratitis, maintain isolation precautions if needed
🔹 4. Monitoring and Reporting
- Monitor for progression of symptoms:
- Increased redness, pain, vision loss, or discharge
- Appearance of hypopyon or signs of corneal perforation
- Watch for medication side effects or allergy
- Record visual changes or difficulty with light sensitivity
🔹 5. Patient Education
| 📘 Topic | 🧾 Teaching Instructions |
|---|---|
| Medication adherence | Complete the full course, even if symptoms improve |
| Contact lens care | Avoid during active infection; sterilize or discard old lenses |
| UV protection | Use protective eyewear during exposure (welders, snow) |
| Avoid self-medication | Especially steroid eye drops, unless prescribed |
| When to seek help | If vision worsens, severe pain, or eye swelling increases |
| Follow-up visits | Emphasize importance of ophthalmologist review and corneal evaluation |
🧾 III. Sample Nursing Diagnoses:
- Acute pain related to inflammation of corneal tissue
- Risk for infection transmission related to infectious keratitis
- Disturbed sensory perception (visual) due to corneal ulceration
- Deficient knowledge regarding eye care and medication regimen
- Anxiety related to sudden visual changes or diagnosis
✅ IV. Evaluation Criteria
- Pain and redness are reduced
- Patient uses medications correctly
- No signs of corneal perforation or vision deterioration
- Patient understands and demonstrates proper eye hygiene and safety measures
- Infection does not spread or recur
🥗 I. Nutritional Considerations
Though keratitis is primarily caused by infection, trauma, or immune dysfunction, nutrition plays a crucial supportive role in promoting corneal healing, immune response, and preventing recurrence, especially in chronic or post-surgical cases.
✅ Essential Nutrients for Corneal and Ocular Health:
| 🧪 Nutrient | 🎯 Function | 🥗 Sources |
|---|---|---|
| Vitamin A | Maintains corneal epithelial integrity, prevents keratinization | Carrots, sweet potatoes, spinach, fish liver oil |
| Vitamin C | Enhances collagen synthesis for corneal healing, antioxidant | Citrus fruits, bell peppers, kiwi, amla |
| Vitamin E | Protects cell membranes from oxidative damage | Almonds, sunflower seeds, avocados |
| Zinc | Aids in vitamin A metabolism and epithelial repair | Pumpkin seeds, nuts, dairy, meat |
| Omega-3 fatty acids | Reduce ocular surface inflammation, improve tear film | Fatty fish (salmon, sardines), flaxseeds, walnuts |
| B Vitamins (especially B2 – Riboflavin) | Prevents corneal ulcers and supports nerve function | Dairy, eggs, whole grains |
| Protein | Tissue repair and immune function | Lean meat, legumes, dairy, soy |
🧑⚕️ Dietary Advice:
- Ensure a balanced diet with all food groups
- Avoid smoking and alcohol — impair healing and immune defense
- Increase hydration to maintain tear film
- Avoid junk and processed foods that cause inflammation
- In Vitamin A-deficient patients (e.g., children in undernourished populations), supplementation may be necessary
⚠️ II. Complications of Keratitis
If not treated promptly and properly, keratitis can result in serious and vision-threatening complications:
🔹 1. Corneal Ulcer
- Progression of untreated keratitis → deep stromal involvement and tissue necrosis
🔹 2. Corneal Scarring
- Leads to permanent visual impairment or blindness
- Especially in central corneal involvement
🔹 3. Corneal Perforation
- Full-thickness destruction of the cornea
- Can cause prolapse of intraocular contents and endophthalmitis
🔹 4. Hypopyon
- Collection of pus in the anterior chamber
- Sign of severe bacterial keratitis
🔹 5. Secondary Glaucoma
- From inflammation or steroid misuse
- Elevated intraocular pressure damaging the optic nerve
🔹 6. Endophthalmitis or Panophthalmitis
- Spread of infection into vitreous humor or entire globe
- Rare but sight-threatening and painful
🔹 7. Loss of Vision or Eye (Enucleation)
- In severe or neglected cases
📌 III. Key Points (Quick Revision)
✔️ Keratitis is inflammation of the cornea, caused by infections (bacterial, viral, fungal, parasitic) or non-infective factors (UV, dryness, autoimmune)
✔️ Prompt diagnosis and treatment are essential to prevent corneal ulceration, scarring, or vision loss
✔️ Clinical features: Eye pain, redness, photophobia, discharge, blurred vision, foreign body sensation
✔️ Diagnosis: Clinical exam + fluorescein staining + microbiological testing (scraping, KOH, PCR)
✔️ Treatment depends on the cause:
- Antibiotics, antivirals, antifungals, anti-amoebic agents
- Cycloplegics and lubricants for pain and protection
- Surgery (TPK, amniotic membrane graft) in non-healing or perforated ulcers
✔️ Nursing care includes:
- Eye drop administration
- Aseptic precautions
- Patient education on hygiene, medication use, and follow-up
✔️ Nutrition supports immune function and corneal healing — emphasize Vitamin A, C, E, zinc, omega-3s
✔️ Complications can be severe — including corneal ulceration, perforation, endophthalmitis, or blindness.
👁️⚕️ Cataract.
📘 Definition:
A cataract is a clouding or opacification of the lens of the eye that leads to a gradual, progressive loss of vision.
The normally clear, transparent lens becomes hazy or opaque, preventing light from properly focusing on the retina.
👁️ It is the leading cause of reversible blindness worldwide, especially in older adults.
🔍 Causes of Cataract:
Cataracts can be age-related, congenital, traumatic, or secondary to other conditions.
🔹 1. Age-related (Senile Cataract) – Most Common
- Natural aging leads to protein denaturation and aggregation in the lens
- Starts after 40–50 years; progresses with age
🔹 2. Congenital Cataract
- Present at birth or develops during infancy
- Causes:
- Genetic disorders
- Intrauterine infections (e.g., rubella, syphilis, toxoplasmosis)
- Metabolic diseases (e.g., galactosemia)
🔹 3. Traumatic Cataract
- Follows blunt or penetrating eye injury
- May occur immediately or after weeks/months
- Also caused by radiation (infrared, UV, X-ray) or electric shock
🔹 4. Secondary Cataract
Occurs as a result of other ocular or systemic conditions:
| Trigger | Examples |
|---|---|
| Systemic diseases | Diabetes mellitus (sorbitol accumulation damages lens) |
| Medications | Long-term corticosteroid use (systemic or topical) |
| Eye diseases | Glaucoma, uveitis, retinal detachment |
| Post-surgical | Following vitrectomy or intraocular surgery |
👁️⚕️ Types of Cataracts
Cataracts are classified based on their location within the lens, cause, or age of onset. Each type has distinctive features and clinical significance.
🔢 I. Based on Location in the Lens:
🔹 1. Nuclear Cataract (Nuclear Sclerosis)
- Affects the central (nuclear) zone of the lens
- Most common age-related cataract
- Lens becomes yellow or brown, affecting distance vision first
🧠 Key Features:
- Gradual progression
- May cause “second sight” (temporary near vision improvement)
- Myopic shift may occur
🔹 2. Cortical Cataract
- Affects the outer layer (cortex) of the lens
- Characterized by wedge-shaped (spoke-like) opacities
🧠 Key Features:
- Glare and light scatter at night
- More noticeable in bright light conditions
- Progresses from outside-in
🔹 3. Posterior Subcapsular Cataract (PSC)
- Opacity forms at the back of the lens, just under the capsule
🧠 Key Features:
- Fastest-progressing among age-related types
- Causes difficulty in reading, glare in bright light, especially during the day
- Common in younger patients, steroid users, and diabetics
🧬 II. Based on Cause:
🔹 4. Senile (Age-Related) Cataract
- Most common type
- Includes nuclear, cortical, and PSC types
🔹 5. Congenital Cataract
- Present at birth or early infancy
- Causes: infections (TORCH), metabolic errors, genetic disorders
Types of Congenital Cataract:
- Lamellar: Opacity in a specific layer (often symmetrical)
- Polar: Affects anterior or posterior pole
- Nuclear: Involves central nucleus from birth
- Sutural: Affects Y-shaped lens sutures
🔹 6. Traumatic Cataract
- Due to penetrating or blunt eye trauma
- Also from radiation (infrared, UV) or electric burns
🧠 May develop:
- Rosette-shaped opacities in blunt trauma
- Anterior/posterior capsule rupture in penetrating injury
🔹 7. Secondary Cataract
- Develops secondary to another disease or condition
Causes:
- Diabetes mellitus
- Chronic uveitis
- High myopia
- Glaucoma
- Long-term corticosteroid use
🔹 8. Metabolic Cataract
- Associated with inborn errors of metabolism
Examples:
- Galactosemia: Oil droplet cataract in infants
- Hypocalcemia: Cataract due to calcium imbalance
- Diabetes mellitus: Sorbitol accumulation → snowflake cataracts
🔹 9. Radiation Cataract
- Due to exposure to UV, infrared, X-rays, or nuclear radiation
- Often posterior subcapsular in nature
🔹 10. Complicated Cataract
- Develops secondary to other ocular diseases such as:
- Retinitis pigmentosa
- Uveitis
- Retinal detachment
- Glaucoma
✅ Summary Table:
| Type | Description | Common Causes |
|---|---|---|
| Nuclear | Central lens opacity | Aging |
| Cortical | Peripheral spoke-like opacity | Aging, UV light |
| PSC | Back of lens, under capsule | Steroids, diabetes, younger age |
| Congenital | Present at birth | TORCH infections, genetics |
| Traumatic | Post-injury | Blunt or penetrating trauma |
| Secondary | From systemic or ocular disease | Diabetes, uveitis |
| Metabolic | Related to systemic metabolism errors | Galactosemia, hypocalcemia |
| Radiation | After radiation exposure | UV, X-rays |
| Complicated | Secondary to eye diseases | Glaucoma, retinal diseases |
👁️⚕️ Pathophysiology of Cataracts – All Types
🔬 What is Cataract Pathophysiology?
Cataract formation involves denaturation, aggregation, and opacification of lens proteins, loss of lens transparency, and disturbance in lens metabolism. The clear crystalline lens becomes cloudy, disrupting the normal passage of light onto the retina.
Each type of cataract has a specific underlying pathological mechanism, depending on age, cause, and location in the lens.
🔢 I. Age-Related Cataracts (Senile Cataract)
🔸 1. Nuclear Cataract
- Oxidative stress causes damage to nuclear lens fibers
- Leads to accumulation of yellow-brown pigments (chromophores) → nuclear sclerosis
- Increased refractive index → early myopia (“second sight”)
🔁 Slow, bilateral, and central opacity
🔸 2. Cortical Cataract
- Disruption of electrolyte balance in the cortex due to aging → Na⁺ and water influx
- Causes swelling of lens fibers, leading to clefts and cracks
- Results in spoke-like (radial) opacities
🔁 Begins in periphery and progresses toward the center
🔸 3. Posterior Subcapsular Cataract (PSC)
- Epithelial cells migrate to the posterior subcapsular region
- Abnormal fibrous metaplasia and protein aggregation beneath posterior capsule
- Interferes with light transmission, especially in bright light
🔁 Rapidly progressive; affects near vision early
🧬 II. Congenital Cataracts
🔸 Causes include: TORCH infections, metabolic disorders, or genetic mutations.
- Genetic mutations → abnormal crystallin proteins
- Intrauterine infections → lens fiber necrosis and calcification
- Metabolic defects (e.g., galactosemia) → accumulation of toxic metabolites like galactitol, drawing water into lens → swelling and opacification
🔁 Symmetrical or asymmetrical opacities; may be lamellar, polar, or nuclear
🧨 III. Traumatic Cataract
🔸 A. Blunt trauma:
- Shock wave passes through the eye → disruption of lens fibers
- Rosette-shaped opacity is typical
🔸 B. Penetrating trauma:
- Damage to the capsular bag allows aqueous humor to enter lens → hydration → opacification
🔸 C. Radiation:
- Ionizing radiation causes DNA damage and oxidative stress in lens epithelial cells
- Leads to posterior subcapsular opacities
🔁 IV. Secondary Cataract (Due to Systemic or Ocular Disease)
🔸 1. Diabetic Cataract:
- Excess glucose → converted to sorbitol via aldose reductase
- Sorbitol accumulates in lens → osmotic swelling, rupture of lens fibers → “snowflake cataract”
🔸 2. Steroid-induced Cataract:
- Corticosteroids alter the lens epithelial metabolism
- Leads to abnormal differentiation and posterior subcapsular opacity
🔸 3. Chronic Uveitis/Glaucoma:
- Long-term inflammation or elevated IOP disturbs lens metabolism
- Inflammatory mediators damage lens fibers
🧫 V. Metabolic Cataracts
🔸 1. Galactosemia:
- Deficiency of galactose-1-phosphate uridyl transferase
- Galactose converts to galactitol, leading to lens hydration and opacification
🔸 2. Hypocalcemia:
- Reduced calcium disrupts lens transparency and cellular function
- Leads to protein aggregation and opacity
🧪 VI. Complicated Cataracts
- Develop secondary to chronic intraocular disease (e.g., retinitis pigmentosa, chronic uveitis)
- Long-standing disease leads to toxic damage to lens epithelial cells
- Results in polychromatic sheen, vacuoles, and eventual opacity
🔁 Common Final Pathways in Cataract Formation:
✅ Protein denaturation & aggregation
✅ Loss of lens transparency
✅ Hydration of lens fibers
✅ Oxidative damage to epithelial cells
✅ Calcium and electrolyte imbalance
👁️⚕️ Cataract – Signs & Symptoms | Diagnosis
⚠️ I. Signs & Symptoms of Cataract
Cataracts typically develop slowly and progressively. Symptoms may vary depending on the type, location, and maturity of the cataract.
👁️ Common Signs & Symptoms:
| Symptom | Description |
|---|---|
| Blurred or dim vision | Most common; occurs gradually |
| Difficulty with night vision | Especially in nuclear and cortical cataracts |
| Glare or halos around lights | Common in posterior subcapsular cataracts |
| Fading or yellowing of colors | Due to lens discoloration |
| Increased sensitivity to light | Photophobia due to scattering of light |
| Double vision in one eye (monocular diplopia) | When the lens causes uneven refraction |
| Frequent changes in glasses prescription | Due to fluctuating lens index (e.g., myopic shift) |
| Need for brighter light for reading | Due to reduced contrast sensitivity |
| Loss of red reflex (in mature cataracts) | Seen on ophthalmoscopic exam |
| White or cloudy pupil (in advanced or congenital cases) | Visible lens opacity |
🔍 Signs Specific to Cataract Types:
- Nuclear cataract → gradual loss of distance vision, yellowish hue
- Cortical cataract → glare in bright light or night driving
- Posterior subcapsular cataract → early near vision difficulty, photophobia
- Congenital cataract → white pupil (leukocoria), nystagmus, poor fixation
🧪 II. Diagnosis of Cataract
Cataract is diagnosed through a combination of history, visual acuity tests, and detailed eye examination.
