BSC SEM 1 UNIT 2 NURSING FOUNDATION 1
UNIT 2 Health Care delivery Systems
Introduction to Health Care Delivery Systems
Definition of Health Care Delivery System
The health care delivery system refers to the organized way in which health care services are provided to the population. It encompasses institutions, resources, policies, and personnel involved in delivering preventive, curative, and rehabilitative health services.
Objectives of Health Care Delivery System
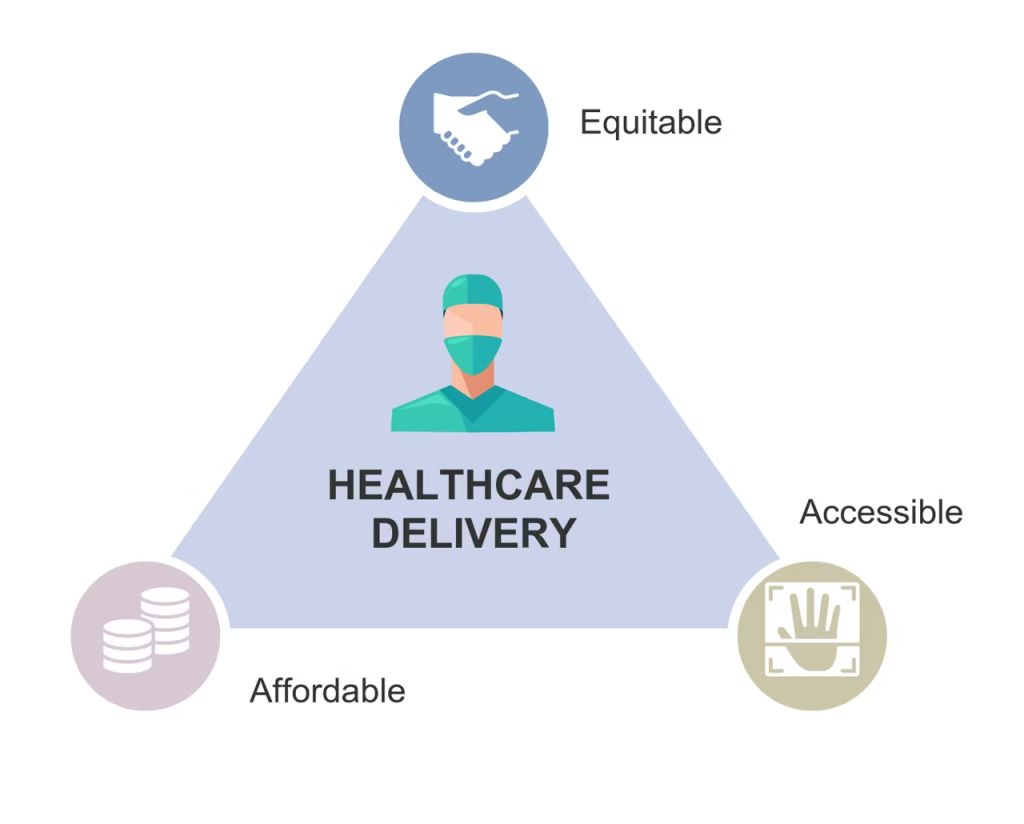
- To provide equitable and accessible health care services to all individuals, regardless of socio-economic status.
- To promote health and prevent diseases through primary health care services.
- To ensure quality and efficiency in treatment and patient care.
- To integrate health services at primary, secondary, and tertiary levels.
- To focus on holistic patient care through multidisciplinary approaches.
Levels of Health Care Delivery System
- Primary Level: Basic health services such as immunization, maternal and child health care, and general outpatient care.
- Secondary Level: Specialized medical care provided in district hospitals and community health centers.
- Tertiary Level: Advanced medical services in multi-specialty hospitals and medical research institutes.
Components of Health Care Delivery System
- Public Sector: Government-funded health programs, hospitals, and health centers.
- Private Sector: Private hospitals, clinics, and diagnostic centers.
- Voluntary and Non-Governmental Organizations (NGOs): Organizations involved in health promotion and outreach services.
- Traditional and Alternative Medicine: Ayurvedic, Homeopathy, and other indigenous practices.
Importance of Health Care Delivery System in Nursing
- Nurses play a critical role in delivering patient-centered care.
- They serve as liaisons between patients and health care providers.
- Nurses participate in health education and disease prevention programs.
- They ensure continuity of care from hospitals to communities.
Challenges in Health Care Delivery
- Shortage of healthcare professionals
- Inadequate health infrastructure
- High cost of medical treatment
- Limited access in rural areas
- Rising burden of chronic diseases
Levels of Illness Prevention: Primary Prevention (Health Promotion)
Introduction
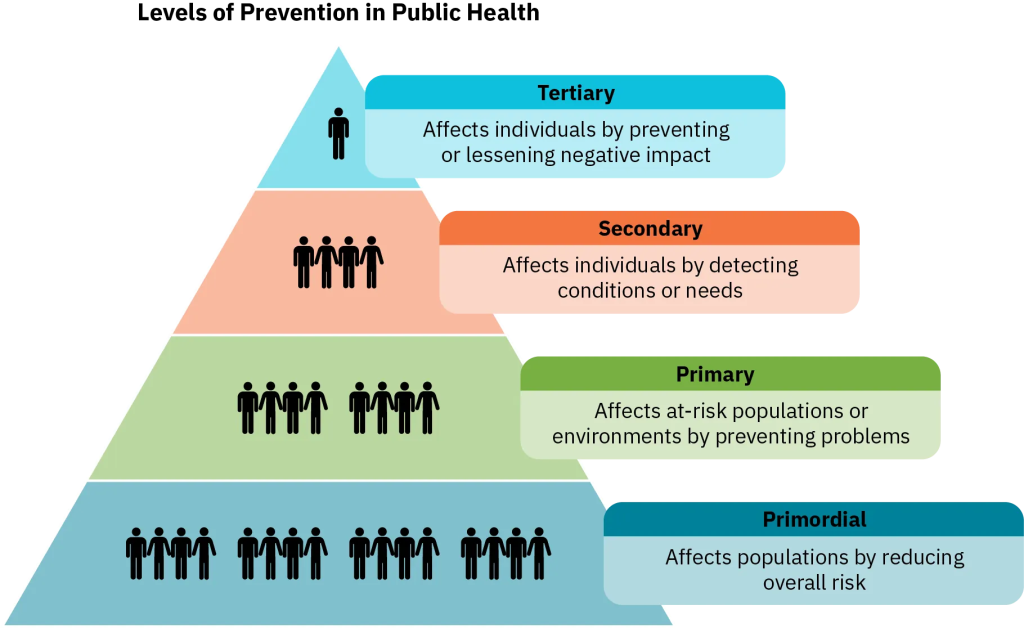
Illness prevention refers to measures taken to prevent diseases and promote overall well-being. It is categorized into three levels:
- Primary Prevention (Health Promotion & Specific Protection)
- Secondary Prevention (Early Diagnosis & Prompt Treatment)
- Tertiary Prevention (Rehabilitation & Restoration)
Among these, primary prevention is the first line of defense, focusing on preventing diseases before they occur. It includes health promotion and specific protection
Primary Prevention: Health Promotion
Definition
Primary prevention involves proactive measures to promote health, prevent diseases, and enhance overall well-being before any illness occurs. It aims to modify lifestyle, behavior, and environmental factors to reduce the risk of disease.
Objectives of Primary Prevention
- To promote positive health behaviors and prevent the onset of diseases.
- To educate individuals and communities on maintaining a healthy lifestyle.
- To reduce risk factors that contribute to chronic and communicable diseases.
- To ensure a safe and healthy environment for all individuals.
Components of Primary Prevention: Health Promotion
1. Health Education
- Spreading awareness about healthy lifestyles, balanced nutrition, exercise, and hygiene.
- Encouraging safe sexual practices to prevent sexually transmitted diseases (STDs).
- Providing information on mental health, stress management, and emotional well-being.
- Teaching proper posture, ergonomics, and injury prevention at workplaces.
2. Nutritional Interventions
- Promoting healthy eating habits and a well-balanced diet.
- Encouraging breastfeeding for infant nutrition.
- Addressing malnutrition, obesity, and vitamin deficiencies through dietary counseling.
3. Physical Activity and Exercise
- Encouraging regular physical activity such as walking, jogging, or yoga.
- Preventing sedentary lifestyle-related diseases like obesity, diabetes, and cardiovascular diseases.
4. Lifestyle Modifications
- Tobacco cessation programs to prevent lung diseases and cancers.
- Alcohol and substance abuse prevention through community programs.
- Sleep hygiene education for better physical and mental health.
5. Mental Health Promotion
- Stress management techniques like meditation, relaxation therapy, and mindfulness.
- Providing counseling and psychological support to prevent depression and anxiety.
- Encouraging social support networks for mental well-being.
6. Environmental and Occupational Health Measures
- Ensuring clean drinking water and sanitation to prevent waterborne diseases.
- Promoting pollution control measures to reduce respiratory illnesses.
- Implementing workplace safety protocols to prevent occupational hazards.
7. Immunization and Specific Protection
- Vaccination programs for diseases like measles, polio, hepatitis, and COVID-19.
- Providing insecticide-treated nets for malaria prevention.
- Encouraging use of helmets and seat belts to prevent injuries.
Examples of Primary Prevention
- School-based nutrition education programs.
- Community smoking cessation campaigns.
- Organizing yoga and fitness camps.
- Encouraging hand hygiene and sanitation programs.
- Promoting safe drinking water and environmental sanitation.
Importance of Primary Prevention
- Reduces the burden on healthcare systems by preventing diseases before they require medical intervention.
- Improves quality of life by maintaining overall health and well-being.
- Decreases healthcare costs by reducing hospital admissions and treatments.
- Empowers individuals and communities to take charge of their health.
Secondary Prevention: Early Diagnosis & Prompt Treatment
Introduction
Secondary prevention focuses on early detection and immediate intervention to halt the progression of diseases or conditions. It involves screening, early diagnosis, and timely treatment to reduce the impact of a disease before it causes significant health issues.
Definition
Secondary prevention refers to strategies that detect diseases at an early stage and provide prompt treatment to prevent complications, disability, or death.
Objectives of Secondary Prevention
- To detect diseases early before symptoms become severe.
- To provide prompt and effective treatment to stop disease progression.
- To reduce the severity and duration of illness through early intervention.
- To prevent complications and limit disability.
- To promote better health outcomes by improving survival rates.
Components of Secondary Prevention
1. Screening and Early Diagnosis
Screening involves medical tests and procedures to identify diseases in individuals who may not yet show symptoms. Common screening methods include:
- Blood pressure screening to detect hypertension.
