B.SC-AHN-1-done-JUHI-MCQ-PENDING-NEED MODIFYING-UPLOAD NO.1
ADULT HEALTH NURSING – PAPER SOLUTION NO.1
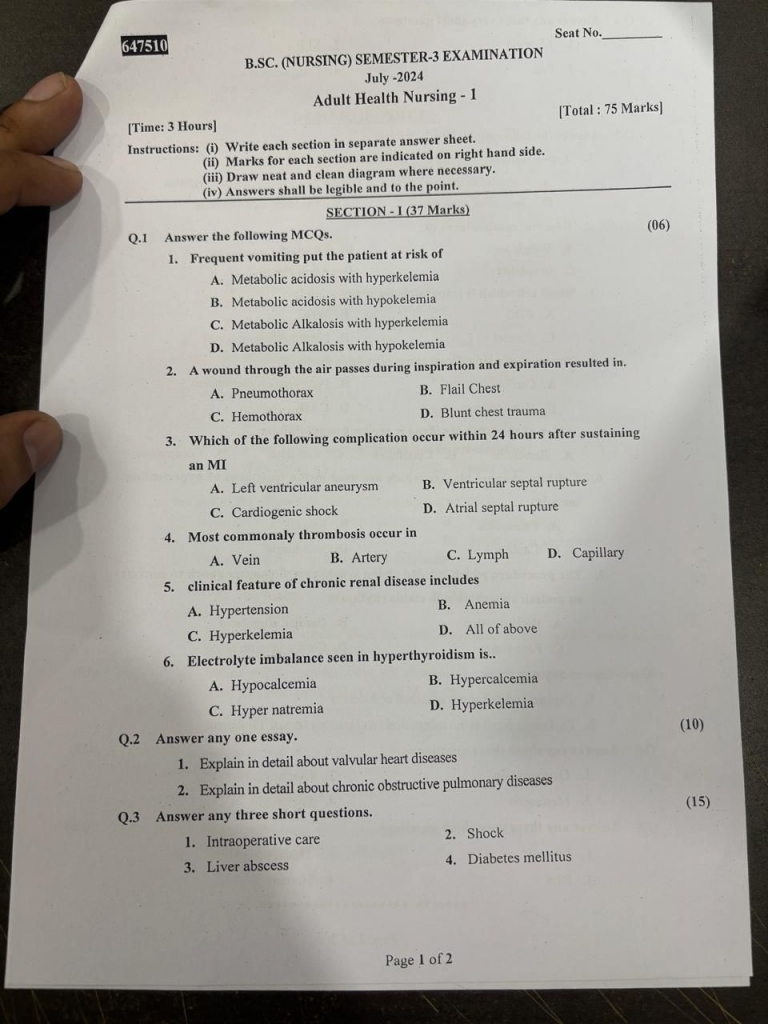
SECTION-1 (37 Marks)
Q.1 Answer the following questions – 6 marks
1. Frequent vomiting put the patient at risk of
A. Metabolic acidosis with hyperkelemia
B. Metabolic acidosis with hypokelemia
C. Metabolic Alkalosis with hyperkelemia
D. Metabolic Alkalosis with hypokelemia
2. A wound through the air passess during inspiration and expiration resulted in
A. Pneumothorax
C. Hemothorax
B. Flail Chest
D. Blunt chest trauma
3. Which of the following complication occur within 24 hours after sustaining an MI
A. Left ventricular aneurysm
B. Ventricular septal rupture
C. Cardiogenic shock
D. Atrial septal rupture
4. Most commonaly thrombosis occur in
A. Vein
B. Artery
C. Lymph
D. Capillary
5. Clinical feature of of chronic renal disease includes
A. Hypertension
B. Anemia
C. Hyperkelemia
D. All of above
6. Electrolyte imbalance seen in hyperthyrodism is
A. Hypocalcemia
B. Hypercalcemia
C. Hyper natremia
D. Hyperkelemia
Q.2 Answer any one assay (10) marks
1. Explain in detail about valvular heart diseases
Definition
Valvular Heart Disease is a condition characterized by damage or a defect in one or more of the heart valves, affecting the flow of blood through the heart. It may involve the mitral, aortic, tricuspid, or pulmonary valves, leading to either stenosis (narrowing) or regurgitation (backflow)
Etiology
Congenital Causes
Bicuspid aortic valve
Congenital stenosis
Valve prolapse syndromes
Acquired Causes
Rheumatic fever
Infective endocarditis
Myocardial infarction
Degenerative changes (aging)
Autoimmune diseases (e.g., SLE)
Radiation therapy
Types of Valvular Heart Disease
Stenosis (Valvular narrowing)
Aortic stenosis
Mitral stenosis
Pulmonary stenosis
Tricuspid stenosis
Regurgitation / Incompetence (Backflow of blood)
Aortic regurgitation
Mitral regurgitation
Tricuspid regurgitation
Pulmonary regurgitation
Mixed lesions
e.g., Mitral stenosis + Mitral regurgitation
Clinical manifestations
Dyspnea on exertion
Fatigue and weakness
Palpitations
Chest pain (angina)
Syncope or dizziness
Orthopnea & PND
Peripheral edema
Heart murmurs
Opening snap
Thrills or clicks
Diagnostic Evaluation
History collection
Physical examination
Chest X-ray
ECG
Echocardiogram (2D/Doppler)
Cardiac catheterization
Blood tests
Stress test
Medical management
Diuretics
↓ Pulmonary congestion & edema (e.g., Furosemide)
ACE Inhibitors / ARBs
↓ Afterload, ↑ cardiac output (e.g., Enalapril, Losartan)
Beta Blockers
Control heart rate, especially in AF (e.g., Metoprolol)
Digoxin
↑ Myocardial contractility, especially in heart failure with AF
Anticoagulants
Prevent thromboembolism in AF or mechanical valves (e.g., Warfarin)
Antiarrhythmics
For rhythm control (e.g., Amiodarone)
Surgical Management
Valve Repair (e.g., commissurotomy, annuloplasty)
Valve Replacement
Mechanical valves – Long-lasting, need lifelong anticoagulation
Bioprosthetic valves – Less durable, no lifelong anticoagulation
Balloon Valvuloplasty – Mainly in mitral stenosis
Nursing management
Decreased Cardiac Output related to altered preload/afterload due to valvular dysfunction evidenced by dyspnea, hypotension, weak peripheral pulses.
