BSC SEM 2 UNIT 1 NURSING FOUNDATION 2
UNIT 1 Hygiene
Hygiene

1. Introduction to Hygiene
Hygiene refers to practices and conditions that help maintain health and prevent the spread of diseases. In nursing, hygiene plays a critical role in patient care, ensuring safety, comfort, and infection control.
2. Importance of Hygiene in Nursing
- Prevention of Infections: Proper hygiene minimizes the risk of nosocomial (hospital-acquired) infections.
- Promotes Comfort: Cleanliness enhances patient comfort and well-being.
- Improves Healing: Wound care hygiene prevents complications.
- Enhances Dignity and Self-Esteem: Especially in dependent patients.
- Ensures Professionalism: Nurses must maintain high hygiene standards in healthcare settings.
3. Types of Hygiene in Nursing
a. Personal Hygiene
- Oral Hygiene: Brushing, flossing, and oral rinses prevent infections.
- Hair Care: Regular washing and combing to prevent lice and dandruff.
- Nail Care: Short and clean nails reduce the risk of bacterial accumulation.
- Hand Hygiene: The most effective way to prevent infections in hospitals.
- Bathing: Includes complete, partial, and therapeutic baths.
- Foot Care: Important for diabetic patients to prevent ulcers.
b. Environmental Hygiene
- Bedside Cleanliness: Ensuring bed linen is clean and dry.
- Waste Disposal: Proper biomedical waste management.
- Air Circulation: Maintaining good ventilation in healthcare settings.
- Surface Cleaning: Disinfecting hospital furniture and equipment.
c. Food Hygiene
- Proper Nutrition Handling: Prevents foodborne illnesses.
- Safe Storage and Preparation: Following proper food safety guidelines.
d. Occupational Hygiene
- Nurse’s Personal Hygiene: Wearing clean uniforms, proper hand washing, and avoiding cross-contamination.
- Protective Measures: Use of gloves, masks, and proper PPE (Personal Protective Equipment).
4. Hygiene Practices in Nursing
a. Hand Hygiene
- Handwashing with Soap and Water: At least 20 seconds.
- Alcohol-Based Hand Sanitizer: Used when hands are not visibly soiled.
- Handwashing Techniques: Follow WHO’s 6-step technique.
b. Bed Bathing
- Types:
- Complete bed bath (for immobilized patients)
- Partial bed bath (focuses on face, hands, underarms, perineal area)
- Therapeutic bath (medicated solutions for skin conditions)
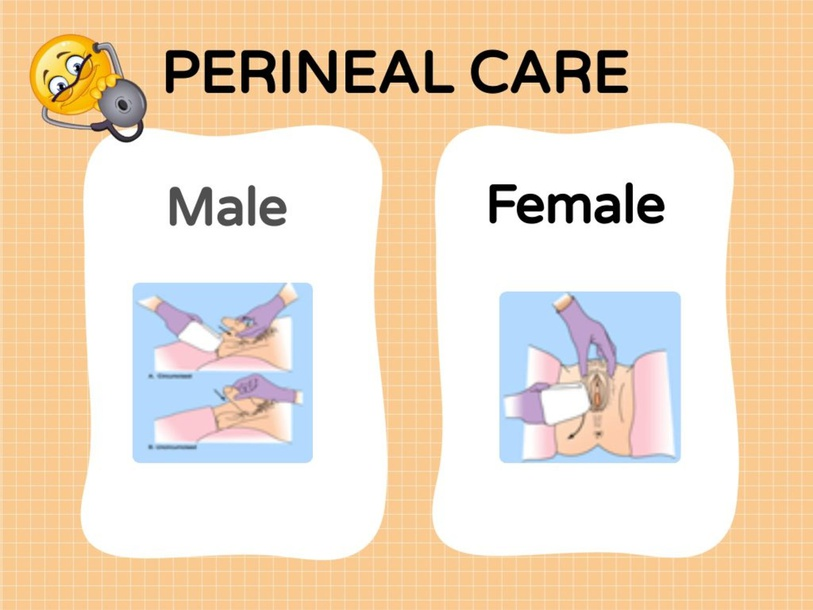
c. Perineal Care
- Importance: Prevents infections, especially in catheterized and postpartum patients.
- Procedure: Use warm water and mild soap, clean front to back for females, and circular motion for males.
d. Oral Care
- For conscious patients: Regular brushing and mouth rinsing.
- For unconscious patients: Use mouth swabs and suction to prevent aspiration.
e. Wound Hygiene
- Aseptic Techniques: Proper cleaning and dressing changes.
- Use of Antiseptics: Betadine, saline solution, or chlorhexidine.
- Sterile Dressing: Prevents secondary infections.
f. Respiratory Hygiene
- Cough Etiquette: Covering mouth with tissue or elbow.
- Use of Masks: For airborne infections.
- Nebulization and Suctioning: Clearing airways for better breathing.
g. Nail and Hair Hygiene
- Short and Clean Nails: Prevents harboring pathogens.
- Hair Care: Regular washing, tied back in clinical settings.
h. Infection Control Measures
- Standard Precautions: Gloves, masks, and gowns in high-risk areas.
- Sterilization and Disinfection: Ensuring instruments are properly cleaned.
- Isolation Techniques: For contagious diseases.
5. Common Hygiene-Related Diseases in Nursing Care
- Nosocomial Infections (HAIs): MRSA, C. difficile, pneumonia, UTIs.
- Skin Infections: Bedsores, fungal infections, dermatitis.
- Gastrointestinal Infections: Food poisoning, diarrhea.
- Respiratory Infections: Tuberculosis, pneumonia.
6. Role of a Nurse in Promoting Hygiene
- Educating Patients: Teaching personal hygiene practices.
- Maintaining Clean Environment: Proper waste disposal and sanitation.
- Adhering to Protocols: Following hand hygiene, PPE, and infection control guidelines.
- Monitoring Patients: Checking for signs of hygiene-related illnesses.
Factors Influencing Hygienic Practice
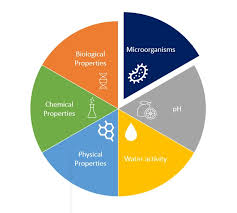
Hygienic practices in nursing are influenced by several factors, which can be broadly categorized into personal, environmental, cultural, psychological, institutional, and economic factors. Understanding these factors helps nurses ensure optimal hygiene standards and improve patient care.
1. Personal Factors
These factors are related to an individual’s awareness, habits, and physical ability.
- Knowledge and Awareness: Nurses and patients must be educated about hygiene and infection prevention.
- Personal Habits: Daily hygiene habits, such as handwashing and bathing, affect overall cleanliness.
- Health Status: Individuals with illnesses, disabilities, or weakened immune systems may require assistance in maintaining hygiene.
- Physical Limitations: Patients with mobility issues, chronic illnesses, or age-related conditions may struggle with personal hygiene.
- Attitude and Motivation: A positive attitude toward hygiene promotes better compliance.
2. Environmental Factors
The surroundings play a crucial role in maintaining hygiene.
- Cleanliness of Healthcare Facilities: Proper sanitation in hospitals prevents infections.
- Water Supply and Quality: Availability of clean water is essential for hand hygiene and patient care.
- Ventilation and Air Quality: Fresh air circulation reduces the spread of airborne infections.
- Sanitation Facilities: Proper waste disposal and clean toilets improve hygiene.
3. Cultural and Social Factors
Different cultures have varying hygiene beliefs and practices.
- Cultural Beliefs and Practices: Some cultures follow traditional hygiene rituals, while others may have restrictions on certain practices.
- Social Norms: The acceptance of hygiene practices is influenced by societal expectations.
- Religious Practices: Some religions have specific hygiene-related customs, such as ritual washing before prayers.
4. Psychological Factors
Mental health and emotional well-being impact hygiene behaviors.
- Cognitive Function: Patients with dementia, Alzheimer’s, or psychiatric disorders may neglect hygiene.
- Depression and Anxiety: Mental health issues can lead to a lack of interest in personal care.
- Fear and Embarrassment: Patients may feel uncomfortable with assisted hygiene care, affecting compliance.
5. Institutional and Policy Factors
Hospitals and healthcare institutions must enforce hygiene policies.
- Hospital Infection Control Policies: Guidelines for hand hygiene, sterilization, and patient care.
- Availability of Hygiene Resources: Access to soap, sanitizers, PPE, and sterile equipment.
- Training and Education: Continuous training of healthcare workers on hygiene best practices.
- Workload and Staffing Levels: Overburdened nurses may struggle to maintain hygiene protocols.
6. Economic Factors
Financial conditions affect hygiene maintenance.
- Affordability of Hygiene Products: Patients in low-income settings may lack access to basic hygiene products.
- Funding for Healthcare Facilities: Proper budget allocation is necessary for sanitation infrastructure.
- Health Insurance Coverage: Insurance policies should include hygiene-related care in hospitals.
7. Technological and Scientific Advances
Modern technology enhances hygiene in healthcare.
- Use of Automated Hand Hygiene Systems: Reduces human errors in hand hygiene compliance.
- Sterilization and Disinfection Technologies: Advanced methods for infection control.
- Electronic Health Records (EHR): Tracking patient hygiene-related conditions and interventions.
8. Climatic and Geographic Factors
Geographical conditions influence hygiene maintenance.
- Hot and Humid Climates: Increase the risk of fungal and bacterial infections.
- Cold Climates: Reduce water availability for hygiene.
- Natural Disasters: Floods, earthquakes, and other disasters affect hygiene infrastructure.
Hygienic Care: Indications and Purposes
Introduction
Hygienic care in nursing refers to a set of practices aimed at maintaining cleanliness, preventing infections, and promoting patient comfort and dignity. It includes activities such as bathing, oral care, perineal care, hair care, hand hygiene, and environmental sanitation. Nurses play a critical role in ensuring proper hygiene for patients, particularly those who are dependent, critically ill, or unable to perform self-care.
