BSC SEM 1 UNIT 12 APPLIED NUTRITION AND DIETETICS
UNIT 12 National Nutritional Programmes and role of nurse
National Nutritional Programmes in India:
Nutrition is a critical determinant of public health, affecting growth, immunity, cognitive development, and overall well-being. India has launched various National Nutritional Programs to combat malnutrition, micronutrient deficiencies, and diet-related diseases. These programs focus on ensuring proper nutritional intake for vulnerable populations, such as children, pregnant and lactating women, and economically disadvantaged communities.
1. Major National Nutritional Programmes in India
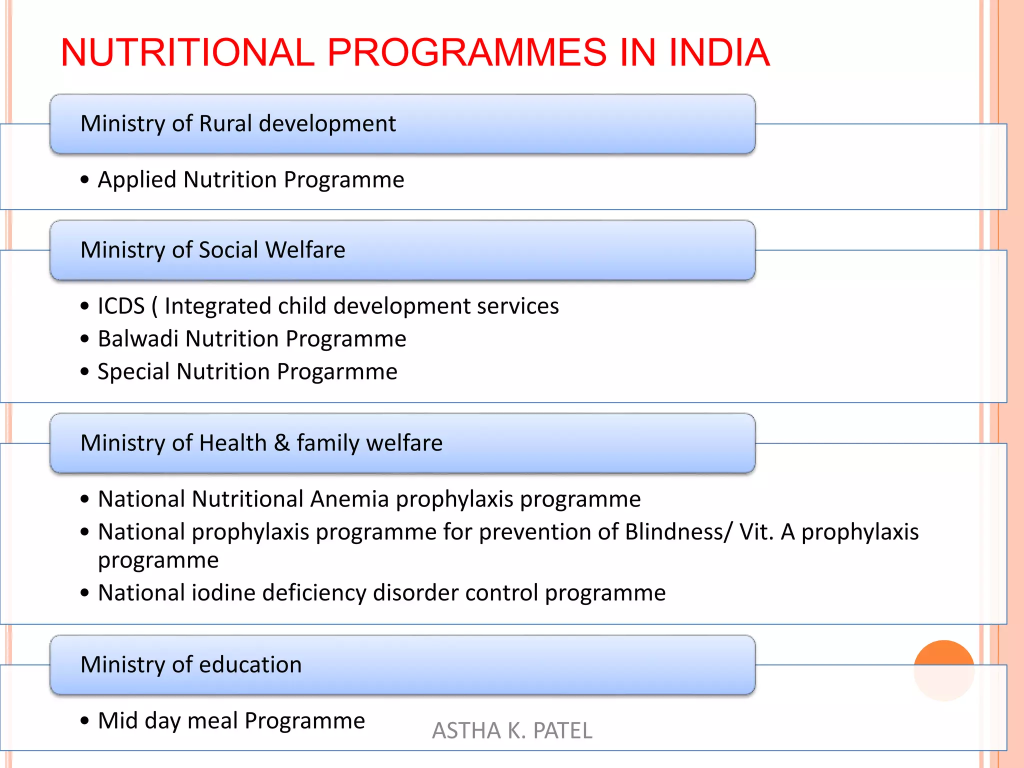
The Government of India has implemented various initiatives to improve nutritional status across different population groups. The following are the key national nutritional programs:
1.1 Integrated Child Development Services (ICDS) (1975)
✅ Objective:
- Improve the nutritional and health status of children (0-6 years), pregnant women, and lactating mothers.
- Reduce malnutrition, morbidity, and mortality among young children.
✅ Key Nutritional Interventions:
- Supplementary Nutrition: Nutritious food is provided through Anganwadi centers.
- Growth Monitoring: Regular weight checks and height measurements.
- Nutrition & Health Education: Educating mothers on breastfeeding, complementary feeding, and hygiene.
- Micronutrient Supplementation: Distribution of iron, folic acid, and vitamin A.
✅ Beneficiaries:
- Children (0-6 years)
- Pregnant and lactating mothers
- Adolescent girls (under SABLA Scheme)
✅ Nutritional Impact:
- Reduction in childhood malnutrition and underweight cases.
- Promotion of breastfeeding and complementary feeding.
✅ Current Updates:
- Now part of POSHAN Abhiyaan for better implementation and monitoring.
1.2 Mid-Day Meal Scheme (MDMS) (1995)

✅ Objective:
- Provide nutritious cooked meals to school children to improve their health and encourage attendance.
✅ Key Nutritional Interventions:
- One-time hot cooked meals providing essential macronutrients and micronutrients.
- Calories: 450 kcal (Primary) & 700 kcal (Upper Primary).
- Protein: 12 gm (Primary) & 20 gm (Upper Primary).
- Fortified foods: Inclusion of fortified rice, wheat, and edible oils.
- Micronutrient Supplementation: Iron, folic acid, and vitamin A.
✅ Beneficiaries:
- Children studying in government and government-aided schools (Class 1-8).
✅ Nutritional Impact:
- Improves child growth and cognitive development.
- Reduces anemia and malnutrition in school-going children.
✅ Current Updates:
- Renamed as PM POSHAN Scheme in 2021.
1.3 National Iodine Deficiency Disorders Control Programme (NIDDCP) (1992)

✅ Objective:
- Eliminate iodine deficiency disorders such as goiter, hypothyroidism, and mental retardation.
✅ Key Nutritional Interventions:
- Universal Salt Iodization: Ensuring that all salt is iodized at ≥15 ppm iodine content.
- Community Awareness: Educating about the benefits of iodized salt.
- Screening and Surveillance: Monitoring iodine levels in urine and salt samples.
✅ Beneficiaries:
- General population, with special focus on pregnant women and children.
✅ Nutritional Impact:
- Reduction in iodine deficiency disorders.
- Improvement in cognitive function and thyroid health.
✅ Current Updates:
- Strict monitoring of iodine levels in salt production and distribution.
1.4 Anemia Mukt Bharat (2018)
✅ Objective:
- Reduce anemia prevalence among women, adolescents, and children.
✅ Key Nutritional Interventions:
- Iron & Folic Acid Supplementation (WIFS): Weekly iron-folic acid (IFA) tablets for schoolchildren and pregnant women.
- Deworming: Biannual Albendazole tablets for children.
- Nutrition Education: Awareness on iron-rich foods like green leafy vegetables, meat, eggs, and legumes.
- Point-of-Care Testing: Hemoglobin monitoring at health centers.
✅ Beneficiaries:
- Children (6-59 months)
- Adolescents (10-19 years)
- Pregnant & lactating women
✅ Nutritional Impact:
- Reduction in anemia cases, especially in pregnant women and schoolchildren.
✅ Current Updates:
- Focus on fortified foods (iron-fortified rice and wheat).
1.5 POSHAN Abhiyaan (2018)
✅ Objective:
- Achieve improved nutritional outcomes in children, pregnant women, and lactating mothers.
✅ Key Nutritional Interventions:
- Growth Monitoring Devices: Digital tracking of child growth.
- Nutrition Counselling: Awareness campaigns for maternal and child nutrition.
- Food Fortification: Promoting fortified staples like rice, wheat, and oil.
- Breastfeeding Promotion: Encouraging exclusive breastfeeding for 6 months.
✅ Beneficiaries:
- Children (0-6 years)
- Pregnant and lactating women
✅ Nutritional Impact:
- Reduction in stunting, wasting, and undernutrition among children.
✅ Current Updates:
- Strengthening Anganwadi Services under Saksham Anganwadi initiative.
1.6 Pradhan Mantri Matru Vandana Yojana (PMMVY) (2017)
✅ Objective:
- Provide financial assistance to pregnant women for proper nutrition and medical care.
✅ Key Nutritional Interventions:
- ₹5000 Cash Incentive: Encourages proper diet and healthcare.
- Maternal Nutrition Counselling: Education on diet diversity and food intake.
✅ Beneficiaries:
- Pregnant and lactating mothers.
✅ Nutritional Impact:
- Improves maternal health and pregnancy outcomes.
✅ Current Updates:
- Integration with POSHAN Abhiyaan for better maternal nutrition.
1.7 National Vitamin A Supplementation Programme
✅ Objective:
- Prevent childhood blindness and reduce mortality due to vitamin A deficiency.
✅ Key Nutritional Interventions:
- Vitamin A supplementation (Every 6 months for children aged 6 months-5 years).
- Dietary Education: Encouraging consumption of vitamin A-rich foods like carrots, mangoes, papaya, and dairy products.
✅ Nutritional Impact:
- Decrease in xerophthalmia (night blindness) and child mortality.
✅ Current Updates:
- Strengthened under Mission Indradhanush.
1.8 National Programme on Prevention and Control of Non-Communicable Diseases (NCDs)
✅ Objective:
- Address lifestyle-related disorders like obesity, diabetes, hypertension through proper diet and physical activity.
✅ Key Nutritional Interventions:
- Nutritional Counseling: Advice on reducing sugar, salt, and processed food intake.
- Healthy Eating Campaigns: Promotion of whole grains, fruits, and vegetables.
✅ Nutritional Impact:
- Prevention of diabetes, obesity, and heart diseases.
✅ Current Updates:
- Collaboration with Food Safety and Standards Authority of India (FSSAI) to promote Eat Right India movement.
Nutritional Problems in India.
Introduction
Nutrition plays a critical role in maintaining health and well-being. In India, malnutrition continues to be a significant public health issue, affecting children, women, and vulnerable populations. The country faces a double burden of malnutrition, which includes undernutrition, micronutrient deficiencies, and overnutrition leading to obesity and non-communicable diseases (NCDs).
Major Nutritional Problems in India
1. Undernutrition (Protein-Energy Malnutrition – PEM)
Undernutrition occurs due to an inadequate intake of calories and proteins, leading to various health issues.
- Affected Groups: Infants, young children, pregnant and lactating women, and people living in poverty.
- Common Conditions:
- Marasmus: Caused by severe calorie deficiency.
- Kwashiorkor: Caused by severe protein deficiency.
- Stunting: Low height-for-age (chronic malnutrition).
- Wasting: Low weight-for-height (acute malnutrition).
- Underweight: Low weight-for-age.
Causes:
- Inadequate food intake.
- Poor maternal nutrition.
- Low birth weight.
- Recurrent infections.
- Poor sanitation and hygiene.
Consequences:
- Increased mortality in children under five.
- Cognitive impairments.
- Reduced productivity in adulthood.
Statistics (India, as per NFHS-5 2019-21):
- Stunting: 35.5% of children under five.
- Wasting: 19.3% of children under five.
- Underweight: 32.1% of children under five.
2. Micronutrient Deficiencies (Hidden Hunger)
Micronutrient deficiencies occur due to a lack of essential vitamins and minerals, leading to long-term health consequences.
a. Iron Deficiency Anemia
- Cause: Inadequate iron intake, poor absorption, parasitic infections.
- Effects: Fatigue, weakness, poor concentration, increased maternal and infant mortality.
- Prevalence (NFHS-5 2019-21):
- 57% of women (15-49 years) are anemic.
- 67% of children (6-59 months) are anemic.
b. Vitamin A Deficiency (VAD)
- Cause: Lack of vitamin A-rich foods (milk, eggs, green leafy vegetables).
- Effects: Night blindness, weakened immune system, increased child mortality.
c. Iodine Deficiency Disorders (IDD)
- Cause: Inadequate iodine intake in diet.
- Effects: Goiter, hypothyroidism, cretinism in children.
- Solution: Universal Salt Iodization (USI).
d. Vitamin D Deficiency
- Cause: Inadequate sun exposure, lack of vitamin D in diet.
- Effects: Rickets in children, osteoporosis in adults.
e. Zinc Deficiency
- Cause: Poor intake of animal-based foods.
- Effects: Poor immune function, delayed growth, increased risk of infections.
f. Vitamin B12 Deficiency
- Cause: Poor intake of animal-based foods, vegetarian diet.
- Effects: Anemia, neurological disorders.
3. Overnutrition (Obesity and Lifestyle Diseases)
With urbanization and lifestyle changes, India faces a rise in obesity and related diseases.
- Causes:
- High consumption of processed and fast foods.
- Sedentary lifestyle.
- Increased intake of sugar and unhealthy fats.
- Health Risks:
- Type 2 diabetes.
- Hypertension.
- Cardiovascular diseases.
- Certain types of cancers.
- Statistics (NFHS-5 2019-21):
- 24% of women and 22.9% of men in India are overweight or obese.
4. Food Insecurity and Malnutrition
- Cause: Poverty, lack of access to nutritious food, high food prices.
- Effect: Chronic hunger, poor health, low productivity.
- Programs to address food insecurity:
- Public Distribution System (PDS).
- Mid-Day Meal Scheme.
- Integrated Child Development Services (ICDS).
- Poshan Abhiyaan.
Government Initiatives to Address Nutritional Problems
- Integrated Child Development Services (ICDS) Scheme: Provides supplementary nutrition, immunization, and preschool education.
- Mid-Day Meal Scheme (MDM): Provides free meals to school children to improve nutrition and school attendance.
- National Food Security Act (NFSA), 2013: Ensures subsidized food grains to poor families.
- Poshan Abhiyaan (National Nutrition Mission): Aims to reduce stunting, undernutrition, and anemia in women and children.
- Anemia Mukt Bharat: Focuses on reducing anemia among children and women through iron supplementation.
- Universal Salt Iodization: Ensures iodized salt availability to prevent iodine deficiency disorders.
National Nutrition Policy of India (1993 & Updates)
Introduction
The National Nutrition Policy (NNP) of India was launched in 1993 to combat malnutrition and improve the overall nutritional status of the population. The policy focuses on a multi-sectoral approach, integrating health, agriculture, education, rural development, and social welfare programs. Over the years, various government initiatives have been introduced under the policy to address undernutrition, micronutrient deficiencies, and overnutrition.
Objectives of the National Nutrition Policy

