(B.Sc.) Semester-2 Examination December-2025-Applied Biochemistry and Applied Nutrition & Dietetics (BKNMU)
Applied Biochemistry and Applied Nutrition & Dietetics (BKNMU) – Semester-2 Examination December-2025
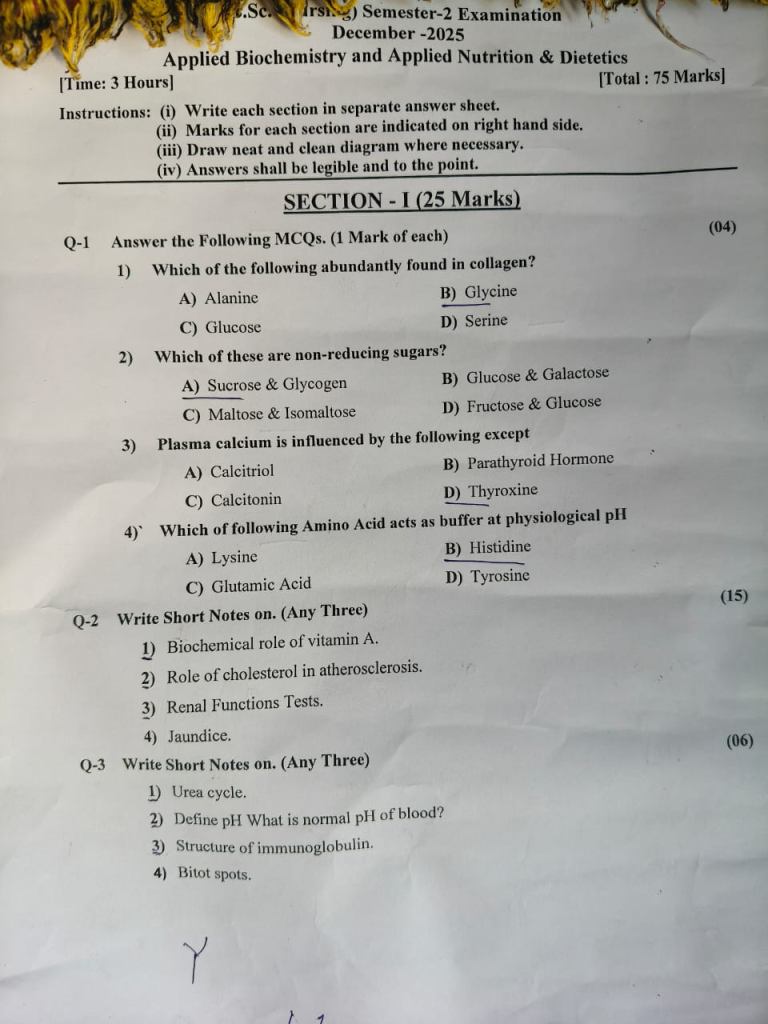
SECTION – I (25 Marks)
Q-1 Answer the Following MCQs. (1 Mark of each) (04)
1. Which of the following abundantly found in collagen?
A) Alanine
B) Glycine
C) Glucose
D) Serine
💥 Glycine is the substance which is abundantly found in collagen, in which it forms nearly 33% (one-third) of the total amino acid composition of collagen protein.
2. Which of these are non-reducing sugars?
A) Sucrose & Glycogen
B) Glucose & Galactose
C) Maltose & Isomaltose
D) Fructose & Glucose
💥 Sucrose is, in which, a non-reducing disaccharide, because both the reducing ends of glucose and fructose are involved in glycosidic bond formation, and therefore no free reducing group is present.
3.Plasma calcium is influenced by the following except
A) Calcitriol
B) Parathyroid Hormone
C) Calcitonin
D) Thyroxine
💥 Plasma calcium level is, in which, mainly regulated by hormones that directly act on bone, kidney, and intestine, and these hormones maintain calcium homeostasis in the body.
Calcitriol (Vitamin D₃) is, in which, a hormone that increases plasma calcium level by enhancing intestinal absorption of calcium, increasing renal reabsorption, and mobilizing calcium from bone.
Parathyroid Hormone (PTH) is, in which, the principal regulator of plasma calcium, and it increases serum calcium by bone resorption, increased renal reabsorption of calcium, and activation of vitamin D.
