BSC SEM 1 UNIT 5 APPLIED NUTRITION AND DIETETICS
UNIT 5 Vitamins

Introduction to Vitamins.
Definition of Vitamins
Vitamins are organic compounds that are essential for normal growth, metabolism, and overall health. They are required in small amounts and must be obtained from food because the human body either does not produce them at all or does not produce them in sufficient quantities.
Classification of Vitamins
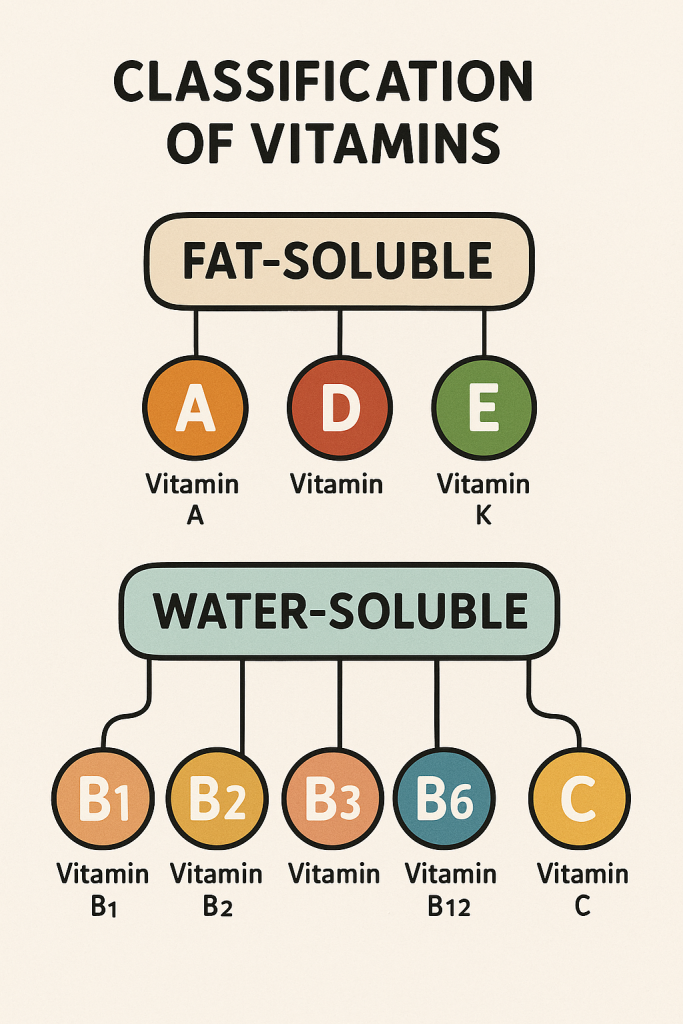
Vitamins are classified into two main categories based on their solubility:
- Fat-Soluble Vitamins: These vitamins are stored in the body’s fatty tissues and liver. They require dietary fat for absorption. Examples include:
- Vitamin A (Retinol)
- Vitamin D (Calciferol)
- Vitamin E (Tocopherol)
- Vitamin K (Phylloquinone, Menaquinone)
- Water-Soluble Vitamins: These vitamins are not stored in the body and must be consumed regularly. Excess amounts are excreted in urine. Examples include:
- Vitamin C (Ascorbic Acid)
- Vitamin B-complex Group:
- B1 (Thiamine)
- B2 (Riboflavin)
- B3 (Niacin)
- B5 (Pantothenic Acid)
- B6 (Pyridoxine)
- B7 (Biotin)
- B9 (Folic Acid)
- B12 (Cobalamin)
Functions of Vitamins
Each vitamin plays a crucial role in the body’s physiological functions:
| Vitamin | Function |
|---|---|
| Vitamin A | Vision, immune function, skin health |
| Vitamin D | Calcium absorption, bone health |
| Vitamin E | Antioxidant, protects cells from damage |
| Vitamin K | Blood clotting, bone metabolism |
| Vitamin C | Antioxidant, wound healing, iron absorption |
| Vitamin B1 (Thiamine) | Energy metabolism, nerve function |
| Vitamin B2 (Riboflavin) | Energy production, skin and eye health |
| Vitamin B3 (Niacin) | Metabolism of carbohydrates, fats, proteins |
| Vitamin B5 (Pantothenic Acid) | Synthesis of coenzyme A, fatty acid metabolism |
| Vitamin B6 (Pyridoxine) | Neurotransmitter function, hemoglobin production |
| Vitamin B7 (Biotin) | Fat and carbohydrate metabolism, skin health |
| Vitamin B9 (Folic Acid) | DNA synthesis, red blood cell production |
| Vitamin B12 (Cobalamin) | Nerve function, red blood cell formation |
Sources of Vitamins
Vitamins are obtained through a balanced diet, including:
- Vitamin A: Carrots, liver, eggs, dairy products
- Vitamin D: Sunlight exposure, fortified milk, fish liver oils
- Vitamin E: Nuts, seeds, vegetable oils
- Vitamin K: Leafy green vegetables, fish, meat
- Vitamin C: Citrus fruits, strawberries, tomatoes
- Vitamin B1: Whole grains, nuts, pork
- Vitamin B2: Dairy products, eggs, green vegetables
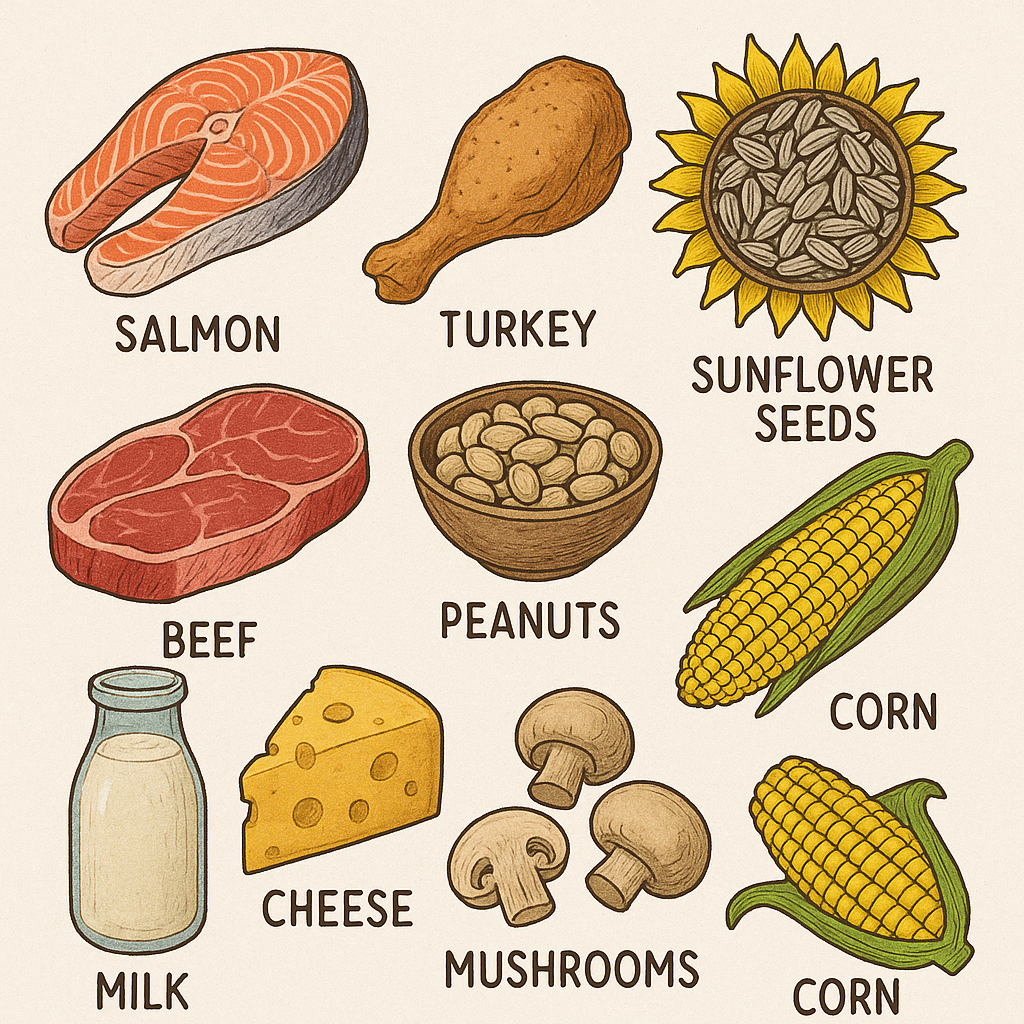
- Vitamin B3: Meat, poultry, fish, whole grains
- Vitamin B5: Meat, dairy, whole grains
- Vitamin B6: Bananas, potatoes, chicken
- Vitamin B7: Eggs, nuts, whole grains
- Vitamin B9: Leafy greens, beans, oranges
- Vitamin B12: Meat, fish, dairy products
Deficiency Disorders and Health Impacts
Vitamin deficiencies can lead to several health conditions:
| Vitamin Deficiency | Associated Disease/Condition |
|---|---|
| Vitamin A | Night blindness, xerophthalmia |
| Vitamin D | Rickets (children), osteomalacia (adults) |
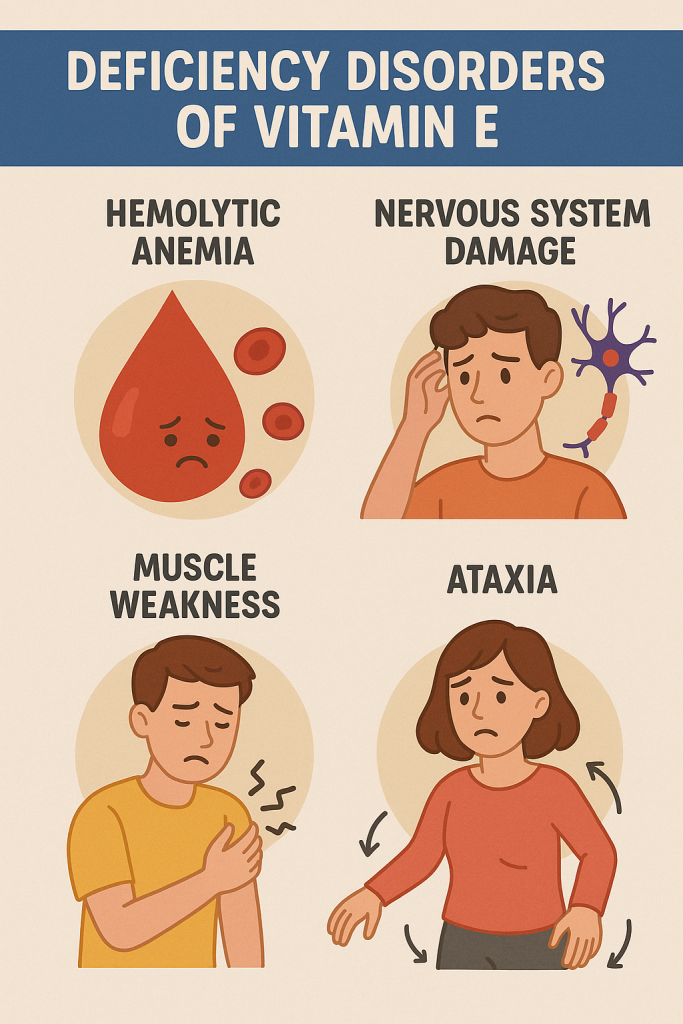
| Vitamin E | Neurological problems, muscle weakness |
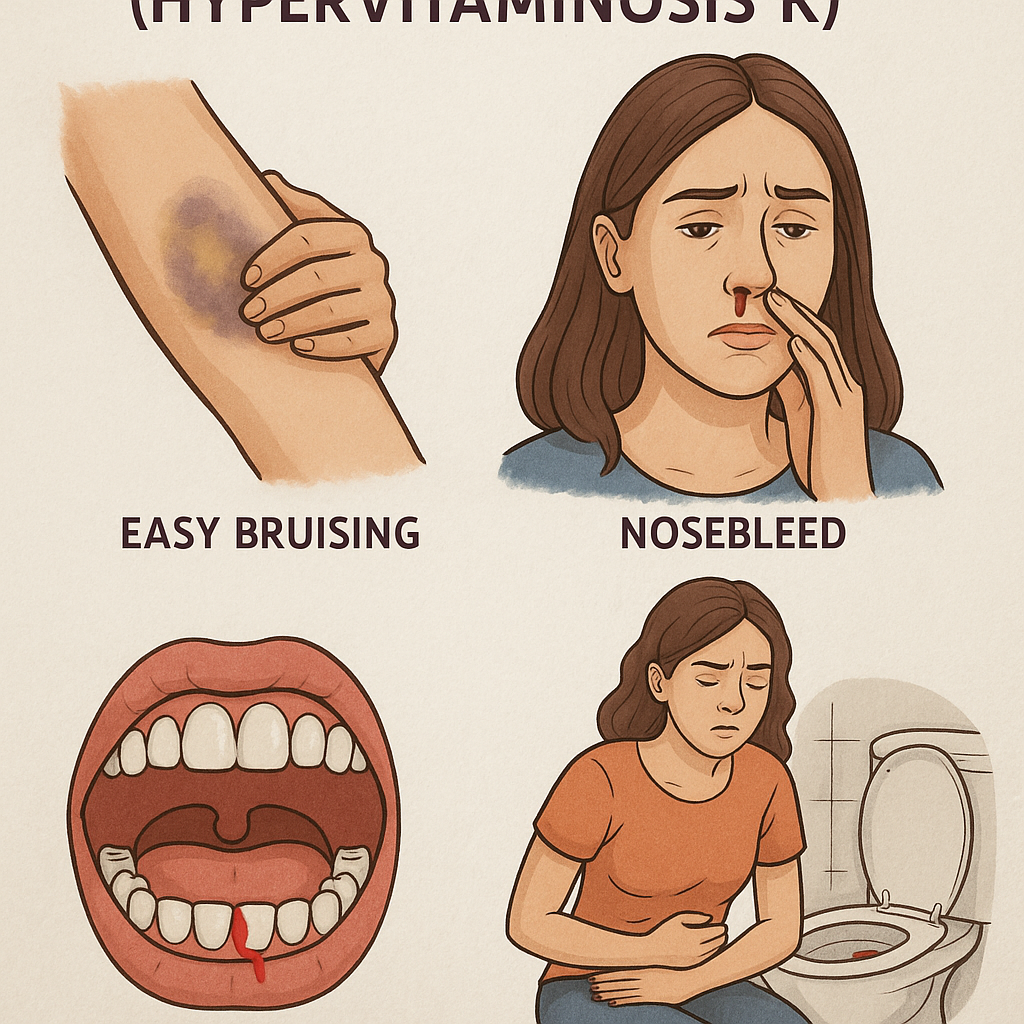
| Vitamin K | Prolonged bleeding, easy bruising |
| Vitamin C | Scurvy (bleeding gums, poor wound healing) |
| Vitamin B1 | Beriberi, Wernicke-Korsakoff syndrome |
| Vitamin B2 | Cracks in mouth, sore throat, anemia |
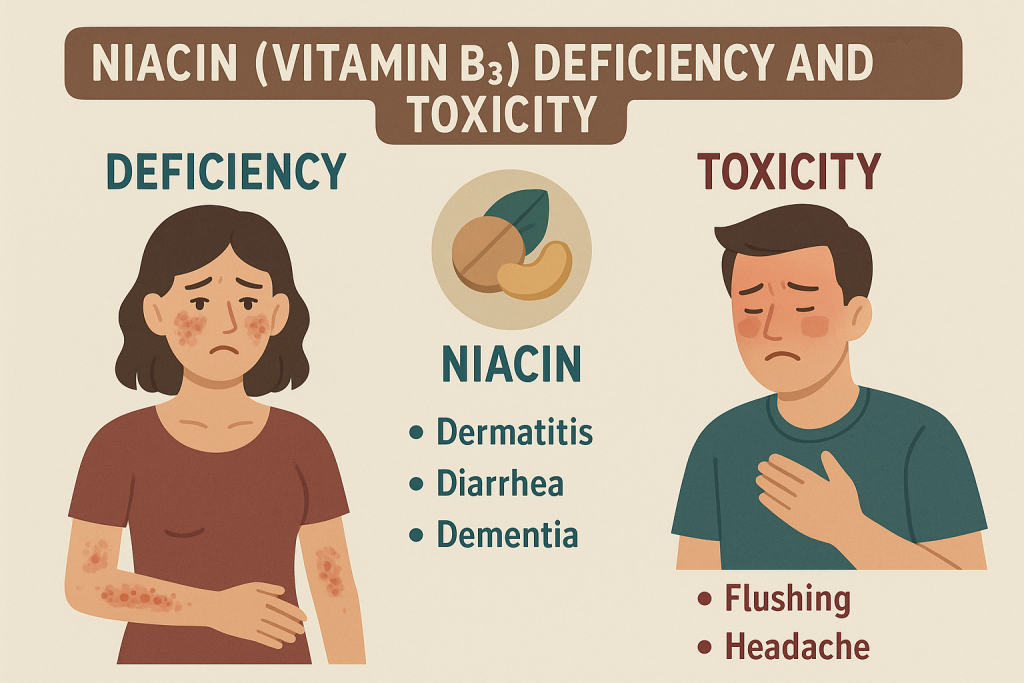
| Vitamin B3 | Pellagra (diarrhea, dermatitis, dementia) |
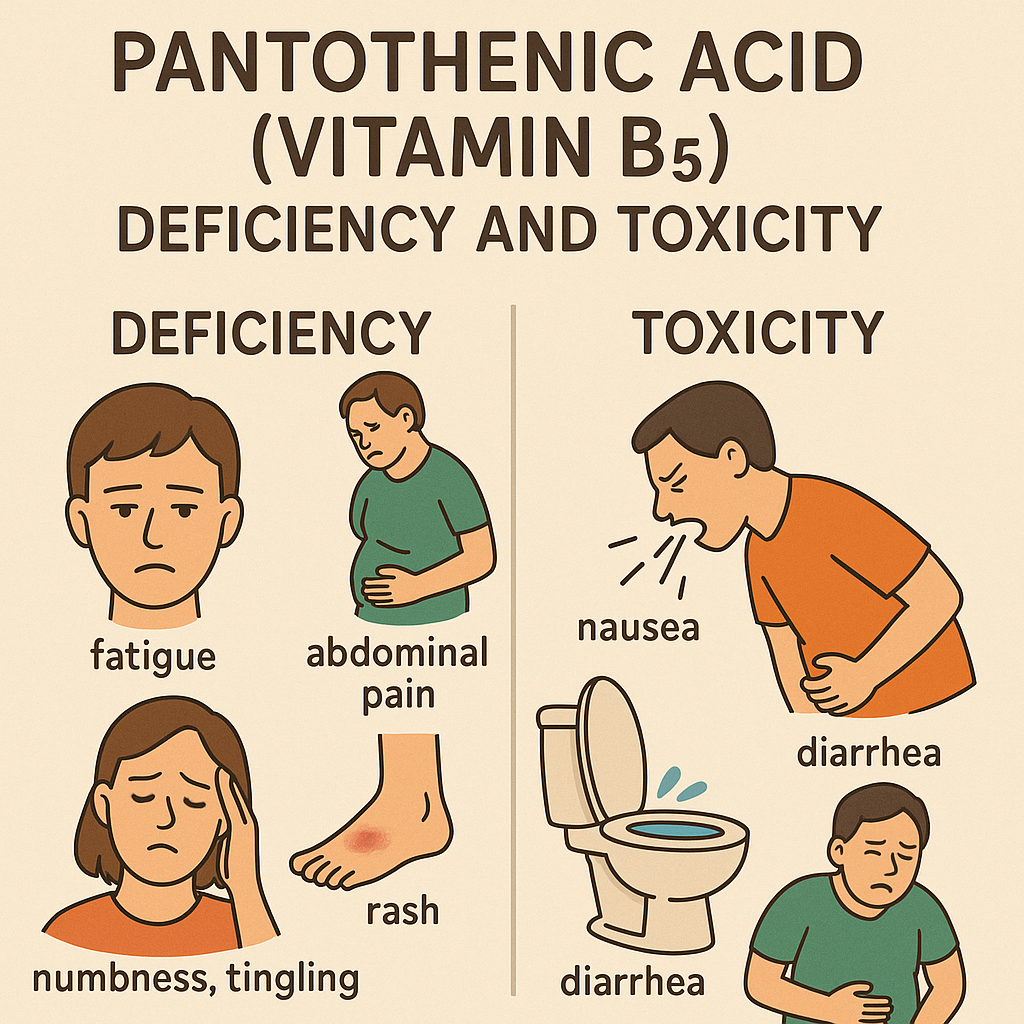
| Vitamin B5 | Fatigue, irritability, numbness |
| Vitamin B6 | Anemia, depression, confusion |
| Vitamin B7 | Hair loss, dermatitis, fatigue |
| Vitamin B9 | Neural tube defects, anemia |
| Vitamin B12 | Pernicious anemia, neurological issues |
Toxicity of Vitamins
While water-soluble vitamins are generally excreted if taken in excess, fat-soluble vitamins can accumulate and cause toxicity. Examples include:
- Vitamin A toxicity: Liver damage, birth defects
- Vitamin D toxicity: Hypercalcemia, kidney damage
- Vitamin E toxicity: Increased risk of bleeding
- Vitamin K toxicity: Blood clotting disorders
Role of Nurses in Vitamin Nutrition
- Assessment of Nutritional Status: Nurses evaluate dietary intake and signs of vitamin deficiencies.
- Patient Education: Nurses educate patients about the importance of vitamins and how to obtain them from food.
- Dietary Planning: Nurses help create meal plans that ensure adequate vitamin intake.
- Administration of Supplements: Nurses may administer vitamin supplements, especially in deficiency cases.
- Monitoring for Deficiencies and Toxicities: Nurses observe patients for symptoms of vitamin imbalance.
Fat-Soluble Vitamins: Classification
Introduction
Fat-soluble vitamins are essential micronutrients that dissolve in fats and are stored in the body’s fat tissues and liver. Unlike water-soluble vitamins, they are not excreted easily through urine and can accumulate in the body, leading to toxicity if consumed in excessive amounts. They require dietary fats for absorption and play vital roles in various physiological processes.
Classification of Fat-Soluble Vitamins
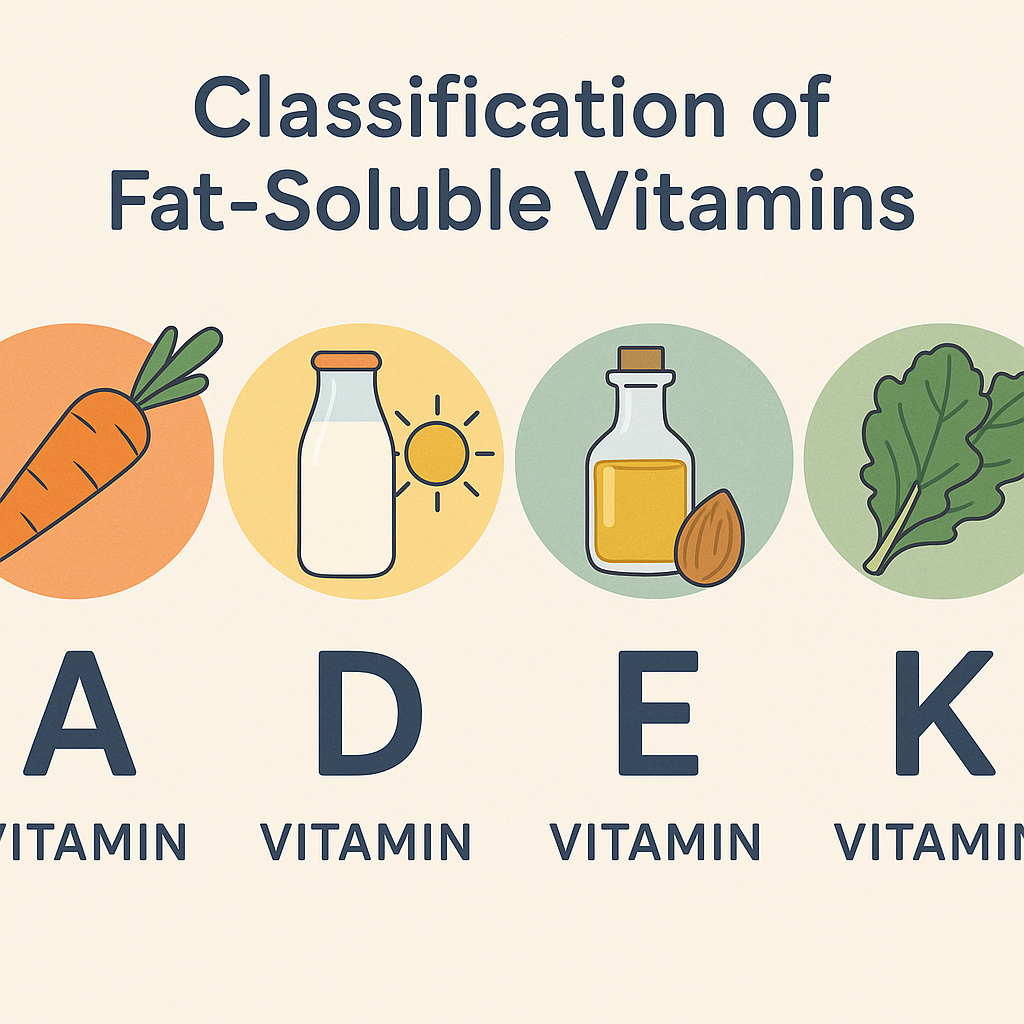
The four fat-soluble vitamins are:
- Vitamin A (Retinol, Beta-Carotene)
- Vitamin D (Calciferol)
- Vitamin E (Tocopherol)
- Vitamin K (Phylloquinone, Menaquinone)
Each of these vitamins has distinct functions, sources, deficiency disorders, and toxicity risks.
1. Vitamin A (Retinol, Beta-Carotene)
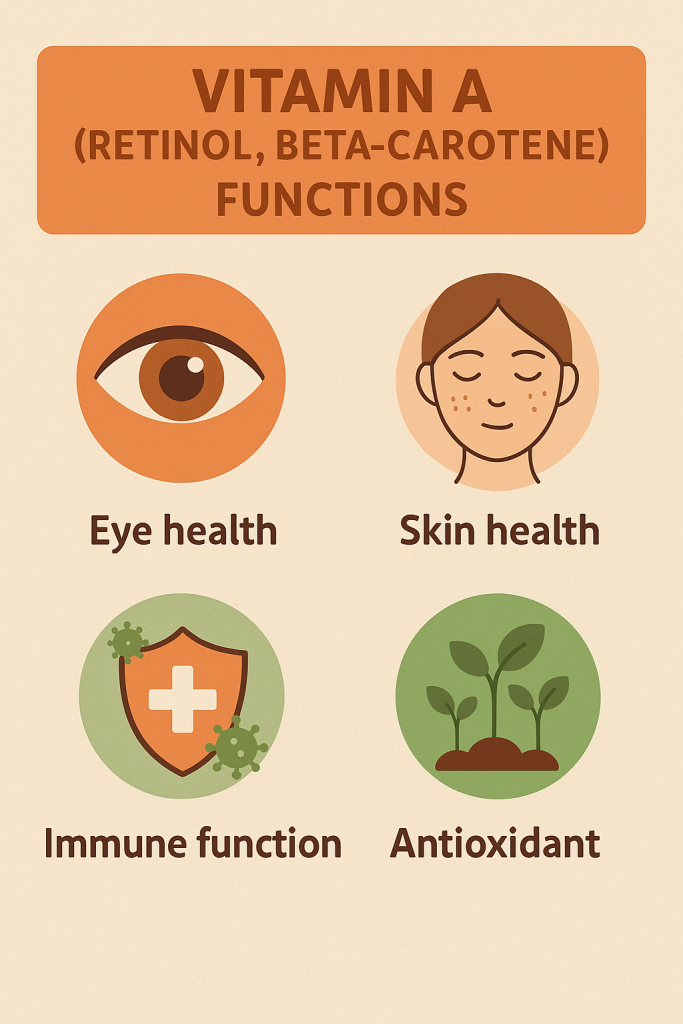
Functions
- Essential for vision (formation of rhodopsin in the retina).
- Promotes growth and development, including bone and skin health.
- Supports the immune system by enhancing white blood cell function.
- Maintains healthy skin and mucous membranes.
- Acts as an antioxidant (beta-carotene).
Sources

- Animal sources (Retinol): Liver, fish oils, dairy products, egg yolk.
- Plant sources (Beta-Carotene): Carrots, spinach, sweet potatoes, pumpkin, mangoes, and papaya.
Deficiency Disorders
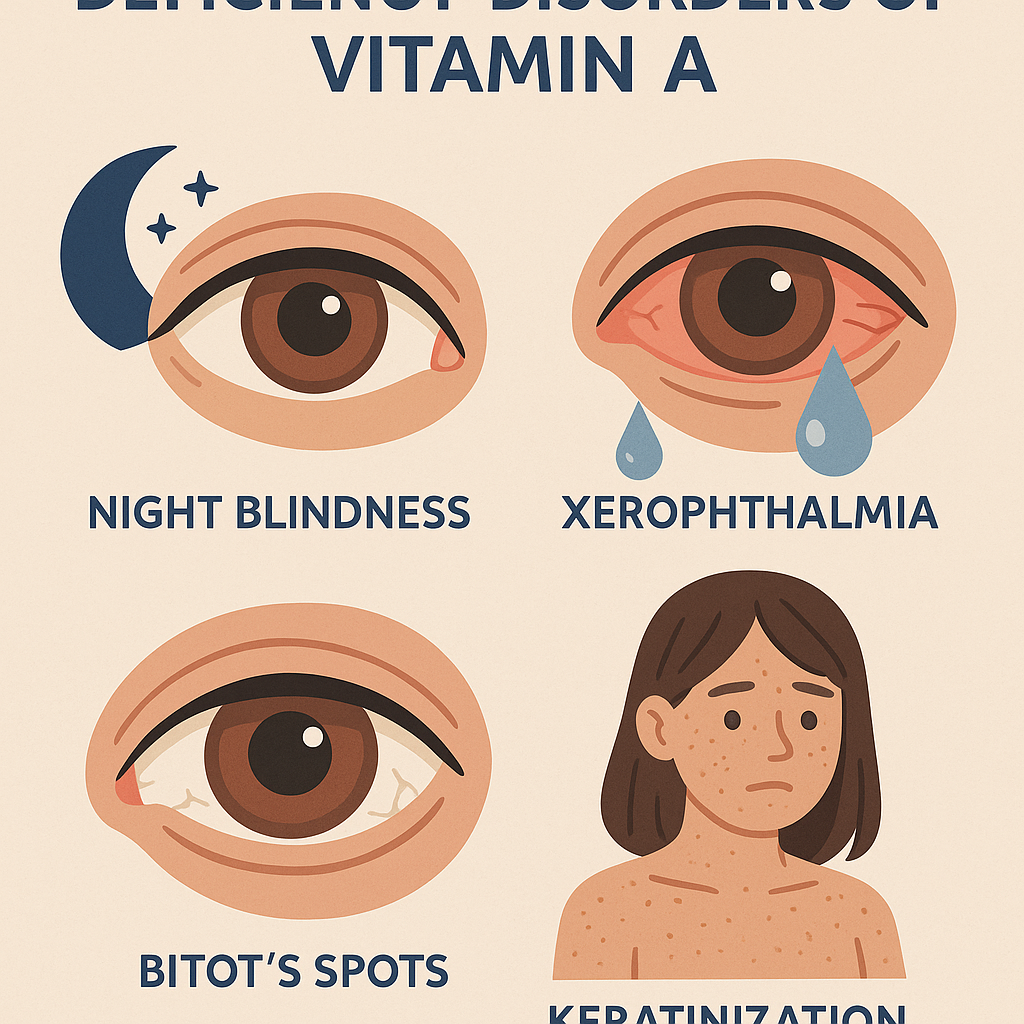
- Night blindness (Nyctalopia) – Inability to see in dim light.
- Xerophthalmia – Dryness and damage to the cornea, leading to blindness.
- Keratomalacia – Softening of the cornea due to severe deficiency.
- Weakened immunity – Increased risk of infections.
