B.SC. FEBRUARY 2019 FIRTS YEAR NURSING FOUNDATION-PAPER SOLUTION NO.7
PAPER SOLUTION NO.7 – FEBRUARY-2019
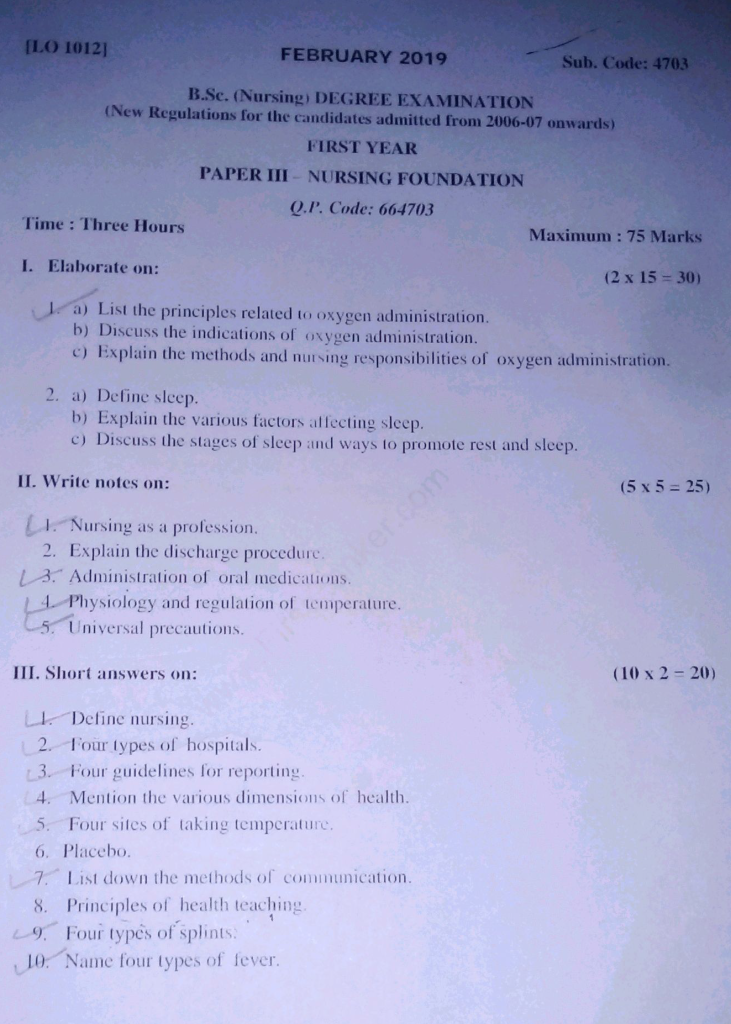
1.Elaborate on:(2×15=30)
a) List the principles related to oxygen administration.
Answer:-
✅ Principles Related to Oxygen Administration
🔸 1. Oxygen is a drug and requires a prescription in most settings
→ It is essential to understand that oxygen is considered a therapeutic agent and should be administered only under medical advice or prescription, except in emergency situations where life support is required.
🔸 2. The correct method and device of oxygen delivery must be selected according to patient need
→ It is important to choose the appropriate oxygen delivery system such as nasal cannula, face mask, non-rebreather mask, or mechanical ventilator depending on the patient’s respiratory status and oxygen requirement.
🔸 3. Humidification is important when oxygen is delivered at high flow rates
→ It is necessary to humidify oxygen, especially when delivered at flow rates above 4 liters per minute, to prevent drying of mucous membranes and avoid airway irritation.
🔸 4. Oxygen supports combustion and must be handled with safety precautions
→ It is essential to follow strict safety measures because oxygen accelerates fire; sources of ignition such as open flames, electrical equipment, and smoking must be avoided in areas where oxygen is administered.
🔸 5. The concentration of oxygen must be carefully monitored and titrated
→ It is important to avoid both hypoxia and oxygen toxicity by continuously monitoring oxygen saturation (SpO₂) and adjusting the flow rate or concentration as per the patient’s response.
🔸 6. Patient’s response to oxygen therapy should be continuously evaluated
→ It is necessary to assess clinical signs like respiratory rate, level of consciousness, color of skin, and pulse oximetry to evaluate whether oxygen therapy is effective or needs adjustment.
🔸 7. Oxygen equipment should be kept clean and in working condition
→ It is vital to regularly check and maintain oxygen cylinders, flow meters, humidifiers, and tubing to ensure proper functioning and prevent contamination or infection.
🔸 8. Proper positioning enhances oxygenation
→ It is advisable to place the patient in a semi-Fowler’s or high Fowler’s position, whenever possible, as this helps expand the lungs and promotes better oxygen exchange.
🔸 9. Documentation of oxygen therapy is mandatory in the patient record
→ It is a professional responsibility to accurately document the type of device used, flow rate, duration, patient’s response, and any adverse effects in the nursing notes or medical record.
🔸 10. Psychological support should be provided to reduce anxiety
→ It is important to explain the purpose and process of oxygen therapy to reduce fear or anxiety, which can otherwise increase oxygen demand due to stress.
🔸 11. Educating patients and caregivers is necessary for home oxygen use
→ In case of home oxygen therapy, it is essential to teach patients and their families about correct usage, maintenance, and safety measures to avoid mishandling and complications.
✅ In brief, the key principles emphasize:
- Safety
- Accuracy in dosage
- Close monitoring
- Proper equipment usage
- Patient-centered care
b) Discuss the indications of oxygen administration.
Oxygen is a vital element required for cellular metabolism and tissue survival. Oxygen administration becomes necessary when the body is unable to maintain adequate oxygen levels either due to respiratory, cardiovascular, hematological, or environmental causes. The following are the detailed clinical situations where oxygen therapy is indicated:
🔹 1. Hypoxemia (Low Arterial Oxygen Levels)
→ Oxygen therapy is strongly indicated when there is a decrease in partial pressure of oxygen in arterial blood (PaO₂ < 60 mmHg) or oxygen saturation (SpO₂ < 90%) as detected by ABG analysis or pulse oximetry.
→ It is essential to restore adequate oxygenation in hypoxemia to prevent tissue hypoxia, metabolic acidosis, brain damage, and multiple organ failure.
