BSC SEM 1 UNIT 9 APPLIED NUTRITION AND DIETETICS
UNIT 9 Therapeutic diets
Therapeutic Diets: Introduction and Definition

Introduction to Therapeutic Diets
Food plays a crucial role in maintaining health and managing diseases. A therapeutic diet is a diet that is modified to meet the nutritional needs of individuals with specific medical conditions. It is used as a part of the treatment plan for various diseases and is prescribed by healthcare professionals such as doctors, dietitians, and nurses.
Therapeutic diets help manage symptoms, control diseases, promote healing, and improve overall health. These diets are tailored according to an individual’s nutritional requirements, medical condition, and dietary preferences.
For example, a diabetic diet helps regulate blood sugar levels, while a low-sodium diet is recommended for individuals with hypertension or heart disease.
Definition of Therapeutic Diet
A therapeutic diet is a planned diet that is modified in consistency, nutrient composition, or food selection to meet the specific nutritional requirements of individuals suffering from medical conditions. It is designed to support medical treatment and improve health outcomes.
According to the American Dietetic Association (ADA): “A therapeutic diet is a meal plan that controls the intake of certain foods or nutrients to maintain health, prevent or treat disease, or support recovery.”
Characteristics of a Therapeutic Diet
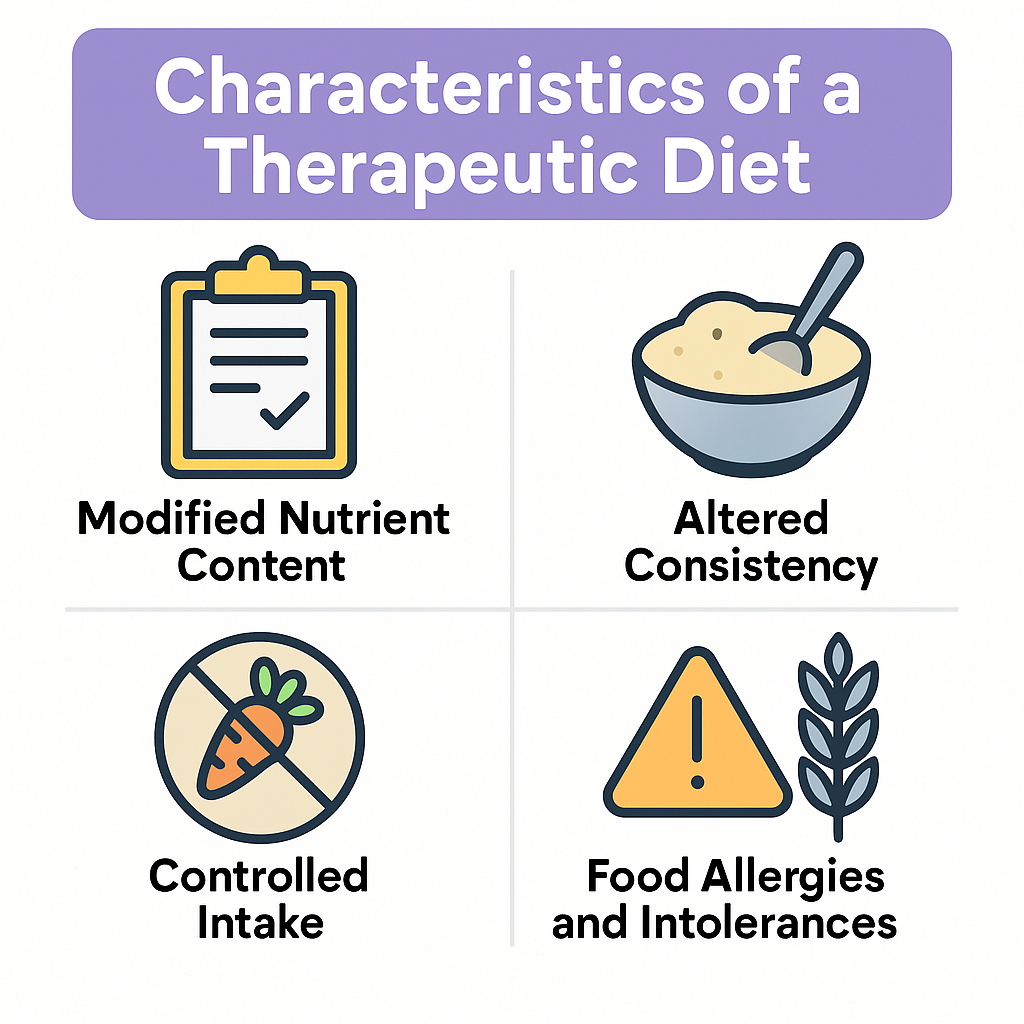
- Modification of Nutrients – Adjusts carbohydrate, protein, fat, vitamins, or minerals.
- Change in Food Texture – May include liquid, soft, or pureed diets.
- Elimination of Certain Foods – Excludes allergenic or harmful foods.
- Caloric Adjustment – Increases or decreases calorie intake based on needs.
- Special Meal Timing – Meals may be spaced or timed for better absorption.
Types of Therapeutic Diets
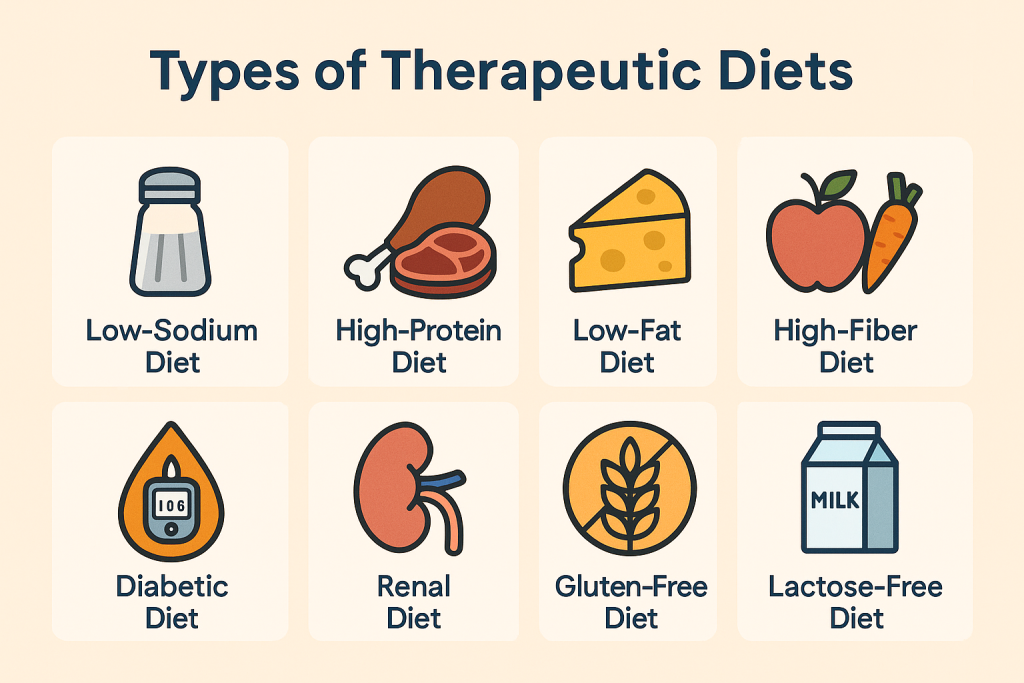
- Clear Liquid Diet – Includes clear fluids like broth, tea, and juice; used for pre/post-surgery and digestive issues.
- Full Liquid Diet – Includes all liquids and semi-liquids such as milk, yogurt, and soups.
- Soft Diet – Soft, easily digestible foods for patients with dental or swallowing issues.
- Bland Diet – Avoids spicy, acidic, or fried foods for digestive disorders.
- High-Protein Diet – Includes eggs, meat, and dairy for healing and muscle-building.
- Low-Protein Diet – Recommended for kidney disease patients to reduce the strain on kidneys.
- Diabetic Diet – Controls carbohydrates and sugars to manage blood glucose levels.
- Low-Sodium Diet – Limits salt intake for hypertension and heart disease patients.
- Low-Fat Diet – Restricts fatty foods to manage cholesterol and heart conditions.
- Renal Diet – Limits sodium, potassium, and phosphorus for kidney disease patients.
- High-Fiber Diet – Promotes digestion and prevents constipation.
- Ketogenic Diet – High-fat, low-carb diet used for epilepsy and weight loss.
- Gluten-Free Diet – Avoids gluten for celiac disease patients.
- Vegetarian or Vegan Diet – Eliminates animal products for health or ethical reasons.
- Enteral and Parenteral Nutrition – Tube feeding or IV nutrition for critically ill patients.
Objectives of Therapeutic Diets

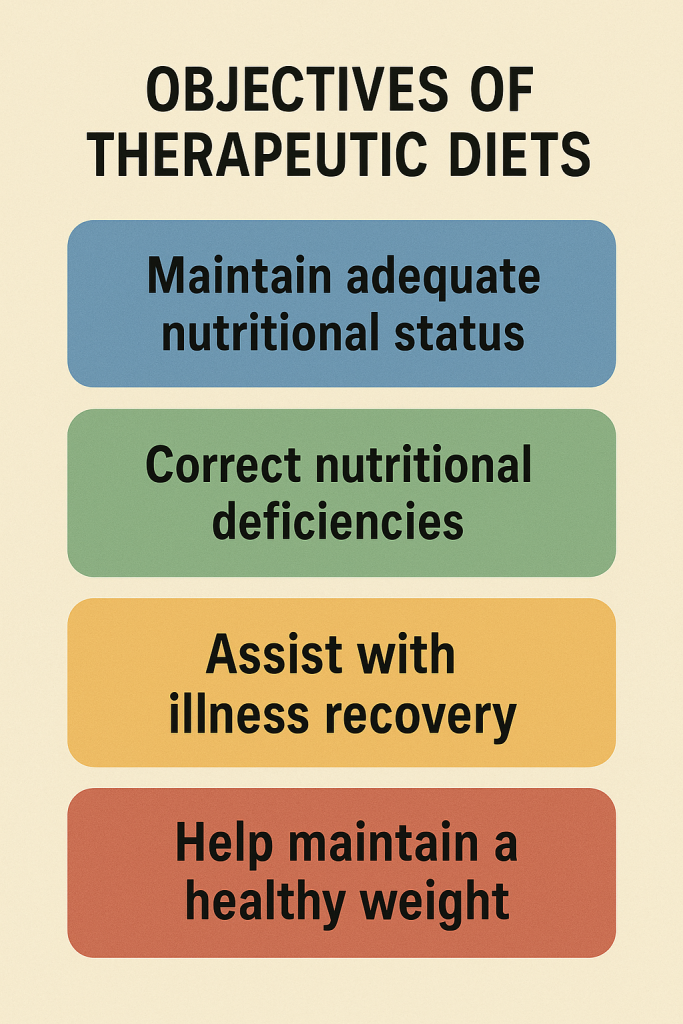
Therapeutic diets are specially designed to meet the nutritional needs of individuals with specific medical conditions. The primary objective is to promote health, aid recovery, and prevent disease progression. The key objectives of therapeutic diets include:
1. To Maintain or Restore Optimal Nutritional Status
- Ensures that the patient receives all essential nutrients to support overall health.
- Prevents malnutrition and deficiencies that may arise due to illness.
2. To Correct Nutritional Deficiencies
- Supplies the body with specific nutrients that may be lacking due to a disease or medical condition.
- Helps replenish vitamins and minerals, such as iron in anemia or calcium in osteoporosis.
3. To Control Disease Progression
- Aims to slow down or prevent the worsening of chronic diseases such as diabetes, kidney disease, or hypertension.
- Example: A low-sodium diet helps in managing hypertension, while a low-protein diet is used for kidney disease.
4. To Aid in Digestion and Absorption
- Modifies the diet to improve digestion and absorption, particularly in patients with gastrointestinal disorders.
- Example: A soft diet is recommended for patients with digestive issues, while a lactose-free diet is suggested for lactose intolerance.
5. To Promote Weight Management
- Helps in weight loss or weight gain, depending on the individual’s condition.
- Example: A high-calorie diet is given for underweight patients, while a calorie-restricted diet is used for obesity management.
6. To Reduce the Workload on Specific Organs
- Adjusts the intake of nutrients to reduce stress on affected organs, such as the liver, kidneys, or heart.
- Example: A low-protein diet in kidney disease minimizes the workload on the kidneys.
7. To Enhance the Body’s Healing Process
- Provides nutrients that promote faster recovery from surgery, injuries, or infections.
- Example: A high-protein diet helps in wound healing and post-operative recovery.
8. To Prevent Food-Drug Interactions
- Ensures that food intake does not interfere with medications.
- Example: Avoiding grapefruit juice with certain cholesterol medications to prevent adverse effects.
9. To Modify Food Consistency for Specific Conditions
- Adapts food texture for patients with swallowing difficulties or dental problems.
- Example: Liquid or pureed diets for stroke patients with dysphagia.
10. To Promote Comfort and Reduce Symptoms
- Helps relieve discomfort caused by certain conditions, such as acidity, bloating, or nausea.
- Example: A bland diet is given to patients with ulcers to avoid irritation.
11. To Prevent or Reduce Risk of Complications
- Reduces the likelihood of complications in high-risk patients, such as those with diabetes, cardiovascular diseases, or metabolic disorders.
- Example: A diabetic diet helps in preventing complications like neuropathy and retinopathy.
12. To Support Mental and Emotional Well-being
- Ensures a well-balanced diet that improves mood and mental health, especially in patients with conditions like depression or eating disorders.
- Example: Omega-3-rich foods are recommended for brain health.
Principles of Therapeutic Diets