🔹 1. Visual Acuity Testing (Snellen’s Chart)
- Assesses clarity of vision
- Shows progressive decrease in visual acuity, usually bilateral but asymmetric
- Near and distant vision both may be affected
🔹 2. Slit-Lamp Examination
- Direct visualization of the lens using a biomicroscope
- Allows assessment of:
- Location of opacity (nuclear, cortical, PSC)
- Stage of cataract (immature, mature, hypermature)
🔹 3. Ophthalmoscopy (Fundus Examination)
- Red reflex is dull or absent in dense cataracts
- Retina may not be visualized in mature cataracts
- Performed to rule out posterior segment disease (after pupil dilation)
🔹 4. Tonometry
- Measures intraocular pressure (IOP)
- Done to rule out associated glaucoma, especially in phacomorphic cataract
🔹 5. Retinoscopy/Refraction
- Measures refractive error
- Detects myopic shift in nuclear cataract
- Frequent changes in spectacles without vision improvement suggest cataract
🔹 6. B-Scan Ultrasound (A-scan if surgical)
- Used when fundus cannot be visualized due to dense cataract
- Evaluates retinal status before surgery
- A-scan also used for IOL (intraocular lens) power calculation
🔹 7. Pupillary Reflex Examination
- In congenital cataract, absence of red reflex or presence of leukocoria may be the only clue
- Important in screening infants
✅ Summary Chart – Clinical Assessment of Cataract
| Test | Purpose |
|---|---|
| Visual acuity | Measures the degree of vision loss |
| Slit-lamp | Visualizes and classifies cataract type |
| Ophthalmoscopy | Assesses red reflex and fundus visibility |
| Tonometry | Detects associated raised IOP |
| B-scan ultrasound | Rules out retinal disease if cataract is dense |
| Pupillary light reflex | Especially in congenital cataract screening |
👁️⚕️ Cataract – Medical Management
⚠️ Important Note:
Cataract is a progressive and irreversible opacity of the lens.
👉 No medication can reverse a cataract once it has formed.
👉 Surgical removal of the cataractous lens is the only definitive treatment.
However, medical (non-surgical) management is used for:
- Early-stage cataracts
- Delaying progression
- Managing symptoms
- Preparing patients for surgery
- Treating underlying or associated conditions
💊 I. Symptom Management in Early-Stage Cataract
🔹 1. Corrective Lenses
- Prescription glasses or contact lenses can temporarily improve vision
- Especially useful in nuclear cataract with myopic shift
🔹 2. Magnifying Lenses or Reading Aids
- Helpful for patients with difficulty in near tasks (e.g., reading, sewing)
🔹 3. Anti-glare Glasses/Sunglasses
- Reduce photophobia and glare, especially in posterior subcapsular cataracts
🔹 4. Stronger Indoor Lighting
- Bright, focused lighting improves reading and daily activities
🧪 II. Medical Therapy (Supportive or Investigational)
Though no proven medical therapy exists to cure cataracts, some pharmacologic agents are under study for delaying onset or progression:
| Drug | Role |
|---|---|
| N-acetylcarnosine eye drops (used in some countries) | Antioxidant effect; claimed to delay cataract progression |
| Aldose reductase inhibitors | Prevent sugar-alcohol accumulation in diabetic cataracts (experimental) |
| Vitamin supplements (A, C, E, lutein, zinc) | Antioxidants believed to reduce oxidative stress in lens |
| NSAIDs (Ketorolac drops) | Sometimes used to manage inflammation in associated uveitis or pre/post-surgery |
⚠️ These treatments are not curative and should not replace surgical referral in visually significant cataracts.
🧬 III. Managing Underlying or Associated Conditions
- Blood glucose control in diabetics to delay cataract progression
- Management of uveitis or glaucoma with topical medications
- Review of steroid usage if suspected as a cause
- Treatment of nutritional deficiencies (e.g., Vitamin A)
🩺 IV. Monitoring and Follow-up
Patients not yet eligible for surgery should be:
- Monitored every 6–12 months
- Referred for surgical evaluation when:
- Vision interferes with daily living or occupational needs
- Cataract threatens complications (e.g., phacomorphic glaucoma)
✅ Summary – Medical Management of Cataract
| Management | Purpose |
|---|---|
| Spectacles/contact lenses | Temporary vision correction |
| Lighting & magnifiers | Improve near vision activities |
| Sunglasses | Reduce glare and photophobia |
| Antioxidant vitamins (optional) | May slow progression |
| Control of systemic diseases | Prevent secondary cataract |
| Follow-up exams | Monitor visual decline and refer timely |
👁️🔬 Cataract – Surgical Management
⚠️ Key Principle:
Cataract surgery is the only definitive treatment that restores vision by removing the opaque lens and replacing it with a clear artificial intraocular lens (IOL).
It is one of the safest and most commonly performed surgeries worldwide, with a very high success rate when done at the right time.
✂️ Types of Cataract Surgery
🔹 1. Phacoemulsification (Phaco) – Most Common
✅ Modern, minimally invasive procedure
🔧 Technique:
- Performed under local anesthesia
- A tiny incision (2–3 mm) is made in the cornea
- Ultrasound waves are used to break (emulsify) the cloudy lens
- Fragments are suctioned out
- A foldable intraocular lens (IOL) is inserted through the same incision
✅ Advantages:
- Stitchless, fast healing
- Minimal complications
- Quick visual recovery
- Done as day-care surgery
🔹 2. Manual Small Incision Cataract Surgery (MSICS)
✅ Used when phaco is not suitable (e.g., very mature cataract, low-resource settings)
🔧 Technique:
- A slightly larger incision (6–7 mm) is made
- Cataractous lens is manually extracted in one piece
- Rigid IOL is implanted
✅ Advantages:
- Cost-effective
- Suitable for dense or hypermature cataracts
- Doesn’t require phaco machine
🔹 3. Extracapsular Cataract Extraction (ECCE)
✅ Traditional surgery; rarely used today
🔧 Technique:
- Large incision (10–12 mm) is made
- Lens is removed in one piece, posterior capsule is left intact
- IOL is implanted into the capsular bag
🔹 4. Intracapsular Cataract Extraction (ICCE)
⚠️ Obsolete technique – used only in rare emergency cases
- Entire lens and capsule are removed
- IOL placed in anterior chamber
🧬 Types of Intraocular Lenses (IOLs)
| Type | Description |
|---|---|
| Monofocal IOL | Corrects vision at one distance (usually far); most common |
| Multifocal IOL | Provides both near and distance vision |
| Toric IOL | Corrects astigmatism |
| Accommodative IOL | Shifts position slightly to mimic natural focus change |
🧾 Pre-operative Preparation
- Detailed eye examination
- Biometry (A-scan) to calculate IOL power
- Blood pressure, sugar control
- Informed consent and education
🩺 Post-operative Care
- Use of antibiotic + steroid eye drops
- Eye shield at night for protection
- Avoid touching/rubbing the eye
- Limit heavy lifting, bending, or water entry into the eye
- Attend follow-up visits
🚨 Indications for Surgery
- Significant visual impairment affecting daily activities (reading, driving)
- Mature cataract with risk of complications (e.g., phacomorphic glaucoma)
- Cataract interferes with treatment of other eye diseases (e.g., diabetic retinopathy, glaucoma)
❌ Contraindications (Temporary or Relative)
- Uncontrolled systemic illness (e.g., severe hypertension, infection)
- Active ocular infections
- Poor retinal or optic nerve function (e.g., end-stage glaucoma, macular degeneration — limited benefit)
✅ Summary Table – Surgical Management at a Glance
| Technique | Incision | IOL | Suitability |
|---|---|---|---|
| Phacoemulsification | Tiny (2–3 mm) | Foldable | Most preferred |
| MSICS | Medium (6–7 mm) | Rigid | Dense cataracts, low-resource |
| ECCE | Large (10–12 mm) | Rigid | Rare use |
| ICCE | Very large | Anterior chamber IOL | Obsolete |
👩⚕️👁️ Nursing Management of Cataract
🎯 Objectives of Nursing Care:
✔️ Support the patient before, during, and after cataract surgery
✔️ Prevent complications (especially infection and injury)
✔️ Promote healing and restore visual function
✔️ Educate patient and family about care and precautions
✔️ Provide emotional support and reduce surgical anxiety
📋 I. Preoperative Nursing Management
🔹 1. Patient Assessment
- Assess visual acuity and baseline vision
- Take complete medical history: diabetes, hypertension, bleeding disorders
- Ask about use of anticoagulants or steroids
- Check for allergies (especially to iodine, anesthetics)
🔹 2. Psychological Preparation
- Provide reassurance; address fear of surgery or vision loss
- Explain the procedure, anesthesia (usually local), and recovery expectations
🔹 3. Preoperative Instructions
- NPO status if general anesthesia (usually not needed in phaco)
- Instruct on face washing, no eye makeup, wear clean clothes
- Instillation of preoperative eye drops:
- Mydriatics (e.g., Tropicamide) to dilate pupil
- Antibiotics to reduce infection risk
- NSAIDs to control inflammation
🔹 4. Consent and Coordination
- Ensure informed consent is signed
- Assist in coordinating lab tests or eye biometry
- Prepare ID band, surgical checklist, and OT documentation
🏥 II. Intraoperative Nursing Management
(Usually performed by operating room nurse or ophthalmic nurse)
- Assist in positioning the patient comfortably in supine position
- Maintain sterile field and aseptic technique
- Provide instruments and IOL to surgeon
- Monitor vital signs if under local anesthesia with sedation
- Provide emotional support throughout procedure
🩺 III. Postoperative Nursing Management
🔹 1. Immediate Post-Op Care
- Monitor for:
- Vital signs (especially if sedated)
- Bleeding, pain, or excessive tearing
- Signs of infection or corneal edema
- Apply eye patch or shield as per doctor’s order
- Ensure patient rests with head elevated (semi-Fowler’s position)
- Provide prescribed eye drops:
- Antibiotic to prevent infection
- Steroid/NSAID to reduce inflammation
- Lubricants for comfort
🔹 2. Patient Education for Home Care
| 💡 Topic | 📝 Instruction |
|---|---|
| Eye protection | Wear protective eye shield at night for 1 week |
| Avoid rubbing/touching the eye | Risk of infection or IOL dislocation |
| Activity restriction | Avoid bending, lifting heavy objects, straining |
| Personal hygiene | Wash hands before touching the face; use clean towels |
| Medication compliance | Instill eye drops correctly and on schedule |
| Signs to report immediately | Pain, vision loss, excessive redness, purulent discharge |
| Follow-up appointments | Essential to monitor healing and check IOL position |
🧾 IV. Common Nursing Diagnoses
- Disturbed sensory perception (visual) related to lens opacity
- Risk for infection related to postoperative eye surgery
- Acute pain related to inflammation or surgical procedure
- Deficient knowledge related to postoperative care
- Anxiety related to surgery and potential vision changes
✅ V. Evaluation Criteria
- Patient reports relief from preoperative symptoms (e.g., blurred vision)
- No signs of infection or complications observed post-op
- Patient demonstrates correct eye drop instillation technique
- Patient verbalizes understanding of self-care and follow-up schedule
- Vision improvement noted on follow-up visual acuity testing
🥗 I. Nutritional Considerations in Cataract
While nutrition cannot reverse a formed cataract, it plays an essential role in:
✅ Delaying onset and progression of age-related cataracts
✅ Supporting recovery post-surgery
✅ Reducing oxidative stress on the lens
✅ Key Nutrients and Their Roles:
| Nutrient | Function | Sources |
|---|---|---|
| Vitamin A | Maintains healthy epithelial tissues of the eye | Carrots, sweet potatoes, spinach |
| Vitamin C | Antioxidant; slows oxidative damage to lens proteins | Citrus fruits, guava, kiwi, broccoli |
| Vitamin E | Protects lens membranes from oxidative damage | Almonds, sunflower seeds, avocados |
| Lutein & Zeaxanthin | Carotenoids concentrated in the lens & retina; protect from UV damage | Kale, spinach, corn, eggs |
| Zinc | Helps transport Vitamin A; essential for retinal health | Pumpkin seeds, legumes, seafood |
| Omega-3 fatty acids | Anti-inflammatory properties; help in dry eye and retinal support | Fatty fish (salmon), flaxseed, walnuts |
💡 Dietary Advice for Cataract Patients:
- Eat a colorful variety of fruits and vegetables
- Avoid smoking and excessive alcohol (increase oxidative stress)
- Stay hydrated for ocular tissue health
- Minimize intake of processed, fried, or sugary foods
- After surgery, focus on protein-rich foods and vitamin C to promote healing
⚠️ II. Complications of Cataract & Its Surgery
🩺 A. Preoperative/Untreated Cataract Complications
| Complication | Description |
|---|---|
| Mature or hypermature cataract | Overripe lens; risk of lens protein leakage |
| Phacomorphic glaucoma | Intumescent lens blocks aqueous outflow → acute glaucoma |
| Phacolytic glaucoma | Leaked lens proteins cause inflammatory glaucoma |
| Lens-induced uveitis | Inflammation from leaking lens material |
| Vision loss or blindness | Especially in developing countries due to delayed treatment |
🔪 B. Postoperative Surgical Complications
| Complication | Description |
|---|---|
| Posterior capsule opacification (PCO) | “Secondary cataract” – common long-term; treated with YAG laser |
| Endophthalmitis | Severe intraocular infection; presents with pain, redness, pus, vision loss |
| Cystoid macular edema (CME) | Swelling of retina; causes blurred central vision |
| Retinal detachment | Rare but serious; flashes, floaters, vision curtain |
| Intraocular lens (IOL) dislocation | Due to capsular rupture or zonular weakness |
| Increased intraocular pressure | From inflammation, retained viscoelastic, or steroid response |
| Corneal edema or decompensation | Especially in older patients or surgical trauma |
✅ III. Key Points (Quick Revision)
✔️ Cataract is clouding of the natural lens, leading to progressive, painless vision loss
✔️ Common in elderly, but can occur congenitally, post-trauma, or secondary to diseases (e.g., diabetes)
✔️ Symptoms include: blurred vision, glare, color fading, frequent prescription changes
✔️ Diagnosis: Visual acuity test, slit-lamp exam, ophthalmoscopy
✔️ Medical management is limited to symptom relief; surgery is definitive treatment
✔️ Surgical methods include: Phacoemulsification (most common), MSICS, ECCE
✔️ Post-op care involves infection prevention, eye protection, and adherence to medications
✔️ Nutrition rich in antioxidants can help delay progression and support healing
✔️ Watch for complications like infection, IOL issues, or macular edema post-surgery
✔️ Nursing care involves education, drop administration, hygiene, emotional support, and follow-up care
👁️⚕️ Glaucoma.
