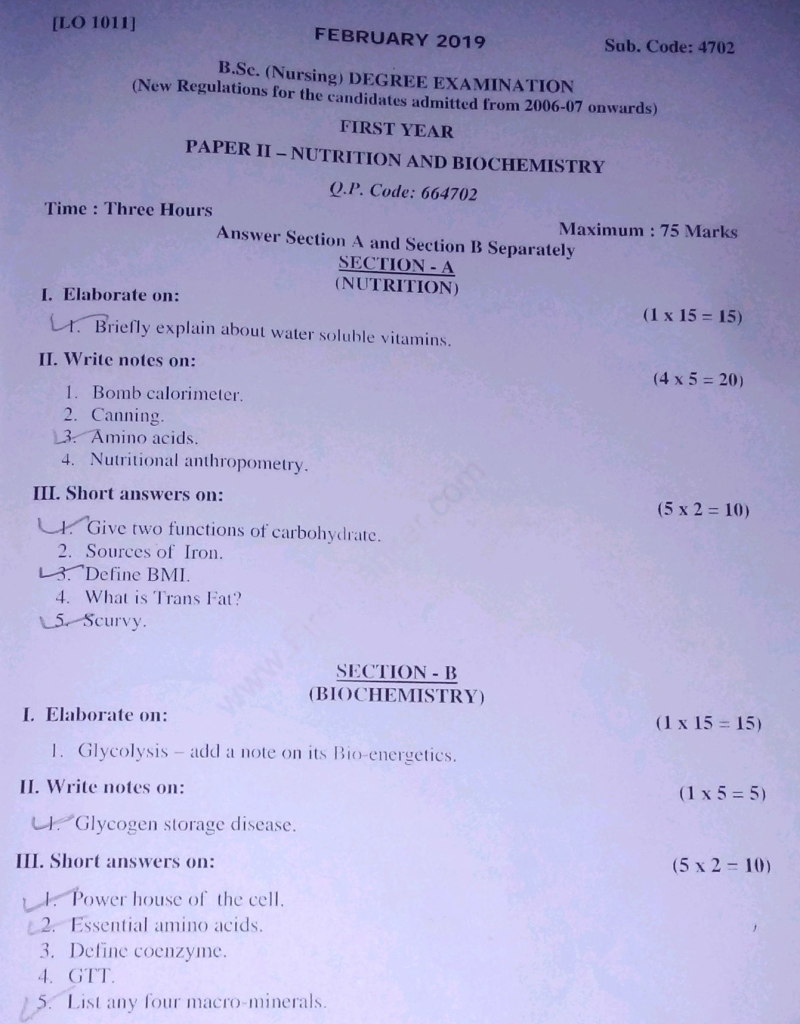
B.SC. FEBRUARY 2019 FIRST YEAR NUTRITION AND BIOCHEMISTRY-paper solution no-09 (MODIFY PENDING)
PAPER SOLUTION NO.09-FEBRUARY-2019
SECTION – A (NUTRITION)
l. Elaborate on: (1 x 15 = 15)
1.Briefly explain about water soluble vitamins.
📘 Definition and Characteristics
1️⃣ It is a group of vitamins that dissolve easily in water and are carried to the body’s tissues but are not stored in significant amounts, requiring daily intake through food or supplements.
2️⃣ It is excreted quickly in urine when consumed in excess, so the risk of toxicity is lower than fat-soluble vitamins (except for high doses of B6).
3️⃣ It is mostly involved in cell metabolism, enzyme cofactor activity, energy production, and tissue repair processes in the human body.
4️⃣ It is destroyed easily by heat, air, and light; therefore, improper cooking and storage methods can significantly reduce their availability.
🔠 Classification of Water-Soluble Vitamins
🔹 Divided into two major groups:
- B-Complex Vitamins – 8 types
- Vitamin C – Ascorbic Acid
🧬 B-COMPLEX VITAMINS: Function, Sources, Deficiency
✅ 1. Vitamin B1 (Thiamine)
🔹 Function:
- It is essential for converting carbohydrates into energy (as part of thiamine pyrophosphate).
- It plays a vital role in nerve impulse conduction, especially in brain and heart tissues.
🔹 Sources:
- Whole grains, fortified cereals, pork, legumes, sunflower seeds, peas.
🔹 Deficiency:
- Beriberi – affects muscles, nerves, and heart (dry and wet types).
- Wernicke-Korsakoff Syndrome – seen in alcoholics with confusion, memory loss, and ataxia.
✅ 2. Vitamin B2 (Riboflavin)
🔹 Function:
- It helps in oxidation-reduction reactions as part of coenzymes FAD and FMN.
- Supports growth, skin health, and mucosal integrity.
🔹 Sources:
- Milk, cheese, eggs, liver, green leafy vegetables, almonds.
🔹 Deficiency:
- Ariboflavinosis, leading to angular stomatitis, glossitis, cheilitis, photophobia.
✅ 3. Vitamin B3 (Niacin/Nicotinic Acid)
🔹 Function:
- Involved in metabolic pathways (NAD/NADP coenzymes), DNA repair, and skin function.
- Helps in reducing LDL cholesterol and increasing HDL.
🔹 Sources:
- Meat, poultry, fish, peanuts, legumes, enriched cereals.
🔹 Deficiency:
- Pellagra – 4 D’s: Dermatitis, Diarrhea, Dementia, Death.