Goal :
To maintain adequate cardiac output and tissue perfusion.
Nursing Interventions :
Monitor vital signs, especially heart rate, BP, oxygen saturation.
Assess for signs of decreased perfusion (cool extremities, low urine output).
Administer prescribed medications: diuretics, ACE inhibitors, beta-blockers.
Monitor for arrhythmias using ECG.
Maintain semi-Fowler’s position to reduce preload.
Educate the patient to avoid activities that increase cardiac workload.
Impaired Gas Exchange related to pulmonary congestion secondary to left-sided valve disease evidenced by dyspnea, tachypnea, crackles on auscultation
Goal :
To promote effective oxygenation and prevent respiratory complications.
Nursing Interventions :
Monitor respiratory rate, rhythm, and effort.
Administer oxygen therapy as prescribed.
Elevate the head of the bed to improve lung expansion.
Encourage deep breathing and incentive spirometry.
Monitor for signs of pulmonary edema (frothy sputum, restlessness).
Collaborate with the physician for diuretic and bronchodilator therapy.
Activity Intolerance related to fatigue and reduced cardiac efficiency as evidenced by dyspnea or fatigue during minimal activity
Goal :
To improve tolerance for daily activities and conserve energy.
Nursing Interventions :
Assess baseline activity level and response to activity.
Schedule rest periods between activities.
Assist with ADLs as needed.
Encourage gradual increase in activity as tolerated.
Teach energy conservation techniques.
Monitor vital signs before, during, and after activity.
1. Explain in detail about chronic obstructive pulmonary diseases
Definition
COPD is a progressive and irreversible lung disease characterized by chronic airflow limitation due to inflammation and structural changes in the airways and alveoli. It includes chronic bronchitis and emphysema.
Etiology
Smoking (most common cause)
Air pollution
Occupational dusts and chemicals
Genetic factors (e.g., α1-antitrypsin deficiency)
Recurrent respiratory infections
Indoor air pollution (biomass fuel exposure)
Pathophysiology
→ Chronic exposure to irritants (e.g., cigarette smoke)
→ Leads to chronic inflammation in the airways and alveoli
→ Causes mucus hypersecretion, airway narrowing, and fibrosis
→ Destruction of alveolar walls (emphysema) and loss of elasticity
→ Results in air trapping and lung hyperinflation
→ Causes ventilation-perfusion mismatch, hypoxia, and hypercapnia
→ Chronic hypoxia → pulmonary hypertension → cor pulmonale
Clinical Manifestations
Chronic cough
Sputum production
Progressive dyspnea
Wheezing
Barrel-shaped chest (in emphysema)
Cyanosis
Clubbing (late stage)
Use of accessory muscles
Fatigue and weight loss
Diagnostic evaluation
History collection
Physical examination
Pulmonary function test
Chest X-ray
CT scan
Alpha 1 antitrypsin level
ABG analysis
CBC
Medical Management :
Bronchodilators
Beta-agonists : Salbutamol, Formoterol
Anticholinergics : Ipratropium, Tiotropium
Methylxanthines : Theophylline
Corticosteroids
Inhaled : Budesonide, Fluticasone
Oral (during exacerbation) : Prednisolone
Antibiotics
During infections/exacerbations
Oxygen Therapy
Low-flow O₂ to maintain SaO₂ ~ 90%
Avoid high O₂ in CO₂ retainers
Pulmonary Rehabilitation
Exercise training
Breathing techniques (pursed-lip)
Vaccination
Influenza and Pneumococcal vaccines
Smoking Cessation
Surgical Management (Advanced COPD)
Lung Volume Reduction Surgery (LVRS)
Bullectomy
Lung Transplantation
Nursing management
Impaired Gas Exchange related to alveolar-capillary membrane changes and airflow limitation
Goal :
Patient will maintain optimal gas exchange as evidenced by normal ABG and oxygen saturation > 90%.
Nursing Interventions :
Monitor respiratory rate, depth, and SpO₂ regularly
Administer supplemental oxygen as prescribed (low-flow if CO₂ retainer)
Position patient in high Fowler’s or tripod position to facilitate lung expansion
Teach pursed-lip breathing and diaphragmatic breathing
Encourage incentive spirometry use
Assess for cyanosis, restlessness, confusion (signs of hypoxia)
Ineffective Airway Clearance related to excessive mucus production and weak cough effort
Goal :
Patient will maintain a clear airway with effective cough and normal breath sounds.
