BSC SEM 1 UNIT 6 APPLIED BIOCHEMISTRY
UNIT 6 Heme catabolism
Heme Catabolism:
Heme catabolism is the biochemical process through which heme is broken down into its degradation products, primarily bilirubin, carbon monoxide (CO), and iron (Fe²⁺). This process occurs predominantly in the reticuloendothelial system (RES), including the liver, spleen, and bone marrow. The breakdown of heme is essential for maintaining iron homeostasis and preventing oxidative damage caused by free heme.
1. Sources of Heme
Heme is derived from:
- Aged and damaged red blood cells (RBCs) (~80%)
- Other heme-containing proteins, such as myoglobin, cytochromes, catalases, and peroxidases (~20%)
2. Steps of Heme Catabolism
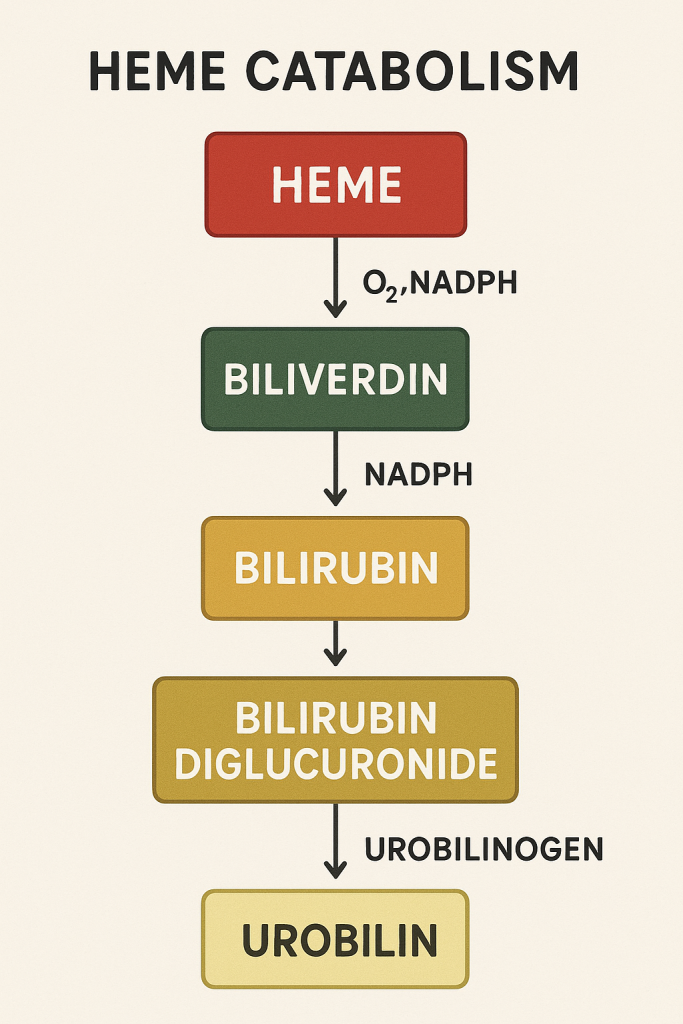
Heme breakdown occurs in several enzymatic steps:
Step 1: Conversion of Heme to Biliverdin
Enzyme: Heme Oxygenase (HO)
- Reaction: Heme + O₂ + NADPH + H⁺ → Biliverdin + Fe²⁺ + CO + NADP⁺
- Location: Macrophages in the spleen and liver
- Significance:
- Opens the porphyrin ring of heme
- Releases iron (Fe²⁺), which is stored as ferritin or transported via transferrin
- Generates carbon monoxide (CO), which acts as a vasodilator and signaling molecule
- Converts heme into biliverdin, a green pigment
Step 2: Conversion of Biliverdin to Bilirubin
Enzyme: Biliverdin Reductase
- Reaction: Biliverdin + NADPH + H⁺ → Bilirubin + NADP⁺
- Significance:
- Converts biliverdin (green) to bilirubin (yellow-orange), which is more lipophilic and less soluble in water
- Bilirubin is an antioxidant that neutralizes free radicals
Step 3: Transport of Bilirubin in Blood
- Unconjugated bilirubin (Indirect bilirubin) is hydrophobic and binds to albumin for transport to the liver.
- Clinical Significance: Unconjugated bilirubin is toxic and can cross the blood-brain barrier, leading to kernicterus in neonates if not properly metabolized.
Step 4: Conjugation in the Liver
Enzyme: UDP-Glucuronosyltransferase (UGT1A1)
- Reaction: Bilirubin + 2 UDP-glucuronic acid → Bilirubin diglucuronide + 2 UDP
- Location: Liver (Hepatocytes)
- Significance:
- Converts lipophilic unconjugated bilirubin into water-soluble conjugated bilirubin (direct bilirubin), which can be excreted into bile.
