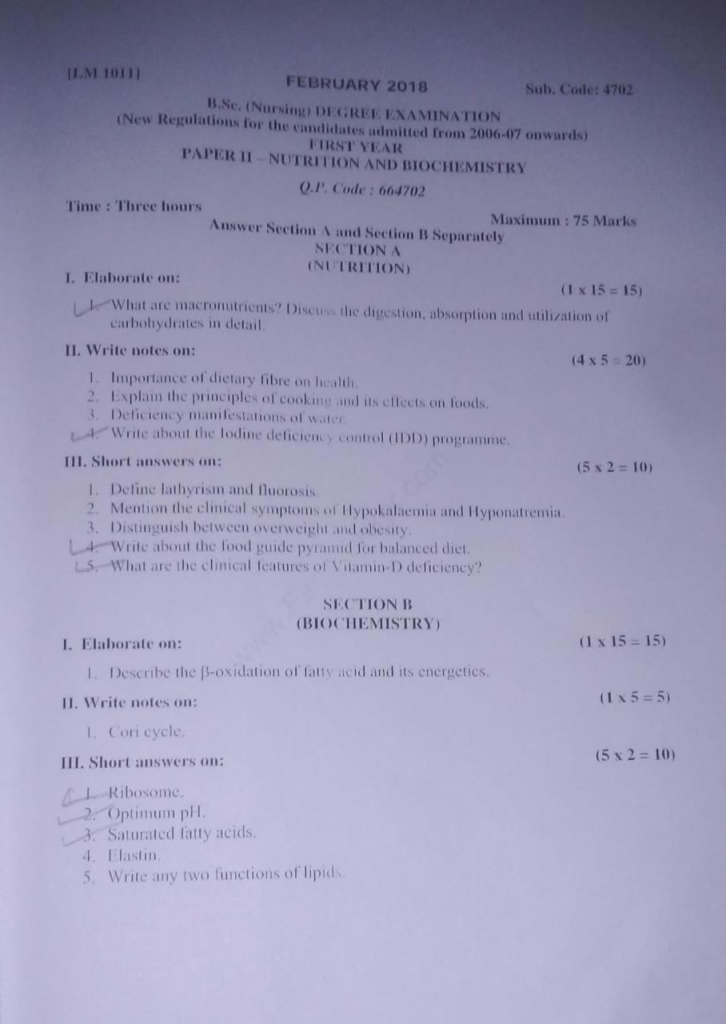
B.SC.FEBRUARY 2018- FIRST YEAR-PAPER SOLUTION UPLOAD NO.09
PAPER SOLUTION NO.09 – FEBRUARY-2018
l.Elaborate on: (1×15=15)
1.What are macronutrients? Discuss the digestion, absorption and utilization of carbohydrates in detail
1️⃣ Macronutrients are nutrients required by the body in large quantities (grams per day) to provide energy, build body tissues, and regulate physiological functions.
2️⃣ They are termed “macro” because they are needed in bulk amounts compared to micronutrients (like vitamins and minerals).
3️⃣ The three primary macronutrients include:
- Carbohydrates – the main source of energy
- Proteins – essential for tissue growth and repair
- Fats (lipids) – energy storage and hormone regulation
🔹 Water is also considered a macronutrient due to its vital physiological roles, although it provides no calories.
🥖 2. Carbohydrates: Introduction and Importance
1️⃣ Carbohydrates are organic compounds composed of carbon (C), hydrogen (H), and oxygen (O), typically in the ratio 1:2:1.
2️⃣ They are the body’s primary source of energy, especially for brain cells, red blood cells, and skeletal muscles during exercise.
3️⃣ Carbohydrates are classified into:
- Monosaccharides – single sugar units (e.g., glucose, fructose, galactose)
- Disaccharides – two sugar units (e.g., sucrose, lactose, maltose)
- Polysaccharides – long chains of glucose (e.g., starch, glycogen, cellulose)
4️⃣ Only monosaccharides are absorbable by the intestinal mucosa; hence all complex carbohydrates must be digested into monosaccharides.
⚗️ 3. Digestion of Carbohydrates
Carbohydrate digestion is a step-wise enzymatic process that occurs in different parts of the gastrointestinal tract.
✅ A. Digestion in the Mouth
- The process begins in the mouth where the enzyme salivary amylase (also called ptyalin) is secreted by salivary glands.
