MICRO-PAPER SOLUTION-B.SC-AUG.2024-Sau.Uni.(NO.1)
PAPER SOLUTION B.SC-APPLIED MICRO & INFECTION CONTROLINCLUDING SAFETY
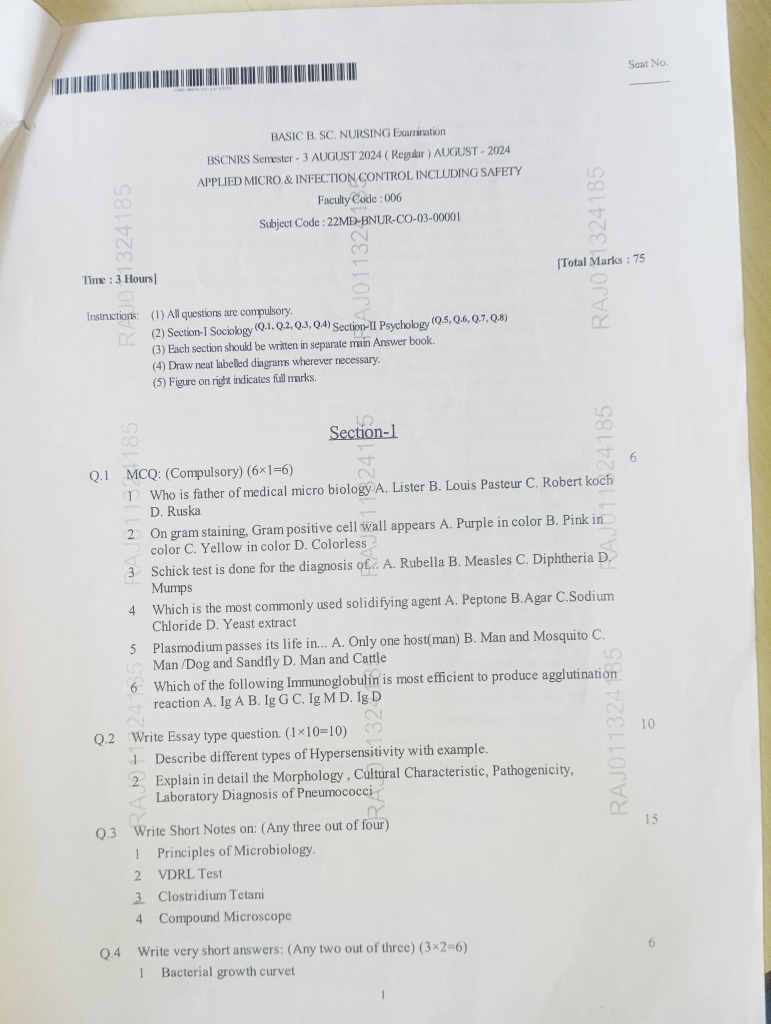
Q.1 MCQ: (Compulsory) (6×1=6)
ANSWER :-
1 Who is father of medical micro biology
A. Lister
B. Louis Pasteur
C. Robert koch 👍
D. Ruska
2 On gram staining, Gram positive cell wall appears
A. Purple in color💜
B. Pink in color
C. Yellow in color
D. Colorless
3 Schick test is done for the diagnosis of. A. Rubella B. Measles C. Diphtheria D. Mumps
4 Which is the most commonly used solidifying agent A. Peptone B.Agar C.Sodium Chloride D. Yeast extract
5 Plasmodium passes its life in… A. Only one host(man) B. Man and Mosquito C. Man/Dog and Sandfly D. Man and Cattle
6 Which of the following Immunoglobulin is most efficient to produce agglutination reaction A. Ig A B. Ig G C. Ig M D. Ig D
Q.2 Write Essay type question (1×10=10)
Q-1.Describe different types of Hypersensitivity with example.
ANSWER :-
Types of Hypersensitivity Reactions (Gell and Coombs Classification)
Hypersensitivity reactions are exaggerated or inappropriate immune responses to antigens, which may lead to tissue injury, inflammation, or dysfunction. These responses are typically classified into four types based on the immune mechanisms involved, as proposed by Gell and Coombs.
Type I: Immediate (Anaphylactic) Hypersensitivity
This type of hypersensitivity is mediated by IgE antibodies and is characterized by an immediate reaction (within seconds to minutes) following exposure to a specific allergen. It is commonly seen in atopic individuals.
- Mechanism: On the first exposure, allergens stimulate B cells to produce IgE antibodies, which bind to Fc receptors on mast cells and basophils (a process called sensitization). Upon re-exposure, the allergen cross-links the bound IgE, causing rapid degranulation of mast cells, releasing histamine, leukotrienes, prostaglandins, and cytokines.
- Pathophysiology: These mediators cause vasodilation, increased vascular permeability, smooth muscle contraction, and mucus secretion, leading to clinical symptoms.
- Onset: Within seconds to minutes.
- Clinical Manifestations:
- Local reactions: Allergic rhinitis (hay fever), bronchial asthma, atopic dermatitis (eczema), urticaria (hives)
- Systemic reaction: Anaphylaxis – a potentially life-threatening condition with hypotension, bronchospasm, and laryngeal edema.
- Examples:
- Allergies to food (e.g., peanuts, shellfish), drugs (e.g., penicillin), insect stings (e.g., bee sting), and pollen.
Type II: Antibody-Mediated (Cytotoxic) Hypersensitivity
Type II reactions are mediated by IgG or IgM antibodies directed against antigens on host cell surfaces or tissues, leading to cell destruction, inflammation, or cellular dysfunction.
- Mechanism: Antibodies bind to self or foreign antigens present on cell membranes or extracellular matrix. These bound antibodies activate the complement system or mediate antibody-dependent cellular cytotoxicity (ADCC), leading to cell lysis or tissue damage.
- Onset: Minutes to hours.
- Three main outcomes:
- Complement-mediated lysis (e.g., in mismatched blood transfusion)
- Opsonization and phagocytosis (e.g., autoimmune hemolytic anemia)
- Cellular dysfunction without destruction (e.g., myasthenia gravis)
- Clinical Manifestations: Hemolysis, thrombocytopenia, inflammation of basement membranes.
- Examples:
- Hemolytic transfusion reactions
- Erythroblastosis fetalis (hemolytic disease of the newborn)
- Goodpasture’s syndrome (anti-GBM disease)
- Autoimmune hemolytic anemia
- Pemphigus vulgaris
- Myasthenia gravis (neuromuscular junction dysfunction)
Type III: Immune Complex-Mediated Hypersensitivity
This type of hypersensitivity involves the formation of immune complexes (antigen-antibody complexes), usually composed of IgG or IgM, which circulate in the bloodstream and deposit in tissues, triggering complement activation and inflammation.
- Mechanism: Soluble antigens combine with antibodies to form immune complexes, which are deposited in various tissues (e.g., blood vessels, kidneys, joints). The deposited complexes activate complement, attracting neutrophils that release enzymes and reactive oxygen species, causing tissue injury.
- Onset: Typically occurs 6–12 hours after antigen exposure.
- Tissue Damage Sites: Glomeruli, synovial membranes, blood vessels, and skin.
- Clinical Manifestations: Fever, rash, arthralgia, proteinuria, vasculitis, nephritis.