Step 5: Excretion via Bile
- Conjugated bilirubin is secreted into the bile canaliculi and transported to the small intestine via the common bile duct.
Step 6: Intestinal Metabolism and Fecal Excretion
- In the intestine, bacterial enzymes convert bilirubin into urobilinogen.
- Some urobilinogen is:
- Reabsorbed into blood and excreted by the kidney as urobilin (yellow color of urine)
- Converted into stercobilin and excreted in feces (brown color)
3. Regulation of Heme Catabolism
- Heme oxygenase (HO) is the rate-limiting enzyme.
- Induced by:
- Increased heme levels
- Oxidative stress
- Inflammation
- Inhibited by:
- Low heme levels
- Presence of metalloporphyrins
4. Clinical Correlations
A. Hyperbilirubinemia and Jaundice
- Pre-hepatic (Hemolytic) Jaundice:
- Excessive RBC breakdown → Increased unconjugated bilirubin
- Causes: Hemolytic anemia, sickle cell disease, hereditary spherocytosis
- Hepatic Jaundice:
- Impaired liver function → Reduced bilirubin conjugation
- Causes: Hepatitis, cirrhosis, Gilbert’s syndrome (UGT1A1 deficiency)
- Post-hepatic (Obstructive) Jaundice:
- Blocked bile flow → Accumulation of conjugated bilirubin
- Causes: Gallstones, tumors, biliary atresia
B. Neonatal Jaundice
- Cause: Immature UDP-glucuronosyltransferase (UGT1A1) → Delayed bilirubin conjugation
- Treatment: Phototherapy (converts bilirubin into a more soluble form)
C. Heme Oxygenase Deficiency and Heme Toxicity
- Deficiency of HO leads to oxidative damage.
- Excess free heme causes oxidative stress, leading to inflammation and vascular damage.
5. Summary of Key Enzymes and Products
| Step | Enzyme | Reactant | Product | Location |
|---|---|---|---|---|
| 1 | Heme Oxygenase | Heme | Biliverdin + Fe²⁺ + CO | Macrophages |
| 2 | Biliverdin Reductase | Biliverdin | Bilirubin | Macrophages |
| 3 | Albumin (Transport) | Unconjugated Bilirubin | Albumin-bound Bilirubin | Blood |
| 4 | UDP-Glucuronosyltransferase (UGT1A1) | Bilirubin | Conjugated Bilirubin | Liver |
| 5 | Gut Bacteria | Conjugated Bilirubin | Urobilinogen | Intestine |
| 6 | Gut Bacteria | Urobilinogen | Stercobilin (Feces) | Colon |
6. Clinical Tests for Bilirubin
- Total Bilirubin Test
- Direct Bilirubin (Conjugated)
- Indirect Bilirubin (Unconjugated)
- Urine Urobilinogen Test
- Van den Bergh Reaction (Direct vs. Indirect Bilirubin Test)
7. Clinical Interventions
- Phototherapy: Used for neonatal jaundice
- Phenobarbital: Induces UDP-glucuronosyltransferase
- Exchange Transfusion: For severe hyperbilirubinemia
- Liver Transplant: In severe liver failure
Heme Degradation Pathway:
Introduction
The heme degradation pathway is a crucial metabolic process that involves the breakdown of heme from hemoglobin, myoglobin, and other heme-containing proteins. This pathway ensures the safe removal of toxic heme while recycling iron and generating biologically significant molecules like bilirubin, carbon monoxide (CO), and iron (Fe²⁺).
The degradation occurs mainly in the reticuloendothelial system (RES), particularly in macrophages of the spleen, liver, and bone marrow.
1. Sources of Heme
Heme is primarily derived from:
- Aged and damaged red blood cells (RBCs) (~80%)
- Other heme-containing proteins (~20%), such as:
- Myoglobin
- Cytochromes (e.g., cytochrome P450)
- Catalase
- Peroxidase
Each day, approximately 6 g of hemoglobin is degraded, producing 250-300 mg of bilirubin.
