BSC SEM 3 UNIT 1 ADULT HEALTH NURSING 1
UNIT 1 Introduction
Introduction to Medical-Surgical Nursing

Medical-Surgical Nursing is the foundation of professional nursing practice. It is a specialty area that focuses on the care of adult patients who are acutely ill or recovering from surgery. Nurses in this field provide comprehensive, evidence-based care across a wide variety of settings, including hospitals, clinics, and long-term care facilities.
This branch of nursing blends the knowledge of medicine and surgery to address physical, emotional, psychological, and social needs of patients. Medical-surgical nurses are skilled in assessing patients, identifying problems, planning and implementing interventions, and evaluating outcomes.
They manage a broad spectrum of conditions, such as:
- Respiratory and cardiovascular disorders
- Gastrointestinal and renal conditions
- Neurological and musculoskeletal problems
- Endocrine and immune system disorders
- Pre-operative and post-operative care
These nurses are also trained in critical thinking, clinical judgment, and patient education, and they often serve as key coordinators in multidisciplinary health care teams.
With advancements in healthcare, medical-surgical nursing is no longer limited to traditional hospital wards. It includes care provided in ambulatory surgical centers, home health settings, and rehabilitation centers.
Evolution of Medical and Surgical Nursing
Medical-Surgical Nursing, once considered a basic aspect of general nursing, has transformed into a dynamic and specialized branch of healthcare. Its development is deeply rooted in the evolution of medicine, surgery, and nursing practice across centuries. This evolution reflects changes in societal needs, healthcare systems, technological advancements, and educational reforms.
1. Prehistoric and Ancient Times
- In ancient times, diseases were often attributed to evil spirits or supernatural forces.
- Treatments were based on spiritual rituals, herbal remedies, and rudimentary surgical procedures like trepanation (drilling into the skull).
- Care was informal and typically provided by family members or tribal healers.
- There was no formal distinction between medical or surgical nursing roles.
Key Influence: Primitive knowledge; care was instinctive and largely spiritual.
2. Classical Era – Egyptian, Greek, and Roman Civilizations
- Egyptians used surgical tools like knives and forceps; they performed amputations and wound treatments.
- Greek medicine, led by Hippocrates, emphasized observation and rational thinking over supernatural beliefs.
- Romans developed military hospitals and emphasized sanitation (aqueducts, baths, drainage systems).
Nursing Care: Mostly provided by slaves, midwives, or menial workers; no formal education.
3. Middle Ages (5th to 15th Century)
- After the fall of the Roman Empire, scientific medical practices declined.
- The Church dominated health care; monasteries provided basic care to the sick and poor.
- Nuns and monks offered hospitality and spiritual care more than scientific treatment.
- Surgery was often performed by barber-surgeons without anesthesia or hygiene.
Significance: Nursing became associated with charity and religious duty; no defined medical-surgical specialty.
4. Renaissance (15th to 17th Century)
- Scientific curiosity revived; anatomy and physiology gained attention through dissection.
- Surgeons began to separate from barbers and form professional guilds.
- Medical schools were established in Europe, but nursing remained untrained and undervalued.
Limitation: Despite medical progress, nursing and surgical care remained crude and unstandardized.
5. 18th Century – Early Hospital Systems
- Hospitals became more common but were often overcrowded and unsanitary.
- Nursing was a low-status job, often performed by untrained women or criminals.
- Surgery advanced slowly with some progress in instruments and techniques, but high mortality due to infection.
Medical-Surgical Care: Still disorganized and informal, with high infection rates and poor outcomes.
6. 19th Century – Florence Nightingale’s Revolution
- Florence Nightingale, during the Crimean War (1853–1856), transformed nursing into a respectable, professional career.
- She introduced:
- Infection control, hygiene, and sanitation
- Use of observation, documentation, and evidence
- Nurse training programs (e.g., Nightingale School of Nursing in London)
- Hospital care improved drastically, and post-operative nursing care began to be emphasized.
Major Shift: Nursing became a scientific and disciplined profession, laying the foundation for medical-surgical specialization.
7. Early 20th Century – Formalization and Specialization
- Advancements in anesthesia, antisepsis (Joseph Lister), antibiotics (like penicillin) revolutionized surgery.
- Medical knowledge expanded, and diseases began to be understood in scientific terms.
- Nursing schools opened globally, often based on Nightingale’s principles.
- Medical-Surgical Nursing emerged as a formal branch taught in nursing curricula.
- Hospitals began to classify units (medical, surgical, orthopedic, etc.).
Role of Nurse: Evolved from caregiver to skilled practitioner involved in assessment, planning, and evaluation of patient care.
8. Mid-20th Century – Growth and Professional Identity
- Medical-Surgical Nursing expanded with the growth of modern hospitals and war-time innovations (World Wars I & II).
- Development of ICUs, operating theaters, blood transfusion, and sterile techniques.
- Nursing became legally recognized in many countries.
- Introduction of nursing theories, research, and licensing exams.
Medical-Surgical Nurse: Began to develop clinical judgment, specialization, and leadership roles.
9. Late 20th Century – Technological Integration and Evidence-Based Practice
- Rapid growth of technology in patient monitoring, imaging (CT, MRI), and minimally invasive surgery.
- Rise of evidence-based practice (EBP) in nursing—using scientific research to guide clinical decisions.
- Expansion into ambulatory surgery centers, home care, and rehabilitation.
- Nurse practitioners and clinical nurse specialists gained advanced roles in medical-surgical care.
Focus: Patient safety, quality of care, interdisciplinary teamwork, and continuing education.
10. 21st Century – Holistic, Patient-Centered, and High-Tech Care
- Integration of:
- Electronic Health Records (EHRs)
- Robotic and laparoscopic surgery
- Telehealth and remote monitoring
- Simulation-based nurse training
- Greater emphasis on holistic, culturally competent care.
- Nurses are involved in policy-making, leadership, education, and specialized roles in surgical units, ICUs, trauma centers, and post-operative rehabilitation.
- Pandemic situations (e.g., COVID-19) redefined roles with focus on infection control, triage, and crisis response.
Modern Role: Medical-surgical nurses are critical thinkers, educators, coordinators, and frontline caregivers who adapt to diverse and evolving healthcare environments.
Trends in Medical and Surgical Nursing

Medical-Surgical Nursing is continuously evolving in response to changes in healthcare delivery, patient needs, technological advancements, and global challenges. Understanding current trends helps nurses remain competent, proactive, and responsive to the dynamic healthcare environment.
1. Patient-Centered and Holistic Care
- Focus is shifting from disease-centered to patient-centered care.
- Emphasis on individualized care plans considering physical, emotional, spiritual, and social needs.
- Nurses assess quality of life, psychological well-being, and family involvement in care decisions.
📝 Example: Incorporating relaxation techniques and family education in post-operative pain management.
2. Evidence-Based Practice (EBP)
- Medical-surgical nursing now heavily relies on scientific evidence to guide interventions.
- Nurses are trained to review, apply, and evaluate research findings.
- EBP improves patient outcomes, reduces errors, and enhances decision-making.
📝 Example: Using updated protocols for catheter care to prevent urinary tract infections.
3. Technological Advancements
- Introduction of smart infusion pumps, electronic health records (EHRs), barcoding for medication safety, etc.
- Use of telehealth and remote monitoring tools in post-discharge follow-up.
- Robotic-assisted surgeries and minimally invasive techniques are common.
📝 Impact: Nurses must be tech-savvy and competent in operating and troubleshooting high-tech equipment.
4. Enhanced Roles and Responsibilities
- Medical-surgical nurses now act as:
- Care coordinators
- Patient educators
- Advocates
- Collaborators in multidisciplinary teams
- In some countries, nurses have expanded scopes such as prescribing medications and managing chronic diseases.
📝 Trend: Greater autonomy and accountability in clinical decision-making.
5. Increased Focus on Chronic Disease Management
- Rise in non-communicable diseases (NCDs) like diabetes, hypertension, cancer, and heart disease.
- Nurses manage long-term care, lifestyle modification education, and adherence to treatment plans.
📝 Role: Monitoring vitals, medication compliance, patient counseling, and dietary guidance.
6. Shorter Hospital Stays and More Outpatient Surgeries
- With improved surgical techniques and early mobilization, patients are discharged earlier.
- Greater emphasis on preoperative teaching, post-op care at home, and telephonic follow-up.
- Nurses must prepare patients and families for self-care at home.
📝 Challenge: Ensuring patients understand wound care, medication use, and signs of complications.
7. Interprofessional Collaboration
- Collaborative care involves nurses, doctors, physiotherapists, dieticians, social workers, etc.
- Communication, documentation, and coordination are essential in ensuring continuity and quality of care.
📝 Example: Discharge planning meetings to transition a surgical patient from hospital to home or rehab.
8. Emphasis on Quality, Safety, and Accreditation
- Nursing practice is increasingly guided by quality standards, such as:
- NABH (India), JCI, QSEN (USA).
- Nurses are involved in infection control, fall prevention, medication safety, and documentation accuracy.
📝 Tools: Use of checklists, clinical audits, and quality improvement (QI) projects.
9. Nursing Informatics
- Nurses are using software for:
- Charting
- Monitoring vitals
- Medication administration
- Data analysis for outcomes
- Informatics improves efficiency and helps in tracking patient progress and outcomes.
📝 Skill: Proficiency in hospital management systems and digital charting.
10. Lifelong Learning and Professional Development
- Nursing councils and institutions emphasize Continuing Nursing Education (CNE).
- Certifications in advanced cardiac life support (ACLS), critical care, and wound management are encouraged.
📝 Outcome: Nurses stay updated and competent in an ever-changing healthcare environment.
11. Culturally Competent and Ethical Care
- With growing diversity, nurses are expected to understand cultural beliefs and values related to illness, surgery, and recovery.
- Ethics in decision-making (like end-of-life care, informed consent) are emphasized.
📝 Practice: Respecting dietary restrictions, gender-sensitive care, or religious practices during hospitalization.
12. Mental Health Integration
- Psychological support is now an essential part of post-op recovery, especially after major surgeries like mastectomy or amputation.
- Nurses are trained to identify anxiety, depression, or post-traumatic stress and refer appropriately.
📝 Intervention: Providing therapeutic communication, emotional support, and referrals.
13. Disaster Preparedness and Infection Control
- After pandemics like COVID-19, nurses are more involved in:
- Triage
- Isolation protocols
- Personal protective equipment (PPE)
- Emergency response systems
- Hospitals provide drills and training for disaster situations.
📝 Preparedness: Ensures safety of both patients and healthcare workers.
14. Rise of Specialized Medical-Surgical Units
- Subspecialties have developed within medical-surgical nursing, including:
- Cardiothoracic
- Neuro-surgical
- Orthopedic
- Oncology
- Nurses receive focused training to meet the complex needs of patients in these areas.
📝 Benefit: Improved clinical expertise and patient outcomes.
15. Emphasis on Rehabilitation and Post-Surgical Recovery
- Recovery doesn’t end in the hospital. There’s a greater focus on:
- Pain management
- Mobility and exercise
- Prevention of complications like bedsores or DVT
- Return to daily life and work
📝 Role: Nurses coordinate with physiotherapists and occupational therapists for recovery goals.
International Classification of Diseases (ICD)

ICD = A standard tool for diagnosis coding and health statistics used worldwide
Introduction
The International Classification of Diseases (ICD) is a global standard developed by the World Health Organization (WHO) for reporting diseases, health conditions, and causes of death. It provides a universal language for classifying health problems and helps in comparing health data across countries and over time.
Purpose of ICD
- Clinical Use – Assists in diagnosis, treatment planning, and monitoring.
- Statistical Use – Collects morbidity (disease) and mortality (death) data.
- Epidemiology – Tracks disease trends and outbreaks.
- Health Insurance & Billing – Used for reimbursement and insurance claims.
- Public Health Policy – Helps design national and international health programs.
- Research – Provides standard data for healthcare research and analysis.
Users of ICD
- Hospitals and clinics
- Physicians and nurses
- Public health officials
- Health insurance companies
- Researchers
- Government and international health agencies
Structure of ICD
Each disease or health condition is assigned a unique alphanumeric code.
For example:
- J18.9 – Pneumonia, unspecified organism
- E11.9 – Type 2 diabetes mellitus without complications
The coding structure usually consists of:
- Letter + Number(s) (e.g., A00–Z99)
- Organized by body systems or disease categories
- Includes guidelines, inclusion/exclusion criteria, and instructions for accurate use
Main Chapters in ICD

There are 22 chapters in ICD-10 (also continued in ICD-11), including:
- Infectious and parasitic diseases
- Neoplasms (tumors)
- Blood and immune disorders
- Endocrine, nutritional, metabolic diseases
- Mental and behavioral disorders
- Nervous system diseases
- Circulatory system diseases
- Respiratory system diseases
- Digestive system diseases
- Skin diseases
- Musculoskeletal diseases
- Genitourinary diseases
- Pregnancy and childbirth
- Perinatal conditions
- Congenital malformations
- Symptoms and signs
- Injuries and poisonings
- External causes of illness/injury
- Factors influencing health status (e.g., social issues)
Versions of ICD
| Version | Year of Adoption | Key Features |
|---|---|---|
| ICD-1 | 1900 | First classification |
| ICD-6 | 1948 | Adopted by WHO |
| ICD-10 | 1990s | Widely used globally |
| ICD-11 | 2019 (effective from 2022) | Digital-friendly, includes new disorders like gaming addiction, improved classification of cancers and antimicrobial resistance |
ICD-10 vs. ICD-11: Key Differences
| Feature | ICD-10 | ICD-11 |
|---|---|---|
| Format | Alphanumeric (A00–Z99) | Extended codes with dot structure |
| Diseases | ~14,000 codes | Over 55,000 codes |
| Technology | Book-based | Designed for electronic use |
| Updates | Manual | Real-time updates possible |
| Examples | E10.9 (Diabetes type 1) | 5A11 (Diabetes mellitus) |
Importance in Nursing
- Helps in accurate documentation of diagnoses and care plans.
- Assists in monitoring patient outcomes.
- Supports evidence-based practice and audit.
- Ensures uniform communication across healthcare settings.
- Used in reporting notifiable diseases and maintaining public health records.
Roles and Responsibilities of a Nurse in Medical and Surgical Nursing

Medical-surgical nurses play a critical role in the assessment, planning, implementation, and evaluation of patient care. They are responsible for managing patients with acute and chronic illnesses, as well as those undergoing preoperative and postoperative care.
I. Roles of a Medical-Surgical Nurse
1. Caregiver
- Provides holistic care to patients including physical, emotional, psychological, and spiritual support.
- Assists in activities of daily living (ADLs) such as bathing, feeding, ambulation, and hygiene.
2. Observer and Assessor
- Continuously monitors patient conditions, including vital signs, consciousness level, fluid balance, wound healing, etc.
