B.SC. FON-FEBRUARY 2017-PAPER SOLUTION NO.8
FEBRUARY 2017-PAPER SOLUTION NO.8
1.Elaborate on:(2 x 15=30)
a) Define primary health care
Primary Health Care (PHC) is defined as essential, universally accessible, and scientifically sound health care made available to individuals and families in the community through their full participation and at a cost the community and country can afford to maintain at every stage of development.
(As defined in the Alma-Ata Declaration, 1978)
b) What are the principles of primary health care?
Primary Health Care (PHC) is built on a strong foundation of principles that aim to ensure equitable, accessible, and affordable health care for all individuals, especially in underserved communities. These principles guide the planning, delivery, and evaluation of basic health services.
🔹 1. Equitable Distribution of Health Services
→ This principle ensures that health services are equitably available to all people, regardless of their geographic location, income, gender, or social class.
→ It focuses especially on rural, tribal, and slum populations, who often have poor access to health services.
→ The goal is to reduce health disparities by prioritizing care for the most vulnerable.
🔹 2. Community Participation
→ PHC encourages active involvement of individuals, families, and communities in health decision-making, planning, and implementation.
→ Community members are seen not as passive recipients but as partners in health care delivery.
→ It helps build trust, awareness, and self-reliance among people.
→ Examples include: village health committees, health awareness drives, and local volunteers.
🔹 3. Inter-sectoral Coordination
→ Health is not the responsibility of the health sector alone; it requires cooperation among various sectors like:
- Education (for health literacy)
- Agriculture (for food and nutrition)
- Water and Sanitation (for disease prevention)
- Social welfare and housing (for better living conditions)
→ This principle emphasizes collaborative planning and resource sharing across departments to address the social determinants of health.
🔹 4. Appropriate Technology
→ PHC should use scientifically sound, affordable, and locally acceptable technology in diagnosis and treatment.
→ It focuses on cost-effective solutions that can be easily maintained and used by trained community workers.
→ Examples include:
- Oral Rehydration Solution (ORS)
- Rapid diagnostic tests
- Use of trained health workers instead of specialists
- Mobile health apps or telemedicine in remote areas
🔹 5. Focus on Prevention and Health Promotion
→ PHC emphasizes preventive, promotive, curative, and rehabilitative services.
→ Preventing disease is more effective and economical than treating it.
→ Health education, immunization, antenatal care, and safe drinking water are key preventive tools.
→ It also promotes healthy behaviors, hygiene practices, and early screening for diseases.
✅ Additional Supporting Values in PHC:
🩺 Accessibility
→ Services should be geographically, financially, and culturally accessible to all individuals and families.
👥 Sustainability
→ Programs should be sustainable long-term and not rely entirely on external funding or imported resources.
🧠 Cultural Sensitivity
→ Health care must respect local traditions, values, and beliefs to ensure acceptance and effectiveness.
The principles of Primary Health Care ensure that health is recognized as a fundamental human right and that care is:
- Equitable,
- People-centered,
- Affordable,
- And community-based.
As future nurses and health professionals, it is important to apply these principles in both clinical and community settings to achieve the goals of “Health for All.”
c) Discuss the role of nurse in primary health care.
The nurse is a key frontline health worker in the Primary Health Care system. In rural, urban, and tribal communities, nurses play a crucial role in delivering essential, accessible, and affordable care through health promotion, disease prevention, and basic treatment.
They serve as care providers, health educators, counselors, coordinators, and advocates for the community.
✅ Roles of Nurse in Primary Health Care
🔹 1. Health Promoter and Educator
→ The nurse educates individuals, families, and communities about healthy behaviors, hygiene, nutrition, maternal health, immunization, and lifestyle diseases.
→ Conducts health education sessions, street plays, posters, and group talks in schools, anganwadis, or village centers.
→ Promotes safe water, sanitation, and cleanliness to prevent communicable diseases.
🔹 2. Preventive Care Provider
→ The nurse helps prevent illness through:
- Immunization programs (e.g., pulse polio, routine vaccines)
- Antenatal and postnatal care (ANC/PNC)
- Health screenings for anemia, hypertension, diabetes, etc.
→ Monitors growth and development in children using growth charts and nutritional assessment.
→ Participates in national health programs like TB (RNTCP), leprosy (NLEP), and malaria control.
🔹 3. Basic Curative Care Provider
→ Provides first aid and basic treatment for minor illnesses like fever, diarrhea, skin infections, injuries, and respiratory infections.
→ Dispenses essential drugs and refers patients to higher centers when needed.
→ Assists in basic procedures such as dressing wounds, temperature monitoring, and oral rehydration therapy.
🔹 4. Maternal and Child Health (MCH) Care Provider
→ Conducts home visits to pregnant women, registers them early, and provides ANC checkups.
→ Educates mothers on nutrition, rest, immunization, and danger signs in pregnancy.
→ Supports safe institutional deliveries and postnatal care for mother and newborn.
→ Promotes exclusive breastfeeding, weaning practices, and family planning.
