BSC – SEM 3 – UNIT 1 – MICROBIOLOGY
Introduction
MICRO:- VERY SMALL, NOT SEEN THROUGH NAKED EYE.
BIO:- LIFE
LOGY:- SCIENTIFIC STUDY
HISTORY OF MICROBIOLOGY :-
Physics began in ancient times, mathematics began even earlier, but the knowledge of small living things, their biology and their impact on human life only dates back to the late 19th century. Until about the 1880s, people still believed that life could be created out of thin air and that illness was caused by sins or bad smells.
Microorganisms may have come to the earth first In the old studies it has been found that even thousands of years ago there were microorganism and epidemics were caused by them. Microbiology is a science that has developed in the last 200 years.Earlier people had little knowledge of medicine but lacked knowledge about the causes of disease.Cultures and sections of society differed in treatment and opinions about why people got diseases. Bad odors were thought to be caused by diseases, treated by removing or masking the offending odors, imbalances in the body’s humors (different fluids), and treated with bleeding (bleeding), sweating (sweat) and vomiting (vomiting) of the spirit. Although the concept of cure for sins, prayers, and rituals was known, it was not attributed to small living creatures but to bad smells or spirits, such as the Devil.
(1). Varo and Columella:- The disease is caused by an invisible organism (Animalia minuta). Which is caused by breathing or eating
(2). 13th Century Roger Bacon :-
It proved that diseases originate from invisible living creatures. They enter the body through breathing or in some other way.
(3). 1546- Fracastorius of Verona:-
He first suggested that diseases are caused by minute “seeds” or “germs” and spread from one person to another.
(4).1675 :- Antony Van Leeuwenhoek:-

Made his own Microscope which could magnify 160 times. With the help of which they found bacteria. He is called FATHER OF MICROSCOPY.
(5).1776:- Edward jenner (Edward Jenner):-
First of all prepared a vaccine against small pox (small pox). Immunization started.
(6). 1762-Von Plenciz :-
It concluded that each disease is caused by a different agent.
(7).1861 – Louis Pasteur :-
It was shown that fermentation takes place in fruits by micro-organism.
In 1856, he gave the Pasteurization method (pasteurization method), which was first used for wine and now used for milk and dairy products, to rid milk and its products of harmful micro-organisms.
In 1881 Anthrax Vaccine was discovered (anthrax is a fever caused by bacteria called anthrax).
In 1885, he developed the Posteure treatment of Rabies, which is still used today. He is known as FATHER OF MICROBIOLOGY.
(8). 1867 – Lord Lister :-
Started using phenol for prevention and treatment of Wound. Started using antiseptic solution for WOUND so that it can be kept free of micro organism. He is known as FATHER OF ANTISEPTIC SURGERY. He used carbolic acid during surgery.
(9) 1876 Robert Koch :-
In 1881, Mycobacterium tuberculosis (Mycobacterium tuberculosis-the bacteria that causes TB) was discovered.
Discovered cholera vibrio in 1883
Anthrax bacteria were isolated
FATHER OF MODERN BACTERIOLOGY
(10) 1925 – Sir Alexander Flemming

He invented the first antibiotic (drug that kills bacteria). He invented the first antibiotic penicillin.