🔹 2. Respiratory Distress or Respiratory Failure
→ It is indicated in patients who show visible signs of labored breathing such as nasal flaring, intercostal or suprasternal retractions, use of accessory muscles, cyanosis, and shallow or rapid respirations.
→ In both acute respiratory failure (type I and II), oxygen supports gas exchange and relieves symptoms of breathlessness and fatigue.
🔹 3. Chronic Obstructive Pulmonary Disease (COPD)
→ In COPD patients, particularly during acute exacerbation, oxygen helps in managing chronic hypoxemia and reducing the workload on the heart and lungs.
→ Low-flow oxygen (usually 1–2 L/min via nasal cannula) is used cautiously to avoid suppression of respiratory drive in CO₂ retainers.
→ Long-term oxygen therapy (LTOT) is often prescribed for home use to improve survival and enhance quality of life.
🔹 4. Acute Myocardial Infarction and Other Cardiac Conditions
→ During a heart attack or myocardial ischemia, oxygen is indicated to improve myocardial oxygen supply and reduce infarct size.
→ It is also used in congestive heart failure (CHF), pulmonary edema, and cardiogenic shock where oxygen delivery to tissues is compromised due to poor cardiac output.
🔹 5. Post-operative Period and Recovery from Anesthesia
→ After surgery, especially under general anesthesia, patients may have hypoventilation or reduced lung expansion (atelectasis), which can cause hypoxia.
→ Supplemental oxygen is given to support tissue oxygenation until the patient is fully awake, mobile, and breathing normally.
🔹 6. Shock (Hypovolemic, Septic, or Cardiogenic)
→ In all types of shock, tissue perfusion and oxygen delivery are impaired due to decreased circulating blood volume or cardiac pump failure.
→ Oxygen therapy helps maintain aerobic metabolism and prevents anaerobic cellular damage during resuscitation.
🔹 7. Severe Anemia or Major Hemorrhage
→ When hemoglobin levels are critically low, oxygen administration can increase the dissolved oxygen content in plasma to partially compensate for reduced oxygen-carrying capacity.
→ It helps support vital organ function until blood transfusion or definitive treatment is provided.
🔹 8. Carbon Monoxide (CO) Poisoning
→ CO binds to hemoglobin 200–250 times more readily than oxygen, forming carboxyhemoglobin and impairing oxygen delivery.
→ High-concentration oxygen or hyperbaric oxygen therapy is indicated to displace CO and reduce half-life of carboxyhemoglobin, preventing neurological damage.
🔹 9. Respiratory Conditions in Neonates and Children
→ It is indicated in newborns with respiratory distress syndrome (RDS), meconium aspiration, congenital pneumonia, or cyanotic heart defects.
→ Supplemental oxygen helps prevent hypoxic brain injury, acidosis, and complications like persistent pulmonary hypertension of the newborn (PPHN).
🔹 10. During Cardiopulmonary Resuscitation (CPR)
→ Oxygen is vital during cardiac arrest to maintain oxygen supply to the brain and heart.
→ It is administered through bag-valve-mask or advanced airway to increase the success of resuscitation efforts and reduce the risk of hypoxic brain damage.
🔹 11. High Altitude Exposure or Hypobaric Environments
→ At high altitudes, the partial pressure of oxygen in the atmosphere is reduced, leading to acute mountain sickness or high-altitude cerebral/pulmonary edema.
→ Oxygen therapy is provided to correct hypoxia and prevent complications related to altitude illness.
🔹 12. During Sedation, Mechanical Ventilation, or General Anesthesia
→ Oxygen is administered to patients who are sedated or ventilated to prevent hypoxia due to drug-induced respiratory depression or impaired gas exchange.
→ It ensures that critical organs continue to receive oxygen during procedures or ICU management.
c) Explain the methods and nursing responsibilities of oxygen administration.
🌬️ I. METHODS OF OXYGEN ADMINISTRATION
Oxygen can be administered through low-flow or high-flow delivery systems, and the choice depends on the patient’s condition, oxygen demand, and age group. Below are the comprehensive methods used in clinical practice:
🔹 1. Nasal Cannula (Nasal Prongs)
→ It delivers low-flow oxygen (1–6 L/min), providing approximately 24–44% FiO₂.
→ It is suitable for stable patients needing minimal support, including in home care or long-term therapy.
→ It allows patient to eat, talk, and is well-tolerated.
🔹 2. Simple Face Mask
→ It delivers oxygen at 5–10 L/min with FiO₂ of 40–60%.
→ Used in mild to moderate hypoxia or post-operative patients.
→ Not suitable for long-term use due to discomfort and difficulty in speaking or eating.
🔹 3. Partial Rebreather Mask
→ It contains a reservoir bag without one-way valves and delivers 6–10 L/min with 60–80% oxygen.
→ The patient rebreathes some exhaled air, which contains oxygen.
→ It is used in short-term oxygen therapy and emergency care.
🔹 4. Non-Rebreather Mask (NRB)
→ It delivers high-flow oxygen at 10–15 L/min with a concentration of 90–100%.
→ One-way valves prevent rebreathing of exhaled air.
→ Used in critically ill patients like shock, trauma, or carbon monoxide poisoning.
🔹 5. Venturi Mask (Air-Entrainment Mask)
→ It delivers precise oxygen concentrations ranging from 24% to 50% by mixing oxygen with room air using color-coded adaptors.
→ It is ideal for patients with COPD, where excessive oxygen can suppress the respiratory drive.
🔹 6. Oxygen Tent
→ A plastic canopy surrounds the patient’s bed or crib, supplying humidified oxygen.
→ Mainly used in pediatric patients with respiratory infections or croup.
→ Provides a cool environment along with oxygen.
🔹 7. Oxygen Hood (Head Box)
→ A small plastic hood encloses the infant’s head and delivers up to 80–90% oxygen at 5–10 L/min.
→ It is suitable for neonates and infants who require higher FiO₂ but cannot tolerate masks.
🔹 8. Oxygen Capsule or Chamber (Hyperbaric Oxygen Therapy)
→ The patient is placed in a chamber where oxygen is delivered at a pressure higher than atmospheric pressure.
→ Used in gas gangrene, decompression sickness, carbon monoxide poisoning, diabetic ulcers, and radiation injuries.