🔹 5. Family and Community Health Care Provider
→ Conducts home visits to assess family health needs and maintain family health records.
→ Identifies and supports vulnerable individuals (e.g., elderly, disabled, malnourished children).
→ Encourages family welfare, birth spacing, and contraceptive use.
→ Supports mental health counseling, stress management, and social issues.
🔹 6. Collaborator and Coordinator
→ Works with ASHA, ANMs, Anganwadi workers (AWWs), and local health volunteers.
→ Coordinates with medical officers, social workers, and health inspectors during outreach programs.
→ Helps organize health camps, pulse polio booths, adolescent health days, and school health checkups.
🔹 7. Health Record Keeper and Reporter
→ Maintains accurate records of:
- Immunizations
- ANC/PNC care
- Family planning acceptors
- TB/leprosy cases
→ Submits monthly reports to health supervisors or PHC Medical Officer.
→ Participates in surveillance of communicable diseases (IDSP).
🔹 8. Advocate for Community Needs
→ Acts as a bridge between the community and health system.
→ Raises awareness about available government schemes, insurance benefits (e.g., Ayushman Bharat), and financial assistance.
→ Encourages community participation in health planning and sanitation drives.
The nurse in Primary Health Care is a multi-skilled professional who ensures continuity of care at the grassroots level.
- By promoting health, preventing illness, and treating minor ailments, the nurse plays a vital role in achieving “Health for All.”
- Nurses must be empathetic, skilled, culturally sensitive, and community-focused to fulfill their roles effectively.
2. a) Define pain.
Pain is defined as an unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage.
→ This definition is given by the International Association for the Study of Pain (IASP).
b) Discuss on assessment of pain
Pain assessment is the foundation for effective pain management.
→ It involves a systematic evaluation of the intensity, location, quality, duration, and impact of pain experienced by the patient.
→ Because pain is a subjective experience, the patient’s self-report is the most reliable indicator of pain.
✅ Purpose of Pain Assessment:
- To identify the presence and severity of pain.
- To understand the characteristics of pain (type, cause, pattern).
- To help select the appropriate pain management strategy.
- To monitor response to treatment and adjust interventions accordingly.
- To evaluate the impact of pain on quality of life, mobility, sleep, and emotional status.
✅ Components of Pain Assessment (Detailed Points)
🔹 1. Location of Pain
→ Ask the patient to point to the area of pain or describe where it hurts.
→ Identify if pain is localized (one area) or radiating (spreads to other areas).
→ Multiple pain sites should be documented individually.
🔹 2. Intensity of Pain
→ Measure how severe the pain is using standardized tools (see below).
→ Use pain rating scales to quantify pain (e.g., 0–10).
→ Observe for non-verbal signs in non-communicative patients (facial grimacing, restlessness).
🔹 3. Quality or Nature of Pain
→ Ask the patient to describe how the pain feels in their own words.
→ Common descriptors include:
- Sharp or stabbing
- Dull or aching
- Burning or throbbing
- Cramping or shooting
→ This helps in identifying neuropathic vs. nociceptive pain.
🔹 4. Duration and Timing
→ Assess when the pain started (onset) and how long it has lasted (duration).
→ Ask whether the pain is intermittent, constant, or comes in waves.
→ Identify any time patterns (e.g., worse at night or after activity).
🔹 5. Aggravating and Relieving Factors
→ Ask what makes the pain worse (e.g., movement, stress, eating).
→ Ask what relieves pain (e.g., rest, medication, heat application).
🔹 6. Effect on Function and Life
→ Assess how pain affects the patient’s:
- Sleep
- Appetite
- Mobility and daily activities
- Mood and concentration
→ Pain often leads to anxiety, depression, and reduced quality of life.
🔹 7. Patient’s Expression of Pain
→ Observe verbal cues (moaning, crying, complaints).
→ Observe non-verbal cues (facial expression, body posture, restlessness).
→ Consider cultural and personal pain expressions.
✅ Pain Assessment Tools Used by Nurses:
🔹 1. Numeric Rating Scale (NRS)
→ Patient rates pain on a scale of 0–10
(0 = no pain, 10 = worst imaginable pain)
🔹 2. Visual Analogue Scale (VAS)
→ Patient marks a point on a line from “no pain” to “worst pain”
🔹 3. Wong-Baker FACES Pain Scale
→ Used for children and non-verbal patients
→ Patient chooses a face image that best describes their pain.
🔹 4. FLACC Scale (Face, Legs, Activity, Cry, Consolability)
→ Used for infants or non-verbal patients
→ Each area scored from 0–2 to assess pain behaviorally.
🔹 5. McGill Pain Questionnaire
→ Provides detailed assessment of pain description, location, and effect.
Pain assessment is a critical nursing skill that guides effective and compassionate care.
- Accurate assessment helps in selecting the right interventions, promoting patient comfort, and improving treatment outcomes.
- Nurses must assess pain consistently, objectively, and empathetically for every patient.
c) Describe the role of nurse in management of pain.
Pain is a subjective, multidimensional experience that requires holistic assessment and individualized care.