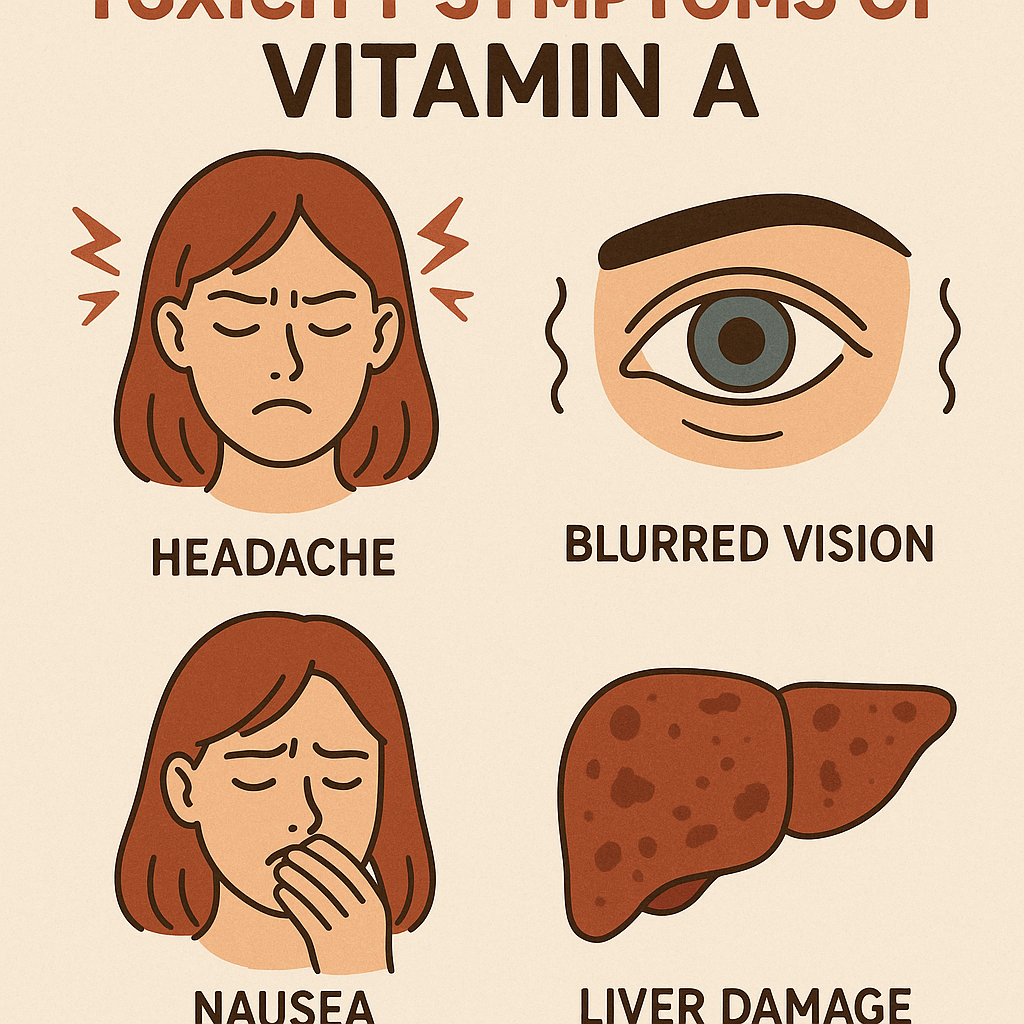
Toxicity Symptoms (Hypervitaminosis A)
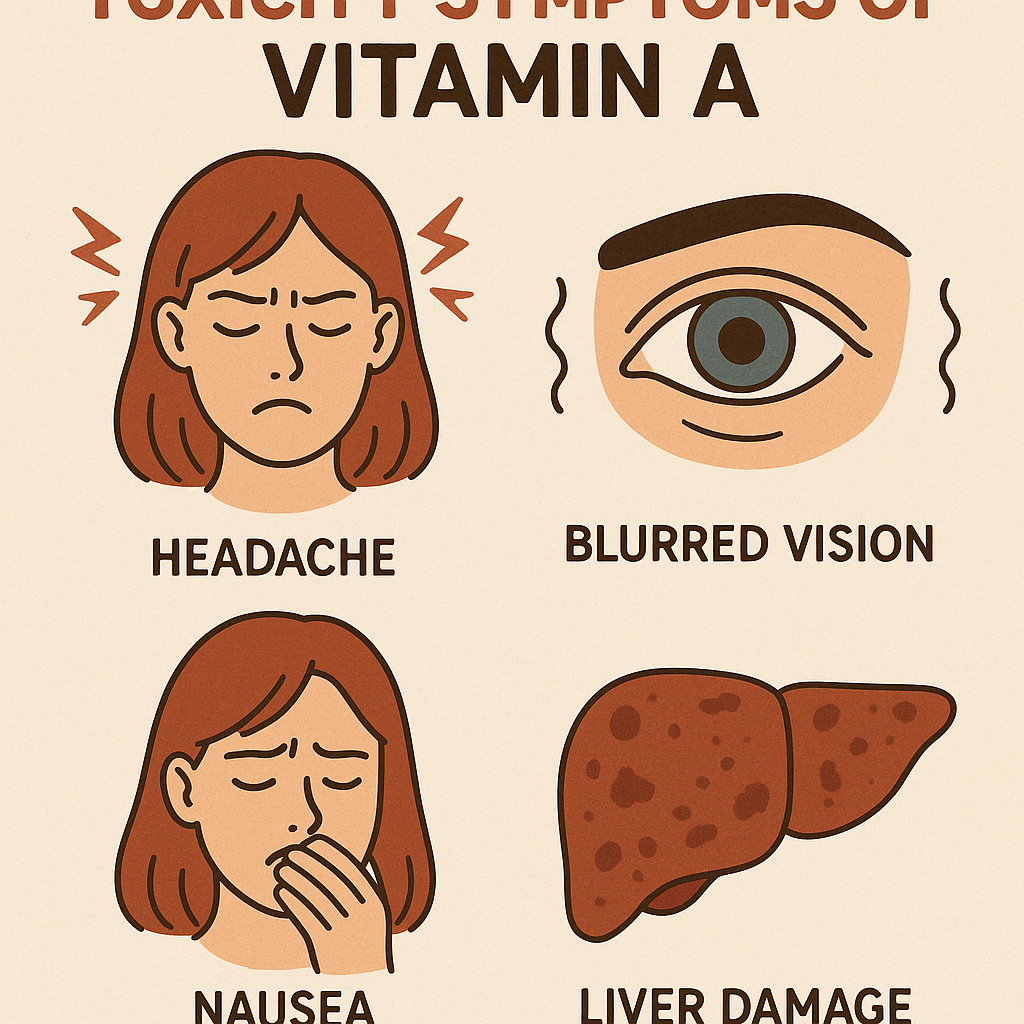
- Acute toxicity: Nausea, headache, dizziness, blurred vision.
- Chronic toxicity: Liver damage, bone pain, birth defects in pregnant women.
2. Vitamin D (Calciferol)
Functions
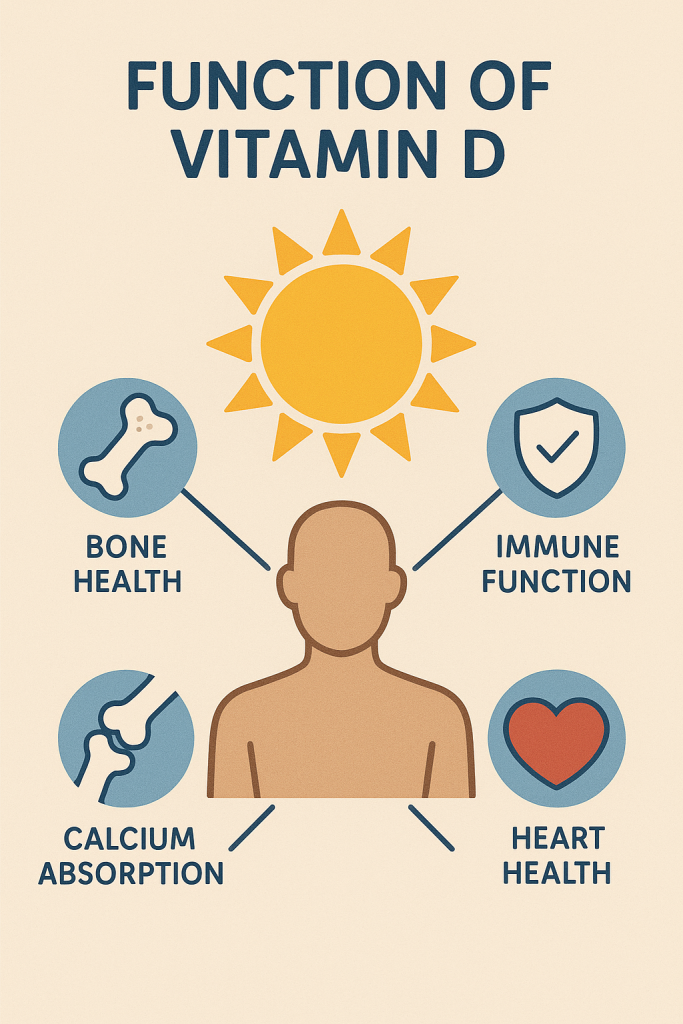
- Regulates calcium and phosphorus metabolism, essential for bone and teeth health.
- Enhances calcium absorption in the intestine.
- Prevents rickets in children and osteomalacia in adults.
- Supports immune function and muscle function.
Sources
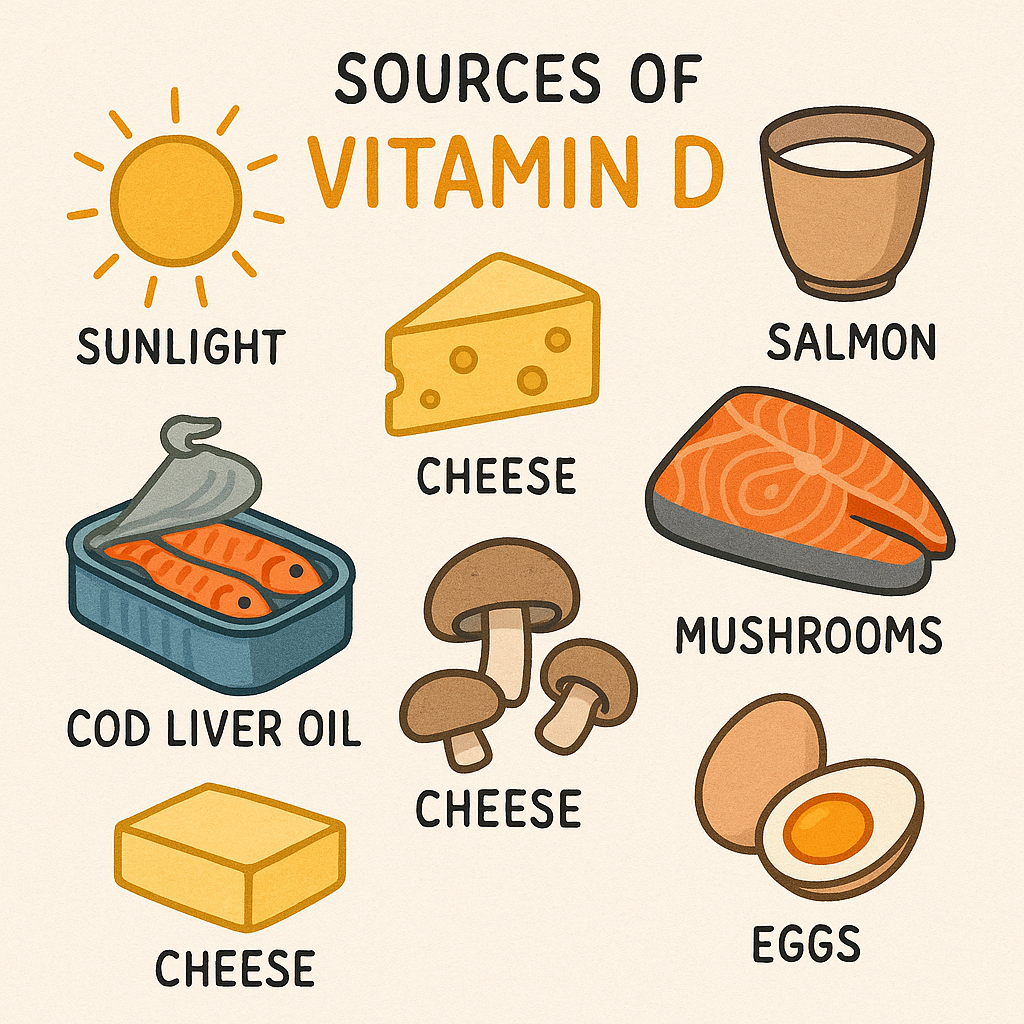
- Sunlight (Primary Source): UV rays convert 7-dehydrocholesterol in the skin to Vitamin D.
- Food Sources: Fatty fish (salmon, mackerel), cod liver oil, egg yolks, fortified milk and cereals.
Deficiency Disorders
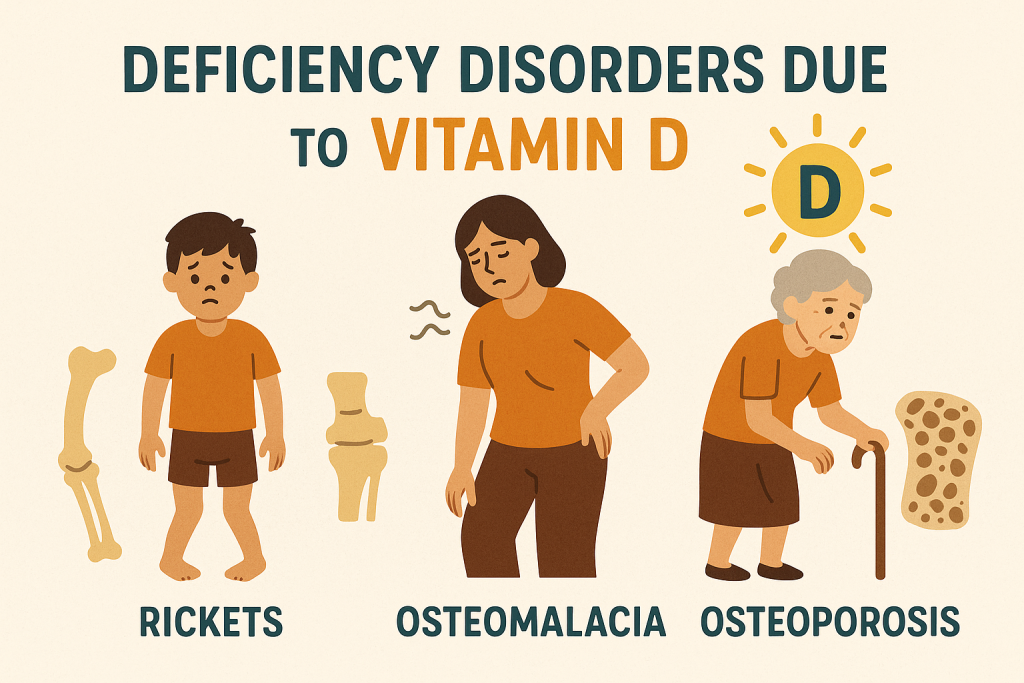
- Rickets (Children): Soft, weak bones, bowed legs, delayed growth.
- Osteomalacia (Adults): Bone pain, muscle weakness, fractures.
- Osteoporosis: Decreased bone density, increased fracture risk.
Toxicity Symptoms (Hypervitaminosis D)
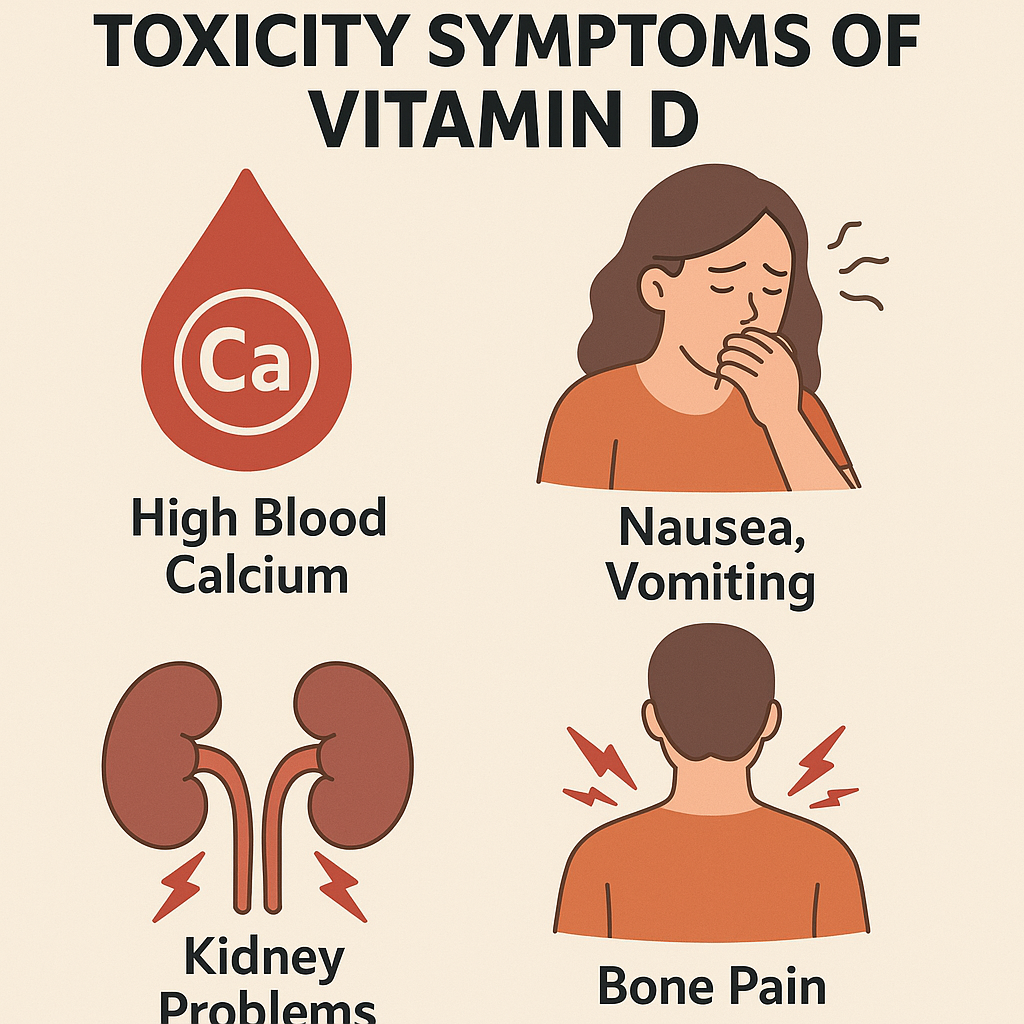
- Hypercalcemia: Excess calcium in blood, leading to kidney stones.
- Nausea, vomiting, weakness, and confusion.
- Kidney damage due to excessive calcium deposition.
3. Vitamin E (Tocopherol)
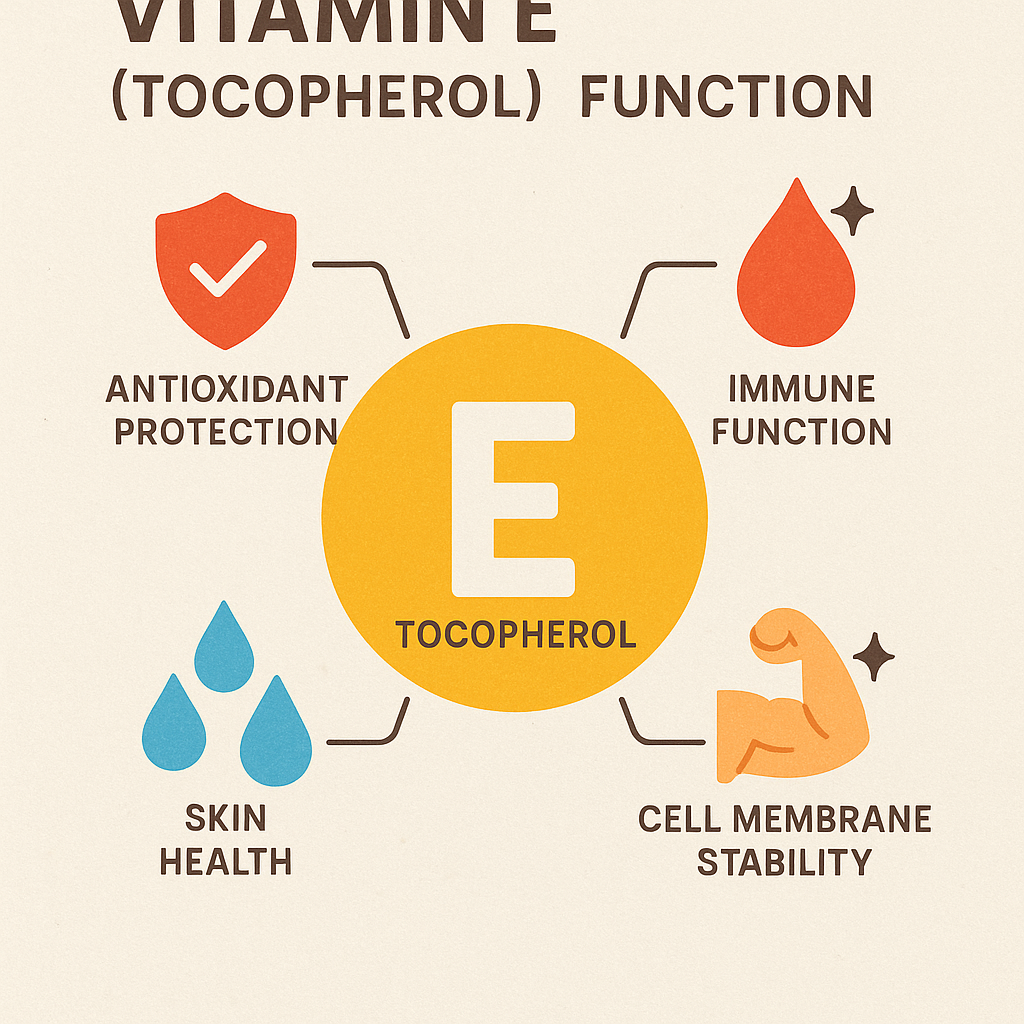
Functions
- Acts as a powerful antioxidant, protecting cells from oxidative damage.
- Supports immune function.
- Helps maintain healthy skin and eyes.
- Prevents oxidation of LDL cholesterol, reducing the risk of heart disease.
Sources

- Vegetable oils: Sunflower, safflower, and wheat germ oil.
- Nuts and seeds: Almonds, hazelnuts, sunflower seeds.
- Leafy greens: Spinach, broccoli.
Deficiency Disorders
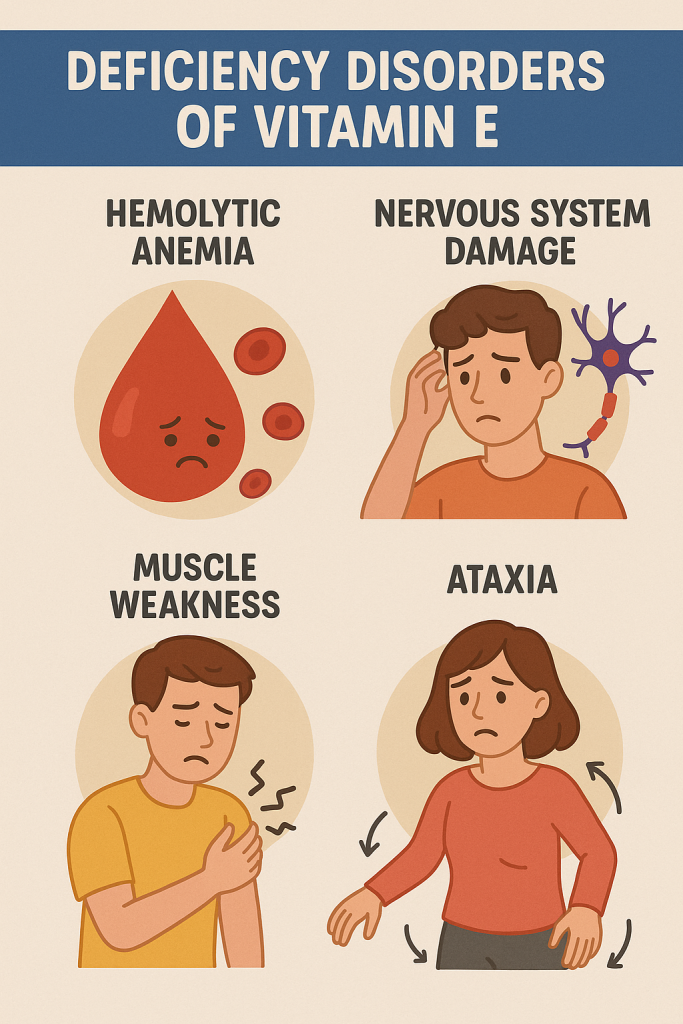
- Neurological problems: Peripheral neuropathy (numbness, tingling).
- Hemolytic anemia: Red blood cells rupture due to oxidative stress.
- Retinopathy: Damage to the retina affecting vision.
- Impaired immune response.
Toxicity Symptoms (Hypervitaminosis E)
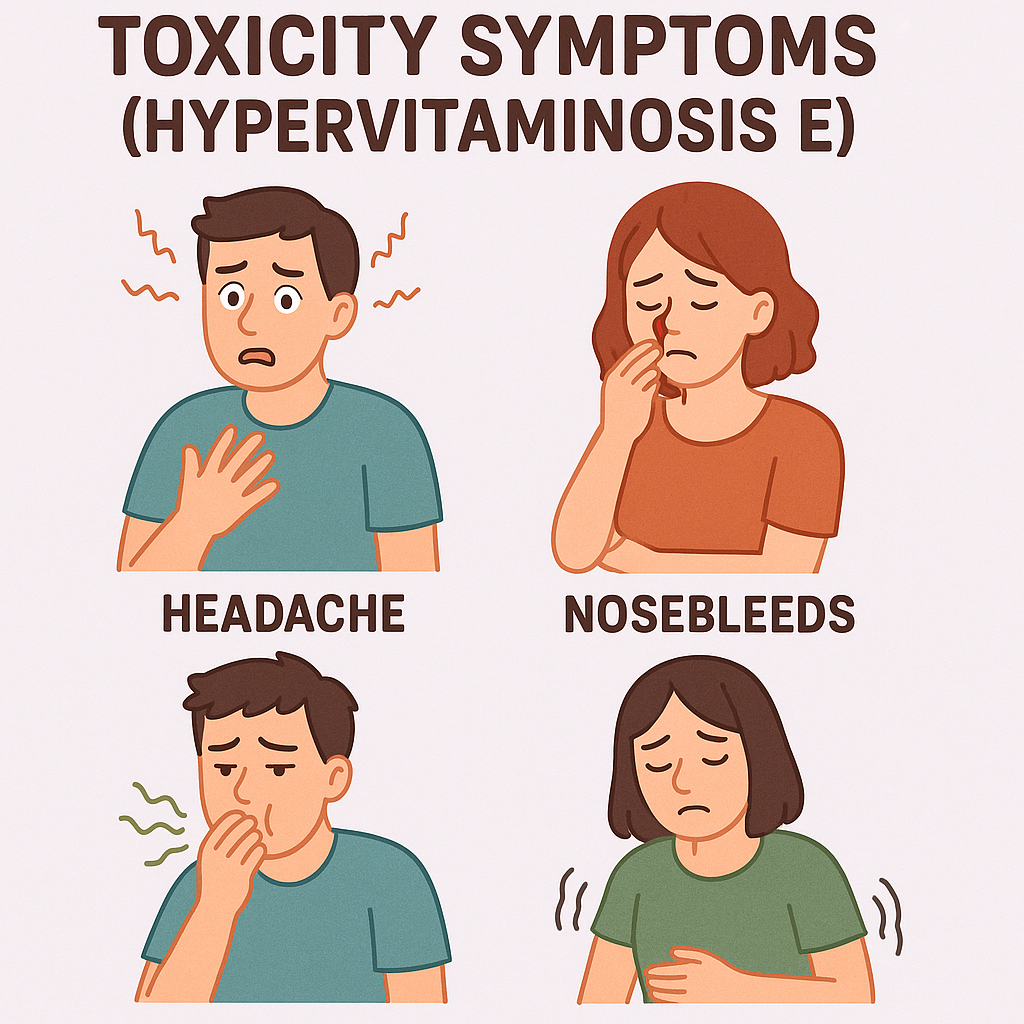
- Increased risk of bleeding (hemorrhage) by interfering with Vitamin K.
- Gastrointestinal disturbances: Nausea, diarrhea.
- Weakness and fatigue.
4. Vitamin K (Phylloquinone, Menaquinone)
Functions
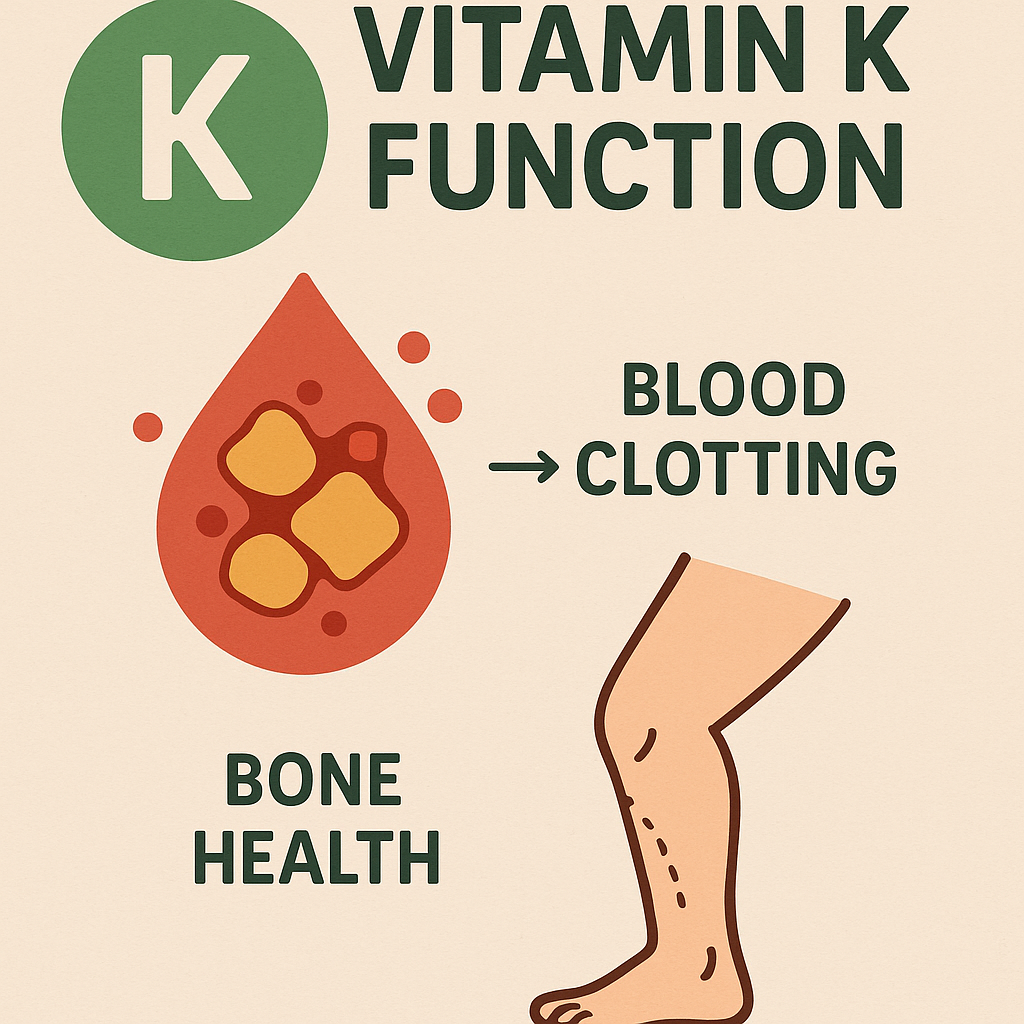
- Essential for blood clotting (coagulation) by activating clotting factors.
- Supports bone health by helping in bone mineralization.
- Prevents excessive calcification of arteries.
Sources

- Leafy green vegetables: Spinach, kale, broccoli.
- Fermented foods: Cheese, natto (fermented soybeans).
- Animal sources: Liver, eggs, meat.
Deficiency Disorders
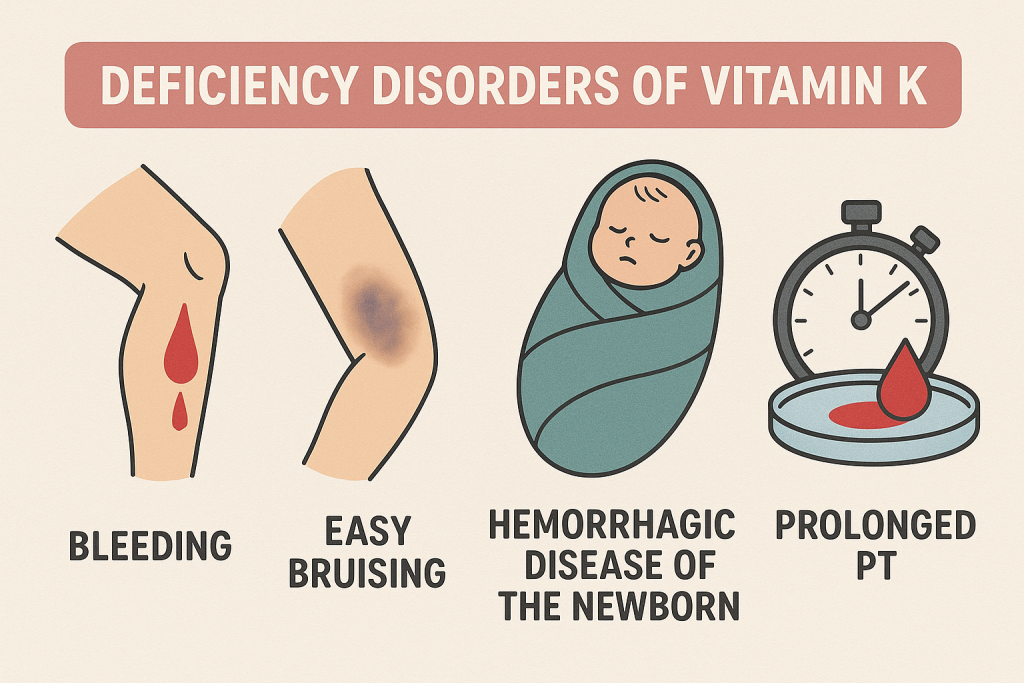
- Increased bleeding tendency (Hemorrhagic disease of the newborn).
- Prolonged blood clotting time (easy bruising, nosebleeds).
- Bone fractures due to reduced bone mineralization.
Toxicity Symptoms (Hypervitaminosis K)
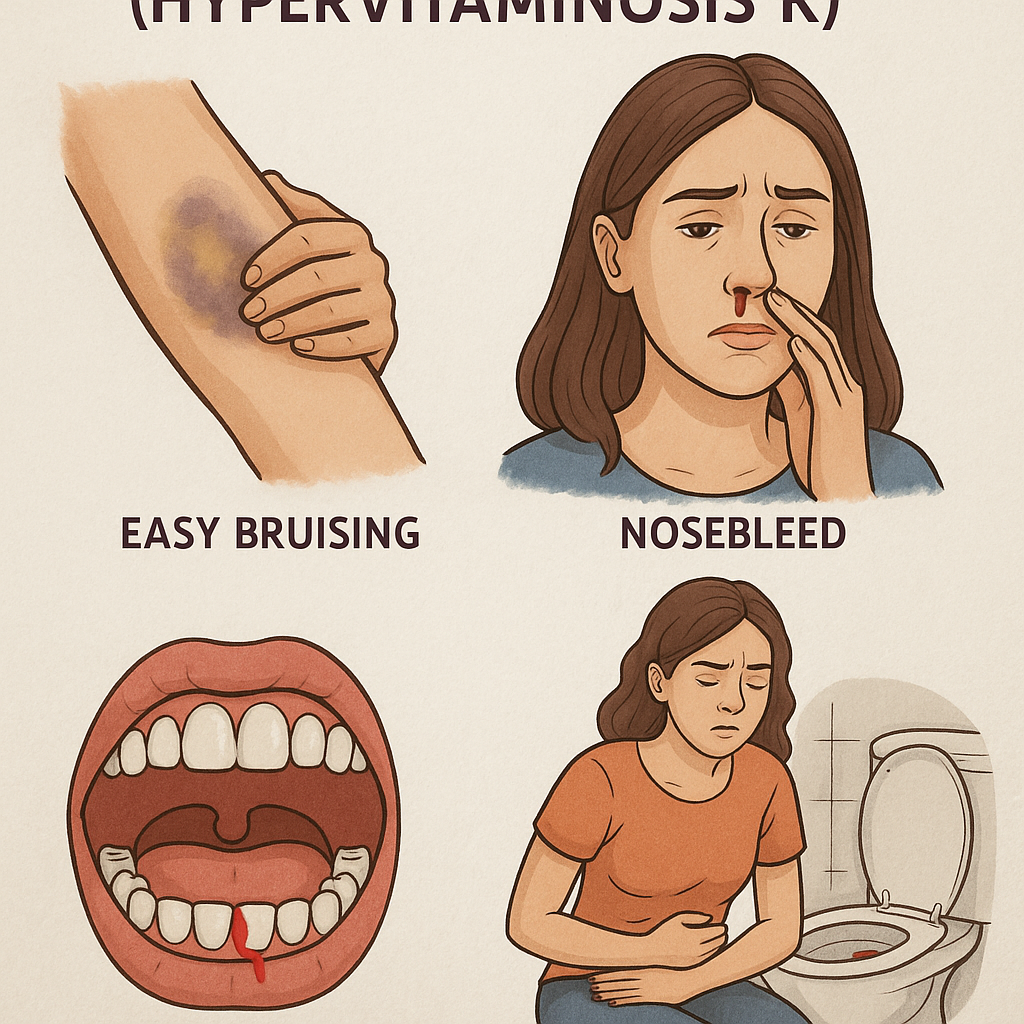
- Rare, but can lead to blood clotting issues.