A therapeutic diet is carefully planned to meet the specific health needs of an individual. The principles of therapeutic diets help in formulating and implementing effective dietary modifications to promote recovery, manage diseases, and improve overall health.
1. Individualization of the Diet
- Every therapeutic diet should be tailored to meet the patient’s unique nutritional requirements.
- Factors considered include age, gender, weight, medical condition, metabolic rate, and dietary preferences.
2. Modification of Nutrient Content
- Adjustments are made in the quantity of macronutrients (carbohydrates, proteins, fats) and micronutrients (vitamins, minerals).
- Example:
- A high-protein diet for wound healing.
- A low-sodium diet for hypertension.
3. Maintenance of Nutritional Adequacy
- The diet should provide all essential nutrients in balanced proportions to prevent deficiencies.
- Even with restrictions, alternative nutrient sources should be included to ensure a complete diet.
4. Control of Energy Intake (Calories)
- The diet should meet the patient’s energy requirements based on their health condition.
- Example:
- A high-calorie diet for undernourished patients.
- A low-calorie diet for weight management in obesity.
5. Modification of Food Consistency
- The texture of food is altered to accommodate patients with chewing, swallowing, or digestive difficulties.
- Types of consistency modification include:
- Liquid diet (clear or full liquid) for post-surgical patients.
- Soft diet for patients with dental or gastrointestinal issues.
- Pureed diet for stroke patients with swallowing difficulties.
6. Adjustment in Meal Frequency and Timing
- Meals may be modified in frequency, timing, or portion sizes for better digestion and absorption.
- Example:
- Small, frequent meals for patients with peptic ulcers or diabetes.
- Restricted fluid intake for kidney disease patients.
7. Elimination or Restriction of Specific Foods
- Certain foods may be avoided due to allergies, intolerances, or disease conditions.
- Example:
- Gluten-free diet for celiac disease.
- Lactose-free diet for lactose intolerance.
- Low-fat diet for gallbladder disease.
8. Therapeutic Diet Should be Appealing and Acceptable
- The food should be visually appealing, flavorful, and culturally acceptable to encourage compliance.
- Use of natural flavors, colors, and proper presentation enhances patient acceptance.
9. Prevention of Food-Drug Interactions
- Some foods interact with medications, affecting their effectiveness.
- Example:
- Avoiding grapefruit juice with cholesterol-lowering drugs.
- Avoiding high-vitamin K foods (like spinach) in patients taking blood thinners.
10. Modification According to Disease Condition
- The diet should be planned in a way that supports medical treatment.
- Example:
- High-fiber diet for constipation.
- Low-protein diet for kidney failure.
11. Monitoring and Evaluation of Dietary Effects
- Regular monitoring ensures the effectiveness of the diet and allows for adjustments based on the patient’s progress.
- Lab tests, weight changes, and patient feedback help in assessing the impact of the diet.
Modifications in Therapeutic Diets: Consistency and Nutrients
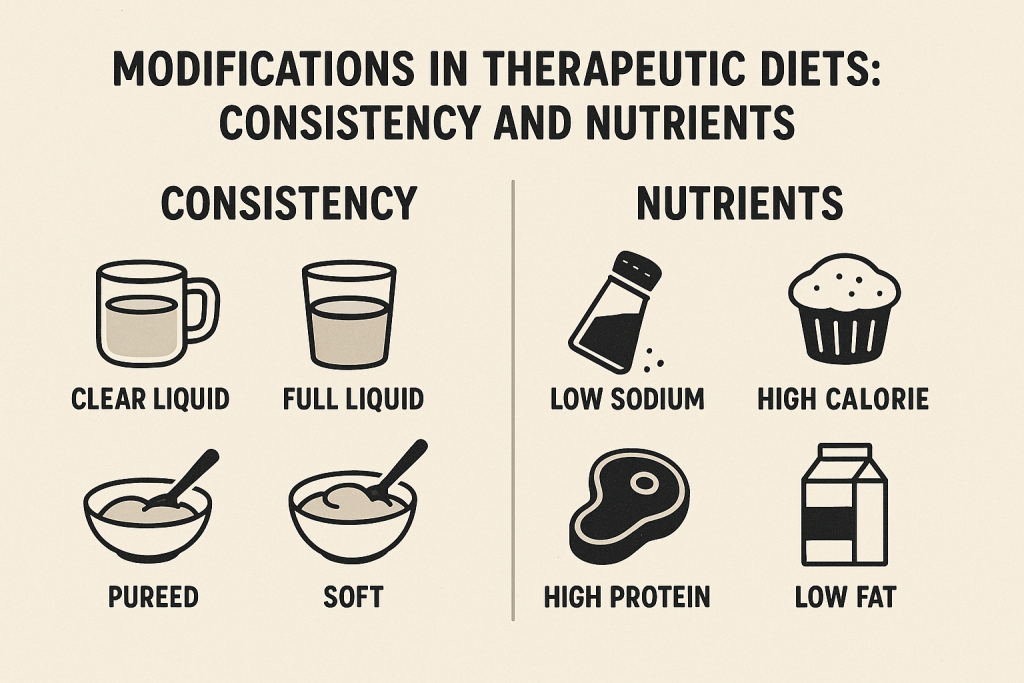
Therapeutic diets are designed to meet specific health needs by modifying consistency and nutrient composition. These modifications help in digestion, absorption, disease management, and overall well-being.
1. Modifications in Consistency of Therapeutic Diets
The texture and consistency of food are adjusted based on a patient’s medical condition, swallowing ability, and digestive health. This is especially important for patients with chewing difficulties, swallowing disorders (dysphagia), post-surgery recovery, or gastrointestinal issues.
Types of Consistency Modifications
1.1 Clear Liquid Diet
✔ Definition:
- A diet consisting only of transparent liquids that leave no residue in the digestive tract.
- Used for patients before or after surgery, during gastrointestinal distress, or as an initial step to reintroduce food.
✔ Examples:
- Water, clear broth, strained fruit juices (apple, cranberry), tea, black coffee, gelatin, electrolyte drinks.
✔ Indications:
- Pre- and post-operative patients.
- Patients with acute vomiting or diarrhea.
- During acute infections or fever.
- Preparation for diagnostic tests (e.g., colonoscopy).
1.2 Full Liquid Diet
✔ Definition:
- Includes all liquids from the clear liquid diet plus opaque and thicker liquids that provide more nutrients.
✔ Examples:
- Milk, yogurt, custards, soups, pureed fruits, pudding, ice cream, nutritional supplements (Ensure, Boost).
✔ Indications:
- Post-surgery recovery when transitioning from clear liquid diet.
- Patients with difficulty chewing/swallowing.
- Gastrointestinal disorders.
1.3 Soft Diet
✔ Definition:
- A diet with easily chewable and digestible foods that are soft in texture.
- Used for patients recovering from surgery, those with dental problems, or mild gastrointestinal conditions.
✔ Examples:
- Soft-cooked rice, mashed potatoes, scrambled eggs, soft vegetables, yogurt, porridge, banana.
✔ Indications:
- Post-surgery patients.
- Patients with difficulty chewing (e.g., dental issues).
- Elderly individuals.
- Patients with digestive disorders (e.g., gastritis, peptic ulcers).
1.4 Pureed Diet
✔ Definition:
- Foods are blended into a smooth, pudding-like consistency to make swallowing easier.
✔ Examples:
- Mashed potatoes, pureed meats, soups, applesauce, blended vegetables.
✔ Indications:
- Patients with swallowing difficulties (dysphagia).
- Stroke patients with impaired swallowing reflex.
- Post-surgical recovery.
1.5 Mechanical Soft Diet
✔ Definition:
- Similar to a soft diet but requires foods to be mechanically altered by chopping, grinding, or blending.
✔ Examples:
- Finely chopped meats, ground vegetables, soft bread, well-cooked pasta.
✔ Indications:
- Patients with jaw surgery or dental issues.
- Patients with neurological disorders affecting chewing/swallowing.
1.6 High-Fiber Diet
✔ Definition:
- Includes fiber-rich foods to promote bowel movement and digestive health.
✔ Examples:
- Whole grains, legumes, fruits with skin, leafy vegetables, nuts.
✔ Indications:
- Patients with constipation.
- Diabetes management.
- Heart disease prevention.
1.7 Low-Residue Diet (Low-Fiber Diet)
✔ Definition:
- Reduces fiber intake to minimize bowel movement frequency.
✔ Examples:
- White rice, refined bread, cooked vegetables, dairy products.
✔ Indications:
- Patients with Crohn’s disease, ulcerative colitis, or gastrointestinal surgery.
2. Modifications in Nutrients of Therapeutic Diets
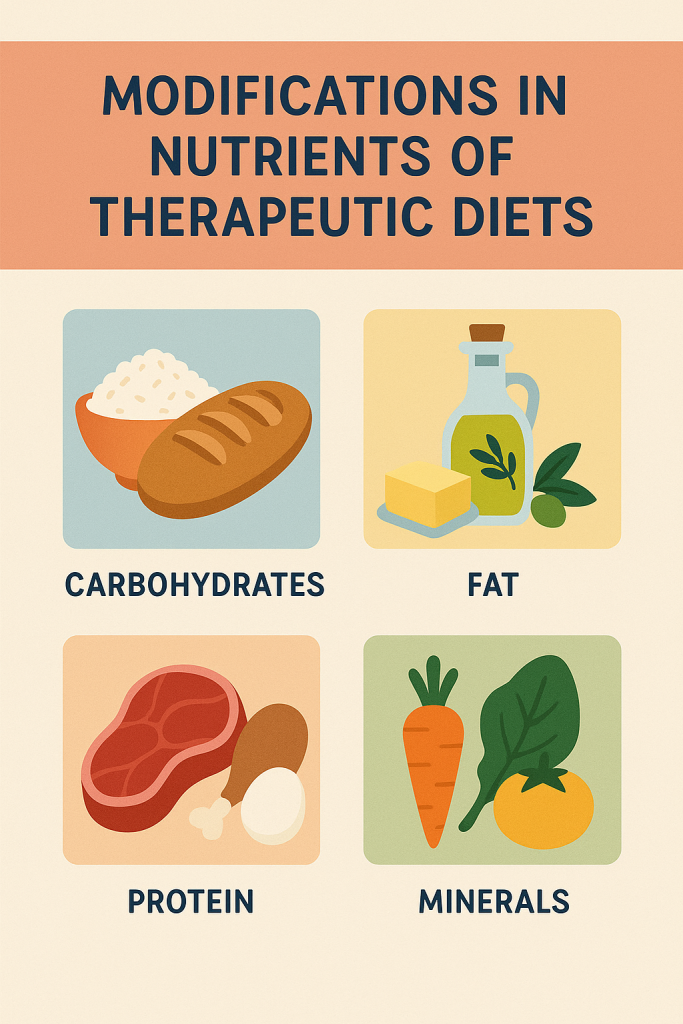
Nutrient modifications help manage diseases by altering the intake of carbohydrates, proteins, fats, vitamins, minerals, and fluids.
2.1 High-Protein Diet
✔ Definition:
- Increases protein intake to support tissue repair, wound healing, and muscle maintenance.
✔ Examples:
- Eggs, lean meats, fish, dairy products, soy, legumes, nuts.
✔ Indications:
- Post-surgical patients.
- Patients with pressure ulcers or burns.
- Cancer patients undergoing chemotherapy.
2.2 Low-Protein Diet
✔ Definition:
- Reduces protein intake to prevent the buildup of nitrogenous waste in the body.
✔ Examples:
- Low-protein grains (corn, rice), fruits, vegetables.
✔ Indications:
- Patients with kidney disease (chronic kidney disease).
- Liver disease (hepatic encephalopathy).
2.3 High-Carbohydrate Diet
✔ Definition:
- Provides energy and prevents muscle breakdown in patients with high metabolic needs.
✔ Examples:
- Whole grains, fruits, potatoes, rice, bread.
✔ Indications:
- Patients with high energy needs (e.g., cancer, hyperthyroidism).
- Post-operative recovery.
2.4 Low-Carbohydrate Diet
✔ Definition:
- Restricts carbohydrate intake to control blood sugar levels.
✔ Examples:
- Non-starchy vegetables, lean meats, nuts, seeds.
✔ Indications:
- Patients with diabetes.
- Weight loss management.
2.5 Low-Fat Diet
✔ Definition:
- Reduces fat intake to manage heart disease and gallbladder disorders.
✔ Examples:
- Lean meats, skim milk, vegetables, fruits, whole grains.
✔ Indications:
- Patients with cardiovascular disease.
- Patients with gallbladder disease.
2.6 High-Fat Diet (Ketogenic Diet)
✔ Definition:
- Increases fat intake while restricting carbohydrates.
✔ Examples:
- Avocado, cheese, nuts, butter, fatty fish.
✔ Indications:
- Used for epilepsy treatment.
- Weight management in certain cases.
2.7 Low-Sodium Diet
✔ Definition:
- Restricts salt intake to prevent fluid retention and high blood pressure.
✔ Examples:
- Fresh fruits, vegetables, unsalted nuts, low-sodium alternatives.
✔ Indications:
- Patients with hypertension.
- Kidney disease patients.
- Heart disease patients.
2.8 High-Calcium Diet
✔ Definition:
- Increases calcium intake to promote bone health.
✔ Examples:
- Dairy products, leafy greens, fortified foods.
✔ Indications:
- Patients with osteoporosis.
- Post-menopausal women.
2.9 Fluid-Restricted Diet
✔ Definition:
- Limits fluid intake to prevent fluid overload.
✔ Examples:
- Measured water intake, avoiding soups and juicy fruits.
✔ Indications:
- Patients with kidney failure.
- Heart failure patients.
2.10 High-Iron Diet
✔ Definition:
- Boosts iron intake to prevent anemia.
✔ Examples:
- Red meat, spinach, beans, fortified cereals.
✔ Indications:
- Patients with anemia.
- Pregnant women.
Feeding Techniques.