2. Steps of Heme Degradation
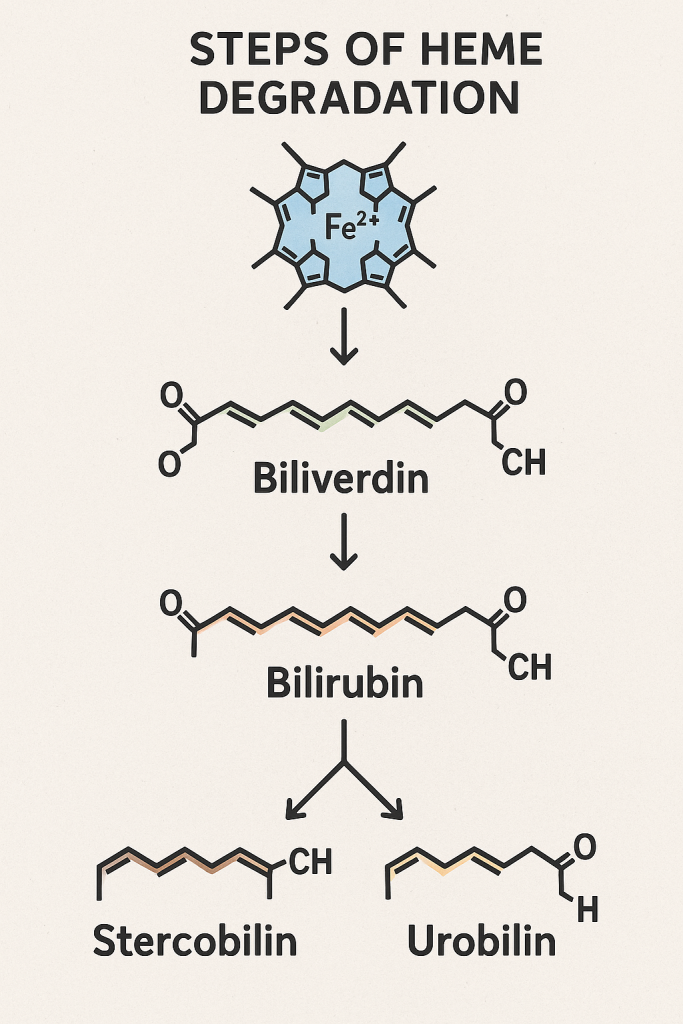
The heme degradation pathway involves multiple enzymatic reactions:
Step 1: Heme Breakdown to Biliverdin
Enzyme: Heme Oxygenase (HO)
- Reaction: Heme+O2+NADPH+H+→Biliverdin+Fe2++CO+NADP+\text{Heme} + O₂ + NADPH + H⁺ → \text{Biliverdin} + Fe²⁺ + CO + NADP⁺Heme+O2+NADPH+H+→Biliverdin+Fe2++CO+NADP+
- Location: Macrophages of the spleen, liver, and bone marrow.
- Mechanism:
- Ring cleavage: Heme oxygenase opens the tetrapyrrole ring of heme.
- Release of iron (Fe²⁺): Stored in macrophages as ferritin or transported via transferrin.
- Formation of carbon monoxide (CO): Acts as a vasodilator and signaling molecule.
- Conversion of heme into biliverdin: A green pigment with antioxidant properties.
Step 2: Reduction of Biliverdin to Bilirubin
Enzyme: Biliverdin Reductase
- Reaction: Biliverdin+NADPH+H+→Bilirubin+NADP+\text{Biliverdin} + NADPH + H⁺ → \text{Bilirubin} + NADP⁺Biliverdin+NADPH+H+→Bilirubin+NADP+
- Significance:
- Bilirubin is yellow-orange and more hydrophobic than biliverdin.
- Acts as an antioxidant, protecting cells from oxidative stress.
Step 3: Transport of Unconjugated Bilirubin
- Unconjugated bilirubin (Indirect Bilirubin) is highly lipophilic (water-insoluble).
- It binds to albumin in plasma for transport to the liver.
- Clinical Relevance:
- Unbound bilirubin is toxic and can cross the blood-brain barrier, leading to kernicterus in neonates.
Step 4: Hepatic Conjugation of Bilirubin
Enzyme: UDP-Glucuronosyltransferase (UGT1A1)
- Reaction: Bilirubin+2UDP-glucuronic acid→Bilirubin diglucuronide+2UDP\text{Bilirubin} + 2 \text{UDP-glucuronic acid} → \text{Bilirubin diglucuronide} + 2 UDPBilirubin+2UDP-glucuronic acid→Bilirubin diglucuronide+2UDP
- Location: Liver (Hepatocytes)
- Significance:
- Converts lipophilic unconjugated bilirubin into water-soluble conjugated bilirubin (direct bilirubin).
- Conjugation prepares bilirubin for excretion via bile.
Step 5: Biliary Excretion of Conjugated Bilirubin
- Conjugated bilirubin is secreted into bile canaliculi and transported via the common bile duct into the duodenum.
- This process is ATP-dependent.
