Anatomy-unit-3-The Digestive system
🌟 Structure of the Alimentary Canal 🌟
The alimentary canal is the complex pathway that helps in the digestion and absorption of nutrients. It extends from the mouth to the anus and consists of several major parts. Let’s explore it in a detailed yet attractive way:
1. Mouth (Oral Cavity) 👄
- Purpose: The gateway to the digestive system! Here, food enters and the journey begins.
- Key Features:
- Teeth: They break food into smaller pieces for easier digestion (mechanical digestion).
- Salivary Glands: These produce saliva that moistens food and contains enzymes like amylase for breaking down starch (chemical digestion).
- Tongue: Helps in mixing food with saliva and pushing it toward the throat for swallowing.
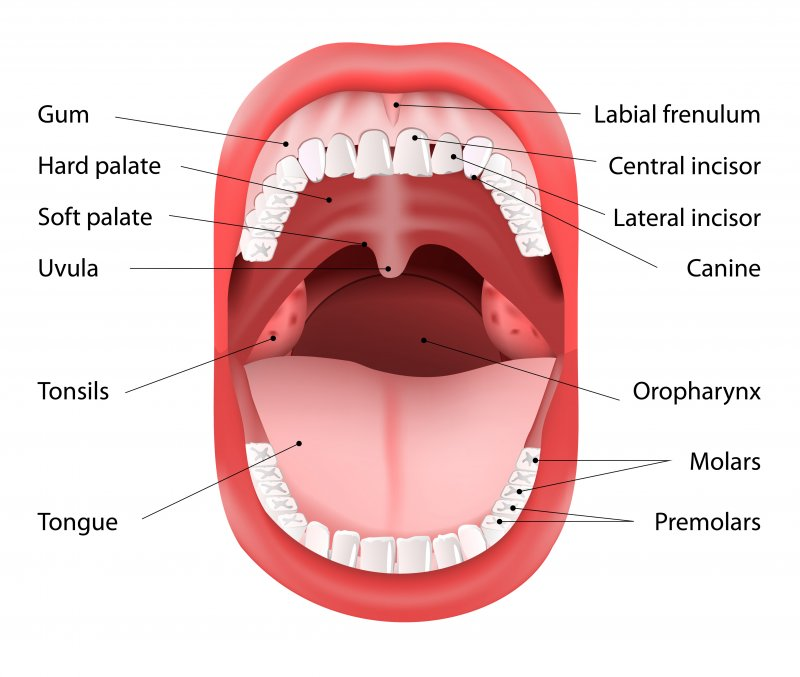
Anatomy of the Mouth (Oral Cavity) 👄
The mouth, or oral cavity, is the entry point for food and plays a crucial role in the first phase of digestion. It’s where mechanical and chemical digestion begins. Let’s break down its detailed anatomy in an engaging way!
1. External Features 🌟
- Lips (Labia):
- Form the boundary of the oral cavity and help keep food in the mouth.
- They also play a role in speech and facial expressions.
- Cheeks:
- Form the lateral walls of the oral cavity.
- Contain the buccinator muscles, which help keep food in the mouth during chewing and assist in the movement of food towards the teeth.
- Palate:
- Hard Palate: The bony front part that forms the roof of the mouth.
- Soft Palate: The muscular part at the back, which rises to close off the nasal passages during swallowing to prevent food from entering the nasal cavity.
2. Internal Features 🦷
- Teeth:
- Function: Teeth break down food mechanically (mastication) into smaller pieces for easier digestion.
- Types of Teeth:
- Incisors: Flat teeth at the front, used for cutting food.
- Canines: Pointed teeth used for tearing food.
- Premolars & Molars: Have broad surfaces for grinding and crushing food.
- Adult Teeth: Typically, an adult has 32 teeth.
- Tongue:
- Function: The tongue is a muscular organ that helps mix food with saliva, form a bolus (chewed food), and push it to the back of the mouth for swallowing.
- Parts:
- Dorsal Surface: The top side, covered with papillae (tiny bumps that house taste buds).
- Taste Buds: Responsible for detecting sweet, sour, salty, and bitter flavors.
- Lingual Frenulum: A fold of tissue under the tongue that limits its movement.
3. Salivary Glands 💦
- Function: Salivary glands secrete saliva, which contains enzymes and mucus to moisten food, start chemical digestion, and help form a bolus for swallowing.
- Types of Salivary Glands:
- Parotid Glands: Located near the upper jaw, in front of the ears. They produce watery saliva rich in amylase (an enzyme that breaks down starch).
- Submandibular Glands: Located below the jaw, these glands produce a mixture of watery and mucus-like saliva.
- Sublingual Glands: Located under the tongue, they secrete mucus-rich saliva, which helps lubricate food.
4. Tonsils 🔰
- Palatine Tonsils: Located at the back of the mouth, these are often the ones removed during a tonsillectomy.
- Lingual Tonsils: Located at the base of the tongue, these help fight infections.
- Pharyngeal Tonsils (Adenoids): Located at the back of the nasal cavity, they are not part of the mouth but play a role in the immune defense of the upper respiratory tract.
5. Pharynx (Throat) 🔄
- Function: The pharynx is a muscular tube that connects the mouth to the esophagus. It acts as a passageway for food and air.
- Parts:
- Oropharynx: The portion of the pharynx located behind the mouth, where food and liquids pass through.
- Nasopharynx: The portion behind the nasal cavity, involved in the passage of air.
- Laryngopharynx: The section closest to the larynx, where food is directed toward the esophagus.
6. Oral Cavity Functions 🏃♂️
- Ingestion: The mouth is the first site where food enters the body.
- Mechanical Digestion: Teeth chew and grind food into smaller pieces.
- Chemical Digestion: Salivary amylase in saliva starts breaking down starches.
- Lubrication: Saliva moistens food to facilitate swallowing and the formation of the bolus.
- Taste: The tongue detects the flavor of food, contributing to the sensory experience of eating.
- Speech: The tongue, lips, and teeth work together to produce sound and speech.
7. The Process of Swallowing (Deglutition) 🔄
- Voluntary Phase: Food is chewed and mixed with saliva to form a bolus, then pushed to the back of the mouth by the tongue.
- Involuntary Phase: Once the bolus reaches the pharynx, the soft palate rises to close the nasal cavity, and the epiglottis closes the trachea to prevent choking. The food enters the esophagus, beginning its journey to the stomach.
