BSC SEM 1 UNIT 7 APPLIED BIOCHEMISTRY
UNIT 7 Organ function tests (biochemical parameters & normal values )
Organ Function Tests, Biochemical Parameters & Normal Values in Biochemistry
Organ function tests (OFTs) assess the health and efficiency of different organs in the body by measuring specific biochemical parameters. These tests help in diagnosing diseases, monitoring disease progression, and evaluating treatment efficacy.
1. Liver Function Tests (LFTs)
Liver function tests assess liver health by measuring enzymes, proteins, and bilirubin levels.
| Test | Biochemical Parameter | Normal Values | Clinical Significance |
|---|---|---|---|
| Serum Bilirubin | Total Bilirubin | 0.3 – 1.2 mg/dL | Increased in liver dysfunction, hemolysis |
| Direct (Conjugated) Bilirubin | 0.1 – 0.4 mg/dL | Increased in obstructive jaundice | |
| Indirect (Unconjugated) Bilirubin | 0.2 – 0.8 mg/dL | Increased in hemolysis, Gilbert’s syndrome | |
| Liver Enzymes | ALT (Alanine Aminotransferase) | 7 – 56 U/L | Increased in liver damage (Hepatitis, Cirrhosis) |
| AST (Aspartate Aminotransferase) | 10 – 40 U/L | Increased in liver & muscle damage | |
| ALP (Alkaline Phosphatase) | 44 – 147 U/L | Increased in cholestasis, bone disease | |
| GGT (Gamma-Glutamyl Transferase) | 8 – 61 U/L | Elevated in alcohol abuse, liver disease | |
| Proteins | Total Protein | 6.0 – 8.3 g/dL | Decreased in malnutrition, liver disease |
| Albumin | 3.5 – 5.0 g/dL | Decreased in liver disease, nephrotic syndrome | |
| Globulin | 2.3 – 3.5 g/dL | Increased in chronic infections | |
| Other Parameters | Prothrombin Time (PT) | 11 – 13.5 sec | Increased in liver dysfunction |
2. Kidney Function Tests (KFTs) / Renal Function Tests (RFTs)
These tests evaluate kidney function by assessing waste elimination and electrolyte balance.
| Test | Biochemical Parameter | Normal Values | Clinical Significance |
|---|---|---|---|
| Serum Creatinine | Creatinine | 0.6 – 1.2 mg/dL | Increased in renal failure |
| Blood Urea Nitrogen | BUN | 6 – 20 mg/dL | Increased in kidney dysfunction |
| Urea | Urea | 15 – 45 mg/dL | Increased in kidney disease |
| Creatinine Clearance | Urinary Creatinine Clearance | 90 – 140 mL/min | Decreased in renal failure |
| Electrolytes | Sodium (Na⁺) | 135 – 145 mEq/L | Altered in dehydration, renal failure |
| Potassium (K⁺) | 3.5 – 5.0 mEq/L | Increased in kidney failure | |
| Chloride (Cl⁻) | 96 – 106 mEq/L | Altered in acid-base imbalance | |
| Bicarbonate (HCO₃⁻) | 22 – 28 mEq/L | Altered in metabolic acidosis/alkalosis |
3. Pancreatic Function Tests
These tests help assess pancreatic enzyme secretion and glucose metabolism.
| Test | Biochemical Parameter | Normal Values | Clinical Significance |
|---|---|---|---|
| Glucose Metabolism | Fasting Blood Glucose | 70 – 100 mg/dL | Increased in diabetes mellitus |
| Postprandial Blood Glucose | <140 mg/dL | Increased in diabetes | |
| HbA1c (Glycated Hemoglobin) | <5.7% (Normal) | >6.5% in Diabetes Mellitus | |
| Pancreatic Enzymes | Amylase | 30 – 110 U/L | Increased in pancreatitis |
| Lipase | 10 – 140 U/L | Increased in pancreatitis |
4. Cardiac Function Tests
Cardiac markers assess heart function and detect myocardial infarction (heart attack).
| Test | Biochemical Parameter | Normal Values | Clinical Significance |
|---|---|---|---|
| Cardiac Enzymes | Troponin I | <0.04 ng/mL | Increased in myocardial infarction |
| CK-MB (Creatine Kinase-MB) | <5% of total CK | Elevated in heart attack | |
| Myoglobin | 25 – 72 ng/mL | Increased in muscle injury | |
| Lipid Profile | Total Cholesterol | <200 mg/dL | Increased in heart disease |
| LDL (Low-Density Lipoprotein) | <100 mg/dL | Increased in atherosclerosis | |
| HDL (High-Density Lipoprotein) | >40 mg/dL (M), >50 mg/dL (F) | Decreased in cardiovascular risk | |
| Triglycerides | <150 mg/dL | Increased in metabolic syndrome |
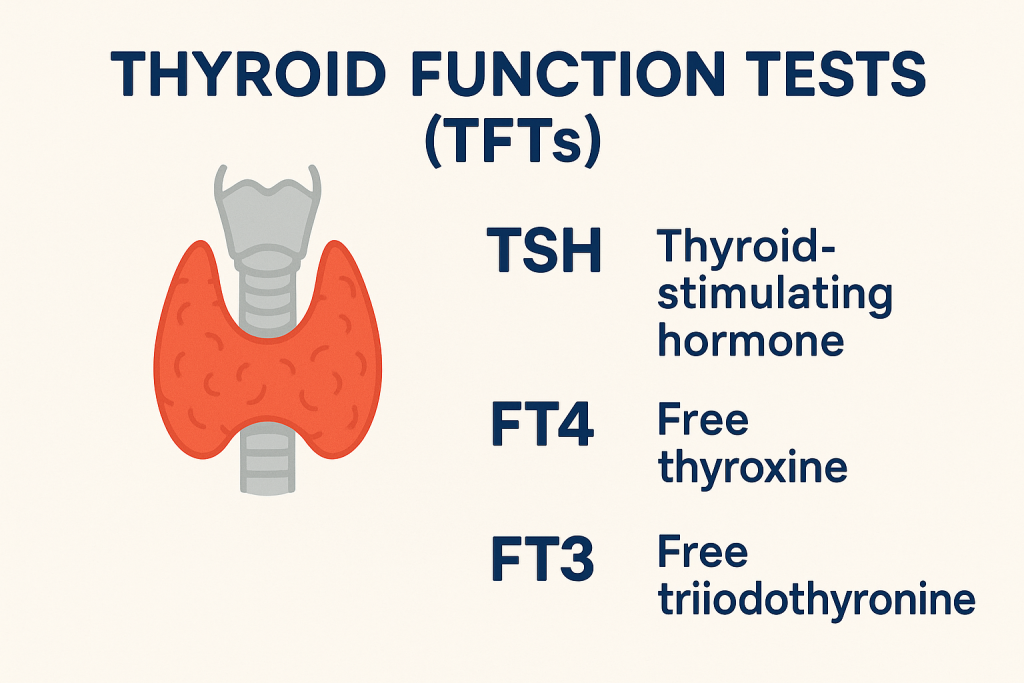
5. Thyroid Function Tests (TFTs)
Thyroid function tests assess thyroid hormone production.