Indications for Hygienic Care
Hygienic care is necessary in various healthcare settings and for different patient conditions. The indications for providing hygienic care include:
1. Patients with Limited Mobility
- Bedridden patients (due to paralysis, fractures, or surgery)
- Patients with chronic illnesses affecting movement (e.g., arthritis, stroke)
- Postoperative patients who need assistance with hygiene
2. Critically Ill and ICU Patients
- Patients on ventilators or with tracheostomies
- Unconscious or sedated patients
- Patients with severe infections requiring strict hygiene measures
3. Patients with Neurological or Psychiatric Disorders
- Patients with Alzheimer’s disease, dementia, or Parkinson’s disease
- Psychiatric patients with poor self-care habits
- Patients with depression or severe mental health disorders affecting hygiene
4. Patients with Infectious Diseases
- Patients with skin infections (e.g., fungal infections, scabies)
- Patients with communicable diseases (e.g., tuberculosis, COVID-19)
- Patients requiring isolation precautions to prevent disease transmission
5. Postpartum and Newborn Care
- Mothers requiring perineal hygiene after childbirth
- Neonatal hygiene to prevent infections such as diaper rash or sepsis
- Umbilical cord care in newborns
6. Patients with Wounds, Burns, and Ulcers
- Patients with pressure ulcers, surgical wounds, or diabetic foot ulcers
- Burn victims requiring frequent wound cleansing and dressing
- Patients with catheters or intravenous lines needing sterile hygiene care
7. Geriatric Patients
- Elderly individuals with incontinence issues
- Patients suffering from degenerative diseases affecting hygiene abilities
- Patients with dry skin or other age-related hygiene needs
8. Patients Undergoing Chemotherapy or Immunosuppressive Treatment
- Cancer patients at risk for infections due to weakened immunity
- Patients on long-term corticosteroid therapy
- Transplant recipients requiring strict hygiene protocols
Purposes of Hygienic Care
The main goals of hygienic care in nursing are to promote well-being, prevent infections, and enhance the quality of life. The purposes include:
1. Preventing Infections
- Reducing the risk of hospital-acquired infections (HAIs)
- Preventing cross-contamination among patients and healthcare workers
- Reducing bacterial growth on the skin, mouth, and perineal areas
2. Promoting Comfort and Well-being
- Ensuring patients feel fresh and comfortable
- Reducing body odor and skin irritation
- Enhancing relaxation and promoting better sleep
3. Enhancing Skin Integrity and Circulation
- Preventing bedsores (pressure ulcers) in bedridden patients
- Promoting blood circulation through massage during hygiene care
- Reducing dryness and cracking of skin, preventing infections
4. Maintaining Oral Health
- Preventing oral infections such as thrush and gingivitis
- Reducing the risk of aspiration pneumonia in bedridden patients
- Ensuring oral hygiene in patients with mechanical ventilation
5. Supporting Dignity and Self-Esteem
- Helping patients maintain personal hygiene when they are unable to do so themselves
- Providing respectful and culturally appropriate care
- Promoting independence in hygiene activities where possible
6. Promoting Faster Recovery
- Keeping wounds clean and preventing infections
- Reducing the bacterial load on the skin and mucous membranes
- Preventing complications related to poor hygiene (e.g., UTIs from poor perineal care)
7. Preventing Skin Diseases and Irritations
- Managing excessive sweating and preventing rashes
- Preventing diaper rash and fungal infections in immobile patients
- Ensuring proper foot hygiene in diabetic patients
8. Meeting Basic Human Needs
- Ensuring proper elimination hygiene for patients with catheters or bowel incontinence
- Providing menstrual hygiene support for female patients
- Helping patients feel comfortable in hospital settings
Components of Hygienic Care
Hygienic care involves various activities depending on the patient’s condition:
1. Bathing and Skin Care
- Types of Baths:
- Complete bed bath (for unconscious or bedridden patients)
- Partial bed bath (face, hands, axilla, perineal area)
- Therapeutic bath (medicated solutions for skin conditions)
- Tub bath/shower (for mobile patients)
- Skin Inspection: Checking for rashes, bedsores, and infections
- Massage: Improving blood circulation and preventing pressure ulcers
2. Oral Hygiene
- Brushing teeth and flossing (for conscious patients)
- Using mouth swabs and antiseptic solutions (for unconscious patients)
- Preventing dry mouth in ventilated patients
3. Perineal Hygiene
- Cleaning the genital and anal area to prevent infections
- Necessary for patients with urinary catheters, postpartum mothers, or incontinent patients
- Reduces the risk of UTIs and skin breakdown
4. Hair and Scalp Care
- Regular hair washing and scalp massage
- Checking for lice and dandruff
- Ensuring proper hair hygiene in bedridden patients
5. Nail and Foot Care
- Trimming nails to prevent infections
- Special foot care for diabetic patients to prevent ulcers
- Moisturizing dry and cracked feet
6. Hand Hygiene
- Handwashing with soap and water
- Use of alcohol-based hand sanitizers
- Preventing the spread of infections among patients and healthcare workers
7. Dressing and Clothing Hygiene
- Ensuring patients wear clean, dry clothes
- Changing soiled hospital gowns or personal clothing
- Maintaining dignity by covering patients appropriately
8. Environmental Hygiene
- Keeping the patient’s bed, room, and surroundings clean
- Proper disposal of medical waste and bedpans
- Reducing contamination through sterilization and disinfection
Special Considerations in Hygienic Care
- For Infants and Neonates: Gentle bathing techniques, umbilical cord care
- For Pregnant and Postpartum Women: Perineal hygiene, breast care
- For Elderly Patients: Prevention of bedsores, assistance with hygiene tasks
- For Patients with Communicable Diseases: Infection control precautions, isolation hygiene measures
- For Unconscious Patients: Proper positioning, preventing aspiration during oral care.
Effects of Neglected Hygienic Care in Nursing

Introduction
Neglecting hygienic care in nursing can have severe consequences for both patients and healthcare professionals. Poor hygiene practices can lead to infections, delayed healing, increased morbidity and mortality, and psychological distress. The impact of neglected care extends beyond individual patients to healthcare institutions and public health systems.
Effects of Neglected Hygienic Care
1. Increased Risk of Infections
- Hospital-Acquired Infections (HAIs): Poor hand hygiene, improper wound care, and lack of environmental sanitation contribute to infections such as:
- Methicillin-resistant Staphylococcus aureus (MRSA)
- Clostridium difficile infections
- Catheter-associated urinary tract infections (CAUTIs)
- Ventilator-associated pneumonia (VAP)
- Sepsis: Neglected hygiene in wound care can lead to bloodstream infections.
- Skin Infections: Bedridden patients are at risk of pressure ulcers and fungal infections due to poor skin hygiene.
2. Delayed Wound Healing and Increased Complications
- Lack of proper wound cleaning and dressing changes can lead to:
- Increased bacterial colonization
- Delayed tissue regeneration
- Wound dehiscence (wound reopening)
- Gangrene and the need for amputations in diabetic patients
3. Poor Oral Health Leading to Systemic Complications
- Oral Infections: Neglected oral care leads to gingivitis, dental caries, and periodontitis.
- Aspiration Pneumonia: Bacteria from the oral cavity can enter the lungs, causing pneumonia in bedridden and ventilated patients.
- Malnutrition: Painful oral infections may reduce a patient’s ability to eat, leading to weight loss and malnutrition.
4. Psychological and Emotional Impact
- Loss of Dignity and Self-Esteem: Patients who are unable to maintain hygiene may feel embarrassed and helpless.
- Depression and Anxiety: Poor hygiene can lead to social withdrawal and a decline in mental well-being.
- Discomfort and Irritability: Patients may experience discomfort due to dirty skin, greasy hair, and foul odors.
5. Increased Morbidity and Mortality
- Higher Death Rates: Patients in critical care settings are at higher risk of mortality due to infections caused by poor hygiene.
- Increased ICU Admissions: Complications from infections may require intensive care, increasing the burden on healthcare systems.
- Spread of Epidemics: Lack of hygiene contributes to the spread of infectious diseases such as COVID-19, tuberculosis, and influenza.
6. Poor Skin Integrity and Bedsores
- Pressure Ulcers: Neglected hygiene and prolonged immobility can lead to skin breakdown, increasing the risk of severe pressure ulcers.
- Fungal and Bacterial Infections: Moisture retention due to infrequent bathing and poor perineal care leads to infections like candidiasis and dermatitis.
7. Gastrointestinal Issues and Malnutrition
- Foodborne Infections: Poor hand hygiene among healthcare workers and improper food handling can lead to gastrointestinal infections.
- Malnutrition: Patients unable to maintain oral hygiene may refuse to eat, leading to nutritional deficiencies.
8. Increased Healthcare Costs
- Extended Hospital Stays: Infections and complications require longer treatment durations, increasing medical costs.
- Additional Medications and Procedures: Neglected hygiene may lead to the need for expensive antibiotics, wound debridement, and surgeries.
- Legal and Ethical Issues: Healthcare facilities may face lawsuits and penalties for failing to maintain hygiene standards.
9. Negative Impact on Healthcare Workers
- Burnout and Stress: Nurses dealing with hygiene-related infections face increased workload and stress.
- Occupational Hazards: Poor hygiene increases the risk of infections among healthcare providers.
Care of the Skin and Bathing
Introduction
Skin care and bathing are essential components of nursing care that help maintain personal hygiene, prevent infections, and promote comfort. The skin is the body’s first line of defense against infections, and maintaining its integrity is crucial for overall health. Bathing serves not only as a cleansing activity but also as an opportunity for nurses to assess the patient’s skin condition and provide therapeutic care.
1. Importance of Skin Care in Nursing
- Prevents infections by removing dirt, bacteria, and dead skin cells.
- Enhances circulation through gentle massage during bathing.
- Prevents pressure ulcers in bedridden or immobile patients.
- Promotes comfort by reducing body odor and refreshing the patient.
- Maintains skin integrity by keeping it clean, hydrated, and free from irritants.
2. Structure and Functions of the Skin
Structure of the Skin
The skin consists of three layers:
- Epidermis – The outermost layer that provides a barrier against microbes and regulates water loss.
- Dermis – Contains blood vessels, nerve endings, and hair follicles.
- Hypodermis (Subcutaneous layer) – Composed of fat and connective tissues that provide insulation.
Functions of the Skin
- Protection against infections, injuries, and UV radiation.
- Regulation of body temperature through sweat glands.
- Sensory perception for touch, pain, and temperature.
- Synthesis of vitamin D.
- Excretion of waste through sweat.
3. General Principles of Skin Care
- Use mild soap and warm water to avoid irritation.
- Moisturize the skin to prevent dryness and cracking.
- Maintain proper nutrition and hydration for healthy skin.
- Regular repositioning to prevent pressure ulcers in immobile patients.
- Use of barrier creams for incontinent patients to prevent skin breakdown.
- Observe and assess the skin for any redness, wounds, or infections.
4. Bathing in Nursing
Definition
Bathing is the process of cleansing the body to maintain hygiene, promote comfort, and stimulate circulation. It can be performed by the patient or assisted by the nurse, depending on the patient’s condition.
Types of Baths
1. Complete Bed Bath
- Given to totally dependent patients who cannot bathe themselves.
- Includes washing the entire body while the patient remains in bed.
2. Partial Bed Bath
- Involves cleaning only specific body parts (face, hands, axilla, perineal area).