- Identifies early signs of complications or deterioration (e.g., post-operative bleeding, infection).
3. Planner and Implementer
- Develops individualized care plans based on diagnosis, surgery type, and patient needs.
- Administers medications, treatments, and nursing interventions according to physician’s orders and nursing judgment.
4. Educator
- Teaches patients and families about:
- Disease process
- Medication regimen
- Post-operative care
- Lifestyle modifications
- Discharge instructions and home care
5. Advocate
- Protects patient rights and interests.
- Ensures informed consent before procedures.
- Speaks up for patient safety and ethical care.
6. Communicator
- Maintains effective communication with:
- Patients and families
- Physicians
- Other healthcare team members
- Documents all nursing care accurately in records.
7. Coordinator
- Coordinates care with the multidisciplinary team (doctors, physiotherapists, dieticians, lab technicians).
- Ensures timely investigations, referrals, and follow-ups.
8. Leader and Manager
- Delegates duties to junior staff and aides.
- Ensures proper use of supplies, cleanliness, infection control, and unit organization.
- Manages emergency situations confidently (e.g., CPR, shock, hemorrhage).
9. Researcher
- Participates in clinical audits, evidence-based practice, and nursing research.
- Collects and reports data that may improve patient care outcomes.
II. Responsibilities of a Nurse in Medical and Surgical Units
A. Pre-Operative Responsibilities
- Prepare the patient physically (shaving, bowel prep, NPO status).
- Provide emotional support to reduce anxiety.
- Obtain and verify informed consent.
- Ensure pre-op checklist completion (labs, vitals, allergy check).
- Teach deep breathing, coughing, leg exercises.
B. Intra-Operative Responsibilities (in OT settings)
- Maintain sterile environment.
- Assist surgeon or anesthetist if scrub or circulating nurse.
- Monitor patient safety and equipment.
C. Post-Operative Responsibilities
- Transfer and receive patient from OT with handover.
- Monitor for post-op complications (e.g., bleeding, infection, respiratory distress).
- Manage pain, IV fluids, catheters, drains.
- Encourage early mobilization, breathing exercises.
- Assess wound site, change dressings aseptically.
D. Daily Responsibilities in Medical-Surgical Ward
- Perform morning and evening care.
- Give oral, IV, topical, or parenteral medications.
- Carry out doctor’s orders.
- Maintain intake/output charts.
- Prepare patients for procedures (e.g., X-ray, biopsy).
- Maintain accurate documentation.
E. Discharge Responsibilities
- Educate the patient/family on:
- Medication and follow-up
- Diet and wound care
- Warning signs to report
- Ensure discharge papers are complete.
Qualities Required for Medical-Surgical Nurses
- Alertness and clinical judgment
- Compassion and patience
- Manual dexterity for procedures
- Team spirit and leadership
- Ability to handle emergencies
- Good communication and documentation skills
Roles and Responsibilities of a Nurse in OPD (Outpatient Department)

The Outpatient Department (OPD) is a critical area in any healthcare facility where patients receive diagnosis, treatment, minor procedures, and follow-up care without hospital admission. Nurses working in Medical and Surgical OPD act as the first point of contact and play a vital role in clinical coordination, patient education, procedural assistance, and administrative tasks.
I. Key Roles of a Nurse in Medical-Surgical OPD
1. Care Provider
- Provides basic nursing care such as checking vitals, administering medications, dressing wounds, and assisting in minor procedures.
- Offers first-aid care for walk-in patients with injuries or acute problems.
2. Patient Assessor
- Gathers detailed patient history and complaints.
- Conducts initial assessment: temperature, pulse, BP, oxygen saturation, weight, etc.
- Screens patients for urgency and refers emergency cases immediately.
3. Assisting the Physician/Specialist
- Prepares examination rooms and assists doctors during physical examinations, procedures, and minor surgeries.
- Prepares sterile trays, instruments, and ensures aseptic techniques.
- Observes patients during procedures and reports any unusual symptoms or reactions.
4. Health Educator
- Educates patients and families about:
- Disease condition
- Lifestyle changes
- Medication usage
- Wound care, hygiene, and follow-up visits
- Provides pre-operative and post-operative teaching to surgical OPD patients.
5. Triage and Prioritization
- Identifies critically ill patients and ensures immediate attention.
- Categorizes patients based on severity of illness or injury.
6. Counselor and Support Provider
- Provides emotional support to anxious or fearful patients.
- Guides patients through hospital processes and helps them understand procedures and next steps.
7. Communicator
- Acts as a liaison between patient, doctor, laboratory, and pharmacy.
- Coordinates follow-up appointments and referrals to inpatient or specialty departments.
8. Documentation and Record-Keeping
- Maintains accurate records of:
- Patient history
- Observations and vitals
- Procedure notes
- Medication administration
- Follow-up instructions
9. Inventory and Supply Manager
- Ensures availability of dressing materials, instruments, sterile gloves, syringes, and emergency medications.
- Reports shortages or maintenance needs of equipment.
10. Infection Control and Safety
- Follows infection prevention protocols.
- Disinfects surfaces, equipment, and ensures proper waste disposal.
- Educates patients about hand hygiene and respiratory hygiene.
Specific Duties in Medical OPD
- Monitor chronic condition patients (e.g., diabetes, hypertension).
- Assist with ECG, nebulization, injections.
- Guide patients for diagnostic tests (blood tests, imaging).
- Educate on medication compliance and disease prevention.
Specific Duties in Surgical OPD
- Assist in wound dressing, suture removal, minor surgical procedures.
- Provide pre-op and post-op counseling.
- Prepare patients for surgical admission, if required.
- Observe wound healing and detect signs of infection.
Professional Skills Required
- Clinical knowledge and manual skills
- Communication and interpersonal skills
- Quick decision-making and triage ability
- Attention to detail and documentation accuracy
- Compassion and patient-friendly attitude
Roles and Responsibilities of a Nurse in Inpatient Unit
The Inpatient Unit is the area of the hospital where patients are admitted for close monitoring, treatment, surgery, and recovery. Nurses working in medical-surgical inpatient wards provide round-the-clock, comprehensive, and individualized care. They are the primary caregivers who bridge the gap between doctors, patients, and families, ensuring smooth recovery and patient safety.
I. Key Roles of a Nurse in Medical-Surgical Inpatient Unit
1. Caregiver
- Provides 24/7 care to admitted patients.
- Helps with activities of daily living (ADLs) – bathing, feeding, toileting, mobility.
- Supports post-operative care, wound management, and vital sign monitoring.
2. Patient Assessor
- Conducts thorough initial assessment upon admission.
- Monitors changes in condition: vital signs, pain level, neurological status, fluid balance, etc.
- Detects early signs of complications such as infections, bleeding, respiratory distress.
3. Medication Administrator
- Administers medications safely via oral, IV, IM, SC, topical routes.
- Maintains medication records and watches for side effects or adverse reactions.
- Follows “Five Rights” of medication administration.
4. Wound and Procedure Care
- Performs and assists with:
- Wound dressing
- Catheter care
- Tracheostomy or colostomy care
- Tube feeding or suctioning
- Ensures aseptic technique is followed during all procedures.
5. Patient Educator
- Provides bedside education about the disease, medications, dietary needs, and post-discharge care.
- Trains patients and caregivers for home care techniques like insulin administration or wound dressing.
6. Coordinator of Care
- Coordinates with doctors, lab technicians, physiotherapists, dieticians, and other healthcare professionals.
- Prepares patients for diagnostic tests, surgeries, or procedures.
- Ensures timely follow-up, referrals, and continuity of care.
7. Documentation and Reporting
- Maintains:
- Nursing care plan
- Intake-output chart
- Daily progress notes
- Incident reports (if any)
- Gives accurate and clear handover during shift changes.
8. Emotional Support and Advocacy
- Provides emotional and psychological support to patients and families.
- Advocates for patient’s rights, preferences, and dignity.
- Informs the doctor of any patient concerns or needs.
9. Infection Control Officer
- Implements hospital infection control protocols.
- Practices hand hygiene, waste disposal, linen management, and use of PPE.
- Educates patients and visitors on hygiene and isolation precautions.
10. Emergency Response
- Responds quickly to:
- Cardiac arrest (performs CPR)
- Bleeding, seizures, or sudden deterioration
- Uses emergency trolleys and assists during code blue situations.
Medical Ward-Specific Duties
- Manage long-term and acute illness patients (e.g., diabetes, pneumonia, renal failure).
- Monitor chronic condition stability, manage multiple medications.
- Administer IV fluids, insulin, nebulization, and oxygen therapy.
Surgical Ward-Specific Duties
- Pre-operative responsibilities: Preparing the patient physically and emotionally, checking consent forms, fasting status, and pre-op checklist.
- Post-operative responsibilities:
- Monitor for shock, infection, hemorrhage, DVT
- Pain management, wound care, drain care
- Encourage deep breathing exercises and mobilization
Professional Qualities Required
- Observation and critical thinking skills
- Emergency response readiness
- Compassion and patience
- Effective communication
- Teamwork and leadership
- Accurate documentation and time management
Roles and Responsibilities of a Nurse in the Intensive Care Unit (ICU)

The Intensive Care Unit (ICU) is a specialized hospital department where critically ill patients receive close monitoring, life support, and advanced medical care. Nurses in the ICU play a highly specialized and demanding role, requiring advanced skills, rapid decision-making, and emotional resilience. ICU nurses provide round-the-clock care to patients who are unstable, unconscious, or dependent on ventilators and monitoring systems.
I. Key Roles of an ICU Nurse
1. Critical Caregiver
- Delivers continuous and comprehensive care to critically ill patients.
- Manages life-threatening conditions like respiratory failure, cardiac arrest, sepsis, multi-organ dysfunction, or trauma.
2. Vigilant Monitor
- Continuously monitors:
- Vital signs (heart rate, BP, temperature, oxygen saturation)
- Cardiac rhythms (ECG)
- Ventilator parameters
- Neurological status (GCS)
- Fluid balance and output (urine, drains, CVP)
- Recognizes early warning signs of deterioration and responds immediately.
3. Advanced Equipment Handler
- Operates and troubleshoots:
- Ventilators
- Infusion pumps
- Cardiac monitors
- Syringe pumps, defibrillators
- Arterial lines, central venous catheters
- Ensures accurate settings and alarms are appropriately managed.
4. Medication Expert
- Administers high-risk drugs, such as:
- Inotropes, vasopressors
- Sedatives and analgesics
- IV antibiotics and fluids
- Calculates accurate dosages based on weight or renal function.
- Watches for side effects, drug interactions, and allergic reactions.
5. Emergency Responder
- Participates in code blue situations (cardiac arrest).
- Performs CPR, defibrillation, and assists during intubation or central line insertion.
- Acts immediately during shock, seizures, arrhythmias, or airway compromise.
6. Infection Control Enforcer
- Maintains strict aseptic technique and follows ICU infection control protocols.
- Prevents hospital-acquired infections like VAP (ventilator-associated pneumonia), CLABSI, and CAUTI.
- Ensures use of PPE, sterile suctioning, catheter care, and proper hand hygiene.
7. Communicator and Coordinator
- Communicates patient status clearly with the ICU team, including intensivists, surgeons, respiratory therapists, and pharmacists.
- Coordinates with labs, radiology, and other departments for tests and reports.
- Updates patient’s family with compassion and clarity.
8. Documentation and Charting
- Maintains:
- Hourly flow charts
- Nursing assessments
- Medication administration records
- Lab results and vitals logs
- ICU scoring tools (APACHE II, SOFA, GCS)
9. Patient and Family Educator
- Guides families about prognosis, ICU protocols, and visitation policies.
- Provides emotional support and answers queries compassionately.
- Prepares patients and caregivers for step-down care or discharge if condition stabilizes.
Specific ICU Responsibilities
Neurological ICU (Neuro ICU)
- Monitor intracranial pressure (ICP), level of consciousness, seizure activity.
- Perform neurological assessments regularly.
Cardiac ICU (CCU)
- Monitor ECG, manage arrhythmias, chest pain, and post-cardiac surgery care.
- Administer thrombolytics, antiarrhythmics, and manage pacemakers or defibrillators.
Medical ICU
- Care for patients with sepsis, ARDS, renal failure, liver disease, or poisoning.
- Manage dialysis, intubation, and sedation protocols.
Surgical ICU
- Monitor post-op patients from major surgeries (e.g., neurosurgery, thoracic surgery).
- Watch for bleeding, wound healing, and organ function restoration.
Qualities and Skills Required in ICU Nurses
- Critical thinking and rapid decision-making
- Technical proficiency with ICU equipment
- Emotional strength and stress tolerance
- Teamwork and communication
- High level of precision, focus, and clinical knowledge
- Empathy and professionalism in high-stress scenarios
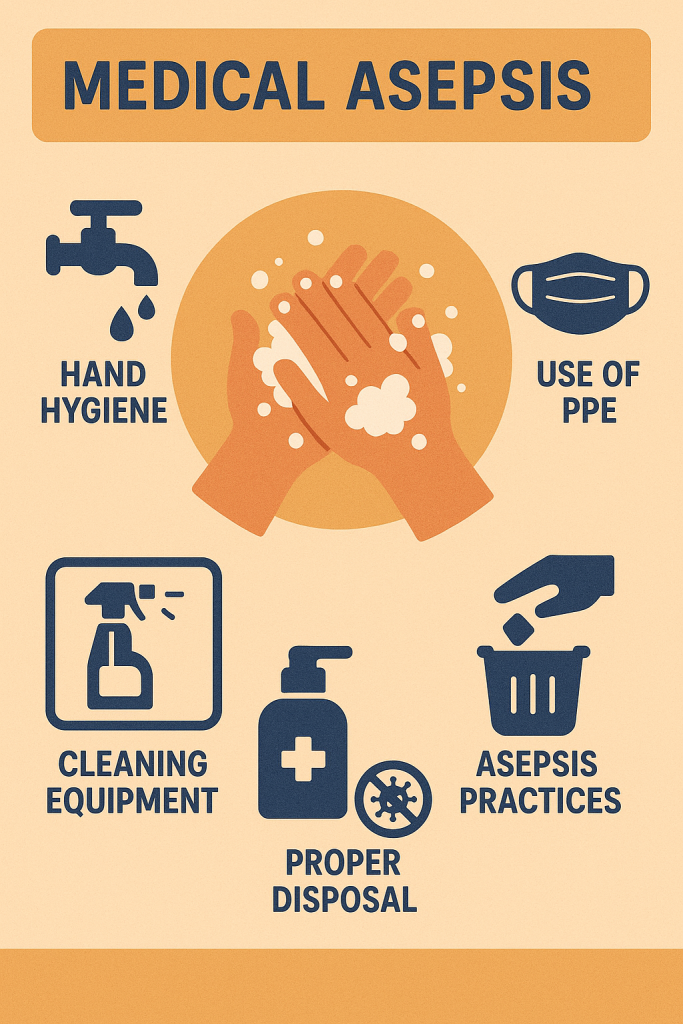
Introduction to Medical Asepsis
Definition
Medical Asepsis, also known as clean technique, refers to practices and procedures used to reduce and control the spread of microorganisms. It is a fundamental concept in healthcare that helps prevent infection transmission among patients, healthcare providers, and the hospital environment.