- Examples:
- Systemic lupus erythematosus (SLE)
- Post-streptococcal glomerulonephritis
- Serum sickness (e.g., following anti-toxin therapy)
- Arthus reaction (localized dermal vasculitis after injection)
- Rheumatoid arthritis (partly)
Type IV: Delayed-Type (Cell-Mediated) Hypersensitivity
Type IV reactions are T-cell-mediated and do not involve antibodies. The reaction occurs 24–72 hours after antigen exposure, hence the name “delayed” hypersensitivity.
- Mechanism:
- CD4+ T-helper (Th1) cells recognize antigens presented by antigen-presenting cells (APCs), leading to cytokine release, macrophage recruitment, and inflammation.
- In some cases, CD8+ cytotoxic T-cells directly destroy target cells (e.g., graft rejection).
- Onset: 24–72 hours after exposure.
- Tissue injury is primarily due to the release of cytokines and the action of recruited macrophages.
- Clinical Manifestations: Erythema, induration, contact skin eruptions, granulomatous inflammation.
- Examples:
- Tuberculin skin test (Mantoux test using PPD)
- Contact dermatitis (e.g., due to nickel, latex, poison ivy)
- Chronic transplant rejection
- Granulomatous diseases (e.g., tuberculosis, leprosy, sarcoidosis)
- Type 1 diabetes mellitus (autoimmune T-cell destruction of β-cells)
Each type of hypersensitivity involves distinct immune players—Type I (IgE), Type II (IgG/IgM against cells), Type III (immune complexes), and Type IV (T-cell-mediated)—and leads to different forms of tissue damage. Correctly identifying the type is crucial for appropriate diagnosis and treatment in clinical immunology.
Q-2 Explain in detail the Morphology. Cultural Characteristic, Pathogenicity, Laboratory Diagnosis of Pneumococci
ANSWER :-
🦠 Streptococcus pneumoniae (Pneumococci)
A Gram-positive, encapsulated diplococcus, S. pneumoniae is a major human pathogen responsible for pneumonia, meningitis, otitis media, sinusitis, and bacteremia.
🔬 1. Morphology
Microscopic Features:
- Shape: Lanceolate (flame-shaped) or oval cocci, with pointed ends.
- Arrangement: Typically in pairs (diplococci); rarely seen singly or in short chains.
- Gram Staining: Gram-positive, appearing deep violet; old cultures may appear Gram-variable.
- Capsule:
- Made of polysaccharide, antiphagocytic, and a major virulence factor.
- Visualized by India ink, negative staining, or Quellung reaction.
- Spores & Motility: Non-spore forming and non-motile.
🧫 2. Cultural Characteristics
Growth Requirements:
- Facultative anaerobe; grows best in 5–10% CO₂ at 35–37°C.
- Requires enriched media such as:
- Blood agar
- Chocolate agar
Colony Morphology (on Blood Agar):
- Small, round, moist, glistening colonies initially.
- Produces alpha-hemolysis: greenish discoloration due to partial hemolysis of RBCs.
- After 24–48 hours, colonies become flattened with central depression – “draughtsman” or coin-shaped appearance due to autolysis.
Special Cultural Features:
- Growth enhanced by blood, serum, or ascitic fluid.
- Inhibited by bile salts, optochin, and sodium deoxycholate – useful for identification.
🧫 3. Pathogenicity
Source & Transmission:
- Part of the normal flora of the human nasopharynx.
- Transmitted via droplet infection or direct contact from infected secretions.
Virulence Factors:
- Capsule: Antiphagocytic and essential for virulence.
- Pneumolysin: Cytotoxin that damages respiratory epithelium and activates complement.
- Autolysin: Helps in the release of pneumolysin and causes autolysis of bacteria.
- IgA protease: Cleaves secretory IgA, helping in mucosal colonization.
Diseases Caused:
- Respiratory:
- Lobar pneumonia (classic presentation in adults)
- Sinusitis
- Otitis media (especially in children)
- Bronchitis
- Invasive diseases:
- Meningitis
- Bacteremia / septicemia
- Peritonitis
- High-risk populations: Children under 5, elderly, immunocompromised individuals, splenectomized patients.
🔍 4. Laboratory Diagnosis
Specimen Collection:
- Depends on site of infection:
- Sputum, blood, CSF, ear discharge, nasal swabs, pleural fluid
Microscopy:
- Gram stain: Shows Gram-positive, lanceolate diplococci, often in pairs.
- India ink or negative staining may show clear capsule.
- Quellung reaction: Capsule swells upon exposure to type-specific antisera (positive reaction is diagnostic).
Culture:
- Inoculate on blood agar or chocolate agar.
- Look for alpha-hemolysis, moist colonies with central umbilication after 24–48 hrs.
- Optochin sensitivity test: Pneumococcus is sensitive (zone of inhibition ≥14 mm).
- Bile solubility test: Pneumococci are bile soluble (colonies dissolve).
Biochemical Tests:
- Catalase test: Negative
- Ferments inulin: Positive (differentiates it from other streptococci)
Antigen Detection:
- Latex agglutination test or countercurrent immunoelectrophoresis can detect pneumococcal capsular antigen in CSF, pleural fluid, or urine.
Molecular Diagnosis:
- PCR for pneumococcal DNA – highly sensitive and specific (used in critical cases).
Serotyping:
- Over 90 capsular serotypes identified.
- Useful for epidemiological surveillance and vaccine development.
💉 Prevention
- Pneumococcal vaccines:
- PCV (Pneumococcal Conjugate Vaccine) – e.g., PCV13
- PPSV (Pneumococcal Polysaccharide Vaccine) – e.g., PPSV23
Q.3 Write Short Notes on: (Any three out of four)
Q-1 Principles of Microbiology.
ANSWER :-
🌿 Principles of Microbiology –
Microbiology is the branch of science that deals with the study of microorganisms—tiny living organisms that are usually invisible to the naked eye. This includes bacteria, viruses, fungi, protozoa, algae, and sometimes microscopic helminths.
The principles of microbiology are foundational concepts that help understand the nature, function, and role of these microorganisms in various environments, including the human body.
1. 🔬 Microbial Ubiquity (Omnipresence of Microbes)
Microorganisms are found everywhere—in the air, water, soil, and even inside the human body. They thrive in extreme environments like hot springs, arctic ice, salty lakes, and deep-sea vents.
🟢 Principle: Microbes are ubiquitous, meaning they exist in every habitat on Earth.
2. 🧫 Cellular Organization
Microbes may be prokaryotic (like bacteria and archaea) or eukaryotic (like fungi, protozoa, and algae).
🟢 Prokaryotes: Lack a true nucleus and membrane-bound organelles.
🟢 Eukaryotes: Have a well-defined nucleus and organelles.
3. 🌱 Growth and Reproduction
Microorganisms grow and reproduce at a rapid rate, mostly via binary fission (asexual) or sometimes sexual reproduction.
Growth depends on environmental conditions like nutrients, pH, temperature, moisture, and oxygen availability
4. 🧪 Metabolism and Biochemical Activity
Microbes carry out all basic metabolic activities such as respiration, fermentation, digestion, and synthesis.
🔹 Chemoautotrophs: Use inorganic compounds
🔹 Photoautotrophs: Use light for energy
🔹 Heterotrophs: Rely on organic carbon from the environment
5. 🧬 Genetic Continuity and Mutation
Microbes have DNA or RNA as genetic material. They replicate through binary fission (bacteria) or by budding/spores (fungi).
They can undergo mutations, which makes them adapt to antibiotics or new environments—important in microbial evolution.
