BSC SEM 1 UNIT 1 NURSING FOUNDATION 1
UNIT 1 Introduction to health and illness
Introduction to Health and Illness

Introduction
Health and illness are fundamental concepts in nursing and healthcare. Understanding these concepts is essential for providing quality patient care, promoting wellness, and preventing diseases. Nurses play a vital role in assessing health status, identifying risk factors, and implementing interventions to improve patient outcomes.
Definition of Health
Health is a dynamic state of well-being in which an individual can function optimally within their physical, mental, social, and spiritual environments. It is not merely the absence of disease but a state of complete well-being.
World Health Organization (WHO) Definition (1948)
“Health is a state of complete physical, mental, and social well-being and not merely the absence of disease or infirmity.”
Florence Nightingale’s Perspective on Health
Florence Nightingale, the founder of modern nursing, emphasized that health is the ability to utilize energy efficiently in daily activities. She believed that good hygiene, sanitation, fresh air, proper nutrition, and nursing care promote health and prevent illness.
Types of Health
- Physical Health: Proper functioning of body systems without diseases or disabilities.
- Mental Health: Emotional and psychological well-being; the ability to cope with stress.
- Social Health: Maintaining healthy relationships and interactions with society.
- Spiritual Health: Finding meaning and purpose in life; alignment with personal beliefs and values.
- Emotional Health: Ability to express emotions appropriately and handle life challenges.
Concept of Illness
Illness is a state in which an individual’s normal functioning is disrupted due to disease, injury, or emotional distress. It can be acute or chronic and may impact various aspects of life.
Types of Illness
- Acute Illness: Sudden onset, short duration (e.g., flu, pneumonia).
- Chronic Illness: Long-term, progressive conditions requiring ongoing care (e.g., diabetes, hypertension).
- Communicable Diseases: Infections spread from person to person (e.g., tuberculosis, COVID-19).
- Non-Communicable Diseases (NCDs): Non-infectious diseases caused by lifestyle, genetics, or environment (e.g., heart disease, cancer).
- Mental Illness: Disorders affecting mood, thinking, and behavior (e.g., depression, schizophrenia).
Stages of Illness
- Stage of Symptom Experience: The person notices signs and symptoms of illness.
- Stage of Assumption of Sick Role: The individual seeks validation and assumes the role of being sick.
- Stage of Medical Care Contact: The person consults healthcare professionals.
- Stage of Dependent Patient Role: The patient follows prescribed treatments and depends on caregivers.
- Stage of Recovery or Rehabilitation: The individual regains health or adapts to chronic illness.
Determinants of Health and Illness
Health and illness are influenced by multiple factors, including:
- Biological Factors: Genetics, hereditary diseases.
- Environmental Factors: Pollution, climate, living conditions.
- Lifestyle Factors: Diet, exercise, smoking, alcohol use.
- Socioeconomic Factors: Income, education, occupation, healthcare access.
- Psychological Factors: Stress, mental health, coping skills.
- Cultural and Religious Factors: Beliefs, practices, and healthcare preferences.
Health–Illness Continuum
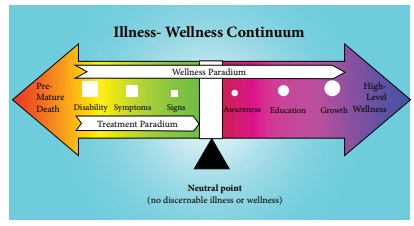
The Health–Illness Continuum explains that health and illness exist on a spectrum, ranging from optimal wellness to severe illness. It helps nurses assess where patients fall on this scale.
Key Points:
- Health is dynamic and changes over time.
- A person may not be completely ill or completely healthy.
- Wellness involves active personal responsibility for health.
Nursing Role in Health Promotion and Illness Prevention

Nurses play a key role in maintaining health, preventing diseases, and managing illness. Their responsibilities include:
1. Health Promotion
Encouraging individuals to adopt a healthy lifestyle through:
- Proper nutrition and exercise.
- Health education and awareness programs.
- Mental well-being and stress management.
2. Disease Prevention
- Primary Prevention: Preventing disease before it occurs (e.g., vaccination, healthy diet, sanitation).
- Secondary Prevention: Early detection and treatment (e.g., screenings, diagnostic tests).
- Tertiary Prevention: Reducing complications and disability (e.g., rehabilitation, chronic disease management).
3. Nursing Process in Health and Illness
Nurses apply the Nursing Process to assess, diagnose, plan, implement, and evaluate patient care.
- Assessment: Collecting health history and physical examination.
- Diagnosis: Identifying health problems based on assessment data.
- Planning: Setting goals for improving health or managing illness.
- Implementation: Carrying out interventions (medications, health teaching, supportive care).
- Evaluation: Checking if the patient’s condition has improved.
Health Education and Patient Empowerment
Health education is an essential nursing function to promote health literacy. Nurses educate patients on:
- Disease prevention and self-care.
- Medication adherence.
- Lifestyle modifications (e.g., quitting smoking, exercising).
Patient empowerment involves encouraging individuals to take control of their health through informed decision-making and self-care strategies.
Importance of Holistic Nursing Care
Holistic nursing considers the physical, emotional, social, and spiritual needs of patients rather than just treating disease symptoms. It involves:
- Therapeutic Communication: Building trust and understanding patient concerns.
- Psychosocial Support: Addressing emotional needs and coping mechanisms.
- Spiritual Care: Respecting cultural and religious beliefs in healthcare.
- Palliative and End-of-Life Care: Providing comfort to terminally ill patients.
Concept of Health

Introduction
Health is a fundamental aspect of life and an essential goal for individuals and societies. It is a dynamic state that includes physical, mental, social, and spiritual well-being. The concept of health has evolved over time, influenced by scientific advancements, cultural beliefs, and public health initiatives. Understanding health is crucial for nurses as they play a pivotal role in health promotion, disease prevention, and patient care.
Definitions of Health
Health has been defined by various scholars and organizations, emphasizing different aspects.
World Health Organization (WHO) Definition (1948)
“Health is a state of complete physical, mental, and social well-being and not merely the absence of disease or infirmity.”
- This definition highlights that health is more than just the absence of disease; it includes overall well-being.
Florence Nightingale’s Concept of Health
- Florence Nightingale, the founder of modern nursing, believed that health is the ability to use energy effectively in daily activities.
- She emphasized environmental factors such as clean air, proper sanitation, hygiene, and nutrition in maintaining health.
Other Definitions
- Dubos (1965): Health is a state of adaptation to one’s environment.
- Ecological Definition: Health is a dynamic balance between humans and their environment.
- Holistic Definition: Health includes physical, emotional, social, and spiritual well-being.
Dimensions of Health
Health is a multidimensional concept, encompassing various aspects:
1. Physical Health
- Proper functioning of body systems.
- Indicators: Normal body temperature, pulse, blood pressure, and absence of disease.
- Influenced by: Nutrition, exercise, rest, and hygiene.
2. Mental Health
- Cognitive and emotional well-being.
- Ability to handle stress, make decisions, and interact positively.
- Influenced by: Emotional stability, self-esteem, and resilience.
3. Social Health
- Ability to form and maintain relationships.
- Involves effective communication and social support.
- Influenced by: Family, friendships, work environment, and cultural norms.
4. Spiritual Health
- Sense of purpose and meaning in life.
- May involve religious beliefs, personal values, and moral principles.
- Influenced by: Faith, meditation, self-reflection, and ethical conduct.
5. Emotional Health
- Ability to express and manage emotions appropriately.
- Involves coping with stress and maintaining psychological balance.
- Influenced by: Emotional intelligence, stress management skills, and support systems.
6. Environmental Health
- The impact of surroundings on health.
- Includes clean air, safe drinking water, proper sanitation, and a healthy work environment.
- Influenced by: Pollution control, waste management, and occupational safety.
7. Occupational Health
- A healthy work-life balance.
- Involves safe working conditions and job satisfaction.
- Influenced by: Ergonomics, workplace policies, and occupational safety.
8. Intellectual Health
- Lifelong learning and problem-solving abilities.
- Encourages creativity, curiosity, and personal growth.
- Influenced by: Education, reading, and critical thinking.
Factors Influencing Health
Health is influenced by biological, environmental, social, and lifestyle factors:
1. Biological Factors
- Genetics: Inherited traits and predisposition to diseases.
- Age and Gender: Different health risks at different life stages.
- Immunity: Ability to fight infections and diseases.
2. Environmental Factors
- Physical Environment: Pollution, climate, housing, and water quality.
- Workplace Conditions: Safety, ergonomics, and stress levels.