- Seen in maize-based diets or in carcinoid syndrome.
✅ 4. Vitamin B5 (Pantothenic Acid)
🔹 Function:
- Component of coenzyme A, needed for fatty acid metabolism and synthesis of steroid hormones.
🔹 Sources:
- Eggs, liver, avocados, mushrooms, whole grains.
🔹 Deficiency:
- Rare, but includes fatigue, insomnia, nausea, and neurological disturbances.
✅ 5. Vitamin B6 (Pyridoxine)
🔹 Function:
- Acts as a coenzyme in amino acid metabolism, neurotransmitter synthesis (serotonin, dopamine), and hemoglobin formation.
🔹 Sources:
- Poultry, fish, bananas, fortified cereals, potatoes.
🔹 Deficiency:
- Causes irritability, peripheral neuropathy, and sideroblastic anemia.
- Common in isoniazid or hydralazine therapy.
🔹 Toxicity Note:
- High-dose supplementation (>100mg/day) may lead to sensory neuropathy.
✅ 6. Vitamin B7 (Biotin)
🔹 Function:
- Functions as a coenzyme in carboxylation reactions (fatty acid synthesis, gluconeogenesis).
- Supports healthy skin, hair, and nails.
🔹 Sources:
- Egg yolk, liver, soybeans, whole grains, cauliflower.
🔹 Deficiency:
- Rare; may result in hair thinning, dermatitis, and depression.
- Raw egg white contains avidin, which binds biotin and prevents absorption.
✅ 7. Vitamin B9 (Folate/Folic Acid)
🔹 Function:
- Essential for DNA synthesis, RBC formation, and neural tube development in fetus.
- Works closely with B12 in homocysteine metabolism.
🔹 Sources:
- Green leafy vegetables, citrus fruits, legumes, fortified grains.
🔹 Deficiency:
- Leads to megaloblastic anemia, fatigue, and neural tube defects (e.g., spina bifida in newborns).
- Common in pregnancy, alcoholics, and elderly.
✅ 8. Vitamin B12 (Cyanocobalamin)
🔹 Function:
- Crucial for nervous system maintenance, myelin synthesis, and DNA production.
- Works with folate in RBC formation.
🔹 Sources:
- Exclusively found in animal products – fish, eggs, milk, liver, meat.
🔹 Absorption Requirement:
- Requires intrinsic factor secreted by parietal cells in stomach.
🔹 Deficiency:
- Causes pernicious anemia, neuropathy, fatigue, memory loss.
- Common in vegans, elderly, and post-gastrectomy patients.
🍊 Vitamin C (Ascorbic Acid)
🔹 Function:
- Potent antioxidant, enhances iron absorption, supports immune response.
- Crucial for collagen synthesis, wound healing, and cartilage integrity.
🔹 Sources:
- Citrus fruits (oranges, lemons), strawberries, kiwi, amla, bell peppers, broccoli.
🔹 Deficiency:
- Scurvy – bleeding gums, petechiae, poor wound healing, joint pain.
🔹 Supplement Use:
- Used in common cold prevention, wound care, and iron deficiency treatment.
🩺 Nursing Considerations for Water-Soluble Vitamins
1️⃣ It is necessary for the nurse to monitor dietary intake of water-soluble vitamins in vulnerable groups like pregnant women, elderly, alcoholics, and vegetarians.
2️⃣ It is important for the nurse to assess for deficiency signs, such as glossitis, irritability, peripheral neuropathy, or anemia.
3️⃣ It is the responsibility of the nurse to educate patients to avoid overcooking vegetables and use methods like steaming to preserve water-soluble vitamins.
4️⃣ It is the nurse’s role to administer oral or parenteral vitamin supplements when needed, especially Vitamin B12 injections in cases of absorption defect.
5️⃣ It is essential to ensure patients understand that daily intake is required as the body cannot store excess amounts for long durations.
🟢 Clinical Importance in Nursing Practice
- Nurses must evaluate for malnutrition or signs of micronutrient deficiencies in chronically ill patients.
- Vitamin C and folate are commonly supplemented in pregnancy, wound care, and surgical recovery.
- Vitamin B12 is essential for patients with gastric resection or vegan diets.
- Vitamin B6 supplementation is routinely given during tuberculosis treatment to prevent peripheral neuropathy.
II. Write notes on:(4 x 5 = 20)
1.Bomb calorimeter.
📘 1. Definition
🔹 A Bomb Calorimeter is a scientific instrument used to measure the amount of heat (energy) released during the complete combustion of a substance, typically food or fuel, in a controlled oxygen-rich environment.
🔹 It is used in nutrition science to determine the caloric value of foods, i.e., how much energy the food will release when metabolized.
⚗️ 2. Principle of Bomb Calorimeter
1️⃣ The principle is based on first law of thermodynamics – energy conservation:
“The heat released by the combustion of the sample is equal to the heat absorbed by the surrounding water and calorimeter components.”
2️⃣ The sample is burned in excess oxygen in a sealed metal container (called a “bomb”), and the heat generated raises the temperature of the surrounding known mass of water.
3️⃣ This temperature change is then used to calculate the caloric value (in kilocalories or joules) of the substance.
🧪 3. Components / Parts of Bomb Calorimeter
🔸 1. Bomb (Combustion Chamber):
It is a strong steel vessel that can withstand high pressure. The sample is placed here for combustion.