- This enzyme acts on starch and glycogen to break them down into maltose and short-chain dextrins.
- However, this enzymatic activity is short-lived because food does not remain in the mouth for long.
✅ B. Digestion in the Stomach
- In the acidic environment of the stomach (due to hydrochloric acid), salivary amylase is inactivated.
- No significant carbohydrate digestion occurs in the stomach.
- The food becomes chyme and is pushed into the small intestine for further digestion.
✅ C. Digestion in the Small Intestine
- The pancreas secretes pancreatic amylase into the duodenum which resumes the breakdown of starch into maltose, isomaltose, and oligosaccharides.
- The final step in carbohydrate digestion occurs at the brush border of the small intestinal villi:
- Maltase hydrolyzes maltose → 2 glucose molecules
- Lactase breaks lactose → glucose + galactose
- Sucrase splits sucrose → glucose + fructose
- Isomaltase cleaves branched dextrins → glucose
- The complete digestion results in three main absorbable sugars: glucose, fructose, and galactose.
🌡️ 4. Absorption of Carbohydrates
Carbohydrate absorption mainly occurs in the jejunum and upper ileum of the small intestine.
1️⃣ Glucose and Galactose are absorbed through active transport mechanisms via SGLT-1 (sodium-glucose co-transporter), which requires energy and sodium gradient.
2️⃣ Fructose is absorbed through facilitated diffusion using GLUT-5 transporter, which does not require energy.
3️⃣ Once inside the intestinal epithelial cells, all monosaccharides are transported into the bloodstream via the GLUT-2 transporter and enter the hepatic portal circulation toward the liver.
⚡ 5. Utilization of Carbohydrates
Once absorbed, carbohydrates are transported to the liver, where they are metabolized and distributed for various functions:
✅ A. In the Liver
- The liver converts galactose and fructose into glucose, which serves as a central fuel for body cells.
- Glucose is:
- Used immediately by tissues for energy via aerobic or anaerobic glycolysis
- Stored as glycogen in liver and muscles (glycogenesis)
- Converted into fat if consumed in excess (lipogenesis)
✅ B. In the Peripheral Tissues
- Glucose is taken up by muscle, adipose, and other tissues via insulin-dependent transport (GLUT-4 transporters).
- Inside cells, glucose is metabolized by glycolysis into pyruvate, which then enters mitochondria to produce ATP through the Krebs cycle and Electron Transport Chain (ETC).
- In the absence of oxygen (anaerobic conditions), pyruvate is converted into lactic acid, especially in muscles.
✅ C. ATP Production from Carbohydrate Metabolism
- One molecule of glucose through aerobic metabolism yields 36–38 ATP molecules.
- This ATP is used for various cellular functions, including muscle contraction, active transport, and biosynthesis.
🩺 6. Clinical and Nutritional Importance
1️⃣ Carbohydrates are essential to prevent protein breakdown (protein sparing action) and maintain muscle mass.
2️⃣ Deficiency of carbohydrates leads to ketosis, fatigue, and poor mental performance.
3️⃣ Excessive intake of refined carbohydrates contributes to obesity, insulin resistance, and type 2 diabetes.
4️⃣ In clinical nutrition, complex carbohydrates like whole grains, fruits, and vegetables are preferred over simple sugars.
5️⃣ In conditions like diabetes mellitus, understanding carbohydrate digestion and absorption is critical for glycemic control and dietary planning.
II. Write notes on (4×5=20)
1.Importance of dietary fibre on health.
1️⃣ Promotes Healthy Digestion:
Dietary fibre increases the bulk of stool and facilitates regular bowel movements, thereby preventing constipation, bloating, and irregularity in defecation.
2️⃣ Prevents Digestive Disorders:
It reduces the risk of colonic diseases such as diverticulosis, hemorrhoids, and may protect against colorectal cancer by enhancing stool transit and reducing exposure to toxins.
3️⃣ Helps Control Blood Sugar Levels:
Soluble fibre slows the absorption of glucose into the bloodstream, preventing sudden spikes in blood sugar and improving glycemic control, especially in diabetic patients.
4️⃣ Lowers Blood Cholesterol Levels:
Soluble fibre binds to cholesterol and bile acids in the intestines and enhances their elimination, which helps to reduce LDL (bad cholesterol) and improve heart health.