(11) Paul Ehrlich:-
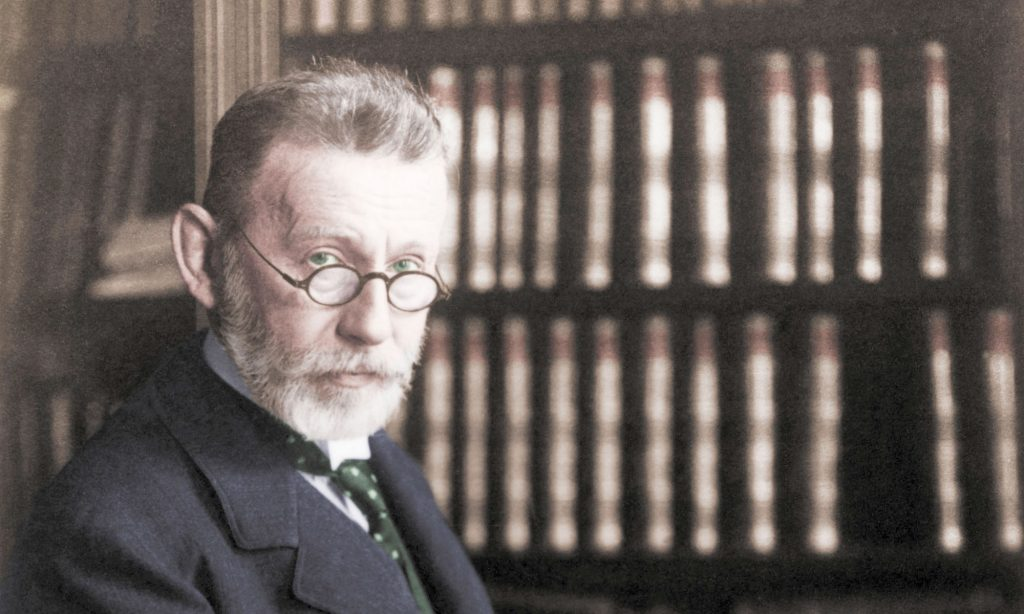
Discovered that the nature of tuberculosis bacteria is acid fast bacilli
Development of staining techniques for tissue and blood cells
Paul Ehrlich is known as the father of chemotherapy.
(12) Hans Christian Gram: Developed the method of ‘Gram stain’.
(13) Ernst Ruska: Invented the electron microscope.
(14) Elie Metchnikoff: Explain how phagocytosis is how the immune system destroys bacteria etc.
(15) Walter Gilbert and Frederick Sanger: 1977* developed the method of DNA sequencing.
(16) Karry B Mullis: Invented polymerase chain reaction (PCR).
SCOPE AND UTILITY OF KNOWLEDGE OF MICROBIOLOGY IN NURSING.
Microorganisms have the power to cause disease in humans so their characteristics and behavior can be known through this study. So that the nurse can better treat and take care of the disease caused by that microorganism.
Microbiology studies how disease occurs. We can know how it spreads and how it can be stopped. Nurses are always in the hospital environment, so knowledge of micro-biology is also necessary for infection control and self-defense.
The need for laboratory tests to identify bacteria. Different tests are done for different diseases to know which type of bacteria causes which disease.
It is well known how important personal health and immune measures are for resistance to microbial diseases.
The prevailing superstitions, ignorance and misconceptions about the diseases caused by microorganisms can be removed and correct understanding can be given. Social beliefs can be changed.
Nurses use microbiology concepts when providing patient care or performing procedures.
Microbial disease can be recognized and measures can be taken to diagnose and prevent its spread.
Nurses use warm water or antiseptic to sterilize surgical knives, needles, scissors, and other metal instruments.
For Knowledge. Importance of Microbiology in Nursing Practice Nurses must have adequate education and training in microbiology to perform many roles in clinical nursing practice. (eg, administering antibiotics, collecting specimens, preparing specimens for transport and distribution, educating patients and families, communicating results to the healthcare team, and developing care plans. Monitoring microbiology study results and patient immune status).
Microbiology: Importance and Relevance to Nursing
Introduction to Microbiology
Microbiology is the study of microorganisms, including bacteria, viruses, fungi, protozoa, and algae. It plays a crucial role in understanding infectious diseases, their prevention, and treatment. In nursing, microbiology is an essential subject as nurses are directly involved in patient care, infection control, and health promotion.
Importance of Microbiology in Nursing
Microbiology is highly relevant to nursing practice in various ways:
1. Understanding Infection and Disease
- Nurses need to understand the causes of infectious diseases, the mode of transmission, and how to break the chain of infection.