Feeding techniques are essential in nursing and healthcare to ensure proper nutrition for patients who cannot eat independently due to medical conditions, disabilities, or recovery from surgery. Proper feeding techniques help prevent complications such as malnutrition, aspiration, choking, and dehydration.
Types of Feeding Techniques
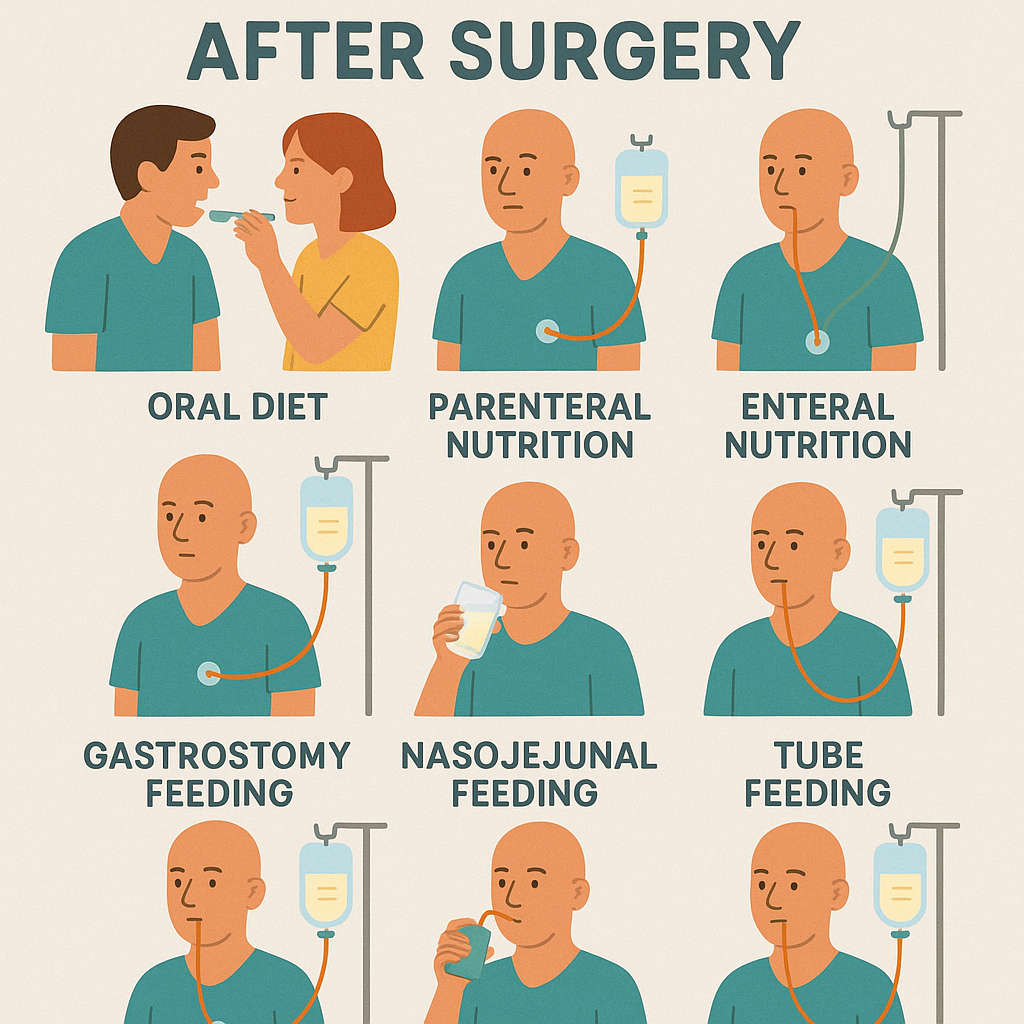
1. Oral Feeding (Self-Feeding & Assisted Feeding)
This is the most common and natural method of feeding, where food is taken through the mouth.
1.1 Self-Feeding
✔ Definition:
- The patient eats independently without assistance.
✔ Considerations:
- Encourage patients to eat slowly and chew properly.
- Provide adaptive utensils if needed (e.g., spoon with grip for arthritis patients).
- Ensure a comfortable sitting position to prevent choking.
1.2 Assisted Oral Feeding
✔ Definition:
- A caregiver or nurse helps the patient eat when they have difficulty feeding themselves.
✔ Indications:
- Patients with neurological disorders (e.g., stroke, Parkinson’s disease).
- Patients with physical disabilities.
✔ Steps for Assisted Feeding:
- Position the patient properly – Keep the patient in an upright sitting position (at least 45–90 degrees).
- Encourage independence – Allow the patient to hold the spoon/cup if possible.
- Use appropriate utensils – Use a soft-tipped spoon for easy feeding.
- Provide small bites and sips – Prevents choking and aspiration.
- Monitor swallowing – Ensure the patient swallows before giving the next bite.
- Observe for signs of difficulty – Coughing, choking, or drooling may indicate swallowing issues.
2. Enteral Feeding (Tube Feeding)
Enteral feeding is used when the patient cannot take food orally but has a functioning gastrointestinal tract.
2.1 Nasogastric (NG) Tube Feeding
✔ Definition:
- A tube is inserted through the nose into the stomach to deliver liquid nutrition.
✔ Indications:
- Patients with swallowing disorders (dysphagia).
- Stroke or unconscious patients.
- Severe malnutrition.
✔ Procedure:
- Verify tube placement (aspiration test or X-ray confirmation).
- Elevate the head of the bed to 30-45 degrees to prevent aspiration.
- Administer liquid feeds using a syringe or feeding pump.
- Flush the tube with water before and after feeding to prevent blockage.
- Monitor for complications (vomiting, diarrhea, tube displacement).
2.2 Orogastric (OG) Tube Feeding
✔ Definition:
- A tube inserted through the mouth into the stomach, used when nasal insertion is not possible.
✔ Indications:
- Neonates and premature babies.
- Patients with nasal obstructions or fractures.
✔ Procedure:
- Similar to NG tube feeding, but the tube is inserted through the mouth instead of the nose.
2.3 Gastrostomy (G-Tube) or Percutaneous Endoscopic Gastrostomy (PEG) Feeding
✔ Definition:
- A tube is surgically placed directly into the stomach through the abdominal wall.
✔ Indications:
- Long-term enteral feeding (e.g., ALS, head & neck cancers).
- Severe swallowing disorders.
✔ Procedure:
- Similar to NG tube feeding but requires sterile care for the insertion site.
2.4 Jejunostomy (J-Tube) Feeding
✔ Definition:
- A feeding tube inserted directly into the jejunum (part of the small intestine).
✔ Indications:
- Patients with severe gastric problems (e.g., gastroparesis, stomach obstruction).
✔ Procedure:
- Similar to PEG feeding but bypasses the stomach.
3. Parenteral Feeding (Intravenous Feeding/TPN)
Parenteral nutrition is used when the gastrointestinal tract is non-functional or cannot be used for feeding.
3.1 Total Parenteral Nutrition (TPN)
✔ Definition:
- A sterile liquid solution containing nutrients is given intravenously through a central vein.
✔ Indications:
- Severe gastrointestinal disorders (e.g., bowel obstruction, Crohn’s disease).
- Severe malnutrition or post-surgical conditions.
✔ Procedure:
- Administered via a central venous catheter (CVC) or peripherally inserted central catheter (PICC line).
- Sterile technique is required to prevent infections.
- Monitor for complications (infection, hyperglycemia, electrolyte imbalance).
4. Specialized Feeding Methods
4.1 Spoon Feeding
✔ Definition:
- Feeding with a spoon for patients who can swallow but cannot feed themselves.
✔ Indications: - Infants, elderly, stroke patients.
✔ Procedure: - Use a small spoon and give food slowly.
- Observe for choking or aspiration signs.
4.2 Cup Feeding
✔ Definition:
- Feeding with a small cup instead of a bottle.
✔ Indications: - Premature babies who cannot suck properly.
✔ Procedure: - Hold the cup at the lips and let the baby sip at their own pace.
4.3 Syringe Feeding
✔ Definition:
- A syringe is used to slowly push liquid food into the mouth.
✔ Indications: - Patients with difficulty swallowing (e.g., after oral surgery).
✔ Procedure: - Administer small amounts at a time to prevent choking.
4.4 Dropper or Paladai Feeding
✔ Definition:
- Using a dropper or paladai (special feeding cup) for feeding small amounts of liquid.
✔ Indications: - Newborns who have difficulty breastfeeding.
Precautions During Feeding
✅ Ensure Proper Positioning – Patients should be seated upright (30-45 degrees) to prevent aspiration.
✅ Monitor for Swallowing Difficulties – Look for coughing, drooling, or difficulty in chewing.
✅ Use the Correct Consistency – Modify food texture (pureed, soft, liquid) as needed.
✅ Prevent Aspiration – Ensure proper pacing, small sips, and checking for food pocketing in the mouth.
✅ Maintain Oral Hygiene – Regular cleaning of the mouth, especially in tube-fed patients.
✅ Check for Food Allergies or Intolerances – Be aware of dietary restrictions.
✅ Monitor for Signs of Malnutrition – Watch for weight loss, weakness, or fatigue.
Diet in Diseases – Obesity
Introduction to Obesity
Obesity is a medical condition characterized by excessive body fat accumulation that increases the risk of various health problems. It is commonly assessed using Body Mass Index (BMI):
- BMI 25-29.9 kg/m² – Overweight
- BMI ≥ 30 kg/m² – Obese
Obesity is associated with diseases such as diabetes, hypertension, heart disease, osteoarthritis, and certain cancers. Proper dietary management is essential in obesity treatment and prevention.
Dietary Management of Obesity
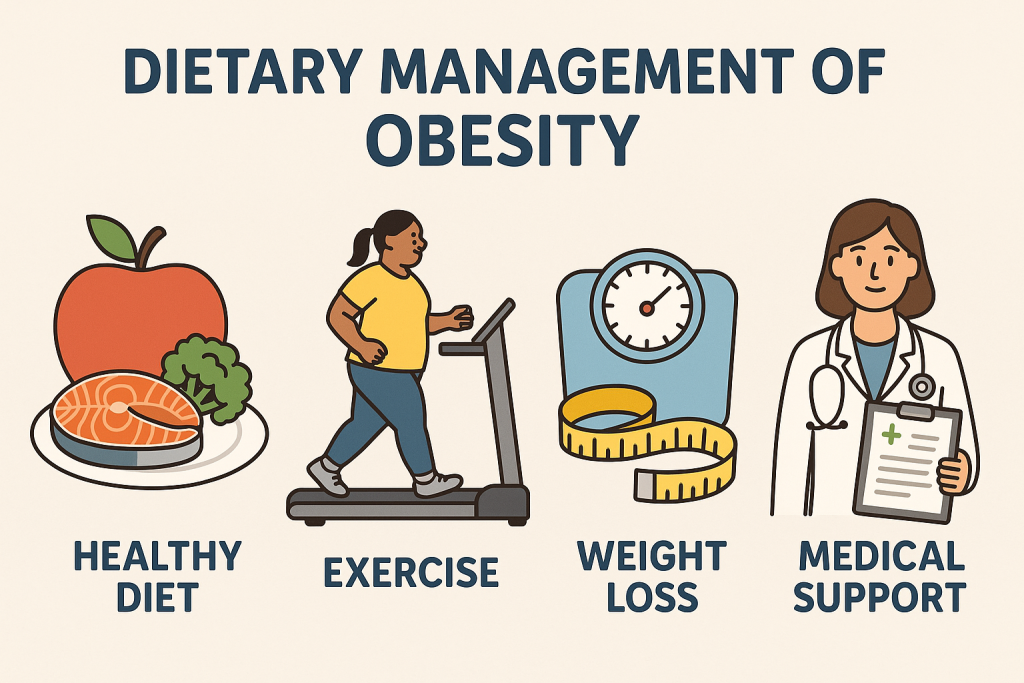
The primary goal of an anti-obesity diet is to promote gradual, sustainable weight loss while ensuring adequate nutrition. The key principles include:
- Caloric Restriction – Reduce total daily caloric intake.
- Balanced Nutrition – Ensure a healthy mix of macronutrients.
- Increased Fiber Intake – Enhances satiety and digestion.
- Reduced Fat and Sugar Intake – Prevents excess calorie consumption.
- Hydration and Meal Planning – Helps control hunger and portion sizes.
Principles of Diet in Obesity Management
1. Caloric Restriction (Energy Balance Control)
- Weight loss occurs when caloric intake is less than energy expenditure.
- A daily 500-1000 kcal deficit can lead to 0.5-1 kg weight loss per week.
- The total calorie requirement depends on age, gender, activity level, and metabolic rate.
- Sedentary – 1200-1500 kcal/day
- Moderate activity – 1500-1800 kcal/day
- Highly active – 1800-2000 kcal/day
2. Macronutrient Distribution
2.1 Low-Fat Diet (Healthy Fat Intake)
✔ Fats should contribute 20-30% of total daily calories
✔ Avoid saturated and trans fats (butter, ghee, fried foods, processed snacks).
✔ Increase healthy fats (avocado, nuts, seeds, olive oil, fish).
📌 Recommended Fat Intake:
- Saturated fat: < 10% of total calories
- Trans fat: Avoid completely
- Omega-3 fatty acids: Include from fish, walnuts, flaxseeds
2.2 Low-Carbohydrate Diet (Quality Carbs)
✔ Focus on complex carbohydrates (whole grains, legumes, vegetables).
✔ Avoid refined carbs and sugars (white rice, white bread, sugary drinks).
✔ Increase fiber intake to 25-30g/day for better digestion and satiety.
📌 Recommended Carbohydrate Intake:
- 45-50% of total calories
- Choose low Glycemic Index (GI) foods to maintain blood sugar levels.
Examples of Healthy Carbs:
✅ Whole wheat, brown rice, quinoa, oats
✅ Green leafy vegetables, carrots, cucumbers
✅ Lentils, chickpeas, beans
2.3 High-Protein Diet for Satiety and Muscle Maintenance
✔ Proteins should contribute 15-20% of total daily calories.
✔ High-protein diets promote fullness and muscle preservation during weight loss.
📌 Recommended Protein Intake:
- 1-1.2g/kg body weight/day
- Lean protein sources – Eggs, chicken, fish, tofu, legumes
✅ Good Protein Sources:
- Animal-based: Lean meat, fish, eggs, low-fat dairy
- Plant-based: Lentils, chickpeas, tofu, soya, nuts
🚫 Avoid processed meats (sausages, bacon, ham) due to high fat and sodium content.
3. High-Fiber Diet for Weight Management
✔ Fiber slows digestion, reduces hunger, and improves gut health.
✔ Daily intake should be 25-30g/day from fruits, vegetables, and whole grains.
✅ Good Fiber Sources:
- Fruits: Apples, pears, oranges, berries
- Vegetables: Broccoli, spinach, carrots
- Whole grains: Brown rice, oats, barley
- Legumes: Beans, lentils, chickpeas
🚫 Avoid low-fiber refined foods (white bread, sugary cereals).
4. Hydration and Meal Timing
✔ Drink 2-3 liters of water per day – Reduces cravings and improves metabolism.
✔ Avoid sugary beverages (soda, energy drinks, fruit juices).
✔ Regular meal timing – Eat small, frequent meals to prevent overeating.
✔ Avoid eating late at night – Helps regulate digestion and weight loss.
Foods to Include and Avoid in Obesity Diet