- Excess Vitamin K can interfere with anticoagulant medications (e.g., Warfarin).
Comparison of Fat-Soluble Vitamins
| Vitamin | Function | Sources | Deficiency Disorders | Toxicity Effects |
|---|---|---|---|---|
| Vitamin A | Vision, immune function, skin health | Liver, dairy, carrots, spinach | Night blindness, xerophthalmia | Liver damage, birth defects |
| Vitamin D | Calcium absorption, bone health | Sunlight, fish, fortified milk | Rickets, osteomalacia, osteoporosis | Hypercalcemia, kidney damage |
| Vitamin E | Antioxidant, immune support | Nuts, seeds, vegetable oils | Neuropathy, anemia, retinopathy | Bleeding risk, nausea |
| Vitamin K | Blood clotting, bone health | Leafy greens, liver, fermented foods | Increased bleeding, weak bones | Blood clotting issues |
Role of Fat-Soluble Vitamins in Nursing
Nurses play a crucial role in ensuring patients receive adequate fat-soluble vitamins by:
- Assessing Nutritional Intake: Identifying deficiencies and guiding patients on dietary sources.
- Educating Patients: Teaching about the importance of fat-soluble vitamins in health maintenance.
- Monitoring for Deficiency Symptoms: Observing signs of night blindness, osteoporosis, excessive bleeding, or neurological issues.
- Preventing Toxicity: Advising patients on safe supplementation, especially with Vitamin A and D.
- Supporting Special Populations: Pregnant women, infants, elderly, and individuals with malabsorption disorders (e.g., Crohn’s disease, celiac disease) require special attention.
Water-Soluble Vitamins: Classification
Introduction
Water-soluble vitamins are essential nutrients that dissolve in water and are not stored in significant amounts in the body. Since they are excreted in urine, they must be consumed regularly through diet. These vitamins play a crucial role in metabolism, energy production, red blood cell formation, and maintaining healthy skin, eyes, and nerves.
Classification of Water-Soluble Vitamins
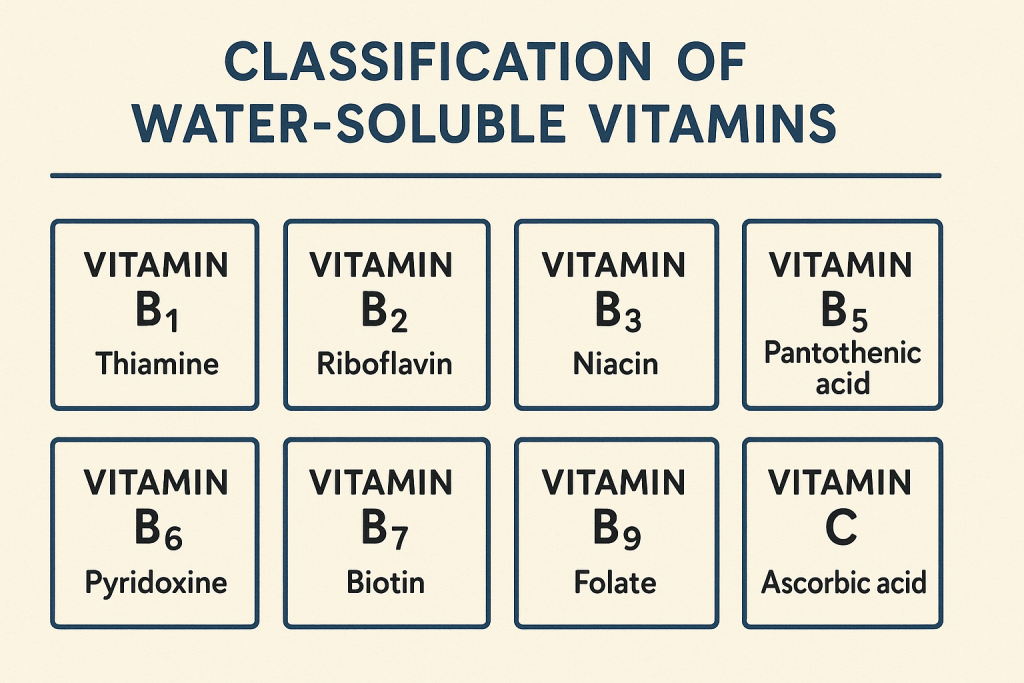
Water-soluble vitamins are classified into two major groups:
- Vitamin C (Ascorbic Acid)
- Vitamin B-Complex Group, which includes:
- B1 (Thiamine)
- B2 (Riboflavin)
- B3 (Niacin)
- B5 (Pantothenic Acid)
- B6 (Pyridoxine)
- B7 (Biotin)
- B9 (Folic Acid)
- B12 (Cobalamin)
Each of these vitamins has distinct functions, dietary sources, deficiency disorders, and toxicity concerns.
1. Vitamin C (Ascorbic Acid)
Functions
- Powerful antioxidant, protects cells from damage.
- Promotes collagen synthesis, essential for skin, cartilage, and wound healing.
- Enhances iron absorption from plant-based foods.
- Supports immune function and helps fight infections.
- Reduces inflammation and supports cardiovascular health.
Sources
- Fruits: Citrus fruits (oranges, lemons), strawberries, kiwi, guava.
- Vegetables: Bell peppers, broccoli, tomatoes, spinach.
Deficiency Disorders
- Scurvy: Symptoms include bleeding gums, bruising, fatigue, poor wound healing.
- Weakened immunity: Increased susceptibility to infections.
- Anemia: Due to impaired iron absorption.
Toxicity Symptoms
- Rare, but excessive intake can cause nausea, diarrhea, and kidney stone formation.
2. Vitamin B-Complex Group
The B-complex vitamins work together to help convert food into energy, support brain function, and maintain healthy skin and blood cells.
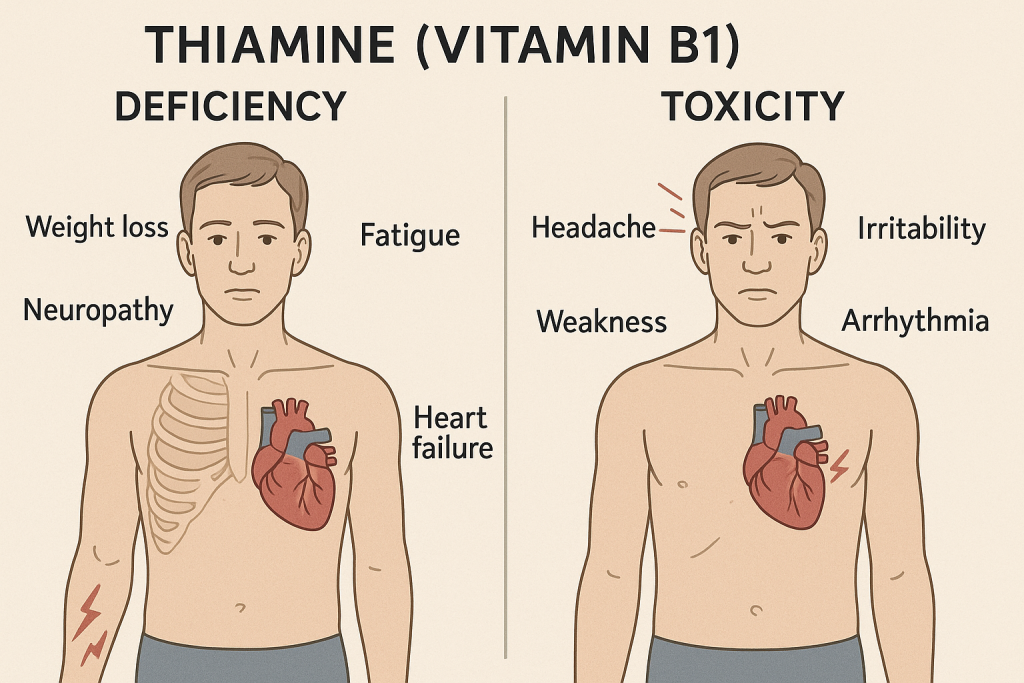
B1 (Thiamine)
Functions
- Helps convert carbohydrates into energy.
- Essential for nerve function and muscle contraction.
Sources
- Whole grains, nuts, pork, legumes.
Deficiency Disorders
- Beriberi: Muscle weakness, nerve damage, heart problems.
- Wernicke-Korsakoff Syndrome: Common in alcoholics, causes confusion and memory loss.
Toxicity Symptoms
- Rare, excess is excreted.
B2 (Riboflavin)
Functions
- Supports energy production and metabolism.
- Maintains healthy skin, eyes, and nerve function.
Sources
- Dairy products, eggs, green leafy vegetables, meat.
Deficiency Disorders
- Cheilitis: Cracks in lips and mouth.
- Glossitis: Swollen, red tongue.
- Eye disorders: Sensitivity to light.
Toxicity Symptoms
- None known; excess is excreted in urine.
B3 (Niacin)
Functions
- Essential for DNA repair and energy metabolism.
- Supports healthy skin and nervous system.
Sources
- Meat, fish, peanuts, whole grains.
Deficiency Disorders
- Pellagra: Symptoms include diarrhea, dermatitis, dementia, and death (4 Ds).
Toxicity Symptoms
- High doses can cause flushing, liver damage, and stomach irritation.
B5 (Pantothenic Acid)
Functions
- Involved in the synthesis of coenzyme A, crucial for energy metabolism.
- Helps in hormone production.
Sources
- Meat, eggs, whole grains, avocados.
Deficiency Disorders
- Rare, but may cause fatigue, irritability, and numbness.
Toxicity Symptoms
- Very rare, may cause diarrhea in high doses.
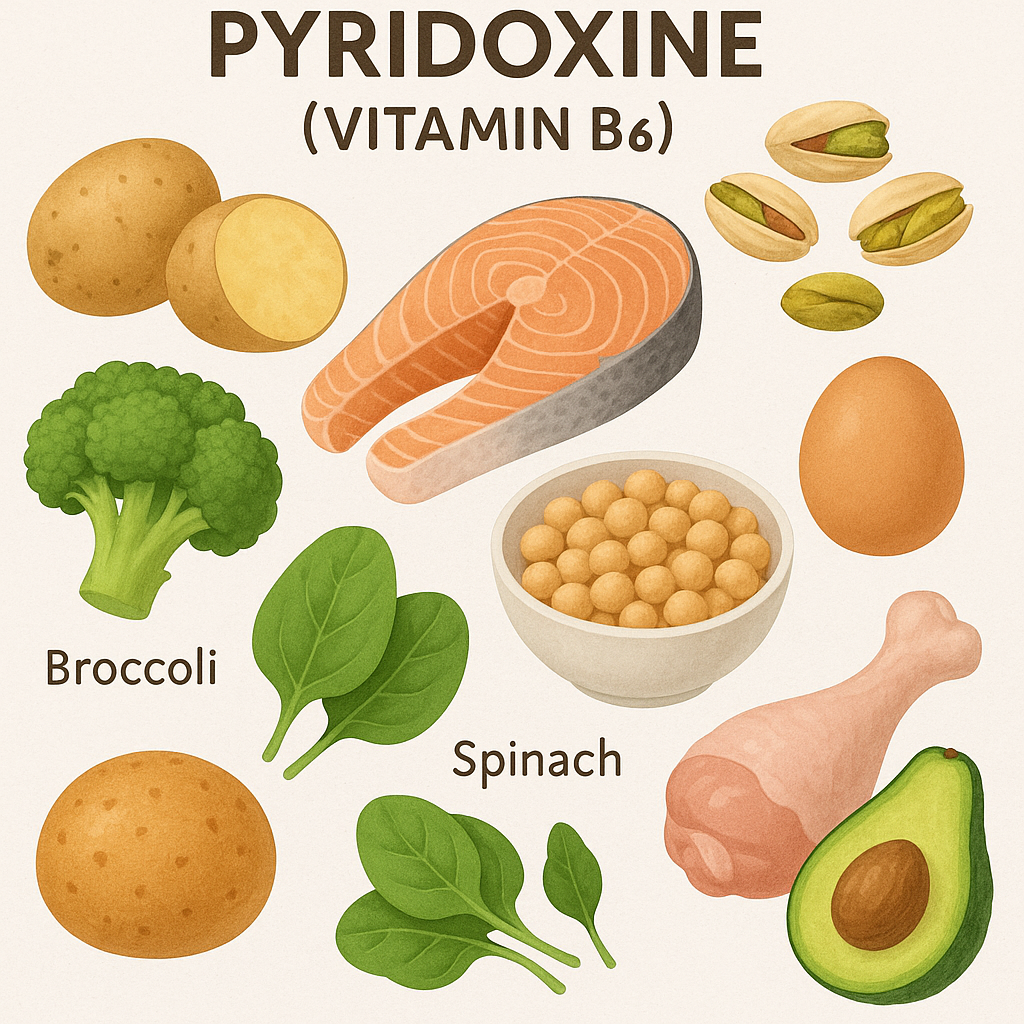
B6 (Pyridoxine)
Functions
- Helps in protein metabolism and neurotransmitter synthesis.
- Essential for hemoglobin formation.
Sources
- Bananas, poultry, fish, potatoes, fortified cereals.
Deficiency Disorders
- Microcytic anemia: Small red blood cells, fatigue.
- Depression, confusion, irritability due to neurotransmitter imbalance.
Toxicity Symptoms
- Nerve damage (neuropathy) in high doses.
B7 (Biotin)
Functions
- Essential for fat and carbohydrate metabolism.
- Supports hair, skin, and nail health.
Sources
- Eggs, nuts, whole grains, liver.
Deficiency Disorders
- Hair loss, brittle nails, skin rashes.
- Neurological symptoms: Depression, hallucinations.
Toxicity Symptoms
- None known, excess is excreted.
B9 (Folic Acid/Folate)
Functions
- Essential for DNA synthesis and cell division.
- Prevents neural tube defects in newborns.
- Supports red blood cell formation.
Sources
- Leafy green vegetables, citrus fruits, beans, fortified cereals.
Deficiency Disorders
- Megaloblastic anemia: Large, immature red blood cells.
- Neural tube defects (Spina bifida) in newborns.
Toxicity Symptoms
- High doses may mask B12 deficiency.
B12 (Cobalamin)
Functions
- Essential for nerve function and red blood cell production.
- Helps in DNA synthesis.
Sources
- Animal products (meat, eggs, dairy, fish).
Deficiency Disorders
- Pernicious anemia: Fatigue, weakness, memory loss.
- Neuropathy: Nerve damage, tingling in hands and feet.
Toxicity Symptoms
- Rare, excess is excreted.
Comparison of Water-Soluble Vitamins
| Vitamin | Function | Sources | Deficiency Disorders | Toxicity Effects |
|---|---|---|---|---|
| Vitamin C | Antioxidant, collagen synthesis, immune support | Citrus fruits, peppers, spinach | Scurvy, weak immunity | Kidney stones, diarrhea |
| B1 (Thiamine) | Energy metabolism, nerve function | Whole grains, pork, nuts | Beriberi, Wernicke-Korsakoff | Rare |
| B2 (Riboflavin) | Skin, eye, nerve health | Dairy, leafy greens | Cracks in lips, swollen tongue | None |
| B3 (Niacin) | DNA repair, energy production | Meat, peanuts, whole grains | Pellagra (4 Ds) | Skin flushing, liver damage |
| B5 (Pantothenic Acid) | Hormone and enzyme synthesis | Meat, avocados, whole grains | Fatigue, irritability | Diarrhea (rare) |
| B6 (Pyridoxine) | Protein metabolism, hemoglobin | Bananas, poultry, fish | Anemia, depression | Nerve damage |
| B7 (Biotin) | Fat and carbohydrate metabolism | Eggs, nuts, whole grains | Hair loss, skin rash | None |
| B9 (Folic Acid) | DNA synthesis, cell growth | Leafy greens, citrus fruits | Megaloblastic anemia, birth defects | Masks B12 deficiency |
| B12 (Cobalamin) | Red blood cell formation, nerve function | Meat, dairy, eggs, fish | Pernicious anemia, nerve damage | Rare |
Role of Water-Soluble Vitamins in Nursing
- Assessment: Nurses check for signs of vitamin deficiencies.
- Education: Teaching patients about dietary sources and the importance of vitamins.
- Supplementation: Administering vitamins when necessary.
- Monitoring for Toxicity: Especially with high doses of Niacin, B6, and Vitamin C.
Vitamin A: Classification, Functions, Sources, and Recommended Dietary Allowance (RDA)
Introduction
Vitamin A is a fat-soluble vitamin essential for vision, immune function, skin health, and cell growth. It exists in two primary forms in the human diet: preformed vitamin A (retinoids) from animal sources and provitamin A (carotenoids) from plant sources. Because it is fat-soluble, vitamin A is stored in the liver and fatty tissues, making toxicity a risk if consumed in excess.
Classification of Vitamin A
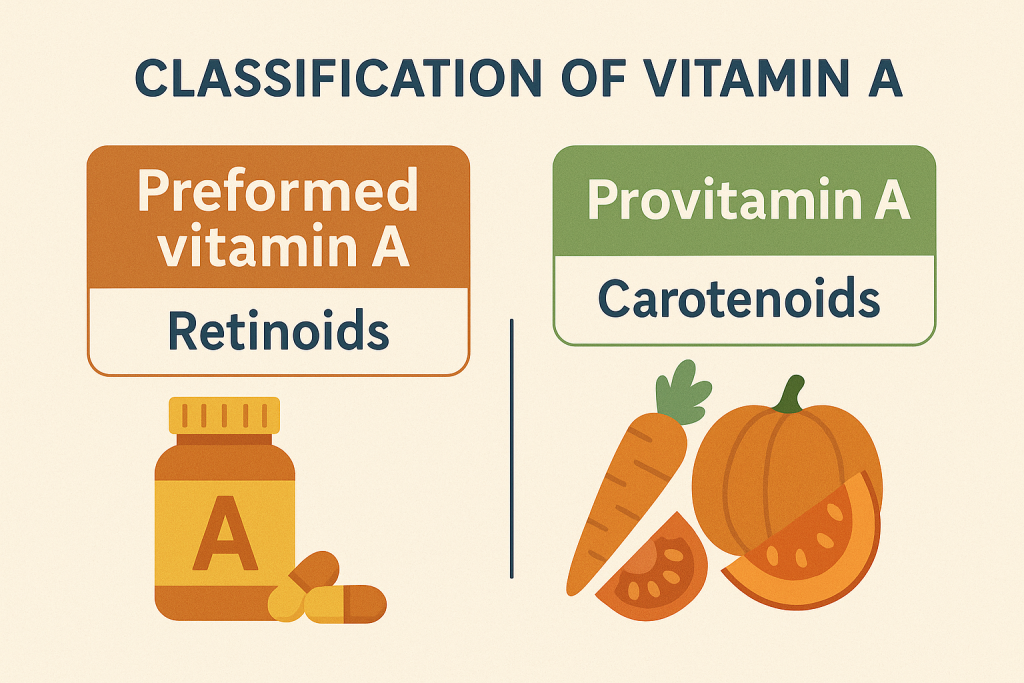
Vitamin A exists in two major forms:
- Preformed Vitamin A (Retinoids)
- Found in animal-based foods.
- Includes Retinol, Retinal, and Retinoic Acid.
- Easily absorbed and directly used by the body.
- Provitamin A (Carotenoids)
- Found in plant-based foods.
- The most important type is Beta-Carotene, which the body converts into retinol.
- Other carotenoids: Alpha-Carotene, Beta-Cryptoxanthin.
Types of Vitamin A Compounds
| Category | Examples | Sources |
|---|---|---|
| Preformed Vitamin A (Active Form) | Retinol, Retinal, Retinoic Acid | Liver, dairy products, fish, eggs |
| Provitamin A (Converted to Active Form in Body) | Beta-Carotene, Alpha-Carotene, Beta-Cryptoxanthin | Carrots, sweet potatoes, green leafy vegetables |
Functions of Vitamin A
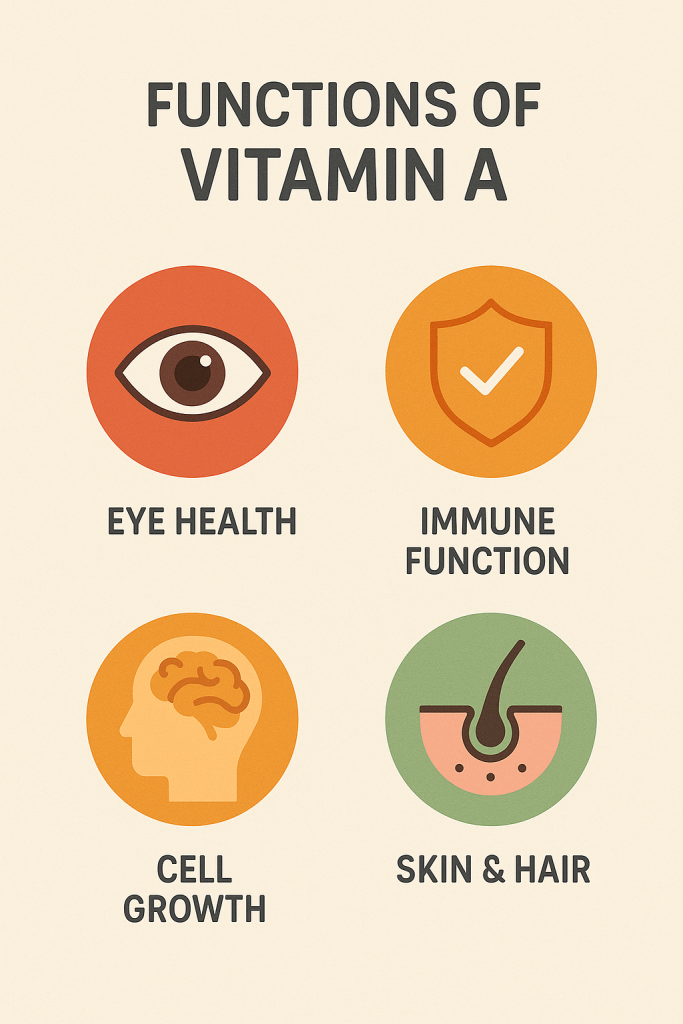
Vitamin A plays a crucial role in various physiological functions:
1. Vision and Eye Health
- Essential for forming rhodopsin, a pigment in the retina necessary for night vision.
- Prevents night blindness and xerophthalmia.
2. Immune System Support
- Helps in the production of white blood cells, which fight infections.
- Supports mucosal barriers in the respiratory and digestive tracts.
3. Growth and Development
- Essential for cell differentiation, ensuring proper organ development in fetuses.
- Supports bone growth and remodeling.
4. Skin and Tissue Health
- Maintains healthy skin and mucous membranes.
- Supports wound healing and reduces the risk of skin infections.
5. Antioxidant Properties (Carotenoids)
- Beta-carotene has antioxidant effects, reducing oxidative stress and protecting against chronic diseases.
6. Reproductive Health
- Supports sperm production in males and fetal development in pregnant women.
Sources of Vitamin A
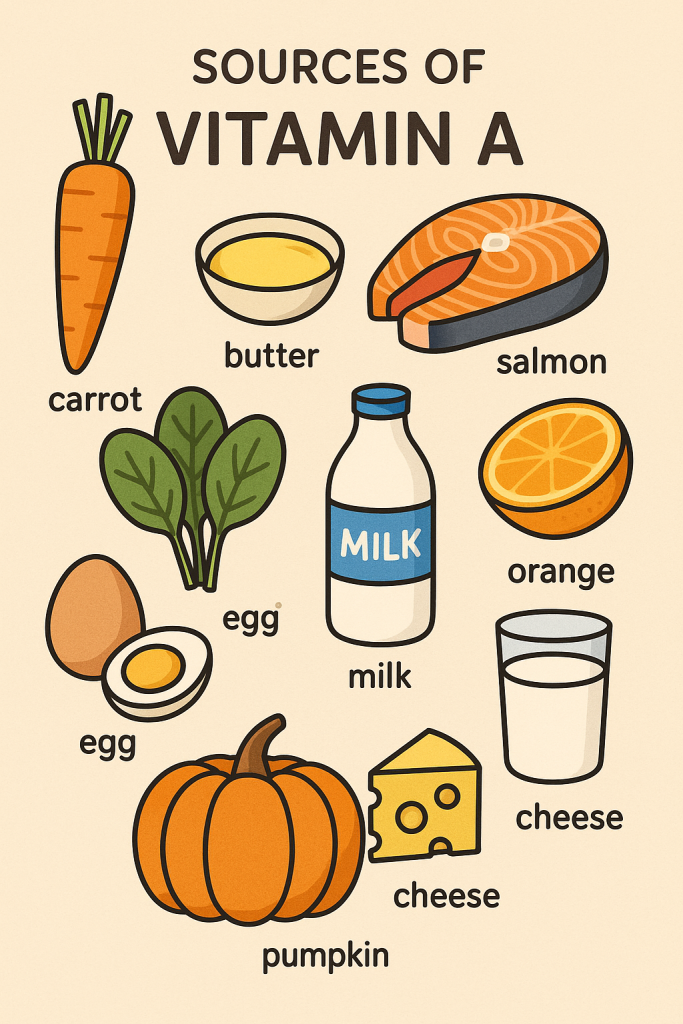
Vitamin A is obtained from both animal-based (preformed vitamin A) and plant-based (provitamin A carotenoids) sources.
Animal Sources (Preformed Vitamin A – Retinol)
- Liver (beef, chicken, cod liver oil) – richest source.
- Dairy products (milk, butter, cheese).
- Egg yolk.
- Fish (salmon, tuna, mackerel).
Plant Sources (Provitamin A – Beta-Carotene)
- Yellow/orange vegetables and fruits:
- Carrots, sweet potatoes, pumpkins, mangoes, apricots.
- Green leafy vegetables:
- Spinach, kale, broccoli.
- Other sources:
- Red bell peppers, papaya.
Fortified Foods
- Many foods, such as milk, margarine, and cereals, are fortified with vitamin A to prevent deficiency.
Recommended Dietary Allowance (RDA) of Vitamin A
The RDA for vitamin A is measured in micrograms of Retinol Activity Equivalents (RAE) because different forms of vitamin A have varying bioavailability.
RDA of Vitamin A (Retinol Activity Equivalents – RAE)
| Age Group | RDA (mcg/day of RAE) | Upper Limit (UL) mcg/day |
|---|---|---|
| Infants (0-6 months) | 400 mcg | 600 mcg |
| Infants (7-12 months) | 500 mcg | 600 mcg |
| Children (1-3 years) | 300 mcg | 600 mcg |
| Children (4-8 years) | 400 mcg | 900 mcg |
| Children (9-13 years) | 600 mcg | 1700 mcg |
| Adolescents (14-18 years, male) | 900 mcg | 2800 mcg |
| Adolescents (14-18 years, female) | 700 mcg | 2800 mcg |
| Adults (male, 19+ years) | 900 mcg | 3000 mcg |
| Adults (female, 19+ years) | 700 mcg | 3000 mcg |
| Pregnant Women (19+ years) | 770 mcg | 3000 mcg |
| Lactating Women (19+ years) | 1300 mcg | 3000 mcg |
Note:
- 1 mcg RAE = 1 mcg Retinol = 12 mcg Beta-Carotene = 24 mcg Alpha-Carotene.
- Excessive intake above the upper limit (UL) can cause toxicity (Hypervitaminosis A).
Vitamin A Deficiency and Toxicity
Deficiency Disorders
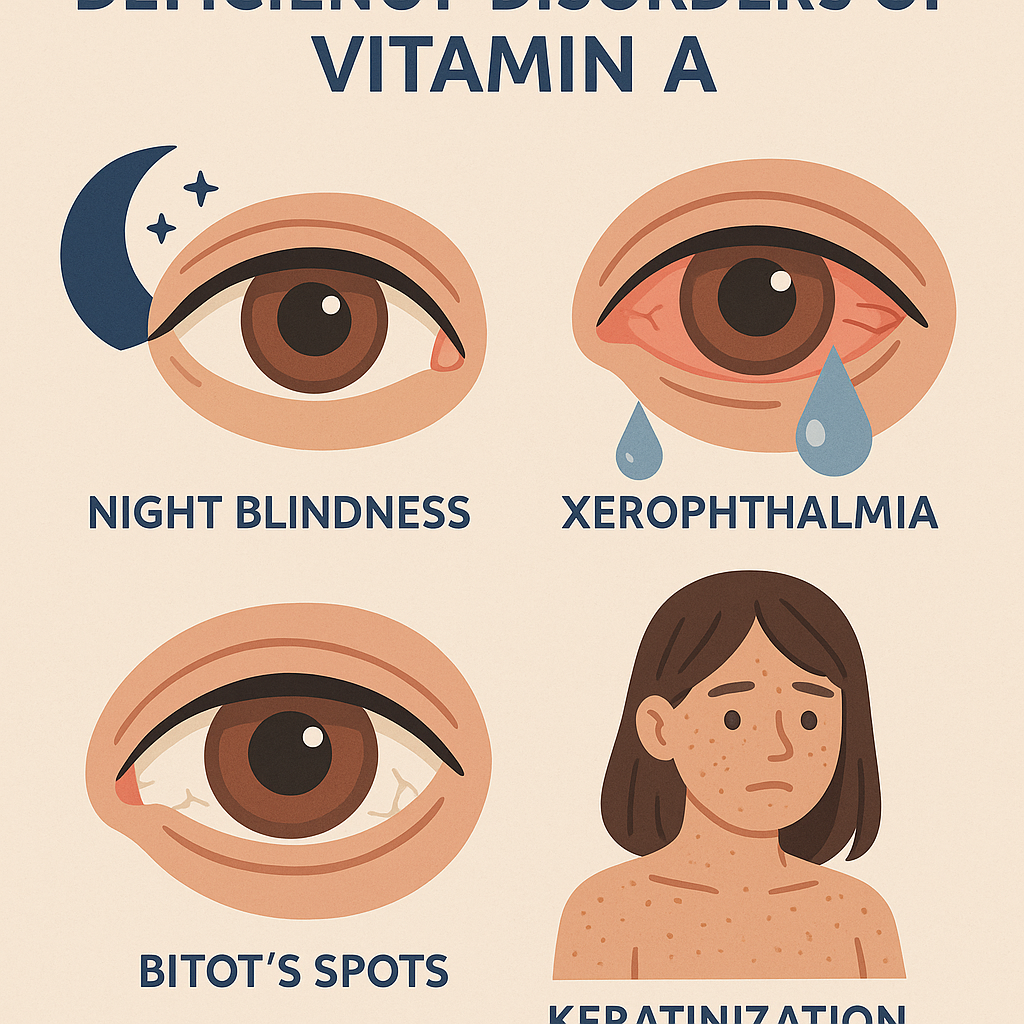
Vitamin A deficiency is a major health problem, particularly in developing countries, leading to:
- Night blindness (Nyctalopia) – Difficulty seeing in dim light.
- Xerophthalmia – Dryness of the conjunctiva and cornea, leading to blindness.
- Bitot’s Spots – Foamy white patches on the eye.
- Increased susceptibility to infections – Due to impaired immune function.
- Growth retardation in children.
- Dry skin and keratinization of epithelial tissues.
Toxicity (Hypervitaminosis A)
Excessive intake of preformed vitamin A (retinol) can cause:
- Acute toxicity: Nausea, vomiting, headache, dizziness, blurred vision.
- Chronic toxicity: Liver damage, osteoporosis, birth defects in pregnant women.
- Teratogenic effects: Birth defects when consumed in high amounts during pregnancy.
Safe Levels of Beta-Carotene
- Beta-carotene from plant sources does not cause toxicity but can lead to carotenemia (yellowing of the skin).
Summary of Vitamin A
| Aspect | Details |
|---|---|
| Classification | Fat-Soluble Vitamin |
| Types | Preformed Vitamin A (Retinol), Provitamin A (Carotenoids – Beta-Carotene) |
| Functions | Vision, immune function, cell growth, skin health, reproduction |
| Sources | Liver, dairy, eggs, fish, carrots, spinach, mangoes |
| RDA | 900 mcg/day (males), 700 mcg/day (females), 770 mcg/day (pregnancy) |
| Deficiency | Night blindness, xerophthalmia, immune dysfunction, growth retardation |
| Toxicity | Liver damage, osteoporosis, birth defects (pregnant women), carotenemia (from excess beta-carotene) |
Vitamin D: Classification, Functions, Sources, and Recommended Dietary Allowance (RDA)
Introduction
Vitamin D is a fat-soluble vitamin essential for calcium and phosphorus metabolism, promoting bone health, immune function, and muscle function. It is unique because it can be synthesized in the skin when exposed to sunlight (UV rays). However, dietary sources and supplements are necessary for those with limited sun exposure.