🔸 2. Oxygen Supply:
Pure oxygen is supplied into the bomb to support complete combustion.
🔸 3. Ignition Coil (Fuse Wire):
A small electric wire ignites the sample using an electric spark.
🔸 4. Calorimeter Vessel (Bucket):
The bomb is immersed in a container filled with a known quantity of water that absorbs the released heat.
🔸 5. Stirrer:
Continuously stirs the water to distribute heat evenly.
🔸 6. Thermometer / Temperature Sensor:
Measures the rise in water temperature accurately.
🔸 7. Insulated Jacket / Outer Container:
Minimizes heat loss to the environment, improving accuracy.
🔸 8. Electronic Unit / Control Panel:
Used for controlling ignition and reading data such as temperature change.
🧮 4. Working Procedure of Bomb Calorimeter
1️⃣ A known weight of dry sample (usually 1 gram of food or chemical) is placed in a crucible inside the bomb.
2️⃣ The bomb is filled with oxygen at high pressure (~25–30 atm).
3️⃣ The bomb is sealed and placed in the calorimeter bucket containing a measured quantity of water.
4️⃣ The ignition system is activated, causing the sample to burn completely in oxygen.
5️⃣ The heat released during combustion is absorbed by the water and metal components of the calorimeter.
6️⃣ The temperature rise (ΔT) is recorded, and the total energy released is calculated using the formula:
🔸 Q = (W × S) × ΔT
Where:
- Q = heat released (in calories or joules)
- W = mass of water
- S = specific heat of water (usually 1 cal/g/°C)
- ΔT = change in temperature
7️⃣ The result gives the gross calorific value of the substance in calories/gram or joules/gram.
🔬 5. Applications in Nursing and Nutrition
🔹 It is used to determine the caloric value of macronutrients –
- Carbohydrates ≈ 4 kcal/g
- Proteins ≈ 4 kcal/g
- Fats ≈ 9 kcal/g
🔹 It helps in formulating balanced diets by understanding the energy contribution of different foods.
🔹 It is useful in clinical dietetics, hospital nutrition services, and research on energy metabolism.
🔹 It is used in laboratories to test caloric value of enteral and parenteral nutrition solutions.
🧾 6. Advantages of Bomb Calorimeter
1️⃣ It provides accurate and reproducible results for energy content.
2️⃣ It can be used for a wide variety of substances: solids, liquids, or even fuels.
3️⃣ It helps in standardization of food labels for calories.
4️⃣ It enables scientific diet planning for patients with special energy requirements.
⚠️ 7. Limitations of Bomb Calorimeter
1️⃣ It measures gross energy, not metabolizable energy (the actual energy used by the human body).
2️⃣ The body cannot use 100% of the energy released from combustion (e.g., nitrogen in protein is excreted).
3️⃣ The process is laboratory-based and not applicable in routine bedside nursing.
4️⃣ Requires trained personnel, costly equipment, and controlled environment.
🩺 8. Nursing Relevance
- Nurses working in clinical nutrition, ICU, or TPN (Total Parenteral Nutrition) units must understand the energy content of prescribed feeds.
- They must collaborate with dietitians to ensure the patient receives the correct caloric intake based on energy expenditure.
- Nurses should educate patients on nutrient density vs caloric value when planning for weight management or chronic disease diets.
- Understanding bomb calorimetry helps in accurate food energy estimation, critical in diabetes, malnutrition, and obesity care.
2.Canning.
📘 1. Definition of Canning
🔹 Canning is a food preservation technique in which food is placed in airtight containers (like metal cans or glass jars) and heat-processed to destroy microorganisms and enzymes that cause spoilage.
🔹 It helps in extending the shelf life of food for months or even years, without the need for refrigeration or freezing.
🧪 2. Principle of Canning
1️⃣ It is based on the principle of sterilization – destroying all microorganisms including spores through heat.
2️⃣ It uses high temperature and airtight sealing, so no microorganisms can re-enter after processing.
3️⃣ The oxygen inside the container is removed or neutralized, which inhibits bacterial growth, especially of aerobic spoilage organisms.
4️⃣ Most canning methods involve temperature around 100°C to 121°C, depending on the type of food.
🧰 3. Materials and Equipment Used in Canning
🔹 Glass jars (mason jars), metal cans (tin-plated), sealing lids.
🔹 Pressure canner or boiling water canner.
🔹 Thermometer, tongs, ladle, funnel, and timer.
🔹 Preservatives, brine or syrup solution depending on food type.
🔄 4. Steps / Procedure of Canning
🟩 Step 1: Selection and Preparation of Food
- Choose fresh, high-quality fruits or vegetables.
- Wash, peel, cut, and blanch as needed.
🟩 Step 2: Filling Containers
- Place prepared food in sterilized jars or cans, leaving proper headspace (usually ½ to 1 inch).
🟩 Step 3: Adding Liquid or Syrup
- Add brine (salt solution), sugar syrup, or boiling water as per recipe to cover the food.
🟩 Step 4: Removing Air Bubbles
- Use a spatula to remove trapped air and ensure even heat distribution.
🟩 Step 5: Sealing the Containers
- Wipe rims clean, place lids tightly (but not overly tight).
🟩 Step 6: Processing the Jars
- Process in a water bath (for acidic foods) or pressure canner (for low-acid foods).