The mouth is not just a passage for food – it’s a dynamic organ that plays a vital role in digesting, tasting, and swallowing food. Through mechanical and chemical actions, the mouth begins the complex process of digestion, preparing food for absorption and nutrient processing further down the alimentary canal.
2. Esophagus 🔄
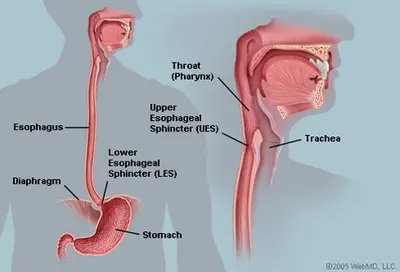
- Purpose: A muscular tube that transports food from the mouth to the stomach.
- Key Features:
- Peristalsis: Wave-like muscle contractions that push food downward.
- Esophageal Sphincter: A valve that prevents food from moving back into the esophagus from the stomach.
Anatomy of the Esophagus 🔄
The esophagus is a muscular tube that serves as a conduit for food and liquids from the mouth to the stomach. It plays a crucial role in the process of swallowing and ensuring the smooth transport of food. Let’s dive into the detailed anatomy of the esophagus:
1. Location and Structure 🗺️
- Position: The esophagus is a muscular tube located behind the trachea (windpipe) and heart, extending from the pharynx (throat) to the stomach.
- Length: It is approximately 25–30 cm (10–12 inches) long in adults.
- Diameter: The diameter of the esophagus is relatively small, about 2–3 cm, but it can stretch to accommodate food.
- Sections: The esophagus can be divided into three parts:
- Cervical Esophagus: The upper portion, located in the neck, just behind the trachea.
- Thoracic Esophagus: The middle section, located within the chest cavity.
- Abdominal Esophagus: The lower part that passes through the diaphragm into the stomach.
2. Layers of the Esophagus 🧱
The wall of the esophagus is made up of several layers that allow for efficient movement of food through peristalsis:
- Mucosa (Innermost Layer):
- Epithelium: This layer is made of stratified squamous epithelium, which provides protection against the abrasion of food particles as they pass through.
- Lamina Propria: A connective tissue layer that houses blood vessels and lymphatic tissue.
- Muscularis Mucosa: A thin layer of smooth muscle that aids in the movement of the mucosal layer.
- Submucosa:
- A layer of connective tissue containing glands that secrete mucus to lubricate the inner surface of the esophagus, aiding in the smooth passage of food.
- This layer also contains blood vessels that supply nutrients to the esophagus.
- Muscularis (Muscle Layer):
- The esophagus is made up of two types of muscle fibers:
- Upper Third: Striated muscle that is under voluntary control, helping initiate the process of swallowing.
- Middle Third: A mix of striated and smooth muscle, allowing for controlled, coordinated movements.
- Lower Third: Smooth muscle that contracts involuntarily to push food down.
- The contractions of this muscular layer help push food through the esophagus in waves (peristalsis).
- The esophagus is made up of two types of muscle fibers:
- Adventitia (Outermost Layer):
- This is a connective tissue layer that helps anchor the esophagus to surrounding structures in the thoracic cavity.
3. Sphincters of the Esophagus 🔒
The esophagus has two important sphincters that help control the flow of food and prevent backflow (reflux):
- Upper Esophageal Sphincter (UES):
- Location: At the junction of the esophagus and pharynx.
- Function: It is made up of striated muscle and is under voluntary control. It opens to allow the passage of food into the esophagus and closes to prevent air from entering the esophagus.
- Action: The UES must relax for food to pass into the esophagus, and then it contracts to prevent food from coming back up.
- Lower Esophageal Sphincter (LES):
- Location: At the junction of the esophagus and the stomach.
- Function: This is a smooth muscle sphincter that prevents the backflow of gastric contents into the esophagus (acid reflux).
- Action: It remains contracted to keep food in the stomach, and relaxes to allow food to pass into the stomach.
4. Peristalsis (Muscle Contractions) 🔄
- Function: The esophagus relies on peristalsis to move food from the mouth to the stomach. Peristalsis is a wave-like motion of muscle contractions that push food through the digestive tract.
- Primary Peristalsis: The initial wave of peristalsis that occurs after swallowing and moves food from the mouth to the stomach.
- Secondary Peristalsis: If food fails to be moved completely through the esophagus, additional peristaltic waves help to push it down.
5. Nerve Supply and Control 🧠
- The vagus nerve (part of the parasympathetic nervous system) controls the peristalsis and muscle contractions of the esophagus.
- The somatic nervous system controls the voluntary aspect of swallowing, particularly the initiation of the swallowing process.
- The enteric nervous system (the “second brain” in the gut) helps coordinate smooth muscle activity.
6. Swallowing Process (Deglutition) 🍽️
- Voluntary Phase: The tongue pushes the food to the back of the mouth, triggering the swallowing reflex.
- Involuntary Phase: The soft palate elevates to prevent food from entering the nasal cavity. The upper esophageal sphincter relaxes to allow food to enter the esophagus. Peristalsis begins as food is pushed down the esophagus.
- Final Phase: The lower esophageal sphincter relaxes, allowing the food bolus to enter the stomach.
7. Common Disorders of the Esophagus ⚠️
- Gastroesophageal Reflux Disease (GERD): A condition where the lower esophageal sphincter does not close properly, allowing stomach acid to flow back into the esophagus, causing heartburn.
- Achalasia: A disorder where the esophagus has difficulty moving food into the stomach due to a failure of peristalsis and relaxation of the lower esophageal sphincter.
- Esophageal Cancer: Malignant growth that can occur in the esophagus, often associated with risk factors like smoking and alcohol use.
The esophagus is a key organ in the digestive process, acting as the conduit that carries food from the mouth to the stomach. With its specialized muscular layers, sphincters, and peristaltic motions, the esophagus ensures the smooth and controlled movement of food, preventing backflow and ensuring proper digestion.