- Sanitation and Hygiene: Proper waste disposal and clean surroundings.
3. Lifestyle and Behavioral Factors
- Nutrition: Balanced diet and hydration.
- Physical Activity: Regular exercise and fitness.
- Substance Abuse: Avoidance of smoking, alcohol, and drug abuse.
- Stress Management: Meditation, relaxation, and mental health care.
4. Socioeconomic Factors
- Income Level: Access to healthcare, education, and nutritious food.
- Education: Awareness about health and disease prevention.
- Employment: Job security and occupational health.
5. Cultural and Religious Factors
- Beliefs and Practices: Influence health behaviors and medical decisions.
- Dietary Restrictions: Religious food habits affecting nutrition.
- Health-Seeking Behavior: Use of alternative medicine, herbal remedies.
6. Psychological Factors
- Emotional Stability: Coping mechanisms and stress tolerance.
- Support System: Family, friends, and professional counseling.
- Mental Health Disorders: Depression, anxiety, and personality disorders.
Health–Illness Continuum
The Health–Illness Continuum (by John Travis, 1972) describes health as a spectrum ranging from optimal wellness to severe illness.
- High-Level Wellness: A proactive approach to maintaining health.
- Neutral Zone: No active disease, but not fully engaged in wellness.
- Illness and Disability: Presence of disease or disability.
This model helps nurses assess a patient’s health status and guide interventions.
Concepts Related to Health
1. Health Promotion
- Process of enabling individuals to increase control over their health.
- Strategies:
- Health education
- Immunization programs
- Lifestyle modifications
2. Disease Prevention
- Primary Prevention: Preventing disease before it occurs (e.g., vaccinations, hygiene).
- Secondary Prevention: Early detection and treatment (e.g., screenings, diagnostic tests).
- Tertiary Prevention: Reducing complications (e.g., rehabilitation, chronic disease management).
3. Holistic Health Care
- Focuses on treating the person as a whole, not just the disease.
- Integrates physical, emotional, social, and spiritual aspects.
- Includes alternative therapies (e.g., yoga, meditation, acupuncture).
4. Determinants of Health
- Social Determinants: Education, income, housing, healthcare access.
- Biological Determinants: Genetics, gender, age.
- Environmental Determinants: Pollution, climate, occupational hazards.
Role of Nurses in Health Promotion
Nurses play a crucial role in maintaining and improving health at various levels:
1. Health Education
- Teaching patients about healthy lifestyles.
- Promoting self-care and disease prevention.
2. Preventive Care
- Conducting health screenings and vaccinations.
- Identifying early signs of diseases.
3. Patient Advocacy
- Ensuring patients receive the best possible care.
- Supporting patient rights and autonomy.
4. Community Health Nursing
- Providing healthcare services at the community level.
- Promoting sanitation, immunization, and maternal-child health.
5. Holistic Nursing Care
- Addressing emotional, social, and spiritual needs.
- Providing comfort and support to patients.
Conclusion
The concept of health is broad, multidimensional, and dynamic. It includes physical, mental, social, and spiritual well-being. Several factors influence health, including genetics, environment, lifestyle, and socioeconomic conditions. Nurses play a vital role in promoting health through education, prevention, and patient-centered care.
Key Takeaways
- Health is more than the absence of disease; it is a state of overall well-being.
- It includes physical, mental, social, spiritual, emotional, and environmental dimensions.
- Health determinants include biological, environmental, lifestyle, and socioeconomic factors.
- The Health-Illness Continuum explains that health is a spectrum, not a fixed state.
- Nurses play a significant role in health promotion, disease prevention, and holistic care.
Dimensions of Health

Introduction
Health is a multidimensional concept that encompasses various aspects of human life. It is not merely the absence of disease but a state of complete well-being in different areas. Understanding the dimensions of health is essential in nursing practice as it helps in providing holistic patient care.
The World Health Organization (WHO) defines health as: “A state of complete physical, mental, and social well-being and not merely the absence of disease or infirmity.”
Health is influenced by multiple factors, and nurses must address all dimensions to ensure comprehensive patient care.
1. Physical Health
Definition:
Physical health refers to the proper functioning of the body and its systems. It is the ability to perform daily activities without physical limitations.
Indicators of Physical Health:
- Normal body temperature, heart rate, and blood pressure.
- Good muscle strength and endurance.
- Proper nutrition and hydration.
- Absence of diseases or infections.
- Ability to perform daily activities without excessive fatigue.
Factors Influencing Physical Health:
- Genetics: Hereditary conditions and predisposition to diseases.
- Nutrition: Balanced diet, vitamins, and minerals.
- Exercise: Regular physical activity for strength and endurance.
- Sleep: Adequate rest for bodily functions.
- Hygiene: Cleanliness and infection control.
- Medical Care: Regular check-ups, vaccinations, and screenings.
Nursing Role:
- Educate patients on proper diet, exercise, and hygiene.
- Monitor vital signs and assess physical health.
- Promote preventive care like immunization and early disease detection.
2. Mental Health
Definition:
Mental health refers to an individual’s emotional and psychological well-being. It includes the ability to cope with stress, solve problems, and maintain relationships.
Indicators of Mental Health:
- Positive self-esteem and self-confidence.
- Ability to handle stress effectively.
- Rational thinking and good decision-making skills.
- Ability to form and maintain relationships.
- Absence of severe mental illnesses like depression or anxiety disorders.
Factors Influencing Mental Health:
- Genetic predisposition: Some mental illnesses are hereditary.
- Stress levels: Work, family, and financial stress.
- Social support: Family, friends, and community relationships.
- Lifestyle habits: Sleep, diet, and recreational activities.
- Trauma: Childhood abuse, accidents, or emotional distress.
Nursing Role:
- Provide emotional support and counseling.
- Identify early signs of mental health disorders.
- Educate on stress management techniques.
- Refer to mental health professionals when needed.
3. Social Health
Definition:
Social health refers to an individual’s ability to form and maintain meaningful relationships with others. It involves communication, social interaction, and adapting to social norms.
Indicators of Social Health:
- Good interpersonal relationships with family, friends, and colleagues.
- Effective communication skills.
- Ability to adapt to different social situations.
- Sense of belonging and community involvement.
Factors Influencing Social Health:
- Family relationships: Supportive family environment.
- Friendships and peer groups: Positive social interactions.
- Work-life balance: Healthy workplace relationships.
- Cultural and religious beliefs: Influence social connections.
- Community involvement: Participation in social events and activities.
Nursing Role:
- Encourage patients to engage in social activities.
- Assess social support systems and refer for counseling if needed.
- Help patients with social reintegration after illness or disability.
4. Emotional Health
Definition:
Emotional health refers to an individual’s ability to manage and express emotions in a healthy way.
Indicators of Emotional Health:
- Self-awareness and emotional stability.
- Ability to express feelings appropriately.
- Coping with stress, sadness, and anxiety.
- Maintaining a positive outlook on life.
Factors Influencing Emotional Health:
- Childhood experiences: Early life emotional support.
- Stress management skills: Techniques like meditation and therapy.
- Support systems: Friends, family, and mentors.
- Personal resilience: Ability to bounce back from adversity.
Nursing Role:
- Encourage patients to express their emotions.
- Provide psychological support and counseling.
- Teach stress-relief techniques such as relaxation exercises.
5. Spiritual Health
Definition:
Spiritual health is a sense of purpose and meaning in life. It includes religious beliefs, personal values, and moral principles.
Indicators of Spiritual Health:
- Having a sense of purpose in life.
- Feeling connected to a higher power or inner self.
- Inner peace and contentment.
- Ethical and moral behavior.
Factors Influencing Spiritual Health:
- Religious beliefs: Practicing faith and religious rituals.
- Personal values: Integrity and moral decision-making.
- Meditation and mindfulness: Spiritual reflection and self-awareness.
- Sense of purpose: Feeling fulfilled and satisfied with life.
Nursing Role:
- Respect patients’ religious beliefs and cultural practices.
- Provide emotional and spiritual support in times of illness.
- Refer to chaplains or spiritual counselors when needed.
6. Environmental Health
Definition:
Environmental health refers to the impact of surroundings on a person’s well-being. A clean and safe environment promotes good health.
Indicators of Environmental Health:
- Access to clean air, water, and sanitation.
- Safe working and living conditions.
- Minimal exposure to pollution and toxins.
- Healthy food availability.
Factors Influencing Environmental Health:
- Pollution levels: Air, water, and noise pollution.
- Sanitation: Proper waste disposal and clean surroundings.
- Climate change: Extreme weather conditions affecting health.