- Boil or steam for required time and temperature.
🟩 Step 7: Cooling and Storage
- Allow to cool undisturbed.
- Check seal integrity (lids should not flex).
- Label and store in a cool, dry, and dark place.
🍓 5. Types of Canning Methods
✅ A. Water-Bath Canning
- Used for acidic foods (pH below 4.6): fruits, pickles, jams.
- Temperature: ~100°C
- Simpler and used at home level.
✅ B. Pressure Canning
- Used for low-acid foods (pH above 4.6): vegetables, meat, poultry.
- Temperature: ~116–121°C
- Kills Clostridium botulinum spores.
⚠️ 6. Safety Concerns in Canning
🔸 Improper canning can lead to botulism, a severe form of food poisoning.
🔸 Always follow tested canning recipes from reputable sources.
🔸 Ensure correct time, temperature, and pressure are used.
🔸 Avoid using rusted cans, broken seals, or bulging containers.
✅ 7. Advantages of Canning
1️⃣ Preserves food for long durations (1–2 years shelf life).
2️⃣ Maintains nutritional value, flavor, and color.
3️⃣ Reduces food waste and allows seasonal food availability year-round.
4️⃣ Useful during emergencies, pandemics, disasters, or long journeys.
5️⃣ Home canning supports self-sufficiency and food security.
❌ 8. Disadvantages of Canning
1️⃣ It requires special equipment and proper knowledge.
2️⃣ Risk of botulism if low-acid food is not pressure canned.
3️⃣ May cause loss of heat-sensitive nutrients like Vitamin C and some B-complex vitamins.
4️⃣ Canned food may contain added sugar or salt, not ideal for diabetics or hypertensive patients.
5️⃣ Metal cans may react with acidic food, leading to metallic taste or leaching.
🩺 9. Importance of Canning in Nursing and Public Health
1️⃣ Canned foods can be an important nutritional resource in rural hospitals, relief camps, or low-resource settings.
2️⃣ Nurses in community health must educate people on safe home-canning practices to prevent foodborne illnesses.
3️⃣ It helps provide nutrient-rich, affordable options to undernourished populations where fresh food isn’t always accessible.
4️⃣ Canned therapeutic foods (like high-protein meat or beans) can be part of nutrition rehabilitation programs.
5️⃣ Nurses in disaster preparedness or emergency nutrition roles should be trained to store and distribute canned food safely.
3.Amino acids.
📘 1. Definition of Amino Acids
🔹 Amino acids are the basic building blocks of proteins, composed of carbon (C), hydrogen (H), oxygen (O), nitrogen (N) and sometimes sulfur (S).
🔹 Each amino acid contains:
- One amino group (–NH₂)
- One carboxyl group (–COOH)
- One hydrogen atom (H)
- One side chain (R-group) that is unique to each amino acid
🔹 These amino acids link together via peptide bonds to form polypeptides or proteins, which are crucial for all biological functions in the body.
🧪 2. General Structure of Amino Acid
Each amino acid has the following basic structure:
H₂N – CH(R) – COOH
- NH₂ = Amino group
- COOH = Carboxyl group
- R = Side chain (determines the nature and function of amino acid)
🔸 Example: Glycine (simplest amino acid):
H₂N – CH₂ – COOH
🔢 3. Number of Amino Acids in Human Body
- There are 20 standard amino acids used in human protein synthesis.
- Some texts include non-standard amino acids, such as selenocysteine and hydroxyproline.
🧩 4. Classification of Amino Acids
🟩 A. Based on Nutritional Requirement
🔹 1. Essential Amino Acids (Cannot be synthesized by the body):
Must be obtained from diet.
✔️ Examples:
- Leucine
- Isoleucine
- Valine
- Lysine
- Methionine
- Phenylalanine
- Threonine
- Tryptophan
- Histidine (essential in infants)
🔹 2. Non-Essential Amino Acids (Can be synthesized in the body):
✔️ Examples:
- Alanine
- Glycine
- Glutamic acid
- Asparagine
- Aspartic acid
- Proline
- Serine
- Cysteine
- Tyrosine
🟩 B. Based on Side Chain Properties (Polarity/Charge)
🔸 1. Non-polar (hydrophobic):
E.g., Alanine, Valine, Leucine
🔸 2. Polar (hydrophilic):
E.g., Serine, Threonine, Glutamine
🔸 3. Acidic (negatively charged):
E.g., Aspartic acid, Glutamic acid
🔸 4. Basic (positively charged):
E.g., Lysine, Arginine, Histidine
🧠 5. Functions of Amino Acids in the Human Body
1️⃣ It is used to synthesize body proteins, including enzymes, hormones, muscle tissue, skin, and hair.
2️⃣ It plays a role in immune function, as many immune cells and antibodies are protein-based.
3️⃣ It acts as precursors for neurotransmitters, e.g., Tryptophan → Serotonin; Tyrosine → Dopamine.
4️⃣ It is involved in wound healing and tissue repair, especially after surgery, injury, or illness.
5️⃣ It is essential for transport and storage of nutrients, such as hemoglobin carrying oxygen.
6️⃣ It provides energy during starvation or intense exercise when glucose is insufficient.
🧬 6. Peptide Bond and Protein Formation
🔹 When amino acids join, the carboxyl group of one reacts with the amino group of another, releasing a water molecule and forming a peptide bond.