| Test | Biochemical Parameter | Normal Values | Clinical Significance |
|---|---|---|---|
| Thyroid Hormones | T3 (Triiodothyronine) | 80 – 200 ng/dL | Altered in hyper/hypothyroidism |
| T4 (Thyroxine) | 4.6 – 12 µg/dL | Increased in hyperthyroidism | |
| TSH (Thyroid-Stimulating Hormone) | 0.5 – 5.0 µU/mL | Increased in hypothyroidism |
6. Bone and Mineral Metabolism Tests
These tests assess calcium metabolism and bone health.
| Test | Biochemical Parameter | Normal Values | Clinical Significance |
|---|---|---|---|
| Calcium Metabolism | Total Calcium | 8.5 – 10.5 mg/dL | Altered in osteoporosis, parathyroid disease |
| Ionized Calcium | 4.5 – 5.6 mg/dL | Important in neuromuscular function | |
| Phosphorus | 2.5 – 4.5 mg/dL | Altered in kidney & bone disorders | |
| Vitamin D (25-hydroxy) | 20 – 50 ng/mL | Decreased in rickets, osteoporosis | |
| Parathyroid Hormone (PTH) | 10 – 55 pg/mL | Increased in hyperparathyroidism |
7. Acid-Base Balance and Arterial Blood Gas (ABG) Analysis
These tests evaluate blood pH, oxygenation, and carbon dioxide balance.
| Test | Biochemical Parameter | Normal Values | Clinical Significance |
|---|---|---|---|
| Blood pH | pH | 7.35 – 7.45 | Altered in acidosis/alkalosis |
| Blood Gases | pCO₂ (Partial CO₂ pressure) | 35 – 45 mmHg | Altered in respiratory conditions |
| pO₂ (Partial O₂ pressure) | 80 – 100 mmHg | Decreased in hypoxia | |
| HCO₃⁻ (Bicarbonate) | 22 – 28 mEq/L | Altered in metabolic acidosis/alkalosis |
Renal Function Tests (RFTs) / Kidney Function Tests (KFTs)
Renal function tests are a set of biochemical assessments that evaluate kidney function, primarily by measuring the clearance of metabolic waste products and maintaining electrolyte and fluid balance. The kidneys play a vital role in homeostasis by regulating blood pressure, producing hormones (erythropoietin, renin), and ensuring acid-base balance. Any dysfunction in renal function can lead to serious systemic conditions, including hypertension, fluid overload, and metabolic imbalances.
1. Serum Creatinine
Serum creatinine is a byproduct of muscle metabolism, specifically from creatine phosphate in muscle cells. The kidneys filter creatinine through the glomeruli and excrete it in urine without reabsorption. Elevated creatinine levels indicate impaired renal function.
- Normal Range: 0.6 – 1.2 mg/dL
- Clinical Significance:
- Increased in chronic kidney disease (CKD), acute kidney injury (AKI), glomerulonephritis, and obstructive uropathy.
- Decreased levels may be seen in muscle wasting diseases and malnutrition.
2. Blood Urea Nitrogen (BUN)
Urea is a waste product formed in the liver as a result of protein metabolism and excreted through the kidneys. BUN levels indicate the efficiency of renal clearance.
- Normal Range: 6 – 20 mg/dL
- Clinical Significance:
- Increased BUN suggests renal failure, dehydration, congestive heart failure, or high-protein intake.
- Decreased BUN is seen in liver disease, low-protein diet, and severe malnutrition.
3. Serum Urea
Urea is the nitrogenous end product of protein catabolism. It is freely filtered by the kidneys, and increased levels reflect impaired kidney excretion.
- Normal Range: 15 – 45 mg/dL
- Clinical Significance:
- Elevated urea levels are associated with kidney disease, dehydration, and high protein turnover.
- Low urea levels can indicate liver dysfunction, inadequate protein intake, or increased protein synthesis.
4. Creatinine Clearance (CrCl)
Creatinine clearance is a measure of how well creatinine is removed from the blood by the kidneys. It provides an estimate of the glomerular filtration rate (GFR). The test is conducted using a 24-hour urine collection.
- Normal Range: 90 – 140 mL/min
- Clinical Significance:
- Decreased CrCl indicates kidney failure, chronic kidney disease (CKD), or nephrotic syndrome.
- Increased CrCl may occur in pregnancy and conditions of increased cardiac output.
5. Estimated Glomerular Filtration Rate (eGFR)
eGFR is the most reliable marker of kidney function, calculated based on serum creatinine levels, age, gender, and body size.
