BSC SEM 2 UNIT 1 COMMUNITY HEALTH NURSING
UNIT 1 Concepts of Community Health and Community Health Nursing
PUBLIC HEALTH
1. Definition of Public Health
Public Health is the science and art of preventing disease, prolonging life, and promoting health through organized efforts of society, organizations (public and private), communities, and individuals.
By C.E.A. Winslow (1920):
“Public health is the science and art of preventing disease, prolonging life and promoting health through the organized efforts of society.”
2. Objectives of Public Health
- Prevention of diseases
- Promotion of health
- Prolongation of life
- Environmental sanitation
- Health education
- Provision of medical and nursing care
3. Community Health Nursing – Definition

Community Health Nursing is a field of nursing that combines public health principles with nursing science to promote and protect the health of populations.
It focuses on health promotion, disease prevention, and health maintenance of individuals, families, and groups in a community setting.
4. Goals of Community Health Nursing
- Improve the health status of the population.
- Reduce health disparities.
- Provide accessible, equitable, and affordable healthcare.
- Promote self-care and independence.
- Increase health awareness and literacy.
5. Principles of Community Health Nursing
- Equity and social justice – Equal health services for all.
- Preventive over curative – Focus on disease prevention.
- Community participation – Involvement of people in planning and decision-making.
- Intersectoral coordination – Cooperation with other departments (education, sanitation, etc.)
- Evidence-based practice – Decisions based on scientific data.
6. Roles and Responsibilities of Community Health Nurse
| Role | Description |
|---|---|
| Care Provider | Provide direct nursing care at home or clinics. |
| Educator | Educate community on hygiene, nutrition, family planning. |
| Counselor | Counsel individuals/families about health practices. |
| Advocate | Speak up for the health rights of the community. |
| Manager | Manage community health programs and field workers. |
| Researcher | Participate in surveys, data collection, and studies. |
| Epidemiologist Assistant | Assist in outbreak investigation and control. |
7. Levels of Prevention in Community Health
- Primordial Prevention – Prevent risk factors (e.g., lifestyle education)
- Primary Prevention – Prevent disease occurrence (e.g., immunization)
- Secondary Prevention – Early diagnosis and treatment (e.g., screening)
- Tertiary Prevention – Rehabilitation and disability limitation
8. Key Activities in Community Health Nursing
- Home visits
- Immunization programs
- Maternal and child health services (ANC, PNC)
- School health services
- Health camps
- Sanitation and safe water programs
- Disease surveillance
- Health education sessions
- Referral services
9. Community Health Nursing Process
- Assessment – Collect data on community health needs
- Planning – Develop interventions
- Implementation – Deliver nursing care/services
- Evaluation – Measure outcomes and impact
10. Essential Skills of a Community Health Nurse
- Communication and interpersonal skills
- Observation and reporting
- Health education and counseling
- First aid and basic emergency care
- Organization and coordination
- Cultural sensitivity and empathy
11. Public Health Infrastructure in India
- Sub-centre (SC) – First contact point
- Primary Health Centre (PHC) – Referral from SC, has a Medical Officer
- Community Health Centre (CHC) – For specialist services
- District Hospital
- Tertiary Hospitals/Medical Colleges
12. Community-Based National Programs in India
- National Tuberculosis Elimination Program (NTEP)
- National Leprosy Eradication Program (NLEP)
- Universal Immunization Program (UIP)
- Reproductive, Maternal, Newborn, Child and Adolescent Health (RMNCH+A)
- National Programme for Non-Communicable Diseases (NPCDCS)
13. Difference between Public Health Nursing and Community Health Nursing
| Public Health Nursing | Community Health Nursing |
|---|---|
| Population-based | Family and individual focused |
| More preventive | Combination of curative and preventive |
| Macro-level planning | Micro-level interventions |
| Government policy emphasis | Service delivery emphasis |
14. Current Trends in Community Health Nursing
- Use of technology (telehealth, mHealth)
- Focus on NCDs
- Community-based rehabilitation
- Mental health integration
- Pandemic preparedness and response
- Strengthening health education and digital health literacy
CONCEPT OF COMMUNITY HEALTH AND COMMUNITY HEALTH NURSING
I. CONCEPT OF COMMUNITY
Community is a social group of people living in a specific geographic area, sharing common culture, values, norms, and often organized through a political or administrative structure.
Characteristics of a Community:
- Geographical area (village, town, city)
- Common interests/needs
- Social interaction
- Sense of belonging
- Shared resources
- Organized structure
II. DEFINITION OF COMMUNITY HEALTH

Community Health is the art and science of maintaining, protecting, and improving the health of people in a community through organized efforts.
It emphasizes preventive, promotive, and rehabilitative aspects rather than just curative.
III. OBJECTIVES OF COMMUNITY HEALTH
- Promote and protect health
- Prevent diseases and disabilities
- Prolong life
- Provide health education
- Improve environmental sanitation
- Encourage healthy behavior and lifestyle
- Increase access to health services
IV. COMPONENTS OF COMMUNITY HEALTH
- Health promotion (education, awareness, lifestyle)
- Disease prevention (vaccination, screening)
- Environmental sanitation (clean water, waste disposal)
- Nutrition (adequate food, diet education)
- Maternal and child health
- Family planning
- Control of endemic diseases
- Health education
- Mental health
- Rehabilitation
V. COMMUNITY HEALTH SERVICES
- School health services
- Immunization programs
- Maternal and child health clinics
- Family planning services
- Communicable disease control
- Water supply and sanitation programs
- Occupational health services
VI. DEFINITION OF COMMUNITY HEALTH NURSING

Community Health Nursing is a field of nursing that integrates nursing science with public health principles to promote and protect the health of populations in the community setting.
It deals with health promotion, disease prevention, and care of individuals, families, and groups in the community.
VII. OBJECTIVES OF COMMUNITY HEALTH NURSING
- Assess the health needs of the community.
- Plan and implement nursing care for individuals, families, and groups.
- Promote health and prevent diseases.
- Provide health education to the community.
- Encourage utilization of health services.
- Develop community participation.
- Support national health programs.
VIII. PRINCIPLES OF COMMUNITY HEALTH NURSING
- Care is based on needs of the community.
- Focus on preventive and promotive services.
- Equal and fair services to all.
- Family and community-centered care.
- Intersectoral collaboration with education, sanitation, etc.
- Encourage self-care and community involvement.
IX. FUNCTIONS OF COMMUNITY HEALTH NURSE
| Area | Functions |
|---|---|
| Direct Care | Provide care during home visits, immunization, MCH services |
| Education | Health education on hygiene, nutrition, family planning |
| Supervision | Supervise health workers, ASHA, ANMs |
| Surveillance | Monitor disease outbreaks, report notifiable diseases |
| Referral | Refer patients to higher health facilities |
| Documentation | Maintain records, reports, registers |
| Advocacy | Promote health rights of vulnerable groups |
X. SETTINGS FOR COMMUNITY HEALTH NURSING
- Homes (Home visits)
- Schools
- Primary Health Centers (PHCs)
- Sub-centers
- Anganwadi centers
- Urban health posts
- Industrial health clinics
- Outreach clinics
- Health camps
XI. COMMUNITY HEALTH NURSING PROCESS
- Assessment – Collect data on population health status.
- Diagnosis – Identify health problems or risks.
- Planning – Set goals and objectives.
- Implementation – Deliver care, education, or services.
- Evaluation – Measure outcomes and effectiveness.
XII. IMPORTANCE OF COMMUNITY HEALTH NURSING
- Helps in early disease detection.