- Knowledge of pathogenic microorganisms helps in identifying symptoms and implementing appropriate interventions.
2. Infection Control and Prevention
- Nurses play a key role in hospital infection control and must follow strict aseptic techniques to prevent the spread of infection.
- Proper knowledge of hand hygiene, sterilization, disinfection, and personal protective equipment (PPE) ensures a safe healthcare environment.
- Helps in implementing isolation precautions such as standard, airborne, droplet, and contact precautions to minimize hospital-acquired infections (HAIs).
3. Antibiotic Stewardship and Drug Resistance
- Understanding microbiology helps nurses administer antibiotics properly, ensuring they are given at the right dose, time, and for the correct duration.
- Awareness of antimicrobial resistance (AMR) prevents the misuse and overuse of antibiotics, which can lead to multidrug-resistant infections.
4. Wound Care and Aseptic Techniques
- Nurses handle surgical wounds, pressure ulcers, and infected wounds. Knowledge of microbiology aids in proper wound cleaning and dressing techniques to prevent infections.
- Helps in identifying signs of wound infection and implementing suitable interventions.
5. Sterilization and Disinfection
- Ensuring that medical equipment and patient-care areas are free from pathogens is essential in hospitals.
- Nurses are responsible for using proper sterilization and disinfection methods, such as:
- Autoclaving for surgical instruments.
- Chemical disinfection for surfaces and non-critical items.
- UV radiation for air sterilization in critical care areas.
6. Immunology and Vaccine Administration
- Microbiology helps in understanding the immune response to infections.
- Nurses play a critical role in vaccination programs, ensuring proper administration of vaccines like:
- BCG (for tuberculosis)
- Hepatitis B
- Influenza
- COVID-19
- Helps in educating patients about vaccine-preventable diseases and addressing vaccine hesitancy.
7. Diagnostic Testing and Laboratory Procedures
- Nurses collect and handle specimens (e.g., blood, urine, sputum, wound swabs) for microbiological testing.
- Understanding lab tests such as:
- Gram staining (bacterial classification)
- Culture and sensitivity tests (antibiotic effectiveness)
- PCR and serology tests (viral infections like COVID-19, HIV)
8. Role in Public Health and Community Nursing
- Nurses educate communities on sanitation, hygiene, safe drinking water, and food safety to prevent infectious diseases.
- Understanding epidemiology (the study of disease outbreaks) helps in preventing the spread of infections like cholera, typhoid, and malaria.
9. Microbiota and Its Role in Health
- Nurses must understand the role of normal flora (beneficial microbes) in maintaining health.
- Helps in advising patients about probiotics and the importance of gut health.
10. Management of Emerging and Re-Emerging Infectious Diseases
- Nurses must stay updated on new and re-emerging infections, such as COVID-19, Ebola, Zika virus, and drug-resistant TB.
- Proper training in outbreak response and emergency care is necessary to manage public health crises.
Relevance of Microbiology in Nursing Practice
| Microbiology Concept | Nursing Relevance |
|---|---|
| Bacteria, Viruses, Fungi, and Parasites | Helps in identifying infections and guiding treatment. |
| Chain of Infection | Guides nurses in infection control strategies. |
| Antibiotic Resistance | Ensures proper medication administration and patient education. |
| Hospital-Acquired Infections (HAIs) | Prevents infections through aseptic techniques. |
| Sterilization & Disinfection | Reduces the spread of infections in healthcare settings. |
| Immunization & Vaccines | Ensures proper vaccine administration and patient education. |
| Laboratory Diagnosis | Helps in specimen collection and understanding test results. |
| Public Health & Community Hygiene | Educates the public on disease prevention measures. |
Microbiology is fundamental to nursing practice as it provides essential knowledge for infection control, disease prevention, and patient safety. Understanding microorganisms, their effects on health, and the application of microbiological principles enable nurses to deliver high-quality, evidence-based care. With the rising threat of antimicrobial resistance and emerging infectious diseases, microbiology remains a critical pillar of modern nursing practice.