✅ Foods to Include (Healthy Choices)
- Whole Grains – Brown rice, whole wheat, oats, quinoa
- Lean Proteins – Chicken breast, fish, eggs, legumes
- Vegetables – Green leafy vegetables, carrots, cucumbers
- Fruits – Apples, oranges, pears, berries
- Healthy Fats – Olive oil, nuts, avocado, flaxseeds
- Low-Fat Dairy – Skimmed milk, yogurt, paneer
- Hydration – Herbal teas, coconut water, plain water
🚫 Foods to Avoid (Unhealthy Choices)
- Refined Carbs – White bread, white rice, pasta
- Sugary Foods – Cakes, pastries, chocolates, sweets
- Fried & Processed Foods – French fries, chips, fast food
- High-Calorie Drinks – Sugary sodas, fruit juices, alcohol
- Full-Fat Dairy – Whole milk, cheese, butter
- Red & Processed Meat – Bacon, sausages, ham
Special Diet Plans for Obesity

1. Mediterranean Diet
- High in: Fruits, vegetables, whole grains, nuts, olive oil
- Moderate in: Fish, poultry, dairy
- Low in: Red meat, processed foods
✔ Promotes heart health and sustainable weight loss.
2. DASH Diet (Dietary Approaches to Stop Hypertension)
- Focuses on: Low-sodium, high-fiber, and lean proteins.
✔ Ideal for obese individuals with high blood pressure.
3. Intermittent Fasting (IF)
- 16:8 method – 16 hours fasting, 8 hours eating.
✔ Helps regulate insulin levels and burn fat.
Lifestyle Modifications Along with Diet
✅ Regular Physical Activity – 30-45 minutes of moderate exercise daily.
✅ Portion Control – Use smaller plates and avoid overeating.
✅ Adequate Sleep – Lack of sleep leads to weight gain.
✅ Stress Management – Practice yoga, meditation, and deep breathing.
Diet in Diabetes Mellitus
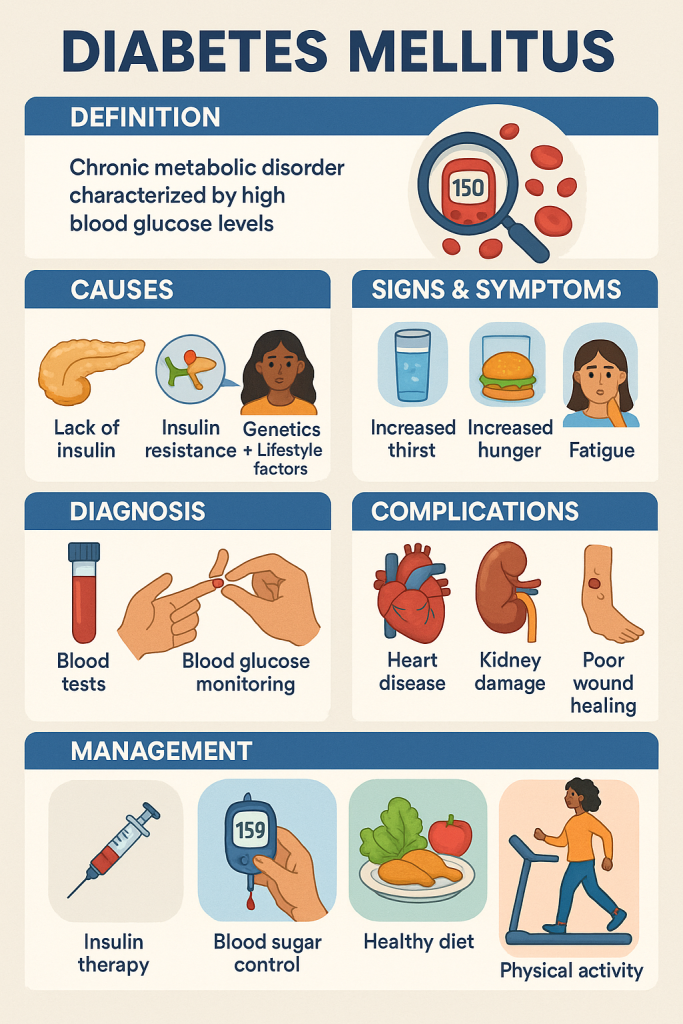
Introduction to Diabetes Mellitus
Diabetes Mellitus is a chronic metabolic disorder characterized by high blood sugar levels (hyperglycemia) due to insufficient insulin production or ineffective insulin utilization. It can lead to complications like heart disease, kidney failure, nerve damage, and vision problems if not managed properly.
Types of Diabetes Mellitus
- Type 1 Diabetes – Autoimmune disorder where the pancreas produces little or no insulin.
- Type 2 Diabetes – Insulin resistance where the body does not use insulin properly.
- Gestational Diabetes – Temporary diabetes during pregnancy.
📌 Dietary management is crucial in controlling blood sugar levels and preventing complications.
Dietary Management in Diabetes Mellitus
The primary goals of a diabetic diet are:
✅ Control blood sugar levels (Glycemic Control)
✅ Maintain a healthy weight
✅ Prevent diabetes-related complications
✅ Ensure balanced nutrition
Principles of Diabetic Diet
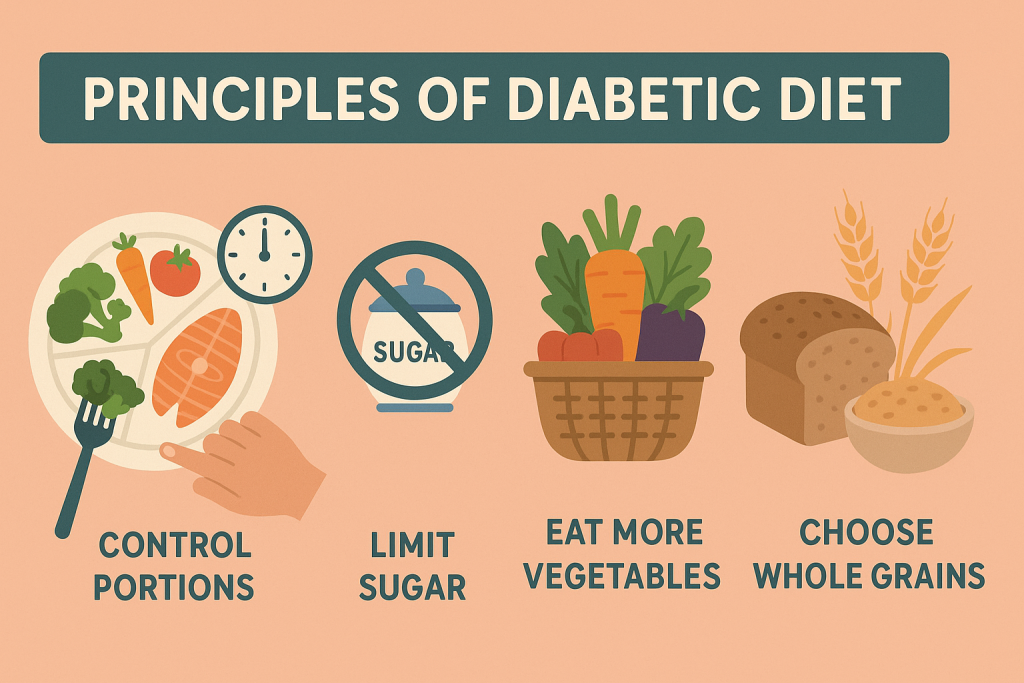
1. Balanced Macronutrient Intake
A well-balanced diet includes controlled portions of carbohydrates, proteins, and fats.
✔ Carbohydrates: 45-50% of daily calories
✔ Proteins: 15-20% of daily calories
✔ Fats: 20-30% of daily calories
2. Carbohydrate Control and Glycemic Index (GI) Management
✔ Avoid refined carbohydrates – White bread, white rice, sweets.
✔ Choose high-fiber complex carbohydrates – Whole grains, legumes, vegetables.
✔ Low-Glycemic Index (GI) foods should be preferred to maintain stable blood sugar levels.
📌 Glycemic Index Categories
- Low GI (Good for Diabetes) – Below 55 (Brown rice, whole wheat, green leafy vegetables)
- Medium GI – 56-69 (Sweet potatoes, corn, bananas)
- High GI (Avoid) – Above 70 (White bread, sugar, soft drinks)
✅ Recommended Carb Sources:
- Whole wheat, brown rice, oats, quinoa
- Green leafy vegetables, carrots, cucumbers
- Lentils, chickpeas, kidney beans
🚫 Avoid: Sugary drinks, refined flour, white rice, sweets.
3. High-Fiber Diet for Blood Sugar Control
✔ Fiber slows glucose absorption, preventing blood sugar spikes.
✔ 25-30g fiber per day is recommended for diabetics.
✅ Good Fiber Sources:
- Fruits: Apples, pears, oranges, guava
- Vegetables: Spinach, broccoli, carrots
- Whole grains: Brown rice, quinoa, oats
- Legumes: Beans, chickpeas, lentils
🚫 Avoid: Processed and low-fiber foods like white bread and fast food.
4. Protein-Rich Diet for Muscle Health
✔ Helps maintain stable blood sugar levels.
✔ 1-1.2g/kg body weight per day is recommended.
✅ Good Protein Sources:
- Animal-based: Lean chicken, fish, eggs, low-fat dairy
- Plant-based: Lentils, chickpeas, tofu, soya, nuts
🚫 Avoid: Red meat, processed meats (bacon, sausage).
5. Healthy Fat Intake
✔ Helps regulate cholesterol and heart health.
✔ Choose unsaturated fats over saturated and trans fats.
✅ Healthy Fats:
- Olive oil, nuts, avocado, flaxseeds
- Fatty fish (salmon, mackerel)
🚫 Avoid: Butter, fried foods, processed oils.
6. Hydration and Meal Planning
✔ Drink 2-3 liters of water daily to flush out excess glucose.
✔ Avoid sugary drinks like soft drinks, energy drinks.
✔ Regular meal timings – Eating at fixed intervals prevents sugar spikes.
✔ Small, frequent meals (every 3-4 hours) help maintain stable blood sugar levels.
Recommended Foods and Foods to Avoid in Diabetes
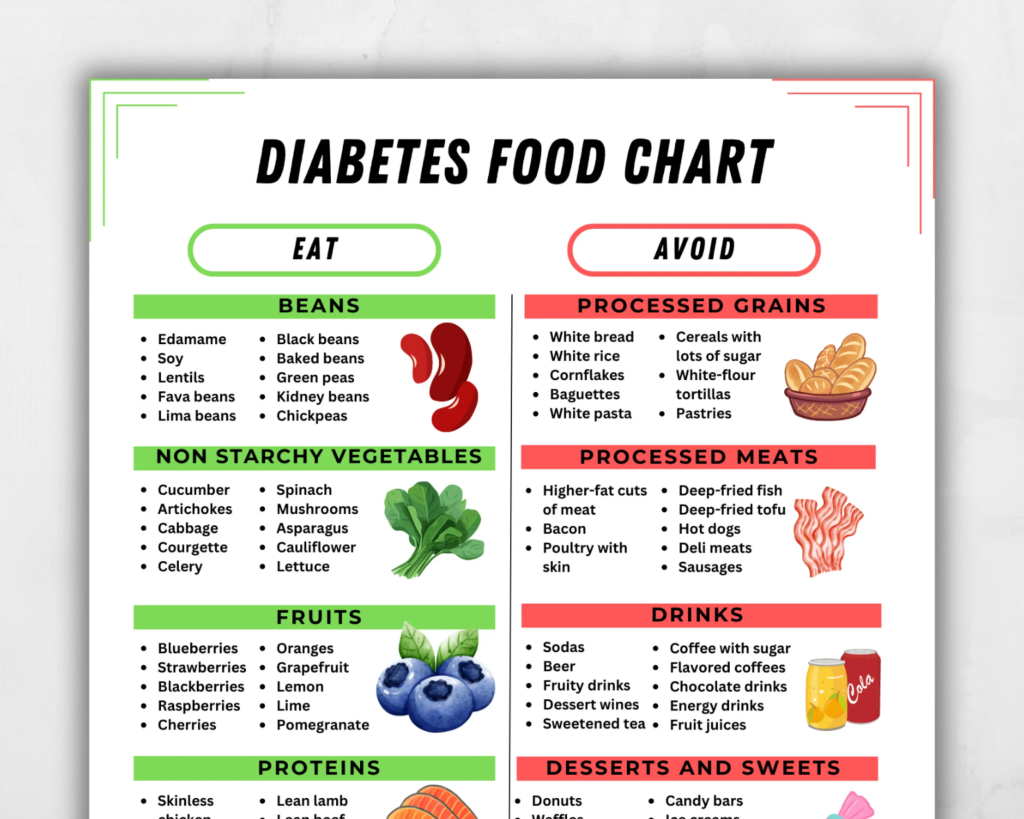
✅ Foods to Include (Diabetic-Friendly Diet)
- Whole Grains – Brown rice, whole wheat, quinoa
- Lean Proteins – Chicken breast, fish, eggs, legumes
- Vegetables – Spinach, carrots, broccoli
- Fruits – Apples, guava, oranges, berries
- Healthy Fats – Olive oil, nuts, avocado
- Low-Fat Dairy – Skimmed milk, yogurt, paneer
- Hydration – Herbal teas, coconut water, plain water
🚫 Foods to Avoid (Unhealthy Choices for Diabetics)
- Refined Carbs – White bread, white rice, pasta
- Sugary Foods – Cakes, pastries, chocolates, sweets
- Fried & Processed Foods – French fries, chips, fast food
- High-Calorie Drinks – Sugary sodas, fruit juices, alcohol
- Full-Fat Dairy – Whole milk, cheese, butter
- Red & Processed Meat – Bacon, sausages, ham
Special Diet Plans for Diabetes
1. Mediterranean Diet for Diabetes
- High in: Whole grains, vegetables, fish, nuts, olive oil
- Moderate in: Poultry, dairy
- Low in: Red meat, processed foods
✔ Promotes heart health and stable blood sugar levels.
2. DASH Diet (Dietary Approaches to Stop Hypertension)
- Low-sodium, high-fiber diet beneficial for diabetics with high BP.
3. Low-Carbohydrate Diet (Keto Diet – Limited Use in Diabetes)
- Reduces sugar intake but requires medical supervision.
Lifestyle Modifications Along with Diet
✅ Regular Physical Activity – 30-45 minutes of walking, yoga, or aerobic exercises.
✅ Weight Management – Maintain a healthy BMI (18.5-24.9 kg/m²).
✅ Adequate Sleep – Helps regulate insulin sensitivity.
✅ Stress Management – Practice yoga, meditation, and deep breathing.
Diet in Cardiovascular Diseases (CVD)
Introduction to Cardiovascular Diseases (CVD)
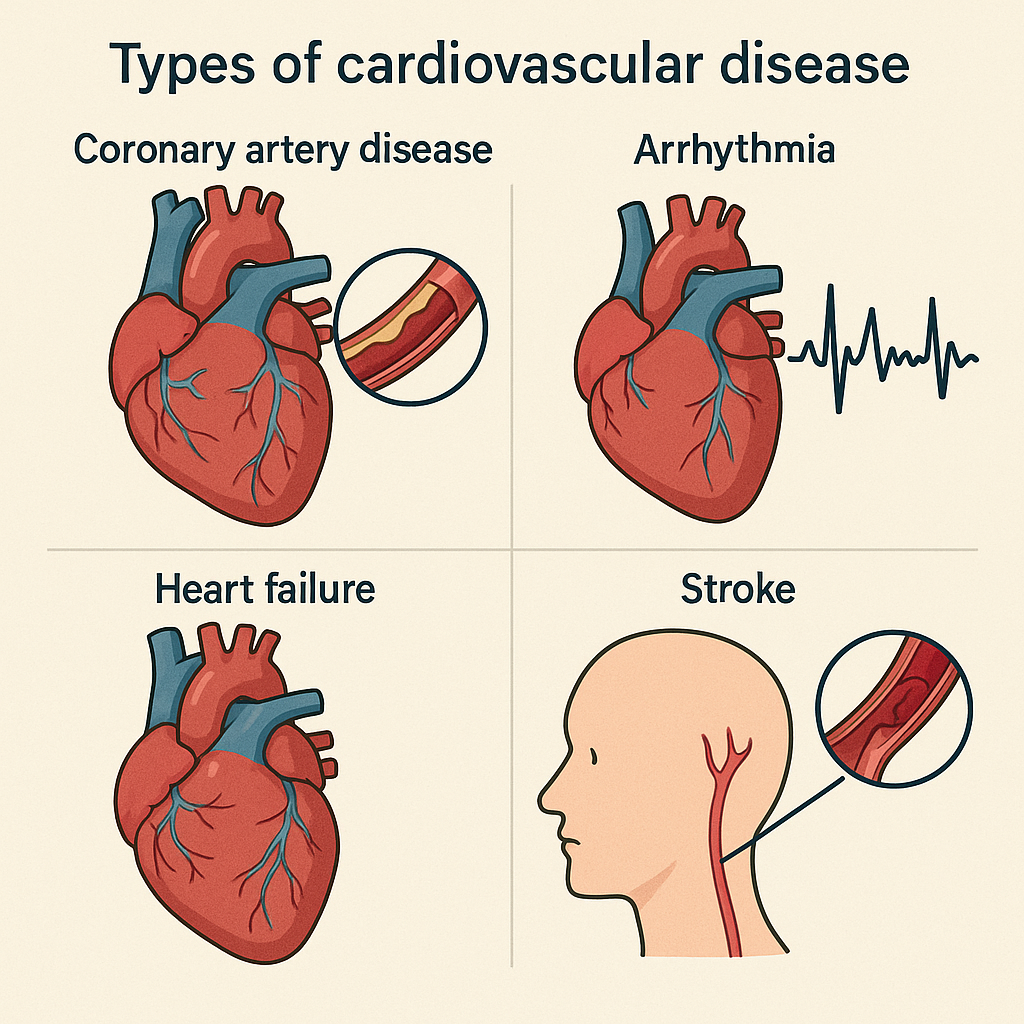
Cardiovascular diseases (CVD) refer to a group of disorders affecting the heart and blood vessels. They include:
- Coronary artery disease (CAD) – Blockage in heart arteries.
- Hypertension (High Blood Pressure) – Increased pressure in arteries.
- Heart failure – Weak heart pumping ability.
- Stroke – Blockage or rupture in brain arteries.
- Peripheral artery disease (PAD) – Narrowing of arteries in limbs.
CVDs are leading causes of death worldwide, but diet plays a crucial role in prevention and management. A heart-healthy diet can reduce risk factors like high cholesterol, high blood pressure, obesity, and diabetes.
Dietary Goals for Cardiovascular Disease (CVD) Management
✅ Lower LDL (bad cholesterol) and increase HDL (good cholesterol).
✅ Control blood pressure.
✅ Reduce inflammation and oxidative stress.
✅ Maintain a healthy weight.
✅ Regulate blood sugar levels in diabetic patients.
Principles of a Heart-Healthy Diet
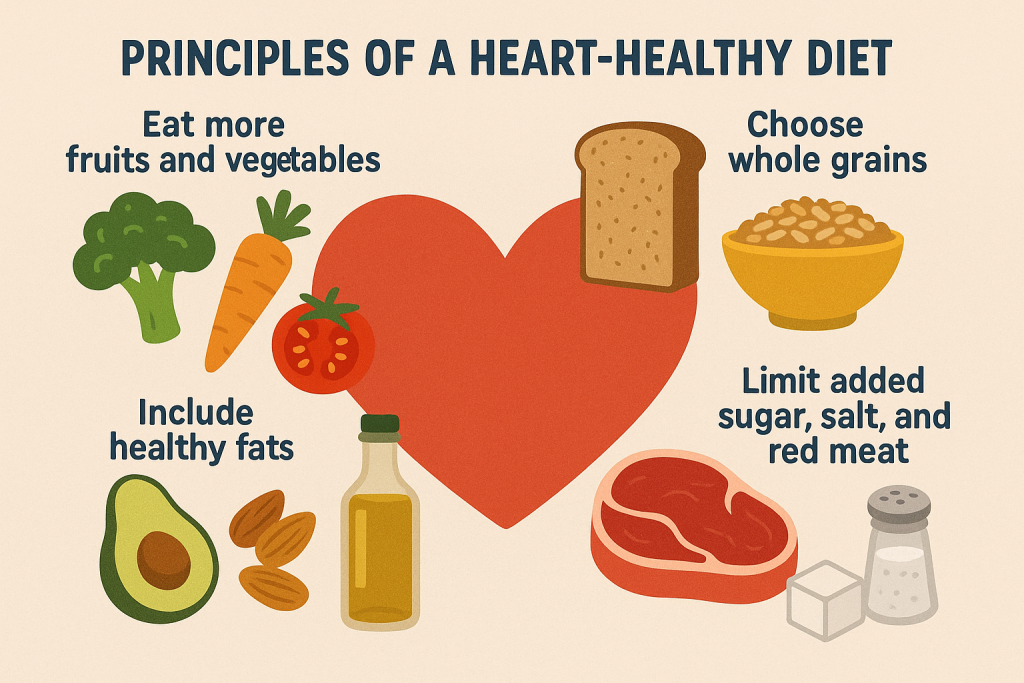
1. Reduce Saturated & Trans Fats (Heart-Healthy Fats Instead!)
✔ Avoid saturated fats from butter, ghee, full-fat dairy, and fatty meats.
✔ Completely avoid trans fats (found in processed foods, margarine, fast food).
✔ Increase healthy fats (monounsaturated and polyunsaturated fats).
✅ Healthy Fat Sources:
- Olive oil, canola oil, avocado, almonds, walnuts.
- Fatty fish (salmon, mackerel, tuna) rich in omega-3 fatty acids.
- Flaxseeds and chia seeds.
🚫 Avoid: Fried foods, processed snacks, full-fat dairy, red meat.
2. Low-Sodium Diet for Blood Pressure Control
✔ Excess sodium leads to high blood pressure (hypertension).
✔ Limit sodium intake to < 1500 mg/day.
✅ Low-Sodium Foods:
- Fresh fruits and vegetables.
- Home-cooked meals (avoid processed foods).
- Herbs and spices (instead of salt).
🚫 Avoid High-Sodium Foods:
- Salted snacks, pickles, processed meats, canned foods, fast food.
3. Increase Fiber Intake (Lowers Cholesterol & Controls Weight)
✔ Fiber helps reduce LDL (bad cholesterol) and improves digestion.
✔ Target: 25-30g of fiber daily.
✅ High-Fiber Foods:
- Whole grains (brown rice, oats, quinoa).
- Fruits (apples, pears, oranges, berries).
- Vegetables (broccoli, carrots, spinach).
- Legumes (lentils, beans, chickpeas).
🚫 Avoid: White bread, white rice, sugary cereals.
4. Lean Proteins for Heart Health
✔ Protein is essential but should be from heart-friendly sources.
✅ Heart-Healthy Protein Sources:
- Plant-based proteins: Lentils, beans, tofu, soya.
- Lean animal proteins: Chicken, turkey, fish.
- Low-fat dairy: Skimmed milk, yogurt, cottage cheese (paneer).
🚫 Avoid: Red meat, processed meats (bacon, sausages), full-fat dairy.
5. Healthy Carbohydrate Choices (Avoid Refined Carbs & Sugars)
✔ Avoid simple carbohydrates that cause blood sugar spikes and weight gain.
✔ Choose whole grains over refined grains.
✅ Healthy Carbs:
- Whole grains (whole wheat, brown rice, quinoa).
- Vegetables (broccoli, carrots, green leafy vegetables).
- Legumes (lentils, chickpeas, kidney beans).
🚫 Avoid:
- White rice, white bread, pastries, sweets.
- Sugar-laden foods like sodas, candies, fruit juices.
6. Antioxidant-Rich Diet to Reduce Inflammation
✔ Antioxidants protect the heart and reduce damage from free radicals.
✔ Include vitamin C, vitamin E, and polyphenols.
✅ Sources of Antioxidants:
- Berries (blueberries, strawberries).
- Dark leafy greens (spinach, kale).
- Nuts & seeds (almonds, sunflower seeds).
- Green tea & dark chocolate (in moderation).
7. Hydration and Alcohol Moderation
✔ Drink at least 2-3 liters of water per day.
✔ Limit alcohol intake – Excess alcohol raises blood pressure and cholesterol.
🚫 Avoid: Sugary sodas, energy drinks, excessive caffeine.
Recommended Foods and Foods to Avoid in CVD Diet

✅ Foods to Include (Heart-Healthy Choices)
- Whole Grains – Brown rice, oats, quinoa, whole wheat.
- Lean Proteins – Chicken, fish, tofu, legumes, low-fat dairy.
- Healthy Fats – Olive oil, avocado, nuts, fatty fish.
- Vegetables – Leafy greens, carrots, bell peppers.
- Fruits – Apples, oranges, guava, berries.
- Low-Sodium Foods – Freshly cooked meals, herbs, and spices.
- Hydration – Water, herbal teas, coconut water.
🚫 Foods to Avoid (Unhealthy for the Heart)
- Fried & Processed Foods – Chips, French fries, fast food.
- Refined Carbs & Sugars – White bread, sweets, sugary drinks.
- High-Sodium Foods – Canned soups, processed meats, salty snacks.
- Unhealthy Fats – Butter, ghee, margarine, full-fat dairy.
- Red Meat & Processed Meats – Bacon, sausages, ham.
- Excess Alcohol & Sugary Beverages – Soft drinks, alcohol, energy drinks.
Special Diet Plans for Cardiovascular Health
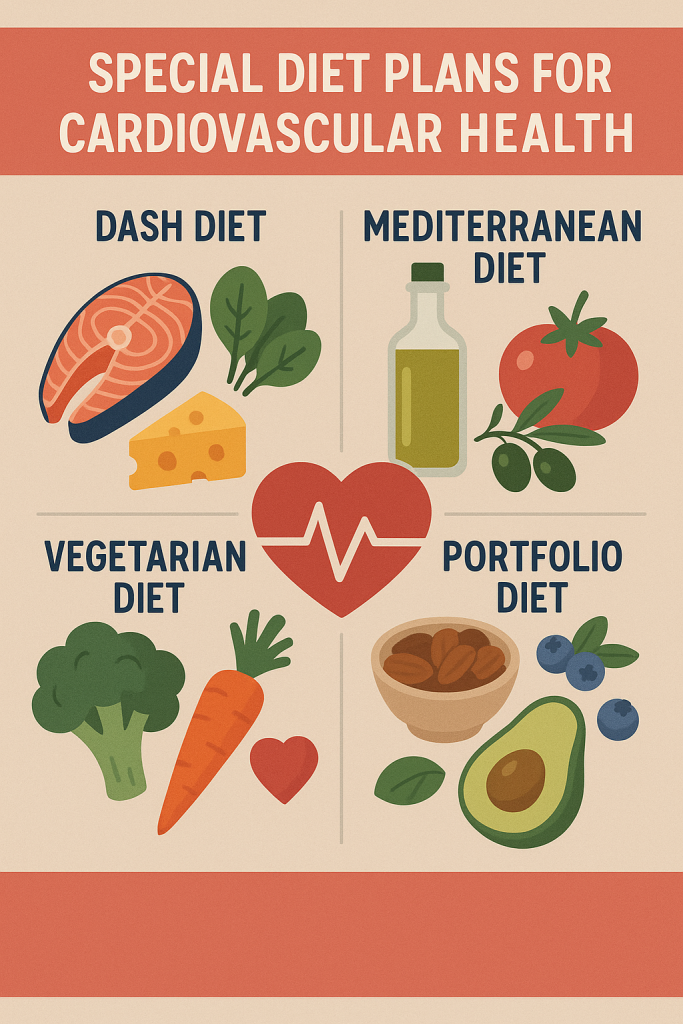
1. DASH Diet (Dietary Approaches to Stop Hypertension)
✔ High in: Fruits, vegetables, whole grains, low-fat dairy.
✔ Low in: Salt, red meat, added sugars.
✔ Ideal for: Patients with hypertension & heart disease.
2. Mediterranean Diet
✔ High in: Healthy fats (olive oil, nuts), vegetables, fish, whole grains.
✔ Low in: Processed foods, sugar, saturated fats.
✔ Ideal for: Heart disease prevention & cholesterol management.
3. TLC Diet (Therapeutic Lifestyle Changes Diet)
✔ Aims to lower cholesterol & improve heart health.
✔ Encourages: High fiber, lean proteins, omega-3 fatty acids.
Lifestyle Modifications Along with Diet
✅ Regular Physical Activity – 30-45 minutes of walking, yoga, or aerobic exercises daily.
✅ Maintain a Healthy Weight – BMI should be 18.5-24.9 kg/m².
✅ Quit Smoking – Smoking damages blood vessels & increases heart disease risk.
✅ Manage Stress – Practice yoga, meditation, and deep breathing exercises.
✅ Monitor Blood Pressure & Cholesterol – Regular check-ups are essential.
Diet in Underweight Conditions
Introduction to Underweight