- Normal Range: >90 mL/min/1.73m²
- Clinical Significance:
- Stage 1 CKD: eGFR >90 (Normal but with kidney damage)
- Stage 2 CKD: eGFR 60-89 (Mild reduction)
- Stage 3 CKD: eGFR 30-59 (Moderate reduction)
- Stage 4 CKD: eGFR 15-29 (Severe reduction)
- Stage 5 CKD (End-Stage Renal Disease – ESRD): eGFR <15 (Dialysis or transplantation required)
6. Serum Electrolytes
The kidneys regulate electrolyte balance, and abnormal levels indicate kidney dysfunction.
- Sodium (Na⁺):
- Normal Range: 135 – 145 mEq/L
- Increased sodium (Hypernatremia): Dehydration, kidney failure, Cushing’s syndrome.
- Decreased sodium (Hyponatremia): SIADH, diuretics, chronic kidney disease.
- Potassium (K⁺):
- Normal Range: 3.5 – 5.0 mEq/L
- Hyperkalemia (high potassium): Seen in acute kidney failure, CKD, and Addison’s disease.
- Hypokalemia (low potassium): Caused by diuretics, vomiting, and diarrhea.
- Chloride (Cl⁻):
- Normal Range: 96 – 106 mEq/L
- Altered levels are seen in metabolic acidosis/alkalosis and kidney disease.
- Bicarbonate (HCO₃⁻):
- Normal Range: 22 – 28 mEq/L
- Helps maintain acid-base balance. Reduced in metabolic acidosis due to kidney dysfunction.
7. Serum Uric Acid
Uric acid is the end product of purine metabolism and is excreted by the kidneys. Elevated levels are associated with renal impairment.
- Normal Range: 3.5 – 7.2 mg/dL
- Clinical Significance:
- Increased uric acid: Gout, kidney disease, high protein intake, metabolic syndrome.
- Decreased uric acid: Liver disease, SIADH, and certain medications.
8. Urine Tests for Kidney Function
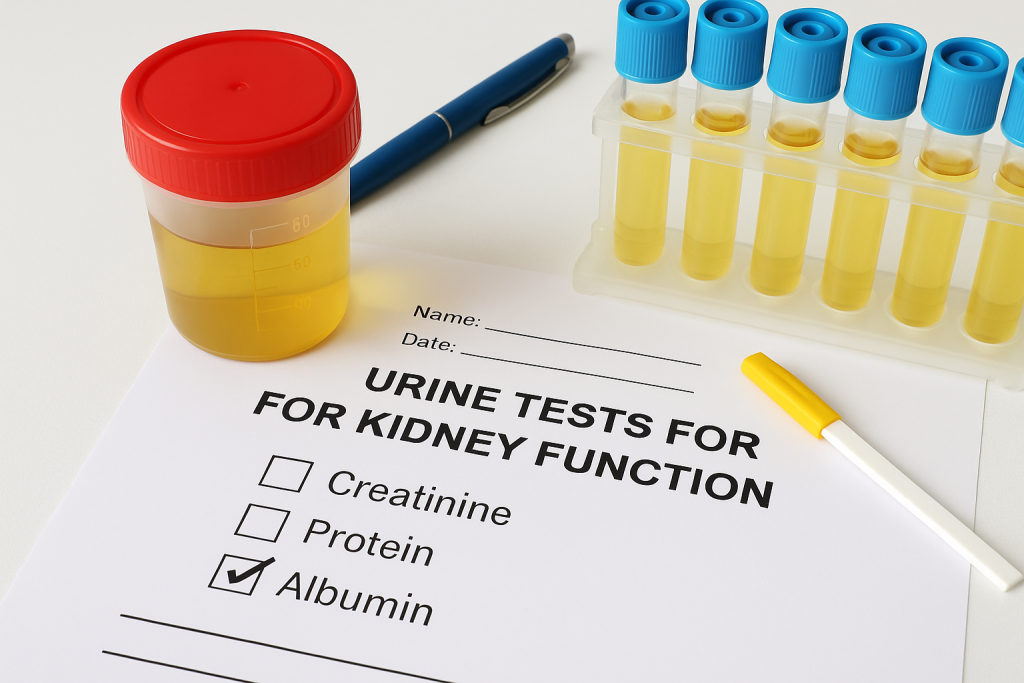
- Urine Protein (Proteinuria / Albuminuria)
- Normal: <150 mg/day
- Microalbuminuria (30 – 300 mg/day): Early kidney disease, diabetic nephropathy.
- Macroalbuminuria (>300 mg/day): Advanced kidney disease.
- Urine Specific Gravity
- Normal Range: 1.005 – 1.030
- Indicates the kidney’s ability to concentrate urine.
- Low specific gravity suggests renal tubular damage.
- Urine pH
- Normal Range: 4.5 – 8.0
- Acidic urine in metabolic acidosis, diabetes, starvation.
- Alkaline urine in urinary tract infections (UTIs), renal tubular acidosis.
- Urine Casts
- Hyaline casts: Normal or seen in dehydration.
- RBC casts: Glomerulonephritis, renal trauma.
- WBC casts: Pyelonephritis.
9. Arterial Blood Gas (ABG) Analysis
Patients with kidney dysfunction may develop metabolic acidosis due to decreased bicarbonate retention.
- pH: 7.35 – 7.45
- HCO₃⁻ (Bicarbonate): 22 – 28 mEq/L
- pCO₂: 35 – 45 mmHg
Metabolic acidosis in kidney failure is indicated by low pH and low HCO₃⁻ levels.
