Anatomy-Unit-4-The Circulatory and Lymphatic system
The Circulatory and Lymphatic system
Structure of blood components, blood vessels – Arterial and Venous system
Position of heart relative to the associated
structures
Chambers of heart, layers of heart
Heart valves, coronary arteries
Nerve and blood supply to heart
Lymphatic tissue
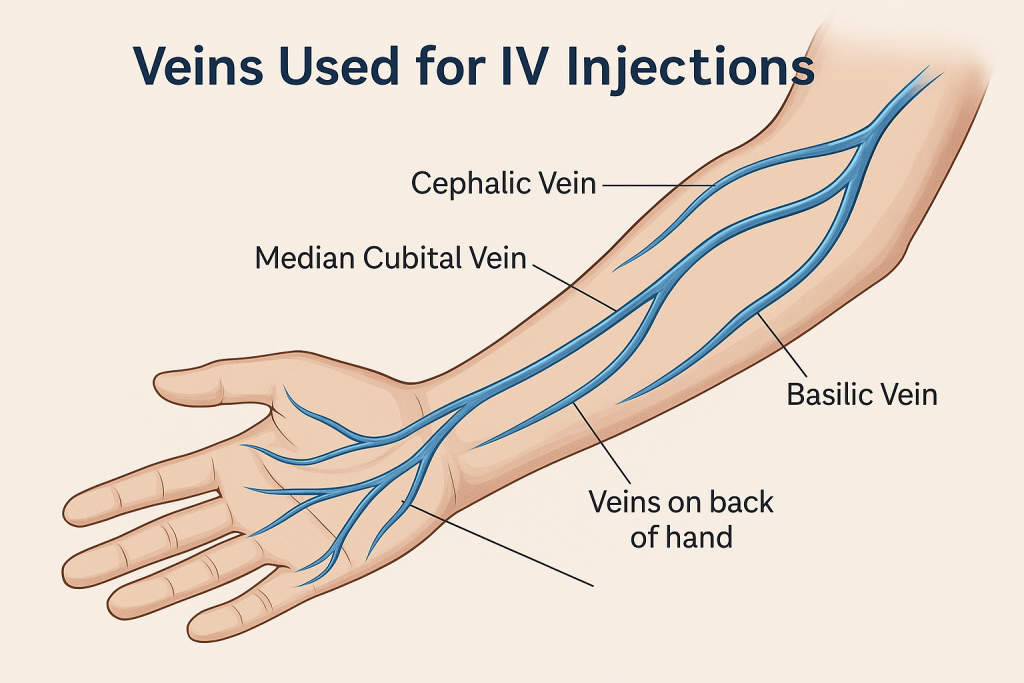
Veins used for IV injections
Application and implication in nursing
The Circulatory and Lymphatic system
Structure of Blood Components 💉
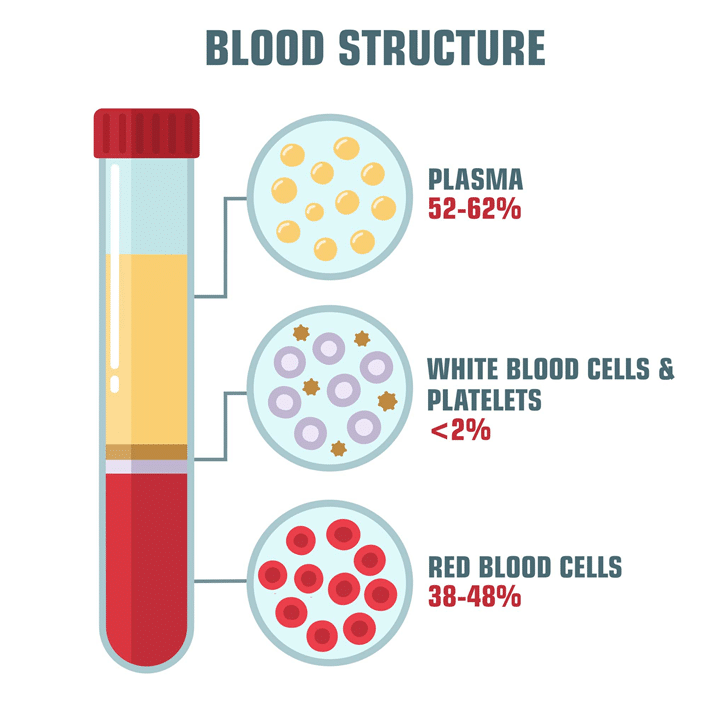
Blood is a vital fluid in the human body, responsible for transporting nutrients, oxygen, waste products, and immune cells. It is composed of both liquid and cellular components, each with specific functions necessary for maintaining homeostasis.
1. Plasma 🌊

Plasma is the liquid portion of blood, making up about 55% of the total blood volume. It is a yellowish liquid that contains water, proteins, electrolytes, hormones, and waste products. Plasma serves as the medium for transporting blood cells and other substances.
- Composition:
- Water: About 90% of plasma, which helps maintain blood volume and pressure.
- Proteins (7-8% of plasma): Plasma proteins are critical for clotting, immune responses, and maintaining osmotic pressure.
- Albumin: The most abundant plasma protein, responsible for maintaining osmotic pressure and transporting various substances, including hormones and fatty acids.
- Globulins: Includes immunoglobulins (antibodies) that help defend the body against infections, and transport proteins like transferrin (iron transport).
- Fibrinogen: A clotting factor that is converted to fibrin during blood clot formation.
- Electrolytes: Such as sodium (Na+), potassium (K+), calcium (Ca2+), chloride (Cl-), and bicarbonate (HCO3-). These are crucial for maintaining the body’s pH balance, muscle function, and nerve transmission.
- Nutrients: Glucose, amino acids, and lipids are transported via plasma to various tissues.
- Hormones: Plasma carries hormones like insulin, thyroxine, and growth hormone that regulate bodily functions.
- Waste Products: Includes urea, creatinine, and bilirubin that are transported to organs like the kidneys and liver for excretion.
- Function:
- Transport: Plasma acts as the vehicle for transporting cells, nutrients, hormones, and waste products.
- Regulation: Maintains blood pressure, body temperature, and pH.
- Defense: Plasma proteins like antibodies and complement proteins play a key role in the immune response.
2. Cellular Components 🩸
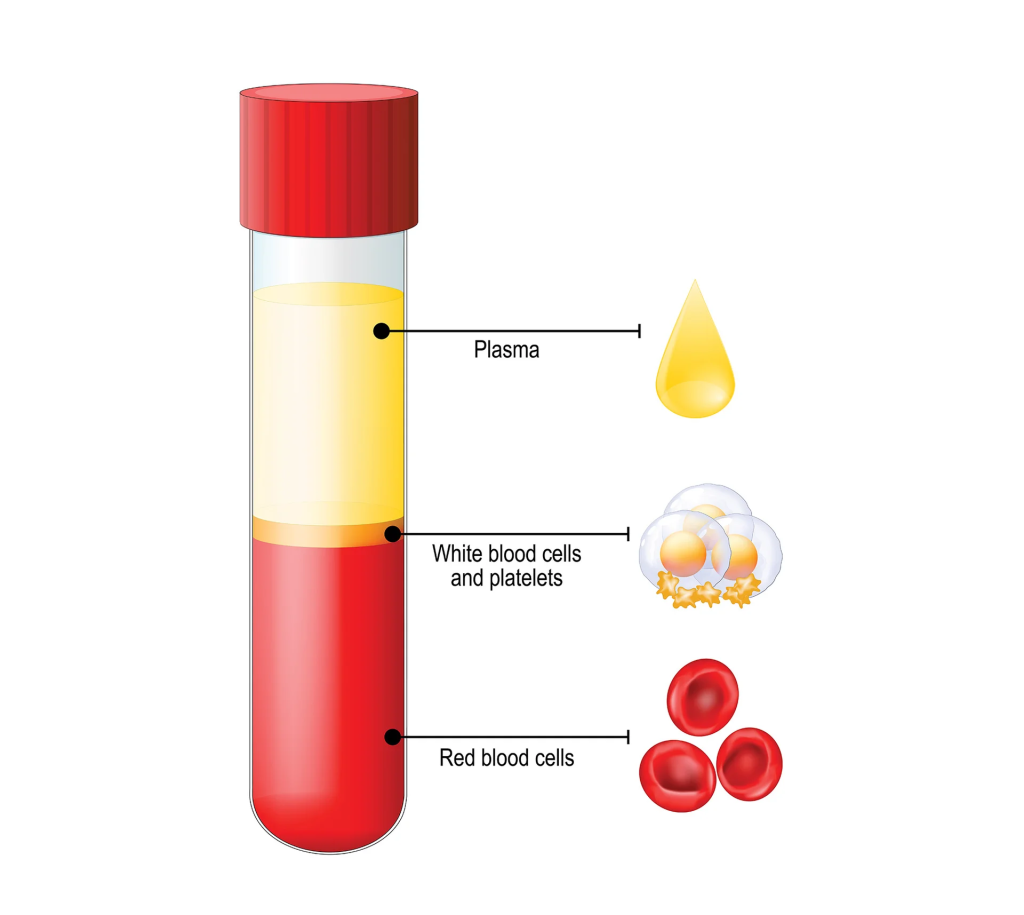
Blood contains three main types of cells, each with distinct structures and functions. These cells make up approximately 45% of blood.
Red Blood Cells (RBCs) / Erythrocytes 🔴
- Structure:
- Shape: RBCs have a biconcave disc shape, which maximizes surface area for gas exchange. This shape also makes them flexible enough to travel through small capillaries.
- Size: RBCs are about 7-8 micrometers in diameter.
- No Nucleus: Mature RBCs lack a nucleus, allowing for more room to carry hemoglobin, the protein that binds oxygen.
- Hemoglobin: The key component of RBCs is hemoglobin, a protein that binds to oxygen (O2) in the lungs and transports it to tissues. Hemoglobin also carries some carbon dioxide (CO2) back to the lungs for exhalation.
- Function:
- Oxygen Transport: RBCs carry oxygen from the lungs to the tissues and return carbon dioxide from the tissues to the lungs for exhalation.
- Carbon Dioxide Transport: Hemoglobin also facilitates the transport of CO2, a waste product of metabolism, back to the lungs.
- Blood pH Regulation: By carrying carbon dioxide, RBCs help regulate blood pH through the carbonic acid-bicarbonate buffer system.
White Blood Cells (WBCs) / Leukocytes ⚪
WBCs are part of the immune system and are responsible for defending the body against infections, foreign invaders, and abnormal cells. There are five main types of white blood cells, classified into granulocytes and agranulocytes.
- Structure:
- Nucleus: Unlike RBCs, WBCs have a prominent nucleus, which can be lobed (in granulocytes) or round (in agranulocytes).
- Size: WBCs are larger than RBCs, typically ranging from 12 to 17 micrometers in diameter.
- Types of WBCs:
- Granulocytes (with granules in their cytoplasm):
- Neutrophils: The most abundant type of WBC. Neutrophils are the first responders to infection, particularly bacterial infections.
- Eosinophils: Involved in allergic reactions and combating parasitic infections.