🔹 9. Tracheostomy Collar or T-Piece
→ Oxygen is delivered directly through a tracheostomy tube in patients who have undergone a tracheostomy.
→ The T-piece provides humidified oxygen without mechanical ventilation.
🔹 10. Bag-Valve-Mask (BVM) Device (Ambu Bag)
→ A manual resuscitation device used to deliver 100% oxygen during CPR or when the patient is apneic or in respiratory failure.
→ Used in emergencies, pre-intubation, or transportation of critical patients.
🔹 11. Mechanical Ventilator
→ A life-support machine used in ICU that delivers oxygen and controls ventilation through an endotracheal or tracheostomy tube.
→ Used for patients with ARDS, coma, neuromuscular disorders, or after major surgery.
👩⚕️ II. NURSING RESPONSIBILITIES IN OXYGEN ADMINISTRATION
🩺 A. Pre-administration Assessment and Monitoring
- The nurse should assess baseline respiratory rate, rhythm, depth, and oxygen saturation (SpO₂).
- It is the nurse’s responsibility to identify signs of hypoxia like cyanosis, restlessness, tachycardia, and altered mental status.
- Evaluate the need and urgency of oxygen therapy and report any signs of acute deterioration.
- Monitor patient’s ABG values if prescribed to determine acid-base balance and oxygen levels.
🔧 B. Selection and Setup of Equipment
- Select the appropriate device (nasal cannula, mask, hood, ventilator, etc.) based on doctor’s order and patient condition.
- Check that all equipment including flowmeter, humidifier, tubing, and connectors are clean, functional, and leak-free.
- Attach the oxygen source to wall-mounted supply or cylinder using regulator and confirm correct flow rate.
🔒 C. Safety and Fire Precautions
- Post “OXYGEN IN USE – NO SMOKING” sign visibly near the patient’s bed.
- Avoid use of alcohol-based solutions, flammable substances, or electrical appliances near oxygen.
- Ensure that the oxygen cylinder is placed upright and secured in a holder or trolley to prevent tipping.
- Educate the patient and visitors not to smoke or use mobile chargers near the oxygen source.
🗣️ D. Patient Education and Psychological Support
- The nurse must explain the procedure, purpose, and duration of oxygen therapy to reduce anxiety.
- Teach patients how to breathe through the nose and avoid mouth breathing while using a cannula.
- Reassure the patient to encourage cooperation and reduce fear of dependency or breathlessness.
- Instruct family members and caregivers on the safe use of oxygen at home if prescribed for long-term therapy.
📋 E. Documentation and Reporting
- Accurately document the start time, flow rate (in L/min), device used, oxygen concentration (FiO₂), and SpO₂ levels.
- Record the patient’s response to therapy, any discomfort, adverse reactions, or complications.
- Communicate with the physician if the oxygen need increases or if there is no improvement in saturation.
- Maintain daily cylinder logs if using portable oxygen to track usage and replacement.
💧 F. Humidification and Comfort Measures
- Use a humidifier when the oxygen flow rate exceeds 4 L/min to prevent drying of nasal and oral mucosa.
- Perform regular mouth care and keep lips and nostrils moist with non-petroleum-based ointment.
- Check for pressure injuries behind the ears, nose bridge, or cheeks where the device touches skin.
- Encourage fluid intake unless contraindicated to keep respiratory secretions moist and easier to expectorate.
🔄 G. During Oxygen Therapy
- Regularly reassess the patient’s need for continued oxygen therapy and reduce flow rate gradually as ordered.
- Ensure the delivery device stays properly positioned on the patient for optimal oxygen delivery.
- Be alert for signs of oxygen toxicity such as chest pain, visual disturbances, dry cough, and drowsiness, especially during high-concentration therapy.
- Provide bronchodilator or respiratory physiotherapy as ordered to enhance oxygenation.
2. a) Define sleep.
🔹 Sleep is defined as a naturally recurring physiological state of rest for the body and mind, during which consciousness is altered, sensory activity is reduced, voluntary muscles are relaxed, and the body undergoes various restorative processes essential for physical and mental health.
🔹 It is a cyclical process regulated by the circadian rhythm and sleep-wake homeostasis, characterized by two major phases:
- Non-Rapid Eye Movement (NREM) Sleep
- Rapid Eye Movement (REM) Sleep
b) Explain the various factors affecting sleep.
Sleep is a complex physiological process essential for restoration of physical, emotional, and mental health. Several intrinsic and extrinsic factors affect the onset, depth, quality, and duration of sleep. Understanding these factors is crucial for nurses to assess sleep disturbances and implement appropriate nursing care.
🔹 1. Physical Health Conditions
→ It is evident that various acute and chronic physical conditions can interfere with both the ability to fall asleep and the maintenance of uninterrupted sleep.
- It is commonly seen that pain from fractures, arthritis, or post-operative wounds interrupts sleep, especially during NREM stages.
- Dyspnea due to asthma, COPD, or congestive heart failure causes frequent awakenings and shallow sleep.
- Nocturia (frequent urination at night), especially in conditions like diabetes mellitus or prostatic hypertrophy, can disturb deep sleep stages.
- Chronic illnesses like renal failure, cancer, or Parkinson’s disease alter neurochemical balance, affecting circadian rhythm.
🔹 2. Emotional and Psychological Factors
→ Emotional distress and mental health issues have a profound impact on sleep quality and pattern.
- Anxiety, grief, fear, anger, and sadness are linked to hyperarousal of the central nervous system, causing difficulty in initiating sleep.
- Depression and mood disorders may lead to early morning awakenings, insomnia, or oversleeping (hypersomnia).
- Post-traumatic stress disorder (PTSD) may result in nightmares or fragmented sleep.
- Emotional exhaustion often leads to non-restorative sleep, where patients wake up tired despite sleeping for hours.
🔹 3. Environmental Factors
→ The sleep environment plays a critical role in regulating sleep behavior and overall comfort.
- Excessive noise, poor ventilation, room lighting, uncomfortable mattresses, or hospital settings can interfere with normal sleep cycles.
- Exposure to blue light from screens or bright lights before bedtime can suppress melatonin release, delaying sleep onset.
- Extreme room temperatures (too hot or too cold) can disturb REM sleep and cause awakenings.