- Workplace safety: Ergonomics and occupational hazards.
Nursing Role:
- Promote environmental hygiene and sanitation.
- Educate communities on pollution control and waste management.
- Advocate for safe working conditions.
7. Occupational Health
Definition:
Occupational health refers to a person’s ability to perform job-related tasks safely and efficiently.
Indicators of Occupational Health:
- Job satisfaction and work-life balance.
- Safe and comfortable working conditions.
- Mental and emotional well-being at work.
- Prevention of workplace injuries.
Factors Influencing Occupational Health:
- Work stress: Job pressures and workload.
- Ergonomics: Proper posture and work habits.
- Safety measures: Workplace policies and protective equipment.
- Job satisfaction: A fulfilling work environment.
Nursing Role:
- Educate employees on occupational hazards.
- Advocate for workplace safety policies.
- Conduct health screenings for workers.
8. Intellectual Health
Definition:
Intellectual health refers to cognitive abilities, learning, and creativity. It is about keeping the brain active and engaged.
Indicators of Intellectual Health:
- Curiosity and a love for learning.
- Good problem-solving and decision-making skills.
- Open-mindedness to new ideas.
- Engaging in mentally stimulating activities.
Factors Influencing Intellectual Health:
- Education level: Access to learning opportunities.
- Lifelong learning: Continuous skill development.
- Reading and creativity: Intellectual stimulation.
- Critical thinking: Ability to analyze and solve problems.
Nursing Role:
- Encourage patients to engage in lifelong learning.
- Promote mental exercises and problem-solving activities.
- Educate on brain health and cognitive stimulation.
Conclusion
The dimensions of health provide a holistic approach to understanding well-being. Nurses must consider physical, mental, social, emotional, spiritual, environmental, occupational, and intellectual health to provide comprehensive care.
Key Takeaways:
- Health is multidimensional, not just the absence of disease.
- Physical health is about bodily functions and fitness.
- Mental and emotional health involve stress management and coping skills.
- Social and spiritual health focus on relationships and personal beliefs.
- Environmental and occupational health ensure a safe and healthy living/workplace.
- Intellectual health emphasizes lifelong learning and cognitive stimulation.
By addressing all these dimensions, nurses can promote overall well-being and contribute to a healthier society.
Maslow’s Hierarchy of Needs:
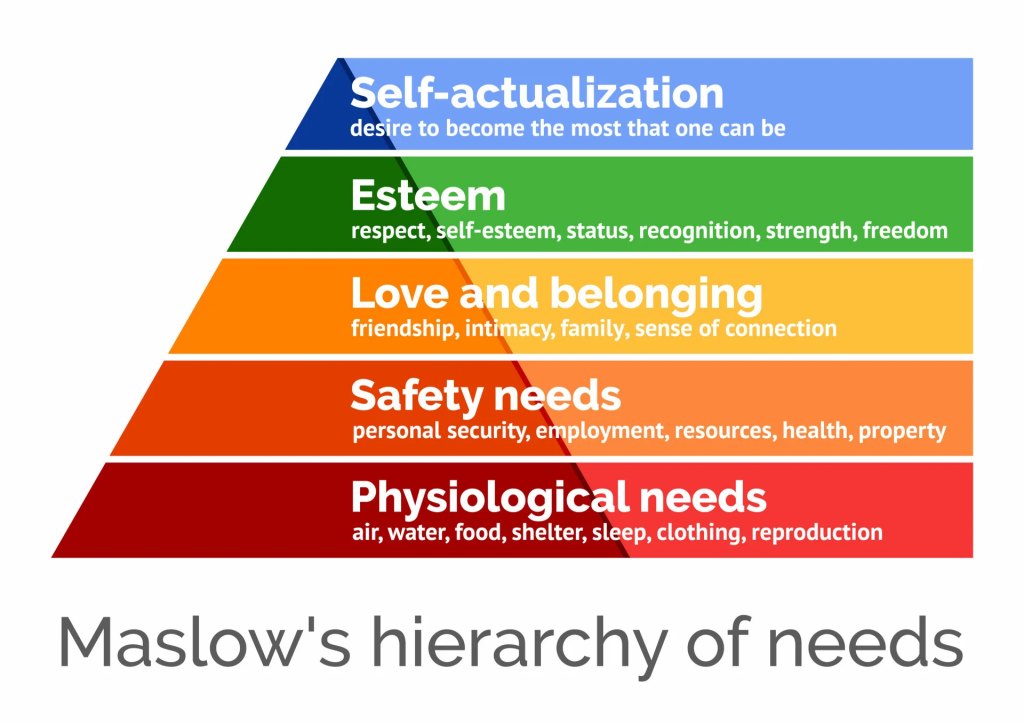
Introduction
Maslow’s Hierarchy of Needs is a psychological theory proposed by Abraham Maslow in 1943 that explains human motivation based on a hierarchy of needs. It is widely used in nursing and healthcare to understand patient care priorities and ensure holistic well-being. Nurses apply Maslow’s theory to prioritize interventions, ensuring that basic physiological and safety needs are met before addressing higher-level psychological and self-fulfillment needs.
Maslow’s Hierarchy of Needs: The Five Levels
Maslow’s hierarchy is structured as a pyramid with five levels, each representing a category of human needs. Lower-level needs must be satisfied before individuals can focus on higher levels.
1. Physiological Needs (Basic Needs)
These are the most fundamental biological needs required for survival.
Examples of Physiological Needs:
- Air (Oxygen): Essential for respiration.
- Water and Hydration: Adequate fluid intake.
- Food and Nutrition: Proper diet for energy and health.
- Sleep and Rest: Recovery and healing.
- Elimination (Excretion): Bowel and urinary function.
- Temperature Regulation: Maintaining body temperature.
- Sexual Activity and Reproduction: Biological drive for species survival.
Application in Nursing:
- Ensuring adequate oxygenation (e.g., administering oxygen therapy).
- Providing nutritional support (e.g., IV fluids, feeding assistance).
- Assisting with elimination needs (e.g., catheter care, bowel management).
- Ensuring proper hygiene and skin care.
- Addressing sleep disturbances and promoting rest.
2. Safety and Security Needs
Once physiological needs are met, individuals seek safety and protection from harm.
Types of Safety Needs:
- Physical Safety: Protection from accidents, falls, and infections.
- Health Security: Access to medical care and treatment.
- Financial Security: Stable income and job security.
- Environmental Safety: Clean and safe living conditions.
- Emotional Security: Freedom from fear and anxiety.
Application in Nursing:
- Preventing fall risks in elderly patients.
- Administering medications safely to prevent errors.
- Ensuring infection control measures (e.g., hand hygiene, PPE).
- Providing patient education on safety precautions.
- Supporting patients facing financial and health insecurities.
3. Love and Belonging Needs (Social Needs)
This level focuses on interpersonal relationships and emotional support.
Examples of Social Needs:
- Family Bonds: Emotional connections with loved ones.
- Friendship and Peer Support: Social interaction and companionship.
- Community and Group Belonging: Cultural and religious connections.
- Love and Affection: Feeling valued and cared for.
Application in Nursing:
- Encouraging family involvement in patient care.
- Providing emotional support through active listening and empathy.
- Addressing social isolation in elderly and chronically ill patients.
- Encouraging peer support groups for patients with chronic diseases.
- Respecting cultural and religious practices.
4. Esteem Needs (Self-Respect and Recognition)
This level focuses on self-worth, confidence, and recognition.
Types of Esteem Needs:
- Self-Esteem: Feeling capable and confident.
- Respect from Others: Recognition, appreciation, and achievements.
- Competence and Independence: Ability to perform tasks independently.
- Status and Prestige: Acknowledgment of one’s role and contributions.
Application in Nursing:
- Encouraging patient autonomy in self-care activities.
- Recognizing patient achievements (e.g., progress in recovery).
- Providing positive reinforcement and motivation.
- Assisting with body image concerns (e.g., post-surgical patients).
- Promoting rehabilitation and independence in disabled individuals.
5. Self-Actualization (Personal Growth and Fulfillment)
The highest level in the hierarchy, where individuals strive to reach their full potential and personal goals.
Characteristics of Self-Actualized Individuals:
- Problem-solving skills
- Creativity and innovation
- Personal growth and fulfillment
- Sense of purpose and meaning in life
- Helping others and giving back to society
Application in Nursing:
- Encouraging patient education and skill development.
- Supporting patients’ personal goals (e.g., returning to work).
- Promoting spiritual well-being.
- Helping patients cope with chronic illness positively.
- Encouraging volunteering and social contribution.
