BSC SEM 1 UNIT 6 APPLIED NUTRITION AND DIETETICS
UNIT 6 Minerals
Introduction to Minerals
Definition of Minerals
Minerals are inorganic nutrients that are essential for various physiological functions in the human body. They play a vital role in maintaining health, supporting metabolic processes, and ensuring proper growth and development.
Importance of Minerals in Human Nutrition
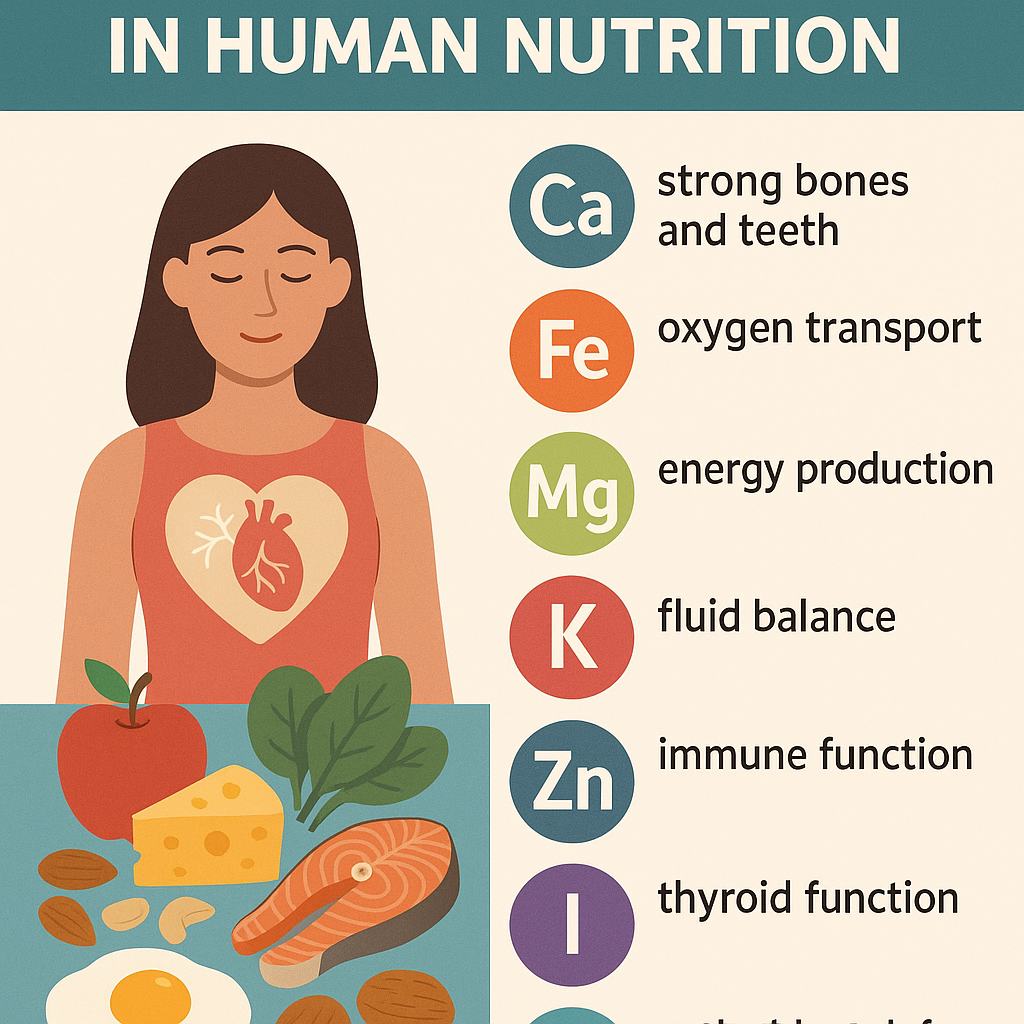
Minerals are classified as macrominerals (major minerals) and microminerals (trace elements) based on the required amounts in the body.
- Macrominerals: Required in larger amounts (>100 mg/day).
- Microminerals (Trace Elements): Required in smaller amounts (<100 mg/day).
These nutrients are involved in:
- Bone and teeth formation (e.g., Calcium, Phosphorus, Fluoride)
- Blood formation and oxygen transport (e.g., Iron)
- Nerve conduction and muscle function (e.g., Sodium, Potassium, Magnesium)
- Enzyme activation and metabolism (e.g., Zinc, Copper, Manganese)
- Fluid balance and acid-base balance (e.g., Sodium, Chloride)
Classification of Minerals
1. Macrominerals (Major Minerals)
| Mineral | Functions | Sources | Deficiency Disorders |
|---|---|---|---|
| Calcium (Ca) | Bone and teeth health, muscle contraction, nerve function, blood clotting | Dairy products, green leafy vegetables, fish with bones | Rickets, Osteoporosis, Tetany |
| Phosphorus (P) | Bone and teeth strength, energy metabolism (ATP), cell repair | Meat, dairy, nuts, whole grains | Weak bones, Muscle weakness |
| Magnesium (Mg) | Nerve and muscle function, enzyme activation | Nuts, seeds, whole grains, leafy vegetables | Muscle cramps, Arrhythmias, Weakness |
| Sodium (Na) | Fluid balance, nerve impulses, blood pressure regulation | Table salt, processed foods, meat | Hyponatremia (muscle cramps, confusion) |
| Potassium (K) | Heart function, muscle contractions, fluid balance | Bananas, oranges, potatoes, leafy vegetables | Hypokalemia (muscle weakness, irregular heartbeat) |
| Chloride (Cl) | Acid-base balance, digestion (HCl production) | Table salt, seafood, vegetables | Muscle cramps, Alkalosis |
| Sulfur (S) | Protein synthesis, detoxification | Eggs, meat, dairy, legumes | Rare (found in protein-rich foods) |
2. Microminerals (Trace Elements)
| Mineral | Functions | Sources | Deficiency Disorders |
|---|---|---|---|
| Iron (Fe) | Hemoglobin synthesis, oxygen transport | Red meat, spinach, legumes, fortified cereals | Anemia, Fatigue, Weakness |
| Zinc (Zn) | Immune function, wound healing, enzyme activity | Meat, seafood, dairy, nuts | Growth retardation, Delayed wound healing |
| Copper (Cu) | Red blood cell production, iron metabolism | Nuts, seeds, whole grains, shellfish | Anemia, Bone abnormalities |
| Iodine (I) | Thyroid hormone synthesis | Iodized salt, seafood, dairy | Goiter, Hypothyroidism |
| Fluoride (F) | Dental health, bone mineralization | Fluoridated water, tea, fish | Dental caries, Weak bones |
| Selenium (Se) | Antioxidant function, thyroid hormone metabolism | Nuts, seafood, eggs | Weak immune system, Keshan disease |
| Manganese (Mn) | Bone formation, metabolism | Whole grains, nuts, tea | Rare, Weak bones |
| Chromium (Cr) | Glucose metabolism, insulin function | Whole grains, meats, broccoli | Impaired glucose tolerance |
| Molybdenum (Mo) | Enzyme activation | Legumes, grains, nuts | Rare |
Functions of Minerals in the Body
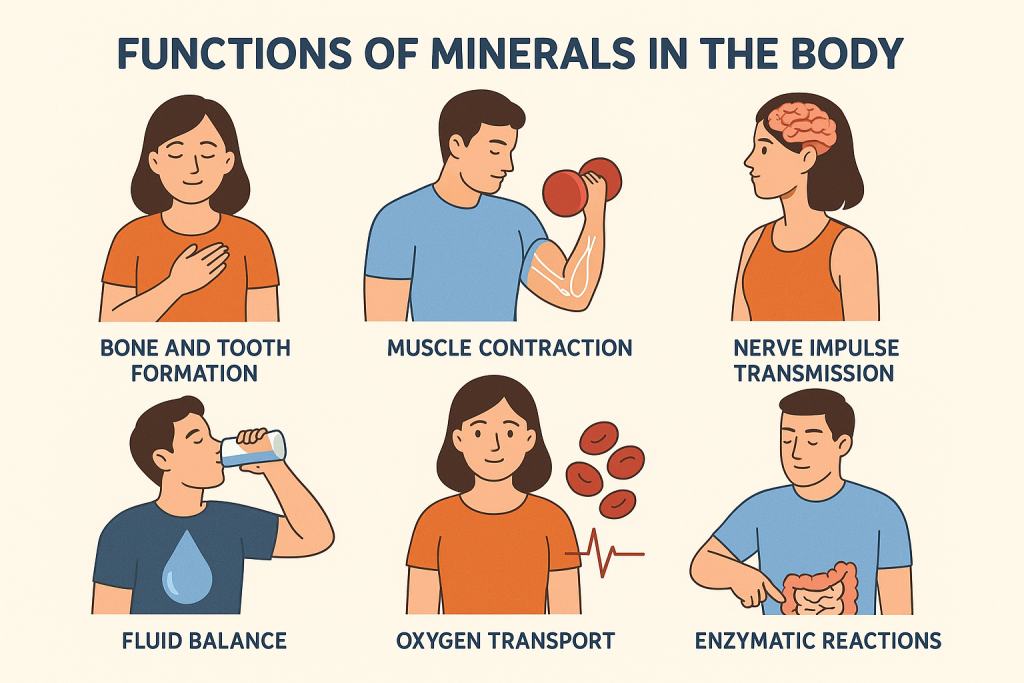
- Structural Role:
- Calcium and phosphorus contribute to the strength of bones and teeth.
- Sulfur is a component of amino acids and proteins.
- Metabolic and Enzymatic Activities:
- Zinc and magnesium act as cofactors for enzymatic reactions.
- Iron is a part of hemoglobin, crucial for oxygen transport.
- Nerve and Muscle Function:
- Sodium, potassium, and magnesium regulate nerve impulses and muscle contractions.
- Fluid and Acid-Base Balance:
- Sodium and potassium help maintain osmotic balance and blood pressure.
- Chloride is essential for gastric acid (HCl) formation.
- Immune and Antioxidant Functions:
- Selenium acts as an antioxidant to protect cells from damage.
- Zinc plays a role in immune responses and wound healing.
Nursing Implications in Mineral Nutrition
- Assessment: Monitor dietary intake, lab values, and signs of deficiency or toxicity.
- Education: Teach patients about mineral-rich foods and supplementation if needed.
- Management: Prevent deficiencies by ensuring a balanced diet, supplementing when necessary, and avoiding excess intake (toxicity risks).
- Special Considerations:
- Pregnant and lactating women require higher amounts of calcium and iron.
- Patients with chronic kidney disease need controlled intake of potassium, sodium, and phosphorus.
- Older adults are at risk of osteoporosis due to decreased calcium absorption.
Classification of Minerals
Minerals are essential inorganic nutrients required for various physiological functions in the human body. They are classified based on the amount required by the body into two main categories:
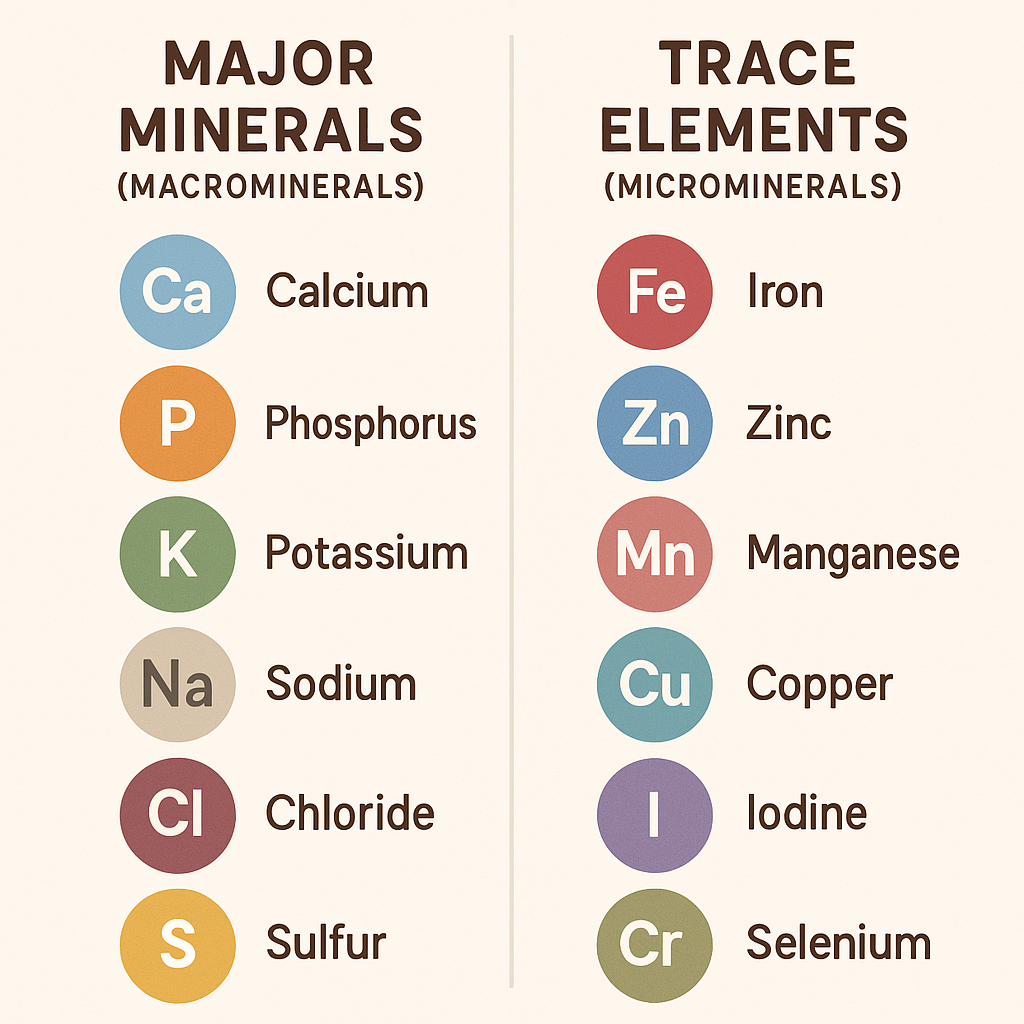
1. Macrominerals (Major Minerals)
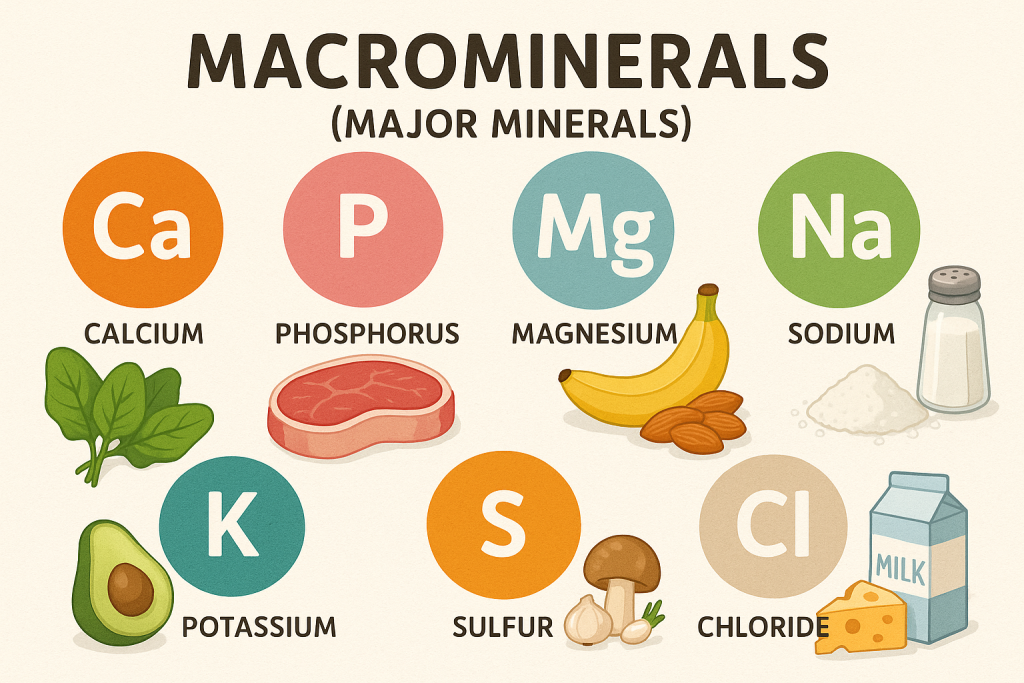
- Required in larger amounts (>100 mg per day)
- Function: Involved in bone health, fluid balance, nerve conduction, and muscle function.