🔹 4. Lifestyle and Sleep Hygiene
→ Daily routines and habits directly influence sleep quality.
- Irregular bedtimes, lack of routine, frequent naps, or using the bed for activities like eating or watching TV can disrupt the body’s internal sleep clock.
- People working night shifts, rotating shifts, or having erratic schedules often experience circadian rhythm disturbances.
- Using mobile phones, laptops, or televisions late at night reduces melatonin levels and leads to insomnia.
🔹 5. Food and Fluid Intake
→ Diet and meal timing can influence the ease of falling asleep and the ability to stay asleep.
- Consumption of heavy or spicy meals before bedtime can cause indigestion or acid reflux, disturbing sleep.
- Intake of excess fluids at night leads to nocturia, interrupting deep sleep.
- Caffeine-containing beverages (tea, coffee, cola) and energy drinks act as central nervous system stimulants and should be avoided in the evening.
- Alcohol, although it may initially induce sleep, causes rebound wakefulness and fragmented sleep later in the night.
🔹 6. Medications and Substance Use
→ Several medications interfere with normal sleep architecture or cause daytime drowsiness.
- Drugs like steroids, beta-blockers, decongestants, diuretics, antidepressants, and antipsychotics can suppress REM sleep or cause restlessness.
- Long-term use of sedative-hypnotics may lead to tolerance, dependency, and rebound insomnia after withdrawal.
- Substance abuse (nicotine, cocaine, marijuana) disrupts the balance of neurotransmitters involved in the sleep-wake cycle.
🔹 7. Age and Developmental Stage
→ Sleep needs and patterns change throughout life.
- Newborns and infants sleep 14–17 hours/day in short intervals, with more REM sleep.
- School-age children and adolescents may have irregular patterns due to academic pressure and screen use.
- Older adults experience lighter and more fragmented sleep, frequent awakenings, and reduced time in deep (NREM) stages due to aging of the brain and decreased melatonin production.
🔹 8. Hormonal Influences
→ Hormones play a vital role in maintaining circadian rhythm and promoting sleep.
- Melatonin, secreted by the pineal gland, regulates sleep-wake cycles; its secretion is affected by light exposure and age.
- Cortisol, a stress hormone, is highest in the morning and lowest at night, but stress can elevate nighttime cortisol, disturbing sleep.
- In women, menstruation, pregnancy, and menopause cause hormonal fluctuations (estrogen and progesterone changes) that affect sleep through hot flashes, discomfort, or frequent urination.
🔹 9. Social and Occupational Factors
→ A person’s social responsibilities and job-related activities can impact their sleep patterns.
- Night shift duties, irregular work hours, or high workload lead to delayed sleep onset, chronic fatigue, and reduced sleep duration.
- Caregiving responsibilities, especially for infants, elderly, or chronically ill family members, often lead to disturbed or insufficient sleep in caregivers.
🔹 10. Psychological or Neurological Disorders
→ Sleep disturbances are common in several psychiatric and neurological conditions.
- Schizophrenia and bipolar disorder can disrupt circadian rhythms and cause both insomnia and hypersomnia.
- Neurological conditions like Alzheimer’s disease and Parkinson’s disease interfere with normal brain signaling for sleep regulation.
- Sleep apnea, restless leg syndrome (RLS), and narcolepsy are primary sleep disorders affecting both quantity and quality of sleep.
c) Discuss the stages of sleep and ways to promote rest and sleep.
🌙 I. Stages of Sleep
Sleep is not a uniform process; it is composed of multiple cycles that alternate between Non-Rapid Eye Movement (NREM) and Rapid Eye Movement (REM) stages.
Each complete cycle lasts approximately 90 to 110 minutes, and the body cycles through these 4–6 times per night.
🌀 1. Non-Rapid Eye Movement (NREM) Sleep
NREM sleep is also known as “quiet sleep” and consists of three stages (as per newer classification):
🔹 Stage 1 – NREM (Light Sleep / Drowsiness)
→ It is the transition phase between wakefulness and sleep.
→ The person is easily arousable, and the muscles start relaxing.
→ Eye movements slow down, and brain waves begin to slow from their daytime wakefulness patterns.
→ It usually lasts for 5–10 minutes.
🔹 Stage 2 – NREM (Onset of True Sleep)
→ In this stage, body temperature drops, heart rate slows, and muscle activity decreases.
→ Brain waves become slower with occasional bursts of rapid waves called “sleep spindles”.
→ The sleeper becomes less responsive to external stimuli.
→ This stage makes up about 40–50% of total sleep.
🔹 Stage 3 – NREM (Deep Sleep / Slow-Wave Sleep)
→ Also known as delta sleep, it is the deepest and most restorative stage of NREM.
→ Blood pressure drops, muscles are fully relaxed, and tissue repair and growth occur.
→ Growth hormone is secreted, and immune functions are strengthened.
→ This stage is essential for physical recovery and usually occurs in the first half of the night.
🌈 2. Rapid Eye Movement (REM) Sleep
→ This is also known as “active sleep” or “paradoxical sleep” because brain activity resembles wakefulness.
→ Eyes move rapidly, but muscles remain temporarily paralyzed (muscle atonia).
→ This stage is when vivid dreams occur and is important for emotional regulation and memory consolidation.
→ REM sleep usually begins 90 minutes after sleep onset and increases in duration with each cycle.
→ It comprises about 20–25% of total sleep time.
✅ Significance of Sleep Stages:
| Sleep Stage | Function |
|---|---|
| NREM Stage 1 | Transition into sleep |
| NREM Stage 2 | Light sleep; body slows down |
| NREM Stage 3 | Deep restorative sleep, physical healing |
| REM Sleep | Dreaming, memory consolidation, emotional balance |
😴 II. Ways to Promote Rest and Sleep-Nursing Interventions
Nurses play a vital role in promoting healthy sleep patterns in hospitalized and home-care patients. Below are the evidence-based interventions:
🛏️ A. Environmental Modifications
- It is important to ensure a quiet, dark, and cool environment by minimizing noise, turning off lights, and ensuring ventilation.
- The nurse should provide comfortable bedding and pillows and adjust the position as per patient need.
- Use of curtains, earplugs, or white noise machines may be advised to block disturbances.
- Limit ward rounds and procedures during night hours to avoid waking the patient.