- Basophils: Release histamine and heparin in response to allergens and play a role in inflammation.
- Agranulocytes (without visible granules):
- Lymphocytes: These include B cells (which produce antibodies), T cells (which attack infected or cancerous cells), and natural killer (NK) cells.
- Monocytes: These mature into macrophages that phagocytize pathogens, dead cells, and debris. They also play a role in antigen presentation.
- Granulocytes (with granules in their cytoplasm):
- Function:
- Immunity: WBCs defend the body against infections, produce antibodies, and destroy foreign invaders.
- Inflammation: They are involved in the inflammatory response, helping to localize and remove infections.
- Surveillance: Some WBCs (especially T cells and NK cells) identify and destroy abnormal or infected cells in the body.
Platelets (Thrombocytes) 🟠
Platelets are small, disc-shaped cell fragments that play a critical role in blood clotting and wound healing.
- Structure:
- Shape: Platelets are small, irregularly shaped cell fragments derived from megakaryocytes (large cells in the bone marrow).
- No Nucleus: Platelets lack a nucleus but contain granules with clotting factors.
- Size: Platelets are about 2-4 micrometers in diameter.
- Function:
- Hemostasis: Platelets play a key role in stopping bleeding by forming clots at injury sites.
- Blood Coagulation: Platelets adhere to damaged blood vessels, aggregate, and release clotting factors that help in the conversion of fibrinogen to fibrin, which forms a stable clot.
- Wound Repair: Platelets also release growth factors that help with tissue repair and wound healing.
3. Blood Grouping 🧬
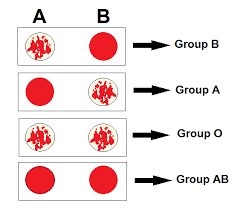
Blood groups are determined by the presence or absence of certain antigens on the surface of RBCs. The two most important blood group systems are the ABO system and the Rh system:
- ABO Blood Group System: This system is based on the presence of A and B antigens on the surface of RBCs. Blood types include A, B, AB, and O.
- Rh Factor: The Rh antigen (also known as the Rh factor) can either be present (Rh-positive) or absent (Rh-negative) on the surface of RBCs. This determines the Rh status of an individual and is crucial in blood transfusions and pregnancy.
4. Blood Composition 🔄
- Plasma: 55% of blood volume, consisting of water, proteins, electrolytes, hormones, and waste products.
- Red Blood Cells (RBCs): 45% of blood volume, responsible for oxygen and carbon dioxide transport.
- White Blood Cells (WBCs): Less than 1% of blood volume, responsible for immune defense.
- Platelets: Less than 1% of blood volume, crucial for blood clotting and wound healing.
Blood is a complex fluid with a variety of components that work together to maintain vital functions such as oxygen transport, immunity, coagulation, and waste removal. Understanding the structure and functions of blood components is essential in healthcare settings for diagnosing and treating various blood-related disorders, such as anemia, infections, clotting disorders, and immune diseases.
Blood Vessels – Arterial and Venous Systems🩸
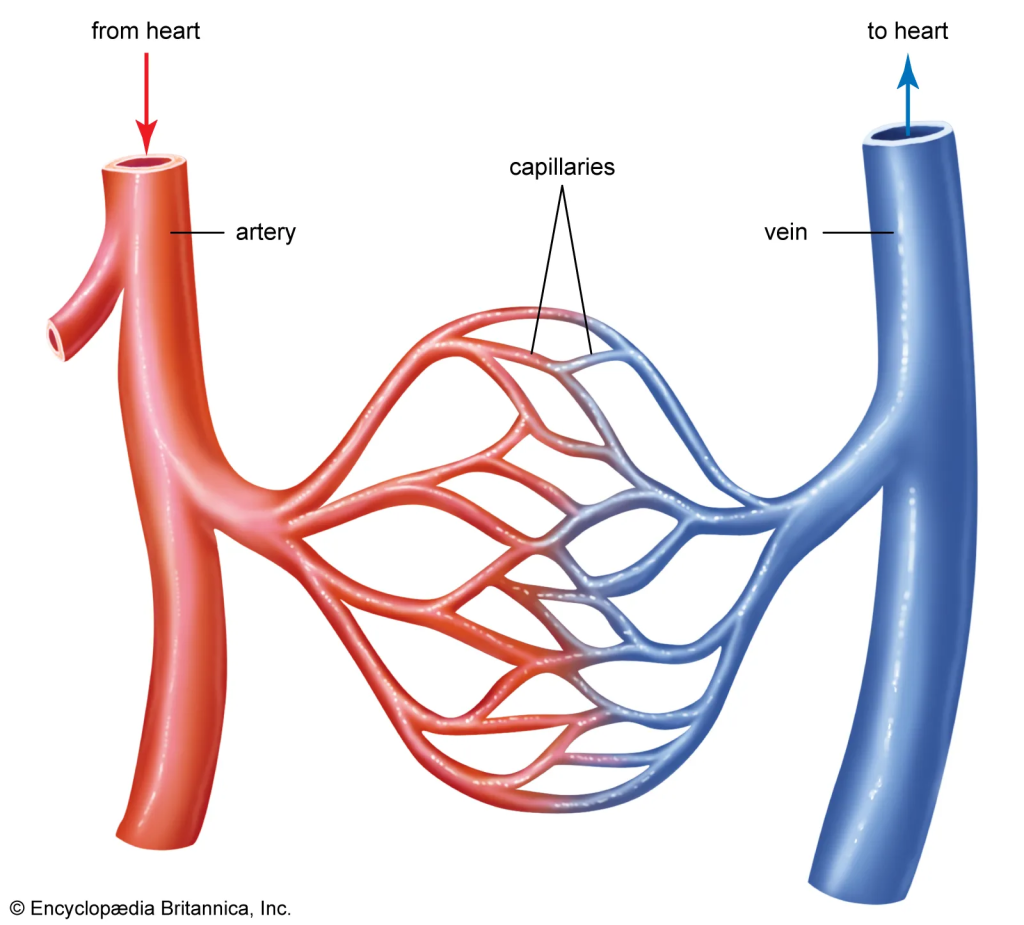
Blood vessels form an extensive network that carries blood throughout the body, ensuring the transport of nutrients, gases, waste products, and immune cells. They are classified into two main types: arteries and veins, each playing distinct roles in the circulatory system. Let’s explore the arterial and venous systems in detail:
1. Arterial System 🚀
The arterial system is responsible for carrying oxygenated blood (except for pulmonary circulation) from the heart to the tissues and organs. It consists of large, muscular vessels that can withstand the high pressure generated by the heart’s pumping action.
Key Arteries and Their Functions:
- Aorta:
- Structure: The largest artery in the body, originating from the left ventricle of the heart. It is about 2.5 cm in diameter and several centimeters long.
- Function: The aorta carries oxygen-rich blood from the heart to the rest of the body. It has several branches that supply blood to the head, neck, upper limbs, and lower limbs.
- Sections:
- Ascending Aorta: The initial portion of the aorta that rises from the heart and gives off the coronary arteries (which supply the heart).
- Aortic Arch: The curved portion of the aorta that gives rise to major branches, including the brachiocephalic trunk, left common carotid artery, and left subclavian artery.
- Descending Aorta: The portion that travels down through the thoracic and abdominal regions, giving rise to arteries that supply the trunk and lower limbs.
- Coronary Arteries:
- Structure: Branches off the ascending aorta to supply the heart muscle (myocardium) with oxygenated blood.
- Function: These arteries are crucial for the heart’s own blood supply and its ability to function effectively.
- Carotid Arteries:
- Structure: The common carotid arteries are located on either side of the neck and bifurcate into the internal carotid artery (supplying the brain) and external carotid artery (supplying the face and neck).
- Function: These arteries provide blood to the head, neck, and brain. The internal carotid artery is especially important for cerebral circulation.
- Subclavian Arteries:
- Structure: These arteries arise from the aortic arch and supply blood to the upper limbs, neck, and brain.
- Function: The right subclavian artery arises from the brachiocephalic trunk, while the left subclavian artery arises directly from the aortic arch.
- Renal Arteries:
- Structure: These arteries branch off the abdominal aorta to supply the kidneys.
- Function: They deliver oxygenated blood to the kidneys for filtration and waste elimination.
- Femoral Arteries:
- Structure: The femoral artery is the main artery that supplies blood to the thigh and lower limb.
- Function: It is a continuation of the external iliac artery and provides blood to the lower extremities.
Artery Structure 🧱:
- Tunica Intima: The innermost layer, made of endothelial cells that reduce friction for blood flow.
- Tunica Media: The middle layer, made of smooth muscle and elastic tissue. This layer allows arteries to withstand high pressure and maintain elasticity, helping them expand and contract as blood is pumped.
- Tunica Externa: The outer layer made of connective tissue, providing structural support and protection.
Arterial Function:
- High Pressure System: Arteries carry blood at high pressure as it is pumped directly from the heart. This high pressure ensures efficient blood flow to organs and tissues.
- Elasticity and Compliance: Arteries are elastic, which allows them to expand when blood is pumped and return to their original shape, ensuring continuous blood flow.
2. Venous System 🧳
The venous system is responsible for carrying deoxygenated blood (except for pulmonary circulation) back to the heart. Veins have thinner walls and larger lumens compared to arteries and are designed to handle the lower pressure of blood returning to the heart.
Key Veins and Their Functions:
- Superior and Inferior Vena Cavae:
- Structure: The superior vena cava returns deoxygenated blood from the head, neck, and upper limbs, while the inferior vena cava returns blood from the lower limbs, abdomen, and pelvis.
- Function: Both veins drain into the right atrium of the heart, completing the circuit of systemic circulation.
- Jugular Veins:
- Structure: The internal jugular veins drain blood from the brain, face, and neck, while the external jugular veins drain blood from the superficial parts of the head and neck.
- Function: These veins return blood from the head and neck to the superior vena cava.
- Pulmonary Veins:
- Structure: These are unique veins because they carry oxygenated blood from the lungs to the left atrium of the heart.
- Function: They complete the pulmonary circulation by returning oxygen-rich blood to the heart for systemic distribution.
- Femoral Vein:
- Structure: The femoral vein is the primary vein in the thigh, draining deoxygenated blood from the lower extremities.
- Function: It is a continuation of the popliteal vein and eventually merges into the external iliac vein.
- Renal Veins:
- Structure: These veins drain the kidneys, returning filtered blood to the inferior vena cava.
- Function: The renal veins carry deoxygenated blood that has been filtered by the kidneys, removing waste products and excess fluid.
Vein Structure 🧱:
- Tunica Intima: The innermost layer, composed of endothelial cells, facilitating smooth blood flow.
- Tunica Media: This layer is thinner in veins than in arteries. It contains some smooth muscle and elastic fibers but is not as thick because veins carry blood under lower pressure.
- Tunica Externa: The outer layer, made of connective tissue, providing structural support and flexibility.
Venous Function:
- Low Pressure System: Veins carry blood back to the heart at low pressure. Because of this, they have one-way valves to prevent backflow, ensuring blood moves toward the heart.
- Reservoir Function: Veins act as blood reservoirs, holding about 60-70% of the body’s total blood volume. This is particularly important for regulating blood volume and returning blood to the heart during increased physical activity.