Step 6: Intestinal Conversion of Bilirubin
In the intestine, conjugated bilirubin is metabolized by gut bacteria into urobilinogen: Bilirubin→Urobilinogen\text{Bilirubin} → \text{Urobilinogen}Bilirubin→Urobilinogen
- Fate of Urobilinogen:
- Reabsorbed into blood and transported to the kidney, where it is oxidized to urobilin (gives urine its yellow color).
- Converted into stercobilin in the colon, which is excreted in feces (gives feces its brown color).
3. Regulation of Heme Degradation
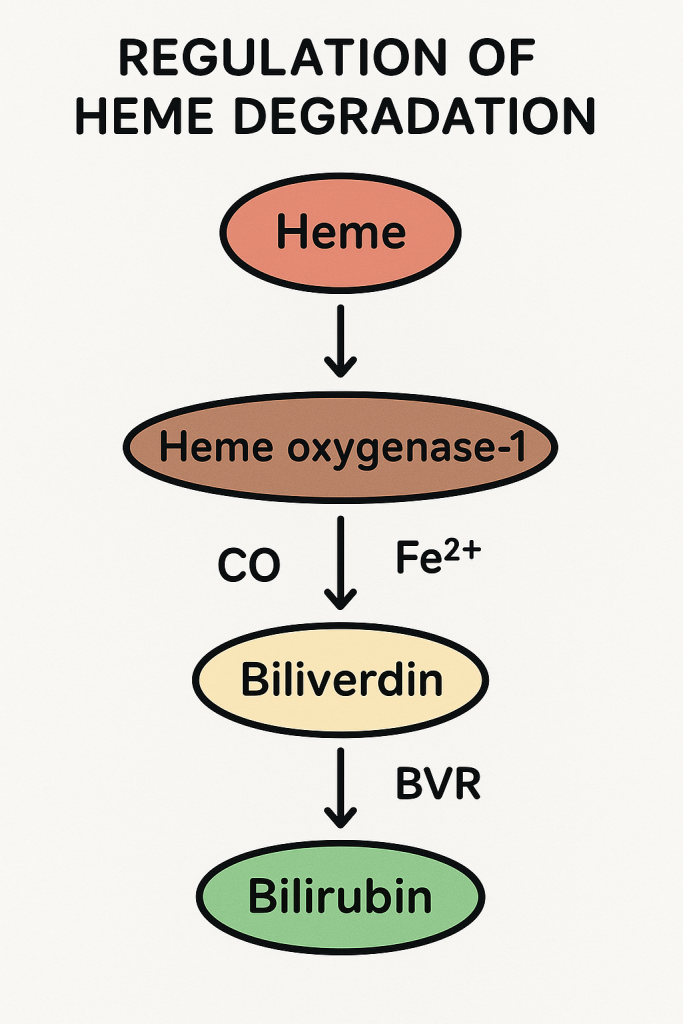
- Heme Oxygenase (HO) is the rate-limiting enzyme.
- Inducers of HO:
- Increased heme levels
- Oxidative stress
- Inflammation
- Inhibitors of HO:
- Low heme levels
- Presence of metalloporphyrins
4. Clinical Correlations
A. Hyperbilirubinemia and Jaundice
- Pre-hepatic (Hemolytic) Jaundice:
- Excessive RBC breakdown → Increased unconjugated bilirubin.
- Causes: Hemolytic anemia, sickle cell disease, hereditary spherocytosis.
- Hepatic Jaundice:
- Impaired liver function → Reduced bilirubin conjugation.
- Causes: Hepatitis, cirrhosis, Gilbert’s syndrome (UGT1A1 deficiency).
- Post-hepatic (Obstructive) Jaundice:
- Blocked bile flow → Accumulation of conjugated bilirubin.
- Causes: Gallstones, tumors, biliary atresia.
B. Neonatal Jaundice
- Cause: Immature UDP-glucuronosyltransferase (UGT1A1) → Delayed bilirubin conjugation.
- Treatment: Phototherapy (converts bilirubin into a more soluble form).
C. Heme Oxygenase Deficiency and Heme Toxicity
- Deficiency of HO leads to oxidative damage.
- Excess free heme causes oxidative stress, leading to inflammation and vascular damage.
5. Summary of Key Enzymes and Products
| Step | Enzyme | Reactant | Product | Location |
|---|---|---|---|---|
| 1 | Heme Oxygenase | Heme | Biliverdin + Fe²⁺ + CO | Macrophages |
| 2 | Biliverdin Reductase | Biliverdin | Bilirubin | Macrophages |
| 3 | Albumin (Transport) | Unconjugated Bilirubin | Albumin-bound Bilirubin | Blood |
| 4 | UDP-Glucuronosyltransferase (UGT1A1) | Bilirubin | Conjugated Bilirubin | Liver |
| 5 | Gut Bacteria | Conjugated Bilirubin | Urobilinogen | Intestine |
| 6 | Gut Bacteria | Urobilinogen | Stercobilin (Feces) | Colon |
6. Clinical Tests for Bilirubin
- Total Bilirubin Test
- Direct Bilirubin (Conjugated)
- Indirect Bilirubin (Unconjugated)
- Urine Urobilinogen Test
- Van den Bergh Reaction (Direct vs. Indirect Bilirubin Test)
7. Clinical Interventions
- Phototherapy: Used for neonatal jaundice.