Classification of Vitamin D
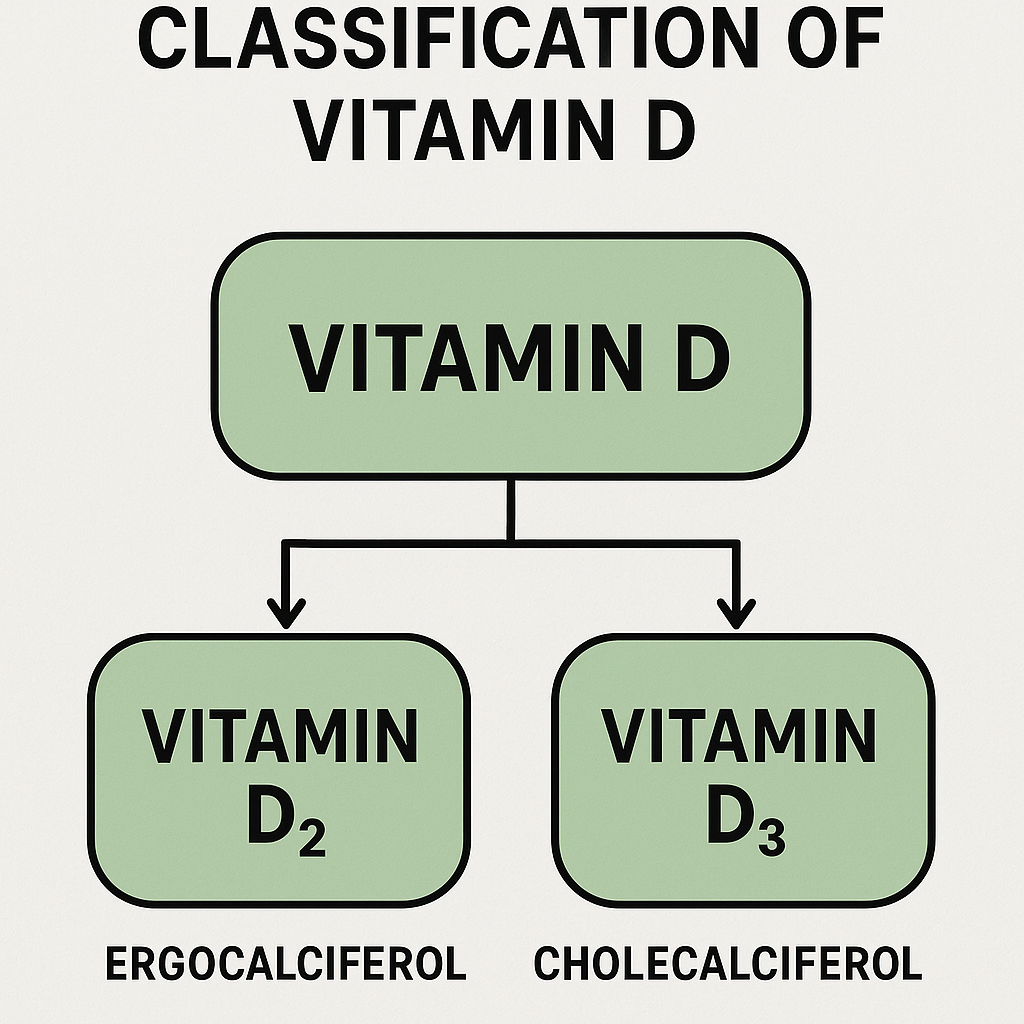
Vitamin D exists in two primary forms:
- Vitamin D2 (Ergocalciferol)
- Found in plant-based foods and fortified products.
- Less effective than Vitamin D3 in raising blood levels.
- Vitamin D3 (Cholecalciferol)
- Found in animal sources and produced in human skin from sunlight.
- More potent and has a longer half-life in the body.
Types of Vitamin D Compounds
| Category | Examples | Sources |
|---|---|---|
| Natural Form (Sunlight, Animal Sources) | Vitamin D3 (Cholecalciferol) | Sunlight, fish, egg yolks, dairy |
| Synthetic/Plant-Based Form | Vitamin D2 (Ergocalciferol) | Mushrooms, fortified foods |
Functions of Vitamin D
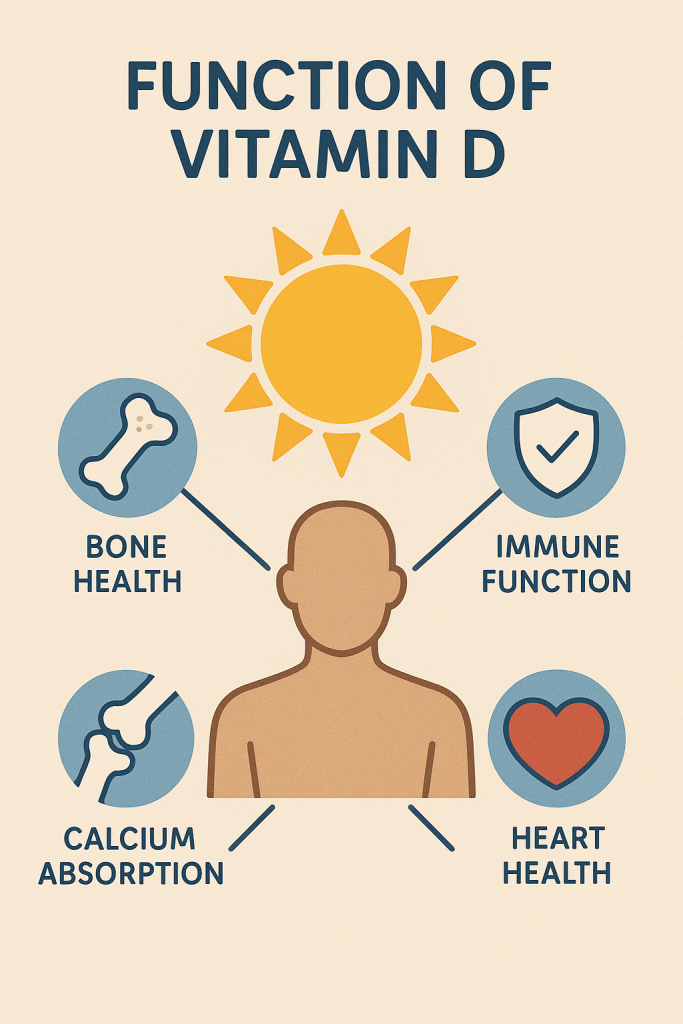
Vitamin D is essential for multiple physiological functions, including:
1. Bone and Teeth Health
- Regulates calcium and phosphorus metabolism.
- Enhances calcium absorption in the intestines.
- Prevents bone diseases like rickets (children) and osteomalacia (adults).
2. Immune System Support
- Enhances immune response to infections.
- Reduces the risk of autoimmune diseases.
3. Muscle Function
- Prevents muscle weakness and reduces fall risk in elderly individuals.
4. Cardiovascular Health
- Helps regulate blood pressure and supports heart function.
5. Neurological and Mental Health
- Plays a role in brain development and may help reduce the risk of depression and cognitive decline.
Sources of Vitamin D
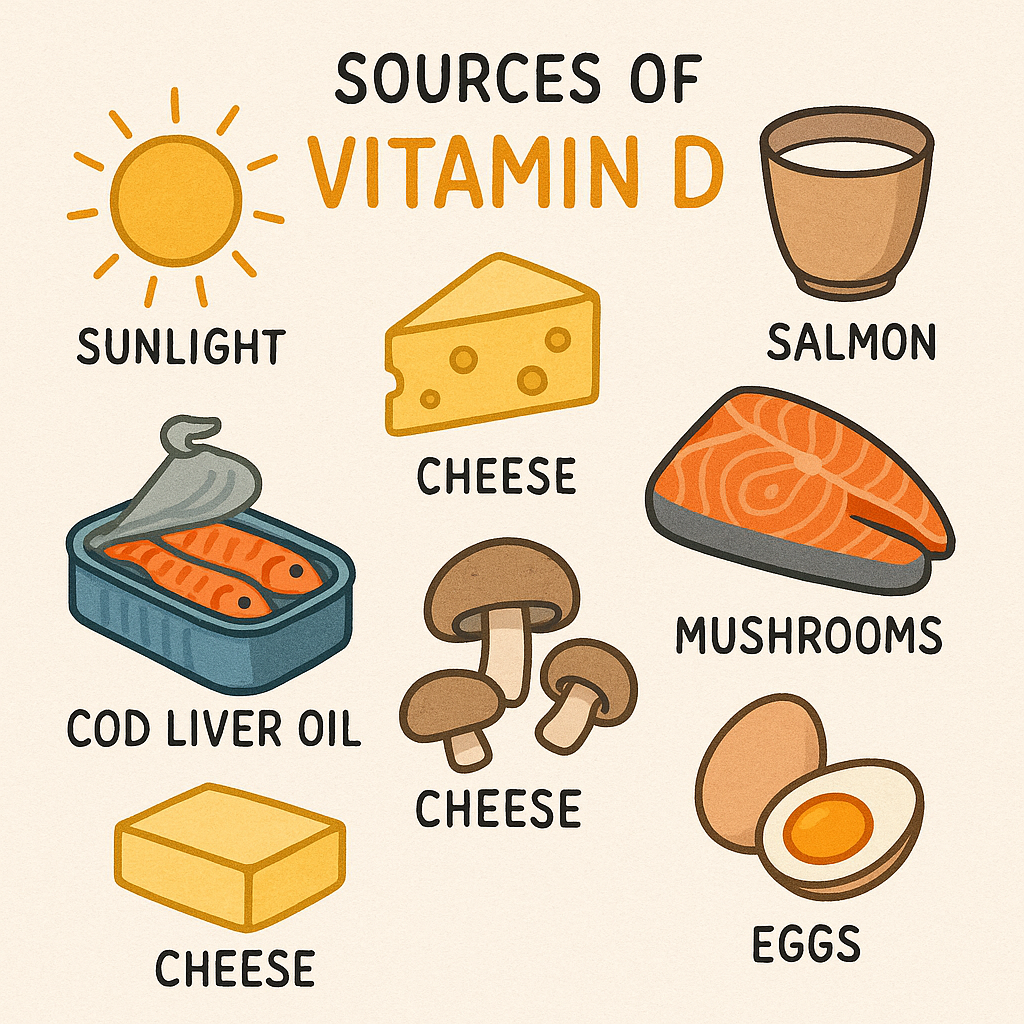
Vitamin D is obtained through sunlight exposure, food sources, and supplements.
Natural Sources
- Sunlight (Primary Source)
- UV rays convert 7-dehydrocholesterol in the skin to Vitamin D3.
- Requires 15–30 minutes of sun exposure on the skin (without sunscreen) for optimal production.
- Animal-Based Food Sources (Rich in Vitamin D3)
- Fatty fish (salmon, mackerel, tuna, sardines).
- Fish liver oils (cod liver oil).
- Egg yolks.
- Dairy products (milk, cheese, butter).
- Plant-Based and Fortified Food Sources (Rich in Vitamin D2)
- Mushrooms (exposed to sunlight).
- Fortified foods (milk, orange juice, cereals, soy products).
Vitamin D Supplements
- Recommended for individuals with low sun exposure (elderly, indoor workers, people in colder climates).
- Available as Vitamin D2 (Ergocalciferol) and Vitamin D3 (Cholecalciferol) (preferred form).
Recommended Dietary Allowance (RDA) of Vitamin D
The RDA for Vitamin D is measured in International Units (IU) or micrograms (mcg).
| Age Group | RDA (mcg/day or IU/day) | Upper Limit (UL) (mcg/day or IU/day) |
|---|---|---|
| Infants (0-6 months) | 10 mcg (400 IU) | 25 mcg (1000 IU) |
| Infants (7-12 months) | 10 mcg (400 IU) | 38 mcg (1500 IU) |
| Children (1-3 years) | 15 mcg (600 IU) | 63 mcg (2500 IU) |
| Children (4-8 years) | 15 mcg (600 IU) | 75 mcg (3000 IU) |
| Adolescents (9-18 years) | 15 mcg (600 IU) | 100 mcg (4000 IU) |
| Adults (19-50 years) | 15 mcg (600 IU) | 100 mcg (4000 IU) |
| Adults (51-70 years) | 15 mcg (600 IU) | 100 mcg (4000 IU) |
| Adults (71+ years) | 20 mcg (800 IU) | 100 mcg (4000 IU) |
| Pregnant Women | 15 mcg (600 IU) | 100 mcg (4000 IU) |
| Lactating Women | 15 mcg (600 IU) | 100 mcg (4000 IU) |
Note:
- 1 mcg Vitamin D = 40 IU.
- Excess intake beyond upper limit (UL) can lead to toxicity.
Vitamin D Deficiency and Toxicity
Deficiency Disorders
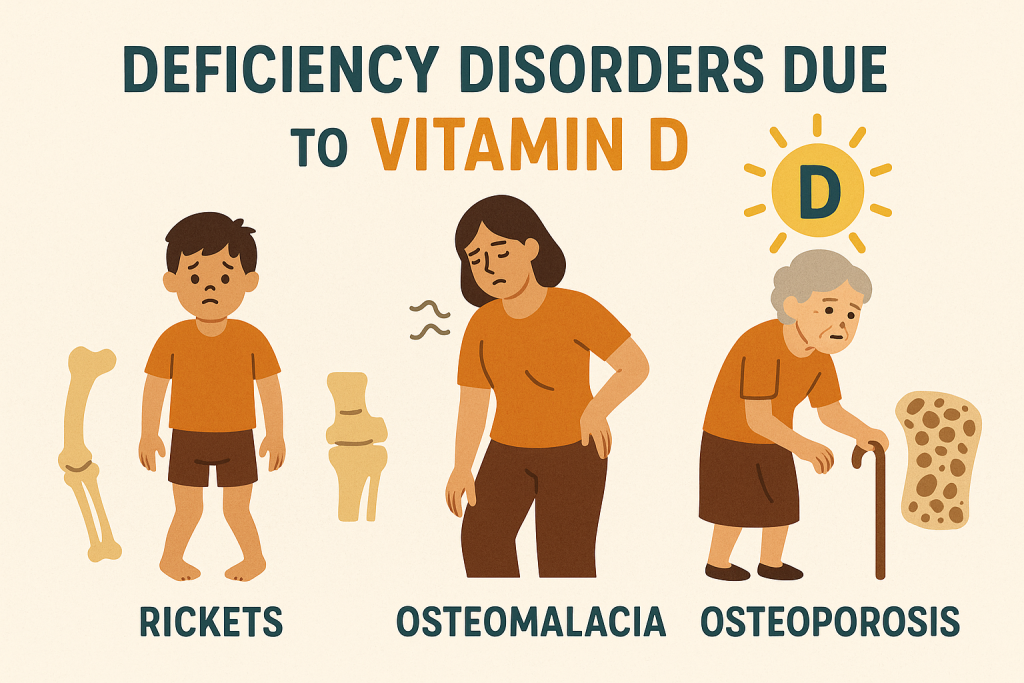
Vitamin D deficiency is common in elderly individuals, people with limited sun exposure, and those with darker skin. It can lead to:
- Children
- Rickets – Weak, soft bones leading to bowed legs and skeletal deformities.
- Delayed growth and dental problems.
- Adults
- Osteomalacia – Soft bones, muscle weakness, and chronic pain.
- Osteoporosis – Reduced bone density, increased risk of fractures.
- Other Effects
- Increased risk of autoimmune diseases, hypertension, and cardiovascular disease.
- Weakened immune function, leading to frequent infections.
- Depression and cognitive decline.
Toxicity (Hypervitaminosis D)
Excessive Vitamin D intake from supplements can cause:
- Hypercalcemia (High Blood Calcium Levels)
- Nausea, vomiting, frequent urination.
- Kidney stones and kidney damage.
- Cardiovascular Issues
- Calcification of arteries, increasing heart disease risk.
- Neurological Symptoms
- Weakness, confusion, and fatigue.
Comparison of Vitamin D Forms
| Aspect | Vitamin D2 (Ergocalciferol) | Vitamin D3 (Cholecalciferol) |
|---|---|---|
| Source | Plant-based, fungi, fortified foods | Animal-based, skin synthesis, supplements |
| Absorption | Less effective | More effective |
| Stability | Less stable | More stable |
| Usage in Supplements | Found in some vegetarian/vegan supplements | Found in most standard supplements |
Role of Vitamin D in Nursing and Healthcare
Nurses play a vital role in ensuring proper Vitamin D intake in patients through:
- Assessment of Deficiency
- Checking for signs of rickets, osteomalacia, bone pain, muscle weakness.
- Blood tests for 25-hydroxyvitamin D levels.
- Patient Education
- Advising on safe sun exposure for natural Vitamin D synthesis.
- Encouraging dietary sources rich in Vitamin D.
- Recommending supplements when necessary.
- Monitoring for Toxicity
- Ensuring that supplement doses are within the safe range.
- Educating about the risks of excess Vitamin D intake.
Summary of Vitamin D
| Aspect | Details |
|---|---|
| Classification | Fat-Soluble Vitamin |
| Types | Vitamin D2 (Ergocalciferol), Vitamin D3 (Cholecalciferol) |
| Functions | Bone health, immune support, muscle function, cardiovascular health |
| Sources | Sunlight, fatty fish, dairy, mushrooms, fortified foods |
| RDA | 600 IU/day (15 mcg) for adults; 800 IU (20 mcg) for elderly |
| Deficiency | Rickets, osteomalacia, osteoporosis, weak immunity |
| Toxicity | Hypercalcemia, kidney damage, cardiovascular issues |
Vitamin E: Classification, Functions, Sources, and Recommended Dietary Allowance (RDA)
Introduction
Vitamin E is a fat-soluble vitamin with powerful antioxidant properties that protect cells from oxidative damage. It plays a crucial role in immune function, skin health, and cardiovascular protection. Unlike some other fat-soluble vitamins, Vitamin E is not stored in the body in large amounts, so a regular dietary intake is essential.
Classification of Vitamin E
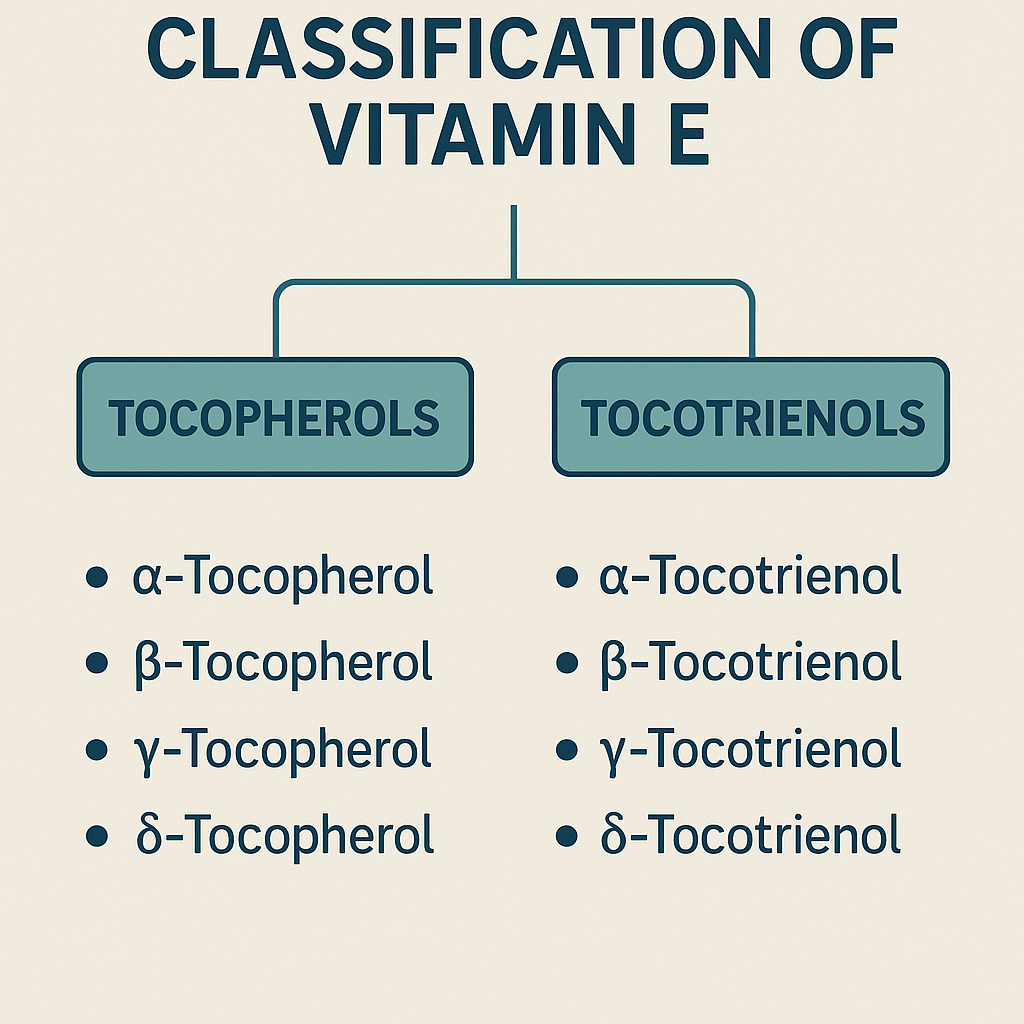
Vitamin E is a group of eight structurally similar compounds, classified into:
1. Tocopherols (Biologically Active Forms)
- Alpha-tocopherol (most active and commonly found in supplements).
- Beta-tocopherol.
- Gamma-tocopherol.
- Delta-tocopherol.
2. Tocotrienols
- Alpha-tocotrienol.
- Beta-tocotrienol.
- Gamma-tocotrienol.
- Delta-tocotrienol.
Among these, alpha-tocopherol is the most biologically significant and is considered the primary active form in the human body.
| Category | Examples | Biological Role |
|---|---|---|
| Tocopherols | Alpha, Beta, Gamma, Delta | Strong antioxidants, cell membrane protection |
| Tocotrienols | Alpha, Beta, Gamma, Delta | Neuroprotective, cardiovascular benefits |
Functions of Vitamin E
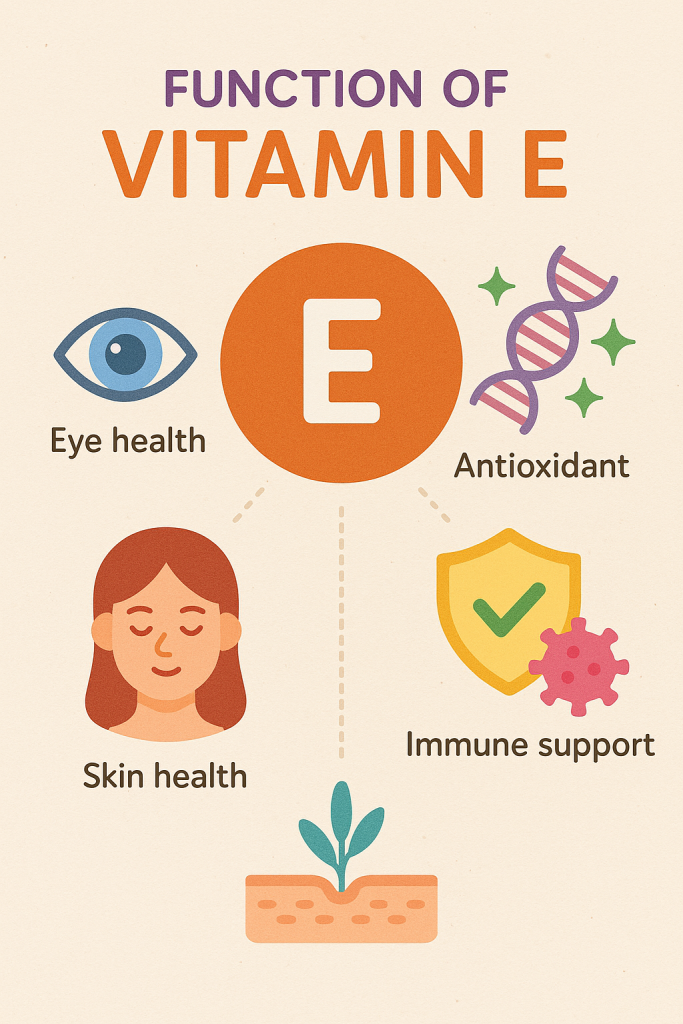
Vitamin E has various physiological and biochemical functions in the body:
1. Antioxidant Protection
- Protects cell membranes from oxidative stress.
- Prevents damage caused by free radicals, reducing the risk of chronic diseases.
2. Immune System Support
- Enhances immune response and protects against infections.
- Helps in T-cell function (a type of white blood cell).
3. Skin and Hair Health
- Promotes wound healing and reduces scars.
- Prevents premature skin aging by neutralizing UV damage.
- Helps in moisturizing skin and reducing dryness.
4. Cardiovascular Health
- Prevents oxidation of LDL cholesterol, reducing the risk of atherosclerosis and heart disease.
- Helps maintain healthy blood circulation.
5. Neurological Health
- Supports brain function and may help in Alzheimer’s disease prevention.
- Helps prevent nerve damage and muscle weakness.
6. Anti-Inflammatory Role
- Reduces chronic inflammation, benefiting people with arthritis and autoimmune diseases.
Sources of Vitamin E
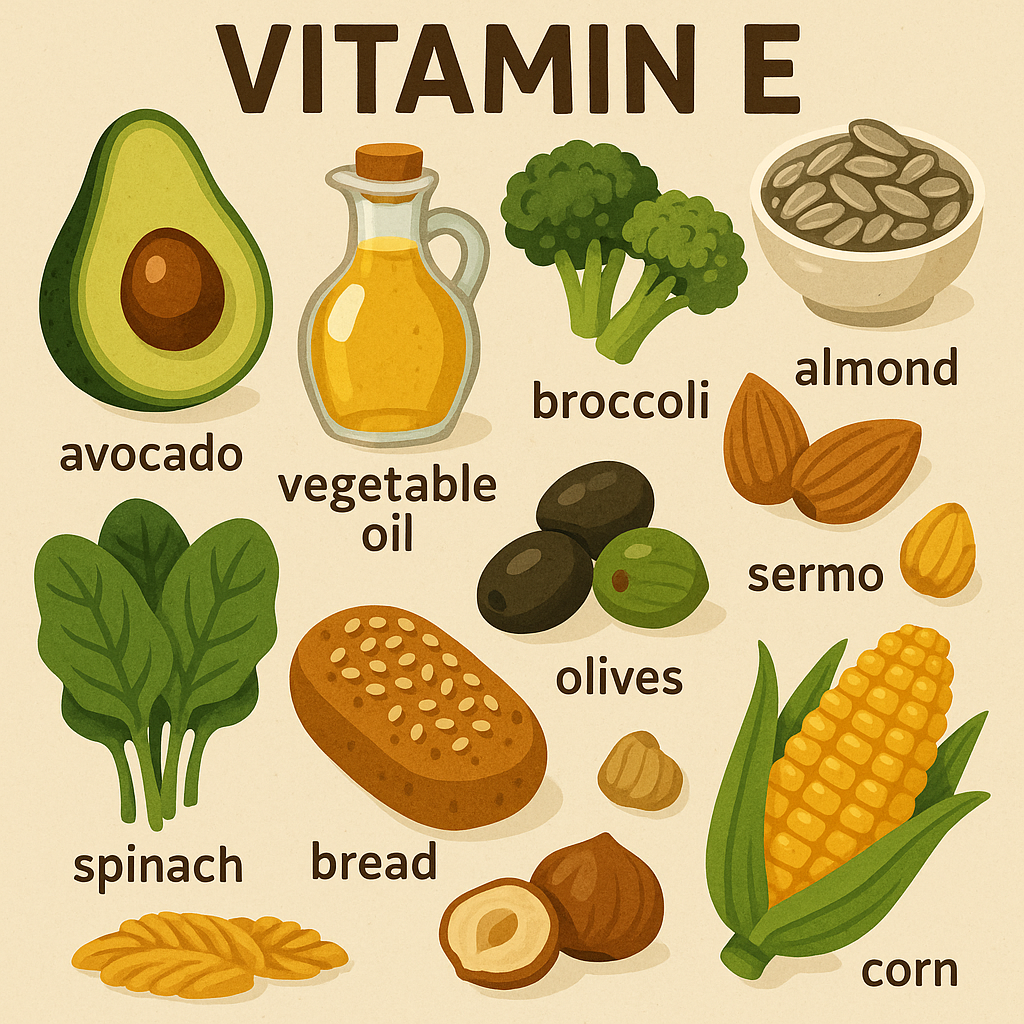
Vitamin E is primarily obtained from plant-based foods, particularly nuts, seeds, and vegetable oils.
Rich Natural Sources
1. Plant-Based Sources
- Nuts and Seeds: Almonds, sunflower seeds, hazelnuts, peanuts.
- Vegetable Oils: Sunflower oil, safflower oil, wheat germ oil, olive oil.
- Green Leafy Vegetables: Spinach, kale, Swiss chard, broccoli.
- Fruits: Avocados, mangoes, kiwis.
2. Animal-Based Sources
- Egg yolk.
- Liver.
- Fatty fish (salmon, trout).
3. Fortified Foods
- Breakfast cereals.
- Margarine.
- Plant-based milk (soy, almond, coconut).
Vitamin E Supplements
- Synthetic Vitamin E (DL-alpha-tocopherol) is commonly found in multivitamins.
- Natural Vitamin E (D-alpha-tocopherol) is more bioavailable and effective.
Recommended Dietary Allowance (RDA) of Vitamin E
The RDA for Vitamin E is measured in milligrams (mg) of alpha-tocopherol equivalents (α-TE).
| Age Group | RDA (mg/day of α-TE) | Upper Limit (UL) (mg/day of α-TE) |
|---|---|---|
| Infants (0-6 months) | 4 mg | Not established |
| Infants (7-12 months) | 5 mg | Not established |
| Children (1-3 years) | 6 mg | 200 mg |
| Children (4-8 years) | 7 mg | 300 mg |
| Children (9-13 years) | 11 mg | 600 mg |
| Adolescents (14-18 years, male and female) | 15 mg | 800 mg |
| Adults (19+ years, male and female) | 15 mg | 1000 mg |
| Pregnant Women | 15 mg | 1000 mg |
| Lactating Women | 19 mg | 1000 mg |
Note:
- 1 mg of alpha-tocopherol = 1.49 IU (International Units).
- The upper limit (UL) is based on avoiding excessive intake that may cause toxicity.
Vitamin E Deficiency and Toxicity
Deficiency Disorders
Vitamin E deficiency is rare but can occur in individuals with:
- Fat malabsorption disorders (Cystic fibrosis, Crohn’s disease, liver disease).
- Premature infants (low birth weight).
- Genetic conditions affecting Vitamin E transport.
Symptoms of Deficiency
- Neurological problems (poor coordination, muscle weakness).
- Peripheral neuropathy (numbness, tingling in hands and feet).
- Weakened immune function (frequent infections).
- Vision problems (retinal degeneration).
- Hemolytic anemia (red blood cell destruction).
Toxicity (Hypervitaminosis E)
Excessive intake of Vitamin E, especially through supplements, can lead to:
Symptoms of Toxicity
- Increased bleeding tendency (interferes with Vitamin K).
- Gastrointestinal issues (nausea, diarrhea, stomach cramps).
- Fatigue and weakness.
- Headaches and blurred vision.
Safe Intake Recommendations
- Avoid exceeding the UL (1000 mg/day) from supplements.
- Natural food sources are safe and unlikely to cause toxicity.
Comparison of Vitamin E Forms
| Aspect | Tocopherols | Tocotrienols |
|---|---|---|
| Common Forms | Alpha, Beta, Gamma, Delta | Alpha, Beta, Gamma, Delta |
| Function | Antioxidant, immune support | Neuroprotective, cardiovascular health |
| Sources | Nuts, seeds, vegetable oils | Rice bran, palm oil, barley |
| Bioavailability | High | Lower than tocopherols |
| Use in Supplements | Mostly Alpha-Tocopherol | Less common |
Role of Vitamin E in Nursing and Healthcare
Nurses play a crucial role in preventing and managing Vitamin E deficiency and toxicity:
- Assessing Nutritional Status
- Identifying signs of deficiency (neuropathy, muscle weakness, vision problems).
- Evaluating dietary intake of Vitamin E-rich foods.
- Educating Patients
- Encouraging a balanced diet with Vitamin E-rich foods.
- Advising against excessive supplement use, especially in patients taking anticoagulants.
- Monitoring at-Risk Patients
- Premature infants, elderly, and those with malabsorption disorders.
- Patients on blood thinners (warfarin, aspirin) to prevent excessive bleeding.
- Managing Toxicity
- Stopping high-dose supplementation in case of bleeding tendencies.
- Supporting patients with gastrointestinal symptoms.
Summary of Vitamin E
| Aspect | Details |
|---|---|
| Classification | Fat-Soluble Vitamin |
| Types | Tocopherols (Alpha, Beta, Gamma, Delta), Tocotrienols |
| Functions | Antioxidant, immune support, skin health, cardiovascular health |
| Sources | Nuts, seeds, vegetable oils, green leafy vegetables, fortified foods |
| RDA | 15 mg/day for adults, 19 mg/day for lactating women |
| Deficiency | Neuropathy, muscle weakness, vision problems, weakened immunity |
| Toxicity | Bleeding disorders, fatigue, nausea, gastrointestinal issues |
Vitamin K: Classification, Functions, Sources, and Recommended Dietary Allowance (RDA)
Introduction
Vitamin K is a fat-soluble vitamin essential for blood clotting (coagulation), bone metabolism, and cardiovascular health. It plays a crucial role in the activation of clotting factors and helps in preventing excessive bleeding. Unlike other fat-soluble vitamins, Vitamin K is not stored in large amounts in the body, so a regular dietary intake is necessary.
Classification of Vitamin K
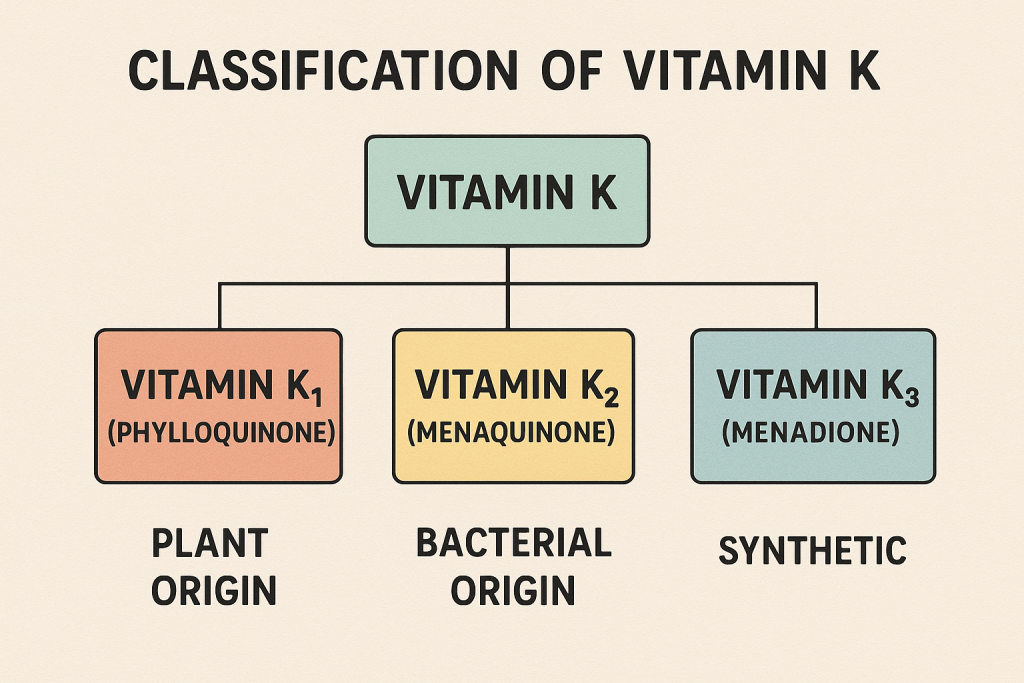
Vitamin K exists in three primary forms:
1. Vitamin K1 (Phylloquinone)
- Found in plant-based foods, especially leafy green vegetables.