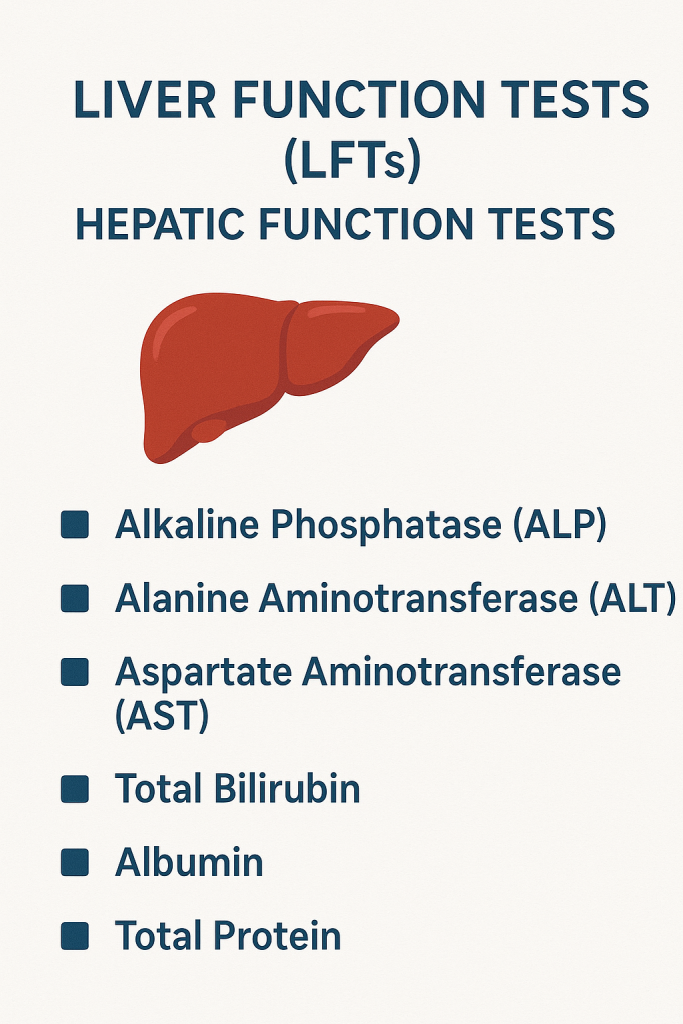
Liver Function Tests (LFTs) / Hepatic Function Tests
Liver function tests (LFTs) are a group of biochemical assessments used to evaluate the liver’s ability to perform its essential functions, including metabolism, detoxification, protein synthesis, and bile production. These tests measure liver enzymes, bilirubin levels, and protein concentrations in the blood to detect liver disease, monitor progression, and assess treatment efficacy.
1. Serum Bilirubin
Bilirubin is a yellow pigment produced from the breakdown of hemoglobin in red blood cells. It is processed in the liver and excreted in bile. Abnormal bilirubin levels indicate liver dysfunction or hemolysis.
- Total Bilirubin (TB): 0.3 – 1.2 mg/dL
- Direct (Conjugated) Bilirubin: 0.1 – 0.4 mg/dL
- Indirect (Unconjugated) Bilirubin: 0.2 – 0.8 mg/dL
Clinical Significance:
- Increased Total & Indirect Bilirubin: Hemolytic anemia, Gilbert’s syndrome, ineffective erythropoiesis.
- Increased Conjugated Bilirubin: Liver diseases like hepatitis, cirrhosis, biliary obstruction (gallstones, tumors).
- Jaundice: Occurs when bilirubin levels exceed 2.5 mg/dL, causing yellow discoloration of the skin and eyes.
2. Liver Enzymes (Hepatic Enzyme Markers)
Liver enzymes are released into the blood when liver cells are damaged. They help in diagnosing different types of liver disease.
a) Alanine Aminotransferase (ALT / SGPT)
ALT is an enzyme found mainly in the liver and is a sensitive marker for liver cell injury.
- Normal Range: 7 – 56 U/L
- Increased in: Hepatitis (viral, alcoholic, autoimmune), liver cirrhosis, fatty liver disease, drug-induced liver injury.
b) Aspartate Aminotransferase (AST / SGOT)
AST is present in the liver, heart, and muscles. It is released when these tissues are damaged.
- Normal Range: 10 – 40 U/L
- Increased in: Liver diseases, myocardial infarction, muscle damage.
- AST/ALT Ratio: A ratio >2 suggests alcoholic liver disease, while a ratio <1 is common in viral hepatitis.
c) Alkaline Phosphatase (ALP)
ALP is found in the liver, bones, and placenta. It is used to assess bile flow and bone metabolism.
- Normal Range: 44 – 147 U/L
- Increased in: Biliary obstruction (gallstones, tumors), cholestatic liver disease, bone diseases (Paget’s disease, osteomalacia).
- Decreased in: Malnutrition, hypothyroidism.
d) Gamma-Glutamyl Transferase (GGT)
GGT is an enzyme involved in bile metabolism. It is highly specific for liver damage and alcohol-related liver disease.
- Normal Range: 8 – 61 U/L
- Increased in: Alcoholic liver disease, bile duct obstruction, fatty liver, drug-induced liver damage.
- GGT/ALP Ratio: Helps differentiate liver disease from bone disease. A high ratio indicates liver dysfunction.
3. Serum Proteins
The liver synthesizes essential proteins, including albumin and globulins. Their levels help assess liver function and systemic conditions.
a) Total Protein
- Normal Range: 6.0 – 8.3 g/dL
- Decreased in: Chronic liver disease (cirrhosis), malnutrition, nephrotic syndrome.
b) Serum Albumin
Albumin is the main protein synthesized by the liver. It maintains oncotic pressure and transports substances in the blood.
- Normal Range: 3.5 – 5.0 g/dL
- Decreased in: Chronic liver disease, malnutrition, nephrotic syndrome, protein-losing enteropathy.
- Albumin-to-Globulin Ratio (A/G Ratio): Normally >1; decreased in liver disease.
c) Serum Globulin
- Normal Range: 2.3 – 3.5 g/dL
- Increased in: Chronic infections, autoimmune liver disease (e.g., primary biliary cholangitis).
4. Prothrombin Time (PT) / International Normalized Ratio (INR)
The liver produces clotting factors, and PT/INR measures blood clotting ability.
- Normal PT: 11 – 13.5 seconds
- Normal INR: 0.8 – 1.2
- Prolonged PT/INR in: Liver failure, vitamin K deficiency, disseminated intravascular coagulation (DIC).
- Used to monitor Warfarin therapy in patients with clotting disorders.