List of Macrominerals
| Mineral | Functions | Sources | Deficiency Disorders |
|---|---|---|---|
| Calcium (Ca) | Bone and teeth health, muscle contraction, blood clotting, nerve transmission | Dairy products, green leafy vegetables, fish with bones | Rickets, Osteoporosis, Tetany |
| Phosphorus (P) | Energy metabolism (ATP), bone mineralization, cell repair | Meat, dairy, nuts, whole grains | Weak bones, Muscle weakness |
| Magnesium (Mg) | Nerve and muscle function, enzyme activation | Nuts, seeds, whole grains, leafy vegetables | Muscle cramps, Arrhythmias, Weakness |
| Sodium (Na) | Fluid balance, nerve impulses, blood pressure regulation | Table salt, processed foods, meat | Hyponatremia (muscle cramps, confusion) |
| Potassium (K) | Heart function, muscle contraction, nerve transmission | Bananas, oranges, potatoes, leafy vegetables | Hypokalemia (muscle weakness, irregular heartbeat) |
| Chloride (Cl) | Acid-base balance, digestion (HCl production) | Table salt, seafood, vegetables | Muscle cramps, Alkalosis |
| Sulfur (S) | Protein synthesis, detoxification | Eggs, meat, dairy, legumes | Rare (found in protein-rich foods) |
2. Microminerals (Trace Elements)
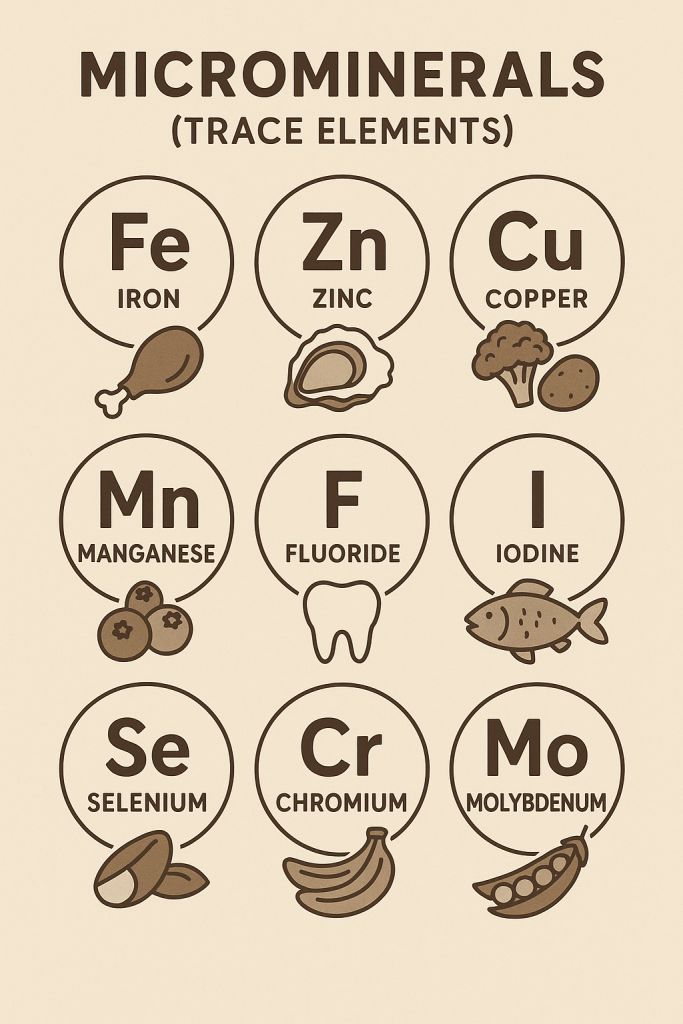
- Required in smaller amounts (<100 mg per day)
- Function: Essential for enzymatic reactions, immune function, metabolism, and oxygen transport.
List of Microminerals (Trace Elements)
| Mineral | Functions | Sources | Deficiency Disorders |
|---|---|---|---|
| Iron (Fe) | Hemoglobin synthesis, oxygen transport | Red meat, spinach, legumes, fortified cereals | Anemia, Fatigue, Weakness |
| Zinc (Zn) | Immune function, wound healing, growth | Meat, seafood, dairy, nuts | Growth retardation, Delayed wound healing |
| Copper (Cu) | Red blood cell production, iron metabolism | Nuts, seeds, whole grains, shellfish | Anemia, Bone abnormalities |
| Iodine (I) | Thyroid hormone synthesis | Iodized salt, seafood, dairy | Goiter, Hypothyroidism |
| Fluoride (F) | Dental health, bone mineralization | Fluoridated water, tea, fish | Dental caries, Weak bones |
| Selenium (Se) | Antioxidant function, thyroid metabolism | Nuts, seafood, eggs | Weak immune system, Keshan disease |
| Manganese (Mn) | Bone formation, metabolism | Whole grains, nuts, tea | Weak bones (rare) |
| Chromium (Cr) | Glucose metabolism, insulin function | Whole grains, meats, broccoli | Impaired glucose tolerance |
| Molybdenum (Mo) | Enzyme activation | Legumes, grains, nuts | Rare |
3. Ultratrace Minerals (Needed in very small amounts)
These minerals are required in extremely small quantities but play a vital role in biological functions.
| Mineral | Functions | Sources |
|---|---|---|
| Nickel (Ni) | Enzyme function, cell metabolism | Nuts, grains, chocolate |
| Silicon (Si) | Bone and connective tissue strength | Whole grains, bananas, green beans |
| Vanadium (V) | Blood sugar control, enzyme regulation | Shellfish, mushrooms, parsley |
| Cobalt (Co) | Component of Vitamin B12 (Cobalamin) | Animal products, dairy |
| Boron (B) | Bone health, hormone regulation | Fruits, nuts, leafy vegetables |
Summary of Mineral Classification
- Macrominerals (Major Minerals) – Required in large amounts (>100 mg/day).
- Microminerals (Trace Elements) – Required in small amounts (<100 mg/day).
- Ultratrace Minerals – Required in minute quantities but essential for enzymatic functions.
Nurses play a crucial role in monitoring, educating, and managing patients’ mineral intake to prevent deficiencies and promote overall health.
Calcium: An Essential Mineral
Calcium is a vital macromineral required for numerous physiological functions, including bone formation, muscle contraction, nerve signaling, and blood clotting. It is the most abundant mineral in the human body, making up about 1-2% of body weight.
1. Classification of Calcium
A. Based on Dietary Requirements
- Macromineral (Major Mineral):
- Calcium is classified as a macromineral because it is required in large amounts (>100 mg/day).
- Essential Nutrient:
- Calcium is classified as an essential nutrient because the body cannot synthesize it, and it must be obtained through diet or supplements.
B. Based on Absorption and Function
- Bound Calcium:
- Found in bones and teeth (99% of body calcium is stored in bones).
- Free (Ionized) Calcium:
- Found in extracellular fluid (ECF) and blood; regulates physiological processes such as nerve impulse transmission and muscle contraction.
C. Based on Dietary Forms
- Calcium Carbonate – Most common supplement form, needs stomach acid for absorption.
- Calcium Citrate – Easily absorbed and does not require stomach acid.
- Calcium Phosphate – Found in bones and teeth.
- Calcium Gluconate and Calcium Lactate – Used in medical treatment for calcium deficiency.
2. Functions of Calcium
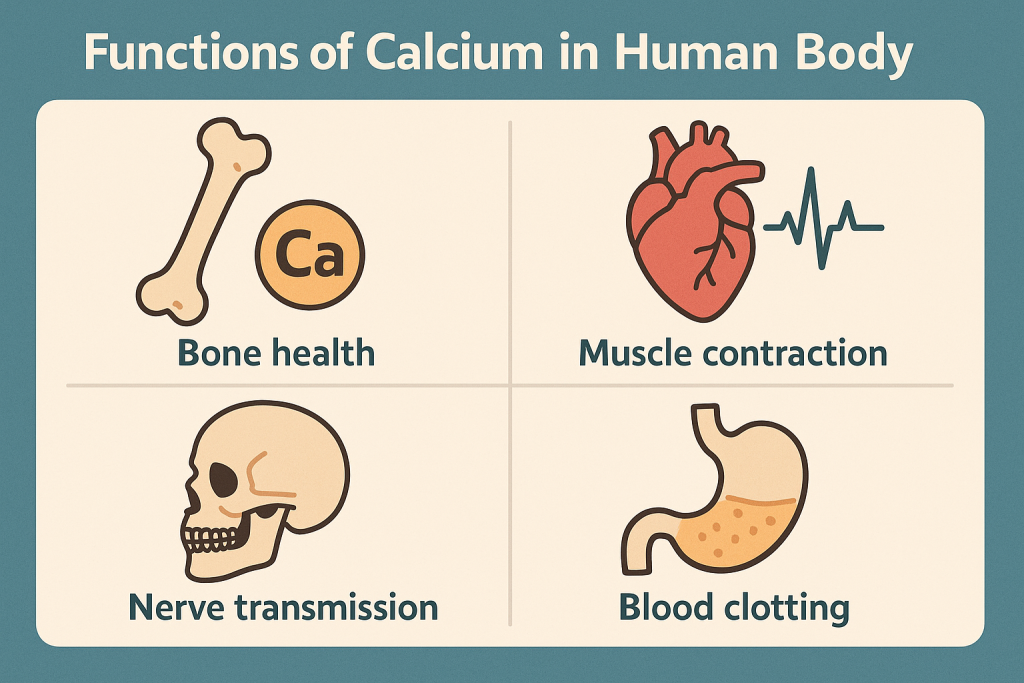
Calcium plays a crucial role in several biological and physiological processes, including:
A. Structural Functions
- Bone and Teeth Formation:
- 99% of the body’s calcium is stored in bones and teeth.
- Provides structural strength and helps in bone remodeling and repair.
B. Physiological and Metabolic Functions
- Muscle Contraction:
- Essential for skeletal, cardiac, and smooth muscle contractions.
- Acts as a trigger for myosin-actin interaction.
- Nerve Impulse Transmission:
- Facilitates nerve conduction and synaptic transmission.
- Helps in the release of neurotransmitters.
- Blood Clotting:
- Acts as a cofactor in the clotting cascade (important for activation of clotting factors like prothrombin to thrombin).
- Enzyme Activation:
- Functions as a cofactor for many enzymes, including those involved in digestion and metabolism.
- Hormone Secretion:
- Regulates the secretion of hormones such as parathyroid hormone (PTH), insulin, and calcitonin.
- Cell Membrane Integrity:
- Maintains cellular structure and permeability.
C. Preventive and Therapeutic Functions
- Prevention of Osteoporosis:
- Adequate calcium intake prevents bone resorption and reduces the risk of osteoporosis in elderly individuals.
- Regulation of Blood Pressure:
- Helps in vasodilation and vasoconstriction, playing a role in blood pressure control.
- Reduces Risk of Colon Cancer:
- Some studies suggest calcium may bind to carcinogens in the intestines, reducing colorectal cancer risk.
3. Dietary Sources of Calcium
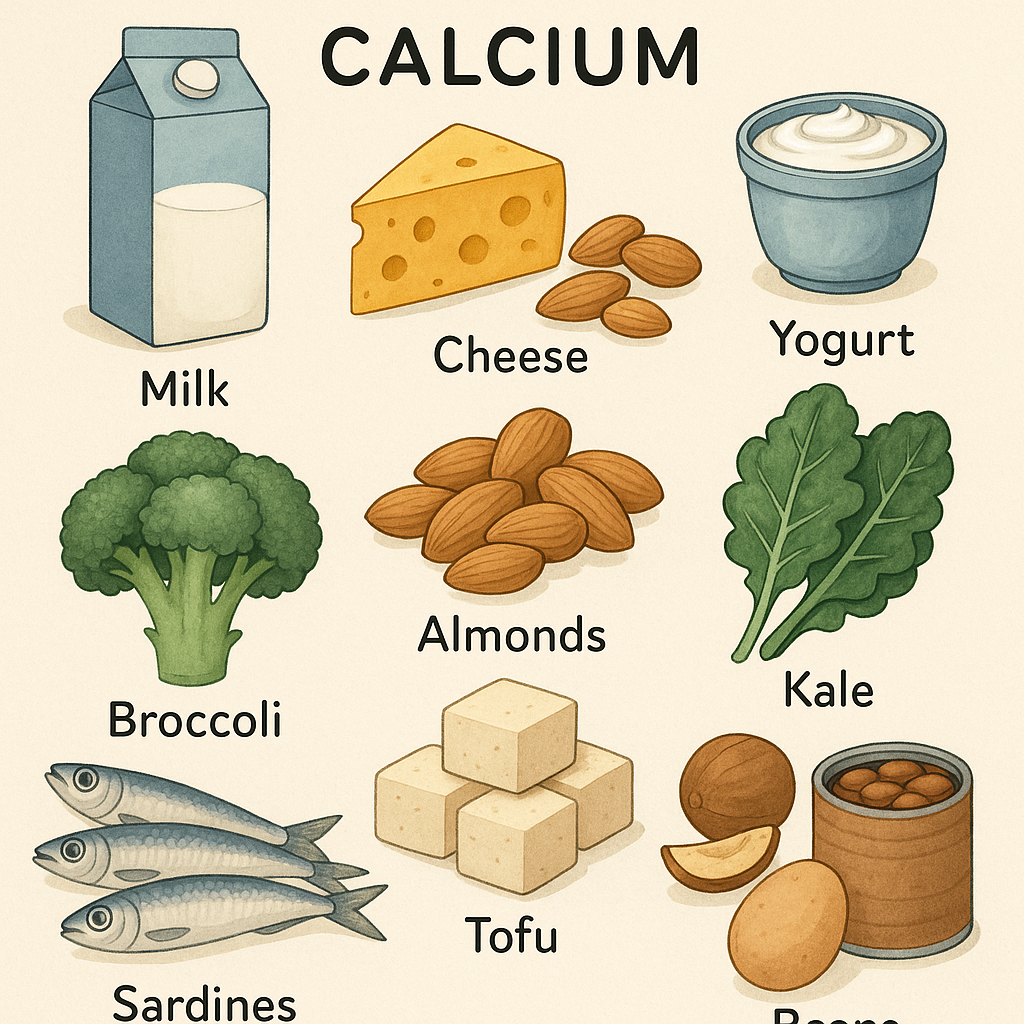
Calcium is obtained from a variety of food sources, categorized as:
A. Animal Sources
- Milk and dairy products (cheese, yogurt, butter, paneer) – Best sources.
- Fish with bones (sardines, salmon).
- Eggs (moderate source).
- Organ meats (moderate source).
B. Plant-Based Sources
- Green leafy vegetables (spinach, kale, amaranth, collard greens).
- Nuts and seeds (almonds, sesame seeds, chia seeds).
- Legumes and pulses (soybeans, chickpeas, lentils).
- Fruits (oranges, figs, apricots).
- Fortified foods (calcium-fortified cereals, tofu, plant-based milk like almond or soy milk).
4. Recommended Dietary Allowance (RDA) of Calcium
The daily calcium requirement varies based on age, gender, and physiological conditions like pregnancy and lactation.
| Age Group | RDA (mg/day) |
|---|---|
| Infants (0-6 months) | 200 mg |
| Infants (7-12 months) | 260 mg |
| Children (1-3 years) | 700 mg |
| Children (4-8 years) | 1,000 mg |
| Adolescents (9-18 years) | 1,300 mg |
| Adults (19-50 years) | 1,000 mg |
| Women (51+ years) | 1,200 mg |
| Men (51-70 years) | 1,000 mg |
| Men (71+ years) | 1,200 mg |
| Pregnant & Lactating Women | 1,000-1,300 mg |
5. Calcium Absorption and Factors Affecting It
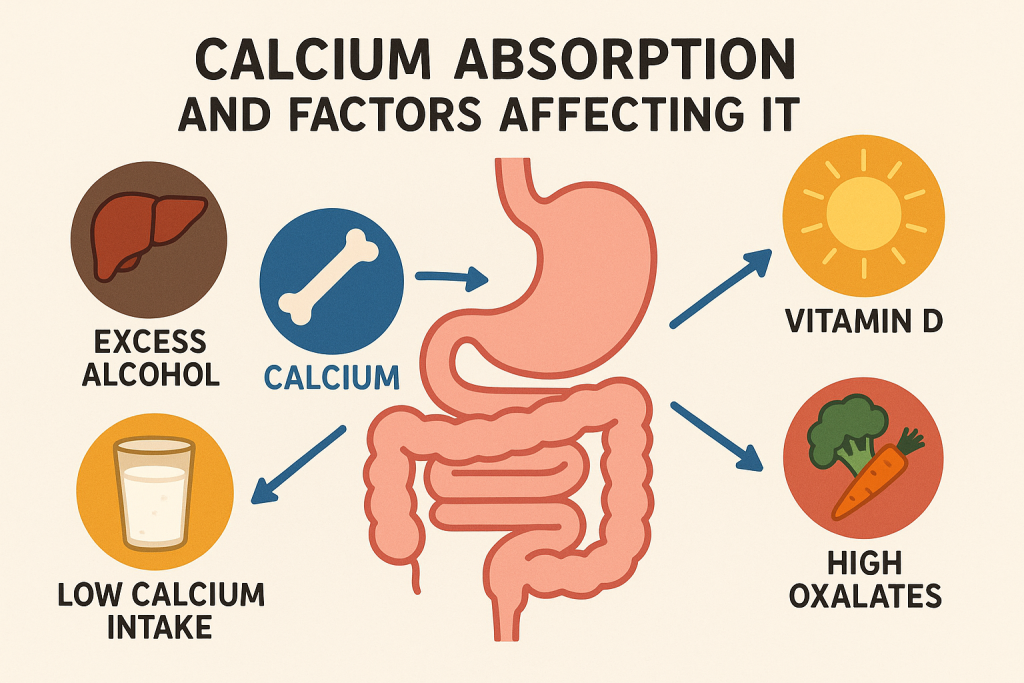
A. Factors Enhancing Calcium Absorption
- Vitamin D:
- Promotes calcium absorption in the intestines.
- Acidic pH in Stomach:
- Enhances solubility of calcium.
- Lactose (Milk Sugar):
- Helps in calcium absorption.
- Parathyroid Hormone (PTH):
- Regulates calcium absorption by increasing Vitamin D activation.
B. Factors Inhibiting Calcium Absorption
- Excess Phytates & Oxalates:
- Found in spinach, whole grains, nuts (bind to calcium and reduce absorption).
- High Sodium Intake:
- Increases calcium excretion through urine.
- Caffeine & Alcohol:
- Reduce calcium absorption.
- Aging:
- Older adults have reduced calcium absorption due to lower gastric acid production.
- High Phosphorus Intake:
- Found in soft drinks, it can hinder calcium balance.