The nurse plays a central role in assessing, planning, implementing, and evaluating pain relief measures using both pharmacological and non-pharmacological approaches.
Effective pain management enhances healing, comfort, emotional well-being, and quality of life.
✅ Role of Nurse in Pain Management
🔹 1. Comprehensive Pain Assessment
→ The nurse must assess pain regularly and systematically using appropriate pain scales (e.g., Numeric Rating Scale, FLACC, Wong-Baker FACES).
- Determine location, intensity, duration, and quality of pain.
- Assess aggravating and relieving factors.
- Observe non-verbal cues of pain in non-communicative patients (grimacing, guarding, restlessness).
- Evaluate the impact of pain on sleep, appetite, mood, and mobility.
🔹 2. Planning Individualized Pain Management
→ Based on the assessment, the nurse collaborates with the healthcare team to plan care.
- Identify short-term and long-term goals of pain control.
- Consider type and source of pain (acute, chronic, neuropathic, etc.).
- Include both drug-based and supportive therapies.
- Address psychological and emotional aspects of pain.
🔹 3. Administering Pain Medications Safely
→ The nurse must follow doctor’s prescription and ensure:
- Correct drug, dose, route, and time (following 10 rights of drug administration).
- Use of opioids, NSAIDs, or adjuvants carefully based on pain severity.
- Monitor for side effects like sedation, nausea, constipation, or respiratory depression.
- Provide breakthrough (PRN) doses as ordered when pain is severe or unexpected.
🔹 4. Using Non-Pharmacological Pain Relief Methods
→ Nurses apply various supportive measures to reduce or distract from pain:
- Positioning and body alignment
- Cold or heat application
- Massage or back rubs
- Distraction techniques (music, TV, conversation)
- Relaxation exercises, deep breathing, guided imagery
- Meditation or prayer, depending on patient’s belief system
→ These methods are especially effective in mild to moderate pain, chronic pain, and post-operative recovery.
🔹 5. Emotional Support and Communication
→ The nurse provides psychological comfort and reassurance to the patient.
- Encourage the patient to express feelings and fears about their pain.
- Maintain a calm, supportive attitude and active listening.
- Involve family members to support pain management at home.
- Reduce anxiety and fear, which can worsen the perception of pain.
🔹 6. Monitoring and Reassessment
→ Evaluate the effectiveness of interventions regularly:
- Reassess pain 30–60 minutes after giving medications.
- Adjust the care plan based on response.
- Inform the doctor if pain is not relieved or worsening.
- Keep a pain management flow chart or record for continuity of care.
🔹 7. Patient and Family Education
→ Educate the patient and caregivers about:
- Purpose and timing of pain medications
- Safe use of analgesics at home
- Importance of reporting pain early rather than tolerating it
- Side effects and when to seek help
- Lifestyle measures like diet, posture, and stress control
🔹 8. Advocating for the Patient
→ The nurse acts as a patient advocate when pain is under-treated or dismissed.
- Communicate with physicians for better pain control options.
- Support the patient’s right to pain relief.
- Ensure ethical, safe, and patient-centered pain management.
The nurse plays a pivotal role in effective pain management through:
- Timely assessment,
- Safe medication administration,
- Supportive therapies, and
- Ongoing evaluation.
With compassionate care and clinical expertise, nurses help patients move from pain to comfort, thereby improving overall health outcomes.
IL . Write notes on:
1.Difference between medical diagnosis and nursing diagnosis
A medical diagnosis refers to the identification of a specific disease or medical condition based on clinical signs, symptoms, physical examination, and diagnostic tests. It reflects the pathological state of the body.
In contrast, a nursing diagnosis refers to the clinical judgment made by a nurse about the patient’s response to actual or potential health problems. It focuses on the human response rather than the disease itself.
🔹 2. Focus:
The medical diagnosis focuses primarily on disease pathology, organ systems, and the treatment or cure of the illness.
On the other hand, the nursing diagnosis focuses on holistic care, which includes physical, psychological, emotional, spiritual, and social responses of the patient to the illness or health condition.
🔹 3. Who Makes the Diagnosis:
A medical diagnosis is made only by a licensed physician or medical practitioner based on diagnostic tools like laboratory investigations, imaging, and physical assessments.
A nursing diagnosis is made by a registered nurse, using data obtained from nursing assessment, observations, and patient interviews.
🔹 4. Basis of Diagnosis:
The medical diagnosis is based on objective clinical data, such as lab reports, radiological findings, and disease-specific signs.
In contrast, the nursing diagnosis is based on subjective and objective nursing data, including patient behavior, lifestyle, verbal statements, and physical symptoms observed during care.
🔹 5. Examples:
An example of a medical diagnosis would be:
- Pneumonia
- Diabetes Mellitus
- Hypertension
An example of a nursing diagnosis would be:
- Ineffective airway clearance related to retained secretions
- Imbalanced nutrition less than body requirements
- Anxiety related to hospitalization or unfamiliar environment
🔹 6. Interventions and Management:
A medical diagnosis requires medical or surgical interventions such as prescribing medications, performing surgery, or other treatments.
