BSC SEM 3 UNIT 2 ADULT HEALTH NURSING 1
UNIT 2 Intraoperative Care
🌟 INTRAOPERATIVE CARE (Intraoperative Nursing)

✅ DEFINITION
Intraoperative Care refers to the care provided to the patient during surgery – from the time the patient is transferred to the operating room (OR) until they are transferred to the post-anesthesia care unit (PACU).
🎯 GOALS OF INTRAOPERATIVE CARE
- Ensure patient safety under anesthesia and during surgery
- Maintain aseptic environment
- Monitor vital signs and complications
- Assist surgical team for efficient functioning
- Provide emotional and physical support to patient
👩⚕️ ROLES OF NURSES IN INTRAOPERATIVE CARE
1. Scrub Nurse (Sterile Role)
- Maintains sterile field
- Prepares sterile instruments, sutures, drapes
- Hands instruments to surgeon during surgery
- Counts instruments/sponges pre- and post-operation
- Maintains surgical asepsis
2. Circulating Nurse (Non-sterile Role)
- Prepares OR environment
- Checks patient identity, consent, surgical site
- Assists anesthesia and positioning
- Monitors patient’s condition and sterile technique
- Documents intraoperative care
- Manages specimens
3. RN First Assistant (in some setups)
- Helps in retraction, hemostasis, suturing
- Works directly under surgeon’s supervision
🛠️ PREPARATION BY NURSING STAFF
✅ Physical Preparation
- OR sterilization, lighting, and instrument check
- Ensure crash cart and suction machine availability
- Arrange and verify surgical instruments and supplies
✅ Patient Preparation
- Verify ID band, consent, NPO status
- Confirm surgical site (marking if required)
- Pre-op checklist: allergies, vitals, last meds, etc.
- Positioning based on surgical procedure (e.g., supine, prone, lithotomy)
- Skin prep with antiseptic
- Insert catheter/IV as ordered
🔬 ANESTHESIA MONITORING
- Assist anesthetist during induction
- Monitor vitals: HR, BP, RR, SpO2, ECG
- Watch for signs of anesthetic complications:
- Malignant Hyperthermia
- Respiratory depression
- Cardiac arrhythmia
🛡️ ASEPSIS AND INFECTION CONTROL
- Proper hand hygiene and PPE use
- Maintain sterile field throughout surgery
- Limit OR traffic
- Handle contaminated instruments properly
- Use of antibiotic prophylaxis as prescribed
📋 INTRAOPERATIVE DOCUMENTATION
- Time in/out of OR
- Type of anesthesia and medications used
- Name of surgeon and staff
- Procedure performed
- Count of instruments, sponges
- Blood/fluid loss
- Any complications/events
⚠️ INTRAOPERATIVE COMPLICATIONS TO WATCH FOR
| Complication | Signs/Symptoms | Nursing Intervention |
|---|---|---|
| Hemorrhage | Low BP, high HR, pallor | Inform surgeon, ensure IV access, prepare transfusion |
| Anaphylaxis | Rash, wheezing, hypotension | Administer epinephrine, support airway |
| Hypothermia | Shivering, low body temp | Warm blankets, warm IV fluids |
| Nerve Injury | Poor positioning | Reposition, use padding |
| Malignant Hyperthermia | High temp, muscle rigidity, tachycardia | Administer dantrolene, cool patient, alert anesthetist |
🧠 SPECIAL CONSIDERATIONS
- Geriatric Patients: fragile skin, slow metabolism, risk of hypothermia
- Pediatric Patients: emotional support, smaller doses of meds
- Obese Patients: higher risk of pressure ulcers, airway issues
- Emergency Surgery: quick assessment, psychological support
📦 TRANSFER TO POSTOPERATIVE CARE
- Hand off report to PACU nurse including:
- Type of surgery, anesthesia, vitals
- Estimated blood loss, I/O
- Medications given
- Any intraoperative events
- Airway status, drain/tubes/catheters
📚 NURSING DIAGNOSES (Intraoperative Phase)
- Risk for infection related to invasive procedure
- Risk for perioperative positioning injury
- Risk for aspiration related to decreased GI motility
- Risk for hypothermia related to surgical exposure
🧾 INTRAOPERATIVE CARE PLAN EXAMPLE
| Nursing Diagnosis | Goal | Nursing Interventions | Evaluation |
|---|---|---|---|
| Risk for infection | Maintain sterile field throughout | Monitor aseptic technique, limit exposure | No signs of infection post-op |
| Risk for injury due to positioning | Maintain safe positioning | Use padding, reposition limbs as needed | No redness, numbness post-op |
| Risk for aspiration | Prevent aspiration during anesthesia | NPO before surgery, suction ready | No aspiration events during OR |
🏥 ORGANIZATION AND PHYSICAL SETUP OF THE OPERATION THEATRE (OT)

✅ DEFINITION
An Operation Theatre (OT) is a specialized sterile facility in a hospital where surgical procedures are performed. It must be well-organized, sterile, and functionally efficient to ensure patient safety and support surgical teams.
🏗️ PHYSICAL SETUP OF THE OPERATION THEATRE
The OT is designed using the Zoning System and includes a variety of structural, functional, and equipment-based requirements.
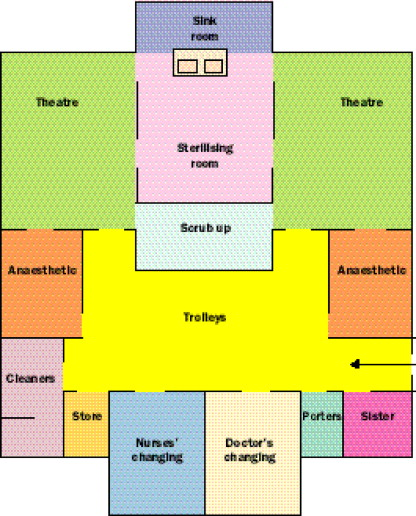
🔹 1. ZONING IN OT COMPLEX
To maintain asepsis, the OT is divided into four zones:
| Zone | Description |
|---|---|
| Unrestricted Zone | Entrance area, change rooms, lounges (street clothes allowed) |
| Semi-restricted Zone | Access corridor, sterile store (only OT dress, hair covers allowed) |
| Restricted Zone | Actual operating room – maximum sterility (OT dress, mask, cap mandatory) |
| Dirty Zone | Area for disposal of waste, cleaning of instruments |
🔹 2. TYPICAL ROOMS IN OT COMPLEX
| Room | Function |
|---|---|
| Operating Room (OR) | Main sterile room for performing surgery |
| Scrub Area | For hand scrubbing and gowning before surgery |
| Anesthesia Room | Prepares patient for anesthesia |
| Pre-op Holding Room | Temporary area for patients before surgery |
| Post-op Recovery Room (PACU) | For monitoring after surgery |
| Sterile Store Room | Stores sterile linen, instruments |
| Soiled Utility Room | Collects contaminated linen/instruments |
| CSSD (Central Sterile Supply Dept.) | Prepares and supplies sterilized instruments and items |
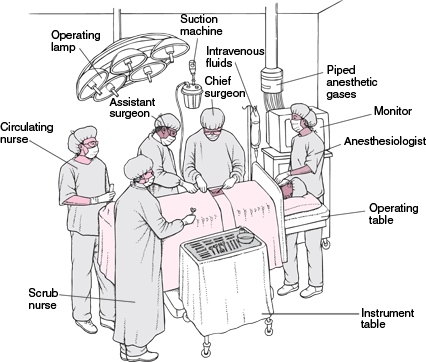
🧰 EQUIPMENT AND FIXTURES IN THE OPERATING ROOM
| Equipment | Use |
|---|---|
| Operating Table | Adjustable, used to position patient |
| Operating Lights | Shadow-free, adjustable for visibility |
| Anesthesia Machine | For gas delivery and monitoring during anesthesia |
| Suction Apparatus | Removes secretions/blood during surgery |
| Electrocautery Unit | For cutting tissue and controlling bleeding |
| Monitors (ECG, SpO2, BP) | To monitor vital signs during surgery |
| Instrument Trolley | Holds surgical tools during procedures |
| Kick Bucket/Foot Stool | Assists in maintaining cleanliness/mobility |
| Defibrillator | For emergency cardiac resuscitation |
| Lead Apron | Used during X-ray guided procedures |
🧼 ASEPTIC DESIGN FEATURES
| Feature | Purpose |
|---|---|
| Seamless walls/flooring | Easy cleaning, prevents dust collection |
| Laminar Air Flow System | Reduces airborne contaminants |
| HEPA Filters | Filter bacteria/viruses from air |
| Positive Pressure Ventilation | Prevents entry of air from non-sterile areas |
| Temperature and Humidity Control | Maintains comfort and inhibits microbial growth |
👩⚕️ ORGANIZATIONAL STRUCTURE OF OT TEAM
| Personnel | Role |
|---|---|
| OT In-charge Nurse | Supervises entire OT setup |
| Circulating Nurse | Manages patient prep, assists sterile team |
| Scrub Nurse | Assists surgeon, maintains sterile field |
| Anesthesiologist | Provides anesthesia, monitors patient |
| Surgeon and Assistants | Perform the surgical procedure |
| Technicians | Operate machines, sterilize instruments |
| Housekeeping Staff | Maintains cleanliness and transport of waste |
🔄 WORKFLOW AND LAYOUT PRINCIPLES
- Unidirectional Movement: From clean → sterile → dirty to avoid cross-contamination
- Separate Entry/Exit for patients, staff, and supplies
- Intercom Systems: For communication without entering the OR
- Color Coding of Areas to indicate zones (optional in modern setups)
📋 KEY POLICIES FOR OT MANAGEMENT
- Scheduling of surgeries
- Infection control protocols (e.g., OT fumigation, UV lights)
- Instrument Count Policies
- Biomedical Waste Segregation
- Maintenance of OT Register & Documentation
🛑 CHALLENGES IN OT MANAGEMENT
- Infection risk
- Equipment malfunction
- Emergency preparedness
- Coordination between multi-disciplinary teams
🏥 CLASSIFICATION OF OPERATION THEATRE
✅ DEFINITION
An Operation Theatre (OT) is a sterile, specialized unit where surgical procedures are carried out under aseptic conditions with the help of trained personnel and equipment.
📚 CLASSIFICATION OF OPERATION THEATRE
Operation theatres are classified based on different criteria, such as case type, sterility, usage, and design. Here’s a detailed classification:
🔹 1. Based on Type of Surgery
| Type of OT | Description |
|---|---|
| General OT | Used for routine general surgeries (e.g., hernia, appendectomy) |
| Specialized OT | Designed for specific disciplines |
| – Cardiac OT (e.g., bypass, valve replacement) | |
| – Neuro OT (e.g., craniotomy) | |
| – Orthopedic OT (e.g., fracture, joint replacement) | |
| – ENT OT, Gynecology OT, Urology OT, etc. |
🔹 2. Based on Level of Asepsis or Sterility
| Type | Description |
|---|---|
| Septic OT | For infected or contaminated surgeries (e.g., gangrene, abscess) |
| Aseptic OT | For clean surgeries (e.g., C-section, hernia, tumor removal) |
⚠️ Septic OT is usually scheduled after clean cases or done in a separate room to avoid contamination.
🔹 3. Based on Usage or Frequency
| Type | Description |
|---|---|
| Elective OT | Pre-planned, scheduled surgeries (e.g., cataract, cholecystectomy) |
| Emergency OT | For urgent/life-threatening cases (e.g., road traffic accident, C-section in fetal distress) |
Emergency OTs are usually available 24×7 and located near casualty/trauma centers.
🔹 4. Based on Setup/Design
| Type | Description |
|---|---|
| Conventional OT | Basic structure with standard lighting and minimal automation |
| Modular OT | Advanced design with laminar airflow, HEPA filters, anti-microbial surfaces, and smart panels for better asepsis and control |
Modular OTs are becoming the modern standard in tertiary care hospitals.
🔹 5. Based on Ownership / Management
| Type | Description |
|---|---|
| Government OT | Found in public hospitals; funded and maintained by the state |
| Private OT | Run by private hospitals or nursing homes |
| Teaching OT | Located in medical colleges with student observation facilities |
🔹 6. Based on Location in Hospital
| Type | Description |
|---|---|
| Central OT Complex | Cluster of all OTs in one area with shared support facilities (CSSD, PACU) |
| Decentralized OT | OTs scattered across hospital departments (e.g., in labor room, trauma unit) |
🔹 7. Based on Functionality
| Type | Description |
|---|---|
| Major OT | Equipped for major surgeries requiring general or spinal anesthesia |
| Minor OT | For minor procedures under local anesthesia (e.g., suturing, biopsy) |
📝 SUMMARY CHART: Classification of Operation Theatre
| Basis | Types |
|---|---|
| Type of surgery | General, Specialized (Cardiac, Neuro, Ortho, ENT, Gynae, etc.) |
| Asepsis level | Septic OT, Aseptic OT |
| Usage | Elective OT, Emergency OT |
| Setup | Conventional OT, Modular OT |
| Ownership | Government, Private, Teaching |
| Location | Centralized, Decentralized |
| Functionality | Major OT, Minor OT |
🏥 OPERATION THEATRE DESIGN
✅ OBJECTIVES OF OT DESIGN
- To maintain maximum sterility and asepsis
- To ensure efficient workflow of patients, staff, and instruments
- To facilitate smooth communication and monitoring
- To provide safety, hygiene, and comfort to both patient and staff
🏗️ KEY PRINCIPLES OF OT DESIGN
- Zoning and Aseptic Technique
- Unidirectional Flow (clean to dirty)
- Separate entry/exit for staff, patients, and materials
- Controlled ventilation and air filtration
- Minimum contamination, easy cleaning surfaces
🧭 ZONING SYSTEM IN OT DESIGN
To prevent infection and maintain asepsis, OTs are designed with four major zones:
| Zone | Description | Example Areas |
|---|---|---|
| Unrestricted Zone | Entry zone; street clothes allowed | Reception, waiting area, staff room |
| Semi-restricted Zone | Only OT attire and hair covering allowed | Corridors, sterile supply storage |
| Restricted Zone | Complete sterility maintained, masks mandatory | Actual Operating Room, Scrub area |
| Dirty Zone | Disposal of used materials and instruments | Dirty utility, disposal chute |
📐 LAYOUT DESIGN OF OT COMPLEX
🟢 Central OT Complex (Modern Design)
- Cluster of multiple OTs with shared support services like:
- Central Sterile Supply Department (CSSD)
- Pre-op holding area
- Post-Anesthesia Care Unit (PACU)
- Scrub areas
- Staff and patient entrances
🧱 STRUCTURAL REQUIREMENTS
| Component | Specifications |
|---|---|
| Walls | Smooth, seamless, anti-microbial, easily washable (e.g., epoxy-coated) |
| Floors | Antistatic, slip-resistant, seamless flooring (e.g., vinyl or PU) |
| Ceiling | Non-porous, anti-bacterial, sealed around fixtures |
| Doors | Sliding/automatic to minimize airflow; ideally hermetically sealed |
| Windows | Minimal or none; if present, must be fixed and sealed |
| Lighting | Shadow-free, ceiling-mounted surgical lights, intensity adjustable |
💨 VENTILATION AND AIRFLOW DESIGN
| Component | Design Consideration |
|---|---|
| Laminar Air Flow System | Vertical or horizontal flow of filtered air to minimize airborne particles |
| HEPA Filters | Remove 99.97% of bacteria and viruses from air |
| Air Exchanges | Minimum 15–20 air changes/hour |
| Positive Pressure | Prevent entry of contaminated air from surrounding areas |
| Temperature Control | Maintained between 20–24°C |
| Humidity Control | 50–60% to prevent infection |
🛠️ OPERATION ROOM DESIGN (INSIDE OT)
| Feature | Description |
|---|---|
| Operating Table | Centrally located, adjustable, radiolucent |
| Operating Light | Ceiling-mounted, movable, with variable intensity |
| Gas Outlets | For O2, N₂O, suction, compressed air |
| Electrical Outlets | Multiple outlets for monitors, cautery, etc. |
| Storage Cabinets | For sterile instruments and consumables (in-wall preferred) |
| Monitors & Control Panels | Touch-screen panels for equipment control, anesthesia monitoring |
🧼 INFECTION CONTROL FEATURES IN OT DESIGN
- Sterile air circulation (HEPA + laminar flow)
- Antimicrobial coatings on surfaces
- Handwashing and scrub stations with sensor taps
- Zoning to separate clean and dirty traffic
- Automatic doors to reduce touch points
- Sealed lighting fixtures and air vents
- Fumigation and UV disinfection systems
📋 OPTIONAL MODERN FEATURES
- Modular prefabricated panels for rapid installation
- CCTV and audio systems for training and monitoring
- RFID tags or barcode for instrument tracking
- PACS integration for imaging access in OT
- Fire safety system, UPS, and backup power
🗺️ SIMPLE OT LAYOUT FLOWCHART (for theory)
mathematicaCopyEditPatient Entry → Pre-op Holding →Anesthesia Room → Operating Room→ Recovery Room (PACU) → Exit
Sterile Corridor → Operating Room ← Scrub Area ←Sterile Store
↓
Dirty Utility →Waste Exit (Dirty Zone)
📝 SUMMARY TABLE
| Feature | Key Points |
|---|---|
| Layout | Centralized preferred; zoning essential |
| Surfaces | Smooth, washable, antimicrobial (epoxy/vinyl) |
| Ventilation | Laminar airflow + HEPA, 20 air exchanges/hour, positive pressure |
| Lighting | Ceiling-mounted, shadowless, variable intensity |
| Infection control | Zoning, UV light, sensor taps, limited personnel movement |
🏥 STAFFING OF OPERATION THEATRE
✅ DEFINITION
OT Staffing refers to the systematic allocation and deployment of trained medical, nursing, technical, and support personnel in the Operation Theatre, ensuring the smooth, safe, and sterile conduct of surgical procedures.
🎯 OBJECTIVES OF OT STAFFING
- To maintain asepsis and infection control
- To ensure smooth workflow during surgery
- To provide adequate and qualified staff for various OT roles
- To enhance efficiency, safety, and patient outcomes
👥 CATEGORIES OF OT STAFF
OT staffing includes a multi-disciplinary surgical team divided into sterile and non-sterile members.
🔹 1. Surgical Team Members
| Personnel | Role |
|---|---|
| Surgeon | Performs surgery; team leader |
| Surgical Assistant | Assists surgeon; may hold instruments, suture, retract |
| Scrub Nurse | Works in sterile field, assists surgeon directly |
| Circulating Nurse | Manages patient, equipment, supplies outside sterile field |
| Anesthesiologist | Administers and monitors anesthesia |
| Anesthesia Technician | Assists anesthetist with machines, drugs, airway support |
🔹 2. Supportive Staff
| Personnel | Role |
|---|---|
| OT Technician | Prepares and maintains instruments, sterilization |
| CSSD Personnel | Sterilize and supply instruments from Central Sterile Supply Dept. |
| Housekeeping Staff | Maintains cleanliness, assists with waste management |
| Transport Attendant | Shifts patients from ward to OT and PACU |
| Reception/Clerical Staff | Manages scheduling, documentation, patient record entry |
🩺 NURSING STAFFING IN OT
| Nurse Role | Responsibility |
|---|---|
| OT In-Charge Nurse | Oversees the functioning of OT; manages staff, supplies, coordination |
| Staff Nurse (Scrub) | Assists surgeon, handles sterile instruments, counts materials |
| Staff Nurse (Circulating) | Provides patient care, fetches materials, maintains records |
| Recovery Room Nurse | Monitors and cares for patient post-op in PACU |
📊 STAFFING NORMS (as per NABH / WHO guidelines)
| Staffing Element | Ideal Ratio or Recommendation |
|---|---|
| Scrub Nurse | 1 per surgery per OT |
| Circulating Nurse | 1 per surgery per OT |
| Technician | 1 per OT (some setups 1 for 2 OTs) |
| Anesthetist | 1 per OT |
| Surgeons | 1 primary + 1 assistant (or more depending on case) |
| Housekeeping Staff | 1 for every 2 OTs (or per shift) |
| On-call backup staff | For night/emergency/ICU transfers |
🕒 SHIFT SYSTEM AND ROTATION
- Usually operates in 3 shifts (Morning, Afternoon, Night)
- Rotational duty to avoid burnout
- Emergency Team On-call 24×7
- Weekly off-day with relievers arranged
👩⚕️ STAFF QUALIFICATIONS AND TRAINING
| Role | Qualification / Training |
|---|---|
| Nurse (OT trained) | BSc/GNM + specialized OT training or diploma |
| OT Technician | Diploma in OT Technology / DMLT |
| Anesthetist | MBBS + MD/DNB/DA in Anesthesia |
| Housekeeping Staff | Basic infection control and OT protocol orientation |
🔁 Regular in-service training is vital:
- Infection control
- Biomedical waste handling
- Surgical handwashing and gowning
- CPR/Code Blue response
- Equipment handling (defibrillator, cautery, suction)
📝 OT STAFFING ROSTER EXAMPLE (for one OT)
| Time | Scrub Nurse | Circulating Nurse | OT Technician | Anesthetist | Housekeeping |
|---|---|---|---|---|---|
| 8 AM – 2 PM | Nurse A | Nurse B | Tech 1 | Dr. X | Staff 1 |
| 2 PM – 8 PM | Nurse C | Nurse D | Tech 2 | Dr. Y | Staff 2 |
| 8 PM – 8 AM | On-call | On-call | On-call | On-call | On-call |
🚨 CONTINGENCY STAFFING (Emergency/Disaster)
- A standby team is always prepared for:
- Mass casualties
- OT fire or equipment failure
- Sudden staff absence
- Quick mobilization with call-in system or emergency staffing app
📋 NURSING MANAGEMENT RESPONSIBILITIES
- Preparing duty rosters
- Ensuring adequate staff per shift
- Conflict resolution and team coordination
- Conducting training and drills
- Evaluating performance and infection audits
🏥 MEMBERS OF THE OPERATION THEATRE (OT) TEAM