Objective of Medical Asepsis
- To limit the number and growth of microorganisms.
- To prevent cross-contamination between patients and healthcare workers.
- To reduce the risk of healthcare-associated infections (HAIs).
- To maintain a safe and clean environment in hospitals, clinics, and homes.
Principle Behind Medical Asepsis
Microorganisms like bacteria, viruses, fungi, and protozoa can spread through:
- Direct contact (e.g., touching infected wounds)
- Indirect contact (e.g., contaminated surfaces, instruments)
- Airborne or droplet transmission
- Body fluids (blood, urine, sputum)
Medical asepsis interrupts this chain of infection through strict hygienic practices and environmental cleanliness.
Key Practices of Medical Asepsis
1. Hand Hygiene
- The most effective way to prevent infection.
- Handwashing with soap and water or using alcohol-based hand sanitizers before and after:
- Patient contact
- Handling food, wounds, or body fluids
- Removing gloves
2. Use of Personal Protective Equipment (PPE)
- Wearing gloves, masks, gowns, face shields to protect against infection.
- Proper donning and doffing techniques must be followed.
3. Environmental Cleaning
- Regular disinfection of surfaces, floors, and frequently touched areas.
- Sterilization or decontamination of reusable medical equipment.
4. Waste Disposal
- Proper segregation of biomedical waste:
- Sharps in puncture-proof containers
- Infectious waste in yellow/red bags
- General waste in black bags
- Follow institutional and governmental guidelines for disposal.
5. Barrier Nursing
- Use of isolation techniques to prevent spread from infectious patients.
- Assigning separate equipment to infected individuals when possible.
6. Respiratory Hygiene/Cough Etiquette
- Use of tissues, masks, and elbow covering when coughing or sneezing.
- Patient and staff education is important.
7. Clean Technique in Procedures
- Use sterile/clean equipment for:
- Catheter insertion
- Dressing changes
- Injections
- IV infusions
- Maintain clean working areas and avoid contaminating sterile items.
8. Linen Handling
- Soiled linen must be handled with gloves.
- Avoid shaking to prevent aerosolization.
- Wash at recommended temperatures and with disinfectants.
Difference Between Medical and Surgical Asepsis
| Feature | Medical Asepsis | Surgical Asepsis |
|---|---|---|
| Goal | Reduce number of microbes | Eliminate all microbes |
| Known as | Clean technique | Sterile technique |
| Use | General care, dressing, oral meds | Surgery, invasive procedures |
| Tools | Clean but not sterile | All tools sterile |
| PPE | As needed | Strict and complete PPE |
Application Areas in Medical-Surgical Nursing
- Bedmaking and patient hygiene
- Wound care and dressing
- IV cannulation and injections
- Catheter care
- Feeding and suctioning
- Linen changing
- Specimen collection (urine, sputum)
Role of the Nurse in Maintaining Medical Asepsis
- Follow hospital infection control protocols.
- Educate patients and visitors on hygiene practices.
- Supervise housekeeping and waste handling.
- Report breaches in aseptic practices.
- Ensure availability and proper use of disinfectants and PPE.
- Maintain personal cleanliness and proper uniform standards.
Consequences of Poor Medical Asepsis
- Hospital-acquired infections (HAIs)
- Increased morbidity and mortality
- Prolonged hospital stay
- Increased healthcare costs
- Antibiotic resistance
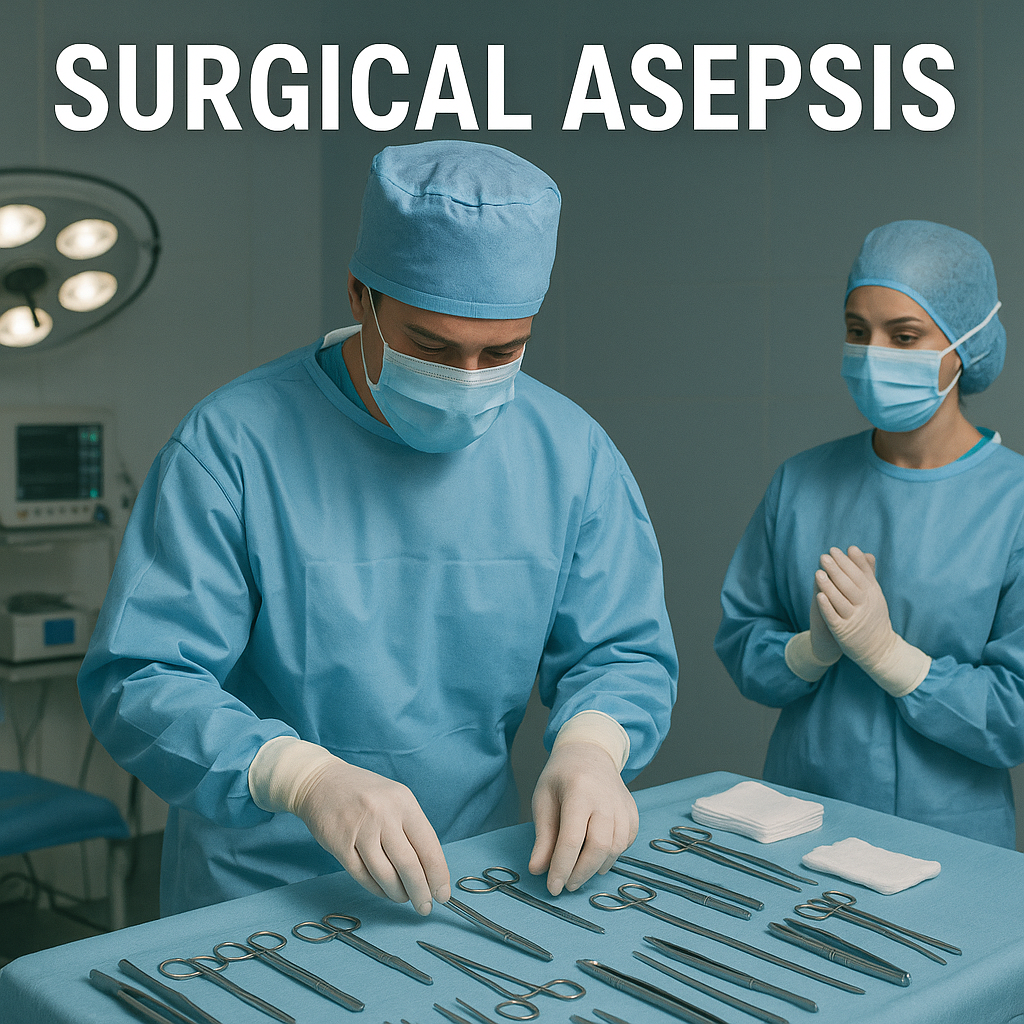
Introduction to Surgical Asepsis
Definition
Surgical Asepsis, also known as sterile technique, refers to the practices and procedures used to eliminate all microorganisms—including pathogens and spores—from an area or object. This technique is crucial in surgical procedures, invasive treatments, and when the integrity of the skin or mucous membranes is compromised. It ensures that sterile conditions are maintained to prevent infections during operations and other critical procedures.
Objective of Surgical Asepsis
- To prevent infections in surgical patients.
- To create a sterile environment for surgeries and invasive procedures.
- To maintain sterile fields to ensure the safety and health of the patient.
- To eliminate all microorganisms that could potentially harm the patient or contaminate surgical sites.
Principle Behind Surgical Asepsis
Surgical asepsis is based on the principle that even microscopic amounts of bacteria, viruses, or spores can lead to infections if they are introduced into sterile areas, such as surgical incisions, wounds, or body cavities. The objective is to create and maintain a sterile field, ensuring that nothing unsterile comes in contact with the sterile area during procedures.
Key Practices of Surgical Asepsis
1. Sterile Field Preparation
- A sterile field refers to a specific area that has been prepared with sterile drapes and equipment.
- Sterile drapes are used to cover areas around the surgical site to maintain a sterile environment.
- Sterile instruments are used within this field, and only sterile objects should touch sterile surfaces.
2. Sterile Gloves
- Sterile gloves must be worn when handling sterile instruments or during any procedure that requires the maintenance of a sterile field.
- Gloves should not be touched with bare hands, and care should be taken not to contaminate them.
3. Sterilization of Equipment
- All equipment and instruments used during surgeries or invasive procedures must be sterilized. This is done through:
- Autoclaving (steam sterilization)
- Chemical sterilization
- Dry heat sterilization
- Radiation sterilization (for sensitive instruments)
- Sterilized items must remain sealed until used in the procedure to maintain sterility.
4. Aseptic Technique during Procedures
- Aseptic technique involves using sterile instruments and maintaining sterile conditions during procedures.
- During surgeries or invasive procedures, anything that comes into contact with the surgical site, such as gauze, drapes, or instruments, must be sterile.
- Hand hygiene is critical; surgical hand scrubbing and wearing sterile gloves are mandatory.
5. Maintaining a Sterile Environment
- Airborne microorganisms are minimized by controlling the operating room environment:
- High-efficiency particulate air (HEPA) filters to purify the air.
- Positive pressure airflow to push out air from the room and prevent contaminants from entering.
- Operating rooms must be cleaned thoroughly and sanitized before and after each procedure.
6. Handling Contaminated Items
- Items that have been used on non-sterile surfaces or that come into contact with body fluids must be handled with caution.
- They should be disposed of properly or cleaned and sterilized before reuse.
7. Patient Preparation
- Preoperative skin preparation: The surgical site must be cleaned and disinfected to remove any potential contaminants.
- Hair removal (if necessary): This should be done carefully with sterile instruments or clippers to avoid nicks or cuts that could introduce bacteria.
- Draping: Surgical drapes are placed over the patient to create a sterile field around the surgical site.
Role of the Nurse in Maintaining Surgical Asepsis
1. Sterile Field Management
- The nurse sets up and maintains a sterile field, ensuring that all instruments, supplies, and equipment are sterile before use.
- During the procedure, the nurse ensures that no sterile instruments or supplies are contaminated.
2. Scrub Nurse
- The scrub nurse is responsible for:
- Assisting with the sterile setup, ensuring that all instruments and materials are sterile.
- Passing sterile instruments to the surgeon during surgery.
- Keeping the sterile field intact and managing any sterile items used.
3. Assisting with Aseptic Technique
- The nurse assists the surgeon and surgical team by:
- Ensuring that all sterile procedures are followed.
- Constantly monitoring the sterile field to avoid contamination.
- Following aseptic techniques during the insertion of catheters, drains, or other invasive equipment.
4. Patient Safety
- The nurse ensures that all procedures are performed according to sterile protocols to prevent postoperative infections.
- The nurse also plays a role in patient education by explaining the importance of sterile technique and post-operative wound care.
5. Disposal and Decontamination
- After the procedure, the nurse assists with the disposal of used materials (sutures, instruments) and ensures that they are disposed of properly.
- The nurse ensures that contaminated items are decontaminated and sterilized as required.
Differences Between Surgical Asepsis and Medical Asepsis
| Aspect | Surgical Asepsis (Sterile Technique) | Medical Asepsis (Clean Technique) |
|---|---|---|
| Goal | Eliminate all microorganisms | Reduce the number of microorganisms |
| Scope | Used for invasive procedures, surgeries | Used for general patient care |
| Equipment | All equipment must be sterile | Equipment can be clean but not sterile |
| Environment | Sterile field must be maintained | Clean, but not sterile environment |
| Examples of Use | Surgeries, catheter insertion, wound care | Routine nursing care, dressing changes, administration of medications |
Application Areas in Surgical Nursing
- Surgical procedures: Ensuring all aspects of the surgery, including instrument handling and surgical site care, are done with sterile techniques.
- Invasive procedures: Insertion of catheters, drains, and IV lines.
- Wound care: Proper dressing and management of surgical wounds.
- Handling of sterile equipment: Ensuring all tools and devices are sterilized before use and handling them appropriately.
Conclusion
Surgical Asepsis (Sterile Technique) is a critical aspect of preventing surgical site infections and maintaining patient safety during surgery or invasive procedures. Adherence to sterile practices ensures that the risk of infection is minimized, ultimately leading to faster recovery and better outcomes for patients. Nurses and healthcare professionals must be well-trained in these techniques to ensure high standards of care and minimize the risk of complications.
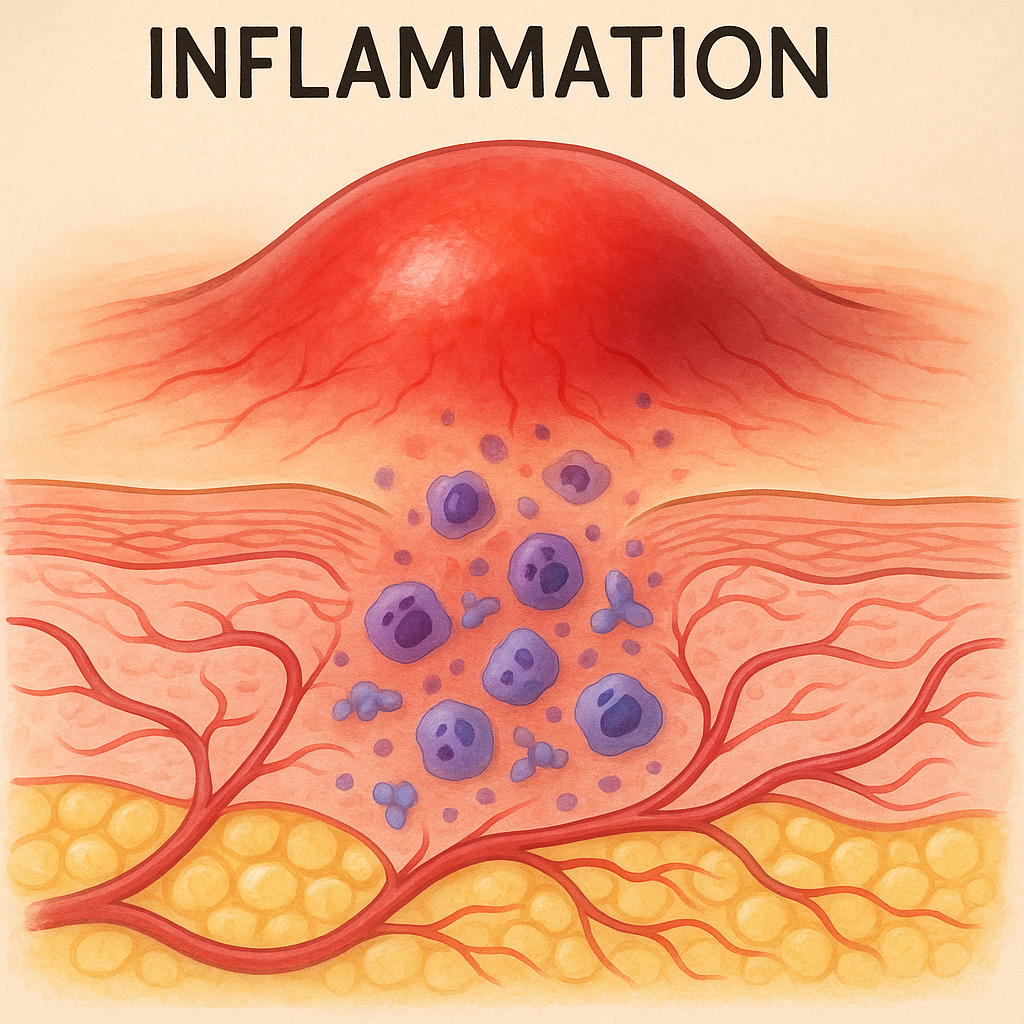
Inflammation
Introduction
Inflammation is a protective response of the body’s immune system to injury, infection, or irritation. It is a natural and essential process that helps the body eliminate harmful stimuli (like pathogens or damaged cells), begin the healing process, and restore tissue function.