Expanded Model: Maslow’s Eight-Stage Hierarchy
Later, Maslow expanded his theory to include three additional levels:
6. Cognitive Needs (Desire for Knowledge and Understanding)
- Curiosity, learning, exploring new ideas.
- Nurses encourage patient education and health literacy.
7. Aesthetic Needs (Appreciation of Beauty and Balance)
- Desire for harmony, beauty, and creativity.
- Nurses create a healing environment (e.g., soothing music, artwork, nature).
8. Transcendence Needs (Helping Others Reach Their Potential)
- Going beyond self-actualization to help others.
- Nurses support palliative care, mentoring, and humanitarian work.
Maslow’s Hierarchy in Nursing Prioritization
Nurses use Maslow’s theory to prioritize patient care, ensuring critical needs are met first.
Example of Nursing Prioritization Using Maslow’s Hierarchy:
| Patient Condition | Priority Level | Maslow’s Level |
|---|---|---|
| Unconscious patient with low oxygen levels | Highest Priority | Physiological Needs |
| Patient at risk of falls | High Priority | Safety Needs |
| Patient feeling lonely in hospital | Moderate Priority | Love and Belonging |
| Patient anxious about body image after surgery | Lower Priority | Esteem Needs |
| Patient planning to volunteer after recovery | Lowest Priority | Self-Actualization |
Key Concept: Nurses always prioritize life-threatening issues first (e.g., airway, breathing, circulation) before addressing psychological and social concerns.
Advantages of Using Maslow’s Theory in Nursing
- Helps prioritize nursing interventions effectively.
- Ensures holistic care by addressing all aspects of well-being.
- Guides patient-centered care based on individual needs.
- Enhances nurse-patient communication by understanding patients’ motivations.
Criticism of Maslow’s Hierarchy
- Needs may not always follow a strict hierarchy (e.g., a starving artist may prioritize self-actualization over food).
- Cultural differences influence how needs are perceived.
- Some individuals may achieve higher-level needs while still struggling with basic needs.
Despite these criticisms, Maslow’s theory remains a valuable tool for understanding human motivation and improving nursing care.
Key Takeaways:
✔ Basic needs must be met first before higher needs can be addressed.
✔ Nurses use Maslow’s theory to prioritize patient care.
✔ Holistic nursing considers all dimensions of health.
✔ Self-actualization is the highest level but may vary among individuals.
Maslow’s hierarchy remains a powerful tool for understanding patient behavior, improving nursing interventions, and promoting health and wellness in all healthcare settings.
Health-Illness Continuum
Introduction
The Health-Illness Continuum is a model that describes health as a dynamic and ever-changing process rather than a fixed state. It was introduced by John Travis in 1972, who emphasized that health and illness exist on a spectrum, ranging from optimal wellness to severe illness.
This model helps nurses assess patients’ health status and determine appropriate interventions to promote well-being and prevent disease.
Definition of Health-Illness Continuum
The Health-Illness Continuum represents a graduated scale with health and wellness on one end and illness and death on the other. It suggests that:
- Health is not merely the absence of disease but a process of continuous adaptation.
- Individuals move back and forth along the continuum depending on various factors, such as lifestyle, environment, genetics, and healthcare access.
Key Concept:
💡 Health is dynamic, not static! A person’s health status changes over time due to various internal and external factors.
Components of the Health-Illness Continuum
The continuum has two major ends:
- High-Level Wellness (Optimal Health)
- A state of physical, mental, and social well-being.
- Involves positive lifestyle choices (e.g., healthy diet, regular exercise, stress management).
- Individuals take proactive steps to maintain and improve health.
- Illness and Premature Death
- A state of declining health due to disease, disability, or unhealthy lifestyle.
- If left untreated, it may lead to death.
- Includes chronic diseases, infections, or mental health disorders.
Between these two extremes, individuals constantly move depending on risk factors, lifestyle choices, and medical care.
Stages of the Health-Illness Continuum
The continuum consists of six stages:
1. Wellness/Optimal Health
- Individuals experience full physical, mental, and social well-being.
- They actively practice healthy behaviors (e.g., balanced diet, regular exercise, mental wellness).
- Preventive measures are in place to reduce disease risks.
2. Good Health
- The person has minor health issues but functions well.
- Lifestyle choices contribute to overall wellness.
- Occasional illnesses (e.g., colds, minor injuries) may occur but do not significantly impact health.
3. Normal Health
- Individuals feel fine but may have some unhealthy habits (e.g., poor diet, stress).
- Risk factors begin to accumulate (e.g., sedentary lifestyle, high blood pressure).
- No significant illness but potential for future health problems.
4. Poor Health
- Signs and symptoms of health issues appear.
- Chronic conditions may develop (e.g., diabetes, hypertension).
- Individuals seek medical help but do not always make lifestyle changes.
5. Illness
- Severe health deterioration occurs.
- The individual requires medical intervention and treatment.
- Conditions like cancer, heart disease, or severe infections significantly impact life.
6. Disability/Premature Death
- The final stage where the individual loses function due to illness.
- If treatment is ineffective, it may lead to permanent disability or death.
💡 Key Point: People move back and forth on this continuum depending on their lifestyle, healthcare, and environmental influences.
Factors Influencing Movement Along the Continuum
Several factors determine where an individual is positioned on the health-illness continuum:
1. Lifestyle Choices
✅ Healthy habits (exercise, balanced diet, stress management) → Move toward wellness
❌ Unhealthy habits (smoking, alcohol, poor diet, inactivity) → Move toward illness
2. Environment
✅ Clean air, safe water, good sanitation → Promotes better health
❌ Pollution, hazardous workplaces, poor hygiene → Increases disease risk
3. Genetics
✅ Good genetic health, family history of longevity → Leads to better health
❌ Genetic predisposition to diseases (diabetes, cancer, heart disease) → Increases illness risk
4. Healthcare Access
✅ Regular check-ups, vaccinations, screenings → Helps detect and prevent diseases early
❌ Lack of healthcare access → Leads to delayed treatment and worsening health conditions
5. Psychological and Social Factors
✅ Strong support system, emotional well-being, mental stability → Improves overall wellness
❌ Chronic stress, depression, social isolation → Contributes to poor health and illness
Application of the Health-Illness Continuum in Nursing
Nurses use the health-illness continuum to assess a patient’s health status and risk factors. This model helps guide care planning, health education, and preventive interventions.
1. Health Promotion and Disease Prevention
- Nurses educate patients about healthy lifestyle choices.
- Encourage vaccination, screening tests, and early disease detection.
- Promote stress management, physical activity, and healthy eating.
2. Patient Assessment and Care Planning
- Assess where the patient falls on the continuum.
- Identify risk factors and suggest appropriate interventions.
- Provide individualized care plans to improve health status.
3. Chronic Disease Management
- Help patients manage conditions like diabetes, hypertension, and asthma.
- Encourage adherence to medications, lifestyle modifications, and regular check-ups.
4. Rehabilitation and Palliative Care
- Support patients in recovering from illness or adjusting to chronic conditions.
- Provide pain management and emotional support in end-of-life care.
Comparison of the Health-Illness Continuum with Other Models
| Model | Focus | Key Concept |
|---|---|---|
| Health-Illness Continuum | Health as a fluid and changing state | Health is dynamic, moving between wellness and illness. |
| Biomedical Model | Focuses on disease diagnosis and treatment | Treats illness without considering psychological or social factors. |
| Holistic Model | Focuses on physical, mental, social, and spiritual health | Health is influenced by multiple dimensions (not just absence of disease). |
💡 Nursing Uses:
- Health-Illness Continuum → Assessing patients’ overall well-being
- Biomedical Model → Medical treatment and disease management
- Holistic Model → Comprehensive patient-centered care
Advantages of the Health-Illness Continuum
✔ Encourages a proactive approach to health rather than just disease treatment.
✔ Helps nurses prioritize care based on the patient’s health status.
✔ Recognizes that health is dynamic and influenced by multiple factors.
✔ Emphasizes disease prevention and early intervention.
Key Takeaways:
✔ Health and illness exist on a continuum, not as fixed states.
✔ People move back and forth along the continuum based on various factors.
✔ Nurses use this model for health promotion, prevention, and care planning.
✔ A proactive approach to health leads to better patient outcomes.
By applying the Health-Illness Continuum, nurses can empower patients to take charge of their health and work towards achieving optimal well-being.
Factors Influencing Health

Introduction
Health is a dynamic state influenced by multiple factors, including biological, environmental, social, and behavioral aspects. Understanding these factors helps nurses and healthcare providers develop effective health promotion strategies, disease prevention programs, and personalized care plans.