5️⃣ Aids in Weight Management:
Fibre-rich foods provide satiety (feeling of fullness), slow gastric emptying, and help control appetite, thereby reducing caloric intake and preventing obesity.
6️⃣ Supports Gut Microbiome:
Fibre acts as a prebiotic, promoting the growth of beneficial gut bacteria which contribute to better digestion, immunity, and nutrient absorption.
7️⃣ Reduces Risk of Cardiovascular Diseases:
By controlling blood sugar and lipid levels, fibre lowers the risk of hypertension, atherosclerosis, and heart attack.
8️⃣ Detoxifies the Body:
Fibre helps in binding and removing toxins, bile salts, and carcinogens from the gastrointestinal tract, supporting natural detoxification.
9️⃣ Regulates Bowel Health:
It maintains bowel regularity, reduces straining during defecation, and helps prevent complications like anal fissures and rectal prolapse.
🔟 Improves Nutritional Quality of Diet:
A fibre-rich diet is usually high in vitamins, minerals, and antioxidants, contributing to overall nutritional well-being.
2.Explain the principles of cooking and its effects on foods
✅ I. Principles of Cooking
🔹 1. Application of Heat to Induce Changes
Cooking is based on the principle of applying controlled heat to food in order to induce chemical and physical transformations. These changes make food safe to eat, palatable, digestible, and nutritionally beneficial.
- Raw food often contains tough fibers, anti-nutrients, and microbes that can be harmful or unpalatable.
- Heat softens food tissues, activates flavors, and improves digestibility.
🔹 2. Use of Moist and Dry Heat Methods
The choice of heat method affects texture, flavor, and nutrient retention:
- Moist heat cooking (e.g., boiling, steaming, stewing) uses water or steam to transfer heat.
→ Suitable for rice, lentils, vegetables, fish. - Dry heat cooking (e.g., baking, roasting, frying, grilling) uses air, oil, or radiation for heat.
→ Suitable for meat, bread, snacks.
Combination methods like braising use both moist and dry techniques for enhanced flavor and tenderness.
🔹 3. Mechanisms of Heat Transfer
- Conduction → Direct transfer of heat from hot surface to food (e.g., frying on a pan).
- Convection → Heat circulates through liquids or gases (e.g., boiling, baking in oven).
- Radiation → Heat is transferred by waves without direct contact (e.g., grilling, microwave cooking).
Each method affects cooking time, energy efficiency, and uniformity of cooking.
🔹 4. Control of Time and Temperature
Proper control of cooking time and temperature is crucial to achieve desired texture and nutrient retention.
- Under-cooking can leave harmful bacteria or make food tough (e.g., meat, legumes).
- Over-cooking can result in nutrient loss, burnt flavor, and undesirable texture.
Low, slow cooking preserves nutrients and develops deep flavors; high heat enhances browning and crispiness.
🔹 5. Preservation of Nutrients and Quality
One important principle of cooking is to retain maximum nutritional value while improving food’s taste, appearance, and shelf-life.
- Use less water, cover cooking vessels, and avoid discarding boiled water to retain water-soluble vitamins.
- Prefer steaming or pressure cooking over deep frying to minimize fat intake and preserve thermolabile nutrients.
- Use fresh ingredients and avoid long exposure to heat, air, and light, which can degrade vitamins like C and B-complex.
✅ II. Effects of Cooking on Foods
🔹 1. Effect on Carbohydrates
- Cooking causes gelatinization of starch—granules absorb water, swell, and soften (e.g., rice, potatoes), enhancing digestibility.
- Sugars caramelize when heated (above 160°C), forming brown color and rich flavor (used in desserts, baked goods).
- It breaks down non-digestible polysaccharides in vegetables, improving nutrient absorption and gut health.
🔹 2. Effect on Proteins
- Heat causes denaturation (unfolding) and coagulation (clumping) of protein molecules (e.g., boiling eggs, cooking meat).
- This improves digestibility but overheating may toughen proteins, reduce nutrient value, and make meat hard to chew.
- Cooking destroys enzyme inhibitors found in raw legumes (like trypsin inhibitors), enhancing protein bioavailability.
🔹 3. Effect on Fats and Oils
- During cooking, fats melt and help transfer heat, contributing to texture and flavor.
- Repeated heating (e.g., reused frying oil) can produce oxidized fats and trans fats, which are linked to cardiovascular disease and cancer.