5. Ammonia (NH₃)
Ammonia is produced by intestinal bacteria and converted into urea by the liver. Impaired liver function leads to ammonia accumulation, causing hepatic encephalopathy.
- Normal Range: 15 – 45 µg/dL
- Increased in: Liver failure, hepatic encephalopathy, portosystemic shunting.
6. Liver Function Test Patterns in Diseases
Different liver diseases show characteristic LFT abnormalities:
- Hepatitis (Viral, Autoimmune, Drug-Induced)
- Elevated ALT & AST (>10 times normal)
- Mild increase in ALP & GGT
- Increased total & direct bilirubin
- Normal to slightly low albumin
- Alcoholic Liver Disease
- AST/ALT ratio >2
- Markedly elevated GGT
- Increased ALP
- Decreased albumin with prolonged PT
- Cirrhosis (Chronic Liver Disease)
- Mildly elevated AST, ALT, and ALP
- Low albumin and total protein
- Prolonged PT/INR
- Increased bilirubin (advanced cases)
- Obstructive Jaundice (Biliary Obstruction)
- High ALP & GGT
- Increased conjugated bilirubin
- Normal to mildly elevated AST & ALT
- Non-Alcoholic Fatty Liver Disease (NAFLD)
- Mild ALT elevation (>AST)
- Normal ALP, bilirubin
- Associated with metabolic syndrome
7. Additional Specialized Liver Tests
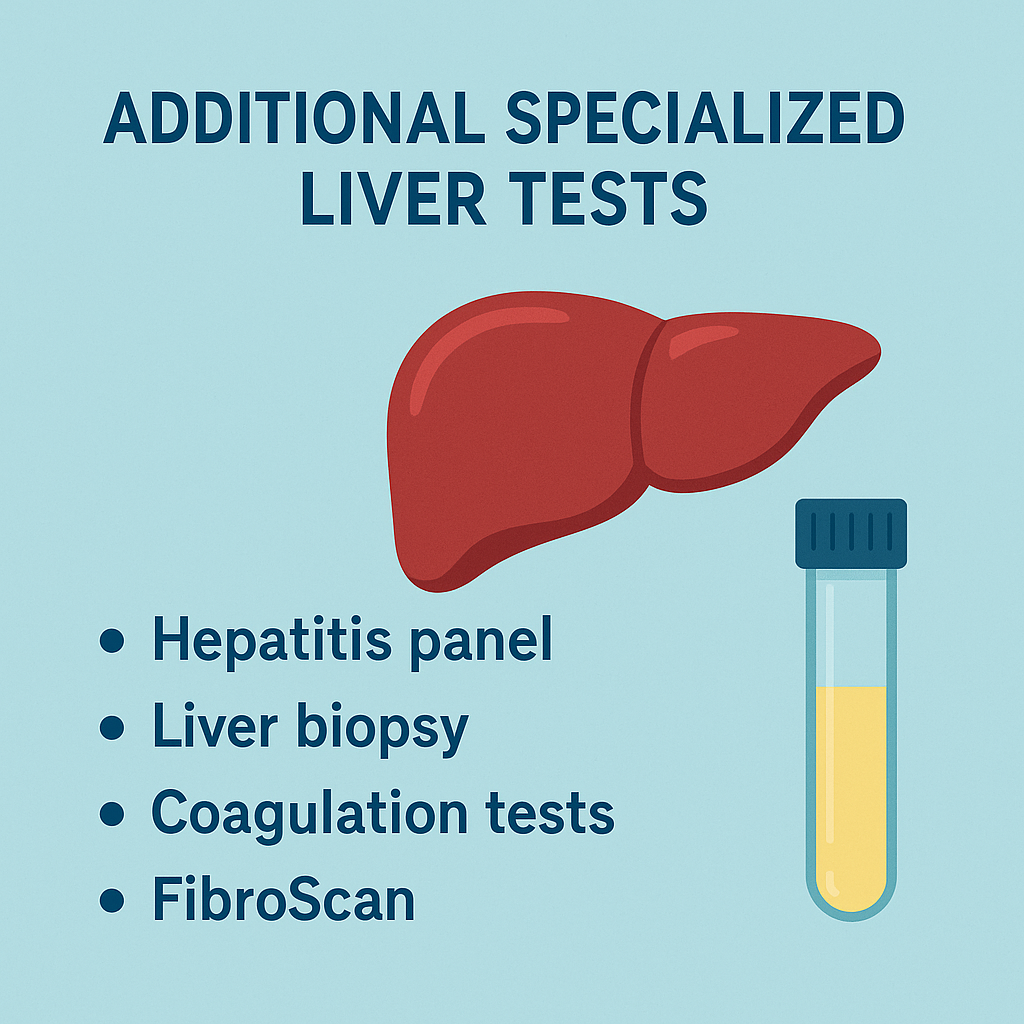
- Hepatitis Serology: Tests for Hepatitis A, B, C, D, and E infections.
- Liver Ultrasound & Imaging: Detects fatty liver, cirrhosis, and tumors.
- Liver Biopsy: Confirms liver fibrosis, cirrhosis, and malignancy.
Thyroid Function Tests (TFTs)
Thyroid function tests (TFTs) are a group of biochemical tests that assess the function of the thyroid gland. The thyroid gland plays a crucial role in regulating metabolism, growth, and energy balance by producing thyroid hormones. Any imbalance in thyroid hormone levels can lead to disorders such as hypothyroidism, hyperthyroidism, and autoimmune thyroid diseases.
1. Thyroid-Stimulating Hormone (TSH)
TSH is a hormone secreted by the anterior pituitary gland that stimulates the thyroid gland to produce T3 (Triiodothyronine) and T4 (Thyroxine).
- Normal Range: 0.5 – 5.0 µU/mL
- Clinical Significance:
- Increased TSH: Suggests hypothyroidism (underactive thyroid) due to primary thyroid failure (Hashimoto’s thyroiditis, iodine deficiency).