The World Health Organization (WHO) defines health as:
“A state of complete physical, mental, and social well-being and not merely the absence of disease or infirmity.”
Health is not only determined by genetics or medical care but also by lifestyle choices, socioeconomic conditions, and environmental factors.
Major Factors Influencing Health
The factors affecting health can be categorized into the following broad groups:
- Biological Factors (Genetics, Age, Gender)
- Behavioral and Lifestyle Factors (Diet, Exercise, Smoking, Alcohol)
- Environmental Factors (Air Quality, Water Sanitation, Housing)
- Socioeconomic Factors (Income, Education, Occupation)
- Psychosocial and Cultural Factors (Stress, Relationships, Religion)
- Health Services and Healthcare Access (Medical Care, Insurance)
- Political and Government Policies (Healthcare Laws, Public Health Initiatives)
1. Biological Factors
Definition:
Biological factors refer to inherited and physiological characteristics that affect an individual’s health.
Key Biological Factors:
| Factor | Influence on Health |
|---|---|
| Genetics | Inherited diseases (e.g., diabetes, hypertension, cancer). |
| Age | Infants, elderly, and adolescents have different health risks. |
| Gender | Women are more prone to osteoporosis; men have a higher risk of heart disease. |
| Immunity | Strong immunity prevents infections; weak immunity increases disease susceptibility. |
Nursing Role:
- Identify genetic risks and provide early screening.
- Educate patients about age-specific health concerns.
- Promote vaccination and immune-boosting measures.
2. Behavioral and Lifestyle Factors
Definition:
Lifestyle and behaviors play a significant role in determining health outcomes. Healthy habits promote wellness, while harmful behaviors increase disease risk.
Key Lifestyle Factors:
| Factor | Healthy Impact | Unhealthy Impact |
|---|---|---|
| Diet and Nutrition | Balanced diet prevents malnutrition, obesity, and heart diseases. | Poor diet leads to obesity, diabetes, and heart disease. |
| Physical Activity | Regular exercise improves heart health, mental well-being. | Sedentary lifestyle increases obesity and diabetes risk. |
| Substance Abuse (Smoking, Alcohol, Drugs) | Avoidance of smoking and alcohol prevents lung and liver diseases. | Smoking causes lung cancer; alcohol damages the liver. |
| Sleep and Rest | 7-9 hours of sleep supports mental and physical health. | Sleep deprivation weakens immunity and increases stress. |
| Stress Management | Relaxation techniques improve mental health. | Chronic stress leads to anxiety, depression, and heart disease. |
Nursing Role:
- Educate patients about healthy eating habits.
- Promote exercise and active living.
- Conduct awareness programs on substance abuse prevention.
3. Environmental Factors
Definition:
The environment consists of physical, chemical, and biological elements that influence health.
Key Environmental Factors:
| Factor | Effect on Health |
|---|---|
| Air Quality | Pollution leads to asthma, lung disease. |
| Water and Sanitation | Poor sanitation causes waterborne diseases (cholera, diarrhea). |
| Housing Conditions | Poor ventilation leads to respiratory infections. |
| Climate and Weather | Extreme heat or cold affects vulnerable populations. |
Nursing Role:
- Promote environmental hygiene and sanitation.
- Educate on safe drinking water and food hygiene.
- Advocate for policies to reduce pollution.
4. Socioeconomic Factors
Definition:
An individual’s financial and social status affects their ability to access healthcare, nutrition, and a safe living environment.
Key Socioeconomic Factors:
| Factor | Influence on Health |
|---|---|
| Income and Poverty | Low income leads to poor nutrition and limited healthcare access. |
| Education | Higher education promotes health awareness and better health choices. |
| Occupation and Work Conditions | Unsafe jobs (e.g., mining, construction) increase injury risks. |
| Healthcare Access | Affordable healthcare ensures better disease prevention and treatment. |
Nursing Role:
- Provide health education programs.
- Advocate for affordable healthcare services.
- Help patients connect with community resources for financial assistance.
5. Psychosocial and Cultural Factors
Definition:
Mental well-being, social relationships, and cultural beliefs impact an individual’s health and healthcare choices.
Key Psychosocial Factors:
| Factor | Influence on Health |
|---|---|
| Stress and Mental Health | Chronic stress leads to hypertension, heart disease, and depression. |
| Social Support and Relationships | Strong family and friendships improve mental well-being. |
| Cultural and Religious Beliefs | Some cultures avoid modern medicine; others prioritize alternative healing methods. |
Nursing Role:
- Provide mental health counseling and stress management support.
- Encourage social engagement and support groups.
- Respect cultural beliefs in patient care plans.
6. Health Services and Healthcare Access
Definition:
The availability and quality of healthcare services play a significant role in maintaining health.
Key Healthcare Factors:
| Factor | Influence on Health |
|---|---|
| Availability of Hospitals and Clinics | Rural areas may have limited access to healthcare. |
| Quality of Care | Poor healthcare services increase disease risks. |
| Health Insurance Coverage | Lack of insurance leads to delayed treatment. |
| Vaccination Programs | Prevents infectious diseases. |
Nursing Role:
- Educate patients about preventive healthcare and screenings.
- Assist patients in navigating healthcare systems.
- Advocate for universal healthcare access.
7. Political and Government Policies
Definition:
Government policies impact public health through regulations, healthcare funding, and disease control measures.
Key Political Factors:
| Factor | Influence on Health |
|---|---|
| Public Health Policies | Regulations on pollution, food safety improve health. |
| Government Healthcare Programs | Free vaccinations and maternal health programs reduce mortality. |
| Emergency Preparedness | Disaster management policies ensure quick response to outbreaks. |
Nursing Role:
- Support public health initiatives.
- Advocate for policy changes to improve healthcare access.
- Participate in disaster response and emergency care training.
Summary: Key Factors Influencing Health
| Category | Examples |
|---|---|
| Biological Factors | Genetics, age, immunity, gender |
| Lifestyle Factors | Diet, exercise, smoking, alcohol, stress |
| Environmental Factors | Pollution, water quality, housing |
| Socioeconomic Factors | Income, education, employment, poverty |
| Psychosocial Factors | Social support, mental health, cultural beliefs |
| Healthcare Factors | Medical access, insurance, vaccination |
| Political Factors | Public health policies, government programs |
Key Takeaways:
✔ Health is not just about disease absence but overall well-being.
✔ Multiple factors affect health, including genetics, lifestyle, environment, and social conditions.
✔ Nurses play a key role in promoting health through education, prevention, and care.
✔ Health policies and government programs significantly impact population health.
By understanding these factors influencing health, nurses can help improve patient outcomes and promote a healthier society.
Causes and Risk Factors for Developing Illnesses:
Introduction
Illnesses do not develop randomly; they are caused by a variety of factors, including biological, environmental, genetic, behavioral, and social determinants. Identifying these causes and risk factors is essential for prevention, early diagnosis, and effective management.
Nurses play a critical role in educating patients about risk factors and encouraging preventive measures to reduce the likelihood of developing diseases.
1. Causes of Illnesses
Illnesses can be caused by several factors, either individually or in combination. The primary causes include:
1.1 Biological Causes
- Infections: Caused by bacteria, viruses, fungi, or parasites.
- Example: Tuberculosis (Mycobacterium tuberculosis), COVID-19 (Coronavirus)
- Genetic Disorders: Inherited conditions due to gene mutations.
- Example: Sickle Cell Anemia, Cystic Fibrosis
- Autoimmune Diseases: The body’s immune system attacks its own cells.
- Example: Rheumatoid Arthritis, Lupus
- Nutritional Deficiencies: Lack of essential nutrients.
- Example: Scurvy (Vitamin C deficiency), Rickets (Vitamin D deficiency)
1.2 Environmental Causes
- Pollution: Air, water, and soil pollution contribute to respiratory diseases and cancer.
- Example: Asthma, Lung Cancer
- Climate Change: Extreme temperatures and natural disasters affect health.
- Example: Heatstroke, Malnutrition due to droughts
- Radiation Exposure: Causes genetic mutations leading to cancer.
- Example: Skin Cancer (UV radiation exposure)
1.3 Lifestyle and Behavioral Causes
- Unhealthy Diet: High-fat, high-sugar diets contribute to obesity, diabetes, and cardiovascular diseases.
- Lack of Physical Activity: Leads to obesity, hypertension, and heart diseases.
- Substance Abuse (Smoking, Alcohol, Drugs): Damages organs and increases cancer risks.