- Certain cooking oils (like olive oil) are more stable than others at high temperatures.
🔹 4. Effect on Vitamins and Minerals
- Water-soluble vitamins (Vitamin C, B1, B2, B9) are sensitive to heat, light, and water, and may be lost during boiling or prolonged cooking.
- Fat-soluble vitamins (A, D, E, K) are more heat-stable, especially when cooking in oil.
- Minerals are not destroyed by heat but may leach into cooking water. Using this water in soups or gravies prevents loss.
🔹 5. Effect on Taste, Texture, and Appearance
- Cooking enhances flavor and aroma through chemical reactions like Maillard browning and caramelization.
- It alters food’s texture, making it soft, flaky, crispy, or tender depending on the method.
- Cooking enhances the visual appeal of food through color changes, especially in vegetables, baked items, and meats.
🔹 6. Effect on Digestibility
- Cooking breaks down tough fibers, starches, and proteins, making food easier to chew, swallow, and absorb.
- It increases nutrient availability, especially from legumes, cereals, and meat.
- Proper cooking reduces anti-nutritional factors like phytic acid and oxalates.
🔹 7. Effect on Food Safety
- Cooking kills pathogenic microorganisms, including bacteria, viruses, fungi, and parasites.
- It inactivates natural toxins in certain foods (e.g., cyanogenic glycosides in cassava).
- Proper cooking prevents foodborne illnesses such as typhoid, cholera, E. coli infection, and salmonellosis.
3.Deficiency manifestations of water
Water is an essential nutrient that plays a vital role in regulating body temperature, transporting nutrients, removing waste, and maintaining electrolyte balance. When the body loses more water than it takes in, it leads to a condition called dehydration or water deficiency.
Even mild dehydration (loss of 1–2% body weight) can affect physical and cognitive performance, while moderate to severe dehydration can result in organ dysfunction and can be fatal if untreated.
⚠️ 2. Causes of Water Deficiency (Dehydration)
(To understand the manifestations, causes must be clear)
- Inadequate fluid intake (e.g., in elderly, unconscious patients, or due to nausea)
- Excessive fluid loss (due to vomiting, diarrhea, fever, sweating, burns)
- Diuretic use or uncontrolled diabetes causing increased urination
- Environmental factors like high temperatures and physical exertion
🚨 3. Clinical Manifestations of Water Deficiency
🔹 1. Increased Thirst and Dry Mouth
- Thirst is the body’s first defense against dehydration.
- Dryness of lips, tongue, and throat is due to reduced salivary secretion.
- Patient may report sticky or cottony mouth and persistent thirst.
🔹 2. Decreased Urine Output and Dark Yellow Urine
- Kidneys conserve water, leading to oliguria (low urine output).
- Urine becomes highly concentrated and dark in color.
- In extreme cases, anuria (no urine) may occur, indicating kidney shutdown.
🔹 3. Dry Skin and Loss of Skin Turgor
- The skin appears rough, dull, and flaky.
- When pinched, the skin returns slowly to its original position, a sign of reduced skin elasticity, especially in the elderly and children.
🔹 4. Sunken Eyes and Hollow Cheeks
- Dehydration leads to reduced tissue fluid volume, causing sunken eyeballs and drawn facial appearance.
- Often seen in infants, malnourished individuals, and those with severe fluid loss.
🔹 5. Headache, Dizziness, and Confusion
- Reduced cerebral perfusion causes headache, vertigo, and irritability.
- In elderly patients, dehydration may mimic dementia or delirium.
- In advanced stages, the patient may become disoriented or unconscious.
🔹 6. Fatigue, Lethargy, and Muscle Weakness
- Reduced fluid volume affects oxygen and nutrient delivery to muscles, causing early fatigue even with light activity.
- Muscle cramps may occur due to electrolyte imbalance, especially low sodium or potassium.
🔹 7. Tachycardia and Hypotension
- The heart rate increases (tachycardia) to compensate for decreased blood volume.
- Blood pressure drops (hypotension), especially when standing – this is called postural hypotension.
- In severe cases, dehydration can lead to circulatory collapse or hypovolemic shock.
🔹 8. Constipation and Hard Stools
- Water is necessary to keep stools soft and easy to pass.
- Its deficiency causes dry, hard stools, leading to constipation, bloating, and abdominal pain.