- Decreased TSH: Indicates hyperthyroidism (overactive thyroid) as seen in Graves’ disease, toxic multinodular goiter, or excessive thyroid hormone intake.
2. Thyroxine (T4) – Total and Free
T4 is the primary hormone produced by the thyroid gland, which is converted into the more active T3 in tissues.
- Total T4 Normal Range: 4.6 – 12.0 µg/dL
- Free T4 (FT4) Normal Range: 0.8 – 2.0 ng/dL
- Clinical Significance:
- Increased T4/FT4: Hyperthyroidism (Graves’ disease, thyroid nodules, excessive iodine intake).
- Decreased T4/FT4: Hypothyroidism (Hashimoto’s thyroiditis, iodine deficiency, pituitary disorders).
3. Triiodothyronine (T3) – Total and Free
T3 is the biologically active form of thyroid hormone and is derived from T4.
- Total T3 Normal Range: 80 – 200 ng/dL
- Free T3 (FT3) Normal Range: 2.3 – 4.1 pg/mL
- Clinical Significance:
- Increased T3/FT3: Hyperthyroidism (Graves’ disease, T3 thyrotoxicosis).
- Decreased T3/FT3: Hypothyroidism, starvation, severe illness (non-thyroidal illness syndrome).
4. Reverse T3 (rT3)
Reverse T3 is an inactive form of T3 produced under stress, starvation, or severe illness.
- Normal Range: 10 – 24 ng/dL
- Clinical Significance:
- Elevated rT3: Seen in non-thyroidal illness syndrome (euthyroid sick syndrome).
- Decreased rT3: Hypothyroidism.
5. Thyroid Antibodies
Thyroid antibody tests help diagnose autoimmune thyroid disorders.
a) Anti-Thyroid Peroxidase (Anti-TPO) Antibodies
- Normal Range: <35 IU/mL
- Clinical Significance:
- Increased in Hashimoto’s thyroiditis (most common cause of hypothyroidism).
- Also seen in Graves’ disease (autoimmune hyperthyroidism).
b) Anti-Thyroglobulin (Anti-Tg) Antibodies
- Normal Range: <20 IU/mL
- Clinical Significance:
- Present in autoimmune thyroid diseases (Hashimoto’s, Graves’ disease).
- Elevated in thyroid cancer.
c) Thyroid-Stimulating Immunoglobulin (TSI)
- Normal Range: <1.3 IU/L
- Clinical Significance:
- Positive in Graves’ disease (stimulates the thyroid to produce excessive hormones).
6. Thyroglobulin (Tg)
Thyroglobulin is a protein produced by the thyroid gland, mainly used as a tumor marker for thyroid cancer.
- Normal Range: 3 – 40 ng/mL
- Clinical Significance:
- Increased in thyroid cancer, hyperthyroidism, and iodine deficiency.
- Used to monitor recurrence of thyroid cancer after surgery.
7. Calcitonin
Calcitonin is a hormone produced by the parafollicular (C-cells) of the thyroid gland and is involved in calcium homeostasis.
- Normal Range:
- Men: <10 pg/mL
- Women: <5 pg/mL
- Clinical Significance:
- Elevated in medullary thyroid carcinoma (MTC), multiple endocrine neoplasia (MEN-2), and C-cell hyperplasia.
8. Radioactive Iodine Uptake (RAIU) Test
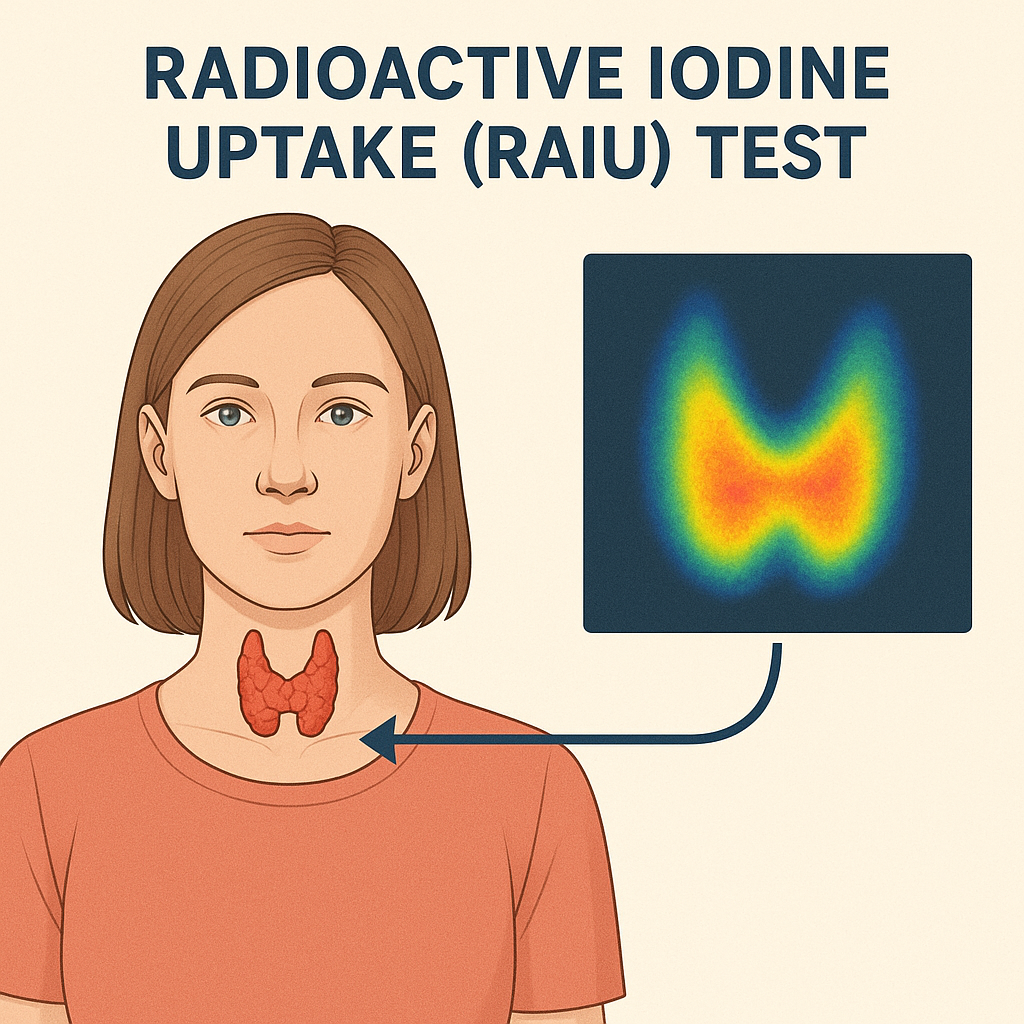
This test measures thyroid iodine uptake and is used to evaluate thyroid function and cause of hyperthyroidism.