- Example: Liver Cirrhosis (Alcohol abuse), Lung Cancer (Smoking)
- Stress and Mental Health Issues: Chronic stress increases the risk of heart disease, stroke, and mental disorders.
1.4 Socioeconomic Causes
- Poverty: Poor access to healthcare, nutrition, and hygiene increases disease risk.
- Education Level: Lack of health awareness leads to preventable illnesses.
- Occupational Hazards: Jobs involving chemicals, heavy lifting, or long hours increase health risks.
- Example: Lung disease in coal miners (Black Lung Disease)
2. Risk Factors for Developing Illnesses
A risk factor is any condition, behavior, or trait that increases the likelihood of developing a disease. Risk factors can be modifiable (changeable) or non-modifiable (unchangeable).
2.1 Non-Modifiable Risk Factors (Unchangeable)
| Risk Factor | Explanation | Example Diseases |
|---|---|---|
| Genetics | Family history of certain conditions. | Hypertension, Diabetes, Cancer |
| Age | Older adults have higher risks for chronic diseases. | Alzheimer’s, Osteoporosis |
| Gender | Some diseases are more common in one gender. | Osteoporosis (women), Prostate Cancer (men) |
| Ethnicity/Race | Certain ethnic groups have higher risks for specific diseases. | Sickle Cell Anemia (African descent), Type 2 Diabetes (South Asians) |
💡 Nursing Role: Educate patients with a family history of diseases to undergo regular screening and adopt preventive health behaviors.
2.2 Modifiable Risk Factors (Changeable)
These are lifestyle and environmental factors that individuals can control to reduce disease risks.
1. Poor Diet and Nutrition
- High intake of processed foods, sugar, and unhealthy fats increases the risk of obesity, diabetes, and cardiovascular diseases.
- Example: Diets high in red meat and fried foods increase the risk of colon cancer.
Nursing Role: Educate patients on balanced diets and encourage intake of fruits, vegetables, whole grains, and lean proteins.
2. Physical Inactivity
- Lack of exercise contributes to obesity, heart disease, and type 2 diabetes.
- Example: A sedentary lifestyle increases the risk of stroke and hypertension.
Nursing Role: Encourage regular physical activity (at least 30 minutes of moderate exercise per day).
3. Smoking and Alcohol Consumption
- Smoking causes lung cancer, heart disease, and chronic obstructive pulmonary disease (COPD).
- Excessive alcohol intake leads to liver cirrhosis, pancreatitis, and high blood pressure.
Nursing Role: Provide smoking cessation programs and educate on alcohol moderation.
4. Stress and Mental Health
- Chronic stress increases the risk of hypertension, heart disease, and depression.
- Example: Long-term stress increases cortisol levels, which contributes to weight gain, anxiety, and high blood pressure.
Nursing Role: Teach stress management techniques (meditation, yoga, deep breathing exercises).
5. Unprotected Sexual Practices
- Leads to sexually transmitted infections (STIs) like HIV, syphilis, gonorrhea.
- Example: Human papillomavirus (HPV) infection can cause cervical cancer.
Nursing Role: Promote safe sex practices and educate on STI prevention.
6. Occupational and Environmental Exposures
- Workers in mines, factories, and construction sites are at risk of lung diseases, hearing loss, and poisoning.
- Example: Asbestos exposure leads to mesothelioma (lung cancer).
Nursing Role: Advocate for workplace safety, protective equipment, and regular health check-ups.
3. Classification of Risk Factors by Disease Type
| Disease Type | Major Risk Factors |
|---|---|
| Cardiovascular Diseases (Heart Attack, Stroke, Hypertension) | Smoking, high cholesterol, high blood pressure, diabetes, obesity, stress, lack of exercise |
| Diabetes (Type 2) | Poor diet, obesity, lack of exercise, genetics |
| Cancer (Lung, Breast, Colon, Skin, etc.) | Smoking, alcohol, UV exposure, obesity, genetic predisposition |
| Respiratory Diseases (COPD, Asthma, Tuberculosis) | Air pollution, smoking, allergens, occupational hazards |
| Mental Health Disorders (Depression, Anxiety, Schizophrenia) | Chronic stress, trauma, family history, substance abuse |
| Infectious Diseases (HIV/AIDS, Tuberculosis, Malaria, Hepatitis) | Poor sanitation, unsafe sex, weak immunity, travel exposure |
4. Prevention and Control of Risk Factors
1. Primary Prevention (Preventing Disease Before It Occurs)
- Vaccinations (e.g., Hepatitis B, HPV vaccine)
- Health education on lifestyle modifications
- Environmental hygiene (clean water, sanitation)
2. Secondary Prevention (Early Detection and Treatment)
- Regular screenings (e.g., blood pressure, cholesterol, cancer screenings)
- Early diagnosis (e.g., detecting diabetes at prediabetes stage)
- Health check-ups and monitoring (e.g., managing hypertension)
3. Tertiary Prevention (Reducing Complications of Diseases)
- Rehabilitation programs (e.g., cardiac rehab after heart attack)
- Chronic disease management (e.g., insulin therapy for diabetes)
- Support groups and mental health therapy
💡 Nursing Role: Provide patient education, conduct early screenings, and encourage lifestyle changes.
Key Takeaways:
✔ Identifying risk factors helps in disease prevention.
✔ Nurses play a key role in educating patients about modifiable risk factors.
✔ Early intervention and lifestyle changes can reduce disease risk.
✔ Primary, secondary, and tertiary prevention are essential in healthcare.
By addressing causes and risk factors, nurses can help individuals achieve better health and prevent chronic diseases.
Illness: Definition, Types, Significance

Introduction
Illness is a universal human experience that affects physical, mental, social, and emotional well-being. It disrupts normal functioning, reduces quality of life, and often requires medical intervention. Understanding illness is essential for nurses, healthcare providers, and individuals to ensure effective prevention, management, and treatment.
Definition of Illness
Illness is a state of poor health, where the body’s normal functions are impaired due to disease, infection, injury, or psychological distress. It can be temporary or chronic, affecting individuals differently based on their genetics, immunity, lifestyle, and environmental factors.
The World Health Organization (WHO) defines illness as:
“A condition that affects the body or mind, leading to discomfort, dysfunction, or distress, requiring intervention for recovery.”
Florence Nightingale, the pioneer of modern nursing, emphasized that illness is influenced by environmental conditions, hygiene, and patient care.
Types of Illness
Illnesses can be classified based on their duration, cause, severity, and impact on health.
1. Acute Illness
Acute illnesses develop suddenly, have a short duration, and often resolve with or without medical treatment. These conditions may be mild, moderate, or severe, requiring immediate attention.
- Examples:
- Common cold
- Influenza (Flu)
- Pneumonia
- Food poisoning
- Appendicitis
- Characteristics:
- Rapid onset of symptoms
- Short-term, usually lasting days to weeks
- Responds well to treatment
- Minimal long-term impact if managed properly
- Significance in Nursing:
- Requires quick assessment and prompt treatment.
- Nurses must provide symptom relief, patient education, and infection control measures.
2. Chronic Illness
Chronic illnesses persist over a long period, often lasting months or years. They usually progress slowly and may require long-term management and lifestyle modifications.
- Examples:
- Diabetes Mellitus
- Hypertension (High Blood Pressure)
- Asthma
- Arthritis
- Chronic Kidney Disease (CKD)
- Cancer
- Characteristics:
- Slow onset and long duration (may last a lifetime)
- Requires continuous medical care and monitoring
- Can be controlled but not always cured
- Impacts daily living, requiring lifestyle adjustments
- Significance in Nursing:
- Nurses play a crucial role in patient education, medication management, lifestyle counseling, and chronic disease monitoring.
- Emphasis on preventing complications and enhancing quality of life.
3. Infectious (Communicable) Illness
Infectious illnesses are caused by pathogens (bacteria, viruses, fungi, or parasites) and can spread from person to person through air, contact, or bodily fluids.
- Examples:
- Tuberculosis (TB)
- COVID-19
- Malaria
- Hepatitis B & C
- Measles
- Characteristics:
- Caused by infectious agents.
- Some are contagious (e.g., Influenza, HIV), while others are vector-borne (e.g., Malaria, Dengue).
- Can lead to outbreaks, epidemics, and pandemics.
- Preventable through vaccination, hygiene, and infection control measures.
- Significance in Nursing:
- Nurses must follow infection prevention protocols (e.g., hand hygiene, PPE use).
- Educate communities about vaccination, hygiene, and early detection.
4. Non-Communicable Illness
Non-communicable diseases (NCDs) are not caused by infectious agents and cannot spread from person to person. They are often linked to genetics, lifestyle, and environmental factors.