A nursing diagnosis guides the nurse to create a nursing care plan involving interventions like repositioning, patient education, monitoring, emotional support, and assisting with activities of daily living.
🔹 7. Duration and Stability:
A medical diagnosis typically remains unchanged during the course of hospitalization unless a new condition develops.
A nursing diagnosis may change frequently based on the patient’s condition, response to care, and recovery status.
🔹 8. Goal of Each Diagnosis:
The goal of a medical diagnosis is to cure or manage the underlying disease or pathology.
The goal of a nursing diagnosis is to promote comfort, prevent complications, enhance recovery, and support patient well-being through nursing interventions.
In summary, the medical diagnosis identifies the disease, while the nursing diagnosis identifies the patient’s response to that disease.
Both are essential for comprehensive, collaborative patient care—the doctor treats the disease, and the nurse cares for the person.
2.Nurses responsibility in caring of unconscious patient.
An unconscious patient is unable to respond to stimuli and lacks awareness of their environment.
Such patients are at high risk of complications like aspiration, pressure sores, contractures, infection, and respiratory failure.
Therefore, the nurse has a vital role in providing holistic, continuous, and vigilant care to ensure the patient’s safety, comfort, and recovery.
✅ Nursing Responsibilities in the Care of an Unconscious Patient
🔹 1. Airway Management and Breathing Support
→ It is the nurse’s first responsibility to maintain a clear and patent airway to prevent aspiration or respiratory arrest.
- Position the patient in a lateral (side-lying) or semi-prone position to facilitate drainage of secretions.
- Use oral or nasal airways if required to prevent tongue obstruction.
- Perform oropharyngeal suctioning to remove mucus and secretions.
- Monitor respiratory rate, oxygen saturation, and chest movements regularly.
- Administer humidified oxygen as per physician’s order.
🔹 2. Circulation and Vital Signs Monitoring
→ Continuous monitoring of circulatory status is essential to detect shock or deterioration.
- Record blood pressure, pulse, temperature, and respiration every 15 minutes to 2 hours, based on condition.
- Maintain intravenous lines for fluid and drug administration.
- Monitor central venous pressure (CVP) if indicated.
- Check for cyanosis, cold extremities, or delayed capillary refill.
🔹 3. Nutrition and Fluid Balance
→ Unconscious patients cannot eat or drink orally, so nutritional support must be ensured.
- Administer IV fluids, enteral feeds via nasogastric tube, or parenteral nutrition as prescribed.
- Monitor input and output (I/O chart) to avoid dehydration or fluid overload.
- Monitor for electrolyte imbalances through laboratory investigations.
🔹 4. Eye Care
→ Lack of blinking in unconscious patients can lead to corneal dryness, ulceration, or infection.
- Clean the eyes with sterile saline or distilled water twice a day.
- Apply lubricating eye drops or ointments to prevent dryness.
- Keep the eyelids closed with moist gauze or tape if ordered.
🔹 5. Mouth and Oral Care
→ Oral hygiene prevents dry mouth, infection, and aspiration pneumonia.
- Provide oral care every 4–6 hours using swabs or toothbrush.
- Clean the tongue, teeth, gums, and inner cheeks gently.
- Use chlorhexidine or saline solution if prescribed.
🔹 6. Skin Integrity and Pressure Ulcer Prevention
→ Immobility increases the risk of bedsores or pressure injuries.
- Turn the patient every 2 hours using a turning schedule.
- Use air, water, or foam mattresses to reduce pressure.
- Perform daily back care and massage pressure points.
- Keep the skin dry, clean, and well-moisturized.
🔹 7. Urinary and Bowel Elimination
→ The nurse must manage incontinence or retention in unconscious patients.
- Insert and maintain a urinary catheter if prescribed; monitor urine output.
- Observe for signs of urinary tract infection.
- Perform rectal care if the patient has diarrhea or incontinence.
- Monitor for constipation or bowel impaction; administer enemas/laxatives as ordered.
🔹 8. Passive Range of Motion (ROM) Exercises
→ To prevent joint stiffness, muscle atrophy, and contractures, the nurse must:
- Perform passive ROM exercises for all joints at least twice daily.
- Encourage limb elevation to reduce swelling and promote circulation.
- Use splints or pillows to maintain body alignment.
🔹 9. Psychological and Emotional Support
→ Even unconscious patients may have some level of awareness.
- Speak calmly and respectfully to the patient.
- Encourage family members to talk, touch, or pray with the patient.
- Provide a calm and quiet environment to promote healing.
🔹 10. Monitoring Neurological Status
→ It is critical to assess and document changes in consciousness.
- Use Glasgow Coma Scale (GCS) to assess level of consciousness regularly.
- Observe for pupil response, limb movement, reflexes, and posturing.
- Report any deterioration in GCS or new signs (e.g., seizures, vomiting).
🔹 11. Documentation and Communication
→ Accurate records support patient safety and continuity of care.