🔹 9. Decreased Sweating and Body Overheating
- With less fluid available, the body reduces sweating, impairing temperature regulation.
- This increases the risk of heat exhaustion and heatstroke, especially in hot climates or during exercise.
🔹 10. Dry and Sticky Mucous Membranes
- The mucosal lining of the mouth, eyes, nose, and vagina becomes dry, irritated, and prone to infections.
- Eyes may appear dull and tearless, and nasal passages may develop crusting or nosebleeds.
🔹 11. Poor Capillary Refill and Cold Extremities
- Capillary refill time (CRT) becomes delayed (>2 seconds), indicating peripheral circulatory failure.
- Hands and feet may feel cold, pale, and clammy, especially in shock.
🔹 12. In Infants and Children
- Sunken fontanelles, decreased number of wet diapers, and irritability are signs of dehydration.
- Lethargy, dry tongue, and crying without tears are red flags requiring immediate attention.
🏥 4. Severe Dehydration Complications
- Electrolyte imbalance (hyponatremia, hypokalemia)
- Renal failure due to reduced perfusion
- Seizures, arrhythmias, and coma in extreme fluid loss
- Hypovolemic shock leading to multi-organ dysfunction
4.Write about the lodine deficiens control (DD) programme.
1️⃣ Iodine is a micronutrient essential for the synthesis of thyroid hormones (T3 and T4), which regulate growth, metabolism, and mental development.
2️⃣ Iodine deficiency is one of the leading causes of preventable mental retardation and developmental delay in children.
3️⃣ To address this, the Government of India launched a national programme originally called the National Goitre Control Programme (NGCP) in 1962, which was renamed in 1992 as the National Iodine Deficiency Disorders Control Programme (NIDDCP) to include all iodine-related disorders.
🎯 2. Objectives of the Programme
1️⃣ To assess the magnitude of iodine deficiency disorders in the country.
2️⃣ To reduce the prevalence of IDDs below 5% in the population.
3️⃣ To ensure universal access to iodized salt by replacing non-iodized salt in the population.
4️⃣ To monitor the iodine content of salt and urinary iodine levels in vulnerable populations.
5️⃣ To conduct Information, Education and Communication (IEC) activities to create public awareness on the importance of iodine.
🧪 3. Iodine Deficiency Disorders Covered
- Goitre (thyroid gland enlargement)
- Cretinism (mental and physical retardation in infants)
- Hypothyroidism
- Stillbirths and abortions
- Mental impairment and learning disabilities
- Growth retardation and speech/hearing defects
🛠️ 4. Key Components and Strategies
✅ A. Universal Salt Iodization (USI)
- The government mandates the use of iodized salt with at least 15 ppm iodine at the consumer level.
- Iodized salt is produced, distributed, and made available through the public distribution system (PDS) and open market.
✅ B. Monitoring and Quality Control
- Iodine content in salt is monitored at production, storage, and household levels.
- Urinary iodine excretion surveys are done to assess iodine status in populations.
✅ C. Health Education and IEC Activities
- Community awareness is created about the importance of iodine through schools, health workers, mass media, and posters.
- Education on using only packaged iodized salt is emphasized.
✅ D. Intersectoral Collaboration
- Ministries of Health, Education, Industry, and Information & Broadcasting work together to ensure programme success.
📊 5. Achievements of the Programme
1️⃣ Salt iodization coverage has significantly increased, with more than 90% households now using iodized salt (as per recent surveys).
2️⃣ Prevalence of goitre and cretinism has reduced significantly in many endemic regions.
3️⃣ Monitoring mechanisms have improved, including quality testing at salt production units and household surveys.
❌ 6. Challenges Faced
- Inadequate awareness in rural and tribal areas.
- Poor monitoring in remote and high-altitude areas.
- Availability of non-iodized salt in unorganized sectors.
- Storage and transport issues that cause iodine loss from salt.
- Resistance from small-scale salt producers due to cost concerns.
👩⚕️ 7. Role of Nurse in IDD Control Programme
1️⃣ Educate the public on the importance of iodine in diet and dangers of deficiency.
2️⃣ Encourage the use of only iodized salt and demonstrate how to check for iodine using test kits.
3️⃣ Participate in screening and surveys to detect goitre in school children and pregnant women.