🍽️ B. Managing Diet and Fluids
- Avoid heavy meals, caffeine, and alcohol at least 2–3 hours before bedtime.
- Provide light snacks like warm milk or herbal tea which may aid sleep.
- Restrict fluid intake in the evening to minimize nighttime urination (nocturia).
- Offer timely evening meals and monitor nutritional deficiencies like magnesium or iron which may impair sleep.
💊 C. Medication and Pain Control
- Administer prescribed analgesics or sedatives on time to relieve pain and promote comfort.
- Assess for side effects of medications that may interfere with sleep (e.g., steroids, diuretics).
- Ensure administration of diuretics in the morning to avoid nocturia.
🧘 D. Relaxation and Stress Reduction Techniques
- Teach the patient deep breathing, progressive muscle relaxation, meditation, or guided imagery.
- A gentle back massage, warm bath, or soothing music can promote relaxation.
- Address patient fears or anxieties through open communication and emotional support.
- Instruct in journaling or reading calming content instead of screen time.
📅 E. Establishing Routine and Sleep Hygiene
- Encourage patients to maintain a consistent sleep-wake schedule, even during weekends.
- Avoid daytime naps, especially after mid-afternoon, as it may disturb nighttime sleep.
- Limit screen use and blue light exposure at least 1 hour before sleep.
- Encourage exposure to natural light during the day to reinforce circadian rhythm.
📋 F. Nursing Assessment and Documentation
- Assess the patient’s sleep pattern, habits, and complaints using sleep diaries or sleep quality tools.
- Document sleep duration, interruptions, and patient feedback on restfulness.
- Monitor for symptoms of sleep disorders such as sleep apnea, insomnia, restless leg syndrome, or nightmares.
Il. Write notes on:(5 x 5=25)
1.Nursing as a professión.
Nursing is not just a job or occupation; it is a profession dedicated to the care of individuals, families, and communities to attain, maintain, or recover optimal health and quality of life. It is guided by scientific knowledge, ethical principles, technical skills, and a strong sense of compassion and service.
✅ Definition of Nursing Profession:
According to the International Council of Nurses (ICN):
“Nursing encompasses autonomous and collaborative care of individuals of all ages, families, groups, and communities, sick or well and in all settings. It includes the promotion of health, prevention of illness, and the care of ill, disabled, and dying people.”
✅ Characteristics of Nursing as a Profession
🔹 1. Systematic Body of Knowledge
→ Nursing is based on a well-defined body of theoretical knowledge drawn from medical science, behavioral science, ethics, sociology, and psychology.
→ It includes concepts of anatomy, physiology, pharmacology, pathology, and evidence-based practice that are continuously updated.
🔹 2. Specialized Education and Training
→ It requires formal education through recognized institutions, such as diploma (GNM), B.Sc., M.Sc. or Ph.D. in Nursing.
→ Nursing students undergo both theoretical instruction and clinical practice, including internships and skill-based learning.
🔹 3. Code of Ethics and Conduct
→ The nursing profession follows a strict code of ethics framed by the Indian Nursing Council (INC) and International Council of Nurses (ICN).
→ Nurses are expected to maintain confidentiality, honesty, dignity, compassion, and patient advocacy in all situations.
🔹 4. Autonomy and Accountability
→ Nurses make independent decisions in patient care based on assessment and critical thinking.
→ They are held legally and professionally accountable for the care they provide, including medication administration, documentation, and patient safety.
🔹 5. Service-Oriented and Humanitarian Nature
→ Nursing is fundamentally a service profession, not merely a business.
→ It aims to relieve suffering, promote health, and provide comfort, especially during illness, trauma, disability, and death.
🔹 6. Professional Organizations and Regulation
→ Nursing is regulated by statutory bodies such as:
- Indian Nursing Council (INC)
- State Nursing Councils
- Trained Nurses’ Association of India (TNAI)
→ These bodies define nursing standards, maintain registration, and promote continuing education and professional growth.
🔹 7. Research and Evidence-Based Practice
→ Nurses actively participate in research to improve patient care outcomes.
→ They apply scientific findings in daily practice to provide safe, effective, and updated care.
🔹 8. Career Advancement and Specialization
→ Nursing offers multiple opportunities for specialization such as:
- Critical Care Nursing
- Pediatric Nursing
- Psychiatric Nursing
- Obstetric & Gynecological Nursing
→ It also allows for teaching, administration, leadership, and research roles, contributing to personal and professional growth.
✅ Importance of Nursing as a Profession:
- It serves as the backbone of the healthcare system by providing round-the-clock patient care.
- It promotes holistic health – addressing physical, emotional, social, and spiritual needs.
- It builds strong therapeutic relationships with patients and families.
- It enhances public health, disease prevention, health promotion, and rehabilitation.
- It ensures patient safety and advocacy, especially for vulnerable populations.
Nursing is a respected, science-based, ethical, and dynamic profession that plays a vital role in global healthcare.
- It requires lifelong learning, empathy, skill, and dedication.
- As a profession, it evolves with medical advancements, but its core value of compassionate care remains unchanged.
2.Explain the discharge procedure.
The discharge procedure refers to the planned process of preparing a patient to leave the hospital and continue recovery at home or in another facility.
It ensures continuity of care, safe transition, and proper instructions for patients and caregivers.
✅ Definition of Discharge:
Discharge is defined as the formal release of a patient from a hospital or healthcare facility after they have received adequate treatment and are deemed fit to leave, either fully recovered or with follow-up care plans.
✅ Types of Discharge:
- Routine discharge: When treatment is complete and the patient is ready to go home.
- Discharge on request: When the patient or family requests discharge before treatment is complete.
- Discharge against medical advice (DAMA/LAMA): When the patient leaves the hospital without the doctor’s approval.
- Referral discharge: When a patient is transferred to another facility for further treatment.
- Absconded discharge: When a patient leaves the hospital without informing the staff.
- Death discharge: In case of death, a formal discharge is done after completing necessary documentation.
✅ Purposes of Discharge Procedure:
- To ensure safe, efficient, and planned departure of the patient.
- To inform the patient about follow-up, medications, and home care.
- To ensure all hospital records, bills, and reports are completed.
- To coordinate with community healthcare services if needed.