6. 🛡️ Pathogenicity vs. Normal Flora
Some microorganisms are pathogenic (disease-causing), while others are commensal or even beneficial (normal flora).
Normal flora plays a vital role in digestion, vitamin production, and immunity.
7. 🧫 Sterilization and Disinfection
Principles of sterilization and disinfection are crucial to prevent infection. Microbiologists study how to eliminate or reduce microbial load using:
- Heat (autoclaving)
- Chemicals (phenol, alcohol)
- Radiation (UV rays)
8. ⚙️ Host-Microbe Interactions
Microorganisms interact with hosts in three main ways:
- Symbiotic (both benefit)
- Commensal (one benefits, the other is unaffected)
- Parasitic (one benefits, the host is harmed)
9. 🦠 Microbial Identification and Classification
Microbes are classified based on morphology, staining, genetic structure, and biochemical reactions. Techniques include:
- Gram staining
- Culture methods
- Serological tests
- Molecular biology (PCR, DNA sequencing)
10. 💊 Antimicrobial Sensitivity
Microbes respond differently to antibiotics. Antibiotic sensitivity testing (AST) determines the most effective drug for treatment.
🔹 Broad-spectrum vs. Narrow-spectrum antibiotics
🔹 Resistance mechanisms: Plasmid transfer, mutation
11. 🔄 Microbial Evolution and Adaptation
Microbes evolve quickly due to high replication rates and genetic variation. This leads to antibiotic resistance, new strains, and emerging infections.
12. 🧫 Use of Microbes in Biotechnology
Microorganisms are used in:
✔️ Vaccine development
✔️ Enzyme production
✔️ Genetic engineering
✔️ Wastewater treatment
✔️ Food industries (cheese, yogurt, bread)
Q-2 VDRL Test
ANSWER :-
🧪 VDRL Test (Venereal Disease Research Laboratory Test)
🔍 Definition
The VDRL (Venereal Disease Research Laboratory) test is a non-treponemal serological test used to detect antibodies in the blood that are produced in response to infection with Treponema pallidum, the bacterium that causes syphilis.
This test does not detect the bacterium itself, but rather the reagin antibodies produced by the body against substances released from damaged host cells.
🎯 Purpose / Uses
- ✅ To screen for syphilis (especially in early stages)
- ✅ To monitor response to syphilis treatment
- ✅ To detect congenital syphilis in newborns
- ✅ Often used in routine prenatal screening
🧬 Principle of the VDRL Test
- The test is based on flocculation reaction.
- When a reagin antibody (produced due to syphilitic infection) reacts with an antigen made of cardiolipin-lecithin-cholesterol, visible clumping or flocculation occurs.
- This clumping is observed under a microscope and indicates a positive result.
🧫 Procedure (Steps)
- Blood Sample Collection: Venous blood is drawn and serum is separated.
- Mixing: A drop of serum is mixed on a slide with a prepared VDRL antigen.
- Rotation: The slide is rotated at a standard speed and time to allow mixing.
- Observation: The slide is examined under a microscope for flocculation (clumping).
📊 Results Interpretation
| Result | Interpretation |
|---|---|
| Reactive | Suggests presence of reagin antibodies – could indicate syphilis. Further treponemal-specific tests are needed (like FTA-ABS). |
| Non-reactive | No reagin antibodies detected – no active syphilis (could still be early stage or treated syphilis). |
| Weakly Reactive | Requires confirmation with more specific tests. |
🔁 Follow-up / Confirmatory Tests
Because VDRL is a non-specific test, false positives may occur. Confirmatory treponemal tests are used:
- ✅ FTA-ABS (Fluorescent Treponemal Antibody Absorption)
- ✅ TPHA (Treponema pallidum Hemagglutination Assay)
⚠️ False Positive Causes
VDRL can show false positives in certain conditions:
- Pregnancy
- Autoimmune diseases (e.g., SLE)
- Viral infections (e.g., hepatitis, mononucleosis)
- Tuberculosis
- Malaria
- Drug addiction
💉 Sample Requirements
- Serum or CSF (Cerebrospinal Fluid) for neurosyphilis detection
- No fasting required
🛡️ Nurse’s Responsibilities
- Explain the purpose of the test to the patient.
- Ensure proper aseptic technique during blood collection.
- Label and transport the sample correctly.
- Maintain confidentiality.
- Educate the patient about the need for follow-up confirmatory testing if positive.
- Support patients emotionally as this is an STD-related test.
🌐 Clinical Importance
- VDRL is commonly used in public health programs for STD control.
- It is cost-effective, easy to perform, and ideal for mass screening.
- VDRL titers can be used to track treatment progress (titers fall after successful treatment).
Q-3.Clostridium Tetani
ANSWER :-
Clostridium tetani is a medically important, Gram-positive, obligate anaerobic, rod-shaped bacterium that causes the disease tetanus. It is widely found in the environment, particularly in soil, animal feces, and dust. The organism produces a powerful neurotoxin called tetanospasmin, which is the primary cause of the clinical symptoms seen in tetanus.
2. Morphology
Clostridium tetani appears as a slender bacillus with terminal, round spores, which give it a unique “drumstick” appearance under the microscope. It is motile due to the presence of peritrichous flagella and lacks a capsule. The organism stains Gram-positive, but in old cultures or under unfavorable conditions, it may appear Gram-variable.
3. Cultural Characteristics
Clostridium tetani is a strict anaerobe and requires oxygen-free conditions for growth. In the laboratory, it grows on blood agar and in Robertson’s cooked meat medium, showing spreading growth with a foul odor. Optimal growth occurs at around 37°C. Colonies may demonstrate hemolysis on blood agar.
4. Toxin Production
The organism produces two important exotoxins:
- Tetanospasmin: This is the major virulence factor, a potent neurotoxin that interferes with neurotransmission by inhibiting the release of GABA and glycine, the inhibitory neurotransmitters in the central nervous system. This results in muscle rigidity and spasms.
- Tetanolysin: A hemolytic toxin with minimal clinical importance, it may contribute to local tissue damage.
5. Pathogenesis
Infection begins when the spores of Clostridium tetani enter the body through deep wounds, punctures, burns, or contaminated instruments. Under anaerobic conditions, the spores germinate into vegetative cells and release tetanospasmin. This neurotoxin is absorbed into the peripheral nerves and travels retrogradely to the spinal cord and brain, where it inhibits the release of inhibitory neurotransmitters. This leads to sustained muscle contractions, a hallmark of tetanus.