Nursing Interventions :
Encourage fluid intake (if not contraindicated) to thin secretions
Provide chest physiotherapy and postural drainage as indicated
Encourage coughing and deep breathing exercises
Suction airway if necessary (esp. in acute phase)
Administer expectorants or bronchodilators as ordered
Activity Intolerance related to imbalance between oxygen supply and demand
Goal :
Patient will perform activities of daily living (ADLs) without excessive fatigue or dyspnea.
Nursing Interventions :
Assess tolerance to activity and fatigue level
Plan activities with rest periods
Provide assistance with ADLs as needed
Educate energy conservation techniques
Administer medications like bronchodilators prior to activities
Anxiety related to breathlessness and fear of suffocation
Goal :
Patient will verbalize reduced anxiety and demonstrate relaxation techniques.
Nursing Interventions :
Stay with patient during episodes of breathlessness
Use calm, reassuring communication
Teach relaxation techniques (e.g., guided imagery, controlled breathing)
Encourage expression of fears
Avoid sudden changes in care or routine
Q.3 Answer any three short questions.(15)
1. Intraoperative care
Definition
Intraoperative care refers to the nursing interventions, monitoring, and assistance provided to a patient during the actual surgical procedure in the operation theatre, from the moment the patient is brought into the operating room until transfer to the post-anesthesia care unit (PACU).
Objectives of Intraoperative Care
To ensure patient safety and comfort
To assist the surgical and anesthesia team
To maintain asepsis and sterile environment
To monitor the patient’s vital signs and overall condition
Roles and Responsibilities of the Nurse During Intraoperative Care
Pre-operative Verification
Verify patient identity, surgical consent, site, and procedure.
Ensure that all required investigations are complete and available.
Confirm NPO (nil per os) status, allergies, and prosthesis removal.
Maintain Asepsis
Follow strict aseptic technique to prevent infection.
Assist in scrubbing, gowning, and gloving of the surgical team.
Ensure all surgical instruments are sterile.
Positioning the Patient
Position the patient correctly based on the type of surgery (e.g., supine, lithotomy, prone).
Use pads and supports to prevent pressure sores and nerve injuries.
Ensure circulation, respiration, and body alignment are maintained.
Monitoring the Patient
Observe and record vital signs : heart rate, blood pressure, respiratory rate, oxygen saturation, and temperature.
Monitor for adverse reactions to anesthesia and surgical complications.
Communicate promptly with the surgical and anesthesia team.
Instrument and Sponge Count
Perform and document instrument, sponge, and needle counts before, during, and after surgery to avoid retention.
Assist the surgeon by passing instruments and handling equipment efficiently (scrub nurse role).
Specimen Handling
Collect and label specimens (e.g., tissue biopsies) accurately.
Ensure proper documentation and transport to the lab.
Documentation
Record all intraoperative events, including time of incision and closure, medications administered, fluids infused, and any complications.
Maintain accurate records in the intraoperative nursing notes.
2. Shock
Definition
Shock is a life-threatening medical emergency characterized by inadequate tissue perfusion and oxygen delivery to the cells and vital organs, leading to cellular dysfunction, organ failure, and if untreated, death
Types of shock
Hypovolemic Shock
It occurs due to a significant loss of blood or fluids from the body. Common causes include hemorrhage (internal or external), burns, vomiting, diarrhea, or severe dehydration.
Cardiogenic Shock
It is results from the heart’s inability to pump blood effectively despite adequate volume. It is most commonly caused by myocardial infarction (heart attack), but it can also result from severe arrhythmias, cardiomyopathy, or valve disorders.
Distributive Shock
It is caused by abnormal distribution of blood flow due to widespread vasodilation and increased capillary permeability. This type includes :
Septic Shock: It is caused by severe infection and release of toxins.
Anaphylactic Shock : It is caused by a severe allergic reaction.
Neurogenic Shock : It is caused by spinal cord injury or damage to the central nervous system, leading to loss of sympathetic tone.
Obstructive Shock
It occurs when there is a mechanical obstruction to blood flow in the heart or great vessels. Conditions such as pulmonary embolism, cardiac tamponade, and tension pneumothorax can impede circulation, reducing cardiac output and leading to shock despite normal heart function and volume.