4️⃣ Collaborate with health workers and local authorities in IEC campaigns at village and community levels.
5️⃣ Help identify areas of high prevalence and report to health authorities for further intervention.
III. Short answers on (5×2=10)
1.Define lathyrism and fluorosis
Lathyrism:
- It is a neurological disorder caused by excessive consumption of Lathyrus sativus (Kesari dal).
- It is mainly due to the neurotoxin BOAA (β-N-oxalyl amino alanine) present in the pulse.
- It leads to spastic paralysis of the lower limbs, especially in young males in drought-prone areas.
🔹 Fluorosis:
- It is a chronic condition caused by excess intake of fluoride, usually through drinking water (>1.5 ppm).
- It leads to dental fluorosis (mottling of teeth), skeletal fluorosis (bone deformities, stiffness), and in severe cases, crippling deformities.
2.Mention the clinical symptoms of Hypokalaemia and Hyponatremia
🔹 Hypokalaemia (↓ Potassium):
- Muscle weakness or cramps
- Fatigue and lethargy
- Constipation
- Arrhythmias (irregular heartbeat)
- Flattened T-waves on ECG
🔹 Hyponatremia (↓ Sodium):
- Nausea and vomiting
- Headache
- Confusion or altered mental status
- Seizures (in severe cases)
- Muscle cramps and weakness
3.Distingush between overweight and obesity
| Criteria | Overweight | Obesity |
|---|---|---|
| Definition | It is a condition where body weight is more than normal, mainly due to excess fat, muscle, or bone. | It is a condition of excessive body fat accumulation that impairs health. |
| BMI Range | BMI between 25–29.9 kg/m² | BMI of 30 kg/m² or more |
| Health Risk | Moderate risk of diseases | High risk of diabetes, heart disease, and hypertension |
| Appearance | May look slightly bulky or heavy | Significant fat deposits, especially around waist or hips |
4.Write about the food guide pyramidd for balanced diet
🔹 The Food Pyramid is a graphical representation used to show a healthy diet by categorizing foods into five main levels:
1️⃣ Base Layer (Bottom) – Cereals & grains
- Includes rice, wheat, maize, and millet
- Provides carbohydrates – energy-giving foods
2️⃣ Second Layer – Fruits and vegetables
- Source of vitamins, minerals, and fibre
- Helps in digestion and boosting immunity
3️⃣ Third Layer – Milk, meat, fish, eggs, and legumes
- Rich in proteins and calcium
- Essential for growth and repair
4️⃣ Fourth Layer – Fats and oils
- Includes butter, ghee, vegetable oils
- Used sparingly as they are energy-dense
5️⃣ Top Layer (Peak) – Sugars, sweets, junk food
- Should be consumed rarely
- May lead to obesity, diabetes if consumed in excess
✅ A balanced diet includes items from all layers in appropriate proporti
5.What are the clinical features of Vitamin D deficiency?
🔹 In children (Rickets):
- Soft and deformed bones
- Bowed legs (genu varum)
- Delayed teething
- Swollen joints and rib cage deformity (rachitic rosary)
🔹 In adults (Osteomalacia):
- Bone pain and muscle weakness
- Fragile bones prone to fractures
- Difficulty in walking or climbing stairs
🔹 Common Symptoms in All Ages:
- Fatigue
- Frequent infections (due to weak immunity)
- Depression or mood changes
SECTION B (BIOCHEMISTRY)
1.Elaborate on: (1 x 15)
1.Describe the B-oxidation of fatty acid and its energetics.
🔷 Definition
- β-oxidation of fatty acids is the major metabolic process by which long-chain fatty acids are broken down inside the mitochondria to produce energy in the form of ATP.
- The name “β-oxidation” is derived from the fact that oxidation occurs specifically at the β-carbon atom (i.e., the third carbon from the carboxyl group) of the fatty acid chain.
- The process results in the progressive cleavage of two-carbon units from the fatty acid, in the form of acetyl-CoA, which then enters the citric acid cycle (Krebs cycle) for further energy production.
🔷 Location of β-Oxidation
- This metabolic pathway occurs mainly in the mitochondrial matrix of cells.
- Tissues that have high-energy demand such as liver, skeletal muscles, cardiac muscles, and kidneys actively perform β-oxidation.
- However, brain cells and red blood cells do not utilize β-oxidation because fatty acids cannot cross the blood–brain barrier and red blood cells lack mitochondria.