✅ INTRODUCTION
The OT team is a multi-disciplinary group of healthcare professionals who work collaboratively to ensure safe and effective surgical procedures while maintaining sterility, patient safety, and team coordination.
They are classified into:
- Sterile Members (Scrubbed-in)
- Non-Sterile Members (Supportive/Monitoring)
👥 CLASSIFICATION OF OT TEAM MEMBERS
🔹 1. Sterile Members (Work in sterile field)
These team members scrub, gown, and glove in for surgery.
| Team Member | Roles & Functions |
|---|---|
| Surgeon | – Leader of the team – Performs the surgical procedure – Makes pre-op and post-op decisions – Ensures the correct procedure and site – Supervises scrubbed staff |
| Assistant Surgeon | – Supports the primary surgeon – Helps in retraction, suturing, suction, exposure – May take over in long/complex surgeries |
| Scrub Nurse (Instrument Nurse) | – Prepares sterile instruments and supplies – Sets up the sterile field – Hands instruments during surgery (sterile technique) – Counts instruments/sponges before and after surgery – Maintains strict asepsis |
🔹 2. Non-Sterile Members (Do not scrub in)
These members provide support and coordination but do not directly touch the sterile field.
| Team Member | Roles & Functions |
|---|---|
| Circulating Nurse | – Prepares patient for surgery – Positions patient with padding – Assists in applying monitor leads, Foley catheter – Opens sterile packs maintaining asepsis – Maintains intraoperative records – Coordinates with other departments |
| Anesthesiologist | – Assesses patient preoperatively – Induces and maintains anesthesia – Monitors patient vitals and airway – Manages pain, fluid balance, and emergency situations – Reverses anesthesia and transfers patient to recovery |
| Anesthesia Assistant / Technician | – Prepares anesthesia machine and circuits – Assists with intubation, ventilation – Draws medications, sets IV fluids – Monitors equipment and alarms – Assists with shifting to recovery |
| OT Technician | – Checks, arranges, and sterilizes instruments – Prepares OT before and after surgery – Assists in suction, cautery machine setup – Maintains and operates equipment |
| Housekeeping Staff (Attendant/Sweeper) | – Cleans OT before and after procedure – Disposes of biomedical waste as per protocols – Helps in shifting patients or equipment |
| Receptionist / OT Clerk | – Maintains OT schedule – Ensures correct documentation – Coordinates with wards, labs, and blood bank |
🩺 SPECIALIZED ROLES (in advanced setups)
| Member | Additional Roles |
|---|---|
| RN First Assistant (RNFA) | – Advanced practice nurse – Assists in tissue handling, suturing – Helps in wound closure, hemostasis |
| PACU Nurse (Recovery Room Nurse) | – Monitors patient post-anesthesia – Manages pain and vitals – Identifies complications like nausea, hypoxia |
| Infection Control Nurse (ICN) | – Audits OT asepsis, fumigation – Tracks infection rates, educates staff |
👩⚕️ QUALIFICATIONS AND TRAINING OF OT TEAM MEMBERS
| Role | Minimum Qualification |
|---|---|
| Surgeon | MBBS + MS/MD/DNB in specialty |
| Anesthesiologist | MBBS + MD/DA/DNB in Anesthesia |
| OT Nurse (Scrub/Circulating) | GNM/BSc Nursing + OT training |
| OT Technician | Diploma in OT Technology / DMLT / BSc OT |
| Housekeeping | Basic infection control orientation |
| Anesthesia Assistant | DOTT or specialized OT technician course |
🛡️ PRINCIPLES FOLLOWED BY OT TEAM MEMBERS
- Aseptic Technique
- Patient Safety First
- Effective Communication (SBAR method)
- Documentation Accuracy
- Team Collaboration and Respect
- Emergency Preparedness
- Count Protocol (instruments, swabs, sharps)
💡 INTRAOPERATIVE TEAM COORDINATION FLOW
makefileCopyEditPRE-OP: Patient ID →Consent → Site Marking → Pre-medication
↓
INTRA-OP: Anesthesia → Scrubbing & Gowning →Surgery Begins
↓
Team Roles in Action(Scrub + Circulator + Anesthetist + Technician)
↓
Closure → Count → Dressing →Transfer to PACU → Documentation
📝 SUMMARY TABLE
| Member | Sterility | Main Functions |
|---|---|---|
| Surgeon | Sterile | Performs surgery |
| Assistant Surgeon | Sterile | Supports primary surgeon |
| Scrub Nurse | Sterile | Handles instruments and maintains asepsis |
| Circulating Nurse | Non-sterile | Coordinates environment and patient care |
| Anesthesiologist | Non-sterile | Manages anesthesia and airway |
| OT Technician | Non-sterile | Prepares and maintains equipment |
| Housekeeping Staff | Non-sterile | Cleaning and waste disposal |
| Receptionist | Non-sterile | Scheduling and documentation |
👩⚕️ SCRUB NURSE IN OT – DUTIES & RESPONSIBILITIES

✅ WHO IS A SCRUB NURSE?
A scrub nurse is a sterile member of the surgical team responsible for maintaining the sterile field, preparing surgical instruments, and directly assisting the surgeon during the procedure.
🩺 QUALIFICATIONS
- GNM / BSc Nursing
- OT Training Certificate or specialized in perioperative nursing
- Strong understanding of aseptic technique and instrument handling
🎯 OBJECTIVES OF A SCRUB NURSE
- Ensure a sterile surgical environment
- Provide correct instruments and materials to the surgeon
- Maintain strict aseptic technique throughout the procedure
- Support the surgical team and prevent complications
📋 DUTIES AND RESPONSIBILITIES OF A SCRUB NURSE
🔹 1. Pre-Operative Responsibilities
| Task | Description |
|---|---|
| 1.1 Scrubbing and gowning | Performs surgical hand scrub, dons sterile gown and gloves |
| 1.2 Equipment check | Ensures surgical instruments, sutures, and drapes are sterilized and ready |
| 1.3 Sterile field setup | Arranges surgical trays and equipment in the sterile field |
| 1.4 Count of items | Performs initial count of sponges, instruments, and sharps with circulating nurse |
| 1.5 Verification | Confirms patient ID, surgical site, and consent (in coordination with the team) |
🔹 2. Intra-Operative Responsibilities
| Task | Description |
|---|---|
| 2.1 Instrument handling | Passes instruments and supplies to the surgeon efficiently |
| 2.2 Tissue handling | Assists in retraction, suction, sponging, or irrigation as needed |
| 2.3 Aseptic maintenance | Maintains strict sterility of self and field throughout the surgery |
| 2.4 Monitoring needs | Anticipates surgeon’s needs and prepares next instruments accordingly |
| 2.5 Count management | Performs sponge/instrument/sharp counts during surgery to prevent retention |
| 2.6 Specimen handling | Assists in proper collection, labeling, and handover of surgical specimens |
| 2.7 Emergency readiness | Prepares and passes emergency instruments or sutures promptly |
🔹 3. Post-Operative Responsibilities
| Task | Description |
|---|---|
| 3.1 Final count | Completes final count with circulator before wound closure |
| 3.2 Instrument care | Separates and sends used instruments for cleaning/sterilization |
| 3.3 Sterile field breakdown | Disposes of waste in biohazard bins following infection control protocol |
| 3.4 Documentation | Assists in completing OT notes, sponge/instrument counts, incident reports if any |
| 3.5 Handover | Updates recovery/PACU nurse about drains, dressing, instruments used, complications |
💡 SKILLS REQUIRED FOR A SCRUB NURSE
| Skill | Importance |
|---|---|
| Knowledge of surgical procedures | Essential to anticipate needs |
| Manual dexterity & speed | To handle and pass instruments efficiently |
| Sterile technique | To prevent infection and maintain field |
| Teamwork and communication | To work smoothly with surgeon and team |
| Crisis management | To act quickly during surgical emergencies |
📑 LEGAL AND ETHICAL RESPONSIBILITIES
- Ensure count protocols are strictly followed
- Maintain patient confidentiality
- Report any break in sterility or errors immediately
- Avoid negligence in handling instruments or tissue
- Document truthfully and responsibly
✅ SUMMARY TABLE: DUTIES OF SCRUB NURSE
| Phase | Duties |
|---|---|
| Pre-operative | Scrubbing, sterile field setup, instrument check, count |
| Intra-operative | Instrument handling, aseptic maintenance, count, specimen handling |
| Post-operative | Final count, instrument care, documentation, sterile field breakdown |
👩⚕️ CIRCULATING NURSE IN OT – DUTIES & RESPONSIBILITIES

✅ WHO IS A CIRCULATING NURSE?
A circulating nurse is a non-sterile member of the OT team responsible for overall coordination, patient care, safety, documentation, and maintaining the sterile environment without directly participating in the surgical field.
🎯 OBJECTIVES OF A CIRCULATING NURSE
- Ensure smooth workflow during surgery
- Provide support to the surgical and sterile team
- Maintain patient safety and dignity
- Assist with preparation, documentation, and emergency support
📋 DUTIES AND RESPONSIBILITIES OF A CIRCULATING NURSE
🔹 1. Pre-Operative Responsibilities
| Task | Description |
|---|---|
| 1.1 OT preparation | Ensures cleanliness, arranges equipment and supplies |
| 1.2 Patient verification | Confirms patient ID, consent form, surgical site, and allergies |
| 1.3 Equipment checks | Checks working condition of monitors, lights, suction, cautery, and anesthesia machine |
| 1.4 Aseptic setup support | Opens sterile packs and supplies for scrub nurse while maintaining sterility |
| 1.5 Patient transfer | Assists in safe shifting and positioning of the patient onto the OT table with support pads |
| 1.6 Skin prep | Assists in prepping the surgical site with antiseptic under sterile guidance |
| 1.7 Informed consent | Confirms and verifies that signed consent is present in file |
🔹 2. Intra-Operative Responsibilities
| Task | Description |
|---|---|
| 2.1 Assist sterile team | Passes extra supplies, medications, and solutions as needed |
| 2.2 Patient monitoring | Assists anesthesiologist in monitoring patient’s vitals and responses |
| 2.3 Count coordination | Assists in counting sponges, sharps, and instruments with scrub nurse |
| 2.4 Specimen care | Labels, documents, and sends surgical specimens to lab with proper identification |
| 2.5 Equipment adjustments | Controls OR lights, monitors, warming devices, suction settings, etc. |
| 2.6 Documentation | Maintains intraoperative records like surgery start/end time, medications given, any incidents |
| 2.7 Environmental safety | Ensures OT temperature, humidity, and lighting are optimal and safe |
🔹 3. Post-Operative Responsibilities
| Task | Description |
|---|---|
| 3.1 Patient transfer | Assists in shifting patient to recovery/PACU along with anesthetist and staff |
| 3.2 Waste disposal | Disposes of used materials in proper biomedical waste bins |
| 3.3 OT reset | Helps in preparing OT for the next case – changes linen, disposes waste, restocks items |
| 3.4 Documentation completion | Final recording in OT register, count sheets, and surgical records |
| 3.5 Incident reporting | Reports any break in asepsis, count discrepancy, or patient-related event immediately |
🩺 ADDITIONAL RESPONSIBILITIES
| Responsibility | Description |
|---|---|
| Communication bridge | Coordinates between scrub team, anesthetist, lab, blood bank, ICU |
| Emotional support | Provides reassurance to the patient pre-op, especially in awake or spinal cases |
| Infection control | Ensures hand hygiene, restricts OT traffic, and monitors sterile practice compliance |
| Fire and safety checks | Verifies electrical safety, presence of fire extinguishers, and crash cart readiness |
💡 KEY SKILLS REQUIRED
| Skill | Importance |
|---|---|
| Knowledge of surgical procedures | To anticipate needs of the team |
| Good communication | Essential for coordination and reporting |
| Observation and alertness | To detect patient or equipment issues |
| Documentation accuracy | Legal and clinical importance |
| Empathy and calmness | To support patient and team under stress |
📑 LEGAL AND ETHICAL RESPONSIBILITIES
- Verify informed consent and patient identity
- Report breaks in sterility or errors
- Maintain accurate legal documentation
- Protect patient privacy and dignity
- Participate in time-out and safety checklists (e.g., WHO Surgical Safety Checklist)
📝 SUMMARY TABLE: CIRCULATING NURSE DUTIES
| Phase | Key Responsibilities |
|---|---|
| Pre-operative | OT setup, patient verification, equipment checks, assisting with sterile setup |
| Intra-operative | Supplies assistance, count coordination, documentation, environment monitoring |
| Post-operative | Waste disposal, patient transfer, OT cleaning, documentation |
🛏️ POSITIONING AND DRAPING FOR COMMON SURGICAL PROCEDURES
✅ INTRODUCTION
Positioning is the technique of placing the patient on the OT table in a way that provides maximum access to the surgical site, while ensuring safety, comfort, and physiological stability.
Draping is the process of covering the patient and surrounding areas with sterile cloths (drapes) after positioning, to create a sterile field and expose only the operative site.
🎯 PURPOSE OF POSITIONING & DRAPING
✳️ Positioning:
- Provide access to surgical site
- Maintain patient’s airway, circulation, and safety
- Prevent nerve damage, pressure ulcers, and musculoskeletal strain
✳️ Draping:
- Maintain aseptic technique
- Isolate surgical area
- Protect the patient’s privacy and body temperature
🛏️ COMMON SURGICAL POSITIONS WITH DETAILS
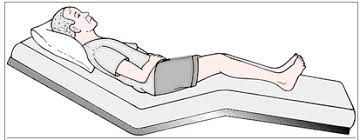
🔹 1. Supine (Dorsal Recumbent) Position
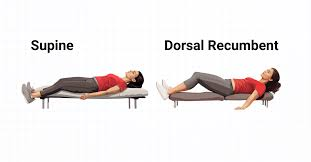
| Details | Description |
|---|---|
| Used for | Abdominal surgeries (e.g., hernia, appendectomy, laparotomy), thoracic surgery, cardiac, breast |
| Positioning | Lying flat on back, arms secured, legs extended |
| Sites Exposed | Abdomen, chest, pelvis |
| Risks | Pressure on heels, sacrum; possible back pain |
| Nursing Role | Pad bony prominences, secure arms, check ECG leads |
🔹 2. Lithotomy Position

| Details | Description |
|---|---|
| Used for | Gynecological (D&C, hysterectomy), urological (cystoscopy), rectal surgeries |
| Positioning | Supine + legs flexed in stirrups above level of hips |
| Sites Exposed | Perineum, rectum, lower pelvis |
| Risks | Nerve injury (femoral/sciatic), hip dislocation, hypotension |
| Nursing Role | Raise legs simultaneously, pad stirrups, check circulation post-op |
🔹 3. Prone Position
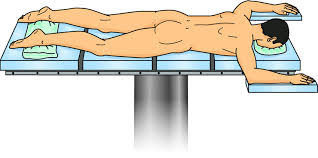
| Details | Description |
|---|---|
| Used for | Spine surgeries, rectal surgeries, posterior head/neck |
| Positioning | Patient lies face-down, arms extended or tucked |
| Sites Exposed | Back, neck, spine, buttocks |
| Risks | Respiratory compromise, pressure on face/chest/genitals |
| Nursing Role | Protect airway, pad face and bony areas, avoid eye/nerve compression |
🔹 4. Lateral (Sims or Kidney) Position
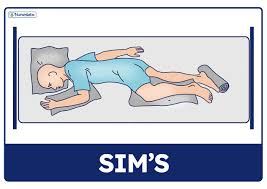
| Details | Description |
|---|---|
| Used for | Kidney, lung, hip surgeries |
| Positioning | Side-lying with lower arm flexed, upper leg flexed |
| Sites Exposed | Flank, thorax, lateral abdomen |
| Risks | Nerve damage, shoulder pressure, lung compression |
| Nursing Role | Place pillow between legs, secure patient, support chest and head |
🔹 5. Trendelenburg Position

| Details | Description |
|---|---|
| Used for | Pelvic/gynecologic surgeries, laparoscopic procedures |
| Positioning | Supine with table tilted head-down (15–30°) |
| Sites Exposed | Pelvis and lower abdomen |
| Risks | Respiratory distress, increased ICP, aspiration |
| Nursing Role | Secure patient with shoulder braces, monitor airway and circulation |
🔹 6. Reverse Trendelenburg

| Details | Description |
|---|---|
| Used for | Head and neck surgeries, laparoscopic upper abdominal |
| Positioning | Supine with table tilted head-up |
| Sites Exposed | Upper abdomen, head, neck |
| Risks | Hypotension, pooling of blood in lower limbs |
| Nursing Role | Secure patient, use anti-embolism stockings if needed |
🔹 7. Fowler’s or Semi-Fowler’s Position
| Details | Description |
|---|---|
| Used for | Craniotomy, thyroidectomy, shoulder or facial surgery |
| Positioning | Head of table elevated 45–90°, knees may be flexed |
| Sites Exposed | Head, neck, chest |
| Risks | Venous pooling in lower body, pressure ulcers |
| Nursing Role | Support head and neck, pad pressure areas, ensure secure straps |
🧼 DRAPING TECHNIQUES IN OT
✅ Principles of Draping:
- Sterile to sterile only
- Handle drapes by corners only
- Avoid touching non-sterile areas
- Drape from the operative site outward
- Use waterproof adhesive drapes when needed
✅ Types of Drapes:
| Drape Type | Use |
|---|---|
| Fenestrated Drape | Central opening for the operative site (e.g., hernia, cataract) |
| Non-Fenestrated Drapes | Used to cover large body areas |
| Laparotomy Sheet | Abdominal surgeries |
| Leggings | Used in lithotomy position |
| Head Drapes | Craniotomies, ENT procedures |
📝 NURSING RESPONSIBILITIES DURING POSITIONING & DRAPING
| Phase | Responsibilities |
|---|---|
| Before Surgery | Identify surgical site, explain procedure, inspect skin integrity |
| During Positioning | Use correct position, apply safety straps, pad bony prominences |
| During Draping | Maintain asepsis, assist surgeon, prevent exposure of non-surgical sites |
| Post-Positioning | Check for pressure areas, evaluate limb circulation and nerve compression |
🔄 SUMMARY TABLE: POSITION, PROCEDURE & PRECAUTIONS
| Position | Procedure Example | Site Exposed | Key Precautions |
|---|---|---|---|
| Supine | Hernia, C-section | Abdomen | Pad heels/sacrum |
| Lithotomy | Hysterectomy, D&C | Perineum | Pad legs, avoid nerve stretch |
| Prone | Spinal surgery | Back | Protect face, chest, genitals |
| Lateral | Nephrectomy | Flank | Support shoulders, hips |
| Trendelenburg | Laparoscopy (pelvis) | Pelvis | Risk of aspiration, eye pressure |
| Reverse Trend. | Thyroidectomy | Head/upper abdomen | Monitor BP, pad feet |
| Fowler’s | Craniotomy | Head, chest | Support head, prevent slumping |
🛠️ COMMON SURGICAL INSTRUMENTS USED IN DIFFERENT TYPES OF SURGERIES

✅ CLASSIFICATION OF SURGICAL INSTRUMENTS
Surgical instruments are commonly classified based on their function:
- Cutting and Dissecting Instruments
- Grasping and Holding Instruments
- Clamping and Occluding Instruments
- Retracting and Exposing Instruments
- Suturing Instruments
- Miscellaneous Instruments
📋 CHART: SURGICAL INSTRUMENTS – TYPES, USES, & EXAMPLES
| Type of Surgery | Common Instruments Used | Purpose / Use |
|---|---|---|
| General Surgery | – Scalpel (No.10, 11) – Dissecting forceps – Mosquito forceps – Mayo scissors – Needle holder – Sponge holding forceps | – Incision and tissue dissection – Holding tissues – Clamping small vessels – Suturing wounds |
| Gynecological Surgery | – Vulsellum forceps – Sim’s speculum – Uterine sound – Hegar’s dilator – Curette | – Cervical grasping – Vaginal examination – Uterine cavity measurement and dilation |
| Orthopedic Surgery | – Bone cutter – Bone nibbler – Periosteal elevator – Gigli saw – Bone holding forceps | – Cutting bone – Lifting periosteum – Sawing bone – Holding fractured segments |
| Neurosurgery | – Hudson brace and burr – Dural scissors – Raney clips – Kerrison punch – Nerve hook | – Skull drilling – Dura cutting – Scalp bleeding control – Bone removal – Nerve lifting |
| ENT Surgery | – Tilley’s forceps – Nasal speculum – Laryngeal mirror – Tonsil snare – Mastoid gouge | – Foreign body removal – Examining nasal cavity – View vocal cords – Tonsil excision – Mastoidectomy |
| Urological Surgery | – Cystoscope – Lithotrite – Bladder sound – Stone forceps – Catheter introducer | – Bladder inspection – Crushing stones – Detecting bladder pathology – Removing calculi |
| Cardiac Surgery | – Rib retractor – Sternal saw – Vascular clamp – Coronary artery probe | – Rib spreading – Cutting sternum – Clamping vessels – Identifying coronary artery |
| Laparoscopic Surgery | – Veress needle – Trocars & cannulas – Laparoscope – Graspers – Endo-scissors | – Pneumoperitoneum – Port access – Internal visualization – Tissue handling |
| Plastic Surgery | – Iris scissors – Fine forceps – Skin hook – Dermatome | – Delicate cutting – Handling fine tissues – Skin grafting |
🔹 SELECTED INSTRUMENTS WITH THEIR USES
| Instrument Name | Category | Primary Use |
|---|---|---|
| Scalpel | Cutting | Making skin/tissue incisions |
| Mayo Scissors | Cutting | Cutting heavy tissues |
| Metzenbaum Scissors | Cutting | Dissecting delicate tissue |
| Mosquito Forceps | Clamping | Clamping small vessels |
| Allis Forceps | Grasping/Holding | Holding soft tissues |
| Kocher’s Forceps | Grasping/Holding | Firm tissue grasping |
| Needle Holder | Suturing | Holding needle during stitching |
| Retractors (Langenbeck, Deaver, Balfour) | Retracting | To retract body wall or organs |
| Sponge Holding Forceps | Miscellaneous | Holding sponges for cleaning or antisepsis |
| Suction Tip (Yankauer, Poole) | Suction | Removing fluids/blood from site |
🧼 STERILIZATION OF INSTRUMENTS
| Instrument Type | Recommended Sterilization Method |
|---|---|
| Metal instruments | Autoclaving (steam under pressure) |
| Endoscopic tools | Gas sterilization (ETO) or plasma |
| Scopes (e.g., laparoscope) | Cold chemical sterilization or high-level disinfection |
📝 NURSING RESPONSIBILITIES RELATED TO SURGICAL INSTRUMENTS
- Count instruments before and after surgery with scrub nurse
- Handle instruments with aseptic technique
- Inspect instruments for functionality, rust, breakage
- Send used instruments for cleaning and sterilization
- Maintain instrument tray sets per type of surgery
- Record in instrument count sheet and register
📌 TIPS TO REMEMBER FOR EXAMS / VIVA
- Scalpel = Skin incision
- Kocher = Grasp firmly
- Langenbeck = Retract soft tissue
- Needle holder = Suturing
- Trocars = Entry in laparoscopy
🛠️ COMMON SURGICAL EQUIPMENTS WITH THEIR USES
✅ DEFINITION
Surgical equipment refers to non-handheld medical machines or devices used to support various surgical procedures by providing functions like lighting, suction, imaging, monitoring, or sterilization.
📋 TABLE: COMMON EQUIPMENT USED IN DIFFERENT SURGERIES
| Type of Surgery | Common Equipment Used | Purpose / Use |
|---|---|---|
| General Surgery | – Electrocautery machine – Suction machine – Surgical lights – Anesthesia machine | – Cuts or coagulates tissue – Removes blood or fluids – Illuminates surgical field – Administers anesthesia gases |
| Laparoscopic Surgery | – Insufflator – Laparoscope with camera & monitor – Trocars and cannulas – Light source and fiber optic cable | – Maintains CO₂ pneumoperitoneum – Internal visualization – Port access – Provides light for laparoscopy |
| Orthopedic Surgery | – C-arm (Image Intensifier) – Orthopedic drill – Bone saw or oscillating saw – Bone plating system | – Real-time imaging of bones – Drilling screws into bone – Cutting bone – Fracture fixation |
| Neurosurgery | – Operating microscope – CUSA (Ultrasonic aspirator) – Neuro navigation system | – Magnifies delicate structures – Removes brain tumors safely – Real-time brain mapping during surgery |
| ENT Surgery | – Endoscope (nasal/laryngeal) – Suction cautery unit – Microscope (for ear) | – Visualization of cavities – Removes bleeding tissue – Ear surgeries (e.g., tympanoplasty) |
| Cardiac Surgery | – Heart-lung bypass machine – Defibrillator – Thermal blanket (warming unit) | – Takes over heart/lung function – Manages cardiac arrest – Maintains body temperature |
| Gynecological Surgery | – Colposcope – Hysteroscope – Electrosurgical unit – Suction curettage unit | – Cervical/vaginal visualization – Uterine endoscopy – Cauterization/cutting tissue |
| Urological Surgery | – Cystoscope with monitor – Lithotripter (ESWL) – Uroflowmetry machine | – Bladder inspection – Break kidney/bladder stones – Measure urine flow |
| Plastic Surgery | – Dermatome – Skin graft mesher – Laser unit (CO₂ laser) | – Skin harvesting – Expands grafts – Precision cutting or resurfacing |
| Emergency/Trauma Surgery | – Portable suction – Crash cart with defibrillator – Portable X-ray machine | – Airway clearance – Life-saving resuscitation – Emergency imaging |
🧰 OTHER ESSENTIAL OT EQUIPMENT (Used Across All Surgeries)
| Equipment Name | Use |
|---|---|
| Operating table | Adjustable table to position patient for surgery |
| Shadowless surgical lights | Provide high-intensity, shadow-free illumination |
| Anesthesia machine | Delivers inhalational agents and oxygen |
| Multiparameter monitor | Displays vital signs (BP, ECG, SpO₂, Temp) |
| Infusion pumps | Delivers fluids/medications at controlled rate |
| Suction apparatus | Removes fluids, blood from surgical site |
| Electrocautery/Diathermy unit | Cuts tissue or coagulates bleeding vessels |
| Sterilizer (Autoclave) | Sterilizes surgical instruments before use |
| Fumigator or UV Light | Maintains asepsis in OT environment |
| Bair Hugger (Warming device) | Prevents hypothermia during long surgeries |
📝 NURSING RESPONSIBILITIES RELATED TO SURGICAL EQUIPMENT
| Phase | Responsibilities |
|---|---|
| Pre-operative | Check equipment functionality, ensure availability, calibrate machines |
| Intra-operative | Monitor settings, assist in operation, alert for alarms/malfunction |
| Post-operative | Turn off, clean, and send for sterilization or maintenance as required |
| Documentation | Record equipment usage, serial numbers (if applicable), malfunctions |
🛑 SAFETY PRECAUTIONS FOR EQUIPMENT USE
- Use checklist before surgery (WHO Surgical Safety)
- Avoid fluid contact with electrical equipment
- Label and report faulty machines immediately
- Maintain battery back-up and power supply
- Trained staff only should operate specialized equipment
🧾 SUMMARY CHART – EQUIPMENT SNAPSHOT
| Surgery Type | Key Equipment | Main Use |
|---|---|---|
| Laparoscopic | Laparoscope, insufflator | Internal view, CO₂ access |
| Orthopedic | C-arm, drill, saw | Bone cutting and fixation |
| Cardiac | Heart-lung machine, defib | Pumping and emergency response |
| ENT | Endoscope, microscope | Ear/nose/throat surgeries |
| Gynecology | Colposcope, hysteroscope | Visualize cervix and uterus |
| Plastic | Dermatome, laser unit | Skin grafting and shaping |
🧵 SUTURES.