clinical manifestations
Hypotension (low BP)
Tachycardia (↑ pulse)
Cold, clammy skin (except in early septic/anaphylactic shock)
Decreased urine output (<30 ml/hr)
Altered mental status – confusion, anxiety
Rapid, shallow breathing
Weak peripheral pulses
Cyanosis or pallor
Management
Airway, Breathing, Circulation (ABC)
Ensure a patent airway
Provide supplemental oxygen (high-flow or mechanical ventilation if needed)
Establish IV access with large-bore cannulas
Begin fluid resuscitation (NS or RL) – especially in hypovolemic and distributive shock
Medications
Vasopressors (e.g., norepinephrine, dopamine) – for hypotension unresponsive to fluids
Inotropes (e.g., dobutamine) – in cardiogenic shock to improve heart contractility
Antibiotics – early broad-spectrum antibiotics in septic shock
Epinephrine – first-line for anaphylactic shock
Antihistamines and corticosteroids – in anaphylaxis
Anticoagulants or thrombolytics – in obstructive shock due to pulmonary embolism
Fluid Replacement
Crystalloids (Normal saline, Ringer’s lactate) – first choice
Colloids or blood products – if there is significant blood loss
Monitor for signs of fluid overload (especially in cardiogenic shock)
Monitoring
Vital signs: BP, HR, RR, SpO₂
Urine output (goal: >30 mL/hour)
Level of consciousness
Blood gases, electrolytes, and lactate levels
Hemodynamic monitoring if available (e.g., CVP, arterial lines)
Nursing management
Continuous vital signs monitoring
Report deterioration immediately
Administer oxygen and medications as prescribed
Ensure IV fluids and blood products are given timely
Maintain asepsis to prevent sepsis
Reassure the patient and explain procedures
Record intake and output, mental status, and skin changes
3. Liver abscess
Definition
A liver abscess is a localized collection of pus within the liver parenchyma caused by infection. It results from invasion by bacteria, parasites, or fungi and leads to inflammation, necrosis, and cavity formation filled with purulent material.
Causes
Pyogenic Abscess – due to bacterial infections (e.g., E. coli, Klebsiella) from biliary tract infections, appendicitis, or trauma.
Amoebic Abscess – caused by Entamoeba histolytica via fecal-oral contamination (contaminated food/water).
Fungal Abscess – seen in immunocompromised individuals (e.g., Candida species).
Pathophysiology
Pathogen reaches the liver via portal circulation, biliary tract, or hematogenous spread
Local immune response → inflammation
Tissue necrosis → formation of cavity
Accumulation of pus → abscess formation
If untreated → rupture → peritonitis or pleural involvement
Clinical manifestations
Right upper quadrant (RUQ) pain
Tender hepatomegaly (enlarged liver)
Right shoulder referred pain (phrenic nerve irritation)
Mild jaundice (in some cases) Fever with chills and rigors
Nausea, vomiting, and anorexia
Malaise and fatigue
Night sweats
Diagnostic Evaluation
Blood Tests : WBC (leukocytosis), ESR, CRP
Liver function tests
Positive serology for Entamoeba histolytica (in ALA)
Ultrasound (USG)
CT scan / MRI
Aspiration
Medical Management
Antibiotic Therapy (Pyogenic Abscess)
Broad-spectrum IV antibiotics → then tailored based on culture
E.g. Ceftriaxone + Metronidazole
Duration : 2–6 weeks
Anti-amoebic Therapy (Amoebic Abscess)
Metronidazole is the drug of choice (7–10 days)
Followed by luminal agents (e.g., Diloxanide furoate) to eradicate intestinal cysts
Surgical Management
Percutaneous needle aspiration under ultrasound or CT guidance
Percutaneous catheter drainage if abscess is large or unresponsive
Surgical drainage – rare, used if rupture or multiple abscesses
Nursing Management
Assessment
Monitor vital signs, pain level, signs of rupture or peritonitis
Assess for dehydration, jaundice
Interventions
Administer IV fluids, antibiotics, and antipyretics as prescribed
Monitor liver function tests
Maintain strict asepsis during drainage
Provide high-protein, easily digestible diet
Educate about personal hygiene and food safety (esp. for amoebic abscess)
4. Diabetes mellitus
Definition
Diabetes Mellitus (DM) is a chronic metabolic disorder characterized by high blood glucose levels (hyperglycemia) due to deficiency or resistance to insulin action.
Types
Type 1 DM :
Insulin-dependent, usually in children
Autoimmune destruction of beta cells
Type 2 DM :
Non-insulin-dependent, common in adults
Due to insulin resistance and relative insulin deficiency
Gestational Diabetes :
Occurs during pregnancy
Usually resolves after delivery
Secondary Diabetes :
Due to other diseases (e.g., pancreatitis, Cushing’s syndrome)
Signs and Symptoms
Polyuria – frequent urination
Polydipsia – excessive thirst
Polyphagia – increased hunger
Weight loss (mostly in Type 1)
Fatigue and weakness
Delayed wound healing
Blurred vision
Diagnostic evalaution
Fasting Blood Sugar (FBS) ≥ 126 mg/dL
Random Blood Sugar (RBS) ≥ 200 mg/dL
Oral Glucose Tolerance Test (OGTT)
HbA1c ≥ 6.5%
Management
Diet control
low sugar, balanced diet
Exercise
regular physical activity
Medications
Oral hypoglycemics (e.g., Metformin) for Type 2
Insulin therapy for Type 1 or uncontrolled cases
Monitoring blood glucose regularly
Nursing management
Check blood glucose levels regularly
Monitor vital signs and signs of hypo/hyperglycemia
Administer insulin or oral hypoglycemics as prescribed
Provide a diabetic diet (low sugar, high fiber, controlled carbs)
Encourage small, frequent meals
Monitor for side effects (e.g., hypoglycemia)
Teach about medication compliance
Instruct on foot care to prevent ulcers
Explain signs of hypoglycemia/hyperglycemia
Encourage regular exercise
Promote weight control
Advise stress reduction techniques
Q.4 Answer any three very short questions.(06)
1. Alopecia
Alopecia is the partial or complete loss of hair from areas of the body, especially the scalp, where hair normally grows. It can be temporary or permanent, and caused by genetic, autoimmune, nutritional, hormonal, or stress-related factors
Common Types :
Androgenetic Alopecia – Hereditary pattern baldness
Alopecia Areata – Autoimmune, patchy hair loss
Telogen Effluvium – Temporary shedding due to stress or illness
2. Pain
Definition
Pain is an unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage. (Defined by the International Association for the Study of Pain – IASP)
Types of Pain
Acute Pain : Short-term, sudden onset (e.g., injury, surgery)
Chronic Pain : Persistent pain lasting >3 months (e.g., arthritis)
Referred pain : Felt in a location different from the source (e.g., chest pain in arm during heart attack)
3. SLE
SLE is a chronic autoimmune disease in which the body’s immune system attacks its own cells, tissues, and organs, leading to widespread inflammation and damage, commonly affecting the skin, joints, kidneys, heart, and brain.