Historical Perspective of Microbiology and Its Relevance to Nursing
Introduction
Microbiology has a rich history that dates back centuries. It has evolved from early observations of invisible organisms to a well-established scientific field that plays a vital role in medicine and nursing. Understanding the historical perspective of microbiology helps nurses appreciate the importance of infection control, vaccination, sterilization, and the development of antibiotics.
Early Concepts of Microorganisms (Before the 17th Century)
Before the discovery of microorganisms, diseases were believed to be caused by supernatural forces, bad air (“miasma”), or an imbalance in body humors. Ancient civilizations, including the Greeks, Egyptians, and Romans, had primitive ideas about disease transmission.
Hippocrates and the Theory of Disease (460–370 BCE)
- Hippocrates, known as the “Father of Medicine,” rejected supernatural explanations for disease and proposed that illnesses had natural causes.
- He emphasized cleanliness, proper sanitation, and the importance of diet and environment in maintaining health.
The Roman Contributions to Public Health (1st Century CE)
- Romans introduced early hygiene and sanitation measures, such as aqueducts and sewage systems, to prevent disease.
- Galen, a Roman physician, proposed the concept of “seeds of disease” but lacked scientific evidence.
Discovery of Microorganisms: The Birth of Microbiology (17th Century)
The field of microbiology began to take shape in the 17th century with advancements in microscopy.
Antonie van Leeuwenhoek (1632–1723) – The Father of Microbiology
- A Dutch scientist, Leeuwenhoek, developed the first simple microscope with powerful magnification.
- In 1676, he observed tiny living organisms (which he called “animalcules”) in water, saliva, and other substances.
- His discoveries laid the foundation for the study of bacteria and protozoa, though their role in disease was still unknown.
Germ Theory of Disease: 19th Century Breakthroughs
Before the germ theory was established, the prevailing belief was that diseases arose spontaneously (spontaneous generation theory). This misconception was debunked by several key scientists.
Louis Pasteur (1822–1895) – The Germ Theory Pioneer
- Pasteur conducted experiments proving that microorganisms were responsible for fermentation and food spoilage.
- In the 1860s, he developed the germ theory of disease, which stated that microorganisms cause infectious diseases.
- His work led to the development of pasteurization (a process that kills harmful bacteria in milk and wine).
- Pasteur also contributed to the development of vaccines, including the rabies vaccine.
Joseph Lister (1827–1912) – Aseptic Surgery and Infection Control
- Lister applied Pasteur’s germ theory to surgery and introduced antiseptic techniques using carbolic acid (phenol).
- His innovations reduced postoperative infections and established aseptic techniques in hospitals.
- His work emphasized the importance of handwashing and sterilization, which remain essential in nursing.
Robert Koch (1843–1910) – Identifying Disease-Causing Microbes
- Koch formulated Koch’s Postulates, a set of principles used to establish a microorganism as the cause of a disease.
- He identified the bacteria responsible for anthrax (Bacillus anthracis), tuberculosis (Mycobacterium tuberculosis), and cholera (Vibrio cholerae).
- His discoveries revolutionized medical microbiology and laid the foundation for infectious disease diagnostics.
The Development of Vaccines and Immunology
The late 19th and early 20th centuries saw the rapid development of vaccines and an improved understanding of immunity.
Edward Jenner (1749–1823) – The Smallpox Vaccine
- Jenner developed the first successful vaccine for smallpox in 1796 by using cowpox material.
- His work marked the beginning of immunization programs, a crucial aspect of nursing and public health.
Paul Ehrlich (1854–1915) – Chemotherapy and Immunology
- Ehrlich introduced the concept of selective toxicity and developed the first chemical treatment for syphilis (Salvarsan).
- His work laid the foundation for antibiotics and antimicrobial therapy.