✅ DEFINITION
A suture is a thread-like medical device used to approximate (bring together) body tissues after injury or surgery to promote healing and prevent infection.
Sutures are used to ligate blood vessels or close surgical incisions, wounds, or lacerations.
🔍 TYPES OF SUTURES
Sutures are classified based on absorbability, origin, structure, and material.
🔹 1. Based on Absorbability
| Type | Description | Examples |
|---|---|---|
| Absorbable Sutures | Get broken down and absorbed by body enzymes over time | – Catgut (plain, chromic) – Vicryl (polyglactin) – Monocryl – PDS |
| Non-absorbable Sutures | Not absorbed by the body; require manual removal or are left permanently | – Silk – Nylon – Prolene – Stainless steel wire |
🔹 2. Based on Structure
| Type | Description | Features |
|---|---|---|
| Monofilament | Single, smooth strand | Less tissue drag, less infection risk |
| Multifilament (Braided) | Multiple strands twisted/braided together | Stronger, more knot security but more infection risk |
🔹 3. Based on Material Source
| Type | Description | Examples |
|---|---|---|
| Natural Sutures | Derived from organic sources | – Catgut (sheep intestine) – Silk |
| Synthetic Sutures | Man-made, polymer-based | – Vicryl – Nylon – Prolene – Monocryl |
🧰 COMMON SUTURE MATERIALS & USES
| Suture Material | Type | Common Use |
|---|---|---|
| Plain Catgut | Absorbable, natural | Mucosal closure, ligating small vessels |
| Chromic Catgut | Absorbable, treated | Peritoneum, GI surgeries |
| Vicryl (Polyglactin 910) | Absorbable, synthetic | Skin, muscle, bowel anastomosis |
| Nylon | Non-absorbable, synthetic | Skin closure, plastic surgery |
| Silk | Non-absorbable, natural | Ligatures, general closure (not often used today) |
| Prolene (Polypropylene) | Non-absorbable, synthetic | Vascular surgery, fascia closure |
| Stainless Steel Wire | Non-absorbable, metal | Bone fixation, sternum, orthopedic use |
🛠️ TYPES OF SUTURING TECHNIQUES
| Technique | Use Case |
|---|---|
| Simple interrupted | Most common; general skin closure |
| Continuous (running) | Fast closure; bowel, fascia |
| Subcuticular suture | Cosmetic skin closure; plastic surgery |
| Mattress suture (vertical/horizontal) | Provides tension relief; scalp, high tension areas |
| Purse-string suture | Circular wound closure; anus, stoma |
| Figure-of-eight suture | Hemostasis; muscle, tendon fixation |
📋 INDICATIONS OF SUTURE USE
- To close surgical incisions after operations
- To approximate wound edges and promote healing
- To ligate bleeding vessels
- To close deep internal layers (muscle, fascia)
- For cosmetic skin closure (e.g., face, breast)
- In trauma cases (lacerations, cuts)
🚫 CONTRAINDICATIONS / PRECAUTIONS
Sutures may be avoided or used cautiously in the following cases:
| Situation | Reason / Alternative |
|---|---|
| Contaminated or infected wounds | May trap infection; consider delayed closure or staples |
| Allergy to suture material (e.g., catgut) | Use synthetic hypoallergenic sutures |
| Wounds under tension | May cause dehiscence; mattress sutures or tension sutures preferred |
| Oozing or bleeding site | Secure hemostasis before suturing |
| Poor vascular supply (e.g., diabetic foot) | Risk of necrosis; suture sparingly |
🧼 NURSING RESPONSIBILITIES IN SUTURING
| Phase | Responsibilities |
|---|---|
| Before | Prepare sterile suture tray, ensure correct suture material and size |
| During | Assist surgeon, handle instruments, maintain asepsis |
| After | Document type/size of suture, observe site for bleeding/infection |
| Suture Removal | Remove non-absorbable sutures as per doctor’s order (usually 5–10 days) |
| Patient Education | Teach wound care, signs of infection, follow-up for suture removal |
📌 SUTURE SIZES (USP SYSTEM)
| Size | Thickness | Common Use |
|---|---|---|
| 0, 1 | Thick | Fascia, tendon |
| 2-0, 3-0 | Medium | Muscle, skin |
| 4-0, 5-0 | Fine | Face, delicate skin |
| 6-0 to 10-0 | Ultra-fine | Microsurgery, eyes, vessels |
✳️ Higher the number, thinner the suture!
📝 SUMMARY CHART
| Category | Types/Examples |
|---|---|
| Absorbable | Catgut, Vicryl, Monocryl, PDS |
| Non-absorbable | Nylon, Silk, Prolene, SS wire |
| Natural | Catgut, Silk |
| Synthetic | Nylon, Vicryl, Prolene |
| Monofilament | Nylon, Prolene |
| Braided | Silk, Vicryl |
🧵 SUTURING:
✅ DEFINITION OF SUTURING
Suturing is the surgical act of stitching body tissues (usually skin, muscles, or organs) together using sutures (threads) to close wounds/incisions and promote healing.
🧰 SUTURING EQUIPMENT (Suture Tray Contents)
| Instrument/Item | Purpose |
|---|---|
| Needle Holder | Holds and drives the suture needle through tissue |
| Surgical Sutures (threads) | For stitching (absorbable or non-absorbable) |
| Suture Needles | Attached to thread; various shapes (e.g., curved, straight) |
| Tissue Forceps (Toothed) | Holds skin/tissue while suturing |
| Scissors (Suture/Dissecting) | Cuts thread or tissue |
| Gauze and Sponge | Cleans blood, maintains visibility |
| Antiseptic Solution | Cleansing and disinfection |
| Gloves and Sterile Drapes | For asepsis |
| Sterile Dressing Material | To cover the wound post-procedure |
✂️ COMMON SUTURE TECHNIQUES
| Technique | Use |
|---|---|
| Simple Interrupted | Skin closure (most common) |
| Continuous (Running) | Long incisions (e.g., bowel, fascia) |
| Subcuticular | Cosmetic closure, minimal scarring |
| Vertical Mattress | High-tension wounds |
| Horizontal Mattress | Fragile skin (e.g., elderly, scalp) |
| Purse-string | Circular openings (e.g., drain sites) |
| Figure-of-eight | Hemostasis in vessels/tendons |
🩺 PROCEDURE STEPS FOR SUTURING
(Aseptic technique must be followed throughout)
🔹 1. Preparation
- Verify doctor’s order for suturing
- Explain procedure to the patient
- Position patient comfortably
- Perform hand hygiene and wear sterile gloves
- Prepare and arrange sterile suture tray
🔹 2. Wound Cleaning
- Clean wound with antiseptic solution (inside to outside)
- Ensure hemostasis (bleeding is controlled)
🔹 3. Anesthetize the Area
- Apply local anesthesia if ordered (e.g., lignocaine)
🔹 4. Suturing Technique
- Hold needle with needle holder at 1/3 distance from the tip
- Use forceps to lift tissue gently
- Pass needle through tissue in a curved motion (entry ~1 cm from wound edge)
- Tie knot securely (usually surgeon’s knot or square knot)
- Cut excess suture ~0.5–1 cm above the knot
- Repeat per required suture technique
🔹 5. Completion
- Final cleaning of suture area
- Apply sterile dressing
- Label dressing with date/time/type of suture
- Discard sharps and used items in biohazard containers
👩⚕️ ROLE OF NURSE IN SUTURING
🟢 Before Procedure
- Prepare patient and explain procedure
- Assemble sterile suture tray
- Maintain sterile environment
- Check for allergies to suture material or anesthesia
🟢 During Procedure
- Assist the surgeon by:
- Passing instruments
- Holding tissue with forceps
- Controlling bleeding with gauze
- Monitor patient’s comfort and vital signs
- Maintain strict asepsis
🟢 After Procedure
- Apply and secure dressing
- Dispose sharps/instruments properly
- Clean and restock instruments
- Document:
- Type of suture, number of sutures applied
- Site and condition of wound
- Patient’s response
🟢 During Suture Removal (If needed later)
- Remove non-absorbable sutures using:
- Suture removal scissor and forceps
- Cut close to skin, pull suture gently
- Observe for signs of infection, gaping, bleeding
- Re-dress wound if needed
- Record suture removal in nursing notes
📌 STERILE TECHNIQUE TIPS
- Always face the sterile field
- Do not cross over sterile tray
- Change gloves if contaminated
- Use sterile dressing after suturing
- Use count protocol if suturing internal structures
📝 DOCUMENTATION SAMPLE (Nursing Record)
✅ “Wound sutured at 10:30 AM by Dr. X using 3-0 Nylon. 6 interrupted sutures applied. No bleeding noted. Dressing applied. Patient tolerated well. Informed for suture removal on 7th day. – Nurse’s Name”
🧾 SUMMARY TABLE
| Step | Action |
|---|---|
| 1 | Prepare sterile tray & patient |
| 2 | Clean wound |
| 3 | Apply local anesthesia |
| 4 | Perform suturing as per technique |
| 5 | Apply dressing |
| 6 | Document and clean area |
🧵 SUTURE MATERIALS –
✅ DEFINITION
Suture material refers to the thread or strand used to approximate tissues, ligate vessels, and support wound healing after a surgical incision or injury.
🧬 CLASSIFICATION OF SUTURE MATERIALS
🔹 1. Based on Absorbability
| Type | Description | Examples |
|---|---|---|
| Absorbable | Broken down and absorbed by body enzymes or hydrolysis | Catgut, Vicryl, Monocryl, PDS |
| Non-Absorbable | Remains in body indefinitely or needs removal | Nylon, Silk, Prolene, Stainless Steel |
🔹 2. Based on Material Origin
| Type | Description | Examples |
|---|---|---|
| Natural | Derived from organic substances | Catgut (sheep intestine), Silk (silkworm) |
| Synthetic | Man-made polymers | Vicryl (polyglactin), Nylon, Prolene, Monocryl |
🔹 3. Based on Structure
| Type | Description | Features |
|---|---|---|
| Monofilament | Single smooth strand | Less tissue drag, less infection risk |
| Multifilament (Braided) | Multiple fibers twisted or braided | Better knot security, but higher infection risk |
📋 DETAILED CHART: COMMON SUTURE MATERIALS
| Suture Material | Absorbability | Origin | Structure | Common Uses |
|---|---|---|---|---|
| Plain Catgut | Absorbable (7–10 days) | Natural | Monofilament | Mucosa, ligatures |
| Chromic Catgut | Absorbable (10–20 days) | Natural | Monofilament | Peritoneum, internal tissue |
| Vicryl (Polyglactin 910) | Absorbable (30–90 days) | Synthetic | Braided | Muscle, fascia, skin |
| Monocryl | Absorbable (20–30 days) | Synthetic | Monofilament | Subcuticular skin closure |
| PDS (Polydioxanone) | Absorbable (up to 180 days) | Synthetic | Monofilament | Deep abdominal wall, pediatric |
| Silk | Non-absorbable | Natural | Braided | Ligatures, GI tract, drains (not commonly used now) |
| Nylon (Ethilon) | Non-absorbable | Synthetic | Monofilament | Skin, plastic surgery |
| Prolene (Polypropylene) | Non-absorbable | Synthetic | Monofilament | Vascular surgery, hernia |
| Stainless Steel Wire | Non-absorbable | Metal | Monofilament or twisted | Orthopedic, sternal closure |
🩺 PROPERTIES OF IDEAL SUTURE MATERIAL
A good suture material should be:
- Sterile
- Tensile strength adequate for tissue
- Minimal tissue reaction
- Easy to handle and knot
- Absorbable or non-absorbable as needed
- Non-toxic, non-allergenic, and economical
📏 SUTURE SIZES (USP SCALE)
| Size | Diameter | Use |
|---|---|---|
| 0, 1 | Thick | Fascia, tendon, ligatures |
| 2-0, 3-0 | Medium | Skin, muscle |
| 4-0, 5-0 | Fine | Face, cosmetic closure |
| 6-0 to 10-0 | Ultra-fine | Ophthalmic, vascular, microsurgery |
📌 Higher the number, thinner the suture (e.g., 6-0 is thinner than 3-0).
📦 PACKAGING OF SUTURE MATERIALS
- Pre-packed sterile packs
- Types: With needle attached (swaged) or without needle (ligature)
- Can be in individual packets or reels
- Marked with:
- Type (absorbable/non)
- Size (USP or metric)
- Needle type (cutting, round, etc.)
- Expiry date
🧵 TYPES OF NEEDLES USED WITH SUTURES
| Needle Type | Shape | Use |
|---|---|---|
| Cutting Needle | Triangular, sharp | Skin, tough tissues |
| Reverse Cutting | Strengthened cutting edge | Cosmetic, skin |
| Taper Point (Round) | Smooth, round body | Soft tissues (muscle, bowel) |
| Blunt Point | Rounded tip | Liver, friable tissues |
💡 SELECTION CRITERIA FOR SUTURE MATERIAL
| Factor | Preferred Suture |
|---|---|
| Skin closure | Nylon, Prolene (non-absorbable) |
| Deep tissue | Vicryl, PDS (absorbable) |
| Vascular surgery | Prolene (non-absorbable) |
| Mucosa (oral, GI) | Plain catgut |
| Tendon repair | PDS, strong non-absorbables |
| Cosmetic surgery | Subcuticular Monocryl or fine Nylon (6-0, 5-0) |
| Pediatric surgery | Absorbable (Monocryl, Vicryl) preferred |
👩⚕️ NURSE’S ROLE IN HANDLING SUTURE MATERIALS
- Select appropriate size/type as per procedure
- Open suture packs using aseptic technique
- Assist surgeon in threading or passing needle
- Count and document number of sutures used
- Dispose of needles in sharps box
- Monitor for allergic reactions or inflammation
📝 SUMMARY TABLE
| Classification Basis | Types/Examples |
|---|---|
| Absorbable | Catgut, Vicryl, Monocryl, PDS |
| Non-absorbable | Nylon, Silk, Prolene, Steel |
| Natural | Catgut, Silk |
| Synthetic | Vicryl, Nylon, PDS |
| Monofilament | Nylon, Prolene, Monocryl |
| Braided | Silk, Vicryl |
🧼 DISINFECTION OF INSTRUMENTS AND EQUIPMENT

✅ DEFINITION
Disinfection is the process of eliminating most pathogenic microorganisms (except spores) from inanimate objects such as instruments and equipment by using chemical agents or physical methods.
🔴 Disinfection ≠ Sterilization
Disinfection kills most microbes, not spores, while sterilization kills all forms of microbial life.
🧪 CLASSIFICATION OF DISINFECTION (Based on Efficacy)
| Level of Disinfection | Microbial Effect | Use |
|---|---|---|
| High-Level | Kills all organisms except spores | Endoscopes, respiratory equipment |
| Intermediate-Level | Kills TB bacteria, most viruses, fungi | Laryngoscope blades, suction tips |
| Low-Level | Kills some bacteria and viruses | BP cuffs, bed rails, stethoscopes |
🧰 TYPES OF INSTRUMENTS & DISINFECTION METHOD
| Instrument Type | Disinfection Method |
|---|---|
| Critical items (enter sterile tissue) | Sterilization (not disinfection) |
| Semi-critical items (contact mucous membranes) | High-level disinfection |
| Non-critical items (contact intact skin) | Low/intermediate disinfection |
🧴 COMMON CHEMICAL DISINFECTANTS USED
| Disinfectant | Type | Uses |
|---|---|---|
| Glutaraldehyde (2%) | High-level | Endoscopes, anesthesia tools (20 mins) |
| Hydrogen Peroxide (6-25%) | High-level | Cold sterilant for delicate equipment |
| Chlorine (Sodium Hypochlorite) | Intermediate | Linen, floors, spills, blood cleanup |
| Alcohol (70% Isopropyl/Ethanol) | Intermediate | Thermometers, stethoscopes, skin |
| Phenol compounds | Low to Intermediate | Bedpans, furniture |
| Quaternary ammonium compounds (QACs) | Low-level | Surfaces, walls, mop handles |
🧼 METHODS OF DISINFECTION (Physical & Chemical)
🔹 Physical Methods
| Method | Description | Used For |
|---|---|---|
| Boiling (100°C for 10–20 mins) | Kills bacteria and viruses | Metal instruments, syringes |
| Pasteurization (70–80°C for 30 mins) | Low heat disinfection | Respiratory therapy items |
| UV Radiation | Damages DNA of microbes | Surface disinfection in OT |
| Hot Water Disinfection (65–75°C) | Often used in washer-disinfectors | Bedpans, utensils |
🔹 Chemical Methods
- Instruments are immersed in liquid disinfectants for specific contact time
- Examples: Glutaraldehyde (Cidex), Alcohol, Formalin, Hypochlorite
📝 STEPS FOR DISINFECTION OF INSTRUMENTS (General Protocol)
🔹 1. Pre-cleaning
- Remove blood, tissue, or debris using detergent and water
- Rinse thoroughly before applying disinfectant
🔹 2. Disinfection Process
- Select appropriate disinfectant
- Immerse instrument completely (no air bubbles)
- Maintain required contact time (e.g., 20 minutes for Glutaraldehyde)
🔹 3. Post-disinfection Handling
- Rinse with sterile water if needed (especially for chemical disinfectants)
- Dry and store in clean area or pack for further sterilization
⚠️ SAFETY PRECAUTIONS FOR DISINFECTION
- Wear gloves, mask, goggles while handling chemicals
- Use disinfectants in well-ventilated areas
- Follow MSDS (Material Safety Data Sheet) for each chemical
- Label chemical containers properly
- Do not mix different disinfectants
- Dispose of used chemicals per biomedical waste guidelines
👩⚕️ NURSE’S ROLE IN DISINFECTION
| Task | Responsibility |
|---|---|
| Selection | Choose appropriate disinfectant per instrument type |
| Preparation | Dilute chemical as per protocol |
| Monitoring | Ensure correct contact time & immersion |
| Safety | Use PPE and follow spill management protocols |
| Documentation | Maintain records of disinfection cycles, logs |
| Storage | Ensure proper drying and clean storage after disinfection |
🧾 SUMMARY TABLE
| Item | Disinfectant / Method | Contact Time |
|---|---|---|
| Endoscopes | 2% Glutaraldehyde | 20–30 mins |
| Thermometers | 70% Alcohol | 2–5 mins |
| Floors, beds, spills | 1% Hypochlorite | 10–15 mins |
| Respiratory items | Hot water / Pasteurize | 30 mins |
| Bedpans, urinals | Phenolic / QAC | 10 mins |
🔥 STERILIZATION OF INSTRUMENTS AND EQUIPMENTS