- Normal Range:
- 6-hour uptake: 3% – 16%
- 24-hour uptake: 8% – 30%
- Clinical Significance:
- Increased uptake (>30%): Graves’ disease, toxic multinodular goiter.
- Decreased uptake (<3%): Thyroiditis, iodine-induced hyperthyroidism, hypothyroidism.
9. Thyroid Ultrasound
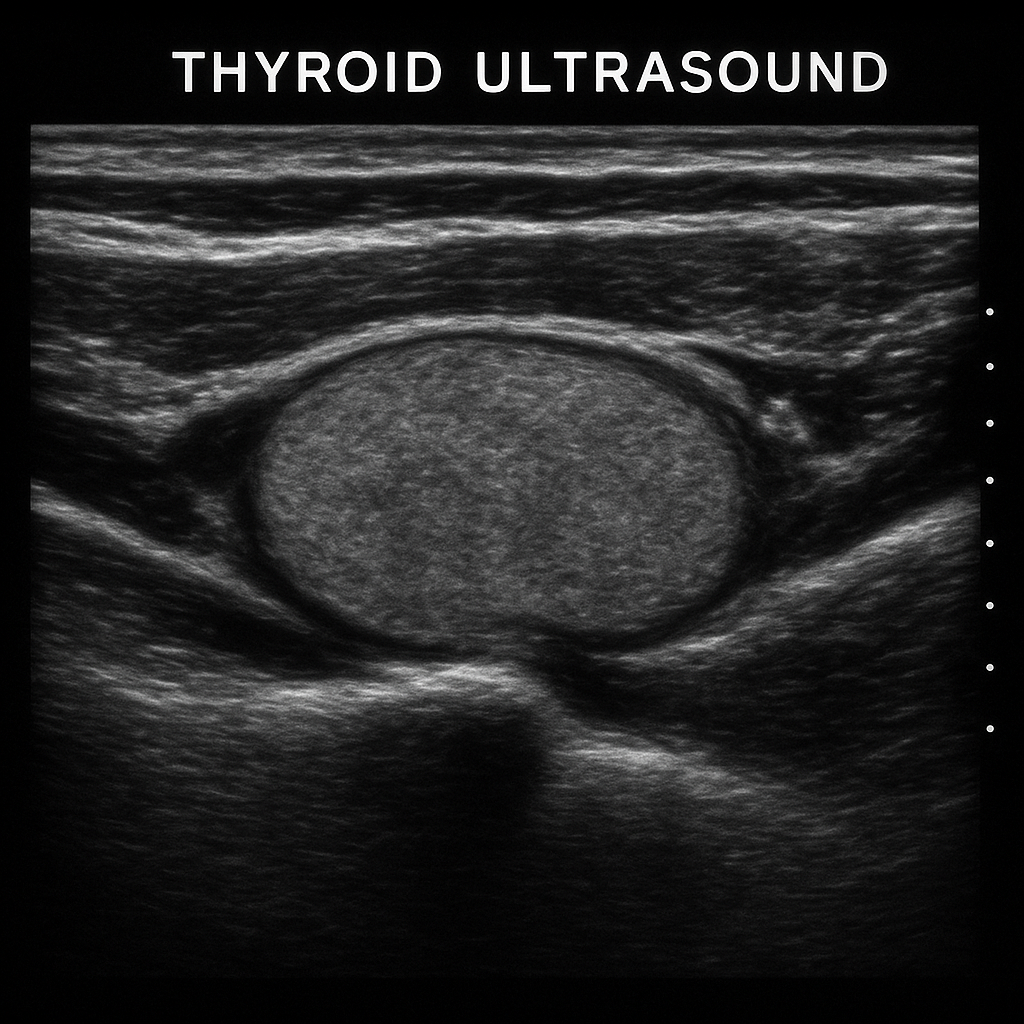
Ultrasound helps in detecting thyroid nodules, goiters, and thyroid cancers.
- Findings of concern:
- Hypoechoic nodules with microcalcifications (suggests thyroid cancer).
- Enlarged thyroid with heterogeneous texture (suggests thyroiditis).