🔹 Multiple amino acids linked together form:
- Dipeptides (2 amino acids)
- Tripeptides (3 amino acids)
- Polypeptides (many amino acids → proteins)
⚕️ 7. Clinical Importance of Amino Acids
1️⃣ Deficiency of essential amino acids leads to protein energy malnutrition (PEM) such as Kwashiorkor or Marasmus.
2️⃣ Branched Chain Amino Acids (BCAAs) are vital in liver disease management and muscle recovery in ICU patients.
3️⃣ Aromatic amino acid buildup occurs in Phenylketonuria (PKU) – a genetic disorder where phenylalanine cannot be broken down.
4️⃣ Some amino acids (e.g., glutamine, arginine) are used as medical nutrition therapy in burns, sepsis, or trauma.
5️⃣ Taurine, glycine, and tryptophan are used in pediatric formulas and in mental health therapy.
🩺 8. Nursing Relevance and Role
1️⃣ It is the nurse’s responsibility to monitor adequate protein intake, especially in pregnant women, children, and postoperative patients.
2️⃣ Nurses must understand IV amino acid therapy in TPN (Total Parenteral Nutrition) for critically ill patients.
3️⃣ It is important to observe for signs of deficiency: edema, fatigue, muscle wasting, slow wound healing.
4️⃣ Nurses should educate patients about dietary sources of complete proteins (milk, eggs, meat) and incomplete ones (pulses, cereals).
5️⃣ Nurses should help assess and implement high-protein diets for malnourished or catabolic state patients.
🍗 9. Dietary Sources of Amino Acids (Proteins)
🔹 Animal sources (complete proteins):
Eggs, milk, chicken, fish, red meat, cheese
🔹 Plant sources (some are incomplete):
Lentils, beans, soy, nuts, seeds, whole grains, tofu
4.Nutritional anthropometry.
📘 1. Definition
🔹 Nutritional anthropometry is the systematic measurement of the physical dimensions and composition of the human body to assess an individual’s nutritional status, growth, and development.
🔹 It includes measurements like height, weight, mid-upper arm circumference (MUAC), skinfold thickness, etc., and is commonly used in clinical settings, community health surveys, and growth monitoring of children.
🎯 2. Objectives of Nutritional Anthropometry
1️⃣ To assess the growth and development of infants, children, and adolescents.
2️⃣ To detect malnutrition (under-nutrition and over-nutrition) in individuals and communities.
3️⃣ To monitor nutritional interventions, treatment response, and public health programs.
4️⃣ To help in diagnosis and surveillance of nutrition-related disorders.
5️⃣ To generate reference data and growth charts for comparison with standard populations.
🧪 3. Common Anthropometric Measurements
✅ A. Weight
- It is used to detect acute changes in nutritional status.
- Sudden weight loss may indicate malnutrition, chronic illness, or dehydration.
✅ B. Height/Length
- Used for calculating height-for-age (to detect stunting in children).
- Measured standing in adults or recumbent (lying down) in infants.
✅ C. Mid-Upper Arm Circumference (MUAC)
- Measured at the midpoint between shoulder and elbow.
- It is used for rapid screening of acute malnutrition, especially in children aged 6 months to 5 years.
✅ D. Head Circumference
- Important in infants under 2 years to assess brain growth.
- Abnormal values may indicate microcephaly or hydrocephalus.
✅ E. Chest Circumference
- Compared with head circumference in newborns to assess normal growth.
- Used in field-based growth monitoring.
✅ F. Skinfold Thickness (Triceps, Subscapular)
- Measures subcutaneous fat and gives an estimate of body fat percentage.
- Requires a skinfold caliper.
✅ G. Body Mass Index (BMI)
- Formula: BMI = Weight (kg) / Height (m²)
- Used to classify underweight, normal, overweight, and obesity in adults.
📊 4. Anthropometric Indices and Interpretation
| Index | Used for | Indicator of |
|---|---|---|
| Weight-for-age | Children | Underweight |
| Height-for-age | Children | Stunting (chronic malnutrition) |
| Weight-for-height | Children | Wasting (acute malnutrition) |
| BMI (adults) | Adults | Underweight/Overweight/Obesity |
| MUAC (<12.5 cm) | Children (6 months–5 yrs) | Severe Acute Malnutrition (SAM) |
🩺 5. Tools Used in Nutritional Anthropometry
🔹 Weighing scale (digital or spring)
🔹 Infantometer or measuring board
🔹 Stadiometer for standing height
🔹 Non-stretchable measuring tape
🔹 Skinfold calipers (Harpenden or Lange)
🔹 MUAC tapes (color-coded for field screening)
🏥 6. Clinical & Public Health Significance
1️⃣ It helps in identifying children at risk of malnutrition or growth failure.
2️⃣ It supports early diagnosis of undernutrition and overnutrition-related diseases such as kwashiorkor, marasmus, or obesity.
3️⃣ It is used in hospital nutrition assessment, especially for ICU patients, pregnant women, and elderly.
4️⃣ It plays a major role in nutrition surveillance programs like ICDS, RCH, and POSHAN Abhiyaan.
5️⃣ It guides policy-makers in designing targeted feeding programs such as Mid-Day Meals or Vitamin A supplementation.
👩⚕️ 7. Role of Nurse in Nutritional Anthropometry
1️⃣ It is the nurse’s role to accurately measure, record, and interpret anthropometric data in clinics, schools, and community settings.