- Reduces healthcare costs by prevention.
- Improves health status of underserved populations.
- Increases community participation in health.
- Strengthens the reach of health services in rural/remote areas.
- Supports national and international health goals (e.g., SDGs).
XIII. ROLE IN NATIONAL HEALTH PROGRAMS
Community health nurses play a vital role in programs like:
- Universal Immunization Program (UIP)
- Reproductive and Child Health (RCH)
- National Tuberculosis Elimination Program (NTEP)
- National Leprosy Eradication Program (NLEP)
- Janani Suraksha Yojana (JSY)
- Integrated Child Development Services (ICDS)
XIV. CURRENT TRENDS IN COMMUNITY HEALTH NURSING
- Digital health and telemedicine
- Mobile health units
- Community-based rehabilitation
- Focus on non-communicable diseases (NCDs)
- Health promotion through social media
- Training of ASHAs, ANMs, community volunteers
PUBLIC HEALTH IN INDIA AND ITS EVOLUTION
I. Definition of Public Health
Public Health is the science and art of preventing disease, prolonging life, and promoting health through the organized efforts of society, public and private sectors, and individuals.
As per WHO: “Public health is all organized measures to prevent disease, promote health, and prolong life among the population as a whole.”
II. ORIGIN AND EVOLUTION OF PUBLIC HEALTH IN INDIA
Public health in India has evolved over centuries, with key developments during ancient, colonial, and post-independence periods.
A. Ancient India (Before British Era)
- Concepts of hygiene and sanitation mentioned in Ayurveda, Charaka Samhita, and Sushruta Samhita.
- Emphasis on:
- Clean water
- Balanced diet
- Personal hygiene
- Yoga and mental well-being
- Existence of hospitals during Maurya and Gupta periods.
B. British Period (1757 – 1947)
During colonial rule, public health infrastructure began to be established due to epidemic outbreaks and military needs.
Key Events:
| Year | Event |
|---|---|
| 1859 | Civil Medical Department established |
| 1869 | Public Health Department established |
| 1881 | First All-India Census |
| 1885 | Local Self-Government Act (municipalities took public health responsibility) |
| 1897 | Epidemic Diseases Act (to control plague, still used today) |
| 1904 | Plague Commission established |
| 1911 | Birth and Death Registration made compulsory |
| 1919 | Montagu-Chelmsford Reforms: Health became a provincial subject |
| 1946 | Bhore Committee Report recommended universal health care |
C. Post-Independence Era (After 1947)
India took major steps to build a public health system aimed at universal health care, disease control, and health promotion.
Important Developments:
| Year | Event |
|---|---|
| 1947 | Independence of India |
| 1948 | India joined World Health Organization (WHO) |
| 1951 | Launch of First Five-Year Plan and National Family Planning Programme |
| 1952 | Establishment of Primary Health Centres (PHCs) |
| 1963 | National Smallpox Eradication Programme |
| 1975 | Integrated Child Development Services (ICDS) |
| 1978 | Alma Ata Declaration – India committed to “Health for All by 2000” |
| 1983 | First National Health Policy formulated |
| 2000s | National Health Mission (NHM) launched (2005) |
| 2017 | Launch of National Health Policy 2017 |
| 2018 | Launch of Ayushman Bharat – Health & Wellness Centres + PMJAY |
III. CURRENT PUBLIC HEALTH STRUCTURE IN INDIA
1. Rural Health Infrastructure (3-tier system):
| Level | Facility | Population Coverage |
|---|---|---|
| 1st | Sub-Centre (SC) | 5,000 (3,000 in tribal areas) |
| 2nd | Primary Health Centre (PHC) | 30,000 (20,000 in tribal) |
| 3rd | Community Health Centre (CHC) | 1,20,000 (80,000 in tribal) |
2. Urban Health Infrastructure:
- Urban Primary Health Centres (UPHCs)
- Urban Community Health Centres (UCHCs)
IV. MAJOR PUBLIC HEALTH PROGRAMMES IN INDIA
| Programme | Purpose |
|---|---|
| UIP (1985) | Universal Immunization Programme |
| RNTCP/NTEP | TB elimination |
| NACP | HIV/AIDS control |
| NLEP | Leprosy elimination |
| RCH | Reproductive and Child Health |
| POSHAN Abhiyaan | Nutrition and child development |
| PMJAY | Free secondary and tertiary care for the poor |
| AB-HWCs | Comprehensive primary healthcare at grassroots |
V. NATIONAL HEALTH POLICIES
| Policy | Focus |
|---|---|
| 1983 | Primary healthcare, rural health services |
| 2002 | Private-public partnership, health financing |
| 2017 | Universal health coverage, digital health, NCD control |
VI. CURRENT CHALLENGES IN PUBLIC HEALTH IN INDIA
- High burden of communicable and non-communicable diseases
- Malnutrition in children and anemia in women
- Lack of access in rural and remote areas
- Shortage of health workforce
- Environmental and occupational health risks
- Inadequate health financing (<2.5% of GDP)
- Rising lifestyle-related illnesses
- Post-COVID mental health issues
VII. ROLE OF PUBLIC HEALTH IN NATIONAL DEVELOPMENT
- Reduces disease burden and mortality
- Improves productivity and economic growth
- Enhances quality of life
- Promotes equity and access
- Supports sustainable development goals (SDGs)
VIII. FUTURE DIRECTIONS
- Strengthening primary health care
- Expanding Ayushman Bharat and HWCs
- Digital Health Mission for e-records
- Focus on preventive and promotive health
- Training of healthcare professionals
- Addressing climate change and health
SCOPE OF COMMUNITY HEALTH NURSING
Definition Recap:
Community Health Nursing is a specialized field of nursing that integrates nursing and public health practices to promote and protect the health of populations, especially in a community setting (homes, schools, clinics, rural/urban areas).
MEANING OF SCOPE
The scope of community health nursing means the range of roles, responsibilities, services, and areas in which community health nurses function to promote health, prevent disease, and ensure well-being of individuals, families, and communities.