- Blood glucose tests to identify diabetes.
- Mammography for early detection of breast cancer.
- Pap smear test for cervical cancer screening.
- Lipid profile tests for early detection of heart disease.
- Tuberculosis screening using Mantoux or sputum tests.
- Vision and hearing tests to detect sensory impairments.
- Regular dental check-ups to prevent oral diseases.
2. Early Treatment and Medical Interventions
Once a disease is detected, immediate treatment is necessary to prevent further progression. Examples include:
- Antibiotic therapy for bacterial infections.
- Insulin or oral hypoglycemic agents for early-stage diabetes.
- Lifestyle modifications and medications for hypertension and heart disease.
- Surgical interventions when necessary (e.g., tumor removal in early-stage cancer).
3. Case Finding
Case finding refers to actively searching for undiagnosed cases in at-risk populations. This is commonly used in:
- Contact tracing for infectious diseases like tuberculosis, HIV, and COVID-19.
- Community outreach programs for identifying undiagnosed chronic diseases.
- Workplace health check-ups to detect occupational illnesses.
4. Preventing Disease Progression
- Monitoring and regular follow-ups for high-risk patients.
- Lifestyle counseling to prevent complications in people diagnosed with chronic conditions.
- Providing early rehabilitation (e.g., physiotherapy for stroke patients).
Examples of Secondary Prevention
- Blood sugar monitoring to detect diabetes early.
- Annual health check-ups for early identification of risk factors.
- Use of ECG (Electrocardiogram) to detect heart disease.
- Routine eye exams to prevent blindness in diabetic patients.
- Screening pregnant women for gestational diabetes and anemia.
- Testing newborns for congenital diseases (e.g., neonatal screening for hypothyroidism).
Importance of Secondary Prevention
- Reduces morbidity and mortality by detecting diseases in early stages.
- Lowers healthcare costs by preventing the need for advanced treatments.
- Improves the quality of life by preventing complications.
- Increases life expectancy through timely intervention.
- Reduces disease burden on healthcare systems.
Tertiary Prevention: Rehabilitation and Restoration
Introduction
Tertiary prevention is the final level of disease prevention and focuses on reducing disability, restoring function, and improving quality of life after a disease has already caused damage. It includes rehabilitation, physical therapy, psychological support, and social integration.
Definition
Tertiary prevention refers to measures taken to reduce complications, manage chronic diseases, and prevent further deterioration in individuals who already have a disease or disability.
Objectives of Tertiary Prevention
- To prevent complications and long-term disabilities.
- To provide rehabilitation services for individuals recovering from illness or injury.
- To help individuals regain maximum functional capacity.
- To promote social and psychological well-being.
- To improve the quality of life for those with chronic diseases or disabilities.
Components of Tertiary Prevention
1. Medical and Surgical Treatment
- Long-term medication management for chronic diseases like diabetes, hypertension, and arthritis.
- Surgical interventions (e.g., joint replacement for severe arthritis, cardiac bypass surgery for heart disease).
- Pain management strategies (e.g., opioids for cancer pain, physiotherapy for back pain).
2. Rehabilitation Services
- Physical rehabilitation:
- Physiotherapy for stroke or spinal cord injury patients.
- Prosthetic limb training for amputees.
- Occupational therapy:
- Helping patients regain daily life skills after injury or illness.
- Speech therapy:
- For patients with communication difficulties after a stroke or neurological disorder.
3. Psychological and Emotional Support
- Counseling and psychotherapy for patients suffering from depression, anxiety, or PTSD.
- Support groups for individuals with chronic illnesses like cancer, HIV/AIDS, or mental health disorders.
4. Social and Community Support
- Vocational training programs to help disabled individuals reintegrate into the workforce.
- Social work interventions to provide financial aid, legal help, and family support.
- Community-based rehabilitation programs for people with disabilities.
5. Disease Management and Preventing Further Complications
- Regular follow-ups and monitoring to prevent disease progression.
- Lifestyle modifications and patient education (e.g., diet and exercise plans for heart disease).
- Surgical and assistive devices (e.g., pacemakers for cardiac patients, mobility aids for paralysis).
Examples of Tertiary Prevention
- Cardiac rehabilitation after a heart attack or stroke.
- Physiotherapy and assistive devices for spinal cord injury patients.
- Dialysis for chronic kidney disease.
- Chemotherapy and radiation therapy for cancer patients.
- Long-term management of mental illnesses like schizophrenia and bipolar disorder.
Importance of Tertiary Prevention
- Improves the quality of life by reducing pain and discomfort.
- Enhances functional independence through rehabilitation and therapy.
- Prevents disease progression and complications.
- Reduces long-term healthcare costs by minimizing hospitalizations.
- Supports emotional well-being by addressing mental health concerns.
Levels of Care : Primary Health Care (PHC)
Introduction
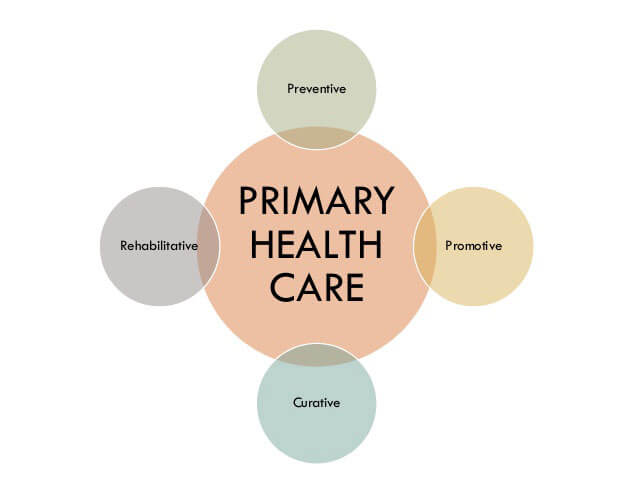
Health care services are categorized into three levels: Primary, Secondary, and Tertiary Care. Among these, Primary Health Care (PHC) is the first and most fundamental level, focusing on preventive, promotive, curative, and rehabilitative health services at the community level.
Definition of Primary Health Care (PHC)
Primary health care is the first level of contact between individuals and the healthcare system. It provides essential, accessible, and affordable healthcare services to the community.
Objectives of Primary Health Care
- To provide basic health care services to individuals and families.
- To promote health and prevent diseases through education and immunization.
- To ensure equitable access to health services in rural and urban areas.
- To integrate preventive, promotive, curative, and rehabilitative care.
- To reduce the burden on secondary and tertiary care hospitals by treating minor ailments at the primary level.
Key Features of Primary Health Care
- Accessibility: Healthcare services are available to all, regardless of economic or social status.
- Community-Based: Services are provided close to where people live.
- Preventive Focus: Emphasizes immunization, health education, and disease prevention.
- Equity: Aims to provide healthcare services to underserved populations.
- Comprehensive Approach: Integrates medical, social, and environmental aspects of health.
Components of Primary Health Care
1. Health Education
- Educating the community about hygiene, sanitation, and nutrition.
- Awareness programs on maternal and child health.
- Information on the prevention of communicable and non-communicable diseases.
2. Promotion of Proper Nutrition
- Encouraging a balanced diet to prevent malnutrition.
- Providing supplementary nutrition in schools and Anganwadi centers.
- Promoting breastfeeding and infant feeding practices.
3. Adequate Supply of Safe Water and Basic Sanitation
- Ensuring clean drinking water and waste disposal.
- Promoting hand hygiene and environmental cleanliness.
- Preventing waterborne diseases like cholera and typhoid.
4. Maternal and Child Health Care (MCH) Including Family Planning
- Antenatal and postnatal care to reduce maternal mortality.
- Child immunization programs to prevent infectious diseases.
- Family planning services to control population growth.
5. Immunization Against Major Infectious Diseases
- Vaccination programs such as BCG, Polio, DPT, MMR, Hepatitis B under the Universal Immunization Program (UIP).
- Immunization of pregnant women with Tetanus Toxoid (TT).
- Mass vaccination campaigns for disease eradication.
6. Prevention and Control of Locally Endemic Diseases
- Surveillance and control measures for diseases like malaria, dengue, tuberculosis, and leprosy.
- Vector control programs to reduce mosquito-borne diseases.
7. Treatment of Common Diseases and Injuries
- First-aid and management of minor injuries.
- Treatment of common ailments like diarrhea, respiratory infections, and skin diseases.
- Referral of complicated cases to secondary or tertiary healthcare facilities.
8. Provision of Essential Drugs
- Availability of life-saving and essential medicines at Primary Health Centers (PHCs) and Sub-Centers.
- Promoting the use of generic medicines under the Jan Aushadhi Scheme.
Structure of Primary Health Care in India
1. Sub-Center (SC)
- The first point of contact between the healthcare system and the community.
- Covers 5,000 people in plains and 3,000 people in hilly/tribal areas.
- Managed by an Auxiliary Nurse Midwife (ANM) and a Multipurpose Health Worker (MPHW).
- Provides immunization, maternal and child health care, and basic treatments.
2. Primary Health Center (PHC)
- Covers 30,000 people in rural areas and 20,000 in tribal areas.
- Acts as a referral unit for sub-centers.
- Staffed with a medical officer, staff nurses, and health workers.
- Provides outpatient services, maternal and child care, and disease control programs.
3. Community Health Center (CHC)
- Covers 1,20,000 people in rural areas.
- 30-bedded hospital with four medical specialists (Physician, Surgeon, Pediatrician, and Gynecologist).
- Acts as a referral unit for PHCs and provides minor surgeries and emergency care.
Examples of Primary Health Care Services
- Anganwadi centers providing maternal and child care.
- Village health camps offering free medical check-ups.
- Mobile health units visiting remote areas.
- School health programs providing deworming and vision screening.
Importance of Primary Health Care
- Reduces the burden on hospitals by treating minor illnesses at the primary level.
- Prevents the spread of diseases through vaccinations and health education.
- Improves overall community health by promoting nutrition and hygiene.
- Cost-effective and accessible for all sections of society.
Levels of Care: Secondary Health Care

Introduction
Secondary health care is the second level of the health care system, providing specialized medical services to patients referred from primary health care. It includes hospitals with specialized departments, diagnostic facilities, and trained medical professionals who treat patients with moderate to severe health conditions.
Definition of Secondary Health Care
Secondary health care refers to specialized medical services provided in district hospitals, community health centers, and referral hospitals where patients receive treatment for conditions that cannot be managed at the primary health care level.
Objectives of Secondary Health Care
- To provide specialized medical treatment for moderate to severe illnesses.
- To diagnose and treat health conditions that require hospitalization or advanced care.
- To offer emergency and surgical services.
- To serve as a referral point from primary health centers.
- To provide early interventions to prevent complications and mortality.