4. Which of following Amino Acid acts as buffer at physiological pH
A) Lysine
B) Histidine
C) Glutamic Acid
D) Tyrosine
💥 Histidine is the amino acid which is, in which, known to act as an effective buffer at physiological pH (around 7.4) because of the chemical nature of its side chain.
Q-2 Write Short Notes on. (Any Three) (5X3=15)
Q-1.Biochemical role of vitamin A.
ANSWER :-
- Vitamin A is, in which, a fat-soluble vitamin stored mainly in the liver in the form of retinyl esters, and it is transported in blood bound to retinol-binding protein (RBP) along with transthyretin.
- Vitamin A exists, in which, in three biologically active forms, namely retinol, retinal, and retinoic acid, and each form performs a distinct biochemical function in the body.
- Role in vision is, in which, one of the most important biochemical roles, because 11-cis-retinal combines with opsin in rod cells to form rhodopsin, which is essential for scotopic (dim-light) vision, and deficiency leads to night blindness.
- Vitamin A is, in which, required for the visual cycle, where light converts 11-cis-retinal to all-trans-retinal, initiating a nerve impulse, and regeneration of retinal is necessary for continuous vision.
- Maintenance of epithelial integrity is, in which, a key role, because retinoic acid regulates gene transcription that maintains normal differentiation of epithelial cells, preventing keratinization and dryness of skin and mucous membranes.
- Vitamin A is, in which, essential for growth and development, as it influences osteoblast and osteoclast activity, thereby contributing to normal bone growth and remodeling, especially during childhood.
- It is, in which, plays a crucial role in cell differentiation and morphogenesis, particularly during embryonic development, and excess or deficiency can lead to congenital abnormalities.
- Role in immune function is, in which, significant, because vitamin A enhances humoral and cell-mediated immunity, maintains lymphocyte proliferation, and supports antibody production, thus reducing susceptibility to infections.
- Vitamin A is, in which, important for reproductive function, because retinol is required for spermatogenesis in males, and retinoic acid is necessary for placental development and fetal growth in females.
- Antioxidant role is, in which, mainly attributed to β-carotene, which scavenges free radicals, protects cell membranes from oxidative damage, and reduces the risk of chronic diseases.
- Vitamin A is, in which, involved in glycoprotein and mucopolysaccharide synthesis, which is essential for mucus secretion, cell adhesion, and maintenance of normal tissue architecture.
- It is, in which, also required for iron metabolism, because vitamin A helps in mobilization of iron from stores, and deficiency can contribute to anemia even when iron intake is adequate.
- Vitamin A is, in which, plays a role in regulation of gene expression, as retinoic acid binds to nuclear receptors (RAR and RXR) that act as transcription factors influencing cell growth and differentiation.
- Nurses should, in which, identify individuals at risk of vitamin A deficiency such as children, pregnant women, malnourished patients, and provide dietary counseling including green leafy vegetables, carrots, milk, egg yolk, and liver.
- Nursing care is, in which, important in vitamin A prophylaxis programs, monitoring for deficiency signs like night blindness and xerophthalmia, and preventing toxicity due to excess supplementation, especially in pregnancy.
Q-2.Role of cholesterol in atherosclerosis.
- Cholesterol is, in which, a major lipid component of plasma lipoproteins, and it plays a central and critical role in the development of atherosclerosis, which is a chronic inflammatory disease of arterial walls.
- Low-density lipoprotein (LDL) cholesterol is, in which, the most atherogenic form of cholesterol, because it transports cholesterol from the liver to peripheral tissues, and excess LDL gets deposited in the intima of arterial walls.
- LDL cholesterol is, in which, subjected to oxidation within the arterial wall, and oxidized LDL acts as a strong stimulus for endothelial injury and inflammation.
- Endothelial damage is, in which, the initial step in atherogenesis, and it increases vascular permeability, allowing more LDL cholesterol to enter the arterial intima.
- Oxidized LDL is, in which, taken up by macrophages through scavenger receptors, leading to the formation of foam cells, which are lipid-laden cells and form the fatty streak, the earliest visible lesion of atherosclerosis.