The Antibiotic Revolution (20th Century)
The discovery of antibiotics changed the course of medicine and nursing by providing effective treatments for bacterial infections.
Alexander Fleming (1881–1955) – Discovery of Penicillin
- In 1928, Fleming accidentally discovered penicillin, the first natural antibiotic, which could kill bacteria.
- This breakthrough led to the development of antibiotics that transformed nursing care and reduced mortality rates from infectious diseases.
Selman Waksman (1888–1973) – Discovery of Streptomycin
- Waksman discovered streptomycin, an antibiotic effective against tuberculosis.
- His work contributed to the development of multiple antibiotics, saving millions of lives.
Modern Advances in Microbiology and Nursing
With advancements in microbiology, nursing practices have evolved to incorporate better infection control, disease prevention, and patient care.
Emergence of Antimicrobial Resistance (AMR)
- Overuse and misuse of antibiotics have led to antimicrobial resistance (AMR), making some infections difficult to treat.
- Nurses play a key role in antibiotic stewardship by ensuring proper medication administration and educating patients.
Molecular Microbiology and Rapid Diagnostics
- The development of PCR (Polymerase Chain Reaction) testing allows for rapid detection of infectious diseases.
- Techniques such as genome sequencing help identify new pathogens and track outbreaks.
COVID-19 and Emerging Infectious Diseases
- The COVID-19 pandemic highlighted the importance of microbiology in epidemiology, vaccine development, and infection control.
- Nurses played a critical role in COVID-19 prevention, vaccination, and patient management.
Relevance of Microbiology in Nursing
- Infection Control: Nurses use microbiology knowledge to prevent hospital-acquired infections (HAIs).
- Sterilization & Disinfection: Proper cleaning and disinfection of medical equipment prevent the spread of pathogens.
- Vaccination: Nurses administer vaccines and educate patients on immunization.
- Antibiotic Administration: Understanding microbiology helps nurses give antibiotics correctly and monitor for resistance.
- Public Health Nursing: Nurses promote hygiene, sanitation, and disease prevention in communities.
- Wound Care Management: Knowledge of microbiology aids in managing and preventing wound infections.
Concepts and Terminology in Microbiology.
Introduction
Microbiology is a vast field that encompasses the study of microorganisms, their characteristics, functions, and their effects on human health. Nurses need to understand key microbiological concepts and terminology to provide effective infection control, patient care, and disease prevention. This knowledge is essential in handling infections, administering antibiotics, maintaining hygiene, and ensuring patient safety.
Basic Concepts in Microbiology
1. Microorganisms
Microorganisms, or microbes, are microscopic organisms that exist everywhere, including the human body, soil, water, and air. They can be beneficial, harmless (commensal), or harmful (pathogenic).
Types of Microorganisms
- Bacteria – Single-celled prokaryotic organisms that can be beneficial or cause diseases such as tuberculosis, pneumonia, and urinary tract infections.
- Viruses – Small infectious agents that require a host cell to replicate, causing diseases like influenza, COVID-19, and hepatitis.
- Fungi – Includes yeasts and molds, some of which cause infections like candidiasis and ringworm.
- Protozoa – Single-celled eukaryotic organisms that cause diseases such as malaria and amoebiasis.
- Helminths – Parasitic worms such as tapeworms and roundworms that cause infections in the intestines and other body parts.
2. Normal Flora (Microbiota)
Normal flora refers to the beneficial microorganisms that naturally reside on the human body without causing disease.
- Resident Flora – Permanent microbes that protect against harmful bacteria.
- Transient Flora – Microbes acquired temporarily, often eliminated by handwashing and hygiene practices.
- Opportunistic Pathogens – Normal flora that can cause disease when the immune system is weakened (e.g., Candida infections in immunocompromised patients).
Relevance to Nursing: Nurses must understand the balance between beneficial and harmful microbes, ensuring that antibiotics do not destroy beneficial bacteria unnecessarily.