Key Features of Secondary Health Care
- Specialized Services – Includes medical specialties such as internal medicine, pediatrics, gynecology, and surgery.
- Hospital-Based Care – Patients are admitted for diagnosis, treatment, or surgery.
- Referral System – Patients are referred from primary health care centers.
- Emergency and Trauma Care – Provides immediate medical intervention for accidents and critical conditions.
- Advanced Diagnostic Facilities – Includes imaging (X-rays, CT scans), laboratory tests, and pathology services.
Components of Secondary Health Care
1. Outpatient and Inpatient Services
- Outpatient services: Specialized consultations without admission.
- Inpatient services: Hospitalization for medical conditions requiring observation and treatment.
2. Specialized Medical Care
- Medical specialties like internal medicine, cardiology, neurology, gastroenterology, dermatology.
- Surgical services like general surgery, orthopedic surgery, ENT, ophthalmology.
- Obstetrics and gynecology: Delivery care, high-risk pregnancy management.
3. Diagnostic and Laboratory Services
- Pathological tests – Blood tests, urine analysis, biopsy.
- Radiology – X-rays, CT scans, MRI, ultrasound.
- Cardiac investigations – ECG, echocardiography.
- Endoscopy and colonoscopy – For digestive tract diagnosis.
4. Emergency and Trauma Care
- Management of accidents and trauma – Road traffic injuries, burns, fractures.
- Cardiac emergencies – Heart attacks, arrhythmias.
- Acute medical conditions – Stroke, respiratory distress, poisoning cases.
5. Surgical and Maternity Services
- Minor and major surgical procedures – Appendectomy, gallbladder removal, cesarean section.
- Management of childbirth complications – Postpartum hemorrhage, fetal distress.
6. Intensive Care Unit (ICU) and Critical Care
- ICU care for critically ill patients.
- Ventilator support and advanced monitoring.
- Post-operative care for high-risk surgical patients.
7. Rehabilitation Services
- Post-operative physiotherapy for stroke and orthopedic patients.
- Mental health and counseling services for psychiatric disorders.
Structure of Secondary Health Care in India
1. Community Health Centers (CHC)
- Covers 1,20,000 population in rural areas.
- 30-bedded hospital with four specialists (Physician, Surgeon, Pediatrician, Gynecologist).
- Provides obstetric care, minor surgeries, and diagnostic services.
- Acts as a referral unit for Primary Health Centers (PHCs).
2. District Hospitals
- Covers 500,000 to 1 million people.
- 100-300 bed capacity.
- Staffed with specialists in multiple medical fields.
- Provides advanced treatment, diagnostics, and emergency care.
Examples of Secondary Health Care
- Management of pneumonia requiring hospitalization.
- Treatment of diabetic complications (e.g., foot ulcers, neuropathy).
- Surgical removal of gallbladder stones or kidney stones.
- Blood transfusions for anemia or sickle cell disease.
- Treatment of heart attack in a cardiac care unit.
- Orthopedic surgeries for fractures and joint replacements.
Importance of Secondary Health Care
- Bridges the gap between primary and tertiary health care.
- Provides life-saving interventions for emergency cases.
- Reduces the burden on tertiary hospitals by treating moderately severe conditions at the district level.
- Ensures access to specialized care for the general population.
- Improves health outcomes through early intervention and treatment.
Levels of Care: Tertiary Health Care
Introduction
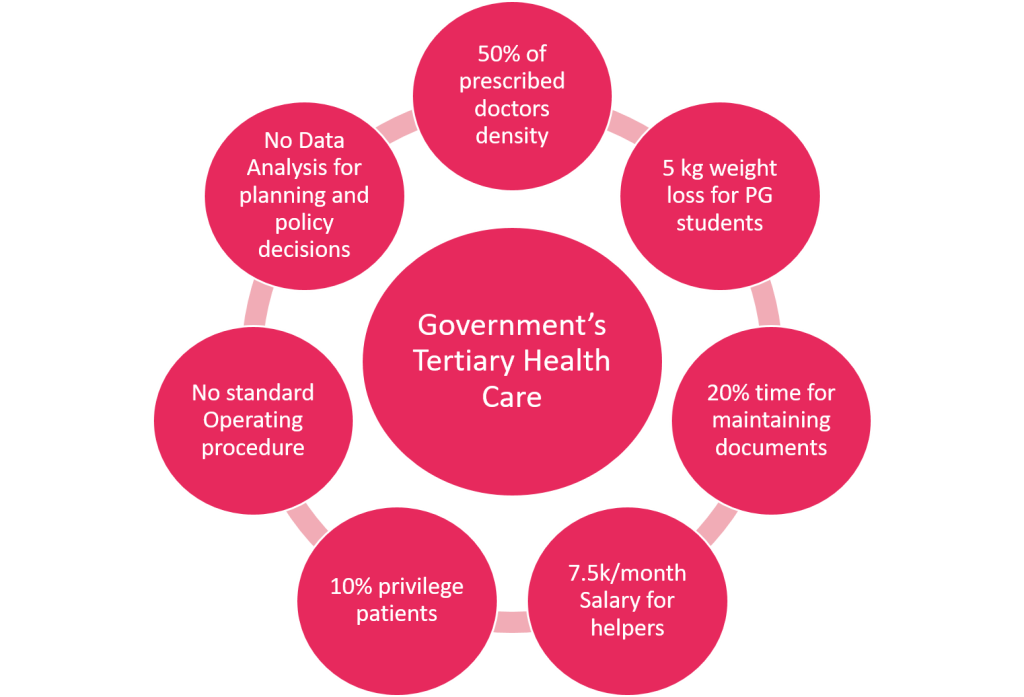
Tertiary health care is the highest level of medical care that provides specialized, advanced, and complex treatments for critical illnesses and life-threatening conditions. It includes multi-specialty hospitals, research institutions, and super-specialty medical centers that offer cutting-edge diagnostic, surgical, and therapeutic interventions.
Definition of Tertiary Health Care
Tertiary health care refers to highly specialized medical care provided in well-equipped hospitals with advanced technology and expert medical professionals to treat severe, complex, or rare medical conditions.
Objectives of Tertiary Health Care
- To provide advanced and specialized treatments for life-threatening diseases.
- To manage complex surgical and medical conditions requiring multidisciplinary care.
- To offer state-of-the-art diagnostic and therapeutic interventions.
- To conduct research and innovation in medical sciences.
- To serve as referral centers for secondary health care facilities.
Key Features of Tertiary Health Care
- Highly Specialized Medical Care – Includes services like neurosurgery, organ transplants, and oncology.
- Cutting-Edge Technology – Advanced diagnostic tools (MRI, PET scans), robotic surgeries, and precision medicine.
- Multidisciplinary Approach – Teams of specialists work together for comprehensive patient management.
- Medical Research and Training – Centers for medical advancements and education.
- Referral-Based Care – Patients are referred from primary and secondary health care facilities.
Components of Tertiary Health Care
1. Advanced Medical and Surgical Services
- Neurosurgery and Neurology – Brain tumor removal, stroke management, epilepsy surgery.
- Cardiac Surgery and Cardiology – Coronary artery bypass grafting (CABG), angioplasty, pacemaker implantation.
- Organ Transplants – Kidney, liver, heart, and lung transplants.
- Cancer Treatment (Oncology) – Chemotherapy, radiation therapy, immunotherapy, and precision medicine.
2. Intensive and Critical Care Units (ICU)
- Neonatal Intensive Care Unit (NICU) for premature and critically ill newborns.
- Pediatric Intensive Care Unit (PICU) for critically ill children.
- Medical and Surgical ICUs for post-operative and severely ill patients.
- Burn Units for treating severe burn injuries.
3. Super-Specialty Diagnostic and Imaging Services
- Magnetic Resonance Imaging (MRI), Positron Emission Tomography (PET) scans.
- Genetic and molecular diagnostics for inherited diseases.
- Interventional radiology for minimally invasive procedures.
4. Advanced Therapeutic Interventions
- Robotic and minimally invasive surgeries for precision treatment.
- Dialysis and renal replacement therapy for kidney failure.
- Stem cell therapy and regenerative medicine for rare disorders.
- Hormonal and metabolic therapies for endocrine disorders.
5. Medical Research and Education
- Clinical trials and drug development for new treatments.
- Medical education and training programs for specialists.
- Public health research on emerging diseases and treatments.
Structure of Tertiary Health Care in India
1. Government Tertiary Hospitals
- All India Institute of Medical Sciences (AIIMS).
- Postgraduate Institute of Medical Education and Research (PGIMER).
- National Institute of Mental Health and Neurosciences (NIMHANS).
- Regional Cancer Centers and Cardiac Institutes.
2. Private Super-Specialty Hospitals
- Apollo Hospitals, Fortis Hospitals, Narayana Health, Max Healthcare.
- Multi-specialty corporate hospitals offering international standards of care.
3. Specialized Medical Research Centers
- Indian Council of Medical Research (ICMR).
- National Cancer Institute (NCI).
- Biotechnology and stem cell research centers.
Examples of Tertiary Health Care
- Open-heart surgery for congenital heart defects.
- Bone marrow transplant for leukemia patients.
- Gamma knife radiosurgery for brain tumors.
- Deep brain stimulation (DBS) for Parkinson’s disease.
- Treatment of multi-drug resistant tuberculosis (MDR-TB).
- Liver transplant for end-stage liver disease.
Importance of Tertiary Health Care
- Provides life-saving treatments for critical and rare diseases.
- Uses the latest technology for accurate diagnosis and precision treatment.
- Enhances survival rates for high-risk patients.
- Advances medical research and education for continuous improvement in healthcare.
- Acts as a referral center for secondary and primary health care services.
Types of Health Care Agencies/Services: Hospitals

Introduction
Hospitals are the backbone of the healthcare system, providing diagnostic, curative, rehabilitative, and preventive health services. They cater to a wide range of patient needs, from routine medical care to specialized treatment and emergency interventions.
Definition of a Hospital
A hospital is a healthcare institution that provides treatment, nursing care, and medical services to patients. It is staffed with doctors, nurses, paramedical staff, and support personnel, equipped with diagnostic, therapeutic, and surgical facilities to manage various health conditions.
Objectives of Hospitals
- To provide medical care for acute and chronic illnesses.
- To perform surgeries and specialized treatments.
- To offer emergency and trauma care for critical conditions.
- To provide preventive healthcare services such as immunizations and health screenings.
- To conduct medical research and education for healthcare professionals.
- To promote rehabilitation and palliative care for patients with long-term illnesses.
Classification of Hospitals
Hospitals can be classified based on ownership, size, services, and specialization.
1. Based on Ownership
A. Government/Public Hospitals
- Owned and operated by central, state, or local governments.