- Primary dietary source of Vitamin K.
- Essential for blood clotting.
2. Vitamin K2 (Menaquinones)
- Found in fermented foods and animal-based products.
- Produced by gut bacteria in the intestine.
- Plays a role in bone metabolism and cardiovascular health.
3. Vitamin K3 (Menadione)
- A synthetic form of Vitamin K.
- Used in some medical treatments but not recommended due to potential toxicity.
Comparison of Vitamin K Forms
| Category | Examples | Sources | Main Functions |
|---|---|---|---|
| Vitamin K1 | Phylloquinone | Leafy greens (spinach, kale), broccoli | Blood clotting |
| Vitamin K2 | Menaquinones (MK-4 to MK-13) | Fermented foods, dairy, meat, gut bacteria | Bone health, cardiovascular protection |
| Vitamin K3 | Menadione (Synthetic) | Supplements, medical use | Used in treatments, but toxic in excess |
Functions of Vitamin K
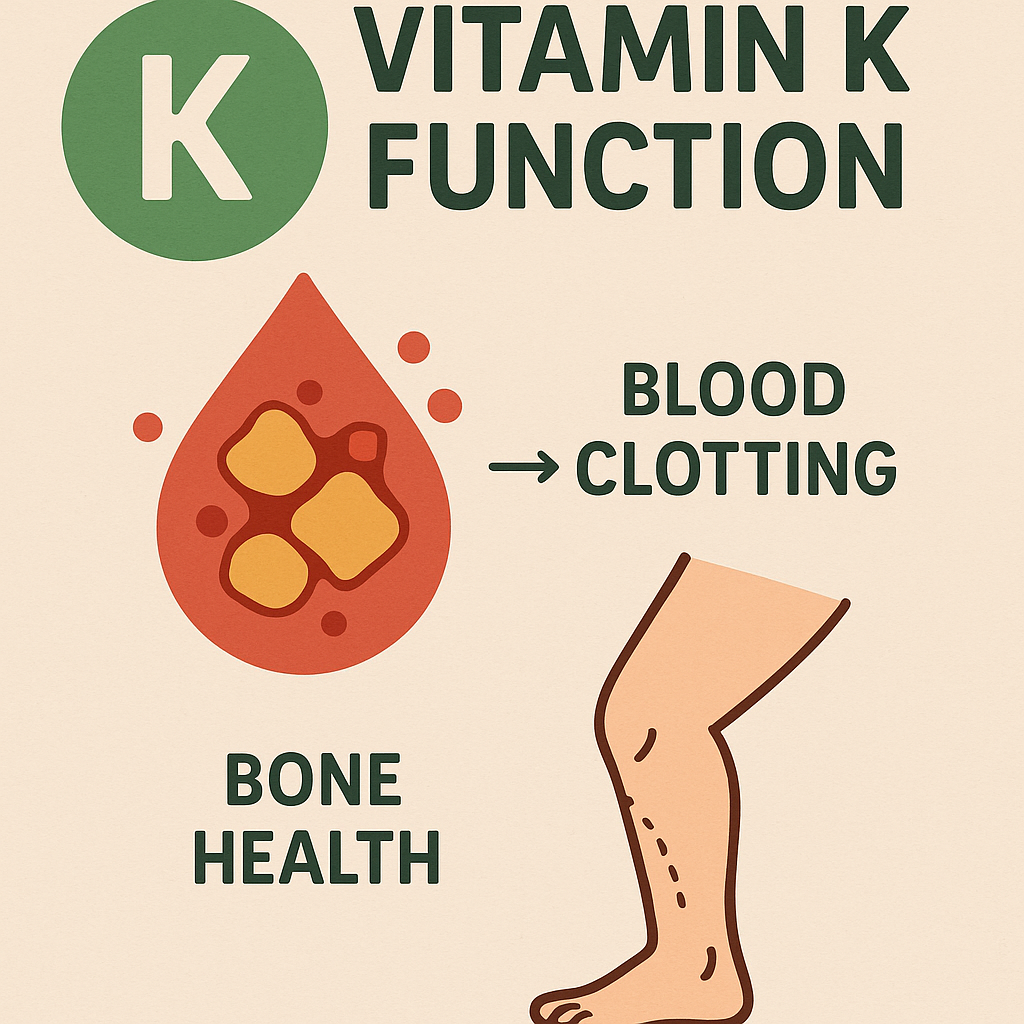
Vitamin K plays an essential role in various physiological functions:
1. Blood Clotting (Coagulation)
- Required for the activation of clotting factors (II, VII, IX, X) in the coagulation cascade.
- Prevents excessive bleeding and hemorrhages.
2. Bone Health and Calcium Metabolism
- Activates osteocalcin, a protein involved in bone formation.
- Helps in calcium deposition in bones, preventing osteoporosis.
- Reduces the risk of fractures in older adults.
3. Cardiovascular Protection
- Prevents calcification of blood vessels, reducing the risk of heart disease.
- Helps regulate blood pressure.
4. Brain Health
- May play a role in preventing cognitive decline and neurodegenerative diseases.
Sources of Vitamin K

Vitamin K is obtained through dietary sources and gut bacteria production.
Natural Sources
1. Plant-Based Sources (Rich in Vitamin K1 – Phylloquinone)
- Leafy Green Vegetables: Spinach, kale, collard greens, Swiss chard.
- Cruciferous Vegetables: Broccoli, Brussels sprouts, cabbage.
- Vegetable Oils: Soybean oil, canola oil, olive oil.
2. Animal-Based and Fermented Sources (Rich in Vitamin K2 – Menaquinone)
- Dairy Products: Cheese, butter.
- Meat and Eggs: Liver, chicken, egg yolks.
- Fermented Foods: Natto (fermented soybeans), sauerkraut, yogurt.
Gut Microbiota Contribution
- Intestinal bacteria synthesize Vitamin K2, but the amount produced is insufficient to meet daily needs.
Vitamin K Supplements
- Found in multivitamins and individual Vitamin K supplements.
- Available in Vitamin K1 (Phylloquinone) and Vitamin K2 (MK-4, MK-7 forms).
Recommended Dietary Allowance (RDA) of Vitamin K
The RDA for Vitamin K is measured in micrograms (mcg/day).
| Age Group | RDA (mcg/day) | Upper Limit (UL) |
|---|---|---|
| Infants (0-6 months) | 2.0 mcg | Not established |
| Infants (7-12 months) | 2.5 mcg | Not established |
| Children (1-3 years) | 30 mcg | Not established |
| Children (4-8 years) | 55 mcg | Not established |
| Children (9-13 years) | 60 mcg | Not established |
| Adolescents (14-18 years, male and female) | 75 mcg | Not established |
| Adults (19+ years, male) | 120 mcg | Not established |
| Adults (19+ years, female) | 90 mcg | Not established |
| Pregnant Women | 90 mcg | Not established |
| Lactating Women | 90 mcg | Not established |
Note:
- There is no established upper limit (UL) for Vitamin K because excess amounts are not toxic in healthy individuals.
- People on blood-thinning medications (e.g., Warfarin) should maintain consistent Vitamin K intake.
Vitamin K Deficiency and Toxicity
Deficiency Disorders
Vitamin K deficiency is rare in healthy adults but can occur in:
- Newborns (low Vitamin K at birth).
- Individuals with fat malabsorption disorders (Cystic fibrosis, Crohn’s disease, liver disease).
- Long-term antibiotic use, which disrupts gut bacteria production.
Symptoms of Deficiency
- Excessive bleeding (hemorrhage) due to impaired clotting.
- Easy bruising and nosebleeds.
- Osteoporosis and bone fractures in elderly individuals.
Newborn Vitamin K Deficiency
- Newborns are at risk of Vitamin K deficiency bleeding (VKDB).
- To prevent this, a Vitamin K injection is given at birth.
Toxicity (Hypervitaminosis K)
Vitamin K toxicity is rare because excess amounts are excreted in bile. However, synthetic Vitamin K3 (Menadione) can cause toxicity.
Symptoms of Toxicity (Menadione Overdose)
- Hemolytic anemia (red blood cell destruction).
- Jaundice (yellowing of skin and eyes).
- Liver toxicity.
Comparison of Vitamin K Forms
| Aspect | Vitamin K1 (Phylloquinone) | Vitamin K2 (Menaquinones – MK-4, MK-7) | Vitamin K3 (Menadione) |
|---|---|---|---|
| Sources | Leafy greens, vegetable oils | Fermented foods, dairy, liver | Synthetic form (not recommended) |
| Function | Blood clotting | Bone health, cardiovascular protection | Medical use (but toxic) |
| Storage | Short-lived in the liver | Long-lasting in tissues | Can cause toxicity |
| Toxicity | Low risk | Low risk | High risk |
Role of Vitamin K in Nursing and Healthcare
Nurses play a crucial role in monitoring Vitamin K intake and preventing deficiencies:
1. Assessing Patients at Risk
- Newborns, elderly, individuals with malabsorption disorders.
- Patients on blood thinners (Warfarin, Heparin).
2. Administering Vitamin K Supplements
- Vitamin K injections for newborns to prevent VKDB.
- Oral or injectable Vitamin K for patients with deficiency-related bleeding.
3. Educating Patients
- Encouraging a diet rich in leafy greens and fermented foods.
- Advising patients on Warfarin to maintain consistent Vitamin K intake to prevent fluctuations in blood clotting.
4. Managing Vitamin K Toxicity
- Identifying signs of synthetic Vitamin K overdose (hemolysis, jaundice).
- Adjusting doses of blood-thinning medications if necessary.
Summary of Vitamin K
| Aspect | Details |
|---|---|
| Classification | Fat-Soluble Vitamin |
| Types | Vitamin K1 (Phylloquinone), Vitamin K2 (Menaquinones), Vitamin K3 (Menadione – synthetic) |
| Functions | Blood clotting, bone health, cardiovascular protection |
| Sources | Leafy greens, vegetable oils, fermented foods, dairy, liver |
| RDA | 90 mcg/day (women), 120 mcg/day (men) |
| Deficiency | Excessive bleeding, easy bruising, osteoporosis |
| Toxicity | Rare (except for synthetic Vitamin K3) |
Thiamine (Vitamin B1): Classification, Functions, Sources, and Recommended Dietary Allowance (RDA)
Introduction
Thiamine (Vitamin B1) is a water-soluble vitamin that plays a crucial role in energy metabolism, nerve function, and muscle activity. Since it is not stored in large amounts in the body, a continuous dietary intake is necessary. Deficiency can lead to severe neurological and cardiovascular disorders such as beriberi and Wernicke-Korsakoff syndrome.
Classification of Thiamine (Vitamin B1)
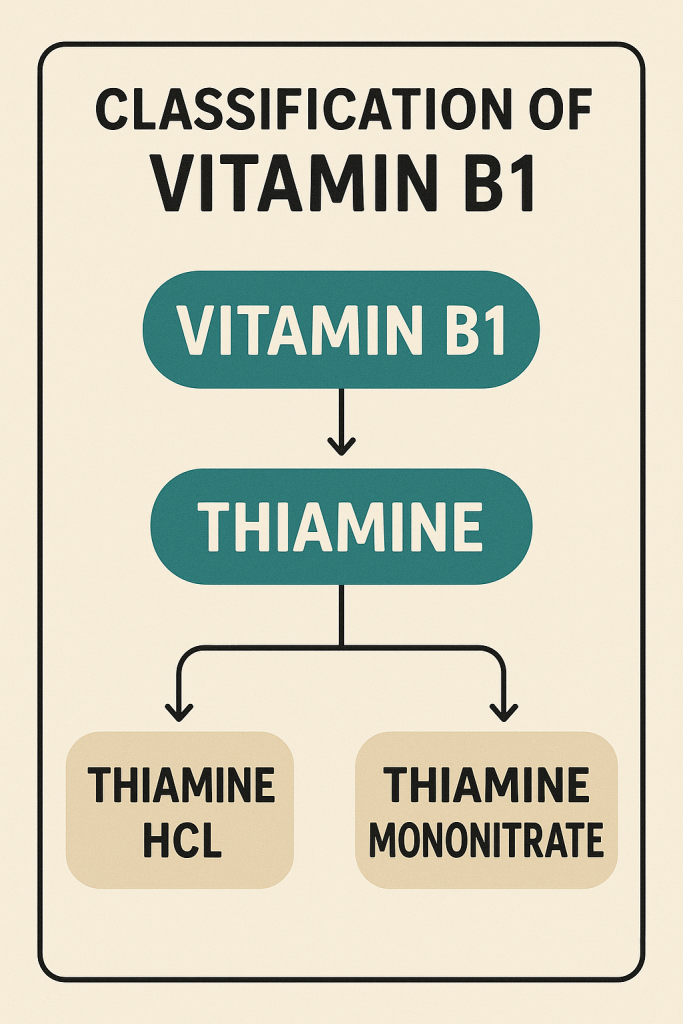
Vitamin B1 is classified based on its active and coenzyme forms:
1. Free Thiamine
- Found in plant-based foods (grains, legumes, nuts).
- Less biologically active than phosphorylated forms.
2. Phosphorylated (Coenzyme) Forms
- Thiamine pyrophosphate (TPP) – the most active form, crucial for energy metabolism.
- Thiamine monophosphate (TMP) and thiamine triphosphate (TTP) – play roles in nerve function.
| Category | Examples | Biological Role |
|---|---|---|
| Free Thiamine | Found in food | Requires phosphorylation for activation |
| Thiamine Pyrophosphate (TPP) | Active coenzyme form | Supports energy metabolism, nerve function |
| Thiamine Monophosphate (TMP) | Intermediate form | Minor role in metabolism |
| Thiamine Triphosphate (TTP) | Found in nerves | Aids in nerve conduction |
Functions of Thiamine (Vitamin B1)
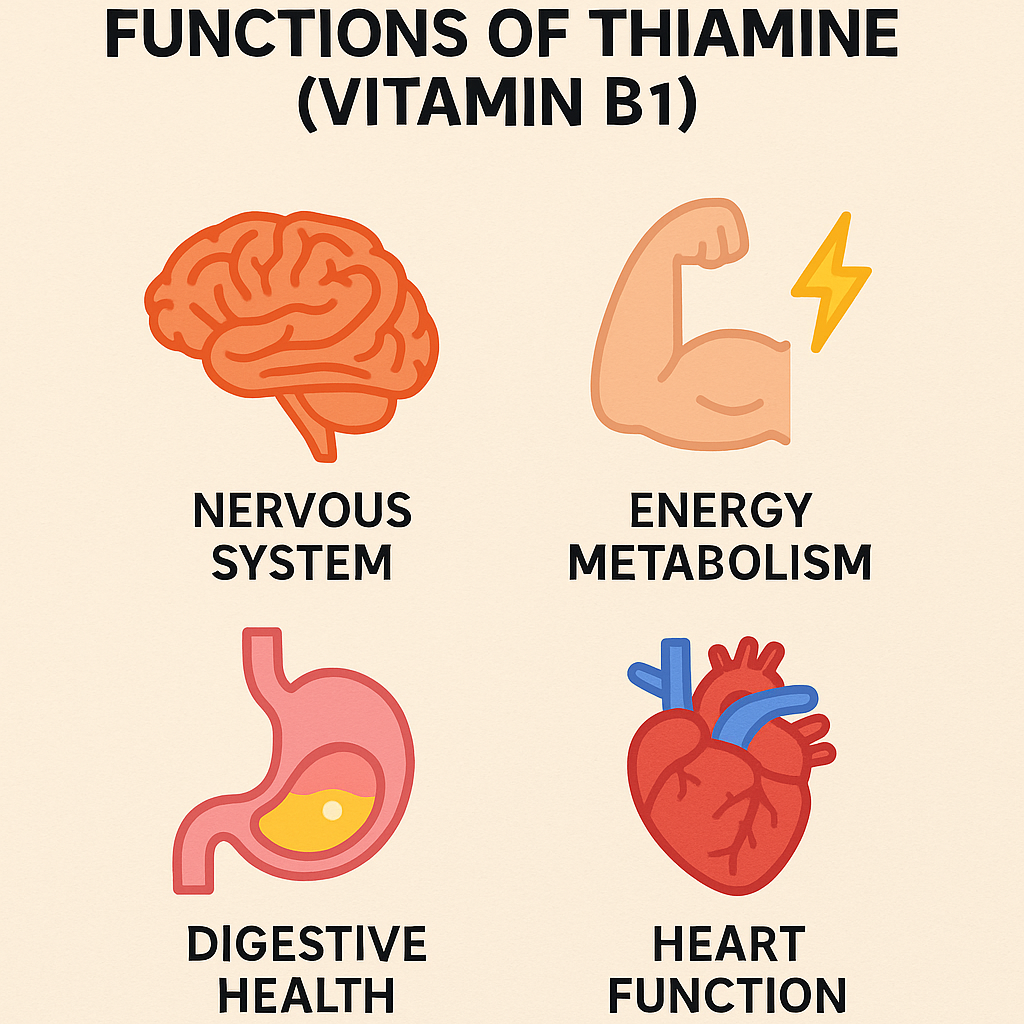
Vitamin B1 is essential for multiple physiological and biochemical processes:
1. Energy Metabolism
- Acts as a coenzyme (TPP) in carbohydrate metabolism.
- Helps convert glucose into ATP (energy).
- Essential for the Krebs cycle and oxidative decarboxylation.
2. Nervous System Health
- Required for nerve impulse transmission.
- Supports the synthesis of neurotransmitters (acetylcholine).
- Prevents nerve damage and muscle weakness.
3. Muscle Function
- Regulates muscle contractions.
- Prevents muscle wasting and fatigue.
4. Cardiovascular Health
- Supports heart muscle function.
- Prevents heart failure associated with beriberi.
5. Digestion and Appetite Regulation
- Helps maintain a healthy digestive system.
- Stimulates appetite and proper digestion.
Sources of Thiamine (Vitamin B1)
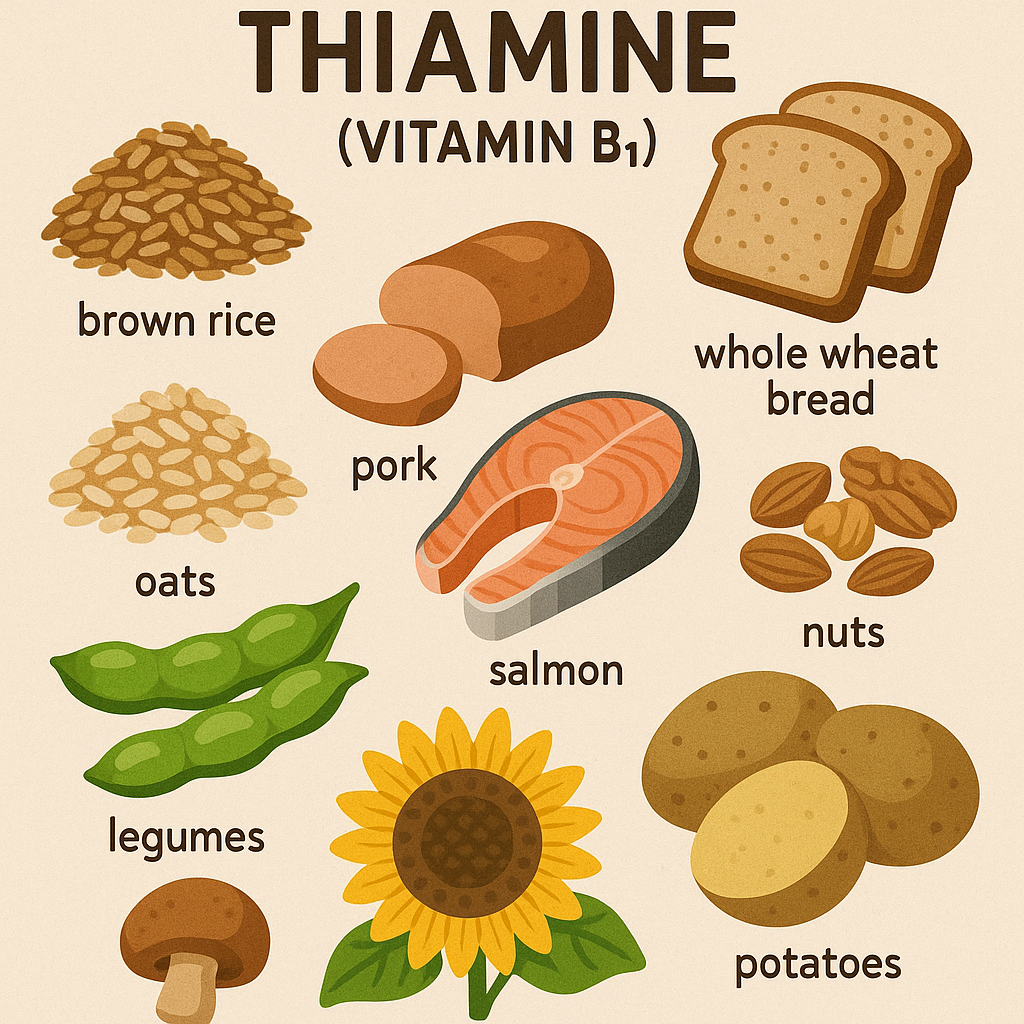
Thiamine is found in a variety of plant and animal-based foods.
Rich Natural Sources
1. Plant-Based Sources
- Whole Grains and Cereals: Brown rice, whole wheat, oats.
- Legumes: Lentils, beans, peas.
- Nuts and Seeds: Sunflower seeds, flaxseeds.
- Vegetables: Spinach, asparagus, Brussels sprouts.
2. Animal-Based Sources
- Meat: Pork (richest source), beef, liver.
- Eggs.
- Dairy Products: Milk, cheese.
3. Fortified Foods
- Breakfast cereals.
- White rice and pasta (enriched with B1).
- Nutritional yeast.
Thiamine Supplements
- Available in multivitamins, B-complex tablets, and individual thiamine supplements.
- Used to treat deficiency conditions like beriberi and Wernicke-Korsakoff syndrome.
Recommended Dietary Allowance (RDA) of Thiamine (Vitamin B1)
The RDA for Thiamine is measured in milligrams (mg/day).
| Age Group | RDA (mg/day) | Upper Limit (UL) |
|---|---|---|
| Infants (0-6 months) | 0.2 mg | Not established |
| Infants (7-12 months) | 0.3 mg | Not established |
| Children (1-3 years) | 0.5 mg | Not established |
| Children (4-8 years) | 0.6 mg | Not established |
| Children (9-13 years) | 0.9 mg | Not established |
| Adolescents (14-18 years, male) | 1.2 mg | Not established |
| Adolescents (14-18 years, female) | 1.0 mg | Not established |
| Adults (19+ years, male) | 1.2 mg | Not established |
| Adults (19+ years, female) | 1.1 mg | Not established |
| Pregnant Women | 1.4 mg | Not established |
| Lactating Women | 1.4 mg | Not established |
Note:
- There is no upper limit (UL) established, as excess thiamine is excreted in urine.
Thiamine (Vitamin B1) Deficiency and Toxicity
Deficiency Disorders
Vitamin B1 deficiency is common in alcoholics, malnourished individuals, and people with malabsorption disorders.
1. Beriberi
- Dry Beriberi: Affects the nervous system, causing muscle weakness, numbness, and paralysis.
- Wet Beriberi: Affects the cardiovascular system, leading to heart failure, fluid retention, and swelling.
2. Wernicke-Korsakoff Syndrome
- Occurs in chronic alcoholics due to impaired thiamine absorption.
- Wernicke’s encephalopathy: Symptoms include confusion, lack of coordination, vision problems.
- Korsakoff’s psychosis: Permanent memory loss, hallucinations, and brain damage.
3. Peripheral Neuropathy
- Numbness, tingling, and burning sensation in hands and feet.
4. Digestive Disorders
- Loss of appetite, constipation, indigestion.
Toxicity (Hypervitaminosis B1)
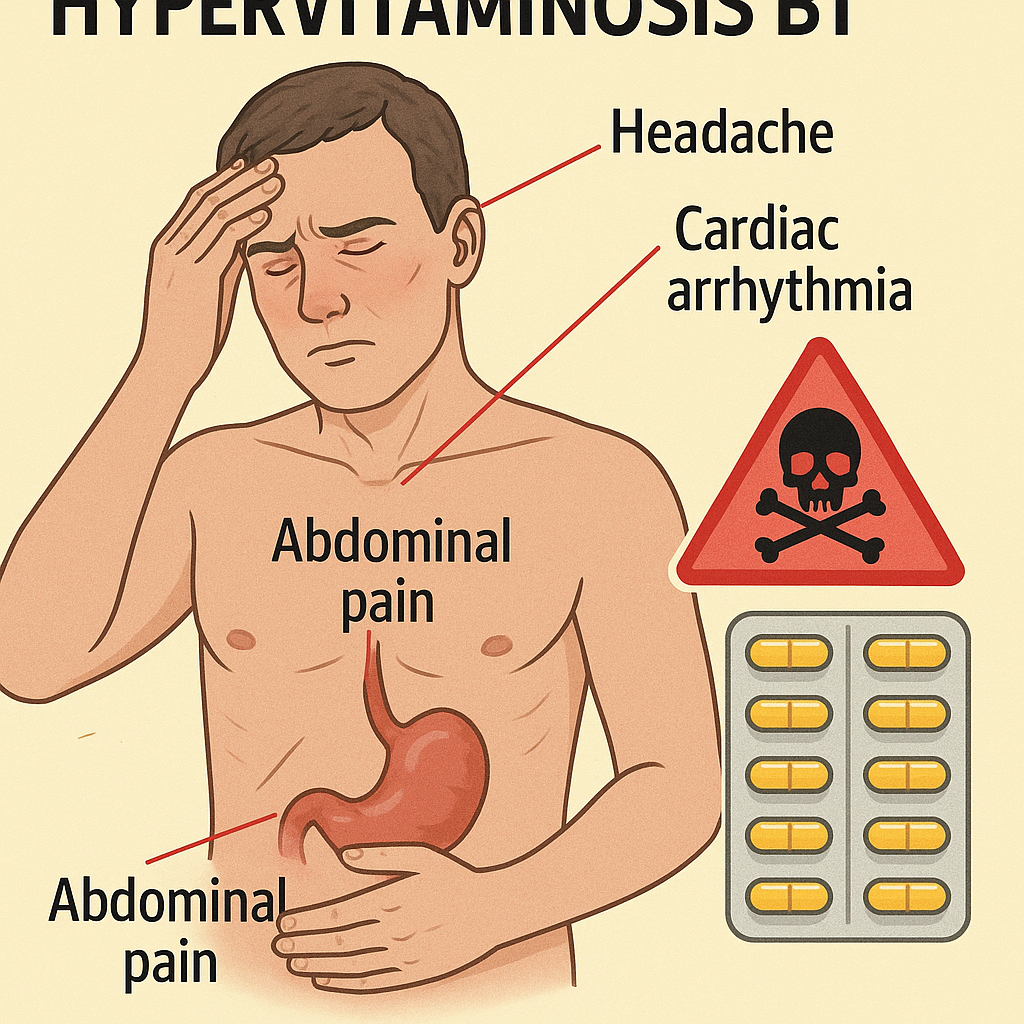
Thiamine toxicity is rare because excess amounts are excreted in urine. However, extremely high doses can cause:
- Nausea, vomiting.
- Low blood pressure.
- Skin rashes or allergic reactions.
Comparison of Thiamine Forms
| Aspect | Thiamine (Vitamin B1) | Synthetic Thiamine (Supplement Form) |
|---|---|---|
| Sources | Whole grains, nuts, pork, legumes | Tablets, injections |
| Function | Energy metabolism, nerve function | Treatment of deficiency |
| Absorption | Well-absorbed from food | More effective for severe deficiency |
| Toxicity Risk | Low (excreted in urine) | Low (unless given in excess) |
Role of Thiamine in Nursing and Healthcare
Nurses play an important role in preventing, identifying, and treating Thiamine deficiency:
1. Identifying At-Risk Patients
- Alcoholics, elderly, malnourished individuals.
- Patients with malabsorption disorders (Crohn’s disease, celiac disease).
- Pregnant and lactating women.
2. Administering Thiamine Supplements
- Oral supplements for mild deficiency.
- Intravenous (IV) or intramuscular (IM) injections for severe deficiency (Wernicke-Korsakoff syndrome).
3. Educating Patients
- Encouraging thiamine-rich diets.
- Advising alcoholics on the importance of Vitamin B1 to prevent Wernicke-Korsakoff syndrome.
- Promoting fortified foods in populations at risk of deficiency.
Summary of Thiamine (Vitamin B1)
| Aspect | Details |
|---|---|
| Classification | Water-Soluble Vitamin |
| Forms | Free Thiamine, Thiamine Pyrophosphate (TPP), Thiamine Monophosphate (TMP), Thiamine Triphosphate (TTP) |
| Functions | Energy metabolism, nerve function, muscle activity, cardiovascular health |
| Sources | Whole grains, nuts, pork, legumes, fortified cereals |
| RDA | 1.2 mg/day (men), 1.1 mg/day (women), 1.4 mg/day (pregnant/lactating) |
| Deficiency | Beriberi, Wernicke-Korsakoff syndrome, neuropathy, loss of appetite |
| Toxicity | Rare, excess excreted in urine |
Riboflavin (Vitamin B2): Classification, Functions, Sources, and Recommended Dietary Allowance (RDA)
Introduction
Riboflavin, also known as Vitamin B2, is a water-soluble vitamin essential for energy production, red blood cell formation, and maintaining healthy skin, eyes, and nervous system function. It serves as a precursor for coenzymes (FAD and FMN), which play a vital role in metabolism. Since Vitamin B2 is water-soluble, the body does not store it in large amounts, requiring a daily intake through diet.
Classification of Riboflavin (Vitamin B2)
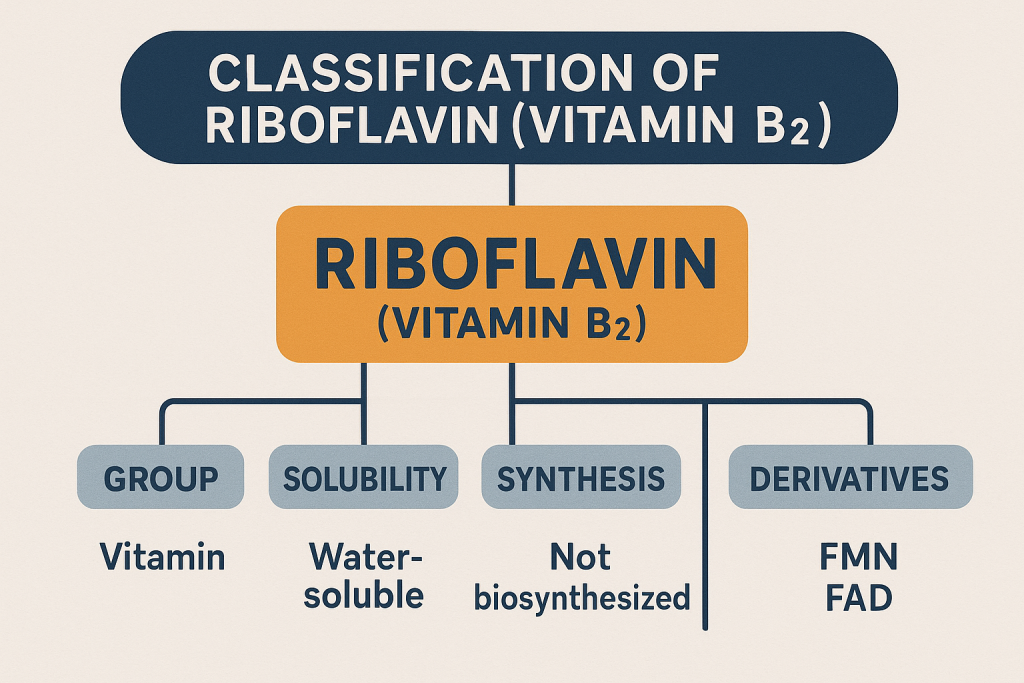
Vitamin B2 exists in two main biologically active coenzyme forms:
1. Flavin Mononucleotide (FMN)
- Also known as Riboflavin-5′-phosphate.
- Participates in oxidation-reduction reactions in metabolism.
2. Flavin Adenine Dinucleotide (FAD)
- Functions as an electron carrier in energy production.