- To reduce the risk of post-discharge complications or readmission.
✅ Steps of Discharge Procedure (Point-wise Explanation)
🔹 1. Physician’s Discharge Order
→ The treating doctor must assess the patient and write a formal discharge order in the patient’s case file.
→ The nurse must verify the doctor’s written instruction before proceeding.
🔹 2. Notification to the Patient and Relatives
→ The nurse must inform the patient and family about the discharge date and time in advance.
→ Clarify any doubts about home care, treatment continuation, or future appointments.
🔹 3. Final Clinical Assessment
→ The nurse should assess vital signs, wound condition, IV lines, and mobility status before discharge.
→ Ensure that the patient is physically and mentally stable for discharge.
🔹 4. Preparing the Discharge Summary
→ The doctor writes a detailed discharge summary, which includes:
- Diagnosis and course of treatment
- Investigations and findings
- Medications given and to be continued
- Diet instructions
- Follow-up visits and date
- Special precautions or rehabilitation advice
🔹 5. Patient Education and Instructions
→ The nurse must provide verbal and written instructions to the patient and family, including:
- How and when to take medicines
- Dietary guidelines
- Activity or mobility restrictions
- Signs and symptoms that require re-admission
- How to care for wounds or drains at home
🔹 6. Medication and Supply Handover
→ Provide a list of prescribed medications, doses, and times.
→ Supply medical aids, equipment, or wound dressing materials if needed.
→ Explain the use of devices like nebulizers, inhalers, insulin pens, etc.
🔹 7. Settling Hospital Bills and Documentation
→ The patient or family must clear all hospital charges at the billing counter.
→ After billing clearance, the nurse ensures all records (nursing notes, medication charts, consent forms) are properly filed.
🔹 8. Returning Patient’s Belongings
→ Return any hospital-issued items, personal clothes, valuables, or identification documents to the patient or family.
→ Cross-check the belongings list maintained at the time of admission.
🔹 9. Discharge from Ward and Final Handover
→ Assist the patient in dressing and preparing for transport home.
→ Help shift the patient to a wheelchair or stretcher if needed.
→ Escort the patient to the exit gate or ambulance along with discharge papers and reports.
🔹 10. Documentation by Nurse
→ The nurse must record the discharge in the nursing record/register, including:
- Date and time of discharge
- Type of discharge (routine, DAMA, etc.)
- Condition of patient at discharge
- Signature of the staff handling the discharge
- Signature or thumb impression of the patient/relative
👩⚕️ Nursing Responsibilities During Discharge:
- Ensure all discharge steps are followed systematically and safely.
- Provide clear instructions and ensure the patient understands their post-hospital care.
- Act as a coordinator between the medical team and the patient’s family.
- Provide emotional support to reduce anxiety or fear of leaving the hospital.
- Arrange follow-up services or referrals to community nursing if needed.
- Maintain complete and legal documentation of the entire discharge process.
The discharge procedure is a critical component of patient care that ensures a smooth and safe transition from hospital to home.
- Nurses have an important role in educating, guiding, and documenting every aspect of the discharge.
- A properly conducted discharge process helps in reducing complications, promotes recovery, and enhances patient satisfaction.
3.Administration of oral medications.
Administration of oral medications is the most common and preferred route of drug delivery. It is safe, convenient, non-invasive, cost-effective, and easily acceptable by patients.
- However, it requires accurate technique, correct patient identification, and awareness of drug actions and side effects to ensure therapeutic effectiveness and safety.
✅ Definition:
Oral medication administration is the process of giving drugs by mouth using various forms like tablets, capsules, liquids, or powders to be swallowed or dissolved in the gastrointestinal tract for absorption into the bloodstream.
✅ Purposes of Oral Medication Administration:
- To achieve systemic therapeutic effect through gastrointestinal absorption.
- To relieve symptoms, cure disease, or maintain health.
- To follow the doctor’s prescribed treatment plan for acute or chronic conditions.
- To allow self-administration at home under nurse supervision or education.
✅ Forms of Oral Medications:
- Tablets – solid, compressed form; may be coated or uncoated.
- Capsules – gelatin containers filled with liquid or powder drugs.
- Syrups – sweet liquid form used mostly in pediatrics.
- Suspensions – liquid with undissolved particles; must be shaken before use.
- Solutions – clear liquids where the drug is completely dissolved.
- Powders or Granules – to be mixed with water or other liquids.
- Lozenges or Troches – to be dissolved slowly in the mouth.
✅ General Principles of Oral Medication Administration:
- The right drug must be administered to the right patient, in the right dose, at the right time, and through the right route.
- Medications must be checked three times – when taken from storage, before preparation, and at bedside before administration.
- Nurse must observe for allergies, contraindications, or swallowing difficulties.
- Explain the drug name, dose, and purpose to the patient and get consent.
- Never leave medications unattended or force a patient to take them.
- Proper documentation is essential after drug administration.
✅ Preparation Before Administration:
🧾 A. Check the Medication Order:
→ Ensure it includes drug name, dose, route, frequency, and duration as prescribed by the physician.
👤 B. Identify the Right Patient:
→ Use at least two identifiers (e.g., name, ID band, photo) to avoid errors.
💊 C. Prepare the Medication:
→ Wash hands, check expiry date, drug label, and calculate dosage if required.
→ Crush tablets or mix medications only if allowed and safe to do so.
🪑 D. Assess the Patient:
→ Check for consciousness, ability to swallow, presence of nausea, vomiting, or fasting status.
✅ Procedure for Administering Oral Medications:
🔹 1. Explain the Procedure to the Patient
→ It helps gain cooperation and reduces anxiety.
🔹 2. Assist the Patient to Sit Upright
→ Preferably in Fowler’s or semi-Fowler’s position to prevent aspiration.
🔹 3. Administer the Medication as Prepared
→ Use a medicine cup for tablets/capsules, or syringe/dosing spoon for liquids.
→ Ensure patient drinks a small amount of water before and after swallowing unless contraindicated.
🔹 4. Observe the Patient Swallow the Drug
→ Ensure the medication is swallowed completely and not kept in the mouth.
🔹 5. Rinse the Mouth if Needed
→ Especially after giving iron, potassium, or bitter-tasting drugs.