6. Transmission
Tetanus is not transmitted from person to person. It is acquired through environmental exposure when spores enter a suitable site within the body. Common portals of entry include:
- Wounds contaminated with soil or feces
- Surgical procedures with improper sterilization
- Umbilical stump in neonates (causing neonatal tetanus)
- Intramuscular injections or tattooing in unsterile conditions
7. Laboratory Diagnosis
Diagnosis is primarily clinical due to the rapid progression and distinct presentation. Laboratory findings may support diagnosis through:
- Microscopy: Gram-stained smears showing Gram-positive rods with terminal spores
- Culture: Growth in anaerobic conditions on appropriate media
- Toxin testing: Toxin detection via mouse inoculation (rarely used today)
- Molecular methods: PCR for detecting the tetanospasmin gene in specialized laboratories
8. Clinical Types of Tetanus
Based on the site and extent of toxin effect, tetanus can be classified into:
- Generalized tetanus: Most common, with widespread muscle rigidity and spasms
- Localized tetanus: Spasms confined near the site of injury
- Cephalic tetanus: Affects cranial nerves, especially after head injuries
- Neonatal tetanus: Affects newborns, often due to contaminated umbilical cords in unclean deliveries
9. Prevention
Prevention is highly effective and based on immunization and wound care:
- Tetanus toxoid vaccination (part of DPT, Td, TT schedules)
- Booster doses every 10 years
- Tetanus Immunoglobulin (TIG) in cases of high-risk wounds or unknown immunization status
- Proper wound cleaning and sterilization techniques
10. Treatment
Management of tetanus includes both symptomatic and specific treatment:
- TIG to neutralize unbound toxin
- Antibiotics like metronidazole or penicillin to kill the bacteria
- Wound debridement to remove necrotic tissue and promote oxygenation
- Sedatives and muscle relaxants (like diazepam) to control spasms
- Supportive care such as ventilatory support in severe cases
- Vaccination should still be administered to ensure active immunity
11. Public Health Importance
Clostridium tetani remains a public health threat in areas with low immunization coverage, poor hygiene, and limited access to healthcare. Neonatal tetanus is a major contributor to infant mortality in developing countries and is targeted by WHO for global elimination.
From a microbiological perspective, Clostridium tetani is a classic example of a toxin-mediated pathogen. It does not invade tissue or multiply aggressively, but its ability to produce tetanospasmin makes it extremely dangerous. Effective prevention through vaccination and hygienic practices remains the cornerstone in the fight against tetanus.
Q-4 Compound Microscope
ANSWER :-
🔬
A compound microscope is a fundamental tool in microbiology that allows us to magnify and visualize microorganisms that are otherwise invisible to the naked eye. It uses two sets of lenses—the objective lens and the ocular (eyepiece) lens—to provide a high degree of magnification and resolution. This instrument revolutionized the field of microbiology by making it possible to study the structure, shape, size, and behavior of bacteria, fungi, protozoa, and other microorganisms.
2. Principle
The compound microscope works on the principle of optical magnification, where light is passed through a specimen and bent (refracted) through a series of lenses to magnify the image. The objective lens forms a real, inverted image, which is then magnified again by the eyepiece, forming a virtual, enlarged image that the observer sees.
3. Structure and Components
A compound microscope has three main systems: optical, mechanical, and illuminating.
- The optical system consists of the lenses—specifically, the objective lenses (typically ranging from 4x to 100x, including oil immersion) and the eyepiece, usually 10x.
- The mechanical system includes the body tube, revolving nosepiece, stage, coarse and fine adjustment knobs, arm, and base. These parts provide support and allow smooth focusing and positioning of the specimen.
- The illumination system involves a light source, a mirror, and a condenser that focuses light onto the specimen, often with an iris diaphragm to regulate intensity.
4. Working Mechanism
To use a compound microscope, the specimen is placed on a glass slide and positioned on the stage using stage clips. Light from the mirror or built-in lamp passes through the condenser and is focused on the specimen. The light then travels through the specimen, and the objective lens magnifies the image. This image is further enlarged by the eyepiece, allowing the observer to see a detailed structure of the microbe.
Focusing is done first using the coarse adjustment (to bring the object roughly into view) and then the fine adjustment (to sharpen the image).
5. Types of Objective Lenses
Most compound microscopes have three or four rotating objective lenses:
- Low power (10x) for scanning and general viewing
- High power (40x) for detailed observation of smaller structures
- Oil immersion lens (100x) used with a drop of immersion oil to increase clarity and resolution, essential for bacterial examination
When combined with a 10x eyepiece, total magnifications are 100x, 400x, and 1000x respectively.
6. Uses in Microbiology
The compound microscope is indispensable in:
- Observing bacterial morphology (cocci, bacilli, spirilla)
- Studying fungi and protozoa
- Performing Gram staining and other differential stains
- Examining blood smears, urine sediments, and clinical specimens
- Identifying structural characteristics of microorganisms such as flagella, spores, capsules, and inclusion bodies
7. Care and Maintenance
Proper care ensures long life and optimal performance of the microscope:
- Always carry it with both hands
- Clean lenses with lens paper, not tissues or cloth
- Never touch lenses with fingers
- After oil immersion use, clean the objective lens immediately
- Store the microscope with the low power objective in place and the dust cover on
The compound microscope is an essential diagnostic and research tool in microbiology. Its ability to magnify objects up to 1000 times with clarity enables students, clinicians, and researchers to observe the microbial world, understand disease processes, and contribute to scientific discoveries. Mastery of its use is fundamental in the field of nursing, medicine, and biological sciences.
Q.4 Write very short answers: (Any two out of three) (3X2=6)
Q-1 Bacterial growth curve
ANSWER :-
🦠 Bacterial Growth Curve
The bacterial growth curve represents the pattern of growth of a bacterial population over time when cultured in a closed system (like a test tube with nutrient broth). It includes four main phases, each showing different cellular activities:
- Lag Phase
This is the initial phase where bacteria are metabolically active but not dividing. They are adapting to the new environment, synthesizing enzymes, and preparing for growth. - Log Phase (Exponential Phase)
In this phase, bacteria undergo rapid cell division at a constant rate. The population doubles at regular intervals, and the growth is exponential. This is the most active phase for metabolism and is ideal for studying antibiotics. - Stationary Phase
Here, the growth rate slows down and number of new cells equals the number of dying cells. Nutrients become limited, and waste products accumulate. The population size reaches a plateau. - Death Phase (Decline Phase)
In this final stage, cells die faster than they reproduce due to exhaustion of nutrients and toxic buildup. The population starts to decline.
Q-2 Lab diagnosis of vibrio cholera
ANSWER :-
The laboratory diagnosis of Vibrio cholerae focuses on detecting the bacteria in stool samples of suspected cholera patients. The key steps include:
- Specimen Collection
Fresh stool sample or rectal swab is collected in the early stages of diarrhea when the bacterial count is highest. - Microscopy (Dark Field or Wet Mount)
A wet mount may reveal actively motile, comma-shaped organisms. Motility is shooting star-like and can be stopped with antiserum (confirmatory). - Culture
Stool is cultured on selective media like:
- Thiosulfate-citrate-bile salts-sucrose (TCBS) agar: Yellow colonies indicate Vibrio cholerae
- Alkaline peptone water is used for enrichment before culture
- Biochemical Tests
The isolated organism is confirmed using biochemical reactions:
- Oxidase positive
- Ferments sucrose
- Grows in alkaline pH
- Serotyping
Agglutination with O1 and O139 antisera helps identify the pathogenic strains. - Molecular & Rapid Tests (Optional)
- PCR and ELISA for toxin gene detection
- Rapid dipstick tests for quick field diagnosis (less reliable)
Q-3 Normal Flora
ANSWER :-
🦠 Normal Flora
Normal flora refers to the microorganisms (mainly bacteria, but also fungi and viruses) that naturally live on and inside the human body without causing disease under normal conditions. They are found in areas like the skin, mouth, nose, throat, gastrointestinal tract, and vagina.
These microbes play a protective and beneficial role by:
- Competing with harmful pathogens
- Producing vitamins (like Vitamin K in the gut)
- Stimulating the immune system
- Helping in digestion
However, if the balance is disturbed or they enter sterile areas (like blood or internal organs), they may become opportunistic pathogens and cause infection.