The key objectives of the policy are:
- Reduce malnutrition among children, pregnant women, and lactating mothers.
- Eradicate micronutrient deficiencies (iron, vitamin A, iodine, etc.).
- Improve food security and dietary diversity.
- Strengthen health and nutrition interventions.
- Promote nutritional awareness and education.
- Encourage food fortification and supplementation.
- Monitor and evaluate nutrition programs regularly.
Strategies of the National Nutrition Policy

The policy follows a dual strategy:
A. Direct Nutrition Interventions (Short-Term Measures)
These interventions aim to provide immediate relief from malnutrition.
- Supplementary Nutrition Programs (SNPs)
- Integrated Child Development Services (ICDS): Provides food, healthcare, and preschool education to children under 6 years, pregnant and lactating women.
- Mid-Day Meal Scheme (MDM): Provides free lunch to school children to improve nutrition and attendance.
- Special Nutrition Programs: Targeted nutrition support for malnourished children.
- Micronutrient Supplementation
- Iron and Folic Acid (IFA) Supplementation for pregnant women and children to reduce anemia.
- Vitamin A Supplementation for children to prevent blindness and boost immunity.
- Iodized Salt Consumption to prevent goiter and iodine deficiency disorders.
- Food Fortification
- Fortification of wheat, rice, salt, milk, and oil with essential micronutrients.
- Health and Nutrition Education
- Awareness campaigns on balanced diets, breastfeeding, and child feeding practices.
- Promotion of Exclusive Breastfeeding (0-6 months)
- Encouraging breastfeeding to reduce infant mortality and improve immunity.
B. Indirect Nutrition Interventions (Long-Term Measures)
These strategies focus on addressing the root causes of malnutrition by improving food production, healthcare, sanitation, and poverty alleviation.
- Food Security Measures
- Public Distribution System (PDS): Provides subsidized food grains to poor households.
- National Food Security Act (NFSA), 2013: Legal framework for food distribution and nutrition.
- Poverty Alleviation Programs
- Mahatma Gandhi National Rural Employment Guarantee Act (MGNREGA): Provides rural employment for food security.
- Rural Development Programs: Ensuring better income and food access.
- Agricultural Policies for Nutrition
- Promotion of nutritious crops (millets, pulses, and vegetables).
- Encouraging kitchen gardens for self-sufficiency.
- Women and Child Development Programs
- POSHAN Abhiyaan (2018): Focuses on reducing stunting, undernutrition, anemia among children and women.
- Janani Suraksha Yojana (JSY): Provides financial assistance for institutional deliveries.
- Pradhan Mantri Matru Vandana Yojana (PMMVY): Maternity benefit scheme to improve maternal nutrition.
- Healthcare and Sanitation Initiatives
- Immunization programs to prevent diseases linked to malnutrition.
- Swachh Bharat Abhiyan (Clean India Mission): Improves sanitation to reduce infections.
- Nutrition Surveillance and Monitoring
- National Family Health Survey (NFHS): Tracks nutritional indicators.
- Rapid Reporting Systems for real-time nutrition monitoring.
Recent Updates and Amendments in Nutrition Policy
- POSHAN Abhiyaan (2018)
- Aims to reduce stunting, undernutrition, anemia, and low birth weight by 2% annually.
- Uses digital technology for real-time nutrition tracking.
- Eat Right India Movement (2018)
- Promotes safe, healthy, and sustainable diets.
- Encourages fortification of rice, oil, and milk.
- National Nutrition Mission (NNM)
- Expands nutrition services to adolescent girls and lactating mothers.
- One Nation, One Ration Card (ONORC)
- Ensures food security for migrant populations.
Challenges in Implementing the Nutrition Policy

Despite these interventions, India continues to face several challenges in improving nutrition levels:
- High Malnutrition Rates: Stunting, wasting, and underweight remain high in children.
- Micronutrient Deficiencies: High prevalence of anemia, vitamin A, and iodine deficiency.
- Food Insecurity and Poverty: Many families cannot afford nutritious food.
- Lack of Awareness: Poor dietary habits and misconceptions about nutrition.
- Inadequate Implementation: Gaps in distribution and delivery of nutrition programs.
- Lifestyle Changes: Increased consumption of processed and unhealthy foods leading to obesity.
Future Strategies and Recommendations

To strengthen the National Nutrition Policy, the government must focus on:
- Expanding Coverage of Nutrition Programs: Ensure that all vulnerable populations benefit.
- Strengthening Fortification Policies: Scale up fortification of staple foods.
- Improving Health and Sanitation: Reduce disease burden that worsens malnutrition.
- Enhancing Public Awareness: Promote healthy eating habits through mass campaigns.
- Integrating Technology for Monitoring: Use real-time data tracking for better policy implementation.
- Promoting Sustainable Agriculture: Encourage the production and consumption of nutrient-rich foods.
National Nutritional Programme: Vitamin A Supplementation in India
Introduction
Vitamin A is an essential fat-soluble vitamin required for maintaining good vision, immune function, and healthy skin. Deficiency of Vitamin A leads to night blindness, xerophthalmia (dry eyes), weakened immunity, and increased child mortality.
To combat Vitamin A Deficiency (VAD), the Government of India has implemented the Vitamin A Supplementation (VAS) Program under the National Programme for Prevention of Nutritional Blindness (NPPNB).
Objectives of the Vitamin A Supplementation Programme
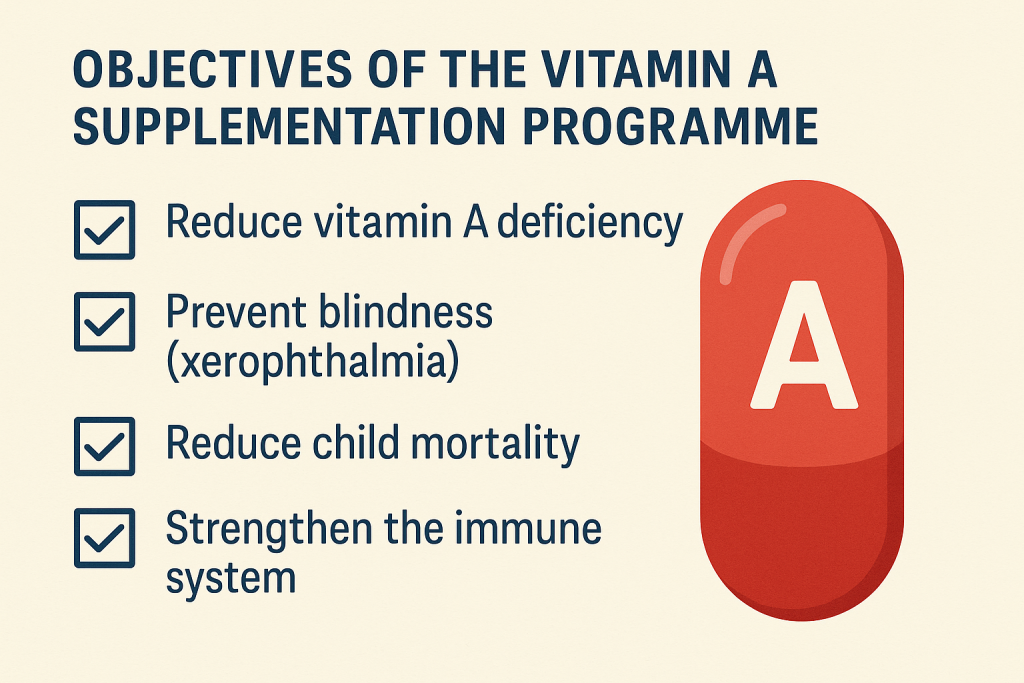
- Prevent and treat Vitamin A deficiency among children.
- Reduce the prevalence of night blindness and xerophthalmia.
- Improve child survival rates by enhancing immunity.
- Reduce mortality from infectious diseases, such as measles and diarrhea.
- Promote awareness about dietary sources of Vitamin A.
Implementation of the Vitamin A Supplementation Programme