3. Differences Between Arteries and Veins 🔍
| Feature | Arteries | Veins |
|---|---|---|
| Function | Carry oxygenated blood away from the heart | Carry deoxygenated blood to the heart |
| Structure | Thicker walls, more elastic | Thinner walls, less elastic |
| Pressure | High pressure (due to heart pumping) | Low pressure (returning to heart) |
| Lumen Size | Smaller lumen | Larger lumen |
| Valves | No valves (except in arteries in the heart) | Contain valves to prevent backflow |
| Flow | Pulse-like flow | Steady flow |
4. Capillaries: The Link Between Arterial and Venous Systems 🌱
- Structure: Capillaries are the smallest blood vessels, with walls that are only one cell thick, allowing for easy exchange of gases, nutrients, and waste products between blood and tissues.
- Function: They connect the arterial and venous systems and facilitate gas exchange (oxygen and carbon dioxide) and the movement of nutrients and waste between blood and surrounding tissues.
- Capillary Beds: Extensive networks of capillaries ensure efficient exchange and nutrient delivery to tissues throughout the body.
The arterial and venous systems work in tandem to transport blood throughout the body, maintaining efficient circulation and supporting vital functions like gas exchange, nutrient delivery, and waste removal. Arteries carry oxygenated blood from the heart to tissues under high pressure, while veins return deoxygenated blood at low pressure, relying on valves to prevent backflow. Understanding the structure and function of these blood vessels is fundamental in diagnosing and treating cardiovascular conditions such as arterial disease, venous insufficiency, and hypertension.
Position of the Heart Relative to the Associated Structures ❤️


The heart is a vital organ that pumps blood throughout the body. Understanding its position in relation to other structures in the body is important for diagnosing and managing cardiovascular conditions. The heart is located in the thoracic cavity (chest), and its position relative to surrounding structures is influenced by factors like the diaphragm, lungs, spine, and sternum.
1. General Location of the Heart 📍
- Thoracic Cavity: The heart is located within the mediastinum, the central compartment of the thoracic cavity, which lies between the lungs.
- Orientation: The heart is positioned slightly to the left of the midline of the body, with about two-thirds of its mass lying to the left of the sternum, and one-third to the right. The apex (the pointed bottom part of the heart) is directed downward, forward, and to the left, while the base (the top part) is directed upward, backward, and to the right.
2. Position Relative to Surrounding Structures 🧭
- Anteriorly (Front):
- The heart is positioned behind the sternum (breastbone), which is a flat bone that serves as the central point of the anterior thoracic wall.
- The costal cartilage of the ribs (the cartilaginous portions of the ribs) lies just in front of the heart. These cartilages protect the heart to some extent but still allow some movement during breathing.
- Posteriorly (Back):
- The heart is positioned in front of the thoracic spine (vertebral column), particularly the T5-T8 vertebrae (in the mid-thoracic region).
- The esophagus (the tube that carries food to the stomach) runs behind the heart. This is why swallowing or eating large meals may sometimes cause pressure or discomfort that can feel similar to chest pain.
- Superiorly (Above):
- The heart is bordered superiorly by the great vessels, which include the aorta (carrying oxygenated blood from the heart to the body) and the superior vena cava (returning deoxygenated blood to the heart). These vessels emerge from the base of the heart, which is the uppermost portion.
- The trachea (windpipe) and bronchi (air passages that lead to the lungs) are also located superiorly to the heart. The thymus gland (in children and adolescents) is also situated in front of the heart but above the sternum.
- Inferiorly (Below):
- The heart sits on top of the diaphragm, a large muscle that separates the thoracic cavity from the abdominal cavity. The diaphragm is crucial for respiration, and its position plays a significant role in the heart’s movement during breathing.
- The liver lies just below the right side of the heart, while the stomach and intestines lie beneath the left side of the heart, specifically under the left ventricle.
- Laterally (Sides):
- On the right side of the heart, it is adjacent to the right lung and the right pleural cavity. The heart is separated from the lungs by the mediastinum.
- On the left side, the heart is adjacent to the left lung and the left pleural cavity, with the left ventricle making up most of the heart’s mass. The left lung is slightly smaller than the right lung due to the position of the heart, which leaves a cardiac notch in the left lung to accommodate the apex of the heart.
3. Heart’s Position Within the Mediastinum 🌟
- The heart is located in the middle mediastinum, which is a region in the thoracic cavity. The mediastinum also houses the trachea, esophagus, thymus gland, and major blood vessels.
- The mediastinum is subdivided into the anterior, middle, posterior, and superior sections:
- Middle Mediastinum: This region contains the heart, the pericardium (the sac-like membrane surrounding the heart), and the major blood vessels connected to the heart (the aorta, superior vena cava, pulmonary arteries, and veins).
- Anterior Mediastinum: Located in front of the heart, it contains the thymus gland, some lymph nodes, and fat.
- Posterior Mediastinum: Located behind the heart, it contains the esophagus, descending aorta, thoracic duct, and sympathetic nerves.
4. Pericardium and Protective Layers 🛡️
The heart is surrounded by a protective membrane called the pericardium, which consists of two layers:
- Fibrous Pericardium: The outer layer that provides structural support and prevents over-expansion of the heart.
- Serous Pericardium: The inner layer that consists of two sub-layers:
- Parietal layer: Lines the fibrous pericardium.
- Visceral layer: Also called the epicardium, this layer is directly attached to the surface of the heart.
- Between these layers is the pericardial cavity, which contains a small amount of fluid that reduces friction as the heart beats.
5. Heart’s Location in Relation to the Chest Wall (Clinical Relevance) 🩺
- Apex Beat: The apex of the heart is located at the 5th intercostal space, at the midclavicular line on the left side of the chest. This is where the heart’s beating can be felt most strongly on physical examination.
- Percussion and Auscultation: During a physical examination, the nurse or healthcare provider may use a stethoscope to listen to the heart sounds over the precordium (the front of the chest). The heart’s location is crucial for accurately assessing heart sounds and murmurs.
- Radiographic Imaging: The position of the heart is important when interpreting chest X-rays and echocardiograms. An understanding of the heart’s position relative to the lungs, diaphragm, and other structures is critical for diagnosing abnormalities.
6. Factors Affecting Heart Position ⚖️
- Body Position: The position of the heart can shift slightly depending on body posture. For example, when a person is lying down, gravity shifts the heart to a more horizontal position. When standing, gravity pulls the heart to a more vertical position.
- Age and Body Size: In children and infants, the heart is positioned more centrally in the chest, whereas in adults, the heart tends to be slightly tilted to the left. Body size and the amount of pericardial fat can also affect the heart’s position.
The heart is centrally located within the thoracic cavity, nestled between the lungs, just behind the sternum, and above the diaphragm. It is surrounded by protective layers, including the pericardium, and its position relative to various structures is important in both clinical practice and diagnostic imaging. Understanding the precise location of the heart and its associated structures helps healthcare professionals assess heart function, diagnose diseases, and interpret imaging results effectively.
Position of the Heart Relative to the Associated Structures ❤️
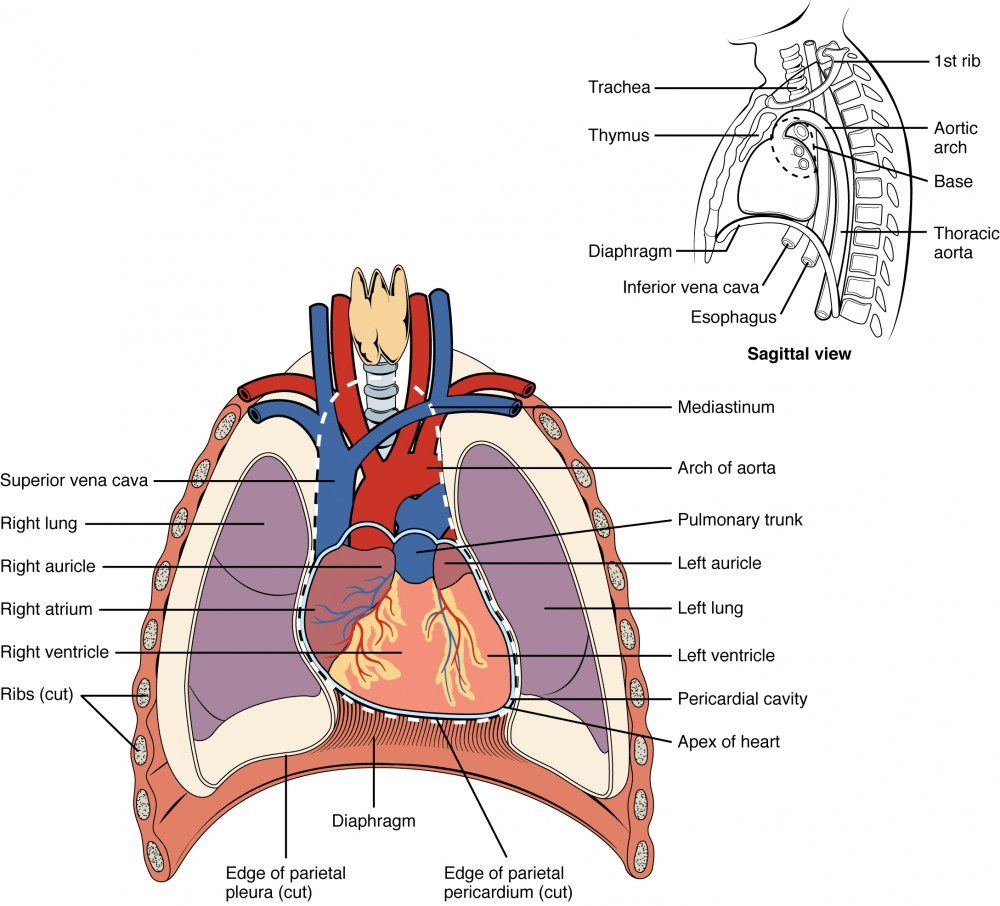
The heart is a vital organ that pumps blood throughout the body. Understanding its position in relation to other structures in the body is important for diagnosing and managing cardiovascular conditions. The heart is located in the thoracic cavity (chest), and its position relative to surrounding structures is influenced by factors like the diaphragm, lungs, spine, and sternum.
1. General Location of the Heart 📍
- Thoracic Cavity: The heart is located within the mediastinum, the central compartment of the thoracic cavity, which lies between the lungs.
- Orientation: The heart is positioned slightly to the left of the midline of the body, with about two-thirds of its mass lying to the left of the sternum, and one-third to the right. The apex (the pointed bottom part of the heart) is directed downward, forward, and to the left, while the base (the top part) is directed upward, backward, and to the right.
2. Position Relative to Surrounding Structures 🧭
- Anteriorly (Front):
- The heart is positioned behind the sternum (breastbone), which is a flat bone that serves as the central point of the anterior thoracic wall.
- The costal cartilage of the ribs (the cartilaginous portions of the ribs) lies just in front of the heart. These cartilages protect the heart to some extent but still allow some movement during breathing.