3. Pathogenicity and Virulence
- Pathogenicity – The ability of a microorganism to cause disease.
- Virulence – The degree of pathogenicity, meaning how severe or harmful the microorganism is.
- Virulence Factors – Traits that help microbes invade and damage the host, such as toxins and enzymes.
Relevance to Nursing: Nurses must recognize highly virulent infections, such as sepsis, and respond quickly with appropriate infection control measures.
4. Chain of Infection
The chain of infection consists of six links necessary for the spread of disease:
- Infectious Agent – The microorganism causing disease.
- Reservoir – The habitat where microbes live (e.g., humans, animals, soil, water).
- Portal of Exit – The route through which the microbe leaves the host (e.g., saliva, blood, feces).
- Mode of Transmission – The way the microorganism spreads (e.g., contact, airborne, droplet).
- Portal of Entry – How the pathogen enters a new host (e.g., open wounds, respiratory tract).
- Susceptible Host – A person at risk of infection due to a weakened immune system.
Relevance to Nursing: Breaking the chain of infection through hand hygiene, PPE, and isolation precautions is a critical nursing responsibility.
5. Modes of Transmission
Microorganisms spread in different ways, requiring different infection control measures.
- Direct Contact – Transmission through physical contact (e.g., touching, kissing).
- Indirect Contact – Transmission via contaminated objects or surfaces (e.g., medical instruments, door handles).
- Droplet Transmission – Large respiratory droplets spread through coughing or sneezing (e.g., influenza, COVID-19).
- Airborne Transmission – Small particles suspended in air over long distances (e.g., tuberculosis, measles).
- Vector-Borne Transmission – Carried by insects such as mosquitoes (e.g., malaria, dengue).
Relevance to Nursing: Nurses implement standard and transmission-based precautions to prevent the spread of infections in healthcare settings.
6. Sterilization and Disinfection
- Sterilization – The complete elimination of all microorganisms, including spores. Methods include:
- Autoclaving (Steam Sterilization) – Uses heat and pressure to kill microbes.
- Chemical Sterilization – Uses chemicals like ethylene oxide gas.
- Disinfection – Reduces microbial load but does not eliminate spores. Methods include:
- Alcohol-based disinfectants (for skin and surfaces).
- Chlorine-based disinfectants (for hospital floors and instruments).
Relevance to Nursing: Proper sterilization and disinfection prevent hospital-acquired infections (HAIs) and ensure patient safety.
7. Immunity and Vaccination
- Innate Immunity – The body’s first line of defense, including skin, mucous membranes, and white blood cells.
- Adaptive Immunity – The body’s learned immune response, including antibodies and memory cells.
- Active Immunity – Immunity developed from infection or vaccination.
- Passive Immunity – Temporary immunity acquired through antibodies (e.g., maternal antibodies in newborns, immunoglobulin injections).
Relevance to Nursing: Nurses administer vaccines and educate patients about immunization schedules, booster doses, and herd immunity.
8. Hospital-Acquired Infections (HAIs)
Also called nosocomial infections, these are infections acquired in healthcare settings, often caused by:
- Methicillin-Resistant Staphylococcus Aureus (MRSA)
- Clostridioides difficile (C. diff)
- Pseudomonas aeruginosa
- Multidrug-Resistant Tuberculosis (MDR-TB)
Relevance to Nursing: Strict hand hygiene, aseptic techniques, and proper use of personal protective equipment (PPE) help prevent HAIs.
9. Antimicrobial Resistance (AMR)
- Antibiotic Resistance – When bacteria mutate and no longer respond to antibiotics.
- Superbugs – Resistant strains such as MRSA, MDR-TB, and carbapenem-resistant Enterobacteriaceae (CRE).
- Causes of AMR – Overuse and misuse of antibiotics, poor infection control, and lack of new antibiotics.
Relevance to Nursing: Nurses must ensure proper antibiotic use, educate patients on completing antibiotic courses, and promote infection prevention measures.