- Suitable for patients who can wash some areas but need assistance with others.
3. Sponge Bath
- A towel soaked in warm water is used to clean the patient.
- Often used for fever management to reduce body temperature.
4. Therapeutic Bath
- Given for medical purposes, such as treating skin conditions or muscle pain.
- Types:
- Sitz bath – Used for perineal or rectal conditions.
- Oatmeal or medicated bath – Used for skin diseases like eczema or psoriasis.
5. Tub Bath or Shower
- Suitable for mobile patients who can stand or sit safely in a tub or under a shower.
- Water temperature should be 37°C to 43°C (98.6°F to 109.4°F) to prevent burns.
5. Steps for Providing a Bed Bath
Preparation
- Explain the procedure to the patient.
- Gather all necessary supplies (soap, water, washcloth, towels, clean clothes).
- Maintain privacy using curtains or screens.
- Ensure room temperature is comfortable.
- Use warm water (not too hot or cold).
Procedure
- Wash hands and wear gloves.
- Start with the face – Use a clean washcloth, avoiding soap near the eyes.
- Clean arms and hands – Wash from the cleanest to the dirtiest areas.
- Wash the chest and abdomen – Use gentle circular motions.
- Clean the legs and feet – Pay attention to between the toes.
- Provide perineal care – Use a separate washcloth to prevent cross-contamination.
- Turn the patient and clean the back and buttocks.
- Dry the skin properly to prevent moisture-related infections.
- Apply lotion or barrier cream if needed.
- Change bed linens and dress the patient in clean clothes.
- Dispose of used items properly and wash hands.
- Document the procedure and report any skin abnormalities.
6. Special Considerations in Bathing
- Elderly patients: Use lukewarm water and mild soap to avoid skin dryness.
- Newborns: Use gentle bathing techniques and maintain warmth.
- Postoperative patients: Avoid getting surgical sites wet unless instructed.
- Patients with wounds: Use antiseptic solutions if required.
- Unconscious patients: Take extra care to prevent aspiration of water.
7. Common Skin Problems and Prevention
| Skin Condition | Cause | Prevention/Treatment |
|---|---|---|
| Pressure ulcers | Prolonged pressure on the skin | Frequent repositioning, use of pressure-relieving mattresses |
| Dry skin (Xerosis) | Aging, dehydration | Apply moisturizer, drink water |
| Rashes | Allergies, infections | Use hypoallergenic products |
| Fungal infections | Warm, moist conditions | Keep skin dry, use antifungal powders |
| Bedsores | Poor hygiene, immobility | Regular turning and hygiene maintenance |
8. Psychological Benefits of Bathing
- Promotes relaxation and relieves stress.
- Enhances self-esteem and confidence.
- Provides a sense of normalcy and dignity to patients.
- Creates an opportunity for nurses to engage in therapeutic communication.
9. Infection Control Measures During Bathing
- Use gloves to prevent cross-contamination.
- Follow hand hygiene before and after the procedure.
- Use separate washcloths for the face and perineal areas.
- Dispose of used materials properly.
- Maintain aseptic techniques for wound care.
10. Documentation and Reporting
After providing skin care or bathing, the nurse must document:
- Type of bath given.
- Condition of the patient’s skin (redness, wounds, dryness).
- Any abnormalities observed (rashes, pressure ulcers, infections).
- The patient’s response to the bath.
- Any interventions required (moisturizing, wound dressing).
Feet and Nail Care

Introduction
Feet and nail care is an essential component of personal hygiene and nursing care. Proper care of the feet and nails helps prevent infections, maintains mobility, and enhances patient comfort. Special attention is required for high-risk patients such as diabetics, elderly individuals, and bedridden patients, who are prone to foot ulcers, infections, and other complications.
1. Importance of Feet and Nail Care in Nursing
- Prevents infections such as fungal infections, ingrown nails, and ulcers.
- Improves circulation through massage and proper hygiene.
- Prevents foot complications in diabetic patients and those with poor circulation.
- Enhances mobility and comfort by reducing pain and discomfort.
- Promotes overall hygiene and self-esteem for patients.
2. Anatomy of the Feet and Nails
Structure of the Feet
- Bones: 26 bones support body weight.
- Muscles and Ligaments: Provide movement and flexibility.
- Skin and Nails: Protect the feet from external damage.
Structure of the Nails
- Nail Plate: The visible hard part of the nail.
- Nail Bed: The tissue underneath the nail plate.
- Cuticle: Protects the new nail from infections.
- Lunula: The white, crescent-shaped part of the nail.
3. Principles of Feet and Nail Care
- Use proper hygiene practices to prevent infections.
- Avoid cutting nails too short to prevent ingrown nails.
- Moisturize the feet but avoid excessive moisture between toes to prevent fungal infections.
- Wear appropriate footwear to prevent pressure sores and calluses.
- Inspect feet regularly for any signs of infection, ulcers, or injuries.
4. Steps for Providing Feet and Nail Care
Preparation
- Explain the procedure to the patient.
- Gather supplies: warm water, mild soap, towel, nail clipper, file, lotion, and gloves.
- Ensure a comfortable and private setting.
- Position the patient properly (seated or lying with feet elevated).
Procedure
- Wash hands and wear gloves.
- Soak the feet in warm water for 10–15 minutes to soften skin and nails.
- Clean the feet with mild soap, paying attention to the areas between the toes.
- Dry thoroughly, especially between the toes.
- Inspect the feet and nails for any redness, sores, or infections.
- Trim nails straight across to prevent ingrown nails (avoid cutting too deep).
- File rough edges to smooth the nails.
- Apply moisturizer to the feet but avoid the space between the toes.
- Massage the feet gently to improve circulation.
- Encourage the patient to wear clean socks and well-fitted shoes.
- Dispose of used items properly and wash hands.
- Document the procedure and findings (e.g., abnormalities like cuts, ulcers, or infections).
5. Special Considerations in Feet and Nail Care
For Diabetic Patients
- Never cut nails too short—risk of slow healing.
- Regularly check for cuts, blisters, or ulcers.
- Avoid walking barefoot to prevent injuries.
- Use mild soap and lukewarm water to prevent skin damage.
For Elderly Patients
- Skin tends to be dry—use moisturizer.
- Nails may be thickened—use proper trimming tools.
- Watch for pressure sores on the heels.
For Bedridden Patients
- Reposition frequently to avoid pressure ulcers on heels.
- Massage to promote circulation.
- Keep feet elevated to reduce swelling.
6. Common Feet and Nail Problems
| Condition | Cause | Prevention/Treatment |
|---|---|---|
| Ingrown Nails | Improper nail trimming, tight shoes | Cut nails straight, wear proper footwear |
| Fungal Infections (Athlete’s Foot) | Moisture, poor hygiene | Keep feet dry, use antifungal powder |
| Corns and Calluses | Pressure, friction | Wear comfortable shoes, use padding |
| Cracked Heels | Dry skin, poor hydration | Apply moisturizer, avoid walking barefoot |
| Foot Ulcers | Poor circulation (especially in diabetes) | Regular foot checks, use diabetic footwear |
| Toenail Fungus | Fungal infections, poor hygiene | Antifungal treatment, proper nail care |
7. Infection Control Measures During Feet and Nail Care
- Use gloves to prevent cross-contamination.
- Sanitize nail clippers and foot care tools before and after use.
- Dispose of used materials properly.
- Maintain hand hygiene before and after the procedure.
8. Patient Education on Feet and Nail Care
- Wash and dry feet daily.
- Trim nails straight across and file sharp edges.
- Moisturize feet but avoid excessive moisture between toes.
- Wear breathable socks and well-fitted shoes.
- Avoid walking barefoot to prevent injuries and infections.
- Seek medical attention for wounds, discoloration, or pain in the feet.
9. Documentation and Reporting
- Condition of feet and nails before care.
- Any abnormalities observed (e.g., ulcers, fungal infections).
- Type of care provided (trimming, moisturizing, massage).
- Patient’s response to care.
- Recommendations or referrals if needed.
Hair Care

Introduction
Hair care is an important aspect of personal hygiene and nursing care, contributing to cleanliness, comfort, and overall well-being. Proper hair care prevents scalp infections, promotes blood circulation, and enhances self-esteem. In a healthcare setting, nurses provide hair care to patients who are unable to maintain it themselves due to illness, immobility, or hospitalization.
1. Importance of Hair Care in Nursing
- Maintains scalp hygiene by removing dirt, oil, and bacteria.
- Prevents scalp infections such as dandruff, lice infestation, and fungal infections.
- Improves blood circulation to the scalp through massaging.
- Enhances patient comfort and dignity by promoting cleanliness.
- Prevents hair tangling and matting, especially in bedridden patients.
- Allows for assessment of scalp conditions, such as wounds, dryness, or infestations.
2. Anatomy of Hair and Scalp
Structure of Hair
- Hair Shaft: The visible part of the hair.
- Hair Follicle: The structure in the scalp where hair grows.
- Sebaceous Glands: Produce oil (sebum) to moisturize the hair and scalp.
- Hair Root and Papilla: Located under the skin, responsible for hair growth.
Functions of Hair
- Protects the scalp from environmental damage.
- Helps in temperature regulation.
- Acts as a sensory organ due to nerve endings in the follicles.
3. General Principles of Hair Care
- Use mild shampoo to avoid scalp irritation.
- Comb hair gently and regularly to prevent tangles.
- Ensure scalp massage to improve blood circulation.
- Dry hair properly after washing to prevent fungal growth.
- Observe for scalp conditions such as dandruff, lice, or infections.
4. Indications for Hair Care in Nursing
Hair care is provided in the following situations:
- Patients who are bedridden due to illness, surgery, or immobility.
- Critically ill patients in ICUs, especially those on ventilators.
- Elderly patients who have difficulty maintaining hair hygiene.
- Postoperative patients who are unable to move freely.
- Patients with skin or scalp conditions requiring special treatment.
- Patients with long-term hospitalization to prevent hygiene-related issues.
5. Steps for Providing Hair Care
Preparation
- Explain the procedure to the patient.
- Gather supplies: Shampoo, conditioner, towel, comb, brush, gloves, and a basin (if washing in bed).
- Maintain privacy using curtains or screens.
- Ensure the patient is in a comfortable position (sitting, lying, or supported in bed).
Procedure for Hair Washing in Bed
- Wash hands and wear gloves.
- Protect the bed with a waterproof sheet.
- Position the patient with head slightly lowered over a basin.
- Wet the hair using lukewarm water.
- Apply mild shampoo and gently massage the scalp.
- Rinse thoroughly to remove all shampoo.
- Apply conditioner if needed and rinse.
- Towel-dry the hair by patting, not rubbing.