- Accumulation of foam cells is, in which, associated with the release of inflammatory cytokines and growth factors, which stimulate smooth muscle cell migration and proliferation in the arterial wall.
- Cholesterol is, in which, deposited along with smooth muscle cells, collagen, and extracellular matrix, forming a fibrofatty plaque (atheromatous plaque) that progressively narrows the arterial lumen.
- With progression, cholesterol-rich plaques are, in which, prone to rupture, exposing thrombogenic material and leading to platelet aggregation and thrombus formation, which can cause acute coronary syndrome, stroke, or peripheral vascular disease.
- High-density lipoprotein (HDL) cholesterol is, in which, considered anti-atherogenic, because it removes excess cholesterol from peripheral tissues and arterial walls by reverse cholesterol transport, thereby reducing plaque formation.
- A high level of total cholesterol and LDL cholesterol with a low level of HDL cholesterol is, in which, a major modifiable risk factor for atherosclerosis.
- Nurses play an important role in atherosclerosis prevention by, in which, educating patients about low-fat and low-cholesterol diet, promoting regular physical activity, encouraging smoking cessation, and ensuring medication adherence such as statins to control cholesterol levels and prevent cardiovascular complications.
Q-3. Renal Functions Tests.
- Renal Function Tests (RFT) are, in which, a group of biochemical and laboratory investigations used to assess the functional status of kidneys, and they help in evaluating glomerular filtration, tubular function, and renal excretory capacity.
- Blood Urea is, in which, one of the most commonly used renal function tests, and it reflects the kidney’s ability to excrete nitrogenous waste products, where increased blood urea indicates impaired renal function, dehydration, or increased protein catabolism.
- Serum Creatinine is, in which, a more reliable indicator of renal function than urea, because it is produced at a relatively constant rate from muscle metabolism and is excreted almost entirely by the kidneys, and its elevation indicates reduced glomerular filtration rate (GFR).
- Creatinine Clearance Test is, in which, used to estimate the glomerular filtration rate, and it measures the volume of plasma cleared of creatinine per minute, thereby providing a more accurate assessment of kidney function.
- Blood Urea Nitrogen (BUN) is, in which, the nitrogenous component of urea, and its level helps in differentiating pre-renal, renal, and post-renal causes of kidney dysfunction when interpreted along with creatinine.
- Serum Uric Acid is, in which, included in renal function assessment because kidneys are responsible for its excretion, and elevated levels may be seen in renal failure, gout, and conditions with increased cell turnover.
- Electrolyte levels such as serum sodium, potassium, chloride, calcium, and phosphate are, in which, essential components of RFT, because kidneys play a key role in maintaining electrolyte balance, and abnormalities indicate renal tubular dysfunction.
- Serum Potassium is, in which, particularly important, because impaired renal excretion can lead to hyperkalemia, which is a life-threatening condition causing cardiac arrhythmias.
- Urinalysis is, in which, a basic but essential renal function test that includes examination of urine volume, color, specific gravity, pH, protein, glucose, ketones, blood, and sediments, and it helps in detecting early kidney damage.
- Urine Protein (Albumin) estimation is, in which, important for detecting glomerular damage, and the presence of albumin in urine (albuminuria) is an early marker of chronic kidney disease and diabetic nephropathy.
- Urine Specific Gravity is, in which, used to assess the kidney’s ability to concentrate and dilute urine, and abnormal values indicate tubular dysfunction.
- Estimated Glomerular Filtration Rate (eGFR) is, in which, calculated using serum creatinine along with age, sex, and body size, and it is widely used for staging chronic kidney disease (CKD).
- Nurses are, in which, responsible for proper sample collection (blood and urine), monitoring intake and output, observing for signs of fluid and electrolyte imbalance, educating patients about hydration and diet, and assisting in early detection and management of acute and chronic renal disorders.
Q-4-Jaundice.
Jaundice in Biochemistry – B.Sc. Nursing exam-oriented explanation (narrative, long sentence but point-wise):
- Jaundice is, in which, a clinical and biochemical condition characterized by yellowish discoloration of skin, sclera, and mucous membranes, and it occurs due to an increase in serum bilirubin level above normal (usually >2–3 mg/dL).