📘 Definition:
Glaucoma is a group of progressive optic neuropathies characterized by:
🔸 Increased intraocular pressure (IOP)
🔸 Damage to the optic nerve head
🔸 Gradual loss of peripheral vision, which may progress to total blindness if untreated
It is often called the “silent thief of sight” because it typically progresses without early symptoms.
🔍 Causes of Glaucoma
Glaucoma may result from various primary or secondary causes that interfere with the drainage of aqueous humor, leading to increased intraocular pressure and optic nerve damage.
🔹 I. Primary Causes (Idiopathic)
These develop without an identifiable external cause.
1. Primary Open-Angle Glaucoma (POAG)
- Most common form
- Chronic, bilateral, slowly progressive
- Drainage angle is anatomically open, but trabecular meshwork function is reduced, impairing aqueous outflow
2. Primary Angle-Closure Glaucoma (PACG)
- Occurs when iris blocks the drainage angle (trabecular meshwork)
- Can be acute (sudden rise in IOP) or chronic (gradual synechial closure)
🔹 II. Secondary Causes (Due to Other Eye or Systemic Conditions)
| Cause Type | Examples |
|---|---|
| Eye diseases | Uveitis, cataract, retinal detachment, tumors |
| Eye trauma | Hyphema, lens dislocation, angle damage |
| Medications | Long-term corticosteroids (topical/systemic) |
| Surgery-related | Post-cataract surgery or laser treatment |
| Systemic diseases | Diabetes mellitus, hypertension, thyroid eye disease |
🔹 III. Congenital / Developmental Causes
| Type | Description |
|---|---|
| Congenital Glaucoma | Occurs at birth or early infancy due to maldevelopment of aqueous drainage channels |
| Juvenile Glaucoma | Onset in children or adolescents; often familial |
🔹 IV. Risk Factors for Glaucoma:
✅ Age > 40 years
✅ Family history of glaucoma
✅ African or Asian ethnicity
✅ High myopia or hyperopia
✅ Diabetes, hypertension
✅ Use of steroids
✅ Thin central cornea
👁️⚕️ Types of Glaucoma
Glaucoma is broadly classified based on:
🔹 The anatomy of the anterior chamber angle (open vs. closed)
🔹 The cause (primary vs. secondary)
🔹 The age of onset (congenital, juvenile, adult)
🔹 The speed of onset (acute vs. chronic)
🔷 I. Primary Glaucomas (No identifiable external cause)
These occur without a pre-existing eye disease, usually due to genetic or anatomical predispositions.
🔹 1. Primary Open-Angle Glaucoma (POAG)
- Most common form
- Angle is open, but trabecular meshwork is functionally impaired, reducing aqueous humor outflow
- Painless, progressive loss of peripheral vision
- Typically bilateral, occurs after age 40
🔹 2. Primary Angle-Closure Glaucoma (PACG)
| Type | Features |
|---|---|
| Acute Angle-Closure Glaucoma | Sudden IOP rise due to pupil block; severe pain, red eye, nausea, halos |
| Chronic Angle-Closure Glaucoma | Gradual angle closure with peripheral anterior synechiae; asymptomatic until advanced |
| Intermittent Angle Closure | Occasional IOP spikes with transient blurring, halos |
➡️ Seen more in hyperopic (small eyes), elderly, Asian ethnicity, and females
🔹 3. Normal-Tension Glaucoma (NTG)
- Optic nerve damage and visual field loss occur despite normal IOP (<21 mmHg)
- Likely due to vascular insufficiency or optic nerve hypersensitivity
- Risk factors: migraine, hypotension, Raynaud’s phenomenon
🔷 II. Secondary Glaucomas (Resulting from other diseases or conditions)
These occur when another eye or systemic disorder interferes with aqueous humor dynamics.
🔹 A. Secondary Open-Angle Glaucomas
| Type | Description |
|---|---|
| Pseudoexfoliative Glaucoma | Flaky protein deposits block trabecular meshwork |
| Pigmentary Glaucoma | Iris pigment granules clog angle; more common in young myopic males |
| Steroid-induced Glaucoma | Long-term corticosteroid use increases IOP |
| Traumatic Glaucoma | Angle recession or damage post blunt trauma |
| Uveitic Glaucoma | Inflammatory debris blocks trabecular meshwork |
🔹 B. Secondary Angle-Closure Glaucomas
| Type | Description |
|---|---|
| Neovascular Glaucoma | New abnormal blood vessels (from diabetes or CRVO) block angle |
| Iridocorneal Endothelial (ICE) Syndrome | Endothelial proliferation causes angle closure |
| Epithelial Ingrowth | Rare post-surgical complication leading to angle blockage |
| Lens-induced Glaucoma | Due to hypermature cataract (phacomorphic/phacolytic) |
🔷 III. Developmental (Congenital and Juvenile) Glaucomas
🔹 1. Primary Congenital Glaucoma (PCG)
- Present at birth or in infancy
- Due to maldevelopment of trabecular meshwork
- Classic signs:
👁️ Buphthalmos (enlarged eyeball)
🌊 Tearing
🌞 Photophobia
💡 Corneal haze
🔹 2. Juvenile Open-Angle Glaucoma
- Occurs in children and adolescents (age 3–40)
- Resembles adult POAG but with more rapid progression
- Often genetic (e.g., MYOC gene mutation)
✅ Summary Table – Types of Glaucoma
| Type | Angle | Cause | Onset | Notes |
|---|---|---|---|---|
| Primary Open-Angle | Open | Unknown | Chronic | Most common, asymptomatic early |
| Angle-Closure (Acute) | Closed | Anatomical block | Sudden | Emergency, severe pain |
| Normal-Tension | Open | Vascular factors | Chronic | Normal IOP with nerve damage |
| Secondary (Trauma, Steroid, Uveitis) | Open/Closed | Underlying disease | Variable | Must treat the root cause |
| Neovascular | Closed | Retinal ischemia | Severe | Poor prognosis |
| Congenital | Variable | Developmental defect | Birth/infancy | Needs surgical correction |
| Juvenile | Open | Genetic | Early | Rapid progression |
👁️⚕️ Pathophysiology of Glaucoma
🔬 Overview:
Glaucoma is a group of eye diseases characterized by progressive damage to the optic nerve, often associated with increased intraocular pressure (IOP).
The optic nerve head (optic disc) is particularly vulnerable to mechanical compression and vascular insufficiency, leading to visual field loss.
🔁 Normal Aqueous Humor Dynamics:
- Aqueous humor is produced by the ciliary body → flows through the posterior chamber
- Passes through the pupil → enters the anterior chamber
- Drains via the trabecular meshwork into the Canal of Schlemm → into episcleral veins
⚠️ Disruption of This Flow → Raised IOP → Optic Nerve Damage
🔹 1. Primary Open-Angle Glaucoma (POAG) – Pathophysiology
| Feature | Description |
|---|---|
| Angle status | Anatomically open (anterior chamber angle remains open) |
| Pathology | Functional resistance to aqueous outflow due to changes in trabecular meshwork and Schlemm’s canal |
| IOP elevation | Gradual and chronic increase in IOP |
| Optic nerve damage | Increased IOP compresses lamina cribrosa, disrupting axoplasmic flow in retinal ganglion cells |
| Result | Cupping of optic disc and progressive peripheral vision loss |
🧠 Even when IOP is within normal limits (normal-tension glaucoma), vascular dysregulation can lead to the same optic nerve damage.
🔹 2. Primary Angle-Closure Glaucoma (PACG) – Pathophysiology
| Feature | Description |
|---|---|
| Angle status | Anatomically narrow or blocked |
| Pupil block mechanism | Iris bulges forward, closing angle and blocking aqueous outflow |
| Sudden IOP spike | Especially in acute angle-closure, can rise rapidly to >40 mmHg |
| Optic nerve ischemia | Due to sudden vascular compromise, leads to acute visual loss |
| Symptoms | Eye pain, redness, nausea, headache, halos around lights |
🔹 3. Secondary Glaucomas – Pathophysiology (Varies by Cause)
| Type | Mechanism |
|---|---|
| Neovascular glaucoma | New blood vessels block trabecular meshwork → closed angle |
| Uveitic glaucoma | Inflammatory debris and synechiae block outflow |
| Steroid-induced | Steroids alter trabecular cell function, increasing resistance |
| Pigmentary glaucoma | Iris pigment clogs outflow pathway |
| Traumatic glaucoma | Damage to angle structure (angle recession) impairs outflow |
🔹 4. Congenital Glaucoma – Pathophysiology
| Feature | Description |
|---|---|
| Cause | Developmental abnormality in trabecular meshwork and anterior chamber angle |
| Result | Ineffective drainage from birth |
| Symptoms | Buphthalmos (enlarged eye), tearing, corneal edema, photophobia |
🔁 Final Common Pathway in All Types of Glaucoma:
✅ Increased IOP (most common mechanism)
✅ ➡️ Compression of optic nerve fibers at lamina cribrosa
✅ ➡️ Interrupted axoplasmic flow in ganglion cells
✅ ➡️ Optic disc cupping and atrophy
✅ ➡️ Irreversible vision loss (starting with peripheral fields)
👁️⚕️ Glaucoma – Signs & Symptoms | Diagnosis
⚠️ I. Signs & Symptoms of Glaucoma
The clinical presentation of glaucoma varies depending on the type, rate of IOP increase, and extent of optic nerve damage.
🔹 A. Primary Open-Angle Glaucoma (POAG)
🔸 “Silent thief of sight” – slow and painless
| Symptom | Description |
|---|---|
| Painless, gradual loss of peripheral vision | Often goes unnoticed until advanced stage |
| Tunnel vision | In late stages |
| No redness or pain | Unlike angle-closure glaucoma |
| Frequent prescription changes | Vision not improving despite new glasses |
| Bilateral involvement | But often asymmetric progression |
🔍 Early stages are typically asymptomatic → routine eye screening is essential!
🔹 B. Primary Angle-Closure Glaucoma (PACG)
🔸 Acute and symptomatic – ophthalmic emergency!
| Symptom | Description |
|---|---|
| Sudden severe eye pain | Often with headache |
| Blurred vision | Due to corneal edema |
| Halos around lights | Especially at night |
| Redness of the eye | Conjunctival congestion |
| Nausea and vomiting | Due to vagal stimulation |
| Fixed mid-dilated pupil | Non-reactive to light |
| Markedly elevated IOP | May exceed 40–60 mmHg |
🔹 C. Congenital Glaucoma
| Symptom | Description |
|---|---|
| Excessive tearing (epiphora) | Due to increased pressure |
| Photophobia | Child avoids light |
| Enlarged eyeball (buphthalmos) | Stretching of sclera and cornea |
| Cloudy or hazy cornea | From edema |
| Poor visual fixation | Indicates vision impairment |
🧪 II. Diagnosis of Glaucoma
Diagnosis requires clinical evaluation, IOP measurement, and optic nerve imaging to detect structural and functional changes.