- Comb and detangle the hair using a wide-toothed comb.
- Style as preferred or tie the hair neatly.
- Dispose of used materials properly and wash hands.
- Document the procedure and any scalp conditions observed.
Procedure for Combing and Brushing Hair
- Use a wide-tooth comb for tangled hair.
- Start from the ends and move upwards to avoid pulling.
- Apply hair oil or moisturizer if needed for dry hair.
- Tie or braid hair to prevent tangling in bedridden patients.
6. Special Considerations in Hair Care
For Bedridden Patients
- Wash hair only when necessary (e.g., every few days).
- Use a dry shampoo alternative when regular washing is not possible.
- Keep hair neatly tied to prevent matting.
For Elderly Patients
- Avoid excessive washing to prevent dryness.
- Use a scalp moisturizer for flaky or dry scalp.
- Be gentle with combing to avoid hair breakage.
For Patients with Lice or Scalp Infections
- Use medicated shampoos as prescribed.
- Isolate personal hair care items to prevent spread.
- Report infestations for further medical treatment.
For Postoperative Patients
- Avoid washing the hair if the surgical wound is near the head.
- Use wet wipes or dry shampoo if necessary.
- Ensure proper positioning to avoid discomfort.
7. Common Scalp and Hair Problems
| Condition | Cause | Prevention/Treatment |
|---|---|---|
| Dandruff | Dry scalp, fungal infection | Use anti-dandruff shampoo, moisturize scalp |
| Lice infestation | Poor hygiene, close contact | Medicated shampoo, avoid sharing combs |
| Fungal infections | Moisture retention, poor hygiene | Keep scalp dry, use antifungal treatment |
| Hair tangling and matting | Lack of combing in bedridden patients | Regular combing and hair tying |
| Alopecia (Hair loss) | Illness, stress, medications | Maintain good nutrition, scalp massage |
8. Infection Control Measures During Hair Care
- Use gloves when dealing with scalp infections or lice.
- Disinfect combs and brushes after each use.
- Use separate towels and hair care items for each patient.
- Dispose of hair clippings and used materials properly.
- Follow standard hand hygiene protocols.
9. Psychological Benefits of Hair Care
- Enhances self-esteem and confidence in patients.
- Promotes relaxation and comfort through scalp massage.
- Provides a sense of normalcy and well-being.
- Encourages therapeutic communication between nurses and patients.
10. Documentation and Reporting
- Condition of the scalp and hair before and after care.
- Any abnormalities observed (e.g., lice, dandruff, infections).
- Type of hair care provided (washing, combing, oiling).
- Patient’s response to hair care.
- Recommendations for further treatment if necessary.
Care of Pressure Points
Introduction
Pressure points are specific areas of the body where bones are close to the skin, making them vulnerable to pressure-related injuries. These areas are at a higher risk for developing pressure ulcers (bedsores or decubitus ulcers) due to prolonged pressure, friction, and moisture. Nursing care focuses on preventing pressure ulcers through proper skin care, repositioning, and maintaining adequate circulation.
1. Importance of Pressure Point Care
- Prevents pressure ulcers that can lead to infections and complications.
- Reduces pain and discomfort in immobile patients.
- Improves circulation and prevents ischemia (lack of blood supply).
- Enhances mobility and recovery in bedridden patients.
- Reduces hospital stay and healthcare costs associated with ulcer treatment.
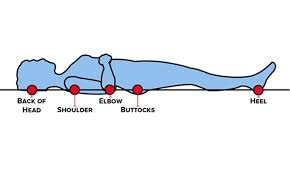
2. Common Pressure Points in the Body
Pressure ulcers commonly develop in areas where there is prolonged pressure against a surface. These areas vary depending on the patient’s position.
Pressure Points in Different Positions
| Position | Common Pressure Points |
|---|---|
| Supine (Lying on Back) | Occiput (back of the head), scapulae (shoulder blades), elbows, sacrum, heels |
| Prone (Lying on Stomach) | Forehead, chin, chest, elbows, knees, toes |
| Side-Lying (Lateral Position) | Ears, shoulders, ribs, hips, knees, ankles |
| Sitting Position | Ischial tuberosities (buttocks), sacrum, coccyx, heels |
3. Factors Contributing to Pressure Ulcers
- Prolonged immobility (paralysis, unconsciousness, post-surgery).
- Poor nutrition and hydration leading to weak skin integrity.
- Moisture and incontinence causing skin breakdown.
- Friction and shear (dragging a patient across a bed).
- Age-related skin changes (thinner, fragile skin in elderly patients).
- Medical conditions (diabetes, poor circulation, spinal cord injuries).
4. Stages of Pressure Ulcers
| Stage | Description |
|---|---|
| Stage 1 | Red, non-blanchable skin, no open wound |
| Stage 2 | Partial-thickness skin loss, blister formation |
| Stage 3 | Full-thickness skin loss, visible fat layer |
| Stage 4 | Deep tissue damage, exposure of muscle, bone, or tendons |
5. Nursing Interventions for Pressure Point Care
1. Repositioning the Patient
- Turn bedridden patients every 2 hours (Supine → Side-lying → Prone).
- Adjust wheelchair-bound patients every 15-30 minutes.
- Use pillows or foam cushions to relieve pressure on bony areas.
2. Skin Care and Hygiene
- Keep skin clean and dry to prevent breakdown.
- Apply moisturizers to prevent dryness and cracking.
- Use barrier creams for patients with incontinence.
3. Pressure Redistribution Devices
- Use air or water mattresses for high-risk patients.
- Heel protectors and elbow pads to cushion bony prominences.
- Use specialized seating cushions for wheelchair users.
4. Massage and Circulation Promotion
- Gentle massage around pressure points to stimulate circulation.
- Encourage active and passive movements for mobility.
5. Nutrition and Hydration
- Ensure protein-rich diets (egg, milk, lean meat) for wound healing.
- Maintain hydration to keep skin supple.
6. Monitoring and Early Detection
- Regular skin assessment (daily for high-risk patients).
- Look for redness, swelling, pain, or open sores.
- Document changes and report to healthcare providers.
6. Special Considerations in Pressure Point Care
For Elderly Patients
- Skin is fragile and prone to tears—use gentle handling.
- Increase hydration and nutrition to maintain skin integrity.
For Diabetic Patients
- Neuropathy (nerve damage) may prevent them from feeling pressure sores.
- Inspect feet and pressure points daily.
For Critically Ill or ICU Patients
- Use frequent turning schedules to prevent ulcers.
- Utilize specialized low-pressure beds.
For Incontinent Patients
- Immediate cleansing after urine or stool exposure.
- Use absorbent pads and skin protectants.
7. Documentation and Reporting
- Condition of skin before and after care.
- Signs of redness, swelling, or ulcers.
- Repositioning schedule followed.
- Preventive measures used (e.g., pillows, air mattress).
- Patient’s response to interventions.
Assessment of Pressure Ulcers Using the Braden Scale
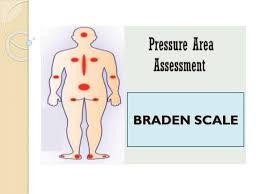
Introduction
The Braden Scale for Predicting Pressure Sore Risk is a standardized tool used in healthcare to assess a patient’s risk of developing pressure ulcers. It helps nurses and clinicians identify at-risk patients early and implement appropriate interventions to prevent pressure ulcers.
1. What is the Braden Scale?
The Braden Scale is a widely used risk assessment tool that evaluates a patient’s risk of developing pressure ulcers based on six key factors. Each factor is scored between 1 to 4, except for friction & shear, which is scored 1 to 3. The total score ranges from 6 to 23, with a lower score indicating a higher risk of developing pressure ulcers.
Scoring and Risk Interpretation
| Braden Score | Risk Level |
|---|---|
| 19 – 23 | No risk |
| 15 – 18 | Mild risk |
| 13 – 14 | Moderate risk |
| 10 – 12 | High risk |
| ≤ 9 | Very high risk |
2. Components of the Braden Scale
The Braden Scale consists of six subscales that assess different factors contributing to pressure ulcer formation.
1. Sensory Perception
- Definition: The ability to respond to discomfort caused by pressure.
- Scoring:
- 1 (Completely Limited) – Unresponsive to pain (e.g., unconscious, sedated, or neurologically impaired).
- 2 (Very Limited) – Responds only to painful stimuli or has limited ability to feel pain.
- 3 (Slightly Limited) – Can express pain but may not always respond appropriately.
- 4 (No Impairment) – Normal sensory perception.
2. Moisture
- Definition: The level of skin exposure to moisture from sweat, urine, feces, or wound drainage.
- Scoring:
- 1 (Constantly Moist) – Skin is always damp; needs frequent linen changes.
- 2 (Often Moist) – Skin is often moist, requiring linen changes at least once a shift.
- 3 (Occasionally Moist) – Skin is occasionally moist; requires extra care.
- 4 (Rarely Moist) – Skin is dry; moisture is minimal.
3. Activity
- Definition: The patient’s level of physical activity.
- Scoring:
- 1 (Bedfast) – Confined to bed.
- 2 (Chairfast) – Can sit but cannot bear weight.
- 3 (Walks Occasionally) – Walks occasionally but may need assistance.
- 4 (Walks Frequently) – Walks independently.
4. Mobility
- Definition: The ability to change and control body positions.
- Scoring:
- 1 (Completely Immobile) – Cannot move independently.
- 2 (Very Limited) – Moves minimally with assistance.
- 3 (Slightly Limited) – Moves independently but with some difficulty.
- 4 (No Limitation) – Moves freely.
5. Nutrition
- Definition: The adequacy of the patient’s nutritional intake.
- Scoring:
- 1 (Very Poor) – Very little or no food intake; may be NPO (nothing by mouth).
- 2 (Probably Inadequate) – Occasionally eats full meals but lacks proper nutrition.
- 3 (Adequate) – Eats most of meals; good protein intake.
- 4 (Excellent) – Well-balanced diet; eats enough food.
6. Friction and Shear
- Definition: The degree to which the patient’s skin is exposed to friction and shear forces.
- Scoring:
- 1 (Problem) – Requires maximum assistance for movement.
- 2 (Potential Problem) – Some assistance needed; occasional sliding.
- 3 (No Apparent Problem) – Moves without difficulty.
3. Clinical Application of the Braden Scale
- When to Use:
- On admission to a hospital or healthcare facility.
- At regular intervals (daily in ICUs, every 48–72 hours in general wards).
- Whenever there is a change in the patient’s condition.
- Who Should be Assessed?
- Bedridden or immobile patients.
- Patients with incontinence (urinary or fecal).
- Elderly individuals with fragile skin.