- Examples:
- Heart disease (Cardiovascular disease)
- Stroke
- Cancer
- Obesity
- Osteoporosis
- Characteristics:
- Long-term conditions requiring lifestyle modifications.
- Often caused by unhealthy diet, lack of exercise, smoking, and alcohol.
- Major cause of morbidity and mortality worldwide.
- Significance in Nursing:
- Nurses must educate patients on disease prevention and encourage healthy lifestyle changes.
- Monitor patients for early signs of complications.
5. Mental Illness
Mental illnesses affect cognitive, emotional, and behavioral health, impacting an individual’s ability to function in daily life.
- Examples:
- Depression
- Anxiety Disorders
- Schizophrenia
- Bipolar Disorder
- Post-Traumatic Stress Disorder (PTSD)
- Characteristics:
- Can be mild, moderate, or severe.
- Often coexists with physical illnesses (e.g., depression in diabetes).
- Requires counseling, therapy, medications, and social support.
- Significance in Nursing:
- Nurses must provide mental health assessments, counseling, and emotional support.
- Encourage stress management, social support, and adherence to therapy.
6. Terminal Illness
Terminal illnesses are progressive, incurable diseases that eventually lead to death. Patients with terminal illnesses require palliative care and pain management.
- Examples:
- Advanced-stage cancer
- End-stage renal failure
- Amyotrophic Lateral Sclerosis (ALS)
- End-stage heart failure
- Characteristics:
- Focus is on comfort care, symptom relief, and quality of life.
- Emotional and spiritual support is crucial for both patients and families.
- Significance in Nursing:
- Nurses provide palliative care and hospice services.
- Focus on pain relief, psychological support, and dignity in dying.
Significance of Illness in Healthcare and Nursing
Illnesses affect individuals, families, and societies, making their prevention, management, and treatment a key priority in nursing practice.
1. Impact on Individuals
- Reduces quality of life and independence.
- Causes physical, emotional, and financial burdens.
- May lead to mental distress and depression.
2. Impact on Families
- Family members may experience stress, anxiety, and emotional suffering.
- Increases financial strain due to medical expenses.
- Leads to changes in family roles and responsibilities.
3. Impact on Healthcare Systems
- Increased demand for medical services and hospital care.
- Puts strain on healthcare professionals and resources.
- Leads to a higher burden of chronic diseases and disabilities.
4. Role of Nurses in Managing Illness
- Prevention: Educating communities on healthy habits, vaccinations, and early detection.
- Care and Treatment: Providing medications, wound care, and monitoring symptoms.
- Support and Rehabilitation: Assisting in recovery, chronic disease management, and mental health support.
- Palliative and End-of-Life Care: Ensuring comfort and dignity in terminal illnesses.
Key Takeaways
✔ Illness is a deviation from normal health, affecting physical, mental, and social well-being.
✔ It can be acute, chronic, infectious, non-infectious, mental, or terminal.
✔ Nurses play a vital role in disease prevention, management, rehabilitation, and palliative care.
✔ Holistic care, patient education, and early interventions improve patient outcomes.
By understanding illness types, causes, and significance, healthcare providers can develop better strategies to improve patient well-being and overall public health.
Illness Behavior
Introduction
Illness behavior refers to how individuals perceive, interpret, and respond to symptoms of illness. It involves attitudes, emotions, beliefs, and actions when experiencing health issues. These behaviors determine whether a person seeks medical help, delays treatment, or ignores symptoms. Understanding illness behavior is essential for nurses and healthcare professionals to provide appropriate care and support.
Different people respond to illness in varied ways based on personal, cultural, social, and psychological factors. Nurses must assess these responses to ensure effective communication, timely intervention, and patient-centered care.
Definition of Illness Behavior
Illness behavior is the way individuals recognize, interpret, and respond to illness symptoms based on their personal experiences, cultural beliefs, and social influences.
According to David Mechanic (1962), illness behavior is “the way in which symptoms are perceived, evaluated, and acted upon by individuals in response to their health status.”
The World Health Organization (WHO) defines illness behavior as “the actions and decisions of individuals regarding their symptoms, including self-care, seeking medical help, and adherence to treatment.”
Key Features of Illness Behavior:
- How a person identifies and reacts to symptoms.
- The decision to self-medicate or seek professional care.
- Compliance with medical advice, treatment, and lifestyle changes.
- The influence of family, culture, and social norms on health-seeking behavior.
Types of Illness Behavior
Illness behavior can be categorized into three main types:
1. Illness Recognition Behavior
This involves how an individual identifies and interprets symptoms.
- Some individuals recognize symptoms early and seek medical help.
- Others may ignore symptoms, assuming they will resolve on their own.
- Denial of illness may lead to delayed treatment and complications.
💡 Example: A person with persistent headaches may self-diagnose as stress-related instead of considering a medical cause.
2. Health-Seeking Behavior
This refers to actions taken after identifying symptoms, including:
- Self-care measures: Home remedies, over-the-counter medications.
- Consulting family and friends for advice.
- Seeking medical attention (general practitioners, specialists, hospitals).
- Ignoring or delaying seeking care, which can worsen the condition.
💡 Example:
- A person with chest pain may rush to the hospital (prompt health-seeking behavior).
- Another may ignore it, assuming it’s gas or indigestion (delayed health-seeking behavior).
3. Adherence (Compliance) Behavior
This involves how well a patient follows medical advice, prescriptions, and lifestyle changes.
- Adherence: Following prescribed medication, dietary restrictions, and therapy.
- Non-Adherence: Ignoring treatment due to forgetfulness, side effects, cost, or cultural beliefs.
💡 Example:
- A diabetic patient who takes insulin regularly and follows a proper diet demonstrates adherence.
- A hypertensive patient who skips medication because they feel fine exhibits non-adherence.
Factors Influencing Illness Behavior
Illness behavior is shaped by personal, social, psychological, and cultural factors.
1. Personal Factors
- Perception of Illness Severity: Mild symptoms are often ignored, while severe symptoms prompt immediate action.
- Pain Tolerance: Some individuals endure pain longer before seeking help.
- Self-Efficacy: Confidence in managing illness affects health decisions.
💡 Example: A young athlete may ignore a minor knee pain, while an elderly person may seek care immediately.
2. Social and Cultural Factors
- Cultural Beliefs: Some cultures rely on traditional medicine and spiritual healing before consulting a doctor.
- Social Support: Family and friends influence health-seeking behavior.
- Gender Norms: Men may delay seeking care due to the belief that they should endure pain.
💡 Example: In some societies, women seek healthcare more frequently than men due to traditional caregiving roles.
3. Psychological Factors
- Fear and Anxiety: Some people avoid doctors due to fear of bad news.
- Denial: Individuals may refuse to accept that they have a serious condition.
- Depression and Mental Health Issues: These can lead to poor self-care and delayed treatment.
💡 Example: A person avoiding cancer screenings due to fear of a positive diagnosis.
4. Economic and Accessibility Factors
- Financial Constraints: High medical costs can prevent people from seeking treatment.
- Healthcare Availability: In rural areas, lack of hospitals and doctors delays treatment.
- Transportation Issues: Difficulty reaching healthcare facilities affects prompt diagnosis and care.
💡 Example: A person with chronic back pain avoiding medical care due to high treatment costs.
Models of Illness Behavior
Several models explain how individuals respond to illness symptoms:
1. Mechanic’s Variables Affecting Illness Behavior
David Mechanic identified 10 factors that influence how people recognize and respond to illness:
- Visibility of Symptoms: More visible symptoms (e.g., rashes) prompt faster action.
- Perceived Severity: Severe pain leads to quicker care-seeking.
- Disruption to Daily Life: If illness affects work, school, or routine, care is sought.
- Tolerance for Symptoms: Some endure pain longer before seeking help.
- Available Information and Knowledge: More awareness leads to earlier diagnosis.
- Competing Needs: Work and family obligations may delay healthcare visits.
- Competing Healthcare Resources: Access to hospitals, clinics, or traditional medicine affects choices.
- Cultural and Social Expectations: Cultural norms dictate whether medical care is sought.
- Denial and Emotional Response: Some may deny illness due to fear or anxiety.
- Accessibility of Healthcare: Geographic location and financial status impact care-seeking behavior.
2. Health Belief Model (HBM)
This model explains why people take or avoid health actions. It includes:
- Perceived Susceptibility: Belief in risk of disease (e.g., smokers and lung cancer).
- Perceived Severity: Belief about the seriousness of illness (e.g., ignoring mild symptoms).
- Perceived Benefits: Understanding that medical care helps recovery.