✅ DEFINITION
Sterilization is the process of destroying all forms of microbial life, including bacteria, viruses, fungi, and spores, on instruments, equipment, or surfaces using physical or chemical methods.
✅ Sterilization is essential for “critical items” (that enter sterile tissues, blood, or body cavities).
🎯 OBJECTIVES OF STERILIZATION
- To ensure patient safety by preventing infections
- To maintain a sterile environment in the OT and wards
- To protect healthcare workers from exposure
- To comply with hospital infection control standards
🧰 CLASSIFICATION OF INSTRUMENTS (Spaulding’s Classification)
| Instrument Type | Examples | Required Process |
|---|---|---|
| Critical Items | Surgical instruments, needles, implants | Sterilization |
| Semi-critical Items | Endoscopes, laryngoscopes | High-level disinfection |
| Non-critical Items | BP cuffs, thermometers | Cleaning or low-level disinfection |
🧪 METHODS OF STERILIZATION
🔹 1. PHYSICAL METHODS
| Method | Principle | Used For |
|---|---|---|
| Autoclaving (Steam under pressure) | 121°C at 15 psi for 15–20 mins or 134°C for 3–5 mins | Surgical instruments, linen, dressing trays |
| Dry Heat (Hot Air Oven) | 160°C–170°C for 1–2 hours | Glassware, metal, powders |
| Radiation (Gamma rays) | Ionizing radiation | Disposable syringes, catheters |
| Boiling (Not sterilization technically) | 100°C for 15–30 mins | Temporary disinfection only |
🔹 2. CHEMICAL METHODS
| Method | Common Chemicals | Used For |
|---|---|---|
| Gas Sterilization (ETO – Ethylene Oxide) | ETO gas | Heat-sensitive items, plastic, endoscopes |
| Chemical immersion | 2% Glutaraldehyde (Cidex), 6% Hydrogen Peroxide | Scopes, laryngoscope blades (with contact time: 6–10 hours for sterilization) |
⚠️ Chemical disinfection ≠ Sterilization, unless used with prolonged contact time (e.g., glutaraldehyde for >10 hrs).
🧪 AUTOCLAVE – MOST COMMON METHOD IN HOSPITALS
| Parameter | Standard Setting |
|---|---|
| Temperature | 121°C or 134°C |
| Pressure | 15 lbs (psi) |
| Time | 15–30 minutes depending on load |
| Items Used For | Gauze, gloves, surgical instruments |
✅ Steps in Autoclave Sterilization:
- Clean and dry instruments
- Pack in autoclave sheets or containers
- Load autoclave ensuring air space
- Set cycle with correct temp/time
- Check chemical indicator (tape color)
- Allow to cool, unload and store
- Record cycle in autoclave logbook
🧼 STERILIZATION INDICATORS
| Type | Purpose |
|---|---|
| Chemical Indicator | Tape that changes color (e.g., white to black) on exposure to correct conditions |
| Biological Indicator | Vials containing heat-resistant spores (e.g., Bacillus stearothermophilus) to confirm sterility |
| Mechanical Indicator | Checks temperature, pressure, and time inside sterilizer |
🟢 Biological indicators are gold standard.
🗂️ STORAGE OF STERILE ITEMS
- Store in clean, dry, dust-free cabinets
- Label with:
- Sterilization date
- Expiry date
- Initials of staff who packed it
- Follow First In, First Out (FIFO) principle
- Avoid touching sterile surfaces or wrapping
👩⚕️ ROLE OF NURSE IN STERILIZATION
✅ 1. Before Sterilization
- Clean and inspect instruments for damage
- Sort and arrange items into instrument sets
- Wrap or pouch items with autoclave indicators
- Label correctly with date and contents
✅ 2. During Sterilization
- Load autoclave correctly (don’t overload)
- Set correct time/temp/pressure
- Check function of sterilizer indicators
- Record details in sterilization logbook
✅ 3. After Sterilization
- Let items cool before opening autoclave
- Inspect chemical indicator for color change
- Store in designated sterile area
- Do not use wet packs or broken wrappings
- Maintain inventory and expiry tracking
🔄 STERILIZATION CYCLE (NURSE’S FLOW)
sqlCopyEditCleaning → Drying → Packaging →Indicator placement → Sterilization →Cooling → Storage → Issue/Use
📝 SUMMARY TABLE
| Sterilization Method | Items Used For | Key Points |
|---|---|---|
| Autoclave (steam) | Surgical tools, dressing, gloves | Fast, effective, most used |
| Hot Air Oven | Glassware, metal instruments | Longer time, for dry items |
| ETO Gas | Plastics, endoscopes | Toxic gas, long cycle |
| Gamma Radiation | Disposable syringes, IV sets | Done industrially |
| Chemical (Glutaraldehyde) | Scopes, delicate equipment | Requires long immersion time |
👩⚕️ ROLE OF NURSE IN DISINFECTION AND STERILIZATION
✅ DEFINITION
- Disinfection: The process of eliminating most pathogenic microorganisms (excluding spores) from instruments or surfaces using chemical or physical agents.
- Sterilization: A process that destroys all forms of microbial life, including bacterial spores, using heat, chemicals, or radiation.
🎯 OBJECTIVES OF NURSE’S ROLE
- To prevent healthcare-associated infections (HAIs)
- To ensure instruments are safe and sterile for patient care
- To follow infection control protocols and guidelines
- To maintain aseptic practices in all procedures
🧰 NURSE’S ROLE IN DISINFECTION OF INSTRUMENTS
| Phase | Responsibilities |
|---|---|
| Before Disinfection | |
| ✔ Sort instruments based on use (critical/semi/non-critical) | |
| ✔ Remove gross contamination (blood, secretions) | |
| ✔ Perform manual or mechanical pre-cleaning using detergent or enzymatic solution | |
| ✔ Use PPE (gloves, apron, mask) |
| During Disinfection |
✔ Prepare correct chemical disinfectant (right concentration and amount)
✔ Immerse instruments completely for required contact time
✔ Use closed container with label
✔ Ensure proper ventilation if using strong chemicals (e.g., glutaraldehyde)
| After Disinfection |
✔ Rinse instruments (especially if high-level disinfectant used)
✔ Dry with sterile cloth or air-dry
✔ Label and store in clean, dry, covered area
✔ Record disinfection date, chemical used, and next due date
🔥 NURSE’S ROLE IN STERILIZATION OF INSTRUMENTS
| Phase | Responsibilities |
|---|---|
| Preparation | |
| ✔ Arrange cleaned instruments into sets/trays | |
| ✔ Wrap using autoclave sheets, indicator tape, or pouches | |
| ✔ Check sterilizer (autoclave) for temperature, pressure, water level |
| During Sterilization |
✔ Load instruments without overpacking
✔ Run the autoclave for appropriate cycle and time
✔ Monitor biological/chemical indicators for sterility assurance
✔ Maintain sterilization logbook
| Post-Sterilization |
✔ Unload only when dry and cool
✔ Check indicator color change for sterility confirmation
✔ Label with date of sterilization and expiry date
✔ Store in dust-free, dry cabinets
📋 DOCUMENTATION RESPONSIBILITIES
- Maintain disinfection/sterilization logbooks
- Record:
- Item name and quantity
- Disinfection/sterilization date and method
- Name of person responsible
- Indicator test results
- Expiry date of sterile packs
- Update maintenance logs for sterilization equipment (autoclave, ETO, etc.)
🧼 MONITORING & QUALITY CONTROL
| Task | Nurse’s Role |
|---|---|
| Indicator Use | Apply chemical indicators (autoclave tape) on every pack |
| Sterility Tests | Ensure weekly biological indicator testing |
| Environmental Cleanliness | Supervise OT and CSSD hygiene |
| Storage | Ensure sterile items are stored correctly to avoid contamination |
⚠️ SAFETY PRECAUTIONS
- Never reuse unsterilized or improperly disinfected items
- Use PPE when handling chemicals (glutaraldehyde, phenol, bleach)
- Avoid cross-contamination by separating clean and used areas
- Properly dispose of outdated or contaminated sterile packs
- Follow hospital infection control committee (HICC) guidelines
📝 SUMMARY TABLE
| Area | Nurse’s Role |
|---|---|
| Pre-cleaning | Wash, rinse, sort instruments |
| Disinfection | Chemical preparation, contact time monitoring |
| Sterilization | Packing, autoclave handling, indicator check |
| Documentation | Maintain logs, labels, sterility records |
| Quality Control | Perform indicator tests, environmental cleaning |
| Safety & Storage | Use PPE, label packs, store correctly |
💡 TIPS FOR EXAM/VIVA
- Disinfection = kills most microbes, used for semi-critical items
- Sterilization = kills all microbes + spores, for critical items
- Autoclaving = best method for metal instruments
- Glutaraldehyde (Cidex) = used for scopes, high-level disinfection
- Chemical indicators = confirm sterilization by color change
- Biological indicators = confirm with spore destruction
🛠️ PREPARATION OF SETS FOR COMMON SURGICAL PROCEDURES

✅ OBJECTIVES OF SET PREPARATION
- To ensure availability of all necessary sterile instruments for a particular surgery
- To save time and improve workflow during surgery
- To promote infection control and aseptic technique
- To allow proper documentation and accountability
🧰 BASIC PRINCIPLES OF SET PREPARATION
- Clean, dry, and inspect all instruments before packing
- Arrange instruments in functional order of use (cutting, clamping, holding, suturing, etc.)
- Use autoclave sheets, wrappers, or boxes to pack
- Add chemical indicator tape/strip for sterilization verification
- Label pack with:
- Procedure name
- Date of sterilization
- Expiry date
- Initials of preparer
📦 COMMON SURGICAL SETS & CONTENTS
🔹 1. Minor Surgical Set
🟢 Used for suturing small wounds, abscess drainage, dressing changes.
| Instrument Name | Quantity |
|---|---|
| Artery forceps (mosquito) | 2 |
| Dissecting forceps (toothed & non-toothed) | 1 each |
| Scissors (straight, curved) | 1 each |
| Needle holder | 1 |
| Suture cutting scissors | 1 |
| Sponge holding forceps | 1 |
| Bowl (for antiseptic) | 1 |
| Towel clips | 2 |
| Kidney tray, gauze pieces, gloves, dressing pack | As required |
🔹 2. Major Surgical Set
🟢 Used for general open surgeries like hernia repair, laparotomy, appendectomy.
| Instrument Name | Quantity |
|---|---|
| Scalpel handle with blades | 1 |
| Artery forceps (medium & long) | 6–8 |
| Needle holder | 2 |
| Mayo scissors | 1 |
| Metzenbaum scissors | 1 |
| Dissecting forceps (toothed & non-toothed) | 1 each |
| Retractors (Langenbeck, Deaver) | 2–4 |
| Towel clips | 4 |
| Sponge holding forceps | 2 |
| Bowl (antiseptic/saline) | 2 |
| Surgical drapes, gauze, dressing items | As required |
🔹 3. Gynecological Set (D&C, Hysterectomy)
🟢 Used for dilation and curettage, uterine procedures.
| Instrument Name | Quantity |
|---|---|
| Sim’s speculum | 1 |
| Auvard weighted speculum | 1 |
| Vulsellum forceps | 1 |
| Uterine sound | 1 |
| Cervical dilators (Hegar’s or Hawkin-Ambler) | Full set |
| Curette (sharp and blunt) | 2 |
| Sponge holding forceps | 2 |
| Ovum forceps | 1 |
| Artery forceps | 4 |
| Bowl | 1 |
🔹 4. Cesarean Section (LSCS) Set
🟢 Used for lower segment C-section.
| Instrument Name | Quantity |
|---|---|
| Scalpel handle with blades | 1 |
| Artery forceps | 6–8 |
| Sponge holding forceps | 2 |
| Needle holder | 2 |
| Mayo scissors | 1 |
| Uterine forceps | 2 |
| Allis tissue forceps | 2 |
| Retractors (Doyen’s, Deaver) | 2 |
| Towel clips | 4 |
| Dressing materials, suction tip, catheter | As required |
🔹 5. Orthopedic Set (Fracture, Plating, Bone Surgery)
🟢 Used in fracture reduction, ORIF (open reduction & internal fixation).
| Instrument Name | Quantity |
|---|---|
| Bone holding forceps | 2–4 |
| Periosteal elevator | 1 |
| Bone nibbler | 1 |
| Bone cutter/saw | 1 |
| Drill machine + bits | 1 |
| Screwdriver and plates/screws | As required |
| Artery forceps | 4–6 |
| Retractors | 2–4 |
🔹 6. Laparoscopic Set (Basic)
🟢 Used in minimally invasive procedures like laparoscopic cholecystectomy, appendectomy.
| Instrument Name | Quantity |
|---|---|
| Veress needle | 1 |
| Trocar and cannula (5mm, 10mm) | 2–4 |
| Laparoscope with camera | 1 |
| Graspers, scissors, dissector | 2–4 |
| Clip applicator | 1 |
| Light source and fiber optic cable | 1 |
| Suction-irrigation cannula | 1 |
🧼 NURSING RESPONSIBILITIES IN SET PREPARATION
| Phase | Responsibilities |
|---|---|
| Before packing | Clean, inspect, and dry instruments thoroughly |
| During packing | Arrange instruments by category, use indicator strips, wrap securely |
| During sterilization | Load autoclave correctly, ensure correct temp/time |
| After sterilization | Check chemical indicators, label pack, store in sterile area |
| Before surgery | Verify expiry date, integrity of sterile pack, and count instruments |
✅ LABELING OF STERILE PACKS
A proper sterile pack should have:
- Name of the procedure (e.g., “Minor Surgical Set”)
- Date of sterilization
- Expiry date (usually 1 week for cloth pack, 30 days for sealed pouch)
- Initials of person who packed
- Chemical indicator tape across the pack
📝 SAMPLE LAYOUT: MINOR SURGICAL SET PACKING (ORDERED)
sqlCopyEditTop Layer:
✔ Gauze swabs
✔ Sponge-holding forceps
✔ Bowl
Middle Layer:
✔ Scissors
✔ Dissecting forceps
✔ Artery forceps
Bottom Layer:
✔ Needle holder
✔ Towel clips
+ Add suture material, gloves, dressing setas per requirement.
🧼 SCRUBBING PROCEDURE.
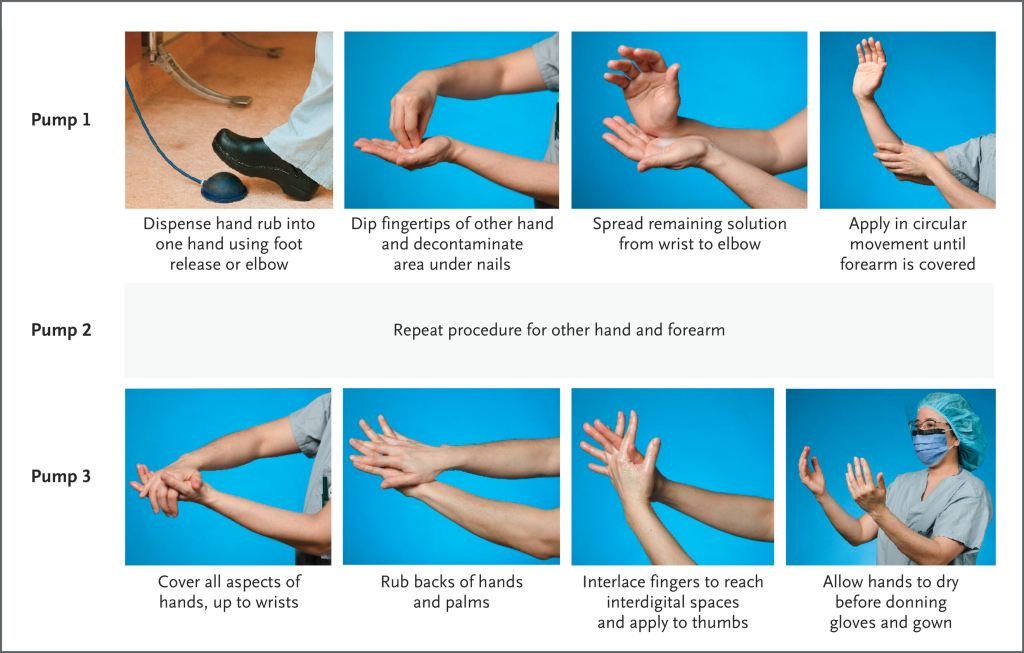
✅ DEFINITION
Surgical hand scrub is a systematic procedure of cleaning the hands, forearms, and nails using antiseptic soap/solution to remove dirt, reduce transient and resident microorganisms before donning sterile gloves and entering the OT.
🎯 Goal: Achieve maximum asepsis and prevent surgical site infections (SSIs).
🎯 OBJECTIVES OF SCRUBBING
- To remove dirt, oil, and transient microorganisms
- To reduce resident skin flora to a minimum
- To prepare hands and arms for aseptic surgical procedures
- To maintain sterility in the operating room
🧴 TYPES OF SCRUBBING METHODS
| Method | Description |
|---|---|
| Timed Scrub | Scrubbing done for a specific time (usually 5–10 minutes) |
| Stroke Count Method | A specific number of brush strokes per surface area (e.g., 20 strokes per surface) |
⏱️ DURATION OF SURGICAL SCRUB
| Case Type | Scrub Time |
|---|---|
| First scrub of the day | 5–10 minutes |
| Subsequent scrubs (if same person and case) | 3–5 minutes |
🧰 ARTICLES REQUIRED FOR SCRUBBING
| Item | Purpose |
|---|---|
| Scrub sink with elbow/foot operated tap | Prevents contamination |
| Antiseptic solution (e.g., Povidone-iodine, Chlorhexidine) | Antimicrobial cleansing |
| Sterile nail pick | Cleans under nails |
| Sterile scrub brush/sponge | Removes debris and bacteria |
| Sterile towel (for drying) | Maintains asepsis |
| Sterile gown and gloves | To wear after scrub |
🩺 SCRUBBING PROCEDURE – STEP-BY-STEP
🔹 1. Preparation
- Remove all jewelry, watch, bangles, rings
- Wear mask, cap, and OT dress before starting
- Check nails – must be short, clean, unpolished, and without extensions
- Open sterile towel and gown packs in the sterile area
🔹 2. Initial Rinse
- Turn on water using elbow, knee, or foot control
- Wet hands and arms up to 2 inches above the elbow
- Keep hands above elbow level at all times
🔹 3. Cleaning Nails
- Take sterile nail pick
- Clean under each nail under running water
- Discard nail pick in sterile discard container
🔹 4. Scrubbing Hands and Arms
- Take sterile brush/sponge with antiseptic
- Use 15–20 strokes or 2 minutes per area:
- Palm
- Back of hand
- Between fingers
- Each finger individually
- Thumb
- Wrist
- Forearm up to 2 inches above elbow
⏱️ Start from fingertips → hand → forearm → elbow
- Repeat on opposite hand and arm using the other side of brush
🔹 5. Rinsing
- Rinse hands and arms from fingertips to elbow
- Let water flow downwards only (hands above elbows)
- Do not touch anything or splash water
🔹 6. Drying
- Take sterile towel (touch only inner side)
- Pat dry one hand and arm with one end of towel
- Use the other end for the opposite hand and arm
- Do not rub, just pat from fingers → elbow
- Discard towel in sterile bin
🔹 7. Gowning and Gloving
- Wear sterile gown using correct technique
- Perform closed gloving or assisted gloving method
- Keep hands above waist level and avoid touching non-sterile surfaces
🚫 THINGS TO AVOID DURING SCRUBBING
- Do not splash or shake hands
- Do not allow water to run back from elbow to fingers
- Do not touch tap or sink after starting scrub
- Do not use the same part of towel on both arms
- Do not lower hands below waist at any time
👩⚕️ NURSE’S ROLE IN SCRUBBING
- Teach and supervise proper scrubbing technique
- Ensure availability of sterile supplies (brush, gown, gloves)
- Monitor compliance with infection control guidelines
- Check that all team members follow hand hygiene protocol
- Report and correct breaks in asepsis
- Keep scrub area clean, dry, and well-stocked
📝 DOCUMENTATION (if applicable)
- Log hand hygiene compliance in infection control audits
- Report any reactions to antiseptic or skin damage
- Maintain scrub register (for procedures involving implants)
🧾 SUMMARY TABLE
| Step | Key Points |
|---|---|
| Preparation | Remove jewelry, wear OT dress, open sterile packs |
| Nail Cleaning | Use sterile nail pick under running water |
| Scrubbing (Timed or Stroke) | Start from fingers → elbow (15–20 strokes per part) |
| Rinsing | Hands above elbows, rinse from fingers downward |
| Drying | Sterile towel, pat dry, one arm at a time |
| Gowning & Gloving | Wear sterile gown and gloves aseptically |
👗 GOWNING.