- Posteriorly (Back):
- The heart is positioned in front of the thoracic spine (vertebral column), particularly the T5-T8 vertebrae (in the mid-thoracic region).
- The esophagus (the tube that carries food to the stomach) runs behind the heart. This is why swallowing or eating large meals may sometimes cause pressure or discomfort that can feel similar to chest pain.
- Superiorly (Above):
- The heart is bordered superiorly by the great vessels, which include the aorta (carrying oxygenated blood from the heart to the body) and the superior vena cava (returning deoxygenated blood to the heart). These vessels emerge from the base of the heart, which is the uppermost portion.
- The trachea (windpipe) and bronchi (air passages that lead to the lungs) are also located superiorly to the heart. The thymus gland (in children and adolescents) is also situated in front of the heart but above the sternum.
- Inferiorly (Below):
- The heart sits on top of the diaphragm, a large muscle that separates the thoracic cavity from the abdominal cavity. The diaphragm is crucial for respiration, and its position plays a significant role in the heart’s movement during breathing.
- The liver lies just below the right side of the heart, while the stomach and intestines lie beneath the left side of the heart, specifically under the left ventricle.
- Laterally (Sides):
- On the right side of the heart, it is adjacent to the right lung and the right pleural cavity. The heart is separated from the lungs by the mediastinum.
- On the left side, the heart is adjacent to the left lung and the left pleural cavity, with the left ventricle making up most of the heart’s mass. The left lung is slightly smaller than the right lung due to the position of the heart, which leaves a cardiac notch in the left lung to accommodate the apex of the heart.
3. Heart’s Position Within the Mediastinum 🌟
- The heart is located in the middle mediastinum, which is a region in the thoracic cavity. The mediastinum also houses the trachea, esophagus, thymus gland, and major blood vessels.
- The mediastinum is subdivided into the anterior, middle, posterior, and superior sections:
- Middle Mediastinum: This region contains the heart, the pericardium (the sac-like membrane surrounding the heart), and the major blood vessels connected to the heart (the aorta, superior vena cava, pulmonary arteries, and veins).
- Anterior Mediastinum: Located in front of the heart, it contains the thymus gland, some lymph nodes, and fat.
- Posterior Mediastinum: Located behind the heart, it contains the esophagus, descending aorta, thoracic duct, and sympathetic nerves.
4. Pericardium and Protective Layers 🛡️
The heart is surrounded by a protective membrane called the pericardium, which consists of two layers:
- Fibrous Pericardium: The outer layer that provides structural support and prevents over-expansion of the heart.
- Serous Pericardium: The inner layer that consists of two sub-layers:
- Parietal layer: Lines the fibrous pericardium.
- Visceral layer: Also called the epicardium, this layer is directly attached to the surface of the heart.
- Between these layers is the pericardial cavity, which contains a small amount of fluid that reduces friction as the heart beats.
5. Heart’s Location in Relation to the Chest Wall (Clinical Relevance) 🩺
- Apex Beat: The apex of the heart is located at the 5th intercostal space, at the midclavicular line on the left side of the chest. This is where the heart’s beating can be felt most strongly on physical examination.
- Percussion and Auscultation: During a physical examination, the nurse or healthcare provider may use a stethoscope to listen to the heart sounds over the precordium (the front of the chest). The heart’s location is crucial for accurately assessing heart sounds and murmurs.
- Radiographic Imaging: The position of the heart is important when interpreting chest X-rays and echocardiograms. An understanding of the heart’s position relative to the lungs, diaphragm, and other structures is critical for diagnosing abnormalities.
6. Factors Affecting Heart Position ⚖️
- Body Position: The position of the heart can shift slightly depending on body posture. For example, when a person is lying down, gravity shifts the heart to a more horizontal position. When standing, gravity pulls the heart to a more vertical position.
- Age and Body Size: In children and infants, the heart is positioned more centrally in the chest, whereas in adults, the heart tends to be slightly tilted to the left. Body size and the amount of pericardial fat can also affect the heart’s position.
The heart is centrally located within the thoracic cavity, nestled between the lungs, just behind the sternum, and above the diaphragm. It is surrounded by protective layers, including the pericardium, and its position relative to various structures is important in both clinical practice and diagnostic imaging. Understanding the precise location of the heart and its associated structures helps healthcare professionals assess heart function, diagnose diseases, and interpret imaging results effectively.
🫀 Chambers of the Heart

The human heart is a muscular, four-chambered organ about the size of your fist, located slightly to the left of the center of your chest. It works like a double pump to circulate blood throughout the body. Let’s explore its four chambers:
❤️ 1. Right Atrium (RA) – The Receiver from the Body
- Location: Upper right side of the heart
- Function: Receives deoxygenated blood from the body
- Receives blood via:
- Superior vena cava (from upper body)
- Inferior vena cava (from lower body)
- Coronary sinus (from heart muscles)
- Passes blood to: Right ventricle through tricuspid valve
🧠 Mnemonic: RA = Receives All used (deoxygenated) blood from the body
💙 2. Right Ventricle (RV) – The Pump to the Lungs
- Location: Lower right side of the heart
- Function: Pumps deoxygenated blood to the lungs
- Through: Pulmonary artery
- Valves involved:
- Receives blood from RA via tricuspid valve
- Sends blood to lungs via pulmonary valve
🚴♂️ Mnemonic: RV = Ride to the lungs for fresh oxygen
❤️ 3. Left Atrium (LA) – The Receiver from the Lungs
- Location: Upper left side of the heart
- Function: Receives oxygenated blood from lungs
- Receives blood via: Four pulmonary veins (2 from each lung)
- Passes blood to: Left ventricle through mitral (bicuspid) valve
🌬️ Mnemonic: LA = Lungs Arrived (oxygen-rich blood)
💪 4. Left Ventricle (LV) – The Main Pump to the Body
- Location: Lower left side of the heart
- Function: Pumps oxygenated blood to the entire body
- Through: Aorta (largest artery)
- Valves involved:
- Receives from LA via mitral valve
- Pumps into aorta via aortic valve
🏋️♂️ Mnemonic: LV = Lifts blood to the whole body
🧭 Summary Table
| Chamber | Blood Type | Source | Valve (Inlet) | Valve (Outlet) | Destination |
|---|---|---|---|---|---|
| Right Atrium | Deoxygenated | Body (via vena cavae) | – | Tricuspid Valve | Right Ventricle |
| Right Ventricle | Deoxygenated | Right Atrium | Tricuspid Valve | Pulmonary Valve | Lungs (via artery) |
| Left Atrium | Oxygenated | Lungs (via veins) | – | Mitral (Bicuspid) | Left Ventricle |
| Left Ventricle | Oxygenated | Left Atrium | Mitral Valve | Aortic Valve | Body (via aorta) |
🎨 Fun Visualization:
Imagine the heart like a house with four rooms:
- 🏠 Two atria upstairs (collect blood)
- 🏠 Two ventricles downstairs (pump blood)
- Valves are like doors that allow one-way flow only!
🫀 Layers of the Heart – The Heart Wall & Protective Coverings
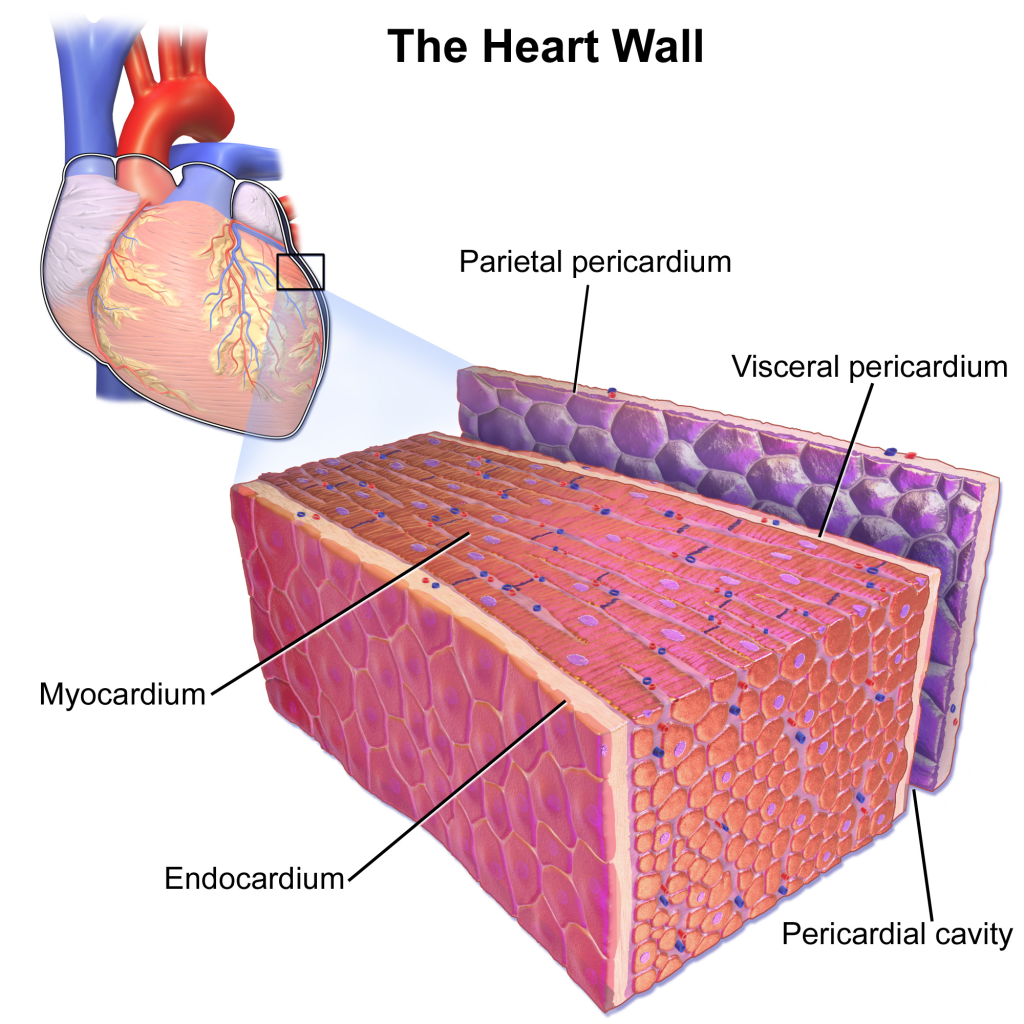
The heart is not just a pump—it’s a structurally sophisticated organ, protected and powered by several carefully organized layers. Each layer plays a specific role in protecting the heart, enabling its pumping action, and maintaining internal flow. Let’s dive deep into the five main layers from outside to inside.
🧣 1. Pericardium – The Double-Layered Protective Sac
The pericardium is like a sturdy double-layered coat for the heart. It shields the heart, allows free movement, and prevents overexpansion.
🧱 A) Fibrous Pericardium (Outer Tough Layer)
- Composition: Dense irregular connective tissue
- Anchors the heart to the diaphragm, sternum, and great vessels
- Prevents overfilling of the heart during high venous return
- Protects from mechanical injury
🧠 Clinical Insight: In cardiac tamponade, fluid accumulation within the pericardium compresses the heart and restricts its filling.