🔷 Prerequisite: Activation and Transport of Fatty Acids
- Before undergoing β-oxidation, the fatty acid must first be activated in the cytoplasm. This process requires the enzyme Acyl-CoA synthetase, which attaches Coenzyme A (CoA) to the fatty acid, converting it into fatty acyl-CoA.
- This activation step requires the consumption of one ATP, but since ATP is hydrolyzed to AMP and pyrophosphate (PPi), it is considered equivalent to the loss of two ATP molecules energetically.
- Long-chain fatty acyl-CoA cannot directly enter the mitochondria. Instead, it must be transported via the carnitine shuttle, involving the enzymes carnitine acyltransferase I and II, and a translocase protein system that facilitates its entry into the mitochondrial matrix.
🔷 Major Steps of β-Oxidation (Each Cycle)
Each cycle of β-oxidation consists of four enzymatic reactions, which successively shorten the fatty acyl-CoA molecule by two carbon atoms. These steps repeat until the entire chain is degraded into acetyl-CoA units:
1️⃣ First Oxidation (Dehydrogenation Reaction)
- In this step, the fatty acyl-CoA undergoes dehydrogenation at the α and β-carbon positions, forming a trans-Δ²-enoyl-CoA.
- This reaction produces one molecule of FADH₂, which enters the electron transport chain and contributes to ATP generation.
- The enzyme catalyzing this reaction is acyl-CoA dehydrogenase.
2️⃣ Hydration Reaction
- The trans-Δ²-enoyl-CoA is hydrated by the enzyme enoyl-CoA hydratase.
- A water molecule is added across the double bond, resulting in the formation of L-β-hydroxyacyl-CoA.
3️⃣ Second Oxidation Reaction
- The hydroxyl group at the β-carbon is oxidized to a keto group by the enzyme β-hydroxyacyl-CoA dehydrogenase.
- This step generates one molecule of NADH, which also enters the electron transport chain and helps in ATP synthesis.
- The product of this step is β-ketoacyl-CoA.
4️⃣ Thiolysis (Cleavage Reaction)
- In this final step, β-ketoacyl-CoA is cleaved by β-ketothiolase, releasing one molecule of acetyl-CoA.
- The remaining fatty acyl-CoA, which is now two carbon atoms shorter, re-enters the β-oxidation cycle for further degradation.
- This cycle continues until the entire fatty acid chain is converted into multiple acetyl-CoA molecules.
🔷 Energetics of β-Oxidation
- Let’s consider a 16-carbon fatty acid (palmitic acid) as a standard example to understand the energy yield.
- The complete β-oxidation of one molecule of palmitic acid involves seven cycles, each cycle shortening the chain by two carbon atoms and producing one FADH₂, one NADH, and one acetyl-CoA (except the final step which produces two acetyl-CoA molecules).
- So, from palmitic acid, a total of 8 acetyl-CoA, 7 NADH, and 7 FADH₂ are produced.
- Each acetyl-CoA enters the citric acid cycle, producing 3 NADH, 1 FADH₂, and 1 GTP (ATP equivalent). This translates to 10 ATP per acetyl-CoA.
- The NADH and FADH₂ from β-oxidation itself enter the electron transport chain, producing approximately 2.5 ATP per NADH and 1.5 ATP per FADH₂.
- The total energy yield is:
- From 7 NADH → 7 × 2.5 = 17.5 ATP
- From 7 FADH₂ → 7 × 1.5 = 10.5 ATP
- From 8 Acetyl-CoA → 8 × 10 = 80 ATP
- Total = 108 ATP
- Subtract 2 ATP for activation step → Net ATP = 106 ATP
🔷 Clinical and Biological Significance
- β-oxidation is a critical source of ATP during fasting, prolonged exercise, low-carbohydrate diets, and starvation.
- It helps maintain blood glucose levels indirectly, by sparing glucose and increasing acetyl-CoA production.
- In the liver, when β-oxidation is excessive and carbohydrate availability is low, acetyl-CoA is diverted to ketone body synthesis, a process important during starvation.
- Impaired β-oxidation, such as in carnitine deficiency or acyl-CoA dehydrogenase deficiency, can result in serious metabolic disorders including hypoglycemia, muscle weakness, and cardiomyopathy.
II. Write notes on:(1×5=5)
1.Cori cycle.