The Ministry of Health and Family Welfare (MoHFW) and ICDS (Integrated Child Development Services) implement this program through Anganwadi centers, primary health centers (PHCs), and sub-centers.
Target Beneficiaries
- Children aged 6 months to 5 years.
- Pregnant and lactating mothers (indirectly through dietary interventions).
Dosage and Administration
As per the Government of India and WHO guidelines, Vitamin A is provided in high-dose liquid form (oral solution).
| Age Group | Dosage of Vitamin A | Administration Frequency |
|---|---|---|
| 6-11 months | 1,00,000 IU (International Units) | Once |
| 12-59 months | 2,00,000 IU | Every 6 months |
- The first dose is given at 9 months along with the measles vaccine.
- The second dose is administered at 18 months.
- The remaining doses are given every 6 months until 5 years of age.
Modes of Delivery
- Routine Immunization Days:
- Vitamin A is administered at immunization sessions in health facilities, Anganwadi centers, and outreach camps.
- Mass Supplementation Campaigns:
- Conducted as Bi-Annual Vitamin A Rounds in collaboration with ICDS and Health Departments.
- Distributed along with deworming tablets to enhance absorption.
- Integrated Child Health and Nutrition Programs:
- Linked with Poshan Abhiyaan and other maternal-child health programs.
- Includes nutrition counseling for mothers.
Impact of the Vitamin A Supplementation Programme
✅ Reduced Prevalence of Vitamin A Deficiency:
- India has seen a decline in childhood blindness due to Vitamin A deficiency.
✅ Lowered Child Mortality:
- Vitamin A supplementation has been linked to a 23% reduction in child mortality due to measles, diarrhea, and respiratory infections.
✅ Improved Immunity & Health Outcomes:
- Strengthened resistance against common childhood infections.
Challenges in Implementation
🔴 Low Coverage in Some Areas – Due to lack of awareness and irregular supply.
🔴 Missed Doses – Many children do not receive all required doses.
🔴 Inadequate Monitoring – Difficulty in tracking Vitamin A deficiency trends.
🔴 Limited Awareness – Mothers are not always aware of the benefits of Vitamin A supplementation.
Government Initiatives & Support Programs
🌿 National Programme for Prevention of Nutritional Blindness (NPPNB)
🌿 POSHAN Abhiyaan (National Nutrition Mission)
🌿 Integrated Child Development Services (ICDS)
🌿 Universal Immunization Programme (UIP)
🌿 National Health Mission (NHM)
These programs integrate Vitamin A supplementation with child health initiatives, ensuring wider reach and higher coverage.
Dietary Sources of Vitamin A
Apart from supplementation, natural dietary intake is encouraged.
| Animal Sources (Rich in Retinol) | Plant Sources (Rich in Beta-Carotene) |
|---|---|
| Liver (chicken, beef) | Carrots 🥕 |
| Egg yolk 🍳 | Sweet potatoes 🍠 |
| Fish 🐟 (cod liver oil) | Pumpkin 🎃 |
| Milk & dairy products 🥛 | Mangoes 🥭 |
| Butter & cheese 🧈 | Green leafy vegetables (Spinach, Methi, Drumstick leaves) 🌿 |
Future Recommendations
✅ Strengthen Vitamin A Supplementation Programs – Ensure 100% coverage.
✅ Improve Awareness among Parents – Educate mothers about the importance of Vitamin A.
✅ Enhance Monitoring & Data Collection – Use digital tracking systems to follow up on children’s supplementation status.
✅ Promote Dietary Diversification – Encourage intake of Vitamin A-rich foods.
✅ Combine with Other Nutrition Programs – Integrate with deworming and immunization programs for maximum benefit.
Anemia Mukt Bharat (AMB) Programme
Introduction
Anemia is a major public health problem in India, especially among children, adolescents, pregnant and lactating women, and women of reproductive age. The Anemia Mukt Bharat (AMB) initiative was launched in 2018 under the National Health Mission (NHM) to reduce anemia prevalence across the country.
The program builds on the National Iron Plus Initiative (NIPI) and aims to reduce anemia prevalence by 3% per year among vulnerable groups.
Objectives of Anemia Mukt Bharat (AMB)
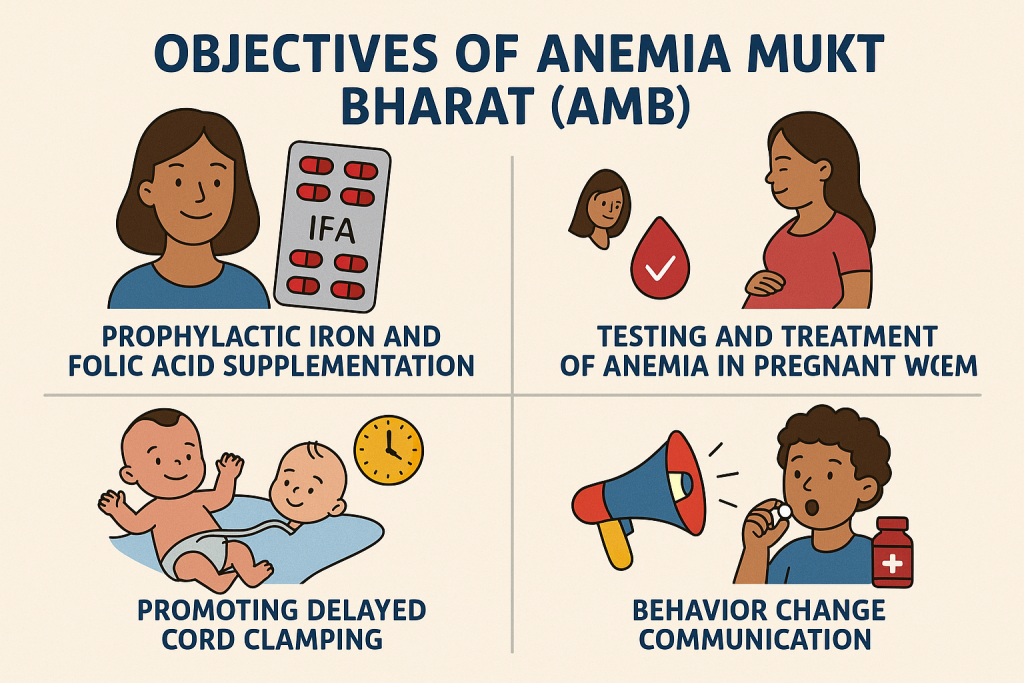
- Reduce anemia prevalence in all age groups (Children, Adolescents, Pregnant & Lactating Women, Women of Reproductive Age, and Men).
- Achieve a 3% annual reduction in anemia until anemia is significantly reduced.
- Strengthen supply chain management for Iron and Folic Acid (IFA) tablets.
- Enhance testing and treatment of anemia at all healthcare levels.
- Improve awareness about anemia prevention through behavior change communication.
Target Population
- Children (6 months – 59 months)
- School-going children (5-9 years, 10-19 years)
- Pregnant and lactating women
- Women of reproductive age (15-49 years)
- Men and elderly (as per health needs)
Implementation: The 6x6x6 Strategy

The AMB program follows a unique “6x6x6 Strategy”, which includes:
1. Six Interventions to Reduce Anemia
- Prophylactic Iron and Folic Acid (IFA) Supplementation
- Distribution of IFA tablets to all high-risk groups.
- Deworming (Bi-Annual Albendazole Supplementation)
- Reducing parasitic infections that contribute to anemia.
- Testing and Treatment of Anemia
- Routine Hemoglobin (Hb) testing and follow-up treatment.
- Addressing Non-Nutritional Causes of Anemia
- Malaria, infections, and genetic disorders (e.g., Sickle Cell Anemia, Thalassemia).
- Behavior Change Communication (BCC)
- Educating communities about anemia, diet, and hygiene practices.
- Strengthening Supply Chain and Logistics
- Ensuring regular availability of IFA tablets and deworming medicines.
2. Six Institutional Mechanisms for Effective Implementation
- POSHAN Abhiyaan: Integrated with maternal and child health programs.
- Jan Andolan Campaign: Community-based awareness activities.
- School-Based and Anganwadi-Based IFA Supplementation.
- Collaboration with Various Ministries (Health, Women & Child Development, Education, etc.).
- Use of Digital Technology for Monitoring (ANMOL app, Poshan Tracker).
- National and State-Level Monitoring and Review Committees.
3. Six Key Indicators for Anemia Reduction
The success of the program is measured using six key monitoring indicators:
- Percentage of children and women receiving IFA supplementation.
- Percentage of children receiving deworming tablets.
- Percentage of pregnant women tested and treated for anemia.
- Reduction in anemia prevalence among target groups.
- Availability of IFA tablets in schools, Anganwadi centers, and health centers.
- Community awareness levels about anemia and its prevention.
Dosage of Iron and Folic Acid (IFA) Supplementation
The AMB program provides different doses of Iron and Folic Acid to different age groups:
| Target Group | IFA Dosage | Frequency |
|---|---|---|
| Children (6-59 months) | 1ml IFA Syrup (20 mg Iron + 100 mcg Folic Acid) | Bi-weekly |
| Children (5-9 years) | 45 mg Iron + 400 mcg Folic Acid | Weekly |
| Adolescents (10-19 years) | 60 mg Iron + 500 mcg Folic Acid | Weekly |
| Pregnant & Lactating Women | 100 mg Iron + 500 mcg Folic Acid | Daily for 180 days |
| Women of Reproductive Age (15-49 years) | 60 mg Iron + 500 mcg Folic Acid | Weekly |
Key Features of Anemia Mukt Bharat
✅ Focus on High-Risk Groups – Children, women, adolescents, pregnant & lactating mothers.
✅ Weekly Iron and Folic Acid Supplementation (WIFS) – School-based program for adolescents.
✅ Deworming Campaigns – Conducted twice a year for children and adolescents.
✅ Behavior Change Communication (BCC) – Awareness programs for dietary iron intake.
✅ Regular Anemia Testing and Treatment – At PHCs, Anganwadis, and hospitals.
✅ Jan Andolan for Community Participation – Mass campaigns for anemia prevention.
Impact of Anemia Mukt Bharat
📉 Reduction in Anemia Prevalence – Target of 3% annual decline in anemia.
📈 Improved Hemoglobin Levels – Increased iron supplementation coverage.
✅ Higher School Attendance and Work Productivity – Reduced anemia-related fatigue.
🔍 Better Maternal and Child Health Outcomes – Lower maternal anemia rates.
Challenges in Implementation
🔴 Low Awareness & Compliance – Many beneficiaries skip IFA supplements.
🔴 Logistics & Supply Chain Issues – Delayed availability of IFA tablets.
🔴 Underreporting of Anemia Cases – Many mild cases go undiagnosed.
🔴 Dietary Habits & Socioeconomic Barriers – Low iron-rich food consumption.
🔴 Lack of Health Facility Access – Rural and tribal areas face implementation gaps.
Strategies to Strengthen AMB
✅ Strengthening Distribution Systems – Ensure uninterrupted IFA tablet supply.
✅ Mass Awareness Campaigns – Promote iron-rich diets and anemia prevention.
✅ Capacity Building of Health Workers – Train ANMs, ASHAs, and Anganwadi workers.
✅ Community Engagement (Jan Andolan) – Encourage self-monitoring and family involvement.
✅ Integration with School Health Program – Expand IFA supplementation in schools.
✅ Targeted Interventions for High-Risk Areas – Special focus on rural, tribal, and urban slums.
Integrated Child Development Services (ICDS) Scheme