- Provide free or low-cost medical care.
- Examples: AIIMS, Civil Hospitals, Military Hospitals.
- Funded through government budgets and national health programs.
B. Private Hospitals
- Owned by individuals, trusts, or corporations.
- Provide paid medical services.
- Examples: Apollo Hospitals, Fortis Healthcare, Max Hospitals.
- Often have better infrastructure, advanced technology, and shorter waiting times.
C. Non-Governmental Organization (NGO) Hospitals
- Run by charitable organizations, religious groups, or trusts.
- Provide subsidized healthcare to underprivileged communities.
- Examples: Mission Hospitals, Red Cross Hospitals.
D. Military and Defense Hospitals
- Operated by the armed forces to provide medical care to soldiers and their families.
- Examples: Military Hospital, Armed Forces Medical College (AFMC) Hospital.
2. Based on Size and Capacity
A. Primary Care Hospitals (Small Hospitals)
- Less than 50 beds.
- Provide basic healthcare services, minor surgeries, and outpatient care.
- Located in small towns and rural areas.
B. Secondary Care Hospitals (Medium-Sized Hospitals)
- 50 to 300 beds.
- Offer specialized care, including surgery, maternity services, and emergency care.
- Often include Community Health Centers (CHCs) and District Hospitals.
C. Tertiary Care Hospitals (Large Hospitals)
- More than 300 beds.
- Provide highly specialized medical care such as organ transplants, neurosurgery, and cancer treatment.
- Examples: AIIMS, PGIMER, Tata Memorial Hospital.
3. Based on Services Provided
A. General Hospitals
- Provide a wide range of healthcare services for all types of illnesses.
- Have departments like medicine, surgery, pediatrics, gynecology, orthopedics, and emergency care.
- Example: Civil Hospitals, District Hospitals.
B. Specialty Hospitals
- Focus on a specific field of medicine.
- Examples:
- Cardiac Hospitals – Narayana Health, Asian Heart Institute.
- Cancer Hospitals – Tata Memorial Hospital.
- Orthopedic Hospitals – Sancheti Hospital.
- Neurology Hospitals – NIMHANS.
C. Teaching and Research Hospitals
- Associated with medical colleges and universities.
- Train medical students, nurses, and healthcare professionals.
- Conduct clinical research and trials.
- Examples: AIIMS, JIPMER, KEM Hospital.
D. Rehabilitation Hospitals
- Provide long-term care for patients recovering from severe illness, stroke, trauma, or surgery.
- Offer physiotherapy, occupational therapy, and speech therapy.
E. Psychiatric Hospitals
- Specialize in the treatment of mental health disorders.
- Offer counseling, therapy, psychiatric medication, and rehabilitation.
- Example: NIMHANS, Institute of Mental Health.
F. Maternity and Childcare Hospitals
- Provide prenatal, delivery, postnatal, and pediatric care.
- Handle high-risk pregnancies and neonatal intensive care (NICU).
- Example: Fernandez Hospital, Rainbow Children’s Hospital.
G. Infectious Disease Hospitals
- Treat infectious diseases like tuberculosis (TB), COVID-19, and HIV/AIDS.
- Have isolation wards and specialized treatments.
H. Palliative and Hospice Care Hospitals
- Provide end-of-life care for terminally ill patients.
- Focus on pain management and emotional support.
- Example: Cancer Hospice Centers, Palliative Care Units.
Departments in a Hospital
1. Emergency and Trauma Care
- 24/7 care for accidents, heart attacks, strokes, and critical conditions.
2. Outpatient Department (OPD)
- Non-admitted patient care, including consultations and minor procedures.
3. Inpatient Department (IPD)
- Admitted patient care for medical or surgical treatment.
4. Intensive Care Unit (ICU)
- Critical care for seriously ill patients.
- Includes NICU (Neonatal ICU), PICU (Pediatric ICU), CCU (Cardiac ICU).
5. Operation Theaters (OT)
- Surgical procedures are performed with sterile conditions.
6. Laboratory and Diagnostic Services
- Includes blood tests, pathology, radiology (X-rays, CT scans, MRI), and genetic testing.
7. Pharmacy
- Dispenses medicines prescribed by doctors.
8. Physiotherapy and Rehabilitation Unit
- Physical and occupational therapy for recovering patients.
9. Medical Records Department
- Maintains patient history, reports, and treatment plans.
10. Administrative and Support Services
- Includes hospital management, housekeeping, and food services.
Functions of a Hospital
- Curative Services: Diagnosis and treatment of diseases.
- Preventive Services: Immunization, health screenings, and awareness programs.
- Emergency and Trauma Care: Critical interventions for life-threatening conditions.
- Rehabilitative Services: Post-surgical recovery, therapy, and palliative care.
- Teaching and Training: Educating medical students and nurses.
- Medical Research: Developing new treatments and conducting clinical trials.
Importance of Hospitals in Healthcare
- Provide life-saving treatments and emergency care.
- Improve public health through vaccinations and screenings.
- Reduce mortality rates by offering specialized care.
- Create employment for doctors, nurses, and medical professionals.
- Support medical advancements through research and innovation.
Types of Health Care Agencies/Services: Clinics

Introduction
Clinics are smaller healthcare facilities that provide outpatient medical services without requiring hospitalization. They offer preventive, diagnostic, and curative care, catering to general and specialized health needs.
Definition of a Clinic
A clinic is a healthcare facility that provides non-emergency medical services, including consultations, minor procedures, diagnostic tests, and preventive care, primarily on an outpatient basis. Clinics can be independent or attached to hospitals.
Objectives of Clinics
- To provide accessible and affordable primary healthcare services.
- To diagnose and treat minor illnesses and injuries.
- To offer preventive care, including vaccinations and screenings.
- To manage chronic diseases like diabetes and hypertension.
- To reduce the burden on hospitals by handling non-emergency cases.
- To serve as referral points for more complex medical cases.
Classification of Clinics
Clinics can be classified based on ownership, size, services provided, and specialization.
1. Based on Ownership
A. Government/Public Clinics
- Funded and operated by the government (national, state, or local).
- Provide free or low-cost healthcare services to the public.
- Located in rural, urban, and underserved areas.
- Example: Primary Health Centers (PHCs), Urban Health Centers (UHCs), and Mobile Clinics.
B. Private Clinics
- Owned by individual doctors, healthcare organizations, or private hospitals.
- Charge consultation and treatment fees.
- Offer personalized and specialized medical care.
- Example: Corporate health clinics, specialty medical centers, and private practice clinics.
C. Non-Governmental Organization (NGO) Clinics
- Run by charitable trusts, religious organizations, or non-profits.
- Provide low-cost or free healthcare to underserved populations.
- Example: Red Cross Clinics, Missionary Clinics, and Mobile Health Units.
D. Workplace or Corporate Clinics
- Set up within corporate offices, factories, or industrial areas.
- Provide on-site medical care for employees.
- Offer routine health check-ups, emergency first aid, and occupational health services.
- Example: Factory Health Clinics, IT Company Wellness Centers.
2. Based on Size and Capacity
A. Small Clinics
- Run by one or two doctors.
- Offer general medical consultations, minor treatments, and first aid.
- Example: Neighborhood Family Doctor Clinics.
B. Medium-Sized Clinics
- Staffed with multiple doctors and paramedical staff.
- Offer diagnostic tests, vaccinations, and chronic disease management.
- Example: Multi-specialty Clinics, Polyclinics.
C. Large Clinics
- Function like mini-hospitals with multiple departments and advanced medical services.
- Offer day-care surgeries, laboratory tests, and radiology services.
- Example: Private Specialty Clinics, Urban Health Centers (UHCs).
3. Based on Services Provided
A. General Clinics
- Provide basic healthcare, first aid, and minor illness treatment.
- Commonly known as family physician or general practitioner (GP) clinics.
- Example: Neighborhood GP Clinics, Urgent Care Centers.
B. Specialized Clinics
- Focus on specific medical specialties.
- Staffed by specialist doctors.
- Examples:
- Cardiology Clinics – Treat heart-related conditions.
- Orthopedic Clinics – Manage bone and joint disorders.
- Dermatology Clinics – Treat skin diseases and cosmetic issues.
- Endocrinology Clinics – Specialize in diabetes and hormonal disorders.
C. Polyclinics
- Multi-specialty clinics with various medical specialists under one roof.
- Provide diagnostic, therapeutic, and minor surgical procedures.
- Example: Urban Polyclinics with multiple doctors from different specialties.
D. Community Health Clinics
- Serve low-income groups, rural populations, and underprivileged communities.
- Provide maternal and child health care, vaccinations, and chronic disease management.
- Example: Government-run CHCs and NGO Clinics.
E. Walk-In and Urgent Care Clinics
- Provide immediate care for non-life-threatening conditions.
- No prior appointments needed.
- Treat minor injuries, infections, allergies, and flu symptoms.
- Example: 24-hour Walk-In Clinics, Emergency OPD Clinics.
F. Specialty Treatment Clinics
- Focus on specific treatments or procedures.
- Examples:
- Dialysis Clinics – For kidney failure patients.
- Fertility Clinics – Provide infertility treatments and IVF.
- Pain Management Clinics – Treat chronic pain conditions.
G. Rehabilitation Clinics
- Help patients recover from injuries, surgeries, or chronic illnesses.
- Provide physical therapy, occupational therapy, and speech therapy.
- Example: Physiotherapy Clinics, Stroke Recovery Centers.
H. Mental Health Clinics
- Provide counseling, psychiatric services, and therapy for mental illnesses.
- Offer substance abuse treatment and stress management programs.
- Example: Psychiatric Clinics, Addiction Recovery Centers.
I. Dental Clinics
- Specialize in oral health, tooth extractions, orthodontics, and cosmetic dentistry.
- Example: Dental Care Clinics, Orthodontic Centers.
J. Mobile Clinics
- Provide healthcare services in remote or underserved areas.
- Offer basic medical check-ups, vaccinations, and maternal care.
- Example: Rural Health Van, Mobile TB Screening Units.
Departments in a Large Clinic
1. Outpatient Consultation
- General physician consultations and specialist visits.
2. Diagnostic Laboratory
- Blood tests, urine analysis, and pathology tests.
3. Imaging and Radiology
- X-rays, ultrasound, ECG, and minor diagnostic imaging.
4. Minor Surgery and Procedures
- Wound suturing, dressing, and day-care surgeries.
5. Vaccination and Immunization Unit
- Routine childhood vaccinations, flu shots, and COVID-19 vaccines.
6. Physiotherapy and Rehabilitation
- Post-operative care, physical therapy, and pain management.
7. Pharmacy
- Dispenses prescribed medications and essential drugs.
Functions of Clinics
- Provide first-line medical care and prevent hospital overcrowding.