- Crucial for the metabolism of carbohydrates, fats, and proteins.
| Category | Examples | Biological Role |
|---|---|---|
| Free Riboflavin | Found in foods | Converted into FMN and FAD |
| Flavin Mononucleotide (FMN) | Active coenzyme | Oxidation-reduction reactions |
| Flavin Adenine Dinucleotide (FAD) | Active coenzyme | Energy production, electron transport |
Functions of Riboflavin (Vitamin B2)
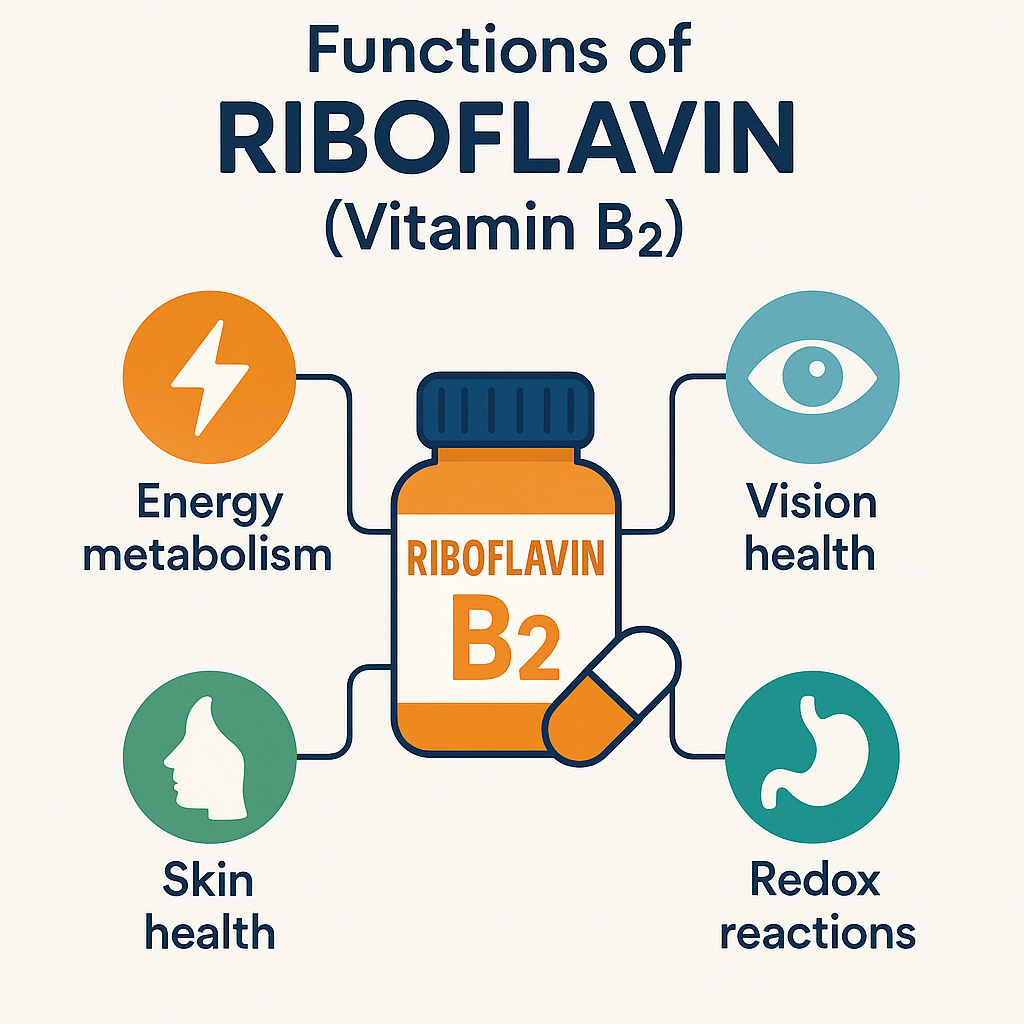
Vitamin B2 is involved in several critical biological functions:
1. Energy Metabolism
- Acts as a coenzyme in the electron transport chain, aiding in ATP production.
- Converts carbohydrates, proteins, and fats into usable energy.
2. Red Blood Cell Formation
- Essential for hemoglobin synthesis, preventing anemia.
- Supports oxygen transport in the blood.
3. Skin, Hair, and Eye Health
- Helps maintain healthy skin and mucous membranes.
- Prevents cracks and sores in the mouth (cheilitis).
- Protects eyes from cataracts and light sensitivity.
4. Antioxidant Function
- FAD is involved in the glutathione antioxidant system, which protects cells from oxidative damage.
5. Nervous System Support
- Helps in the synthesis of neurotransmitters.
- Prevents migraine headaches.
Sources of Riboflavin (Vitamin B2)
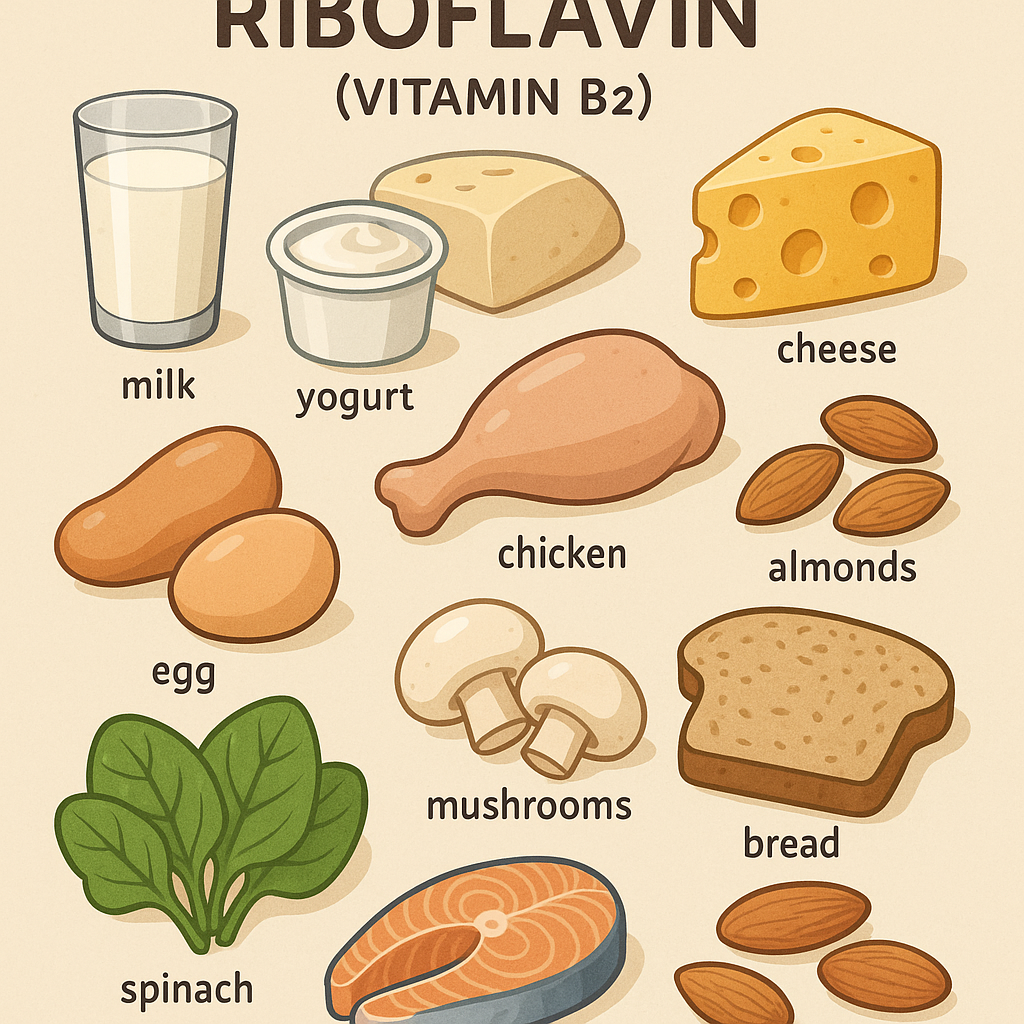
Vitamin B2 is found in both plant-based and animal-based foods.
Rich Natural Sources
1. Animal-Based Sources
- Dairy Products: Milk, cheese, yogurt.
- Eggs.
- Meat and Poultry: Beef liver (richest source), chicken, turkey.
- Fish: Salmon, trout, mackerel.
2. Plant-Based Sources
- Leafy Green Vegetables: Spinach, kale, broccoli.
- Whole Grains: Brown rice, whole wheat bread, oats.
- Legumes: Lentils, beans, peas.
- Nuts and Seeds: Almonds, sunflower seeds.
- Fruits: Avocados, bananas.
3. Fortified Foods
- Breakfast cereals.
- Enriched flour, bread, and pasta.
- Fortified plant-based milk (soy, almond).
Riboflavin Supplements
- Found in multivitamins and B-complex supplements.
- Used to prevent and treat riboflavin deficiency.
Recommended Dietary Allowance (RDA) of Riboflavin (Vitamin B2)
The RDA for Riboflavin is measured in milligrams (mg/day).
| Age Group | RDA (mg/day) | Upper Limit (UL) |
|---|---|---|
| Infants (0-6 months) | 0.3 mg | Not established |
| Infants (7-12 months) | 0.4 mg | Not established |
| Children (1-3 years) | 0.5 mg | Not established |
| Children (4-8 years) | 0.6 mg | Not established |
| Children (9-13 years) | 0.9 mg | Not established |
| Adolescents (14-18 years, male) | 1.3 mg | Not established |
| Adolescents (14-18 years, female) | 1.0 mg | Not established |
| Adults (19+ years, male) | 1.3 mg | Not established |
| Adults (19+ years, female) | 1.1 mg | Not established |
| Pregnant Women | 1.4 mg | Not established |
| Lactating Women | 1.6 mg | Not established |
Note:
- No upper limit (UL) is established, as excess Riboflavin is excreted in urine.
Riboflavin (Vitamin B2) Deficiency and Toxicity
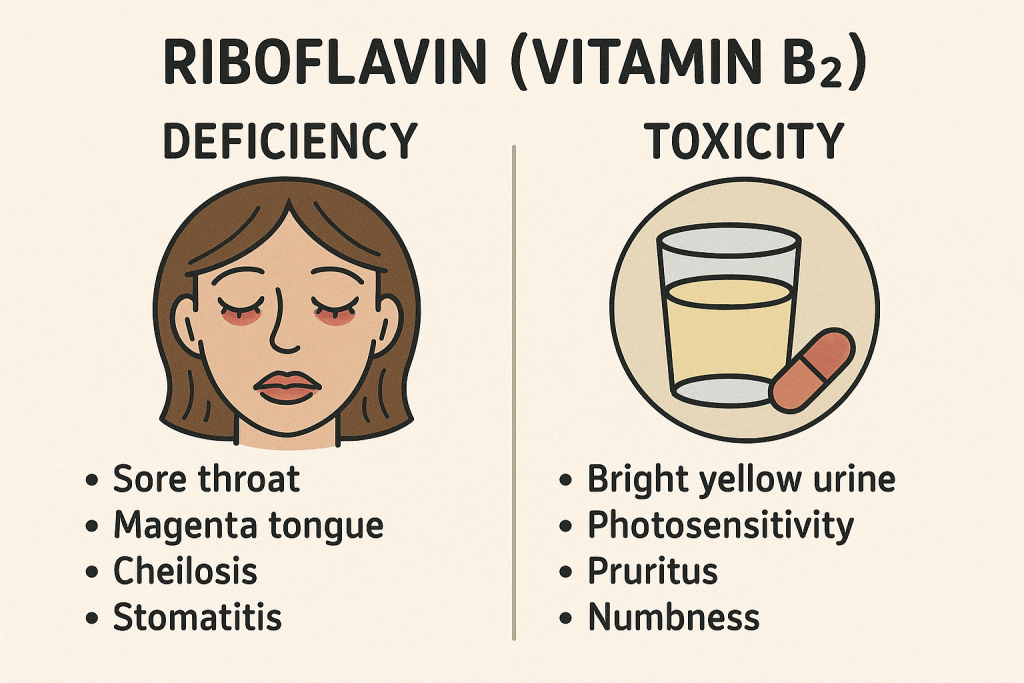
Deficiency Disorders
Vitamin B2 deficiency is rare but can occur in individuals with:
- Poor diet (malnutrition).
- Chronic alcoholism.
- Malabsorption disorders (Crohn’s disease, celiac disease).
- Elderly individuals.
Symptoms of Deficiency (Ariboflavinosis)
- Cracked lips and mouth sores (Cheilitis).
- Glossitis (swollen, red tongue).
- Sore throat and mouth ulcers.
- Skin inflammation (Seborrheic dermatitis).
- Light sensitivity (Photophobia) and eye fatigue.
- Anemia (due to impaired red blood cell production).
Toxicity (Hypervitaminosis B2)
Riboflavin toxicity is rare because excess amounts are excreted in urine. However, excessive intake may cause:
- Bright yellow urine (harmless).
- Mild nausea.
- Increased risk of kidney stones (in very high doses).
Comparison of Riboflavin Forms
| Aspect | Riboflavin (Vitamin B2) | Synthetic Riboflavin (Supplement Form) |
|---|---|---|
| Sources | Dairy, meat, eggs, whole grains, leafy greens | Tablets, injections |
| Function | Energy metabolism, antioxidant, red blood cell formation | Used for treating deficiency |
| Absorption | Well-absorbed from food | Rapidly excreted in urine |
| Toxicity Risk | Low (excreted in urine) | Low (except in kidney disorders) |
Role of Riboflavin in Nursing and Healthcare
Nurses play a key role in preventing, diagnosing, and treating Riboflavin deficiency:
1. Identifying At-Risk Patients
- Malnourished individuals, alcoholics, elderly, and those with gastrointestinal disorders.
- Patients with light sensitivity, cracked lips, and mouth ulcers.
2. Administering Riboflavin Supplements
- Oral supplements for mild deficiency.
- Intravenous (IV) or intramuscular (IM) injections for severe deficiency.
3. Educating Patients
- Encouraging a diet rich in dairy, meat, eggs, and green vegetables.
- Advising vegetarians and vegans on fortified food options.
- Informing patients that bright yellow urine after supplement intake is normal.
4. Managing Riboflavin Toxicity
- Reassuring patients that excess riboflavin is not harmful.
- Monitoring kidney function in individuals with renal diseases.
Summary of Riboflavin (Vitamin B2)
| Aspect | Details |
|---|---|
| Classification | Water-Soluble Vitamin |
| Forms | Free Riboflavin, Flavin Mononucleotide (FMN), Flavin Adenine Dinucleotide (FAD) |
| Functions | Energy metabolism, red blood cell formation, antioxidant, eye health |
| Sources | Dairy, meat, eggs, whole grains, green vegetables, fortified foods |
| RDA | 1.3 mg/day (men), 1.1 mg/day (women), 1.4-1.6 mg/day (pregnant/lactating) |
| Deficiency | Cheilitis, glossitis, photophobia, anemia, mouth ulcers |
| Toxicity | Rare, excess excreted in urine |
Nicotinic Acid (Niacin, Vitamin B3): Classification, Functions, Sources, and Recommended Dietary Allowance (RDA)
Introduction
Nicotinic acid, commonly known as Niacin (Vitamin B3), is a water-soluble vitamin that plays a crucial role in energy metabolism, DNA repair, and maintaining healthy skin, nerves, and digestion. It is unique among vitamins because the body can synthesize it from the amino acid tryptophan. Niacin is used both as a nutrient and a medication, especially in managing cholesterol levels.
Classification of Niacin (Vitamin B3)
Niacin exists in two biologically active forms:
1. Nicotinic Acid (Niacin)
- Found in plant-based and animal-based foods.
- Used as a cholesterol-lowering medication.
2. Nicotinamide (Niacinamide)
- Found in meats, dairy, and supplements.
- Does not cause flushing, unlike nicotinic acid.
- Preferred for therapeutic use in skin and neurological disorders.
3. Coenzyme Forms
- Nicotinamide Adenine Dinucleotide (NAD+) – Essential for cellular metabolism and energy production.
- Nicotinamide Adenine Dinucleotide Phosphate (NADP+) – Plays a role in antioxidant functions and biosynthesis reactions.
| Category | Examples | Biological Role |
|---|---|---|
| Nicotinic Acid (Niacin) | Found in grains, meats, and supplements | Cholesterol metabolism, energy production |
| Nicotinamide (Niacinamide) | Found in meats, dairy, supplements | Supports brain and skin health, anti-inflammatory |
| NAD+ / NADP+ (Coenzymes) | Active cellular forms | Energy metabolism, DNA repair, antioxidant function |
Functions of Niacin (Vitamin B3)
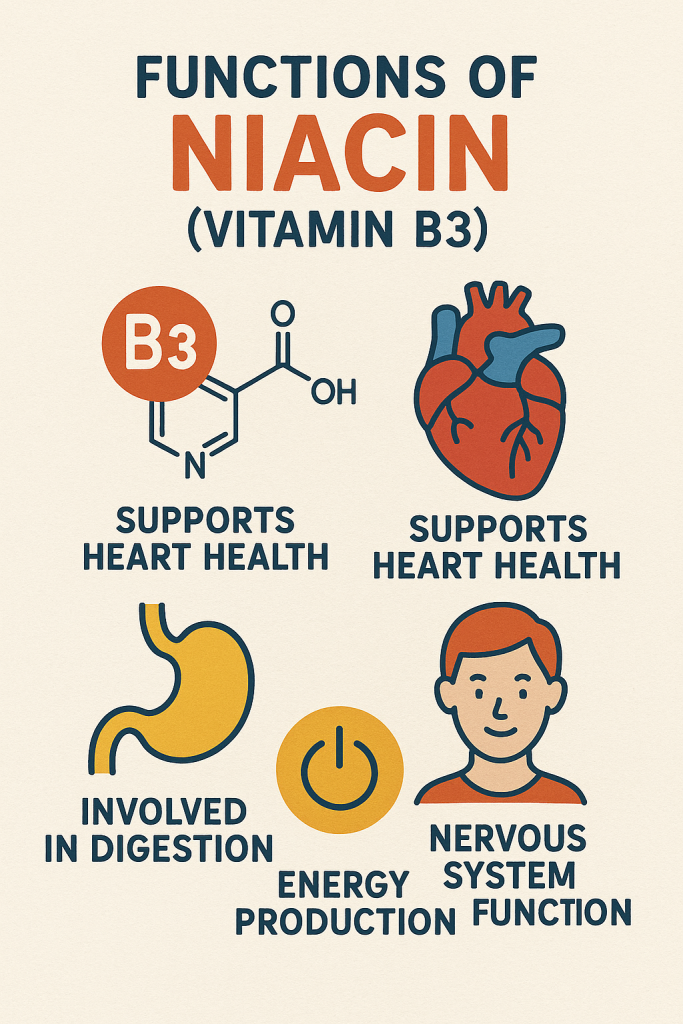
Niacin is involved in multiple critical physiological functions:
1. Energy Metabolism
- Functions as a coenzyme (NAD+ and NADP+) in the metabolism of carbohydrates, fats, and proteins.
- Aids in ATP production in mitochondria.
2. Cholesterol and Heart Health
- Lowers LDL (bad cholesterol) and increases HDL (good cholesterol).
- Reduces triglyceride levels, lowering the risk of cardiovascular diseases.
3. DNA Repair and Antioxidant Function
- Helps in DNA synthesis and repair.
- Acts as an antioxidant, reducing oxidative stress.
4. Nervous System and Mental Health
- Supports brain function and neurotransmitter synthesis.
- May help in treating schizophrenia, depression, and neurodegenerative diseases.
5. Skin and Digestive Health
- Maintains healthy skin and prevents sun sensitivity.
- Essential for digestive enzyme function and nutrient absorption.
Sources of Niacin (Vitamin B3)
Niacin is found in a variety of plant-based and animal-based foods. The body can also synthesize niacin from tryptophan (60 mg of tryptophan = 1 mg niacin equivalent).
Rich Natural Sources
1. Animal-Based Sources
- Meat: Chicken, turkey, beef, pork.
- Fish: Tuna, salmon, mackerel.
- Dairy Products: Milk, cheese, yogurt.
- Eggs.
2. Plant-Based Sources
- Whole Grains: Brown rice, whole wheat, oats.
- Legumes: Peanuts, lentils, beans.
- Nuts and Seeds: Sunflower seeds, almonds.
- Vegetables: Mushrooms, potatoes, avocados.
3. Fortified Foods
- Breakfast cereals.
- White rice and flour (enriched with niacin).
Niacin Supplements
- Available as nicotinic acid, niacinamide, and sustained-release niacin.
- Used for cholesterol management and treating niacin deficiency.
Recommended Dietary Allowance (RDA) of Niacin (Vitamin B3)
The RDA for Niacin is measured in milligrams (mg/day) of Niacin Equivalents (NE).
| Age Group | RDA (mg/day NE) | Upper Limit (UL) (mg/day NE) |
|---|---|---|
| Infants (0-6 months) | 2 mg | Not established |
| Infants (7-12 months) | 4 mg | Not established |
| Children (1-3 years) | 6 mg | 10 mg |
| Children (4-8 years) | 8 mg | 15 mg |
| Children (9-13 years) | 12 mg | 20 mg |
| Adolescents (14-18 years, male) | 16 mg | 30 mg |
| Adolescents (14-18 years, female) | 14 mg | 30 mg |
| Adults (19+ years, male) | 16 mg | 35 mg |
| Adults (19+ years, female) | 14 mg | 35 mg |
| Pregnant Women | 18 mg | 35 mg |
| Lactating Women | 17 mg | 35 mg |
Note:
- 1 mg Niacin Equivalent (NE) = 1 mg Niacin OR 60 mg Tryptophan.
- The upper limit (UL) applies only to synthetic supplements, not food sources.
Niacin (Vitamin B3) Deficiency and Toxicity
Deficiency Disorders
Niacin deficiency can occur due to malnutrition, chronic alcoholism, and digestive disorders.
1. Pellagra (“The 4 D’s”)
A severe niacin deficiency leads to pellagra, characterized by:
- Dermatitis – Dark, scaly rashes on sun-exposed skin.
- Diarrhea – Digestive issues and malabsorption.
- Dementia – Memory loss, confusion, and neurological symptoms.
- Death – If untreated, deficiency can be fatal.
2. Neurological Symptoms
- Depression, headaches, fatigue.
- Cognitive impairment, irritability.
3. Digestive Issues
- Loss of appetite, nausea, vomiting.
- Glossitis (inflamed tongue), mouth ulcers.
Toxicity (Hypervitaminosis B3)
High doses of niacin from supplements can lead to:
1. Niacin Flush (Vasodilation)
- Redness, warmth, and tingling sensation on the skin.
- Temporary and harmless but uncomfortable.
2. Liver Damage
- Excessive niacin intake can cause hepatotoxicity.
3. Gastrointestinal Issues
- Nausea, vomiting, stomach pain.
4. Increased Blood Sugar Levels
- Can worsen diabetes control.
Safe Limits:
- Avoid exceeding 35 mg/day from supplements.
Comparison of Niacin Forms
| Aspect | Nicotinic Acid (Niacin) | Nicotinamide (Niacinamide) |
|---|---|---|
| Function | Cholesterol lowering, energy metabolism | Skin health, neurological support |
| Side Effects | Flushing, liver toxicity (high doses) | No flushing, safer alternative |
| Sources | Meat, grains, supplements | Meats, dairy, legumes |
| Use in Supplements | Common in cholesterol management | Used in skincare and anti-inflammatory therapy |
Role of Niacin in Nursing and Healthcare
Nurses play a vital role in monitoring Niacin intake, preventing deficiency, and managing side effects:
1. Identifying At-Risk Patients
- Malnourished individuals, alcoholics, elderly, and those with digestive disorders.
- Patients with neurological symptoms or skin rashes.
2. Administering Niacin Supplements
- Oral supplements for mild deficiency.
- High-dose niacin therapy for cholesterol management.
3. Educating Patients
- Encouraging a diet rich in whole grains, meats, and legumes.
- Advising patients on niacin therapy about possible flushing side effects.
- Monitoring patients with diabetes or liver disease on high-dose niacin.
Summary of Niacin (Vitamin B3)
| Aspect | Details |
|---|---|
| Classification | Water-Soluble Vitamin |
| Forms | Nicotinic Acid, Nicotinamide, NAD+, NADP+ |
| Functions | Energy metabolism, cholesterol regulation, DNA repair, brain function |
| Sources | Meat, fish, dairy, grains, nuts, legumes |
| RDA | 16 mg/day (men), 14 mg/day (women), 18 mg/day (pregnant) |
| Deficiency | Pellagra (4 D’s – Dermatitis, Diarrhea, Dementia, Death) |
| Toxicity | Flushing, liver damage, nausea, increased blood sugar |
Pyridoxine (Vitamin B6): Classification, Functions, Sources, and Recommended Dietary Allowance (RDA)
Introduction
Pyridoxine, commonly known as Vitamin B6, is a water-soluble vitamin essential for protein metabolism, neurotransmitter synthesis, red blood cell production, and immune function. It plays a significant role in over 100 enzymatic reactions in the body. Since Vitamin B6 is not stored in large amounts, a continuous dietary intake is required.
Classification of Pyridoxine (Vitamin B6)
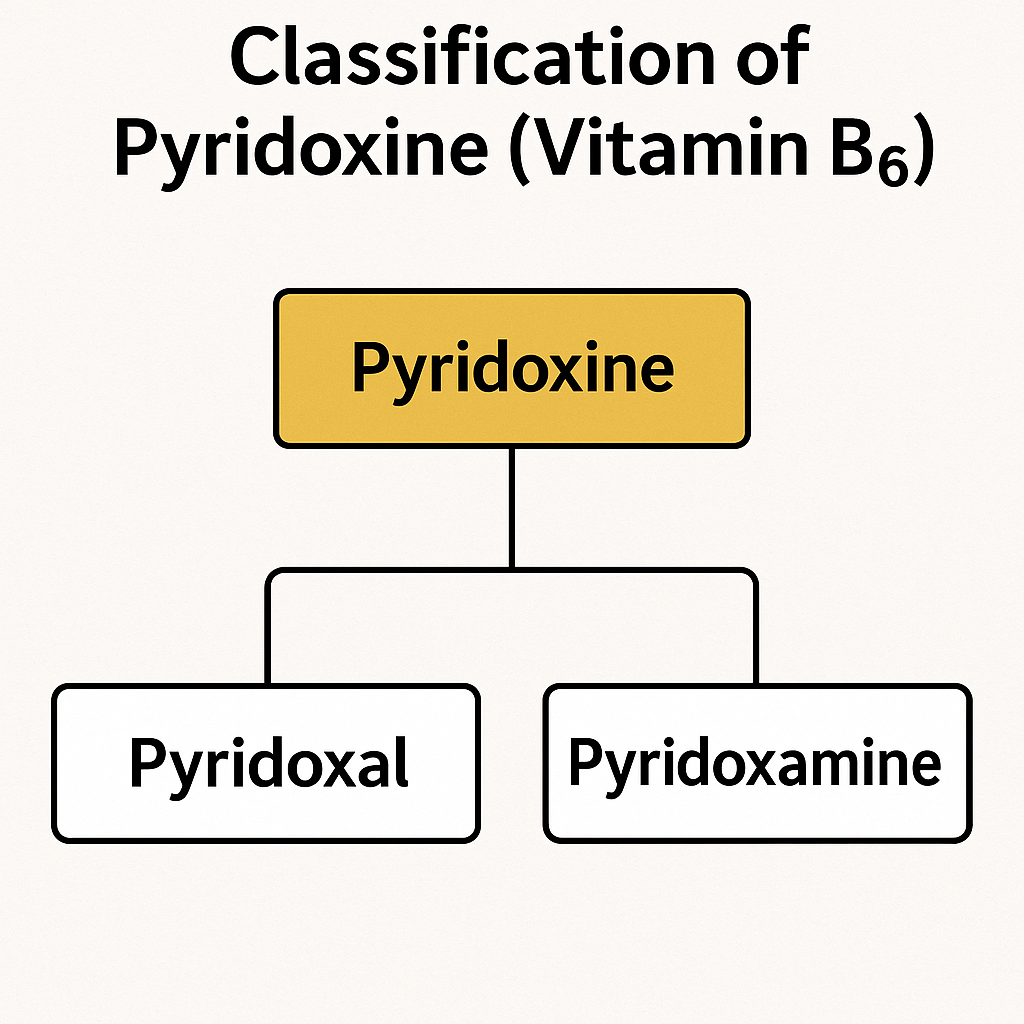
Vitamin B6 exists in six interconvertible forms, with Pyridoxal Phosphate (PLP) being the most active coenzyme form:
1. Pyridoxine (PN)
- Found in plant-based foods.
- Stable in food but less bioavailable.
2. Pyridoxal (PL)
- Found in animal-based foods.
- Easily converted into PLP.
3. Pyridoxamine (PM)
- Found in animal sources.
- Precursor for PLP synthesis.
4. Coenzyme Forms
- Pyridoxal Phosphate (PLP) – Active coenzyme involved in metabolism.
- Pyridoxamine Phosphate (PMP) – Important for amino acid metabolism.
| Category | Examples | Biological Role |
|---|---|---|
| Free Vitamin B6 | Pyridoxine (PN), Pyridoxal (PL), Pyridoxamine (PM) | Found in plant and animal foods |
| Coenzyme Forms | Pyridoxal Phosphate (PLP), Pyridoxamine Phosphate (PMP) | Active in protein metabolism, neurotransmitter function |
Functions of Pyridoxine (Vitamin B6)
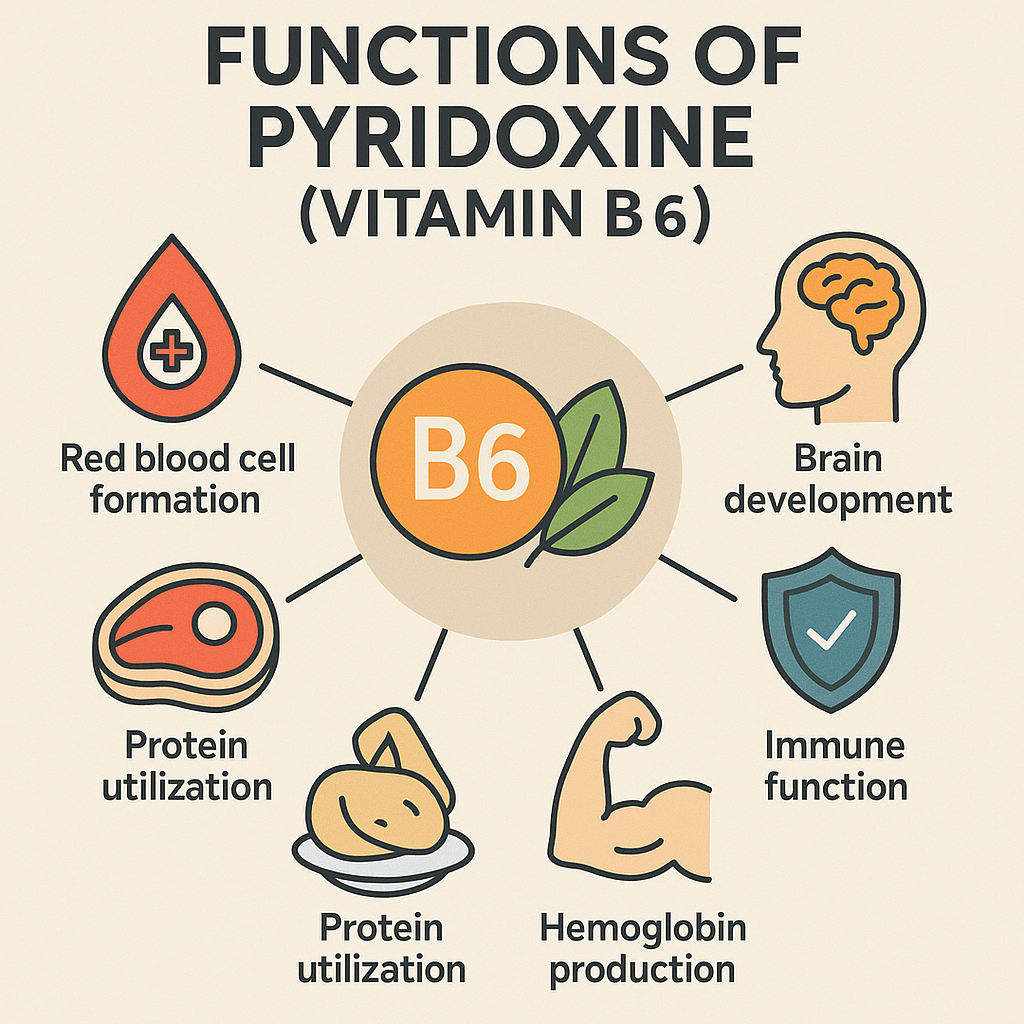
Vitamin B6 is essential for various biochemical and physiological functions:
1. Protein and Amino Acid Metabolism
- Breaks down and synthesizes amino acids for energy production.
- Converts tryptophan into niacin (Vitamin B3).
2. Neurotransmitter Synthesis
- Helps in the production of serotonin, dopamine, norepinephrine, and GABA.
- Supports brain function and mental health.
3. Red Blood Cell Formation
- Involved in hemoglobin production, preventing anemia.
- Maintains oxygen transport in the blood.
4. Immune System Support
- Enhances white blood cell function.
- Helps regulate inflammation.
5. Cardiovascular Health
- Lowers homocysteine levels, reducing the risk of heart disease.
- Supports healthy blood pressure regulation.
6. Hormonal Regulation
- Helps in mood regulation and reduces PMS symptoms.
- Supports hormonal balance during pregnancy.
Sources of Pyridoxine (Vitamin B6)
Vitamin B6 is found in a variety of plant-based and animal-based foods.
Rich Natural Sources
1. Animal-Based Sources
- Meat: Chicken, turkey, beef, pork.
- Fish: Salmon, tuna, mackerel.
- Eggs.
- Dairy Products: Milk, cheese, yogurt.
2. Plant-Based Sources
- Whole Grains: Brown rice, whole wheat, oats.
- Legumes: Lentils, beans, chickpeas.
- Nuts and Seeds: Sunflower seeds, walnuts.
- Vegetables: Potatoes, spinach, bananas, carrots.
3. Fortified Foods
- Breakfast cereals.
- Nutritional yeast.
- Fortified plant-based milk (soy, almond).
Pyridoxine Supplements
- Available as individual Vitamin B6 supplements or B-complex vitamins.
- Used for treating deficiency, pregnancy-related nausea, and nervous system disorders.
Recommended Dietary Allowance (RDA) of Pyridoxine (Vitamin B6)
The RDA for Vitamin B6 is measured in milligrams (mg/day).
| Age Group | RDA (mg/day) | Upper Limit (UL) (mg/day) |
|---|---|---|
| Infants (0-6 months) | 0.1 mg | Not established |
| Infants (7-12 months) | 0.3 mg | Not established |
| Children (1-3 years) | 0.5 mg | 30 mg |
| Children (4-8 years) | 0.6 mg | 40 mg |
| Children (9-13 years) | 1.0 mg | 60 mg |
| Adolescents (14-18 years, male) | 1.3 mg | 80 mg |
| Adolescents (14-18 years, female) | 1.2 mg | 80 mg |
| Adults (19-50 years, male and female) | 1.3 mg | 100 mg |
| Adults (51+ years, male) | 1.7 mg | 100 mg |
| Adults (51+ years, female) | 1.5 mg | 100 mg |
| Pregnant Women | 1.9 mg | 100 mg |
| Lactating Women | 2.0 mg | 100 mg |
Note:
- The upper limit (UL) applies to synthetic supplements, not food sources.