- Record all care given, vital signs, neurological status, and interventions.
- Notify the physician of any abnormal findings or deterioration.
- Coordinate with doctors, physiotherapists, dietitians, and family for holistic care.
The care of an unconscious patient requires vigilance, compassion, skill, and scientific knowledge.
- Nurses must deliver meticulous care to maintain vital functions, prevent complications, and promote recovery.
- The nurse plays a central role in ensuring the patient’s safety, dignity, and comfort during this vulnerable state.
3.Oxygen administration.
Oxygen administration is a therapeutic procedure used to deliver oxygen gas to a patient to maintain or restore normal oxygen levels in the blood.
→ It is considered a drug and must be administered with care and precision to prevent both hypoxia (low oxygen) and oxygen toxicity.
✅ Definition:
Oxygen administration is the process of providing supplemental oxygen to individuals who are unable to maintain adequate oxygen saturation through room air alone.
✅ Purpose of Oxygen Therapy:
- To prevent or correct hypoxemia (low blood oxygen).
- To reduce work of breathing and relieve dyspnea.
- To enhance oxygen delivery to tissues and organs.
- To maintain oxygen saturation (SpO₂) at or above target levels.
- To support recovery in post-operative or critically ill patients.
✅ Indications for Oxygen Administration:
- Hypoxia and hypoxemia
- Respiratory distress or respiratory failure
- Chronic obstructive pulmonary disease (COPD)
- Cardiac conditions (e.g., myocardial infarction, heart failure)
- Shock and trauma
- Post-operative recovery
- Anemia or major blood loss
- Carbon monoxide poisoning
- Neonatal respiratory distress syndrome
- During cardiopulmonary resuscitation (CPR)
✅ Methods of Oxygen Administration:
Oxygen is delivered using various low-flow or high-flow systems depending on patient needs:
🔹 1. Nasal Cannula
→ Delivers 1–6 L/min of oxygen (24%–44% FiO₂)
→ Used for mild hypoxia in conscious, cooperative patients.
🔹 2. Simple Face Mask
→ Delivers 5–10 L/min (40%–60% oxygen)
→ Used when higher oxygen concentration is needed.
🔹 3. Non-Rebreather Mask (NRB)
→ Delivers 10–15 L/min (up to 90%–100% oxygen)
→ Used in emergency or critical care settings.
🔹 4. Venturi Mask
→ Provides a fixed, precise oxygen concentration (24%–50%)
→ Preferred in COPD patients to avoid over-oxygenation.
🔹 5. Oxygen Hood or Tent
→ Used in neonates and small children to provide humidified oxygen.
🔹 6. Mechanical Ventilation
→ Used in ICU settings for patients who are intubated or unable to breathe independently.
🔹 7. Bag-Valve-Mask (BVM) or Ambu Bag
→ Used in CPR or when patient is apneic, delivering 100% oxygen.
✅ Principles of Oxygen Administration:
- Oxygen is considered a drug and requires a physician’s order.
- Always use the appropriate delivery device based on the patient’s need.
- Use humidification for flow rates above 4 L/min to avoid mucosal dryness.
- Monitor oxygen saturation (SpO₂) and adjust flow rate accordingly.
- Avoid sources of ignition or sparks near oxygen – oxygen supports combustion.
- Provide oxygen in the lowest effective concentration to avoid toxicity.
✅ Nursing Responsibilities in Oxygen Administration:
🔸 1. Assessment Before and During Therapy:
- Check for signs of hypoxia (cyanosis, restlessness, tachypnea).
- Measure SpO₂ using a pulse oximeter.
- Monitor vital signs and level of consciousness.
- Observe for breathing pattern, rate, and effort.
🔸 2. Equipment Handling:
- Select the correct oxygen delivery device.
- Ensure the flow meter is set correctly and tubing is not kinked.
- Use a humidifier if needed.
- Check the oxygen source (central supply or cylinder) for adequate pressure.
🔸 3. Safety Measures:
- Keep “No Smoking – Oxygen in Use” signs near patient’s bed.
- Ensure there are no open flames, alcohol, or electrical sparks.
- Keep oxygen cylinders upright and secured to prevent falling.
🔸 4. Patient Education and Support:
- Explain the purpose and process of oxygen therapy.
- Encourage the patient not to remove the device unnecessarily.
- Offer emotional support to reduce anxiety or fear.
🔸 5. Documentation:
- Record the date, time, device used, flow rate, and patient response.
- Report any adverse reactions such as oxygen toxicity or discomfort.
✅ Complications of Oxygen Therapy (to Monitor For):
- Oxygen toxicity (especially in high concentrations for long duration)
- Dryness of nasal passages or mucosa
- Skin breakdown or pressure ulcers from mask or cannula
- Fire hazard in the presence of flammable materials
- Suppression of respiratory drive in COPD patients (if excessive oxygen is given)
Oxygen administration is a life-saving nursing intervention that must be performed with clinical skill, attention to safety, and proper monitoring.
- Nurses play a central role in assessing the need, delivering the therapy, preventing complications, and ensuring patient comfort and recovery.