Underweight is a condition where an individual has a Body Mass Index (BMI) below 18.5 kg/m². It indicates insufficient body weight for height and can lead to malnutrition, weakened immunity, osteoporosis, anemia, and infertility.
📌 Common Causes of Underweight:
- Poor dietary intake (lack of calories, proteins, and fats).
- Chronic illnesses (cancer, tuberculosis, hyperthyroidism).
- Eating disorders (anorexia nervosa, bulimia).
- High metabolism (burning more calories than consumed).
- Malabsorption issues (Crohn’s disease, celiac disease).
Dietary Goals for Underweight Management
✅ Increase calorie intake healthily (without excessive junk food).
✅ Improve muscle mass and strength through protein-rich foods.
✅ Enhance nutrient absorption and digestion.
✅ Maintain energy balance for sustained weight gain.
Principles of a Diet for Underweight Individuals
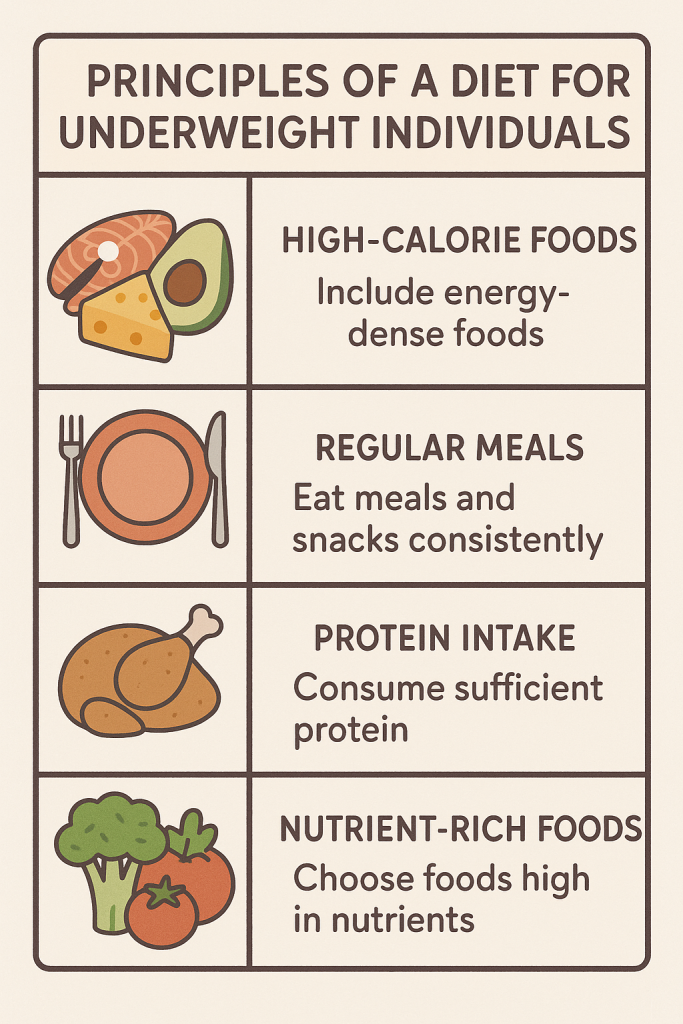
1. High-Calorie Diet (Energy-Dense Foods)
✔ Increase total daily calorie intake by 500-1000 kcal/day.
✔ Aim for small, frequent meals (5-6 times a day).
✔ Choose nutrient-dense foods over empty-calorie junk food.
✅ Healthy High-Calorie Foods:
- Whole grains, brown rice, oats, quinoa
- Nuts and seeds (almonds, walnuts, peanuts, flaxseeds)
- Dairy products (cheese, yogurt, milk)
- Healthy oils (olive oil, coconut oil, ghee in moderation)
- Lean meats, eggs, legumes
🚫 Avoid empty-calorie foods: Chips, soda, candy, processed foods.
2. High-Protein Diet for Muscle Gain
✔ Protein is essential for muscle building and healthy weight gain.
✔ Target: 1.2-2g protein/kg body weight/day.
✅ Protein-Rich Foods:
- Animal-based: Chicken, fish, eggs, dairy products
- Plant-based: Lentils, chickpeas, tofu, soya, quinoa, nuts
🚫 Avoid excessive red meat and processed meats (bacon, sausages).
3. Healthy Fat Intake (Good Fats for Weight Gain)
✔ Fat should contribute 25-35% of total daily calories.
✔ Choose unsaturated fats over unhealthy trans fats.
✅ Healthy Fat Sources:
- Nuts (almonds, cashews, peanuts)
- Seeds (flaxseeds, chia seeds)
- Avocado, olive oil, ghee (in moderation)
- Fatty fish (salmon, mackerel)
🚫 Avoid unhealthy fats: Deep-fried foods, processed oils, trans fats.
4. Complex Carbohydrates for Energy
✔ Carbohydrates should be 50-55% of daily calories.
✔ Opt for complex carbs instead of refined carbs.
✅ Healthy Carbohydrate Sources:
- Whole wheat, brown rice, oats, quinoa
- Vegetables (sweet potatoes, carrots, green peas)
- Legumes (beans, lentils, chickpeas)
🚫 Avoid refined carbohydrates: White bread, sugary cereals, pastries.
5. High-Fiber Diet for Better Digestion
✔ Helps with nutrient absorption and prevents digestive issues.
✅ Fiber-Rich Foods:
- Fruits: Bananas, mangoes, apples, pears
- Vegetables: Carrots, broccoli, spinach
- Whole grains: Oats, brown rice, whole wheat
🚫 Avoid excessive fiber intake as it may cause bloating.
6. Hydration and Meal Timing
✔ Drink at least 2-3 liters of water daily.
✔ Avoid excessive fluids before meals (prevents early satiety).
✔ Drink high-calorie beverages like smoothies, milkshakes, fresh juices.
🚫 Avoid: Soft drinks, energy drinks, caffeine overdose.
Recommended Foods and Foods to Avoid for Weight Gain
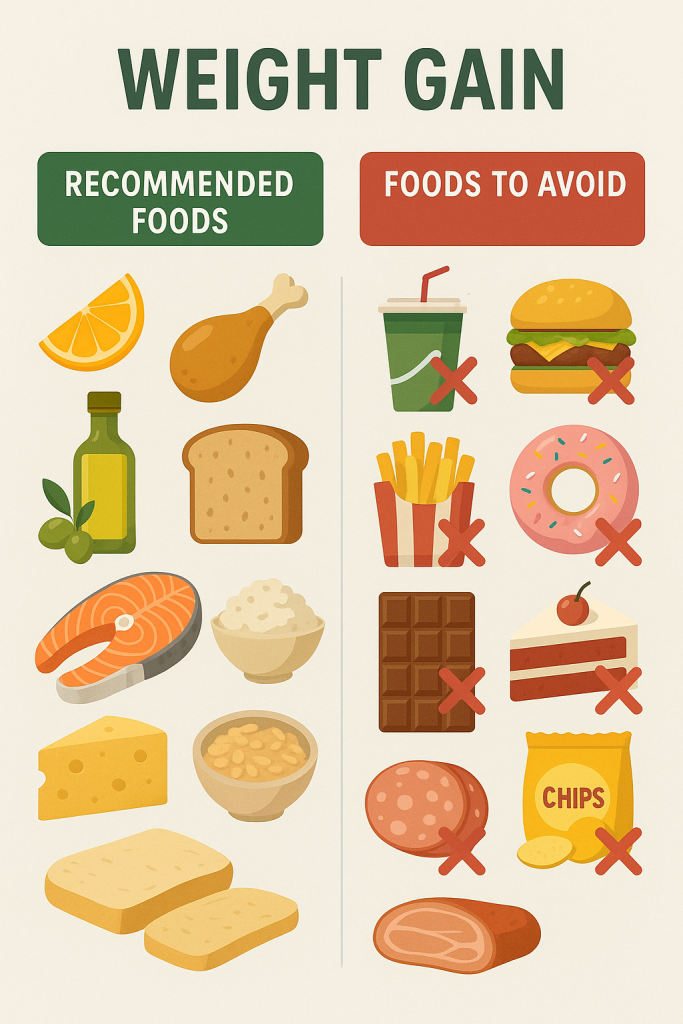
✅ Foods to Include (Healthy Weight Gain Choices)
- Whole Grains – Brown rice, oats, quinoa, whole wheat.
- Lean Proteins – Chicken, fish, tofu, eggs, dairy, legumes.
- Healthy Fats – Nuts, avocado, olive oil, coconut oil.
- Fruits & Vegetables – Mangoes, bananas, sweet potatoes, carrots.
- Dairy Products – Full-fat milk, yogurt, cheese, paneer.
- Hydration – Smoothies, milkshakes, fruit juices.
🚫 Foods to Avoid (Unhealthy for Weight Gain)
- Fried & Processed Foods – Chips, French fries, fast food.
- Sugary & Refined Carbs – White bread, pastries, sweets.
- High-Sodium Foods – Canned soups, processed meats, salted snacks.
- Unhealthy Fats – Butter, margarine, full-fat cream.
- Alcohol & Sugary Beverages – Soft drinks, alcohol, energy drinks.
Special Diet Plans for Underweight Individuals
1. High-Calorie Nutrient-Dense Diet
✔ Focuses on healthy calorie-dense foods like nuts, dairy, healthy fats.
✔ Includes snacks between meals to increase total energy intake.
2. Protein-Rich Muscle Gain Diet
✔ Ideal for underweight individuals looking to build lean muscle mass.
✔ Includes high-protein meals with good fats and complex carbs.
3. Mediterranean Diet for Weight Gain
✔ Incorporates healthy fats (olive oil, nuts), whole grains, and lean proteins.
✔ Encourages balanced nutrition for long-term health.
Lifestyle Modifications Along with Diet
✅ Strength Training & Exercise – Resistance training helps gain muscle mass.
✅ Adequate Sleep – 7-9 hours per night for better metabolism.
✅ Stress Management – Practice yoga, meditation, relaxation techniques.
✅ Monitor Progress – Regular weight checks and diet adjustments.
Diet in Renal Diseases
Introduction to Renal Diseases
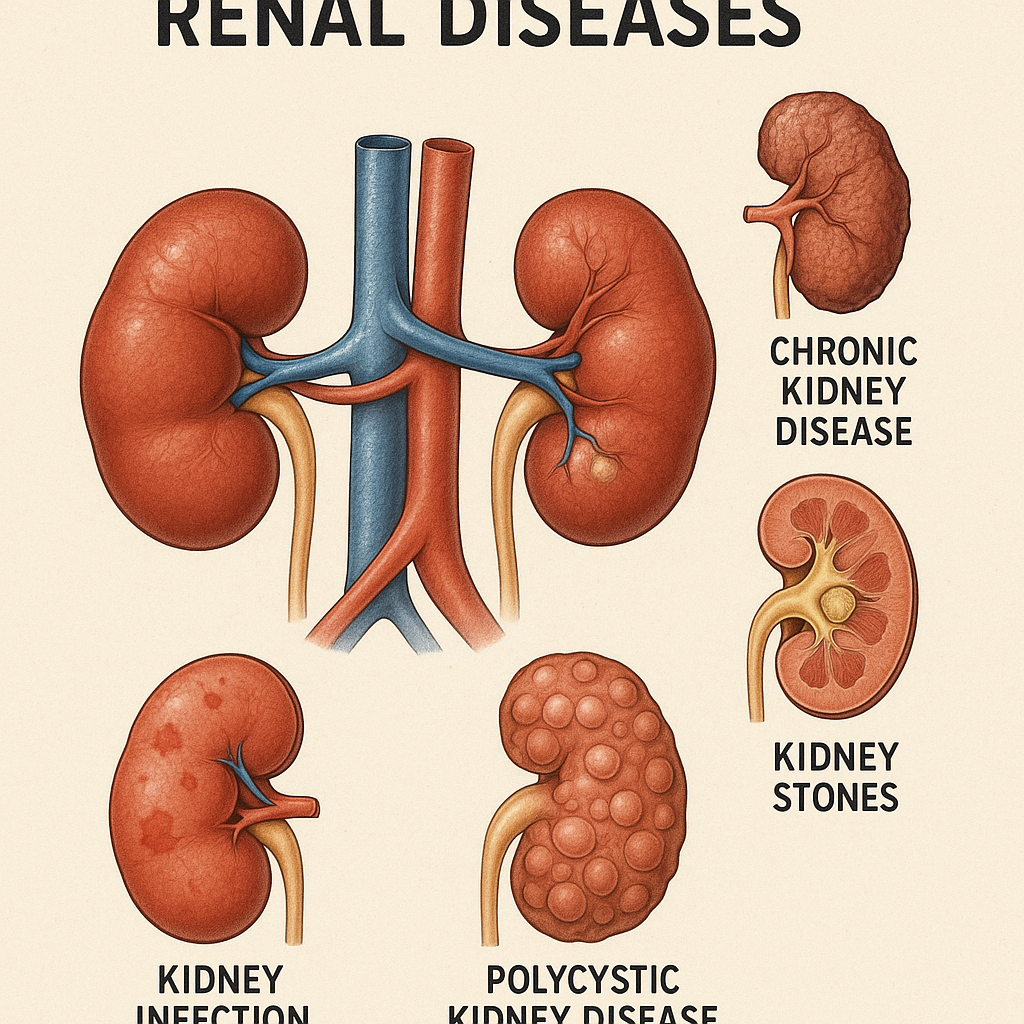
Renal (kidney) diseases affect the body’s ability to filter waste, regulate fluid balance, and maintain electrolyte levels. Chronic kidney disease (CKD), acute kidney injury (AKI), nephrotic syndrome, and kidney stones require dietary modifications to manage symptoms and prevent complications.
📌 Functions of the Kidneys:
- Filter waste and excess fluids.
- Regulate electrolytes (sodium, potassium, phosphorus).
- Maintain acid-base balance.
- Produce hormones for blood pressure control and red blood cell production.
Dietary Goals for Renal Disease Management
✅ Control sodium, potassium, phosphorus, and protein intake to reduce kidney workload.
✅ Maintain fluid balance to prevent swelling and complications.
✅ Ensure adequate calories to prevent malnutrition.
✅ Prevent accumulation of waste products in the blood (uremia).
Principles of a Renal Diet
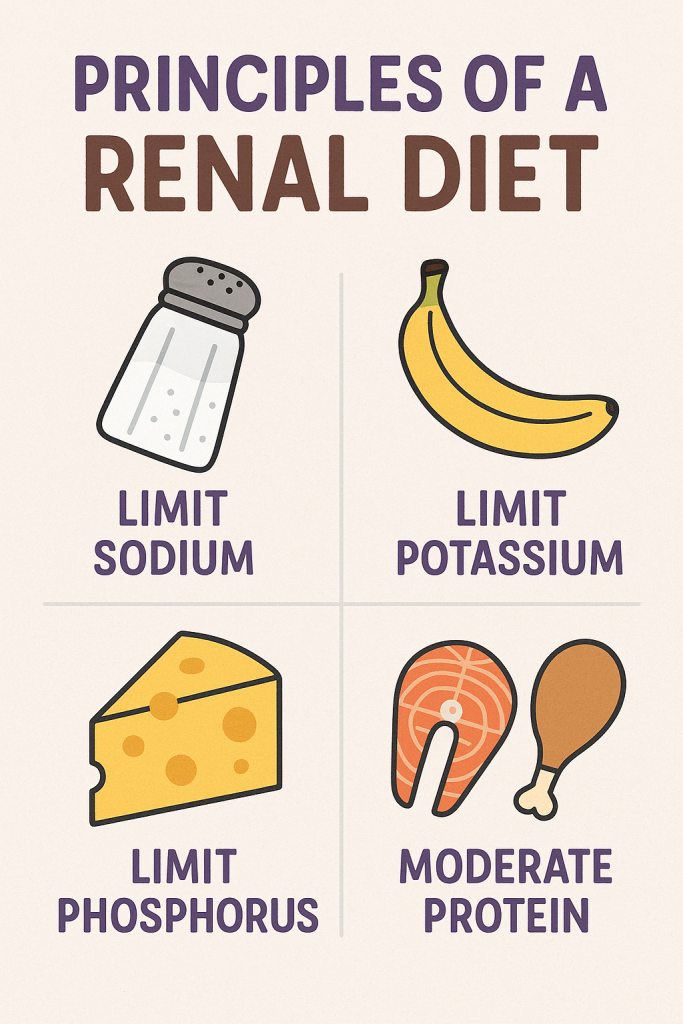
1. Low-Protein Diet (in CKD, Pre-Dialysis Patients)
✔ Reduces nitrogenous waste buildup in blood.
✔ Protein intake: 0.6-0.8 g/kg body weight/day (pre-dialysis).
✔ Higher protein intake (1.2-1.5 g/kg/day) for dialysis patients.
✅ Good Protein Sources (Moderation Required):
- Lean meats (chicken, fish – in limited quantity).
- Egg whites.
- Low-fat dairy (restricted in high phosphorus cases).
🚫 Avoid: High-protein foods like red meat, processed meats, full-fat dairy.
2. Low-Sodium Diet (Salt Restriction for Blood Pressure Control)
✔ Excess sodium leads to high blood pressure, fluid retention, and swelling (edema).
✔ Limit sodium to <1500 mg/day.
✔ Avoid table salt and processed foods.
✅ Low-Sodium Foods:
- Fresh fruits and vegetables.
- Herbs and spices (instead of salt).
- Home-cooked meals.
🚫 Avoid High-Sodium Foods:
- Canned foods, pickles, processed meats, instant noodles, chips.
3. Potassium Control (Hyperkalemia Prevention)
✔ Kidney dysfunction leads to potassium accumulation, causing heart problems.
✔ Limit potassium intake to 2,000-3,000 mg/day in CKD.
✅ Low-Potassium Foods (Safer Choices):
- Apples, grapes, berries, pears.
- Cabbage, cauliflower, bell peppers.
- White rice, white bread.
🚫 Avoid High-Potassium Foods:
- Bananas, oranges, potatoes, tomatoes.
- Dried fruits, avocados, spinach.
📌 Tip: Boil high-potassium vegetables and discard water to reduce potassium levels.
4. Phosphorus Restriction (Bone Health in CKD)
✔ High phosphorus leads to weak bones and calcium loss.
✔ Limit phosphorus intake to 800-1,000 mg/day.
✅ Low-Phosphorus Foods:
- Fresh fruits and vegetables.
- White rice, corn, refined grains.
🚫 Avoid High-Phosphorus Foods:
- Processed meats, soft drinks, chocolates, nuts, dairy.
📌 Tip: Phosphate binders may be prescribed to prevent phosphorus absorption.
5. Fluid Restriction (Prevents Overload & Swelling)
✔ Limited urine output in kidney disease causes fluid retention.
✔ Monitor fluid intake based on urine output and swelling (edema).
✅ Safe Fluids in Limited Quantities:
- Water, herbal teas, clear soups.
- Ice chips (to control thirst).
🚫 Avoid Excess Fluids:
- Sugary drinks, soft drinks, soups.
📌 Tip: Suck on ice cubes or chew sugar-free gum to control thirst.
6. Carbohydrates & Fats (For Energy in Low-Protein Diet)
✔ Healthy fats and complex carbs provide energy without straining kidneys.
✔ Choose unsaturated fats (olive oil, nuts, avocado).
✅ Healthy Carbs:
- White bread, rice, refined grains (low-phosphorus).
- Fruits (except high-potassium ones).
🚫 Avoid: Processed sweets, excess sugar, fried foods.
Recommended Foods & Foods to Avoid in Kidney Disease