- Phenobarbital: Induces UDP-glucuronosyltransferase.
- Exchange Transfusion: For severe hyperbilirubinemia.
- Liver Transplant: In severe liver failure.
Jaundice: Types, Causes, Urine & Blood Investigations
Introduction
Jaundice (Icterus) is a yellow discoloration of the skin, sclera, and mucous membranes due to elevated bilirubin levels in the blood. It is a result of an imbalance in bilirubin production, metabolism, and excretion.
Normal serum bilirubin levels:
- Total bilirubin: 0.3 – 1.2 mg/dL
- Direct (conjugated) bilirubin: 0 – 0.3 mg/dL
- Indirect (unconjugated) bilirubin: 0.2 – 0.8 mg/dL
When total bilirubin >2.5 mg/dL, jaundice becomes clinically visible.
1. Types of Jaundice and Causes
Jaundice is classified based on the stage of bilirubin metabolism affected:
| Type | Pathophysiology | Causes | Bilirubin Type |
|---|---|---|---|
| Pre-hepatic (Hemolytic) Jaundice | Increased breakdown of RBCs → Excess unconjugated bilirubin | – Hemolytic anemia (sickle cell, G6PD deficiency) – Malaria – Hereditary spherocytosis – Blood transfusion reactions | Unconjugated (Indirect) ↑↑ |
| Hepatic (Hepatocellular) Jaundice | Liver unable to conjugate bilirubin due to hepatocyte dysfunction | – Hepatitis (viral, alcoholic, autoimmune) – Cirrhosis – Liver failure – Gilbert’s Syndrome (UGT1A1 deficiency) | Mixed (Unconjugated ↑, Conjugated ↑) |
| Post-hepatic (Obstructive) Jaundice | Obstruction in bile flow → Reduced bilirubin excretion | – Gallstones – Biliary atresia – Pancreatic cancer – Cholestasis | Conjugated (Direct) ↑↑ |
2. Causes of Jaundice
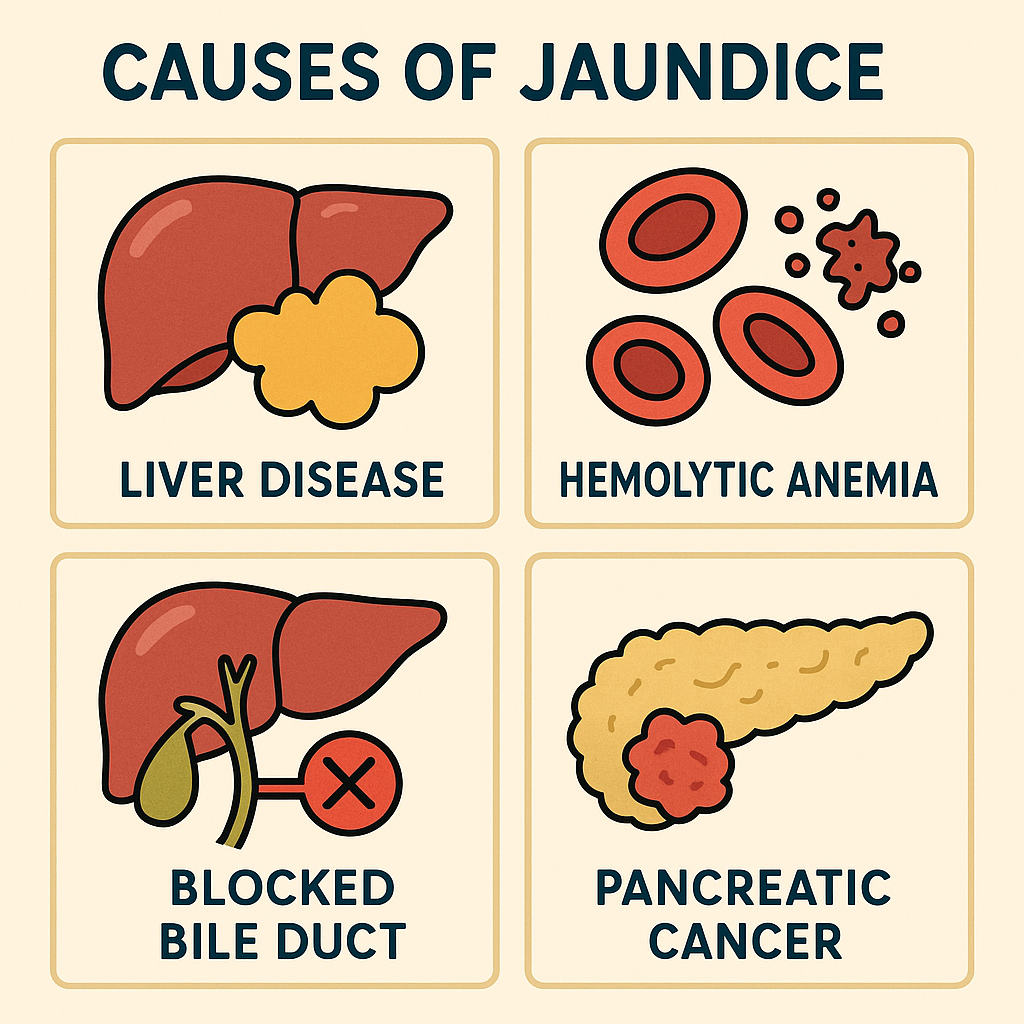
A. Pre-hepatic (Hemolytic) Jaundice Causes
- Excessive RBC destruction → Increased unconjugated bilirubin
- Causes:
- Hemolytic anemia (sickle cell disease, hereditary spherocytosis)
- Glucose-6-phosphate dehydrogenase (G6PD) deficiency
- Malaria
- Blood transfusion reaction
- Spleen disorders (hypersplenism)
B. Hepatic (Hepatocellular) Jaundice Causes
- Liver dysfunction → Impaired bilirubin conjugation
- Causes:
- Viral hepatitis (Hepatitis A, B, C, D, E)
- Liver cirrhosis (alcoholic, non-alcoholic fatty liver disease)
- Gilbert’s Syndrome (UDP-glucuronosyltransferase deficiency)
- Crigler-Najjar Syndrome (severe UGT deficiency)
- Liver cancer/metastasis
C. Post-hepatic (Obstructive) Jaundice Causes
- Obstruction of bile flow → Increased conjugated bilirubin
- Causes:
- Gallstones (Cholelithiasis)
- Pancreatic carcinoma
- Biliary atresia
- Cholestasis (drug-induced, pregnancy-related)
- Primary biliary cirrhosis
3. Urine & Blood Investigations for Jaundice
Jaundice diagnosis is based on serum bilirubin, liver function tests (LFTs), urine tests, and imaging studies.