Though inflammation is vital for survival, excessive or chronic inflammation can lead to tissue damage and various diseases like arthritis, asthma, or autoimmune conditions.
Definition
Inflammation is defined as:
“A local physiological response of vascularized tissues to injury or infection, characterized by redness, heat, swelling, pain, and loss of function.”
It involves a complex process including:
- Vascular changes (increased blood flow)
- Cellular responses (migration of white blood cells)
- Release of chemical mediators (e.g., histamine, cytokines, prostaglandins)
Cardinal Signs of Inflammation (described by Celsus and Galen):
- Rubor (Redness)
- Calor (Heat)
- Tumor (Swelling)
- Dolor (Pain)
- Functio laesa (Loss of function) – added later by Virchow
Types of Inflammation
Inflammation can be classified based on duration, cause, or type of cells involved.
1. Based on Duration
a) Acute Inflammation
- Sudden onset, short duration (minutes to days)
- Characterized by fluid exudation, vascular changes, and migration of neutrophils
- Protective and often resolves with healing
Examples:
- Sore throat from viral infection
- Skin wound
- Appendicitis
b) Chronic Inflammation
- Slow onset, long duration (weeks to years)
- Involves lymphocytes, macrophages, and tissue destruction
- Often associated with autoimmune diseases, persistent infections, or prolonged exposure to irritants
Examples:
- Rheumatoid arthritis
- Tuberculosis
- Asthma
- Ulcerative colitis
2. Based on Type of Exudate or Inflammatory Response
a) Serous Inflammation
- Watery, clear fluid (serum-like)
- Seen in mild injuries
Example: Blisters from burns
b) Fibrinous Inflammation
- Rich in fibrinogen, forming thick, sticky exudate
- Common in body cavities (pleura, pericardium)
Example: Rheumatic pericarditis
c) Purulent (Suppurative) Inflammation
- Formation of pus due to infection by pyogenic bacteria
- Contains dead neutrophils, tissue debris, and bacteria
Example: Abscess, boils, pus in wounds
d) Hemorrhagic Inflammation
- Presence of red blood cells in the exudate
- Severe damage to blood vessels
Example: Hemorrhagic dengue fever
e) Catarrhal Inflammation
- Occurs in mucous membranes
- Excess mucus production
Example: Common cold, allergy
1Signs and Symptoms of Inflammation (General)
The five classic signs and symptoms of inflammation (applicable to most types) are:
| Latin Term | Meaning | Cause |
|---|---|---|
| Rubor | Redness | Vasodilation (↑ blood flow) |
| Calor | Heat | Increased blood supply |
| Tumor | Swelling | Fluid leakage (exudate) |
| Dolor | Pain | Pressure on nerves, chemicals |
| Functio laesa | Loss of function | Due to pain/swelling |
Signs and Symptoms According to Types of Inflammation
A. Acute Inflammation
- Sudden onset
- Short duration (days)
- Main symptoms:
- Redness and warmth
- Swelling
- Throbbing pain
- Fever
- Loss of function (temporary)
- Possible discharge (serous or purulent)
Examples:
- Cellulitis: swollen, red, painful skin
- Acute appendicitis: abdominal pain, fever, vomiting
B. Chronic Inflammation
- Slow, persistent, or recurring
- Symptoms may be subtle or less intense but long-lasting
Main symptoms:
- Dull, continuous pain
- Fatigue and malaise
- Low-grade fever
- Weight loss (in some chronic diseases)
- Swelling or stiffness (e.g., in joints)
- Organ dysfunction (if internal organs involved)
Examples:
- Rheumatoid arthritis: joint stiffness and swelling
- Tuberculosis: chronic cough, fever, weight loss
C. Serous Inflammation
- Mild inflammation
- Symptoms:
- Clear fluid accumulation (e.g., blister)
- Local redness
- Mild pain and itching
Example: Burn blisters
D. Fibrinous Inflammation
- Thick, fibrin-rich exudate
- Symptoms:
- Severe pain
- Friction rub (if on heart/lungs)
- May lead to fibrous scarring
Example: Rheumatic pericarditis
E. Purulent (Suppurative) Inflammation
- Characterized by pus formation
- Symptoms:
- Swelling with pus
- Intense localized pain
- Redness and warmth
- Fever and chills
- Abscess or wound discharge
Example: Boils, abscesses
F. Hemorrhagic Inflammation
- Involves bleeding in the inflamed area
- Symptoms:
- Bloody discharge
- Severe tissue damage
- Risk of shock (in severe cases)
Example: Hemorrhagic cystitis, severe viral infections
G. Catarrhal Inflammation
- Occurs in mucous membranes
- Symptoms:
- Excessive mucus
- Nasal congestion or cough
- Sneezing or sore throat
Example: Common cold, allergic rhinitis
Diagnosis of Inflammation
Inflammation is diagnosed through clinical examination, laboratory tests, and imaging studies, depending on location and severity.
A. Clinical Assessment
- Observation of redness, swelling, and warmth
- Palpation for tenderness and pain
- Functional assessment (mobility, organ function)
B. Laboratory Tests
| Test Name | Purpose |
|---|---|
| Complete Blood Count (CBC) | ↑ WBC count (especially neutrophils in acute, lymphocytes in chronic) |
| Erythrocyte Sedimentation Rate (ESR) | ↑ in chronic/systemic inflammation |
| C-Reactive Protein (CRP) | ↑ in acute inflammation |
| Procalcitonin | Marker for bacterial infection/inflammation |
| Rheumatoid Factor / ANA | For autoimmune inflammation |
| Culture and Sensitivity | Identify infective organism (if pus/discharge present) |
C. Imaging Studies
- X-ray: Bone or joint inflammation (arthritis)
- Ultrasound: Fluid collection or abscess
- CT scan/MRI: Organ inflammation (e.g., appendicitis, brain)
- Endoscopy: Gastrointestinal mucosal inflammation
D. Biopsy (if required)
- For confirming chronic or granulomatous inflammation (e.g., tuberculosis, cancer suspicion)
Summary Table: Types, Signs, and Diagnosis
| Type of Inflammation | Key Signs/Symptoms | Common Tests |
|---|---|---|
| Acute | Redness, swelling, heat, pain | CBC, CRP |
| Chronic | Dull pain, stiffness, fatigue | ESR, RF, ANA |
| Serous | Clear fluid, blisters | Clinical exam |
| Fibrinous | Thick exudate, organ friction rub | Imaging, pericardial fluid |
| Purulent | Pus, abscess, fever | WBC count, culture |
| Hemorrhagic | Bleeding, shock | CBC, imaging |
| Catarrhal | Mucous discharge, congestion | Physical exam |
Stages of Inflammation
Inflammation is a complex, protective process that occurs in response to injury, infection, or harmful stimuli. It unfolds in three primary stages, each with specific physiological events aimed at eliminating the cause of injury, containing damage, and initiating tissue repair.
Overview of the 3 Main Stages of Inflammation
| Stage | Main Events |
|---|---|
| 1. Vascular (Vasodilation) Phase | Blood flow changes, increased permeability |
| 2. Cellular (Phagocytic) Phase | Migration of WBCs, engulfing pathogens and debris |
| 3. Tissue Repair (Healing) Phase | Regeneration or repair of damaged tissue |
Stage 1: Vascular Response (Vasodilation & Increased Permeability)
Duration: Immediate to several minutes after injury
Key Features:
- Blood vessels in the affected area dilate (vasodilation) → increased blood flow (causes redness & heat).
- Increased vascular permeability → leakage of fluid, proteins, and immune cells into tissues (causes swelling).
- Chemical mediators like histamine, prostaglandins, bradykinin, serotonin are released by mast cells and damaged tissues.
Clinical Signs:
- Redness (rubor)
- Heat (calor)
- Swelling (tumor)
- Pain (dolor) due to pressure and chemical irritation
Stage 2: Cellular Response (Phagocytic Phase)
Duration: Within hours of injury
Key Features:
- White blood cells (especially neutrophils and macrophages) migrate to the site via chemotaxis.
- Phagocytosis occurs—WBCs engulf and digest pathogens, dead cells, and debris.
- Formation of pus if there is infection (purulent inflammation).
- Cytokines (chemical messengers) are released to regulate and amplify the immune response.
Clinical Signs:
- Formation of exudate (serous, purulent, or hemorrhagic)
- Localized warmth
- Possible fever and fatigue (systemic signs)
- Enlarged lymph nodes (lymphadenopathy)
Stage 3: Tissue Repair and Healing Phase
Duration: Starts after infection/injury is controlled; may last days to weeks
Key Features:
- Removal of exudate and dead cells.
- Regeneration: Replacement of damaged cells with new cells (if possible).
- Fibrosis: Formation of scar tissue (if cells cannot regenerate).
- Involvement of fibroblasts, collagen, and angiogenesis (formation of new blood vessels).
- Return of tissue function, unless scarring impairs it.
Outcome:
- Resolution (complete healing) if damage is minor.
- Repair with scar if damage is deep or permanent cells are lost.
- Chronic inflammation may occur if cause is persistent or unresolved.
Summary Chart: Stages of Inflammation
| Stage | Main Event | Outcome |
|---|---|---|
| Vascular | Vasodilation, fluid leakage | Redness, heat, swelling, pain |
| Cellular | WBC migration, phagocytosis | Destruction of pathogens, pus formation |
| Repair/Healing | Tissue regeneration or fibrosis | Healing, scar formation, or chronicity |
Conclusion
Inflammation follows a sequential and overlapping set of stages, each essential to defense and recovery. Understanding these stages enables healthcare professionals to:
- Identify inflammation early
- Monitor its progression
- Apply appropriate interventions (antibiotics, anti-inflammatories, wound care)
Medical Management of Inflammation
The goal of medical management in inflammation is to:
- Relieve symptoms (pain, swelling, fever)
- Eliminate the cause (infection, injury, allergen, etc.)
- Prevent complications
- Promote tissue healing and recovery
Treatment may vary depending on whether the inflammation is acute or chronic, infectious or non-infectious, and localized or systemic.
1. Pharmacological Management
A. Non-Steroidal Anti-Inflammatory Drugs (NSAIDs)
These are the most commonly used drugs to treat inflammation.
| Examples | Ibuprofen, Diclofenac, Naproxen, Aspirin |
|---|---|
| Action | Inhibit prostaglandin synthesis (↓ pain & swelling) |
| Used for | Musculoskeletal pain, fever, arthritis, injuries |
⚠️ Caution: Long-term use can cause *gastric ulcers, kidney damage, and bleeding. Always give after food.
B. Corticosteroids
Powerful anti-inflammatory drugs that suppress the immune response.
| Examples | Prednisolone, Dexamethasone, Hydrocortisone |
|---|---|
| Action | Reduce inflammation by blocking multiple inflammatory pathways |
| Used for | Severe allergies, autoimmune diseases, asthma, chronic inflammation |
⚠️ Caution: Long-term use may cause osteoporosis, infections, hyperglycemia, and adrenal suppression.
C. Analgesics (Pain Relievers)
Used to relieve pain associated with inflammation.
| Examples | Paracetamol (Acetaminophen), Tramadol |
|---|---|
| Action | Inhibits pain sensation in the brain |
| Used for | Mild to moderate pain without strong anti-inflammatory effect |
D. Antibiotics / Antimicrobials
Used only when inflammation is due to infection (e.g., bacterial abscess, cellulitis, pneumonia).
| Examples | Amoxicillin, Ciprofloxacin, Azithromycin |
|---|---|
| Action | Kill or inhibit growth of bacteria |
| Note | Should be used only with confirmed or suspected infection |
E. Immunosuppressants / DMARDs (for chronic inflammation)
Used in autoimmune or chronic inflammatory diseases like rheumatoid arthritis, lupus.
| Examples | Methotrexate, Azathioprine, Sulfasalazine |
|---|---|
| Action | Suppress abnormal immune activity |
| Used for | Autoimmune arthritis, inflammatory bowel disease, etc. |
2. Supportive and Non-Pharmacological Measures
A. Rest and Immobilization
- Rest the inflamed area to prevent further injury and allow healing.
- Use of splints, slings, or bandages for joint inflammation.
B. Ice and Heat Therapy
- Ice: Useful in acute inflammation to reduce swelling and pain (first 24–48 hrs).
- Heat: Useful in chronic inflammation to improve blood flow and flexibility.
C. Elevation
- Raising the affected limb helps reduce swelling (e.g., in cellulitis or sprain).
D. Compression
- Using elastic bandages or stockings to prevent fluid accumulation in inflamed limbs.
E. Nutritional Support
- Anti-inflammatory diet rich in:
- Omega-3 fatty acids (fish, flaxseed)
- Fruits and vegetables (antioxidants)
- Low saturated fats and processed sugars
3. Surgical Management (if required)
Used when inflammation leads to abscess formation, severe infection, or tissue necrosis.
| Procedures | Drainage of abscess, debridement of necrotic tissue, joint replacement (in arthritis) |
4. Lifestyle and Long-Term Management (for chronic inflammation)
- Stress management: Chronic stress can worsen inflammation.
- Regular exercise: Reduces inflammation and improves immunity.
- Avoid smoking and alcohol: Both increase systemic inflammation.
- Weight control: Obesity is linked to chronic inflammatory diseases.
5. Nursing Role in Inflammation Management
- Administer prescribed medications safely.
- Monitor for side effects (e.g., gastric irritation from NSAIDs).
- Educate patient on correct use of ice/heat therapy.
- Promote proper nutrition and hydration.