Pyridoxine (Vitamin B6) Deficiency and Toxicity
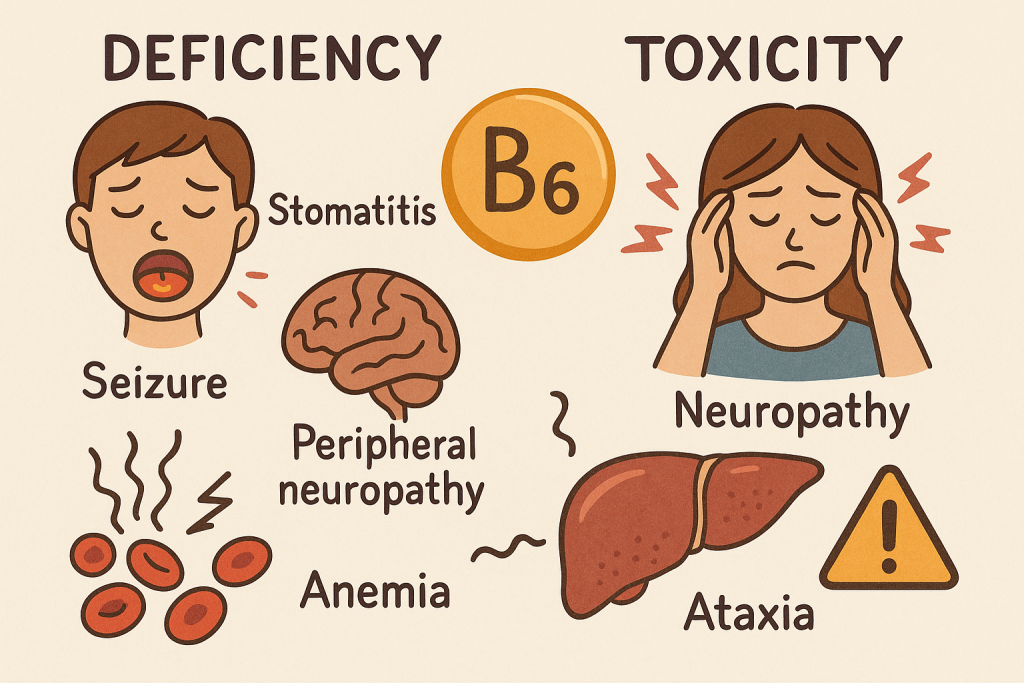
Deficiency Disorders
Vitamin B6 deficiency is rare but can occur in alcoholics, pregnant women, and those with malabsorption disorders.
Symptoms of Deficiency
- Neurological issues: Depression, irritability, confusion.
- Peripheral neuropathy: Numbness, tingling in hands and feet.
- Anemia: Due to impaired hemoglobin production.
- Skin disorders: Cracks in the mouth, inflammation.
- Weakened immune function: Frequent infections.
At-Risk Groups for Deficiency
Toxicity (Hypervitaminosis B6)
Excessive intake of Vitamin B6 from supplements (above 100 mg/day) can cause:
Symptoms of Toxicity
- Nerve damage (Peripheral neuropathy) – Tingling, numbness, difficulty walking.
- Ataxia – Loss of muscle coordination.
- Nausea, vomiting, stomach pain.
- Skin lesions and photosensitivity.
Safe Limits:
- Avoid exceeding 100 mg/day from supplements.
Comparison of Pyridoxine Forms
| Aspect | Pyridoxine (Vitamin B6) | Synthetic Pyridoxine Supplements |
|---|---|---|
| Function | Protein metabolism, neurotransmitter function | Used in treating neurological disorders |
| Sources | Meat, fish, grains, vegetables | Tablets, injections |
| Absorption | Well-absorbed from food | More effective for severe deficiency |
| Toxicity Risk | Low (from food sources) | High in megadoses (nerve toxicity) |
Role of Pyridoxine in Nursing and Healthcare
Nurses play an essential role in monitoring, preventing, and treating Vitamin B6 deficiency and toxicity.
1. Identifying At-Risk Patients
- Pregnant women, alcoholics, elderly, kidney dialysis patients.
- Patients with nerve disorders or anemia.
2. Administering Pyridoxine Supplements
- Oral supplements for mild deficiency.
- IV or IM injections for severe deficiency.
3. Educating Patients
- Encouraging a diet rich in whole grains, fish, meat, and vegetables.
- Advising pregnant women on adequate B6 intake.
- Warning against high-dose supplementation to prevent toxicity.
4. Managing Vitamin B6 Toxicity
- Monitoring patients on high-dose B6 therapy.
- Identifying early signs of neuropathy and ataxia.
Summary of Pyridoxine (Vitamin B6)
| Aspect | Details |
|---|---|
| Classification | Water-Soluble Vitamin |
| Forms | Pyridoxine (PN), Pyridoxal (PL), Pyridoxamine (PM), PLP (Active Form) |
| Functions | Protein metabolism, neurotransmitter function, immune support, hemoglobin synthesis |
| Sources | Meat, fish, whole grains, vegetables, nuts |
| RDA | 1.3 mg/day (adults), 1.9-2.0 mg/day (pregnant/lactating) |
| Deficiency | Depression, anemia, skin issues, nerve damage |
| Toxicity | Nerve damage, nausea, loss of muscle coordination |
Pantothenic Acid (Vitamin B5): Classification, Functions, Sources, and Recommended Dietary Allowance (RDA)
Introduction
Pantothenic acid, also known as Vitamin B5, is a water-soluble vitamin essential for energy metabolism, hormone production, and red blood cell formation. It is a key component of coenzyme A (CoA), which is involved in the breakdown of carbohydrates, fats, and proteins. Since Vitamin B5 is found in almost all foods, deficiency is rare.
Classification of Pantothenic Acid (Vitamin B5)
Pantothenic acid exists in various forms, with Coenzyme A (CoA) and Acyl Carrier Protein (ACP) being the most active forms in the body.
1. Free Pantothenic Acid
- Found in food sources.
- Readily absorbed in the intestine.
2. Coenzyme Forms
- Coenzyme A (CoA) – Plays a crucial role in energy production, fatty acid synthesis, and detoxification.
- Acyl Carrier Protein (ACP) – Involved in fatty acid metabolism.
| Category | Examples | Biological Role |
|---|---|---|
| Free Pantothenic Acid | Found in food sources | Absorbed in the intestine |
| Coenzyme A (CoA) | Active form | Energy metabolism, fatty acid synthesis |
| Acyl Carrier Protein (ACP) | Component of CoA | Involved in lipid metabolism |
Functions of Pantothenic Acid (Vitamin B5)
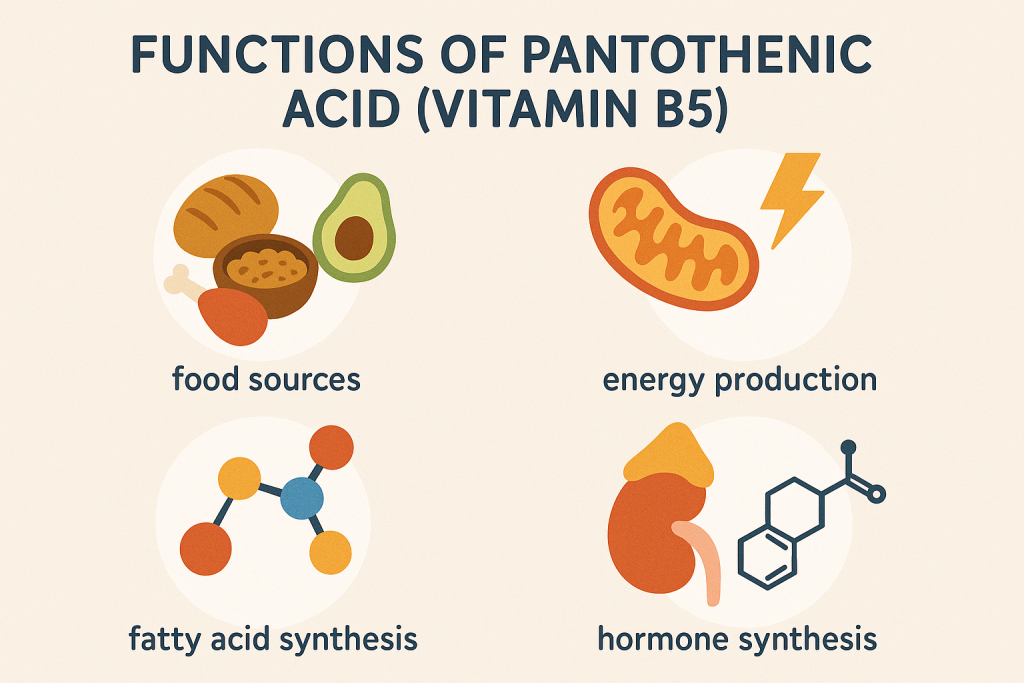
Vitamin B5 plays a critical role in various metabolic and physiological processes:
1. Energy Metabolism
- Component of Coenzyme A (CoA), which is essential for:
- Breakdown of carbohydrates, fats, and proteins to produce ATP.
- Krebs cycle (Citric Acid Cycle) for energy production.
2. Synthesis of Hormones and Neurotransmitters
- Involved in the production of steroid hormones (cortisol, testosterone, estrogen).
- Supports the synthesis of acetylcholine, an important neurotransmitter for nerve function.
3. Fatty Acid and Cholesterol Synthesis
- Helps synthesize cholesterol, phospholipids, and essential fatty acids.
- Supports the formation of cell membranes.
4. Red Blood Cell Formation
- Necessary for the production of heme, a component of hemoglobin.
5. Wound Healing and Skin Health
- Promotes tissue repair and wound healing.
- Used in skincare products for hydration and healing.
Sources of Pantothenic Acid (Vitamin B5)
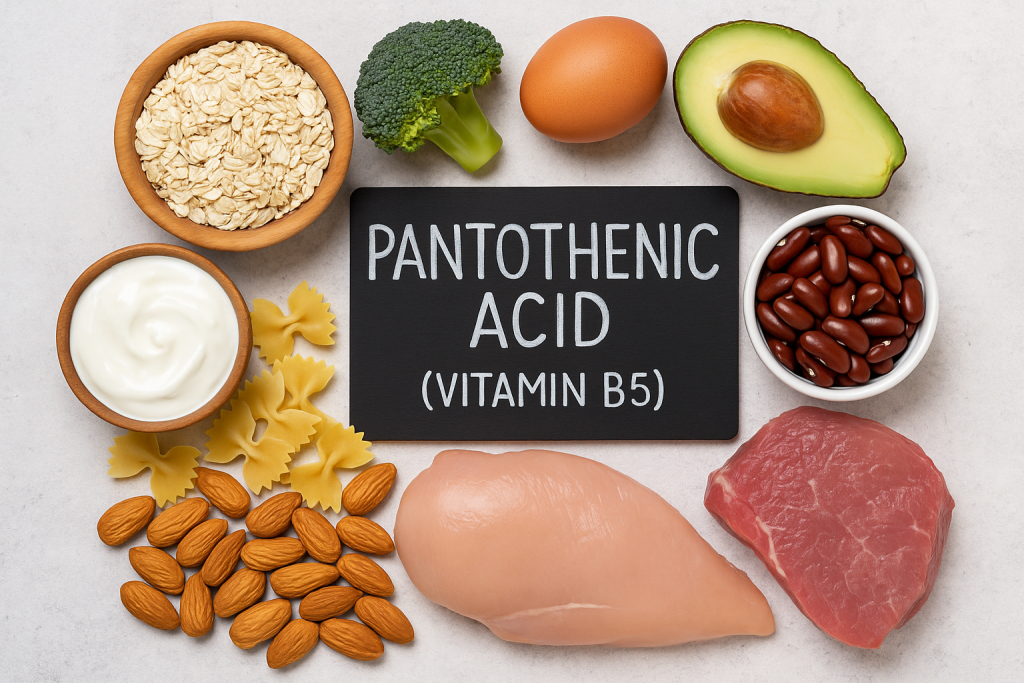
Vitamin B5 is widely available in both plant-based and animal-based foods.
Rich Natural Sources
1. Animal-Based Sources
- Meat: Chicken, turkey, beef, pork.
- Fish: Salmon, trout.
- Eggs.
- Dairy Products: Milk, cheese, yogurt.
2. Plant-Based Sources
- Whole Grains: Brown rice, whole wheat, oats.
- Legumes: Lentils, beans, peas.
- Nuts and Seeds: Sunflower seeds, peanuts.
- Vegetables: Mushrooms, avocados, broccoli, sweet potatoes.
3. Fortified Foods
- Breakfast cereals.
- Nutritional yeast.
- Fortified plant-based milk (soy, almond).
Pantothenic Acid Supplements
- Found in B-complex vitamins and multivitamins.
- Used to treat deficiency and support adrenal function.
Recommended Dietary Allowance (RDA) of Pantothenic Acid (Vitamin B5)
The RDA for Pantothenic Acid is measured in milligrams (mg/day).
| Age Group | Adequate Intake (AI) (mg/day) | Upper Limit (UL) (mg/day) |
|---|---|---|
| Infants (0-6 months) | 1.7 mg | Not established |
| Infants (7-12 months) | 1.8 mg | Not established |
| Children (1-3 years) | 2 mg | Not established |
| Children (4-8 years) | 3 mg | Not established |
| Children (9-13 years) | 4 mg | Not established |
| Adolescents (14-18 years, male and female) | 5 mg | Not established |
| Adults (19+ years, male and female) | 5 mg | Not established |
| Pregnant Women | 6 mg | Not established |
| Lactating Women | 7 mg | Not established |
Note:
- There is no upper limit (UL) established because excess pantothenic acid is excreted in urine.
Pantothenic Acid (Vitamin B5) Deficiency and Toxicity
Deficiency Disorders
Vitamin B5 deficiency is very rare because it is found in almost all foods. However, deficiency can occur in cases of severe malnutrition.
Symptoms of Deficiency
- Fatigue and weakness due to impaired energy metabolism.
- Irritability and mood disturbances (depression, anxiety).
- Numbness and tingling (paresthesia) in hands and feet.
- Digestive issues: Nausea, vomiting, abdominal cramps.
- Burning feet syndrome: A rare condition causing burning pain in the feet, commonly seen in malnourished prisoners of war.
At-Risk Groups for Deficiency
- Severely malnourished individuals.
- Alcoholics.
- Diabetics (due to increased excretion).
- People with gastrointestinal disorders (Crohn’s disease, celiac disease).
Toxicity (Hypervitaminosis B5)
Pantothenic acid toxicity is rare because it is water-soluble and excess is excreted in urine.
Symptoms of Excess Intake
- Mild diarrhea (in doses above 10 g/day).
- Gastrointestinal discomfort (bloating, cramps).
- Increased thirst and urination.
Safe Limits:
- Although there is no established upper limit (UL), doses above 1,000 mg/day may cause mild side effects.
Comparison of Pantothenic Acid Forms
| Aspect | Pantothenic Acid (Vitamin B5) | Synthetic Pantothenic Acid Supplements |
|---|---|---|
| Function | Energy metabolism, hormone production | Used for adrenal support, skincare |
| Sources | Meat, fish, whole grains, vegetables | Tablets, injections, creams |
| Absorption | Well-absorbed from food | More effective for specific treatments |
| Toxicity Risk | Low (from food sources) | Mild gastrointestinal discomfort in high doses |
Role of Pantothenic Acid in Nursing and Healthcare
Nurses play a crucial role in monitoring, preventing, and treating Vitamin B5 deficiency and toxicity.
1. Identifying At-Risk Patients
- Malnourished individuals, alcoholics, elderly, people with GI disorders.
- Patients with neurological symptoms, fatigue, or burning feet syndrome.
2. Administering Pantothenic Acid Supplements
- Oral supplements for mild deficiency.
- IV or IM injections in severe cases.
3. Educating Patients
- Encouraging a diet rich in whole grains, meat, fish, vegetables.
- Informing patients on high-dose supplements about potential mild side effects.
- Recommending fortified foods in populations at risk of deficiency.
4. Managing Vitamin B5 Toxicity
- Monitoring patients on high-dose therapy for digestive discomfort.
- Adjusting supplement dosage if symptoms occur.
Summary of Pantothenic Acid (Vitamin B5)
| Aspect | Details |
|---|---|
| Classification | Water-Soluble Vitamin |
| Forms | Free Pantothenic Acid, Coenzyme A (CoA), Acyl Carrier Protein (ACP) |
| Functions | Energy metabolism, hormone production, fatty acid synthesis, red blood cell formation |
| Sources | Meat, fish, whole grains, vegetables, nuts, fortified foods |
| RDA | 5 mg/day (adults), 6-7 mg/day (pregnant/lactating) |
| Deficiency | Fatigue, irritability, numbness, burning feet syndrome |
| Toxicity | Mild diarrhea, GI discomfort (high doses) |
Folic Acid (Vitamin B9): Classification, Functions, Sources, and Recommended Dietary Allowance (RDA)
Introduction
Folic acid, also known as Vitamin B9, is a water-soluble vitamin essential for DNA synthesis, cell division, red blood cell formation, and fetal development. It plays a crucial role in preventing neural tube defects (NTDs) during pregnancy. Folic acid is the synthetic form found in supplements and fortified foods, whereas folate is the naturally occurring form in foods.
Classification of Folic Acid (Vitamin B9)
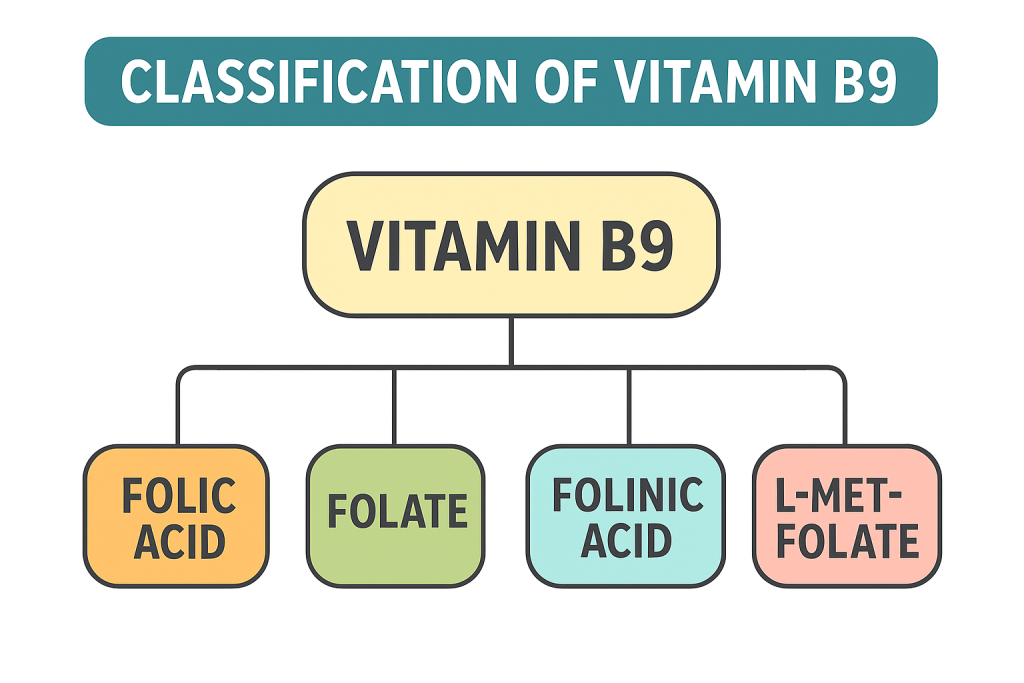
Vitamin B9 exists in two major forms:
1. Natural Form (Folate)
- Found in plant-based and animal-based foods.
- Exists as polyglutamate, which is converted into monoglutamate for absorption.
2. Synthetic Form (Folic Acid)
- Found in fortified foods and supplements.
- More stable and bioavailable than natural folate.
- Converted into tetrahydrofolate (THF), the active form.
3. Coenzyme Forms
- Tetrahydrofolate (THF) – Active coenzyme involved in DNA and RNA synthesis.
- 5-Methyltetrahydrofolate (5-MTHF) – Involved in homocysteine metabolism.
| Category | Examples | Biological Role |
|---|---|---|
| Natural Folate | Found in leafy greens, legumes, eggs | DNA synthesis, cell growth |
| Folic Acid (Synthetic Form) | Found in supplements, fortified foods | More bioavailable, used for prevention of NTDs |
| Coenzyme Forms | THF, 5-MTHF | DNA replication, amino acid metabolism |
Functions of Folic Acid (Vitamin B9)
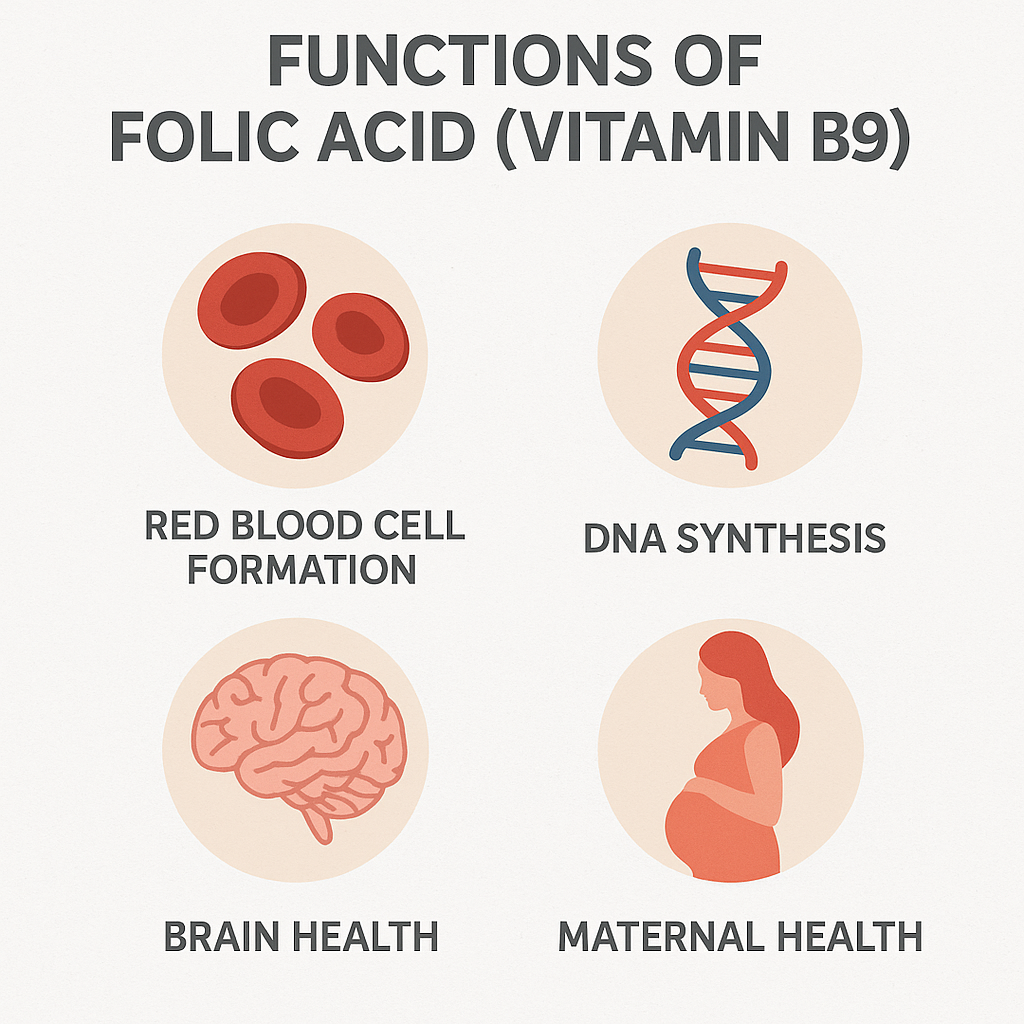
Vitamin B9 plays a critical role in various physiological and biochemical processes:
1. DNA Synthesis and Cell Growth
- Essential for cell division and replication.
- Supports tissue growth and repair.
2. Red Blood Cell Formation
- Prevents megaloblastic anemia by supporting hemoglobin production.
- Aids in the formation of healthy red blood cells.
3. Fetal Development and Pregnancy Health
- Prevents neural tube defects (spina bifida, anencephaly).
- Supports placental growth and fetal brain development.
4. Homocysteine Metabolism (Heart Health)
- Works with Vitamin B12 and B6 to reduce homocysteine levels, lowering the risk of cardiovascular diseases.
5. Brain and Nervous System Function
- Supports neurotransmitter function, reducing the risk of depression and cognitive decline.
- May help prevent Alzheimer’s disease.
Sources of Folic Acid (Vitamin B9)
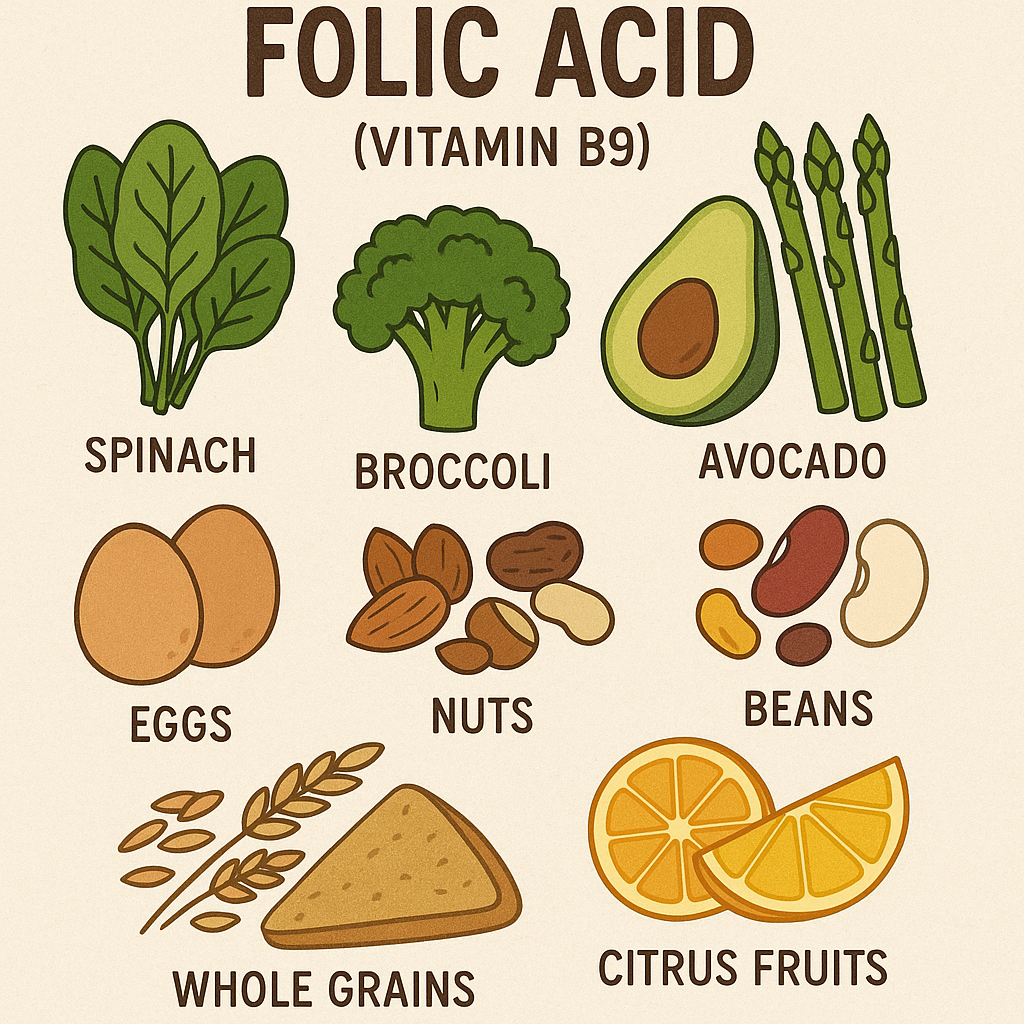
Folic acid is found in both natural and fortified sources.
Rich Natural Sources (Folate)
1. Plant-Based Sources
- Leafy Green Vegetables: Spinach, kale, lettuce, asparagus.
- Legumes: Lentils, chickpeas, black beans.
- Nuts and Seeds: Sunflower seeds, peanuts.
- Fruits: Oranges, bananas, avocados.
2. Animal-Based Sources
- Eggs.
- Liver and Meat.
- Dairy Products: Cheese, milk.
3. Fortified Foods (Folic Acid)
- Fortified cereals, bread, rice, and pasta.
- Fortified plant-based milk (soy, almond).
- Nutritional yeast.
Folic Acid Supplements
- Found in prenatal vitamins and multivitamins.
- Used to prevent and treat folate deficiency, pregnancy-related complications, and anemia.
Recommended Dietary Allowance (RDA) of Folic Acid (Vitamin B9)
The RDA for folic acid is measured in micrograms (mcg) of Dietary Folate Equivalents (DFE).
| Age Group | RDA (mcg DFE/day) | Upper Limit (UL) (mcg/day) |
|---|---|---|
| Infants (0-6 months) | 65 mcg | Not established |
| Infants (7-12 months) | 80 mcg | Not established |
| Children (1-3 years) | 150 mcg | 300 mcg |
| Children (4-8 years) | 200 mcg | 400 mcg |
| Children (9-13 years) | 300 mcg | 600 mcg |
| Adolescents (14-18 years, male and female) | 400 mcg | 800 mcg |
| Adults (19+ years, male and female) | 400 mcg | 1000 mcg |
| Pregnant Women | 600 mcg | 1000 mcg |
| Lactating Women | 500 mcg | 1000 mcg |
Note:
- 1 mcg DFE = 1 mcg food folate = 0.6 mcg folic acid (from fortified foods) = 0.5 mcg folic acid (from supplements).
- Upper limit (UL) applies only to synthetic folic acid from supplements and fortified foods.
Folic Acid (Vitamin B9) Deficiency and Toxicity
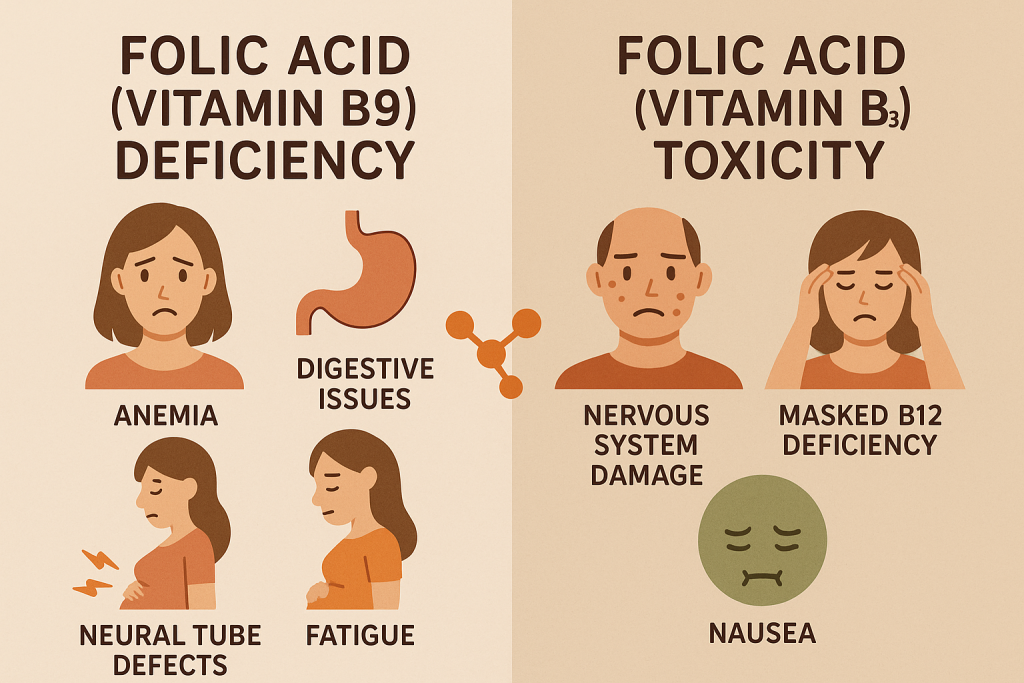
Deficiency Disorders
Vitamin B9 deficiency is common in pregnancy, alcoholics, and individuals with malabsorption disorders.
Symptoms of Deficiency
- Megaloblastic anemia: Enlarged, immature red blood cells.
- Fatigue, weakness, and pale skin.
- Neural tube defects (NTDs) in newborns.
- Depression, memory issues, and cognitive decline.
- Glossitis (swollen tongue) and mouth ulcers.
At-Risk Groups for Deficiency
- Pregnant women.
- Alcoholics.
- People with gastrointestinal disorders (Crohn’s disease, celiac disease).
- Individuals on certain medications (Methotrexate, Anticonvulsants).
Toxicity (Hypervitaminosis B9)
Excess folic acid from supplements can lead to:
Symptoms of Excess Intake
- Masking of Vitamin B12 deficiency, leading to neuropathy.
- Increased risk of colorectal cancer (controversial in high doses).
- Sleep disturbances and irritability.
Safe Limits:
- Do not exceed 1000 mcg/day from supplements unless prescribed.
Comparison of Folate and Folic Acid
| Aspect | Folate (Natural Form) | Folic Acid (Synthetic Form) |
|---|---|---|
| Sources | Leafy greens, legumes, fruits | Supplements, fortified foods |
| Function | DNA synthesis, cell division | More bioavailable, used for pregnancy and anemia |
| Absorption | Lower than folic acid | Higher (converted to active form in the liver) |
| Toxicity Risk | Low (excess excreted) | Can mask Vitamin B12 deficiency |
Role of Folic Acid in Nursing and Healthcare
Nurses play an essential role in monitoring, preventing, and treating folic acid deficiency.
1. Identifying At-Risk Patients
- Pregnant women, alcoholics, elderly, patients with malabsorption disorders.
- Patients with anemia or neurological symptoms.
2. Administering Folic Acid Supplements
- Oral supplements for mild deficiency.
- IV or IM injections in severe cases.
3. Educating Patients
- Encouraging a diet rich in leafy greens, beans, and fortified cereals.
- Advising pregnant women to take 400-600 mcg/day to prevent NTDs.
- Warning against high-dose supplementation without medical supervision.
4. Managing Folic Acid Toxicity
- Monitoring patients on high-dose therapy for Vitamin B12 deficiency symptoms.
- Adjusting dosages if side effects occur.
Summary of Folic Acid (Vitamin B9)
| Aspect | Details |
|---|---|
| Classification | Water-Soluble Vitamin |
| Forms | Folate (Natural), Folic Acid (Synthetic), THF, 5-MTHF |
| Functions | DNA synthesis, red blood cell formation, fetal development, heart health |
| Sources | Leafy greens, legumes, fortified cereals, supplements |
| RDA | 400 mcg/day (adults), 600 mcg/day (pregnancy) |
| Deficiency | Megaloblastic anemia, neural tube defects, cognitive issues |
| Toxicity | Masks B12 deficiency, possible cancer risk |
Vitamin B12 (Cobalamin): Classification, Functions, Sources, and Recommended Dietary Allowance (RDA)
Introduction
Vitamin B12, also known as Cobalamin, is a water-soluble vitamin essential for DNA synthesis, red blood cell formation, nerve function, and energy metabolism. Unlike other water-soluble vitamins, Vitamin B12 is stored in the liver, so deficiency symptoms may take years to appear. It is unique because it is only found in animal-based foods and requires intrinsic factor for absorption in the intestine.