✅ DEFINITION
Gowning is the aseptic technique of donning a sterile surgical gown after scrubbing, to maintain a sterile barrier between the surgical team and the patient’s sterile field.
🎯 Goal: Prevent transfer of microorganisms from the staff to the surgical wound.
🎯 OBJECTIVES OF GOWNING
- To create a sterile field around the person performing the surgery
- To protect the patient from contamination
- To reduce the risk of surgical site infections (SSIs)
- To ensure aseptic surgical practice
🧰 ARTICLES REQUIRED FOR GOWNING
| Item | Purpose |
|---|---|
| Sterile surgical gown | Worn after scrubbing to maintain asepsis |
| Sterile gloves | To be worn after gowning (closed gloving method) |
| Sterile drape or wrapper | Used to keep gown sterile inside the sterile pack |
| OT mask, cap, and dress | Worn before scrub to maintain cleanliness |
| Assistant (optional) | Helps in assisted gowning method |
🧼 TYPES OF GOWNING METHODS
| Type | Description |
|---|---|
| Self Gowning | Performed by individual after scrubbing using sterile technique |
| Assisted Gowning | Done with the help of a circulating nurse or another sterile team member |
🧼 PREPARATION BEFORE GOWNING
- Wear surgical cap, mask, and OT dress
- Perform surgical hand scrub (as per protocol)
- Keep hands above waist and below shoulders
- Open sterile gown pack carefully or ask assistant to open for you
👗 SELF GOWNING PROCEDURE – STEP BY STEP
| Step | Action |
|---|---|
| 1 | Pick the sterile gown by grasping the inner folded surface near the neck (inside part is considered clean, outside is sterile) |
| 2 | Hold gown away from body and allow it to unfold, touching only the inner part |
| 3 | Insert arms into sleeves (only till the wrist), keeping hands inside the gown to maintain sterility |
| 4 | Let the assistant pull the gown over shoulders and tie it at the back (back side is non-sterile) |
| 5 | Proceed to closed gloving while keeping hands inside the gown sleeves |
| 6 | Once gloved, secure the waist ties (either self-tie or ask circulating nurse to assist using sterile technique) |
👬 ASSISTED GOWNING PROCEDURE (By Scrub Nurse or Circulator)
| Step | Action |
|---|---|
| 1 | Scrub nurse presents the sterile gown to the surgeon by unfolding it at the shoulders (sterile side facing the surgeon) |
| 2 | Surgeon inserts arms, keeping hands inside sleeves |
| 3 | Assistant pulls the gown over shoulders and ties the neck and waist ties at the back |
| 4 | Surgeon performs closed gloving next, followed by final waist tie adjustment |
🧤 FOLLOW-UP: GLOVING AFTER GOWNING
Immediately after gowning, perform closed gloving to complete the sterile barrier.
📌 Do not touch the outer gown surface with bare hands!
⚠️ PRECAUTIONS DURING GOWNING
- Do not touch the outer (sterile) surface of the gown with bare hands
- Hands must remain inside sleeves until gloves are on
- Gown must not touch non-sterile surfaces
- Discard gown immediately if sterility is broken
- If gown is contaminated, change it before touching the sterile field
🧺 DISPOSAL AFTER SURGERY
| Gown Type | Disposal |
|---|---|
| Disposable gown | Disposed in yellow biomedical waste bag |
| Reusable cloth gown | Sent to laundry and re-sterilized via autoclaving |
📋 NURSE’S RESPONSIBILITIES DURING GOWNING
| Role | Responsibilities |
|---|---|
| Before gowning | Ensure sterile gown is available and opened aseptically |
| During gowning | Assist in back tying if needed, supervise sterile technique |
| After gowning | Help with closed gloving or final waist tie |
| Monitoring | Check for any breaks in asepsis, report contamination |
| Inventory | Ensure gowns are restocked and labeled correctly after sterilization |
📝 SUMMARY TABLE
| Step | Key Point |
|---|---|
| Open gown | Touch only inner folded part |
| Insert arms | Keep hands inside sleeves |
| Assistant help | Pull gown over shoulders |
| Closed gloving | Before exposing hands |
| Secure ties | Back and waist using sterile technique |
🧾 BONUS: IDENTIFICATION – GOWN AREAS
| Gown Part | Sterility |
|---|---|
| Front (chest to waist) | Sterile |
| Sleeves (above elbow to cuff) | Sterile |
| Back of gown | Non-sterile |
| Underarm area | Non-sterile |
😷 MASKING.
✅ DEFINITION
Masking refers to the correct application and removal of a surgical face mask to prevent the spread of microorganisms from the healthcare provider’s mouth and nose to the patient or sterile field.
🎯 Purpose: To act as a barrier protecting both patient and staff from cross-contamination during surgical and sterile procedures.
🎯 OBJECTIVES OF MASKING
- To prevent droplets, saliva, and microorganisms from contaminating sterile fields
- To protect the wearer from exposure to blood, body fluids, and airborne particles
- To reduce the risk of infection during surgery or close patient contact
🧢 PARTS OF A SURGICAL MASK
| Part | Description |
|---|---|
| Outer layer | Water-repellent surface (colored side – usually worn outward) |
| Middle filter layer | Filters bacteria and viruses |
| Inner layer | Absorbs moisture from the wearer’s breath |
| Nose strip | Malleable metal strip for sealing over the bridge of the nose |
| Ear loops or tie strings | For securing the mask on the face |
😷 TYPES OF MASKS USED IN CLINICAL SETTINGS
| Type of Mask | Description | Use |
|---|---|---|
| Surgical Mask | 3-layer mask; filters large droplets | OT, general patient care |
| N95 Respirator Mask | Filters ≥95% of airborne particles | TB, COVID-19, airborne infections |
| Cloth Mask (not for OT) | Washable, reusable | Community or non-clinical use |
| Duckbill Mask | Folded shape for comfort and filtration | Used in certain sterile procedures |
📌 Surgical masks are used in sterile environments like OT, not cloth masks.
📝 INDICATIONS FOR MASK USE
- During surgery or invasive procedures
- While assisting in sterile dressing changes
- In delivery rooms or NICUs
- During outbreaks of airborne/droplet diseases (e.g., flu, COVID-19, TB)
- While caring for immunocompromised patients
- In infection isolation units
⚠️ CONTRAINDICATIONS / PRECAUTIONS
| Situation | Action |
|---|---|
| Moist or wet mask | Must be changed immediately |
| Soiled/damaged mask | Discard and replace |
| Patient with difficulty breathing | Use only if medically tolerated |
| Latex allergy (in some elastic straps) | Choose latex-free versions |
🧼 PROCEDURE FOR WEARING (DONNING) A MASK
| Step | Action |
|---|---|
| 1 | Perform hand hygiene before touching the mask |
| 2 | Check mask for tears or damage |
| 3 | Identify top edge (with nose strip) and colored side (outer) |
| 4 | Hold mask by ear loops or tie strings |
| 5 | Place mask over nose, mouth, and chin completely |
| 6 | Press nose strip to mold it securely over nose bridge |
| 7 | Secure ear loops or tie top strings at crown, bottom strings at nape |
| 8 | Avoid touching the front of the mask once worn |
🗑️ PROCEDURE FOR REMOVING (DOFFING) A MASK
| Step | Action |
|---|---|
| 1 | Perform hand hygiene |
| 2 | Do not touch front of the mask |
| 3 | Remove mask using ear loops or tie strings (untie bottom, then top) |
| 4 | Discard in yellow biomedical waste bin if used in OT |
| 5 | Perform hand hygiene again |
📋 NURSE’S RESPONSIBILITIES DURING MASKING
| Task | Responsibility |
|---|---|
| Availability | Ensure sterile masks are available in sufficient quantity |
| Instruction | Teach staff and patients about proper use |
| Monitoring | Check compliance in OT, wards, ICU |
| Changing | Instruct staff to change masks after 6–8 hours or when moist |
| Disposal | Ensure masks are discarded safely in biomedical waste |
| Training | Demonstrate correct donning and doffing methods to new staff or students |
🔁 WHEN TO CHANGE THE MASK
- After every surgery or sterile procedure
- When the mask becomes wet, soiled, or loose
- Every 6–8 hours during routine clinical use
- Immediately after splash or contamination
🧾 SUMMARY TABLE
| Step | Key Points |
|---|---|
| Before Wearing | Hand hygiene, check mask, identify sides |
| Wearing | Cover nose-mouth-chin, mold nose strip, secure ties |
| After Wearing | Avoid touching, do not pull mask under chin |
| Removing | Remove by straps only, discard properly, wash hands |
🧤 GLOVING.

✅ DEFINITION
Gloving is the process of wearing sterile gloves to prevent transmission of microorganisms and maintain asepsis during sterile procedures or surgery.
🎯 Gloves create a protective barrier between healthcare workers and patients during sterile or invasive procedures.
🎯 OBJECTIVES OF GLOVING
- To protect patients from infection during surgical or sterile procedures
- To protect the healthcare worker from blood, body fluids, and harmful organisms
- To maintain a sterile field during surgeries and invasive care
🧤 TYPES OF GLOVES
| Type | Description | Use |
|---|---|---|
| Sterile Gloves | Individually packed, free from microorganisms | Surgery, wound dressing, invasive procedures |
| Non-Sterile Gloves | Not guaranteed sterile, used for general care | Bed making, handling waste, cleaning |
| Latex Gloves | Made from natural rubber (may cause allergy) | Common but requires allergy screening |
| Nitrile Gloves | Latex-free, chemical-resistant | For latex-sensitive individuals |
| Vinyl Gloves | Loose-fitting, less durable | Short, low-risk procedures |
🧴 TYPES OF GLOVING TECHNIQUES
| Technique | Description | When Used |
|---|---|---|
| Open Gloving | Hands are exposed; gloves are worn individually | Catheterization, minor dressing |
| Closed Gloving | Hands remain inside sleeves of gown | During surgery (after gowning) |
| Assisted Gloving | Helped by a sterile team member | During major surgeries or assisted setup |
🧼 ARTICLES REQUIRED
- Sterile gloves (correct size)
- Sterile gown (for closed gloving)
- Sterile field or table
- Hand scrub facilities
- Waste bin for disposal
🧤 PROCEDURE FOR OPEN GLOVING (STEP-BY-STEP)
🔹 Indications: Minor sterile procedures (e.g., catheter insertion, dressing change)
| Step | Action |
|---|---|
| 1 | Perform hand hygiene and dry hands properly |
| 2 | Open sterile glove pack on a sterile surface |
| 3 | Pick up first glove by inside of the cuff (only touch the inner surface) |
| 4 | Insert one hand into the glove, fingers first |
| 5 | With gloved hand, slide fingers under cuff of second glove (touch only outside) |
| 6 | Pull second glove onto the opposite hand |
| 7 | Adjust both gloves without touching skin or non-sterile surfaces |
| 8 | Keep hands above waist level and do not touch anything unsterile |
🧤 PROCEDURE FOR CLOSED GLOVING (AFTER GOWNING)
🔹 Indications: Major surgeries where full sterile technique is required.
| Step | Action |
|---|---|
| 1 | After gowning, keep hands inside sleeves of the gown |
| 2 | Pick up sterile glove (palm down) using covered hand inside sleeve |
| 3 | Place glove palm against the palm of the corresponding hand and align |
| 4 | With opposite sleeve-covered hand, pull glove over gown sleeve and hand |
| 5 | Repeat for other hand – do not allow bare hands to touch outside of gloves |
| 6 | Adjust fingers inside gloves without touching skin or unsterile areas |
🗑️ GLOVE REMOVAL (DOFFING TECHNIQUE)
| Step | Action |
|---|---|
| 1 | Grasp outside of one glove at wrist and peel it off, turning inside out |
| 2 | Hold removed glove in the opposite hand |
| 3 | Slide fingers of ungloved hand under the wrist of remaining glove |
| 4 | Peel it off over the first glove (both gloves now inside out) |
| 5 | Discard gloves in yellow biomedical waste bin |
| 6 | Perform hand hygiene immediately |
👩⚕️ NURSE’S RESPONSIBILITIES DURING GLOVING
| Responsibility | Action |
|---|---|
| Preparation | Ensure correct glove size and sterility |
| Teaching | Educate students or staff on correct technique |
| Monitoring | Observe compliance with aseptic technique |
| Assisting | Help in assisted gloving (if needed) |
| Changing gloves | Encourage changing gloves if torn, wet, or after contamination |
| Waste disposal | Discard in correct biomedical waste bin |
❌ COMMON MISTAKES TO AVOID
- Touching outside of gloves with bare hands
- Wearing gloves over wet hands
- Not changing gloves between procedures
- Letting gloves fall below waist level
- Reusing disposable gloves
- Touching mask, hair, or face while wearing gloves
📝 SUMMARY TABLE
| Step | Key Action |
|---|---|
| Hand hygiene | Before and after gloving |
| Open gloving | Touch inside of 1st glove, outside of 2nd |
| Closed gloving | Hands inside gown sleeves |
| During use | Keep hands sterile and above waist |
| After use | Remove safely, discard, and wash hands |
👩⚕️ MONITORING THE PATIENT DURING PROCEDURES.

✅ DEFINITION
Monitoring during surgical or invasive procedures refers to the continuous observation, assessment, and documentation of the patient’s physiological status to ensure safety, stability, and timely identification of complications.
🎯 Goal: To maintain homeostasis, detect changes early, and prevent complications during surgery or procedures.
🩺 PURPOSE OF PATIENT MONITORING
- To maintain hemodynamic stability (BP, pulse, oxygenation)
- To detect anesthetic or surgical complications
- To guide intraoperative decision-making
- To ensure timely intervention in case of deterioration
- To provide a baseline for post-operative care
📋 PARAMETERS MONITORED DURING PROCEDURES
| Parameter | Why It’s Monitored |
|---|---|
| Heart rate (Pulse) | Detects arrhythmias, stress, bleeding |
| Blood pressure (BP) | Monitors perfusion, fluid balance |
| Respiratory rate (RR) | Detects apnea, anesthesia effect |
| Oxygen saturation (SpO₂) | Prevents hypoxia |
| Temperature | Detects hypothermia or fever |
| Electrocardiogram (ECG) | Continuous cardiac monitoring |
| End-tidal CO₂ (ETCO₂) | Measures ventilation during anesthesia |
| Urine output | Indicates kidney function and fluid status |
| Neurological status | Especially in local/regional anesthesia |
| Level of consciousness | Sedation or anesthesia monitoring |
🧰 EQUIPMENT USED FOR MONITORING
| Equipment Name | Function |
|---|---|
| Multiparameter monitor | Shows ECG, BP, SpO₂, temperature, RR |
| Pulse oximeter | Measures oxygen saturation |
| Non-invasive BP cuff (NIBP) | Tracks blood pressure trends |
| Capnograph | Monitors exhaled CO₂ |
| Thermometer/Temperature probe | Measures body temp |
| ECG electrodes and leads | Tracks cardiac rhythm |
| Foley catheter with urometer | Measures urine output |
| Infusion pump | Controls IV fluids/medications |
| Defibrillator (standby) | For emergency cardiac events |
🧪 TYPES OF MONITORING
| Type of Monitoring | Description |
|---|---|
| Non-invasive Monitoring | Pulse, BP, SpO₂, temp (external tools) |
| Invasive Monitoring | Arterial line, central venous pressure (CVP), intubation (critical cases) |
| Neuromuscular Monitoring | Measures level of muscle relaxation in anesthesia |
| Anesthesia Depth Monitoring | BIS monitor, verbal response (in conscious sedation) |
📝 RESPONSIBILITIES OF THE NURSE DURING MONITORING
| Phase | Role of the Nurse |
|---|---|
| Pre-procedure | – Record baseline vitals |
- Verify identity, consent, and allergies
- Ensure monitors are attached and functioning
| | During procedure | – Continuously monitor and document vitals every 5–15 mins - Inform anesthetist/surgeon of any changes
- Maintain airway patency and oxygen flow
- Monitor IV fluids, blood transfusions
- Observe surgical site (bleeding, reaction)
- Maintain patient dignity, positioning, and comfort
| | Post-procedure | – Continue monitoring during recovery - Record vitals every 15 minutes (as per protocol)
- Assess pain, consciousness, nausea, bleeding
- Document all findings and report abnormalities immediately
⛑️ SIGNS OF DETERIORATION TO WATCH FOR
- Sudden drop in BP or SpO₂
- Bradycardia or tachycardia
- Respiratory depression or apnea
- Cyanosis or pallor
- Decreased urine output
- Excessive bleeding from surgical site
- Change in level of consciousness
🚨 These signs require immediate intervention and team notification.
📋 DOCUMENTATION DURING MONITORING
| What to Document | Why |
|---|---|
| Time and type of monitoring started | To track the duration of procedure |
| Baseline and periodic vital signs | For trend observation |
| Fluids administered, blood loss | Maintain fluid balance record |
| Any unusual findings | Legal and clinical importance |
| Names of personnel involved | For accountability |
🧾 SUMMARY TABLE
| Parameter | Normal Range | Monitored How? |
|---|---|---|
| Pulse | 60–100 bpm | ECG, palpation |
| BP | 90/60–140/90 mmHg | NIBP or arterial line |
| SpO₂ | ≥ 95% | Pulse oximeter |
| RR | 12–20/min | Observation, monitor |
| Temp | 36.5–37.5°C | Thermometer, probe |
| ETCO₂ | 35–45 mmHg | Capnograph |
| Urine Output | ≥ 30 ml/hr | Foley catheter |
🩺 NURSE’S ALERTNESS TIPS DURING MONITORING
- Double-check all monitor connections
- Set alarm limits on machines
- Ensure backup equipment is available (e.g., oxygen, suction)
- Watch for artifacts (false signals) due to movement or poor electrode contact
- Maintain a calm and responsive environment
🏥 MAINTENANCE OF THE THERAPEUTIC ENVIRONMENT IN OT.
✅ DEFINITION
A therapeutic environment in OT refers to a controlled, sterile, safe, and supportive surgical setting that promotes optimal patient outcomes, prevents infections, and ensures efficient teamwork during operative procedures.
🎯 Goal: To ensure a sterile, safe, and psychologically supportive environment for both patient and surgical team.
🎯 OBJECTIVES
- To maintain strict asepsis and infection control
- To provide patient safety and comfort during surgery
- To ensure operational efficiency for the surgical team
- To maintain psychological calm and privacy for the patient
- To reduce risks of surgical site infections (SSIs)
🧱 COMPONENTS OF THE THERAPEUTIC ENVIRONMENT IN OT
| Component | Description |
|---|---|
| Sterility & Asepsis | Sterile instruments, gowns, gloves, drapes, and strict aseptic practices |
| Cleanliness | Regular cleaning and disinfection of OT surfaces and floors |
| Temperature & Humidity | OT temp (20–22°C), humidity (50–60%) for infection control |
| Ventilation/Air Flow | Laminar airflow systems, HEPA filters to remove contaminants |
| Lighting & Visibility | Shadowless surgical lights, adjustable lighting for different procedures |
| Noise Control | Quiet environment to support concentration and safety |
| Safety Equipment | Fire extinguishers, emergency exits, backup power, suction, oxygen |
| Organization of Equipment | All instruments and machines properly placed and checked |
| Communication | Clear, respectful, and calm communication among team members |
🧹 CLEANLINESS & ASEPSIS MAINTENANCE
| Task | Action |
|---|---|
| Pre-operative cleaning | OT walls, floors, lights, and trolleys cleaned before the first case |
| Between cases | Table, instruments, suction jar, and floor cleaned between surgeries |
| Post-operative terminal cleaning | Entire OT mopped with disinfectants (e.g., 1% hypochlorite) |
| Fumigation (weekly/monthly) | Formalin/automated fumigation to eliminate microbes |
| UV disinfection (optional) | UV lights used when OT is unoccupied to reduce microbial load |
🌬️ AIR QUALITY CONTROL
| Method | Purpose |
|---|---|
| Laminar Airflow System | Delivers HEPA-filtered air in a unidirectional flow to maintain sterility |
| Positive Pressure Ventilation | Prevents outside air from entering the sterile OT |
| HEPA Filters | Trap airborne particles and microorganisms |
🌡️ TEMPERATURE & HUMIDITY CONTROL
| Parameter | Ideal Range | Purpose |
|---|---|---|
| Temperature | 20–22°C | Comfort & microbial control |
| Humidity | 50–60% | Reduces risk of static and airborne contamination |
🧤 NURSE’S ROLE IN MAINTAINING OT ENVIRONMENT
🔹 Before Surgery
- Check availability and sterility of instrument trays, linen, drapes
- Ensure OT is cleaned and disinfected
- Verify functioning of monitors, cautery, suction, anesthesia machine
- Ensure sterile packs are labeled and within expiry date
- Regulate room temperature and lighting as per need
- Assist in preparing sterile field and positioning the patient
🔹 During Surgery
- Maintain strict asepsis – no touching of non-sterile surfaces
- Monitor traffic control – restrict entry/exit to prevent contamination
- Replace soiled drapes or gloves if contamination occurs
- Dispose sharps and waste in proper bio-medical bins
- Communicate clearly and assist surgical team efficiently
🔹 After Surgery
- Help in cleaning and disinfecting all surfaces, instruments
- Send instruments for sterilization
- Replace soiled linen and disinfect OT table and floor
- Update records and checklists for next case preparation
- Report any equipment malfunction or contamination immediately
⚠️ SAFETY MEASURES IN OT ENVIRONMENT
| Area | Safety Practice |
|---|---|
| Fire Safety | No open flames, check cautery machine, fire extinguisher availability |
| Electrical Safety | Check all cords, plugs, avoid wet surfaces |
| Sharps Disposal | Use puncture-proof yellow bins |
| Emergency Preparedness | Crash cart and defibrillator checked daily |
| Patient Identification & Site Marking | Prevent surgical errors |
| OT Zoning System | Follow sterile vs non-sterile zones strictly (e.g., sterile zone, clean zone, disposal zone) |
📋 OT NURSE’S CHECKLIST (Sample)
| Task | Done (✔) |
|---|---|
| OT cleaned and disinfected before case | |
| Sterile packs checked and arranged | |
| Equipment functioning properly | |
| OT temperature and airflow normal | |
| Bio-waste bins labeled and placed | |
| Hand hygiene stations filled and functional |
🧾 SUMMARY TABLE
| Component | Maintained How? |
|---|---|
| Sterility | Aseptic technique, sterile supplies |
| Cleanliness | Routine cleaning, disinfection, waste disposal |
| Air quality | HEPA filters, laminar airflow |
| Temperature & humidity | Set via central system (20–22°C, 50–60%) |
| Lighting & equipment | Pre-use check, shadowless lighting |
| Communication | Clear, calm, respectful team interaction |
📌 KEY PRINCIPLES
- Asepsis is the core of therapeutic environment in OT
- Safety + Sterility + Support = Optimal patient outcomes
- Nurse’s vigilance ensures prevention of infections and errors
🏥 ASSISTING IN MAJOR OPERATION.