- Deliver preventive care like vaccinations and health screenings.
- Offer specialist consultations for specific health conditions.
- Manage chronic diseases like diabetes, hypertension, and asthma.
- Conduct minor surgeries and procedures without hospitalization.
- Serve as referral points for serious or complicated cases.
Examples of Clinic-Based Services
- A general physician treating cold, flu, and infections.
- A dermatology clinic providing acne and eczema treatment.
- An orthopedic clinic treating joint pain and fractures.
- A pediatric clinic offering child vaccinations and nutrition advice.
- A cardiology clinic managing hypertension and heart disease.
- A mental health clinic providing therapy for anxiety and depression.
Importance of Clinics in Healthcare
- Increase accessibility to healthcare in rural and urban areas.
- Reduce hospital burden by managing minor cases at the community level.
- Promote early detection and treatment of diseases.
- Improve public health through preventive and primary care.
- Save time and cost for patients by providing quick medical attention.
Types of Health Care Agencies/Services: Hospice Care

Introduction
Hospice care is a specialized form of healthcare focused on providing comfort, pain management, and emotional support to patients who are in the final stages of a terminal illness. Unlike curative treatments, hospice care prioritizes quality of life, dignity, and emotional well-being for both patients and their families.
Definition of Hospice Care
Hospice care is a compassionate approach to end-of-life care that provides medical, emotional, and psychological support to terminally ill patients. It is designed to help patients live as comfortably as possible during their remaining days, weeks, or months.
Objectives of Hospice Care
- To provide pain relief and symptom control for terminally ill patients.
- To enhance the quality of life rather than prolong it with aggressive treatments.
- To offer emotional and spiritual support to both the patient and their family.
- To support families with grief counseling before and after the patient’s passing.
- To respect the patient’s dignity and personal choices regarding end-of-life care.
Key Features of Hospice Care
- Patient-Centered Approach – Focuses on the patient’s comfort rather than curing the illness.
- Holistic Care – Addresses physical, emotional, spiritual, and psychological needs.
- Family Support – Provides counseling and bereavement support to family members.
- Home-Based or Facility-Based Care – Can be provided at home, in a hospice facility, or in a hospital.
- Interdisciplinary Team – Involves doctors, nurses, social workers, counselors, and chaplains.
Classification of Hospice Care
Hospice care can be classified based on setting, services provided, and funding sources.
1. Based on Setting
A. Home Hospice Care
- Most patients prefer to receive hospice care at home.
- Care is provided by visiting nurses, caregivers, and family members.
- Medical equipment like hospital beds, oxygen supplies, and pain relief medications are provided.
B. Inpatient Hospice Facilities
- Standalone hospice centers that provide 24/7 care.
- Ideal for patients who need continuous medical supervision.
- Provide a peaceful and comfortable environment for end-of-life care.
C. Hospice Care in Hospitals
- Some hospitals have hospice units for terminally ill patients.
- Provides access to advanced pain management and medical support.
D. Hospice Care in Nursing Homes
- Provides end-of-life care for elderly patients residing in long-term care facilities.
- Ensures patients receive comfort-focused care instead of aggressive treatments.
2. Based on Services Provided
A. Routine Home Care
- Patients receive regular visits from hospice nurses and caregivers at home.
- Medications and equipment are provided to manage symptoms.
B. Continuous (Crisis) Home Care
- For patients experiencing severe pain or distressing symptoms.
- Hospice nurses stay at the patient’s home for extended hours.
C. Inpatient Respite Care
- Short-term care (5 days max) provided in a hospice or hospital.
- Gives family caregivers a break while ensuring the patient receives proper care.
D. General Inpatient Hospice Care
- For patients with severe symptoms that cannot be managed at home.
- Care is provided in a hospice unit, hospital, or specialized facility.
3. Based on Funding Sources
A. Government-Funded Hospice Care
- Provided free or subsidized by the government.
- Examples: Medicare and Medicaid hospice programs in the USA, Ayushman Bharat Health Scheme in India.
B. Private Hospice Care
- Paid services offered by private healthcare providers.
- Often includes luxury hospice centers with personalized care.
C. Charitable/NGO Hospice Care
- Run by non-profit organizations or religious groups.
- Provides free or low-cost care to underprivileged patients.
- Example: Cancer Hospice Centers, Missionary Hospice Services.
Services Provided in Hospice Care
1. Pain and Symptom Management
- Relief from pain, breathlessness, nausea, and anxiety.
- Medications like opioids and sedatives are used for comfort.
- Oxygen therapy, physiotherapy, and nutrition support are provided.
2. Emotional and Psychological Support
- Counseling sessions for patients and families.
- Therapies like music, art, and pet therapy to ease stress.
- Support groups for coping with terminal illness.
3. Spiritual and Religious Support
- Helps patients find peace and meaning in their final days.
- Religious leaders or chaplains provide prayers, rituals, and end-of-life guidance.
4. Family and Caregiver Support
- Counseling and training for family members on how to care for the patient.
- Respite care to give caregivers a break.
5. Bereavement and Grief Support
- Helps family members cope with the loss of a loved one.
- Includes grief counseling, therapy, and memorial services.
Hospice vs. Palliative Care
| Feature | Hospice Care | Palliative Care |
|---|---|---|
| Focus | End-of-life comfort care | Symptom relief at any stage of illness |
| Treatment Goal | No curative treatments | Can include curative treatments |
| Where Provided | Home, hospice, hospital, nursing home | Hospital, home, long-term care facilities |
| Life Expectancy | For patients with 6 months or less to live | For patients at any stage of a serious illness |
| Family Support | Extensive family and bereavement support | Focus on patient care, but family support is also available |
Examples of Hospice Care Facilities
- Cancer Hospice Centers – For patients in the final stages of cancer.
- HIV/AIDS Hospice Homes – Provide end-of-life care for AIDS patients.
- Children’s Hospice Centers – Special facilities for terminally ill children.
Importance of Hospice Care
- Provides dignity and comfort in the final stages of life.
- Prevents unnecessary medical interventions and hospitalizations.
- Supports emotional, social, and spiritual needs.
- Reduces caregiver stress through respite care and counseling.
- Allows patients to spend their last days in peace.
Types of Health Care Agencies/Services: Rehabilitation Centers

Introduction
Rehabilitation centers are specialized healthcare facilities that focus on helping individuals recover from injuries, illnesses, surgeries, or substance abuse. They aim to restore physical, mental, and social well-being through structured therapy, medical support, and counseling.
Definition of Rehabilitation Centers
A rehabilitation center is a healthcare facility that provides physical, occupational, psychological, and medical therapies to help individuals regain independence and improve their quality of life after illness, injury, disability, or substance addiction.
Objectives of Rehabilitation Centers
- To restore physical and functional abilities after injury or illness.
- To provide therapy and counseling for addiction recovery.
- To help patients regain independence in daily activities.
- To improve psychological and emotional well-being.
- To integrate patients back into society and support employment readiness.
Key Features of Rehabilitation Centers
- Patient-Centered Approach – Tailored recovery programs for each patient.
- Multidisciplinary Team – Includes physicians, therapists, psychologists, social workers, and nurses.
- Long-Term or Short-Term Care – Based on the severity of the condition.
- Medical and Psychological Support – Combines physical therapy with emotional and behavioral counseling.
- Focus on Functional Recovery – Aims to restore mobility, communication, and daily living skills.
Classification of Rehabilitation Centers
Rehabilitation centers can be classified based on type of treatment, medical condition, or service setting.
1. Based on Medical Condition
A. Physical Rehabilitation Centers
- Focus on recovering physical functions after injuries or surgeries.
- Provide physiotherapy, mobility training, and pain management.
- Examples:
- Stroke Rehabilitation Centers – Help stroke survivors regain movement.
- Spinal Cord Injury Rehab – Support for patients with paralysis.
- Orthopedic Rehabilitation – Recovery after fractures or joint replacements.
B. Neurological Rehabilitation Centers
- Treat patients with brain injuries, Parkinson’s disease, multiple sclerosis, and cerebral palsy.
- Offer neurotherapy, speech therapy, and cognitive rehabilitation.
C. Cardiac Rehabilitation Centers
- For patients recovering from heart attacks, bypass surgery, or heart failure.
- Provide exercise training, diet counseling, and lifestyle management.
D. Pulmonary (Respiratory) Rehabilitation Centers
- Help patients with chronic obstructive pulmonary disease (COPD), asthma, or lung infections.
- Include breathing exercises, oxygen therapy, and lifestyle changes.
E. Addiction Rehabilitation Centers
- Provide detoxification, counseling, and therapy for drug and alcohol addiction.
- Offer support groups, relapse prevention, and life skill training.
F. Psychiatric and Mental Health Rehabilitation Centers
- Treat patients with schizophrenia, depression, anxiety, and PTSD.
- Provide cognitive behavioral therapy (CBT), group therapy, and medication management.
G. Pediatric Rehabilitation Centers
- Support children with developmental disorders, autism, and cerebral palsy.
- Provide physical, speech, and occupational therapy.
2. Based on Services Provided
A. Inpatient Rehabilitation Centers
- Patients stay in the facility for intensive treatment and medical supervision.
- Suitable for severe conditions like spinal cord injuries, post-surgical recovery, or drug addiction.
B. Outpatient Rehabilitation Centers
- Patients visit the center for scheduled therapy sessions but live at home.
- Used for mild to moderate conditions like sports injuries, speech disorders, or depression.
C. Community-Based Rehabilitation (CBR)
- Services provided at home or in community centers.
- Helps people with disabilities integrate into society.
- Common for elderly, disabled, or remote area populations.
D. Work/Occupational Rehabilitation Centers
- Help patients regain skills for employment after illness or injury.
- Offer vocational training and workplace readiness programs.
Services Provided in Rehabilitation Centers
1. Physical Therapy (Physiotherapy)
- Exercises and treatments to restore mobility, strength, and flexibility.
- Used after stroke, fractures, spinal cord injuries, and muscle weakness.
2. Occupational Therapy
- Helps patients regain skills needed for daily life (e.g., dressing, eating, working).
- Beneficial for stroke survivors, amputees, and mentally challenged individuals.
3. Speech and Language Therapy
- Helps patients regain communication abilities after stroke, brain injuries, or autism.
- Includes speech exercises, sign language, and assistive devices.
4. Psychological and Behavioral Therapy
- Supports patients with mental health issues, trauma, and substance addiction.
- Includes cognitive-behavioral therapy (CBT), counseling, and group therapy.
5. Pain Management
- Used for chronic pain conditions, arthritis, and post-surgical pain.
- Includes medication, physiotherapy, and alternative therapies (e.g., acupuncture, massage therapy).