- Perceived Barriers: Fear of cost, pain, or inconvenience delays seeking care.
- Cues to Action: Media campaigns, health check-ups, and family influence trigger action.
💡 Example: A person who believes that regular exercise prevents heart disease will engage in physical activity.
Role of Nurses in Managing Illness Behavior
Nurses play a key role in shaping positive illness behavior by:
- Patient Education
- Teaching early symptom recognition.
- Explaining disease prevention and treatment.
- Encouraging Health-Seeking Behavior
- Addressing fears and misconceptions about medical care.
- Promoting regular check-ups and vaccinations.
- Improving Adherence
- Educating patients about medication schedules and lifestyle changes.
- Identifying barriers to adherence and providing support solutions.
- Providing Emotional and Psychological Support
- Counseling patients with fear, denial, or anxiety.
- Encouraging social support and peer groups.
- Advocating for Accessible Healthcare
- Helping patients navigate healthcare services.
- Promoting affordable treatment options.
Key Takeaways
✔ Illness behavior is how individuals perceive and respond to health symptoms.
✔ It includes recognizing symptoms, seeking medical help, and adhering to treatment.
✔ Factors such as culture, education, finances, and psychological state influence behavior.
✔ Nurses play a crucial role in promoting health awareness and positive illness behavior.
By educating patients, reducing fears, and improving access to care, healthcare providers can help individuals make better health decisions and improve overall well-being.
Impact of Illness on the Patient and Family
Introduction
Illness not only affects the individual experiencing it but also has a profound impact on family members, caregivers, and society. When a person becomes ill, their physical, emotional, financial, and social life changes, often leading to stress, adjustments, and challenges for both the patient and their family.
Nurses play a vital role in helping patients and families cope with the effects of illness, providing support, education, and intervention strategies to improve their quality of life.
1. Impact of Illness on the Patient
Illness brings physical, emotional, psychological, social, and financial changes to a person’s life. The severity of the impact depends on factors such as type of illness, duration, treatment options, and support system.
1.1 Physical Impact
- Pain and Discomfort: Many illnesses cause pain, fatigue, and physical discomfort, affecting daily activities.
- Loss of Function or Disability: Some diseases lead to temporary or permanent disability, limiting movement or independence.
- Side Effects of Treatment: Medications, surgeries, and therapies may cause nausea, fatigue, weakness, and hair loss (e.g., chemotherapy side effects).
- Weakened Immunity: Patients with chronic conditions or infections may become more susceptible to secondary infections.
- Fatigue and Weakness: Many illnesses lead to loss of energy, reducing the patient’s ability to work or engage in social activities.
💡 Example: A stroke patient may experience paralysis on one side of the body, requiring long-term physiotherapy and mobility aids.
1.2 Emotional and Psychological Impact
- Fear and Anxiety: Patients may fear death, disability, or worsening health conditions.
- Depression: Long-term illness can cause hopelessness, sadness, and withdrawal.
- Loss of Self-Esteem and Confidence: Physical changes, scars, or disabilities can affect a patient’s body image and self-worth.
- Frustration and Anger: Chronic pain or limitations can lead to irritability and mood swings.
- Stress and Guilt: Patients may feel guilty about being a burden on family members.
💡 Example: A cancer patient undergoing chemotherapy may experience hair loss, weight loss, and fatigue, leading to self-esteem issues and depression.
1.3 Social Impact
- Social Isolation: Patients with chronic or infectious diseases may experience reduced social interaction due to stigma, mobility issues, or fatigue.
- Relationship Strain: Family and friends may find it difficult to adjust to the patient’s illness.
- Work and Career Challenges: Illness may force early retirement, job loss, or frequent absences, affecting financial stability.
💡 Example: A patient with tuberculosis (TB) may experience social stigma due to fear of spreading the infection.
1.4 Financial Impact
- Medical Expenses: The cost of medications, hospital visits, and surgeries can be overwhelming.
- Loss of Income: Patients who cannot work may face financial instability.
- Travel and Accommodation Costs: Long-term treatment often requires traveling to hospitals, adding extra expenses.
💡 Example: A patient with chronic kidney disease may need frequent dialysis, leading to high medical bills and financial burden.
2. Impact of Illness on the Family
Illness affects not just the patient but also their family, caregivers, and loved ones, leading to emotional, financial, and social strain.
2.1 Emotional and Psychological Impact on Family
- Stress and Anxiety: Family members worry about the patient’s health, treatment, and financial burden.
- Depression and Emotional Burnout: Long-term caregiving can lead to mental exhaustion, sadness, and hopelessness.
- Guilt and Helplessness: Family members may feel guilty for not being able to do enough.
- Fear of Losing the Patient: Terminal illnesses create fear and emotional distress.
💡 Example: A mother caring for a child with cerebral palsy may experience severe emotional stress and exhaustion.
2.2 Financial Burden on Family
- Loss of Family Income: If the main earner is sick, the family may face financial difficulties.
- Medical Bills and Treatment Costs: Long-term illnesses require continuous medical expenses.
- Additional Expenses: Home modifications, assistive devices, and caregiver services add to financial stress.
💡 Example: A family supporting a patient with Alzheimer’s disease may struggle with home nursing costs, medications, and therapy sessions.
2.3 Changes in Family Roles and Responsibilities
- Increased Responsibilities: Family members may have to take on new roles (e.g., a child caring for a sick parent).
- Neglect of Other Family Members: Focus on the patient may lead to less attention to other children or partners.
- Relationship Strain: Stress may cause conflicts, disagreements, and emotional distance among family members.
💡 Example: A wife caring for a husband with Parkinson’s disease may struggle with household chores, finances, and emotional support.
2.4 Social and Lifestyle Changes
- Reduced Social Interaction: Caregivers may withdraw from social life due to caregiving duties.
- Time Constraints: Managing illness may require sacrificing personal activities, hobbies, or vacations.
- Changes in Daily Routine: Family members may need to adjust their work schedules, meal plans, and daily habits.
💡 Example: Parents caring for a child with autism may have limited time for social gatherings and personal activities.
3. Coping Strategies for Patients and Families
To reduce stress, manage illness, and improve well-being, patients and families can adopt the following coping strategies:
3.1 Emotional and Psychological Coping
- Counseling and Therapy: Professional support can reduce stress and anxiety.
- Support Groups: Connecting with others facing similar challenges can provide emotional relief.
- Mindfulness and Relaxation Techniques: Practices like yoga, meditation, and deep breathing help manage stress.
- Spiritual and Religious Support: Faith-based activities can bring comfort and hope.
3.2 Financial Management
- Health Insurance: Helps cover hospital bills and medications.
- Government and NGO Assistance: Many organizations offer financial aid for medical expenses.
- Budgeting and Planning: Families should prioritize essential healthcare costs and seek discounted medical services.
3.3 Social Support and Lifestyle Adjustments
- Seeking Help from Relatives and Friends: Sharing responsibilities reduces caregiver burden.
- Community Resources: Utilizing home nursing, transportation services, and disability assistance programs can help.
- Maintaining Work-Life Balance: Caregivers should find time for self-care and relaxation.
3.4 Adapting to New Roles and Responsibilities
- Time Management: Prioritizing tasks reduces caregiver stress.
- Home Modifications: Simple changes, like installing ramps and handrails, improve patient mobility.
- Encouraging Patient Independence: Helping the patient regain self-care skills improves their self-esteem.
💡 Example: Teaching a stroke patient to use assistive devices for eating and dressing can restore confidence.
4. Role of Nurses in Supporting Patients and Families
Nurses play a key role in minimizing the negative impact of illness on patients and families through education, counseling, and compassionate care.
4.1 Providing Emotional and Psychological Support
- Offer counseling services to patients and caregivers.
- Encourage mental health support through therapy and self-care.
4.2 Educating Patients and Families
- Teach self-care practices and medication management.
- Guide families on preventing complications and managing symptoms.
4.3 Connecting Families with Resources
- Refer patients to support groups, rehabilitation centers, and financial aid programs.
- Advocate for affordable healthcare services and insurance benefits.
Key Takeaways:
✔ Illness affects physical, emotional, financial, and social aspects of life.
✔ Family members experience stress, financial burden, and role changes.
✔ Coping strategies include counseling, social support, and financial planning.
✔ Nurses provide guidance, education, and emotional support to both patients and caregivers.
By addressing these challenges holistically, healthcare providers can help patients and families achieve better health outcomes and improved quality of life.
FOR UNLOCK 🔓 FULL COURSE NOW. MORE DETAILS CALL US OR WATSAPP ON- 8485976407