3. Stomach 🍲
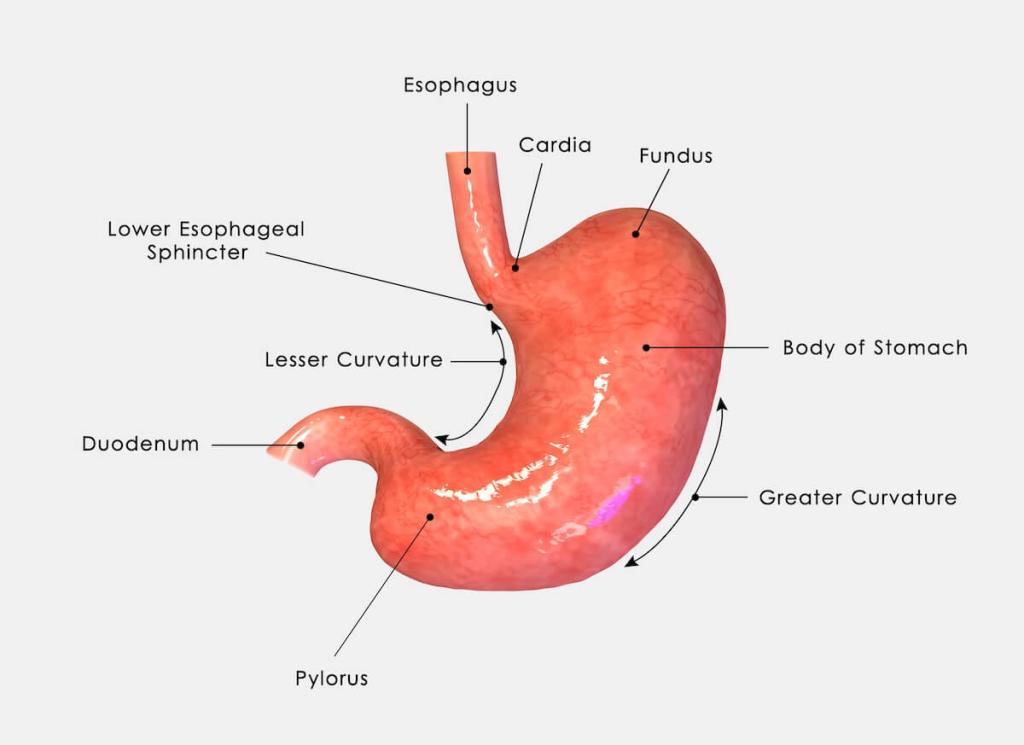
- Purpose: The food blender! It breaks down food further using gastric juices.
- Key Features:
- Gastric Juices: Contain hydrochloric acid and digestive enzymes (like pepsin) to break down proteins.
- Churning: The stomach muscles mix food with gastric juices, turning it into a semi-liquid called chyme.
- Pyloric Sphincter: Controls the release of chyme into the small intestine.
Anatomy of the Stomach 🍲
The stomach is a muscular organ that plays a crucial role in the digestion of food. It’s where food is mixed with gastric juices to break it down into a more digestible form before it moves to the small intestine. Let’s explore the detailed anatomy of the stomach!
1. Location and Structure 📍
- Position: The stomach lies in the upper left part of the abdomen, just beneath the diaphragm and to the left of the liver. It is positioned between the esophagus and the small intestine (duodenum).
- Size: The stomach can expand to hold approximately 1-1.5 liters of food, though its size can vary depending on the individual and the amount of food consumed.
- Shape: The stomach is J-shaped and can be divided into several regions that each perform specific functions in digestion.
2. Parts of the Stomach 🧩
The stomach can be divided into four main parts, each with specific roles in digestion:
- Cardia:
- Location: This is the upper portion of the stomach where the esophagus joins the stomach.
- Function: The cardiac sphincter (or lower esophageal sphincter) controls the entry of food from the esophagus into the stomach and prevents stomach acid from refluxing back into the esophagus.
- Fundus:
- Location: The rounded, upper part of the stomach, situated above the body.
- Function: The fundus temporarily stores food that is swallowed and contains gastric glands that secrete gastric juices. It also acts as a gastric reservoir.
- Body:
- Location: The central portion of the stomach, located between the fundus and the pylorus.
- Function: This is where the majority of gastric digestion occurs. The stomach walls here churn food and mix it with gastric juices to form a semi-liquid substance called chyme.
- Pylorus:
- Location: The lower portion of the stomach that connects to the duodenum (the first part of the small intestine).
- Function: The pyloric sphincter controls the movement of chyme from the stomach into the small intestine and prevents backflow. It also regulates the release of chyme in small amounts for proper digestion in the small intestine.
3. Layers of the Stomach Wall 🧱
The stomach wall is composed of four main layers, each contributing to digestion and the stomach’s protective mechanisms:
- Mucosa (Innermost Layer):
- Structure: The mucosa is lined with columnar epithelial cells, which secrete mucus to protect the stomach lining from its own acidic contents.
- Function: It contains gastric glands that secrete gastric juice, including hydrochloric acid (HCl) and digestive enzymes like pepsin, which begin breaking down proteins.
- Submucosa:
- Structure: This layer consists of connective tissue that contains blood vessels to supply the stomach with nutrients and oxygen.
- Function: It also houses lymphatic vessels that help protect the stomach from infections and allow for immune response.
- Muscularis Externa:
- Structure: The muscular layer has three sub-layers of smooth muscle:
- Longitudinal muscle: The outer layer, which shortens the stomach.
- Circular muscle: The middle layer, which constricts and helps churn food.
- Oblique muscle: The innermost layer, which helps in mixing food and creating strong churning motions (important for the mechanical breakdown of food).
- Function: The coordinated contraction of these muscles helps churn the food and mix it with gastric juices to form chyme.
- Structure: The muscular layer has three sub-layers of smooth muscle:
- Serosa (Outer Layer):
- Structure: The outermost layer is a smooth membrane that is part of the peritoneum (a membrane that surrounds the abdominal organs).
- Function: It protects the stomach and helps reduce friction between the stomach and surrounding organs.
4. Gastric Juices and Secretions 💧
The stomach secretes a variety of substances that aid in digestion:
- Hydrochloric Acid (HCl):
- Purpose: Acid helps break down food, kills bacteria, and provides an acidic environment for the enzyme pepsin to work.
- Pepsinogen:
- Purpose: The inactive precursor of pepsin, an enzyme that begins the digestion of proteins. It is activated by the acidic environment of the stomach.
- Mucus:
- Purpose: Secreted by goblet cells to form a protective layer over the stomach lining, preventing the stomach from digesting itself with its own acid.
- Intrinsic Factor:
- Purpose: A glycoprotein that is essential for the absorption of vitamin B12 in the small intestine.