- Patients with chronic illnesses (diabetes, spinal cord injuries).
- Postoperative patients.
4. Nursing Interventions Based on Braden Scale Scores
| Risk Level | Intervention Strategies |
|---|---|
| No Risk (19–23) | Routine skin care and hygiene. |
| Mild Risk (15–18) | Frequent repositioning, ensuring dry skin, monitoring nutrition. |
| Moderate Risk (13–14) | Pressure redistribution mattress, moisture management, mobility assistance. |
| High Risk (10–12) | Specialized pressure-relieving devices, repositioning every 2 hours, nutritional support. |
| Very High Risk (≤9) | Intensive skin care, frequent monitoring, aggressive wound prevention measures. |
5. Documentation and Reporting
- Braden Scale Score and date of assessment.
- Signs of skin breakdown (redness, blisters, ulcers).
- Interventions provided (position changes, skin care, nutrition support).
- Patient response to interventions.
6. Advantages of Using the Braden Scale
✅ Standardized tool used globally.
✅ Early identification of at-risk patients.
✅ Guides nursing interventions to prevent pressure ulcers.
✅ Reduces healthcare costs by preventing complications.
7. Limitations of the Braden Scale
❌ Does not account for individual pain tolerance and subjective factors.
❌ May overestimate or underestimate risk in some patients.
❌ Requires consistent training and accurate assessment for reliability.
Assessment of Pressure Ulcers Using the Norton Scale
Introduction
The Norton Scale is a standardized tool used to assess the risk of pressure ulcer (bedsore) development in patients. It was developed in 1962 by Doreen Norton, Rhoda McLaren, and Susan Exton-Smith and is widely used in hospitals, nursing homes, and long-term care facilities. The lower the score, the higher the risk of developing pressure ulcers.
1. What is the Norton Scale?
The Norton Scale is a five-category scoring system that evaluates a patient’s risk of developing pressure ulcers. Each category is scored between 1 (poor) to 4 (good), with a total possible score of 5 to 20. A score of 14 or lower indicates a significant risk of pressure ulcers.
Scoring and Risk Interpretation
| Norton Score | Risk Level |
|---|---|
| 16 – 20 | Low or No Risk |
| 12 – 15 | Moderate Risk |
| < 12 | High Risk |
2. Components of the Norton Scale
The Norton Scale consists of five factors that contribute to pressure ulcer development:
1. Physical Condition
- Assesses overall health status.
- Scoring:
- 1 (Very Bad) – Critically ill, severely compromised.
- 2 (Bad) – Poor condition, weak, chronically ill.
- 3 (Fair) – Stable health, moderate illness.
- 4 (Good) – Normal health, active.
2. Mental Condition
- Evaluates the patient’s awareness and ability to recognize pain or discomfort.
- Scoring:
- 1 (Stuporous or Unconscious) – No response to stimuli.
- 2 (Confused or Disoriented) – Poor response to discomfort.
- 3 (Apathetic or Drowsy) – Some awareness but reduced response.
- 4 (Alert and Oriented) – Fully aware and responsive.
3. Activity Level
- Determines the patient’s mobility and ability to move independently.
- Scoring:
- 1 (Bedfast) – Completely immobile, bedridden.
- 2 (Chairfast) – Confined to a wheelchair.
- 3 (Walks with Help) – Requires assistance to walk.
- 4 (Fully Mobile) – Moves independently.
4. Mobility
- Measures the ability to change and control body position.
- Scoring:
- 1 (Completely Immobile) – Unable to move without assistance.
- 2 (Very Limited Mobility) – Minimal ability to reposition.
- 3 (Slightly Limited Mobility) – Moves independently but with some restrictions.
- 4 (No Limitations) – Moves freely.
5. Incontinence
- Assesses the risk of skin breakdown due to moisture exposure.
- Scoring:
- 1 (Doubly Incontinent) – Loss of bowel and bladder control.
- 2 (Urinary or Fecal Incontinence) – Either urine or fecal incontinence.
- 3 (Occasional Incontinence) – Occasional loss of bladder or bowel control.
- 4 (Continent) – Normal control over bladder and bowel.
3. Clinical Application of the Norton Scale
- When to Use:
- On admission to a healthcare facility.
- Regularly during hospitalization (every 24-48 hours).
- When the patient’s condition changes (e.g., after surgery or illness).
- Who Should be Assessed?
- Bedridden patients in hospitals or nursing homes.
- Elderly patients at risk of skin breakdown.
- Postoperative patients with limited mobility.
- Patients with neurological disorders (e.g., stroke, paralysis).
- Patients with incontinence leading to skin moisture exposure.
4. Nursing Interventions Based on Norton Scale Scores
| Risk Level | Intervention Strategies |
|---|---|
| No Risk (16-20) | Routine skin care, maintain hygiene, encourage movement. |
| Moderate Risk (12-15) | Repositioning every 2 hours, pressure-relieving mattresses, moisture control. |
| High Risk (<12) | Intensive skin monitoring, special cushions, strict repositioning schedules, aggressive ulcer prevention measures. |
5. Advantages of Using the Norton Scale
✅ Simple and easy to use for rapid assessment.
✅ Requires minimal training for healthcare providers.
✅ Can be integrated into daily nursing routines.
✅ Helps in early detection of high-risk patients.
6. Limitations of the Norton Scale
❌ Less detailed than the Braden Scale, does not assess nutrition.
❌ May underestimate risk in some patients.
❌ Requires clinical judgment for accuracy.
7. Documentation and Reporting
- Norton Score and assessment date.
- Signs of skin breakdown (redness, blisters, ulcers).
- Interventions provided (position changes, skin care, nutrition support).
- Patient’s response to interventions.
Assessment of Pressure Ulcers
Introduction
Pressure ulcers, also known as bedsores or decubitus ulcers, are localized injuries to the skin and underlying tissue, primarily caused by prolonged pressure on bony prominences. Accurate assessment is essential to determine risk, severity, and appropriate intervention. Several assessment tools and scales are used in nursing practice to evaluate and prevent pressure ulcers.
1. Methods of Assessing Pressure Ulcers
A. Physical Examination
- Skin Inspection: Checking for redness, discoloration, wounds, and moisture.
- Palpation: Assessing skin temperature, firmness, and edema.
- Measurement of Ulcer Size: Documenting length, width, and depth using a sterile ruler.
- Assessment of Exudate: Evaluating the amount, color, and odor of wound drainage.
- Pain Assessment: Using a pain scale to determine the severity of discomfort.
- Tissue Involvement Check: Identifying necrotic, sloughy, or granulation tissue.
B. Risk Assessment Scales
Several validated risk assessment tools help predict the likelihood of developing pressure ulcers and assist in preventive care.
2. Pressure Ulcer Risk Assessment Scales
A. Braden Scale for Predicting Pressure Sore Risk
- Components:
- Sensory Perception
- Moisture
- Activity
- Mobility
- Nutrition
- Friction and Shear
- Scoring: 6 to 23 (Lower score = Higher risk)
- Interpretation:
- ≥19: No Risk
- 15–18: Mild Risk
- 13–14: Moderate Risk
- 10–12: High Risk
- ≤9: Very High Risk
B. Norton Scale
- Components:
- Physical Condition
- Mental Condition
- Activity
- Mobility
- Incontinence
- Scoring: 5 to 20 (Lower score = Higher risk)
- Interpretation:
- ≥16: No Risk
- 12–15: Moderate Risk
- <12: High Risk
C. Waterlow Pressure Ulcer Risk Assessment Scale
- Developed in 1985 and commonly used in the UK.
- Components:
- Age
- Skin Type & Visual Assessment
- Sex & Weight
- Malnutrition Status
- Continence
- Mobility
- Special Risks (e.g., tissue malnutrition, neurological deficit)
- Scoring:
- <10: Low Risk
- 10–14: Moderate Risk
- 15–19: High Risk
- ≥20: Very High Risk
D. Cubbin and Jackson Scale
- Specifically designed for ICU patients.
- Components:
- General Physical Condition
- Mental Status
- Mobility
- Hemodynamics
- Oxygenation Status
- Nutrition
- Sensory Perception
- Medication Use
- Scoring: Ranges from 6 to 48 (Lower score = Higher risk)
3. Pressure Ulcer Severity Assessment Tools
A. National Pressure Injury Advisory Panel (NPIAP) Staging System
- Stage 1: Non-blanchable redness, skin intact.
- Stage 2: Partial-thickness skin loss (blister-like wound).
- Stage 3: Full-thickness skin loss with exposed fat.
- Stage 4: Deep ulcer with exposed muscle, tendon, or bone.
- Unstageable: Covered by necrotic tissue, preventing depth assessment.
- Deep Tissue Injury (DTI): Persistent non-blanchable deep red or purple discoloration.
B. PUSH (Pressure Ulcer Scale for Healing) Tool
- Developed by the National Pressure Ulcer Advisory Panel (NPUAP).
- Measures wound healing progress over time.
- Components:
- Wound Size (cm²)
- Exudate Amount
- Tissue Type (necrotic, slough, granulation)
- Total Score: 0 (healed) to 17 (severe wound).
C. Bates-Jensen Wound Assessment Tool (BWAT)
- A detailed assessment tool for monitoring wound healing.
- Components:
- Wound size, depth, edges, color, necrosis, drainage, and odor.
- Evaluates skin condition around the ulcer.
4. Advanced Diagnostic Methods for Pressure Ulcers
A. Infrared Thermography
- Measures temperature changes around the wound.
- Helps detect early-stage tissue damage before ulcer formation.
B. Ultrasonography
- Assesses subcutaneous tissue damage not visible on the surface.
- Helps evaluate deep tissue injuries (DTI).
C. Laser Doppler Flowmetry
- Measures blood perfusion to identify areas at risk of ischemia.
D. Biopsy and Microbial Swabs
- Used to diagnose infected or non-healing ulcers.
- Helps in determining appropriate antibiotic therapy.
5. Clinical Application of Assessment Tools
| Assessment Tool | Purpose | Application |
|---|---|---|
| Braden Scale | Predicts ulcer risk | General hospital settings |
| Norton Scale | Predicts ulcer risk | Nursing homes, long-term care |
| Waterlow Scale | Predicts ulcer risk | UK healthcare settings |
| Cubbin & Jackson Scale | Predicts ulcer risk | ICU patients |
| NPIAP Staging | Classifies ulcer severity | Clinical wound assessment |
| PUSH Tool | Monitors healing progress | Chronic wound care |
| BWAT | Detailed wound evaluation | Wound care nursing |
6. Nursing Interventions Based on Assessment Findings
| Assessment Finding | Nursing Intervention |
|---|---|
| High-Risk Braden Score (<12) | Turn patient every 2 hours, use pressure relief mattresses. |
| Stage 1 Ulcer | Keep skin clean and dry, reposition frequently. |
| Stage 2 Ulcer | Apply moisture-retentive dressings, reduce friction. |
| Stage 3-4 Ulcer | Debridement, advanced wound care, nutrition support. |
| Deep Tissue Injury (DTI) | Avoid excessive pressure, use protective padding. |
7. Documentation and Reporting
- Risk assessment score (Braden, Norton, etc.).