Key Features
Butterfly-shaped rash on face
Joint pain, fatigue, fever
Photosensitivity and renal involvement
4. Lung abscess
A lung abscess is a localized collection of pus within the lung tissue caused by bacterial infection, leading to necrosis and formation of a cavity filled with purulent material. Usually occurs due to aspiration of infected material, especially in unconscious or debilitated patients. Common organisms include Staphylococcus aureus, Klebsiella pneumoniae, and anaerobes
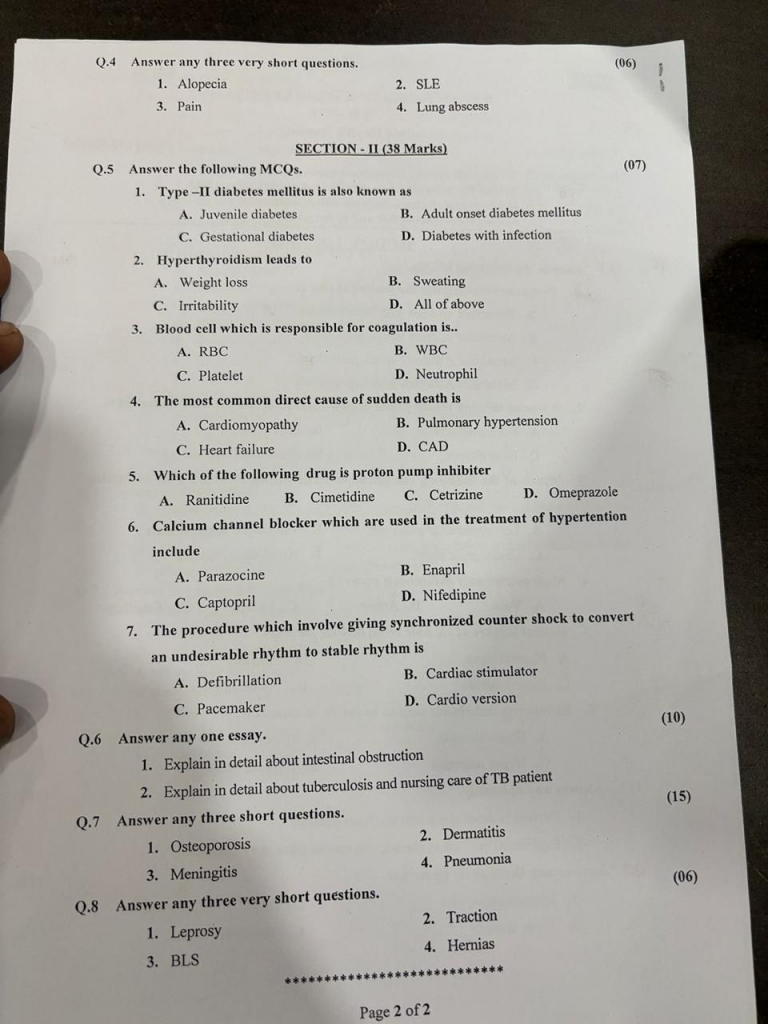
SECTION-II (38 Marks)
Q.5 Answer the following MCQs.(07)
1.Type-II diabetes mellitus is also known as
A. Juvenile diadetes
B. Adult onset diabetes mellitus
C. Gestational diabetes
D. Diabetes with infection
2. Hyperthyroidism leads to
A. Weight loss
B. Sweating
C. Irritability
D. All of above
3. Blood cell which is responsible for coagulation is…
A. RBC
B. WBC
C. Platelet
D. Neutrophil
4. The most common direct cause of sudden death is
A. Cardiomyopathy
B. Pulmonary hypertension
C. Heart failure
D. CAD
5. Which of the following drug is proton pump inhibiter
A. Ranitidine
B. Cimetidine
C. Cetrizine
D. Omeprazole
6. Calcium channel blocker which are used in the treatment of hypertention include
A. Parazocine
B. Enapril
C. Captopril
D. Nifedipine
7. The procedure which involve giving synchronized counter shock to convert an undesirable rhythm to stable rhythm is
A. Defibrillation
B. Cardiac stimulator
C. Pacemaker
D. Cardio version
Q.6 Answer any one essay (10) marks
1.Explain in detail about intestinal obstruction
Definition
Intestinal obstruction is a blockage in the intestinal tract that prevents the normal flow of gastric contents, either partially or completely. It can affect the small or large intestine, leading to distension, fluid accumulation, and compromised blood supply.