5. Role in Digestion 🏃♂️
The stomach plays a central role in both mechanical and chemical digestion:
- Mechanical Digestion: The muscles of the stomach wall churn and mix food with gastric juices to form chyme. This helps break down food into smaller, more manageable pieces.
- Chemical Digestion: Gastric acid and pepsin begin the breakdown of proteins into smaller peptides. The acidic environment also helps in the denaturation of proteins, making them easier to digest.
- Storage: The stomach serves as a temporary storage chamber, holding food for several hours while it is digested.
- Controlled Release: The pyloric sphincter regulates the release of chyme into the small intestine in small, manageable amounts for further digestion and absorption.
6. Regulation of Gastric Secretion 🧠
Gastric secretion is regulated by several factors:
- Cephalic Phase: The sight, smell, or thought of food triggers the brain to send signals via the vagus nerve to stimulate gastric juices production.
- Gastric Phase: When food enters the stomach, stretch receptors are activated, triggering the release of more gastric acid and pepsinogen to aid digestion.
- Intestinal Phase: Once chyme enters the small intestine, it signals the stomach to reduce gastric secretion and slow down the release of more food.
7. Common Disorders of the Stomach ⚠️
- Gastritis: Inflammation of the stomach lining, often caused by infections (like H. pylori), alcohol use, or long-term use of nonsteroidal anti-inflammatory drugs (NSAIDs).
- Peptic Ulcers: Open sores or lesions in the stomach lining, often caused by an imbalance between the digestive acids and protective mucus.
- Gastroesophageal Reflux Disease (GERD): When stomach acid flows backward into the esophagus, causing irritation and discomfort.
- Stomach Cancer: A form of cancer that develops in the lining of the stomach.
The stomach is a muscular, flexible organ that is essential in the early stages of digestion. It breaks down food chemically and mechanically, turning it into a semi-liquid substance (chyme) that can be further processed in the small intestine. Through the secretion of gastric juices, coordinated muscle contractions, and the controlled release of food, the stomach prepares food for nutrient absorption and plays a vital role in overall digestion.
4. Small Intestine 🧑⚕️💧
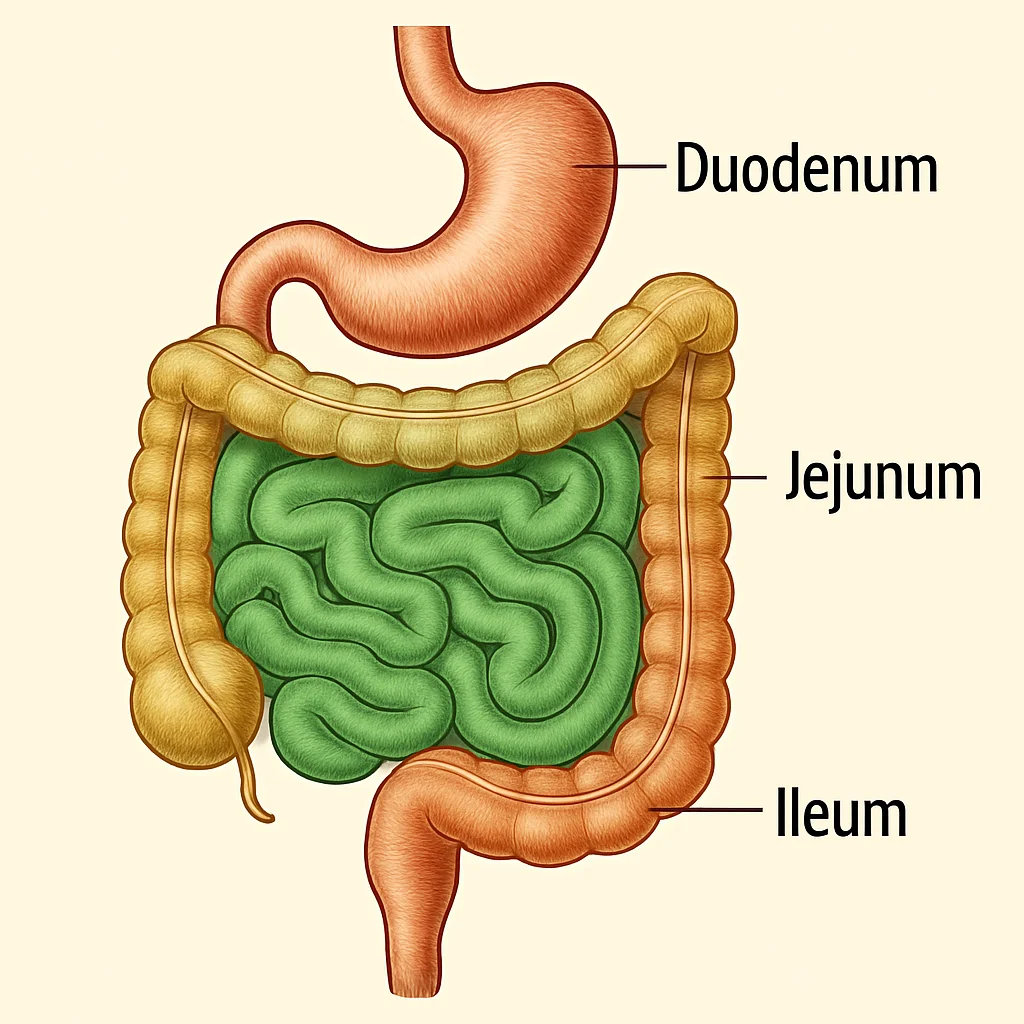
- Purpose: The primary site for digestion and absorption of nutrients.
- Key Features:
- Duodenum: The first part of the small intestine where bile and pancreatic enzymes further break down food.
- Jejunum: Absorption of nutrients begins here.
- Ileum: The final part where absorption of nutrients, including vitamins and minerals, takes place.
- Villi and Microvilli: Tiny finger-like projections that increase the surface area for nutrient absorption.
Anatomy of the Small Intestine 🥗
The small intestine is a vital part of the digestive system where the majority of digestion and nutrient absorption occurs. It is a long, coiled tube that follows the stomach and leads to the large intestine. Let’s take an in-depth look at its structure and functions!
1. Overview and Structure 🌍
- Length: The small intestine is approximately 6 meters (20 feet) long in adults, making it the longest part of the digestive tract.
- Diameter: It has a relatively small diameter (about 2.5-4 cm), which increases significantly due to its internal folds.