🩺 1. Intraocular Pressure Measurement (Tonometry)
- Normal IOP: 10–21 mmHg
- Elevated in most glaucomas (not always in NTG)
- Goldmann applanation tonometer is the gold standard
🔬 2. Gonioscopy
- Evaluates the anterior chamber angle
- Differentiates open-angle vs. angle-closure glaucoma
🔍 3. Ophthalmoscopy (Fundus Examination)
- Assesses optic nerve head (optic disc)
| Finding | Meaning |
|---|---|
| Increased cup-to-disc ratio | >0.6 is suspicious |
| Disc notching | Sign of glaucomatous damage |
| Pallor of the optic disc | Indicates atrophy |
🎯 4. Visual Field Testing (Perimetry)
- Detects functional visual field defects
- Typical in glaucoma:
- Paracentral scotoma
- Nasal step
- Arcuate scotoma
- Tunnel vision (late stage)
🖥️ 5. Optical Coherence Tomography (OCT)
- Measures retinal nerve fiber layer (RNFL) thickness
- Detects early glaucomatous changes even before visual field loss
🔁 6. Pachymetry
- Measures corneal thickness
- Important for interpreting IOP values accurately
✅ Summary Table: Signs & Diagnosis
| Type | Symptoms | Diagnostic Tools |
|---|---|---|
| POAG | Gradual, painless peripheral vision loss | IOP, perimetry, fundus exam, OCT |
| PACG (Acute) | Severe eye pain, halos, nausea, red eye | IOP (↑↑), gonioscopy, slit-lamp |
| Congenital | Tearing, photophobia, buphthalmos | IOP, corneal diameter, B-scan |
💊 I. Medical Management of Glaucoma
🎯 Goals of Medical Treatment:
- Lower intraocular pressure (IOP) to prevent or slow optic nerve damage
- Maintain visual function
- Improve aqueous outflow or reduce aqueous production
🔹 1. First-Line Medications (Eye Drops)
| Drug Class | Examples | Mechanism | Notes |
|---|---|---|---|
| Prostaglandin analogs | Latanoprost, Travoprost, Bimatoprost | ↑ Uveoscleral outflow | Once daily; most effective IOP-lowering |
| Beta-blockers | Timolol, Betaxolol | ↓ Aqueous humor production | Avoid in asthma/COPD patients |
| Alpha-agonists | Brimonidine, Apraclonidine | ↓ Production & ↑ Outflow | May cause allergic conjunctivitis |
| Carbonic anhydrase inhibitors (CAIs) | Dorzolamide (topical), Acetazolamide (oral) | ↓ Aqueous humor production | Oral form for acute IOP spike |
| Rho kinase inhibitors | Netarsudil | ↑ Trabecular outflow | Newer class |
🔹 2. Hyperosmotic Agents (Used in Acute Angle Closure)
- Mannitol IV
- Glycerol PO
➡️ Used in emergencies to rapidly lower IOP by drawing fluid from the eye
🔹 3. Miotics (Pilocarpine)
- ↑ Trabecular outflow by contracting ciliary muscle
- Mainly used in acute angle-closure
⚠️ Side effects: brow ache, blurred vision, miosis
🔹 4. Systemic Management
- Control underlying conditions: Diabetes, hypertension, thyroid eye disease
- Monitor for drug interactions and compliance issues
🧪 Monitoring During Medical Treatment:
- Regular IOP checks
- Monitor optic nerve head with OCT/fundus exam
- Visual field testing every 6–12 months
- Educate patients on adherence to drops
🔪 II. Surgical Management of Glaucoma
Surgical intervention is considered when:
- Medical therapy is ineffective or poorly tolerated
- There is rapid progression despite controlled IOP
- In acute angle-closure crises or congenital glaucoma
🔹 1. Laser Procedures
A. Laser Trabeculoplasty (for POAG)
- Types: Argon Laser Trabeculoplasty (ALT) or Selective Laser Trabeculoplasty (SLT)
- Enhances aqueous outflow through trabecular meshwork
- Outpatient, quick recovery
B. Laser Peripheral Iridotomy (LPI) (for PACG)
- Creates a small hole in peripheral iris to relieve pupil block
- First-line treatment for acute angle-closure and prophylaxis in fellow eye
C. Cyclophotocoagulation (for refractory glaucoma)
- Laser applied to ciliary body to reduce aqueous production
- Used in advanced or painful blind eyes
🔹 2. Incisional Surgeries
A. Trabeculectomy
- Gold standard surgical procedure for POAG
- A fistula is created from anterior chamber to subconjunctival space
- Forms a bleb through which aqueous drains
B. Glaucoma Drainage Devices (Tubes or Shunts)
- Used when trabeculectomy fails or in neovascular, uveitic glaucoma
- Example: Ahmed Valve, Baerveldt implant
C. Minimally Invasive Glaucoma Surgeries (MIGS)
- Safer, quicker recovery, less IOP lowering
- Examples: iStent, Hydrus Microstent
- Suitable for mild-to-moderate glaucoma, often combined with cataract surgery
D. Goniotomy/Trabeculotomy (for Congenital Glaucoma)
- Incision made in trabecular meshwork to open the angle
- Performed under general anesthesia in infants and young children
✅ Summary Table – Management at a Glance
| Type | Medical Treatment | Surgical Option |
|---|---|---|
| POAG | Eye drops (1st line) | Trabeculectomy, SLT |
| PACG (Acute) | Mannitol, pilocarpine, IOP-lowering drops | Laser iridotomy (urgent) |
| Normal-Tension | Neuroprotection, mild IOP reduction | Rarely surgical |
| Neovascular | Anti-VEGF, CAIs, beta-blockers | Tube shunt, cyclophotocoagulation |
| Congenital | Often resistant to drops | Goniotomy, trabeculotomy |
👩⚕️👁️🦠 Nursing Management of Glaucoma
🎯 Objectives of Nursing Care:
✔️ Prevent further optic nerve damage and vision loss
✔️ Ensure adherence to treatment regimen
✔️ Support IOP control through medication or surgical care
✔️ Provide preoperative and postoperative care
✔️ Educate patient and family on lifestyle modifications, eye care, and follow-up
📋 I. Assessment Phase
🔍 Subjective Assessment:
- Ask about eye discomfort, vision changes, halos, headache
- Inquire about medication use and compliance
- Assess patient understanding of glaucoma and eye care routines
🔬 Objective Assessment:
- Monitor for:
- Redness, cloudiness, or corneal haziness
- Pupil shape, reaction to light, or visual field constriction
- Post-op: eye patch integrity, drainage, and vital signs
💊 II. Nursing Interventions
🔹 1. Medication Administration & Monitoring
| Task | Nursing Action |
|---|---|
| Eye drop instillation | Administer as prescribed (e.g., beta-blockers, prostaglandins, CAIs) using aseptic technique |
| Patient positioning | Tilt head back, pull down lower lid, avoid touching dropper tip |
| Punctal occlusion | Apply gentle pressure to the inner canthus for 1–2 minutes after drop instillation to reduce systemic absorption |
| Monitor for side effects | E.g., bradycardia (beta-blockers), stinging (prostaglandins), fatigue (CAIs) |
| Encourage compliance | Use reminder charts or alarms; explain that glaucoma requires lifelong therapy |
🔹 2. Preoperative Nursing Care (if surgery planned)
- Educate patient about the procedure (laser or trabeculectomy)
- Ensure patient receives pre-op eye drops (e.g., miotics or antibiotics)
- NPO if required, check consent, assist with psychological preparation
- Monitor BP, blood sugar, coagulation status if patient has comorbidities
🔹 3. Postoperative Nursing Care
| Task | Nursing Action |
|---|---|
| Eye protection | Ensure use of eye shield, especially at night |
| Positioning | Keep head elevated (semi-Fowler’s) to reduce IOP |
| Activity restriction | Avoid bending, straining, lifting, or rubbing eyes |
| Pain control | Administer prescribed analgesics and cold compresses if needed |
| Monitor for complications | Redness, purulent discharge, sudden pain, decreased vision → report immediately |
🔹 4. Patient Education & Counseling
| Topic | Key Instructions |
|---|---|
| Lifelong nature of glaucoma | It cannot be cured, only controlled |
| Importance of follow-up | Regular IOP checks and optic nerve evaluations |
| Correct eye drop technique | Demonstrate and have patient return-demonstrate |
| Avoiding self-medication | Especially steroid eye drops (can worsen IOP) |
| Lifestyle tips | Avoid tight collars, heavy lifting, smoking; manage diabetes and BP |
| Family screening | Encourage screening for first-degree relatives (hereditary risk) |
🧾 III. Sample Nursing Diagnoses
- Disturbed sensory perception (visual) related to optic nerve damage
- Deficient knowledge regarding disease condition and treatment regimen
- Risk for noncompliance related to long-term therapy and asymptomatic early phase
- Anxiety related to potential vision loss or surgical intervention
- Risk for injury due to impaired peripheral vision and depth perception
✅ IV. Evaluation Criteria
- Patient demonstrates correct eye drop technique and understands dosage schedule
- IOP is maintained within target range
- No postoperative complications or vision worsening
- Patient reports reduction in anxiety and increased awareness
- Family members are informed about hereditary risk and screening
🥗 I. Nutritional Considerations in Glaucoma
While nutrition cannot cure glaucoma, a healthy diet can:
✅ Support optic nerve health
✅ Reduce oxidative stress and inflammation
✅ Promote vascular health, especially in normal-tension glaucoma
✅ Aid in overall eye and systemic wellness
✅ Key Nutrients for Glaucoma Management
| Nutrient | Function | Sources |
|---|---|---|
| Vitamin A | Maintains epithelial and retinal health | Carrots, spinach, sweet potatoes |
| Vitamin C | Antioxidant, improves ocular circulation | Citrus fruits, strawberries, broccoli |
| Vitamin E | Protects cells from oxidative damage | Almonds, sunflower seeds, avocado |
| Omega-3 Fatty Acids | Supports blood flow to optic nerve | Salmon, walnuts, flaxseeds |
| Zinc | Helps enzyme function in the eye | Pumpkin seeds, legumes, whole grains |
| Lutein & Zeaxanthin | Concentrated in the eye; protect from light damage | Kale, spinach, corn, egg yolk |
| Magnesium | Enhances blood flow to optic nerve | Bananas, legumes, dark chocolate |
⚠️ Foods to Limit:
- Caffeine in excess: Can temporarily raise IOP
- High-sodium foods: May increase fluid retention and IOP
- Trans fats: Promote inflammation and vascular constriction
- Sugar-laden foods: May worsen diabetic control in diabetic glaucoma
⚠️ II. Complications of Glaucoma
Untreated or poorly controlled glaucoma can lead to:
🔹 1. Irreversible Vision Loss
- Permanent damage to optic nerve fibers → tunnel vision → total blindness
🔹 2. Acute Angle-Closure Crisis
- Ophthalmic emergency
- Sudden rise in IOP may cause:
- Severe eye pain
- Nausea/vomiting
- Loss of vision within hours if untreated
🔹 3. Ocular Surface Damage
- Long-term use of multiple topical medications can lead to:
- Dry eye syndrome
- Conjunctival inflammation
🔹 4. Postoperative Complications
| Complication | Description |
|---|---|
| Bleb infection (blebitis) | After trabeculectomy |
| Hyphema | Blood in anterior chamber post-surgery |
| Endophthalmitis | Serious intraocular infection |
| IOL displacement | Especially in combined cataract + glaucoma surgery |
| Failure of drainage implant | Requires revision or repeat surgery |
📌 III. Key Points (Quick Revision)
✔️ Glaucoma is a chronic optic nerve disease, often associated with elevated intraocular pressure (IOP)
✔️ It leads to progressive, irreversible peripheral vision loss
✔️ Types:
- Primary Open-Angle (most common, painless, slow)
- Primary Angle-Closure (acute, painful, emergency)
- Normal-Tension, Secondary, and Congenital forms exist
✔️ Early stages are asymptomatic, hence routine eye screening (especially after 40 years) is vital
✔️ Diagnosis: IOP measurement, optic disc assessment, perimetry, OCT
✔️ Medical management: Eye drops to reduce IOP, oral CAIs, emergency use of mannitol/glycerol
✔️ Surgical management: Laser (SLT, iridotomy), trabeculectomy, tube shunts, MIGS
✔️ Nursing care includes:
- Drop administration
- Pre- and post-op care
- Patient and family education
- Lifestyle guidance
✔️ Nutrition rich in antioxidants, omega-3s, and lutein supports optic nerve health
✔️ Complications include vision loss, acute angle closure, ocular surface disease, and surgical risks..
👁️⚕️ Retinal Detachment.
📘 Definition:
Retinal detachment is a sight-threatening condition in which the neurosensory retina separates from the underlying retinal pigment epithelium (RPE).
This disrupts blood and nutrient supply to the retina and can lead to permanent vision loss if not treated promptly.
🛑 It is considered a medical emergency requiring immediate ophthalmic intervention.
🔍 Causes of Retinal Detachment:
Retinal detachment usually results from retinal breaks, tractional forces, or fluid accumulation under the retina.
🔹 1. Mechanical or Structural Causes
- Retinal tears or holes due to posterior vitreous detachment (PVD)
- Aging-related degeneration of the vitreous body
🔹 2. Traumatic Causes
- Blunt or penetrating ocular trauma
- Head injury with rapid acceleration-deceleration
- Post-surgical trauma (e.g., after cataract surgery)
🔹 3. Inflammatory or Exudative Causes
- Severe inflammatory conditions (e.g., uveitis, scleritis)
- Tumors (choroidal melanoma)
- Systemic diseases like hypertension, lupus
🔹 4. Vascular Causes
- Proliferative diabetic retinopathy (PDR)
- Retinopathy of prematurity (ROP)
- Sickle cell retinopathy
🔹 5. Risk Factors
- Age > 50 years
- High myopia (long eyeball)
- Family history of retinal detachment
- Lattice degeneration of retina
- Previous eye surgery (esp. cataract extraction)
- Diabetic eye disease
- Ocular inflammation
🔢 Types of Retinal Detachment
Retinal detachment is classified into three main types, based on the underlying mechanism:
🔸 1. Rhegmatogenous Retinal Detachment (RRD)
(Most common type)
Definition:
Occurs due to a break or tear in the retina, allowing liquefied vitreous humor to seep between the retina and RPE.
Mechanism:
- Posterior vitreous detachment (PVD) pulls on the retina
- A tear or hole forms → fluid accumulates beneath retina
- The retina lifts away from the RPE
Risk factors: Myopia, aging, trauma, retinal thinning (lattice degeneration)
🔸 2. Tractional Retinal Detachment (TRD)
Definition:
Caused by fibrous or fibrovascular membranes on the retinal surface pulling the retina away from the RPE.
Mechanism:
- Seen in proliferative diabetic retinopathy, sickle cell disease, retinopathy of prematurity
- Scar tissue contracts and pulls on retina
- No retinal break is needed
🔸 3. Exudative (Serous) Retinal Detachment
Definition:
Occurs due to accumulation of subretinal fluid without any retinal tear or traction.
Mechanism:
- Caused by inflammatory, neoplastic, or vascular conditions
- Fluid leaks from choroidal circulation into subretinal space
Common causes:
- Choroidal tumors
- Vogt–Koyanagi–Harada syndrome
- Severe hypertensive retinopathy
✅ Quick Summary Table – Types of Retinal Detachment
| Type | Mechanism | Retinal Tear? | Common Causes |
|---|---|---|---|
| Rhegmatogenous | Retinal tear + fluid entry | ✅ Yes | Aging, myopia, trauma |
| Tractional | Membrane pulls retina | ❌ No | Diabetic retinopathy, sickle cell |
| Exudative | Fluid leaks under retina | ❌ No | Tumors, inflammation, vascular disorders |
🔬 I. Pathophysiology of Retinal Detachment
Retinal detachment occurs when the sensory (neurosensory) retina separates from the retinal pigment epithelium (RPE), disrupting the retina’s nutrient supply and leading to retinal ischemia and cell death if untreated.
🔹 A. Rhegmatogenous Retinal Detachment (Most Common)
- Vitreous liquefaction occurs with aging → posterior vitreous detachment (PVD)
- PVD exerts traction on the retina → causes a tear or hole
- Liquefied vitreous humor enters through the break
- Fluid collects between retina and RPE, lifting the retina
- Detached retina becomes ischemic, leading to photoreceptor degeneration
🔹 B. Tractional Retinal Detachment
- Fibrovascular membranes (e.g., from diabetes) contract
- This pulls the retina away from the RPE without a tear
- Chronic traction leads to retinal ischemia and loss of function
🔹 C. Exudative Retinal Detachment
- Inflammatory or vascular disease causes fluid to leak into the subretinal space
- No tear or traction present
- Retinal detachment is due to fluid accumulation under the retina
🔁 Final Consequence (All Types):
✅ Separation of retina from RPE
✅ Disruption of photoreceptor metabolism
✅ Retinal ischemia → photoreceptor cell death
✅ Permanent vision loss if not treated promptly
⚠️ II. Signs and Symptoms of Retinal Detachment
Symptoms depend on the extent, location, and type of detachment.