- Bilirubin is, in which, a yellow pigment formed from the breakdown of heme of hemoglobin in reticuloendothelial cells, mainly in the spleen, liver, and bone marrow.
- In biochemistry, jaundice is, in which, explained based on bilirubin metabolism, which includes formation, transport, hepatic uptake, conjugation, and excretion of bilirubin.
Biochemical metabolism of bilirubin
- Hemoglobin is, in which, broken down into heme and globin, where globin forms amino acids and heme is converted into biliverdin and then into unconjugated bilirubin.
- Unconjugated bilirubin is, in which, water-insoluble, and it circulates in blood bound to albumin to reach the liver.
- In the liver, unconjugated bilirubin is, in which, taken up by hepatocytes and conjugated with glucuronic acid by the enzyme UDP-glucuronyl transferase, forming conjugated bilirubin, which is water-soluble.
- Conjugated bilirubin is, in which, excreted into bile and enters the intestine, where it is converted into urobilinogen, part of which is excreted in urine and stool.
Biochemical classification of jaundice
1. Hemolytic (Pre-hepatic) Jaundice
- Hemolytic jaundice is, in which, caused by excessive destruction of red blood cells, leading to increased production of unconjugated bilirubin.
- In this type, liver function is, in which, normal, but it cannot conjugate the excess bilirubin load.
- Biochemically, there is increase in unconjugated bilirubin, no bilirubin in urine, and increased urobilinogen in urine and stool.
- Examples include hemolytic anemia, malaria, incompatible blood transfusion.
2. Hepatocellular (Hepatic) Jaundice
- Hepatic jaundice is, in which, due to damage to liver cells, leading to impaired uptake, conjugation, or excretion of bilirubin.
- Biochemically, there is increase in both unconjugated and conjugated bilirubin.
- Liver enzymes such as ALT and AST are, in which, markedly elevated.
- Urine shows bilirubin present, and urobilinogen may be increased or decreased.
- Examples include viral hepatitis, alcoholic liver disease, drug-induced liver injury.
3. Obstructive (Post-hepatic) Jaundice
- Obstructive jaundice is, in which, caused by blockage in bile ducts, preventing excretion of conjugated bilirubin into the intestine.
- Biochemically, there is a marked increase in conjugated (direct) bilirubin.
- Alkaline phosphatase (ALP) is, in which, significantly elevated.
- Urine contains bilirubin, stool becomes clay-colored, and urobilinogen is absent.
- Examples include gallstones, carcinoma of pancreas, bile duct obstruction.
Biochemical laboratory findings in jaundice
- Serum bilirubin estimation is, in which, the most important test, and it includes total, direct, and indirect bilirubin.
- Liver function tests (LFTs) such as ALT, AST, ALP, serum albumin, and prothrombin time are, in which, used to identify the type and severity of jaundice.
- Urine examination is, in which, useful to detect bilirubin and urobilinogen, helping in differentiation of jaundice types.
- Knowledge of jaundice in biochemistry is, in which, essential for nurses to interpret laboratory values, identify type of jaundice, monitor liver function, provide dietary and medication guidance, and detect complications early in patients with liver and hemolytic disorders.
Q-3 Write Short Notes on. (Any Three) (06)
Q-1. Urea cycle.
- Urea cycle is, in which, a biochemical pathway responsible for conversion of toxic ammonia into non-toxic urea, and it mainly occurs in the liver.
- It is, in which, also called the Ornithine cycle, because ornithine acts as a carrier molecule and is regenerated at the end of the cycle.
- The cycle is, in which, essential for removal of excess nitrogen produced during amino acid metabolism.
- The first two reactions of the urea cycle are, in which, carried out in the mitochondria, while the remaining reactions take place in the cytosol of hepatocytes.
- Carbamoyl phosphate synthetase-I (CPS-I) is, in which, the rate-limiting enzyme, and it requires N-acetylglutamate as an activator.
- The nitrogen atoms of urea are, in which, derived from ammonia and aspartate, while the carbon atom comes from carbon dioxide.
- The urea cycle is, in which, an energy-dependent process, requiring three ATP molecules (four high-energy phosphate bonds) for synthesis of one molecule of urea.