✅ DEFINITION
Assisting in a major operation refers to the active participation of nurses and OT technicians in preparing, supporting, and maintaining the surgical field, instruments, patient safety, and asepsis during major surgical procedures.
🎯 Goal: To ensure safe, smooth, sterile, and successful completion of a major surgery.
🧠 WHAT IS A MAJOR SURGERY?
Major surgery involves:
- Penetration of a body cavity (abdomen, thorax, cranium)
- Use of general/spinal anesthesia
- Greater risk of complications
- Longer operative time
- Involves major organs or extensive tissues
🛠️ Examples:
- Laparotomy, Hysterectomy, Appendectomy, Cholecystectomy, Cesarean Section, Hernia Repair, CABG, Craniotomy, ORIF (Orthopedic)
👩⚕️ NURSE’S ROLES IN ASSISTING MAJOR SURGERY
🔷 1. Circulating Nurse (Non-sterile)
| Responsibility | Description |
|---|---|
| Patient prep | Verifies consent, ID, allergies, site marking |
| Equipment setup | Ensures all monitors, suction, cautery, anesthesia machine working |
| Positioning | Assists in safe patient positioning with padding |
| Asepsis support | Opens sterile packs, adds instruments to sterile field |
| Documentation | Records procedure details, sponge/needle counts |
| Communication | Liaison between scrub team and outside personnel |
🔷 2. Scrub Nurse (Sterile Role)
| Responsibility | Description |
|---|---|
| Sterile field prep | Arranges instruments, drapes, and solutions |
| Instrument handling | Passes correct instruments using proper technique |
| Sponge/needle count | Conducts counts with circulator at start, before closure, and end |
| Tissue handling | May assist surgeon with sponging, retracting, suction |
| Specimen care | Receives and labels biopsy or surgical specimens |
| Asepsis maintenance | Monitors sterility and reports any breaks immediately |
🧰 PREPARATION BEFORE A MAJOR OPERATION
🔹 A. Patient Preparation
- Confirm ID, consent, surgical site, fasting status
- Shave/prep surgical site as per protocol
- Remove jewelry, dentures, nail polish
- Ensure IV line is working
- Pre-op medication as per order
🔹 B. OT Setup
- Clean and disinfect OT before the procedure
- Arrange instrument sets, suture materials, linen, drapes
- Check electrosurgical unit, suction, cautery, monitors
- Maintain correct temperature (20–22°C) and lighting
👗 ASEPTIC PRACTICES DURING SURGERY
| Aseptic Practice | Description |
|---|---|
| Scrubbing | Surgical hand wash before gowning and gloving |
| Gowning & gloving | Sterile attire for scrub team |
| Draping | Sterile drapes over patient to isolate surgical site |
| Sterile field | Maintain sterility; do not cross or contaminate |
| Traffic control | Limit personnel and entry during surgery |
🔄 DURING THE PROCEDURE – STEP-BY-STEP SUPPORT
| Phase | Circulating Nurse Tasks | Scrub Nurse Tasks |
|---|---|---|
| Induction | Assist anesthesia, apply monitors | Standby with sterile field ready |
| Incision | Document time, help with lights | Pass scalpel and initial tools |
| Dissection & Exposure | Provide additional items | Suctioning, retraction |
| Hemostasis | Monitor cautery unit | Pass clamps, ligatures |
| Suturing/Closure | Prepare dressing, document count | Pass needle, scissors |
| Specimen Handling | Label and send to lab | Transfer from field safely |
| Wound Dressing | Provide sterile dressing pack | Apply or assist dressing |
| Post-op Transfer | Help shift patient to recovery | Clean instruments for CSSD |
📝 COUNTING PROTOCOL
| When to Count | Items Counted |
|---|---|
| Before incision | Sponges, needles, instruments |
| Before closure of a cavity | Same items |
| At final skin closure | Final count to confirm none retained |
❗ Discrepancy in count must be reported immediately and resolved before closure.
🧼 POST-OPERATIVE CLEANING
- Used instruments sent for decontamination and sterilization
- OT table and surfaces disinfected
- Linen disposed of or sent for laundering
- Waste segregated per BMW guidelines
- Documentation of procedure, counts, and specimens
⛑️ EMERGENCY PREPAREDNESS DURING SURGERY
- Crash cart and defibrillator available
- Know emergency codes (Code Blue, Code Red)
- Be ready to assist in cardiac arrest, bleeding, allergic reaction
📋 DOCUMENTATION BY NURSE
| What to Document |
|---|
| Time of incision and closure |
| Instruments and sutures used |
| Blood loss estimation (EBL) |
| Medications given intraoperatively |
| Specimens collected and sent |
| Name of surgeon and team members |
| Any intraoperative events or breaks in sterility |
🧾 SUMMARY TABLE
| Role | Key Actions |
|---|---|
| Circulating Nurse | Patient prep, supply, documentation, safety |
| Scrub Nurse | Sterile field, instrument handling, asepsis |
| Nurse’s Focus | Aseptic technique, patient safety, smooth workflow |
| Equipment Used | Monitor, suction, cautery, anesthesia machine, crash cart |
🏥 ASSISTING IN MINOR OPERATION.
✅ DEFINITION
Assisting in a minor operation means supporting the doctor/surgeon in performing a short, less invasive surgical procedure, usually under local anesthesia and involving minimal risk, time, and tissue penetration.
🎯 Goal: To provide safe, sterile, supportive care for minor surgical interventions and ensure patient comfort and quick recovery.
💉 EXAMPLES OF MINOR OPERATIONS
- Incision and drainage (I&D) of abscess
- Suturing of lacerations
- Excision of small cysts, warts, lipoma
- Wound debridement
- Foreign body removal
- Circumcision
- Skin biopsy
- Nail removal (partial/complete)
🎯 OBJECTIVES OF NURSE IN MINOR OPERATIONS
- Prepare sterile field and equipment
- Maintain asepsis throughout procedure
- Provide emotional support to patient
- Assist surgeon with instruments and materials
- Monitor patient’s comfort and safety
- Handle specimens (if any) and dispose of waste properly
🧰 EQUIPMENT & INSTRUMENTS USED (Minor Surgical Set)
| Instrument | Quantity |
|---|---|
| Artery forceps (mosquito) | 2 |
| Dissecting forceps (toothed and non-toothed) | 1 each |
| Surgical scissors (straight/curved) | 1 each |
| Needle holder | 1 |
| Sterile surgical gloves | 1 pair (per person) |
| Sponge holding forceps | 1 |
| Surgical blades and handle | 1 |
| Bowl (for antiseptic/normal saline) | 1 |
| Sterile drapes and gauze | As required |
| Sutures | As per need |
| Local anesthetic (e.g., Lignocaine) with syringe & needle | 1 set |
🧼 NURSE’S RESPONSIBILITIES IN ASSISTING MINOR SURGERY
🔹 1. Pre-Procedure Responsibilities
| Task | Description |
|---|---|
| Patient Preparation | – Explain procedure |
- Obtain consent
- Ensure patient comfort and privacy
- Shave or clean site (if required)
- Assist in positioning | | Room and Equipment Setup | – Clean the minor OT or procedure room
- Assemble and arrange sterile tray
- Check all instruments and equipment
- Pour antiseptic into bowl
- Assist in handwashing and gloving | | Aseptic Setup | – Open sterile packs
- Arrange drapes, gowns, gloves
- Avoid contamination of sterile field |
🔹 2. During the Procedure
| Task | Description |
|---|---|
| Assist the doctor | – Pass instruments |
- Maintain clean and dry field
- Blot blood using gauze with sponge forceps
- Cut suture thread on instruction | | Monitor patient | – Observe for discomfort, pain, or fainting
- Reassure and talk to conscious patients
- Adjust position if needed | | Specimen handling | – Label and send any biopsy/tissue samples to lab in proper container |
🔹 3. Post-Procedure Responsibilities
| Task | Description |
|---|---|
| Wound Care | – Apply sterile dressing |
- Secure with bandage or tape
- Give post-op instructions | | Waste Disposal | – Dispose sharps in puncture-proof container
- Discard used materials in appropriate biomedical waste bins | | Instrument Care | – Rinse instruments
- Send for sterilization | | Documentation | – Record procedure, findings, patient response, and follow-up plan |
🧪 ASEPTIC TECHNIQUES TO FOLLOW
- Perform surgical handwashing
- Wear mask, cap, gown, and sterile gloves
- Use sterile drapes and gauze
- Do not touch sterile items with bare hands
- Avoid unnecessary talking or movement around sterile field
- Change gloves or instruments if contamination occurs
😷 SAFETY PRECAUTIONS
- Check for allergy to local anesthetic (e.g., lignocaine)
- Watch for signs of vasovagal shock (fainting, sweating, nausea)
- Ensure patient is in a comfortable and safe position
- Prepare emergency tray (if needed) for allergic reaction or bleeding
📋 DOCUMENTATION BY NURSE
- Date and time of procedure
- Type of procedure performed
- Name of surgeon/doctor
- Site of operation
- Local anesthesia used
- Instruments and sutures used
- Patient’s response and condition post-procedure
- Any specimen collected and sent
🧾 SUMMARY TABLE
| Phase | Nurse’s Key Role |
|---|---|
| Pre-procedure | Prepare patient, equipment, sterile field |
| During procedure | Assist doctor, pass instruments, monitor patient |
| Post-procedure | Dressing, waste disposal, documentation |
| Asepsis | Maintain sterile environment at all times |
🧫 HANDLING SPECIMENS.

✅ DEFINITION
Specimen handling refers to the correct collection, labeling, preservation, transportation, and documentation of biological materials (e.g., tissue, blood, fluid) obtained during a surgical procedure or investigation for diagnostic purposes.
🎯 Goal: To maintain the integrity, sterility, and identity of the specimen and prevent contamination, errors, or loss.
🧪 TYPES OF SPECIMENS COLLECTED
| Specimen Type | Examples |
|---|---|
| Tissue Biopsy | Tumors, lymph nodes, organ parts (e.g., liver, uterus) |
| Fluid Specimens | Peritoneal fluid, pleural fluid, CSF |
| Swabs | Wound swabs, throat swabs, pus swabs |
| Body Parts (Whole) | Appendix, gall bladder, amputated limbs |
| Stones/Foreign bodies | Renal stones, bullets, orthopedic implants |
📦 CONTAINERS USED FOR SPECIMENS
| Specimen Type | Container Type |
|---|---|
| Tissue biopsy | Sterile container with 10% formalin (unless for culture) |
| Body fluids | Sterile screw-cap container or syringe |
| Microbiology swabs | Sterile culture tube or swab kit |
| Blood or CSF | Sterile test tubes (plain, EDTA, or citrate tubes) |
| Frozen sections | Dry container without formalin, labeled for urgent histopathology |
🔁 STEPS IN SPECIMEN HANDLING (SURGICAL OR CLINICAL)
🔹 1. Receiving the Specimen from Surgeon
- Receive directly into a sterile container
- Do not touch specimen with bare hands
- Ask for confirmation: what it is, where from, and intended test
🔹 2. Proper Labeling
Label immediately using a permanent marker or printed label:
- Patient’s full name and ID number
- Date and time of collection
- Type and site of specimen
- Name of the procedure
- Ward/OT and surgeon’s name
- Mention if it’s for: Histopathology, Culture, Biopsy, Cytology
⚠️ Unlabeled or mislabelled specimens can lead to legal and diagnostic errors.
🔹 3. Preservation
| Type | Preservation Method |
|---|---|
| Histopathology | 10% formalin (volume should be 10x the size of specimen) |
| Microbiology (Culture) | No formalin – keep in sterile container only |
| Frozen section | Dry sterile container; sent immediately to lab |
🔹 4. Documentation
Record details in:
- Specimen register (OT or ward)
- Patient’s nursing notes or intraoperative record
- Handover to porter/lab technician with signature
🔹 5. Transportation
- Send promptly to lab with requisition form
- Use biohazard-labeled, leak-proof containers if applicable
- Maintain cold chain if required (e.g., for certain blood or urine tests)
⚠️ PRECAUTIONS IN SPECIMEN HANDLING
- Do not spill, dry, or crush the specimen
- Never put tissue for culture in formalin – it kills microorganisms
- Handle with gloved hands only
- Avoid delay – tissue degeneration may alter results
- Ensure correct fixation and closure of the container
- Use color-coded biohazard bags for transport as per BMW rules
👩⚕️ NURSE’S RESPONSIBILITIES
| Phase | Responsibility |
|---|---|
| Before Collection | – Ensure sterile container is ready |
- Know what type of specimen is being collected | | During Collection | – Accept specimen aseptically
- Label container immediately and correctly | | After Collection | – Preserve as required (formalin or dry)
- Complete lab form and attach securely
- Send specimen quickly and safely
- Record in OT register and nursing notes
- Communicate clearly to lab/porter |
🧾 SUMMARY TABLE
| Task | Action |
|---|---|
| Collect specimen | Using sterile technique |
| Label specimen | Name, ID, date, site, test type |
| Preserve specimen | Formalin (for histopath); sterile (for culture) |
| Document | In OT register, patient file |
| Transport | Leak-proof, sealed container with lab form |
❌ COMMON MISTAKES TO AVOID
- Delayed transport leading to tissue decay
- Formalin used for microbiology specimen
- Improper or missing label
- Incomplete requisition form
- Not documenting collection in records
⚠️ PREVENTION OF ACCIDENTS AND HAZARDS IN OT.

✅ DEFINITION
Prevention of accidents and hazards in the OT refers to all the safety measures and protocols implemented to protect patients, staff, and equipment from injury, contamination, fire, electrical shock, or procedural errors during surgical care.
🎯 Goal: To maintain a safe, sterile, and secure surgical environment for all members of the surgical team and the patient.
🔍 COMMON ACCIDENTS & HAZARDS IN OT
| Type of Hazard | Examples |
|---|---|
| Fire and Explosion | Alcohol-based prep catching fire, electrical sparks |
| Infection/Biohazard | Surgical site infections (SSIs), needlestick injuries |
| Electrical Hazards | Faulty wires, improper use of cautery machines |
| Chemical Hazards | Exposure to formalin, glutaraldehyde, anesthetic gases |
| Mechanical Injuries | Falls, patient injury due to improper positioning |
| Sharps Injury | Needle prick, blade cuts |
| Radiation Exposure | C-arm/X-ray without protection |
| Latex Allergy | Reaction to latex gloves or materials |
🧤 NURSE’S ROLE IN PREVENTION OF OT ACCIDENTS
🔷 1. Aseptic Measures & Infection Control
- Follow surgical hand scrub, gowning, and gloving protocols
- Sterilize instruments and use sterile drapes, gowns, gloves
- Maintain proper zoning in OT (sterile, clean, dirty zones)
- Avoid overcrowding and unnecessary movement
- Use PPE (mask, cap, goggles, apron) appropriately
- Follow biomedical waste segregation and disposal guidelines
🔷 2. Fire and Explosion Prevention
- Avoid use of spirit near cautery machine
- Keep fire extinguishers and sand buckets ready and functional
- Maintain good ventilation to prevent gas accumulation
- Do not overload electrical points or use wet equipment
- Train staff in fire drills and emergency exits
🔷 3. Safe Equipment Handling
- Check equipment for damaged cords, exposed wires, loose connections
- Calibrate and test suction machines, cautery units, anesthesia machines before use
- Use earth grounding for electric devices
- Ensure backup power (UPS/generator) is available
- Keep floors dry to avoid electric shock and slips
🔷 4. Sharps and Instrument Safety
- Handle needles and scalpels with care
- Use needle holders, not fingers, to pass sutures
- Dispose sharps immediately in puncture-proof yellow bins
- Do not recap used needles
- Perform sponge and instrument count strictly to avoid retained items
🔷 5. Patient Positioning and Physical Safety
- Use positioning aids and padding to prevent nerve injury or pressure sores
- Secure patient properly with safety straps
- Protect eyes, limbs, and genitalia with drapes
- Ensure bedding is dry and free of wrinkles
- Check operating table locks and brakes
🔷 6. Chemical and Gas Safety
- Use formalin and glutaraldehyde in ventilated areas
- Store chemicals with proper labeling and PPE instructions
- Use scavenging systems for anesthetic gas disposal
- Avoid direct inhalation of ETO, nitrous oxide, etc.
🔷 7. Radiation Protection (C-Arm/X-ray in OT)
- Use lead aprons, thyroid shields, lead goggles
- Post warning signs when radiation is in use
- Minimize exposure time and increase distance
- Pregnant staff should avoid radiation zones
🔷 8. Emergency Preparedness
- Keep crash cart stocked and checked daily
- Train staff in BLS (Basic Life Support), ACLS, code blue response
- Maintain emergency contact numbers visibly posted
- Ensure ambulance and backup support is available
📋 SAFETY CHECKLIST FOR OT NURSES
| Safety Item | Check ✔ |
|---|---|
| Sterility of all equipment | |
| Cautery machine and suction tested | |
| Fire extinguisher ready | |
| OT temperature and ventilation OK | |
| Biomedical bins labeled and available | |
| Patient consent and ID verified | |
| Instrument and sponge count done | |
| Emergency drugs and defibrillator available |
🚨 SAFETY SIGNS TO WATCH FOR
- Burning smell or electrical spark
- Fluid leakage near machines
- Patient becoming restless or cyanotic
- Staff dizziness (gas leak)
- Broken lights or table dysfunction
- Sharp objects lying exposed
🧾 SUMMARY TABLE
| Hazard Type | Prevention Measures |
|---|---|
| Infection Control | Asepsis, PPE, sterilization |
| Fire & Explosion | Avoid alcohol + cautery, fire equipment |
| Electric Shock | Dry floors, check equipment |
| Sharp Injury | Use containers, no recapping |
| Radiation Exposure | Use lead protection |
| Chemical Exposure | Ventilation, correct storage |
| Physical Injury | Proper positioning and padding |
💉 ANAESTHESIA.