🚨 Early Warning Signs (All Types):
| Symptom | Description |
|---|---|
| Photopsia (flashes of light) | Sudden brief flashes, especially in peripheral vision |
| Floaters | Black spots or cobweb-like shadows in the visual field |
| Blurred or distorted vision | Due to retinal separation from the visual axis |
| Shadow or curtain over vision | Classic symptom; described as a gray curtain moving across the field of view |
| Reduced peripheral vision | Progressive constriction of the visual field |
| Sudden vision loss | If macula is involved (central retina) or large area detaches |
🔍 Symptoms by Type:
| Type | Symptoms |
|---|---|
| Rhegmatogenous | Flashes, floaters, curtain over vision |
| Tractional | Often painless and gradual vision loss (esp. in diabetics) |
| Exudative | No flashes or floaters, but blurry or distorted vision with possible metamorphopsia |
🧪 III. Diagnosis of Retinal Detachment
Diagnosis involves clinical evaluation, ophthalmoscopic examination, and imaging studies.
🔹 1. Visual Acuity Test
- Decreased acuity if the macula is detached
🔹 2. Slit-Lamp Examination + Indirect Ophthalmoscopy
- Gold standard for diagnosis
- Reveals:
- Retinal breaks or tears
- Detached, billowing retina
- Pigment cells in vitreous (“tobacco dust” or Shafer’s sign – indicates RRD)
🔹 3. B-scan Ocular Ultrasound
- Used when fundus view is obscured (e.g., dense cataract or vitreous hemorrhage)
- Confirms retinal elevation and mobility
🔹 4. Optical Coherence Tomography (OCT)
- High-resolution scan to detect subretinal fluid
- Useful in macular or subtle detachments (esp. exudative)
🔹 5. Fundus Fluorescein Angiography (FFA)
- Helpful in exudative detachment
- Shows leakage from choroidal vessels or tumors
✅ Quick Summary Table
| Aspect | Findings |
|---|---|
| Symptoms | Flashes, floaters, shadow over vision, reduced peripheral vision |
| Slit-lamp/Indirect ophthalmoscopy | Detached retina, retinal tear, Shafer’s sign |
| B-scan | Confirms RD when fundus is not visible |
| OCT | Detects macular involvement or exudative RD |
| FFA | Used for inflammatory/tumor-related RD |
💊 I. Medical Management of Retinal Detachment
Medical (non-surgical) treatment is limited in retinal detachment. However, it plays a role in:
✅ Stabilizing the patient before surgery
✅ Managing associated risk factors and symptoms
✅ Preventing progression in early retinal tears (pre-detachment stage)
🔹 1. Retinal Tear (No Detachment Yet) – Preventive Treatment
- Laser photocoagulation or cryotherapy (see surgical section) is used to seal the tear before fluid accumulates underneath
- Advised bed rest and limited physical activity if detachment is minimal or pending surgery
🔹 2. Symptom Control & Supportive Care
| Purpose | Management |
|---|---|
| Inflammation control | Topical or systemic corticosteroids (in exudative RD or uveitis) |
| Intraocular pressure (IOP) control | Anti-glaucoma drops if IOP is high |
| Systemic control | Manage diabetes, hypertension, autoimmune disorders |
| Positioning | Head positioning may help in some detachments (especially post-op gas tamponade) |
⚠️ Medical management alone cannot reattach a detached retina. Prompt surgical intervention is essential to restore vision.
🔪 II. Surgical Management of Retinal Detachment
Surgical treatment depends on:
🔹 Type of detachment
🔹 Extent and location
🔹 Patient’s eye condition (e.g., lens status, previous surgeries)
🔹 1. Laser Photocoagulation (for Retinal Tear or Small Detachment)
- Uses a laser to create thermal burns around the retinal tear
- Produces scar tissue that seals the edges and prevents fluid seepage
- Outpatient, painless, often done before detachment develops
🔹 2. Cryopexy (Cryotherapy)
- Freezing probe applied to external sclera to seal retinal breaks
- Often used in conjunction with scleral buckling or gas tamponade
🔹 3. Pneumatic Retinopexy
✅ Minimally invasive; for small, uncomplicated retinal detachments
| Step | Description |
|---|---|
| Gas bubble injection | Inject a gas (SF6 or C3F8) into the vitreous cavity |
| Head positioning | Patient keeps head in a specific position to press bubble over tear |
| Laser or cryotherapy | Then used to seal the break after reattachment |
🧠 Requires strict posturing for several days!
🔹 4. Scleral Buckling Surgery
✅ Used for rhegmatogenous RD with larger or multiple tears
| Step | Description |
|---|---|
| Silicone band | Placed around the eye (under conjunctiva) |
| Indentation | Band pushes eye wall inward toward retina |
| Drainage of fluid | May be done if detachment is large |
| Cryopexy/laser | Used to seal breaks during surgery |
📌 Often performed under local or general anesthesia.
🔹 5. Pars Plana Vitrectomy (PPV)
✅ Preferred for complex, large, or tractional retinal detachments
| Step | Description |
|---|---|
| Removal of vitreous | Eliminates traction on retina |
| Membrane peeling | In TRD, fibrovascular tissue is removed |
| Retinal reattachment | Retina is flattened and laser or cryo used to seal breaks |
| Tamponade | Gas or silicone oil is injected to hold retina in place |
🧠 Silicone oil may need removal after weeks/months.
🧾 Postoperative Care (All Surgeries):
- Topical antibiotics and steroids to prevent infection/inflammation
- Strict head positioning (especially after gas injection)
- Avoid:
- Air travel or high altitude if gas is inside the eye
- Heavy lifting, bending, eye rubbing
✅ Summary Table – Surgical Options
| Surgery | Indication | Key Features |
|---|---|---|
| Laser Photocoagulation | Retinal tear (no detachment) | Preventive; outpatient |
| Pneumatic Retinopexy | Small, superior RDs | Gas bubble + posture |
| Scleral Buckling | Rhegmatogenous RD | External band; pushes retina |
| Vitrectomy | Large, tractional, or complex RD | Removes vitreous, internal repair |
| Cryotherapy | Supplement to others | Freezes and seals retinal break |
👩⚕️👁️ Nursing Management of Retinal Detachment
🎯 Objectives of Nursing Care:
✔️ Prevent further retinal damage or detachment
✔️ Support the patient through surgical treatment and recovery
✔️ Promote healing and restore visual function
✔️ Educate the patient and family for long-term eye health and safety
✔️ Monitor for complications and ensure timely intervention
📋 I. Preoperative Nursing Management
🔹 1. Assessment
- Obtain history of flashes, floaters, visual field loss
- Assess visual acuity and extent of peripheral vision loss
- Check for medical comorbidities (diabetes, hypertension)
- Ensure informed consent and allergy status is reviewed
🔹 2. Patient Preparation
- Restrict activity to minimize further retinal detachment
- Explain the importance of eye rest and reduced head movement
- Administer prescribed pre-op eye drops (e.g., mydriatics, antibiotics)
- Maintain NPO status if surgery under general anesthesia
- Provide emotional reassurance and reduce anxiety about surgery
🏥 II. Postoperative Nursing Management
🔹 1. Positioning Care
- Strict head positioning is vital (especially after pneumatic retinopexy)
- E.g., face-down or side-lying, depending on tear location
- Ensures the gas bubble or silicone tamponade remains in correct position
🔹 2. Eye Care
- Apply eye shield to prevent injury
- Administer eye drops as prescribed:
- Antibiotics (infection prevention)
- Steroids/NSAIDs (reduce inflammation)
- Cycloplegics (relieve pain/spasm)
🔹 3. Activity Restriction
- Instruct to avoid bending, lifting heavy objects, or sudden head movement
- Avoid straining, coughing, or sneezing forcefully
- No rubbing of eyes or water entry during the first week
🔹 4. Pain and Symptom Monitoring
- Monitor for:
- Severe pain, increased redness
- Sudden decrease in vision or new floaters
- Signs of infection (discharge, swelling, fever)
- Administer prescribed analgesics if discomfort occurs
🔹 5. Patient Education
| Topic | Teaching Tips |
|---|---|
| Medication adherence | Show drop instillation technique; explain schedule |
| Eye protection | Wear eye shield at night and when outdoors |
| Signs of complications | Pain, loss of vision, flashes – report immediately |
| Diet and hydration | Normal unless otherwise advised |
| Gas bubble alert | Avoid air travel or high altitudes until gas is absorbed (usually 2–8 weeks) |
🧾 III. Rehabilitation & Follow-Up
- Encourage gradual return to normal activity after 4–6 weeks
- Assist in low-vision aids or occupational therapy if vision is permanently reduced
- Reinforce follow-up appointments for:
- Visual acuity testing
- Intraocular pressure monitoring
- Retinal examination
- Possible silicone oil removal if used
✅ IV. Sample Nursing Diagnoses
- Disturbed sensory perception (visual) related to retinal separation
- Risk for injury related to visual impairment post-surgery
- Acute pain related to surgical intervention or inflammation
- Deficient knowledge regarding home care, medication, and follow-up
- Anxiety related to fear of vision loss or surgery outcome
🎯 Evaluation Criteria
- Patient maintains correct posture and eye protection
- Eye remains free from infection, excessive swelling, or pain
- Vision is preserved or gradually improving post-surgery
- Patient demonstrates correct medication use and reports any warning signs
- Patient attends all follow-up visits and understands activity restrictions
🥗 I. Nutritional Considerations
While nutrition cannot reverse a retinal detachment, it plays a supportive role in retinal health, recovery, and the prevention of further retinal degeneration, especially in high-risk individuals (e.g., diabetics, elderly, or highly myopic patients).
✅ Essential Nutrients for Eye and Retinal Health
| Nutrient | Role | Sources |
|---|---|---|
| Vitamin A | Maintains photoreceptor function and vision in dim light | Carrots, sweet potatoes, spinach |
| Vitamin C | Antioxidant; supports collagen in eye tissues and blood vessels | Citrus fruits, guava, kiwi |
| Vitamin E | Protects photoreceptors from oxidative damage | Almonds, sunflower seeds, avocados |
| Lutein & Zeaxanthin | Carotenoids that filter harmful light and reduce oxidative stress in retina | Kale, spinach, corn, egg yolk |
| Zinc | Assists in Vitamin A transport and retinal enzyme activity | Pumpkin seeds, lentils, red meat |
| Omega-3 Fatty Acids | Anti-inflammatory; supports retinal and macular health | Fatty fish (salmon, sardines), flaxseed, walnuts |
| Protein | Needed for tissue repair post-surgery | Eggs, lean meat, dairy, legumes |
💡 Dietary Tips Post-Surgery:
- Encourage small, frequent, nutrient-rich meals
- Maintain good hydration
- If prone-positioning is required (as in gas tamponade), suggest soft foods or meals that are easy to eat in that position
- Avoid caffeine and high sodium if IOP is a concern
- Ensure blood glucose is controlled in diabetic patients to avoid post-op complications
⚠️ II. Complications of Retinal Detachment
If untreated or if surgical recovery is not properly managed, retinal detachment can lead to serious complications.
🧠 A. Visual Complications
| Complication | Description |
|---|---|
| Permanent vision loss | Especially if macula is involved or surgery is delayed |
| Macular pucker | Scar tissue forms on macula causing distortion |
| Recurrent retinal detachment | Due to new tears or inadequate reattachment |
| Vitreous hemorrhage | Bleeding into vitreous cavity; obscures vision |
| Photoreceptor cell death | From prolonged retinal separation; irreversible |
🧪 B. Postoperative Complications
| Complication | Description |
|---|---|
| Infection (Endophthalmitis) | Rare but sight-threatening intraocular infection |
| Increased intraocular pressure (IOP) | From gas, silicone oil, or steroid use |
| Cataract formation | Common after vitrectomy |
| Retinal scarring or fibrosis | Leads to traction and redetachment |
| Silicone oil complications | Emulsification, corneal toxicity if not removed timely |
📌 III. Key Points (Quick Revision)
✔️ Retinal detachment is a medical emergency where the neurosensory retina separates from the RPE, leading to vision loss
✔️ Common symptoms: flashes, floaters, and a curtain-like shadow
✔️ Types:
- Rhegmatogenous (tear + fluid entry)
- Tractional (pull from fibrovascular tissue)
- Exudative (fluid leak from inflammation/tumors)
✔️ Diagnosis involves slit-lamp exam, indirect ophthalmoscopy, B-scan, and OCT
✔️ Surgical management is essential:
- Laser photocoagulation
- Cryopexy
- Pneumatic retinopexy
- Scleral buckle
- Vitrectomy
✔️ Nursing care includes:
- Eye drop instillation
- Positioning (esp. post gas-bubble procedures)
- Monitoring for signs of complications
- Patient education on lifestyle changes and follow-up
✔️ Nutrition rich in antioxidants, carotenoids, omega-3s, and vitamins A, C, E supports retinal health and surgical healing
✔️ Complications include vision loss, recurrence, infection, cataract, and macular problems…
👁️⚕️ Blindness.
📘 Definition:
Blindness refers to a condition where there is complete or significant loss of vision, rendering a person unable to perform daily activities requiring sight, even with corrective measures like glasses or surgery.
🧠 According to the World Health Organization (WHO):
- Blindness is defined as: “Visual acuity less than 3/60 (or 20/400) in the better eye with best possible correction or a visual field of less than 10 degrees from fixation.”
This means the person can only see at 3 meters what a normal person can see at 60 meters.
📊 Legal Definitions of Blindness (India – RPwD Act, 2016):
According to Indian standards:
- Total absence of sight, or
- Visual acuity not exceeding 3/60 (20/400) in the better eye with correcting lenses, or
- Limitation of the field of vision subtending an angle of less than 10 degrees
🔍 Causes of Blindness
Blindness can result from congenital, acquired, or preventable causes affecting the eye or the visual pathway.