2️⃣ Nurses must use proper technique and tools to prevent measurement errors.
3️⃣ They must identify high-risk individuals based on anthropometric indices and refer for further assessment or intervention.
4️⃣ It is essential for nurses to educate families and mothers on normal growth patterns and nutritional needs of children.
5️⃣ Nurses should help in maintaining growth monitoring charts and ensuring follow-up for malnourished children.
6️⃣ In field visits, nurses use MUAC tape and growth charts to screen and counsel families on child nutrition.
✅ 8. Advantages of Nutritional Anthropometry
1️⃣ It is non-invasive, low-cost, and repeatable.
2️⃣ Provides a quantitative and objective assessment of nutritional status.
3️⃣ Can be used on large scale in surveys and public health monitoring.
4️⃣ Allows early detection of nutrition problems before clinical symptoms arise.
5️⃣ Helps in tracking progress of nutritional therapy and growth.
❌ 9. Limitations of Nutritional Anthropometry
1️⃣ It does not assess micronutrient deficiencies (e.g., iron, iodine).
2️⃣ It can be affected by edema, dehydration, or measurement errors.
3️⃣ Standard growth charts may not apply to all populations due to genetic and ethnic differences.
4️⃣ Cannot directly measure body composition (fat vs lean mass) without additional tools.
IIl.Short answers on:(5 x 2 = 10)
1.Give two functions of carbohydrate.
1️⃣ Primary energy source:
Carbohydrates are the main source of energy for the body; they provide 4 kcal per gram and are especially essential for the brain and muscles during activity.
2️⃣ Protein sparing action:
When adequate carbohydrates are consumed, the body spares proteins from being used for energy, allowing them to be used for growth and repair.
2.Sources of Iron.
🔹 Animal sources (heme iron):
- Liver, red meat, chicken, fish, egg yolk
🔹 Plant sources (non-heme iron):
- Green leafy vegetables (like spinach), legumes, jaggery, whole grains, dry fruits (raisins, apricots), fortified cereals
- Iron from animal sources is better absorbed than from plant sources. Vitamin C enhances iron absorption.
3.Define BMI.
BMI or Body Mass Index is a numerical value derived from a person’s height and weight that is used to assess if they are underweight, normal, overweight, or obese.
🔸 Formula:
BMI = Weight (kg) / Height (m²)
🔸 Example Interpretation:
- <18.5 = Underweight
- 18.5–24.9 = Normal
- 25–29.9 = Overweight
- ≥30 = Obese
4.What is Trans Fat?
🔹 Trans fats are a type of unsaturated fat that have been chemically modified by hydrogenation, often found in processed and fried foods.
🔹 They increase bad cholesterol (LDL) and lower good cholesterol (HDL), significantly raising the risk of heart disease, stroke, and diabetes.
🔹 Common sources: Packaged snacks, margarine, bakery items, fast foods.
5.Scurvy.
🔹 Scurvy is a disease caused by a deficiency of Vitamin C (Ascorbic acid).
🔹 Symptoms include:
- Bleeding gums
- Loose teeth
- Poor wound healing
- Fatigue
- Swollen joints
🔹 Common in:
People with poor fruit and vegetable intake, alcoholics, elderly, or those with malabsorption disorders.
SECTION-B (BIOCHEMISTRY)
1.Elaborate on:(1 x 15 = 15)
1.Glycolysis add a note on its Bio-energetics.
📘 1. Definition of Glycolysis
Glycolysis is defined as the metabolic breakdown of one molecule of glucose (6-carbon compound) into two molecules of pyruvate (3-carbon compound) through a series of enzymatically catalyzed reactions. This process occurs in the cytoplasm of all living cells and is anaerobic in nature, meaning it does not require oxygen. It is the first and essential step of cellular respiration, serving as a universal pathway for energy generation.
📍 2. Location of Glycolysis
Glycolysis takes place in the cytoplasm of both prokaryotic and eukaryotic cells. It is the only energy-yielding pathway that can function in cells lacking mitochondria, such as red blood cells.
⚗️ 3. Phases of Glycolysis
Glycolysis occurs in two distinct phases – the energy investment phase and the energy payoff phase, comprising a total of ten enzymatic steps.
🔹 In the energy investment phase (also known as preparatory phase), two molecules of ATP are used to phosphorylate glucose and convert it into Fructose-1,6-bisphosphate, which is then split into two 3-carbon molecules: Glyceraldehyde-3-phosphate (G3P) and Dihydroxyacetone phosphate (DHAP). DHAP is isomerized into another molecule of G3P, so the pathway continues with two molecules of G3P.
🔹 In the energy payoff phase, each G3P molecule undergoes further conversion to generate ATP and NADH. Through a series of reactions, the final product pyruvate is formed, along with the production of ATP and NADH.
🧪 4. End Products of Glycolysis
At the end of glycolysis, from one molecule of glucose, the process yields two molecules of pyruvate, two molecules of NADH, and a net gain of two molecules of ATP. Additionally, two molecules of water and two hydrogen ions are released. Since two ATP molecules are consumed in the early steps and four are produced later, the net gain of ATP is two.
🔬 5. Bioenergetics of Glycolysis
The bioenergetics of glycolysis deals with the energy balance and ATP production during the process. Although four ATP molecules are produced in the later steps, two ATP molecules are consumed in the beginning for phosphorylation of glucose and fructose-6-phosphate. This results in a net gain of two ATP molecules per molecule of glucose.