Introduction
The Integrated Child Development Services (ICDS) is one of India’s flagship welfare programs aimed at improving maternal and child health and nutrition. Launched in 1975, ICDS is a comprehensive early childhood development program that provides nutrition, health, and education services to children under 6 years, pregnant women, and lactating mothers.
The program is implemented by the Ministry of Women and Child Development (MWCD), Government of India, and operates through Anganwadi Centers (AWCs) at the grassroots level.
Objectives of ICDS
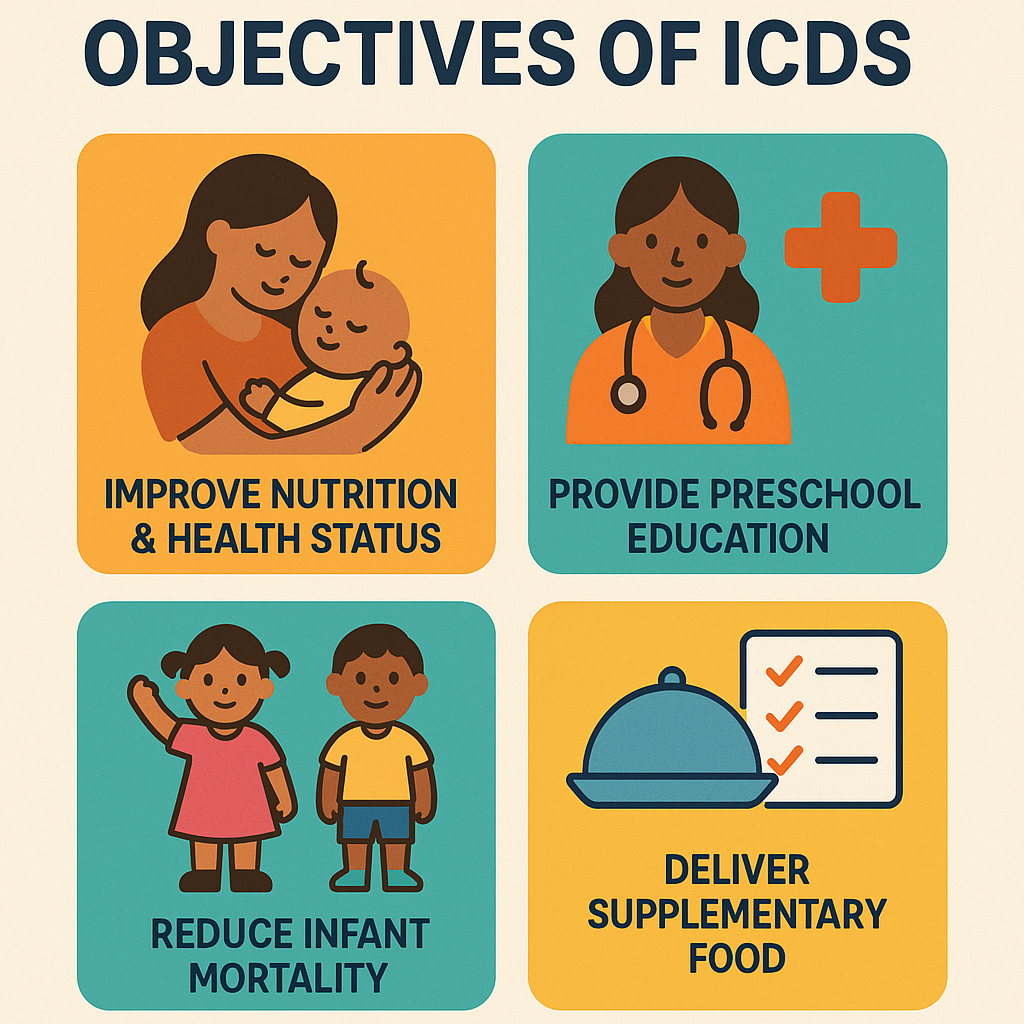
- Improve the nutritional and health status of children (0-6 years).
- Reduce child mortality, morbidity, malnutrition, and school dropout rates.
- Provide pre-school education to children (3-6 years).
- Enhance maternal nutrition and health during pregnancy and lactation.
- Break the cycle of malnutrition, ill-health, and poverty.
- Coordinate various policies and programs for child development.
Target Beneficiaries
The ICDS scheme primarily targets:
✔ Children (0-6 years) – Nutritional support and early childhood education.
✔ Pregnant and Lactating Women – Nutrition and healthcare services.
✔ Adolescent Girls (11-18 years) – Nutrition, health awareness, and vocational training.
✔ Mothers and Families – Nutrition education and awareness programs.
Services Provided Under ICDS
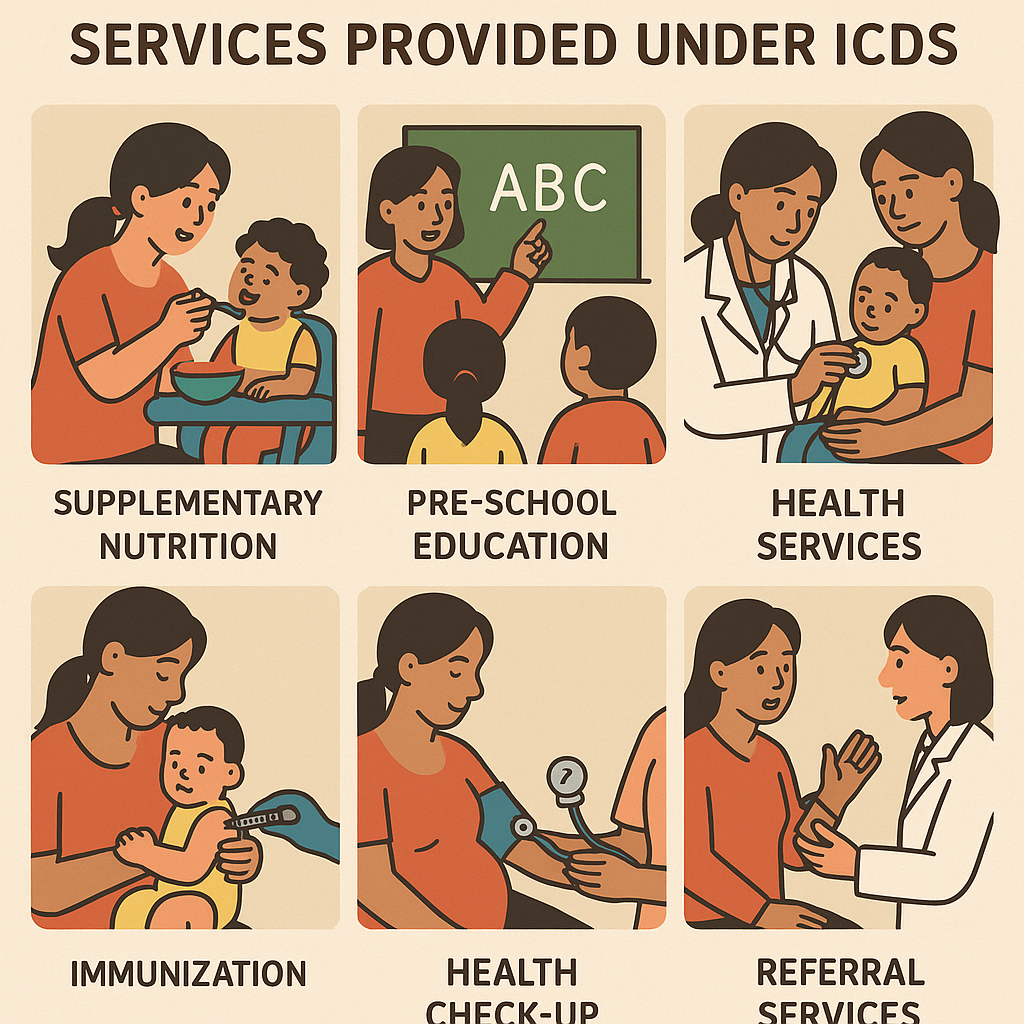
ICDS follows a multi-sectoral approach and provides six essential services through Anganwadi Centers (AWCs):
1. Supplementary Nutrition Programme (SNP)
- Hot cooked meals and take-home rations (THR) for children (6 months – 6 years).
- Nutritional support for pregnant and lactating women.
- Special food for malnourished children.
- Micronutrient supplementation (iron, folic acid, vitamin A).
2. Immunization
- Administered in coordination with the National Health Mission (NHM).
- Essential vaccines: BCG, DPT, Polio, Measles, Hepatitis B, and Vitamin A.
- Reduces infant mortality and childhood infections.
3. Health Check-ups
- Regular health check-ups for children, pregnant and lactating women.
- Growth monitoring and early detection of malnutrition and illnesses.
- Antenatal (ANC) and postnatal (PNC) care for mothers.
4. Referral Services
- Early identification and treatment of severe malnutrition and illnesses.
- Linkages with Primary Health Centers (PHCs) and hospitals.
5. Pre-School Non-Formal Education
- Early childhood education (ECE) for children aged 3-6 years.
- Prepares children for formal schooling.
- Uses play-based and activity-based learning.
6. Nutrition & Health Education (NHED)
- Awareness programs for mothers and families on:
- Balanced diet and hygiene.
- Breastfeeding and complementary feeding.
- Immunization and family planning.
- Conducted through Anganwadi workers and ASHAs.
Structure of ICDS Implementation
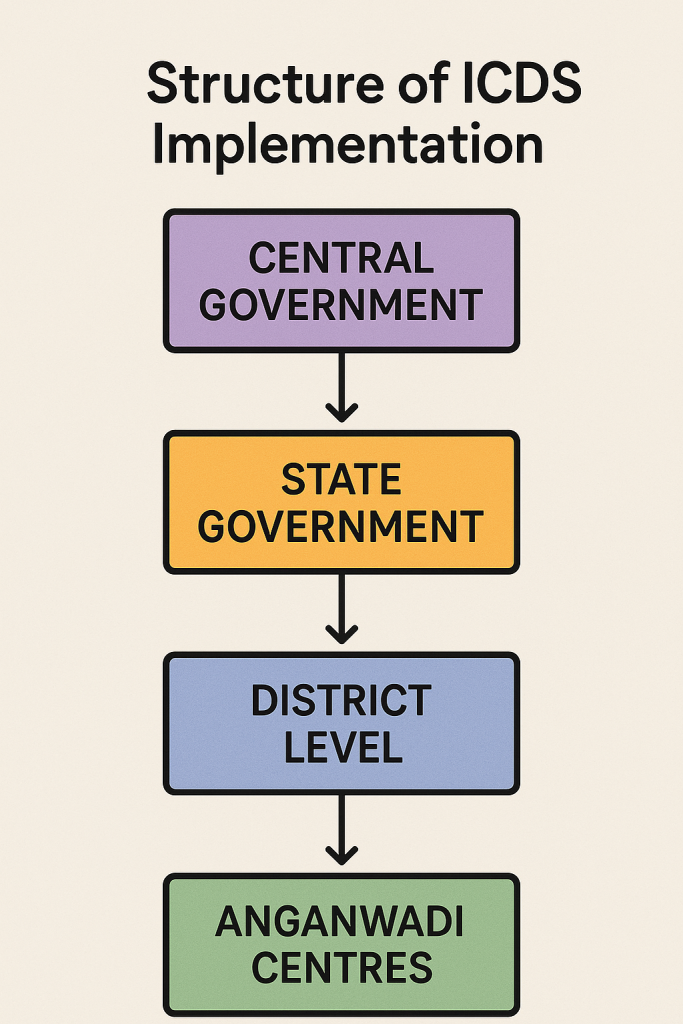
ICDS services are delivered through a three-tier system:
1. Anganwadi Centers (AWCs)
- The primary unit of service delivery.
- Each AWC covers a population of about 1000 in rural areas and 700 in tribal areas.
- Anganwadi Worker (AWW) and Helper manage the center.
2. District Level Administration
- The District Programme Officer (DPO) supervises ICDS operations.
- Each block has a Child Development Project Officer (CDPO).
3. State and National Level
- The State Government implements the ICDS with financial and technical support from the Central Government.
Nutritional Support Under ICDS
ICDS provides supplementary nutrition to different groups:
| Beneficiary | Type of Food Provided | Calories | Protein |
|---|---|---|---|
| Children (6 months – 3 years) | Take-Home Ration (THR) | 500 kcal | 12-15g |
| Children (3-6 years) | Hot cooked meal | 500 kcal | 12-15g |
| Severely Malnourished Children | Special Nutritional Supplements | 800 kcal | 20-25g |
| Pregnant & Lactating Women | Take-Home Ration (THR) | 600 kcal | 18-20g |
Key Government Initiatives Under ICDS
1. POSHAN Abhiyaan (2018)
- Focuses on reducing stunting, undernutrition, and anemia.
- Uses real-time monitoring (Poshan Tracker App) for better implementation.
2. Pradhan Mantri Matru Vandana Yojana (PMMVY)
- Provides financial assistance (₹5000) to pregnant women for improved nutrition.
3. Saksham Anganwadi and Poshan 2.0 (2021)
- Strengthens Anganwadi infrastructure and digital tracking of nutrition services.
- Integrates POSHAN Abhiyaan and ICDS for better outcomes.
Impact of ICDS Programme
✅ Reduced Malnutrition – ICDS has helped in lowering stunting, wasting, and underweight prevalence among children.
✅ Improved Immunization Coverage – Better vaccination rates for infants and children.
✅ Increased School Readiness – Pre-school education under ICDS improves cognitive development.
✅ Better Maternal and Child Health – Improved nutrition during pregnancy and lactation.
Challenges in ICDS Implementation
🔴 Inadequate Infrastructure – Many Anganwadi centers lack proper buildings and facilities.
🔴 Irregular Supply of Nutrition – Delays in food distribution affect program effectiveness.
🔴 Poor Awareness & Community Participation – Many beneficiaries are unaware of ICDS services.
🔴 Overburdened Anganwadi Workers – AWWs have multiple responsibilities with low salaries.
🔴 Urban Slum Coverage Issues – ICDS coverage is weaker in urban areas compared to rural areas.
Recommendations to Strengthen ICDS
✅ Strengthen Anganwadi Infrastructure – Improve facilities and ensure proper storage of food.
✅ Enhance Monitoring & Digital Tracking – Use Poshan Tracker App for real-time data collection.
✅ Improve Training for Anganwadi Workers – Provide better salaries and skill development programs.
✅ Increase Community Awareness – Conduct mass campaigns to encourage participation.
✅ Expand Urban ICDS Coverage – Focus on slums and migrant populations.
Mid-Day Meal Scheme (MDMS)
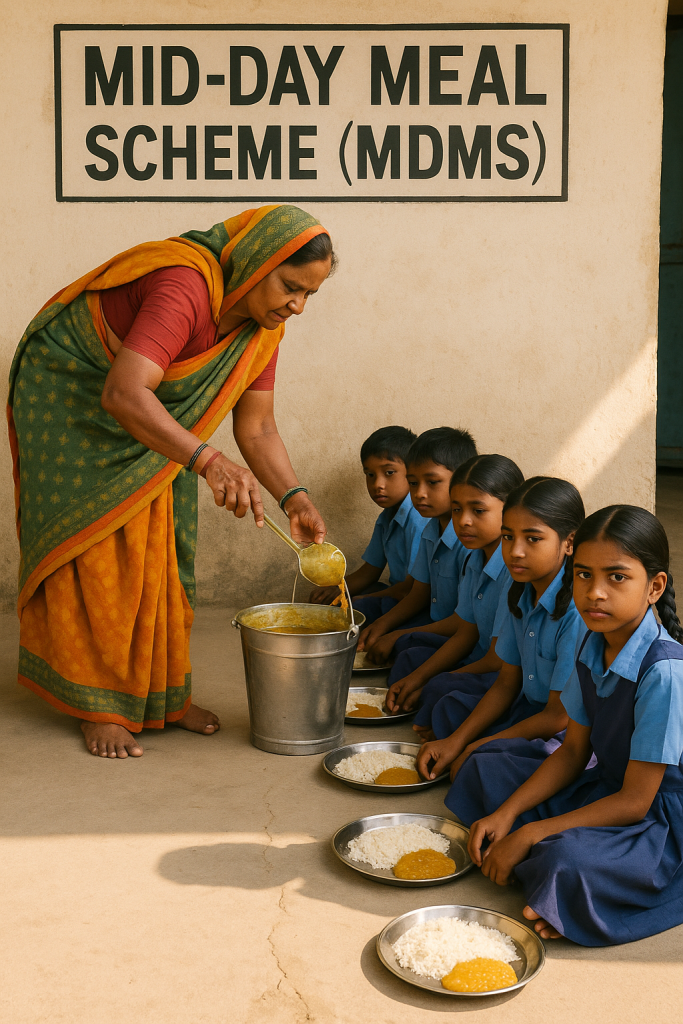
Introduction
The Mid-Day Meal Scheme (MDMS) is the largest school feeding program in the world, aimed at improving the nutritional status of children in government and government-aided schools in India. Launched in 1995 under the National Programme of Nutritional Support to Primary Education (NP-NSPE), it provides free, cooked meals to school-going children, helping to improve school enrollment, attendance, and learning outcomes.
The scheme was later revamped as PM POSHAN (Pradhan Mantri Poshan Shakti Nirman Yojana) in 2021 to further strengthen its impact.
Objectives of the Mid-Day Meal Scheme