💦 B) Serous Pericardium (Thin, Moist Inner Layer)
This is a double-layered serous membrane that secretes fluid to reduce friction.
- Parietal Layer: Lines the fibrous pericardium internally
- Visceral Layer (Epicardium): Adheres directly to the surface of the heart
🧴 Pericardial Cavity: Space between parietal and visceral layers, filled with ~15–50 mL of pericardial fluid (lubricant that prevents friction during heartbeat)
💗 2. Epicardium – The Slippery Outer Layer of the Heart Wall
- Structure: Mesothelial cells + connective tissue + adipose tissue
- Contains: Coronary arteries, lymphatics, and autonomic nerves
- Function: Reduces surface friction; serves as protective covering
🎨 Analogy: Like the smooth outer glaze on a cake – protective, slippery, and smooth.
🧠 Clinical Note: In pericarditis, inflammation of the epicardium can lead to chest pain and pericardial rub.
💪 3. Myocardium – The Muscular Middle Layer (The Pump)
- Structure: Specialized cardiac muscle fibers
- Striated, branched, and interconnected by intercalated discs
- Involuntary, rich in mitochondria for endurance
- Thickness varies:
- Thickest in Left Ventricle (systemic circulation)
- Thinner in Atria
- Function: Contracts to pump blood into circulation
🧠 Clinical Insight:
- Myocardial infarction (MI) = death of myocardial tissue due to interrupted blood supply
- Cardiomyopathy = disease of myocardium affecting its contractile function
🩸 4. Endocardium – The Smooth Inner Lining
- Structure: Thin layer of simple squamous epithelium (endothelium) + connective tissue
- Lines: All heart chambers, valves, and is continuous with vascular endothelium
- Function: Provides non-thrombogenic surface, supports valve function, ensures smooth blood flow
🧠 Clinical Insight:
- Endocarditis is the infection of this layer, often affecting heart valves (can be bacterial or fungal in origin)
📊 Summary Table of Heart Wall Layers
| Layer | Location | Main Components | Functions | Clinical Relevance |
|---|---|---|---|---|
| Fibrous Pericardium | Outermost sac | Dense connective tissue | Protects, anchors, prevents overfilling | Tamponade risk with fluid accumulation |
| Parietal Pericardium | Inner lining of fibrous layer | Serous membrane | Secretes pericardial fluid | Part of pericardial friction rub in pericarditis |
| Visceral Pericardium / Epicardium | Outermost layer of heart wall | Mesothelium + CT + fat | Protects, lubricates, houses coronary vessels | Involved in pericarditis |
| Myocardium | Middle, thickest layer | Cardiac muscle | Pumps blood through contraction | Site of infarction, hypertrophy |
| Endocardium | Inner lining | Endothelium + connective tissue | Prevents blood clotting, smoothens blood flow | Site of endocarditis |
🧠 Mnemonic to Recall Layers (Outer to Inner)
“For Pure Vital Muscle Energy”
- Fibrous Pericardium
- Parietal Pericardium
- Visceral Pericardium (Epicardium)
- Myocardium
- Endocardium
🫀 Heart Valves – The Gatekeepers of the Heart!
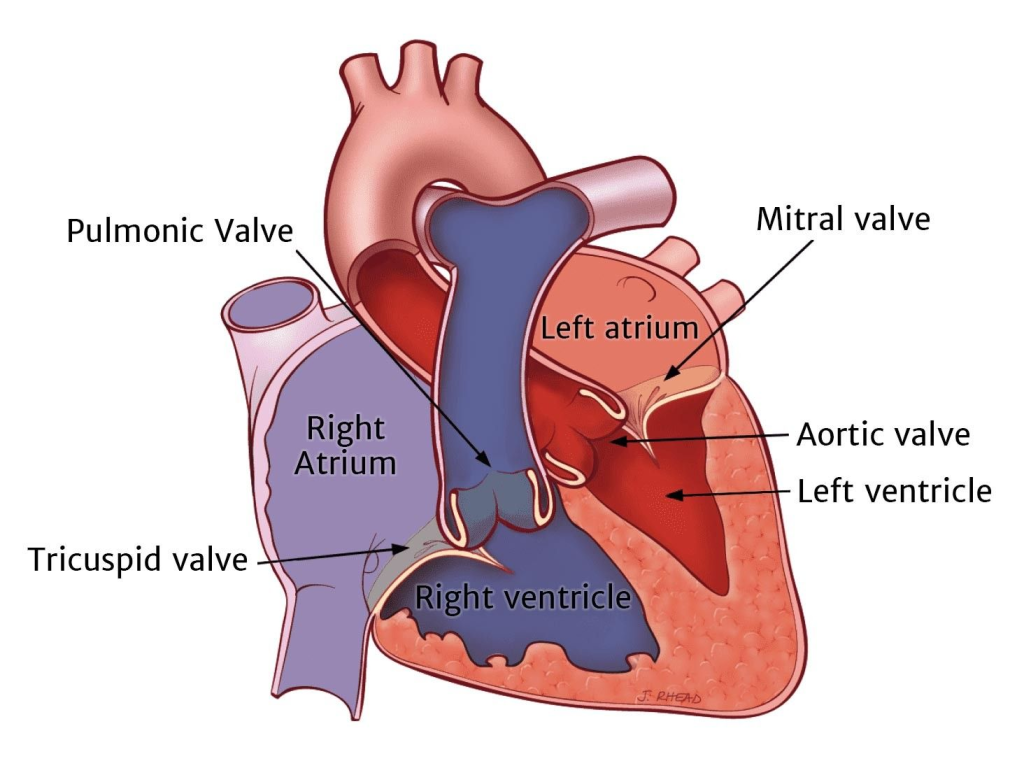
The heart has four main valves that act like one-way doors or traffic signals – they open and close with every heartbeat to ensure unidirectional blood flow and prevent backflow.
🔑 The 4 Heart Valves (Easy Breakdown)
| Type | Valve Name | Location | Function |
|---|---|---|---|
| Atrioventricular (AV) | 1. Tricuspid Valve | Between Right Atrium & Right Ventricle | Prevents backflow into RA during RV contraction |
| 2. Mitral Valve (Bicuspid) | Between Left Atrium & Left Ventricle | Prevents backflow into LA during LV contraction | |
| Semilunar (SL) | 3. Pulmonary Valve | Between Right Ventricle & Pulmonary Artery | Prevents backflow from pulmonary artery into RV |
| 4. Aortic Valve | Between Left Ventricle & Aorta | Prevents backflow from aorta into LV |
🪜 Let’s Understand Each Valve in Detail
🟤 1. Tricuspid Valve – The Right-Sided AV Valve
- Has 3 cusps (leaflets)
- Located between right atrium and right ventricle
- Opens when RA contracts → allows blood into RV
- Closes when RV contracts → prevents regurgitation into RA
🧠 Mnemonic: “Tri to do the right thing” (Tricuspid = Right side)
🔴 2. Mitral Valve (Bicuspid) – The Left-Sided AV Valve
- Has 2 cusps (resembles a bishop’s mitre hat)
- Located between left atrium and left ventricle
- Opens during diastole → blood flows from LA to LV
- Closes during systole → prevents backflow into LA
🧠 Mnemonic: “Bi-cuspid is on the Left” (Bi = 2, Left = L for Love)
🩺 Clinical Tip: Mitral valve prolapse is a common condition where the valve bulges back into the LA.
🟡 3. Pulmonary Valve – The Right-Sided Semilunar Valve
- Between right ventricle and pulmonary artery
- Semilunar (half-moon shaped cusps)
- Opens during ventricular systole → sends blood to lungs
- Closes during diastole → prevents backflow into RV
🧠 Think: “Pulmonary = Lungs” → sends blood to lungs
🔵 4. Aortic Valve – The Left-Sided Semilunar Valve
- Between left ventricle and aorta
- Opens during ventricular contraction (systole) → sends oxygen-rich blood to body
- Closes during relaxation (diastole) → prevents return of blood to LV
🧠 Aorta = main highway to the body → needs a strong valve!
🩺 Clinical Tip: Aortic stenosis is a condition where this valve becomes narrowed and stiff.
🧬 Histology Tip – Valve Structure
- Made of connective tissue core (collagen + elastin)
- Covered by endocardium
- No muscle in valves – they open/close passively due to pressure changes
💡 How Do the Valves Work?
Valves open and close in response to pressure gradients:
- When pressure in atria > ventricles, AV valves open.
- When pressure in ventricles > arteries, semilunar valves open.
- Chordae tendineae (heart strings) and papillary muscles prevent AV valves from inverting.
📊 Summary Table of Valves
| Valve | Cusps | Location | Opens During | Prevents Backflow To |
|---|---|---|---|---|
| Tricuspid | 3 | RA → RV | Atrial systole | Right Atrium |
| Mitral (Bicuspid) | 2 | LA → LV | Atrial systole | Left Atrium |
| Pulmonary | 3 | RV → Pulmonary Artery | Ventricular systole | Right Ventricle |
| Aortic | 3 | LV → Aorta | Ventricular systole | Left Ventricle |
🧠 Mnemonics to Remember All:
🔹 “Try Pulling My Aorta”
→ Tricuspid – Pulmonary – Mitral – Aortic
🔸 AV vs SL:
- AV = between Atria & Ventricles (Tri & Mitral)
- SL = leaving the heart to Lungs & body (Pulmonary & Aortic)
💉 Clinical Conditions Involving Valves:
| Condition | Affected Valve(s) | Description |
|---|---|---|
| Stenosis | Any valve | Narrowed valve → obstructed blood flow |
| Regurgitation | Usually mitral/aortic | Backward flow due to improper valve closure |
| Valve Prolapse | Mostly mitral | Valve flops backward during contraction |
| Infective Endocarditis | Any valve | Infection/inflammation damaging valve tissue |
❤️🔥 Coronary Arteries – The Lifelines of the Heart
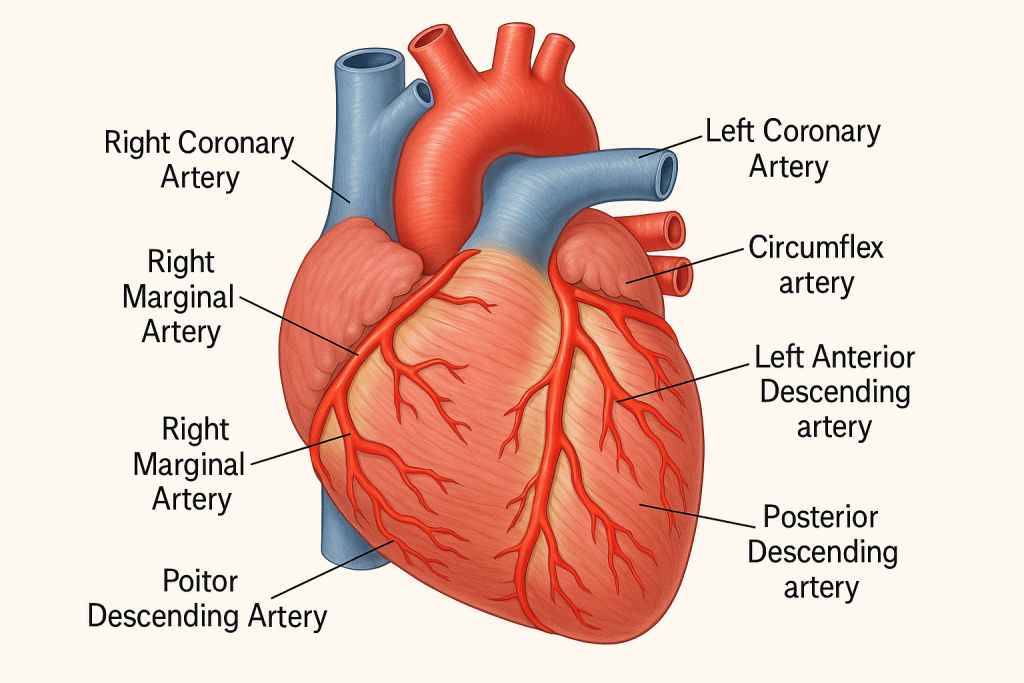
While the heart pumps blood to the entire body, it also needs its own blood supply to survive. This essential nourishment comes from the coronary arteries, which supply oxygen-rich blood to the heart muscle (myocardium) itself.