✅ Foods to Include (Kidney-Friendly Choices)
- Low-Protein Sources (Pre-Dialysis) – Egg whites, fish (small amounts), tofu.
- Low-Sodium Foods – Fresh fruits & vegetables, homemade meals.
- Low-Potassium Choices – Apples, grapes, berries, cauliflower.
- Low-Phosphorus Grains – White rice, refined grains, corn-based cereals.
- Healthy Fats – Olive oil, unsalted nuts, avocado (limited).
🚫 Foods to Avoid (Harmful for Kidney Disease)
- High-Protein Foods (Pre-Dialysis) – Red meat, full-fat dairy, processed meats.
- High-Sodium Foods – Pickles, canned foods, chips, fast food.
- High-Potassium Foods – Bananas, oranges, potatoes, tomatoes.
- High-Phosphorus Foods – Soft drinks, processed cheese, chocolates.
- Sugary Foods & Beverages – Sweets, sodas, alcohol.
Special Diet Plans for Kidney Disease
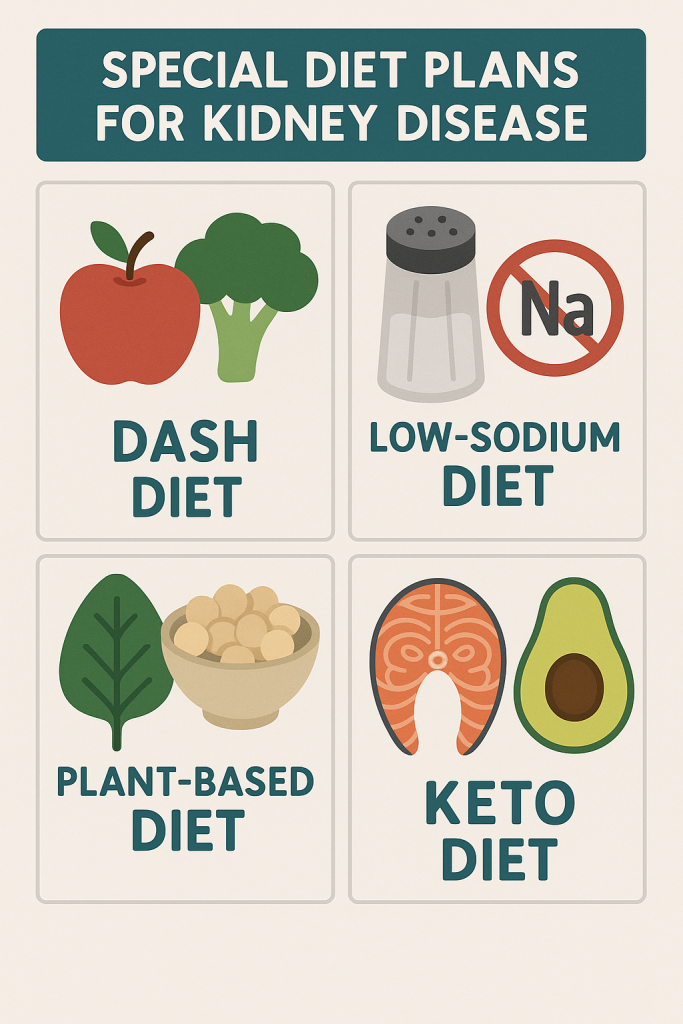
1. Low-Protein Diet (CKD, Pre-Dialysis)
✔ Moderate protein intake to reduce kidney workload.
✔ Focus on energy-dense foods (carbs & healthy fats).
2. High-Protein Diet (For Dialysis Patients)
✔ Higher protein needs (1.2-1.5g/kg/day) to compensate for dialysis loss.
✔ Lean proteins (egg whites, fish, poultry) are recommended.
3. Renal Diabetic Diet (For CKD with Diabetes)
✔ Controlled carbs (low GI foods).
✔ Low-sodium, low-potassium, and low-phosphorus diet.
Lifestyle Modifications Along with Diet
✅ Monitor Blood Pressure & Blood Sugar – Essential for kidney health.
✅ Regular Weight Monitoring – Avoid excessive weight loss or gain.
✅ Limit Alcohol & Smoking – Reduces kidney damage risk.
✅ Exercise Moderately – Walking, light yoga (avoid strenuous workouts).
✅ Follow Medical Guidance – Regular kidney function tests, prescribed medications.
Diet in Hepatic Disorders (Liver Diseases)
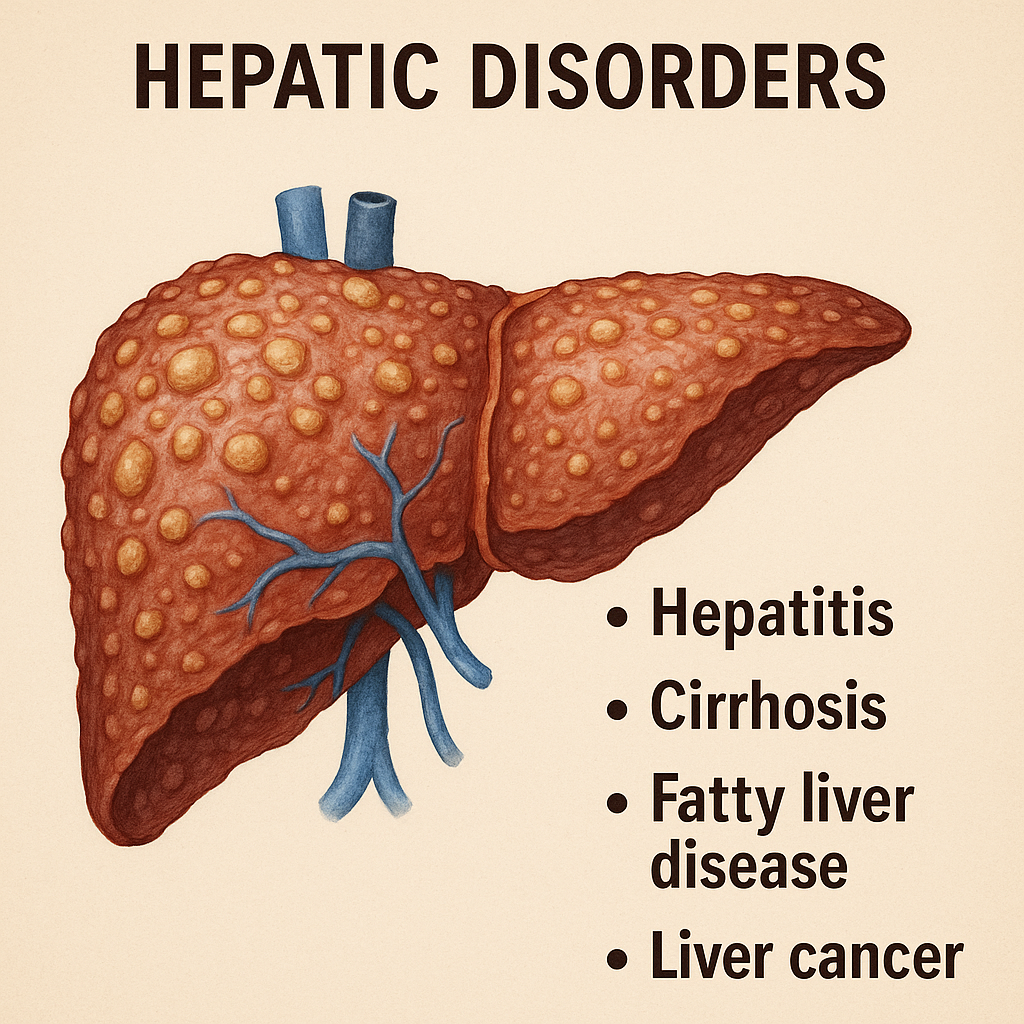
Introduction to Hepatic Disorders
Hepatic (liver) disorders affect liver function, leading to impaired metabolism, digestion, and detoxification. Common liver diseases include:
- Hepatitis (A, B, C, D, E) – Inflammation of the liver.
- Cirrhosis – Chronic liver scarring due to alcohol, viral infections, or fatty liver disease.
- Non-Alcoholic Fatty Liver Disease (NAFLD) – Excess fat accumulation in the liver.
- Liver Failure – Loss of liver function due to severe damage.
- Jaundice – Yellowing of the skin and eyes due to bilirubin buildup.
📌 Functions of the Liver:
- Metabolism of proteins, fats, and carbohydrates.
- Detoxification of toxins, drugs, and waste.
- Production of bile for fat digestion.
- Storage of vitamins (A, D, B12) and minerals (iron, copper).
Dietary Goals for Hepatic Disease Management
✅ Support liver function with balanced nutrition.
✅ Reduce liver workload by controlling protein and fat intake.
✅ Prevent fluid retention (ascites) and toxin buildup.
✅ Manage symptoms like jaundice, fatigue, and weakness.
Principles of a Liver-Friendly Diet
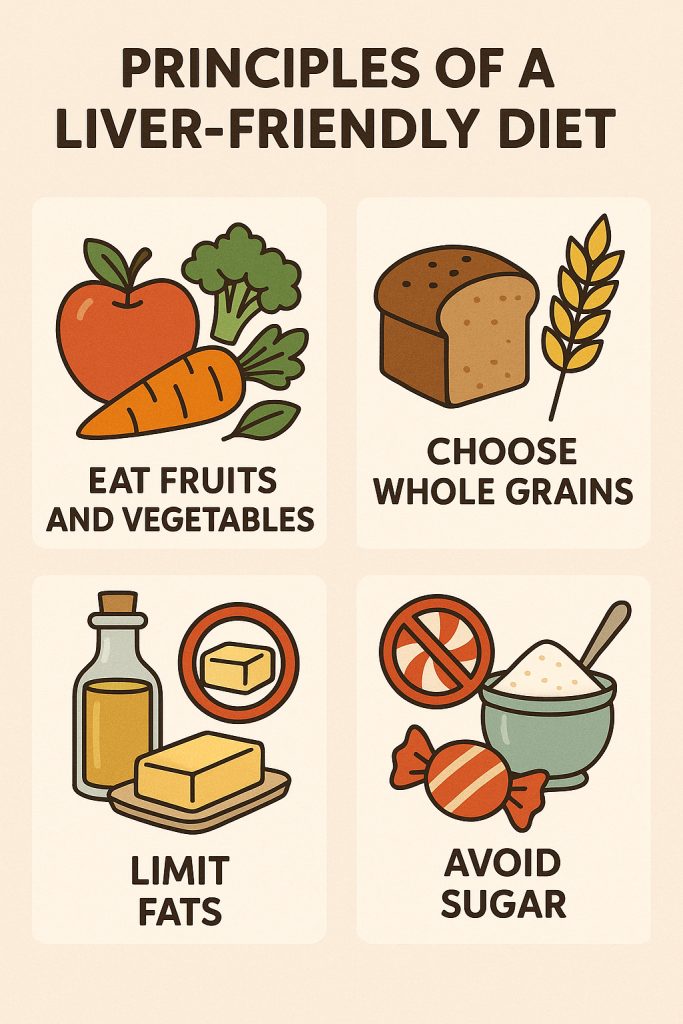
1. High-Carbohydrate, Moderate-Protein Diet
✔ Carbohydrates should make up 55-65% of total calories.
✔ Protein intake: 1-1.2g/kg body weight/day.
✅ Good Carbohydrate Sources:
- Whole grains (brown rice, oats, quinoa).
- Starchy vegetables (sweet potatoes, carrots).
- Fruits (bananas, apples, papaya).
✅ Moderate Protein Sources:
- Lean meat (chicken, fish, turkey).
- Low-fat dairy (curd, paneer, skimmed milk).
- Plant proteins (tofu, lentils, beans).
🚫 Avoid: Red meat, processed meats, high-fat dairy.
2. Low-Fat Diet (Eases Liver Stress)
✔ Fats should be 20-30% of total calories.
✔ Choose unsaturated fats, avoid trans fats.
✅ Healthy Fats:
- Olive oil, flaxseeds, nuts, avocado.
- Fatty fish (rich in omega-3).
🚫 Avoid: Fried foods, butter, margarine, processed snacks.
3. Low-Sodium Diet (Prevents Fluid Retention & Ascites)
✔ Limit sodium intake to <2000 mg/day.
✅ Low-Sodium Foods:
- Fresh vegetables, unsalted nuts.
- Herbs and spices instead of salt.
🚫 Avoid: Pickles, canned food, salty snacks.
4. High-Fiber Diet for Digestion
✔ Prevents constipation and supports gut health.
✅ High-Fiber Foods:
- Whole grains, oats, vegetables.
- Legumes, beans, and nuts.
🚫 Avoid: Processed foods, refined grains.
5. Hydration & Alcohol Avoidance
✔ Drink 2-3 liters of water per day.
✔ Avoid alcohol completely.
🚫 Avoid: Sugary sodas, artificial fruit juices.
Recommended & Avoided Foods for Liver Disease

✅ Foods to Include
- Whole Grains – Brown rice, oats, quinoa.
- Lean Proteins – Chicken, fish, tofu, eggs.
- Healthy Fats – Nuts, olive oil, seeds.
- Low-Sodium Choices – Fresh vegetables, unsalted foods.
- Fruits & Vegetables – Apples, bananas, carrots, spinach.
🚫 Foods to Avoid
- Alcohol & Sugary Drinks – Beer, wine, soda.
- High-Fat Foods – Butter, full-fat dairy, fried foods.
- Processed Meats – Bacon, sausages, ham.
- High-Sodium Foods – Pickles, processed snacks.
- Refined Carbs & Sugars – White bread, sweets, pastries.
Special Diet Plans for Liver Disorders
1. Low-Fat, High-Carb Diet (For Fatty Liver & Cirrhosis)
✔ Encourages complex carbs & moderate protein.
2. High-Protein Diet (For Hepatitis Recovery)
✔ Boosts muscle mass & immune function.
3. Fluid-Restricted Diet (For Ascites & Edema)
✔ Controls water retention in severe liver damage.
Lifestyle Modifications Along with Diet
✅ Exercise Regularly – Low-impact activities like walking, yoga.
✅ Quit Smoking & Alcohol – Reduces liver stress.
✅ Monitor Liver Enzymes & Symptoms – Regular check-ups.
✅ Manage Stress – Meditation, breathing exercises.
Conclusion
A liver-friendly diet should be high in carbohydrates, moderate in protein, and low in fat & sodium to reduce liver workload, support healing, and prevent complications. Combined with exercise and medical monitoring, dietary changes can significantly improve liver health.
Diet in Constipation
Introduction to Constipation