SCOPE OF COMMUNITY HEALTH NURSING – KEY AREAS

1. Family Health Care
- Home visits
- Health education
- Care during pregnancy, childbirth, and postnatal period
- Newborn and child care
- Support for elderly and chronically ill family members
2. Maternal and Child Health (MCH)
- Antenatal and postnatal care
- Safe delivery support
- Immunization
- Growth monitoring
- Nutritional counseling
- Prevention of child mortality
3. School Health Nursing
- Health screening of school children
- First aid and basic treatment
- Personal hygiene education
- Counseling on nutrition, adolescence, reproductive health
- Early detection of health problems (vision, hearing, mental health)
4. Occupational Health Nursing
- Health care in industrial and workplace settings
- Monitoring for occupational diseases
- Ensuring safety standards (PPE, sanitation)
- Health education and emergency care
5. Geriatric (Elderly) Nursing
- Home-based care for aging population
- Management of chronic diseases (BP, diabetes)
- Fall prevention, diet, mobility assistance
- Counseling and emotional support
6. Rehabilitation Nursing
- Post-operative care at home
- Support after stroke, injury, or surgery
- Rehabilitation of disabled individuals
- Coordination with physiotherapists, speech therapists
7. Communicable Disease Control
- Surveillance of diseases like TB, malaria, dengue
- Health education on hygiene and sanitation
- Contact tracing, isolation, and follow-up
- Promoting immunization
8. Non-Communicable Disease (NCD) Prevention
- Screening for hypertension, diabetes, cancer
- Lifestyle counseling (diet, exercise, stress management)
- Tobacco and alcohol de-addiction programs
9. Environmental Health
- Safe drinking water and sanitation
- Waste disposal practices
- Vector control (mosquito breeding sites)
- Air and noise pollution awareness
10. Disaster Management and Emergency Nursing
- First aid during floods, earthquakes, accidents
- Organizing health camps
- Psychological support to victims
- Mobilizing community resources
11. Health Education and Promotion
- Organizing health awareness programs
- Use of IEC (Information, Education, Communication) materials
- Community meetings, street plays, posters
- Behavior change communication
12. Implementation of National Health Programs
- Participation in programs like:
- Universal Immunization Program (UIP)
- Reproductive and Child Health (RCH)
- National Tuberculosis Elimination Program (NTEP)
- National Leprosy Eradication Program (NLEP)
- Ayushman Bharat Health & Wellness Centres (HWCs)
13. Research and Data Collection
- Community health surveys
- Disease reporting and surveillance
- Assessment of health needs
- Evaluation of health programs
SPECIAL AREAS IN MODERN COMMUNITY HEALTH NURSING
- Digital Health (Telehealth)
- Community Mental Health
- Palliative Care at Home
- Health Counseling in Remote Areas
- Training ASHAs and community volunteers
REVIEW: CONCEPTS OF HEALTH & ILLNESS/DISEASE
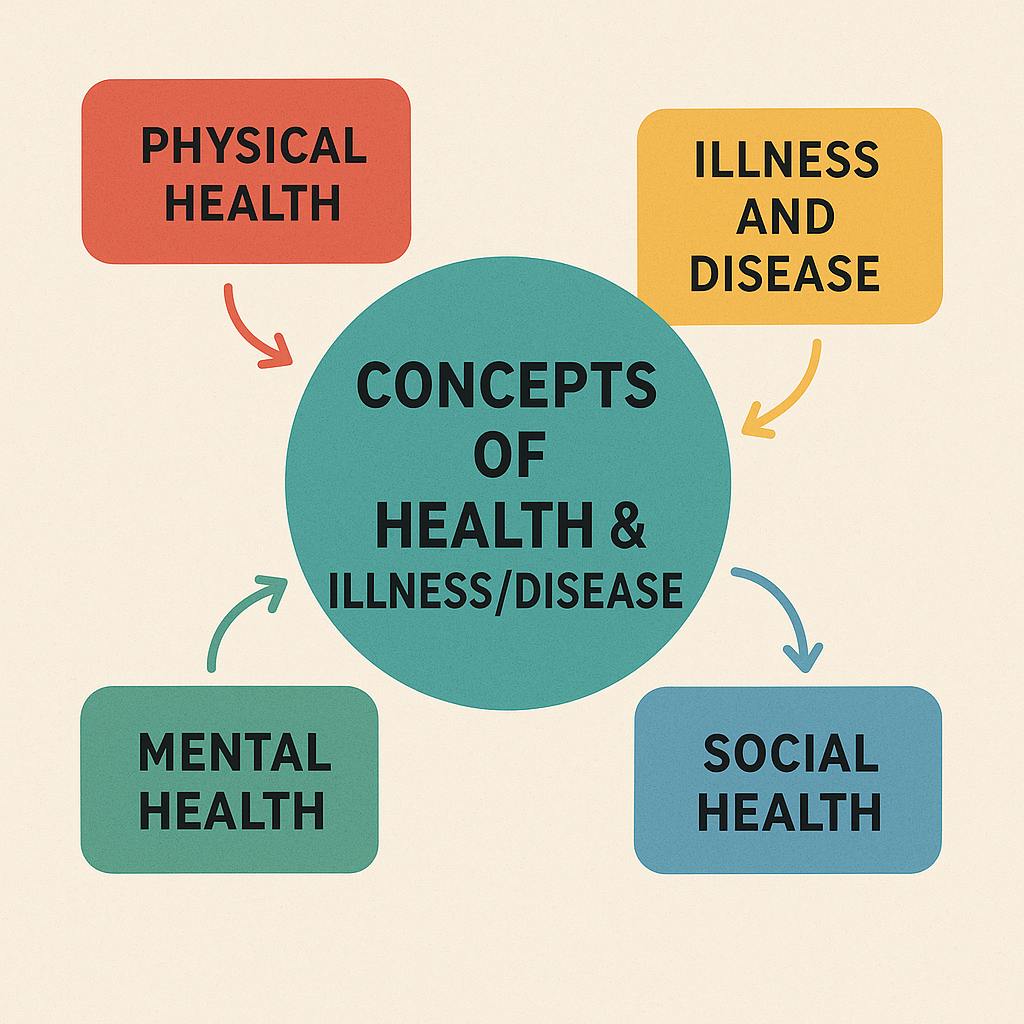
I. CONCEPT OF HEALTH

According to WHO (1948):
“Health is a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity.”
Other Definitions:
- Ottawa Charter for Health Promotion (1986):
“Health is a resource for everyday life, not the objective of living.”
II. DIMENSIONS OF HEALTH
Health is a multidimensional concept. It includes:
| Dimension | Description |
|---|---|
| Physical | Body functions properly, no disease |
| Mental | Positive thinking, emotional balance |
| Social | Ability to maintain good relationships |
| Spiritual | Sense of purpose, inner peace |
| Emotional | Coping with life stress and feelings |
| Vocational | Job satisfaction and productivity |
| Environmental | Safe, clean, and healthy surroundings |
III. DETERMINANTS OF HEALTH
Health is influenced by a combination of internal and external factors:
| Factor | Examples |
|---|---|
| Biological | Age, sex, heredity |
| Environmental | Clean water, sanitation, pollution |
| Lifestyle | Diet, exercise, smoking, alcohol |
| Socioeconomic | Education, income, housing |
| Healthcare Services | Access, availability, quality of care |
| Cultural & Spiritual | Beliefs, practices, traditions |
IV. LEVELS OF HEALTH
Health is not just “healthy” or “sick.” It exists on a continuum:
- Optimum Health – Full functioning and well-being.
- Good Health – No symptoms or problems.
- Average Health – Minor issues but manageable.
- Poor Health – Frequent or chronic illnesses.
- Illness/Disease – Diagnosed pathological state.
- Death – End of life.
V. CONCEPT OF ILLNESS
Illness is a subjective experience of feeling unwell.
It refers to how an individual perceives and responds to a health condition.
Characteristics of Illness:
- Personal experience
- May not have a visible cause
- Varies from person to person
- Includes both physical and emotional discomfort
VI. STAGES OF ILLNESS BEHAVIOR (By Suchman)
| Stage | Description |
|---|---|
| 1. Symptom Experience | Person notices symptoms |
| 2. Assumption of Sick Role | Accepts illness and seeks rest/care |
| 3. Medical Care Contact | Consults healthcare professional |
| 4. Dependent Role | Accepts treatment and care |
| 5. Recovery/ Rehabilitation | Returns to normal or adapted lifestyle |
VII. CONCEPT OF DISEASE

Disease is an objective, medically diagnosable condition with identifiable signs and symptoms.
Key Characteristics:
- Biological or psychological dysfunction
- Diagnosed by healthcare providers
- Often measurable (e.g., blood tests, scans)
VIII. DIFFERENCE BETWEEN ILLNESS AND DISEASE
| Aspect | Illness | Disease |
|---|---|---|
| Definition | Subjective feeling of being unwell | Objective diagnosis of pathology |
| Nature | Personal, emotional experience | Biological, measurable condition |
| Diagnosis | May not always be diagnosed | Requires medical diagnosis |
| Treatment | May need rest/support | Needs clinical management |
IX. CLASSIFICATION OF DISEASES
- By Cause:
- Infectious: TB, Malaria, COVID-19
- Non-infectious: Diabetes, Hypertension
- By Duration:
- Acute: Short duration (flu, cold)
- Chronic: Long duration (asthma, arthritis)
- By Mode of Transmission:
- Communicable: Spread person to person
- Non-communicable: Not spread (cancer)
- By System Affected:
- Respiratory, Gastrointestinal, Cardiovascular, etc.