Classification of Vitamin B12 (Cobalamin)
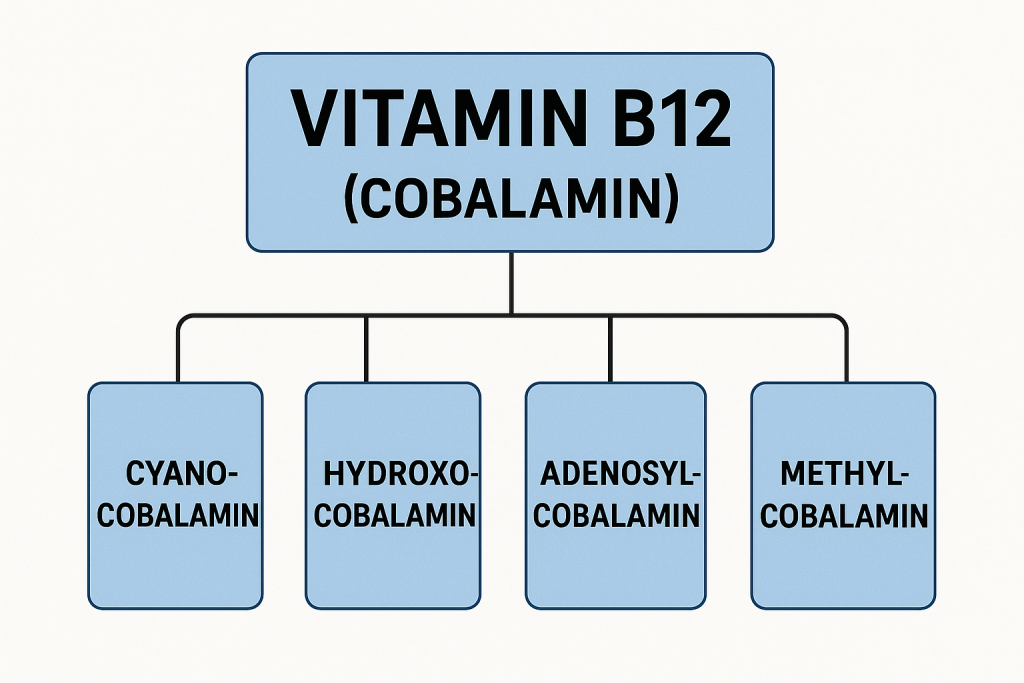
Vitamin B12 exists in four primary forms, with Methylcobalamin and Adenosylcobalamin being the most biologically active:
1. Cyanocobalamin (Synthetic Form)
- Found in supplements and fortified foods.
- Needs to be converted into active forms in the body.
2. Hydroxocobalamin
- Found in animal foods and used for B12 injections.
- Converts into Methylcobalamin in the body.
3. Methylcobalamin (Active Form)
- Found in some supplements.
- Used in nerve function and DNA synthesis.
4. Adenosylcobalamin (Active Form)
- Stored in the mitochondria.
- Helps in energy metabolism.
| Category | Examples | Biological Role |
|---|---|---|
| Synthetic Form | Cyanocobalamin | Found in supplements, requires conversion |
| Natural Forms | Hydroxocobalamin, Methylcobalamin, Adenosylcobalamin | Found in food, used in metabolic function |
Functions of Vitamin B12 (Cobalamin)
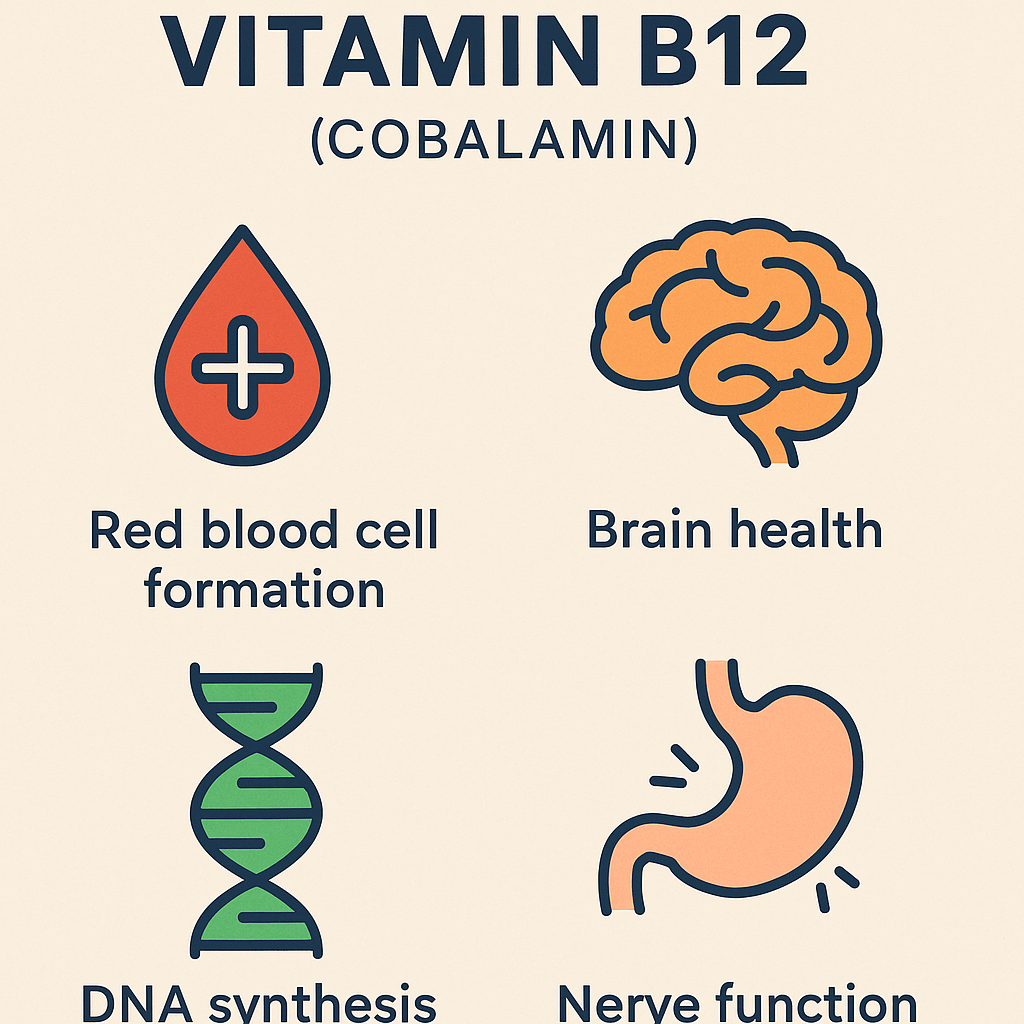
Vitamin B12 is critical for multiple physiological and biochemical processes:
1. Red Blood Cell Formation and DNA Synthesis
- Helps in the production of healthy red blood cells.
- Prevents megaloblastic anemia (large, immature red blood cells).
- Essential for cell division and DNA replication.
2. Nervous System Function
- Maintains myelin sheath around nerves.
- Prevents neuropathy, numbness, and nerve damage.
- Supports brain function and mental clarity.
3. Energy Metabolism
- Helps convert carbohydrates, fats, and proteins into energy.
- Prevents fatigue and weakness.
4. Heart Health
- Lowers homocysteine levels, reducing the risk of heart disease.
- Works with Folic Acid (Vitamin B9) and Vitamin B6 in methylation.
5. Bone Health
- Maintains bone mineral density, reducing the risk of osteoporosis.
6. Fetal Development and Pregnancy Health
- Supports brain and nervous system development in the fetus.
- Prevents congenital neurological disorders.
Sources of Vitamin B12 (Cobalamin)
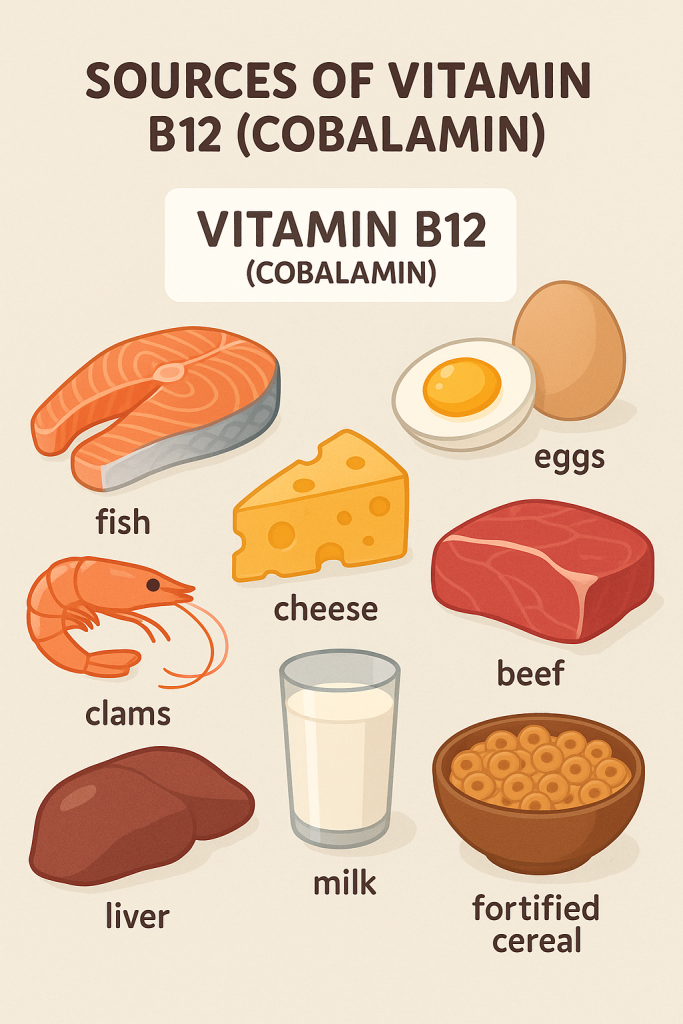
Vitamin B12 is only found in animal-based foods and fortified sources.
Rich Natural Sources
1. Animal-Based Sources
- Meat: Beef, chicken, pork.
- Fish and Seafood: Salmon, tuna, clams, shrimp.
- Dairy Products: Milk, cheese, yogurt.
- Eggs.
- Liver and Organ Meats: The richest source of Vitamin B12.
2. Fortified Plant-Based Sources
- Fortified cereals.
- Fortified plant-based milk (soy, almond, oat).
- Nutritional yeast (fortified).
Vitamin B12 Supplements
- Available as Cyanocobalamin, Methylcobalamin, and Hydroxocobalamin.
- Used for deficiency treatment, energy boost, and neurological health.
Recommended Dietary Allowance (RDA) of Vitamin B12 (Cobalamin)
The RDA for Vitamin B12 is measured in micrograms (mcg/day).
| Age Group | RDA (mcg/day) | Upper Limit (UL) (mcg/day) |
|---|---|---|
| Infants (0-6 months) | 0.4 mcg | Not established |
| Infants (7-12 months) | 0.5 mcg | Not established |
| Children (1-3 years) | 0.9 mcg | Not established |
| Children (4-8 years) | 1.2 mcg | Not established |
| Children (9-13 years) | 1.8 mcg | Not established |
| Adolescents (14-18 years, male and female) | 2.4 mcg | Not established |
| Adults (19+ years, male and female) | 2.4 mcg | Not established |
| Pregnant Women | 2.6 mcg | Not established |
| Lactating Women | 2.8 mcg | Not established |
Note:
- No upper limit (UL) is established, as excess Vitamin B12 is excreted in urine.
- Absorption decreases with age, so adults over 50 years should take B12 supplements.
Vitamin B12 (Cobalamin) Deficiency and Toxicity
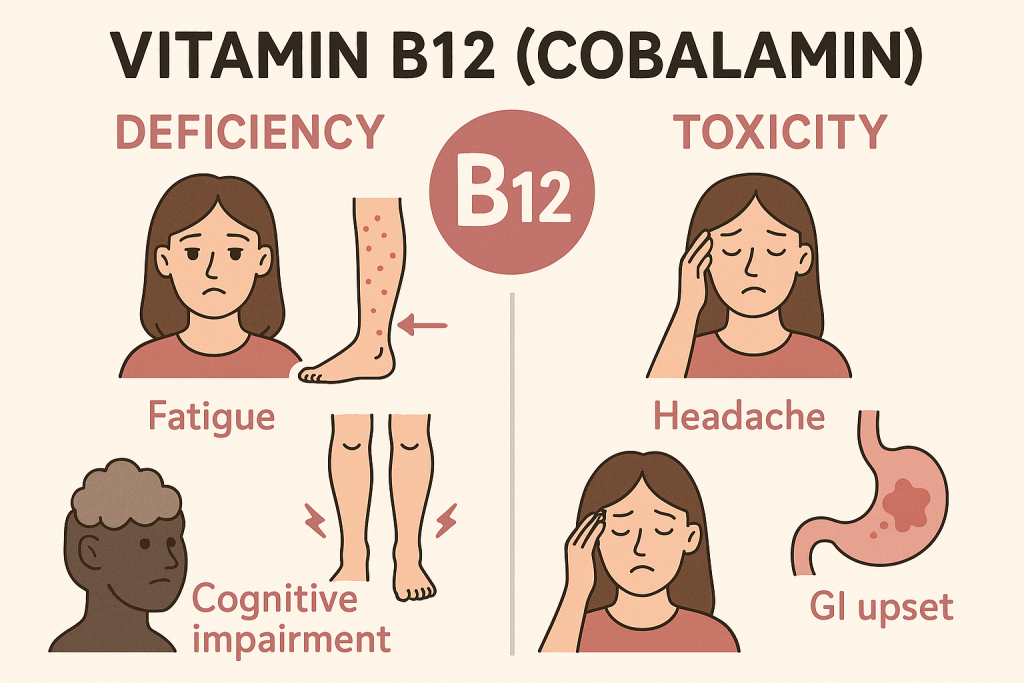
Deficiency Disorders
Vitamin B12 deficiency is common in vegetarians, elderly individuals, and those with absorption disorders.
Symptoms of Deficiency
- Megaloblastic anemia (Pernicious anemia): Weakness, fatigue, pale skin.
- Neuropathy: Tingling, numbness, burning sensation in hands and feet.
- Cognitive Decline: Memory loss, confusion, dementia-like symptoms.
- Depression and mood changes.
- Glossitis (swollen tongue) and mouth ulcers.
- Difficulty walking and balance issues.
At-Risk Groups for Deficiency
- Vegetarians and vegans.
- Elderly individuals (low stomach acid reduces absorption).
- People with gastrointestinal disorders (Crohn’s, Celiac disease).
- Pregnant and lactating women (higher demand).
- Patients on long-term metformin or proton pump inhibitors (PPIs).
Toxicity (Hypervitaminosis B12)
Vitamin B12 toxicity is rare, as excess amounts are excreted in urine.
Symptoms of Excess Intake
- Mild acne or skin rash (very high doses).
- Increased red blood cell production (polycythemia).
- Temporary nausea or diarrhea (high supplement intake).
Safe Limits:
- There is no established upper limit (UL), but megadoses should only be taken under medical supervision.
Comparison of Vitamin B12 Forms
| Aspect | Cyanocobalamin (Synthetic) | Methylcobalamin (Active Form) | Hydroxocobalamin (Injectable) |
|---|---|---|---|
| Sources | Supplements, fortified foods | Supplements, some food sources | Found in meat, used in injections |
| Absorption | Requires conversion in the liver | Readily available | High bioavailability |
| Function | General supplementation | Supports nerve function | Used for severe deficiency |
| Toxicity Risk | Low | Low | Low |
Role of Vitamin B12 in Nursing and Healthcare
Nurses play an important role in identifying, preventing, and treating Vitamin B12 deficiency.
1. Identifying At-Risk Patients
- Vegetarians, elderly, pregnant women, patients with GI disorders.
- Patients with neuropathy, fatigue, or cognitive decline.
2. Administering Vitamin B12 Supplements
- Oral supplements for mild deficiency.
- Intramuscular (IM) injections for severe deficiency.
- Sublingual supplements for better absorption.
3. Educating Patients
- Encouraging B12-rich diets (meat, eggs, dairy, fortified cereals).
- Advising vegetarians and elderly to take supplements.
- Monitoring patients on long-term medication that affects B12 absorption.
4. Managing Vitamin B12 Toxicity
- Reassuring patients that excess B12 is excreted in urine.
- Adjusting supplement dosage if needed.
Summary of Vitamin B12 (Cobalamin)
| Aspect | Details |
|---|---|
| Classification | Water-Soluble Vitamin |
| Forms | Cyanocobalamin, Methylcobalamin, Hydroxocobalamin, Adenosylcobalamin |
| Functions | Red blood cell formation, nerve function, DNA synthesis, heart health |
| Sources | Meat, fish, dairy, eggs, fortified foods, supplements |
| RDA | 2.4 mcg/day (adults), 2.6-2.8 mcg/day (pregnant/lactating) |
| Deficiency | Megaloblastic anemia, neuropathy, cognitive decline |
| Toxicity | Rare, mild digestive issues (high doses) |
Ascorbic Acid (Vitamin C): Classification, Functions, Sources, and Recommended Dietary Allowance (RDA)
Introduction
Ascorbic acid, commonly known as Vitamin C, is a water-soluble vitamin essential for immune function, collagen synthesis, wound healing, and antioxidant protection. Unlike most animals, humans cannot synthesize Vitamin C, making dietary intake crucial. It is a potent antioxidant that protects cells from oxidative damage and enhances iron absorption.
Classification of Ascorbic Acid (Vitamin C)
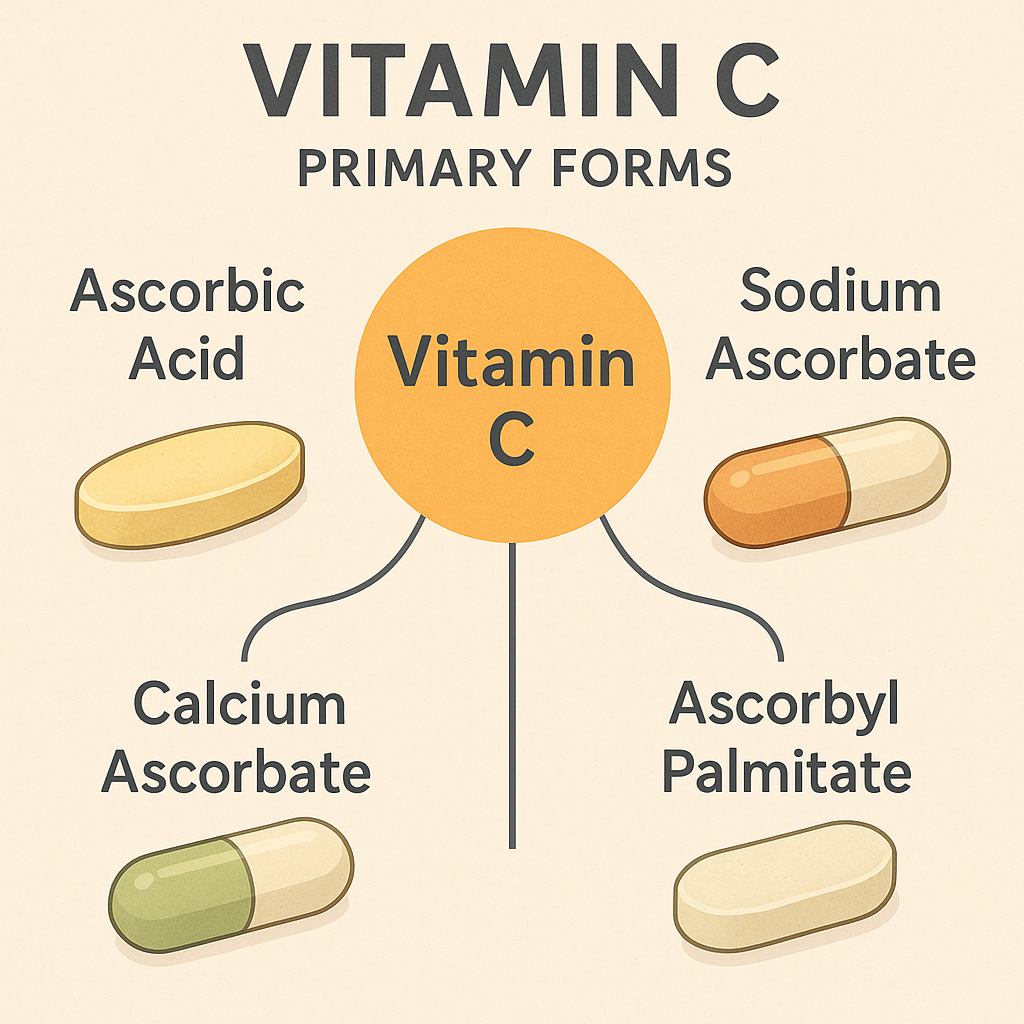
Vitamin C exists in two primary forms, with Ascorbic Acid being the most common:
1. Ascorbic Acid (Active Form)
- Found in natural sources and supplements.
- Acts as an antioxidant and enzyme cofactor.
2. Dehydroascorbic Acid (Oxidized Form)
- Can be converted back into ascorbic acid.
- Absorbed by cells via glucose transporters.
| Category | Examples | Biological Role |
|---|---|---|
| Active Form | Ascorbic Acid | Found in food, supplements, and body fluids |
| Oxidized Form | Dehydroascorbic Acid | Can be reduced back to active form |
Functions of Ascorbic Acid (Vitamin C)
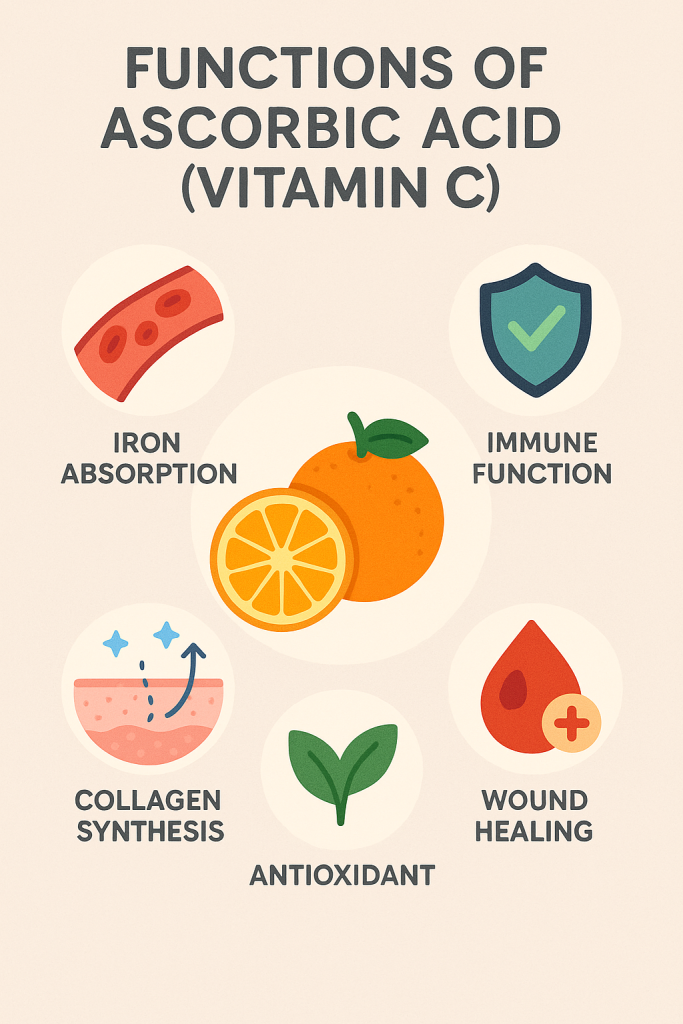
Vitamin C plays a vital role in multiple biochemical and physiological functions:
1. Antioxidant Protection
- Neutralizes free radicals, preventing oxidative stress.
- Regenerates Vitamin E and glutathione, enhancing antioxidant capacity.
2. Collagen Synthesis (Skin, Joints, and Wound Healing)
- Essential for the production of collagen, a structural protein in skin, bones, tendons, and blood vessels.
- Promotes faster wound healing and tissue repair.
- Prevents skin aging and wrinkles.
3. Immune System Support
- Enhances white blood cell function, improving immunity.
- Reduces the severity and duration of common colds.
- Supports antiviral and antibacterial defenses.
4. Iron Absorption and Anemia Prevention
- Increases non-heme iron absorption from plant-based foods.
- Prevents iron deficiency anemia.
5. Cardiovascular Health
- Reduces blood pressure and strengthens blood vessels.
- Lowers LDL (bad cholesterol) and triglycerides.
6. Brain Function and Mental Health
- Helps in the production of neurotransmitters (serotonin, dopamine).
- Reduces the risk of neurodegenerative diseases (Alzheimer’s, Parkinson’s).
Sources of Ascorbic Acid (Vitamin C)
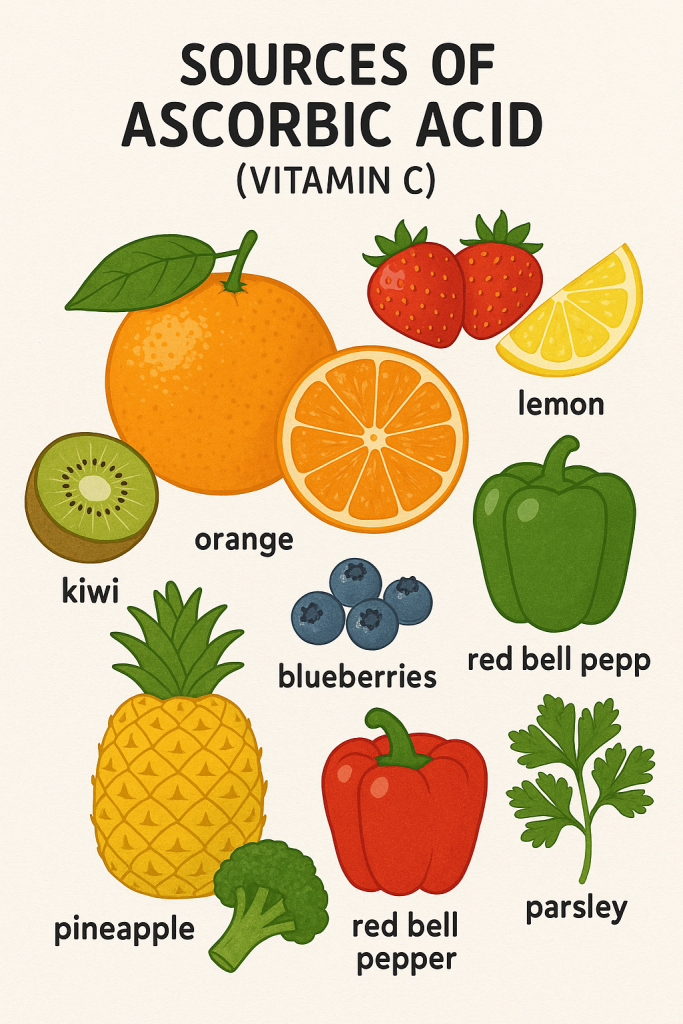
Vitamin C is primarily found in fruits and vegetables.
Rich Natural Sources
1. Fruits
- Citrus Fruits: Oranges, lemons, limes, grapefruits.
- Berries: Strawberries, blueberries, raspberries.
- Tropical Fruits: Pineapple, mango, papaya, guava.
- Other Fruits: Kiwi, watermelon, cantaloupe.
2. Vegetables
- Leafy Greens: Spinach, kale, Swiss chard.
- Cruciferous Vegetables: Broccoli, Brussels sprouts, cauliflower.
- Bell Peppers (Red and Yellow): One of the highest sources.
- Tomatoes, Potatoes, and Sweet Potatoes.
3. Fortified Foods
- Breakfast cereals.
- Juices.
- Vitamin C-enriched beverages.
Ascorbic Acid Supplements
- Available as tablets, chewable forms, and effervescent powders.
- Used for preventing deficiency, boosting immunity, and reducing oxidative stress.
Recommended Dietary Allowance (RDA) of Ascorbic Acid (Vitamin C)
The RDA for Vitamin C is measured in milligrams (mg/day).
| Age Group | RDA (mg/day) | Upper Limit (UL) (mg/day) |
|---|---|---|
| Infants (0-6 months) | 40 mg | Not established |
| Infants (7-12 months) | 50 mg | Not established |
| Children (1-3 years) | 15 mg | 400 mg |
| Children (4-8 years) | 25 mg | 650 mg |
| Children (9-13 years) | 45 mg | 1200 mg |
| Adolescents (14-18 years, male) | 75 mg | 1800 mg |
| Adolescents (14-18 years, female) | 65 mg | 1800 mg |
| Adults (19+ years, male) | 90 mg | 2000 mg |
| Adults (19+ years, female) | 75 mg | 2000 mg |
| Pregnant Women | 85 mg | 2000 mg |
| Lactating Women | 120 mg | 2000 mg |
Note:
- Smokers need an additional 35 mg/day due to increased oxidative stress.
- Upper Limit (UL) is 2000 mg/day to prevent toxicity.
Ascorbic Acid (Vitamin C) Deficiency and Toxicity
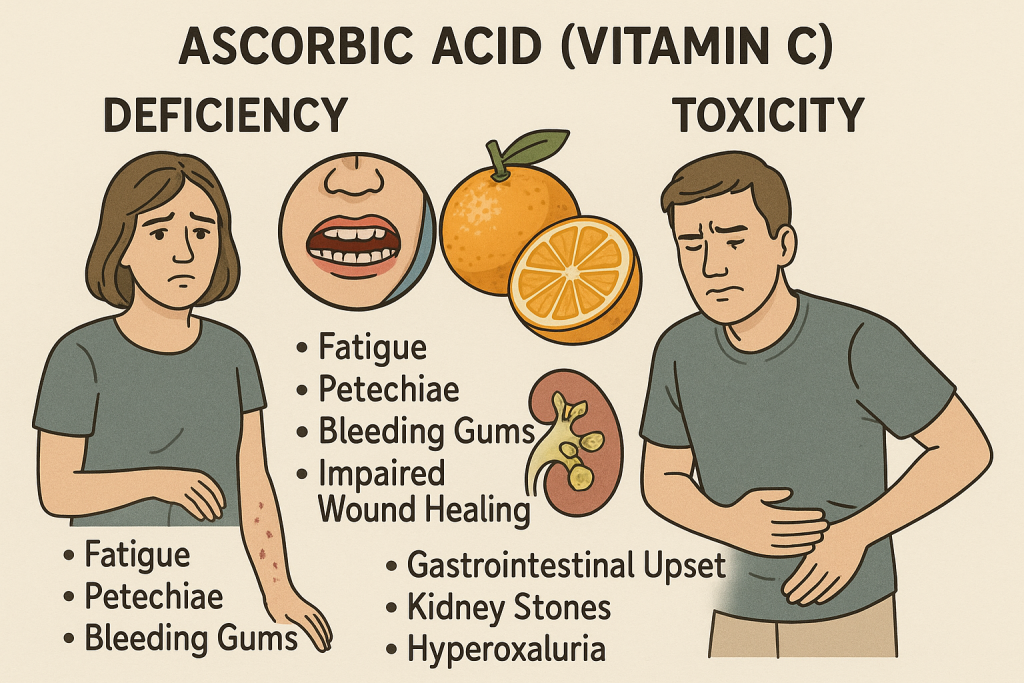
Deficiency Disorders
Vitamin C deficiency is common in malnourished individuals, alcoholics, and smokers.
1. Scurvy (Severe Deficiency)
- Bleeding gums, tooth loss.
- Poor wound healing, bruising easily.
- Fatigue, weakness, joint pain.
- Dry skin, hair loss.
2. Mild Deficiency Symptoms
- Frequent infections and colds.
- Anemia due to poor iron absorption.
- Skin dryness and premature aging.
- Slow wound healing.
At-Risk Groups for Deficiency
- Elderly individuals (low dietary intake).
- Smokers (higher oxidative stress).
- Alcoholics and drug users.
- Pregnant and breastfeeding women (higher demand).
- People with malabsorption disorders (Crohn’s disease, celiac disease).
Toxicity (Hypervitaminosis C)
Vitamin C toxicity is rare because excess amounts are excreted in urine. However, very high doses (above 2000 mg/day) can cause:
Symptoms of Excess Intake
- Diarrhea and stomach cramps.
- Kidney stones (due to increased oxalate production).
- Nausea and bloating.
- Iron overload in people with hemochromatosis.
Safe Limits:
- Do not exceed 2000 mg/day unless prescribed.
Comparison of Ascorbic Acid Forms
| Aspect | Ascorbic Acid (Natural) | Synthetic Ascorbic Acid (Supplement) |
|---|---|---|
| Sources | Citrus fruits, vegetables | Tablets, powders, injections |
| Function | Antioxidant, immune booster, collagen synthesis | Used for immune support and deficiency treatment |
| Absorption | High from food sources | High but may cause mild GI issues in excess |
| Toxicity Risk | Low (excreted in urine) | Possible GI distress at high doses |
Role of Ascorbic Acid in Nursing and Healthcare
Nurses play a key role in preventing, identifying, and managing Vitamin C deficiency.
1. Identifying At-Risk Patients
- Malnourished individuals, smokers, pregnant women, elderly.
- Patients with bleeding gums, easy bruising, or slow wound healing.
2. Administering Vitamin C Supplements
- Oral supplements for mild deficiency.
- IV Vitamin C for severe cases or wound healing.
3. Educating Patients
- Encouraging a diet rich in citrus fruits, bell peppers, and leafy greens.
- Advising smokers and pregnant women on increased Vitamin C needs.
- Warning against high-dose supplementation and potential kidney stone risk.
4. Managing Vitamin C Toxicity
- Monitoring patients on high-dose therapy for GI discomfort.
- Adjusting dosages if necessary.
Summary of Ascorbic Acid (Vitamin C)
| Aspect | Details |
|---|---|
| Classification | Water-Soluble Vitamin |
| Forms | Ascorbic Acid, Dehydroascorbic Acid |
| Functions | Antioxidant, immune support, collagen synthesis, wound healing, iron absorption |
| Sources | Citrus fruits, vegetables, fortified foods, supplements |
| RDA | 90 mg/day (men), 75 mg/day (women), 85-120 mg/day (pregnant/lactating) |
| Deficiency | Scurvy, bleeding gums, weak immunity, anemia |
| Toxicity | GI issues, kidney stones, iron overload |