🫀 No coronary arteries = no oxygen = no heartbeat = cardiac arrest! 🫀
🌟 2 Main Coronary Arteries
The coronary arteries originate from the ascending aorta, just above the aortic valve, and divide into:
🔴 1. Right Coronary Artery (RCA)
- Arises from: Right aortic sinus of ascending aorta
- Travels in: Right atrioventricular (coronary) sulcus
- Supplies:
- Right atrium
- Right ventricle
- Inferior part of left ventricle
- Posterior 1/3 of interventricular septum
- SA node (60%) and AV node (80%)
📍Branches of RCA:
- Right marginal artery → Supplies right ventricle
- Posterior descending artery (PDA)
(a.k.a. posterior interventricular artery) → Supplies posterior interventricular septum and both ventricles
🧠 Mnemonic: “RCA Passes Many Structures”
→ PDA, Marginal artery, SA node
🔵 2. Left Coronary Artery (LCA)
- Arises from: Left aortic sinus of ascending aorta
- Very short main trunk, then divides into:
🔹 A) Left Anterior Descending (LAD) artery
- Runs in anterior interventricular groove
- Supplies:
- Anterior wall of LV
- Anterior 2/3 of interventricular septum
- Apex of the heart
- Bundle of His & right/left bundle branches
🧠 “Widow-maker artery” – blockage here can cause massive anterior MI
🔹 B) Left Circumflex artery (LCx)
- Travels in left coronary sulcus
- Supplies:
- Left atrium
- Lateral & posterior walls of LV
- SA node (40%)
🗺️ Distribution Map of Coronary Arteries
| Region Supplied | Main Artery Involved |
|---|---|
| Right Atrium | Right Coronary Artery (RCA) |
| Right Ventricle | RCA, Right Marginal Branch |
| Left Atrium | Left Circumflex Artery (LCx) |
| Left Ventricle (anterior) | Left Anterior Descending (LAD) |
| Left Ventricle (lateral/posterior) | LCx, RCA |
| Interventricular Septum (ant. 2/3) | LAD |
| Interventricular Septum (post. 1/3) | PDA (from RCA or LCx) |
| SA Node | RCA (60%), LCx (40%) |
| AV Node | RCA (80%) |
🔁 Coronary Circulation Types (Dominance)
🧩 Coronary dominance is defined by which artery gives rise to the posterior descending artery (PDA):
| Type | Definition | Frequency |
|---|---|---|
| Right dominant | PDA arises from RCA | ~70–85% |
| Left dominant | PDA arises from LCx | ~10–15% |
| Co-dominant | PDA from both RCA and LCx | ~5–10% |
🚨 Clinical Significance of Coronary Arteries
| Condition | Description |
|---|---|
| Coronary Artery Disease (CAD) | Atherosclerosis → narrowing/blockage of coronary arteries |
| Myocardial Infarction (MI) | Complete blockage of an artery → heart muscle death |
| Angina Pectoris | Chest pain due to reduced coronary blood flow |
| Coronary Artery Bypass Grafting (CABG) | Surgery to bypass blocked artery using graft |
| Stents/Angioplasty | Ballooning & stenting blocked arteries to restore blood flow |
🧠 Mnemonic: “A Crown for the Heart”
CROWN = Coronary Right, Oxygen Works Now!
- C – Circumflex (LCx)
- R – Right Coronary Artery (RCA)
- O – Oxygen (main job of these arteries)
- W – Widow-maker (LAD)
- N – Nodes (SA & AV) supplied
🧠🫀 Nerve and Blood Supply to the Heart
Understanding the neurovascular supply of the heart is crucial because it controls both contraction and circulation.
🔌 Nerve Supply of the Heart (Autonomic Nervous System)
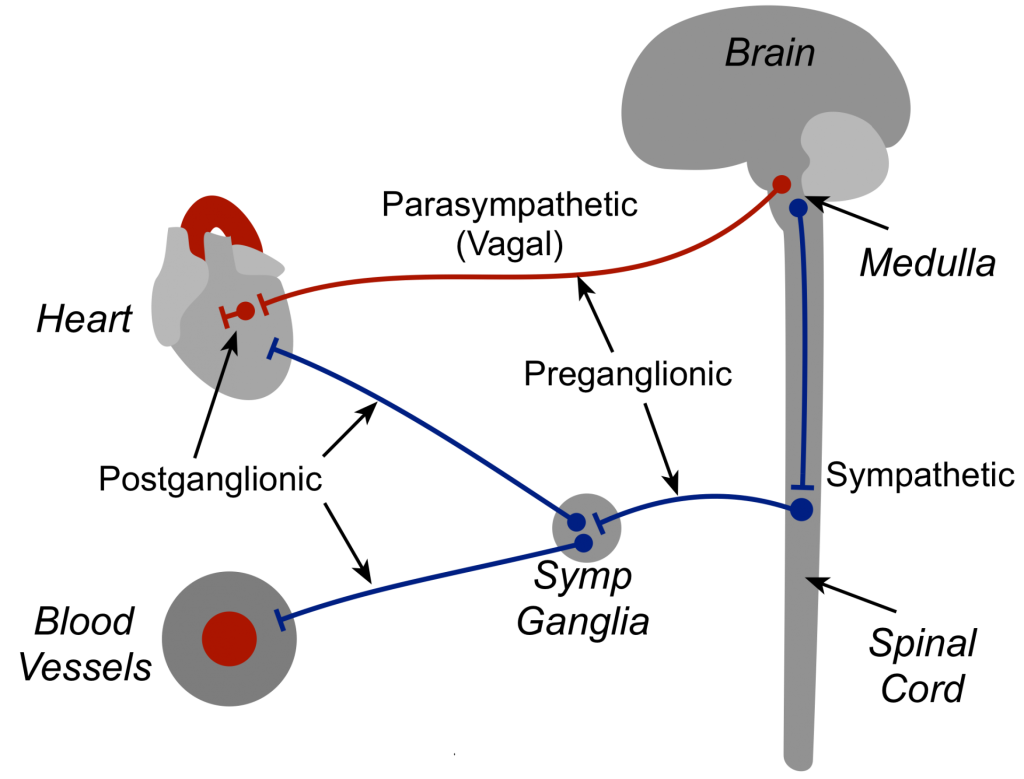
The heart is innervated by both sympathetic and parasympathetic nerves, which regulate heart rate, force of contraction, and coronary vessel tone.
🔸 A) Sympathetic Nerve Supply
- Origin: Thoracic spinal segments (T1–T5)
- Fibers travel via: Cardiac nerves from the sympathetic chain
- Effects:
- ⬆️ Heart rate (positive chronotropy)
- ⬆️ Force of contraction (positive inotropy)
- ⬆️ Conduction speed (positive dromotropy)
- Vasodilation of coronary vessels during stress/exercise
🧠 Fight or flight = faster, stronger heartbeat
🔹 B) Parasympathetic Nerve Supply
- Origin: Vagus nerve (Cranial Nerve X)
- Fibers synapse in cardiac plexus and wall of the heart
- Effects:
- ⬇️ Heart rate
- ⬇️ Force of contraction (mainly atria)
- Vasoconstriction of coronary vessels (mild)
🧠 Rest and digest = slower, calmer heartbeat
📍 Cardiac Plexus (Integration Center)
- Located anterior to the tracheal bifurcation, behind the ascending aorta
- Divides into:
- Superficial cardiac plexus (beneath arch of aorta)
- Deep cardiac plexus (in front of tracheal bifurcation)
🩸 Blood Supply to the Heart (Coronary Circulation)
As covered previously, blood is supplied by two main coronary arteries:
- Left Coronary Artery (LCA): branches into LAD and LCx
- Right Coronary Artery (RCA): branches into PDA and right marginal artery
🩻 Venous Drainage of the Heart
- Major drainage via the coronary sinus, which opens into the right atrium
- Collects blood from:
- Great cardiac vein (from LAD)
- Middle cardiac vein (from PDA)
- Small cardiac vein (from RCA region)
- Minor veins:
- Anterior cardiac veins (drain directly into RA)
- Thebesian veins (tiny vessels that drain directly into all chambers)
🧠 Clinical Relevance
| Condition | Affected Structure |
|---|---|
| MI (Heart Attack) | Coronary artery occlusion |
| Bradycardia | Vagal overactivity (parasympathetic) |
| Tachycardia | Sympathetic overactivity |
| Arrhythmias | Disruption in autonomic control |
🧬 Lymphatic Tissue – The Body’s Immune Defense Network
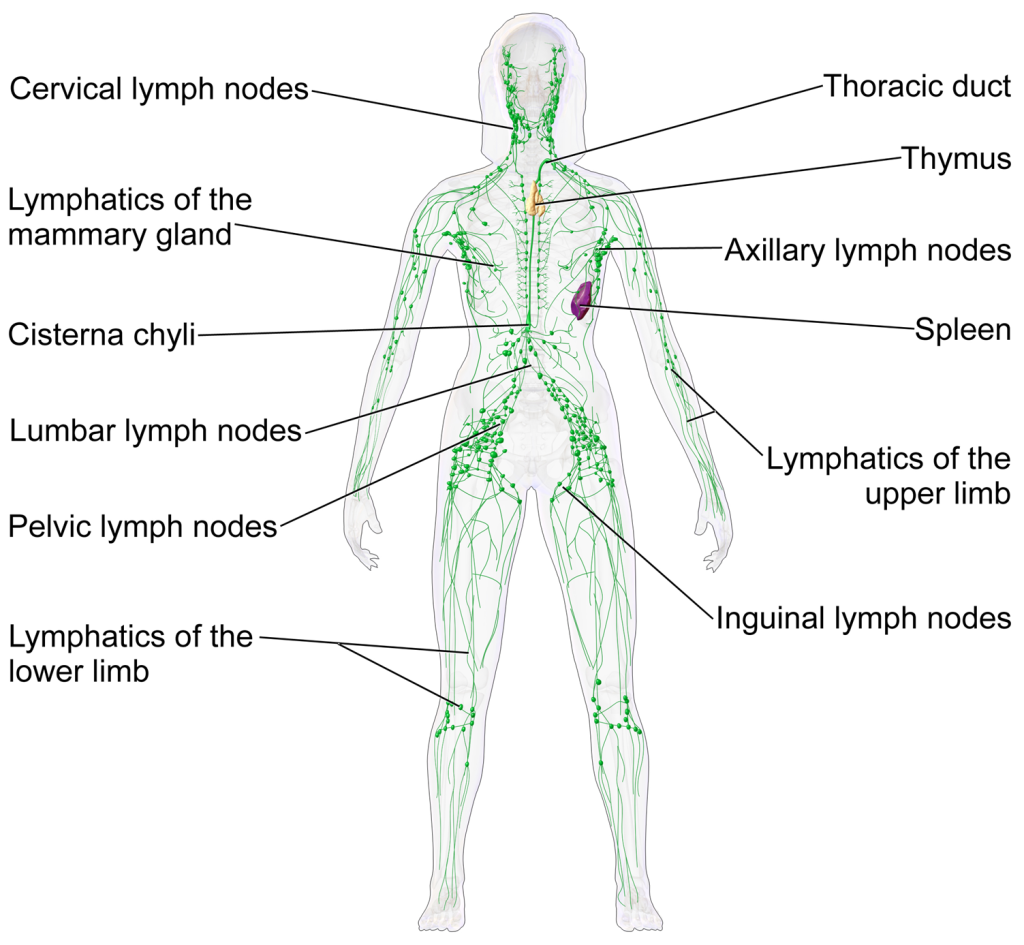
Lymphatic tissue, also called lymphoid tissue, is a type of specialized connective tissue that plays a crucial role in immune defense. It is composed primarily of lymphocytes (B and T cells) and reticular connective tissue, and it acts as a surveillance and filtration system to protect the body from infections and foreign substances.