6. Calcium Deficiency (Hypocalcemia)
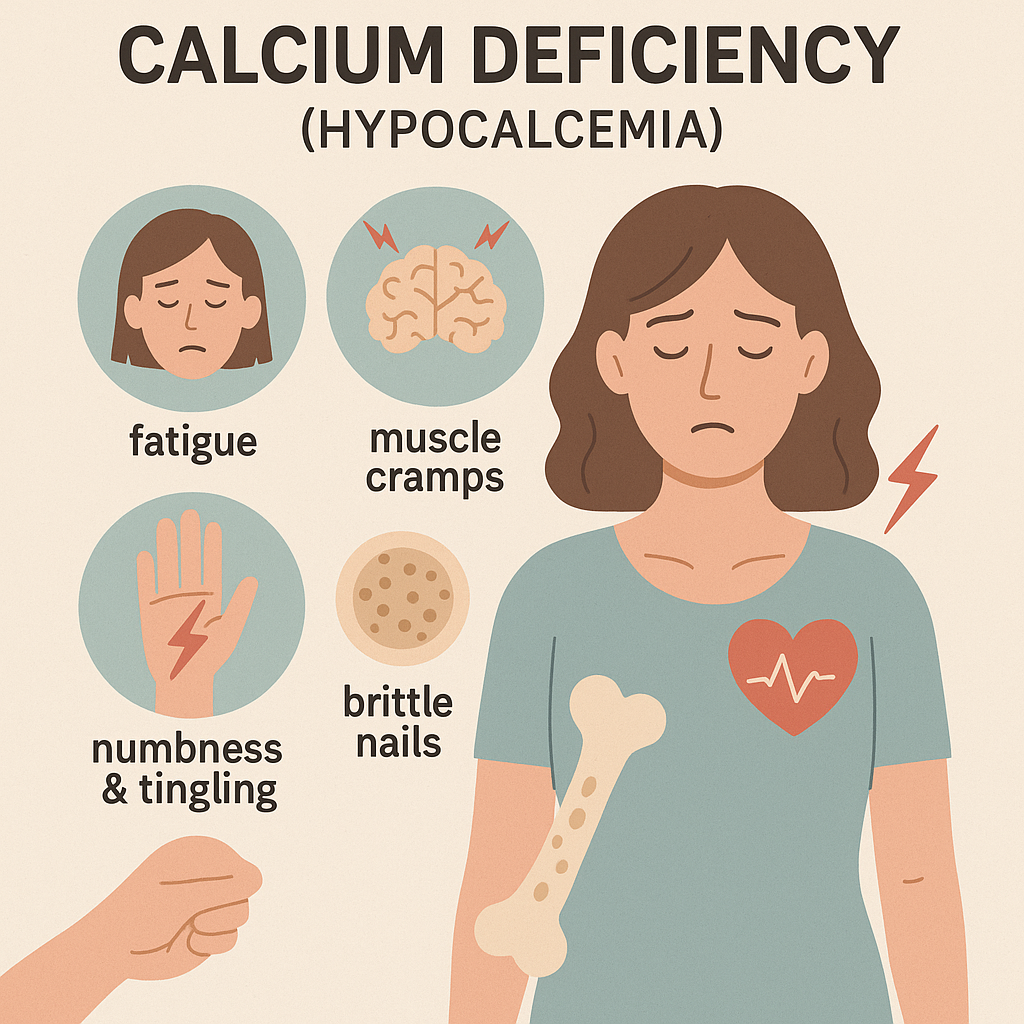
Causes
- Inadequate dietary intake.
- Vitamin D deficiency.
- Malabsorption disorders (Celiac disease, Crohn’s disease).
- Parathyroid gland dysfunction (Hypoparathyroidism).
- Excessive loss due to kidney disease.
Signs & Symptoms
- Muscle cramps and spasms (Tetany).
- Numbness and tingling (especially in hands and feet).
- Bone fractures and osteoporosis.
- Delayed wound healing.
- Dental problems (weak enamel, brittle teeth).
- Cardiac arrhythmias.
7. Calcium Toxicity (Hypercalcemia)
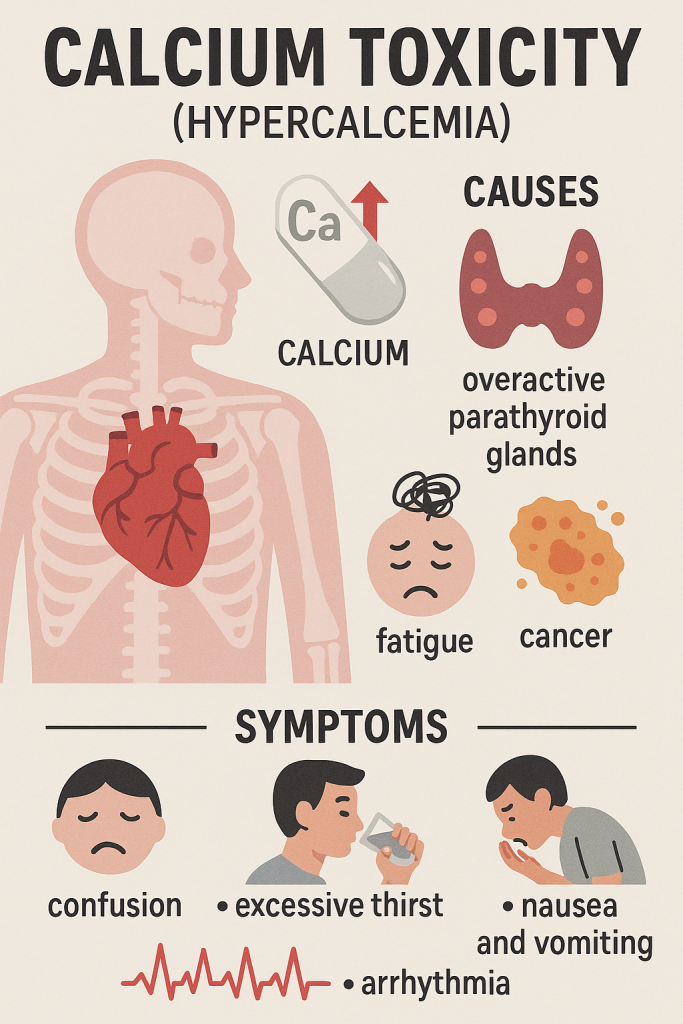
Causes
- Excessive calcium supplementation.
- Hyperparathyroidism.
- Chronic kidney disease.
- Vitamin D overdose.
Signs & Symptoms
- Kidney stones (nephrolithiasis).
- Nausea, vomiting, and constipation.
- Muscle weakness.
- Confusion and fatigue.
- Increased risk of cardiovascular issues.
8. Nursing Implications in Calcium Nutrition
- Patient Assessment:
- Check dietary intake, lab values (serum calcium levels), and signs of deficiency or excess.
- Education:
- Educate patients about calcium-rich foods and the importance of Vitamin D.
- Supplementation Management:
- Recommend appropriate calcium supplements when dietary intake is insufficient.
- Bone Health Promotion:
- Encourage weight-bearing exercises to maintain bone density.
- Monitoring for Toxicity:
- Avoid excessive supplementation to prevent kidney stones and hypercalcemia.
Phosphorus:
Phosphorus is a macromineral that plays a key role in bone health, energy metabolism, and cell function. It is the second most abundant mineral in the human body after calcium, with 85% stored in bones and teeth. It is essential for maintaining acid-base balance, DNA synthesis, and enzymatic functions.
1. Classification of Phosphorus
A. Based on Dietary Requirements
- Macromineral (Major Mineral) – Required in large amounts (>100 mg/day).
- Essential Nutrient – The body cannot synthesize phosphorus, so it must be obtained through food or supplements.
B. Based on Physiological Role
- Structural Phosphorus – Found in bones and teeth as hydroxyapatite.
- Metabolic Phosphorus – Present in ATP, DNA, RNA, and cell membranes (phospholipids).
- Buffer System Phosphorus – Helps maintain acid-base balance in blood.
C. Based on Dietary Forms
- Organic Phosphorus – Found in plant-based foods and animal products.
- Inorganic Phosphorus – Found in food additives and processed foods.
2. Functions of Phosphorus
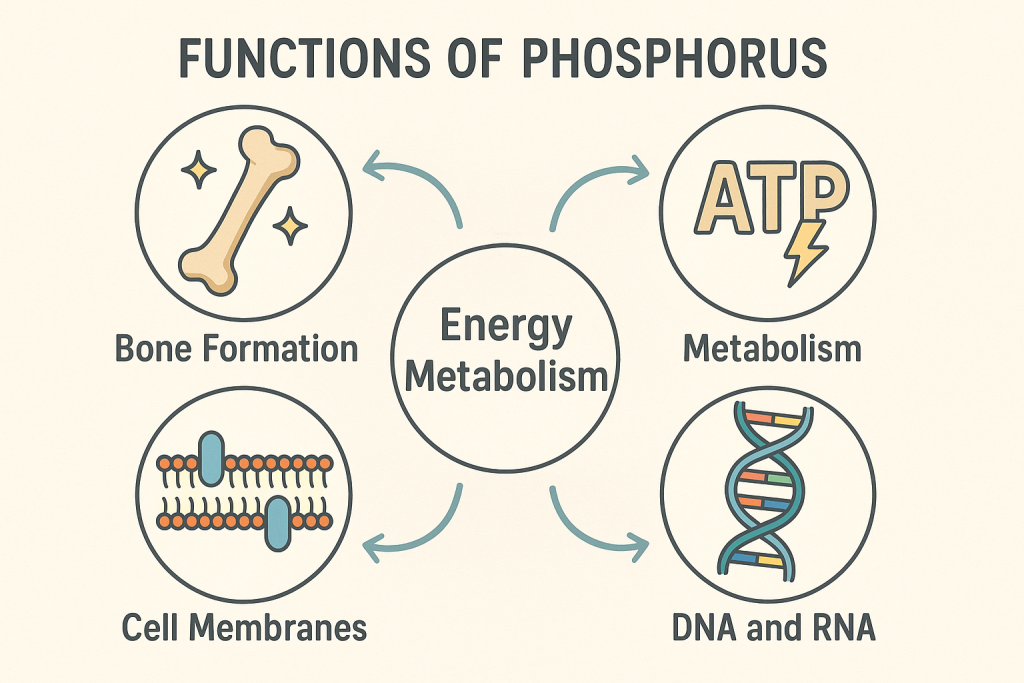
Phosphorus is involved in multiple biological processes essential for health.
A. Structural Functions
- Bone and Teeth Formation:
- 85% of body phosphorus is stored in bones and teeth, providing strength and rigidity.
- Works with calcium and vitamin D for bone mineralization.
B. Physiological and Metabolic Functions
- Energy Metabolism:
- Forms Adenosine Triphosphate (ATP), the body’s main energy molecule.
- Essential for muscle contractions and nerve impulses.
- DNA and RNA Synthesis:
- A key component of genetic material (DNA & RNA), vital for cell replication and protein synthesis.
- Cell Membrane Structure:
- Forms phospholipids, which maintain cell integrity and function.
- Acid-Base Balance:
- Acts as a buffer system in the blood to maintain pH homeostasis.
- Enzyme Activation:
- Plays a role in activating enzymes for metabolism, digestion, and cellular functions.
- Hormone Regulation:
- Helps in hormone signaling pathways and protein activation.
- Oxygen Delivery:
- Forms 2,3-DPG (Diphosphoglycerate) in red blood cells, which helps release oxygen to tissues.
C. Preventive and Therapeutic Functions
- Supports Kidney Function:
- Helps in waste elimination and prevents kidney stones.
- Reduces Muscle Fatigue:
- Helps in ATP synthesis for muscle energy and recovery.
- Aids in Digestion:
- Involved in the metabolism of carbohydrates, fats, and proteins.
3. Dietary Sources of Phosphorus
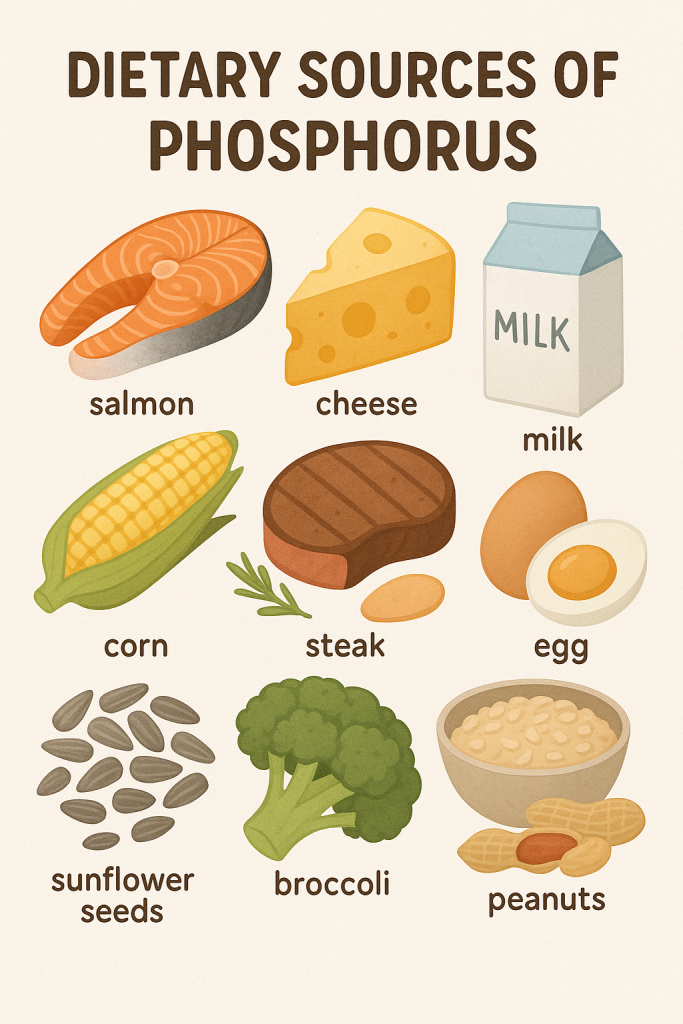
Phosphorus is widely available in both plant-based and animal-based foods.
A. Animal Sources
- Dairy products (milk, cheese, yogurt).
- Meat, poultry, and fish (beef, chicken, turkey, salmon).
- Eggs (moderate source).
- Organ meats (liver, kidney).
B. Plant-Based Sources
- Nuts and seeds (almonds, sunflower seeds, pumpkin seeds).
- Legumes and pulses (lentils, chickpeas, soybeans).
- Whole grains (brown rice, oats, wheat).
- Vegetables (potatoes, garlic, mushrooms).
- Fruits (bananas, raisins, dates).
C. Fortified and Processed Sources
- Soft drinks and colas (contain phosphoric acid).
- Food additives in processed foods (preservatives in canned foods, baked goods).
4. Recommended Dietary Allowance (RDA) of Phosphorus
The RDA for phosphorus varies based on age, gender, and physiological needs.
| Age Group | RDA (mg/day) |
|---|---|
| Infants (0-6 months) | 100 mg |
| Infants (7-12 months) | 275 mg |
| Children (1-3 years) | 460 mg |
| Children (4-8 years) | 500 mg |
| Adolescents (9-18 years) | 1,250 mg |
| Adults (19+ years) | 700 mg |
| Pregnant & Lactating Women | 700 mg |
5. Phosphorus Absorption and Factors Affecting It
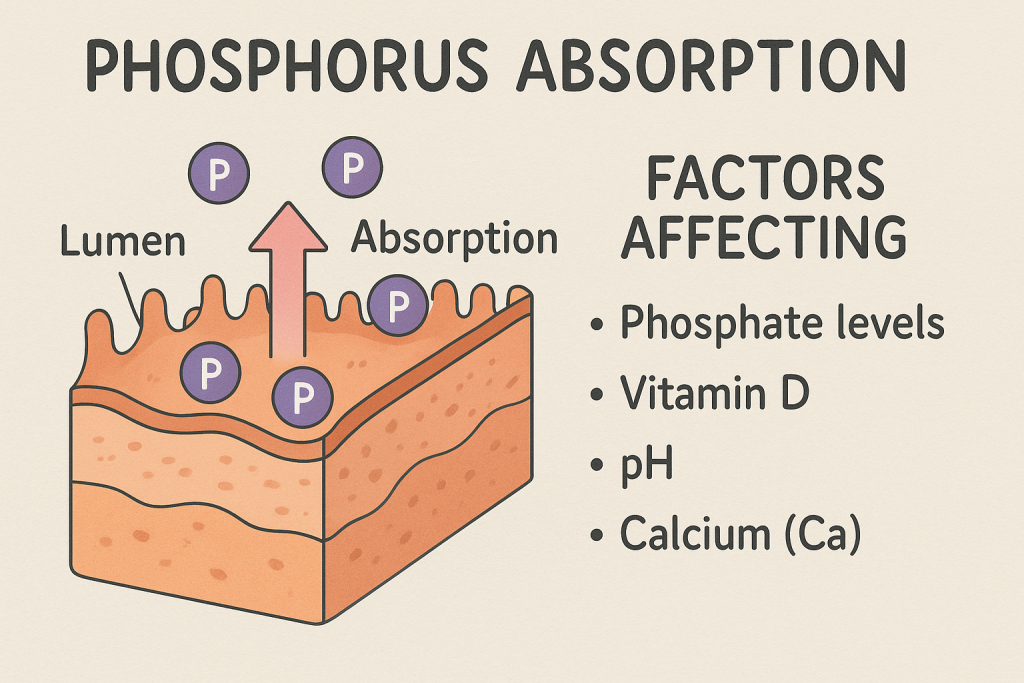
A. Factors Enhancing Phosphorus Absorption
- Vitamin D – Helps in phosphorus absorption from the intestines.
- Calcium-Phosphorus Ratio – Balanced levels prevent bone resorption.
- Acidic pH in the Stomach – Enhances phosphorus solubility.
B. Factors Inhibiting Phosphorus Absorption
- Excess Calcium Intake – High calcium can reduce phosphorus absorption.
- High Phytate Content – Found in whole grains, it binds phosphorus and reduces bioavailability.
- Certain Medications – Antacids containing aluminum interfere with absorption.
- Chronic Kidney Disease (CKD) – Can lead to phosphorus retention, causing imbalances.