A. Blood Investigations
| Test | Findings in Different Types of Jaundice | Significance |
|---|---|---|
| Total Bilirubin | ↑ in all types | Confirms jaundice |
| Unconjugated (Indirect) Bilirubin | ↑ in pre-hepatic & hepatic | Hemolysis or liver dysfunction |
| Conjugated (Direct) Bilirubin | ↑ in hepatic & post-hepatic | Liver disease or bile obstruction |
| Alanine aminotransferase (ALT/SGPT) | ↑ in hepatic jaundice | Liver cell injury |
| Aspartate aminotransferase (AST/SGOT) | ↑ in hepatic jaundice | Liver damage indicator |
| Alkaline Phosphatase (ALP) | ↑ in post-hepatic jaundice | Biliary obstruction marker |
| Gamma-glutamyl transferase (GGT) | ↑ in post-hepatic jaundice | Differentiates hepatobiliary vs. bone disease |
| Hemoglobin (Hb) | ↓ in pre-hepatic jaundice | Indicates hemolysis |
| Reticulocyte count | ↑ in pre-hepatic jaundice | Increased RBC production |
| Lactate dehydrogenase (LDH) | ↑ in hemolysis | Marker of RBC destruction |
B. Urine Investigations
| Test | Findings in Different Types of Jaundice | Significance |
|---|---|---|
| Urine color | Dark (tea-colored) in obstructive jaundice | Conjugated bilirubin excretion |
| Urine Bilirubin | Present in post-hepatic jaundice | Indicates cholestasis |
| Urine Urobilinogen | ↑ in hemolytic jaundice | Excess RBC breakdown |
| Urine Urobilinogen | ↓ in post-hepatic jaundice | Obstruction prevents bilirubin reaching intestine |
C. Stool Examination
| Test | Findings in Different Types of Jaundice | Significance |
|---|---|---|
| Stool color | Pale/clay-colored in post-hepatic jaundice | Absence of stercobilin |
| Stercobilin level | ↓ in post-hepatic jaundice | Bile obstruction |
D. Imaging Studies
| Test | Used for Diagnosing |
|---|---|
| Ultrasound (USG Abdomen) | Gallstones, biliary obstruction |
| CT Scan/MRI Abdomen | Liver tumors, pancreatic cancer |
| Magnetic Resonance Cholangiopancreatography (MRCP) | Bile duct obstruction |
| Endoscopic Retrograde Cholangiopancreatography (ERCP) | Gallstones, biliary atresia |
4. Summary of Jaundice Types & Key Findings
| Feature | Pre-Hepatic Jaundice | Hepatic Jaundice | Post-Hepatic Jaundice |
|---|---|---|---|
| Total Bilirubin | ↑ | ↑ | ↑ |
| Unconjugated Bilirubin | ↑↑ | ↑ | Normal |
| Conjugated Bilirubin | Normal | ↑ | ↑↑ |
| Urine Bilirubin | Absent | Present | Present |
| Urine Urobilinogen | ↑↑ | Normal/↑ | ↓ |
| Stool Color | Normal/Dark | Normal | Pale (Clay-colored) |
| ALT/AST | Normal | ↑↑ | Normal |
| ALP/GGT | Normal | ↑ | ↑↑ |
5. Treatment Approaches
- Pre-hepatic Jaundice:
- Treat underlying hemolysis (e.g., blood transfusion, steroids).