6. Social and Vocational Rehabilitation
- Helps individuals reintegrate into society and the workforce.
- Provides career counseling, skill-building, and job training.
Examples of Rehabilitation Centers
- AIIMS Physical Rehabilitation Unit (India) – Provides physiotherapy and prosthetic limb support.
- National Institute of Mental Health and Neurosciences (NIMHANS, India) – Specializes in psychiatric rehabilitation.
- Alcoholics Anonymous (AA) Centers – Support groups for alcohol addiction recovery.
- Johns Hopkins Cardiac Rehab Center (USA) – Offers cardiac rehabilitation programs.
- Spinal Injury Rehabilitation Centers – Assist patients with mobility training and therapy.
Importance of Rehabilitation Centers
- Enhance patient independence after serious illness or injury.
- Reduce long-term disability and improve quality of life.
- Support addiction recovery and prevent relapse.
- Help reintegrate individuals into work and society.
- Reduce healthcare costs by minimizing hospital readmissions.
Types of Health Care Agencies/Services: Extended Care Facilities

Introduction
Extended care facilities (ECFs) are long-term healthcare institutions that provide ongoing medical, nursing, and rehabilitative care to individuals who need assistance with daily activities or medical supervision over an extended period. These facilities serve elderly individuals, chronically ill patients, disabled individuals, and those recovering from surgeries or serious illnesses.
Definition of Extended Care Facilities (ECFs)
An Extended Care Facility (ECF) is a healthcare institution that provides long-term medical, nursing, and rehabilitative care for individuals who require continuous assistance and monitoring beyond what a traditional hospital or clinic offers.
Objectives of Extended Care Facilities
- To provide continuous medical and nursing care to chronically ill, elderly, or disabled individuals.
- To assist individuals in regaining independence after illness or surgery.
- To offer rehabilitative services such as physical therapy and occupational therapy.
- To ensure a safe and supportive environment for individuals unable to care for themselves.
- To provide palliative and end-of-life care for terminally ill patients.
Key Features of Extended Care Facilities
- 24/7 Medical and Nursing Care – Patients receive round-the-clock supervision.
- Long-Term Support – Designed for individuals requiring months or years of care.
- Comprehensive Services – Includes medical treatment, rehabilitation, and daily living assistance.
- Residential or Facility-Based – Patients may live in the facility full-time or receive care as needed.
- Interdisciplinary Team – Includes doctors, nurses, physiotherapists, occupational therapists, dietitians, and social workers.
Classification of Extended Care Facilities
Extended care facilities are classified based on type of service, level of medical supervision, and patient needs.
1. Based on Type of Care Provided
A. Skilled Nursing Facilities (SNFs)
- Provide 24/7 nursing care for seriously ill or disabled patients.
- Offer post-hospitalization recovery, medication management, and therapy.
- Example: Elderly care homes with full-time medical staff.
B. Intermediate Care Facilities (ICFs)
- Provide less intensive medical supervision but still offer assistance with daily activities.
- Suitable for patients with mild disabilities, dementia, or stable chronic illnesses.
C. Assisted Living Facilities (ALFs)
- Designed for older adults who need help with daily tasks but do not require intensive medical care.
- Offer independent living with assistance in meals, medication, and personal care.
D. Rehabilitation Centers with Extended Care
- For patients who require long-term therapy after a major surgery, stroke, or injury.
- Includes physical therapy, speech therapy, and occupational therapy.
E. Long-Term Acute Care Hospitals (LTACHs)
- Provide care for patients with serious medical conditions requiring hospital-level treatment for an extended period.
- Examples: Ventilator-dependent patients, organ transplant recovery patients.
F. Hospice and Palliative Care Facilities
- Focus on comfort care for terminally ill patients.
- Offer pain management, emotional support, and end-of-life care.
2. Based on Patient Needs
A. Geriatric Extended Care Facilities
- Designed for elderly patients with chronic diseases, mobility issues, or dementia.
- Offer social engagement, physical therapy, and mental health support.
B. Pediatric Extended Care Facilities
- Provide long-term medical care for children with congenital disorders, disabilities, or chronic illnesses.
- Include specialized pediatric nursing and rehabilitation services.
C. Psychiatric Extended Care Facilities
- Treat patients with severe mental illnesses requiring long-term psychiatric care.
- Offer therapy, medication management, and behavioral counseling.
D. Disability Support Centers
- Designed for individuals with physical or intellectual disabilities.
- Provide specialized therapies and assistive devices.
E. Post-Surgical or Post-Trauma Extended Care
- Focus on recovery after major surgeries or injuries.
- Provide wound care, pain management, and physical rehabilitation.
Services Provided in Extended Care Facilities
1. Medical and Nursing Care
- Regular health monitoring for chronic conditions like diabetes, heart disease, and respiratory illnesses.
- Administration of medications, IV fluids, and oxygen therapy.
- Management of feeding tubes, catheters, and wound care.
2. Rehabilitative Therapy
- Physical Therapy – Helps regain mobility after stroke or fractures.
- Occupational Therapy – Supports daily living skills for disabled patients.
- Speech Therapy – Assists with communication and swallowing disorders.
3. Personal Care and Assistance
- Bathing, dressing, and grooming support for dependent individuals.
- Meal planning and feeding assistance.
- Mobility assistance (wheelchair use, walking aids, bed transfers).
4. Social and Recreational Activities
- Group therapy and social interaction to prevent isolation.
- Music, art, and cognitive therapy for mental stimulation.
- Community outings and activities to improve quality of life.
5. Psychological and Emotional Support
- Counseling and mental health services for patients with depression or anxiety.
- Dementia and Alzheimer’s support programs.
- Family support and caregiver counseling.
6. End-of-Life and Palliative Care
- Pain and symptom management for terminally ill patients.
- Emotional and spiritual support for patients and families.
- Hospice care services within extended care facilities.
Examples of Extended Care Facilities
- Government-Run Nursing Homes – Provide subsidized long-term care for the elderly and disabled.
- Private Assisted Living Homes – Offer customized residential care with nursing support.
- Rehabilitation Centers with Extended Care Units – Help stroke and surgery patients recover.
- Psychiatric Residential Facilities – Support individuals with severe mental disorders.
- Specialized Pediatric Extended Care Facilities – Care for children with chronic illnesses or disabilities.
Importance of Extended Care Facilities
- Provide long-term healthcare solutions for the elderly, disabled, and chronically ill.
- Reduce hospital readmissions by offering continuous medical supervision.
- Improve the quality of life for dependent individuals.
- Support families and caregivers by easing the burden of home care.
- Enhance recovery and rehabilitation through specialized therapies.
Types of Hospitals
Introduction
Hospitals are essential healthcare institutions that provide medical diagnosis, treatment, surgical interventions, rehabilitation, and emergency care. They serve patients with acute and chronic illnesses, injuries, and other medical conditions. Hospitals vary in size, specialization, ownership, and level of care they provide.
Definition of a Hospital
A hospital is a healthcare facility that offers medical, surgical, diagnostic, and therapeutic services to patients under the supervision of trained healthcare professionals such as doctors, nurses, and specialists.
Objectives of Hospitals
- To provide medical care and treatment for illnesses and injuries.
- To perform surgical and therapeutic procedures.
- To offer emergency and trauma care.
- To conduct health screenings and preventive care.
- To facilitate medical education and research.
- To support rehabilitation and palliative care.
Types of Hospitals
Hospitals can be classified based on ownership, function, level of care, and specialization.
1. Based on Ownership
A. Government/Public Hospitals
- Funded and managed by central, state, or local governments.
- Provide free or low-cost medical services.
- Serve a large population, including economically weaker sections.
- Example: AIIMS (All India Institute of Medical Sciences), Civil Hospitals, Military Hospitals.
B. Private Hospitals
- Owned by individuals, trusts, or corporations.
- Offer paid medical services with better facilities.
- Examples: Apollo Hospitals, Fortis Healthcare, Max Hospitals.
C. Non-Governmental Organization (NGO) Hospitals
- Run by charitable organizations, religious groups, or trusts.
- Provide subsidized or free healthcare to underprivileged patients.
- Examples: Mission Hospitals, Red Cross Hospitals.
D. Military and Defense Hospitals
- Managed by armed forces to provide medical care to soldiers, veterans, and their families.
- Examples: Military Hospital, Armed Forces Medical College (AFMC) Hospital.
2. Based on Level of Care
A. Primary Care Hospitals
- Provide basic medical services and first aid.
- Offer general outpatient consultations, minor treatments, and preventive care.
- Located in rural areas and small towns.
- Example: Primary Health Centers (PHCs), Rural Hospitals.
B. Secondary Care Hospitals
- Offer specialized medical services such as surgeries, maternity care, and emergency treatment.
- Include district hospitals and community health centers (CHCs).
- Example: District Hospitals, Sub-District Hospitals.
C. Tertiary Care Hospitals
- Provide advanced medical care and specialized treatment.
- Equipped with modern technology, ICUs, and super-specialty units.
- Serve as referral centers for primary and secondary hospitals.
- Example: AIIMS, PGIMER, JIPMER, Tata Memorial Hospital.
D. Quaternary Care Hospitals
- Offer highly specialized medical care, including organ transplants, genetic therapies, and experimental treatments.
- Engage in medical research and cutting-edge technologies.
- Example: Johns Hopkins Hospital (USA), Mayo Clinic (USA), AIIMS (India – Certain Departments).
3. Based on Function or Purpose
A. General Hospitals
- Provide a wide range of medical services.
- Have departments like medicine, surgery, pediatrics, gynecology, orthopedics, cardiology, and emergency care.
- Example: Civil Hospitals, District Hospitals.
B. Specialty Hospitals
- Focus on a specific field of medicine.
- Staffed by specialists in a particular discipline.
- Examples:
- Cardiology Hospitals – Narayana Health, Asian Heart Institute.
- Cancer Hospitals – Tata Memorial Hospital.
- Orthopedic Hospitals – Sancheti Hospital.
- Neurology Hospitals – NIMHANS.
C. Teaching and Research Hospitals
- Affiliated with medical colleges and universities.
- Train medical students, nurses, and healthcare professionals.
- Conduct clinical research and medical trials.
- Examples: AIIMS, JIPMER, KEM Hospital.
D. Rehabilitation Hospitals
- Provide long-term care for patients recovering from severe illness, stroke, trauma, or surgery.
- Offer physiotherapy, occupational therapy, and speech therapy.
- Examples: Spinal Injury Rehabilitation Centers, Stroke Recovery Centers.
E. Psychiatric Hospitals
- Specialize in the treatment of mental health disorders.
- Offer counseling, therapy, psychiatric medication, and rehabilitation.
- Examples: NIMHANS, Institute of Mental Health.