- Record and report changes in symptoms (e.g., increased redness, pus, fever).
- Ensure rest and support for the inflamed area.
- Provide emotional support and patient education, especially in chronic conditions.
Surgical Management of Inflammation
While most inflammatory conditions can be managed through medications and conservative methods, some cases require surgical intervention—especially when inflammation leads to complications such as pus collection, tissue necrosis, organ dysfunction, or obstruction. Surgical management aims to:
- Remove the source of infection or irritation
- Drain abscesses or fluid collections
- Excise necrotic or inflamed tissue
- Restore anatomical and functional integrity
Indications for Surgical Management of Inflammation
Surgery is indicated when:
- There is failure of medical therapy
- Inflammation results in abscess formation
- There is obstruction, perforation, or gangrene of an organ
- Infected tissue requires debridement
- Chronic inflammation has caused structural damage
Common Surgical Procedures in Inflammatory Conditions
1. Incision and Drainage (I&D)
- Purpose: To drain pus from abscesses, boils, or cellulitis.
- Procedure:
- A sterile incision is made over the abscess.
- Pus is drained, and the cavity is cleaned.
- A drain may be placed, and dressing is applied.
Examples:
- Skin abscess
- Perianal abscess
- Breast abscess
2. Debridement
- Purpose: Removal of dead, infected, or necrotic tissue to prevent spread and promote healing.
- Types:
- Surgical debridement
- Mechanical, enzymatic, or autolytic (non-surgical) methods
Examples:
- Infected diabetic foot ulcer
- Pressure sore with necrosis
- Gangrene
3. Appendectomy
- Purpose: Surgical removal of the inflamed appendix in acute appendicitis.
- Urgency: Emergency surgery to prevent rupture and peritonitis.
4. Cholecystectomy
- Purpose: Removal of inflamed gallbladder (cholecystitis).
- Approach: Laparoscopic or open surgery depending on severity.
5. Bowel Resection / Repair
- Purpose: To manage severe inflammatory bowel diseases (IBD) like Crohn’s disease, ulcerative colitis, or perforated intestine.
- May involve:
- Removing inflamed/obstructed sections
- Creating colostomy or ileostomy
6. Tonsillectomy / Adenoidectomy
- Indicated in chronic or recurrent inflammation of tonsils/adenoids.
- Reduces symptoms like sore throat, difficulty swallowing, or breathing issues.
7. Drainage of Joint Effusion
- In case of septic arthritis or inflammatory effusion, surgery may be needed to aspirate fluid or wash out the joint.
8. Synovectomy
- Surgical removal of inflamed synovial tissue in chronic inflammatory joint diseases like rheumatoid arthritis.
9. Surgical Wound Management
- In post-operative infections or inflamed wounds:
- Opening of wound
- Irrigation with antiseptic/antibiotic solutions
- Drainage and re-dressing under sterile conditions
10. Drain Insertion
- Tube drains (e.g., intercostal drainage, pigtail catheter) are used to:
- Remove infected fluids, pus, or air from pleural cavity, abdomen, or other spaces.
Pre- and Post-Surgical Considerations
Pre-operative:
- Control infection with antibiotics if needed.
- Ensure sterile environment.
- Obtain informed consent.
- Prepare patient physically and emotionally.
Post-operative:
- Monitor for signs of wound infection, bleeding, fever, or recurrence.
- Ensure proper pain management and wound care.
- Educate the patient on hygiene, follow-up, and red flags.
Nursing Role in Surgical Inflammation Management
- Pre-op preparation (consent, NPO status, skin prep)
- Assisting in surgical procedures
- Post-op monitoring (vitals, wound inspection, drain output)
- Pain assessment and medication administration
- Educating patients on discharge care and hygiene
- Preventing complications (DVT, bedsores, infection)
Nursing Management of Inflammation
Inflammation is a protective response of the body to injury, infection, or irritation. While it aids in healing, uncontrolled or severe inflammation can lead to tissue damage, pain, and systemic complications. The role of the nurse is crucial in:
- Monitoring signs of inflammation
- Providing symptom relief
- Preventing complications
- Promoting healing and recovery
Nursing Assessment
A thorough nursing assessment helps determine the type, severity, and impact of inflammation.
Subjective Data:
- Patient reports pain, swelling, warmth, or stiffness
- Fatigue or discomfort
- History of injury, infection, or autoimmune disease
Objective Data:
- Redness, heat, swelling at the site
- Fever or chills
- Elevated vital signs (e.g., temperature, pulse)
- Laboratory results: ↑ WBC count, ↑ CRP, ↑ ESR
- Presence of exudate, pus, or drainage
- Impaired mobility or function
Nursing Diagnoses (Examples)
- Acute Pain related to inflammatory response
- Risk for Infection related to inflamed tissue
- Impaired Physical Mobility related to pain/swelling
- Risk for Impaired Skin Integrity due to inflammation or drainage
- Deficient Knowledge regarding self-care and disease process
Nursing Interventions
1. Pain Management
- Administer prescribed analgesics or anti-inflammatory drugs (e.g., NSAIDs, corticosteroids)
- Use cold compresses in acute stages to reduce pain and swelling
- Promote rest of the affected area to prevent further injury
- Use positioning and support devices (e.g., pillows, splints)
2. Monitoring and Observation
- Monitor:
- Vital signs (especially temperature and pulse)
- Local signs (redness, swelling, tenderness)
- Signs of infection (purulent discharge, spreading redness)
- Record and report changes in symptoms or worsening of inflammation
- Check lab reports (WBC count, ESR, CRP)
3. Promote Healing
- Maintain proper nutrition: high-protein, vitamin-rich diet
- Encourage fluid intake unless contraindicated
- Assist with mobility exercises if inflammation affects joints (to prevent stiffness)
- Support wound care if inflammation involves skin or surgical sites
4. Infection Prevention
- Use aseptic techniques during dressing changes
- Ensure hand hygiene, PPE, and waste disposal
- Educate patient about personal hygiene
- Isolate patient if inflammation is due to contagious infection
5. Patient and Family Education
- Teach about:
- Medication adherence and possible side effects
- Signs of worsening inflammation or infection
- Importance of follow-up appointments
- Use of home remedies (e.g., cold packs, elevation) if advised
- Advise on lifestyle changes for chronic inflammation (e.g., arthritis): weight control, exercise, joint care
6. Psychological and Emotional Support
- Provide reassurance and support for anxiety or fear due to illness
- Involve family in care if appropriate
- Offer spiritual or social support when needed
Evaluation
- Patient reports reduced pain and discomfort
- Swelling, redness, and temperature have decreased
- Vital signs stabilized
- Patient demonstrates understanding of care and self-management
- Wound (if present) shows signs of healing
Infection
Definition
An infection is defined as:
“The invasion and multiplication of microorganisms such as bacteria, viruses, fungi, or parasites in the body, which may cause tissue damage and disease.”
Infections may be localized or systemic, symptomatic or asymptomatic, and acute or chronic.
Types of Infection
Infections can be classified in multiple ways:
A. Based on Causative Agent
| Type | Example |
|---|---|
| Bacterial | Tuberculosis, pneumonia, UTI |
| Viral | Influenza, COVID-19, Hepatitis |
| Fungal | Candidiasis, ringworm |
| Parasitic | Malaria, amoebiasis |
| Rickettsial | Typhus, scrub typhus |
B. Based on Location
| Type | Description | Example |
|---|---|---|
| Localized | Limited to one area | Boil, ear infection |
| Systemic | Affects entire body, spread via blood | Sepsis, HIV |
C. Based on Mode of Onset
| Type | Characteristics |
|---|---|
| Acute | Rapid onset, short duration (days) |
| Chronic | Slow onset, prolonged (weeks/months) |
| Latent | Dormant phase before reactivation |
D. Based on Source
| Type | Example |
|---|---|
| Community-acquired | Common infections outside hospitals |
| Hospital-acquired (Nosocomial) | Surgical site infection, VAP |
| Opportunistic | Occurs in immunocompromised (e.g., HIV) |
Causes of Infection
Infections are caused by pathogenic microorganisms, often influenced by:
1. Causative Agents:
- Bacteria – E. coli, Staphylococcus aureus
- Viruses – HIV, Influenza
- Fungi – Candida, Aspergillus
- Parasites – Plasmodium, Entamoeba
- Prions – Abnormal proteins (e.g., in Mad Cow Disease)
2. Routes of Transmission:
- Direct contact (person-to-person)
- Indirect contact (contaminated surfaces)
- Airborne (cough, sneezing)
- Droplet (flu, COVID-19)
- Vector-borne (mosquitoes, ticks)
- Bloodborne (transfusions, needles)
- Feco-oral route (contaminated food/water)
Signs and Symptoms of Infection
Signs and symptoms depend on the site, severity, and type of infection. However, common features include:
General/Systemic Signs:
- Fever and chills
- Fatigue or malaise
- Loss of appetite
- Increased pulse and respiratory rate
- Sweating
Localized Signs:
| Site of Infection | Signs & Symptoms |
|---|---|
| Skin/Wound | Redness, warmth, swelling, pus |
| Respiratory | Cough, sputum, breathlessness, chest pain |
| Urinary tract | Burning urination, frequency, lower abdominal pain |
| Gastrointestinal | Nausea, vomiting, diarrhea, cramps |
| Central nervous system | Headache, stiff neck, altered consciousness (e.g., meningitis) |
Diagnosis of Infection
1. Clinical Examination
- History taking (onset, exposure, symptoms)
- Physical exam (temperature, site-specific inspection)
2. Laboratory Tests
| Test | Purpose |
|---|---|
| Complete Blood Count (CBC) | ↑ WBC count in bacterial infections |
| CRP & ESR | Markers of inflammation |
| Procalcitonin | Marker for bacterial sepsis |
| Urine Examination | For UTI detection |
| Blood culture | To detect systemic infections (bacteremia) |
| Sputum culture | To detect lung infections |
| Wound swab culture | Identify organisms from wounds |
| Stool test | To detect intestinal infections |
| PCR/Serological tests | For viral infections (HIV, hepatitis, COVID-19) |
3. Imaging Tests
- Chest X-ray – Pneumonia, TB
- Ultrasound/CT scan – Abscess, organ infections
- MRI – CNS infections or deep-seated abscesses
Medical Management of Infection
A. Antimicrobial Therapy
These are drugs that kill or inhibit the growth of microorganisms.
| Type | Examples | Used For |
|---|---|---|
| Antibiotics | Amoxicillin, Ceftriaxone, Azithromycin | Bacterial infections |
| Antivirals | Acyclovir, Oseltamivir, Zidovudine | Viral infections (e.g. Herpes, Flu, HIV) |
| Antifungals | Fluconazole, Amphotericin B | Fungal infections (e.g. Candidiasis) |
| Antiparasitics | Metronidazole, Albendazole | Protozoal/helminthic infections |
⚠️ Note: Proper drug selection, dose, route, and duration are crucial to avoid resistance and ensure recovery.
B. Symptomatic Management
- Antipyretics (e.g., Paracetamol) – for fever
- Analgesics (e.g., Ibuprofen) – for pain relief
- Anti-inflammatory drugs – to reduce swelling and discomfort
- Antiemetics, antidiarrheals – if GI symptoms are present
- IV fluids – to maintain hydration in febrile/toxic patients
C. Supportive Therapy
- Oxygen therapy – in respiratory infections (e.g., pneumonia, COVID-19)
- Nutritional support – to boost immunity and recovery
- Blood transfusion – in severe infections causing anemia or sepsis
- Monitoring – vital signs, fluid balance, organ function (especially in systemic infections)
D. Isolation and Infection Control
- Use of PPE (gloves, masks, gowns)
- Isolation rooms for contagious infections
- Strict hand hygiene and disinfection protocols
- Waste disposal as per biomedical guidelines
E. Patient Education
- Medication adherence
- Prevention of spread (cough etiquette, hand hygiene)
- Nutrition and hydration
- Importance of follow-up
Surgical Management of Infection
Surgery is required when infection leads to abscess, tissue death, obstruction, or failure of medical therapy.
A. Incision and Drainage (I&D)
- To drain pus from abscesses or boils
- Reduces pressure, pain, and speeds up healing
- Often followed by antibiotic therapy
Examples: Skin abscess, breast abscess, perianal abscess
B. Debridement
- Removal of necrotic (dead), infected, or devitalized tissue
- Prevents the spread of infection and promotes wound healing
- May be done surgically or through enzymatic agents
Examples: Diabetic foot ulcer, gangrenous wounds
C. Amputation
- In extreme cases (e.g., uncontrolled gangrene or necrotizing fasciitis)
- To save the patient’s life by removing the source of infection
D. Abscess Drainage (Deep-Seated)
- For internal organ abscesses (e.g., liver, brain, lung), guided by ultrasound or CT scan
- May require surgical or image-guided catheter drainage
E. Removal of Infected Devices or Implants
- Catheters, prosthetic joints, pacemakers may become infected
- Must be removed if infection does not respond to antibiotics
F. Organ-Specific Surgery
| Infection | Surgical Procedure |
|---|---|
| Appendicitis | Appendectomy |
| Cholecystitis | Cholecystectomy |
| Infected kidney stone | Nephrostomy or pyelolithotomy |
| Intestinal obstruction | Resection and anastomosis |
Combined Approach
Often, both medical and surgical treatment are needed:
Example: A diabetic foot ulcer with abscess may require:
- IV antibiotics (medical)
- Surgical debridement and dressing (surgical)
Nursing Management
Nursing Assessment
Accurate and timely assessment is the foundation of effective nursing care.
Subjective Data
- Patient complaints: fever, pain, chills, fatigue
- History of recent injury, surgery, hospital stay, or contact with infected persons
- Appetite changes, malaise, or sore throat
Objective Data
- Vital signs: ↑ temperature, ↑ pulse, ↑ respiratory rate
- Inspection of infection site: redness, swelling, pus, warmth
- Lab reports: ↑ WBC count, ↑ CRP, ↑ ESR
- Culture/sensitivity results, if available
Common Nursing Diagnoses Related to Infection
- Hyperthermia related to infectious process
- Acute Pain related to inflammatory response
- Risk for Spread of Infection related to poor hygiene or open wound
- Impaired Skin Integrity related to wound infection
- Imbalanced Nutrition: Less than body requirements related to infection
- Fatigue related to systemic infection
- Deficient Knowledge related to disease process and self-care
Nursing Interventions
1. Monitor and Assess
- Monitor vital signs, especially temperature and heart rate
- Assess for signs of local or systemic infection (pus, rashes, cough, UTI symptoms)
- Observe the progress of the infection site (size, color, drainage)
- Evaluate lab reports (CBC, culture, ESR, CRP)
2. Administer Medications as Prescribed
- Antibiotics, antivirals, antifungals – monitor for side effects/allergies
- Antipyretics (e.g., paracetamol) – to reduce fever
- Analgesics – to manage pain
- Ensure timing, dosage, and route are correct
3. Prevent the Spread of Infection
- Practice strict hand hygiene
- Follow infection control protocols (use gloves, masks, PPE)
- Isolate patient if necessary (airborne, droplet, contact precautions)
- Encourage respiratory hygiene, cough etiquette
- Proper disposal of contaminated items/waste
4. Provide Symptomatic and Supportive Care
- Cool compresses or tepid sponging for fever
- Encourage fluid intake to prevent dehydration
- Offer nutritious, high-protein, easy-to-digest meals
- Provide rest and comfort measures
- Promote skin care to prevent pressure ulcers
5. Maintain Skin Integrity and Wound Care
- Perform regular dressing changes using aseptic technique
- Inspect for signs of worsening (odor, pus, discoloration)
- Encourage position changes in bed-bound patients
- Apply topical antibiotics if prescribed
6. Educate the Patient and Family
- Explain the nature and course of infection
- Teach importance of completing full course of antibiotics
- Instruct on hygiene, handwashing, and care of wounds or catheters
- Educate about nutrition, hydration, and signs of worsening infection
- Encourage follow-up visits and vaccination if needed
Evaluation
- Fever reduced; vital signs return to normal
- Infection site healing with no spread
- Patient reports pain relief and improved energy
- Lab values improved (↓ WBC, CRP, etc.)