X. FACTORS AFFECTING ILLNESS BEHAVIOR
- Education level
- Cultural beliefs
- Family support
- Financial condition
- Accessibility of health services
- Past experiences
- Health literacy
XI. NURSING IMPLICATIONS
Community and clinical nurses should:
- Understand cultural and emotional responses to illness
- Educate patients and families
- Promote health-seeking behavior
- Encourage lifestyle modification
- Provide physical and emotional support
CONCLUSION
Understanding the concepts of health, illness, and disease helps nurses to:
- Promote holistic health
- Recognize early signs of illness
- Educate individuals and communities
- Provide patient-centered care
- Reduce stigma and improve quality of life
DIMENSIONS OF HEALTH AND DISEASE
I. DIMENSIONS OF HEALTH
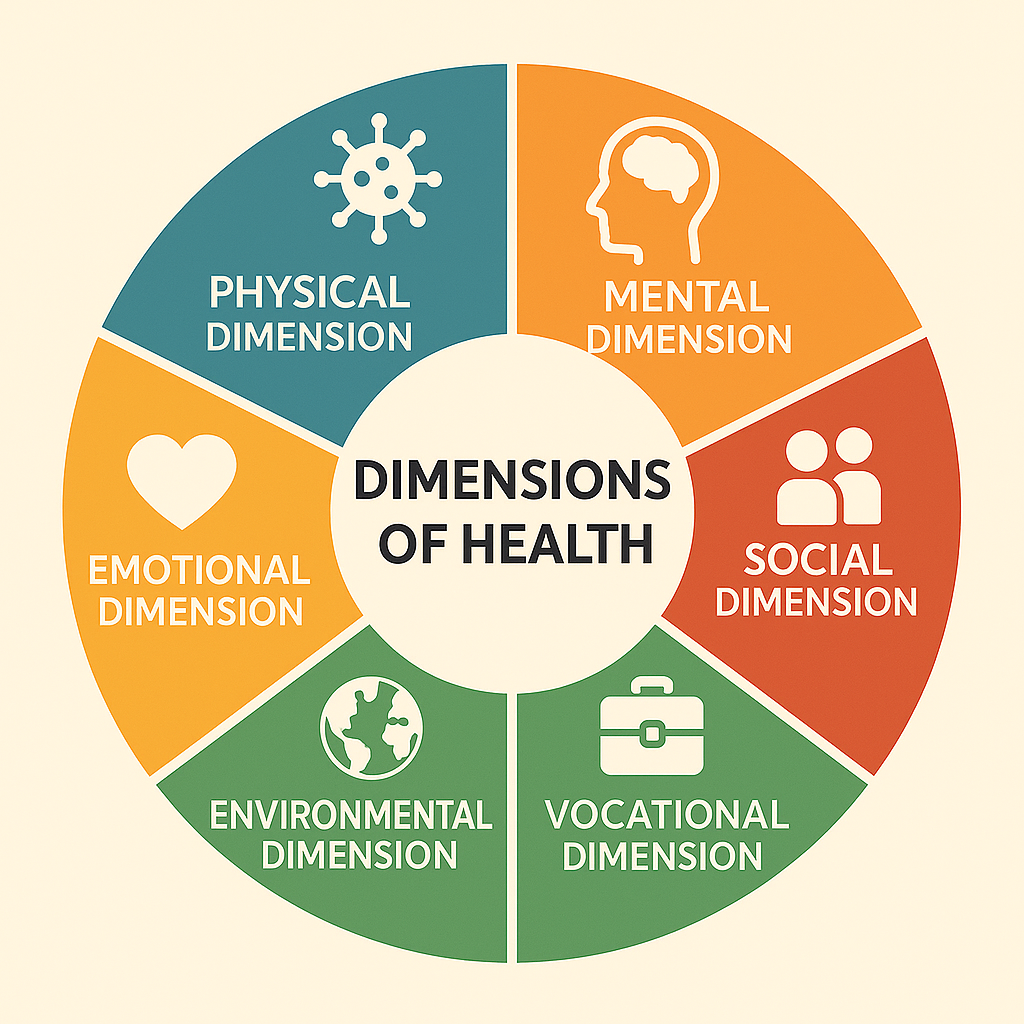
According to the World Health Organization (WHO), health is a multidimensional concept, not just the absence of disease, but a state of complete physical, mental, and social well-being.
Let’s explore the main and extended dimensions of health:
1. Physical Dimension
- Refers to the normal functioning of the body and all organ systems.
- A person is physically healthy if they:
- Are free from diseases or disabilities
- Have good energy levels
- Can perform daily activities without fatigue
Indicators: BMI, pulse rate, BP, lab test reports, strength, immunity
2. Mental Dimension
- Refers to emotional and psychological well-being.
- A mentally healthy person:
- Copes well with stress
- Thinks clearly and logically
- Has good self-esteem and decision-making ability
Examples: Ability to handle pressure, no depression/anxiety, positive thinking
3. Social Dimension
- Refers to the ability to maintain satisfying interpersonal relationships and fulfill social roles.
- A socially healthy person:
- Has good communication skills
- Adjusts in society
- Maintains friendships and family relations
Examples: Participating in community work, cooperation with others
4. Emotional Dimension
- Refers to the ability to recognize, express, and manage emotions such as joy, anger, fear, and sadness.
- Includes emotional intelligence.
Examples: Coping with grief, controlling anger, being empathetic
5. Spiritual Dimension
- Involves the search for meaning and purpose in life.
- It is not limited to religious beliefs but includes inner peace, harmony, and moral values.
Examples: Faith, meditation, yoga, moral values, peace of mind
6. Vocational Dimension
- Refers to job satisfaction and work-life balance.
- A vocationally healthy person:
- Finds purpose in work
- Has good work relationships
- Is productive and happy with their role
Examples: Career growth, satisfaction from nursing profession
7. Environmental Dimension
- Refers to clean, safe, and supportive surroundings that contribute to good health.
- Includes physical, biological, and social environment.