F. Maternity and Childcare Hospitals
- Provide prenatal, delivery, postnatal, and pediatric care.
- Handle high-risk pregnancies and neonatal intensive care (NICU).
- Examples: Fernandez Hospital, Rainbow Children’s Hospital.
G. Infectious Disease Hospitals
- Treat infectious diseases like tuberculosis (TB), COVID-19, and HIV/AIDS.
- Have isolation wards and specialized treatments.
H. Palliative and Hospice Care Hospitals
- Provide end-of-life care for terminally ill patients.
- Focus on pain management and emotional support.
- Examples: Cancer Hospice Centers, Palliative Care Units.
4. Based on Size and Capacity
A. Small Hospitals
- Have less than 50 beds.
- Provide basic healthcare services, minor surgeries, and outpatient care.
- Located in small towns and rural areas.
B. Medium-Sized Hospitals
- Have 50 to 300 beds.
- Offer specialized care, including surgery, maternity services, and emergency care.
- Often include Community Health Centers (CHCs) and District Hospitals.
C. Large or Multi-Specialty Hospitals
- Have more than 300 beds.
- Provide highly specialized medical care such as organ transplants, neurosurgery, and cancer treatment.
- Examples: AIIMS, PGIMER, Tata Memorial Hospital.
Departments in a Hospital
1. Emergency and Trauma Care
- 24/7 care for accidents, heart attacks, strokes, and critical conditions.
2. Outpatient Department (OPD)
- Non-admitted patient care, including consultations and minor procedures.
3. Inpatient Department (IPD)
- Admitted patient care for medical or surgical treatment.
4. Intensive Care Unit (ICU)
- Critical care for seriously ill patients.
- Includes NICU (Neonatal ICU), PICU (Pediatric ICU), CCU (Cardiac ICU).
5. Operation Theaters (OT)
- Surgical procedures are performed with sterile conditions.
6. Laboratory and Diagnostic Services
- Includes blood tests, pathology, radiology (X-rays, CT scans, MRI), and genetic testing.
7. Pharmacy
- Dispenses medicines prescribed by doctors.
8. Physiotherapy and Rehabilitation Unit
- Physical and occupational therapy for recovering patients.
9. Medical Records Department
- Maintains patient history, reports, and treatment plans.
Importance of Hospitals in Healthcare
- Provide life-saving treatments and emergency care.
- Improve public health through vaccinations and screenings.
- Reduce mortality rates by offering specialized care.
- Create employment for doctors, nurses, and medical professionals.
- Support medical advancements through research and innovation.
Organization of Hospitals
Introduction
The organization of hospitals is a structured system that ensures the efficient delivery of healthcare services to patients. It involves hierarchical divisions, specialized departments, and coordinated management systems to provide quality medical care, administrative efficiency, and patient safety.
Definition of Hospital Organization
Hospital organization refers to the systematic arrangement of departments, personnel, and facilities within a hospital to provide effective patient care, manage resources efficiently, and ensure smooth operations.
Objectives of Hospital Organization
- To ensure efficient management of hospital resources.
- To provide coordinated healthcare services through different departments.
- To improve patient safety, quality of care, and medical outcomes.
- To establish a structured hierarchy for smooth administration.
- To facilitate medical research and education in teaching hospitals.
Types of Hospital Organization
Hospital organizations can be classified based on ownership, function, hierarchy, and administrative structure.
1. Based on Ownership
A. Government/Public Hospitals
- Owned and operated by government authorities.
- Funded through tax revenues and government budgets.
- Serve all sections of society, including low-income groups.
- Example: Civil Hospitals, AIIMS, PGIMER, NHS Hospitals (UK).
B. Private Hospitals
- Owned by individuals, trusts, or corporate organizations.
- Operate on fee-for-service or insurance-based models.
- Offer advanced medical technology and specialized services.
- Example: Apollo Hospitals, Fortis Healthcare, Mayo Clinic.
C. Non-Governmental Organization (NGO) Hospitals
- Run by charitable organizations or religious institutions.
- Provide low-cost or free healthcare to underserved populations.
- Example: Mission Hospitals, Red Cross Hospitals.
D. Military and Defense Hospitals
- Operated by the armed forces to provide medical care for soldiers and their families.
- Example: Armed Forces Medical Services (AFMS), Military Hospitals.
2. Based on Administrative Structure
A. Centralized Hospital Organization
- Decision-making is controlled by a central authority (government or private management).
- Policies and protocols are standardized across all hospital units.
- Example: Government Hospitals, Multi-Branch Corporate Hospitals (Apollo Hospitals).
B. Decentralized Hospital Organization
- Authority is distributed among different departments or branches.
- Each unit has independent decision-making power within its area.
- Example: University Teaching Hospitals, Community Health Centers.
C. Hierarchical Hospital Organization
- The hospital is structured in multiple levels, including:
- Top-level management (Hospital Directors, Board of Trustees).
- Middle-level management (Department Heads, Chief Medical Officers).
- Lower-level management (Nurses, Technicians, Support Staff).
3. Based on Function and Service Delivery
A. General Hospitals
- Provide a wide range of healthcare services, including emergency care, surgery, internal medicine, pediatrics, and maternity care.
- Example: Civil Hospitals, District Hospitals.
B. Specialty Hospitals
- Focus on specific medical fields such as cardiology, oncology, neurology, and orthopedics.
- Example: Tata Memorial Cancer Hospital, NIMHANS for Neurology.
C. Teaching and Research Hospitals
- Affiliated with medical colleges to train medical students, nurses, and healthcare professionals.
- Conduct clinical research and medical innovations.
- Example: AIIMS, JIPMER, KEM Hospital.
D. Community and Rural Hospitals
- Serve rural populations with basic healthcare, maternal care, and disease prevention programs.
- Example: Primary Health Centers (PHCs), Rural Hospitals.
E. Rehabilitation and Palliative Care Hospitals
- Provide long-term care and rehabilitation services for patients recovering from strokes, surgeries, trauma, or chronic diseases.
- Example: Rehabilitation Centers, Hospice Care Units.
Hospital Organizational Structure
Hospitals operate with a multi-tiered structure, ensuring coordination among medical, administrative, and support staff.
1. Administrative Structure
| Position | Role & Responsibility |
|---|---|
| Hospital Director/CEO | Oversees overall hospital operations and decision-making. |
| Medical Superintendent | Manages medical staff, patient care policies, and quality control. |
| Chief Nursing Officer (CNO) | Supervises nursing staff and ensures patient care standards. |
| Finance and Accounts Head | Handles hospital budgeting, billing, and financial management. |
| Human Resource (HR) Department | Manages hospital staff recruitment, training, and welfare. |
2. Medical Departments
| Department | Function |
|---|---|
| Emergency Department (ER) | Provides urgent care for accidents, heart attacks, strokes, and trauma cases. |
| Outpatient Department (OPD) | Manages consultations for non-admitted patients. |
| Inpatient Department (IPD) | Provides care for admitted patients requiring long-term treatment. |
| Intensive Care Unit (ICU) | Treats critically ill patients requiring close monitoring. |
| Operation Theaters (OT) | Performs surgical procedures under sterile conditions. |
| Radiology and Imaging | Conducts X-rays, CT scans, MRIs, and ultrasounds. |
| Pathology and Laboratory Services | Performs blood tests, biopsies, and diagnostic procedures. |
| Pharmacy Department | Dispenses prescribed medications. |
3. Support Services
| Service | Function |
|---|---|
| Medical Records & IT Department | Maintains electronic health records and patient databases. |
| Housekeeping and Sanitation | Ensures hospital cleanliness and infection control. |
| Biomedical Engineering | Maintains medical equipment and technology. |
| Security Services | Provides hospital security and patient safety. |
Hospital Committees for Quality Control
To maintain efficiency, safety, and ethical practices, hospitals establish various committees:
- Hospital Ethics Committee – Monitors medical ethics and patient rights.
- Infection Control Committee – Ensures hygiene and prevents hospital-acquired infections.
- Medical Audit Committee – Evaluates clinical practices and treatment effectiveness.
- Pharmacy and Therapeutics Committee – Regulates medication usage and drug safety.
- Disaster Management Committee – Prepares for emergency responses during natural disasters or pandemics.
Examples of Well-Organized Hospitals
- AIIMS (India) – Government-run multi-specialty hospital with research and teaching facilities.
- Mayo Clinic (USA) – One of the most advanced medical research hospitals in the world.
- Apollo Hospitals (India) – A leading private healthcare organization offering specialized treatments.
- Johns Hopkins Hospital (USA) – A pioneer in medical education and research.
- Tata Memorial Hospital (India) – Specializes in cancer treatment and research.
Importance of Hospital Organization
- Enhances patient safety and quality of care through structured management.
- Optimizes hospital workflow and resource utilization.
- Ensures compliance with healthcare regulations and medical ethics.
- Improves coordination among different healthcare departments.
- Supports medical research, innovation, and academic training.
Functions of a Hospital
Introduction
A hospital is a multifunctional healthcare institution that provides medical, surgical, diagnostic, preventive, and rehabilitative services to individuals in need. It plays a crucial role in patient care, medical research, education, and public health promotion.
Definition of Hospital Functions
The functions of a hospital refer to the various roles and responsibilities it undertakes to provide comprehensive healthcare services to the community. These include curative, preventive, diagnostic, rehabilitative, administrative, and research-based functions.
Objectives of Hospital Functions
- To provide medical care and treatment for acute and chronic illnesses.
- To conduct surgical procedures and specialized medical interventions.
- To prevent diseases through health education and immunization programs.
- To offer diagnostic services for early disease detection.
- To rehabilitate patients recovering from injuries, illnesses, or disabilities.
- To train healthcare professionals through medical education.
- To support medical research and advancements in healthcare.
Major Functions of a Hospital
1. Curative (Therapeutic) Functions
- Primary responsibility of a hospital is to treat diseases and injuries.
- Includes medical and surgical interventions.
- Examples:
- Medication administration for chronic diseases (diabetes, hypertension).
- Emergency care for accidents, strokes, and heart attacks.
- Surgical procedures such as appendectomy, organ transplants.
2. Preventive Functions
- Focus on disease prevention and health promotion.
- Hospitals organize health awareness programs, screenings, and vaccinations.
- Examples:
- Immunization programs for diseases like polio, hepatitis, and COVID-19.
- Cancer screenings (mammograms, Pap smears, colonoscopies).
- Health education on hygiene, nutrition, and lifestyle modifications.
3. Diagnostic Functions
- Hospitals provide laboratory and imaging services to detect diseases.
- Early diagnosis leads to effective treatment and better prognosis.
- Examples:
- Blood tests (CBC, liver function tests, glucose levels).
- Imaging tests (X-rays, CT scans, MRI, ultrasound).