- Ulcer location and stage (if present).
- Size, depth, and exudate amount.
- Interventions provided (turning schedule, dressings, etc.).
- Response to treatment and healing progress.
- Any signs of infection (redness, warmth, foul odor).
Pressure Ulcers
Introduction
Pressure ulcers, also known as bedsores or decubitus ulcers, are localized injuries to the skin and underlying tissue caused by prolonged pressure, friction, shear, or moisture. They commonly occur over bony prominences such as the sacrum, heels, elbows, and hips, especially in immobile patients. Early identification and intervention are crucial to prevent complications such as infections and sepsis.
1. Causes of Pressure Ulcers
A. Mechanical Causes
- Prolonged Pressure: Restricts blood flow to tissues, leading to ischemia and necrosis.
- Shear Forces: Sliding movement of skin layers over deeper tissues, causing tissue damage.
- Friction: Rubbing of the skin against bed sheets or clothing, leading to skin breakdown.
B. Contributing Factors
- Immobility: Patients confined to bed or wheelchair.
- Poor Circulation: Conditions like diabetes, peripheral artery disease.
- Moisture: Incontinence (urine, feces) softens the skin and increases breakdown risk.
- Malnutrition & Dehydration: Weakens skin integrity and delays wound healing.
- Neurological Impairment: Reduced pain sensation in spinal cord injuries or stroke patients.
- Aging: Thin and fragile skin in elderly individuals.
- Obesity or Underweight: Increased pressure or lack of fat padding over bony areas.
2. Stages of Pressure Ulcers and Their Manifestations
The National Pressure Injury Advisory Panel (NPIAP) classifies pressure ulcers into four stages, along with unstageable wounds and deep tissue injuries (DTI).
Stage 1: Non-Blanchable Erythema
Manifestations:
- Intact skin with persistent redness (erythema).
- Non-blanchable (does not turn white when pressed).
- Possible warmth, pain, or itching in the area.
- Reversible with immediate intervention.
Stage 2: Partial-Thickness Skin Loss
Manifestations:
- Break in skin integrity (shallow open wound or blister).
- Red or pink wound bed, without slough (dead tissue).
- May appear as an intact or ruptured blister.
- Painful but no deep tissue exposure.
Stage 3: Full-Thickness Skin Loss
Manifestations:
- Loss of entire epidermis and dermis, exposing fat layer.
- Wound may appear as a deep crater.
- Slough or necrotic tissue may be present.
- Possible signs of infection (redness, odor, drainage).
- May include undermining or tunneling (tissue loss under intact skin).
Stage 4: Full-Thickness Tissue Loss
Manifestations:
- Deep wound exposing muscle, tendon, or bone.
- Extensive necrosis with slough/eschar (black dead tissue).
- High risk of osteomyelitis (bone infection).
- Severe pain or loss of sensation in affected area.
- Long-term healing required with potential for surgical intervention.
Unstageable Pressure Ulcers
Manifestations:
- Full-thickness tissue loss covered by eschar or slough.
- Depth cannot be determined until necrotic tissue is removed.
- Requires debridement to assess severity.
Deep Tissue Injury (DTI)
Manifestations:
- Dark purple/maroon discoloration due to deep tissue damage.
- Skin is intact but feels boggy, warm, or painful.
- High risk of progressing to deeper ulcer if not managed.
3. Diagnosis of Pressure Ulcers
A. Clinical Assessment
- Skin Inspection: Identifying early signs such as redness, swelling, or open wounds.
- Palpation: Checking for temperature changes, firmness, or bogginess.
- Wound Measurement: Documenting size, depth, and tissue type.
- Pain Evaluation: Using pain scales to assess discomfort levels.
- Exudate (Drainage) Assessment: Identifying amount, color, and odor of wound fluid.
B. Risk Assessment Tools
- Braden Scale: Assesses sensory perception, moisture, activity, mobility, nutrition, and friction/shear.
- Norton Scale: Evaluates physical condition, mental state, activity, mobility, and incontinence.
- Waterlow Scale: Includes age, sex, weight, skin type, and special risk factors.
C. Advanced Diagnostic Tests
- Wound Culture & Sensitivity: Identifies bacterial infections for targeted antibiotic therapy.
- Tissue Biopsy: Determines depth of necrosis and presence of infection.
- Infrared Thermography: Detects early-stage tissue damage.
- Ultrasound/Doppler Imaging: Assesses blood circulation around the ulcer.
4. Nursing Care and Management
A. Wound Care
- Stage 1: Keep skin dry, apply barrier creams, reposition frequently.
- Stage 2: Use moisture-retentive dressings (hydrocolloid, foam).
- Stage 3-4: Requires debridement (removal of necrotic tissue), infection control, and specialized dressings.
B. Pain Management
- Analgesics: NSAIDs or opioids for severe cases.
- Topical Anesthetics: Lidocaine or numbing creams for pain relief.
C. Nutritional Support
- High-protein diet with vitamin C, zinc, and iron for wound healing.
- Hydration to maintain skin elasticity.
D. Pressure Relief Measures
- Repositioning every 2 hours in bedridden patients.
- Use of pressure-relieving devices (air or foam mattresses, cushions).
- Avoid dragging patients to prevent friction injuries.
E. Infection Control
- Antibiotics for infected wounds.
- Sterile dressing changes to prevent cross-contamination.
F. Surgical Interventions
- Skin grafting or flap surgery for large ulcers.
- Negative Pressure Wound Therapy (NPWT) to promote faster healing.
5. Prevention of Pressure Ulcers
| Preventive Measure | Key Strategies |
|---|---|
| Skin Care | Keep skin clean and dry, apply barrier creams. |
| Repositioning | Turn every 2 hours in bed, shift weight every 15-30 minutes for wheelchair users. |
| Support Surfaces | Use pressure-relieving mattresses, heel protectors. |
| Nutrition | Ensure adequate protein, vitamin C, and zinc intake. |
| Hydration | Drink at least 2-3 liters of water daily to maintain skin integrity. |
| Activity & Mobility | Encourage movement and exercise to improve circulation. |
| Moisture Management | Change wet clothes/bedding promptly, use absorbent pads for incontinence. |
6. Key Points
✅ Pressure ulcers result from prolonged pressure, friction, shear, and moisture.
✅ They progress in stages from non-blanchable erythema to deep tissue destruction.
✅ Early diagnosis using risk assessment tools (Braden, Norton, Waterlow) is crucial.
✅ Prevention includes skin care, repositioning, nutrition, and pressure-relief devices.
✅ Treatment involves wound care, pain management, infection control, and surgical options.
✅ Education and early interventions reduce complications and improve healing.
Perineal Care & Meatal Care
Introduction
Perineal care (peri-care) and meatal care are essential nursing procedures that involve cleansing the perineal and genital areas to maintain hygiene, prevent infections, and promote patient comfort. These procedures are particularly important for bedridden, incontinent, postpartum, and catheterized patients, as they are at higher risk of urinary tract infections (UTIs), skin irritation, and fungal infections.
1. Definition
- Perineal Care: The process of cleaning the perineal area (genital and anal region) to maintain hygiene and prevent infections.
- Meatal Care: The cleansing of the urinary meatus (opening of the urethra) to prevent infections, especially in catheterized patients.
2. Importance of Perineal and Meatal Care
✅ Prevents infections such as urinary tract infections (UTIs) and perineal dermatitis.
✅ Reduces skin irritation caused by moisture, sweat, or incontinence.
✅ Enhances patient comfort and dignity, reducing discomfort and odor.
✅ Prevents pressure ulcers in immobile or incontinent patients.
✅ Promotes healing in postpartum or post-surgical patients.
3. Indications for Perineal and Meatal Care
- Incontinent patients (urinary or fecal incontinence)
- Postpartum women (after vaginal delivery or episiotomy)
- Patients with urinary catheters
- Postoperative perineal surgery patients
- Elderly or bedridden individuals
- Patients with fungal or bacterial infections in the perineal area
4. Anatomy of the Perineal and Meatal Areas
A. Perineal Region
The perineum is the area between the genitalia and the anus. It includes:
- Male perineum: Scrotum, penis, and anus.
- Female perineum: Labia, vaginal opening, clitoris, and anus.
B. Meatal Region
- The urinary meatus is the opening of the urethra, where urine exits the body.
- It is more prone to bacterial entry in females due to its short length.
- In males, the urethral meatus is located at the tip of the penis.
5. Principles of Perineal and Meatal Care
- Maintain privacy using curtains or screens.
- Use warm water and mild soap to avoid irritation.
- Clean from front to back (especially in females) to prevent fecal contamination.
- Use separate washcloths for different areas to avoid cross-contamination.
- Ensure proper drying to prevent moisture-related infections.
- Use gloves and follow infection control measures.
6. Equipment Needed
- Clean gloves
- Warm water in a basin
- Mild soap or perineal cleanser
- Washcloths or disposable wipes
- Towels
- Bedpan or absorbent pad (if needed)
- Moisturizer or barrier cream (for incontinent patients)
- Catheter cleansing solution (for catheterized patients)
7. Procedure for Perineal Care
A. For Female Patients
- Explain the procedure to the patient.
- Ensure privacy using curtains or a drape.
- Position the patient in a dorsal recumbent position (lying on back with knees bent).
- Wear gloves and place a waterproof pad under the patient.
- Expose only the perineal area, keeping the rest covered.
- Clean from front to back:
- Separate the labia and clean with a warm, moist washcloth.
- Wipe each side separately to prevent contamination.
- Clean the urinary meatus and vaginal opening.
- Rinse thoroughly and pat dry gently.
- Clean the anal area last, using a new washcloth and wiping front to back.
- Apply barrier cream or moisturizer if needed.
- Dispose of materials properly, remove gloves, and wash hands.
- Document any abnormalities (redness, discharge, foul odor).
B. For Male Patients
- Explain the procedure to the patient.
- Ensure privacy and position the patient in a supine position.
- Wear gloves and place a waterproof pad under the patient.
- Expose only the perineal area.
- Clean the penis:
- If uncircumcised, retract the foreskin gently and clean the glans.
- Wipe in a circular motion from the meatus outward.
- Rinse and return the foreskin to prevent paraphimosis.