🔹 1. Congenital Causes (present at birth)
| Cause | Description |
|---|---|
| Congenital cataract | Clouding of lens from birth |
| Congenital glaucoma | Raised IOP damaging optic nerve |
| Retinopathy of prematurity (ROP) | In premature babies exposed to high oxygen |
| Inherited retinal dystrophies | E.g., Leber’s congenital amaurosis |
| Microphthalmos/anophthalmos | Small or absent eyeball |
🔹 2. Acquired Causes
| Cause | Description |
|---|---|
| Trachoma | Chronic chlamydial infection causing scarring |
| Cataract | Clouding of lens (most common cause worldwide) |
| Glaucoma | Increased IOP leading to optic nerve damage |
| Diabetic retinopathy | Retinal damage due to diabetes |
| Age-related macular degeneration (AMD) | Central vision loss in elderly |
| Corneal opacity | From infections (keratitis), trauma, ulcers |
| Retinal detachment | Separation of retina leading to sudden vision loss |
| Onchocerciasis (river blindness) | Parasitic infection in endemic areas (Africa) |
| Trauma | Mechanical, chemical, or radiation injury |
| Vitamin A deficiency | Causes xerophthalmia and corneal ulcers in children |
🔹 3. Neurological Causes
| Cause | Description |
|---|---|
| Optic neuritis | Inflammation of optic nerve (e.g., multiple sclerosis) |
| Brain tumors/stroke | Affecting visual cortex or pathways |
| Head injury | Damage to optic nerve or brain |
🔢 Types of Blindness
Blindness is classified based on severity, onset, duration, and cause.
🔸 1. Based on Severity:
| Type | Visual Acuity | Description |
|---|---|---|
| Total blindness | No perception of light (NPL) | Complete absence of vision |
| Partial blindness | Some vision remains | Can perceive light or shapes |
| Low vision | VA < 6/18 but ≥ 3/60 | Can use aids or magnifiers |
| Legal blindness | VA < 3/60 or VF < 10° | Recognized for disability benefits |
🔸 2. Based on Onset:
| Type | Description |
|---|---|
| Congenital blindness | Present at birth |
| Developmental blindness | Occurs in early childhood |
| Acquired blindness | Occurs later due to disease or injury |
🔸 3. Based on Duration:
| Type | Description |
|---|---|
| Temporary blindness | Reversible (e.g., due to corneal edema, trauma) |
| Permanent blindness | Irreversible vision loss |
| Progressive blindness | Vision deteriorates gradually (e.g., glaucoma) |
| Sudden blindness | Acute loss (e.g., retinal artery occlusion, trauma) |
🔸 4. Based on Cause:
| Type | Example |
|---|---|
| Corneal blindness | Infections, vitamin A deficiency, trauma |
| Lens-related blindness | Cataract |
| Retinal blindness | Diabetic retinopathy, AMD |
| Neurogenic blindness | Optic neuritis, brain injury |
| Cortical blindness | Visual cortex damage from stroke/tumor |
🔬 I. Pathophysiology of Blindness
Blindness results from disruption or damage at any point along the visual pathway, including the eye, optic nerve, or visual cortex.
🔁 Normal Visual Pathway:
- Light enters the cornea → passes through aqueous humor, lens, and vitreous
- Focuses on the retina, stimulating photoreceptors (rods and cones)
- Nerve impulses are transmitted via optic nerve → optic chiasm → optic tracts
- Signals are processed in the occipital lobe (visual cortex)
❌ Pathological Disruptions That Lead to Blindness:
| Site of Damage | Mechanism |
|---|---|
| Cornea | Scarring or opacity blocks light (e.g., trauma, infection) |
| Lens | Cataract causes blurred, dimmed vision |
| Retina | Photoreceptor or retinal detachment causes image loss |
| Optic nerve | Compression (tumor), ischemia (glaucoma), or inflammation (optic neuritis) disrupt signal transmission |
| Visual cortex | Stroke, tumors, or trauma to occipital lobe cause cortical blindness |
➡️ If the macula is affected → central vision loss
➡️ If the optic nerve is compressed or inflamed → complete or partial field loss
🔁 Common Pathophysiological Mechanisms:
- Ischemia: In diabetic retinopathy, retinal artery occlusion
- Degeneration: In retinitis pigmentosa, AMD
- Increased intraocular pressure: In glaucoma
- Neuronal loss: In optic neuropathies
- Infections/inflammation: In uveitis, keratitis
- Deficiency-related: Vitamin A deficiency → xerophthalmia → corneal melt
⚠️ II. Signs & Symptoms of Blindness
Symptoms vary depending on the cause, location of the damage, and severity of vision loss.
🔹 Early/Gradual Symptoms:
| Symptom | Cause |
|---|---|
| Blurry or dim vision | Cataract, diabetic retinopathy |
| Loss of peripheral vision | Glaucoma |
| Difficulty seeing at night (nyctalopia) | Retinitis pigmentosa, vitamin A deficiency |
| Distorted or wavy vision (metamorphopsia) | Macular degeneration |
| Frequent changes in glasses | Diabetic eye disease |
🔹 Sudden or Acute Symptoms:
| Symptom | Cause |
|---|---|
| Sudden vision loss in one eye | Retinal artery occlusion, optic neuritis |
| Flashes of light and floaters | Retinal detachment |
| Complete loss of light perception | Advanced glaucoma, trauma |
| Loss of central vision | Age-related macular degeneration |
| Visual hallucinations (in total blindness) | Charles Bonnet syndrome |
🔹 Congenital or Childhood Symptoms:
| Observation | Suggestive of |
|---|---|
| No eye contact / poor tracking | Congenital blindness |
| Frequent eye poking or pressing | Leber’s congenital amaurosis |
| White pupil (leukocoria) | Congenital cataract, retinoblastoma |
| Nystagmus | Early-onset blindness or optic nerve disorders |
🧪 III. Diagnosis of Blindness
Diagnosis includes visual acuity testing, eye examination, and imaging to identify the underlying cause.
🔹 1. Visual Acuity Testing (Snellen’s Chart)
- Measures sharpness of vision
- Legal blindness: Best-corrected visual acuity <3/60 (20/400) in better eye
🔹 2. Visual Field Testing (Perimetry)
- Assesses peripheral vision loss
- Useful in glaucoma, optic nerve disorders, and neurological causes
🔹 3. Slit-Lamp Examination
- Detects corneal opacities, cataracts, uveitis, and anterior segment disease
🔹 4. Fundus Examination (Ophthalmoscopy)
- Evaluates retina and optic disc
- Detects diabetic retinopathy, retinal detachment, optic atrophy
🔹 5. Optical Coherence Tomography (OCT)
- High-resolution scan of retina and macula
- Identifies retinal edema, macular degeneration, optic nerve thinning
🔹 6. Electroretinogram (ERG) & Visual Evoked Potential (VEP)
- Used in children or non-communicative patients
- Evaluates retinal and visual pathway function
🔹 7. B-Scan Ultrasound
- Performed if media is opaque (e.g., dense cataract or vitreous hemorrhage)
- Detects retinal detachment, tumors, or posterior segment pathology
🔹 8. Imaging (CT/MRI)
- Used in neurological blindness to assess optic nerves or occipital cortex
💊 I. Medical Management of Blindness
Medical management aims to prevent progression, restore partial vision (when possible), and treat the underlying cause. It depends on the etiology (e.g., glaucoma, cataract, infection, systemic disease).
🔹 1. Nutritional and Deficiency-Related Blindness
✅ Vitamin A Deficiency (Xerophthalmia)
- High-dose Vitamin A supplementation:
- 200,000 IU orally for 2 days, followed by a third dose after 2 weeks
- Eye lubrication and antibiotics for secondary infections
- Nutrition counseling and community supplementation programs
🔹 2. Infective or Inflammatory Causes
| Condition | Management |
|---|---|
| Trachoma | Oral Azithromycin + tetracycline eye ointment (SAFE strategy: Surgery, Antibiotics, Facial cleanliness, Environmental improvement) |
| Keratitis | Topical antibiotics, antifungals, antivirals depending on cause |
| Uveitis | Corticosteroids (topical/systemic), cycloplegics, immunosuppressants |
| Onchocerciasis | Ivermectin (community-based treatment) |
🔹 3. Glaucoma
- Eye drops to lower intraocular pressure (e.g., Timolol, Latanoprost, Brimonidine)
- Systemic CAIs (e.g., Acetazolamide) in acute angle-closure
- Laser trabeculoplasty or surgery if not controlled medically
🔹 4. Diabetic Retinopathy & AMD
| Disease | Medical Treatment |
|---|---|
| Diabetic Retinopathy | Tight glycemic and BP control, anti-VEGF injections (e.g., Bevacizumab), steroids |
| Macular Degeneration | Antioxidant-rich supplements (AREDS formula), anti-VEGF therapy for wet AMD |
🔹 5. Neurological Causes
- Corticosteroids for optic neuritis
- Anti-epileptics or tumor management if cortical blindness is due to structural brain causes
- Neuro-rehabilitation for permanent visual loss due to stroke
🩺 II. Surgical Management of Blindness
Surgery is effective in curable causes of blindness, such as cataracts, glaucoma, corneal opacity, and retinal diseases.
🔹 1. Cataract Surgery (Most Common Cause of Reversible Blindness)
| Procedure | Description |
|---|---|
| Phacoemulsification | Ultrasound breaks the lens; IOL inserted |
| Small Incision Cataract Surgery (SICS) | Manual removal of cataract; IOL implanted |
| Extracapsular Cataract Extraction (ECCE) | Large incision; used in mature cataracts |
| Intraocular lens (IOL) implantation | Replaces the opacified lens to restore vision |
📌 Most surgeries are day care procedures with high success rates
🔹 2. Corneal Transplant (Keratoplasty)
- Used for corneal blindness from scarring, ulcers, or trauma
- Types:
- Penetrating keratoplasty (PKP) – full thickness
- Lamellar keratoplasty – partial thickness
- Requires donor cornea (from eye donation)
🔹 3. Retinal Surgery
| Condition | Surgery |
|---|---|
| Retinal detachment | Vitrectomy, scleral buckle, or pneumatic retinopexy |
| Diabetic retinopathy (proliferative) | Pan-retinal photocoagulation (laser) |
| Macular diseases | Anti-VEGF injections + vitrectomy (in select cases) |
🔹 4. Glaucoma Surgery
- Trabeculectomy – creates a new drainage pathway
- Tube shunts or valve implants in refractory glaucoma
- Laser iridotomy in angle-closure glaucoma
🔹 5. Ocular Prosthesis (Cosmetic Rehabilitation)
- In irreversible or disfiguring blindness (e.g., phthisis bulbi, trauma), artificial eyes can be implanted for cosmetic and psychological support
🔹 6. Rehabilitative Surgical Aids
- Low vision aids (e.g., magnifiers, talking books, Braille readers)
- Vision therapy, orientation, and mobility training for permanent blindness
- Use of bionic implants or retinal prostheses (in advanced research stages)
✅ Summary Table – Common Medical vs. Surgical Treatments
| Cause | Medical | Surgical |
|---|---|---|
| Cataract | — | Phaco, IOL |
| Vitamin A deficiency | High-dose Vitamin A | — |
| Glaucoma | Eye drops, systemic meds | Trabeculectomy, laser |
| Diabetic retinopathy | Anti-VEGF, steroids | Laser photocoagulation |
| Corneal scarring | Lubricants, antibiotics | Corneal transplant |
| Retinal detachment | Pre-op meds | Vitrectomy, scleral buckle |
| Onchocerciasis, trachoma | Antiparasitic, antibiotics | Lid surgery in trachoma |
| Neurological causes | Steroids, rehab | Neurosurgery (if tumor) |
👩⚕️👁️🦯 Nursing Management of Blindness
🎯 Objectives of Nursing Care:
✔️ Prevent further visual deterioration
✔️ Promote adaptation to vision loss
✔️ Assist in safe mobility and daily living
✔️ Educate patients and families
✔️ Support emotional and psychological well-being
✔️ Promote rehabilitation and community reintegration
📋 I. Assessment Phase
🔹 1. Physical Assessment
- Check visual acuity (if partial sight remains)
- Assess for associated conditions: diabetes, trauma, infection
- Inspect for eye redness, discharge, deformity, or white reflex (leukocoria)
🔹 2. Functional & Environmental Assessment
- Identify patient’s ability to perform ADLs (activities of daily living)
- Evaluate home environment for potential hazards
- Observe mobility patterns and use of aids
🔹 3. Psychosocial Assessment
- Assess for fear, denial, anxiety, depression, or withdrawal
- Understand the patient’s support system and coping mechanisms
🩺 II. Nursing Interventions
🔹 1. Ensuring Eye Safety & Preventing Complications
| Task | Nursing Action |
|---|---|
| Protect remaining vision (if partial sight exists) | Administer prescribed eye drops/medications regularly |
| Infection control | Maintain clean eye dressing, educate on hand hygiene |
| Avoid injury to the blind eye | Use eye shield, educate on avoiding trauma |
🔹 2. Promoting a Safe Environment
| Area | Action |
|---|---|
| Hospital | Keep call bell within reach, orient patient to bed and room layout |
| Home | Remove tripping hazards, install grab bars, mark edges or steps with tactile indicators |
| Mobility aids | Encourage use of white cane, mobility training with physiotherapist or orientation therapist |
🔹 3. Assisting with ADLs
| ADL | Nursing Role |
|---|---|
| Feeding | Explain food position using clock method (e.g., rice at 12 o’clock) |
| Dressing | Allow independence but help match clothing |
| Toileting & hygiene | Use consistent placement of items and verbal cues |
| Communication | Always announce yourself when entering; use normal tone of voice |
🔹 4. Patient & Family Education
| Topic | Teaching Tips |
|---|---|
| Condition explanation | Use simple, clear terms to explain diagnosis and prognosis |
| Use of visual aids | Magnifiers, Braille readers, talking watches, screen readers |
| Orientation training | Refer to low vision clinics and rehabilitation services |
| Self-care training | Labeling clothes, identifying medications tactically or with apps |
| Eye donation awareness | Especially in irreversible corneal blindness needing transplant |
🔹 5. Psychological & Emotional Support
- Encourage verbal expression of fear or frustration
- Involve counselors or support groups for the visually impaired
- Promote independence to maintain self-esteem
- In children: Support inclusive education and peer integration
🧾 III. Sample Nursing Diagnoses
- Disturbed sensory perception (visual) related to loss of vision
- Risk for injury related to environmental hazards and poor visibility
- Self-care deficit related to vision loss
- Social isolation related to inability to interact freely
- Ineffective coping related to sudden or progressive loss of sight
- Deficient knowledge regarding rehabilitation and support resources
✅ IV. Evaluation Criteria
- Patient demonstrates safe mobility with or without assistive devices
- Patient adheres to medication regimen or postoperative care plan
- Patient and family verbalize understanding of the condition and care strategies
- Home is modified for safety and accessibility
- Patient is emotionally stable and adapting to vision changes
- Rehabilitation services have been initiated or referred
🥗 I. Nutritional Considerations in Blindness
Nutrition plays a vital role in both the prevention of blindness and supporting ocular health, especially in children, elderly, and patients with chronic conditions like diabetes.