🔹 6. Record the Administration
→ Note the drug name, dose, time, and route in the patient’s medication chart.
✅ Aftercare and Observation:
- Monitor for side effects or allergic reactions (e.g., rashes, nausea, drowsiness).
- Report refusal to take medicine, vomiting after intake, or other issues to the physician.
- Ensure comfort and position after drug administration.
- Provide reassurance and education about the drug and its importance.
👩⚕️ Nursing Responsibilities in Oral Medication Administration:
- It is the nurse’s duty to follow the Ten Rights of Medication Administration.
- The nurse must assess the patient’s ability to swallow and check for contraindications (e.g., unconsciousness, NPO status, aspiration risk).
- The nurse should never crush enteric-coated or sustained-release tablets unless prescribed.
- Ensure patient completes the full course of treatment, especially in antibiotics or chronic conditions.
- Provide patient education on timing, side effects, and storage of home medications if being discharged.
- In case of medication error, report immediately and follow institutional protocol.
Oral medication administration is a routine yet highly responsible nursing task that requires precision, knowledge, and patient-centered care.
- Following proper technique and professional accountability helps prevent errors, improve therapeutic outcomes, and promote patient safety.
4.Physiology and regulation of temperature.
Body temperature is a vital sign and a key indicator of the body’s internal environment.
- It refers to the balance between heat production and heat loss in the body.
- Normal core body temperature in adults is around 36.5°C to 37.5°C (97.7°F to 99.5°F).
- The process of temperature regulation is known as thermoregulation and is essential for enzymatic activity, metabolic function, and survival.
✅ I. Physiology of Body Temperature
🔹 1. Heat Production (Thermogenesis)
→ The body generates heat mainly through metabolism of nutrients and muscle activity.
→ Sources of heat production include:
- Basal metabolic rate (BMR): The energy required to maintain vital functions at rest.
- Muscle activity: Shivering, exercise, and movement increase heat output.
- Hormonal activity: Hormones like thyroxine, epinephrine, and norepinephrine increase metabolic rate and heat production.
- Digestion (Diet-Induced Thermogenesis): After eating, heat is produced during food metabolism.
🔹 2. Heat Loss (Thermolysis)
→ The body loses heat through the skin, lungs, urine, and feces.
→ Major methods of heat loss are:
- Radiation: Loss of heat from a warm body to a cooler environment (e.g., uncovered head).
- Conduction: Direct transfer of heat through contact (e.g., lying on a cold metal surface).
- Convection: Transfer of heat through air or fluid movement (e.g., cool breeze over skin).
- Evaporation: Loss of heat through sweating and respiration, especially in warm environments.
🔹 3. Sites for Measuring Temperature
→ Oral, rectal, axillary, tympanic (ear), and temporal artery (forehead).
→ Rectal temperature is usually 0.5°C higher, and axillary is 0.5°C lower than oral.
✅ II. Regulation of Body Temperature
The body maintains a stable internal temperature through a feedback mechanism controlled by the hypothalamus, a part of the brain.
🔹 1. Role of Hypothalamus (Body’s Thermostat)
→ The anterior hypothalamus controls heat loss.
→ The posterior hypothalamus controls heat production and conservation.
→ It receives information from thermoreceptors in the skin, spinal cord, and internal organs, and initiates appropriate responses.
🔹 2. Mechanisms to Increase Body Temperature (When Cold)
- Shivering: Rapid, involuntary muscle contractions generate heat.
- Vasoconstriction: Peripheral blood vessels narrow, reducing blood flow to the skin and preventing heat loss.
- Piloerection: “Goosebumps” trap air for insulation (minor role in humans).
- Increased metabolic rate due to thyroid and adrenal hormones.
🔹 3. Mechanisms to Decrease Body Temperature (When Hot)
- Vasodilation: Blood vessels widen to bring heat to the surface for dissipation.
- Sweating: Evaporation of sweat cools the body.
- Reduced muscle activity: Reduces internal heat production.
- Increased respiratory rate: Promotes heat loss through expiration.
🔹 4. Role of Hormones in Thermoregulation
- Thyroxine: Increases BMR and heat production.
- Epinephrine and norepinephrine: Increase metabolism and peripheral vasoconstriction during cold stress.
- Estrogen and progesterone: Affect body temperature variations during menstrual cycle.
🔹 5. Behavioral Control of Temperature
→ Individuals take conscious actions to regulate body temperature, such as:
- Wearing more or fewer clothes
- Moving to warmer or cooler places
- Drinking hot or cold fluids
- Using fans or heaters
✅ III. Factors Affecting Body Temperature
- Age: Infants and elderly have less efficient thermoregulation.
- Exercise: Increases body heat production.
- Hormones: Menstrual cycle and ovulation raise core temperature.
- Circadian rhythm: Body temperature is lowest in the morning and highest in the evening.
- Stress: Increases cortisol and adrenaline, raising temperature.
- Environment: High or low ambient temperatures affect thermoregulation capacity.
✅ IV. Clinical Conditions Related to Temperature Regulation
- Fever (Pyrexia): Elevated temperature due to infection or inflammation.
- Hyperthermia: Abnormally high temperature due to failed heat loss (e.g., heat stroke).
- Hypothermia: Abnormally low temperature due to cold exposure.
- Heat exhaustion and heatstroke: From excessive heat and dehydration.
- Chills and rigors: Sudden cold sensations due to infection or exposure.
5.Universal precautions.
Universal precautions are infection control practices used to prevent transmission of bloodborne pathogens and infectious agents during patient care, regardless of the patient’s diagnosis or infection status.
These precautions are based on the principle that all blood, body fluids, secretions, excretions (except sweat), non-intact skin, and mucous membranes may carry infectious agents.
✅ Definition:
Universal precautions refer to a set of standard safety measures used by healthcare workers to minimize the risk of transmission of infection, especially from bloodborne pathogens like HIV, hepatitis B (HBV), and hepatitis C (HCV).
✅ Objectives of Universal Precautions:
- To protect healthcare workers (HCWs) from occupational exposure to blood and body fluids.
- To prevent cross-contamination between patients.
- To promote safe practices in all healthcare settings.
- To reduce the risk of hospital-acquired infections (HAIs).
✅ Key Principles of Universal Precautions:
🔹 1. Hand Hygiene
→ Handwashing is the single most important practice in infection control.