- Improve the nutritional status of children in primary and upper primary schools.
- Encourage school enrollment and attendance, especially among disadvantaged children.
- Reduce dropout rates and improve learning outcomes.
- Address classroom hunger and improve concentration levels.
- Promote social equity by encouraging children of all backgrounds to eat together.
- Support women’s employment by hiring female cooks from weaker sections.
Target Beneficiaries
The Mid-Day Meal Scheme covers:
✔ Children in Classes I-VIII (Primary and Upper Primary levels).
✔ Government Schools, Government-Aided Schools, and Special Training Centers (STCs).
✔ Madrasas and Maqtabs supported under the Sarva Shiksha Abhiyan (SSA).
Nutritional Norms of Mid-Day Meal
The meal provided under MDMS must meet specific caloric and protein requirements:
| Category | Calories (kcal per meal) | Protein (grams per meal) |
|---|---|---|
| Primary (Class I-V) | 450 kcal | 12g protein |
| Upper Primary (Class VI-VIII) | 700 kcal | 20g protein |
The menu includes:
- Rice/Wheat-based dishes (roti, khichdi, pulao, etc.).
- Dal, vegetables, and pulses for protein.
- Milk, eggs, and fruits (as per state policies).
- Fortified foods (iron, folic acid, vitamin A, etc.).
Key Features of the Mid-Day Meal Scheme
1. Free Cooked Mid-Day Meals
- Meals are prepared fresh every day and served hot.
- Cooked by women from Self-Help Groups (SHGs) or Anganwadi workers.
2. Decentralized Implementation
- State governments and local authorities manage meal preparation and distribution.
- Schools, NGOs, and Self-Help Groups (SHGs) play a role in food supply.
3. Community Participation
- Mothers and community members are encouraged to oversee meal preparation.
- Panchayati Raj Institutions (PRIs) ensure quality control.
4. Food Safety and Hygiene
- Schools follow strict guidelines on food safety, hygiene, and quality control.
- Automated Monitoring System (AMS) tracks meal distribution.
Government Support & Funding
The Mid-Day Meal Scheme is a centrally-sponsored scheme, meaning both the Central Government and State Governments share funding.
Cost-Sharing Structure
| Category | Central Government Share | State Government Share |
|---|---|---|
| Food Cost | 100% for UTs; 60% for States | 40% for States |
| Cooking Cost | 60% (Centre) | 40% (State) |
| Honorarium for Cooks | ₹1000 per month per cook | State covers the rest |
Annual Budget Allocation (2022-23)
- The Government allocated ₹12,800 crore under PM POSHAN.
Role of PM POSHAN (Revamped MDMS in 2021)
In September 2021, the Mid-Day Meal Scheme was renamed PM POSHAN (Pradhan Mantri Poshan Shakti Nirman Yojana).
New Features Introduced in PM POSHAN:
✅ Extension to Pre-Primary Students (before only Class I-VIII students were covered).
✅ Focus on Nutrient-Rich Foods (fortified foods with iron, vitamin A, folic acid).
✅ School Nutrition Gardens (encouraging schools to grow their own vegetables).
✅ Women’s Empowerment (preference for female workers from SC/ST/OBC communities).
✅ Health Check-Ups and Deworming (linked with Rashtriya Bal Swasthya Karyakram – RBSK).
Impact of the Mid-Day Meal Scheme
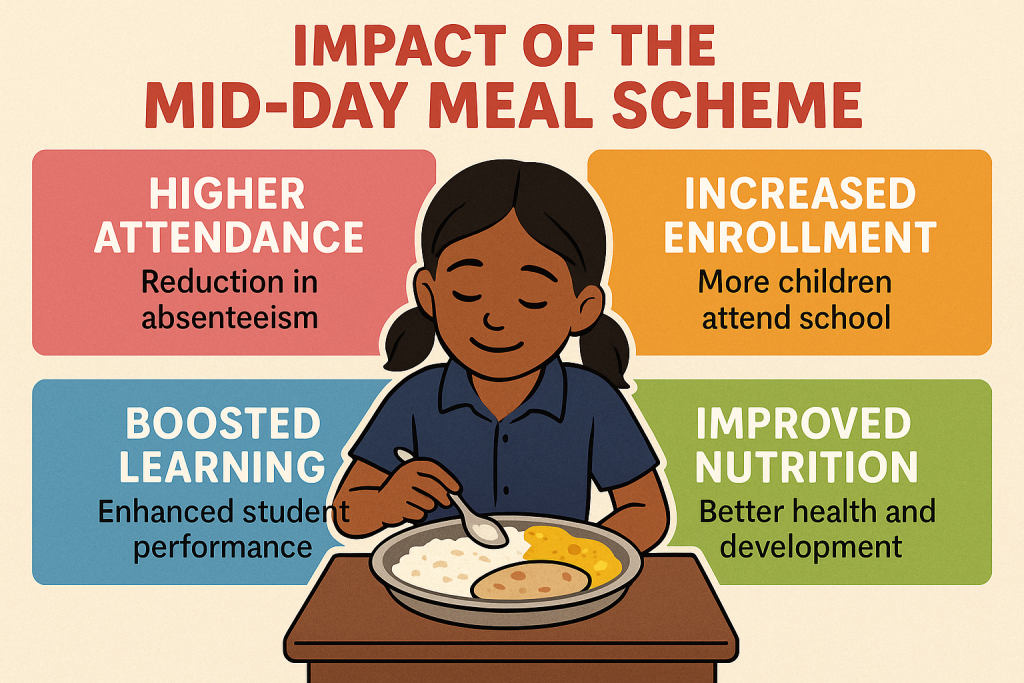
📉 Reduction in Malnutrition & Classroom Hunger
- Improved weight and height among children.
- Decline in anemia and vitamin deficiencies.
📈 Increased School Enrollment & Attendance
- More children from poor backgrounds attend school regularly.
- Reduced dropout rates, especially among girls.
👩⚕️ Improved Health & Immunity
- Better nutritional intake helps in reducing illness and infections.
🤝 Social Equity & Gender Inclusion
- Children from different castes, religions, and backgrounds eat together.
- Empowers women by providing employment as cooks.
Challenges in Implementation
🚨 Irregular Food Supply – Delays in distribution affect meal quality.
🚨 Food Safety Issues – Contaminated food incidents raise concerns.
🚨 Leakages & Corruption – Diversion of funds and food supply.
🚨 Poor Infrastructure in Schools – Lack of clean kitchens and dining areas.
🚨 Inadequate Monitoring & Evaluation – Some schools report fake attendance to receive more funds.
Steps to Improve the Scheme
✅ Stronger Monitoring & Digital Tracking – Using real-time data tracking (AMS – Automated Monitoring System).
✅ Strict Quality Control Measures – Regular food safety inspections.
✅ Expanding Fortification & Nutrient-Rich Meals – Adding millets, dairy, and protein sources.
✅ Better Infrastructure & Kitchen Facilities – Constructing modern kitchens & dining halls.
✅ Community Involvement – Parents and local bodies should monitor meal quality.
National Iodine Deficiency Disorders Control Programme (NIDDCP)
Introduction
Iodine is an essential micronutrient required for the production of thyroid hormones, which regulate growth, brain development, and metabolism. Iodine Deficiency Disorders (IDDs) are a major public health problem in India, affecting pregnant women, children, and adults.
To eliminate iodine deficiency, the Government of India launched the National Goiter Control Programme (NGCP) in 1962, which was later renamed as the National Iodine Deficiency Disorders Control Programme (NIDDCP) in 1992.
Objectives of NIDDCP
The primary aim of the program is to eliminate iodine deficiency disorders (IDDs) and ensure universal iodized salt consumption.
Specific Objectives:
- Ensure adequate iodine intake for all individuals, especially pregnant women and children.
- Achieve and maintain universal household use of iodized salt.
- Prevent and reduce iodine deficiency disorders such as goiter, cretinism, and mental retardation.
- Monitor and regulate salt iodization at production and distribution levels.
- Educate the public on the importance of iodine in diet.
- Strengthen surveillance through laboratory testing of salt and urine iodine levels.
Iodine Deficiency Disorders (IDDs) and Health Impacts
Iodine deficiency affects people of all ages and leads to serious health consequences:
| Age Group | Disorder Due to Iodine Deficiency |
|---|---|
| Fetus (Unborn Child) | Cretinism, brain damage, miscarriage, stillbirth |
| Infants & Young Children | Mental retardation, stunted growth, speech & hearing impairment |
| School-Age Children | Poor concentration, learning disabilities, goiter |
| Adults | Hypothyroidism, goiter, reduced productivity |
| Pregnant Women | Miscarriages, premature births, low birth weight |
Common Iodine Deficiency Disorders (IDDs)
- Goiter – Swelling of the thyroid gland.
- Cretinism – Severe mental and physical retardation in newborns.
- Hypothyroidism – Slow metabolism, fatigue, weight gain.
- Mental Impairment – Reduced IQ and cognitive ability.
Key Components of NIDDCP
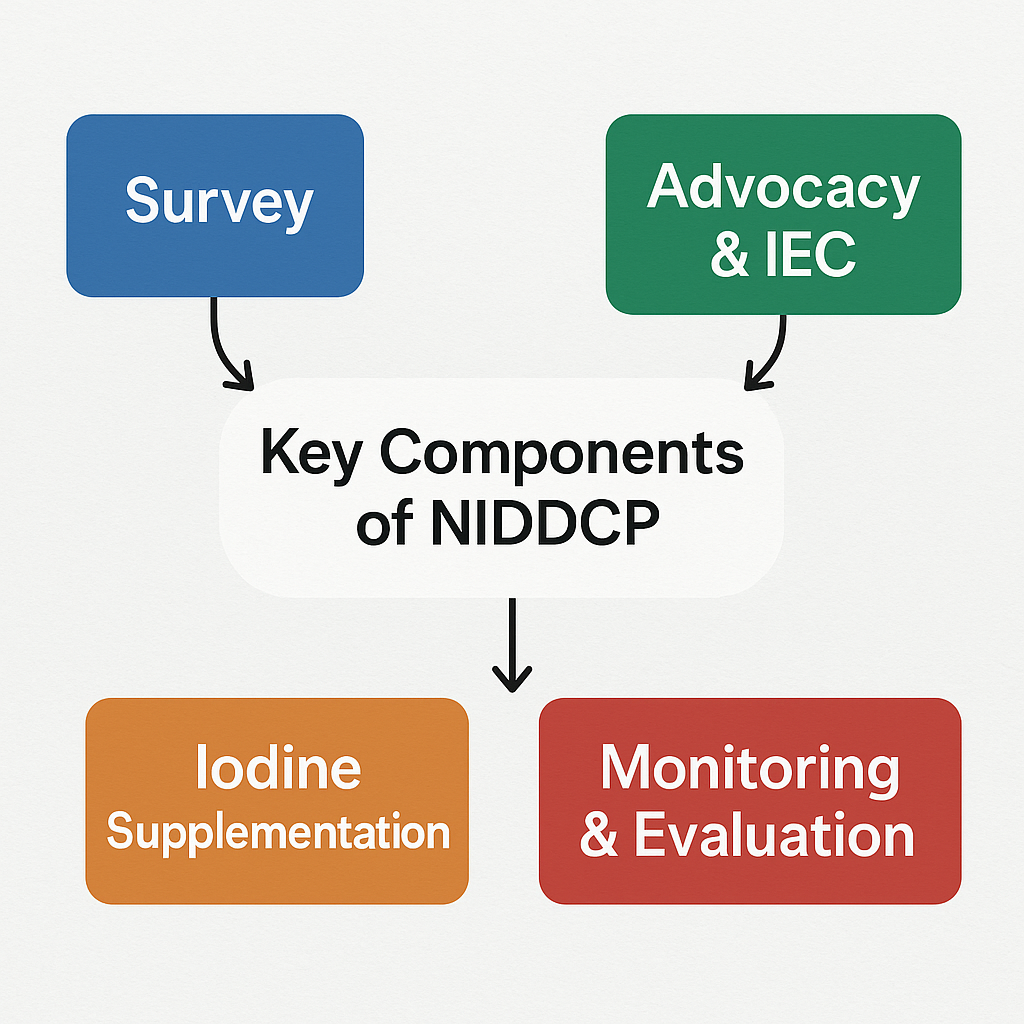
To eliminate IDDs, NIDDCP focuses on five major components:
1. Universal Salt Iodization (USI)
✅ Mandatory iodization of salt (40 ppm at production and 15 ppm at consumer level).
✅ Ban on non-iodized salt for human consumption (1998).
✅ Fortification of salt with iodine to ensure 100% iodized salt consumption.
2. IDD Monitoring & Surveillance
✅ Testing salt and urine iodine levels through laboratory surveillance.
✅ Annual surveys to track iodine deficiency trends.
✅ Strengthening district and state-level laboratories for IDD detection.
3. Public Awareness & Education
✅ Mass media campaigns on the importance of iodine (TV, radio, newspapers).
✅ IEC (Information, Education & Communication) programs in schools and villages.
✅ Promotion of iodized salt use through community awareness.
4. Capacity Building & Training
✅ Training of health workers, Anganwadi workers, and teachers on iodine deficiency.
✅ Regular workshops for salt producers and distributors on quality control.
5. Law Enforcement & Regulation
✅ Mandatory Salt Iodization Laws – Ban on non-iodized salt production & sale.
✅ Strict quality control of salt at production, wholesale, and retail levels.
Implementation & Structure of NIDDCP
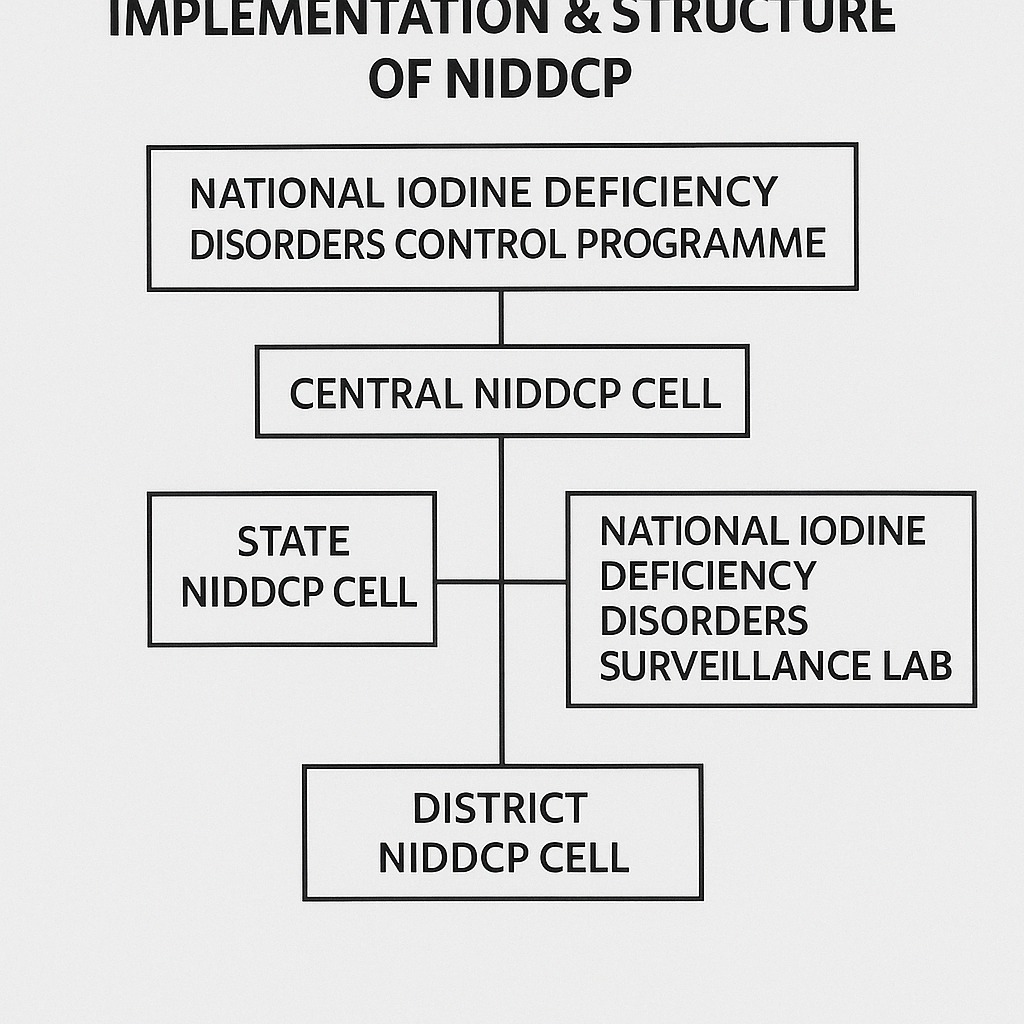
The Ministry of Health & Family Welfare (MoHFW) implements the program in collaboration with State Governments, Food Safety Authorities, and NGOs.
NIDDCP Organizational Structure
- National Level – Policy-making, funding, nationwide monitoring (MoHFW).
- State Level – Implementation through health departments & IDD cells.
- District Level – Salt testing labs, school screening programs, community awareness.
Impact of NIDDCP in India
📈 Increased Iodized Salt Consumption – Over 92% of Indian households now use iodized salt.
📉 Reduction in Goiter & IDDs – Significant decline in goiter cases.
🔬 Better Monitoring & Testing – 30+ state IDD monitoring labs established.
📢 Increased Awareness – More people understand the role of iodine in health.
Success Stories
- Tamil Nadu & Gujarat achieved near-total IDD elimination through strict monitoring.
- Himachal Pradesh & West Bengal reduced IDD prevalence through school programs.
Challenges in NIDDCP Implementation
🚨 Non-Compliance by Salt Manufacturers – Some producers sell low-iodine salt.
🚨 Weak Monitoring & Enforcement – Limited salt quality checks in some states.
🚨 Public Misconceptions – Many believe sea salt naturally contains iodine (it does not).
🚨 Ineffective Distribution in Rural Areas – Poor logistics lead to low iodine levels in certain regions.
Future Strategies for Strengthening NIDDCP
✅ Strict Enforcement of Salt Iodization Laws – Regular factory inspections.
✅ Expanding Digital Tracking of Salt Testing – Mobile-based salt monitoring.
✅ Strengthening Public Awareness Campaigns – Use of social media, school programs.
✅ Improving Supply Chain & Distribution – Ensure iodized salt availability in remote areas.
✅ Integrating IDD Screening in Routine Health Check-ups – Thyroid testing in high-risk groups.
Weekly Iron Folic Acid Supplementation (WIFS) Programme
Introduction
The Weekly Iron Folic Acid Supplementation (WIFS) Programme was launched in 2012 by the Ministry of Health and Family Welfare (MoHFW), Government of India, to combat iron deficiency anemia among adolescents. The program provides weekly iron and folic acid (IFA) tablets to school-going and out-of-school adolescents to prevent and control anemia.
Anemia is a major public health problem in India, affecting 50% of adolescents due to poor dietary intake of iron, rapid growth during puberty, and menstrual blood loss in girls. The WIFS program is a part of the Anemia Mukt Bharat (AMB) initiative under the National Health Mission (NHM).
Objectives of WIFS Programme
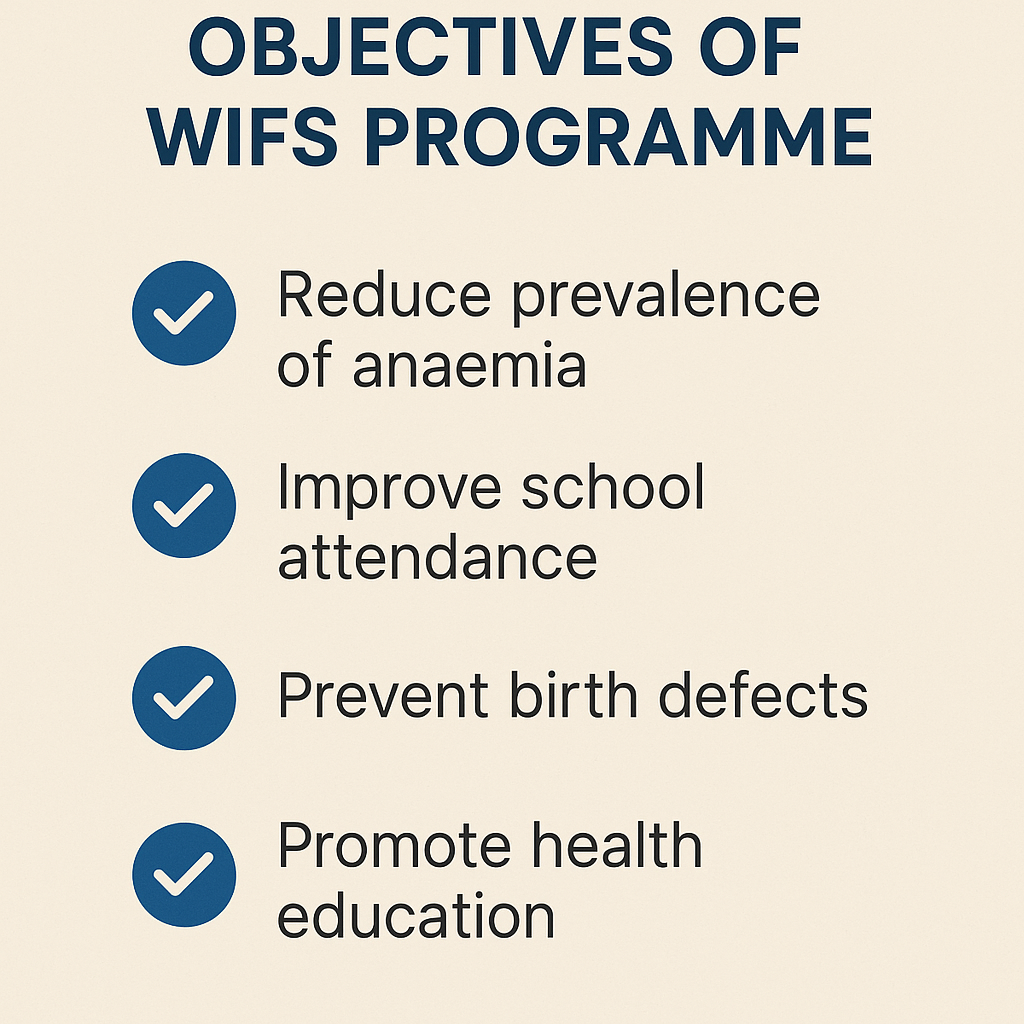
- Reduce the prevalence of anemia among adolescents (10-19 years).
- Provide weekly iron and folic acid supplementation (IFA) tablets to prevent and control anemia.
- Promote health and nutrition awareness among adolescents.
- Encourage dietary diversification with iron-rich foods.
- Enhance school-based health services for adolescent well-being.
Target Beneficiaries
The WIFS program covers:
✔ School-going adolescents (10-19 years) – Students from Class VI-XII in government, government-aided, and municipal schools.
✔ Out-of-school adolescents (10-19 years) – Covered through Anganwadi Centers (AWCs) and ASHAs.
✔ Both girls and boys receive IFA supplementation.
Components of WIFS Programme