✅ Key Nutrients to Support Vision and Prevent Blindness
| Nutrient | Function | Food Sources |
|---|---|---|
| Vitamin A | Maintains healthy cornea and night vision; deficiency causes xerophthalmia | Carrots, sweet potatoes, spinach, dairy, liver |
| Lutein & Zeaxanthin | Protect retina from oxidative damage; important for macular health | Kale, spinach, corn, egg yolk |
| Vitamin C | Antioxidant; supports retinal blood vessels and collagen | Citrus fruits, guava, bell peppers |
| Vitamin E | Prevents oxidative damage to photoreceptors | Almonds, sunflower seeds, avocado |
| Zinc | Helps vitamin A metabolism; found in retina | Meat, legumes, seeds |
| Omega-3 fatty acids | Maintain retinal structure; anti-inflammatory | Salmon, flaxseed, walnuts |
| Vitamin B12 & Folate | Support optic nerve function | Eggs, dairy, leafy greens, legumes |
🍲 Dietary Recommendations for Visually Impaired Patients:
- Encourage colorful fruits and vegetables high in antioxidants
- Ensure adequate hydration
- In children with Vitamin A deficiency, follow WHO or national protocols for high-dose supplementation
- For diabetic patients, follow low glycemic index diets to control blood sugar and prevent diabetic retinopathy
- Encourage soft, easy-to-handle meals for patients with blindness and feeding difficulties
- Label foods or organize meals in predictable patterns (e.g., clock face method)
⚠️ II. Complications of Blindness
Blindness—whether partial or total—can result in multiple physical, psychological, and social complications if not managed holistically.
🔹 Physical Complications
| Complication | Description |
|---|---|
| Injury/falls | Due to poor mobility or environmental hazards |
| Poor hygiene | Difficulty in self-care (bathing, grooming) |
| Malnutrition | In children and elderly due to feeding difficulties |
| Pressure sores | In bed-bound patients with dual disabilities |
| Delayed developmental milestones | In children with congenital blindness |
🔹 Psychological Complications
| Complication | Description |
|---|---|
| Depression or anxiety | Common in acquired or progressive blindness |
| Social isolation | Due to lack of mobility, dependence on others |
| Low self-esteem | Due to dependency or job loss |
| Frustration or aggression | Especially in children or those with sudden vision loss |
🔹 Educational and Occupational Challenges
- Difficulty accessing mainstream education or employment
- Need for assistive devices, special education, or vocational rehabilitation
- Economic burden on families and caregivers
📌 III. Key Points (Quick Summary)
✔️ Blindness is partial or complete loss of vision; can be congenital or acquired, temporary or permanent
✔️ Leading causes include:
- Cataract (most common reversible cause)
- Glaucoma, diabetic retinopathy
- Corneal opacities, vitamin A deficiency
- Neurological and traumatic causes
✔️ Early signs: difficulty seeing at night, blurry vision, halos, visual field loss, or white pupillary reflex (in children)
✔️ Diagnosis: Visual acuity tests, perimetry, slit-lamp exam, fundus exam, OCT, ERG, VEP, imaging (MRI/CT if neurological)
✔️ Treatment options:
- Medical: Vitamin supplementation, eye drops, anti-VEGF, corticosteroids
- Surgical: Cataract surgery, corneal transplant, glaucoma procedures, retinal surgeries
✔️ Nursing care focuses on:
- Preventing complications
- Teaching safe mobility
- Promoting independence in ADLs
- Psychological support and rehabilitation
✔️ Nutritional support includes:
- High intake of vitamin A, antioxidants, omega-3s, and zinc
- Preventing malnutrition in children and elderly
✔️ Complications include:
- Physical injury, malnutrition, depression, and delayed development (especially in children)
👁️🏦 Eye Banking.
📘 Definition:
Eye banking refers to the organized collection, preservation, evaluation, and distribution of donated human eyes (primarily corneas) for transplantation, research, and education.
👁️ The primary goal of eye banking is to restore sight through corneal transplantation and support eye-related research and education.
🎯 Main Objectives / Purposes of Eye Banking:
✔️ Restore vision by providing corneal tissue for transplantation
✔️ Promote eye donation awareness and registration
✔️ Provide tissue for research and medical training
✔️ Maintain ethical and safe handling of human tissues
✔️ Reduce corneal blindness in the community
🧠 Why Eye Banking is Important:
- Corneal blindness accounts for a significant portion of preventable blindness in India and worldwide
- Eye banks help reduce surgical backlogs for corneal transplants
- Only the cornea can be transplanted from a deceased donor — so timely retrieval is critical
- Promotes public health, community participation, and scientific advancement
⚠️ Causes/Need for Eye Banking (Why We Need Donor Eyes):
| Cause | Description |
|---|---|
| Corneal blindness | Due to trauma, ulcers, infections, chemical burns, dystrophies |
| Congenital disorders | Like Peter’s anomaly or sclerocornea |
| Corneal dystrophies | Genetic thinning or clouding of cornea (e.g., Fuchs’ dystrophy) |
| Corneal degenerations | From aging, surgeries, or disease |
| Failed grafts | Repeat transplant required |
| Therapeutic keratoplasty | For non-healing ulcers or infections unresponsive to treatment |
🔢 Types of Eye Banks
Eye banks can be classified based on their functions, level of infrastructure, or purpose served.
🔹 1. Based on Functionality/Level:
| Type | Description |
|---|---|
| Primary Eye Collection Center (PECC) | Collects eyes locally and transports to main eye bank |
| Secondary Eye Bank (SEB) | Performs retrieval, screening, evaluation, and short-term storage |
| Tertiary Eye Bank (TEB) | Full-service bank including tissue evaluation, cornea distribution, research, and training |
| Eye Donation Centers (EDCs) | May only conduct awareness and donor registration campaigns |
🔹 2. Based on Affiliation or Ownership:
| Type | Examples |
|---|---|
| Government Eye Banks | Attached to government hospitals or institutions |
| NGO-run Eye Banks | Run by charitable trusts or foundations |
| Private Eye Banks | Usually within private hospitals or eye institutes |
| Medical College Eye Banks | Involved in research, education, and tissue supply |
🔹 3. Based on Purpose:
| Purpose | Type |
|---|---|
| Therapeutic | Provide corneal grafts to restore vision |
| Research | Supply tissue for experimental and scientific study |
| Educational | Help in medical training and surgical skill practice (e.g., wet labs) |
🌍 Eye Banking in India – Key Points:
- Governed by the Transplantation of Human Organs and Tissues Act (THOTA), 1994
- Coordinated by the National Programme for Control of Blindness (NPCB)
- The Eye Bank Association of India (EBAI) promotes awareness and standardizes protocols
- Eye donation is voluntary and can be done up to 6–8 hours after death
🔬 I. Pathophysiology – Why Corneas Become Non-Functional
The cornea is the transparent, avascular, dome-shaped front surface of the eye. It functions to:
✔️ Refract (bend) light
✔️ Protect internal ocular structures
✔️ Provide a smooth optical surface
🧠 In corneal blindness, any of the following processes can occur:
🔹 1. Infective Damage
- Bacterial, viral, fungal, or parasitic infections (e.g., keratitis) invade the corneal layers
- Leads to inflammation, ulceration, and scarring
🔹 2. Traumatic Injury
- Mechanical trauma, burns, or chemical exposure disrupts the corneal epithelium and stroma
- Results in opacity, edema, or perforation
🔹 3. Degenerative or Dystrophic Changes
- In Fuchs’ endothelial dystrophy or keratoconus, corneal layers thicken, thin, or distort
- Leads to corneal clouding, reduced clarity, and eventual vision loss
🔹 4. Autoimmune or Nutritional Disorders
- Conditions like Stevens-Johnson Syndrome, ocular cicatricial pemphigoid, or vitamin A deficiency can cause corneal melting or xerophthalmia
🔹 5. Graft Failure
- Previously transplanted cornea may reject, fail, or scar, requiring repeat transplantation
🔁 Final Common Pathway:
☑️ Loss of corneal transparency
☑️ Irregular surface or scarring
☑️ Light scattering or blocked entry into the eye
☑️ Reduced visual acuity or complete loss of vision
⚠️ II. Signs & Symptoms of Corneal Disease/Blindness
The signs may vary depending on the cause and stage of disease:
👁️ Early Symptoms:
| Symptom | Explanation |
|---|---|
| Blurry or foggy vision | Due to corneal edema or mild scarring |
| Photophobia (light sensitivity) | Especially in keratitis or dystrophies |
| Foreign body sensation | Often reported in corneal erosions or abrasions |
| Eye redness and watering | Due to inflammation or infection |
| Decreased contrast sensitivity | Especially in dystrophic changes |
👁️🦯 Advanced Symptoms:
| Symptom | Explanation |
|---|---|
| Severe vision loss or blindness | From central scarring or graft failure |
| Visible white spot or opacity | Leucoma seen in healed ulcers |
| Corneal ulcer | Open sore with possible discharge |
| No perception of light | In total corneal or ocular surface failure |
🧪 III. Diagnosis of Corneal Blindness (For Eye Bank Referral & Surgical Planning)
Diagnosis is made through clinical examination and investigations to assess the viability of the eye for corneal transplant:
🔹 1. Slit-Lamp Examination
- Visualizes:
- Corneal ulcers
- Opacity
- Edema
- Neovascularization
- Endothelial dystrophy signs
🔹 2. Visual Acuity Test (Snellen’s chart)
- Measures degree of visual impairment
- Legal blindness is when visual acuity <3/60 in the better eye
🔹 3. Corneal Topography
- Maps the surface curvature of the cornea
- Useful for detecting keratoconus or irregular astigmatism
🔹 4. Specular Microscopy
- Measures endothelial cell density
- Determines the health of corneal endothelium (vital for transplant success)
🔹 5. Pachymetry
- Measures corneal thickness
- Thinning suggests keratoconus or corneal melt
- Thickening may indicate edema
🔹 6. Microbiology Tests (in active infections)
- Scraping for culture & sensitivity to identify infectious organisms
🔹 7. OCT (Optical Coherence Tomography) of Anterior Segment
- Detailed view of corneal layers
- Especially useful in planning lamellar vs full-thickness grafts
💊 I. Medical Management
Medical management is often supportive and focuses on:
✔️ Treating underlying eye conditions to prevent blindness
✔️ Managing post-transplant complications
✔️ Promoting eye health while awaiting transplantation
🔹 A. Before Corneal Transplantation (Pre-operative Medical Management)
| Condition | Medical Treatment |
|---|---|
| Corneal ulcers/infections | Antibiotics, antivirals, antifungals (based on culture reports) |
| Keratitis | Topical corticosteroids (after infection is controlled), lubricants |
| Dry eye or ocular surface disorders | Tear substitutes, cyclosporine drops |
| Nutritional causes | Vitamin A supplementation, multivitamins |
| Pain or photophobia | Cycloplegics and anti-inflammatory eye drops |
💡 Medical treatment cannot reverse corneal opacity — it prepares the eye for surgical intervention or prevents worsening.
🔹 B. After Corneal Transplantation (Post-operative Medical Management)
| Goal | Medications |
|---|---|
| Prevent graft rejection | Topical corticosteroids (e.g., Prednisolone acetate) |
| Prevent infection | Antibiotic eye drops (e.g., Moxifloxacin) |
| Reduce inflammation | NSAID eye drops |
| Lubricate ocular surface | Artificial tears (especially in dry eye) |
| Manage IOP (if raised) | Antiglaucoma medications |
✅ Close monitoring of signs of rejection, such as:
- Redness
- Pain
- Photophobia
- Decreased vision
🔪 II. Surgical Management – Corneal Transplantation (Keratoplasty)
Corneal transplantation is the main surgical treatment offered through eye banking. The damaged or opaque cornea is replaced with donor corneal tissue.
🔹 A. Types of Corneal Transplants
| Procedure | Description | Indication |
|---|---|---|
| Penetrating Keratoplasty (PK) | Full-thickness corneal replacement | Deep corneal scarring, failed graft |
| Anterior Lamellar Keratoplasty (ALK/DALK) | Replaces anterior layers only (epithelium + stroma) | Keratoconus, anterior dystrophies |
| Endothelial Keratoplasty (DSEK/DSAEK/DMEK) | Replaces only inner layers (Descemet’s membrane + endothelium) | Fuchs’ dystrophy, bullous keratopathy |
| Therapeutic Keratoplasty | Emergency graft to remove infected tissue | Resistant corneal ulcers or perforation |
| Tectonic Keratoplasty | Restores corneal integrity | Corneal thinning, laceration |
🔹 B. Eye Banking Role in Surgery
- Donor Eye Collection within 6–8 hours of death
- Screening for infections, diseases (HIV, Hep B, Hep C, syphilis)
- Evaluation of corneal clarity and endothelial count
- Storage in media (MK medium or Optisol-GS)
- Distribution to ophthalmic surgeons for keratoplasty
🔹 C. Postoperative Follow-Up
- Regular slit-lamp evaluation for graft clarity
- Monitor for signs of rejection or infection
- Re-suture removal (if non-absorbable)
- Rehabilitation with spectacles or contact lenses for residual refractive errors
✅ Summary Table
| Phase | Management Approach |
|---|---|
| Pre-op | Control infection/inflammation, prepare eye |
| Surgery | Type of keratoplasty based on condition |
| Post-op | Steroids, antibiotics, follow-up for graft survival |
| Eye bank role | Donor eye retrieval, evaluation, preservation, tissue distribution |
👩⚕️👁️ Nursing Management in Eye Banking
🎯 Objectives of Nursing Management:
✔️ Promote safe eye donation practices
✔️ Assist in donor screening and eye retrieval support
✔️ Provide pre- and post-operative care for corneal transplant patients
✔️ Educate patients, families, and the public about eye donation
✔️ Prevent complications and promote graft survival
📋 I. Role of Nurse in Eye Donation & Eye Banking
🔹 1. Identification & Counseling of Potential Donors
- Coordinate with intensive care units or mortuary staff to identify brain-dead or deceased donors
- Provide emotional support to grieving families and sensitively counsel them about eye donation
- Maintain respectful, ethical communication respecting cultural and religious beliefs
- Obtain legal and informed consent
🔹 2. Assisting in Donor Eye Collection Process
- Support ophthalmic team during enucleation (eye removal)
- Ensure aseptic technique and timely preservation of the tissue
- Help in labeling, packaging, and transporting the eye safely to the eye bank
🔹 3. Documentation & Coordination
- Maintain accurate donor records, consent forms, and donor history
- Coordinate with eye bank officials, blood testing labs, and surgeons
- Ensure timely screening for communicable diseases (HIV, Hep B, etc.)