- Patient understands medication regimen and self-care
Nurse’s Role in Infection Control
- Follow hospital infection prevention protocols
- Act as advocate for early isolation and hygiene enforcement
- Coordinate with infection control nurse if needed
- Report hospital-acquired infections (HAIs) as per policy
Wound Healing
Definition
Wound healing is defined as:
“The complex physiological process by which the skin or any body tissue repairs itself after injury.”
It involves a series of coordinated cellular and biochemical events that lead to tissue repair, regeneration, and restoration of integrity.
Types of Wound Healing (Based on Intention)
| Type | Description |
|---|---|
| Primary Intention | Healing of clean, surgical wounds with edges approximated (sutured). Minimal scarring. |
| Secondary Intention | Wounds left open to heal naturally (e.g., ulcers, infected wounds). Longer healing, more scarring. |
| Tertiary Intention | Delayed primary closure after infection control or drainage. Sutured later. |
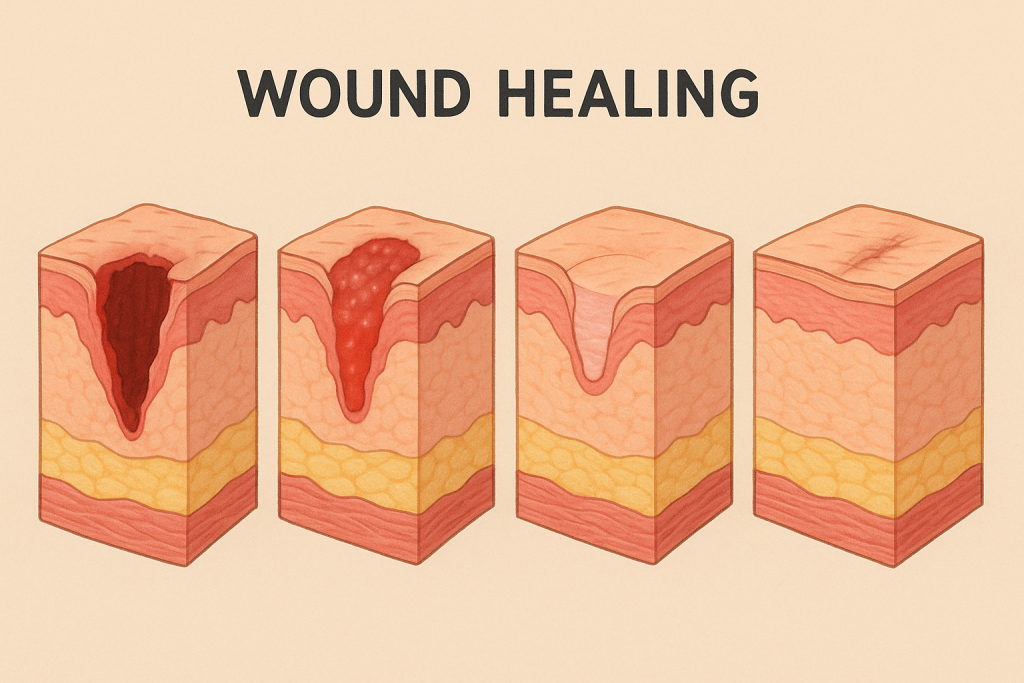
Stages/Phases of Wound Healing
Wound healing occurs in four overlapping stages:
1. Hemostasis Phase (Immediate)
Duration: Minutes to hours after injury
Main Events:
- Vasoconstriction and platelet aggregation
- Formation of a blood clot to stop bleeding
- Release of chemical mediators like thrombin, fibrin
Purpose: Control bleeding and create a stable environment for healing.
2. Inflammatory Phase (Day 1–3)
Main Events:
- Vasodilation increases blood flow to the area
- White blood cells (neutrophils, macrophages) migrate to wound
- Removal of pathogens, dead cells, debris (phagocytosis)
Signs: Redness, swelling, warmth, pain
Purpose: Prevent infection and prepare wound for repair.
3. Proliferative Phase (Day 3–21)
Main Events:
- Formation of granulation tissue (new connective tissue and capillaries)
- Fibroblasts produce collagen
- Re-epithelialization: new skin cells migrate to cover the wound
- Angiogenesis: new blood vessels grow
Purpose: Build new tissue and close the wound.
4. Maturation or Remodeling Phase (Day 21 to months/years)
Main Events:
- Collagen remodeling and strengthening
- Reduction of blood vessels in the wound area
- Scar tissue forms
Purpose: Restore tissue strength and function
Types of Wounds That Undergo Healing
- Surgical wounds
- Traumatic wounds (cuts, lacerations)
- Chronic wounds (pressure ulcers, diabetic foot ulcers)
- Burns
- Infected wounds
Factors Affecting Wound Healing
Local Factors
- Infection
- Oxygenation and blood supply
- Pressure/friction at wound site
- Presence of foreign body or necrotic tissue
- Type and depth of wound
Systemic Factors
- Age (healing slower in elderly)
- Nutrition (protein, Vitamin C, zinc deficiency delays healing)
- Diabetes or chronic illnesses
- Medications (e.g., corticosteroids slow healing)
- Smoking and alcohol
- Immunosuppression
Complications of Wound Healing
| Complication | Description |
|---|---|
| Infection | Redness, pus, fever, foul odor |
| Dehiscence | Wound edges separate after closure |
| Evisceration | Internal organs protrude from wound |
| Hypertrophic scar | Excessive collagen within wound margins |
| Keloid | Overgrowth of scar tissue beyond wound |
| Chronic non-healing | Due to poor circulation, diabetes, etc. |
Nursing Management in Wound Healing
Assessment
- Inspect wound size, depth, drainage, color, odor
- Monitor for signs of infection
- Check for pain, swelling, or changes in temperature
Wound Care
- Perform dressing changes using aseptic technique
- Use appropriate dressings (gauze, hydrocolloid, alginate, etc.)
- Maintain moist wound environment (not too dry or too wet)
- Assist in debridement if needed (mechanical or enzymatic)
- Monitor and manage drains or sutures
Pain Management
- Administer prescribed analgesics
- Minimize handling during dressing
Nutrition Support
- Encourage high-protein, vitamin C, iron, and zinc-rich diet
- Ensure adequate fluid intake
Patient Education
- Teach wound care at home
- Educate on signs of infection
- Emphasize hand hygiene and wound protection
- Encourage smoking cessation and diabetes control
Conclusion
Wound healing is a natural, but complex process influenced by many local and systemic factors. Nurses play a key role in promoting healing by providing effective wound care, preventing infections, supporting nutrition, and educating patients. Prompt action and appropriate care ensure faster recovery and minimal complications.
Factors Influencing Wound Healing
Wound healing is a complex, multi-stage biological process. Several factors can promote or delay healing. These are broadly classified into local (at the wound site) and systemic (related to the patient’s overall health).
1. Local Factors (Directly Affect the Wound Site)
A. Infection
- Presence of bacteria increases inflammation, delays healing, and may lead to wound breakdown or abscess formation.
- Infected wounds often show redness, pus, odor, and increased pain.
B. Oxygenation and Blood Supply
- Adequate blood flow provides oxygen and nutrients for healing.
- Conditions like anemia, vascular disease, or pressure ulcers impair blood supply and delay healing.
C. Moisture Balance
- A moist wound environment promotes cell growth and epithelial migration.
- Too dry: delays healing.
- Too wet: leads to maceration of skin.
D. Foreign Bodies
- Presence of dirt, sutures, or necrotic tissue in the wound can prolong inflammation and prevent healing.
E. Pressure and Trauma
- Repeated movement, pressure (especially in bedridden patients), or trauma disrupts healing tissues.
F. Type and Size of Wound
- Surgical wounds (clean and closed) heal faster than traumatic or infected wounds.
- Larger and deeper wounds take more time to heal than smaller ones.
2. Systemic Factors (Affect Overall Healing Ability)
A. Age
- Elderly patients have slower cell regeneration, reduced immune function, and thinner skin, leading to delayed healing.
B. Nutrition
- Protein is needed for tissue repair.
- Vitamin C aids in collagen formation.
- Zinc, iron, and vitamin A are essential for immunity and cell growth.
- Malnutrition or poor dietary intake slows down healing.
C. Chronic Diseases
- Diabetes mellitus impairs blood flow, immune response, and increases infection risk.
- Kidney, liver, or heart diseases reduce circulation and metabolism, delaying healing.
D. Medications
- Corticosteroids suppress inflammation and collagen formation.
- Chemotherapy and immunosuppressants reduce immune cell function.
- NSAIDs may delay healing in high doses.
E. Smoking and Alcohol
- Nicotine reduces blood flow and oxygenation.
- Alcohol impairs immune function and liver detoxification, delaying repair.
F. Immune Status
- Immunocompromised individuals (e.g., HIV, cancer, transplant patients) heal slower due to weak immune responses.
G. Stress and Psychological State
- High stress increases cortisol levels, which suppress immunity and delay healing.
H. Obesity
- Adipose tissue has poor blood supply, which delays oxygen and nutrient delivery.
- Increased risk of wound dehiscence and infection.
Summary Table: Factors Affecting Wound Healing
| Local Factors | Systemic Factors |
|---|---|
| Infection | Age |
| Blood supply | Nutritional status |
| Wound size & depth | Chronic illnesses (e.g., diabetes) |
| Foreign bodies | Medications (steroids, chemo) |
| Moisture balance | Smoking and alcohol |
| Pressure or trauma | Immune status |
| Type of wound (clean vs. dirty) | Stress and psychological state |
Wound Care

Introduction
Wound care is the systematic assessment, cleaning, dressing, and monitoring of a wound to promote healing, prevent infection, and minimize complications. It is a vital component of nursing care and plays a significant role in preventing chronic wounds, infections, and improving patient comfort and recovery.
Definition
Wound care refers to the medical and nursing management of a wound, involving procedures to clean, dress, and monitor the wound while supporting the natural healing process.
Objectives of Wound Care
- Promote fast and effective healing
- Prevent or control infection
- Maintain a moist wound environment
- Protect the wound from trauma and contamination
- Reduce pain and discomfort
- Minimize scarring
- Support tissue regeneration
Types of Wounds (Needing Wound Care)
| Type of Wound | Examples |
|---|---|
| Acute wounds | Surgical incisions, cuts, abrasions |
| Chronic wounds | Pressure ulcers, diabetic foot ulcers, venous ulcers |
| Infected wounds | Abscesses, infected surgical sites |
| Open wounds | Lacerations, burns, bites |
| Closed wounds | Bruises, hematomas |
Principles of Wound Care
- Use aseptic technique to prevent infection
- Cleanse wound gently with sterile solution (e.g., normal saline)
- Debride necrotic tissue (if present) to promote healing
- Maintain a moist wound environment to aid tissue repair
- Choose appropriate wound dressing
- Manage pain and discomfort
- Observe for signs of infection (e.g., pus, redness, fever)
- Support nutrition and hydration
- Educate the patient on self-care and hygiene
- Document wound size, appearance, drainage, and progress regularly
Steps in Wound Care Procedure (General)
1. Preparation
- Explain the procedure to the patient
- Gather sterile equipment: gloves, dressing set, sterile gauze, saline, disposal bags
- Position the patient comfortably
- Perform hand hygiene and use PPE if needed
2. Removal of Old Dressing
- Use non-touch technique
- Inspect dressing for amount, color, and odor of drainage
- Discard used dressing properly
3. Wound Cleaning
- Use sterile normal saline or prescribed solution
- Clean wound from least contaminated (center) to most contaminated (periphery)
- Do not rub harshly—gentle patting or irrigation is preferred
4. Debridement (if indicated)
- Remove dead/necrotic tissue using sterile instruments or enzymatic agents
- May be done mechanically, surgically, or autolytically
5. Dressing the Wound
- Apply appropriate dressing based on wound type and condition (e.g., hydrocolloid, alginate, foam)
- Secure dressing with tape or bandage
- Label with date/time if needed
6. Documentation
- Note size, depth, color, exudate, odor, condition of surrounding skin, and patient’s response
- Update wound chart or electronic health record
Types of Dressings
| Type of Dressing | Used For |
|---|---|
| Gauze dressing | Clean, dry wounds; primary or secondary use |
| Hydrocolloid dressing | Moist healing; minor burns, ulcers |
| Foam dressing | Moderate to heavy exudate wounds |
| Alginate dressing | Bleeding or draining wounds |
| Film dressing | Superficial wounds, IV sites |
| Antimicrobial dressing | Infected or high-risk wounds (e.g., silver-based) |
Signs of Wound Infection to Monitor
- Increased redness, warmth, or swelling
- Foul-smelling or purulent (pus) discharge
- Fever or chills
- Pain or tenderness increases
- Wound not healing or worsening
Factors Promoting Effective Wound Healing
- Good nutrition (high-protein, vitamin C, zinc)
- Adequate hydration
- Blood sugar control (in diabetics)
- No smoking or alcohol use
- Regular wound monitoring and dressing changes
- Clean, hygienic environment
Nursing Responsibilities in Wound Care
- Perform wound assessment and dressing using proper technique
- Administer medications as prescribed (e.g., antibiotics, painkillers)
- Educate patient/family on wound care and hygiene
- Encourage good nutrition and lifestyle habits
- Report any complications or delay in healing to the doctor
- Maintain accurate records and follow infection control protocols
Dressing Technique
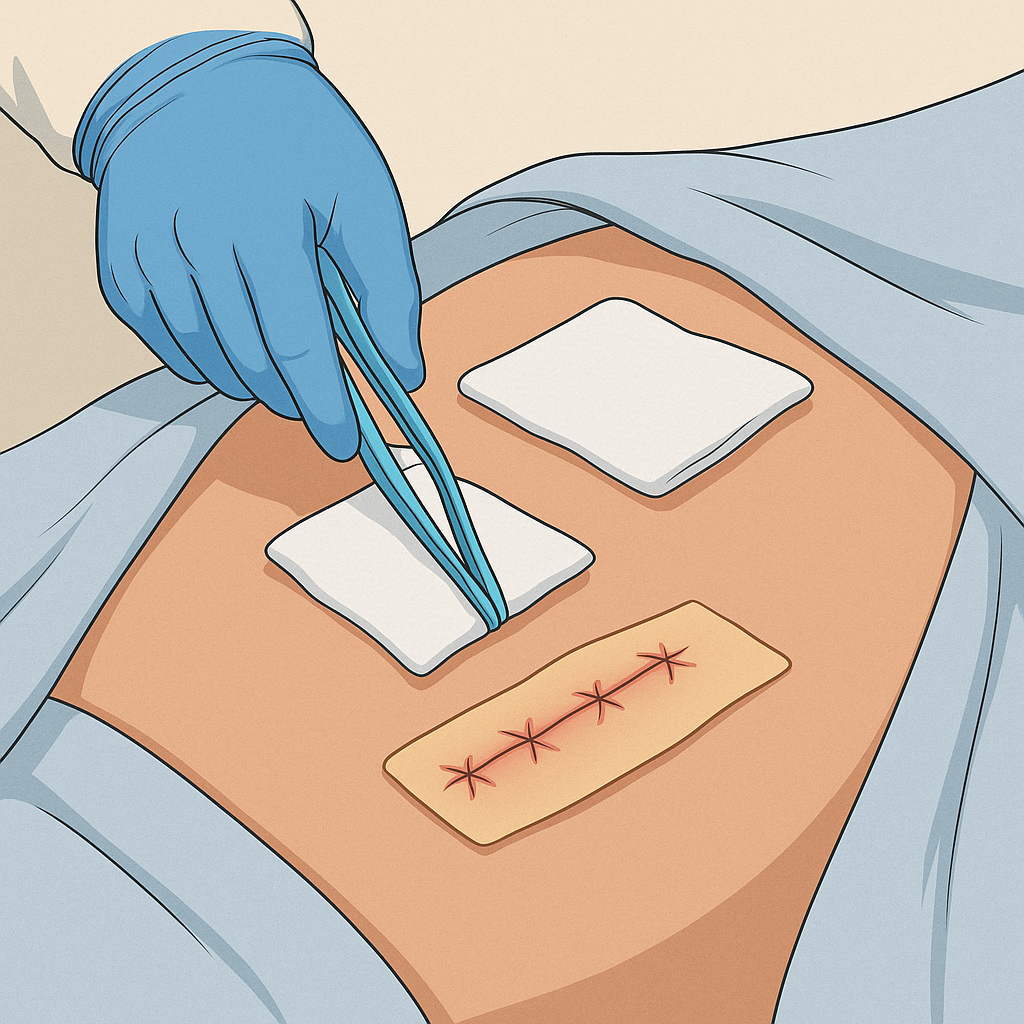
Definition
Dressing technique refers to the aseptic procedure used to clean, inspect, and cover a wound with a sterile or appropriate dressing to promote healing and prevent infection.