10. Fine Needle Aspiration (FNA) Biopsy
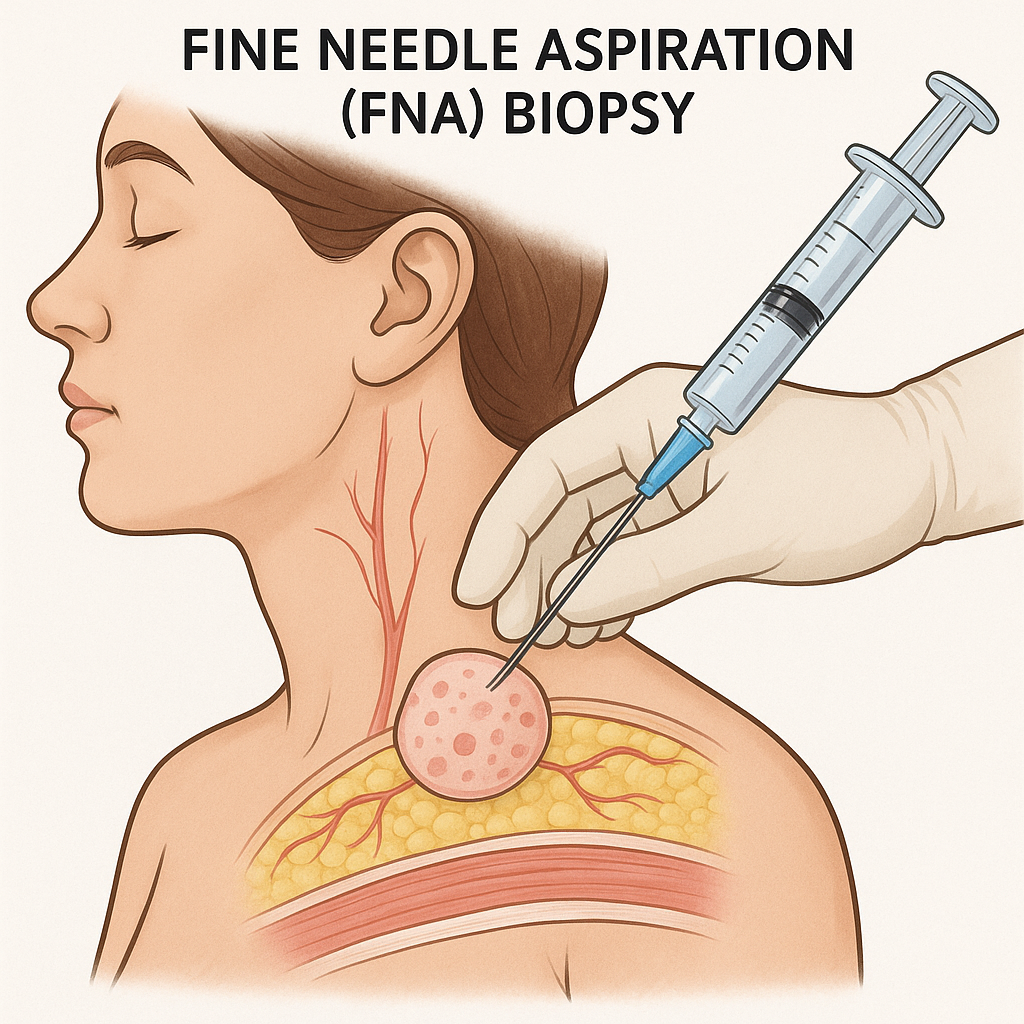
Used to evaluate thyroid nodules for malignancy. If a nodule is >1 cm with suspicious features, FNA is performed.
Thyroid Function Test Patterns in Diseases
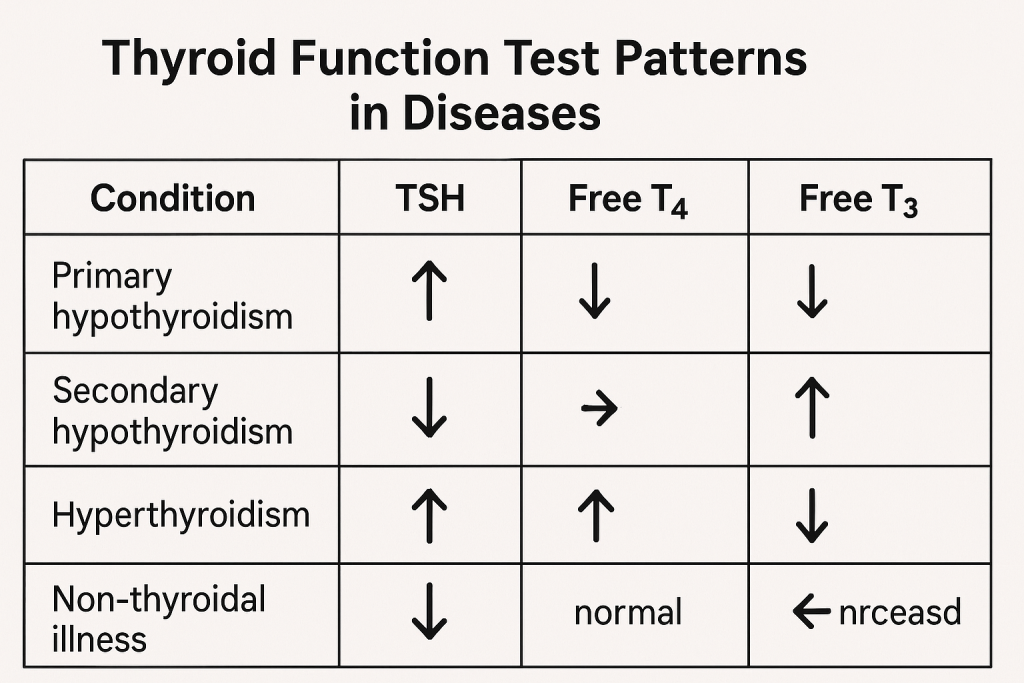
1. Hypothyroidism (Underactive Thyroid)
- Primary Hypothyroidism (Thyroid Failure)
- High TSH, Low T4 & T3
- Common causes: Hashimoto’s thyroiditis, iodine deficiency, post-thyroidectomy.
- Secondary Hypothyroidism (Pituitary Failure)
- Low TSH, Low T4 & T3
- Pituitary tumor, Sheehan’s syndrome.
- Subclinical Hypothyroidism
- Mildly high TSH, Normal T4 & T3
- Seen in early thyroid dysfunction.
2. Hyperthyroidism (Overactive Thyroid)
- Primary Hyperthyroidism (Thyroid Overactivity)
- Low TSH, High T4 & T3
- Causes: Graves’ disease (TSI positive), toxic multinodular goiter, thyroid adenoma.
- Secondary Hyperthyroidism (Excess TSH from Pituitary)
- High TSH, High T4 & T3
- Cause: TSH-secreting pituitary tumor.
- Subclinical Hyperthyroidism
- Low TSH, Normal T4 & T3
- May be due to excessive thyroid hormone intake.