✅ DEFINITION
Anesthesia is the controlled, reversible loss of sensation (with or without consciousness) induced by drugs to allow surgical or diagnostic procedures to be performed without pain or distress.
🎯 Goal: To relieve pain, relax muscles, control physiological responses, and enable surgery safely.
🔍 TYPES OF ANAESTHESIA
1. General Anesthesia (GA)
🟢 Complete loss of consciousness and sensation.
| Feature | Details |
|---|---|
| Drugs Used | Propofol, Thiopentone, Sevoflurane, Nitrous oxide, Ketamine |
| Routes | IV, Inhalation |
| Airway Management | Endotracheal tube, Laryngeal mask |
| Uses | Major surgeries (abdominal, thoracic, neuro) |
2. Regional Anesthesia
🟢 Loss of sensation in a specific region of the body.
| Type | Description | Example Use |
|---|---|---|
| Spinal | Drug injected into subarachnoid space | Lower limb, cesarean |
| Epidural | Drug injected into epidural space | Labor analgesia |
| Nerve block | Injection near a nerve/plexus | Arm/leg surgery |
| Field block | Localized area blocked | Hernia repair |
3. Local Anesthesia
🟢 Loss of sensation in a small area without affecting consciousness.
| Route | Topical or infiltration | | Examples | Lignocaine, Bupivacaine | | Use | Suturing, minor procedures |
4. Conscious Sedation (Procedural Sedation)
🟢 Patient remains awake but relaxed and pain-free.
| Drugs | Midazolam, Fentanyl | | Use | Endoscopy, colonoscopy, minor ortho |
📈 STAGES OF GENERAL ANESTHESIA
| Stage | Description |
|---|---|
| Stage I: Analgesia | Induction phase, drowsy but conscious |
| Stage II: Excitement | Loss of consciousness, involuntary movements, irregular breathing |
| Stage III: Surgical anesthesia | Ideal stage: unconscious, no reflexes |
| Stage IV: Medullary paralysis | Overdose – danger zone (requires resuscitation) |
🛠️ COMMON ANAESTHESIA EQUIPMENT
| Equipment | Purpose |
|---|---|
| Anesthesia machine | Delivers gases (O₂, N₂O) and anesthetic agents |
| Laryngoscope | Helps visualize the airway for intubation |
| Endotracheal tube (ETT) | Maintains open airway |
| Face mask | Initial induction or maintenance |
| IV cannula and fluids | Drug administration |
| Pulse oximeter | Oxygen monitoring |
| ECG monitor, NIBP cuff | Monitor vitals |
| Suction apparatus | Removes secretions |
| Resuscitation equipment | In case of emergency |
💢 COMPLICATIONS OF ANESTHESIA
| System Affected | Complications |
|---|---|
| Respiratory | Airway obstruction, aspiration, hypoventilation |
| Cardiovascular | Hypotension, arrhythmia, cardiac arrest |
| Neurological | Delirium, delayed recovery, nerve injury |
| Gastrointestinal | Nausea, vomiting |
| Allergic | Anaphylaxis, rashes |
| Other | Malignant hyperthermia (life-threatening reaction to GA), headache after spinal |
👩⚕️ NURSE’S ROLE IN ANAESTHESIA
🔹 1. Pre-Anesthesia Phase
- Ensure informed consent is signed
- Confirm NPO (nil per oral) status (6–8 hours fasting)
- Check vitals, allergies, lab results, ECG
- Remove dentures, jewelry, nail polish
- Prepare and check IV line
- Prepare anesthesia trolley and resuscitation equipment
🔹 2. During Anesthesia
- Monitor vital signs continuously
- Assist anesthesiologist with positioning and airway management
- Support oxygen administration and suction
- Observe for signs of distress or complications
- Keep environment quiet and calm
- Maintain sterile field (if assisting regional block)
🔹 3. Post-Anesthesia (PACU – Recovery Room)
- Place patient in lateral (recovery) position to prevent aspiration
- Monitor:
- Airway, breathing, circulation (ABC)
- Consciousness level
- O₂ saturation, BP, pulse
- Watch for shivering, nausea, pain, delayed awakening
- Provide warmth and reassurance
- Document patient’s status and handover to post-op ward
🧾 SUMMARY TABLE
| Type | Consciousness | Area Affected | Use |
|---|---|---|---|
| General | Unconscious | Whole body | Major surgeries |
| Regional | Conscious | Large area | Lower limb, delivery |
| Local | Conscious | Small area | Minor procedures |
| Sedation | Conscious but drowsy | Targeted relaxation | Endoscopy, minor OT |
💉 GENERAL ANAESTHESIA.
✅ DEFINITION
General Anaesthesia (GA) is a medically induced reversible loss of consciousness, along with loss of sensation and reflexes, to allow painless surgical procedures.
🎯 The patient is unconscious, unaware, pain-free, and immobile.
🎯 OBJECTIVES OF GENERAL ANAESTHESIA
- Induce loss of consciousness
- Prevent pain (analgesia)
- Provide muscle relaxation
- Cause amnesia (no memory of procedure)
- Suppress reflexes during surgery
🔍 TYPES OF GENERAL ANAESTHESIA
| Type | Description |
|---|---|
| Inhalational GA | Anaesthetic gases or vapors are inhaled into the lungs |
| Intravenous (IV) GA | Drugs injected into the vein to induce anaesthesia |
| Balanced Anaesthesia | Combination of inhalational + IV drugs for optimal effect |
| Total Intravenous Anaesthesia (TIVA) | Only IV drugs used throughout procedure (no inhalation) |
🛑 INDICATIONS FOR GENERAL ANAESTHESIA
- Major surgeries (abdominal, thoracic, neurosurgery, cardiac)
- Uncooperative patients (e.g., children or psychiatric conditions)
- Long surgical duration
- When regional or local anesthesia is not feasible
- Procedures requiring muscle relaxation (e.g., laparotomy)
❌ CONTRAINDICATIONS
| Contraindication Type | Examples |
|---|---|
| Absolute | Allergy to anesthetic agents |
| Relative |
- Severe cardiopulmonary disease
- Raised intracranial pressure
- Malignant hyperthermia history
- Poor liver or kidney function
- Active respiratory infection or asthma exacerbation |
📈 STAGES OF GENERAL ANAESTHESIA (Guedel’s Classification)
| Stage | Description |
|---|---|
| Stage I – Analgesia | Conscious but drowsy; reduced pain sensation |
| Stage II – Excitement | Loss of consciousness, involuntary movements, irregular breathing |
| Stage III – Surgical Anesthesia | Ideal stage: unconscious, muscle relaxation, regular breathing |
| Stage IV – Medullary Paralysis | Dangerous: vital centers depressed, may cause respiratory/cardiac arrest |
⚠️ Surgery should be conducted during Stage III.
💊 METHODS OF ADMINISTRATION
🔹 1. Inhalational Route
- Delivered through face mask, ET tube, or laryngeal mask airway (LMA)
- Examples: Sevoflurane, Isoflurane, Nitrous Oxide
- Absorbed via lungs → bloodstream → brain
🔹 2. Intravenous Route
- Rapid onset through IV injection
- Examples: Propofol, Thiopentone, Ketamine, Etomidate
- Often used for induction, then maintained with inhalation
🔹 3. Balanced Technique
- Combination of IV induction + inhalation for maintenance
- Provides better control, faster recovery
🧰 EQUIPMENT USED IN GENERAL ANAESTHESIA
| Equipment | Purpose |
|---|---|
| Anaesthesia Machine | Delivers oxygen, nitrous oxide, and volatile agents |
| Laryngoscope | Assists intubation (placing ET tube) |
| Endotracheal Tube (ETT) | Maintains airway and ventilation |
| Face Mask / LMA | For non-invasive airway management |
| Pulse Oximeter | Monitors SpO₂ (oxygen saturation) |
| ECG Monitor | Heart rate and rhythm monitoring |
| BP Monitor (NIBP) | Blood pressure monitoring |
| Capnograph (ETCO₂) | Measures exhaled CO₂ |
| Suction Machine | Clears airway secretions or vomitus |
| Crash Cart / Defibrillator | For emergency resuscitation |
💉 COMMONLY USED GENERAL ANAESTHETIC DRUGS
🔹 Induction Agents (IV)
| Drug | Use |
|---|---|
| Propofol | Fast, smooth induction |
| Thiopentone Sodium | Short-acting barbiturate |
| Ketamine | Increases HR and BP, used in trauma, children |
| Etomidate | Cardio-stable, used in heart disease |
🔹 Inhalation Agents
| Drug | Use |
|---|---|
| Sevoflurane | Common for maintenance |
| Isoflurane | Potent, slower onset |
| Nitrous Oxide | Used with oxygen as carrier gas |
🔹 Muscle Relaxants
| Type | Drug | Use |
|---|---|---|
| Depolarizing | Succinylcholine | Rapid muscle relaxation (intubation) |
| Non-depolarizing | Vecuronium, Atracurium | Maintenance of muscle relaxation |
🔹 Analgesics and Sedatives
| Drug | Use |
|---|---|
| Fentanyl | Potent opioid analgesic |
| Midazolam | Anxiolytic, sedative |
| Morphine | Pain relief in longer surgeries |
🩺 NURSE’S RESPONSIBILITIES DURING GENERAL ANAESTHESIA
✅ 1. Preoperative Phase
- Confirm patient’s identity, consent, fasting status
- Assess allergies, past anesthetic history
- Monitor baseline vitals, blood glucose, ECG
- Prepare IV line, shave site if required
- Ensure emergency drugs and suction are ready
- Support patient psychologically before induction
✅ 2. Intraoperative Phase
- Assist in positioning patient properly
- Monitor vital signs continuously
- Provide sterile assistance if needed
- Watch for signs of hypoxia, hypotension, or reaction
- Record time of induction, maintenance, and events
✅ 3. Post-Anesthesia Care
- Position in lateral recovery position
- Maintain airway and oxygen support
- Monitor SpO₂, BP, pulse, consciousness
- Observe for vomiting, shivering, restlessness
- Report delayed awakening or complications
❗ COMPLICATIONS OF GENERAL ANAESTHESIA
| System | Possible Complication |
|---|---|
| Respiratory | Airway obstruction, aspiration, hypoxia |
| Cardiovascular | Hypotension, arrhythmia, arrest |
| CNS | Delirium, confusion, delayed recovery |
| Allergic | Anaphylaxis |
| Rare | Malignant hyperthermia (genetic reaction to GA drugs) |
🧾 SUMMARY TABLE
| Component | Details |
|---|---|
| Types | Inhalational, IV, Balanced, TIVA |
| Indications | Major surgeries, unconscious procedures |
| Contraindications | Cardiac disease, respiratory failure, MH risk |
| Stages | Analgesia → Excitement → Surgical → Paralysis |
| Equipment | Anesthesia machine, monitors, ETT |
| Drugs | Propofol, Sevoflurane, Succinylcholine, Fentanyl |
| Nursing Role | Monitoring, airway support, emergency prep |
👩⚕️ ROLE OF NURSE IN GENERAL ANESTHESIA.
✅ DEFINITION
The nurse’s role in general anesthesia involves providing comprehensive care and support before, during, and after the administration of general anesthesia to ensure patient safety, maintain sterility, monitor vital signs, and assist the anesthesiologist.
🎯 Goal: Ensure smooth, safe anesthesia care and early detection of complications.
🧭 PHASE-WISE ROLE OF THE NURSE
🔷 1. Pre-Anesthetic Phase (Before Anesthesia)
| Task | Nurse’s Responsibility |
|---|---|
| Assessment | – Check patient identity, consent, allergies, fasting status |
- Review investigations (ECG, CBC, X-ray, etc.)
- Obtain baseline vitals | | Psychological support | – Calm and reassure anxious patient
- Provide clear explanation of procedure | | Preparation of patient | – Remove dentures, jewelry, nail polish
- Assist in bladder emptying
- Position patient on OT table | | Preparation of equipment | – Ensure suction, oxygen, anesthesia machine, airway devices (ET tube, mask) are ready and working
- Check IV line and fluid availability | | Drug preparation | – Label and prepare emergency drugs as per protocol
- Assist anesthetist in drawing up or passing drugs |
🔷 2. Intra-Anesthetic Phase (During Anesthesia)
| Task | Nurse’s Responsibility |
|---|---|
| Airway support | – Assist in intubation (pass laryngoscope/ETT) |
- Provide suction and secure airway | | Vital sign monitoring | – Observe ECG, BP, SpO₂, respiration
- Record vitals at regular intervals | | Positioning | – Maintain safe and comfortable position with padding
- Avoid pressure sores or nerve injuries | | Observation for reaction | – Watch for signs of allergy, hypoxia, hypotension, arrhythmias | | Assistance to anesthetist| – Pass instruments or adjust gas flow/masks as instructed
- Help monitor fluid balance and IV medications | | Aseptic technique | – Maintain sterile field when assisting in induction or suctioning | | Documentation | – Record time of induction, airway device used, vitals, drugs given |
🔷 3. Post-Anesthetic Phase (Recovery Room / PACU)
| Task | Nurse’s Responsibility |
|---|---|
| Airway maintenance | – Place in lateral recovery position |
- Monitor for obstruction, stridor, or choking | | Monitoring vitals | – Check BP, pulse, respiratory rate, SpO₂ every 15 minutes (or as ordered) | | Consciousness check | – Assess response to verbal commands and orientation | | Observation for complications | – Watch for nausea, vomiting, shivering, delayed awakening, cyanosis, bleeding | | Pain relief | – Administer analgesics as per doctor’s order | | Documentation | – Record anesthesia type, recovery status, complications, handover to ward staff |
🧰 EMERGENCY PREPAREDNESS BY NURSE
- Keep crash cart, defibrillator, airway equipment ready
- Know dosages and uses of emergency drugs (Adrenaline, Atropine, Dopamine, etc.)
- Recognize and respond to code blue situations (cardiac arrest)
- Monitor for malignant hyperthermia signs (rigidity, high fever, tachycardia)
📋 DOCUMENTATION BY NURSE
| What to Record |
|---|
- Time of induction and recovery
- Type and dose of drugs given
- Vitals before, during, after anesthesia
- Airway device used (ETT, LMA)
- Any adverse events or complications
- Name of anesthetist and surgical team
- Transfer and handover details
🧾 SUMMARY TABLE
| Phase | Nurse’s Role Highlights |
|---|---|
| Pre-anesthesia | Patient prep, psychological support, equipment & drug check |
| During GA | Monitor vitals, assist airway management, ensure safety |
| Post-GA | Recovery position, airway care, observe for complications |
| Emergency role | Prepare crash cart, assist in resuscitation |
| Documentation | Record all actions, drugs, vitals, and outcomes accurately |
💡 KEY PRINCIPLES FOR NURSES IN GA CARE
- Safety first – airway, oxygen, vital signs
- Sterility – maintain aseptic technique
- Support – reassure and comfort patient
- Surveillance – early detection of danger signs
- Speed – respond quickly in emergencies
- Systematic documentation – legal and clinical importance
💉 SPINAL ANAESTHESIA.

✅ DEFINITION
Spinal anaesthesia is a type of regional anaesthesia where a local anesthetic drug is injected into the subarachnoid space (cerebrospinal fluid) of the lumbar spine to induce temporary loss of sensation and movement in the lower part of the body.
🎯 The patient remains conscious but experiences complete pain relief below the level of the block.
📍 SITE OF INJECTION
- Into the subarachnoid space between the L3–L4 or L4–L5 intervertebral space
- Below the end of the spinal cord (L1–L2 in adults) to avoid injury
🔍 TYPES OF SPINAL ANAESTHESIA
| Type | Description |
|---|---|
| Low spinal | Block level up to T12 (perineal procedures) |
| Mid spinal | Block level up to T6–T10 (C-section, hernia repair) |
| High spinal | Block level above T4 (rare; risk of respiratory depression) |
| Single-shot spinal | One-time injection (common method) |
| Continuous spinal | Using a catheter for prolonged anesthesia (less common) |
💉 METHOD OF ADMINISTRATION (STEP-BY-STEP)
| Step | Action |
|---|---|
| 1 | Explain procedure, obtain consent |
| 2 | Ensure NPO status, IV line, and baseline vitals |
| 3 | Position patient in sitting or lateral position with spine flexed |
| 4 | Clean back with antiseptic, drape with sterile towel |
| 5 | Identify L3–L4 space, inject local anesthetic (e.g., lignocaine) to numb skin |
| 6 | Insert spinal needle (22G–25G) until CSF flows |
| 7 | Inject anesthetic drug slowly (usually 2–4 ml) |
| 8 | Remove needle, apply sterile dressing |
| 9 | Position patient supine and monitor vitals |
🛑 INDICATIONS FOR SPINAL ANAESTHESIA
- Lower abdominal and pelvic surgeries:
- Cesarean section
- Inguinal hernia repair
- Hysterectomy
- Lower limb surgeries:
- Knee replacement
- Hip surgeries
- Varicose vein surgeries
- Urological procedures:
- TURP (transurethral resection of prostate)
- Bladder stones
❌ CONTRAINDICATIONS
| Type | Example |
|---|---|
| Absolute |
- Patient refusal
- Local infection at puncture site
- Coagulation disorders (bleeding risk)
- Raised intracranial pressure (risk of brain herniation)
| Relative | - Hypovolemia
- Severe spinal deformity
- Aortic or mitral stenosis
- Allergy to local anesthetics |
🔄 PHYSIOLOGICAL EFFECTS
| System Affected | Effect |
|---|---|
| Nervous system | Loss of sensation, reflexes, and motor activity below block level |
| Cardiovascular | Bradycardia, hypotension due to sympathetic block |
| Respiratory | Minimal effect unless block is too high |
| Urinary | Urinary retention (monitor output) |
📈 STAGES OF SPINAL ANAESTHESIA (Onset Process)
| Stage | Description |
|---|---|
| 1. Sensory Block | Loss of pain and temperature below block |
| 2. Motor Block | Paralysis of lower limbs (depending on drug dose) |
| 3. Autonomic Block | Vasodilation, drop in BP, loss of bladder control |
| Duration | 1.5 to 3 hours (depends on drug used) |
🧰 EQUIPMENT USED
| Equipment | Purpose |
|---|---|
| Sterile spinal needle (22–25G) | For injecting into subarachnoid space |
| Syringe (2–5 ml) | For anesthetic agent |
| Sterile gloves and drapes | Maintain asepsis |
| Antiseptic solution (Betadine/Chlorhexidine) | Skin prep |
| Tray with spinal set | Contains all needed items |
| IV fluids and cannula | To maintain BP |
| Monitoring devices | ECG, BP, pulse oximeter |
| Emergency drugs | Atropine, Ephedrine (for bradycardia or hypotension) |
| Oxygen supply | If patient becomes hypoxic |
💊 COMMON DRUGS USED
| Drug Name | Type | Duration |
|---|---|---|
| Lignocaine (2%) | Short-acting local anesthetic | 1–1.5 hrs |
| Bupivacaine (0.5%) | Long-acting anesthetic | 2–3 hrs |
| Adrenaline (optional) | Vasoconstrictor (prolongs action) | Prolongs effect |
| Fentanyl (add-on) | Opioid for pain relief | Enhances effect |
👩⚕️ NURSE’S RESPONSIBILITIES IN SPINAL ANAESTHESIA
🔹 Before Procedure
- Explain procedure, check consent
- Verify NPO status, allergies, and lab results
- Assist in positioning and ensure privacy
- Prepare spinal tray and ensure sterile field
- Monitor baseline BP, pulse, SpO₂
🔹 During Procedure
- Monitor vitals every 2–5 minutes
- Observe for signs of hypotension, bradycardia, headache
- Reassure the patient and keep them calm
- Provide oxygen support if needed
- Assist anesthetist with sterile handling
🔹 After Procedure
- Keep patient supine for 6–8 hours
- Monitor for urinary retention, back pain, headache
- Check return of motor and sensory function
- Encourage oral fluids (unless contraindicated)
- Document drug used, dose, time, vitals, and complications
⚠️ COMPLICATIONS
| Complication | Description |
|---|---|
| Post-spinal headache | Due to CSF leakage |
| Hypotension | Due to vasodilation |
| Bradycardia | Due to sympathetic block |
| Urinary retention | Common; may require catheterization |
| Total spinal block | Dangerous; high block causing respiratory arrest |
| Infection or abscess | Rare but serious |
| Nerve damage | Very rare |
🧾 SUMMARY TABLE
| Item | Details |
|---|---|
| Site | Subarachnoid space at L3–L4 or L4–L5 |
| Patient status | Conscious but pain-free |
| Indications | C-section, hernia, limb surgery |
| Contraindications | Infection, bleeding disorders, raised ICP |
| Drugs | Bupivacaine, Lignocaine, Adrenaline |
| Duration | 1.5–3 hours |
| Monitoring | Vitals every 5–10 minutes |
| Nurse’s Role | Assist, monitor, position, observe complications |
👩⚕️ ROLE OF NURSE IN SPINAL ANAESTHESIA.
✅ DEFINITION
The nurse’s role in spinal anesthesia includes preparing the patient and environment, assisting the anesthetist, monitoring the patient throughout the procedure, and ensuring safe recovery—with a focus on asepsis, patient safety, and comfort.
🎯 Spinal anesthesia is administered into the subarachnoid space, and nurses play a vital role in ensuring the procedure is safe, sterile, and effective.
🔷 PHASE-WISE ROLE OF THE NURSE
🟢 1. Pre-Anesthesia Phase (Before the Procedure)
| Responsibility | Details |
|---|---|
| Assessment | – Check patient identity, consent, NPO status |
- Confirm allergy history, lab reports (coagulation profile, etc.) | | Patient Preparation | – Remove jewelry, dentures, nail polish
- Assist in emptying bladder
- Establish IV line and baseline vitals (BP, HR, SpO₂) | | Psychological Support | – Explain the procedure
- Reduce fear and anxiety with reassurance | | Positioning | – Help patient into sitting or lateral position with spine flexed (arched back)
- Maintain privacy and comfort | | Equipment & Tray Setup | – Prepare sterile spinal tray (needle, syringe, gloves, antiseptic)
- Ensure emergency drugs and suction are ready
- Provide sterile drapes and anesthetic solutions | | Aseptic Technique | – Assist with hand hygiene, sterile gloves, and maintain sterile field |
🟢 2. During Anesthesia Administration
| Responsibility | Details |
|---|---|
| Assist the Anesthetist | – Pass sterile equipment (syringe, needle, local anesthetic) |
- Support patient to remain still during injection | | Monitor Patient | – Observe for signs of discomfort, hypotension, bradycardia
- Record vital signs every 2–5 minutes | | Ensure Safety | – Monitor for dizziness, nausea, or anxiety
- Ensure patient is not left unattended | | Provide Oxygen (if needed) | – Assist with nasal oxygen administration in case of low SpO₂ |
🟢 3. Post-Anesthesia (Recovery Phase)
| Responsibility | Details |
|---|---|
| Positioning | – Keep patient in supine or slightly elevated head position for 6–8 hours to prevent spinal headache |
| Monitor Vitals | – Check BP, pulse, respiratory rate, SpO₂ regularly |
- Look for signs of delayed complications | | Assess Sensory/Motor Return | – Check movement and sensation in lower limbs
- Record time of return to normal function | | Observe for Complications | – Monitor for:
- Headache
- Urinary retention
- Hypotension
- Back pain
- Nausea | | Documentation | – Record:
- Name and dose of anesthetic
- Time of injection and recovery
- Patient’s response and complications (if any)
- Vitals before/during/after the procedure |
🚨 EMERGENCY PREPAREDNESS
| Task | Action |
|---|---|
| Crash cart check | Ensure emergency equipment is nearby |
| Emergency drugs ready | Atropine, Ephedrine, Oxygen |
| Rapid response | Be prepared for hypotension, bradycardia, respiratory depression, or seizure |
📝 NURSE’S DOCUMENTATION RESPONSIBILITIES
- Name of the anesthetic agent and its concentration
- Dose and site of administration
- Time of administration
- Level of sensory/motor block
- Vitals at intervals
- Patient’s recovery time and complications
- Name of anesthetist and assisting staff
❗ NURSE’S OBSERVATION FOR COMPLICATIONS
| Complication | Nursing Observation |
|---|---|
| Hypotension | Sudden drop in BP, dizziness |
| Bradycardia | Pulse < 60 bpm |
| Post-Spinal Headache | Occurs when patient sits up too early |
| Urinary Retention | Bladder fullness, no voiding |
| Back Pain | Pain at injection site |
| High Spinal Block | Difficulty breathing, unconsciousness (emergency) |
🧾 SUMMARY TABLE
| Phase | Nurse’s Key Role |
|---|---|
| Before | Consent, preparation, positioning, tray setup |
| During | Assist anesthetist, monitor vitals, reassure patient |
| After | Monitor vitals, assess recovery, prevent complications |
| Always | Maintain asepsis, ensure documentation, emergency readiness |
💉 REGIONAL & LOCAL ANAESTHESIA.