Constipation is a digestive condition characterized by infrequent, hard, or difficult bowel movements. It is commonly caused by:
- Low fiber intake.
- Inadequate hydration.
- Lack of physical activity.
- Certain medications.
- Hormonal or metabolic disorders.
📌 Symptoms of Constipation:
- Hard, dry stools.
- Straining during bowel movements.
- Incomplete evacuation.
- Bloating and abdominal discomfort.
Dietary Goals for Constipation Management
✅ Increase fiber intake to promote bowel movement.
✅ Improve hydration for stool softening.
✅ Encourage healthy fats for lubrication.
✅ Promote gut health with probiotics.
Principles of a High-Fiber Diet for Constipation
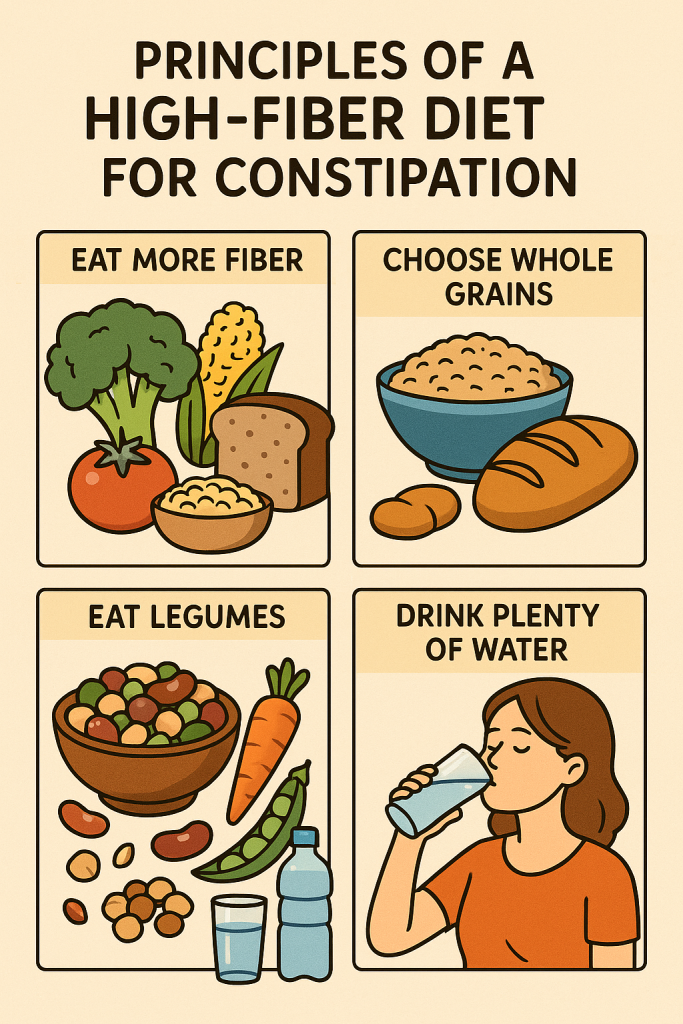
1. High-Fiber Diet (Promotes Regular Bowel Movements)
✔ Target: 25-35g fiber per day.
✅ High-Fiber Foods:
- Whole grains (brown rice, quinoa, oats).
- Vegetables (broccoli, carrots, spinach).
- Fruits (apples, pears, bananas, berries).
- Legumes (beans, lentils, chickpeas).
🚫 Avoid Low-Fiber Foods:
- White bread, processed foods, instant noodles.
📌 Tip: Gradually increase fiber intake to prevent bloating.
2. Increase Hydration (Prevents Hard Stools)
✔ Drink at least 2-3 liters of water daily.
✅ Best Hydration Sources:
- Water, herbal teas, coconut water.
- Fresh fruit juices (without added sugar).
🚫 Avoid: Alcohol, caffeine, sugary drinks.
📌 Tip: Warm water with lemon in the morning can stimulate digestion.
3. Include Healthy Fats (Lubricates Intestines)
✔ Supports smooth bowel movement.
✅ Healthy Fat Sources:
- Olive oil, flaxseeds, chia seeds.
- Nuts (almonds, walnuts).
- Fatty fish (salmon, mackerel).
🚫 Avoid: Excess saturated fats and fried foods.
4. Probiotic-Rich Diet (Improves Gut Flora for Digestion)
✔ Probiotics help maintain gut bacteria balance.
✅ Probiotic Sources:
- Yogurt, kefir, buttermilk.
- Fermented foods (kimchi, sauerkraut).
🚫 Avoid: Processed foods and excessive antibiotics.
Recommended & Avoided Foods for Constipation
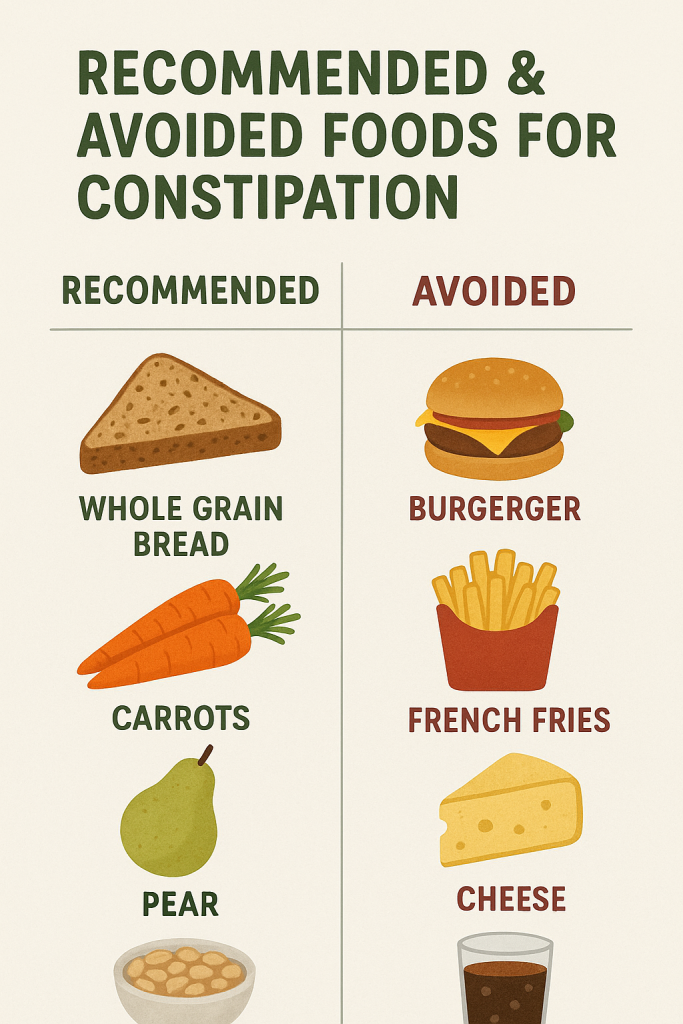
✅ Foods to Include
- Whole Grains – Oats, quinoa, brown rice.
- Fruits & Vegetables – Apples, pears, spinach, carrots.
- Nuts & Seeds – Chia, flaxseeds, almonds.
- Hydration – Water, herbal teas, fresh juices.
🚫 Foods to Avoid
- Low-Fiber Foods – White bread, pasta, processed snacks.
- Sugary Foods – Sweets, cakes, pastries.
- Caffeinated Drinks – Coffee, energy drinks.
- Alcohol & Processed Foods – Causes dehydration.
Diet in Diarrhea
Introduction to Diarrhea

Diarrhea is a digestive disorder characterized by frequent, loose, or watery stools, often accompanied by abdominal cramps, dehydration, and electrolyte imbalances. It can be acute (lasting a few days) or chronic (persisting for weeks due to underlying conditions).
📌 Common Causes of Diarrhea:
- Infections (viral, bacterial, parasitic).
- Food poisoning.
- Irritable Bowel Syndrome (IBS) or Inflammatory Bowel Disease (IBD).
- Lactose intolerance or food allergies.
- Certain medications (antibiotics, laxatives).
- Excessive caffeine or alcohol consumption.
Dietary Goals for Diarrhea Management
✅ Prevent dehydration and electrolyte loss.
✅ Restore gut health and normal bowel movements.
✅ Provide easily digestible, low-fiber foods.
✅ Avoid foods that worsen irritation.
Principles of a Diarrhea-Control Diet
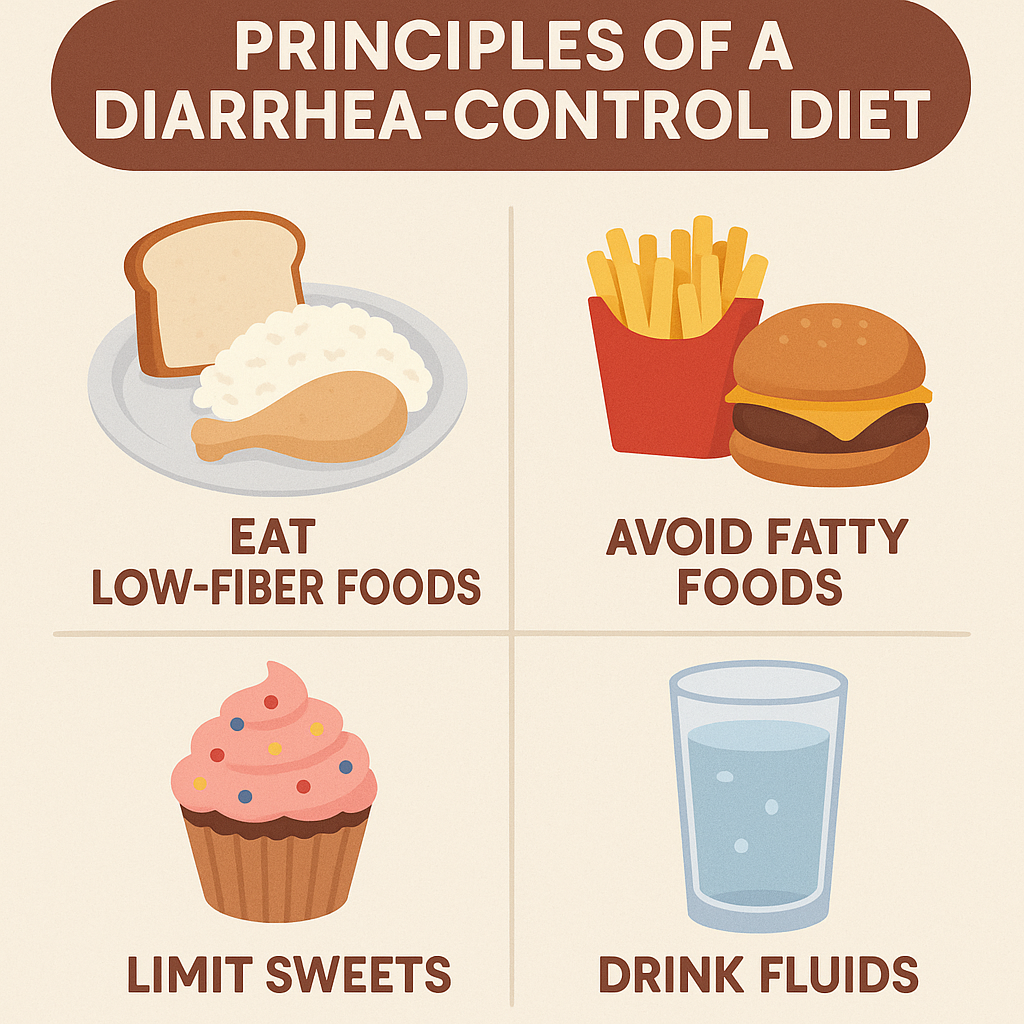
1. Fluid & Electrolyte Replacement (Prevents Dehydration)
✔ Frequent watery stools cause fluid and mineral loss.
✔ Drink 2.5-3 liters of fluids per day.
✅ Best Hydration Options:
- Oral Rehydration Solution (ORS) (Homemade: 1L water + ½ tsp salt + 6 tsp sugar).
- Coconut water, buttermilk, clear vegetable broth.
- Weak tea, diluted fruit juices (without pulp).
🚫 Avoid: Caffeinated drinks (coffee, soda), alcohol, artificial juices.
2. BRAT Diet (Bland, Easy-to-Digest Foods)
✔ The BRAT diet (Banana, Rice, Applesauce, Toast) is recommended for diarrhea relief.
✅ Best Low-Fiber, Easily Digestible Foods:
- Bananas – Rich in potassium and easy to digest.
- White Rice – Provides energy and helps firm stools.
- Applesauce – Pectin-rich, binds stools.
- Toast (white bread) – Low fiber, easy on digestion.
🚫 Avoid: Whole grains, raw vegetables, beans (high-fiber foods).
3. Low-Fiber Diet (Reduces Bowel Irritation)
✔ Limit insoluble fiber to prevent excessive bowel movements.
✅ Safe Low-Fiber Foods:
- Cooked carrots, potatoes (without skin), pumpkin.
- Well-cooked, soft cereals (semolina, white oats).
🚫 Avoid High-Fiber Foods:
- Raw vegetables, whole grains, legumes, nuts, and seeds.
4. Probiotics (Restore Gut Flora)
✔ Beneficial bacteria help restore the balance of gut microbiota.
✅ Best Probiotic Foods:
- Yogurt (plain, unsweetened).
- Buttermilk, kefir.
- Fermented foods (kimchi, sauerkraut, miso).
🚫 Avoid: Artificially flavored yogurt with added sugars.
5. Moderate Protein Intake (Supports Recovery)
✔ Soft, easy-to-digest protein helps repair the gut lining.
✅ Recommended Protein Sources:
- Boiled eggs, soft tofu.
- Lean chicken, fish (boiled or grilled).
- Lentil soups (thin, without spices).
🚫 Avoid: Spicy meats, fried chicken, red meat.
6. Avoid Dairy (If Lactose Intolerant)
✔ Lactose can worsen diarrhea in some individuals.
✅ Low-Lactose Alternatives:
- Lactose-free milk.
- Almond or soy milk.
🚫 Avoid: Whole milk, cheese, butter.
7. Limit Fatty, Spicy & Sugary Foods
✔ Fatty foods increase intestinal motility and worsen diarrhea.
🚫 Avoid:
- Deep-fried foods, heavy gravies.
- Spicy sauces, chili, black pepper.
- Sweets, chocolates, desserts (high sugar).
Recommended & Avoided Foods for Diarrhea

✅ Foods to Include (Gentle on Stomach & Easy to Digest)
- BRAT Diet Foods – Bananas, rice, applesauce, toast.
- Low-Fiber Vegetables – Cooked carrots, zucchini, potatoes.
- Probiotic-Rich Foods – Yogurt, buttermilk, fermented foods.
- Mild Proteins – Boiled eggs, soft tofu, chicken, fish.
- Hydration Sources – ORS, coconut water, weak tea.
🚫 Foods to Avoid (Trigger Diarrhea & Irritation)
- High-Fiber Foods – Whole grains, raw vegetables, beans, nuts.
- Dairy Products – Milk, cheese (if lactose intolerant).
- Spicy & Fried Foods – Chili, black pepper, deep-fried snacks.
- Caffeinated & Sugary Drinks – Coffee, soft drinks, fruit juices.
- Alcohol & Processed Foods – Beer, sodas, packaged snacks.
Special Diet Plans for Diarrhea

1. BRAT Diet (For Acute Diarrhea Relief)
✔ Mild, low-fiber, binding foods to firm up stools.
2. Low-FODMAP Diet (For Chronic IBS-Related Diarrhea)
✔ Reduces fermentable carbs that worsen bloating & diarrhea.
3. Probiotic-Based Diet (For Antibiotic-Related Diarrhea)
✔ Restores gut bacteria balance with yogurt, kefir, buttermilk.
Lifestyle Modifications Along with Diet
✅ Eat Small, Frequent Meals – Prevents bloating and digestion strain.
✅ Maintain Proper Hygiene – Wash hands and food to prevent infections.
✅ Rest & Avoid Stress – Stress can worsen IBS-related diarrhea.
✅ Monitor Symptoms – Seek medical help if diarrhea persists for >3 days.
Pre-Operative Diet: Nutrition Before Surgery
Introduction to Pre-Operative Diet