6. Phosphorus Deficiency (Hypophosphatemia)
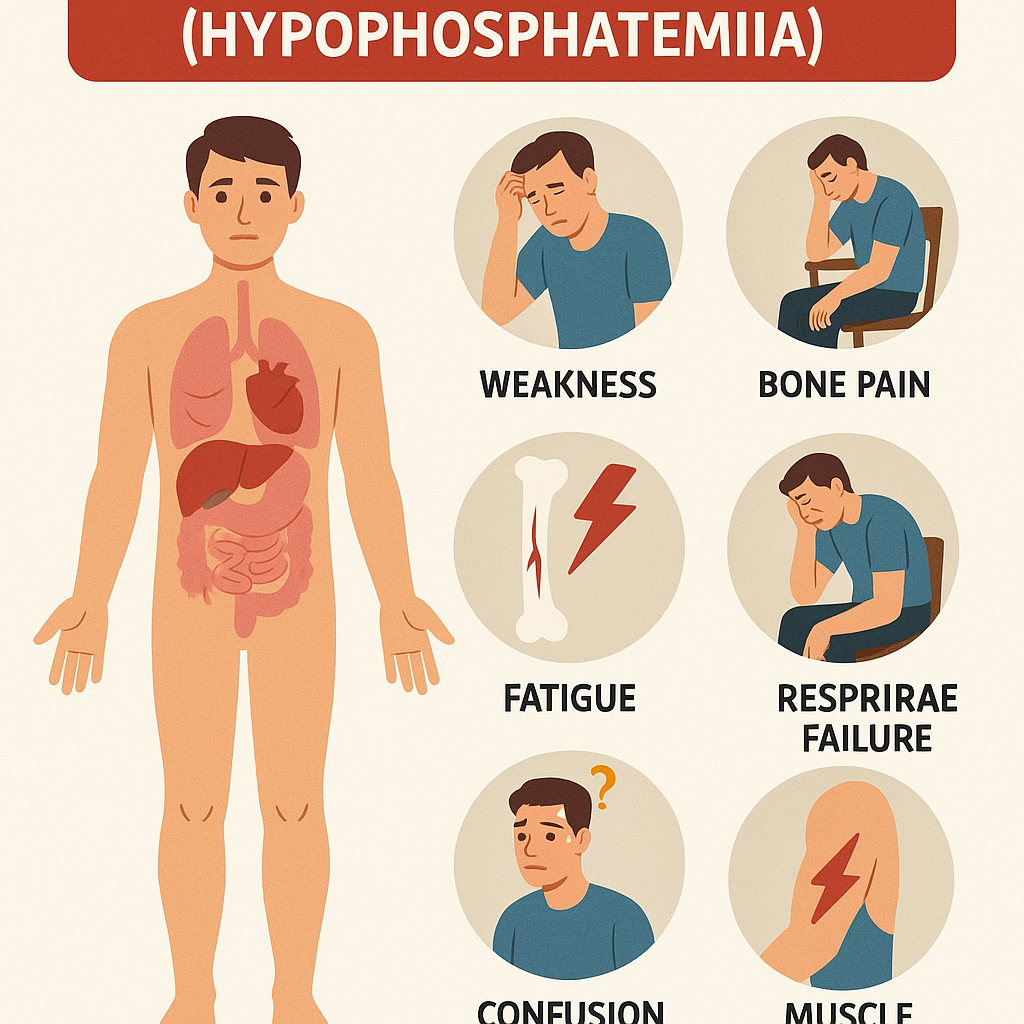
Causes
- Inadequate dietary intake.
- Malabsorption syndromes (Crohn’s disease, celiac disease).
- Chronic alcoholism.
- Hyperparathyroidism (increased PTH lowers phosphorus).
- Excessive use of antacids (aluminum-containing).
Signs & Symptoms
- Weak bones (Osteomalacia, Rickets).
- Muscle weakness and pain.
- Fatigue and irritability.
- Respiratory failure (severe cases).
- Neurological issues (confusion, seizures).
7. Phosphorus Toxicity (Hyperphosphatemia)
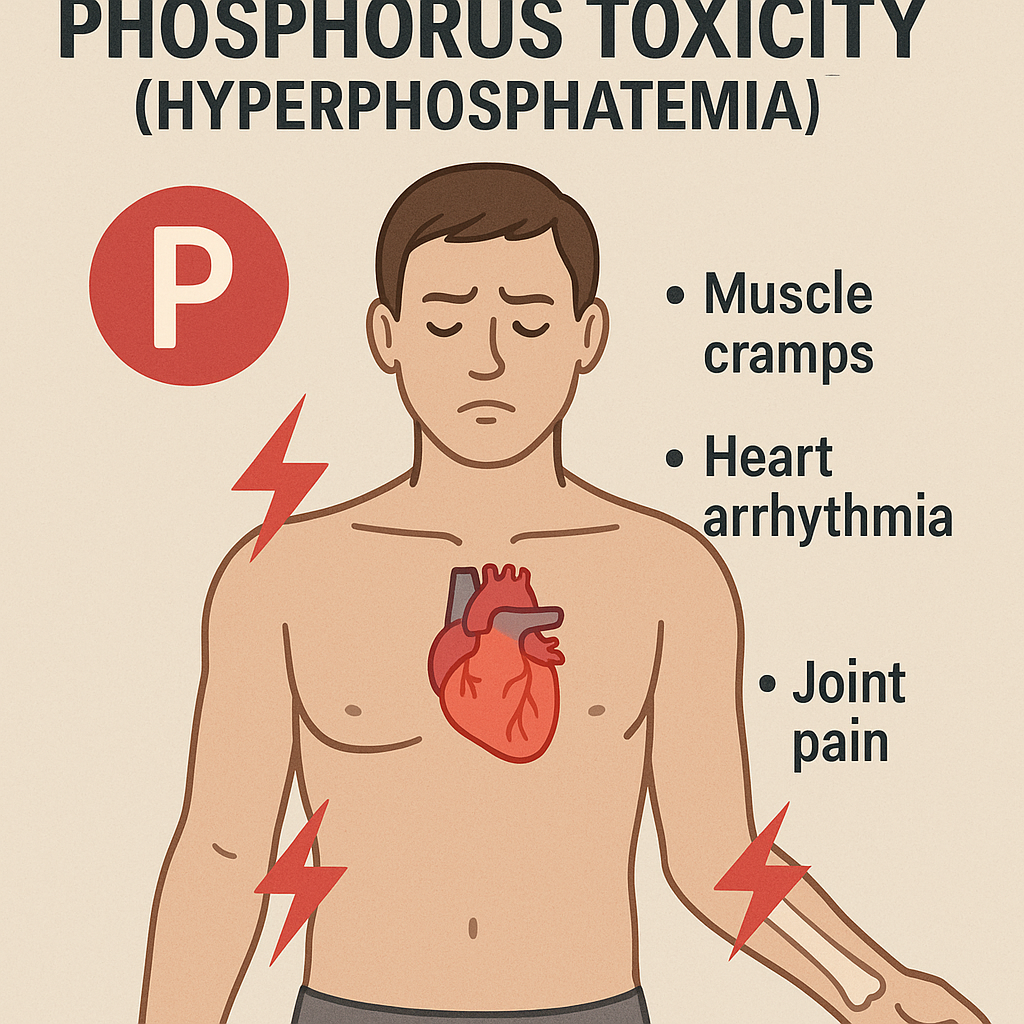
Causes
- Kidney disease (impaired excretion).
- Excess phosphorus intake from soft drinks and processed foods.
- Vitamin D toxicity (increased absorption).
Signs & Symptoms
- Calcium-phosphorus imbalance (leading to bone loss).
- Kidney damage (calcification in soft tissues).
- Muscle cramps and joint pain.
- Cardiovascular issues (risk of heart disease).
8. Nursing Implications in Phosphorus Nutrition
- Patient Assessment:
- Monitor dietary phosphorus intake, lab values (serum phosphorus levels), and signs of deficiency or toxicity.
- Education:
- Teach patients about phosphorus-rich foods and the importance of a balanced calcium-phosphorus ratio.
- Supplementation Management:
- Encourage proper intake for at-risk groups (children, elderly, kidney disease patients).
- Chronic Disease Management:
- Educate kidney disease patients to limit phosphorus intake to prevent complications.
- Monitoring for Toxicity:
- Prevent excessive intake of processed foods, colas, and phosphate additives.
Summary
- Phosphorus is a macromineral essential for bone health, energy production, and DNA synthesis.
- It is abundant in both plant and animal foods, but high phosphorus intake from processed foods can be harmful.
- Deficiency (hypophosphatemia) leads to muscle weakness, bone disorders, and neurological symptoms, while toxicity (hyperphosphatemia) can cause kidney and cardiovascular problems.
- Nurses play a crucial role in educating patients, monitoring phosphorus intake, and managing imbalances to promote optimal health and prevent complications.
Sodium:
Sodium is a macromineral that plays a vital role in fluid balance, nerve impulse transmission, and muscle contraction. It is an essential electrolyte in the body, primarily found in extracellular fluid (ECF). Sodium works closely with potassium and chloride to maintain homeostasis.
1. Classification of Sodium
A. Based on Dietary Requirements
- Macromineral (Major Mineral) – Required in larger amounts (>100 mg/day).
- Essential Electrolyte – Sodium is necessary for survival and must be obtained through food.
B. Based on Physiological Role
- Extracellular Sodium – Found in blood plasma and interstitial fluid, regulates osmotic balance and blood pressure.
- Intracellular Sodium – Found inside cells in smaller amounts, helps in nerve conduction.
- Bound Sodium – Stored in bones and soft tissues, released during deficiency states.
C. Based on Dietary Forms
- Sodium Chloride (NaCl) – Common table salt.
- Sodium Bicarbonate (NaHCO₃) – Found in baking soda, used for acid-base balance.
- Sodium Nitrate/Nitrite – Found in processed meats, used as preservatives.
- Sodium Phosphate – Used as a food additive and in medications.
2. Functions of Sodium
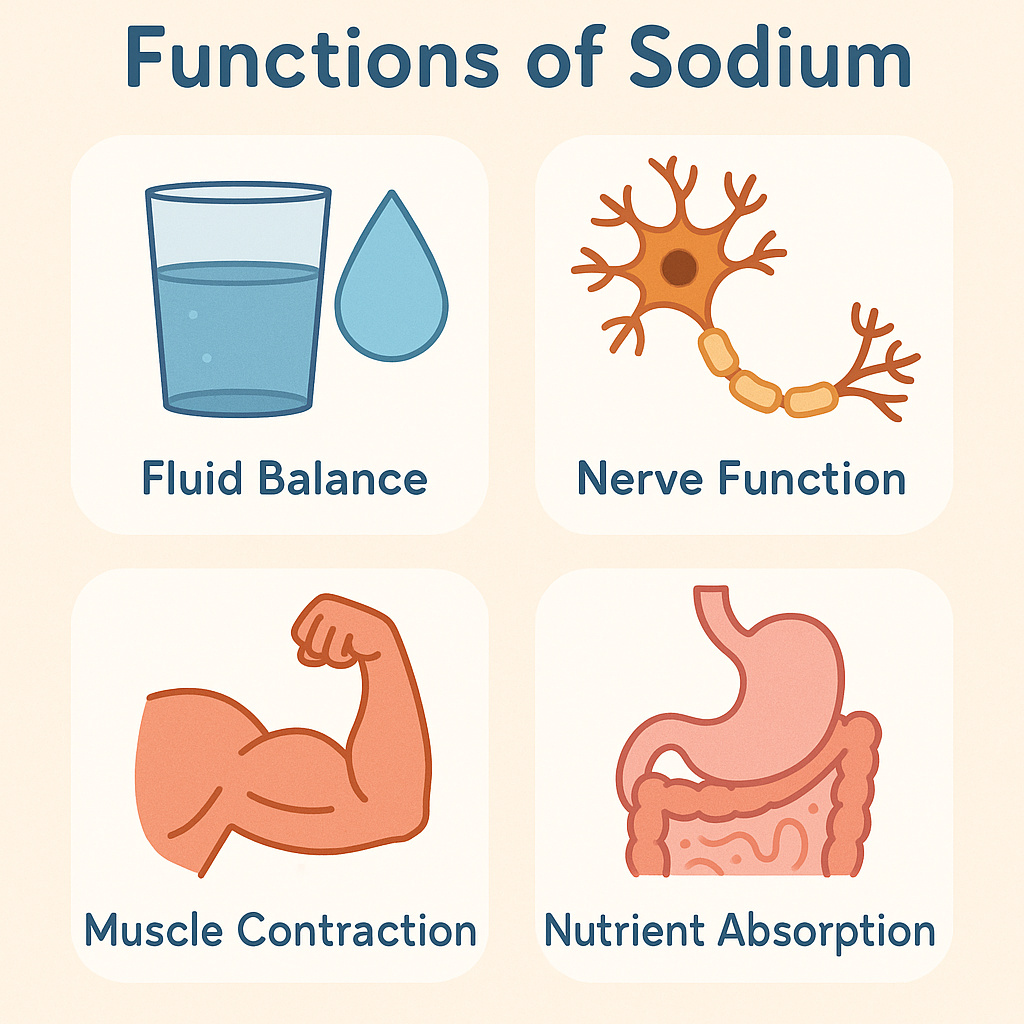
Sodium is essential for several key biological and physiological functions:
A. Structural and Homeostatic Functions
- Maintains Fluid and Electrolyte Balance:
- Sodium regulates water distribution between cells and extracellular fluids.
- Helps prevent dehydration and edema.
- Acid-Base Balance:
- Acts as a buffer system, helping maintain normal blood pH (7.35–7.45).
B. Physiological and Metabolic Functions
- Nerve Impulse Transmission:
- Essential for nerve signal conduction via the sodium-potassium (Na+/K+) pump.
- Helps in muscle coordination and brain function.
- Muscle Contraction and Relaxation:
- Works with calcium and potassium for normal skeletal, cardiac, and smooth muscle contractions.
- Blood Pressure Regulation:
- Sodium levels affect blood pressure, with high intake linked to hypertension.
- Glucose and Nutrient Absorption:
- Sodium plays a role in glucose and amino acid transport in the intestines.
C. Preventive and Therapeutic Functions
- Regulates Sweating and Body Temperature:
- Prevents excessive fluid loss during sweating.
- Shock Prevention:
- Sodium solutions (IV saline) are used to treat hypovolemic shock and dehydration.
- Supports Kidney Function:
- Helps in waste elimination and urine production.
3. Dietary Sources of Sodium
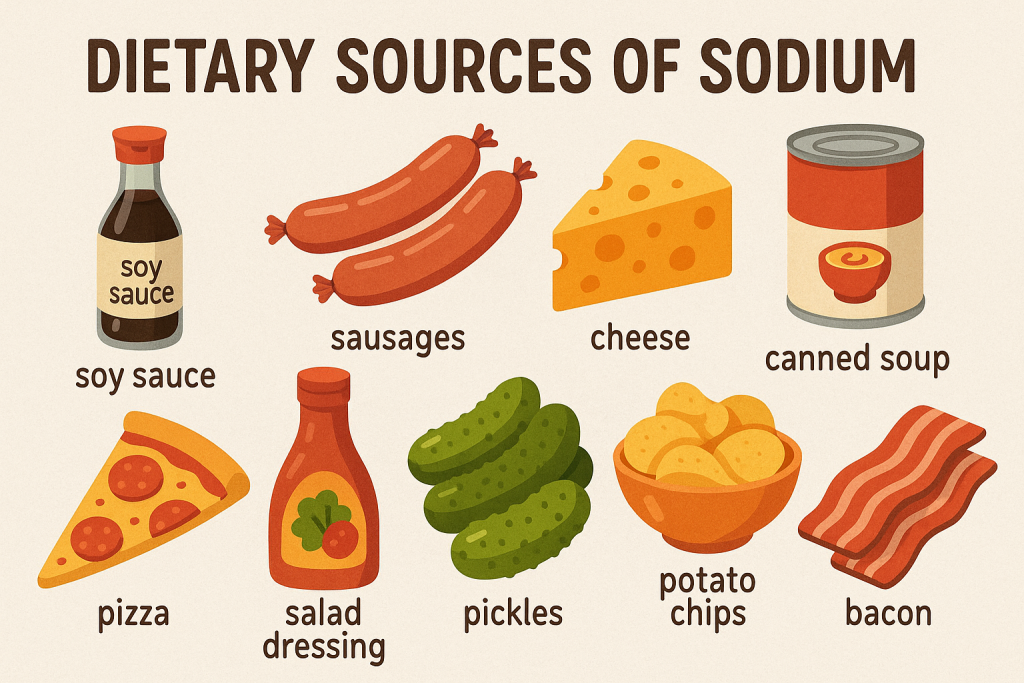
Sodium is present in various natural and processed foods.
A. Natural Sources
- Table salt (sodium chloride) – Primary source.
- Milk and dairy products (cheese, butter).
- Seafood (fish, shellfish, seaweed).
- Eggs (moderate source).
- Vegetables (beets, celery, spinach).
B. Processed and Fortified Sources
- Processed meats (sausages, bacon, ham).
- Canned foods (soups, vegetables, pickles).
- Fast food and snacks (chips, pizza, instant noodles).
- Bakery products (bread, biscuits, cakes, pastries).
- Soft drinks and energy drinks (contain sodium preservatives).
4. Recommended Dietary Allowance (RDA) of Sodium
The daily sodium requirement varies depending on age, health conditions, and activity levels.
| Age Group | RDA (mg/day) |
|---|---|
| Infants (0-6 months) | 120 mg |
| Infants (7-12 months) | 370 mg |
| Children (1-3 years) | 800 mg |
| Children (4-8 years) | 1,000 mg |
| Adolescents (9-18 years) | 1,500 mg |
| Adults (19-50 years) | 1,500 mg |
| Older Adults (51-70 years) | 1,300 mg |
| Elderly (71+ years) | 1,200 mg |
| Pregnant & Lactating Women | 1,500 mg |
Upper Limit (UL):
- The safe upper limit for adults is 2,300 mg/day (≈1 teaspoon of salt).