- Clean the scrotum and groin area, lifting gently.
- Clean the anal area last, using a new washcloth.
- Apply barrier cream if needed.
- Dispose of materials, remove gloves, and wash hands.
- Document any redness, swelling, or discharge.
8. Procedure for Meatal Care (For Catheterized Patients)
- Perform hand hygiene and wear gloves.
- Expose the urinary meatus while maintaining privacy.
- Use a sterile wipe or gauze soaked in saline solution.
- Clean the urinary meatus:
- For males: Clean the glans and catheter entry point in circular motions outward.
- For females: Clean the labia, perineum, and around the catheter.
- Do not tug or pull the catheter while cleaning.
- Dry the area gently and remove excess moisture.
- Secure the catheter properly to prevent movement and irritation.
- Document any redness, pain, or discharge.
9. Special Considerations
- For Postpartum Patients: Use warm water or a sitz bath for comfort.
- For Incontinent Patients: Apply a barrier cream to prevent skin breakdown.
- For Elderly Patients: Use gentle, hypoallergenic products to prevent dryness.
- For Catheterized Patients: Clean twice daily and after bowel movements to prevent UTIs.
10. Common Perineal and Meatal Issues
| Condition | Cause | Prevention/Treatment |
|---|---|---|
| UTIs | Poor hygiene, catheter use | Clean perineal area regularly, encourage hydration |
| Yeast Infections | Moisture, poor drying | Keep area dry, use antifungal powder |
| Fecal Incontinence Dermatitis | Prolonged exposure to stool | Use barrier creams, frequent cleansing |
| Paraphimosis | Improper foreskin retraction | Always return foreskin after cleaning |
| Catheter-Associated Infections | Bacteria at meatal site | Regular meatal care, sterile catheter insertion |
11. Documentation and Reporting
- Condition of the skin and meatus (redness, swelling, lesions).
- Presence of foul odor, unusual discharge, or pain.
- Type of cleaning agent used (soap, antiseptic).
- Patient’s tolerance to the procedure.
- Any abnormalities reported to the healthcare provider.
12. Key Points for Nursing Practice
✅ Always maintain privacy and dignity during the procedure.
✅ Use front-to-back cleaning technique to prevent infections.
✅ For catheterized patients, clean the meatal area at least twice daily.
✅ Avoid using harsh soaps or excessive moisture to prevent skin breakdown.
✅ Document and report any signs of infection or discomfort.
Oral Care

Introduction
Oral care is a fundamental aspect of nursing practice that ensures good hygiene, prevents infections, and promotes overall well-being. It is particularly important for critically ill, unconscious, elderly, and bedridden patients who may not be able to maintain their oral hygiene independently. Proper oral care prevents dental problems, reduces the risk of aspiration pneumonia, and enhances patient comfort.
1. Definition of Oral Care
Oral care is the practice of cleaning the mouth, teeth, gums, tongue, and lips to maintain hygiene, prevent infections, and promote overall health. It includes brushing, flossing, moisturizing, and using antiseptic mouth rinses.
2. Importance of Oral Care in Nursing
✅ Prevents infections such as pneumonia and oral thrush.
✅ Reduces the risk of aspiration pneumonia in ventilated and unconscious patients.
✅ Prevents halitosis (bad breath) and enhances patient comfort.
✅ Promotes appetite and proper digestion by maintaining oral health.
✅ Prevents oral ulcers, gum diseases, and dental decay.
✅ Enhances communication and social confidence in patients.
3. Indications for Oral Care
- Conscious patients who require assistance in maintaining oral hygiene.
- Unconscious, intubated, or ventilated patients who cannot clean their mouths.
- Patients with dysphagia (difficulty swallowing) to prevent aspiration.
- Postoperative patients recovering from surgery, especially head, neck, or oral surgeries.
- Patients undergoing chemotherapy or radiation therapy (at risk for oral mucositis).
- Elderly patients with reduced salivation due to aging or medications.
- Diabetic patients who are at higher risk of oral infections.
- Patients with neurological disorders such as stroke or Parkinson’s disease.
4. Anatomy of the Oral Cavity
The oral cavity consists of:
- Teeth: Help in chewing and speech.
- Gums (Gingiva): Support and protect teeth.
- Tongue: Aids in speech, taste, and digestion.
- Salivary Glands: Produce saliva that lubricates and protects oral tissues.
- Mucosa (Oral Lining): Protects against infections and injuries.
5. Principles of Oral Care in Nursing
- Maintain privacy and dignity of the patient.
- Use a gentle approach to prevent injury or discomfort.
- Ensure infection control by using clean gloves and sterile equipment.
- Position the patient properly to prevent aspiration.
- Assess oral health for any signs of infection, bleeding, or ulcers.
- Encourage self-care if the patient is capable.
6. Equipment Needed for Oral Care
- Soft-bristled toothbrush or sponge toothbrush for delicate gums.
- Fluoride toothpaste (if appropriate).
- Mouthwash or antiseptic rinse (chlorhexidine for high-risk patients).
- Suction apparatus (for unconscious or ventilated patients).
- Gauze pads and tongue depressors.
- Lip moisturizer (to prevent chapped lips).
- Cup of clean water for rinsing.
- Gloves and protective apron.
7. Procedure for Oral Care
A. Oral Care for Conscious Patients
- Explain the procedure to the patient.
- Ensure privacy and maintain a comfortable environment.
- Assist the patient to a sitting or semi-Fowler’s position.
- Perform hand hygiene and wear gloves.
- Encourage the patient to brush their teeth or provide assistance.
- Use a soft toothbrush and toothpaste to clean teeth gently.
- Brush in circular motions, ensuring coverage of:
- Front and back of the teeth
- Chewing surfaces
- Gumline
- Clean the tongue gently to remove bacteria.
- Rinse the mouth with water or mouthwash and spit into a basin.
- Moisturize lips with petroleum jelly or a lip balm.
- Dispose of waste properly, remove gloves, and wash hands.
- Document the procedure and any abnormalities.
B. Oral Care for Unconscious or Ventilated Patients
- Explain the procedure to the family if present.
- Maintain proper positioning (side-lying or semi-Fowler’s) to prevent aspiration.
- Use suction equipment to remove excess saliva.
- Wear gloves and protective gear.
- Use a soft toothbrush or sponge applicator soaked in antiseptic solution.
- Gently clean the teeth, gums, and tongue.
- Use a suction catheter to remove saliva and debris.
- Apply lip balm or moisturizer.
- Document the findings, including oral hygiene status and any abnormalities.
C. Special Oral Care for Specific Conditions
| Condition | Special Considerations |
|---|---|
| Patients with dentures | Remove and clean dentures separately with denture cleaner. |
| Chemotherapy patients | Use mild mouthwash; avoid alcohol-based rinses. |
| Diabetic patients | Monitor for signs of gum disease and oral infections. |
| Stroke or Parkinson’s patients | Use thickened fluids to prevent aspiration. |
8. Common Oral Health Problems and Nursing Interventions
| Oral Condition | Cause | Nursing Intervention |
|---|---|---|
| Halitosis (Bad Breath) | Poor hygiene, infections | Regular brushing, mouthwash use |
| Xerostomia (Dry Mouth) | Medications, aging | Hydration, saliva substitutes |
| Oral Thrush (Candidiasis) | Fungal infection | Antifungal mouthwash |
| Gingivitis | Poor oral hygiene | Frequent brushing, antiseptic rinse |
| Oral Mucositis | Chemotherapy, radiation | Saline rinse, pain relief |
9. Infection Control in Oral Care
- Use separate toothbrushes for each patient.
- Follow hand hygiene protocols before and after care.
- Dispose of used items properly to prevent cross-contamination.
- Use suction for ventilated patients to prevent pneumonia.
10. Documentation and Reporting
- Condition of teeth, gums, and oral mucosa.
- Presence of ulcers, sores, bleeding, or dryness.
- Type of oral care provided (brushing, mouthwash, moisturizing).
- Patient’s response to care and tolerance of the procedure.
- Any referrals to a dentist or specialist if required.
11. Key Points for Nursing Practice
✅ Perform oral care at least twice daily for all patients.
✅ Use a soft toothbrush and gentle motions to prevent gum damage.
✅ Keep the patient in a semi-Fowler’s or side-lying position to prevent aspiration.
✅ Assess the oral cavity for redness, sores, or signs of infection.
✅ Encourage self-care for patients who can participate in their hygiene.
✅ Provide mouth moisturizing for ventilated, unconscious, or elderly patients.
✅ Document findings and interventions for continuity of care.
Care of the Eyes

Introduction
Eye care is an essential aspect of nursing practice aimed at maintaining eye hygiene, preventing infections, and ensuring patient comfort. Proper eye care is particularly important for bedridden, unconscious, post-surgical, elderly, and critically ill patients who may be unable to care for their own eyes. Good eye care helps prevent dryness, infections, corneal abrasions, and vision complications.
1. Definition of Eye Care
Eye care in nursing refers to the procedures performed to clean, protect, and maintain the health of the eyes in patients who cannot do so themselves. It includes regular cleaning, infection prevention, lubrication, and assessment of eye conditions.
2. Importance of Eye Care in Nursing
✅ Prevents eye infections such as conjunctivitis.
✅ Reduces the risk of corneal ulcers in unconscious or ventilated patients.
✅ Prevents eye dryness and irritation in patients with reduced blinking.
✅ Enhances comfort and prevents foreign body accumulation.
✅ Aids in early detection of eye disorders such as cataracts, glaucoma, or diabetic retinopathy.
✅ Prevents complications in post-operative eye surgery patients.
3. Indications for Eye Care
Eye care is essential for patients in various conditions, including:
- Unconscious or comatose patients (reduced blinking increases dryness and infection risk).
- Elderly patients (prone to dry eyes and cataracts).
- Post-operative eye surgery patients (cataract surgery, corneal transplant).
- Critically ill or ventilated patients (ICU patients on mechanical ventilation).
- Patients with eye infections (conjunctivitis, blepharitis).
- Newborns (risk of neonatal conjunctivitis or ophthalmia neonatorum).
- Patients with neurological disorders (stroke, Parkinson’s, Bell’s palsy).
4. Anatomy of the Eye
The eye consists of:
- Conjunctiva: The thin, transparent membrane covering the sclera.
- Cornea: The clear outer layer that protects the eye.
- Sclera: The white part of the eye.
- Lacrimal Glands: Produce tears to keep the eyes moist.
- Pupil and Iris: Control the amount of light entering the eye.
- Lens and Retina: Focus images and transmit signals to the brain.
5. Principles of Eye Care
- Use sterile equipment to prevent infections.