✅ DEFINITIONS
- Regional Anesthesia: A type of anesthesia where a large area or region of the body is anesthetized by blocking nerve conduction, while the patient remains conscious.
- Local Anesthesia: Loss of sensation in a small, specific area of the body, usually by injecting an anesthetic near the nerves, with no effect on consciousness.
🔍 TYPES OF REGIONAL ANESTHESIA
| Type | Description | Example Procedures |
|---|---|---|
| Spinal Anesthesia | Drug injected into subarachnoid space (L3–L4) | C-section, lower limb surgery |
| Epidural Anesthesia | Drug injected into epidural space | Labor, abdominal surgeries |
| Caudal Block | Anesthesia via sacral canal | Pediatric surgeries |
| Nerve Block | Local anesthetic injected near specific nerve/plexus | Brachial plexus block for arm surgery |
| Field Block | Anesthetic injected in a pattern to block nerves in an area | Hernia repair |
| IV Regional (Bier Block) | Anesthetic injected into a vein with tourniquet | Short limb surgeries |
🔍 TYPES OF LOCAL ANESTHESIA
| Type | Method | Example Use |
|---|---|---|
| Surface (Topical) | Applied to mucosa or skin | Throat spray before endoscopy |
| Infiltration | Injected into tissues directly | Wound suturing |
| Ring Block | Anesthetic injected around a digit | Finger/toe surgery |
| Tumescent | Large volume for liposuction | Cosmetic procedures |
💉 METHODS OF ADMINISTRATION
| Route | Description |
|---|---|
| Injection | Infiltration, nerve block, epidural/spinal |
| Topical Application | Creams, gels, sprays on mucosa or skin |
| Catheter Technique | Continuous infusion (e.g., epidural catheter for labor) |
🩺 INDICATIONS
🔹 Regional Anesthesia
- Cesarean section
- Hernia repair
- Lower limb surgeries
- Urological procedures
- Labor pain management
- Orthopedic or trauma surgeries
🔹 Local Anesthesia
- Minor surgical procedures (suturing, wart/cyst removal)
- Dental procedures
- Skin biopsy
- Foreign body removal
🚫 CONTRAINDICATIONS
🔹 Regional Anesthesia
| Absolute | Relative |
|---|---|
| Patient refusal | Coagulopathy |
| Infection at site | Deformity/spinal surgery |
| Allergy to drugs | Hypovolemia |
| Raised ICP (for spinal) | Sepsis |
🔹 Local Anesthesia
- Known allergy to local anesthetic (e.g., lignocaine)
- Inflamed/infected injection site
- Vascular disease at site (risk of necrosis)
🔄 PHYSIOLOGICAL EFFECTS
| Effect | Description |
|---|---|
| Sensory block | Loss of pain and temperature sensation |
| Motor block | Paralysis (depending on depth of block) |
| Sympathetic block | Vasodilation, hypotension (especially spinal/epidural) |
| Minimal systemic effect | Patient remains conscious and awake |
🧬 STAGES (Mostly for Regional Blocks)
| Stage | Description |
|---|---|
| Onset | Within 5–15 mins post-injection |
| Full Effect | Complete loss of pain, possible motor block |
| Recovery | Gradual return of sensation/movement |
| Duration | Varies from 30 minutes to 4 hours depending on drug |
🧰 EQUIPMENT USED
| Equipment | Use |
|---|---|
| Sterile gloves and drapes | Aseptic technique |
| Syringes (2–10 ml) | For drug injection |
| Needles (different lengths) | Spinal: long; Nerve block: short or guided |
| Spinal/Epidural needle | Tuohy needle (epidural), Quincke (spinal) |
| Local anesthetic drugs | Lignocaine, Bupivacaine |
| Antiseptic solution | Skin preparation |
| Monitoring devices | ECG, BP cuff, Pulse oximeter |
| Emergency drugs & oxygen | For management of complications |
💊 COMMONLY USED DRUGS
| Drug | Concentration | Duration | Notes |
|---|---|---|---|
| Lignocaine (Xylocaine) | 1–2% | Short-acting (1–1.5 hr) | Quick onset |
| Bupivacaine | 0.25–0.5% | Long-acting (2–4 hr) | Common for spinal/epidural |
| Ropivacaine | 0.2–0.75% | Long duration | Less cardiotoxic |
| Adrenaline | Mixed with local | Prolongs action | Vasoconstriction |
| Fentanyl, Morphine | Epidural/spinal add-on | Enhances pain relief |
👩⚕️ NURSE’S ROLE IN REGIONAL & LOCAL ANAESTHESIA
✅ Before Procedure
- Explain procedure and obtain informed consent
- Assess allergies, vital signs, NPO status (for regional)
- Prepare sterile tray with correct drugs and equipment
- Assist in positioning (sitting or lateral for spinal/epidural)
- Provide emotional support and maintain privacy
✅ During Procedure
- Maintain aseptic technique
- Monitor BP, pulse, SpO₂, LOC
- Assist anesthetist with drug administration and instruments
- Watch for discomfort, hypotension, nausea, or anxiety
- Document drug used, dose, and site
✅ After Procedure
- Monitor return of motor/sensory function
- Watch for complications (headache, hypotension, urinary retention)
- Reassure patient and provide fluids if not contraindicated
- Record vital signs and document recovery
⚠️ POSSIBLE COMPLICATIONS
| Regional Anesthesia | Local Anesthesia |
|---|---|
| Hypotension, bradycardia | Localized swelling, pain |
| Spinal headache | Allergic reaction |
| Urinary retention | Numbness/tingling |
| Nerve injury (rare) | Accidental vascular injection |
| Total spinal (emergency) | Toxicity (seizure, CNS depression) |
🧾 SUMMARY TABLE
| Feature | Regional Anesthesia | Local Anesthesia |
|---|---|---|
| Consciousness | Awake | Awake |
| Area affected | Larger region | Small localized area |
| Drugs used | Bupivacaine, Lignocaine | Lignocaine, Prilocaine |
| Duration | 1–4 hours | 15 min to 1.5 hours |
| Indications | C-section, limb surgery | Suturing, dental, minor skin surgery |
| Nurse’s Role | Prep, assist, monitor, document | Same |
👩⚕️ ROLE OF NURSE IN REGIONAL ANESTHESIA.
✅ DEFINITION
Regional Anesthesia is a technique that involves injecting an anesthetic near a cluster of nerves to numb a specific region of the body (e.g., spinal, epidural, nerve blocks), while the patient remains conscious.
The nurse’s role is to prepare the patient and environment, assist the anesthetist, monitor the patient, and provide post-anesthesia care and safety.
🧭 PHASE-WISE NURSING RESPONSIBILITIES IN REGIONAL ANESTHESIA
🟢 1. Pre-Anesthetic Phase (Before Administration)
| Responsibility | Description |
|---|---|
| Assessment | – Verify identity, check consent, allergies, NPO status |
- Review investigations (CBC, PT/INR, ECG, X-ray) | | Psychological Support | – Explain the procedure
- Alleviate patient fears (common with spinal/epidural) | | Patient Preparation | – Assist in removing jewelry, dentures
- Ensure bladder is emptied
- Obtain baseline vitals (BP, pulse, SpO₂)
- Maintain privacy | | Equipment Preparation | – Prepare regional anesthesia tray
- Check availability of drugs (e.g., bupivacaine, lignocaine)
- Arrange sterile gloves, drapes, monitoring equipment, emergency drugs |
🟢 2. During Administration
| Responsibility | Description |
|---|---|
| Patient Positioning | – Assist into sitting or lateral curled position (especially for spinal/epidural) |
- Maintain comfort and safety | | Aseptic Assistance | – Pass sterile instruments to anesthetist
- Maintain sterile field and handle only sterile items as needed | | Monitoring | – Observe patient continuously
- Monitor BP, pulse, SpO₂, LOC every 2–5 minutes | | Emotional Support | – Reassure and speak calmly to patient
- Watch for signs of anxiety, dizziness, or discomfort | | Documentation | – Note drug name, dose, site, time, and patient response |
🟢 3. Post-Anesthesia (Recovery Phase)
| Responsibility | Description |
|---|---|
| Positioning | – Keep patient flat or slightly elevated (especially after spinal) |
- Encourage rest to prevent post-spinal headache | | Monitoring | – Continue to monitor vitals every 15 minutes
- Watch for complications (hypotension, headache, urinary retention) | | Assess Recovery | – Check return of sensation and movement
- Encourage oral fluids when allowed | | Manage Complications| – Prepare to manage:
- Bradycardia
- Hypotension
- Nausea/vomiting
- Retention or delayed recovery | | Documentation | – Record full recovery time, vitals, complications, drug effects, and handover to ward staff |
🚨 EMERGENCY PREPAREDNESS
- Keep crash cart nearby
- Prepare Atropine, Ephedrine, Oxygen
- Monitor for total spinal block, respiratory distress, allergic reactions
- Be ready to initiate code blue and assist resuscitation if needed
📝 NURSE’S DOCUMENTATION RESPONSIBILITIES
- Name and dose of anesthetic used
- Time and site of injection
- Patient’s position during procedure
- Vitals before, during, and after
- Any adverse effects or reactions
- Patient’s recovery time and response
- Name of anesthetist and assisting nurse
⚠️ COMPLICATIONS TO WATCH FOR
| Complication | Nurse’s Response |
|---|---|
| Hypotension | Lower head, give IV fluids, inform doctor |
| Bradycardia | Monitor closely, prepare atropine |
| Spinal headache | Keep patient flat, provide fluids, inform doctor |
| Urinary retention | Monitor output, catheterize if needed |
| Respiratory distress (rare) | Oxygen support, call anesthetist |
| Total spinal (emergency) | Assist resuscitation immediately |
🧾 SUMMARY TABLE
| Phase | Nurse’s Key Role |
|---|---|
| Before | Consent, prep, position, asepsis, vitals |
| During | Assist, monitor, support, document |
| After | Monitor recovery, check motor/sensory return, observe complications |
| Always | Maintain aseptic technique, ensure safety, be ready for emergencies |
💉 GENERAL ANESTHESIA – ADVANTAGES & DISADVANTAGES
✅ ADVANTAGES OF GENERAL ANESTHESIA
| Advantage | Explanation |
|---|---|
| Complete Unconsciousness | Patient is unaware, feels no pain, and does not recall the procedure |
| Full Muscle Relaxation | Useful for surgeries requiring deep muscle dissection (e.g., abdominal, thoracic) |
| Airway Control (Intubation) | Secure airway allows control of ventilation and oxygenation |
| Suitable for Long Surgeries | Ideal for procedures lasting >2 hours |
| Controlled Environment | Depth of anesthesia, vitals, and response can be precisely monitored and adjusted |
| Patient Cooperation Not Needed | Useful in children, mentally ill, anxious, or uncooperative patients |
| Can Be Used in Any Surgical Area | Head, neck, thorax, abdomen, limbs – no regional limitation |
❌ DISADVANTAGES OF GENERAL ANESTHESIA
| Disadvantage | Explanation |
|---|---|
| Loss of Protective Reflexes | Risk of aspiration due to loss of cough and gag reflex |
| Airway Management Required | Requires intubation, suctioning, and close respiratory monitoring |
| Post-Operative Nausea/Vomiting (PONV) | Common side effect after waking up |
| Cardio-Respiratory Depression | Risk of hypotension, bradycardia, arrhythmias, or respiratory arrest |
| Delayed Recovery | Especially in elderly or liver/kidney-compromised patients |
| Higher Cost and Equipment Needs | Requires anesthesia machine, gas supplies, trained personnel |
| More Monitoring Required | ECG, SpO₂, BP, ETCO₂, etc. needed throughout procedure |
| Rare but Serious Risks | Malignant hyperthermia, allergic reactions, aspiration pneumonia |
🧾 QUICK COMPARISON CHART
| Feature | General Anesthesia |
|---|---|
| Patient Conscious? | No (completely unconscious) |
| Pain-Free? | Yes |
| Airway Support Needed? | Yes (ET tube, mask) |
| Used For? | Major, long, complex surgeries |
| Recovery Time | Longer |
| Risks | More systemic effects |
💉 SPINAL ANAESTHESIA – ADVANTAGES & DISADVANTAGES
✅ ADVANTAGES OF SPINAL ANAESTHESIA
| Advantage | Explanation |
|---|---|
| Rapid Onset | Provides immediate pain relief (within 2–5 minutes) |
| Effective Analgesia and Anesthesia | Produces profound sensory and motor block below the level of injection |
| Avoids Airway Manipulation | No need for intubation or ventilator support (patient breathes spontaneously) |
| Patient Remains Conscious | Suitable for patients who wish to avoid general anesthesia |
| Reduced Risk of Nausea/Vomiting | Less post-operative nausea compared to general anesthesia |
| Minimal Drug Requirement | Requires a small dose of anesthetic for effective action |
| Lower Blood Loss | Sympathetic block leads to vasodilation and reduced bleeding |
| Faster Post-Operative Recovery | Earlier return to eating, mobility, and discharge in some cases |
| Useful for High-Risk Patients | Safer in elderly or those with cardiac/respiratory compromise (if stable) |
❌ DISADVANTAGES OF SPINAL ANAESTHESIA
| Disadvantage | Explanation |
|---|---|
| Limited to Lower Body Surgeries | Not suitable for upper abdominal, thoracic, or head/neck surgeries |
| Risk of Hypotension | Due to vasodilation from sympathetic block |
| Post-Spinal Headache | Common complication if patient sits up too early or CSF leak occurs |
| Urinary Retention | May delay voiding and require catheterization |
| Back Pain or Soreness | Possible at injection site |
| Shorter Duration | Not suitable for long surgeries unless additives or repeat doses used |
| Patient Cooperation Required | Patient must remain still during the procedure |
| Contraindicated in Some Cases | Not safe in patients with bleeding disorders, infection at site, or raised ICP |
| Rare Neurological Complications | Nerve damage, abscess, meningitis (very rare but possible) |
🧾 COMPARISON SNAPSHOT
| Feature | Spinal Anesthesia |
|---|---|
| Consciousness | Patient remains awake |
| Onset | Fast (2–5 minutes) |
| Duration | 1.5 to 3 hours |
| Suitable for | Lower limb, pelvic, C-section |
| Airway Control Needed? | No |
| Monitoring Required | Moderate |
| Common Side Effects | Hypotension, headache, urinary retention |
💉 REGIONAL ANESTHESIA – ADVANTAGES & DISADVANTAGES
✅ ADVANTAGES OF REGIONAL ANESTHESIA
| Advantage | Explanation |
|---|---|
| Patient Remains Conscious | Suitable for patients who want or need to avoid general anesthesia |
| Effective Pain Control | Offers good post-operative analgesia, especially with continuous epidural |
| No Airway Manipulation | No intubation needed; lower risk of airway complications |
| Fewer Systemic Side Effects | Less nausea, vomiting, sedation compared to general anesthesia |
| Less Blood Loss | Vasodilation due to sympathetic block reduces bleeding during surgery |
| Early Mobilization | Patients can often ambulate earlier, especially after epidurals |
| Useful in High-Risk Patients | Better option for elderly, respiratory-compromised, or cardiac patients (if vitals stable) |
| Cost-Effective | Uses fewer drugs and less recovery time compared to general anesthesia |
| Postoperative Pain Relief | Can continue analgesia post-op through catheter (epidural/nerve block) |
❌ DISADVANTAGES OF REGIONAL ANESTHESIA
| Disadvantage | Explanation |
|---|---|
| Limited to Certain Surgeries | Suitable only for specific regions (e.g., limbs, pelvis, lower abdomen) |
| Requires Patient Cooperation | Patient must remain still during the block |
| Risk of Hypotension | Due to sympathetic nerve blockade, especially in spinal/epidural |
| Inadequate Block | May need to convert to general anesthesia if block fails |
| Complications at Injection Site | Bleeding, infection, nerve injury (rare) |
| Technical Expertise Required | Needs skilled anesthesiologist for accurate administration |
| Urinary Retention | Due to autonomic block, especially with spinal or epidural |
| Contraindicated in Certain Patients | E.g., bleeding disorders, infection at site, severe hypovolemia |
| Post-Anesthesia Headache or Backache | Common after spinal anesthesia |
🧾 QUICK SUMMARY TABLE
| Feature | Regional Anesthesia |
|---|---|
| Consciousness | Awake |
| Airway Management Needed? | No |
| Best For | Lower abdomen, limb surgeries |
| Common Complications | Hypotension, failed block, headache |
| Advantages | Less systemic risk, better post-op pain control |
| Disadvantages | Limited use, requires skill and patient cooperation |
💉 ANAESTHESIA.
✅ DEFINITION
Anesthesia is a medical technique that causes reversible loss of sensation, with or without loss of consciousness, to allow surgical or diagnostic procedures to be carried out without pain.
🎯 Purpose: To relieve pain, suppress reflexes, ensure patient immobility and comfort during procedures.
🔍 TYPES OF ANAESTHESIA
| Type | Description |
|---|---|
| General Anesthesia (GA) | Total loss of consciousness and sensation; patient is completely asleep |
| Regional Anesthesia | Loss of sensation in a large area by blocking nerve supply; patient remains awake |
| Local Anesthesia | Numbs a small area of the body; patient is fully conscious |
| Conscious Sedation (Moderate Sedation) | Patient remains relaxed and drowsy, but responsive and able to breathe independently |
💉 METHODS OF ADMINISTRATION
| Type of Anaesthesia | Route of Administration |
|---|---|
| General | Inhalation (mask, ET tube), IV injection |
| Regional | Injection near nerves (e.g., spinal, epidural, nerve block) |
| Local | Infiltration, topical application, spray |
| Sedation | IV injection (e.g., midazolam, fentanyl) |
🩺 INDICATIONS FOR ANAESTHESIA
| Type | Indicated for |
|---|---|
| General | Major surgeries: abdominal, thoracic, neuro, cardiac |
| Regional | C-section, limb surgery, hernia repair, urology procedures |
| Local | Minor surgery: wound suturing, dental, skin biopsy |
| Sedation | Diagnostic procedures: endoscopy, colonoscopy, minor OT procedures |
🚫 CONTRAINDICATIONS
| Type | Contraindications |
|---|---|
| General | Severe cardiopulmonary disease, allergy to anesthetic, raised ICP |
| Regional | Infection at injection site, coagulopathy, patient refusal, spine deformity |
| Local | Allergy to local anesthetics, infection at application site |
| Sedation | Severe respiratory depression, uncooperative patient without airway support |
🧬 PHYSIOLOGICAL EFFECTS
| System | Effect |
|---|---|
| Nervous system | Loss of consciousness or sensation |
| Muscular system | Muscle relaxation (GA, regional) |
| Cardiovascular | May cause hypotension, bradycardia (especially in spinal) |
| Respiratory | May depress breathing (GA, sedation) |
| Gastrointestinal | Nausea, vomiting (mostly with GA) |
| Urinary system | Retention or suppression (spinal/epidural) |
📈 STAGES OF GENERAL ANAESTHESIA (Guedel’s Classification)
| Stage | Description |
|---|---|
| Stage I – Analgesia | Consciousness with decreased pain awareness |
| Stage II – Excitement | Loss of consciousness with uncontrolled movements |
| Stage III – Surgical Anesthesia | Ideal stage for surgery; no movement, no pain, regular breathing |
| Stage IV – Medullary Paralysis | Overdose stage; depression of vital centers – emergency condition |
✔️ Surgical procedures should occur in Stage III.
🛠️ EQUIPMENT USED IN ANAESTHESIA
| Equipment | Use |
|---|---|
| Anesthesia machine | Delivers anesthetic gases and oxygen |
| Pulse oximeter | Monitors oxygen saturation |
| ECG monitor | Tracks heart rate and rhythm |
| BP monitor (NIBP) | Measures blood pressure |
| Capnograph | Measures exhaled CO₂ |
| Laryngoscope | Used for intubation |
| Endotracheal tube (ETT) | Maintains airway in GA |
| Suction machine | Removes secretions |
| Oxygen mask/nasal cannula | Delivers oxygen |
| Crash cart | Emergency medications and equipment |
💊 COMMON ANAESTHETIC DRUGS
🔹 General Anesthesia
| Type | Drug Examples | Purpose |
|---|---|---|
| Induction agents | Propofol, Thiopentone, Ketamine | To induce unconsciousness |
| Inhalational agents | Sevoflurane, Isoflurane, Nitrous Oxide | To maintain anesthesia |
| Muscle relaxants | Succinylcholine, Vecuronium | For intubation and relaxation |
| Opioids | Fentanyl, Morphine | Pain relief |
| Anticholinergics | Atropine, Glycopyrrolate | Reduce secretions, prevent bradycardia |
🔹 Regional & Local Anesthesia
| Drug | Type | Use |
|---|---|---|
| Lignocaine (2%) | Local anesthetic | Infiltration, nerve block |
| Bupivacaine (0.5%) | Long-acting local anesthetic | Spinal, epidural anesthesia |
| Ropivacaine | Newer long-acting anesthetic | Safer alternative |
| Adrenaline (optional) | Vasoconstrictor | Prolongs duration of action |
👩⚕️ NURSE’S ROLE IN ANAESTHESIA CARE
| Phase | Role |
|---|---|
| Pre-operative | Check consent, allergies, fasting status, prepare equipment |
| During anesthesia | Monitor vitals, assist anesthetist, manage airway |
| Post-operative | Monitor recovery, position patient, manage pain, watch for complications |
⚠️ COMPLICATIONS OF ANAESTHESIA
| Type | Examples |
|---|---|
| General | Hypotension, bradycardia, aspiration, airway obstruction, malignant hyperthermia |
| Regional | Post-spinal headache, hypotension, nerve damage, urinary retention |
| Local | Allergic reaction, tissue necrosis, toxicity (if injected into a vessel) |
| Sedation | Hypoventilation, drowsiness, airway obstruction |
🧾 SUMMARY TABLE
| Feature | General | Regional | Local | Sedation |
|---|---|---|---|---|
| Consciousness | Unconscious | Conscious | Fully conscious | Drowsy but responsive |
| Airway control | Required | Not needed | Not needed | May be needed |
| Area affected | Whole body | Large region | Small area | None – for pain relief |
| Used for | Major surgeries | Limb/lower body surgeries | Minor surgeries | Endoscopy, dental |
| Onset | Rapid | Moderate | Quick | Quick |
⚖️ LEGAL ASPECTS IN INTRAOPERATIVE CARE.
✅ DEFINITION
Legal aspects in intraoperative care refer to the laws, ethical standards, and professional responsibilities that nurses and surgical staff must follow to ensure patient safety, protect patient rights, and avoid legal liability during surgery.
🎯 Goal: To ensure that all intraoperative activities are performed safely, ethically, and within the law.
📋 KEY LEGAL CONSIDERATIONS IN INTRAOPERATIVE CARE
🔹 1. Informed Consent (Legal Requirement Before Surgery)
| Point | Details |
|---|---|
| What is it? | A written and signed document that confirms the patient agrees to undergo surgery after full explanation |
| Who obtains it? | The surgeon is responsible for obtaining it; the nurse witnesses it |
| Nurse’s duty | – Ensure consent is taken before shifting to OT |
- Confirm that the consent form is signed, dated, and complete
- If unconscious/emergency: doctor may proceed with life-saving measures, but must document clearly |
🔹 2. Patient Identification and Procedure Verification (Right Patient, Right Surgery)
| Legal Safeguard | Description |
|---|---|
| Patient ID check | Use at least 2 identifiers (name, ID band, DOB) before surgery |
| Surgical site marking | Must be done by the surgeon on the correct side or limb |
| Nurse’s responsibility | – Verify patient identity |
- Cross-check consent form, OT list, and site marking
- Be part of the “Time-Out” protocol before incision to confirm right patient, right site, right procedure |
🔹 3. Maintaining Aseptic Technique (Negligence Risk)
| Legal Concern | Description |
|---|---|
| Infections due to negligence | Hospital-acquired infections (e.g., surgical site infection) due to break in asepsis may lead to legal action |
| Nurse’s role | – Follow infection control protocols strictly |
- Report and correct any break in sterility
- Maintain accurate instrument count to prevent retained foreign bodies |
🔹 4. Accurate Documentation (Legal Record)
| Why Important? | Legal proof of what happened in OT | | Nurse must document | – Start and end time of surgery
- Names of surgical and anesthesia team
- Instrument/sponge counts (before & after surgery)
- Type of anesthesia and drugs used
- Any intraoperative events or complications
- Patient’s condition during and after surgery |
🔹 5. Accountability and Scope of Practice
| Legal Principle | Description |
|---|---|
| Duty of care | Nurse is legally responsible for following standards of practice |
| Acting beyond scope | Performing tasks meant for doctors (e.g., injecting drugs without order) can lead to legal action or license cancellation |
| OT nurse’s scope | – Prepare sterile field |
- Assist with instruments
- Monitor patient
- Maintain records, not perform surgery or anesthesia independently |
🔹 6. Patient Safety (Legal Right)
| Legal Obligation | Nurse’s Role |
|---|---|
| Prevent burns, falls, pressure sores | – Use safety straps |
- Pad bony prominences
- Check cautery machine wiring | | Correct positioning | – Avoid nerve damage, pressure ulcers
- Record position used in OT notes | | Equipment safety | – Check machines, avoid use of faulty tools
- Report to biomedical team if needed |
🔹 7. Confidentiality and Privacy (Legal and Ethical)
| Legal Right | Patient has right to privacy | | Nurse’s Responsibility | – Do not discuss patient details in public areas
- Keep records secure
- Only share info with authorized staff |
🔹 8. Handling Specimens and Biomedical Waste
| Legal Rule | Biomedical Waste Management Rules, 2016 | | Nurse’s Role | – Label and send specimens correctly
- Use color-coded bins
- Avoid mixing infectious waste with general waste
- Record waste disposal (especially cytotoxic, body parts) |
🔹 9. Emergency Situations Without Consent
| Legal Doctrine | Doctrine of Implied Consent | | When Applicable | If patient is unconscious and needs life-saving surgery, doctor may proceed | | Nurse’s Duty | Document clearly that procedure was done as an emergency and consent could not be obtained in time |
⚖️ LEGAL TERMS NURSES SHOULD KNOW
| Term | Meaning |
|---|---|
| Negligence | Failure to provide expected standard of care |
| Malpractice | Professional misconduct or lack of skill |
| Battery | Performing a procedure without consent |
| Assault | Threatening to perform a procedure without consent |
| Autonomy | Patient’s right to make decisions |
| Documentation | Legal record of nursing care and activities |
🧾 SUMMARY TABLE
| Legal Aspect | Nurse’s Responsibility |
|---|---|
| Informed consent | Ensure obtained & witnessed |
| Patient identification | Verify ID, surgery site |
| Asepsis & safety | Maintain sterile field, avoid injury |
| Documentation | Accurate, timely, detailed records |
| Confidentiality | Respect privacy and secure information |
| Scope of practice | Do not act beyond training |
| Waste/specimen handling | Follow correct procedures |
| Emergency action | Document and report when consent not possible |