- High sodium intake increases hypertension risk.
5. Sodium Absorption and Factors Affecting It
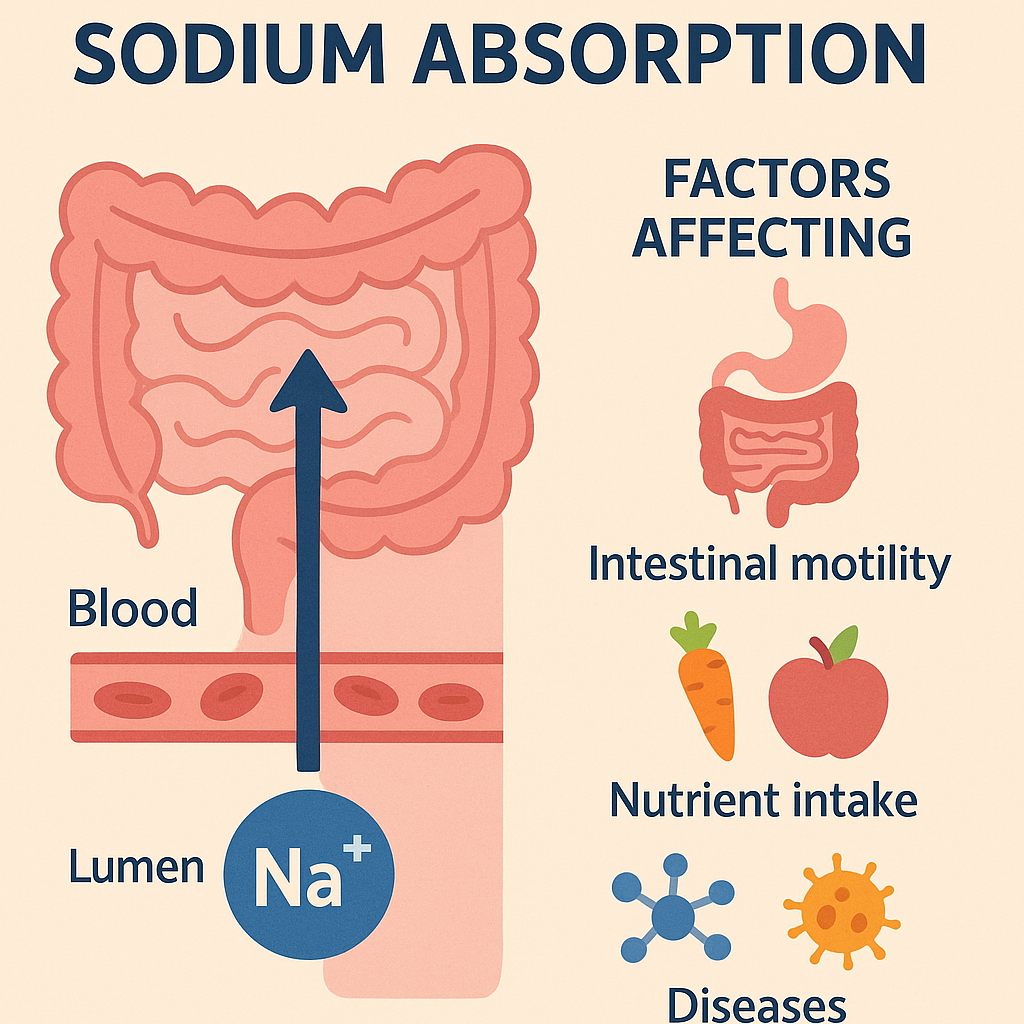
A. Factors Enhancing Sodium Absorption
- Aldosterone Hormone:
- Regulates sodium retention in kidneys.
- Sodium-Potassium Pump:
- Maintains balance between intracellular and extracellular sodium levels.
- Hydration Levels:
- More sodium is retained when fluid intake is low.
B. Factors Inhibiting Sodium Absorption
- Excess Water Intake:
- Leads to dilution and hyponatremia (low sodium levels).
- Diuretics and Medications:
- Cause increased sodium excretion.
- High Potassium Intake:
- Can reduce sodium retention in the body.
6. Sodium Deficiency (Hyponatremia)
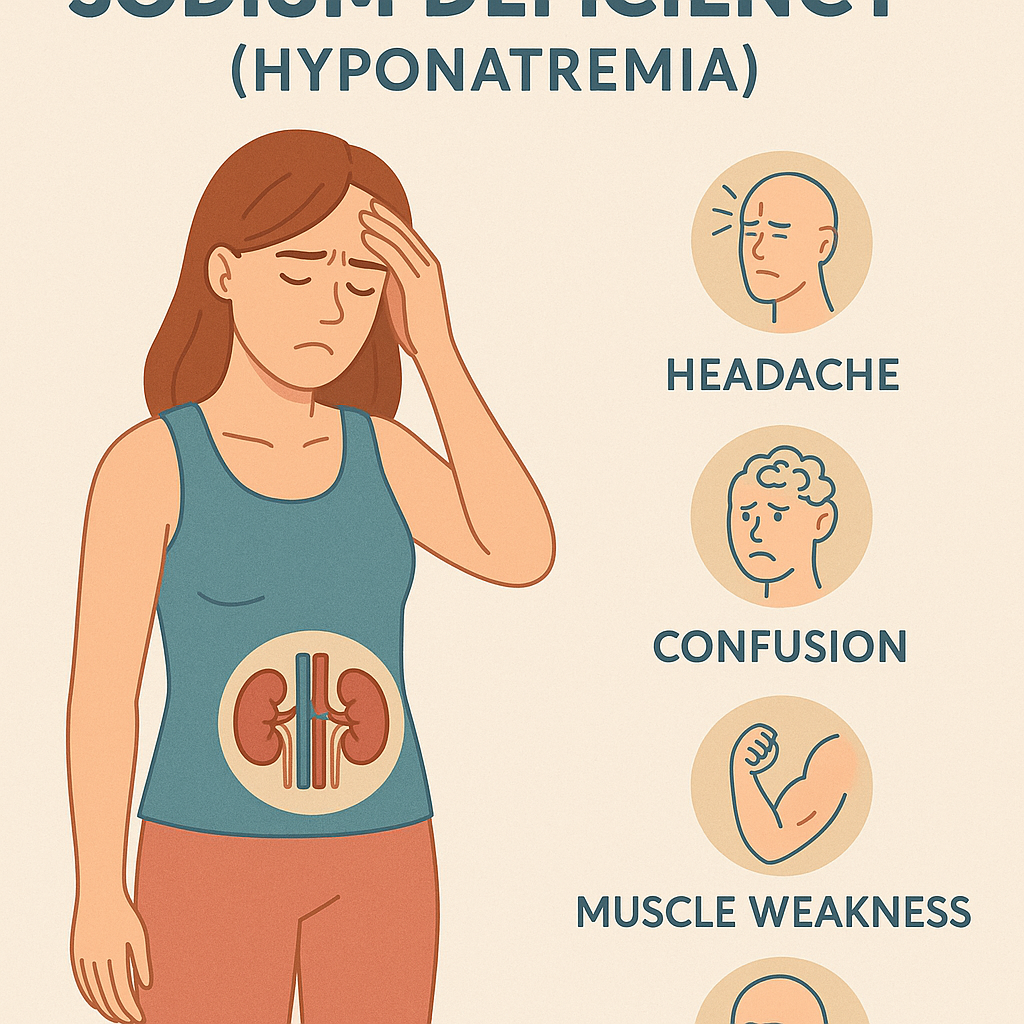
Causes
- Excessive sweating (heatstroke, vigorous exercise).
- Severe vomiting and diarrhea (gastroenteritis).
- Kidney disease (excessive sodium loss).
- Diuretic medications (increased excretion).
- Low-sodium diet (rare but possible).
Signs & Symptoms
- Fatigue and weakness.
- Dizziness and confusion.
- Muscle cramps and twitching.
- Low blood pressure (hypotension).
- Severe cases: Seizures, coma, or death.
7. Sodium Toxicity (Hypernatremia)
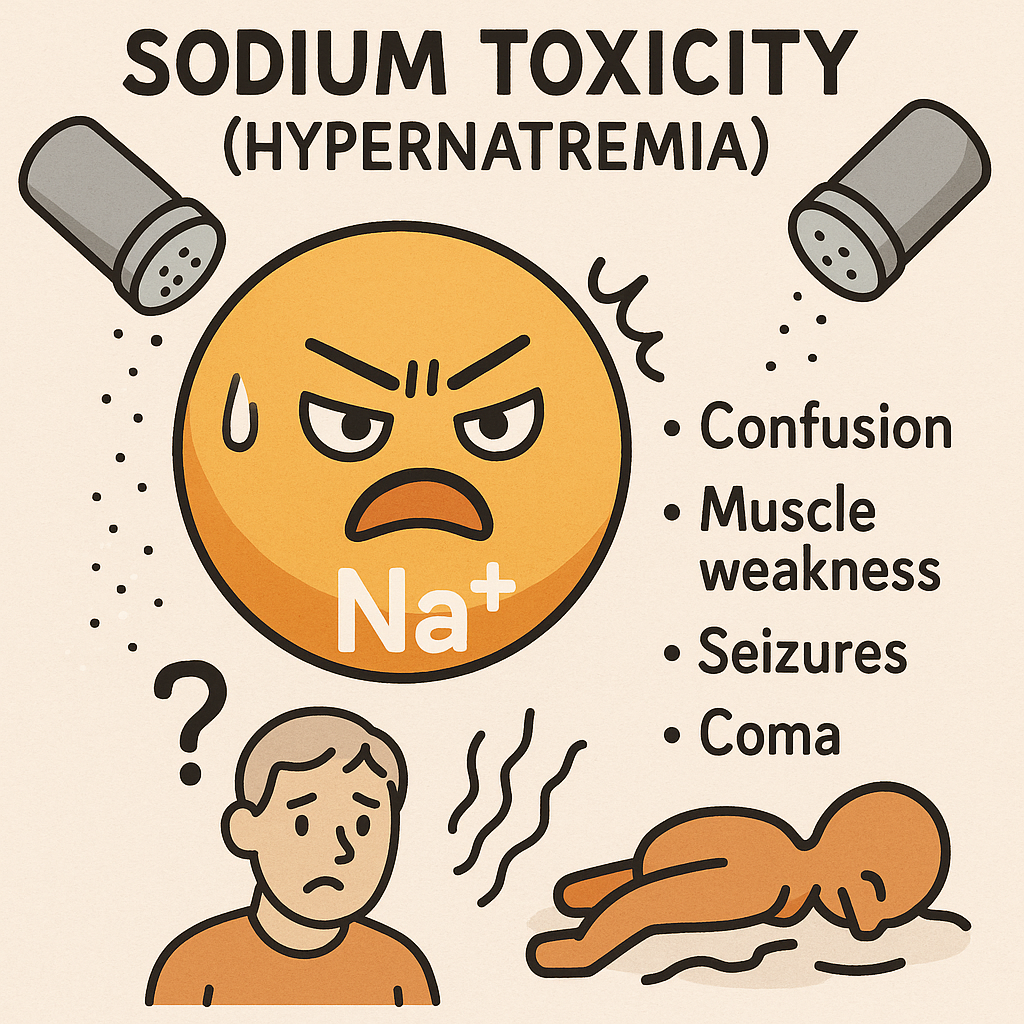
Causes
- Excess dietary sodium intake.
- Dehydration (not drinking enough water).
- Kidney dysfunction (reduced sodium excretion).
- Cushing’s syndrome (excess aldosterone production).
Signs & Symptoms
- Increased thirst (polydipsia).
- High blood pressure (hypertension).
- Swelling (edema) in hands, feet, and face.
- Headaches and confusion.
- Severe cases: Stroke, heart disease, kidney failure.
8. Nursing Implications in Sodium Nutrition
- Patient Assessment:
- Monitor sodium levels (serum sodium levels: 135–145 mEq/L).
- Check for fluid imbalance symptoms (dehydration, edema, blood pressure changes).
- Education:
- Educate patients on limiting processed foods and excessive salt intake.
- Encourage hydration and balanced electrolyte intake.
- Dietary Management:
- Hypertension patients: Low-sodium diet (<1,500 mg/day).
- Dehydrated patients: Oral rehydration therapy (ORS).
- Medication Considerations:
- Monitor sodium balance in patients on diuretics or IV fluids.
- Chronic Disease Management:
- Sodium restriction for hypertension, heart disease, and kidney disease patients.
Summary
- Sodium is a macromineral and an essential electrolyte that plays a role in fluid balance, nerve conduction, and muscle function.
- It is abundant in both natural and processed foods, but excessive intake is linked to hypertension and cardiovascular disease.
- Deficiency (hyponatremia) leads to confusion, muscle cramps, and low blood pressure, while toxicity (hypernatremia) increases the risk of stroke, kidney damage, and high blood pressure.
- Nurses play a key role in monitoring sodium intake, educating patients, and managing sodium-related disorders to maintain overall health.
Potassium:
Potassium is a macromineral and an essential electrolyte that plays a vital role in fluid balance, nerve transmission, muscle contraction, and heart function. It is primarily found inside cells (intracellular fluid) and works with sodium and chloride to regulate body functions.
1. Classification of Potassium
A. Based on Dietary Requirements
- Macromineral (Major Mineral): Required in large amounts (>100 mg/day).
- Essential Electrolyte: The body cannot store excess potassium, so a regular dietary intake is required.
B. Based on Physiological Role
- Intracellular Potassium:
- 98% of body potassium is inside cells, regulating cell function and metabolism.
- Extracellular Potassium:
- 2% of body potassium is found in extracellular fluid (blood plasma), essential for nerve transmission and muscle activity.
C. Based on Dietary Forms
- Potassium Chloride (KCl): Found in food and used in potassium supplements.
- Potassium Citrate: Found in fruits, helps prevent kidney stones.
- Potassium Phosphate: Used in energy metabolism and pH balance.
2. Functions of Potassium
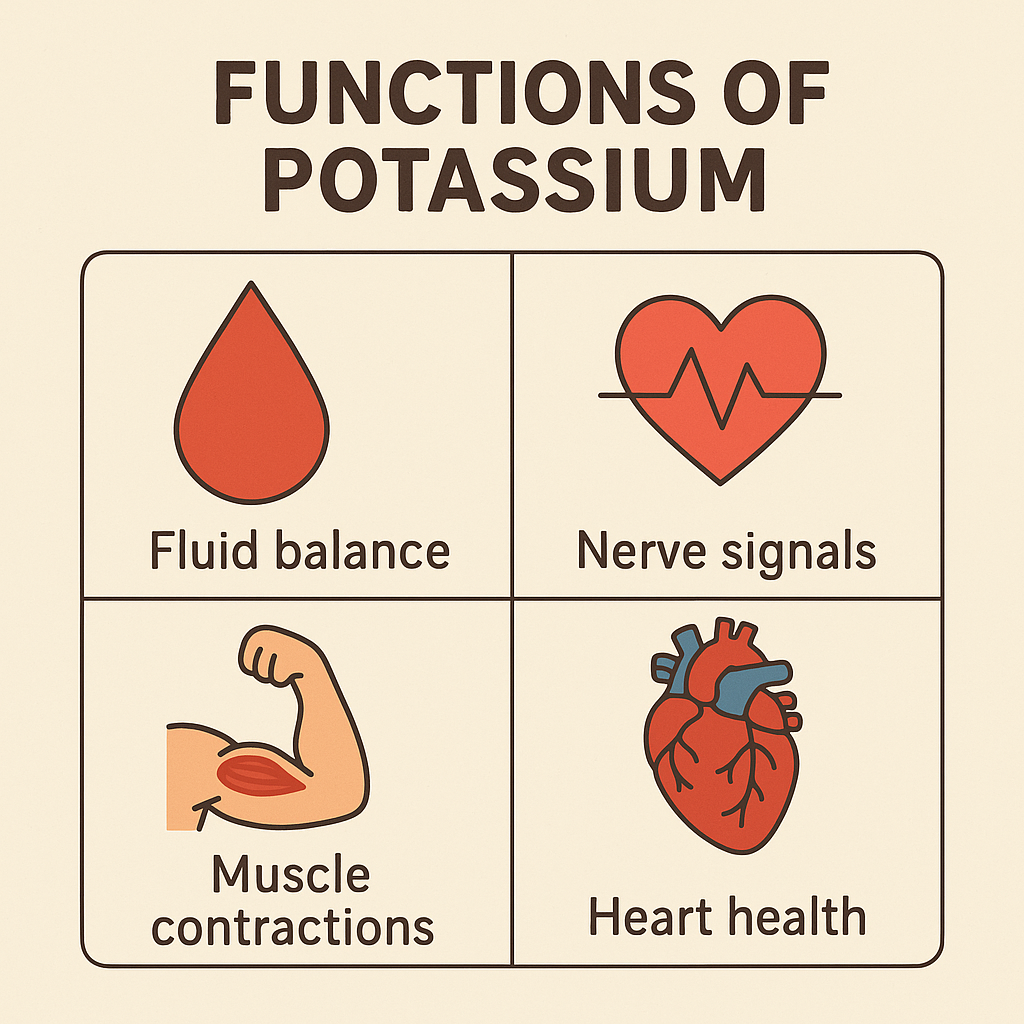
Potassium is involved in multiple biological processes essential for overall health.
A. Structural and Homeostatic Functions
- Maintains Fluid and Electrolyte Balance:
- Regulates intracellular and extracellular osmotic balance.
- Prevents dehydration and fluid retention.
- Acid-Base Balance:
- Helps maintain pH levels (7.35–7.45) in blood.
B. Physiological and Metabolic Functions
- Nerve Impulse Transmission:
- Works with sodium in the sodium-potassium (Na+/K+) pump for proper nerve function.