Types of Intestinal Obstruction
Mechanical Obstruction – Physical blockage
Examples : Hernia, tumors, adhesions, volvulus, intussusception, strictures
Non-mechanical / Functional Obstruction (Paralytic Ileus) – Absence of peristalsis
Causes : Post-operative state, electrolyte imbalance, infection, drugs
Etiology
Mechanical Causes
Post-surgical adhesions (most common cause)
Incarcerated hernia
Tumors (e.g., colorectal cancer)
Intussusception (common in children)
Volvulus (twisting of bowel)
Foreign bodies or impacted feces
Non-Mechanical Causes
Paralytic ileus (post-operative or due to infection)
Neurological disorders (e.g., Parkinson’s)
Electrolyte imbalance (especially hypokalemia)
Medications (e.g., opioids, anticholinergics)
Clinical Features / Symptoms
Abdominal pain and cramping
Abdominal distension
Nausea and vomiting (may be fecal-smelling in severe cases)
Constipation and obstipation (no flatus or feces passed)
Hyperactive bowel sounds (early) or absent bowel sounds (late)
Signs of dehydration and electrolyte imbalance
Diagnostic Evaluation
X-ray Abdomen (erect) – shows air-fluid levels
CT scan – identifies the site and cause of obstruction
Ultrasound – especially useful in intussusception
CBC – shows leukocytosis in infection
Electrolyte panel – to assess imbalances
Lactate levels – to detect ischemia or perforation
Initial (Conservative) Management
NPO (Nil per oral) – Rest the bowel
IV fluids – Correct dehydration
Electrolyte correction – Especially potassium
Nasogastric tube (NGT) – For decompression
Analgesics & Antiemetics – For pain and vomiting
Antibiotics – If infection or perforation suspected
Surgical Management (if needed)
Exploratory laparotomy – To identify and relieve obstruction
Resection and anastomosis – For necrotic bowel
Colostomy/Ileostomy – In selected cases
Reduction of volvulus or intussusception
Pre-operative Nursing Management
Assessment and Monitoring
Monitor vital signs (especially temperature, pulse, BP, respiration)
Assess abdominal distension, bowel sounds, and pain
Monitor intake-output chart, watch for dehydration
Gastrointestinal Rest
Keep patient NPO (Nil Per Os = nothing by mouth)
Insert and maintain nasogastric (NG) tube for decompression
Monitor NG output: color, amount, consistency
Fluid and Electrolyte Balance
Start IV fluids (e.g., Normal saline with KCl)
Correct electrolyte imbalances (especially sodium, potassium)
Medication Administration
Administer antibiotics, antiemetics, and analgesics as prescribed
Avoid opioid overuse (as it slows bowel motility)
Psychological Support
Provide emotional reassurance to reduce anxiety
Explain the need for surgery and procedure in simple terms
Pre-op Preparation
Assist in obtaining informed consent
Ensure pre-op investigations are completed: CBC, ECG, LFTs, X-ray, CT
Perform skin preparation (abdominal area shaved and cleaned)
Check for NPO compliance and remove dentures/jewelry
Post-operative Nursing Management
Monitoring and Assessment
Regularly monitor vital signs, especially for signs of shock, bleeding, infection
Assess surgical site for redness, discharge, swelling
Observe for return of bowel sounds and flatus
Pain Management
Administer analgesics as prescribed
Encourage early reporting of severe pain or abdominal tightness
Wound and Drain Care
Perform dressing changes under sterile technique
Monitor surgical drains or stoma, if present
Early Ambulation and DVT Prevention
Encourage deep breathing exercises, leg movements, and walking as early as possible
Use compression stockings or low-dose heparin if prescribed
Nutrition and Fluids
Gradual reintroduction of oral fluids → soft diet → regular diet
Continue IV fluids until bowel function resumes
Elimination and NG Tube Care
Continue NG suctioning if needed
Monitor for signs of ileus (no bowel movement after surgery)
Patient and Family Education
Educate about wound care, diet, medication adherence
Teach signs of complications like infection, hernia, constipation
2.Explain in detail about tuberculosis and nursing care of TB patient
Definition
Tuberculosis (TB) is a chronic, contagious bacterial infection caused by Mycobacterium tuberculosis, mainly affecting the lungs (pulmonary TB), but it can also affect other organs (extrapulmonary TB).