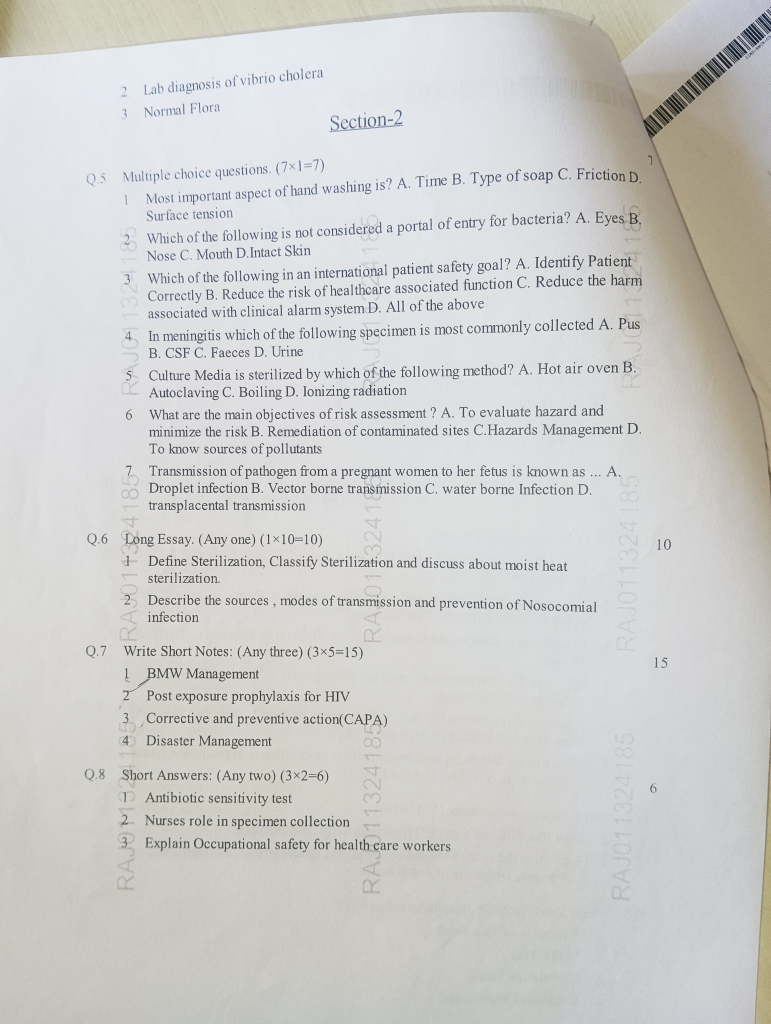
Section-2
Q5 Multiple choice questions. (7×1=7)
ANSWER :-
1. Most important aspect of hand washing is? A. Time B. Type of soap C. Friction D. Surface tension
2. Which of the following is not considered a portal of entry for bacteria? A. Eyes B. Nose C. Mouth D. Intact Skin
3.Which of the following in an international patient safety goal?A. Identify Patient Correctly B. Reduce the risk of healthcare associated function C. Reduce the harm associated with clinical alarm system D. All of the above
4.In meningitis which of the following specimen is most commonly collected A. Pus B. CSF C. Faeces D. Urine
5.Culture Media is sterilized by which of the following method? A. Hot air oven B. Autoclaving C. D. Ionizing radiation
6 What are the main objectives of risk assessment? A. To evaluate hazard and minimize the risk B. Remediation of contaminated sites C.Hazards Management D. To know sources of pollutants
7. Transmission of pathogen from a pregnant women to her fetus is known as …A. Droplet infection B. Vector borne transmission C. water borne Infection D. transplacental transmission
Q.6 Long Essay. (Any one) (1×10=10)
Q-1.Define Sterilization, Classify Sterilization and discuss about moist heat sterilization.
ANSWER :-
✅ Definition of Sterilization
Sterilization is defined as the complete destruction or removal of all forms of microbial life, including bacteria, viruses, fungi, and spores, from an object, surface, or medium. It ensures that no living microorganisms remain, thereby making the object or substance completely free from any potential infection.
Sterilization is essential in medical, microbiological, pharmaceutical, and surgical fields to prevent infection, contamination, and disease transmission.
📚 Classification of Sterilization
Sterilization methods can be broadly classified into Physical, Chemical, and Physicochemical methods:
1. Physical Methods
These use heat or radiation to achieve sterilization and are the most commonly used in laboratories and healthcare settings.
- Heat Sterilization:
- Moist Heat (e.g., autoclaving, boiling, pasteurization)
- Dry Heat (e.g., hot air oven, flaming, incineration)
- Radiation:
- Ionizing radiation (gamma rays, X-rays)
- Non-ionizing radiation (UV light)
- Filtration:
- Membrane filters for heat-sensitive liquids and air
2. Chemical Methods
Use of antimicrobial chemicals to sterilize instruments, surfaces, or liquids:
- Gaseous agents: Ethylene oxide, formaldehyde
- Liquid agents: Glutaraldehyde, peracetic acid, phenol, alcohols
3. Physicochemical Methods
A combination of physical and chemical techniques, such as:
- Plasma sterilization
- Vaporized hydrogen peroxide
💦 Moist Heat Sterilization
Moist heat sterilization uses steam or hot water to kill microorganisms by denaturing their proteins, which leads to irreversible damage and cell death. This method is more effective and faster than dry heat because water conducts heat better and penetrates deeper.
🔹 Mechanism of Action
Moist heat kills microbes by:
- Denaturation and coagulation of proteins
- Disruption of cell membranes and enzymes
- Destruction of spores at higher temperatures and pressures
🔧 Types of Moist Heat Sterilization
- Autoclaving (Steam under pressure)
- Most reliable and widely used method
- Standard condition: 121°C temperature at 15 psi (pounds per square inch) pressure for 15–20 minutes
- Kills all forms of microorganisms including bacterial spores
- Used for sterilizing surgical instruments, dressings, glassware, media, rubber items
- Boiling
- Involves boiling items in water at 100°C for 15–30 minutes
- Kills most vegetative bacteria and viruses, but not spores
- Not considered a reliable method for sterilization in clinical settings
- Pasteurization
- Used in food industry (especially milk)
- Kills pathogenic microbes without affecting the quality of the product
- Common methods:
- Holder method: 63°C for 30 minutes
- Flash method: 72°C for 15 seconds
- Tyndallization (Intermittent boiling/Steam at 100°C)
- Involves heating at 100°C for 30 minutes on three consecutive days
- Allows spores to germinate between sessions, which are then killed
- Used for heat-sensitive materials like culture media with sugars or gelatin
🧪 Uses of Moist Heat Sterilization
- Sterilization of culture media and liquids
- Surgical dressings, linen, gowns
- Glassware, rubber gloves, plastic syringes (autoclavable)
- Disinfection of metal instruments (autoclaving or boiling)
⚠️ Precautions for Autoclaving
- Items must be steam permeable and arranged loosely
- Do not overfill the chamber
- Use autoclave tape or indicators to confirm sterilization
- Do not open the autoclave immediately after the cycle; allow pressure to normalize
🧷 Advantages of Moist Heat Sterilization
- Rapid and efficient
- Effective against spores and viruses
- Non-toxic, environmentally safe
- Suitable for reusable surgical items
❌ Limitations
- Not suitable for heat-sensitive materials (e.g., powders, oils, some plastics)
- Can cause corrosion of metal instruments if not dried properly
- Cannot sterilize materials that are not water-resistant
Moist heat sterilization, particularly autoclaving, is the gold standard in healthcare and laboratory settings due to its reliability, speed, and effectiveness. Understanding its mechanism, applications, and limitations helps ensure safe and infection-free clinical practices. It is a critical pillar of infection control and aseptic techniques in all microbiology and nursing procedures.