Examples: Clean water, safe housing, pollution-free air, safe community
Summary Table: Dimensions of Health
| Dimension | Key Features |
|---|---|
| Physical | Body fitness, absence of disease |
| Mental | Logical thinking, emotional balance |
| Social | Relationships, community engagement |
| Emotional | Emotional control and expression |
| Spiritual | Faith, inner peace, life purpose |
| Vocational | Job satisfaction, productivity |
| Environmental | Clean and safe surroundings |
II. DIMENSIONS OF DISEASE
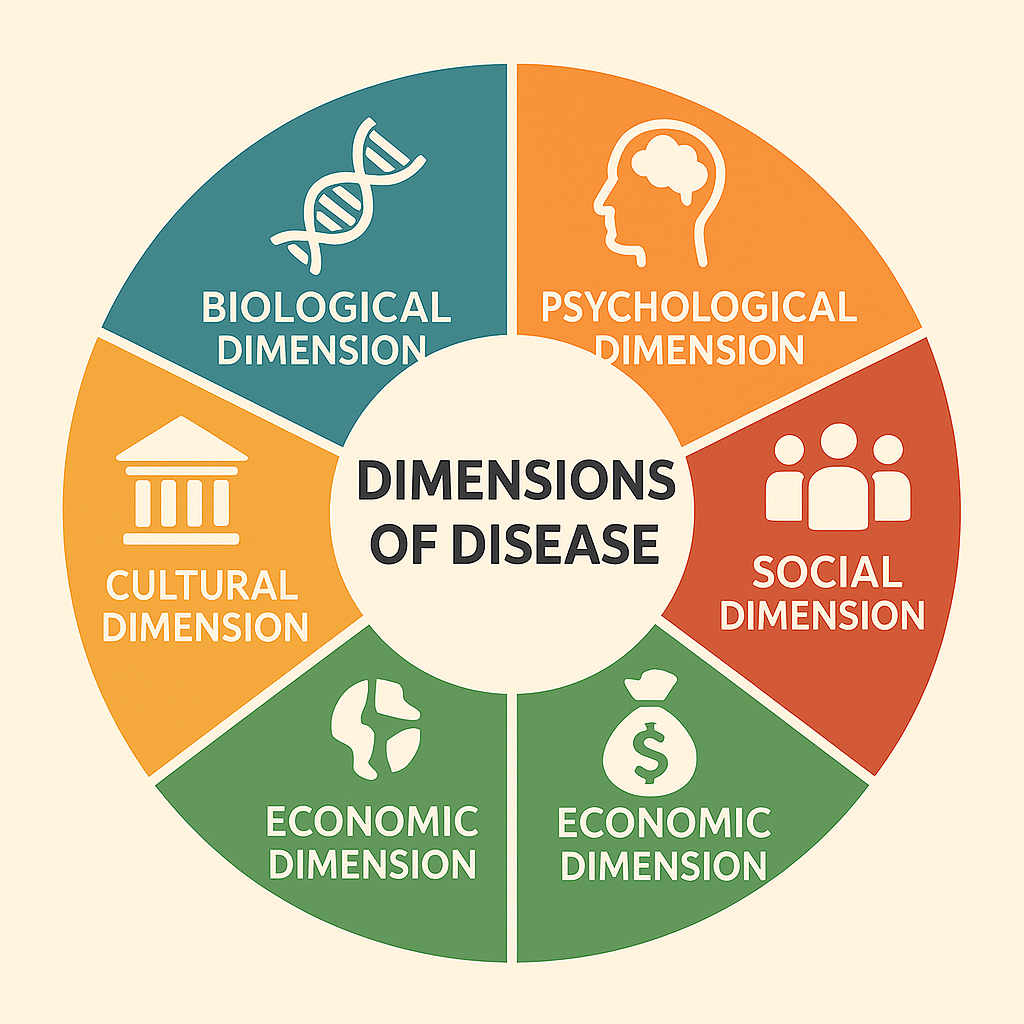
While health has positive dimensions, disease also can be studied across different dimensions. Disease affects multiple aspects of a person’s life.
1. Biological Dimension
- Involves structural or functional abnormalities in the body (organs, cells, tissues).
Examples:
- Bacterial infection causing pneumonia
- Diabetes due to insulin deficiency
2. Psychological (Mental/Emotional) Dimension
- Disease affects emotional well-being or causes psychological disorders.
Examples:
- Depression after chronic illness
- Anxiety due to prolonged treatment
3. Social Dimension
- Long-term illness may cause isolation, social stigma, discrimination, or job loss.
Examples:
- Leprosy or HIV/AIDS stigma
- Exclusion due to mental illness
4. Economic Dimension
- Illness can lead to loss of income, high treatment costs, or poverty.
Examples:
- Family burden due to cancer treatment
- Loss of job due to disability
5. Cultural Dimension
- Cultural beliefs and values affect how disease is perceived and treated.
Examples:
- Belief that mental illness is due to evil spirits
- Use of home remedies instead of medical care
DETERMINANTS OF HEALTH AND DISEASE –
I. WHAT ARE DETERMINANTS?
Determinants are the factors that influence the health status of individuals or populations — they can either promote good health or contribute to disease and ill health.
They include both biological and environmental causes, as well as social, economic, behavioral, and political influences.
II. DETERMINANTS OF HEALTH
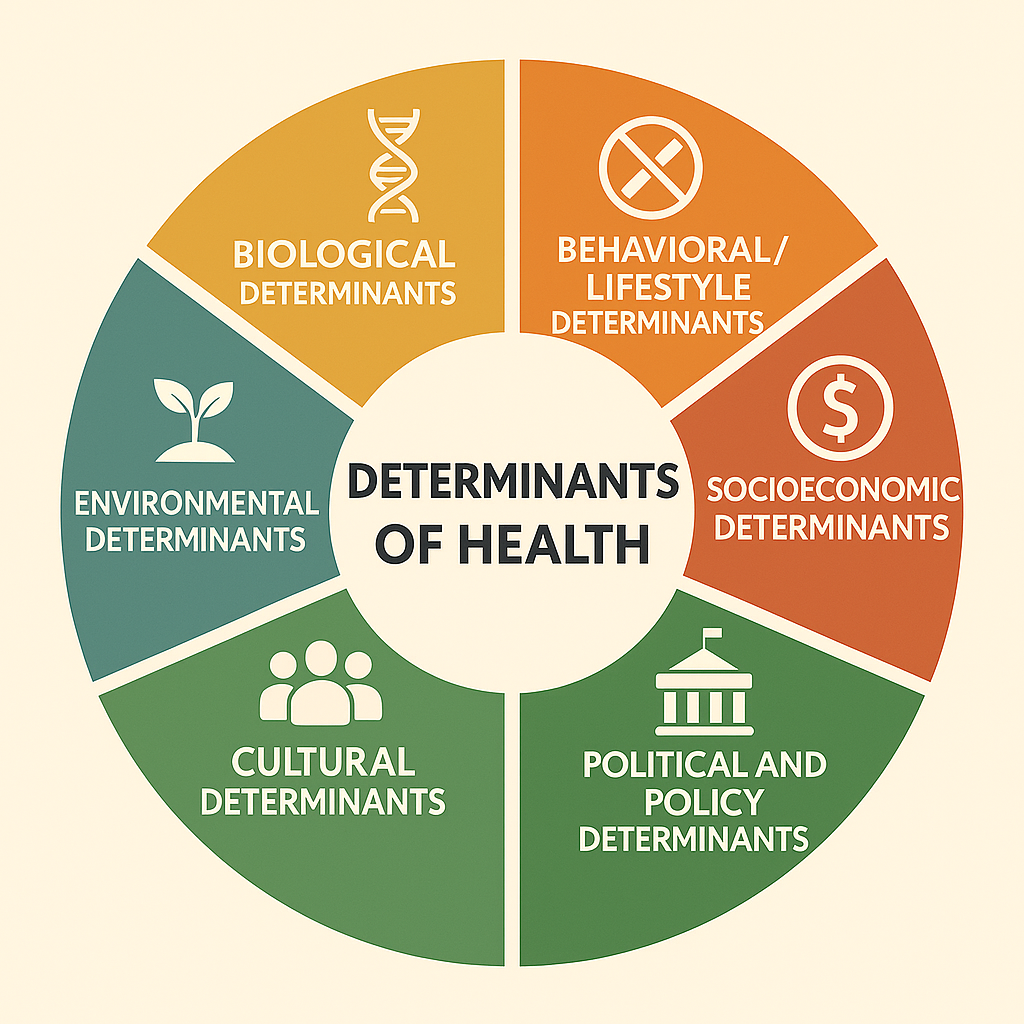
WHO has grouped determinants into the following major categories:
1. Biological Determinants
These are internal to the individual and influence health from birth.