Causative Organism
Mycobacterium tuberculosis – an acid-fast bacillus
Other species: M. bovis, M. africanum
Mode of Transmission
Airborne droplets released when an infected person coughs, sneezes, or speaks
Close and prolonged person-to-person contact
Types of TB
Pulmonary TB – Lungs
Extrapulmonary TB – Lymph nodes, bones, kidneys, brain, spine
Miliary TB – Widespread TB throughout body via bloodstream
Latent TB – Infection present but no active disease or symptoms
Clinical manifestations
Persistent cough (>2 weeks)
Fever with evening rise of temperature
Night sweats
Weight loss, loss of appetite
Hemoptysis (blood in sputum)
Chest pain and difficulty in breathing
Diagnostic Evaluation
Sputum AFB smear (Ziehl-Neelsen stain)
CBNAAT / GeneXpert test for rapid TB DNA detection
Chest X-ray
Mantoux test (Tuberculin skin test)
Blood tests: ESR, CBC
CT Scan/MRI in extrapulmonary TB
Medical Management
Under DOTS (Directly Observed Treatment Short-course) program:
Intensive Phase (2 months):
H = Isoniazid
R = Rifampicin
Z = Pyrazinamide
E = Ethambutol
Continuation Phase (4 months):
H + R (Isoniazid and Rifampicin)
Nursing care of TB patient
Assessment
Monitor vital signs regularly (especially temperature and respiratory rate)
Observe for cough characteristics (productive, blood-tinged)
Assess for weight loss, fatigue, appetite loss
Check for compliance with treatment (DOTS)
Medication Administration
Administer anti-tubercular drugs (ATT) as prescribed
(e.g., Isoniazid, Rifampicin, Ethambutol, Pyrazinamide)
Watch for side effects (e.g., liver toxicity, visual disturbances)
Ensure Directly Observed Treatment Short-course (DOTS) for compliance
Infection Control & Isolation
Place patient in a well-ventilated room or isolation if infectious
Use N95 mask or triple-layer surgical mask
Practice cough etiquette and hand hygiene
Educate family on infection prevention
Nutritional Support
Provide high-protein, high-calorie diet
Encourage vitamin-rich foods (Vitamin A, C, B-complex)
Monitor weight gain or loss weekly
Ensure adequate hydration
Health Education
Educate patient and family about:
Importance of drug adherence
6–9 months therapy duration
Prevention of drug resistance
Avoiding alcohol and smoking
Follow-up and sputum testing
Psychosocial Support
Provide emotional support (due to stigma and isolation)
Encourage expression of fears and concerns
Support continuation of work/school with precautions
Documentation
Record medication given, response, side effects
Document patient education and family teaching
Maintain DOTS records if applicable
Complication Prevention
Monitor for signs of hepatotoxicity, drug resistance, hemoptysis
Ensure prompt referral if complications arise
Q.7 Answer any three short questions (15) marks
1. Osteoporosis
Definition
Osteoporosis is a chronic, progressive metabolic bone disease characterized by low bone mass, deterioration of bone tissue, and increased bone fragility, leading to a higher risk of fractures — especially in the hip, spine, and wrist.
Causes / Risk Factors
Aging (postmenopausal women at higher risk)
Hormonal imbalance (↓ Estrogen, ↓ Testosterone)
Calcium or Vitamin D deficiency
Sedentary lifestyle
Long-term corticosteroid use
Smoking and alcohol consumption
Family history of osteoporosis
Clinical manifestations
Back pain (due to vertebral compression)
Loss of height over time
Stooped posture (kyphosis)
Fragile bones and frequent fractures
Often asymptomatic until a fracture occurs
Diagnostic Evaluation
History collection
Physical examination
Bone Mineral Density (BMD) Test – DEXA scan
X-rays (may show fractures or bone thinning)
Blood tests – calcium, vitamin D, thyroid levels
Medical Management
Calcium and Vitamin D supplementation
Bisphosphonates (e.g., Alendronate, Risedronate) – to reduce bone loss
Hormone Replacement Therapy (HRT) (for postmenopausal women)
Calcitonin, Selective Estrogen Receptor Modulators (SERMs)
Weight-bearing exercises to strengthen bones
Nursing Management
Educate patient on fall prevention and home safety
Promote calcium-rich diet (milk, leafy greens, tofu)
Encourage regular exercise like walking or yoga
Monitor for signs of fracture or mobility issues
Ensure adherence to medication and supplement regimen
2. Meningitis
Definition
Meningitis is an inflammation of the meninges, the protective membranes covering the brain and spinal cord, usually caused by bacteria, viruses, fungi, or other microorganisms.
Etiology
Bacterial : Neisseria meningitidis, Streptococcus pneumoniae, Haemophilus influenzae
Viral : Enteroviruses, Herpes simplex virus (HSV), Mumps virus
Fungal : Cryptococcus neoformans (common in immunocompromised patients)
Others : Tuberculous meningitis, parasitic causes, drug-induced
Clinical manifestations
High fever and chills
Severe headache
Neck stiffness (nuchal rigidity)
Nausea and vomiting
Photophobia (sensitivity to light)
Altered level of consciousness or confusion
Seizures (in severe cases)
Positive Kernig’s and Brudzinski’s signs
Diagnostic evaluation
History collection
Physical examination
Lumbar puncture – CSF analysis (gold standard)
CT or MRI brain (if raised ICP suspected)
Blood cultures
CBC, CRP, ESR
Medical Management
Antibiotics : Ceftriaxone, Vancomycin (for bacterial meningitis)
Antiviral drugs : Acyclovir (for HSV meningitis)
Antifungals : Amphotericin B (for fungal meningitis)
Corticosteroids : To reduce inflammation
Antipyretics and analgesics for symptom relief
IV fluids and oxygen therapy if required
Nursing Management
Monitor neurological status and vital signs
Maintain isolation precautions (especially for bacterial meningitis)
Ensure quiet and dim environment
Administer medications as prescribed
Provide fluid balance and prevent complications like seizures
Educate family on vaccination and follow-up
3. Deamatitis
Definition
Dermatitis is a general term for inflammation of the skin, characterized by redness, itching, swelling, and sometimes blistering or oozing. It may be acute or chronic, and caused by allergic, irritant, or autoimmune factors.