Additionally, two molecules of NADH are produced, which can yield approximately 5 to 6 ATP molecules when transferred to the electron transport chain under aerobic conditions. Therefore, the total ATP yield from glycolysis can be estimated as seven to eight ATP molecules aerobically, but only two ATPs anaerobically when NADH is not used for oxidative phosphorylation.
🧫 6. Fate of Pyruvate
The fate of pyruvate depends on the availability of oxygen in the cell:
✅ Under aerobic conditions, pyruvate is transported into the mitochondria, where it is converted to Acetyl-CoA and enters the Krebs cycle (Citric Acid Cycle) for further oxidation, leading to the production of additional ATP, CO₂, and water.
❌ Under anaerobic conditions, such as in active skeletal muscles, red blood cells, or oxygen-deprived tissues, pyruvate is reduced to lactic acid by the enzyme lactate dehydrogenase. This allows for the regeneration of NAD⁺ from NADH, which is essential for the continuation of glycolysis under anaerobic conditions.
🧬 7. Important Enzymes Involved
Several key enzymes control the steps of glycolysis. Among these, the most important include Hexokinase, which phosphorylates glucose in the first step; Phosphofructokinase-1 (PFK-1), which is the rate-limiting enzyme and controls the committed step; and Pyruvate kinase, which catalyzes the final step leading to pyruvate formation and ATP release.
⚡ 8. Significance and Functions of Glycolysis
Glycolysis serves as a universal energy-producing process, especially vital for cells without mitochondria. It provides quick energy in the form of ATP and biosynthetic intermediates like glyceraldehyde-3-phosphate and 3-phosphoglycerate, which are used in synthesis of nucleotides, amino acids, and fatty acids. It is particularly crucial during intense muscular activity and in tissues with low oxygen supply.
It also plays an essential role in glucose homeostasis and is involved in several clinical conditions such as cancer metabolism, diabetes, and inborn errors of metabolism like pyruvate kinase deficiency.
🩺 9. Clinical and Nursing Significance
Glycolysis has wide relevance in clinical practice and nursing care. In critically ill patients, hypoxia leads to a shift toward anaerobic glycolysis, resulting in lactic acid accumulation and metabolic acidosis, which nurses should monitor through arterial blood gas (ABG) analysis.
In cancer care, glycolytic activity is often increased in tumor cells—a phenomenon known as the Warburg effect—and is utilized in imaging techniques like PET scans. In nutritional therapy and TPN (Total Parenteral Nutrition), understanding glycolysis helps in calculating energy requirements. In anemia management, defects in enzymes like pyruvate kinase affecting glycolysis may lead to hemolytic anemia.
II. Write notes on: (1 x 5 = 5)
1.Glycogen storage disease.
📘 1. Definition
Glycogen Storage Diseases (GSDs) are a group of inherited metabolic disorders that result from deficiencies or defects in enzymes involved in glycogen synthesis or glycogen breakdown (glycogenesis or glycogenolysis).
Due to these enzyme deficiencies, glycogen either accumulates in tissues in an abnormal form or cannot be mobilized properly for energy, especially in liver, muscles, and heart, leading to organ dysfunction and metabolic complications.
🧬 2. Pathophysiology
In a healthy body, glycogen acts as a storage form of glucose and is broken down when the body needs energy, especially during fasting or exercise.
In GSD:
- The deficiency of specific enzymes prevents normal breakdown (glycogenolysis) or formation (glycogenesis) of glycogen.
- As a result, glycogen accumulates in tissues or is improperly formed.
- This leads to organ enlargement, hypoglycemia, muscle weakness, and other metabolic disturbances depending on the type of GSD.
🔢 3. Classification / Types of Glycogen Storage Diseases
There are more than 12 types, but the most common include the following:
🔹 Type I (Von Gierke’s Disease):
- Enzyme Defect: Glucose-6-phosphatase
- Organs Affected: Liver, kidney
- Features: Severe fasting hypoglycemia, lactic acidosis, hepatomegaly, growth retardation
🔹 Type II (Pompe’s Disease):
- Enzyme Defect: Lysosomal acid alpha-glucosidase
- Organs Affected: Heart, muscle
- Features: Cardiomegaly, muscle weakness, respiratory failure (infantile fatal form)
🔹 Type III (Cori’s or Forbes Disease):
- Enzyme Defect: Debranching enzyme
- Organs Affected: Liver, muscle
- Features: Milder hypoglycemia, hepatomegaly, growth delay
🔹 Type IV (Andersen’s Disease):
- Enzyme Defect: Branching enzyme
- Organs Affected: Liver, heart, muscle
- Features: Cirrhosis, liver failure, failure to thrive
🔹 Type V (McArdle’s Disease):
- Enzyme Defect: Muscle phosphorylase
- Organs Affected: Skeletal muscles
- Features: Muscle cramps, exercise intolerance, myoglobinuria
🔹 Type VI (Hers’ Disease):
- Enzyme Defect: Liver phosphorylase
- Organs Affected: Liver
- Features: Mild hypoglycemia, hepatomegaly
🧪 4. Causes and Risk Factors
1️⃣ The primary cause is genetic mutation in the gene encoding a specific enzyme in glycogen metabolism.