- Endoscopy and biopsy for detecting cancers and gastrointestinal disorders.
4. Rehabilitative Functions
- Support recovery and restore functionality after illness or surgery.
- Hospitals have rehabilitation units that help patients regain independence.
- Examples:
- Physiotherapy for stroke patients and post-surgical recovery.
- Speech therapy for individuals with communication disorders.
- Occupational therapy for disabled or injured individuals.
5. Emergency and Trauma Care Functions
- Hospitals provide 24/7 emergency care for critically ill and injured patients.
- Equipped with ambulances, trauma units, and intensive care units (ICU).
- Examples:
- Immediate treatment of accident victims in the emergency room.
- CPR and defibrillation for cardiac arrest patients.
- Management of burns, fractures, and poisonings.
6. Maternity and Childcare Functions
- Hospitals ensure safe childbirth and maternal care.
- Provide neonatal care for premature and high-risk infants.
- Examples:
- Antenatal care for pregnant women.
- Safe deliveries and cesarean sections.
- Postnatal care and breastfeeding support.
7. Teaching and Training Functions
- Hospitals serve as teaching institutions for medical, nursing, and paramedical students.
- Associated with medical colleges and universities for clinical training.
- Examples:
- Internship programs for medical students.
- Hands-on training for nurses and paramedics.
- Residency and specialization programs for doctors.
8. Research and Development Functions
- Hospitals conduct medical research to advance healthcare.
- Involves clinical trials, drug testing, and epidemiological studies.
- Examples:
- Developing new treatment methods for cancer or infectious diseases.
- Testing new vaccines and medications.
- Genetic research and stem cell therapy innovations.
9. Palliative and Hospice Care Functions
- Hospitals provide end-of-life care for terminally ill patients.
- Focuses on pain management, emotional support, and quality of life.
- Examples:
- Cancer hospice care for pain relief and symptom control.
- Dementia care for elderly patients.
- Psychological and emotional counseling for families.
10. Administrative and Managerial Functions
- Efficient hospital administration ensures smooth operations.
- Includes budgeting, human resources, legal compliance, and hospital logistics.
- Examples:
- Hospital accreditation and licensing.
- Staff management and scheduling.
- Financial planning and billing systems.
11. Social and Community Services
- Hospitals engage in community outreach programs.
- Support health awareness and rural healthcare initiatives.
- Examples:
- Mobile health camps for remote villages.
- Blood donation drives.
- Mental health awareness programs.
Departments Involved in Hospital Functions
| Department | Function |
|---|---|
| Emergency Department (ER) | Handles urgent and life-threatening cases. |
| Outpatient Department (OPD) | Manages non-admitted patient care. |
| Inpatient Department (IPD) | Provides care for admitted patients. |
| Surgery & Operating Theaters (OT) | Conducts surgical procedures. |
| Intensive Care Unit (ICU) | Treats critically ill patients. |
| Radiology & Imaging | Conducts X-rays, CT scans, MRIs. |
| Pathology & Laboratory | Performs diagnostic tests. |
| Pharmacy | Dispenses medicines and maintains drug inventory. |
| Nursing Services | Provides bedside care and patient monitoring. |
| Medical Records & IT | Maintains patient records and digital data. |
Examples of Well-Functioning Hospitals
- AIIMS (India) – Multi-specialty hospital providing medical education and research.
- Mayo Clinic (USA) – Leading hospital for research-based healthcare.
- Tata Memorial Hospital (India) – Specializes in oncology and cancer treatment.
- Johns Hopkins Hospital (USA) – Pioneer in innovative medical procedures.
- Red Cross Hospitals – Focus on humanitarian and emergency healthcare.
Importance of Hospital Functions
- Ensure accessible and efficient healthcare delivery.
- Prevent, diagnose, and treat illnesses effectively.
- Provide emergency and life-saving treatments.
- Support medical research and technological advancements.
- Train future healthcare professionals.
- Promote public health and disease prevention.
Health Care Teams in Hospitals: Members and Their Roles
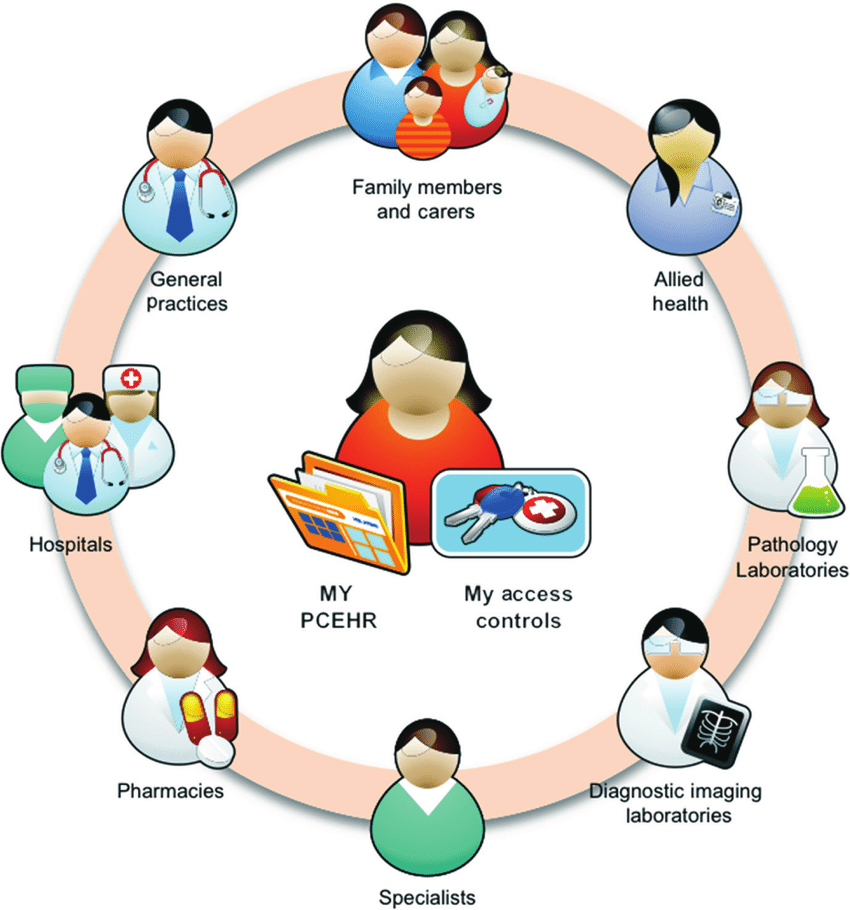
Introduction
A healthcare team in a hospital consists of various professionals working together to provide comprehensive and high-quality patient care. Each member has a specific role and responsibility that contributes to the effective functioning of the hospital.
Definition of a Health Care Team
A healthcare team is a group of medical professionals with different expertise who collaborate to diagnose, treat, and support patients in a hospital setting.
Objectives of a Health Care Team
- To provide patient-centered care through teamwork.
- To ensure safety and quality treatment for all patients.
- To promote communication and coordination among healthcare providers.
- To enhance efficiency in medical procedures and hospital operations.
- To ensure holistic care covering physical, emotional, and psychological well-being.
Members of a Hospital Health Care Team and Their Roles
A hospital healthcare team includes clinical staff, administrative personnel, and support workers, each playing a vital role in patient care.
1. Medical Team
A. Doctors/Physicians
- Role: Diagnose illnesses, prescribe treatments, perform surgeries, and oversee patient care.
- Types:
- General Physicians (GPs): Provide primary healthcare.
- Specialists: Focus on specific medical fields (Cardiologists, Neurologists, Oncologists).
- Surgeons: Perform operations and surgical procedures.
- Emergency Physicians: Handle critical cases in the Emergency Room (ER).
B. Nurses
- Role: Provide direct patient care, administer medications, assist doctors, and monitor patients.
- Types:
- Registered Nurses (RNs): Provide bedside care and administer treatments.
- Nurse Practitioners (NPs): Diagnose, treat, and prescribe medication.
- Critical Care Nurses: Work in ICUs and handle serious cases.
- Midwives: Assist in childbirth and maternal care.
- Community Health Nurses: Provide preventive healthcare.
C. Pharmacists
- Role: Dispense medications, educate patients about drug use, and ensure safe medication administration.
D. Medical Laboratory Technologists (MLTs)
- Role: Perform diagnostic tests on blood, urine, and tissue samples to help doctors diagnose diseases.
E. Radiologists & Imaging Technicians
- Role: Conduct imaging tests (X-rays, MRIs, CT scans, ultrasounds) to assist in diagnosis.
F. Physiotherapists
- Role: Help patients recover mobility and function after injuries, strokes, or surgeries.
G. Occupational Therapists
- Role: Assist patients in regaining daily living skills and independence.
H. Speech Therapists
- Role: Help patients recover speech abilities after strokes, brain injuries, or developmental disorders.
I. Dietitians/Nutritionists
- Role: Plan patient diets, manage nutritional therapy, and support weight management.
J. Psychiatrists and Psychologists
- Role: Provide mental health support, therapy, and treatment for psychological disorders.
K. Social Workers
- Role: Assist patients with emotional support, counseling, and accessing healthcare services.
2. Emergency and Critical Care Team
A. Emergency Medical Technicians (EMTs) and Paramedics
- Role: Provide first aid and life-saving interventions before hospital admission.
B. Intensive Care Unit (ICU) Staff
- Role: Monitor critically ill patients in ICUs, manage ventilators, and handle complex cases.
C. Anesthesiologists
- Role: Administer anesthesia and pain management before surgeries.
3. Hospital Administrative Team
A. Hospital Administrators
- Role: Manage hospital operations, finances, human resources, and compliance with regulations.
B. Medical Record Officers
- Role: Maintain and manage patient records and medical histories.
C. IT Specialists
- Role: Oversee hospital information systems, telemedicine, and electronic health records.
D. Finance & Billing Team
- Role: Handle hospital payments, insurance claims, and patient billing.
4. Support Services Team
A. Housekeeping Staff
- Role: Ensure cleanliness and hygiene in hospital premises.
B. Security Personnel
- Role: Maintain hospital safety and manage visitor access.
C. Biomedical Engineers
- Role: Maintain and repair medical equipment and devices.
D. Transport & Ambulance Team
- Role: Transport patients safely within and outside the hospital.
Importance of a Health Care Team in a Hospital
- Ensures holistic patient care by integrating multiple disciplines.
- Improves patient safety through coordinated teamwork.
- Enhances efficiency in healthcare delivery.
- Reduces hospital errors through better communication among staff.
- Provides emotional and psychological support for patients and families.
FOR UNLOCK 🔓 FULL COURSE NOW. MORE DETAILS CALL US OR WATSAPP ON- 8485976407