🌱 Types of Lymphatic Tissue
Lymphatic tissue is broadly classified into:
🔸 1. Primary (Central) Lymphatic Organs
These are the sites where lymphocytes are produced and mature.
a) Bone Marrow
- Located inside long and flat bones
- B lymphocytes mature here
- Produces all blood cells (RBCs, WBCs, platelets)
b) Thymus
- Located in the upper chest (anterior mediastinum)
- T lymphocytes mature here
- Most active in childhood, shrinks after puberty (involution)
🧠 Primary organs = Birthplaces of immunity cells
🔹 2. Secondary (Peripheral) Lymphatic Organs/Tissues
These are the sites where mature lymphocytes encounter antigens and become activated.
a) Lymph Nodes
- Bean-shaped structures located along lymphatic vessels
- Filter lymph and trap pathogens
- Contains B and T cells, macrophages
- Enlarges during infection (lymphadenopathy)
b) Spleen
- Largest lymphatic organ
- Located in the left upper abdomen
- Filters blood, removes old RBCs, stores platelets
- Contains white pulp (lymphocytes) and red pulp (RBCs)
c) Mucosa-Associated Lymphoid Tissue (MALT)
- Diffuse lymphatic tissue found in mucous membranes
- Includes:
- Tonsils (palatine, pharyngeal, lingual)
- Peyer’s patches in small intestine
- Appendix
🧠 Secondary organs = Battlefield where immune cells fight antigens
🧩 Structure of Lymphatic Tissue
| Component | Description |
|---|---|
| Lymphocytes | Key immune cells (B and T cells) |
| Reticular fibers | Form a supporting meshwork (reticular CT) |
| Macrophages | Engulf pathogens and present antigens to lymphocytes |
| Dendritic cells | Specialized antigen-presenting cells (APCs) |
| Germinal centers | Sites of B cell activation, proliferation, and mutation |
🧬 Histological Types of Lymphatic Tissue
| Type | Description | Examples |
|---|---|---|
| Diffuse lymphatic tissue | Scattered lymphocytes without capsule | MALT, respiratory & GI mucosa |
| Nodular (follicular) lymphatic tissue | Densely packed with germinal centers | Lymph nodes, tonsils, spleen |
| Encapsulated lymphatic organs | Surrounded by a connective tissue capsule | Lymph nodes, thymus, spleen |
🛡️ Functions of Lymphatic Tissue
- Immune surveillance – Monitors body fluids for pathogens
- Filtration – Removes foreign particles from lymph/blood
- Immune cell production – Generates and activates B and T cells
- Antibody production – B cells transform into plasma cells
- Memory formation – Stores memory cells for faster future response
📍 Clinical Importance
| Condition | Associated Lymphatic Tissue | Description |
|---|---|---|
| Lymphoma | Lymph nodes or lymphatic organs | Cancer of lymphocytes |
| Tonsillitis | Tonsils (MALT) | Inflammation due to infection |
| Splenomegaly | Spleen | Enlargement due to infection, cancer, etc. |
| Thymic aplasia | Thymus | Congenital T cell deficiency (e.g., DiGeorge) |
| HIV/AIDS | General lymphoid tissues | Gradual destruction of immune system |
🧠 Mnemonic to Remember Lymphatic Organs
“Boys That Sing Loud Songs Might Always Perform”
- Bone Marrow
- Thymus
- Spleen
- Lymph Nodes
- Skin (has immune cells)
- MALT
- Appendix
- Peyer’s patches
🧠🛡️ Major Lymphatic Organs & Tissues –
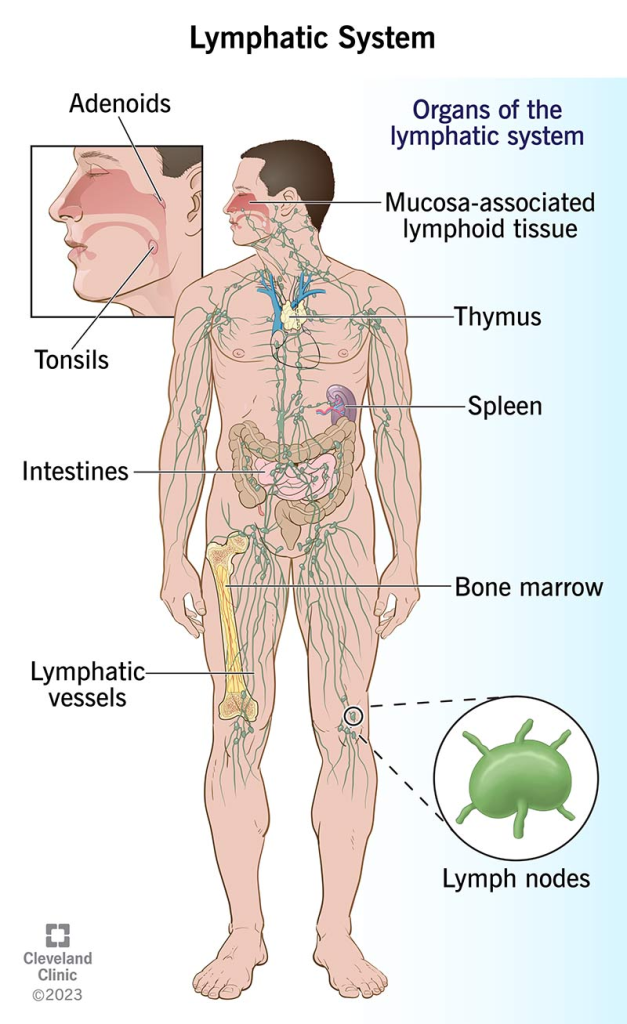
🧬 1. Bone Marrow – The Birthplace of Blood & Immunity
- Location: Found inside long bones (e.g., femur, humerus) and flat bones (e.g., sternum, pelvis)
- Type: Primary lymphoid organ
- Function:
- Produces all blood cells: RBCs, WBCs (lymphocytes, monocytes), and platelets
- B lymphocytes mature here (hence, “B” for Bone marrow)
- Structure:
- Red marrow: active in hematopoiesis
- Yellow marrow: mainly fat, becomes red during extreme need
- Clinical relevance:
- Leukemia: abnormal proliferation of immature WBCs
- Bone marrow biopsy: used to diagnose blood disorders
🌟 2. Thymus – The T Cell University
- Location: Behind the sternum in the anterior mediastinum
- Type: Primary lymphoid organ
- Function:
- Site of T cell maturation and differentiation
- Educates T cells to recognize “self vs. non-self”
- Structure:
- Cortex: immature T cells
- Medulla: mature T cells, contains Hassall’s corpuscles
- Unique feature: Active in children, shrinks (involutes) after puberty
- Clinical relevance:
- DiGeorge Syndrome: congenital absence → no T cells
- Thymoma: tumor, associated with myasthenia gravis
🩸 3. Spleen – The Blood Filter and Lymphocyte Factory
- Location: Left upper quadrant, behind the stomach
- Type: Secondary lymphoid organ
- Function:
- Filters blood, not lymph
- Removes old RBCs, damaged cells, and pathogens
- Stores platelets and blood for emergency use
- Initiates immune responses to blood-borne antigens
- Structure:
- White pulp: lymphocytes (immunity)
- Red pulp: blood-filled sinuses, removes aged cells
- Clinical relevance:
- Splenomegaly: enlargement due to infections, cancer
- Asplenia (removal): ↑ risk of infection, needs vaccination
🧱 4. Lymph Nodes – Immune Checkpoints
- Location: Throughout the body (neck, axilla, groin, abdomen)
- Type: Secondary lymphoid organ
- Function:
- Filter lymph fluid
- Trap bacteria, viruses, cancer cells
- Site for antigen presentation and lymphocyte activation
- Structure:
- Capsule, cortex (B cells), medulla (plasma cells, macrophages)
- Afferent vessels in, efferent vessel out
- Clinical relevance:
- Lymphadenopathy: swollen nodes due to infection or malignancy
- Metastasis: cancer often spreads via lymph nodes
🧴 5. Skin – The Immune Sensor
- Type: Non-classical lymphoid tissue (part of innate immunity)
- Function:
- Acts as first-line barrier to pathogens
- Contains Langerhans cells (specialized dendritic cells)
- Alerts the immune system to danger
- Clinical relevance:
- Dermatitis: allergic/autoimmune response
- Psoriasis: autoimmune inflammation of skin immune response
🧫 6. MALT – Mucosa-Associated Lymphoid Tissue
- Location: Found in mucous membranes of respiratory, digestive, urinary, and reproductive tracts
- Type: Diffuse secondary lymphoid tissue
- Function:
- Provides local immunity at points of entry
- Contains B cells, T cells, plasma cells, and macrophages
- Clinical relevance:
- Tonsillitis, appendicitis, inflammatory bowel disease (IBD) involve MALT
🍽️ 7. Appendix – A Gut-Immune Booster
- Location: Attached to cecum (beginning of large intestine)
- Type: MALT (part of GALT – gut-associated lymphoid tissue)
- Function:
- Stores beneficial bacteria
- Contains lymphoid follicles – immune surveillance in gut
- Clinical relevance:
- Appendicitis: inflammation, often requiring surgical removal
- May play a role in immune memory and gut flora balance
🌾 8. Peyer’s Patches – Gut’s Immune Scouts
- Location: Lining of ileum (last part of small intestine)
- Type: MALT/GALT
- Function:
- Detect and respond to pathogens in the gut
- Sample antigens from intestinal lumen via M cells
- Activate local B and T cell responses
- Structure: Aggregates of lymphoid follicles embedded in the mucosa/submucosa
- Clinical relevance:
- Typhoid fever can ulcerate Peyer’s patches
- Involved in oral vaccine responses
📚 Summary Table
| Organ/Tissue | Type | Main Role | Location |
|---|---|---|---|
| Bone Marrow | Primary | Produces and matures B cells | Inside bones |
| Thymus | Primary | T cell maturation | Mediastinum (chest) |
| Spleen | Secondary | Filters blood, recycles RBCs | LUQ (left upper abdomen) |
| Lymph Nodes | Secondary | Filter lymph, activate lymphocytes | Throughout body |
| Skin | Innate defense | First-line immune protection | Outer body layer |
| MALT | Secondary | Local mucosal immunity | Gut, lungs, genitourinary tract |