A pre-operative diet is a carefully planned eating regimen followed before surgery to prepare the body, improve recovery, and reduce complications. Proper nutrition before surgery ensures:
- Optimal energy levels for healing.
- Reduced risk of infection.
- Improved digestion and gut health.
- Prevention of surgical complications like aspiration and dehydration.
📌 The pre-op diet varies based on:
- Type of surgery (minor, major, gastrointestinal, cardiac).
- Patient’s health condition (diabetes, kidney disease, obesity).
- Doctor’s recommendations (fasting periods, liquid diet).
Goals of a Pre-Operative Diet
✅ Ensure adequate nutrition before surgery.
✅ Maintain hydration and electrolyte balance.
✅ Reduce bowel content for a cleaner surgical site.
✅ Minimize digestive discomfort and bloating.
✅ Support a strong immune system for post-op recovery.
Principles of a Pre-Operative Diet
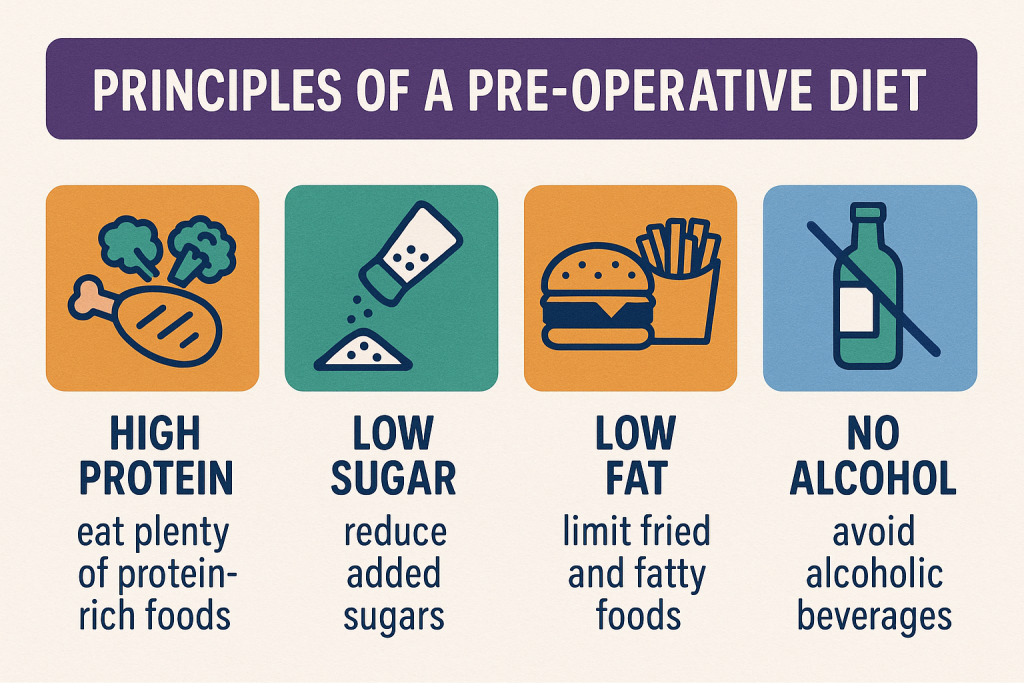
1. High-Protein, Balanced Diet (For Faster Recovery & Healing)
✔ Protein supports tissue repair and immune function.
✔ Include lean protein sources 1-2 weeks before surgery.
✅ Best Protein Sources:
- Chicken, fish, eggs.
- Dairy (low-fat milk, yogurt, paneer).
- Plant proteins (tofu, lentils, soya, nuts).
🚫 Avoid: Processed meats, deep-fried protein sources.
2. High-Carbohydrate Diet (For Energy & Glycogen Storage)
✔ Complex carbohydrates provide sustained energy.
✔ Simple carbs should be limited.
✅ Good Carbohydrate Sources:
- Whole grains (brown rice, oats, quinoa).
- Starchy vegetables (sweet potatoes, carrots).
- Fruits (bananas, apples, oranges).
🚫 Avoid: Sugary foods, refined carbs (white bread, cakes).
3. Healthy Fats (Support Cellular Function & Inflammation Control)
✔ Include healthy unsaturated fats for wound healing and immunity.
✅ Healthy Fat Sources:
- Olive oil, nuts, avocado.
- Fatty fish (salmon, tuna).
🚫 Avoid: Butter, margarine, trans fats, fried foods.
4. Adequate Hydration (Prevents Dehydration & Supports Circulation)
✔ Drink at least 2-3 liters of water daily before surgery.
✔ Hydration prevents dizziness, nausea, and complications.
✅ Best Fluids:
- Water, coconut water.
- Clear vegetable broth.
- Herbal teas (chamomile, ginger).
🚫 Avoid: Alcohol, carbonated drinks, excessive caffeine.
5. Low-Fiber Diet (For Bowel Preparation in GI Surgeries)
✔ Some surgeries require a reduced fiber intake to clear the bowels.
✅ Allowed Low-Fiber Foods:
- White rice, white bread.
- Peeled fruits, boiled vegetables.
🚫 Avoid High-Fiber Foods:
- Whole grains, raw vegetables, legumes, nuts.
6. Low-Sodium Diet (For Heart & Kidney Patients)
✔ Reduces fluid retention and high blood pressure risks.
✅ Use: Herbs, lemon juice, garlic for flavoring.
🚫 Avoid: Canned foods, salty snacks, pickles.
Pre-Operative Fasting Guidelines (Nil Per Os – NPO Policy)
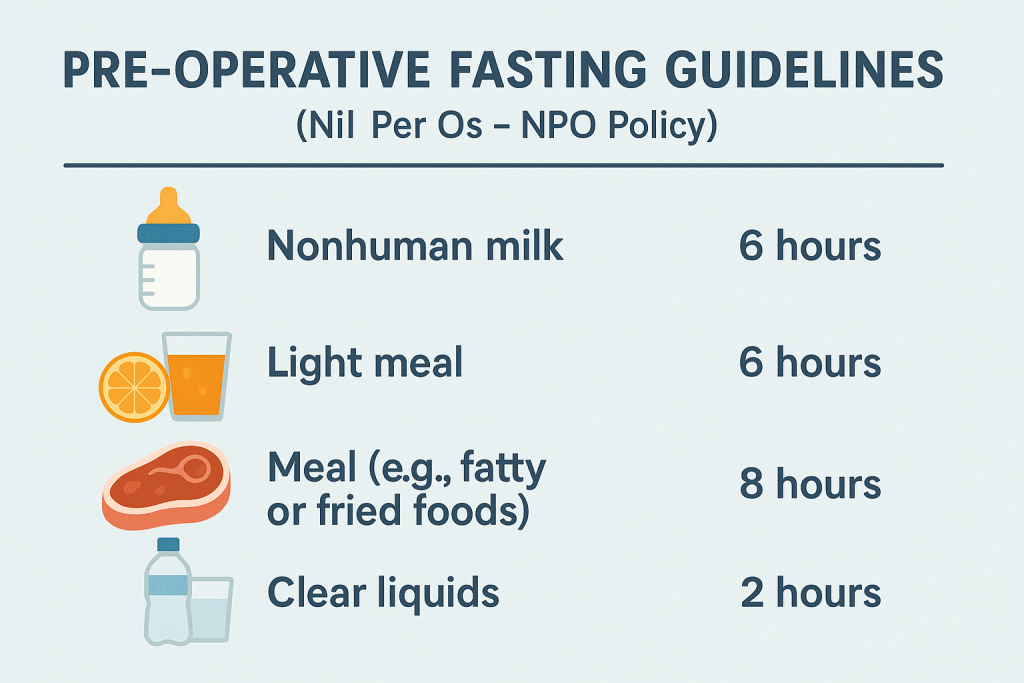
Doctors may recommend fasting before surgery to prevent aspiration risks.
Standard Pre-Surgery Fasting Recommendations:
✅ Solid Food: Stop 6-8 hours before surgery.
✅ Clear Liquids (Water, Tea, Apple Juice): Allowed up to 2 hours before surgery.
✅ Dairy & Heavy Meals: Stop 8 hours before surgery.
🚫 Avoid: Alcohol, fatty foods, caffeine before fasting.
Recommended & Avoided Foods for Pre-Operative Diet
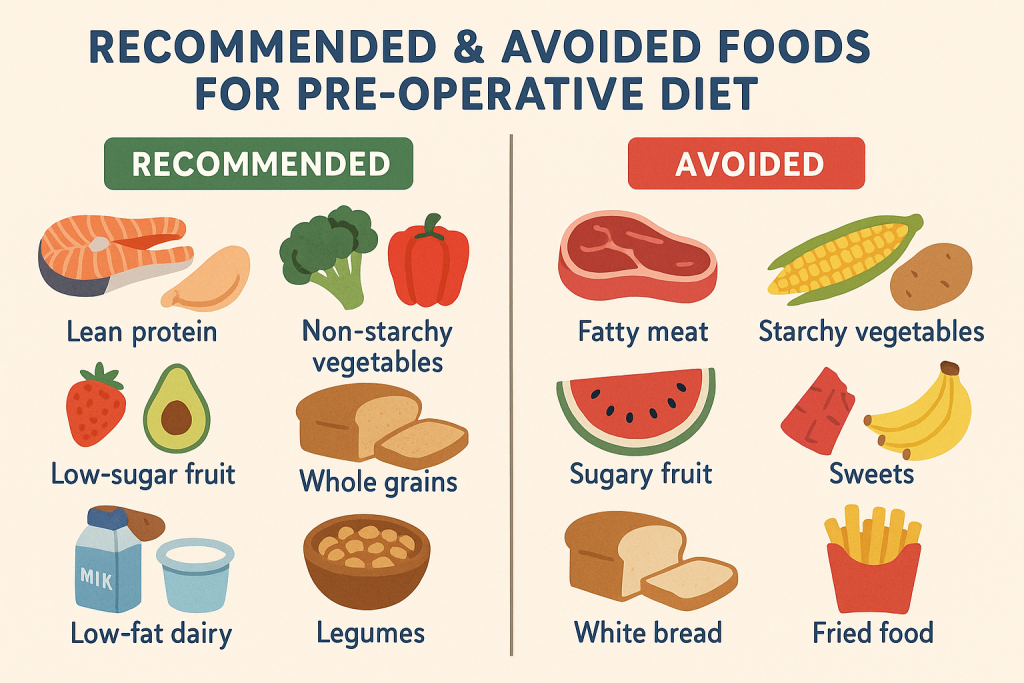
✅ Foods to Include (Pre-Surgery Nutrition Boost)
- Lean Proteins – Chicken, fish, eggs, tofu.
- Healthy Carbs – Whole grains, fruits, starchy vegetables.
- Healthy Fats – Olive oil, nuts, avocado.
- Hydration – Water, coconut water, herbal tea.
- Low-Fiber Options (if recommended) – White rice, white bread, peeled fruits.
🚫 Foods to Avoid (Pre-Surgery Risks)
- Fried & Fatty Foods – Greasy snacks, junk food.
- High-Sodium Foods – Processed foods, canned soups.
- High-Fiber Foods (For GI Surgeries) – Whole grains, legumes, nuts.
- Sugary Foods & Drinks – Soda, sweets, pastries.
- Alcohol & Caffeine – Increases dehydration and digestive irritation.
Special Diet Plans for Different Surgeries
1. Clear Liquid Diet (For Gastrointestinal Surgeries)
✔ Purpose: Cleanses the digestive tract before surgery.
✔ Includes: Water, clear broth, apple juice, herbal teas.
2. High-Protein, Low-Fat Diet (For Major Surgeries & Recovery)
✔ Promotes wound healing & muscle repair.
✔ Includes: Chicken, fish, eggs, tofu, yogurt.
3. Low-Residue Diet (For Colon/Bowel Surgeries)
✔ Limits fiber intake to reduce bowel bulk.
✔ Includes: White rice, peeled fruits, soft bread.
Lifestyle Modifications Along with Diet
✅ Follow Pre-Op Fasting Instructions Strictly.
✅ Avoid Alcohol & Smoking for at least 1-2 weeks pre-surgery.
✅ Exercise Lightly (Walking, Yoga) for Better Circulation.
✅ Get Enough Sleep (7-8 hours) to Enhance Recovery.
✅ Manage Stress Through Meditation & Deep Breathing.
Post-Operative Diet: Nutrition for Recovery After Surgery
Introduction to Post-Operative Diet
A post-operative diet is a carefully structured meal plan designed to support healing, prevent complications, and restore strength after surgery. Proper nutrition plays a crucial role in wound healing, immune function, pain management, and digestive recovery.
📌 The type of post-operative diet varies depending on:
- Type of surgery (minor, major, gastrointestinal, orthopedic, cardiac).
- Patient’s condition (diabetes, kidney disease, weakened immunity).
- Doctor’s instructions (clear liquid, soft, or normal diet progression).
Goals of a Post-Operative Diet
✅ Promote tissue healing and wound recovery.
✅ Support immune function to prevent infections.
✅ Maintain hydration and electrolyte balance.
✅ Prevent digestive discomfort (bloating, nausea, constipation).
✅ Reintroduce normal foods gradually to avoid stress on the digestive system.
Principles of a Post-Operative Diet
1. High-Protein Diet (Tissue Repair & Healing)
✔ Protein is essential for muscle repair, wound healing, and immune function.
✔ Post-surgery requirement: 1.2-2.0 g/kg body weight per day.
✅ Best Protein Sources:
- Lean meats (chicken, turkey, fish).
- Eggs, dairy (milk, yogurt, paneer).
- Plant-based proteins (lentils, chickpeas, tofu, soya).
🚫 Avoid: Processed meats, deep-fried foods.
2. Hydration (Prevents Dehydration & Supports Recovery)
✔ Water is essential for digestion, kidney function, and circulation.
✔ Drink 2-3 liters of fluids per day.
✅ Best Hydration Options:
- Water, coconut water.
- Herbal teas (chamomile, ginger).
- Clear soups, bone broth.
🚫 Avoid: Sugary drinks, caffeinated beverages, alcohol.
3. High-Fiber Diet (Prevents Post-Surgery Constipation)
✔ Pain medications and reduced mobility can lead to constipation.
✔ Increase fiber intake gradually to prevent bloating.
✅ Best Fiber Sources:
- Whole grains (brown rice, oats, quinoa).
- Fruits (apples, pears, bananas).
- Vegetables (spinach, carrots, zucchini).
- Nuts & seeds (flaxseeds, chia seeds, almonds).
🚫 Avoid: Gas-forming foods (beans, cabbage, cauliflower).
4. Adequate Healthy Fats (Reduces Inflammation & Supports Healing)
✔ Healthy fats provide energy and reduce post-surgical inflammation.
✅ Healthy Fat Sources:
- Olive oil, avocado, nuts.
- Fatty fish (salmon, mackerel, tuna).
🚫 Avoid: Fried foods, trans fats, heavy creams.
5. Low-Sodium Diet (For Cardiac & Kidney Patients)
✔ Excess sodium can cause swelling (edema) and high blood pressure.
✅ Use: Herbs, lemon juice, garlic for flavoring.
🚫 Avoid: Canned foods, salty snacks, pickles.
6. Vitamin & Mineral-Rich Diet (Boosts Immune System & Healing)
✔ Vitamins & minerals are essential for tissue repair and immunity.
✅ Essential Nutrients & Food Sources:
- Vitamin C (oranges, strawberries, bell peppers) – Wound healing.
- Vitamin A (carrots, spinach, mango) – Skin regeneration.
- Iron (lean meats, lentils, leafy greens) – Blood production.
- Zinc (pumpkin seeds, nuts, dairy) – Faster recovery.
🚫 Avoid: Nutrient-poor processed foods.
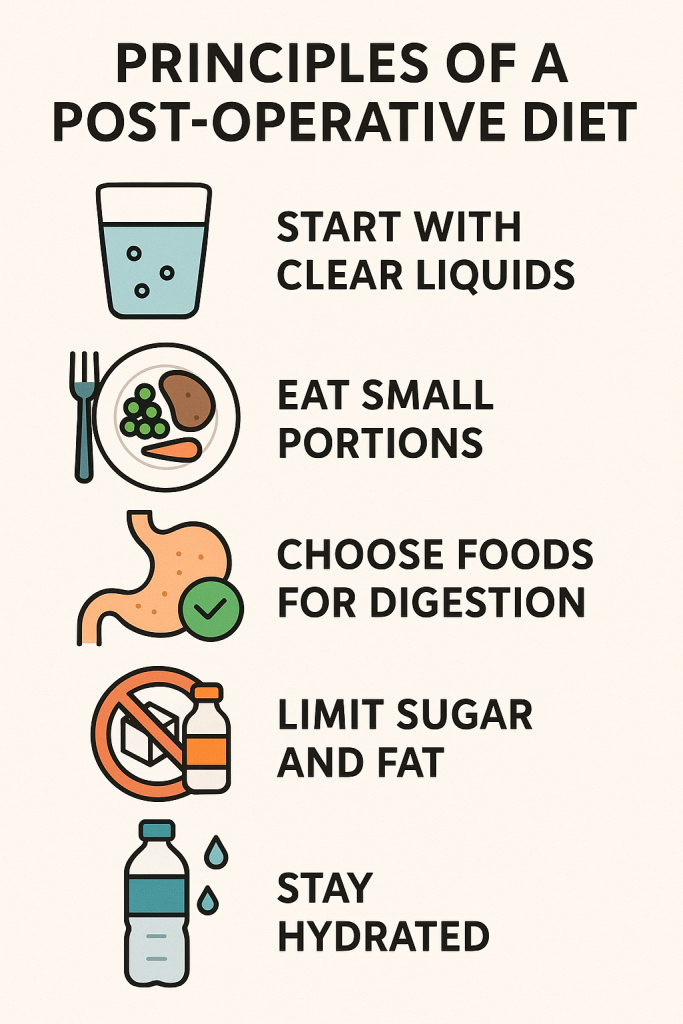
Stages of a Post-Operative Diet (Gradual Food Introduction)

1. Clear Liquid Diet (First 12-24 Hours Post-Surgery)
✔ Provides hydration and electrolytes without stressing digestion.
✅ Allowed Foods:
- Water, electrolyte drinks, coconut water.
- Clear soups, bone broth.
- Herbal teas, diluted apple juice.
🚫 Avoid: Dairy, caffeine, carbonated drinks.
2. Full Liquid Diet (24-48 Hours Post-Surgery)
✔ Introduces more calories and nutrients in liquid form.
✅ Allowed Foods:
- Milk, yogurt, blended soups.
- Smoothies, fruit juices without pulp.
- Porridge, custards.
🚫 Avoid: Spicy or acidic foods.
3. Soft Diet (2-5 Days Post-Surgery)
✔ Easily chewable and digestible foods.
✅ Allowed Foods:
- Mashed potatoes, soft rice, pasta.
- Boiled vegetables (carrots, pumpkin).
- Scrambled eggs, soft cheese.
🚫 Avoid: Hard, crunchy, or fibrous foods.
4. Normal Diet (1 Week Post-Surgery & Beyond)
✔ Return to a balanced, high-protein, fiber-rich diet.
✅ Allowed Foods:
- Whole grains, lean proteins, healthy fats.
- Fruits, vegetables, nuts, seeds.
🚫 Avoid: Alcohol, fried foods, excessive salt.
Recommended & Avoided Foods for Post-Operative Diet

✅ Foods to Include (Nutrient-Dense Choices for Recovery)
- Lean Proteins – Chicken, fish, eggs, tofu, lentils.
- Whole Grains – Oats, brown rice, quinoa.
- Healthy Fats – Nuts, olive oil, avocado, fatty fish.
- Fruits & Vegetables – Oranges, bananas, spinach, carrots.
- Hydration Sources – Water, herbal teas, soups, broths.
🚫 Foods to Avoid (Delay Healing & Cause Discomfort)
Special Diet Plans for Different Surgeries
1. Low-Residue Diet (For Gastrointestinal Surgeries)
✔ Limits fiber to reduce bowel movement frequency.
✔ Includes: White rice, soft bread, clear broths.
2. High-Protein Diet (For Major Surgeries & Recovery)
✔ Supports muscle repair and wound healing.
✔ Includes: Lean meats, eggs, dairy, legumes.
3. Low-Sodium Diet (For Cardiac & Kidney Patients Post-Surgery)
✔ Reduces fluid retention and blood pressure.
✔ Includes: Fresh vegetables, low-salt options.
Lifestyle Modifications Along with Diet
✅ Eat Small, Frequent Meals – Helps digestion and energy maintenance.
✅ Avoid Lying Down Immediately After Eating – Prevents reflux and indigestion.
✅ Start Light Physical Activity – Walking helps circulation and prevents constipation.
✅ Follow Doctor’s Instructions – Medications, supplements, and diet restrictions.
✅ Monitor Healing Progress – Watch for signs of infection or nutritional deficiencies.