4.Types of biomedical wastes and its hazards.
Biomedical waste (BMW) refers to any waste generated during diagnosis, treatment, or immunization of humans or animals or during research activities involving biological materials.
Improper handling or disposal of biomedical waste can pose serious health and environmental hazards to patients, healthcare workers, waste handlers, and the public.
✅ Types of Biomedical Waste
(As per Bio-Medical Waste Management Rules, 2016 – Government of India)
Biomedical waste is broadly categorized into four color-coded types based on segregation and disposal method:
🔹 1. Yellow Category – Infectious & Anatomical Waste
Includes:
- Human and animal anatomical waste (body parts, tissues)
- Soiled waste (dressings, bandages, cotton with blood/body fluids)
- Expired or discarded medicines
- Chemical waste (liquid waste from disinfectants)
- Microbiology and biotechnology waste
Disposal: Incineration or deep burial
🔹 2. Red Category – Contaminated Recyclable Waste
Includes:
- Tubing, catheters, IV sets, gloves
- Syringes (without needles), urine bags, suction sets
- Plastic containers and bags that have come in contact with body fluids
Disposal: Autoclaving or microwaving followed by shredding and recycling
🔹 3. White Category (Translucent) – Sharps Waste
Includes:
- Needles, syringes with fixed needles
- Scalpel blades, broken glass, razors
Disposal: Disinfection/autoclaving followed by encapsulation or shredding
🔹 4. Blue Category – Glass and Metallic Waste
Includes:
- Broken or discarded glassware
- Medicine vials and ampoules
- Metallic implants
Disposal: Disinfection or autoclaving followed by recycling
✅ Hazards of Biomedical Waste
Biomedical waste poses serious risks if not managed properly. These hazards affect healthcare workers, waste handlers, the environment, and the community.
🔸 1. Infectious Hazards
→ Waste contaminated with blood, secretions, or microbial cultures can transmit infections such as:
- HIV/AIDS
- Hepatitis B and C
- Tuberculosis, Tetanus
→ Needlestick injuries and improper handling of sharps increase risk.
🔸 2. Chemical Hazards
→ Chemical disinfectants, reagents, and drugs can cause:
- Skin burns, eye injuries, allergic reactions
- Toxic effects if inhaled or ingested (e.g., formalin, phenol)
🔸 3. Genotoxic and Cytotoxic Hazards
→ Exposure to cytotoxic drugs used in cancer treatment can cause:
- Genetic mutations
- Birth defects
- Hormonal disturbances
→ Waste handlers are especially at risk.
🔸 4. Environmental Hazards
→ Improper disposal (e.g., open burning or landfilling) causes:
- Air pollution (dioxins, furans)
- Water and soil contamination
- Harm to wildlife and aquatic life
🔸 5. Physical Hazards
→ Sharp instruments like needles, broken glass, and blades can cause:
- Cuts, punctures, and accidental injuries
- May lead to infections if contaminated
🔸 6. Social and Legal Hazards
→ Mismanagement of biomedical waste leads to:
- Public nuisance and bad image of the hospital
- Legal action under the Environment Protection Act and BMW Rules
- Potential damage to institutional credibility and compliance penalties
Biomedical waste must be handled and disposed of with strict adherence to national guidelines.
- Nurses play a key role in segregation, storage, labeling, and reporting of biomedical waste.
- Proper training, use of PPE, color-coded bins, and awareness can prevent serious health and environmental hazards.
5.Stages of wound healing.
Wound healing is a complex biological process by which the body repairs tissue damage caused by injury, surgery, or disease.
→ It involves cellular, vascular, and biochemical mechanisms and proceeds in phases, each with distinct functions and timelines.
→ Successful healing depends on oxygenation, nutrition, infection control, and overall patient health.
✅ Main Stages of Wound Healing:
There are four classic stages (or phases) of wound healing:
🔹 1. Hemostasis Phase (Immediate – within minutes of injury)
→ This is the first response to any injury, aiming to stop bleeding.
→ It begins immediately after the wound occurs.
Key events:
- Blood vessels constrict (vasoconstriction) to reduce blood flow.
- Platelets aggregate at the site to form a blood clot.
- Clot releases fibrin to form a mesh and seal the wound.
- Platelets also release cytokines and growth factors that attract immune cells.
Clinical note:
- Hemostasis is critical for initiating the healing process and preventing hemorrhage.
🔹 2. Inflammatory Phase (0–3 days post-injury)
→ This phase is marked by inflammation, redness, heat, swelling, and pain.
→ It prepares the wound for tissue repair.
Key events:
- Blood vessels dilate (vasodilation), allowing WBCs to enter the wound.
- Neutrophils arrive first to clear bacteria and debris.
- Macrophages follow, cleaning dead tissue and releasing growth factors.
- The wound may appear swollen, warm, or slightly painful.
Clinical note:
- Prolonged inflammation may delay healing or cause chronic wounds.
- Proper wound hygiene is crucial in this phase.