Q-2 Describe the sources, modes of transmission and prevention of Nosocomial infection
ANSWER :-
Nosocomial infections, also known as hospital-acquired infections (HAIs), are infections that patients acquire during the course of receiving treatment in a healthcare setting, such as a hospital or nursing home. These infections develop after 48 hours of admission, are not present or incubating at the time of admission, and can also occur after discharge or among healthcare workers.
Nosocomial infections are a major cause of morbidity and mortality worldwide, and they increase the length of hospital stay, financial burden, and risk of antimicrobial resistance. They are commonly caused by multidrug-resistant organisms (MDROs) such as Staphylococcus aureus, Pseudomonas aeruginosa, Klebsiella pneumoniae, Escherichia coli, and Acinetobacter baumannii.
🔍 1. Sources of Nosocomial Infections
Nosocomial infections arise from endogenous (patient’s own flora) or exogenous (environmental) sources.
🔸 a) Endogenous Sources
These infections arise when microorganisms that are part of the patient’s normal flora become opportunistic pathogens due to:
- Immunosuppression
- Surgery or trauma that breaches normal barriers
- Invasive devices (catheters, tubes)
- Antibiotic therapy altering flora balance (e.g., Clostridium difficile colitis)
🔸 b) Exogenous Sources
These are external sources of infection, which include:
- Contaminated hands of healthcare workers
- Infected patients or asymptomatic carriers
- Contaminated instruments and devices
- Airborne particles and droplets
- Contaminated surfaces, bedding, or fluids
- Unsterile procedures and poor hand hygiene
🔄 2. Modes of Transmission
The spread of nosocomial infections occurs through various well-established routes:
🔹 a) Contact Transmission
Most common mode in hospital settings.
- Direct Contact: Physical interaction between an infected person and another (e.g., touching wounds without gloves).
- Indirect Contact: Transfer via contaminated items such as thermometers, bed linens, IV poles, or stethoscopes.
🔹 b) Droplet Transmission
Occurs when large respiratory droplets (≥5 µm) carrying pathogens are expelled during coughing, sneezing, or talking, and come into contact with the mucous membranes of another individual.
Examples: Influenza, COVID-19, Pertussis
🔹 c) Airborne Transmission
Infectious particles (<5 µm) remain suspended in the air and are inhaled by susceptible individuals, even over long distances.
Examples: Tuberculosis, Measles, Varicella
🔹 d) Common Vehicle Transmission
Infections spread through shared contaminated sources, such as:
- IV fluids
- Blood products
- Food or water Examples: Salmonella, Listeria
🔹 e) Vector-Borne Transmission
Though rare in hospitals, insects like mosquitoes, flies, or cockroaches may carry pathogens, especially in poorly maintained healthcare settings.
🛡️ 3. Prevention of Nosocomial Infections
🧼 a) Strict Hand Hygiene
- Most effective method of prevention.
- Use of alcohol-based hand rubs or handwashing with soap and water.
- Follows WHO’s 5 Moments for Hand Hygiene:
- Before touching a patient
- Before clean/aseptic procedures
- After body fluid exposure/risk
- After touching a patient
- After touching patient surroundings
🧤 b) Use of Personal Protective Equipment (PPE)
- Gloves, gowns, masks, eye shields reduce the risk of cross-transmission.
- Used especially during handling of infectious materials, wounds, or invasive procedures.
🧪 c) Aseptic Techniques
- Follow strict asepsis during:
- Catheter insertion
- Venipuncture
- Wound dressing changes
- Surgical procedures
- Use sterile instruments, drapes, and gloves.
🧹 d) Environmental Sanitation
- Routine cleaning and disinfection of:
- Bed rails, doorknobs, toilets
- Operating theaters, ICUs
- Reusable medical equipment
- Use of disinfectants such as hypochlorite, glutaraldehyde.
📊 e) Hospital Infection Surveillance Programs
- Maintain records of infection rates.
- Identify and manage outbreaks quickly.
- Establish an infection control team and committee.
💊 f) Antibiotic Stewardship
- Rational use of antimicrobials to prevent resistance.
- Avoid overuse and misuse of broad-spectrum antibiotics.
- De-escalate therapy based on culture and sensitivity.
👩⚕️ g) Education and Training of Healthcare Workers
- Regular workshops on infection control policies
- Updates on emerging resistant strains
- Training in wound care, IV therapy, catheter management
💉 h) Vaccination of Staff and Patients
- Mandatory vaccines: Hepatitis B, Influenza, COVID-19, etc.
- Reduces transmission of vaccine-preventable infections within healthcare settings.
🚫 i) Proper Handling of Invasive Devices
- Regularly assess the need for urinary catheters, central lines, ventilators.
- Remove devices as early as possible.
- Ensure aseptic insertion and maintenance.
🗑️ j) Biomedical Waste Management
- Follow color-coded segregation and disposal protocols.
- Prevents indirect spread of pathogens through waste handling.
💡 Examples of Common Nosocomial Infections
- Urinary Tract Infections (UTIs) – often from indwelling catheters
- Ventilator-Associated Pneumonia (VAP)
- Surgical Site Infections (SSIs)
- Central Line-Associated Bloodstream Infections (CLABSIs)
- Clostridium difficile-associated diarrhea due to antibiotic use
Nosocomial infections represent a serious threat to patient safety and health outcomes. Their sources are both endogenous and exogenous, and transmission primarily occurs through contact, droplets, or airborne means. Prevention relies heavily on strict hand hygiene, aseptic techniques, rational use of antibiotics, and environmental cleanliness.
Healthcare workers, especially nurses, play a central role in preventing these infections through vigilant practice, education, and adherence to protocols. Establishing a culture of safety, cleanliness, and accountability is vital in minimizing the occurrence of hospital-acquired infections and improving patient care outcomes.
Q.7 Write Short Notes: (Any three) (3×5=15)
Q-1.BMW Management
ANSWER :-
Biomedical Waste (BMW) refers to any waste generated during diagnosis, treatment, immunization, or research activities related to humans or animals. It includes potentially infectious, hazardous, and contaminated materials that can pose serious health risks to healthcare workers, patients, and the environment if not handled properly.
Effective BMW management is a legal, ethical, and professional responsibility of every healthcare provider and facility to ensure safety, reduce infection risks, and protect the environment.
♻️ 2. Definition
According to the Biomedical Waste Management Rules, 2016 (India), biomedical waste is defined as:
“Any waste that is generated during the diagnosis, treatment, or immunization of human beings or animals, or in research activities or in the production/testing of biologicals.”