- Location: The small intestine is located in the abdomen, positioned between the stomach and the large intestine. It is coiled and occupies a central position in the abdominal cavity.
2. Parts of the Small Intestine 🧩
The small intestine is divided into three parts, each with specific functions related to digestion and absorption:
- Duodenum (First Part):
- Length: Approximately 25-30 cm (10-12 inches).
- Function: This is the shortest and widest section. The duodenum is where most of the chemical digestion takes place. It receives bile from the liver and gallbladder, which emulsifies fats, and pancreatic juices, which contain enzymes to break down carbohydrates, proteins, and fats.
- Digestive Secretions:
- Bile: Produced by the liver, stored in the gallbladder, and released into the duodenum to help digest fats.
- Pancreatic Enzymes: Released by the pancreas, these enzymes help in the breakdown of proteins (protease), fats (lipase), and carbohydrates (amylase).
- Hormones: It secretes hormones like secretin and cholecystokinin (CCK), which regulate the release of bile and pancreatic juices.
- Jejunum (Middle Part):
- Length: Approximately 2.5 meters (8 feet).
- Function: This is the primary site for nutrient absorption. The walls of the jejunum are lined with villi and microvilli that increase the surface area for absorption.
- Structure: It has a rich blood supply to help absorb the nutrients (like carbohydrates, proteins, lipids, vitamins, and minerals) into the bloodstream.
- Ileum (Last Part):
- Length: Approximately 3-4 meters (10-13 feet).
- Function: The ileum absorbs nutrients that were not absorbed in the jejunum. It also absorbs vitamin B12 and bile salts, which are needed to recycle bile.
- Structure: Similar to the jejunum, the ileum also contains villi and microvilli. At its end is the ileocecal valve, which controls the flow of material from the ileum to the large intestine.
3. Layers of the Small Intestinal Wall 🧱
The wall of the small intestine is composed of four layers, which help facilitate digestion and absorption:
- Mucosa (Innermost Layer):
- Structure: Lined with simple columnar epithelial cells and specialized cells that secrete digestive enzymes, mucus, and hormones.
- Villi and Microvilli: The mucosa is covered in tiny finger-like projections called villi, which are lined with even smaller projections known as microvilli. These structures greatly increase the surface area for nutrient absorption.
- Crypts of Lieberkühn: Glands located between the villi that secrete intestinal juices and enzymes for digestion.
- Submucosa:
- Structure: A layer of connective tissue containing blood vessels and lymphatic vessels (lacteals).
- Function: It supports the mucosa and helps transport absorbed nutrients. The lacteals in the submucosa are especially important for the absorption of lipids (fats).
- Muscularis Externa:
- Structure: Composed of two smooth muscle layers:
- Circular Muscle Layer: Constricts the intestine, aiding in the mixing of contents and propulsion.
- Longitudinal Muscle Layer: Shortens the intestine and helps move food forward through peristalsis (wave-like contractions).
- Function: This layer facilitates the mixing of food with digestive enzymes and moves the digested food through the small intestine.
- Structure: Composed of two smooth muscle layers:
- Serosa (Outer Layer):
- Structure: The outermost layer, which is part of the peritoneum, a membrane that lines the abdominal cavity and covers the organs within it.
- Function: Provides structural support and protection for the intestine.
4. Digestive Process in the Small Intestine 🏃♂️
The small intestine plays a central role in digestion and absorption:
- Chemical Digestion:
- Pancreatic Enzymes: These break down carbohydrates, proteins, and fats into smaller molecules.
- Bile: Emulsifies fats, breaking them down into smaller droplets for easier digestion by lipase.
- Absorption:
- The villi and microvilli are crucial for absorbing nutrients from digested food. Nutrients like glucose, amino acids, fatty acids, vitamins, and minerals pass through the epithelial cells of the villi into the bloodstream or lymphatic system.
- Water: The small intestine also absorbs a significant amount of water, which is needed for digestion and to maintain body fluid balance.
5. Villi and Microvilli: The Absorptive Surface 🏞️
- Villi: These are tiny, finger-like projections in the mucosa that contain blood vessels and lymphatic vessels. The blood vessels absorb water-soluble nutrients, while the lymphatic vessels (called lacteals) absorb fat-soluble nutrients.
- Microvilli: The villi are lined with even smaller hair-like structures called microvilli, which form the brush border. These microvilli contain enzymes that aid in the final stages of nutrient breakdown (like lactase for breaking down lactose).
6. Hormonal Regulation 🧠
Several hormones are involved in regulating the digestive process in the small intestine:
- Secretin: Stimulates the pancreas to release bicarbonate, which neutralizes the acidic chyme coming from the stomach.
- Cholecystokinin (CCK): Stimulates the release of bile from the gallbladder and pancreatic enzymes for fat and protein digestion.
- Gastric Inhibitory Peptide (GIP): Inhibits gastric motility and secretion, slowing down the rate of food moving into the small intestine.
7. Common Disorders of the Small Intestine ⚠️
- Celiac Disease: An autoimmune disorder where the ingestion of gluten damages the small intestine’s lining, impairing nutrient absorption.
- Crohn’s Disease: A chronic inflammatory bowel disease that affects the lining of the digestive tract, particularly the small intestine, causing pain, diarrhea, and malnutrition.
- Irritable Bowel Syndrome (IBS): A functional gastrointestinal disorder that can cause cramping, bloating, and changes in bowel movements, including diarrhea and constipation.
- Intestinal Obstruction: A blockage in the small intestine that prevents food, fluids, and gas from passing through. This can be caused by adhesions, tumors, or hernias.
The small intestine is the primary site for nutrient digestion and absorption. Through its specialized structure, including villi, microvilli, and digestive enzymes, it breaks down food into its simplest forms and absorbs the necessary nutrients for the body. The small intestine’s role is critical in maintaining overall health and providing the nutrients needed for the body’s functions.