🔹 3. Proliferative Phase (Day 4 to Day 21)
→ This phase focuses on tissue rebuilding and granulation.
Key events:
- Fibroblasts produce collagen and extracellular matrix.
- Angiogenesis occurs – formation of new capillaries for blood supply.
- Granulation tissue forms – pink/red, moist, and bumpy in appearance.
- Re-epithelialization begins – new skin cells migrate over the wound surface.
- Wound edges start contracting to reduce the wound size.
Clinical note:
- Healthy granulation tissue is a sign of progressing healing.
- Any foul odor, discoloration, or increased pain may suggest infection.
🔹 4. Maturation or Remodeling Phase (Up to 1 year)
→ This is the final phase where the wound gains tensile strength and functionality.
Key events:
- Collagen remodeling occurs – Type III collagen is replaced by Type I.
- Scar tissue forms and reorganizes along tension lines.
- Blood vessels formed during proliferation decrease in number.
- Wound becomes stronger and flatter over time.
Clinical note:
- Scar tissue may never be as strong as the original tissue (about 70–80%).
- This phase can last weeks to months, especially in larger wounds.
✅ Summary of the Four Phases:
- Hemostasis – Immediate clot formation
- Inflammatory – Cleansing and defense
- Proliferative – Tissue growth and granulation
- Maturation – Scar formation and tissue remodeling
Wound healing is a dynamic and coordinated process involving multiple cells, growth factors, and tissue responses.
- Nurses must monitor each phase, observe for signs of infection or delayed healing, and provide appropriate care like dressing, nutrition support, hydration, and patient education to ensure optimal recovery.
III. Short answers on:(10×2=20)
1.Define sterilization.
Sterilization is defined as the complete destruction or elimination of all forms of microbial life, including bacteria, viruses, fungi, and spores, from an object or surface.
→ It is achieved through physical methods (such as heat, radiation) or chemical methods (such as gases or liquid sterilants).
2.What is haematuria
Haematuria is defined as the presence of red blood cells (RBCs) in the urine, which gives the urine a pink, red, or cola-colored appearance, depending on the amount of blood present.
✅ Types of Haematuria:
- Gross (Visible) Haematuria
→ When blood is clearly visible in the urine with the naked eye.- Microscopic Haematuria
→ When blood is not visible, but is detected during urine microscopic examination or dipstick test.
3.Define blood pressure.
Blood Pressure (BP) is defined as the force exerted by circulating blood on the walls of the arteries as it is pumped by the heart.
→ It is measured in millimeters of mercury (mmHg) and expressed as two values:
- Systolic Pressure – the pressure during heart contraction (when blood is ejected)
- Diastolic Pressure – the pressure during heart relaxation (when the heart refills)
✅ Normal Range of Blood Pressure:
- Normal BP: 120/80 mmHg
- The first number (systolic) indicates maximum pressure, and the second (diastolic) shows minimum pressure in arteries.
✅ Clinical Significance:
- BP is a vital sign indicating cardiovascular health.
- Abnormal readings may indicate hypertension, hypotension, or shock.
- It helps in diagnosing and monitoring heart diseases, kidney disorders, and stroke risk.
4.List down the sources of infection
🔹 1. Human Sources
→ Infected individuals (patients) or carriers of pathogens (e.g., tuberculosis, hepatitis).
🔹 2. Animal Sources (Zoonotic)
→ Infected animals transmitting diseases (e.g., rabies, anthrax).
🔹 3. Air
→ Droplet infections from sneezing, coughing (e.g., influenza, COVID-19).
🔹 4. Water
→ Contaminated water spreading diseases (e.g., cholera, typhoid).
🔹 5. Food
→ Spoiled or contaminated food items (e.g., food poisoning, salmonella).
🔹 6. Soil
→ Soil contaminated with bacteria or spores (e.g., tetanus, hookworm).
🔹 7. Fomites
→ Inanimate objects like linens, instruments, door handles carrying infection.
🔹 8. Insects/Vectors
→ Mosquitoes, flies, fleas transmitting diseases (e.g., malaria, dengue).