🔍 3. Sources of Biomedical Waste
Biomedical waste is generated in:
- Hospitals and nursing homes
- Clinics and dispensaries
- Pathology and diagnostic labs
- Blood banks
- Veterinary institutions
- Pharmaceutical companies
- Research centers and teaching institutions
⚗️ 4. Categories of Biomedical Waste
BMW is categorized based on its nature and risk, and segregated into four major color-coded categories under the 2016 rules:
- Yellow:
- Human anatomical waste (body parts)
- Soiled waste (dressings, bandages)
- Expired or discarded medicines
- Microbiology lab waste
- Red:
- Contaminated but recyclable items (IV sets, catheters, gloves)
- White (Translucent):
- Sharps (needles, blades, scalpels)
- Blue:
- Broken glassware, discarded vials, ampoules (non-contaminated)
🗂️ 5. Segregation at Source
One of the most critical steps in BMW management is segregation at the point of generation. Waste must be placed directly into color-coded, labeled containers or bags to:
- Avoid mixing of hazardous and non-hazardous waste
- Ensure safe handling and disposal
- Minimize infection and chemical hazards
Each container must be properly labeled with the biohazard symbol and contents.
🧼 6. Collection, Storage, and Transportation
- Collection: Done at regular intervals by trained personnel using protective gear.
- Storage: Must not exceed 48 hours. Kept in a designated, ventilated, secure area.
- Transportation: Waste is moved to Common Biomedical Waste Treatment Facilities (CBWTFs) using authorized vehicles with leak-proof containers.
🧯 7. Treatment and Disposal Methods
Different types of biomedical waste require different treatment methods:
- Incineration (for yellow category):
- High-temperature combustion of anatomical and soiled waste
- Reduces volume and destroys pathogens
- Autoclaving / Microwaving (for red and white category):
- Moist heat sterilization to disinfect waste
- Used for plastic and sharp items
- Chemical Disinfection:
- Used for liquid waste (e.g., blood, body fluids)
- Chlorine-based chemicals are used
- Deep Burial / Secured Landfill:
- For rural areas or waste not suitable for incineration
- Must be done as per CPCB guidelines
🛡️ 8. Health Hazards of Poor BMW Management
Improper handling of biomedical waste can lead to:
- Infections: HIV, Hepatitis B & C, Tuberculosis
- Injuries from sharps
- Soil and water contamination
- Air pollution from burning
- Antibiotic resistance due to indiscriminate disposal
📋 9. Role of Nurses in BMW Management
Nurses are frontline health workers and play a key role in:
- Educating other staff and patients about segregation
- Ensuring proper collection and disposal
- Wearing Personal Protective Equipment (PPE)
- Following infection control protocols
- Reporting spills or accidents immediately
- Maintaining documentation and records
📜 10. Legal and Regulatory Framework in India
- Biomedical Waste Management Rules, 2016 (and amendments in 2018, 2019, 2022) issued under the Environment Protection Act, 1986
- CPCB (Central Pollution Control Board) monitors enforcement
- All healthcare facilities must obtain authorization, submit annual reports, and follow record-keeping protocols
Q-2 Post exposure prophylaxis for HIV
ANSWER :-
Post Exposure Prophylaxis (PEP) is a short-term course of antiretroviral medications given to a person after potential exposure to HIV, to prevent infection. PEP is not a cure for HIV but is highly effective if started early, ideally within 2 hours, and no later than 72 hours (3 days) after exposure.
PEP is recommended when a person is exposed to HIV through:
- Needlestick injury or sharps accident in a healthcare setting
- Mucosal exposure (e.g., splash into eyes, mouth)
- Non-intact skin exposure (open cuts, wounds)
- Unprotected sexual contact
- Sexual assault
- Exposure to blood or body fluids of known or suspected HIV-positive individuals
⏳ Time Window for PEP Initiation
- Best if started within 2 hours
- Must be started within 72 hours
- After 72 hours, PEP is not recommended as it becomes ineffective
💊 Medications Used in PEP
The standard PEP regimen consists of a three-drug combination for 28 days (4 weeks).
Recommended first-line regimen:
- Tenofovir disoproxil fumarate (TDF) 300 mg +
- Lamivudine (3TC) 300 mg (or Emtricitabine 200 mg) +
- Dolutegravir (DTG) 50 mg once daily
These drugs are well-tolerated, potent, and have minimal side effects.
🧪 Baseline and Follow-Up Testing
Before starting PEP, the following tests are done:
- HIV testing (baseline) to ensure the person is not already HIV-positive
- HBV and HCV status of both source and exposed person
- Complete blood count (CBC) and renal/liver function tests
Follow-up testing schedule:
- HIV test at baseline, 6 weeks, 12 weeks, and 6 months
- Monitor for side effects of antiretrovirals
- Adherence counseling is crucial for success
👩⚕️ Role of Nurse or Healthcare Provider
- Assess the type and risk of exposure
- Ensure PEP is started urgently
- Provide counseling and consent
- Monitor for adherence and side effects
- Provide psychological support, especially in sexual assault cases
- Encourage completion of 28-day course
Q-3 Corrective and preventive action(CAPA)
ANSWER :-
In microbiology, particularly within clinical laboratories, pharmaceutical settings, infection control programs, and quality assurance systems, CAPA plays a crucial role in ensuring product and patient safety by systematically identifying, investigating, and eliminating the causes of microbial contamination, laboratory errors, and non-compliance.
CAPA stands for:
- ✅ Corrective Action: Steps taken to eliminate the root cause of a detected problem or deviation.
- ✅ Preventive Action: Measures taken to prevent the occurrence or recurrence of a similar problem in the future.
CAPA is an essential component of Good Laboratory Practice (GLP) and Good Manufacturing Practice (GMP) and ensures regulatory compliance in microbiological processes.
🔍 Importance of CAPA in Microbiology
Microbiology involves sensitive testing and sterile processes. Even small deviations or microbial contamination can result in:
- False lab reports
- Product recalls
- Infections in patients
- Regulatory action against institutions
CAPA ensures:
- Consistent accuracy of microbiological testing
- Minimized risk of contamination in pharmaceutical products
- Reliable sterility and asepsis protocols
- Compliance with WHO, ISO, NABL, FDA, and GLP/GMP standards
🧫 Examples of CAPA Triggers in Microbiology
CAPA is implemented in response to incidents such as:
- Positive sterility test in a cleanroom environment
- Deviations in media preparation or culture incubation conditions
- Contamination in a laminar airflow cabinet
- Inconsistent colony counts or unexpected test results
- Improper labeling or documentation errors
- Failure in autoclave validation or disinfection protocol
- Non-conforming results in quality control
⚙️ Steps of CAPA in Microbiology
🔸 1. Problem Identification
Clearly define the non-conformity or microbiological deviation. This could be a failed sterility test, microbial contamination, or unexpected lab result.
🔸 2. Investigation
Conduct a root cause analysis (RCA) using tools like:
- 5 Whys analysis
- Fishbone (Ishikawa) diagram
- FMEA (Failure Mode and Effects Analysis)
Identify what exactly led to the error—was it due to:
- Operator error?
- Equipment malfunction?
- Inadequate cleaning or sterilization?
- Poor environmental conditions?