🔷 Definition:
- The Cori cycle is a metabolic pathway that describes the transport of lactate produced by anaerobic glycolysis in the muscles to the liver, where it is converted back to glucose, and then returned to the muscles for energy use.
- It helps in maintaining glucose homeostasis and managing lactate accumulation during intense muscular activity.
🔷 Site of Occurrence:
- This cycle occurs between skeletal muscles and liver cells.
- It involves anaerobic metabolism in muscles and gluconeogenesis in the liver.
🔷 Steps of the Cori Cycle (With Explanation):
1️⃣ Anaerobic Glycolysis in Muscle:
- During intense physical activity or oxygen deficit, the muscles switch to anaerobic glycolysis.
- In this process, glucose is broken down to pyruvate, and due to lack of oxygen, pyruvate is converted into lactate.
- Enzyme involved: Lactate dehydrogenase (LDH).
- This process produces a small amount of ATP for immediate energy but accumulates lactic acid in the muscle tissue.
2️⃣ Transport of Lactate to Liver:
- The lactate produced in muscle cells is released into the bloodstream.
- It is then taken up by the liver for further processing.
3️⃣ Conversion of Lactate to Glucose in Liver (Gluconeogenesis):
- In the liver, lactate is converted back into pyruvate by lactate dehydrogenase.
- Then, through the process of gluconeogenesis, pyruvate is converted into glucose.
- This process requires ATP and energy input, which is available due to oxygen-rich liver metabolism.
4️⃣ Return of Glucose to Muscle:
- The newly synthesized glucose is transported back into the bloodstream and taken up again by muscle cells.
- It is then reused for energy production, completing the cycle.
🔷 Importance of the Cori Cycle:
- ✅ It allows muscles to function under low oxygen conditions (anaerobic state) by removing lactate.
- ✅ It prevents lactic acid accumulation in muscles, thereby delaying fatigue.
- ✅ It helps in recycling lactate into usable glucose during prolonged physical activity.
- ✅ It ensures energy availability to muscle cells, even during intense work or fasting.
- ✅ It plays a key role in glucose-lactate interconversion between liver and muscle.
🔷 Energy Consideration:
- The muscle produces 2 ATP per glucose during anaerobic glycolysis.
- The liver uses 6 ATP molecules to convert lactate back into glucose (gluconeogenesis).
- Hence, the Cori cycle results in a net energy loss for the body but allows continued muscular activity under oxygen-limited conditions.
🔷 Clinical Significance:
- The Cori cycle is highly active in intense exercise, hypoxia, hemorrhagic shock, and sepsis.
- In liver dysfunction (like liver failure), lactate cannot be cleared efficiently, leading to lactic acidosis.
- It is also important in neonatal glucose metabolism and muscle disorders involving anaerobic pathways.
III. Short answers on:(5×2=10)
1.Ribosome.
- Ribosomes are small, dense, granular organelles found in the cytoplasm and on the rough endoplasmic reticulum.
- They are responsible for protein synthesis by translating messenger RNA (mRNA) into polypeptides.
- Ribosomes consist of ribosomal RNA (rRNA) and proteins and are found in both prokaryotic and eukaryotic cells.
2 Optimum pH.
- Optimum pH is the specific pH level at which an enzyme shows its maximum activity.
- For most enzymes in the human body, this is around pH 7.4 (neutral), but some enzymes like pepsin work best at acidic pH (around 2).
- Deviations from optimum pH reduce enzyme activity.
3.Saturated fatty acids.
- Saturated fatty acids are fatty acids with no double bonds between carbon atoms.
- All carbon atoms are saturated with hydrogen.
- They are typically found in animal fats, butter, ghee, and coconut oil.
- These fats are solid at room temperature and excessive intake may lead to cardiovascular diseases.
4.Elastin
Elastin is a fibrous protein found in connective tissues, especially in skin, blood vessels, and lungs.
It provides elasticity and resilience, allowing tissues to stretch and return to original shape.
It is particularly abundant in arterial walls and ligaments.
5.Write any two functions of lipids
1️⃣ Energy Storage:
Lipids store energy in the form of triglycerides, providing more energy (9 kcal/g) than carbohydrates or proteins.
2️⃣ Structural Role:
They form the basic structure of cell membranes as phospholipids, maintaining integrity and fluidity of cells.