5. Liver 🍏
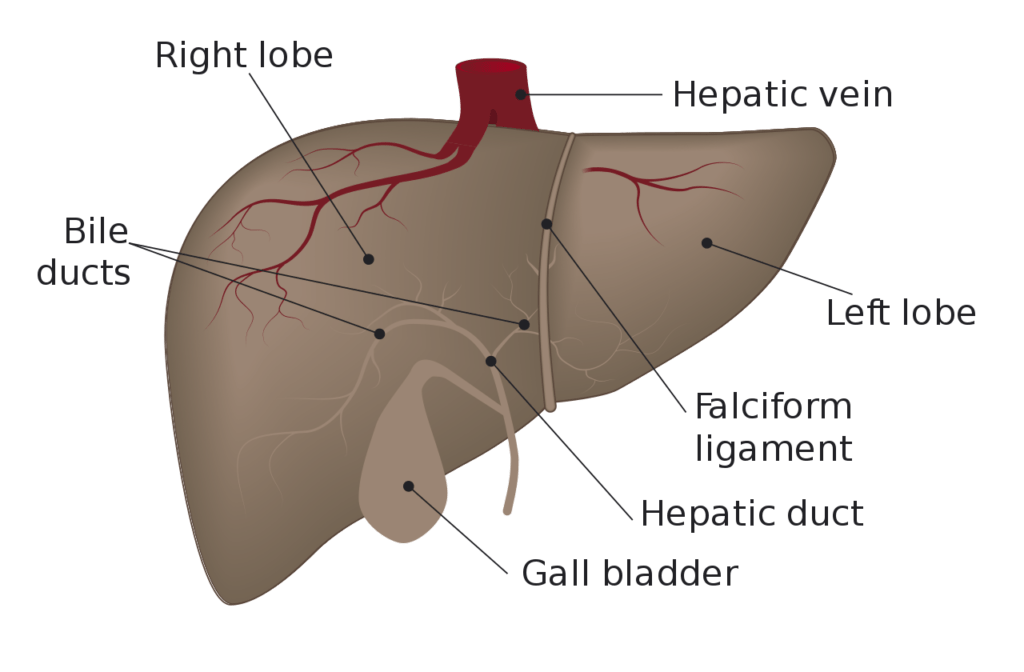
- Purpose: A powerhouse for metabolism and detoxification!
- Key Features:
- Bile Production: The liver produces bile, stored in the gallbladder, which helps break down fats.
- Detoxification: The liver filters out toxins from the blood.
Anatomy of the Liver 🍏
The liver is one of the most important organs in the body, playing a crucial role in digestion, metabolism, and detoxification. It is the largest solid organ and gland in the human body. Let’s dive into its detailed anatomy and its various functions.
1. Location and Structure 📍
- Position: The liver is located in the upper right quadrant of the abdomen, just beneath the diaphragm and above the stomach. It is tucked in on the right side of the body and extends toward the left.
- Size: The liver weighs approximately 1.4-1.6 kg (3-3.5 pounds) in adults and has a reddish-brown color.
- Shape: The liver is triangular in shape, with a smooth and lobulated surface.
2. Lobes of the Liver 🧩
The liver is divided into two main lobes:
- Right Lobe: The larger of the two, covering about 75% of the liver’s mass.
- Left Lobe: The smaller lobe located to the left of the right lobe.
- Caudate Lobe: Located on the back of the liver, near the inferior vena cava, this is a smaller lobe.
- Quadrate Lobe: Positioned near the gallbladder and the lower surface of the liver.
3. Liver Lobules 🧬
The liver is made up of thousands of tiny functional units called lobules:
- Structure: Each lobule is made up of hepatocytes (liver cells) arranged in a hexagonal pattern around a central vein.
- Blood Flow: Blood flows through the lobule from the portal triad (which consists of the portal vein, hepatic artery, and bile duct), and moves toward the central vein, where it then drains into the hepatic veins and finally enters the inferior vena cava.
- Hepatocytes: These are the main functional cells of the liver and are responsible for carrying out many of the liver’s functions, such as metabolism, detoxification, and protein synthesis.
4. Blood Supply of the Liver 💉
The liver has a unique dual blood supply:
- Hepatic Artery: Carries oxygenated blood from the heart to the liver.
- Portal Vein: Carries deoxygenated blood from the digestive organs (stomach, intestines, spleen, and pancreas) that contains nutrients and toxins to be processed by the liver.
- Blood from both the hepatic artery and portal vein flows into the sinusoids (specialized blood vessels) within the liver lobules, where exchange with hepatocytes takes place.
5. Bile Production and Flow 🧃
- Bile: The liver produces bile, a digestive fluid that is essential for fat digestion. It is made up of water, bile acids, cholesterol, and waste products like bilirubin (a byproduct of the breakdown of red blood cells).
- Bile Secretion: Bile is secreted into the bile canaliculi, small ducts within the liver lobules, and flows toward the hepatic duct.
- Storage: From the hepatic duct, bile flows into the gallbladder, where it is concentrated and stored.
- Bile Release: When food enters the small intestine, the gallbladder contracts and releases bile into the duodenum through the common bile duct to aid in fat digestion.
6. Functions of the Liver ⚙️
The liver is involved in a vast range of essential functions in the body:
- Metabolism:
- Carbohydrate Metabolism: Converts glucose to glycogen for storage (glycogenesis) and converts glycogen back to glucose when needed (glycogenolysis).
- Lipid Metabolism: Synthesizes cholesterol and lipoproteins and is involved in the breakdown of fats.
- Protein Metabolism: The liver synthesizes important proteins like albumin, clotting factors, and enzymes needed for digestion. It also breaks down amino acids.
- Detoxification:
- The liver filters toxins, drugs, and harmful substances from the blood and converts them into less toxic compounds, which are then excreted through bile or urine.
- Storage:
- The liver stores vitamins (A, D, B12), minerals (iron, copper), and glycogen for energy.
- Bile Production:
- As mentioned, the liver produces bile, which helps in the emulsification and absorption of fats in the small intestine.
- Immune Function:
- The liver plays a role in the immune system by producing acute phase proteins that help fight infections. It also filters bacteria and pathogens from the blood.
- Blood Clotting:
- The liver synthesizes blood-clotting factors (such as fibrinogen and prothrombin), which are essential for the blood clotting process.
7. Hepatic Portal System 🔄
The liver plays a key role in processing nutrients absorbed from the digestive tract:
- Portal Vein: After food is digested in the stomach and intestines, the nutrients are absorbed into the blood and carried to the liver via the portal vein.
- Processing: The liver processes nutrients (like glucose, amino acids, and fats) and detoxifies harmful substances.
- Metabolism: The liver regulates blood sugar levels by converting glucose to glycogen and vice versa, as well as managing lipid and protein metabolism.
8. Gallbladder 🏖️
- Location: The gallbladder is a small, pear-shaped organ located underneath the liver.