- The final product urea is, in which, transported from liver to kidneys and excreted in urine.
- Defects in urea cycle enzymes are, in which, associated with hyperammonemia, leading to neurological manifestations.
- The urea cycle is, in which, clinically important in liver diseases, where impaired function leads to accumulation of ammonia.
- Nurses should, in which, understand the urea cycle to recognize signs of ammonia toxicity, monitor laboratory values, and assist in dietary and medical management of patients with hepatic disorders.
Q-2. Define pH What is normal pH of blood?
- pH is, in which, defined as the negative logarithm of hydrogen ion concentration of a solution, and it is used to express the degree of acidity or alkalinity of body fluids.
- Mathematically, pH is, in which, expressed as pH = –log₁₀ [H⁺], where [H⁺] represents the hydrogen ion concentration in the solution.
- pH is, in which, an important biochemical parameter, because even small changes in hydrogen ion concentration can significantly affect enzyme activity, protein structure, and metabolic reactions.
- The normal pH of blood is, in which, maintained within a narrow range of 7.35 to 7.45, which indicates that blood is slightly alkaline in nature.
- This normal blood pH is, in which, essential for normal physiological functions, and it is tightly regulated by buffer systems, lungs, and kidneys.
- Any deviation of blood pH below 7.35 is, in which, referred to as acidosis, and any increase above 7.45 is, in which, referred to as alkalosis.
- Knowledge of pH and normal blood pH is, in which, crucial for nurses to interpret arterial blood gas (ABG) reports, recognize acid–base imbalances, and provide appropriate nursing care in patients with respiratory or metabolic disorders.
Q-3. Structure of immunoglobulin.
- Immunoglobulins (Ig) are, in which, antibody glycoproteins produced by plasma cells, and they play a central role in humoral immunity.
- The basic structure of an immunoglobulin molecule is, in which, Y-shaped, and it is composed of four polypeptide chains held together by disulfide bonds.
- An immunoglobulin consists of two identical heavy (H) chains and two identical light (L) chains, in which the heavy chains determine the class of immunoglobulin.
- The light chains are, in which, of two types, namely kappa (κ) and lambda (λ), and each antibody molecule contains only one type of light chain.
- Each polypeptide chain is, in which, divided into a variable (V) region and a constant (C) region, where the variable region is responsible for antigen binding.
- The antigen-binding site is, in which, formed by the variable regions of one heavy chain and one light chain, creating a highly specific binding area.
- The Fab region (Fragment antigen binding) is, in which, the arm of the Y-shaped structure, and it is responsible for recognition and binding of antigen.
- The Fc region (Fragment crystallizable) is, in which, the stem of the Y-shaped structure, and it mediates biological functions such as complement activation, placental transfer, and binding to cell receptors.
- A hinge region is, in which, present between Fab and Fc portions, and it provides flexibility to the antibody molecule for effective antigen binding.
- Immunoglobulins are, in which, glycoproteins, and carbohydrate components are mainly attached to the Fc region of heavy chains.
- Understanding the structure of immunoglobulin is, in which, important for nurses to comprehend immune responses, vaccine action, hypersensitivity reactions, and immunodeficiency disorders, which are frequently encountered in clinical practice.
Q-4. Bitot spots.
- Bitot’s spots are, in which, dry, foamy, whitish or grayish patches seen on the conjunctiva of the eye, usually on the temporal side.
- They are, in which, caused due to vitamin A deficiency, leading to xerophthalmia.
- Biochemically, Bitot’s spots are, in which, due to keratinization of conjunctival epithelium and accumulation of keratin debris.
- They are, in which, considered an early clinical sign of chronic vitamin A deficiency, especially in children.
- Presence of Bitot’s spots is, in which, an indicator of malnutrition and poor dietary intake of vitamin A.
- Nurses should, in which, identify Bitot’s spots early, provide vitamin A supplementation, counsel on diet rich in vitamin A, and help prevent progression to corneal ulceration and blindness.