Dressing changes are a critical part of wound care and must be performed using aseptic or clean technique, depending on the wound type and healthcare setting.
Purposes of Wound Dressing
- To protect the wound from contamination and trauma
- To absorb exudate and promote healing
- To maintain a moist environment
- To reduce pain and prevent infection
- To support tissue regeneration
Equipment Used for Dressing
| Basic Items | Purpose |
|---|---|
| Sterile dressing pack | Contains gauze, forceps, towel, etc. |
| Sterile gloves | Maintain aseptic technique |
| Sterile cotton swabs/gauze | Wound cleaning and dressing |
| Normal saline or prescribed antiseptic | Wound cleaning |
| Dressing material (gauze pad, hydrocolloid, etc.) | Cover and protect wound |
| Adhesive tape or bandage | Secure the dressing |
| Scissors (sterile) | Cut dressing material |
| Waste disposal bag / kidney tray | Collect used items |
| PPE (gloves, mask, apron if needed) | Infection control |
| Towel or waterproof sheet | To protect patient bed or clothes |
| Documentation sheet/pen | To record procedure and wound status |
Pre-Procedure Preparation
Nurse’s Preparation
- Wash hands and wear clean gloves.
- Assemble all necessary supplies.
- Ensure good lighting and privacy.
- Maintain a sterile field for sterile dressings.
Patient Preparation
- Explain the procedure to relieve anxiety.
- Position the patient comfortably.
- Provide adequate lighting and exposure of the wound site.
- Protect bed linen with a towel or mackintosh.
Procedure Steps for Sterile Dressing Technique
Follow Aseptic Technique Throughout
1. Remove Old Dressing
- Wear clean gloves.
- Carefully remove the existing dressing.
- Observe and note the type, color, odor, and amount of exudate.
- Discard used dressing in appropriate waste bin.
- Remove gloves and perform hand hygiene.
2. Set Up Sterile Field
- Open the sterile dressing pack without touching contents.
- Pour sterile solution (e.g., normal saline) into the tray using no-touch technique.
- Wear sterile gloves.
3. Clean the Wound
- Use sterile gauze/cotton swabs soaked in saline or antiseptic.
- Clean from cleanest area (center) to dirtiest area (periphery).
- Use one gauze per stroke — never reinsert used swab into solution.
- If wound is infected, clean surrounding skin last.
4. Inspect the Wound
- Check wound for:
- Redness, swelling
- Exudate (type and quantity)
- Odor
- Size, depth, granulation tissue, necrosis
5. Apply New Dressing
- Place the appropriate sterile dressing over the wound.
- Use secondary dressing or padding if required.
- Secure the dressing with adhesive tape or bandage.
6. Dispose of Waste
- Remove gloves and dispose of all used items properly.
- Follow biomedical waste segregation rules.
7. Post-Procedure Care
- Make the patient comfortable.
- Wash hands.
- Document:
- Wound condition
- Type of dressing applied
- Patient response
- Date/time of dressing change
Key Nursing Points
- Always follow aseptic technique to prevent cross-infection.
- Choose the dressing material based on wound type, exudate level, and healing stage.
- Educate the patient on wound hygiene, signs of infection, and when to return for dressing.
- Monitor healing progress and report abnormal signs like delayed healing, pus, increased pain, or bleeding.
- Coordinate with the doctor for dressing orders and changes in wound management plan.
Role of Nurse in Dressing of Wound
Introduction
Wound dressing is a critical nursing responsibility that not only promotes healing but also prevents infection and provides comfort. The nurse plays a central role in all stages of the wound dressing process — from assessment to documentation and patient education.
1. Assessment Role
- Inspect the wound before, during, and after dressing:
- Size, depth, color, exudate (type & amount)
- Signs of infection (redness, odor, pus, heat)
- Wound edges (healthy or necrotic)
- Assess pain level before and after the procedure.
- Monitor the condition of surrounding skin.
- Evaluate patient’s nutritional status, diabetes control, mobility, etc., which affect healing.
2. Preparation Role
- Prepare the environment: ensure privacy, adequate light, and sterile setup.
- Explain the procedure to reduce anxiety and gain cooperation.
- Assemble and check all sterile equipment needed for dressing.
- Perform hand hygiene and wear PPE as per standard precautions.
- Ensure the patient is comfortably positioned to expose the wound site.
3. Procedural Role
- Maintain aseptic technique throughout the procedure.
- Gently remove old dressing, observe and discard it properly.
- Clean the wound using appropriate solution and technique:
- From center to periphery (least to most contaminated)
- One swab per stroke rule
- Apply correct dressing material as per wound type (e.g., hydrocolloid, alginate, gauze).
- Secure the dressing using tape or bandage without restricting circulation.
- Minimize pain and discomfort by working gently and efficiently.
4. Infection Control Role
- Follow standard infection prevention protocols.
- Use sterile gloves, dressing kits, and disinfectants.
- Ensure proper disposal of used materials in biomedical waste containers.
- Prevent cross-contamination by not touching clean areas with used items.
- Educate the patient about signs of infection and when to seek help.
5. Pain Management and Comfort
- Administer prescribed analgesics before dressing if wound is painful.
- Provide emotional support and reassurance during the procedure.
- Use gentle handling and appropriate non-pharmacological comfort measures (distraction, breathing techniques).
6. Documentation Role
- Record in the nurse’s notes or wound chart:
- Date and time of dressing
- Wound condition (size, color, drainage, signs of healing/infection)
- Type of dressing material used
- Patient’s response to the procedure
- Any instructions given or abnormalities observed
7. Educational Role
- Instruct the patient/family on:
- How to care for the wound at home
- Importance of hand hygiene and dressing changes
- Nutritional needs to support healing (e.g., protein, vitamins)
- Follow-up appointments and wound reassessment
- Early signs of complications (infection, bleeding, reopening)
8. Collaborative Role
- Collaborate with the physician, wound care specialist, and dietician.
- Report any worsening condition or delay in healing.
- Participate in multidisciplinary wound management teams when needed.
Preoperative Care of Surgical Patient
Introduction
Preoperative care refers to all the physical, psychological, and educational preparation provided to a patient before undergoing surgery. It begins from the time the surgery is planned until the patient is transferred to the operating room. Effective preoperative care helps:
- Reduce anxiety and fear
- Prevent complications
- Improve surgical outcomes
- Promote faster recovery
Objectives of Preoperative Care
- To prepare the patient physically and emotionally for surgery
- To identify and minimize surgical risks
- To promote understanding and cooperation
- To ensure all pre-surgical requirements are met (consent, labs, etc.)
1. Physical Preparation
A. Personal Hygiene and Skin Preparation
- Instruct patient to take a bath or shower with antiseptic soap
- Shave or clip hair at the surgical site (as per protocol)
- Remove nail polish, makeup, jewelry, dentures, contact lenses
B. Bowel Preparation
- For abdominal or pelvic surgery, enema or laxative may be given
- Ensure bowel is empty to avoid contamination during surgery
C. Fasting (NPO Status)
- Patient is usually kept nil by mouth for 6–8 hours before surgery to prevent aspiration
- Document and monitor NPO status
D. Bladder Emptying
- Ask the patient to void urine before surgery
- Insert a catheter if ordered (especially in long or abdominal surgeries)
E. Vital Signs Monitoring
- Record temperature, pulse, respiration, and blood pressure
- Notify surgeon/anesthetist of any abnormalities
2. Psychological Preparation
A. Reduce Anxiety and Fear
- Talk to the patient calmly
- Provide emotional support and reassurance
- Allow the patient to express fears and ask questions
B. Preoperative Teaching
- Explain the surgical procedure (as much as allowed)
- Inform about pre-op and post-op routines (fasting, anesthesia, pain, breathing exercises)
- Teach deep breathing, coughing, and leg exercises to prevent complications
3. Legal and Administrative Preparation
A. Informed Consent
- Ensure patient/legal guardian signs the informed consent form
- Verify that the patient understands the procedure, risks, and alternatives
- Witness the signature as a nurse (as per hospital policy)
B. Identification and Documentation
- Confirm patient identity (ID band, name, age, operation details)
- Complete nursing assessment forms and checklist
- Ensure availability of:
- Lab reports
- ECG/X-ray
- Blood availability (cross-match if needed)
4. Preoperative Medications
- Administer pre-op medications as prescribed:
- Sedatives or anti-anxiety drugs (e.g., diazepam)
- Anticholinergics to reduce secretions (e.g., atropine)
- Antibiotics to prevent infection
- Explain the purpose and monitor for reactions
5. Other Essential Preoperative Tasks
| Task | Purpose |
|---|---|
| Removal of prostheses (dentures, hearing aids) | Prevent injury or obstruction |
| Proper surgical gown/drape | Maintain sterility and comfort |
| Check allergy history | Avoid allergic reactions to anesthesia or drugs |
| Secure valuables | Ensure patient belongings are safe |
| Escort to the operation theatre | Ensure safe transfer |
Nurse’s Role in Preoperative Care
- Perform complete physical and psychological assessment
- Prepare the patient physically (bathing, shaving, fasting, etc.)
- Communicate clearly and provide emotional support
- Ensure all documents and reports are completed
- Coordinate with surgical and anesthesia teams
- Provide education on what to expect before and after surgery
- Monitor for changes in patient condition before surgery
Postoperative Care of Surgical Patient
Introduction
Postoperative care refers to the care given to a patient after a surgical procedure, starting from the moment the patient leaves the operating room until full recovery. The goal is to ensure safe recovery, early detection of complications, pain control, wound healing, and patient education.
Nurses play a critical role in the monitoring, support, and rehabilitation of postoperative patients.
Objectives of Postoperative Care
- Monitor the patient’s recovery from anesthesia and surgery
- Detect and prevent complications
- Promote healing and comfort
- Maintain fluid, electrolyte, and respiratory balance
- Educate the patient for home care and rehabilitation
Phases of Postoperative Care
- Immediate Postoperative Phase (PACU or recovery room)
- Intermediate Postoperative Phase (first 24–72 hours in the ward)
- Extended Postoperative Phase (until discharge and home care)
1. Immediate Postoperative Care (PACU/Recovery Room)
A. Airway, Breathing, Circulation (ABC)
- Ensure patent airway (oral/nasal airway or oxygen support)
- Monitor respiratory rate, depth, oxygen saturation
- Assess circulation: pulse, BP, skin color, temperature
B. Monitor Vital Signs
- Every 15 mins × 1 hour → 30 mins × 2 hours → hourly, then as ordered
C. Consciousness and Neurological Response
- Use Glasgow Coma Scale (GCS) if needed
- Check response to verbal command, limb movements
D. Pain Assessment and Management
- Use pain scale (e.g., 0–10)
- Administer prescribed analgesics or PCA (Patient-Controlled Analgesia)
E. Monitor Surgical Site
- Check dressing for bleeding, discharge, or swelling
- Note drain output if present (e.g., Hemovac, Jackson-Pratt)
2. Intermediate/Postoperative Care in the Ward
A. Respiratory Care
- Encourage deep breathing, coughing, incentive spirometry
- Monitor for signs of atelectasis or pneumonia
- Turn patient every 2 hours to prevent hypostatic pneumonia
B. Cardiovascular Monitoring
- Check BP, pulse, skin color regularly
- Monitor for signs of shock, hemorrhage, or DVT
- Apply anti-embolism stockings or pneumatic devices as ordered
C. Pain and Comfort Measures
- Continue analgesic schedule
- Maintain comfortable position and environment
- Support incision during coughing (splinting)
D. Gastrointestinal Care
- Monitor bowel sounds and flatus
- Begin oral fluids only after bowel sounds return
- Watch for signs of nausea, vomiting, constipation, or ileus
E. Urinary Care
- Monitor urine output (should be ≥30 mL/hour)
- Assist with voiding or manage urinary catheter
- Report signs of retention or infection
F. Wound Care
- Inspect wound site for redness, swelling, pus, bleeding
- Change dressing using aseptic technique
- Monitor drain output (color, amount, type)
G. Mobilization and Exercise
- Encourage early ambulation (as per doctor’s advice)
- Prevent complications like DVT, constipation, pneumonia
- Assist with leg exercises, dangling, walking
3. Discharge Planning and Patient Education
A. Educate the Patient On:
- Wound care and signs of infection
- Medication schedule
- Importance of hydration, nutrition, and rest
- Resuming daily activities gradually
- Follow-up appointments
- When to seek medical attention (e.g., fever, heavy bleeding, shortness of breath)
Common Postoperative Complications to Monitor
| Complication | Signs/Symptoms |
|---|---|
| Hemorrhage | Drop in BP, increased HR, wound bleeding |
| Shock | Cold, clammy skin, hypotension, weak pulse |
| Infection | Fever, redness, pus, elevated WBC count |
| Deep Vein Thrombosis (DVT) | Leg swelling, pain, redness |
| Pulmonary embolism | Chest pain, dyspnea, cyanosis |
| Urinary retention | Inability to urinate, bladder distension |
| Constipation/Paralytic ileus | Absent bowel sounds, bloating |
Nurse’s Role in Postoperative Care
- Monitor vitals, wound, drains, and overall condition regularly
- Maintain fluid/electrolyte balance
- Administer medications and pain relief
- Encourage early mobility and breathing exercises
- Provide psychological support and reassurance
- Educate the patient and coordinate discharge planning
Role of Nurse in Preoperative Care
Introduction
The preoperative phase is the period before a surgical procedure. During this phase, the nurse plays a crucial role in preparing the patient physically, emotionally, and psychologically for surgery, ensuring safety and reducing the risk of complications.