| Examples |
|---|
| Heredity/genetics |
| Age and gender |
| Immunity and hormonal balance |
| Congenital conditions |
| Pregnancy and lactation |
2. Behavioral/Lifestyle Determinants
These are personal habits and behaviors that affect health positively or negatively.
| Positive Behaviors | Negative Behaviors |
|---|---|
| Healthy diet, exercise | Smoking, alcohol, drug abuse |
| Stress management | Physical inactivity |
| Safe sexual practices | Reckless driving |
3. Environmental Determinants
Conditions in our surroundings (physical, chemical, biological, and social) affect health.
| Examples |
|---|
| Clean air and water |
| Sanitation and waste disposal |
| Safe housing and roads |
| Noise and radiation exposure |
| Vector breeding sites (e.g., mosquitoes) |
4. Socioeconomic Determinants
Social and economic status plays a major role in access to health and quality of life.
| Examples |
|---|
| Education level |
| Employment and occupation |
| Income and poverty |
| Social support and community |
| Gender equality |
5. Health Services Determinants
The quality and accessibility of healthcare services directly impact health.
| Examples |
|---|
| Availability of health centers (PHC, CHC) |
| Immunization services |
| Trained health personnel (nurses, doctors) |
| Emergency care and ambulances |
| Health education and awareness programs |
6. Political and Policy Determinants
Government actions and public health policies shape health systems and outcomes.
| Examples |
|---|
| Health insurance schemes (e.g., Ayushman Bharat) |
| Laws on pollution, tobacco, alcohol |
| Regulation of drug prices |
| Public health campaigns and missions |
7. Cultural Determinants
Health beliefs and practices rooted in culture influence health behaviors and decision-making.
| Examples |
|---|
| Beliefs about illness and healing |
| Use of traditional/home remedies |
| Religious fasting |
| Attitudes towards vaccines or mental illness |
III. DETERMINANTS OF DISEASE
Just like health, disease also has multi-factorial causes. These determinants are risk factors that increase the likelihood of disease.
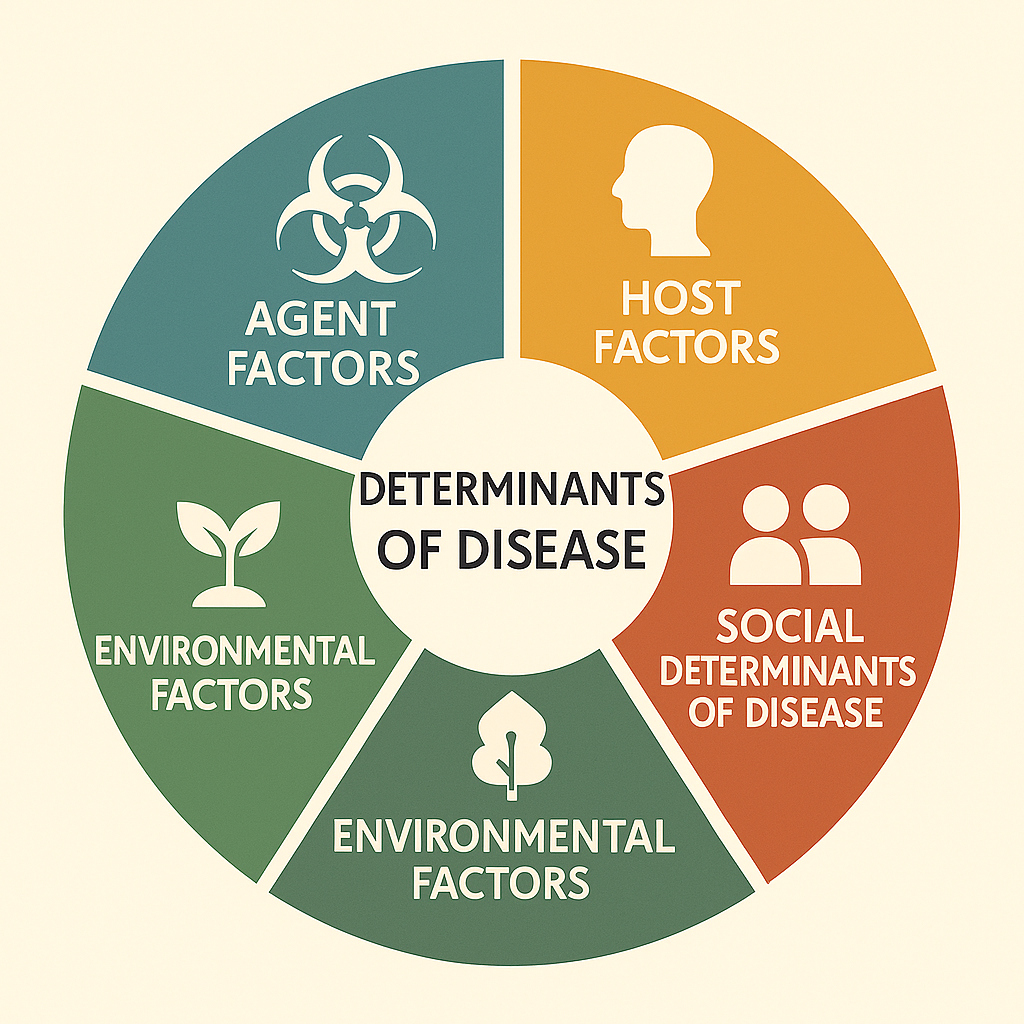
1. Agent Factors
Refers to the biological, chemical, or physical agents that cause disease.
| Examples |
|---|
| Bacteria, viruses, parasites (TB, malaria) |
| Chemicals/toxins (poisoning) |
| Physical agents (heat, radiation, trauma) |
2. Host Factors
Related to the individual’s resistance or vulnerability to disease.
| Examples |
|---|
| Age, sex |
| Immunity |
| Genetic predisposition |
| Nutritional status |
| Lifestyle (smoking, alcohol use) |
3. Environmental Factors
Influence disease transmission and exposure to risks.
| Examples |
|---|
| Contaminated water (cholera) |
| Poor housing, overcrowding (TB) |
| Climate and sanitation |
| Vector breeding sites |
4. Social Determinants of Disease
| Examples |
|---|
| Poverty and unemployment |
| Illiteracy and ignorance |
| Poor access to health services |
| Stigma and discrimination (e.g., HIV) |
IV. INTERRELATIONSHIP – WEB OF CAUSATION
Disease is rarely caused by a single factor—it usually results from an interaction of multiple determinants, also known as the web of causation.