- Muscle Contraction and Relaxation:
- Essential for skeletal, smooth, and cardiac muscle function.
- Helps prevent muscle cramps and weakness.
- Heart Function and Blood Pressure Regulation:
- Maintains normal heart rhythm and prevents arrhythmias.
- Counteracts the effects of sodium, reducing hypertension.
- Enzyme Activation and Energy Production:
- Required for protein synthesis and glucose metabolism.
- Activates enzymes involved in ATP (energy) production.
- Regulation of Kidney Function:
- Prevents kidney stone formation and flushes excess sodium.
C. Preventive and Therapeutic Functions
- Prevents Stroke and Heart Disease:
- Lowers blood pressure and improves cardiovascular health.
- Protects Bone Health:
- Reduces calcium loss from bones, preventing osteoporosis.
- Enhances Digestive Health:
- Maintains smooth muscle function, preventing constipation and bloating.
3. Dietary Sources of Potassium
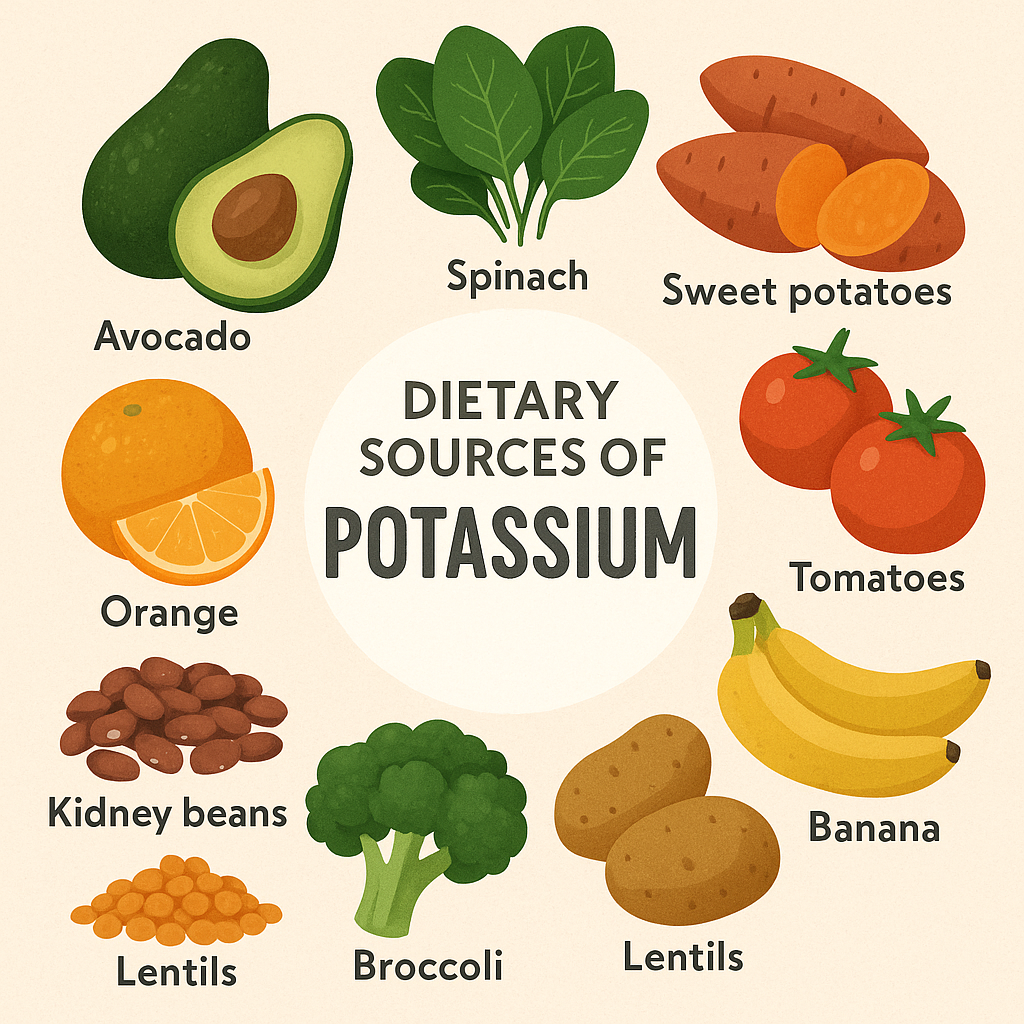
Potassium is widely available in both plant-based and animal-based foods.
A. Rich Natural Sources
- Fruits: Bananas, oranges, kiwis, cantaloupes, apricots, avocados.
- Vegetables: Potatoes (with skin), tomatoes, spinach, mushrooms, sweet potatoes, cucumbers.
- Legumes: Beans, lentils, chickpeas, soybeans.
- Dairy Products: Milk, yogurt, cheese.
- Nuts and Seeds: Almonds, peanuts, sunflower seeds.
- Seafood: Salmon, tuna, clams.
- Whole Grains: Brown rice, quinoa, oats.
B. Processed and Fortified Sources
- Sports drinks and electrolyte solutions (ORS).
- Salt substitutes containing potassium chloride (used for hypertension patients).
4. Recommended Dietary Allowance (RDA) of Potassium
The daily potassium requirement varies based on age, gender, and health conditions.
| Age Group | RDA (mg/day) |
|---|---|
| Infants (0-6 months) | 400 mg |
| Infants (7-12 months) | 700 mg |
| Children (1-3 years) | 3,000 mg |
| Children (4-8 years) | 3,800 mg |
| Adolescents (9-18 years) | 4,500 mg |
| Adults (19+ years) | 4,700 mg |
| Pregnant Women | 4,700 mg |
| Lactating Women | 5,100 mg |
5. Potassium Absorption and Factors Affecting It
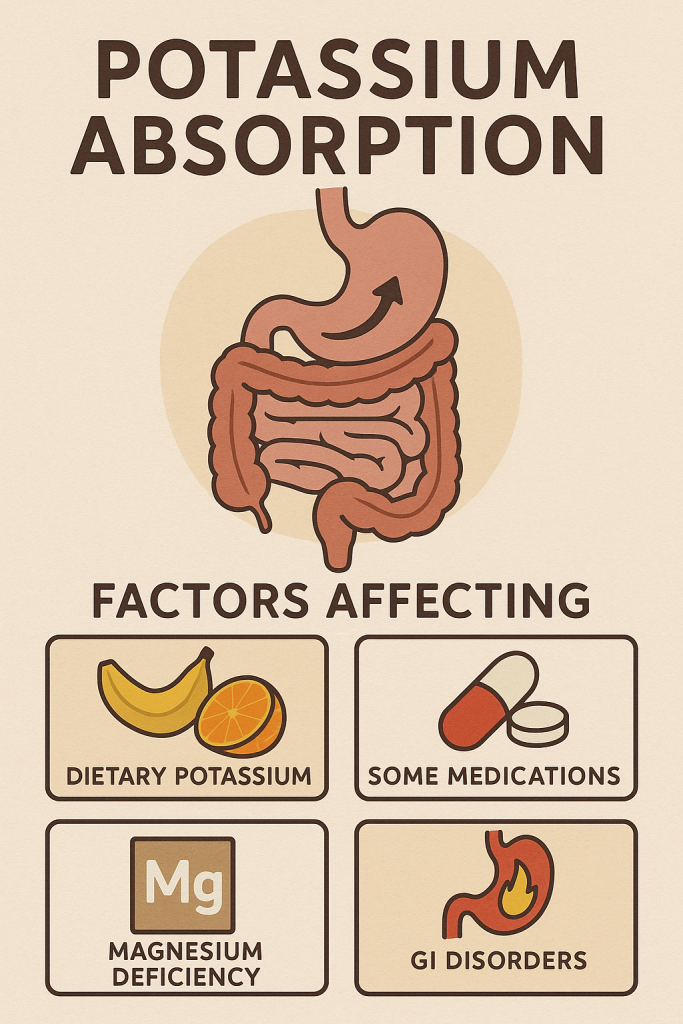
A. Factors Enhancing Potassium Absorption
- Adequate Water Intake:
- Ensures proper potassium distribution in body fluids.
- Normal Kidney Function:
- Regulates potassium balance by excreting excess potassium.
- Insulin:
- Helps in potassium uptake into cells.
B. Factors Inhibiting Potassium Absorption
- Excess Sodium Intake:
- High sodium reduces potassium retention.
- Diuretics (Water Pills):
- Increase potassium loss through urine.
- Chronic Kidney Disease (CKD):
- Leads to potassium accumulation and potential toxicity.
6. Potassium Deficiency (Hypokalemia)
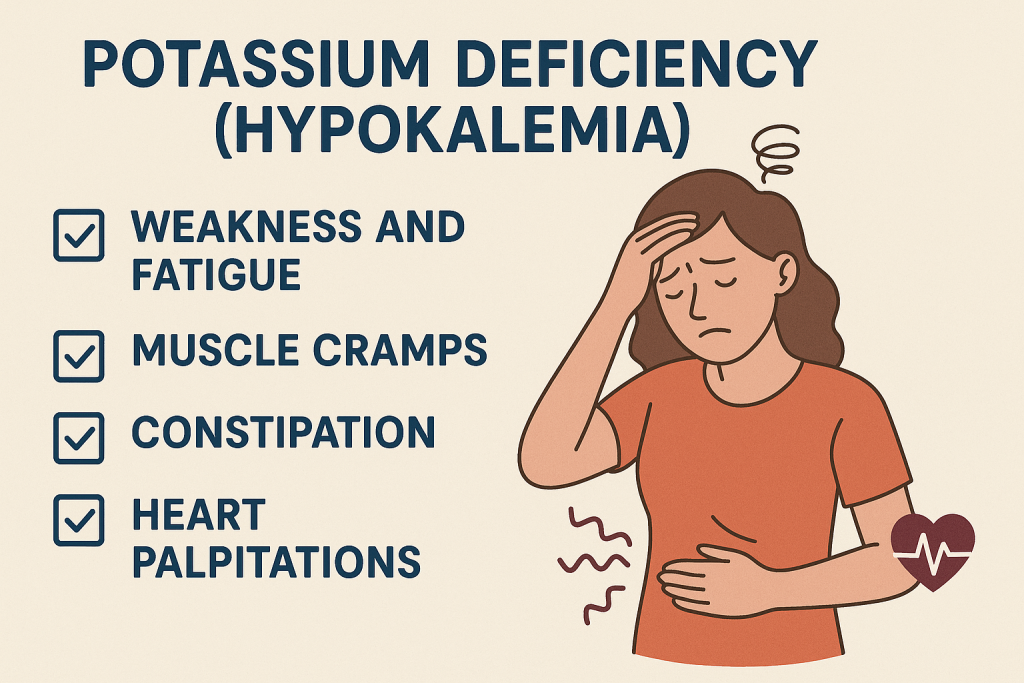
Causes
- Inadequate dietary intake (malnutrition, fasting).
- Excessive sweating, vomiting, diarrhea.
- Diuretic and laxative overuse.
- High sodium intake.
- Kidney disease or hormonal imbalances.
Signs & Symptoms
- Muscle weakness and cramps.
- Irregular heartbeats (arrhythmia).
- Fatigue and drowsiness.
- Numbness or tingling sensations.
- High blood pressure and kidney problems.
- Severe cases: Paralysis, respiratory failure.
7. Potassium Toxicity (Hyperkalemia)
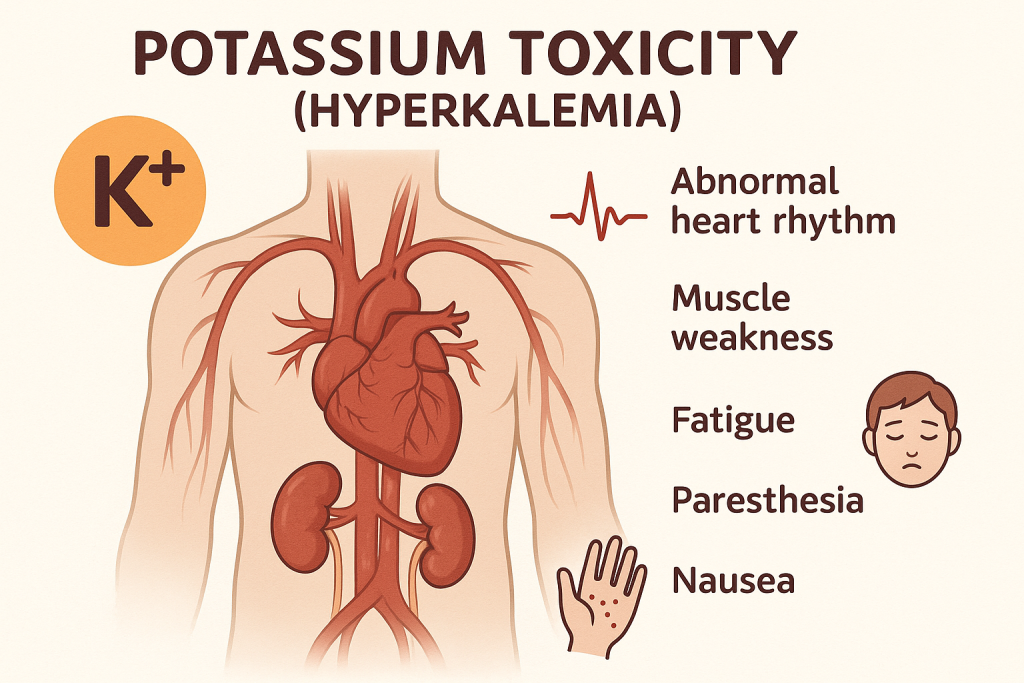
Causes
- Excess potassium intake (supplements, salt substitutes).
- Kidney failure (reduced potassium excretion).
- Severe dehydration.
- Hormonal disorders (Addison’s disease).
Signs & Symptoms
- Irregular heartbeat (bradycardia or tachycardia).
- Nausea, vomiting, and diarrhea.
- Muscle weakness or paralysis.
- Numbness or tingling in extremities.
- Severe cases: Cardiac arrest, death.
8. Nursing Implications in Potassium Nutrition
- Patient Assessment:
- Monitor serum potassium levels (normal range: 3.5–5.0 mEq/L).
- Check for signs of hypokalemia (weakness, arrhythmia) or hyperkalemia (cardiac issues, paralysis).
- Education:
- Teach patients about potassium-rich foods and the importance of hydration.
- Encourage low-sodium, high-potassium diets for hypertension patients.
- Dietary Management:
- Hypokalemia patients: Increase potassium intake through fruits, vegetables, and legumes.
- Hyperkalemia patients: Reduce potassium intake and monitor kidney function.
- Medication Considerations:
- Monitor potassium levels in patients on diuretics, insulin, or kidney medications.
- Administer potassium supplements cautiously in hypokalemia.
- Chronic Disease Management:
- Educate renal patients to limit potassium intake.
- Monitor potassium balance in diabetic patients receiving insulin therapy.
Summary
- Potassium is a macromineral and an essential electrolyte needed for nerve function, muscle contraction, and blood pressure regulation.
- It is abundant in fruits, vegetables, dairy, and seafood, but deficiency (hypokalemia) can lead to muscle weakness, arrhythmias, and paralysis.
- Excess potassium (hyperkalemia) can cause cardiac arrest and kidney damage.
- Nurses play a critical role in monitoring, educating, and managing potassium balance to prevent life-threatening complications.
Magnesium:
Magnesium is a macromineral that plays a crucial role in nerve and muscle function, enzyme activation, bone health, and cardiovascular regulation. It is the fourth most abundant mineral in the human body, with 60% stored in bones and the rest distributed in muscles, soft tissues, and blood.
1. Classification of Magnesium
A. Based on Dietary Requirements
- Macromineral (Major Mineral): Required in large amounts (>100 mg/day).
- Essential Nutrient: The body cannot produce magnesium; it must be obtained from diet or supplements.
B. Based on Physiological Role
- Structural Magnesium:
- Stored in bones (60%), contributing to bone density and strength.
- Metabolic Magnesium:
- Involved in enzyme activation, muscle function, and nerve signaling.
- Circulating Magnesium:
- Found in blood plasma (1%), essential for heart function and blood pressure regulation.
C. Based on Dietary Forms
- Magnesium Oxide: Common supplement form, used for digestion and constipation.
- Magnesium Citrate: Easily absorbed, used for muscle relaxation and heart health.
- Magnesium Sulfate (Epsom Salt): Used in medical treatment for hypomagnesemia and pre-eclampsia.
- Magnesium Chloride: Used in topical applications and supplements.
2. Functions of Magnesium
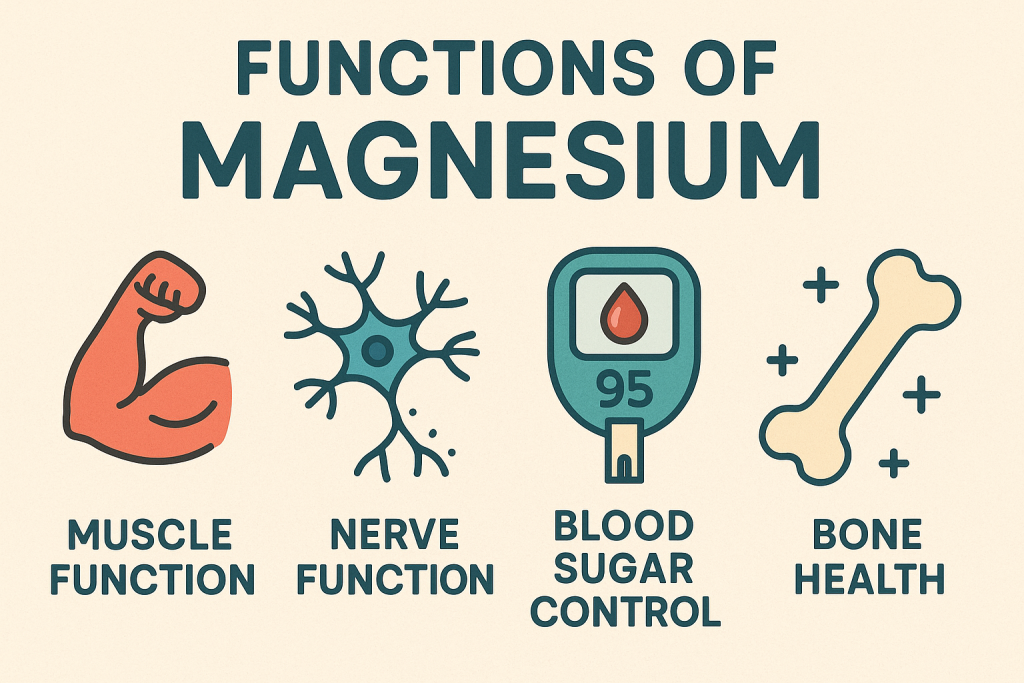
Magnesium is involved in more than 300 enzymatic reactions that regulate biological functions.