The program consists of four major components:
1. Weekly Iron and Folic Acid (IFA) Supplementation
- One IFA tablet per week (60 mg elemental iron + 500 mcg folic acid).
- Distributed through schools, Anganwadi centers, and ASHA workers.
2. Bi-Annual Deworming (Albendazole Tablets)
- Given twice a year to improve iron absorption.
- Administered during National Deworming Day (February & August).
3. Nutrition and Health Education (NHE)
- Awareness sessions on anemia prevention, balanced diet, and menstrual hygiene.
- Conducted by teachers, health workers, and peer educators.
4. Screening & Treatment of Moderate to Severe Anemia
- Hemoglobin testing and referral of severely anemic adolescents to healthcare facilities.
- Management of cases through Primary Health Centers (PHCs) and hospitals.
Dosage of Iron Folic Acid (IFA) Supplementation
The WIFS program follows specific dosage guidelines:
| Target Group | IFA Dosage | Frequency |
|---|---|---|
| Adolescents (10-19 years, school-going & out-of-school) | 60 mg elemental iron + 500 mcg folic acid | Weekly (once a week) |
| Pregnant adolescents (10-19 years) | 100 mg elemental iron + 500 mcg folic acid | Daily for 180 days |
| Deworming (Albendazole tablet) | 400 mg Albendazole | Twice a year |
Implementation of WIFS Programme
The program is implemented through:
🔹 Schools (for school-going adolescents) – Teachers distribute IFA tablets every week.
🔹 Anganwadi Centers (for out-of-school adolescents) – ASHA workers provide IFA supplements.
🔹 Primary Health Centers (PHCs) – Manage anemic cases and provide treatment.
🔹 Monitoring System – Schools and Anganwadi centers maintain IFA consumption records.
Role of Various Functionaries in WIFS Implementation
✔ Teachers & School Health Coordinators – Distribute IFA tablets and conduct awareness sessions.
✔ ANMs (Auxiliary Nurse Midwives) & ASHAs – Provide IFA to out-of-school adolescents and report compliance.
✔ State & District Health Officials – Oversee program implementation and monitor anemia prevalence.
✔ Panchayati Raj Institutions (PRIs) & NGOs – Support community awareness and outreach efforts.
Impact of WIFS Programme
✅ Reduced Anemia Prevalence – Helps lower iron deficiency anemia among adolescents.
✅ Improved School Attendance & Performance – Prevents fatigue and enhances concentration.
✅ Better Maternal & Child Health Outcomes – Reduces anemia-related complications during pregnancy.
✅ Increased Awareness About Nutrition & Hygiene – Promotes healthy eating habits and menstrual hygiene.
Challenges in WIFS Implementation
🚨 Low Compliance & Irregular Consumption – Adolescents may skip weekly IFA intake.
🚨 Supply Chain Issues – Delays in the distribution of IFA tablets in some areas.
🚨 Lack of Awareness Among Parents & Adolescents – Many do not understand the importance of IFA supplementation.
🚨 Misinformation About IFA Side Effects – Fear of nausea and dark stools leads to discontinuation.
Future Strategies to Strengthen WIFS
✅ Strengthening Supply Chain Management – Ensure regular availability of IFA tablets.
✅ Using Digital Tracking & Mobile Apps – Monitor IFA consumption and anemia prevalence.
✅ Enhancing Peer Educator Networks – Train adolescents as “Anemia Awareness Ambassadors”.
✅ Integration with POSHAN Abhiyaan & Anemia Mukt Bharat – Improve coordination between health and education sectors.
✅ Expanding Awareness Campaigns – Use social media, school events, and local community programs for better reach.
Additional National Nutrition and Health Programs in India
Apart from the Mid-Day Meal Scheme, ICDS, Anemia Mukt Bharat, WIFS, and NIDDCP, India has several other nutrition and health programs to tackle malnutrition, micronutrient deficiencies, and food insecurity. Below are some important ones:
1. Poshan Abhiyaan (National Nutrition Mission) – 2018