- Function: It stores and concentrates bile produced by the liver until it is needed for digestion.
- Bile Release: When fat is detected in the duodenum, the gallbladder releases bile into the small intestine to help break down fats.
9. Common Disorders of the Liver ⚠️
- Hepatitis: Inflammation of the liver, often caused by viral infections (such as hepatitis B and C) or alcohol use.
- Cirrhosis: A condition where the liver becomes severely scarred, usually due to long-term liver damage from alcohol abuse or chronic viral infections.
- Fatty Liver Disease: The accumulation of fat in the liver cells, often related to obesity, diabetes, and alcohol consumption.
- Liver Cancer: Cancer that develops in the liver, often as a result of cirrhosis or chronic hepatitis infection.
- Liver Failure: A life-threatening condition where the liver loses its ability to perform its essential functions.
The liver is a highly functional organ that plays a central role in digestion, metabolism, detoxification, and immune defense. Its ability to process nutrients from the digestive tract, produce bile for fat digestion, and regulate various metabolic processes is vital to the body’s overall health and homeostasis.
6. Pancreas 🥄
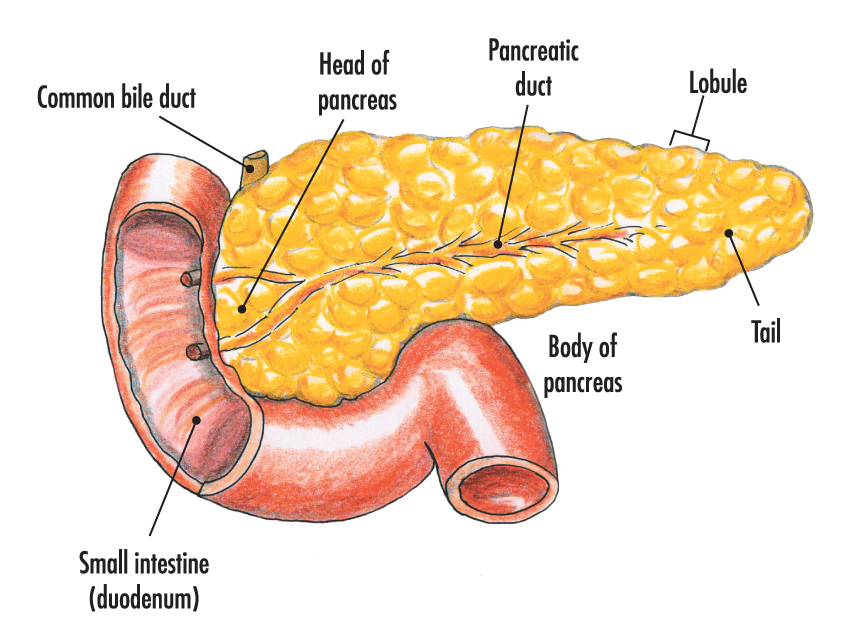
- Purpose: A digestive aid and hormone producer.
- Key Features:
- Digestive Enzymes: The pancreas produces enzymes like amylase, lipase, and proteases to break down carbohydrates, fats, and proteins.
- Insulin Production: Regulates blood sugar levels by producing insulin.
Anatomy of the Pancreas 🍯
The pancreas is a vital organ in both the digestive and endocrine systems. It plays a crucial role in digestion by producing digestive enzymes and hormones that regulate blood sugar levels. Let’s take a detailed look at its anatomy and functions!
1. Location and Structure 📍
- Position: The pancreas is located in the upper abdomen, behind the stomach and near the duodenum (the first part of the small intestine). It is positioned across the back of the abdominal cavity, extending from the duodenum on the right side to the spleen on the left.
- Size: The pancreas is about 6-8 inches (15-20 cm) long and weighs approximately 70 grams in adults.
- Shape: The pancreas has an elongated, triangular shape with a head, body, and tail:
- Head: The broader end, located near the duodenum.
- Body: The central portion of the pancreas.
- Tail: The narrower end, near the spleen.
2. Exocrine and Endocrine Functions ⚙️
The pancreas has both exocrine and endocrine functions, each responsible for different roles in digestion and metabolic regulation.
Exocrine Function (Digestive Role) 🥄
- Exocrine Glands: The majority of the pancreas is composed of exocrine tissue. This tissue produces and secretes digestive enzymes into the duodenum through a duct system.
- Digestive Enzymes:
- Amylase: Breaks down carbohydrates (starch) into simple sugars like glucose.
- Lipase: Breaks down fats into fatty acids and glycerol.
- Proteases (e.g., Trypsin, Chymotrypsin): Break down proteins into smaller peptides and amino acids.
- Bicarbonate: The pancreas also secretes bicarbonate ions, which neutralize the acidic chyme coming from the stomach into the duodenum, providing an optimal environment for the digestive enzymes to function.
- Pancreatic Duct System: Digestive enzymes and bicarbonate are transported through the pancreatic duct, which joins with the common bile duct from the liver and gallbladder. Together, they empty into the duodenum via the ampulla of Vater (also known as the hepatopancreatic ampulla), which is regulated by the sphincter of Oddi.
Endocrine Function (Hormonal Role) 🧠
- Endocrine Glands (Islets of Langerhans): The Islets of Langerhans are clusters of cells in the pancreas that secrete hormones directly into the bloodstream. These hormones play a key role in regulating blood glucose levels.
- Key Hormones:
- Insulin: Produced by beta cells, insulin helps lower blood sugar levels by promoting the uptake of glucose into cells for energy production or storage as glycogen in the liver and muscles.
- Glucagon: Produced by alpha cells, glucagon raises blood sugar levels by stimulating the liver to release stored glycogen (glycogenolysis) and produce new glucose from amino acids (gluconeogenesis).
- Somatostatin: Produced by delta cells, somatostatin inhibits the release of both insulin and glucagon, helping to regulate the balance of glucose.
- Pancreatic Polypeptide: Produced by PP cells, this hormone regulates the secretion of digestive enzymes and affects appetite and nutrient absorption.
3. Blood Supply 💉
- The pancreas has a rich blood supply that is primarily derived from the celiac trunk and the superior mesenteric artery.
- Pancreatic Arteries: Blood is supplied to the pancreas via branches of these arteries, including the splenic artery (supplying the tail and body) and the pancreaticoduodenal arteries (supplying the head and duodenum).
- Venous Drainage: Blood from the pancreas is drained into the portal vein, which directs it to the liver for processing.