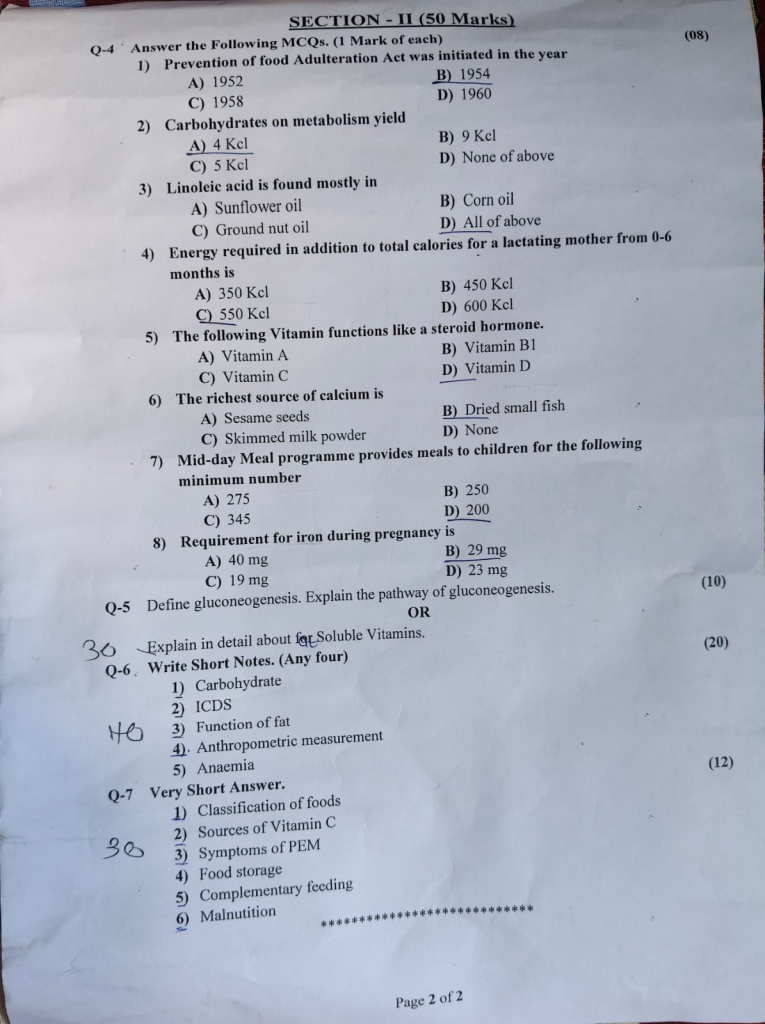
SECTION – II (50 Marks)
Q-4 Answer the Following MCQs. (1 Mark of each) (08)
1.Prevention of food Adulteration Act was initiated in the year
A) 1952
C) 1958
B) 1954
D) 1960
initiated and passed in the year 1954, and it came into force to ensure purity, quality, and safety of food items sold to the public.
2.Carbohydrates on metabolism yield
A) 4 Kcl
C) 5 Kcl
B) 9 Kcl
D) None of above
3.Linoleic acid is found mostly in
A) Sunflower oil
C) Ground nut oil
B) Corn oil
D) All of above
4. Energy required in addition to total calories for a lactating mother from 0-6 months is
A) 350 Kcl
C) 550 Kcl
B) 450 Kel
D) 600 Kcl
5. The following Vitamin functions like a steroid hormone.
A) Vitamin A
C) Vitamin C
B) Vitamin B1
D) Vitamin D
6. The richest source of calcium is
A) Sesame seeds
C) Skimmed milk powder
B) Dried small fish
D) None
7. Mid-day Meal programme provides meals to children for the following minimum number
A) 275
C) 345
B) 250
D) 200
8. Requirement for iron during pregnancy is
A) 40 mg
C) 19 mg
B) 29 mg
D) 23
Q-5 Define gluconeogenesis. Explain the pathway of gluconeogenesis. (10)
OR
Explain in detail about fat Soluble Vitamins.
Q-6 Write Short Notes. (Any four) (20)
1.Carbohydrate
2.ICDS
3.Function of fat
4.Anthropometric measurement
5.Anaemia
Q-7 Very Short Answer. (12)
1.Classification of foods
2.Sources of Vitamin C
3.Symptoms of PEM
4.Food storage
5.Complementary feeding
6.Malnutition