1. Physical Preparation
A. Skin and Hygiene Care
- Assist the patient with bathing and oral hygiene using antiseptic soap.
- Clip or shave hair at the surgical site as per protocol.
- Remove nail polish, makeup, jewelry, dentures, hearing aids, etc.
B. Bowel and Bladder Preparation
- Administer enema or laxatives if ordered.
- Ensure the patient has emptied the bladder before surgery.
- Insert a urinary catheter if prescribed.
C. Nutrition and Fasting (NPO)
- Enforce nil by mouth (NPO) status as ordered (usually 6–8 hours before surgery).
- Educate the patient about the importance of fasting.
D. Vital Signs Monitoring
- Record temperature, pulse, respiration, and blood pressure.
- Report any abnormalities to the surgeon or anesthetist.
2. Psychological Preparation
A. Emotional Support
- Talk calmly to the patient and offer reassurance.
- Listen to fears and concerns without judgment.
- Provide spiritual or family support if needed.
B. Preoperative Teaching
- Explain:
- What will happen before, during, and after surgery.
- Importance of deep breathing, coughing, and leg exercises.
- Expected pain and its management.
📌 Proper education reduces anxiety and improves cooperation post-surgery.
3. Legal and Administrative Responsibilities
A. Informed Consent
- Ensure that informed consent has been obtained and signed.
- Verify that the patient or legal guardian understands the procedure.
- Witness the signature if required by hospital policy.
B. Identification and Verification
- Confirm:
- Patient name, age, ID band
- Surgical procedure and site
- Ensure surgical checklist is complete.
C. Availability of Reports
- Ensure presence of:
- Blood reports, ECG, chest X-ray
- Crossmatched blood units (if needed)
4. Preoperative Medications
- Administer prescribed pre-op medications:
- Sedatives (to reduce anxiety)
- Anticholinergics (to reduce secretions)
- Antibiotics (to prevent infection)
- Observe for allergic reactions or side effects.
5. Coordination and Communication
- Communicate with surgical, anesthesia, and diagnostic departments.
- Coordinate investigations, transport, and special instructions.
- Inform family about surgical timing and updates.
6. Documentation
- Record:
- Completion of pre-op checklist
- Medication administration
- Patient education given
- Consent verification
- Vitals and physical status
Role of Nurse in Postoperative Care
✅ Introduction
Postoperative care begins immediately after surgery and continues until the patient has fully recovered. The nurse plays a vital role in monitoring, supporting, and rehabilitating the patient, preventing complications, managing pain, and promoting recovery.
🔷 1. Immediate Postoperative Care (PACU/Recovery Room)
✅ A. Airway, Breathing, and Circulation (ABC)
- Ensure patent airway (position, oxygen therapy, suction if needed)
- Monitor respiratory rate, oxygen saturation, breath sounds
- Check pulse, blood pressure, skin color, and temperature
- Watch for signs of shock, hemorrhage, or respiratory distress
✅ B. Level of Consciousness
- Assess neurological status and response to stimuli
- Use the Glasgow Coma Scale if needed
- Monitor return from anesthesia
✅ C. Pain Management
- Assess pain using pain scale (0–10)
- Administer prescribed analgesics or sedatives
- Provide comfort measures like positioning and reassurance
✅ D. Monitoring Surgical Site and Dressings
- Inspect for bleeding, swelling, or discharge
- Check and manage surgical drains or catheters
- Reinforce or change dressings using aseptic technique
🔷 2. Ongoing Postoperative Care (Ward/ICU)
✅ A. Vital Signs Monitoring
- Monitor temperature, pulse, BP, and respiration frequently
- Watch for fever, hypotension, tachycardia, or hypoxia
✅ B. Respiratory Support
- Encourage deep breathing and coughing exercises
- Use incentive spirometry
- Monitor for signs of atelectasis or pneumonia
✅ C. Fluid and Electrolyte Balance
- Monitor IV fluids and intake/output chart
- Watch for dehydration, fluid overload, or electrolyte imbalances
- Report urine output less than 30 mL/hour
✅ D. Gastrointestinal Care
- Monitor bowel sounds and abdominal distension
- Start oral fluids when bowel sounds return
- Prevent nausea, vomiting, constipation, or paralytic ileus
✅ E. Urinary Care
- Assist with voiding or manage urinary catheter
- Monitor for retention or urinary tract infection
✅ F. Wound Care
- Assess wound for infection signs: redness, heat, discharge, foul odor
- Change dressings as per protocol
- Record drain output (color, amount, consistency)
✅ G. Mobility and Early Ambulation
- Encourage movement and ambulation as soon as possible
- Perform leg exercises and help with position changes
- Prevent DVT, bedsores, and pneumonia
🔷 3. Psychosocial and Emotional Support
- Offer emotional reassurance and reduce anxiety
- Explain procedures and progress to the patient
- Encourage family involvement and communication
- Address fear, confusion, or post-op depression
🔷 4. Patient Education
- Teach about wound care, medications, and physical activity
- Educate on nutrition for healing (high protein, vitamins, fluids)
- Instruct on signs of complications (fever, bleeding, infection)
- Explain discharge instructions and follow-up care
🔷 5. Documentation
- Record:
- Vital signs and pain level
- Wound status and dressing changes
- Medications given and patient response
- Intake/output and drain status
- Teaching provided and patient understanding
🏥 Immediate Postoperative Care
✅ Introduction
Immediate postoperative care refers to the care given to a patient immediately after surgery, usually in the Post Anesthesia Care Unit (PACU) or recovery room. This critical period lasts for the first 1–4 hours post-surgery, and the main goal is to stabilize the patient, manage recovery from anesthesia, and detect life-threatening complications early.
🎯 Objectives of Immediate Postoperative Care
- Ensure airway patency and adequate breathing
- Maintain circulation and hemodynamic stability
- Relieve pain and discomfort
- Monitor for postoperative complications
- Support safe transition to the surgical ward
🔷 Key Components of Immediate Postoperative Care
🔸 1. Airway, Breathing, and Oxygenation (ABO)
- Check airway patency: Ensure tongue, secretions, or vomit is not obstructing.
- Position the patient: Lateral or semi-Fowler’s to prevent aspiration.
- Assess respiratory rate, depth, rhythm.
- Auscultate breath sounds.
- Monitor oxygen saturation (SpO₂).
- Administer oxygen therapy as prescribed.
🔸 2. Circulatory Status
- Monitor pulse, blood pressure, and heart rate frequently (every 15 minutes).
- Observe skin color, warmth, and capillary refill.
- Check for signs of shock or hemorrhage:
- Pale or cold skin
- Rapid, thready pulse
- Low blood pressure
- Increased bleeding at the surgical site
- Monitor IV fluids, rate, and site for patency.
🔸 3. Level of Consciousness and Neurological Assessment
- Assess for return of consciousness and orientation.
- Check response to verbal and painful stimuli.
- Use the Glasgow Coma Scale (GCS) if necessary.
- Monitor pupil reaction and limb movement.
🔸 4. Pain Management
- Ask about pain level using numeric pain scale (0–10).
- Administer prescribed analgesics, including PCA (Patient-Controlled Analgesia) if applicable.
- Use non-pharmacological comfort measures (positioning, reassurance).
🔸 5. Surgical Site Monitoring
- Inspect dressing for:
- Bleeding or drainage
- Soakage or loosening
- Check drain output (Hemovac, Jackson-Pratt, etc.): type, color, amount.
- Maintain aseptic precautions when handling wounds or drains.
🔸 6. Temperature Regulation
- Monitor for hypothermia or fever.
- Use warm blankets or warming devices if patient is cold.
- Observe for shivering, which increases oxygen demand.
🔸 7. Urine Output and Elimination
- Check for urinary output via catheter (should be ≥30 mL/hour).
- Monitor for urinary retention or bleeding.
- Document bowel sounds if abdominal surgery was performed.
🔸 8. Nausea, Vomiting, and Aspiration Prevention
- Monitor for nausea and vomiting due to anesthesia.
- Administer antiemetics if ordered.
- Keep suction equipment ready at bedside.
🔸 9. Emotional Reassurance
- Orient the patient to time, place, and surroundings.
- Reassure about safety and that the surgery is over.
- Allow family communication when appropriate.
🧾 Documentation in Immediate Postoperative Care
- Time of arrival in PACU
- Vital signs trends
- Pain score and analgesics given
- Oxygen saturation and respiratory status
- IV fluid and urine output
- Dressing and drain status
- Any adverse reactions or complications
- Time and condition on transfer to ward
🔴 Common Complications to Monitor
| Complication | Signs to Watch For |
|---|---|
| Airway obstruction | Noisy breathing, cyanosis |
| Hemorrhage | Hypotension, rapid pulse, wound soakage |
| Shock | Cold, clammy skin, restlessness |
| Nausea/Vomiting | Vomiting, retching, risk of aspiration |
| Hypothermia | Shivering, low body temp |
| Pain | High pain score, restlessness |
✅ Conclusion
Immediate postoperative care is critical for patient safety and successful recovery. Nurses in the recovery room must be highly vigilant, skilled, and quick to respond to any sign of distress. Monitoring ABCs (Airway, Breathing, Circulation), pain, consciousness, and wound status is key to preventing complications and ensuring a smooth transition to the next phase of care.
🌿 Alternative Therapies Used in Caring for Patients with Medical-Surgical Disorders
✅ Introduction
Alternative therapies, also referred to as complementary or integrative therapies, are non-conventional treatment approaches used alongside or instead of standard medical care. In medical-surgical settings, these therapies aim to reduce pain, anxiety, stress, and promote overall well-being, enhancing recovery and patient satisfaction.
Nurses often play a key role in educating, administering, or referring patients to appropriate alternative therapies.
🔷 Common Alternative Therapies in Medical-Surgical Care
🔸 1. Aromatherapy
- Use of essential oils (lavender, peppermint, eucalyptus) for healing and relaxation.
- Helps in:
- Reducing anxiety and stress before/after surgery
- Managing postoperative nausea
- Improving sleep quality
🔸 2. Massage Therapy
- Manipulation of soft tissues to relieve pain and tension.
- Benefits:
- Reduces muscle stiffness and post-op pain
- Enhances blood circulation and relaxation
- Promotes mobility and comfort in surgical recovery
🔸 3. Music Therapy
- Use of calming or therapeutic music to influence emotional and physical well-being.
- Helps in:
- Lowering pain perception and anxiety
- Distracting from procedures or post-op discomfort
- Improving mood and sleep
🔸 4. Guided Imagery / Visualization
- Patient is guided to imagine soothing and healing mental images.
- Used for:
- Stress and anxiety reduction
- Managing chronic pain or post-surgical discomfort
- Enhancing emotional coping with illness
🔸 5. Relaxation Techniques & Deep Breathing
- Include progressive muscle relaxation, yoga breathing, mindfulness.
- Benefits:
- Reduces postoperative stress response
- Stabilizes heart rate and BP
- Enhances respiratory function, especially after thoracic/abdominal surgery
🔸 6. Acupuncture and Acupressure
- Traditional Chinese medicine technique using fine needles or finger pressure on specific points.
- Benefits:
- Pain relief after orthopedic or abdominal surgeries
- Managing nausea/vomiting post-anesthesia
- Reducing inflammation and spasms
🔸 7. Herbal Medicine
- Use of plant-based substances for healing.
- Examples:
- Aloe vera for skin wounds/burns
- Turmeric (anti-inflammatory)
- Ginger for nausea
⚠️ Always check for interactions with prescribed medications.
🔸 8. Reiki / Therapeutic Touch
- Energy-based healing methods where hands are placed lightly on or above the patient.
- Used for:
- Promoting relaxation and energy balance
- Reducing pain and fatigue
- Supporting emotional well-being
🔸 9. Yoga and Meditation
- Involves gentle physical postures, breathing, and mindfulness.
- Benefits:
- Improves mobility and circulation
- Reduces anxiety, insomnia, and chronic pain
- Supports long-term recovery in cardiac or surgical rehab patients
🔸 10. Homeopathy and Naturopathy
- Use of natural remedies and body’s self-healing capacity.
- Not typically first-line in hospitals but may be used under supervision for long-term support.
🧠 Nurse’s Role in Integrating Alternative Therapies
- Assess patient’s interest and cultural beliefs in alternative therapies
- Educate about safe and evidence-based use of therapies
- Monitor for side effects or interactions with medical treatment
- Collaborate with alternative therapy practitioners as needed
- Document patient response to therapy and changes in symptoms
- Encourage but never force patients to use alternative methods
⚠️ Precautions and Consideration
- Not all alternative therapies are scientifically proven.
- Some may interact with medications or delay recovery if misused.
- Always consult with the physician before initiating certain therapies (especially herbal remedies).
- Respect patient preferences, culture, and autonomy.
FOR UNLOCK 🔓 FULL COURSE NOW. MORE DETAILS CALL US OR WATSAPP ON- 8485976407