→ Hands must be washed:
- Before and after each patient contact
- After contact with blood, body fluids, or contaminated surfaces
- After removing gloves
→ Use soap and water or alcohol-based hand rubs.
🔹 2. Use of Personal Protective Equipment (PPE)
→ PPE should be worn based on the anticipated exposure.
- Gloves – When touching blood, body fluids, secretions, or contaminated surfaces
- Gowns or aprons – During procedures likely to generate splashes or sprays
- Masks and eye protection/face shields – When performing activities that may involve splashes to the face
- Shoe covers and caps – In operation theatres or high-risk zones
🔹 3. Safe Injection and Sharp Practices
→ Use a new sterile syringe and needle for each injection.
→ Do not recap needles after use – use a one-hand scoop technique if needed.
→ Dispose of used sharps in puncture-proof, labeled containers.
→ Avoid passing sharp instruments hand-to-hand.
🔹 4. Proper Handling of Specimens
→ All blood and body fluid specimens should be considered potentially infectious.
→ Place specimens in leak-proof, labeled containers.
→ Avoid contamination of the external surface of containers.
🔹 5. Environmental Cleaning and Decontamination
→ Surfaces contaminated with blood or body fluids should be cleaned using 1% sodium hypochlorite solution.
→ Spills must be cleaned immediately with appropriate disinfectants and protective gear.
→ All reusable equipment must be properly cleaned, disinfected, or sterilized before reuse.
🔹 6. Proper Waste Disposal
→ Biomedical waste must be segregated using color-coded bags as per hospital or government protocols.
→ Infectious waste should be incinerated or treated before disposal.
→ Follow hospital’s waste management policies strictly to avoid exposure.
🔹 7. Respiratory Hygiene/Cough Etiquette (Extension from standard precautions)
→ Encourage patients to:
- Cover mouth and nose when coughing or sneezing
- Use tissues or elbow crease
- Wear a surgical mask if respiratory symptoms are present
→ Provide hand hygiene resources and masks in waiting areas.
🔹 8. Patient Placement
→ Place patients with known or suspected infections in isolation or designated rooms.
→ Use barrier nursing techniques as required for diseases like TB, COVID-19, or MRSA.
✅ Universal Precautions Apply To:
- Blood
- All body fluids (except sweat)
- Non-intact skin (wounds, cuts)
- Mucous membranes (eyes, mouth, genitals)
- Needles, sharp instruments, and invasive procedures
✅ Conditions Requiring Universal Precautions:
- HIV/AIDS
- Hepatitis B and C
- COVID-19
- Tuberculosis (for airborne precautions)
- Invasive procedures (surgery, catheterization, wound care)
✅ Nursing Responsibilities in Universal Precautions:
- Adhere strictly to hand hygiene and PPE protocols in all procedures.
- Educate other staff and caregivers on the importance of universal precautions.
- Report and manage needlestick injuries or exposure incidents immediately.
- Ensure proper waste disposal and equipment sterilization.
- Maintain up-to-date immunization status (e.g., Hepatitis B vaccine).
- Promote patient safety and prevent cross-infection in clinical practice.
III. Short answers on (10×2-20)
1.Define nursing.
Nursing is defined as a profession and a science focused on the care of individuals, families, and communities to help them achieve, maintain, or recover optimal health and quality of life.
→ It involves a combination of knowledge, skills, attitudes, and compassionate care to address physical, emotional, psychological, social, and spiritual needs.
According to the International Council of Nurses (ICN):
“Nursing encompasses autonomous and collaborative care of individuals of all ages, families, groups, and communities, sick or well and in all settings. It includes the promotion of health, prevention of illness, and the care of ill, disabled, and dying people.”
→ This modern definition highlights that nursing is not limited to the hospital but also includes community health, preventive care, health education, and advocacy.
2.Four types of hospitals.
General Hospital – Provides wide range of medical and surgical services to all age groups.
Specialty Hospital – Focuses on specific diseases or systems (e.g., cancer hospital, cardiac hospital).
Teaching Hospital – Attached to medical/nursing colleges for clinical education and training.
District Hospital – Government-run hospital serving rural and semi-urban areas.
3.Four guidelines for reporting
- Be clear, accurate, and concise – Avoid vague terms and state facts.
- Report promptly and timely – Especially in emergencies or changes in condition.
- Maintain confidentiality – Only share information with authorized personnel.
- Use proper channels of communication – Follow hierarchy (e.g., report to head nurse or physician).
4.Mention the various dimensions of health.
- Physical Health – Functioning of body systems and absence of disease.
- Mental/Emotional Health – Stability of thoughts, feelings, and behavior.
- Social Health – Ability to form satisfying relationships and social well-being.
- Spiritual Health – Sense of purpose, beliefs, and values guiding life.
(Optional additions: Vocational, Environmental, Intellectual)
5.Four sites of taking temperature.
Oral (mouth)
Rectal (anus)
Axillary (armpit)
Tympanic (ear canal)
6.Placebo.
→ A placebo is a substance or treatment with no active therapeutic effect, often used in clinical trials or psychologically to satisfy a patient’s expectation of treatment (e.g., sugar pill).
7.List down the methods of communication,
Verbal Communication – Spoken or written words
Non-verbal Communication – Gestures, posture, facial expressions
Visual Communication – Signs, symbols, charts, posters
Electronic Communication – Emails, messages, telehealth platforms
8.Principles of health teaching
Interest and Need-Based – Should match the learner’s needs and interest
Participation – Encourage active involvement of the learner
Comprehension – Use simple, understandable language
Reinforcement – Repeating and revising helps retain the knowledge
9.Four types of splints.
- Arm Splint – For immobilizing arm fractures
- Leg Splint – Used in lower limb injuries
- Finger Splint – For finger fractures or dislocations
- Thomas Splint – Used for femur (thigh bone) fractures
10.Name four types of fever.
- Continuous Fever – Temperature remains above normal and does not fluctuate much (e.g., typhoid)
- Remittent Fever – Temperature fluctuates but never returns to normal (e.g., infective endocarditis)
- Intermittent Fever – Fever comes and goes with normal temperature in between (e.g., malaria)
- Relapsing Fever – Fever subsides for a few days and returns again (e.g., relapsing fever)