- Aim: Reduce stunting, undernutrition, anemia, and low birth weight in children, adolescents, and women.
- Key Features:
- ICT-based real-time monitoring (Poshan Tracker App).
- Jan Andolan (Mass Movement) to spread nutrition awareness.
- Home-based nutrition counseling by Anganwadi workers.
- Focus on first 1,000 days of a child’s life.
- Target Reduction:
- 2% reduction per year in stunting & undernutrition.
- 3% reduction per year in anemia.
2. National Food Security Act (NFSA) – 2013
- Aim: Provide subsidized food grains to poor households to ensure food security.
- Key Features:
- “One Nation, One Ration Card” (ONORC) for migrant beneficiaries.
- Rice at ₹3/kg, Wheat at ₹2/kg, and Coarse Grains at ₹1/kg for eligible families.
- Covers 75% of rural and 50% of urban populations under food security schemes.
3. Pradhan Mantri Matru Vandana Yojana (PMMVY) – 2017
- Aim: Provide financial assistance (₹5,000) to pregnant women for better maternal nutrition.
- Key Features:
- ₹5,000 is given in three installments (early pregnancy, institutional delivery, and child vaccination).
- Linked with ICDS and NHM to improve maternal care.
- Encourages institutional deliveries and exclusive breastfeeding.
4. Rashtriya Bal Swasthya Karyakram (RBSK) – 2013
- Aim: Early identification and treatment of diseases, deficiencies, disabilities, and developmental delays in children.
- Key Features:
- Free health screening for children aged 0-18 years.
- Covers nutritional deficiencies like anemia, malnutrition, Vitamin A & D deficiencies.
- Provides free treatment and referral services for severe cases.
5. National Programme on Prevention & Control of Non-Communicable Diseases (NP-NCD)
- Aim: Reduce the burden of obesity, diabetes, hypertension, and cardiovascular diseases caused by poor nutrition.
- Key Features:
- Screening of school children and adults for obesity and related conditions.
- Promotion of healthy eating habits and lifestyle changes.
- Linked with Anemia Mukt Bharat and Poshan Abhiyaan.
6. Pradhan Mantri Garib Kalyan Anna Yojana (PMGKAY) – 2020 (COVID-19 Relief)
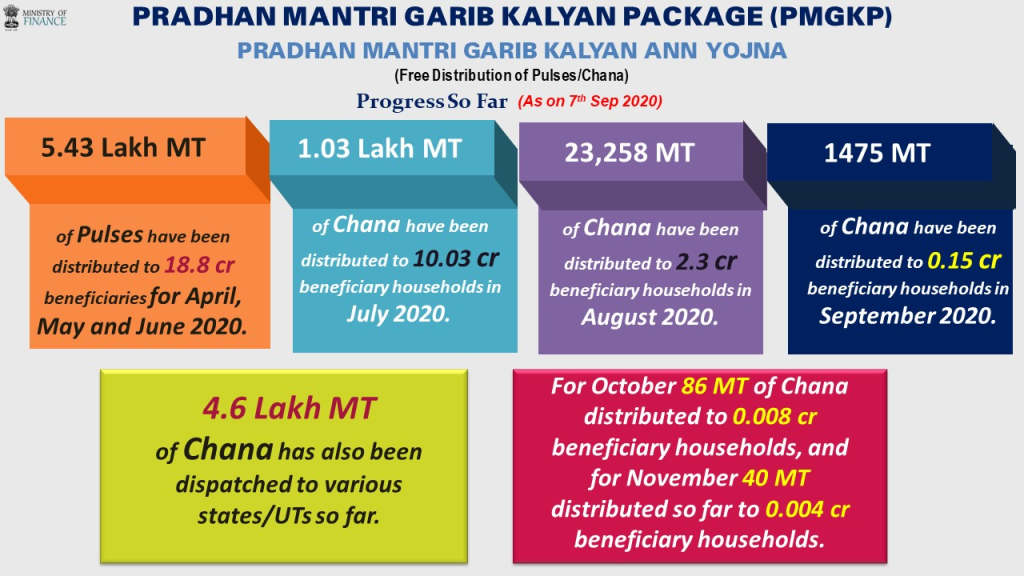
- Aim: Provide free food grains (5 kg of rice/wheat + 1 kg of dal per person per month) to poor families during COVID-19.
- Key Features:
- Covered 80 crore people under NFSA.
- Distributed free wheat/rice, pulses, and cooking oil.
- Continued in 2021-2023 to ensure food security post-pandemic.
7. Eat Right India Movement – 2018

- Aim: Promote safe, healthy, and sustainable diets among Indians.
- Key Features:
- Fortification of rice, milk, and edible oils with micronutrients.
- Awareness campaigns on reducing sugar, salt, and fat intake.
- Encourages healthy eating in schools and workplaces.
8. National Deworming Day (NDD) – Bi-Annual (February & August)