Etiology
Irritants : Soaps, detergents, acids, or chemicals
Allergens : Plants (e.g., poison ivy), cosmetics, jewelry (nickel), dust mites
Infections : Fungal or bacterial infections
Autoimmune conditions : Eczema, seborrheic dermatitis
Genetic predisposition (e.g., in atopic dermatitis)
Types of Dermatitis
Atopic Dermatitis (Eczema)
Contact Dermatitis (Irritant or Allergic)
Seborrheic Dermatitis
Nummular Dermatitis
Stasis Dermatitis (related to poor circulation)
Clinical manifestation
Redness and rash
Itching and irritation
Swelling and pain
Dry, flaky, or scaly skin
Blisters or oozing lesions (in acute phase)
Cracking or thickened skin (in chronic phase)
Medical Management
Topical corticosteroids (e.g., Hydrocortisone)
Antihistamines (e.g., Cetirizine) to relieve itching
Moisturizers and emollients for hydration
Antibiotics (if secondary infection present)
Avoidance of known irritants/allergens
Nursing Management
Educate the patient on skin care and avoiding triggers
Monitor for secondary infection
Encourage cool compresses for symptom relief
Administer prescribed topical and oral medications
Promote psychological comfort due to appearance concerns
4. Pneumonia
Definition
Pneumonia is an inflammatory condition of the lung parenchyma, primarily affecting the alveoli, caused by infection with bacteria, viruses, fungi, or other organisms.
Causes
Bacterial: Streptococcus pneumoniae, Haemophilus influenzae
Viral: Influenza virus, Respiratory syncytial virus (RSV)
Fungal: Pneumocystis jirovecii (especially in immunocompromised patients)
Aspiration: Inhalation of food, fluid, or vomitus
Types
Community-acquired pneumonia (CAP)
Hospital-acquired pneumonia (HAP)
Aspiration pneumonia
Ventilator-associated pneumonia (VAP)
Clinical manifestations
Fever and chills
Productive or dry cough
Chest pain (pleuritic)
Dyspnea (difficulty breathing)
Fatigue, weakness
Crackles or decreased breath sounds on auscultation
Diagnostic evaluation
History collection
Physical examination
Chest X-ray
Complete blood count (CBC)
Sputum culture
Pulse oximetry
Arterial Blood Gas (ABG)
Management
Antibiotic Therapy (for bacterial pneumonia):
First-line: Amoxicillin, Azithromycin, Ceftriaxone, Levofloxacin
Based on sputum culture sensitivity
Antiviral Therapy (for viral pneumonia):
E.g., Oseltamivir for Influenza
Symptomatic management for mild cases
Antifungal Therapy:
E.g., Amphotericin B, Fluconazole (for fungal pneumonia)
Supportive Medications:
Antipyretics (Paracetamol) – for fever
Bronchodilators (Salbutamol) – to ease breathing
Mucolytics/Expectorants (Ambroxol) – to loosen mucus
Corticosteroids (in severe inflammation)
Oxygen Therapy
Administered if SpO₂ < 92%
Nasal cannula or face mask, depending on severity
Continuous monitoring of oxygen saturation
Nursing management
Monitor vital signs (especially temperature, respiratory rate, and oxygen saturation).
Assess for breath sounds (crackles, wheezes, decreased sounds).
Evaluate cough characteristics (productive/non-productive, sputum color).
Observe for signs of hypoxia (cyanosis, confusion).
Administer Medications as Prescribed.
Administer oxygen as per doctor’s order if SpO₂ < 92%.
Encourage oral fluids (2–3 L/day) to loosen secretions.
Maintain IV fluids if patient is unable to take orally
Position in semi-Fowler’s or high Fowler’s to promote lung expansion.
Encourage frequent position changes to prevent hypostatic pneumonia.
Promote rest and limit strenuous activity.
Teach and encourage deep breathing and coughing exercises.
Q.8 Answer any three very short questions (6) marks
1. Leprosy
Leprosy is also called Hansen’s Disease. It is a chronic infectious disease caused by Mycobacterium leprae that primarily affects the skin, peripheral nerves, mucosa of the upper respiratory tract, and eyes. It spreads through prolonged close contact via nasal droplets. Early diagnosis and multi-drug therapy (MDT) are essential to prevent deformities and transmission.
2. BLS
Basic Life Support (BLS) is an emergency medical procedure used to maintain airway, breathing, and circulation in a person experiencing cardiac arrest, respiratory failure, or choking. It includes CPR (cardiopulmonary resuscitation), rescue breathing, and use of an AED (automated external defibrillator) until advanced care is available.
3. Traction
Traction is a therapeutic method used to align and stabilize fractured bones or dislocated joints by applying a steady pulling force. It helps in reducing pain, correcting deformities, and maintaining proper bone position during healing. Types include skin traction and skeletal traction.
4. Hernia
A hernia is the protrusion of an organ or tissue through a weak spot in the surrounding muscle or connective tissue. It commonly occurs in the abdominal wall, especially in areas like the inguinal, umbilical, or femoral region. Symptoms may include a visible bulge, pain, or discomfort, especially while lifting or coughing.
💥WELCOME TO MY NURSING APP FAMILY💥
KINDLY SEND YOUR UNIVERSITY PAPER FOR SAMPLE SOLUTION OR FOR MORE INFO CONTACT US ON-CALL/WATSAPP – 8485976407