- Manage infections (e.g., malaria).
- Hepatic Jaundice:
- Antiviral therapy for hepatitis.
- Stop hepatotoxic drugs.
- Supportive therapy for liver failure.
- Post-hepatic Jaundice:
- ERCP for bile duct obstruction.
- Cholecystectomy (gallstone removal).
- Surgery for biliary atresia or cancer.
Van den Bergh Test:

Introduction
The Van den Bergh test is a biochemical test used to differentiate between conjugated (direct) and unconjugated (indirect) bilirubin in the blood. It is essential in diagnosing different types of jaundice.
- Developed by: Albert van den Bergh in 1913.
- Principle: Based on the diazo reaction, where bilirubin reacts with diazotized sulfanilic acid to form a colored compound.
1. Principle of the Van den Bergh Test
- Conjugated bilirubin (Direct bilirubin) is water-soluble and reacts immediately with diazotized sulfanilic acid to form a red/purple color (direct reaction).
- Unconjugated bilirubin (Indirect bilirubin) is water-insoluble and does not react with diazotized sulfanilic acid unless alcohol is added (indirect reaction).
- The test helps determine whether jaundice is pre-hepatic, hepatic, or post-hepatic.
2. Reagents Required
- Diazotized sulfanilic acid (Diazo reagent)
- Sulfanilic acid
- Sodium nitrite (NaNO₂)
- Hydrochloric acid (HCl)
- Serum sample (Patient’s blood serum)
- Methanol or ethanol (for indirect bilirubin reaction)
3. Procedure of the Van den Bergh Test
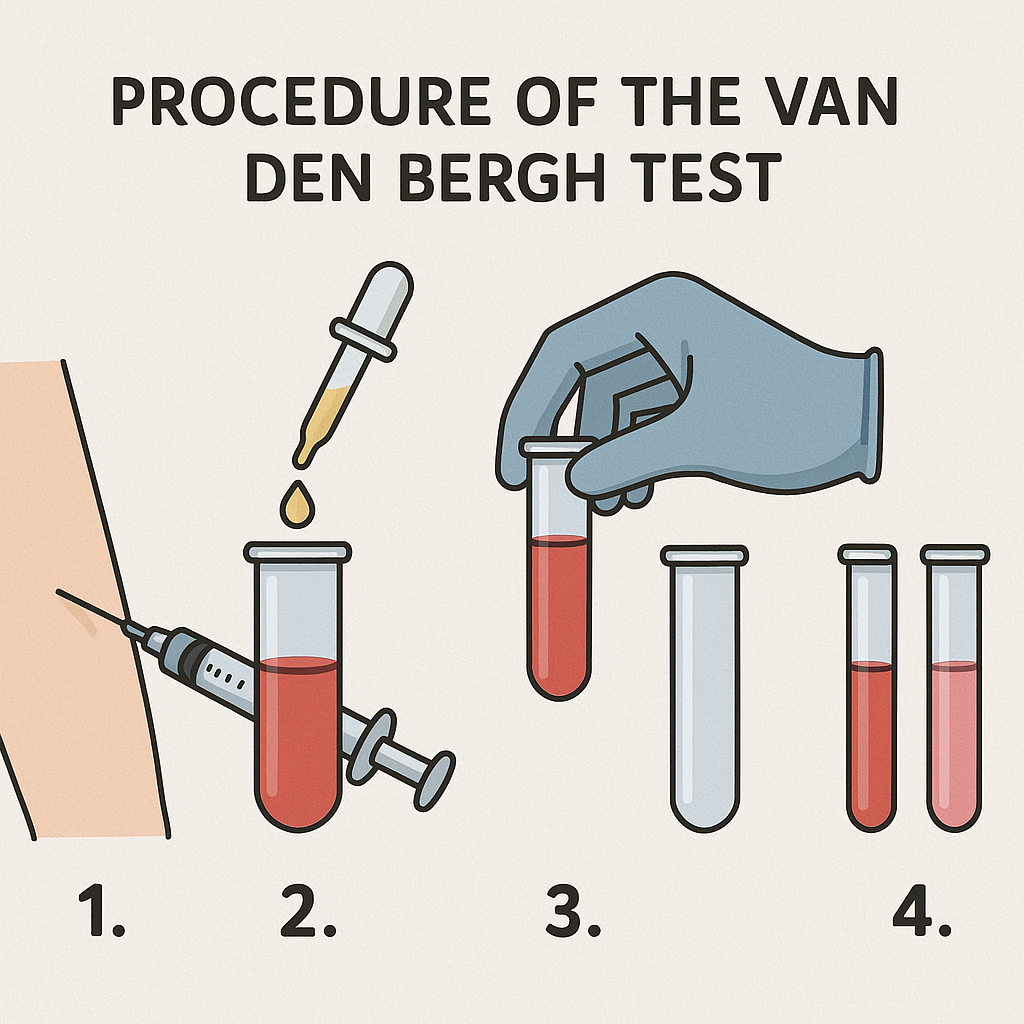
Step 1: Direct Reaction (Conjugated Bilirubin)
- Take 1 mL of patient’s serum in a test tube.
- Add 0.5 mL of diazotized sulfanilic acid.
- Observe the color change:
- If color appears immediately → Direct (Conjugated) bilirubin is present.
- No immediate color change → Proceed to the indirect reaction.
Step 2: Indirect Reaction (Unconjugated Bilirubin)
- To the same tube, add methanol or ethanol.
- Observe the color change:
- If color appears after alcohol addition → Indirect (Unconjugated) bilirubin is present.