- Aim: Reduce worm infestations in children that cause malnutrition and anemia.
- Key Features:
- Albendazole tablets (400 mg) given to children (1-19 years) in schools and Anganwadi centers.
- Linked with Anemia Mukt Bharat & WIFS.
- Helps improve nutrient absorption and immunity in children.
9. Pradhan Mantri Kisan Samman Nidhi (PM-KISAN) – 2019
- Aim: Provide financial support to small and marginal farmers to improve food production and nutrition security.
- Key Features:
- ₹6,000 per year given in three installments to eligible farmers.
- Ensures better access to nutritious food for rural families.
10. Fortification of Rice & Other Staples – 2021
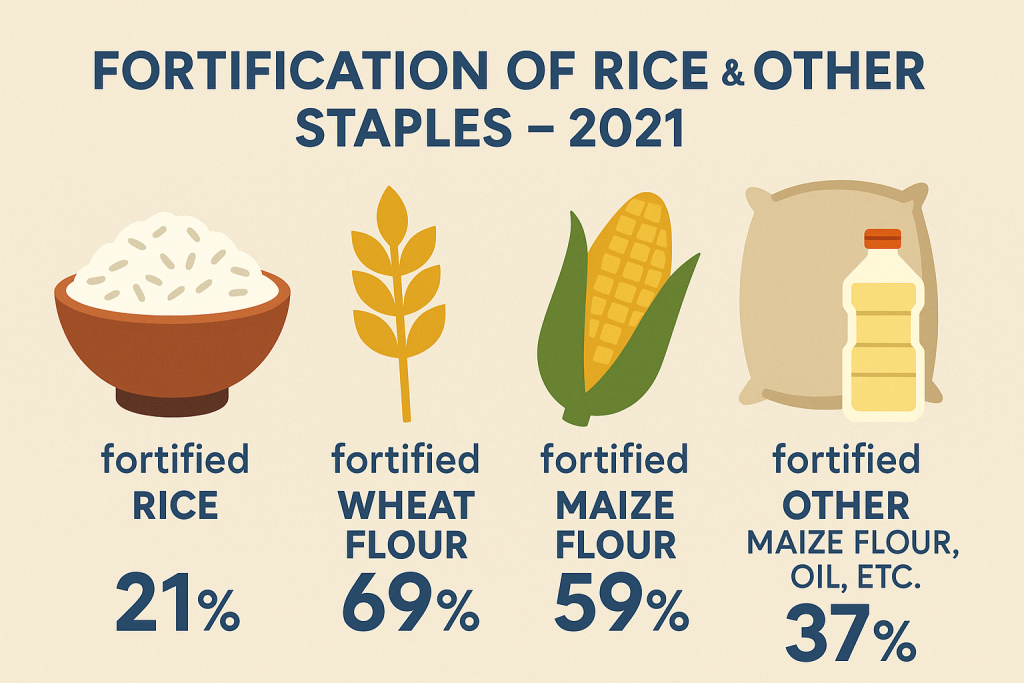
- Aim: Combat hidden hunger (micronutrient deficiencies) through fortified staple foods.
- Key Features:
- Iron, folic acid, and vitamin B12-fortified rice supplied through PDS, ICDS, and MDMS.
- Encourages use of fortified wheat flour, oil, and milk.
- Helps in reducing anemia and neural tube defects.
11. National Programme for Health Care of the Elderly (NPHCE) – 2010

- Aim: Improve nutrition and healthcare for senior citizens.
- Key Features:
- Special diet plans for elderly patients with diabetes, hypertension, and malnutrition.
- Linked with POSHAN Abhiyaan for better geriatric nutrition.
12. Mission Indradhanush – 2014
- Aim: Improve vaccination coverage for infants and pregnant women to prevent infections linked to malnutrition.
- Key Features:
- Covers diseases like measles, tuberculosis, polio, and diphtheria.
- Linked with Vitamin A supplementation to prevent childhood blindness.
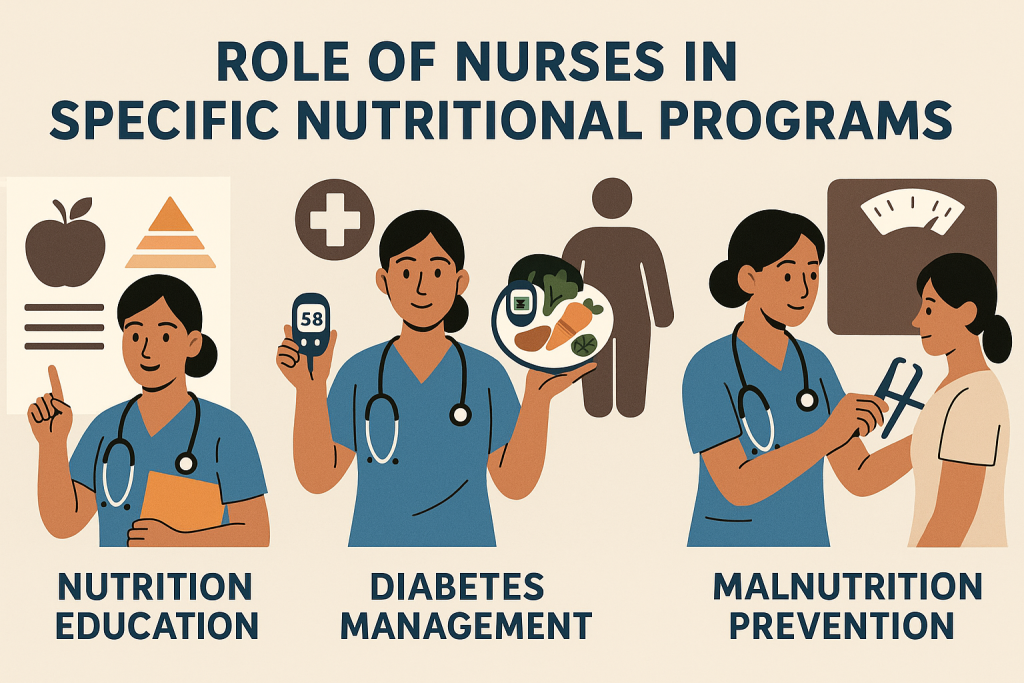
Role of Nurses in National Nutritional Programs.
Nurses play a vital role in the implementation, monitoring, and success of national nutritional programs in India. As frontline healthcare providers, they act as educators, caregivers, counselors, and facilitators in ensuring effective nutrition delivery to vulnerable populations.
General Responsibilities of Nurses in Nutritional Programs

- Nutritional Assessment
- Identify malnourished children, pregnant women, and elderly patients.
- Conduct BMI measurements, growth monitoring, and anemia screening.
- Detect micronutrient deficiencies (iron, vitamin A, iodine, etc.).
- Health Education & Awareness
- Educate mothers, adolescents, and community members on:
✔ Balanced diets and nutritional needs.
✔ Importance of breastfeeding and complementary feeding.
✔ Prevention of anemia, vitamin deficiencies, and lifestyle diseases.
- Educate mothers, adolescents, and community members on:
- Supplementary Nutrition & Micronutrient Distribution
- Administer Iron-Folic Acid (IFA), Vitamin A, deworming tablets, and iodized salt.
- Ensure regular distribution of fortified food items in Anganwadis and schools.
- Immunization & Disease Prevention
- Link vaccination programs (Mission Indradhanush) with nutrition programs.
- Ensure Vitamin A supplementation along with routine immunization.
- Monitoring & Follow-up
- Track nutritional progress using growth charts and hemoglobin levels.
- Conduct home visits for severely malnourished children and at-risk mothers.
- Collaboration with Government & NGOs
- Work with Anganwadi Workers (AWWs), ASHAs, and ANMs to implement programs.
- Coordinate with schools, community leaders, and self-help groups.
Role of Nurses in Specific Nutritional Programs
1. POSHAN Abhiyaan (National Nutrition Mission)
✔ Identify undernourished children and pregnant women.
✔ Educate mothers on early childhood nutrition and breastfeeding.
✔ Refer severely malnourished children to Nutritional Rehabilitation Centers (NRCs).
✔ Conduct community-based nutrition awareness programs.
2. Integrated Child Development Services (ICDS)
✔ Work with Anganwadi workers to provide supplementary nutrition.
✔ Conduct monthly weight monitoring of children under 6 years.
✔ Assist in pre-school health check-ups and deworming.
✔ Provide maternal nutrition counseling for pregnant and lactating mothers.
3. Mid-Day Meal Scheme (MDMS / PM POSHAN)
✔ Monitor quality and safety of school meals.
✔ Ensure iron and protein-rich foods are included in meals.
✔ Identify and report cases of malnourishment among school children.
✔ Conduct nutrition education sessions in schools.
4. Anemia Mukt Bharat (AMB)
✔ Conduct hemoglobin testing and screen for anemia in adolescents and women.
✔ Distribute weekly Iron-Folic Acid (IFA) tablets to adolescent girls and boys.
✔ Educate on iron-rich diets and prevention of anemia.
✔ Ensure bi-annual deworming (Albendazole distribution).
5. Weekly Iron-Folic Acid Supplementation (WIFS)
✔ Ensure weekly administration of IFA tablets in schools and Anganwadis.
✔ Monitor compliance and track anemia reduction in adolescents.
✔ Conduct awareness programs on menstrual hygiene and anemia prevention.
6. National Iodine Deficiency Disorders Control Programme (NIDDCP)
✔ Educate people about iodine-rich diets and iodized salt usage.
✔ Conduct urine iodine testing for early detection of iodine deficiency.
✔ Monitor goiter cases and hypothyroidism in communities.
7. Pradhan Mantri Matru Vandana Yojana (PMMVY)
✔ Assist in registering pregnant women for financial benefits.
✔ Ensure mothers receive proper antenatal care and nutrition counseling.
✔ Encourage institutional deliveries for maternal and neonatal health.
8. Rashtriya Bal Swasthya Karyakram (RBSK)
✔ Conduct growth monitoring and developmental screening in children.
✔ Identify malnourished children and refer them for medical intervention.
✔ Provide nutritional supplements and health education to families.
9. National Deworming Day (NDD)
✔ Administer Albendazole tablets to prevent worm infections.
✔ Educate children and parents on hygiene and sanitation.
✔ Monitor and report deworming coverage in schools and Anganwadis.
10. Eat Right India Movement
✔ Promote fortified foods (iodized salt, iron-fortified rice, fortified oil & milk).
✔ Educate people on reducing sugar, salt, and unhealthy fats in diet.
✔ Encourage healthy lifestyle habits and disease prevention.
11. Pradhan Mantri Garib Kalyan Anna Yojana (PMGKAY)
✔ Ensure nutritious food distribution in Anganwadis and ration shops.
✔ Educate families about balanced diet options using PDS grains.
12. Mission Indradhanush
✔ Ensure vaccination coverage for children and pregnant women.
✔ Administer Vitamin A supplementation to children under 5 years.
Challenges Faced by Nurses in Nutrition Programs
🚨 Low Awareness & Cultural Beliefs – Many rural families do not understand the importance of balanced diets.
🚨 Shortage of Staff & Resources – Nurses often handle multiple roles with limited facilities.
🚨 Non-Compliance with Supplementation – People may avoid taking IFA, Vitamin A, or deworming tablets due to myths.
🚨 Geographical Barriers – Remote areas face logistical challenges in food and medicine supply.
Recommendations to Strengthen the Role of Nurses
✅ Enhanced Training & Capacity Building – Regular workshops on nutrition counseling and supplement administration.
✅ Stronger Community Engagement – Work with self-help groups (SHGs) and Panchayati Raj Institutions (PRIs).
✅ Digital Tracking & Monitoring – Use Poshan Tracker App, Anemia Mukt Bharat App for better implementation.
✅ Strengthening Public-Private Partnerships – Collaborate with NGOs and private healthcare organizations.