For example:
Heart Disease = Genetics + Poor diet + Smoking + Stress + Lack of exercise
V. IMPORTANCE FOR NURSES AND PUBLIC HEALTH WORKERS
- Identifying risk factors and planning preventive strategies
- Promoting health education on lifestyle modification
- Improving access to health care in vulnerable communities
- Advocating for policy changes that support public health
NATURAL HISTORY OF DISEASE
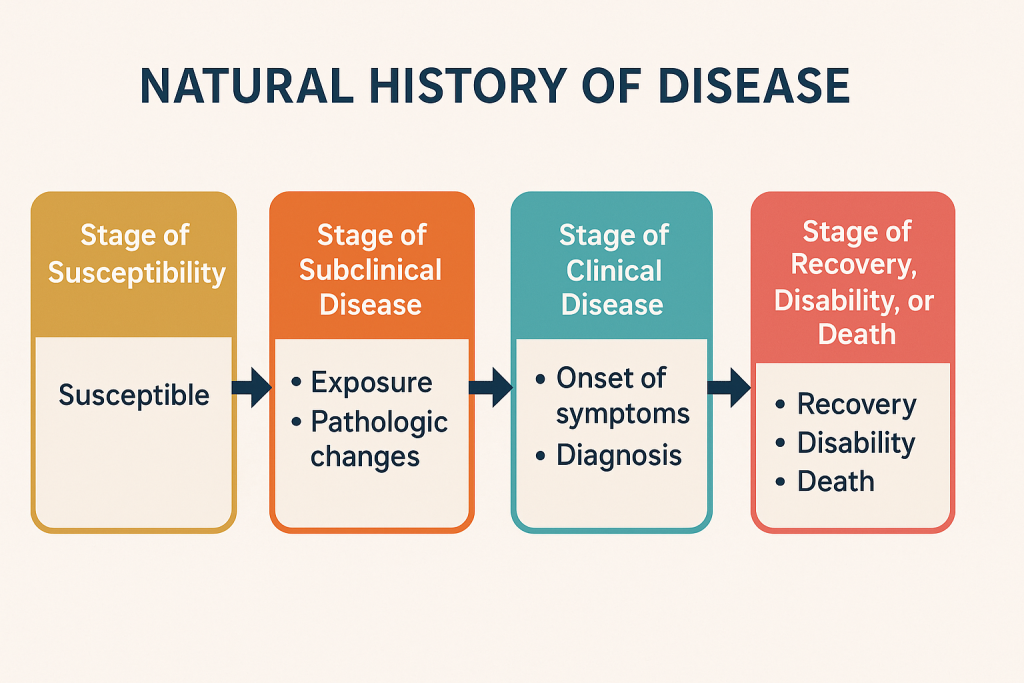
I. DEFINITION
Natural History of Disease refers to the course of a disease from its onset (without medical intervention) to its final outcome — whether recovery, disability, or death.
It helps in understanding how diseases progress within an individual or a population over time, especially in the absence of treatment.
II. IMPORTANCE OF STUDYING NATURAL HISTORY
- To identify stages of disease and plan interventions
- To develop preventive measures (primary, secondary, tertiary)
- To design screening programs at the right time
- To reduce complications and control epidemics
III. STAGES OF NATURAL HISTORY OF DISEASE
It is broadly divided into two phases:
A. Pre-pathogenesis Phase
(Before disease agent enters the host)
Focuses on risk factors and disease prevention.
| Element | Description |
|---|---|
| Agent | Bacteria, virus, parasite, chemical, etc. |
| Host | Individual susceptible to disease |
| Environment | Factors that support transmission or exposure |
At this stage, primary prevention (e.g., immunization, health education) is possible.
B. Pathogenesis Phase
(After the agent has entered the body and disease begins)
Includes both clinical and subclinical phases.
➤ 1. Early Pathogenesis / Subclinical Stage
- Disease process has started
- No signs or symptoms yet
- Disease can be detected only by screening tests
🟢 Example: Positive Mantoux test for TB before symptoms begin
Secondary prevention (e.g., early diagnosis and treatment) is effective here.
➤ 2. Clinical Stage
- Appearance of signs and symptoms
- Disease is now recognizable and diagnosable
- If untreated, may lead to complications
🟢 Example: Cough, fever, night sweats in active pulmonary TB
➤ 3. Complication or Outcome Stage
- Outcome may be:
- Recovery
- Disability
- Death
Tertiary prevention (e.g., rehabilitation, supportive care) is applicable here.
IV. NATURAL HISTORY OF DISEASE – DIAGRAM
A simple flowchart:
scssCopyEditPre-pathogenesis → Subclinical Disease → Clinical Disease → Outcome
↑ ↑ ↑
(Screening) (Signs/Symptoms) (Recovery/Death)
V. EXAMPLE: NATURAL HISTORY OF TUBERCULOSIS (TB)
| Stage | Description |
|---|---|
| Pre-pathogenesis | Exposure to TB bacilli, malnutrition, crowded living |
| Subclinical | Latent TB infection (positive Mantoux) |
| Clinical | Cough, fever, weight loss, sputum positive |
| Complication/Outcome | Recovery with treatment, disability (lung damage), or death |
VI. LEVELS OF PREVENTION AND STAGES OF DISEASE
| Level of Prevention | Applied at Which Stage | Example |
|---|---|---|
| Primary Prevention | Pre-pathogenesis | Vaccination, health education |
| Secondary Prevention | Early pathogenesis | Screening, early treatment |
| Tertiary Prevention | Late pathogenesis/outcome | Rehabilitation, physiotherapy |
VII. NURSING IMPLICATIONS
Community health nurses must:
- Identify risk factors and educate during pre-pathogenesis
- Encourage screening and early diagnosis
- Ensure adherence to treatment
- Provide rehabilitation and home care
LEVELS OF PREVENTION
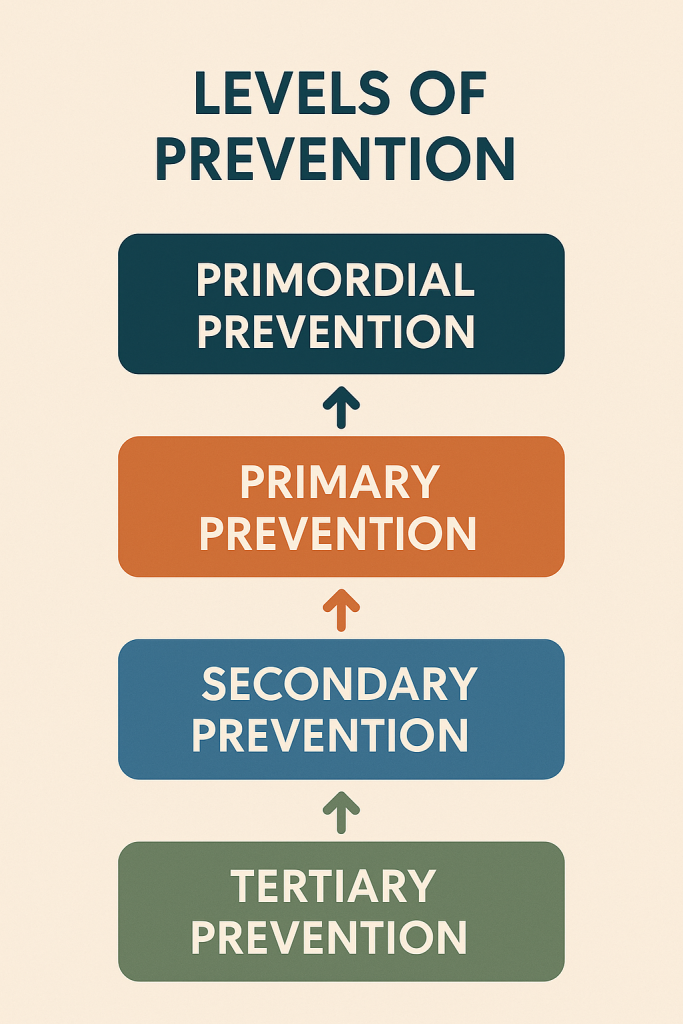
I. DEFINITION
Prevention refers to actions taken to avoid the occurrence of disease, halt its progress, or minimize its impact on individuals and communities.
The concept of levels of prevention was introduced by Leavell and Clark in 1965.
There are four recognized levels of prevention:
- Primordial prevention
- Primary prevention
- Secondary prevention
- Tertiary prevention
Let’s focus on the main three levels: Primary, Secondary, and Tertiary.