- Clean from inner to outer canthus to avoid contamination.
- Use a separate swab for each eye to prevent cross-infection.
- Avoid excessive pressure on the eyeball while cleaning.
- Keep the eyes moist using lubricating drops or artificial tears.
- Ensure proper hand hygiene before and after the procedure.
6. Equipment Needed for Eye Care
- Sterile gloves
- Sterile gauze or cotton swabs
- Normal saline or sterile water
- Lubricating eye drops (if needed)
- Eye shields or patches (for post-surgical care)
- Prescribed medications (antibiotic or anti-inflammatory eye drops)
7. Procedure for Eye Care
A. General Eye Cleaning for Conscious Patients
- Explain the procedure to the patient.
- Perform hand hygiene and wear sterile gloves.
- Position the patient in a semi-Fowler’s position with head slightly tilted back.
- Moisten sterile gauze with normal saline or sterile water.
- Wipe from inner canthus (corner) to outer canthus using gentle strokes.
- Use a new gauze for each eye to prevent cross-infection.
- Dry the area gently with a clean gauze pad.
- Apply prescribed eye drops or ointment if needed.
- Dispose of used materials properly, remove gloves, and wash hands.
- Document the procedure and any findings (e.g., redness, discharge).
B. Eye Care for Unconscious Patients
- Ensure head is slightly elevated to allow drainage.
- Use artificial tears or lubricating ointment to prevent dryness.
- Clean the eyes gently using the inner to outer technique.
- Tape the eyelids shut if needed (for long-term unconscious patients).
- Protect the eyes with an eye shield if necessary.
C. Administration of Eye Drops/Ointment
- Check the doctor’s prescription for correct medication.
- Wash hands and wear gloves.
- Ask the patient to look up to expose the lower conjunctival sac.
- Pull down the lower eyelid gently.
- Instill 1-2 drops of the medication into the lower conjunctival sac.
- Ask the patient to close the eyes gently (do not squeeze shut).
- Press lightly on the inner corner (nasolacrimal duct) for 30 seconds to prevent systemic absorption.
- Remove excess medication with a sterile swab.
- Avoid touching the dropper to the eye to prevent contamination.
- Document the medication administration and patient response.
D. Special Eye Care for Specific Conditions
| Condition | Special Considerations |
|---|---|
| Conjunctivitis (Pink Eye) | Use antibiotic eye drops, separate towels for the patient. |
| Post-Surgical Patients | Avoid rubbing eyes, use eye shields, and administer prescribed medication. |
| Dry Eyes (Xerophthalmia) | Use artificial tears regularly. |
| Corneal Ulcers | Administer prescribed antibiotic/antifungal drops, prevent eye strain. |
| Bell’s Palsy | Keep the affected eye lubricated and protected with an eye patch. |
8. Preventive Measures for Eye Care
- Encourage regular blinking in patients using screens for long hours.
- Protect the eyes from direct sunlight using sunglasses.
- Encourage hydration to maintain tear production.
- Maintain hygiene by avoiding eye rubbing.
- Use protective eyewear in workplaces with dust or chemicals.
9. Common Eye Disorders and Nursing Interventions
| Condition | Symptoms | Nursing Intervention |
|---|---|---|
| Conjunctivitis | Redness, swelling, discharge | Clean eyes, use prescribed antibiotic drops |
| Dry Eye Syndrome | Itchy, gritty feeling | Use artificial tears, avoid direct air exposure |
| Cataracts | Blurry vision, glare sensitivity | Pre & post-op care for cataract surgery |
| Glaucoma | Increased eye pressure, vision loss | Administer eye drops to reduce pressure |
| Corneal Abrasion | Pain, tearing, redness | Cover eye with patch, avoid rubbing |
10. Documentation and Reporting
- Condition of the eyes (redness, discharge, swelling).
- Type of care provided (cleaning, medication, lubrication).
- Patient’s response to care.
- Any abnormalities observed (pain, sensitivity, vision changes).
- Follow-up instructions or referrals to an ophthalmologist.
11. Key Points for Nursing Practice
✅ Always clean from inner to outer canthus to prevent infection spread.
✅ Use a separate swab for each eye to avoid cross-contamination.
✅ Ensure proper lubrication for unconscious or ventilated patients.
✅ Monitor for signs of infection such as redness, swelling, or discharge.
✅ Educate patients on proper eye care post-surgery or for dry eye conditions.
✅ Use prescribed medications correctly, ensuring aseptic administration.
Care of Ears, Nose, and Assistive Devices

Introduction
The care of the ears, nose, and assistive devices is an important part of nursing to ensure proper hygiene, prevent infections, and improve patient comfort and communication. Many patients, especially elderly or disabled individuals, require assistance with maintaining these body parts and their assistive devices, such as eyeglasses, contact lenses, dentures, and hearing aids.
I. CARE OF THE EARS
1. Importance of Ear Care
✅ Prevents infections such as otitis externa (swimmer’s ear) and otitis media.
✅ Removes excess earwax (cerumen) that can cause hearing problems.
✅ Prevents hearing loss and discomfort due to blockages.
✅ Ensures proper function of hearing aids in hearing-impaired individuals.
2. Anatomy of the Ear
The ear consists of three main parts:
- External Ear: Includes the auricle (pinna) and the ear canal.
- Middle Ear: Contains the eardrum, ossicles (tiny bones), and Eustachian tube.
- Inner Ear: Contains the cochlea and semicircular canals responsible for hearing and balance.
3. Procedure for Ear Cleaning
A. Routine External Ear Care
- Perform hand hygiene and wear gloves.
- Use a damp washcloth or cotton pad to clean the outer ear and behind the ears.
- Do not insert cotton swabs or sharp objects inside the ear canal.
- Dry the ears gently with a soft towel.
B. Removing Excess Earwax (Cerumen)
- Use a few drops of mineral oil, baby oil, or saline solution to soften earwax.
- Ask the patient to tilt the head and apply drops into the ear.
- After a few minutes, flush the ear with warm water using a syringe (if prescribed).
- Do not force wax out; refer to a healthcare provider if blockage persists.
C. Care for Patients with Hearing Aids
- Ensure ears are clean and dry before inserting a hearing aid.
- Clean hearing aids daily with a dry cloth.
- Remove the hearing aid at night to allow the ear to rest.
- Check battery life regularly and replace as needed.
- Store in a dry, safe place when not in use.
4. Common Ear Conditions and Nursing Interventions
| Condition | Cause | Nursing Intervention |
|---|---|---|
| Otitis Media (Middle Ear Infection) | Bacteria, viruses | Administer antibiotics, manage pain |
| Impacted Earwax (Cerumen Impaction) | Excess wax production | Use prescribed ear drops to soften wax |
| Tinnitus (Ringing in the Ears) | Aging, ear damage, noise exposure | Reduce exposure to loud noise, manage stress |
| Hearing Loss | Aging, infection, trauma | Encourage hearing aid use, assist with communication |
II. CARE OF THE NOSE
1. Importance of Nose Care
✅ Prevents nasal congestion and infections.
✅ Ensures proper breathing and oxygen intake.
✅ Removes mucus and foreign particles from the nasal passages.
✅ Prevents complications from nasal dryness in oxygen therapy patients.
2. Anatomy of the Nose
The nose consists of:
- External nose (nostrils)
- Nasal cavity (lined with mucosa)
- Sinuses (air-filled spaces in the skull)
- Olfactory receptors (responsible for smell)
3. Procedure for Nasal Care
A. General Nose Cleaning
- Wash hands and wear gloves.
- Use a soft damp cloth to clean the external nose.
- For dry nasal passages, apply saline nasal spray or petroleum jelly.
- Encourage proper blowing of the nose to prevent mucus buildup.
- Avoid using sharp objects or cotton swabs inside the nostrils.
B. Nasal Suctioning for Patients with Secretions
- Position the patient upright or in a semi-Fowler’s position.
- Insert a suction catheter gently into the nostril.
- Apply suction while withdrawing the catheter to remove mucus.
- Monitor for breathing difficulty and document the procedure.
C. Care for Patients on Oxygen Therapy
- Check for nasal dryness and irritation.
- Use a humidifier with oxygen therapy to prevent dryness.
- Encourage frequent hydration to keep nasal passages moist.
4. Common Nasal Conditions and Nursing Interventions
| Condition | Cause | Nursing Intervention |
|---|---|---|
| Rhinitis (Runny Nose) | Allergies, infections | Encourage hydration, use saline spray |
| Sinusitis | Bacterial or viral infection | Steam inhalation, antibiotics if bacterial |
| Nasal Dryness | Oxygen therapy, dry climate | Apply saline spray, use humidifiers |
III. CARE OF ASSISTIVE DEVICES
Patients use assistive devices such as eyeglasses, contact lenses, dentures, and hearing aids to improve vision, hearing, or dental function. Proper care ensures long-term functionality, comfort, and hygiene.
1. Care of Eyeglasses
- Clean daily with a microfiber cloth and lens cleaner.
- Avoid touching lenses with dirty hands.
- Store in a protective case when not in use.
- Adjust frames properly to avoid pressure on the nose or ears.
2. Care of Contact Lenses
- Wash hands before handling lenses.
- Use prescribed lens solution (never use tap water).
- Store in a clean case with fresh solution daily.
- Avoid wearing lenses overnight unless recommended.
- Monitor for redness, irritation, or blurred vision (signs of infection).
3. Care of Dentures
- Remove dentures after meals and rinse with water.
- Brush with a denture cleaner, not regular toothpaste.
- Soak in a denture solution overnight to prevent dryness.
- Ensure proper fit to avoid gum irritation.
- Store in water or a damp cloth when not in use.
4. Care of Hearing Aids
- Clean daily with a dry cloth (avoid water exposure).
- Remove at bedtime to allow ears to rest.
- Check battery function regularly.
- Store in a dry place when not in use.
- Monitor for feedback (whistling sound) which may indicate improper fit.
IV. Documentation and Reporting
- Condition of ears, nose, and assistive devices.
- Presence of redness, discharge, or irritation.
- Any hearing or vision changes.
- Patient response to care and interventions.
- Repairs or replacements needed for assistive devices.
V. Key Points for Nursing Practice
✅ Use proper infection control measures when handling ears, nose, and assistive devices.
✅ Encourage self-care for patients who can manage their devices independently.
✅ Monitor for signs of infection, irritation, or malfunction of assistive devices.
✅ Educate patients and caregivers on proper maintenance of glasses, contact lenses, dentures, and hearing aids.
✅ Provide emotional support for patients adjusting to assistive devices.
FOR UNLOCK 🔓 FULL COURSE NOW. MORE DETAILS CALL US OR WATSAPP ON- 8485976407