🔸 3. Corrective Action
Once the root cause is identified, take immediate action to eliminate the cause and restore compliance. For example:
- Retrain staff on aseptic techniques
- Replace faulty incubators
- Improve media preparation protocols
- Repeat testing with strict controls
🔸 4. Preventive Action
Implement long-term strategies to prevent recurrence:
- Review and revise SOPs (Standard Operating Procedures)
- Increase frequency of environmental monitoring
- Improve equipment maintenance schedule
- Conduct periodic audits and mock drills
- Develop a preventive checklist for daily microbiological tasks
🔸 5. Effectiveness Check
After implementing corrective and preventive measures, evaluate their success through:
- Follow-up audits
- Trend analysis of contamination reports
- Retesting or verification procedures
- Documentation and reporting to quality assurance team
📑 Documentation and Reporting
Proper documentation is critical in microbiology CAPA:
- Maintain a CAPA logbook
- Use CAPA forms to track issues, actions, and resolutions
- Record who identified, who approved, and who implemented the action
- Submit reports to regulatory authorities or internal quality departments
🛡️ Benefits of CAPA in Microbiology
- Enhances quality control in microbiological testing
- Minimizes microbial contamination risk in production
- Reduces cost of reprocessing or recall
- Ensures regulatory compliance
- Strengthens confidence in lab reports
- Builds a culture of accountability and improvement
🧼 Microbiology-Specific Preventive Examples
- Routine validation of autoclaves and sterilizers
- Air sampling and surface swabbing in cleanrooms
- Regular staff training on asepsis
- Bioburden and endotoxin testing
- Proper segregation of contaminated and sterile items
In microbiology, where the margin for error is small and the consequences can be significant, the implementation of a robust CAPA system is vital. CAPA helps in identifying deviations, correcting errors, and preventing future failures through structured, documented, and science-based approaches. It is a proactive defense mechanism that ensures safe, accurate, and contamination-free microbiological practices, especially in clinical diagnostics, pharmaceutical manufacturing, and infection control.
Q-4 Disaster Management
ANSWER :-
Disaster Management refers to the organized efforts to deal with the mitigation, preparedness, response, and recovery from disasters. It involves planning, coordinating, and implementing activities before, during, and after a disaster to minimize the impact on human life, property, and the environment.
A disaster is a sudden, catastrophic event that disrupts normal life, causes loss of life and property, and exceeds the capacity of the affected community to cope with using its own resources.
🔥 2. Types of Disasters
Disasters can be broadly classified into two categories:
A. Natural Disasters
- Earthquakes
- Floods
- Cyclones and hurricanes
- Tsunamis
- Landslides
- Droughts
- Volcanic eruptions
- Epidemics and pandemics (e.g., COVID-19)
B. Man-made Disasters
- Industrial accidents (chemical spills, gas leaks)
- Nuclear/radiation disasters
- Fires and explosions
- Transportation accidents (road, rail, air)
- Terrorist attacks and bombings
- Biological or chemical warfare
- Environmental pollution (air, water, soil contamination)
🎯 3. Objectives of Disaster Management
- To reduce the risk of disaster through hazard assessment and mitigation
- To prepare and train communities and responders
- To respond effectively to emergency situations
- To ensure quick recovery and rehabilitation of affected populations
- To protect human lives, livestock, infrastructure, and the environment
- To establish disaster-resilient communities
🛠️ 4. Phases of Disaster Management
Disaster Management is a continuous and integrated process divided into four main phases:
1. Mitigation
- Activities aimed at reducing the impact or likelihood of disasters
- Examples: Building flood barriers, enforcing building codes, planting trees, earthquake-resistant structures
2. Preparedness
- Planning and organizing before a disaster occurs
- Includes:
- Emergency drills
- First aid training
- Stockpiling of supplies
- Communication systems
- Evacuation plans
3. Response
- Immediate actions taken during or just after a disaster
- Includes:
- Search and rescue operations
- Emergency medical services
- Shelter and food distribution
- Crowd control
- Psychological support
4. Recovery
- Long-term efforts to rebuild and restore the affected area
- Includes:
- Rebuilding infrastructure
- Rehabilitation of victims
- Livelihood support
- Review of policies to improve future responses
🧩 5. Components of Effective Disaster Management
- Hazard identification and risk assessment
- Early warning systems
- Community awareness and education
- Disaster management planning (DMP)
- Resource mobilization and coordination
- Inter-agency collaboration (government, NGOs, army, UN)
- Post-disaster assessment and feedback loop
🏥 6. Role of Healthcare and Nurses in Disaster Management
Nurses are frontline responders and play a critical role:
- Triage and emergency care
- Infection control during epidemics
- Wound and trauma management
- Psychosocial support to victims and families
- Health education and awareness campaigns
- Assisting in evacuation and resettlement
- Participating in mock drills and training programs
- Maintaining medical records and documentation
- Supporting public health surveillance and vaccination drives
🧑⚕️ 7. Role of Government and National Bodies
In India, disaster management is governed by:
- Disaster Management Act, 2005
- National Disaster Management Authority (NDMA)
- State and District Disaster Management Authorities (SDMA, DDMA)
- NDRF (National Disaster Response Force)
- Ministry of Home Affairs, Ministry of Health, Indian Meteorological Department, and others
Q.8 Short Answers: (Any two) (3×2=6)
Q-1.Antibiotic sensitivity test
ANSWER :-
Antibiotic Sensitivity Test:
It is a laboratory method used to determine the effectiveness of specific antibiotics against bacteria isolated from a patient’s infection. This helps in selecting the most appropriate antibiotic for treatment. Common methods include the disc diffusion method (Kirby-Bauer test) and MIC (Minimum Inhibitory Concentration) testing.
Q-2.Nurses role in specimen collection
ANSWER :-
Nurse’s Role in Specimen Collection:
- ✅ Patient Identification: Confirm the patient’s identity using at least two identifiers (e.g., name and ID number).
- ✅ Patient Education: Explain the purpose and procedure of specimen collection to gain cooperation.
- ✅ Aseptic Technique: Use sterile equipment and maintain asepsis to prevent contamination.
- ✅ Correct Method: Collect the right type of specimen (urine, stool, blood, sputum, etc.) as per the doctor’s order.
- ✅ Proper Labeling: Label the specimen container with patient details, date, time, and type of specimen.
- ✅ Timely Transport: Send the specimen to the laboratory immediately to ensure accurate results.
- ✅ Documentation: Record the procedure, time of collection, patient’s condition, and any abnormalities.
- ✅ Follow-up: Monitor for any post-collection complications (e.g., bleeding after blood draw).
- ✅ Maintain Confidentiality: Ensure the patient’s information and results are kept private.
- ✅ Ensure Safety: Use personal protective equipment (PPE) to protect self and others from exposure.
Q-3.Explain Occupational safety for health care workers
ANSWER :-
Occupational Safety for Health Care Workers refers to the protection of healthcare staff from hazards and risks in the workplace to ensure their health, safety, and well-being. Healthcare settings pose various physical, chemical, biological, ergonomic, and psychosocial hazards.
- 🧫 Biological Hazards:
- Exposure to infectious diseases (e.g., TB, HIV, Hepatitis B/C).
- Needlestick injuries and contact with blood/body fluids.
- Prevention: Use of PPE, vaccination, safe needle disposal, hand hygiene.
- 🧪 Chemical Hazards:
- Exposure to disinfectants, chemotherapy drugs, anesthetic gases.
- Prevention: Proper storage, ventilation, and use of gloves/masks.
- 🦴 Ergonomic Hazards:
- Lifting patients, repetitive movements, awkward postures.
- Prevention: Use of assistive devices, proper body mechanics, ergonomically designed workspaces.
- 🔥 Physical Hazards:
- Slips, trips, falls, noise, radiation exposure, fire risks.
- Prevention: Safety training, warning signs, maintenance of equipment.
- 🧠 Psychosocial Hazards:
- Stress, long shifts, workplace violence, emotional burnout.
- Prevention: Counseling, adequate staffing, rest periods, support systems.