🩺 II. Nursing Management in Corneal Transplant (Recipient) Care
🔹 1. Preoperative Nursing Care
| Task | Nursing Action |
|---|---|
| Patient education | Explain procedure, risks, recovery, and lifestyle adjustments |
| Pre-op medications | Instill prescribed eye drops (e.g., antibiotics, cycloplegics) |
| Consent & allergy check | Ensure informed consent and check for medication allergies |
| Emotional support | Alleviate anxiety; allow time for questions |
🔹 2. Postoperative Nursing Care
| Focus Area | Nursing Management |
|---|---|
| Eye protection | Apply eye shield, especially during sleep |
| Positioning | Maintain head elevation (especially after endothelial graft) |
| Medications | Administer antibiotic, steroid drops as per schedule |
| Hygiene | Teach hand hygiene before instilling drops |
| Pain management | Provide prescribed analgesics, cold compress if needed |
| Monitoring | Watch for signs of rejection, infection, or inflammation: |
- Redness
- Pain
- Photophobia
- Sudden drop in vision
🔹 3. Discharge Education
- Emphasize strict adherence to medications
- Avoid:
- Eye rubbing
- Heavy lifting or bending
- Contact with water or dust
- Instruct on follow-up schedule and early reporting of symptoms
- Encourage protective eyewear outdoors
📢 III. Role of Nurse in Awareness & Community Programs
| Activity | Description |
|---|---|
| Community outreach | Organize awareness sessions in schools, villages, hospitals |
| Mass media participation | Use pamphlets, posters, street plays on eye donation |
| Celebrate Eye Donation Fortnight (Aug 25 – Sep 8 in India) | Promote registration drives |
| Myth-busting | Educate that eye donation is: |
- Painless
- Respectful of body
- Can be done within 6–8 hours after death |
🧾 IV. Sample Nursing Diagnoses
- Deficient knowledge related to eye donation or post-transplant care
- Risk for infection related to recent eye surgery
- Disturbed sensory perception (visual) related to pre- and post-op visual changes
- Anxiety related to surgical outcome or graft rejection
- Ineffective health maintenance related to non-compliance with post-op regimen
✅ V. Evaluation Criteria
- Patient completes eye drop regimen correctly
- No signs of graft rejection or infection observed
- Donor eye is retrieved and preserved within time frame
- Family and community members show awareness of eye donation
- Recipient adapts well post-transplant with gradual vision improvement
🥗 I. Nutritional Considerations
Nutrition plays a significant role in:
✅ Maintaining corneal and ocular surface health
✅ Supporting post-operative healing after corneal transplant
✅ Preventing nutritional-related corneal blindness, especially in children
✅ Essential Nutrients for Eye and Corneal Health
| Nutrient | Function | Food Sources |
|---|---|---|
| Vitamin A (Retinol) | Maintains corneal epithelium, prevents xerophthalmia and keratomalacia | Carrots, spinach, liver, dairy, sweet potatoes |
| Omega-3 fatty acids | Support tear film, reduce ocular surface inflammation | Salmon, flaxseed, walnuts |
| Vitamin C | Promotes collagen synthesis and wound healing | Citrus fruits, guava, bell peppers |
| Zinc | Essential for vitamin A metabolism and immune defense | Meat, seeds, legumes |
| Vitamin E | Antioxidant, protects eye tissues from oxidative damage | Almonds, sunflower seeds |
| Lutein & Zeaxanthin | Filter harmful blue light, protect retina | Leafy greens (kale, spinach), corn, egg yolk |
| Protein | Required for tissue repair and immune function | Eggs, milk, legumes, lean meat |
💡 Special Focus: Vitamin A Deficiency
- Leading nutritional cause of corneal blindness in children
- Can cause Bitot’s spots, xerosis, corneal ulceration, and perforation
- Requires prophylactic and therapeutic high-dose supplementation in undernourished children
🍽️ Post-Transplant Nutritional Tips
- Encourage small, nutrient-dense meals for surgical patients
- Promote hydration to maintain tear production and corneal integrity
- Avoid processed, high-sugar foods that impair wound healing
- Suggest soft and easy-to-eat meals if the patient is required to maintain positioning (e.g., face-down after surgery)
⚠️ II. Complications in Eye Banking & Corneal Transplantation
🔹 A. Complications Related to Corneal Donation
| Complication | Description |
|---|---|
| Delay in retrieval | Reduces tissue viability; must be collected within 6–8 hours |
| Improper preservation | Leads to corneal edema or loss of transparency |
| Infectious transmission risk | Donor screening failure can transmit HIV, Hepatitis B/C |
| Legal or consent issues | Lack of consent or documentation can delay use of tissue |
🔹 B. Post-Transplant Complications in Recipients
| Complication | Description |
|---|---|
| Graft rejection | Immune response causes pain, redness, decreased vision |
| Graft failure | Clouding due to endothelial cell loss or infection |
| Infection (endophthalmitis) | Rare but sight-threatening infection inside the eye |
| Raised intraocular pressure (IOP) | Due to steroids or post-op inflammation |
| Recurrence of original disease | In hereditary dystrophies or immune-related corneal diseases |
| Astigmatism or poor vision | May require corrective lenses even after a successful graft |
🔹 Psychosocial Complications
- Depression or anxiety post-surgery
- Fear of vision loss again due to graft failure
- Lack of awareness about required precautions
📌 III. Key Points (Quick Revision)
✔️ Eye banking involves the collection, evaluation, preservation, and distribution of donor eyes for corneal transplantation and research
✔️ Corneal blindness is the main indication for transplantation, caused by infections, trauma, scarring, vitamin A deficiency, and dystrophies
✔️ Eye donations are accepted within 6–8 hours of death, and tissues are stored in MK medium or Optisol-GS
✔️ Surgical options include:
- Penetrating Keratoplasty (full thickness)
- Lamellar Keratoplasty (partial)
- Endothelial Keratoplasty (posterior layers)
- Therapeutic Keratoplasty (infection or perforation cases)
✔️ Nurses play a key role in:
- Donor eye retrieval coordination
- Pre/post-operative care
- Eye drop administration
- Patient/family education
- Awareness and community mobilization
✔️ Post-transplant patients must be educated on:
- Eye protection
- Avoiding strain, eye rubbing, or infection
- Strict adherence to eye drops and follow-up
✔️ Nutrition rich in Vitamin A, antioxidants, omega-3s, and zinc supports:
- Corneal health
- Immune defense
- Faster post-operative recovery
✔️ Complications can include graft rejection, infection, astigmatism, or systemic issues — prompt nursing care and follow-up are essential.
📘 Eye Donation:
Eye donation is the voluntary act of donating one’s eyes (corneas) after death to be used for the restoration of sight through corneal transplantation, research, or education.
🧠 Only the cornea (the transparent front layer of the eye) is used for transplantation — not the entire eyeball.
Eyes must be donated within 6–8 hours of death for the tissue to remain viable for surgery.
💡 Importance of Eye Donation:
✔️ Helps restore vision in people suffering from corneal blindness
✔️ Reduces the burden of preventable blindness, especially in low-resource settings
✔️ One donor can give sight to two blind individuals
✔️ Supports medical education and research on eye diseases
✔️ Encourages a culture of organ and tissue donation
🔢 Types of Eye Donation / Tissue Use
Eye donation can be classified based on type of donor, purpose of donation, or use of tissue.
🔹 1. Based on Donor Type:
| Type | Description |
|---|---|
| Voluntary Eye Donation (VED) | Eyes donated by individuals/families after natural death |
| Hospital Cornea Retrieval Program (HCRP) | Eyes collected from medico-legal or brain-dead donors in ICUs with consent |
| Unclaimed Body Donation | Eyes retrieved from unclaimed dead bodies in accordance with legal procedures (as per THOTA Act, India) |
🔹 2. Based on Purpose of Use:
| Purpose | Description |
|---|---|
| Therapeutic Use | Corneas transplanted into patients with corneal blindness |
| Research Use | Donated eyes used for medical studies (e.g., stem cells, corneal healing) |
| Educational Use | Eyes used for training ophthalmologists in surgical procedures |
🔹 3. Based on What is Retrieved:
| Type | Description |
|---|---|
| Whole Globe Enucleation | Entire eyeball removed (common method) |
| In-situ Corneoscleral Button Removal | Only the cornea with a rim of sclera is excised — reduces tissue handling |
| Anterior/Posterior Lamellae (Advanced centers) | Specific corneal layers used for targeted surgeries (e.g., DALK, DMEK) |
🔹 4. Based on Time of Retrieval:
| Type | Description |
|---|---|
| Timely Eye Donation | Within 6 hours of death – ensures maximum viability of tissue |
| Delayed Eye Donation | Up to 12 hours (with body refrigeration) – limited use for research or education only |
📘 Indications for Eye Donation (Use of Donated Eyes)
Donated eyes (specifically corneas) are used for restoring sight and other medical purposes.
✅ Therapeutic Indications:
| Condition | Explanation |
|---|---|
| Corneal Opacity/Scarring | From trauma, infections, or burns |
| Corneal Degenerations | Like Salzmann’s nodular or band keratopathy |
| Corneal Dystrophies | E.g., Fuchs’ endothelial dystrophy, keratoconus |
| Corneal Perforations | Due to ulcers or autoimmune conditions |
| Failed Previous Corneal Graft | Repeat keratoplasty needed |
| Corneal Blindness (non-retinal origin) | Main cause of avoidable blindness treated by eye donation |
❌ Contraindications for Eye Donation (When Donated Eyes Cannot Be Used)
| Type | Specific Conditions |
|---|---|
| Systemic infections | HIV/AIDS, Hepatitis B & C, Sepsis, Rabies, Syphilis |
| Cancer with metastasis | Eye tissue may carry cancerous cells |
| Certain eye diseases | Retinoblastoma, endophthalmitis, corneal malignancy |
| Unknown cause of death | Medico-legal restriction if cause is not verified |
| Severe systemic illness | Like leukemia or lymphoma affecting the eye |
| Diseased or damaged cornea | Clouded, scarred, or chemically damaged corneas not suitable for transplant |
| Refractive surgery history | LASIK/PRK may affect the usability for some transplant types (case-dependent) |
🔍 However, even if tissue is not suitable for transplant, it may still be used for medical education or research.
🧰 Equipment Needed for Eye Donation (Eye Retrieval / Enucleation)
🧪 Sterile Tray Set Up:
- Eye Speculum
- Castroviejo scissors
- Enucleation scissors
- Corneal trephine or blade
- Forceps (toothed and plain)
- Sterile gloves
- Eye drape
- Sterile gauze
- 5% Povidone-iodine solution
- Sterile normal saline
- Preservation medium (MK medium or Optisol-GS)
- Corneal excision container with label
- Biohazard transport box
🩺 Procedure Steps of Eye Donation (Corneal Retrieval)
To be completed within 6–8 hours after death for transplant use.
🔹 A. Preparation
- Confirm time of death and consent form from next of kin
- Ensure cooling of the body if there is any delay
- Explain procedure and maintain dignity of the body
🔹 B. Eye Retrieval Steps (Corneoscleral Button or Enucleation)
| Step | Description |
|---|---|
| 1. Positioning | Place the body supine in a clean, well-lit area |
| 2. Disinfection | Clean eyelids and surrounding skin with 5% povidone-iodine |
| 3. Eye Closure | Use eye speculum to gently open eyelids |
| 4. Corneal excision or enucleation | Carefully cut and remove corneoscleral button (preferred) or entire eyeball |
| 5. Hemostasis | Apply pressure with gauze or sterile sponge |
| 6. Insert prosthesis (if desired) | To maintain appearance post-removal |
| 7. Transport | Place eye/cornea in preservation media and transport to eye bank at 2–8°C |
| 8. Documentation | Label with donor ID, time of death, and retrieval details |
👩⚕️ Role of Nurse in Eye Donation
Nurses are key in facilitating, supporting, and advocating eye donation.
✅ 1. Before Donation (Community/Public Role)
- Educate patients and families about the importance and impact of eye donation
- Promote eye donation pledge campaigns and awareness in health camps, schools, and media
- Counsel grieving families sensitively and support consent process
✅ 2. In Hospital or Retrieval Setting
| Responsibility | Description |
|---|---|
| Donor Identification | Recognize potential donors (brain-dead, post-mortem) |
| Consent | Support team in getting informed written consent from relatives |
| Coordination | Inform and coordinate with eye bank team or retrieval technician |
| Asepsis | Maintain sterile field during enucleation or corneal excision |
| Documentation | Help with forms, time of death, medical history records |
| Preservation | Assist in placing the tissue in appropriate medium and labeling correctly |
✅ 3. After Donation
- Provide emotional support to family
- Ensure the body is respectfully restored (eye prosthetics if needed)
- Encourage registration of other family members
- Follow up with eye bank for tissue usage updates (if requested by family)
📌 Key Points (Quick Summary)
✔️ Eye donation is a noble act of giving vision after death
✔️ Only the cornea is used for transplantation — not the whole eyeball
✔️ Eyes should be donated within 6–8 hours of death
✔️ One person can give sight to two individuals
✔️ Nurses play a critical role in:
- Counseling families
- Coordinating donation
- Supporting retrieval and asepsis
- Promoting awareness
✔️ Contraindications include infectious diseases (HIV, Hep B/C), eye cancers, and unknown cause of death
✔️ Tissue can be used for transplant, education, or research depending on quality
💡 Other Useful Details
- Eye Donation Fortnight in India: Observed from August 25 to September 8 every year
- Eye Bank Association of India (EBAI): National body promoting eye donation
- 24×7 Eye Donation Helplines: Available in many cities to support retrieval coordination
- Donors of any age, gender, religion, or spectacle use can donate
- No disfigurement to the face or delay in funeral ceremonies