10. Microbiological Diagnostic Tests
Nurses assist in specimen collection and interpretation of lab reports.
- Gram Staining – Differentiates bacteria into Gram-positive (purple) and Gram-negative (pink).
- Culture and Sensitivity Testing – Identifies bacteria and determines the best antibiotic treatment.
- Polymerase Chain Reaction (PCR) – Detects viral infections like COVID-19 and HIV.
- Serology Tests – Detects antibodies for diseases such as hepatitis and syphilis.
Relevance to Nursing: Nurses collect blood, urine, and sputum samples correctly and follow lab protocols to ensure accurate diagnosis.
Principles of Microbiology.
Introduction
Microbiology is the study of microorganisms, including bacteria, viruses, fungi, protozoa, and parasites. Understanding the fundamental principles of microbiology is essential for nurses to prevent and manage infections, promote hygiene, and ensure patient safety. These principles guide nursing practice in infection control, sterilization, disease transmission, immunity, and the responsible use of antibiotics.
1. Principle of Microbial Structure and Classification
Microorganisms vary in size, shape, and complexity. They are classified based on their structure, function, and effects on humans.
Types of Microorganisms:
- Bacteria – Single-celled prokaryotes that reproduce rapidly and can be pathogenic or beneficial. They are classified into:
- Gram-positive bacteria (e.g., Staphylococcus aureus, Streptococcus pneumoniae).
- Gram-negative bacteria (e.g., Escherichia coli, Pseudomonas aeruginosa).
- Aerobic and anaerobic bacteria (oxygen-dependent vs. oxygen-independent).
- Viruses – Tiny infectious agents that require a host cell to multiply (e.g., influenza, HIV, COVID-19).
- Fungi – Includes yeasts and molds, some of which cause opportunistic infections (e.g., Candida albicans, Aspergillus).
- Protozoa – Single-celled parasites that cause diseases like malaria and amoebiasis.
- Helminths – Parasitic worms, including tapeworms and roundworms, that cause infections in the intestines and other organs.
Relevance to Nursing:
- Understanding the structure and classification of microorganisms helps nurses identify infections and choose appropriate treatments.
- Knowledge of bacterial staining (Gram-positive vs. Gram-negative) guides antibiotic selection.
2. Principle of Microbial Growth and Reproduction
Microorganisms grow and multiply under favorable conditions, including warmth, moisture, nutrients, and proper pH levels.
Factors Affecting Microbial Growth:
- Temperature – Some bacteria thrive in body temperature (37°C), while others survive in extreme heat or cold.
- pH Level – Most human pathogens grow best in a neutral pH (around 7).
- Oxygen Requirement:
- Aerobes – Require oxygen (e.g., Mycobacterium tuberculosis).
- Anaerobes – Do not need oxygen (e.g., Clostridium tetani).
- Nutrient Availability – Microbes need carbohydrates, proteins, and other nutrients to grow.
- Moisture – Bacteria multiply faster in moist environments.
Relevance to Nursing:
- Nurses must maintain proper hygiene, moisture control, and temperature regulation in healthcare settings to prevent microbial growth.
- Proper food handling and storage prevent bacterial contamination and foodborne illnesses.
3. Principle of Microbial Pathogenicity and Virulence
Pathogenic microorganisms have specific features that help them invade and harm the host.
Virulence Factors:
- Toxins – Microbes release harmful substances that damage tissues (e.g., tetanus toxin, botulinum toxin).
- Enzymes – Some bacteria produce enzymes that destroy host cells (e.g., streptokinase).
- Capsules – A protective outer layer that helps bacteria evade immune defense (e.g., Streptococcus pneumoniae).
- Adhesion Factors – Microbes attach to host tissues using pili or fimbriae.
Relevance to Nursing:
- Nurses must recognize highly virulent pathogens and implement strict infection control measures.
- Understanding bacterial toxins helps in diagnosing and managing infections effectively.