II. 1. PRIMARY PREVENTION
Definition:
Actions taken before the onset of disease to prevent its occurrence by eliminating risk factors or enhancing resistance.
Focus:
- Health promotion
- Specific protection
Examples:
| Health Promotion | Specific Protection |
|---|---|
| Health education | Immunization |
| Personal hygiene | Use of mosquito nets |
| Physical exercise | Iron & folic acid tablets |
| Nutrition awareness | Chlorination of water |
| Anti-smoking campaigns | Safe sex practices (condoms) |
Goal:
To keep people healthy and prevent disease before it starts.
III. 2. SECONDARY PREVENTION
Definition:
Actions taken to detect a disease in its early stages and provide prompt treatment to halt its progression.
Focus:
- Early diagnosis
- Prompt and adequate treatment
Examples:
- Screening for:
- Breast cancer (mammography)
- Hypertension (BP check)
- Diabetes (blood sugar test)
- TB (sputum test)
- Early treatment of:
- Tuberculosis
- Pneumonia
- Sexually transmitted infections
Goal:
To detect and treat disease early to prevent complications or spread.
IV. 3. TERTIARY PREVENTION
Definition:
Actions taken after the disease has been diagnosed and treated, aiming to restore function, limit disability, and rehabilitate the individual.
Focus:
- Disability limitation
- Rehabilitation
Examples:
- Physiotherapy after stroke
- Rehabilitation of leprosy patients
- Support for cancer survivors
- Artificial limbs for amputees
- Special education for mentally challenged children
- Counseling for mental illness or substance abuse
Goal:
To reduce suffering, prevent disability, and improve quality of life.
V. COMPARISON TABLE
| Level | Stage of Disease | Focus | Target Group | Examples |
|---|---|---|---|---|
| Primary | Before onset | Prevent disease | Healthy population | Immunization, nutrition |
| Secondary | Early disease | Early detection & treatment | At-risk or suspected cases | Screening, early treatment |
| Tertiary | Established disease | Limit disability, restore function | Patients | Rehab, disability care |
VI. BONUS: PRIMORDIAL PREVENTION (Emerging Concept)
Preventing the development of risk factors themselves.
Examples:
- Promoting healthy eating habits in children
- Avoiding sedentary lifestyle in youth
- Discouraging junk food advertisements
VII. NURSING IMPLICATIONS
Nurses play a vital role in all levels of prevention:
- Primary: Health education, immunization drives, nutrition counseling
- Secondary: Conduct screening camps, assist in early diagnosis
- Tertiary: Provide rehabilitation, emotional support, palliative care
VIII. CONCLUSION
The levels of prevention provide a framework for planning public health and nursing interventions to:
- Reduce disease burden
- Improve early detection
- Minimize disability
- Enhance overall community well-being
HEALTH PROBLEMS (HEALTH PROFILE) OF INDIA
I. INTRODUCTION
India is a diverse country with vast differences in geography, socio-economic status, literacy, and healthcare access. As a result, it faces a triple burden of disease:
- Communicable diseases
- Non-communicable diseases
- Nutritional and environmental health problems
II. MAJOR HEALTH PROBLEMS IN INDIA

1. Communicable Diseases (Infectious diseases)
Despite progress, communicable diseases still pose a major threat.
| Disease | Issues |
|---|---|
| Tuberculosis (TB) | High incidence, MDR-TB cases increasing |
| Malaria | Endemic in many states |
| Dengue, Chikungunya | Rising due to urbanization & poor sanitation |
| HIV/AIDS | Declining but still present in high-risk groups |
| Hepatitis B and C | Common in some regions |
| Diarrheal Diseases | Major cause of death in children under 5 |
| Acute Respiratory Infections (ARIs) | High child morbidity |
| Leprosy | India has the highest number of leprosy cases globally |
2. Non-Communicable Diseases (NCDs)
NCDs are responsible for over 60% of total deaths in India.
| NCD | Details |
|---|---|
| Hypertension | 1 in 4 adults affected |
| Diabetes | India is the diabetes capital of the world |
| Cardiovascular diseases | Leading cause of death |
| Cancer | Breast, cervical, oral cancers most common |
| Stroke | Increasing due to lifestyle changes |
| Mental Illness | Depression, anxiety, addiction underreported |
| Chronic respiratory diseases | Asthma, COPD due to pollution and smoking |
3. Nutritional Problems
| Issue | Details |
|---|---|
| Malnutrition in children | Wasting, stunting, underweight |
| Anemia in women | Especially pregnant and adolescent girls |
| Vitamin and mineral deficiencies | Vitamin A, D, Iodine |
| Obesity and Overnutrition | Growing problem in urban areas |
| Protein-Energy Malnutrition (PEM) | Kwashiorkor and Marasmus still reported |
4. Maternal and Child Health Problems
| Indicator | Current Challenges |
|---|---|
| Maternal Mortality Rate (MMR) | Improved but still high in rural/tribal areas |
| Infant Mortality Rate (IMR) | Due to preterm birth, infection, malnutrition |
| Low birth weight | Linked to poor maternal nutrition |
| High teenage pregnancy | Related to early marriage |
5. Environmental and Occupational Health Problems
| Problem | Impact |
|---|---|
| Air pollution | Major cause of respiratory diseases |
| Water pollution | Leads to diarrhea, cholera, hepatitis |
| Poor sanitation | Contributes to parasitic infections |
| Occupational diseases | Silicosis, asbestosis, pesticide poisoning |
6. Population Explosion
- India has over 1.4 billion people.
- Leads to pressure on:
- Health services
- Housing
- Employment
- Education
- Increases maternal and child health burden
7. Geriatric Health Problems
| Issues | Details |
|---|---|
| Chronic illnesses | Diabetes, hypertension, arthritis |
| Mental health | Depression, loneliness, dementia |
| Neglect and abuse | Social isolation, elder neglect cases rising |
8. Accidents and Injuries
- Road traffic accidents: One of the leading causes of death in youth
- Occupational injuries
- Burns, falls, drowning, and poisoning
9. Mental Health Problems
- Growing due to stress, unemployment, substance abuse
- Suicide rate increasing among youth
- Lack of mental health awareness and stigma
III. HEALTH INDICATORS OF INDIA (Approximate)
| Indicator | Latest Data (may vary slightly) |
|---|---|
| IMR (Infant Mortality Rate) | ~28 per 1,000 live births |
| MMR (Maternal Mortality Ratio) | ~97 per 100,000 live births |
| Life Expectancy | ~70 years |
| Total Fertility Rate (TFR) | ~2.0 (declining trend) |
| Under-5 Mortality Rate | ~36 per 1,000 |
| Malnutrition in under-5 | ~35% stunted |
IV. NATIONAL HEALTH PROGRAMS TO ADDRESS THESE PROBLEMS
- National Health Mission (NHM)
- Reproductive and Child Health (RCH)
- Universal Immunization Program (UIP)
- POSHAN Abhiyaan (Nutrition)
- National TB Elimination Program (NTEP)
- National Mental Health Program (NMHP)
- National Programme for Prevention and Control of NCDs (NP-NCD)
- Ayushman Bharat – PMJAY and Health & Wellness Centres
V. ROLE OF COMMUNITY HEALTH NURSE
- Health education on hygiene, nutrition, lifestyle
- Immunization and MCH care
- Early screening and referral
- Home visits and community mobilization
- Support in national health programs
FOR UNLOCK 🔓 FULL COURSE NOW. MORE DETAILS CALL US OR WATSAPP ON- 8485976407