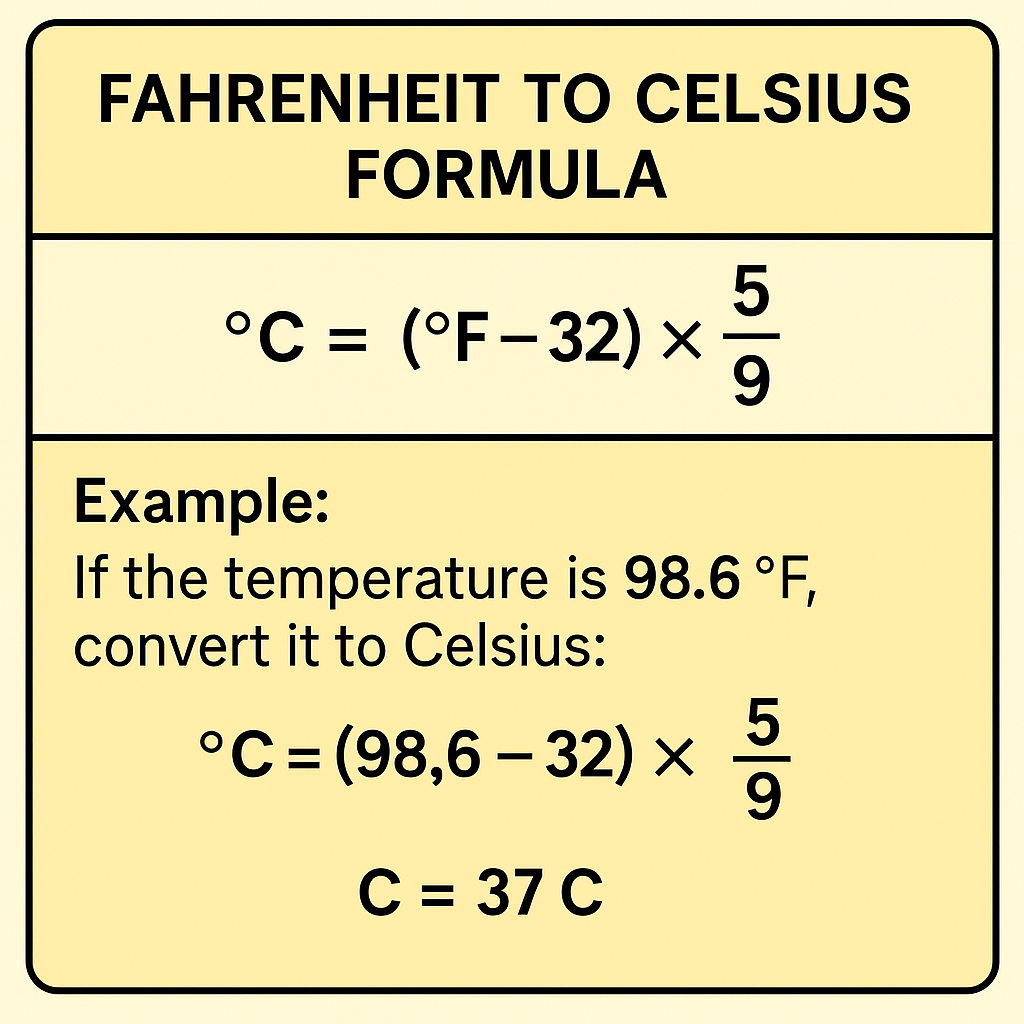
5.Formula to convert tempetature from Fahrenheit to Celsius,
6.Define respiration
Respiration is defined as a biological process in which the body breaks down glucose (or other nutrients) in the presence or absence of oxygen to produce energy, usually in the form of adenosine triphosphate (ATP), which is essential for cellular functions.
🔸 In Simple Terms:
It is the process by which oxygen is taken in, carbon dioxide is given out, and energy is produced inside the cells for body activities.
🔹 Types of Respiration:
- External Respiration
→ It is the process of exchange of gases (O₂ and CO₂) between the lungs and the environment. - Internal Respiration
→ It refers to exchange of gases between blood and body cells. - Cellular Respiration
→ It is the intracellular breakdown of glucose into ATP in the mitochondria of cells.
7.Define enema.
Enema is defined as the introduction of fluid into the rectum and lower colon through the anus for the purpose of stimulating bowel movement, relieving constipation, cleansing the bowel, or administering medications.
8 What are the complications of intravenous infusion?
Infiltration – Accidental leakage of IV fluid into surrounding tissues, causing swelling, pain, and coolness at the site.
Phlebitis – Inflammation of the vein due to irritation, presenting with redness, warmth, and tenderness along the vein.
Thrombophlebitis – Formation of a clot along with vein inflammation, leading to pain, swelling, and hardened vein.
Air Embolism – Entry of air into the vein, which may cause chest pain, dyspnea, or even cardiac arrest in severe cases.
Infection – Local or systemic infection may occur due to poor aseptic technique or prolonged IV use.
Fluid Overload – Excessive fluid administration can lead to pulmonary edema, breathlessness, and hypertension.
Allergic Reaction – Sensitivity to the infused fluid or medication may cause rash, itching, or anaphylaxis.
Hematoma – Leakage of blood into tissues due to vein injury, causing bruising and pain at the site.
9.Write four names of hospital records
Admission Register – Contains details of all patients admitted to the hospital.
Outpatient Department (OPD) Register – Records information of patients visiting for outpatient consultation.
Medical Records File – Includes patient’s history, diagnosis, treatment, and progress notes.
Discharge Summary – A report prepared at the time of patient discharge, including diagnosis, treatment given, and advice.
10 What are the contplications of immobility
Admission Register – Contains details of all patients admitted to the hospital.
Outpatient Department (OPD) Register – Records information of patients visiting for outpatient consultation.
Medical Records File – Includes patient’s history, diagnosis, treatment, and progress notes.
Discharge Summary – A report prepared at the time of patient discharge, including diagnosis, treatment given, and advice.