| Appendix | MALT/GALT | Gut immunity, flora reservoir | Cecum (lower right abdomen) |
| Peyer’s Patches | GALT/MALT | Detect pathogens in intestines | Ileum (small intestine) |
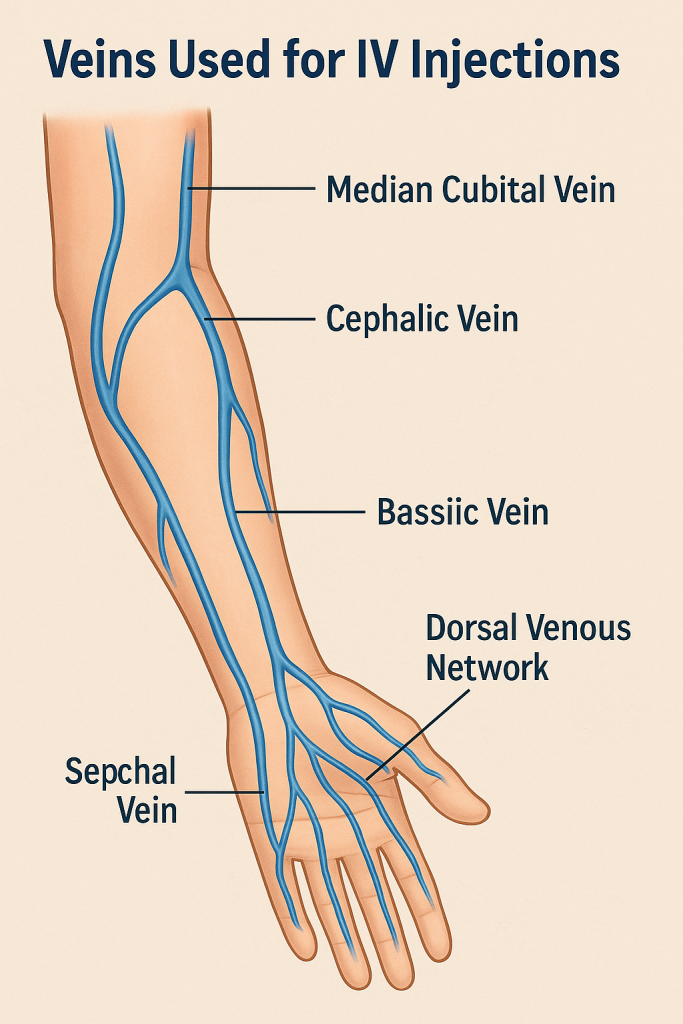
Here’s a comprehensive, clinical, and educational explanation of the veins commonly used for intravenous (IV) injections – ideal for nursing, paramedical, or medical students.
💉 Veins Used for IV Injections – Your Clinical Access Guide

Intravenous (IV) injections involve delivering fluids, medications, or nutrients directly into the bloodstream through a vein. The choice of vein depends on the purpose, urgency, duration, patient’s age, and condition of veins.
📌 1. Veins Commonly Used for IV Injections in Adults
🔹 A. Superficial Veins of the Upper Limb (Most Common)
✅ i. Cephalic Vein
- Location: Lateral (thumb side) of the forearm and upper arm
- Advantages:
- Large and easy to access
- Less likely to roll
- Disadvantage:
- May be more painful or hard to visualize in some patients
✅ ii. Basilic Vein
- Location: Medial (little finger side) of forearm and arm
- Advantages:
- Larger than cephalic vein in many people
- Disadvantages:
- Lies close to artery and nerve – more risk of injury
✅ iii. Median Cubital Vein
- Location: In the antecubital fossa (elbow crease), connects cephalic and basilic veins
- Most commonly used for:
- IV access
- Blood collection
- Advantages:
- Superficial, well-fixed, rarely painful
🎯 Best site for quick access (but not for long-term IV use)
🔹 B. Dorsal Veins of the Hand
- Includes: Dorsal metacarpal veins
- Advantages:
- Good visibility
- Away from large arteries/nerves
- Disadvantages:
- Smaller and more mobile
- May be painful, especially for long-term use
🧠 Used in short-term therapy or when other veins are unavailable
🧒 2. Veins Commonly Used in Children / Infants
👶 A. Scalp Veins (Infants)
- Examples: Temporal, posterior auricular veins
- Used when: Upper limb veins are not visible
- Advantage: Easy access in infants with minimal subcutaneous fat
👣 B. Veins of the Foot
- Examples: Dorsal venous arch, great saphenous vein
- Use with caution due to movement and infection risk
🏥 3. Central Veins for IV (in emergencies or long-term therapy)
These are used when peripheral access is not possible, or for long-term medication (e.g., chemotherapy, TPN).
🟠 i. Internal Jugular Vein
- In the neck, guided by ultrasound
- Good for temporary central lines
🟠 ii. Subclavian Vein
- Below clavicle, good for long-term access
- Risk of pneumothorax
🟠 iii. Femoral Vein
- In the groin; quick access in emergencies
- Higher risk of infection and immobility
🧠 Used for central venous catheterization or CVP monitoring
📋 Summary Table
| Vein Name | Location | Usage | Common For |
|---|---|---|---|
| Median Cubital | Antecubital fossa | Short-term IV, blood draws | Adults |
| Cephalic | Lateral forearm/arm | IV fluids, medications | Adults |
| Basilic | Medial forearm/arm | IV infusions | Adults |
| Dorsal Hand Veins | Back of hand | Short-term meds | Adults, children |
| Scalp Veins | Forehead, temporal | Emergency access | Infants |
| Great Saphenous | Leg/ankle | Peripheral IV | Children, special cases |
| Internal Jugular | Neck | Central line | Emergencies, ICU |
| Subclavian | Below collarbone | Central venous access | Long-term therapy |
| Femoral | Groin | Emergency central access | Critically ill patients |
💡 Tips for Selecting IV Sites
✅ Choose distal to proximal (start low, go higher if needed)
✅ Avoid areas near joints if long-term infusion is needed
✅ Use non-dominant arm if possible
✅ Avoid veins over bruises, scars, infection, or inflammation
⚠️ Clinical Considerations & Complications
| Complication | Description |
|---|---|
| Infiltration | Fluid leaks into surrounding tissue |
| Phlebitis | Inflammation of the vein |
| Thrombosis | Clot formation in the vein |
| Air Embolism | Air enters circulation (central lines) |
| Infection | Entry point or systemic (sepsis) |
🫀🧬 The Circulatory & Lymphatic Systems – Applications & Implications in Nursing
🩸🧠 I. The Circulatory System in Nursing Practice
🔍 Overview
The circulatory (cardiovascular) system includes the heart, blood vessels, and blood. It is responsible for:
- Transporting oxygen, nutrients, hormones, and waste
- Thermoregulation
- Immune support
- Acid–base balance
💉 A. Nursing Applications of Circulatory System Knowledge
| Application | Nursing Actions/Examples |
|---|---|
| 1. Monitoring vital signs | Measure blood pressure, pulse, temperature regularly |
| 2. Managing cardiovascular conditions | Recognize signs of MI, angina, heart failure, arrhythmias |
| 3. Administering IV therapy safely | Identify suitable veins; prevent infiltration or phlebitis |
| 4. Preventing thrombosis | Encourage early mobilization, compression stockings, LMWH use |
| 5. Blood transfusion care | Monitor for reactions, compatibility, documentation |
| 6. Patient education | Teach about low-sodium diets, medications, lifestyle changes |
| 7. Postoperative circulatory assessment | Check capillary refill, pulses, warmth, early signs of embolism |
| 8. CPR and emergency response | Apply BLS/ACLS during cardiac arrest |
🩺 Common Nursing Diagnoses (Circulatory-Related)
- Decreased cardiac output
- Ineffective tissue perfusion (cerebral, renal, peripheral)
- Risk for bleeding
- Fluid volume deficit or excess
- Activity intolerance (cardiac origin)
🧬🛡️ II. The Lymphatic System in Nursing Practice
🔍 Overview
The lymphatic system includes:
- Lymph vessels, lymph nodes, lymph fluid
- Organs like spleen, thymus, tonsils, bone marrow
- Helps in:
- Fluid balance
- Fat absorption
- Immunity
💉 B. Nursing Applications of Lymphatic System Knowledge
| Application | Nursing Actions/Examples |
|---|---|
| 1. Infection detection | Monitor for swollen lymph nodes in neck, axilla, groin |
| 2. Post-mastectomy care | Lymphedema prevention – no BP/IV on affected arm |
| 3. Immunization and vaccine education | Explain how vaccines stimulate lymphocyte memory |
| 4. Monitoring for lymphatic disorders | Recognize signs of lymphoma, leukemia, lymphadenopathy |
| 5. Wound and infection management | Assess local immune response; report signs of delayed healing |
| 6. Nutritional support | Understand fat absorption via lacteals in lymphatics (GI care) |
🦠 Common Nursing Diagnoses (Lymphatic-Related)
- Risk for infection
- Impaired lymphatic drainage
- Risk for fluid imbalance
- Risk for altered immune response
🔗 III. Interrelationship Between the Two Systems
- Blood plasma leaks into tissues → becomes interstitial fluid
- Lymphatic system returns excess fluid to circulatory system
- Lymph nodes filter pathogens before returning fluid to veins
- Both systems are vital in infection control, fluid balance, and immunity
🧠 Clinical Implications for Nurses
| Area | Circulatory System | Lymphatic System |
|---|---|---|
| Assessment | Pulse, BP, edema, cyanosis | Swollen nodes, signs of infection or lymphedema |
| Intervention | Oxygen, IV meds, CPR, fluids | Infection control, lymphedema care |
| Prevention | DVT prophylaxis, cardiac education | Vaccination, hygiene, nutrition |
| Education | Heart health, low-sodium diet, exercise | Self-check for lymph node swelling, immunization |
📚 Summary for Student Nurses
| System | Key Organs | Main Function | Key Nursing Role |
|---|---|---|---|
| Circulatory | Heart, vessels | Transport, perfusion | Monitor BP, pulses, fluids, detect shock |
| Lymphatic | Lymph nodes, spleen | Immunity, drainage | Detect infections, educate, prevent lymphedema |