4. Principle of Disease Transmission
Microorganisms spread through different transmission routes, leading to infections in individuals and communities.
Modes of Transmission:
- Direct Contact – Person-to-person transfer of microbes through touch, sexual contact, or open wounds.
- Indirect Contact – Contaminated objects (fomites) like medical instruments, doorknobs, and utensils spread infection.
- Droplet Transmission – Respiratory droplets from coughing, sneezing, or talking spread infections like flu and COVID-19.
- Airborne Transmission – Tiny particles remain suspended in air and infect individuals over long distances (e.g., tuberculosis, measles).
- Vector-Borne Transmission – Infections spread through insects like mosquitoes (Plasmodium causing malaria) and ticks (Borrelia causing Lyme disease).
- Fecal-Oral Transmission – Contaminated food and water spread diseases like cholera and typhoid.
Relevance to Nursing:
- Nurses break the chain of infection by using hand hygiene, PPE, and isolation precautions.
- Preventing cross-contamination and ensuring proper waste disposal reduce hospital-acquired infections (HAIs).
5. Principle of Infection Control and Sterilization
Infection control minimizes the spread of microorganisms in healthcare settings.
Methods of Infection Control:
- Hand Hygiene – The most effective way to prevent infections. Washing hands with soap or using alcohol-based sanitizers reduces microbial load.
- Personal Protective Equipment (PPE) – Masks, gloves, gowns, and face shields protect against infections.
- Aseptic Techniques – Practices such as using sterile instruments, disinfecting wounds, and wearing gloves prevent contamination.
Sterilization and Disinfection:
- Sterilization – Kills all microorganisms, including spores. Common methods include:
- Autoclaving (steam sterilization).
- Chemical sterilization (ethylene oxide gas).
- Disinfection – Reduces microbial load but does not eliminate spores.
- Alcohol, chlorine, and formaldehyde are common disinfectants.
Relevance to Nursing:
- Nurses ensure proper instrument sterilization and environmental cleanliness to prevent nosocomial infections.
- Adhering to hand hygiene and PPE guidelines reduces infection risks.
6. Principle of Immunity and Vaccination
The immune system protects the body from harmful microbes and infections.
Types of Immunity:
- Innate Immunity – The body’s first defense, including skin, mucous membranes, and white blood cells.
- Adaptive Immunity – The immune response that develops after infection or vaccination.
- Active Immunity – Developed after exposure to pathogens or vaccines.
- Passive Immunity – Temporary immunity acquired through antibodies from mother to baby or through immunoglobulin therapy.
Role of Vaccines:
- Vaccines stimulate the immune system to build resistance against diseases like hepatitis, measles, and polio.
- Types of Vaccines:
- Live Attenuated Vaccines (e.g., MMR vaccine).
- Inactivated Vaccines (e.g., Hepatitis A).
- mRNA Vaccines (e.g., COVID-19 vaccines).
Relevance to Nursing:
- Nurses play a critical role in administering vaccines and educating patients about immunization.
- Understanding immune responses helps in managing autoimmune disorders and immunocompromised patients.
7. Principle of Antibiotic Action and Resistance
Antibiotics are used to treat bacterial infections, but misuse can lead to resistance.
How Antibiotics Work:
- Bactericidal Antibiotics – Kill bacteria (e.g., penicillin, cephalosporins).
- Bacteriostatic Antibiotics – Inhibit bacterial growth (e.g., tetracyclines, macrolides).
Antibiotic Resistance (AMR):
- Overuse and misuse of antibiotics lead to drug-resistant infections, such as MRSA and MDR-TB.
- Causes of AMR include:
- Incomplete antibiotic courses.
- Overprescription of antibiotics.
- Poor infection control practices.
Relevance to Nursing:
- Nurses ensure proper antibiotic administration and educate patients on completing their prescribed courses.
- Monitoring for signs of antibiotic resistance helps in timely intervention.