2️⃣ Most types of GSD are autosomal recessive, meaning both parents must pass on the defective gene.
3️⃣ Family history of metabolic or liver disorders increases risk.
4️⃣ Consanguineous marriages may raise the risk in communities with limited genetic diversity.
⚠️ 5. Clinical Features of GSD
The symptoms vary depending on the type of enzyme deficiency and organ involved, but may include:
🔹 Hepatomegaly (enlarged liver)
🔹 Severe hypoglycemia during fasting
🔹 Muscle weakness and cramps (especially in exercise-related types)
🔹 Growth retardation or failure to thrive in infants and children
🔹 Enlarged kidneys (Type I)
🔹 Cardiomegaly in infantile Pompe disease
🔹 Lactic acidosis, ketosis, and hyperlipidemia (Type I)
🔹 Fatigue and intolerance to exercise
🧫 6. Diagnostic Evaluation
1️⃣ Blood glucose levels – low during fasting
2️⃣ Liver function tests – elevated enzymes, hepatomegaly
3️⃣ Lactic acid, uric acid, triglyceride levels – may be elevated
4️⃣ Urinalysis – may show ketones or myoglobin (in McArdle’s)
5️⃣ Muscle or liver biopsy – shows abnormal glycogen accumulation
6️⃣ Genetic testing – confirms the specific enzyme deficiency
7️⃣ Enzyme activity assays – in fibroblasts, liver, or muscle tissue
🧾 7. Treatment and Management
There is no permanent cure for most GSDs, but management is aimed at:
🔹 Dietary Modification
- Frequent small meals with high complex carbohydrate content
- Uncooked cornstarch is used in Type I to provide slow-release glucose
- Avoidance of fasting and high-protein diet in muscle types
- Supplemental vitamins, minerals, and glucose as needed
🔹 Supportive Medical Care
- Monitoring blood sugar and lactate levels
- Use of allopurinol for hyperuricemia
- Treat infections promptly
- Physical therapy for muscle weakness
🔹 Advanced Therapy
- Liver transplantation in severe cases (especially Type I and IV)
- Enzyme replacement therapy (ERT) in Pompe’s disease (Type II)
🩺 8. Nursing Responsibilities in GSD Care
1️⃣ It is essential for the nurse to monitor blood glucose levels regularly, especially during illness or fasting.
2️⃣ The nurse should educate caregivers or parents about the need for frequent feeding schedules, including nighttime feeding.
3️⃣ Nurses must ensure the administration of uncooked cornstarch therapy (for Type I), which helps prevent fasting hypoglycemia.
4️⃣ The nurse should monitor for signs of metabolic acidosis, such as deep breathing, vomiting, or altered sensorium.
5️⃣ It is important to assist with growth monitoring, record weight and height regularly, and report any developmental delays.
6️⃣ Nurses should help in emergency preparedness for managing hypoglycemic episodes, including administration of IV glucose when required.
7️⃣ It is the nurse’s duty to coordinate multidisciplinary care involving pediatricians, dietitians, physiotherapists, and genetic counselors.
III. Short answers on: (5 x2=10)
1.Power house of the cell.
The mitochondria is called the powerhouse of the cell because it is the site where aerobic respiration occurs and ATP (adenosine triphosphate) – the energy currency of the cell – is produced. It converts glucose and oxygen into usable cellular energy.
2.Essential amino acids.
Essential amino acids are those which cannot be synthesized by the human body and must be obtained from the diet.
🔹 Examples of essential amino acids:
- Leucine
- Isoleucine
- Valine
- Lysine
- Methionine
- Phenylalanine
- Threonine
- Tryptophan
- Histidine (essential during infancy)
These are crucial for protein synthesis, tissue repair, and enzyme formation.
3.Define coenzyme.
A coenzyme is a non-protein organic molecule that binds with an enzyme and is required for the enzyme’s biological activity. It acts as a helper molecule that assists in the catalysis of biochemical reactions.
🔸 Example:
NAD⁺ (Nicotinamide adenine dinucleotide) is a coenzyme for dehydrogenase enzymes involved in energy metabolism.
4.GTT.
GTT (Glucose Tolerance Test) is a diagnostic test used to assess the body’s ability to metabolize glucose and detect conditions like diabetes mellitus, gestational diabetes, and insulin resistance.
🔹 In this test, the patient is given a measured oral dose of glucose (usually 75g), and blood glucose levels are checked at fasting, 30 minutes, 1 hour, 2 hours, and sometimes 3 hours after ingestion.
🔹 It helps evaluate how efficiently glucose is cleared from the blood, and abnormal results may indicate impaired glucose tolerance (IGT) or diabetes.
🔹 Commonly used in:
- Screening for gestational diabetes in pregnancy
- Confirming type 2 diabetes diagnosis
5.List any four macro-minerals
Macrominerals are minerals that are required by the body in larger amounts (more than 100 mg/day) for normal physiological functions.
🔸 Four examples include:
1️⃣ Calcium – Needed for bone and teeth formation, muscle contraction, and nerve transmission.
2️⃣ Phosphorus – Important for ATP production, bone structure, and cell membrane function.
3️⃣ Magnesium – Involved in enzyme activation, nerve function, and muscle relaxation.
4️⃣ Sodium – Essential for fluid balance, nerve impulse transmission, and muscle function.
Other macrominerals include potassium, chloride, and sulfur.