- No color change → Bilirubin is absent.
4. Interpretation of the Van den Bergh Test
| Type of Reaction | Bilirubin Type | Jaundice Type | Examples |
|---|---|---|---|
| Immediate (Direct) Positive | Conjugated Bilirubin (Water-soluble) | Post-hepatic (Obstructive) Jaundice | Gallstones, Biliary Atresia, Pancreatic Tumor |
| Delayed (Indirect) Positive | Unconjugated Bilirubin (Water-insoluble) | Pre-hepatic (Hemolytic) Jaundice | Hemolytic Anemia, Malaria, G6PD Deficiency |
| Mixed Reaction (Both Direct & Indirect Positive) | Both Conjugated & Unconjugated Bilirubin | Hepatic Jaundice | Hepatitis, Cirrhosis, Liver Failure |
5. Clinical Significance of the Van den Bergh Test
- Differentiates types of jaundice:
- Pre-hepatic jaundice (Hemolytic jaundice) → Indirect bilirubin predominates.
- Hepatic jaundice (Liver disease) → Both direct and indirect bilirubin increase.
- Post-hepatic jaundice (Obstructive jaundice) → Direct bilirubin predominates.
- Helps monitor liver function in liver diseases.
6. Summary of Results & Their Meaning
| Van den Bergh Reaction | Type of Jaundice | Causes |
|---|---|---|
| Direct (Immediate Positive Reaction) | Post-hepatic (Obstructive) Jaundice | Gallstones, Cholestasis, Biliary Atresia |
| Indirect (Delayed Positive Reaction) | Pre-hepatic (Hemolytic) Jaundice | Hemolysis, Malaria, G6PD Deficiency |
| Mixed (Both Immediate & Delayed Reaction) | Hepatic Jaundice | Hepatitis, Cirrhosis, Liver Failure |
7. Limitations of the Van den Bergh Test
- Cannot measure exact bilirubin concentration (requires bilirubin assay).
- Cannot differentiate between mild liver dysfunction and Gilbert’s syndrome.
- Not useful in detecting bilirubin metabolites.
8. Modern Alternative Tests for Bilirubin Measurement
- Total & Direct Bilirubin Test (Spectrophotometry)
- Liver Function Tests (LFTs) (AST, ALT, ALP, GGT)
- Urine Bilirubin & Urobilinogen Test
- High-Performance Liquid Chromatography (HPLC)
- Immunoassays for Bilirubin Detection