A. Structural and Homeostatic Functions
- Bone and Teeth Health:
- Essential for bone mineralization and calcium absorption.
- Works with calcium, phosphorus, and vitamin D for bone strength.
- Protein and DNA Synthesis:
- Required for cell division, growth, and repair.
B. Physiological and Metabolic Functions
- Nerve Impulse Transmission:
- Helps in nerve conduction and muscle coordination.
- Prevents neuromuscular excitability and spasms.
- Muscle Contraction and Relaxation:
- Works with calcium and potassium for normal skeletal, cardiac, and smooth muscle function.
- Prevents cramps, spasms, and muscle fatigue.
- Enzyme Activation and Energy Production:
- Required for ATP (Adenosine Triphosphate) production, the body’s energy molecule.
- Activates enzymes involved in metabolism of carbohydrates, proteins, and fats.
- Blood Pressure and Cardiovascular Health:
- Regulates heart rhythm and blood vessel relaxation.
- Helps prevent hypertension, arrhythmias, and stroke.
- Blood Sugar Control:
- Improves insulin sensitivity and glucose metabolism.
- Helps prevent Type 2 Diabetes.
- Electrolyte Balance:
- Works with sodium, potassium, and calcium to maintain fluid balance.
- Regulation of Mental Health:
- Helps in the production of neurotransmitters like serotonin, reducing anxiety and depression.
C. Preventive and Therapeutic Functions
- Prevents Migraines:
- Reduces migraine frequency and severity.
- Aids Digestion:
- Relieves constipation and indigestion by relaxing bowel muscles.
- Regulates Sleep and Stress:
- Helps in melatonin production, promoting better sleep and relaxation.
3. Dietary Sources of Magnesium
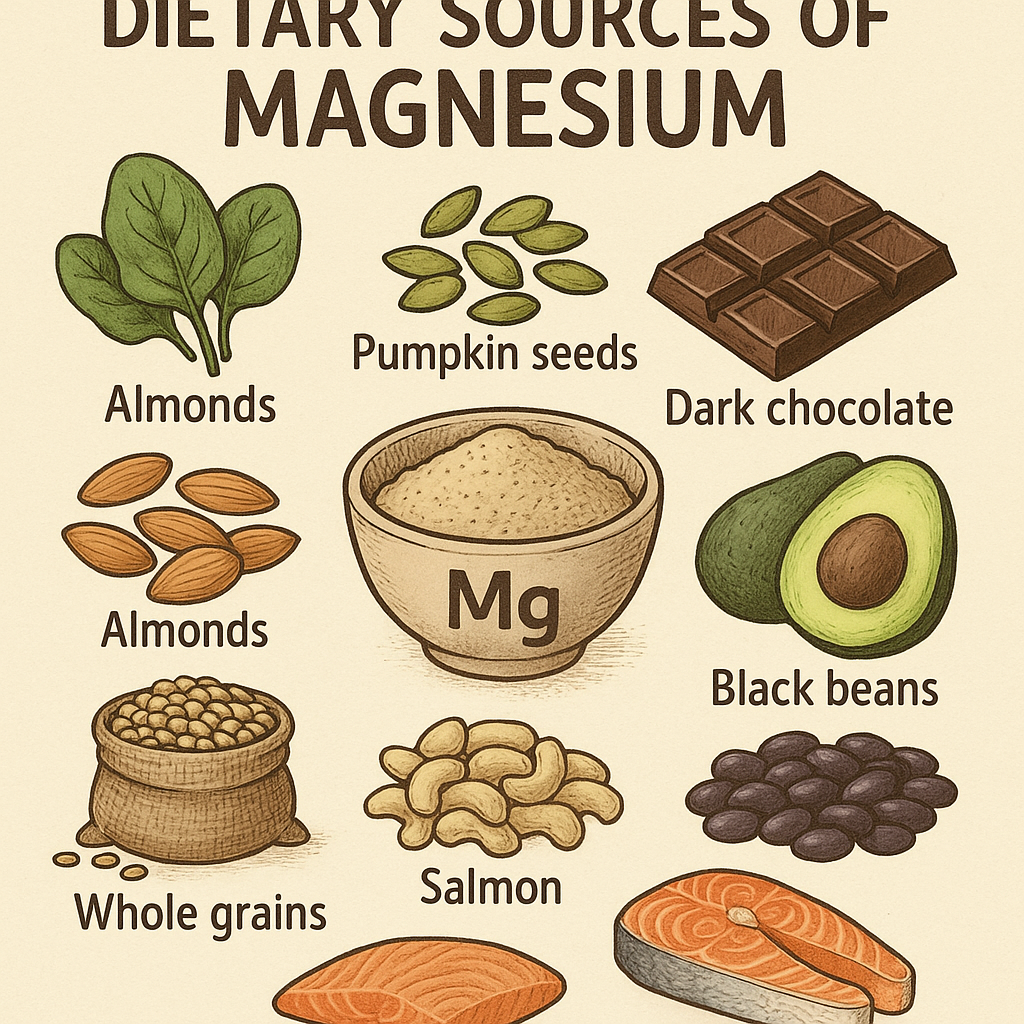
Magnesium is widely available in plant-based and animal-based foods.
A. Rich Natural Sources
- Green Leafy Vegetables: Spinach, kale, Swiss chard.
- Nuts and Seeds: Almonds, cashews, sunflower seeds, pumpkin seeds.
- Whole Grains: Brown rice, oats, quinoa, whole wheat.
- Legumes: Lentils, chickpeas, black beans, soybeans.
- Seafood: Salmon, mackerel, tuna.
- Dairy Products: Yogurt, milk, cheese.
- Fruits: Bananas, avocados, figs.
- Dark Chocolate and Cocoa: Excellent source of magnesium.
B. Fortified and Processed Sources
- Fortified cereals and grains.
- Magnesium supplements (Magnesium Oxide, Citrate, Sulfate).
4. Recommended Dietary Allowance (RDA) of Magnesium
The daily magnesium requirement varies based on age, gender, and physiological needs.
| Age Group | RDA (mg/day) |
|---|---|
| Infants (0-6 months) | 30 mg |
| Infants (7-12 months) | 75 mg |
| Children (1-3 years) | 80 mg |
| Children (4-8 years) | 130 mg |
| Adolescents (9-13 years) | 240 mg |
| Males (14-18 years) | 410 mg |
| Females (14-18 years) | 360 mg |
| Adult Males (19-30 years) | 400 mg |
| Adult Females (19-30 years) | 310 mg |
| Adult Males (31+ years) | 420 mg |
| Adult Females (31+ years) | 320 mg |
| Pregnant Women | 350-400 mg |
| Lactating Women | 310-360 mg |
Upper Limit (UL):
- Safe limit: 350 mg/day from supplements.
- Excess magnesium from food does not cause toxicity as kidneys regulate excretion.
5. Magnesium Absorption and Factors Affecting It
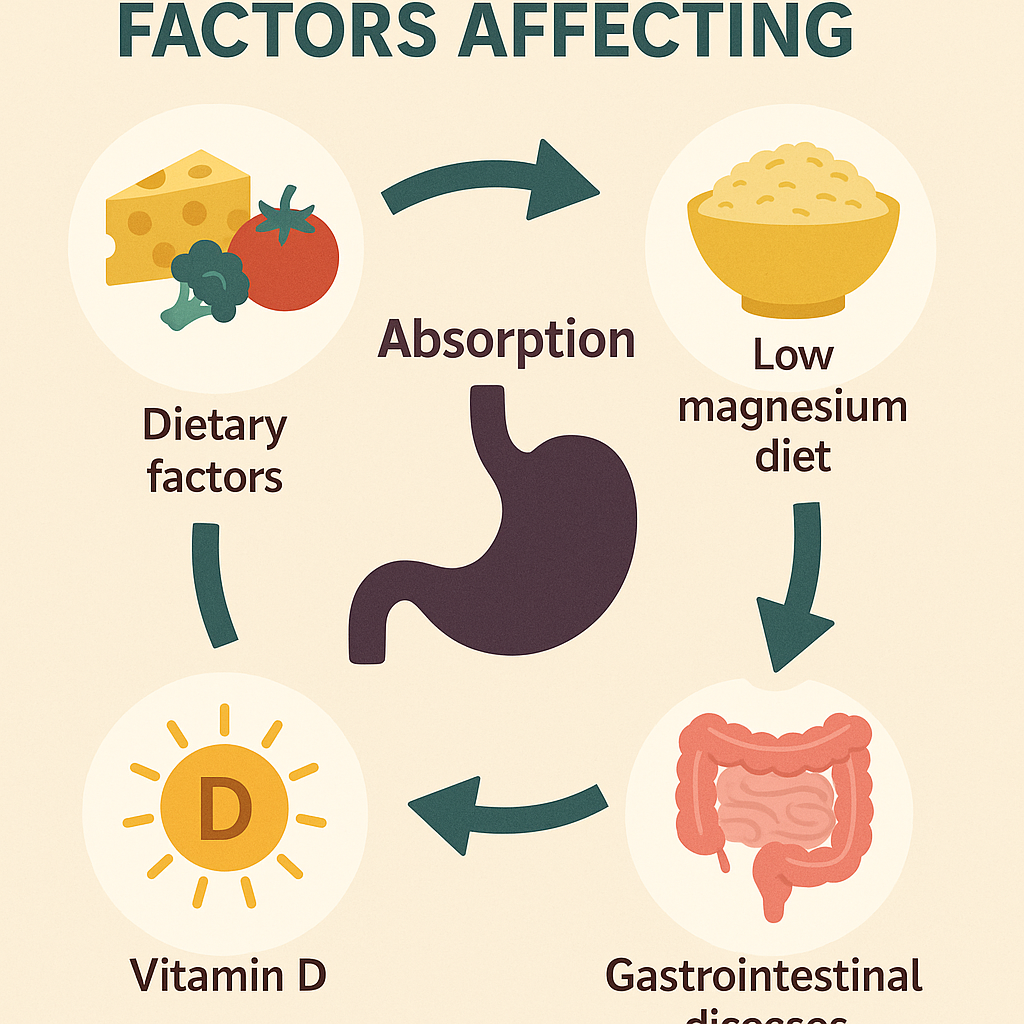
A. Factors Enhancing Magnesium Absorption
- Vitamin D and Calcium: Improve magnesium absorption in intestines.
- Protein Intake: Helps bind magnesium for better absorption.
- Adequate Stomach Acid: Enhances magnesium solubility.
B. Factors Inhibiting Magnesium Absorption
- Excess Alcohol and Caffeine: Increase magnesium excretion.
- Diuretics and Medications: Cause magnesium loss through urine.
- High Fat Intake: Binds magnesium, reducing absorption.
- Certain Health Conditions: Diabetes, kidney disease, and Crohn’s disease impair absorption.
6. Magnesium Deficiency (Hypomagnesemia)
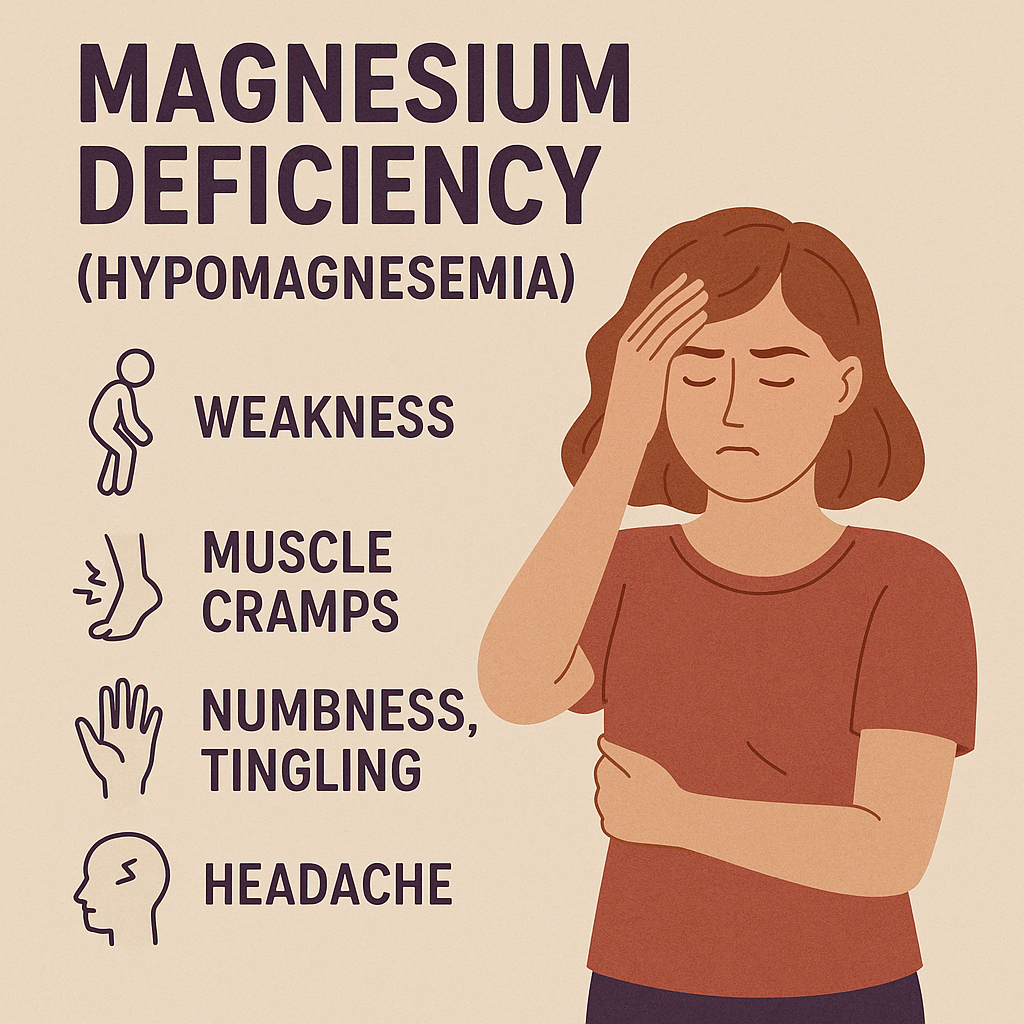
Causes
- Inadequate dietary intake.
- Chronic diarrhea or vomiting.
- Alcoholism.
- Diabetes and kidney disease.
- High intake of processed foods (low in magnesium).
Signs & Symptoms
- Muscle cramps and weakness.
- Tingling or numbness in hands and feet.
- Irregular heartbeat (arrhythmias).
- Fatigue and confusion.
- Seizures in severe cases.
7. Magnesium Toxicity (Hypermagnesemia)
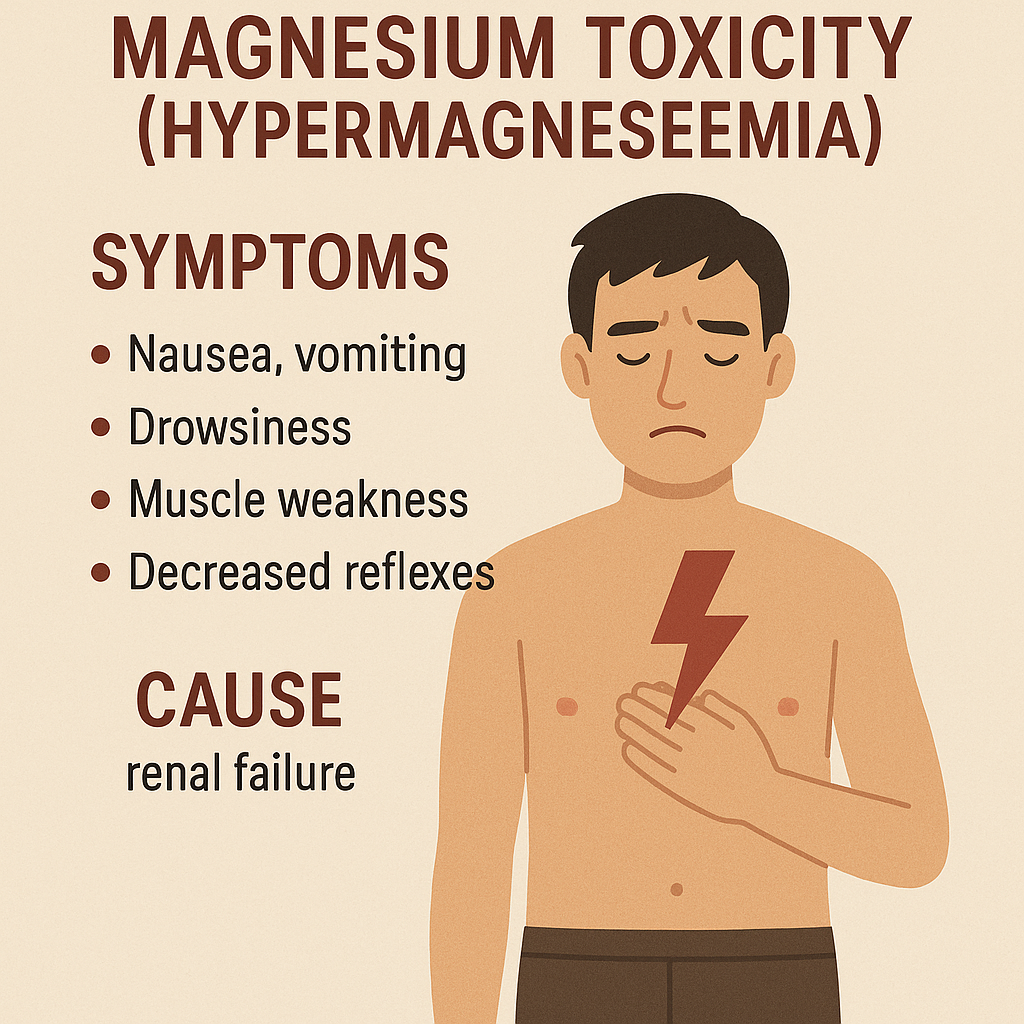
Causes
- Excess magnesium supplements.
- Kidney failure (reduced excretion).
- Overuse of laxatives containing magnesium.
Signs & Symptoms
- Nausea, vomiting, and diarrhea.
- Low blood pressure (hypotension).
- Slow heart rate (bradycardia).
- Muscle weakness and difficulty breathing.
- Severe cases: Coma or cardiac arrest.
8. Nursing Implications in Magnesium Nutrition
- Patient Assessment:
- Monitor serum magnesium levels (normal: 1.7–2.2 mg/dL).
- Check for signs of deficiency (cramps, arrhythmias) or toxicity (low BP, slow heart rate).
- Education:
- Encourage patients to eat magnesium-rich foods.
- Limit alcohol and processed food consumption.
- Dietary and Supplement Management:
- Hypomagnesemia: Magnesium-rich diet or supplements.
- Hypermagnesemia: Monitor kidney function and adjust intake.
Summary
- Magnesium is a macromineral essential for nerve function, muscle contraction, bone health, and enzyme activation.
- Deficiency (hypomagnesemia) leads to muscle weakness, arrhythmias, and seizures.
- Excess magnesium (hypermagnesemia) can cause low blood pressure, slow heart rate, and cardiac arrest.
- Nurses play a crucial role in monitoring, educating, and managing magnesium intake to prevent health complications.
Trace Elements:
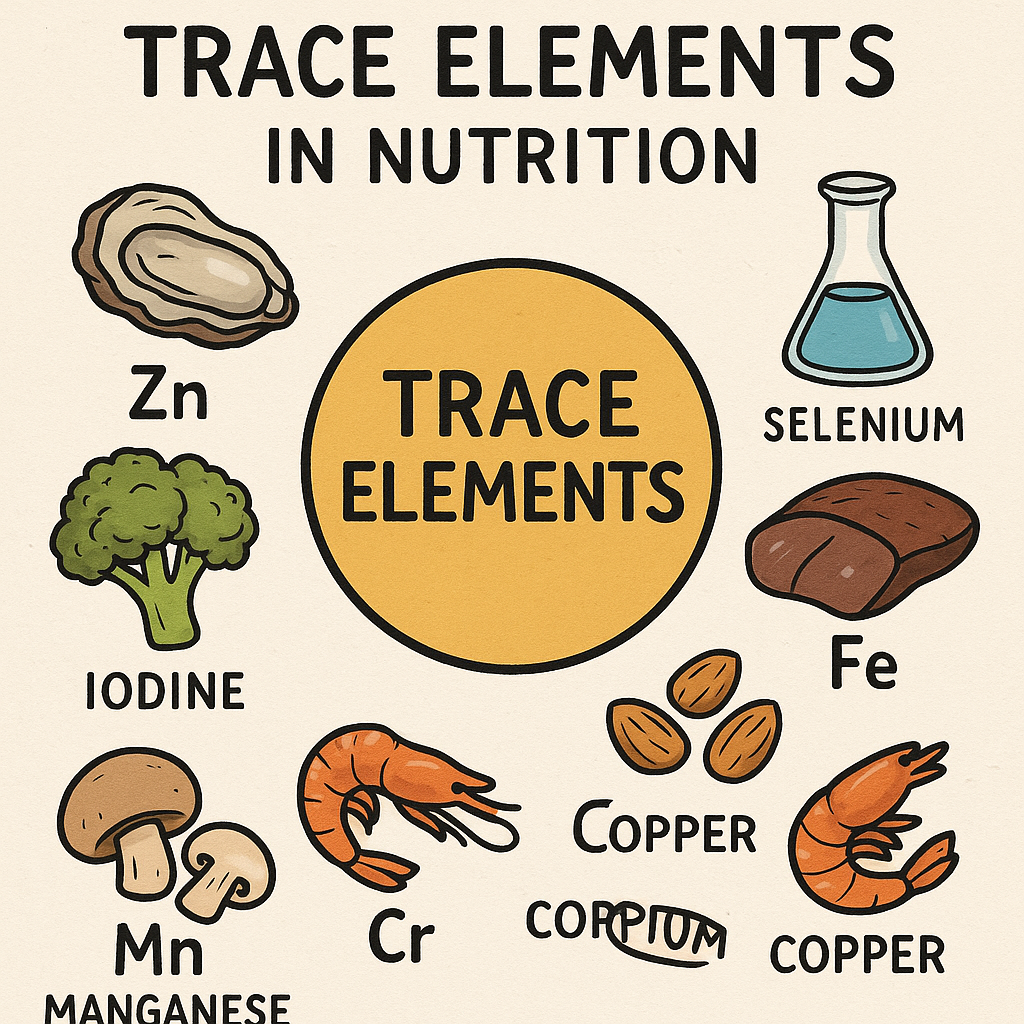
Trace elements (also known as microminerals) are essential minerals required in very small amounts (<100 mg/day) for various physiological and biochemical functions in the human body. Though needed in minute quantities, they play a crucial role in enzyme function, metabolism, immune system regulation, and growth.
1. Classification of Trace Elements
A. Based on Dietary Requirements
- Microminerals (Trace Elements): Required in small amounts (<100 mg/day).
- Essential Nutrients: Must be obtained from diet since the body cannot synthesize them.
B. Based on Physiological Role
- Structural Elements:
- Iron, Zinc, Copper – Essential for blood formation, bones, and cell membranes.
- Enzymatic Cofactors:
- Selenium, Manganese, Chromium – Regulate enzyme activation and metabolic reactions.
- Immune and Antioxidant Elements:
- Zinc, Selenium, Copper – Play a role in immune function and protection against oxidative stress.
C. Based on Dietary Forms
- Organic Forms: Found in animal and plant-based foods.
- Inorganic Forms: Present in supplements and fortified foods.
2. Functions of Trace Elements
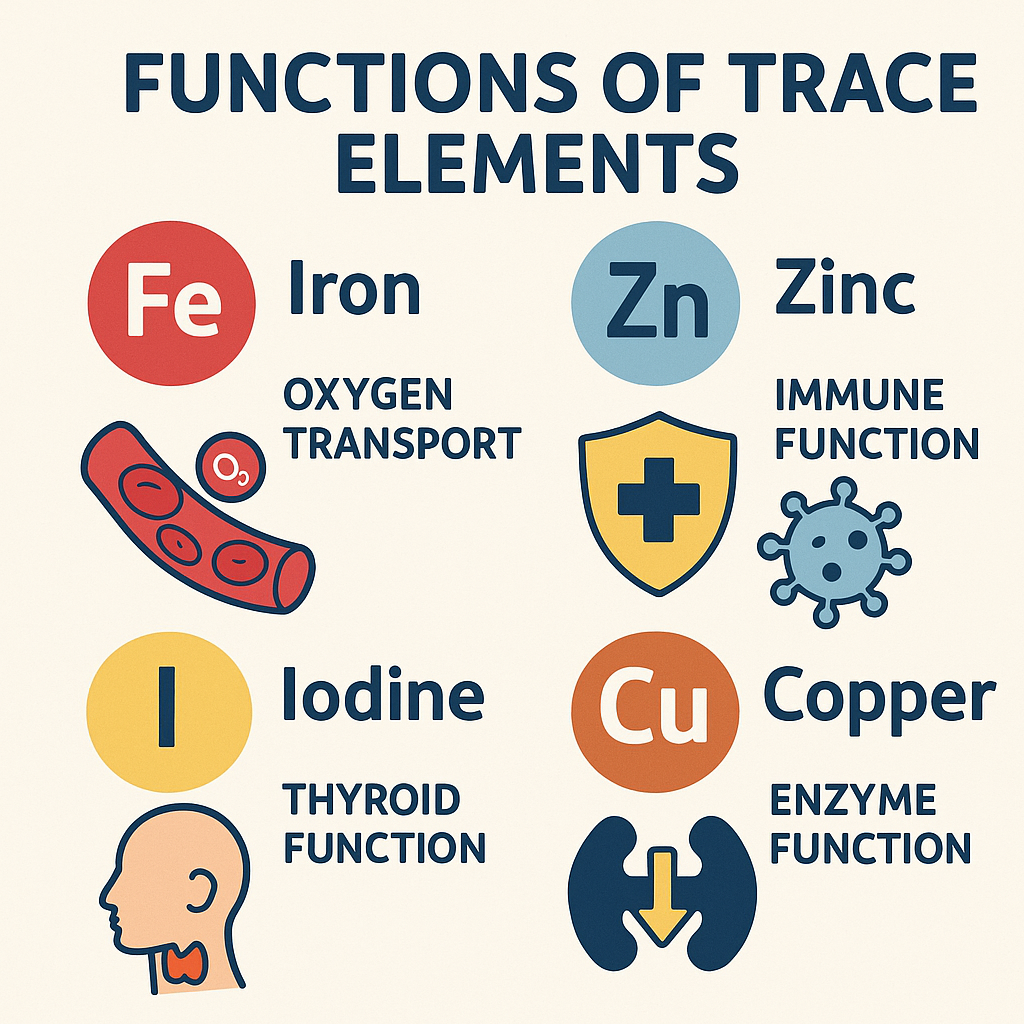
Trace elements perform critical functions that regulate growth, metabolism, and immunity.
| Trace Element | Functions |
|---|---|
| Iron (Fe) | Oxygen transport (Hemoglobin), Enzyme function, Energy production |
| Zinc (Zn) | Wound healing, Growth, Immunity, Enzyme activation |
| Copper (Cu) | Red blood cell formation, Iron metabolism, Connective tissue strength |
| Iodine (I) | Thyroid hormone production (T3, T4), Metabolism regulation |
| Selenium (Se) | Antioxidant function, Thyroid metabolism, Immune function |
| Manganese (Mn) | Bone formation, Metabolism, Antioxidant activity |
| Chromium (Cr) | Insulin function, Blood sugar control, Carbohydrate metabolism |
| Molybdenum (Mo) | Enzyme activation, Detoxification, DNA repair |
| Fluoride (F) | Tooth enamel protection, Bone mineralization |
3. Dietary Sources of Trace Elements
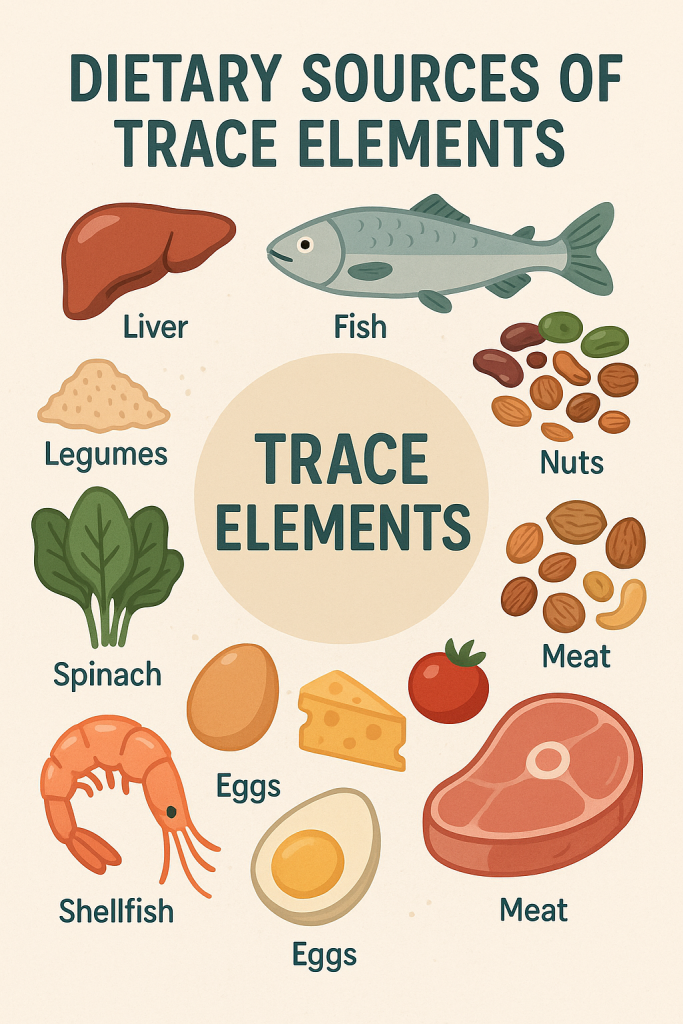
A. Animal Sources
- Iron: Red meat, poultry, fish, eggs, liver
- Zinc: Seafood (oysters, crab), beef, dairy
- Copper: Shellfish, liver, nuts
- Iodine: Fish, seaweed, dairy
- Selenium: Seafood, eggs, chicken
- Manganese: Shellfish, nuts
- Chromium: Meat, eggs
- Molybdenum: Dairy, eggs
- Fluoride: Fish, fluoridated water
B. Plant-Based Sources
- Iron: Leafy vegetables, legumes, whole grains
- Zinc: Nuts, seeds, beans
- Copper: Whole grains, mushrooms
- Iodine: Seaweed, iodized salt
- Selenium: Brazil nuts, whole grains
- Manganese: Nuts, tea, grains
- Chromium: Broccoli, whole grains
- Molybdenum: Legumes, cereals
- Fluoride: Tea, fluoridated water
4. Recommended Dietary Allowance (RDA) of Trace Elements
| Trace Element | RDA (mg/day) (Adults) |
|---|---|
| Iron | Males: 8 mg, Females: 18 mg |
| Zinc | Males: 11 mg, Females: 8 mg |
| Copper | 0.9 mg |
| Iodine | 150 µg |
| Selenium | 55 µg |
| Manganese | Males: 2.3 mg, Females: 1.8 mg |
| Chromium | Males: 35 µg, Females: 25 µg |
| Molybdenum | 45 µg |
| Fluoride | 3-4 mg |
5. Absorption and Factors Affecting Trace Element Bioavailability
A. Factors Enhancing Absorption
- Vitamin C: Enhances iron absorption.
- Animal Protein: Improves zinc and iron bioavailability.
- Stomach Acid: Helps in better absorption of iron, zinc, and calcium.
B. Factors Inhibiting Absorption
- Phytates (Whole Grains, Legumes): Reduce iron and zinc absorption.
- Oxalates (Spinach, Tea): Reduce calcium and iron absorption.
- Excess Calcium Intake: Interferes with zinc and magnesium absorption.
- High Fiber Diets: Can bind to minerals, reducing absorption.
6. Deficiency Disorders of Trace Elements
| Trace Element | Deficiency Disorder | Symptoms |
|---|---|---|
| Iron | Iron Deficiency Anemia | Fatigue, Pale skin, Weakness |
| Zinc | Growth Retardation | Delayed wound healing, Hair loss |
| Copper | Anemia, Bone disorders | Fatigue, Weak bones |
| Iodine | Goiter, Hypothyroidism | Swollen neck, Weight gain |
| Selenium | Keshan Disease | Weak immune system, Heart disease |
| Manganese | Bone Deformities | Poor growth, Joint pain |
| Chromium | Impaired Glucose Tolerance | Insulin resistance |
| Molybdenum | Rare | Seizures, Brain dysfunction |
| Fluoride | Dental Caries | Weak tooth enamel, Cavities |
7. Toxicity of Trace Elements
| Trace Element | Toxicity Symptoms |
|---|---|
| Iron | Liver damage, Diabetes risk |
| Zinc | Nausea, Immune suppression |
| Copper | Nerve damage, Vomiting |
| Iodine | Thyroid dysfunction, Goiter |
| Selenium | Hair loss, Nerve damage |
| Manganese | Neurological issues |
| Chromium | Kidney damage (rare) |
| Molybdenum | Gout-like symptoms |
| Fluoride | Fluorosis (tooth discoloration) |
8. Nursing Implications in Trace Element Nutrition
- Patient Assessment:
- Monitor serum levels of iron, zinc, and iodine.
- Assess for deficiency symptoms (anemia, goiter, slow wound healing).
- Education:
- Encourage balanced diets with trace element-rich foods.
- Advise pregnant women on iodine and iron intake.
- Dietary and Supplementation Management:
- Iron Deficiency: Recommend iron-rich foods and supplements.
- Goiter Prevention: Use iodized salt in cooking.
- Selenium Deficiency: Encourage consumption of Brazil nuts, seafood.
- Medication Considerations:
- Monitor patients on iron supplements for side effects (constipation, nausea).
- Avoid excess fluoride consumption to prevent fluorosis.
Summary
- Trace elements (microminerals) are essential nutrients required in small amounts (<100 mg/day).
- They are critical for enzyme function, immunity, growth, and metabolism.
- Deficiency can lead to anemia (iron), goiter (iodine), weak immunity (zinc), and bone deformities (manganese).
- Excess intake (toxicity) can cause organ damage, neurological issues, and metabolic disorders.
- Nurses play a crucial role in monitoring, educating, and managing trace element intake to prevent deficiencies and ensure optimal health.