4. Ductal System 🧪
The pancreatic duct system is responsible for transporting digestive enzymes and bicarbonate to the duodenum:
- Main Pancreatic Duct: This duct runs the length of the pancreas, carrying digestive enzymes from the exocrine cells to the duodenum.
- Accessory Pancreatic Duct: In some people, there is an additional duct that empties directly into the duodenum, bypassing the main duct.
- Sphincter of Oddi: The sphincter regulates the flow of digestive enzymes and bile into the duodenum. It opens when food enters the duodenum and closes to prevent reflux.
5. Functions of the Pancreas 🧠
The pancreas has two main functions, as both an exocrine and an endocrine gland:
- Exocrine Function:
- Secretes digestive enzymes (amylase, lipase, and proteases) into the duodenum to help break down food.
- Releases bicarbonate to neutralize stomach acid, creating the right pH for enzymatic digestion.
- Endocrine Function:
- Regulates blood glucose levels through the secretion of insulin (lowers blood sugar) and glucagon (raises blood sugar).
- Helps maintain overall metabolic homeostasis by balancing glucose storage, production, and uptake.
6. Common Disorders of the Pancreas ⚠️
- Pancreatitis: Inflammation of the pancreas, often caused by gallstones, alcohol use, or certain medications. It can lead to pain, digestive problems, and in severe cases, organ failure.
- Diabetes Mellitus: A condition where the pancreas does not produce enough insulin or the body does not respond to insulin effectively. This leads to high blood sugar levels and a range of complications.
- Pancreatic Cancer: A form of cancer that begins in the pancreas. It is often diagnosed late because symptoms may not appear until the cancer has spread.
- Cystic Fibrosis: A genetic disorder that affects the pancreas and other organs, leading to thick mucus production, which can obstruct the pancreatic ducts and cause digestive issues.
- Pancreatic Insufficiency: A condition where the pancreas does not produce enough digestive enzymes, leading to malabsorption and nutritional deficiencies.
The pancreas is a dual-function organ that plays a vital role in both digestion and the regulation of blood glucose. As an exocrine gland, it produces digestive enzymes and bicarbonate, which are essential for breaking down food and neutralizing stomach acid. As an endocrine gland, it produces hormones like insulin and glucagon that regulate blood sugar levels, ensuring metabolic balance.
7. Large Intestine (Colon) 🚶♂️
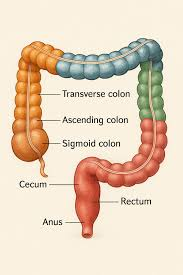
- Purpose: Absorbs water and salts from the remaining indigestible food matter.
- Key Features:
- Cecum: Where the small intestine joins the large intestine.
- Ascending, Transverse, and Descending Colon: Sections where water and electrolytes are absorbed, and the remaining matter becomes more solid.
- Rectum & Anus: Stores and expels waste from the body.
Anatomy of the Large Intestine 🚶♂️
The large intestine is the final part of the digestive system, playing a key role in absorbing water and electrolytes from the remaining indigestible food matter and forming solid waste (feces) for elimination. It is wider and shorter than the small intestine but just as important in the digestive process. Let’s explore the detailed anatomy of the large intestine.
1. Location and Structure 📍
- Position: The large intestine is located in the abdominal cavity. It frames the small intestine, running along the perimeter of the abdomen. It starts at the ileocecal valve (the junction between the small and large intestines) and ends at the anus.
- Size: The large intestine is about 1.5 meters (5 feet) long but is wider (about 6 cm in diameter) than the small intestine.
- Shape: The large intestine has a C-shape, forming an arc that encircles the small intestine. It is divided into several distinct regions.
2. Parts of the Large Intestine 🧩
The large intestine is made up of several sections, each with specific functions:
Cecum 🍂
- Location: The cecum is the first part of the large intestine, located at the junction of the small and large intestines, below the ileocecal valve.
- Structure: The cecum is a pouch-like structure that serves as a storage area for chyme (partially digested food) from the small intestine.
- Function: It absorbs fluids and salts that remain after the digestion of food in the small intestine. The cecum also houses the appendix.
Appendix 🍏
- Location: The appendix is a small, finger-like projection attached to the cecum.
- Structure: It is about 9 cm long in adults and contains lymphoid tissue, which plays a role in immune function.
- Function: While the appendix has a debated role in digestion, it is thought to function in the immune system by harboring beneficial bacteria. Infections or blockages can lead to appendicitis (inflammation of the appendix), often requiring surgical removal.
Ascending Colon 🔼
- Location: The ascending colon starts at the cecum and moves upward along the right side of the abdomen.
- Function: It absorbs water and salts from the remaining chyme, concentrating it into a more solid form. It also houses bacteria that help break down remaining nutrients and produce gases.
- Structure: The ascending colon moves food material upward and is connected to the next segment by a right-angle bend at the hepatic flexure (near the liver).
Transverse Colon ➡️
- Location: The transverse colon crosses the abdomen horizontally from the hepatic flexure to the splenic flexure (near the spleen).
- Function: It continues absorbing water, electrolytes, and some vitamins produced by gut bacteria. It also acts as a temporary storage site for waste material.
- Structure: The transverse colon is longer and more mobile than the ascending or descending portions, suspended by the mesocolon.
Descending Colon ⬇️
- Location: The descending colon runs down the left side of the abdomen, from the splenic flexure to the sigmoid colon.
- Function: It continues the absorption of water and electrolytes, with further compaction of fecal matter. It prepares waste for excretion.
- Structure: The descending colon is somewhat fixed in position by the mesocolon, with a more rigid structure compared to the ascending and transverse colon.
Sigmoid Colon ⛔
- Location: The sigmoid colon is the S-shaped portion of the large intestine, located in the lower abdomen, just before the rectum.
- Function: It stores the formed stool before it is eliminated from the body. The sigmoid colon also plays a role in absorbing any remaining water and electrolytes.
- Structure: The sigmoid colon leads into the rectum and is more flexible, allowing for storage and movement of waste.
Rectum and Anus 🚽
- Rectum: The rectum is the final section of the large intestine, located just before the anus. It stores feces until they are ready to be expelled.
- Function: The rectum has stretch receptors that signal the brain when it is full, initiating the urge to defecate.
- Anus: The anus is the opening at the end of the digestive tract through which feces are expelled. It contains two sphincters:
- Internal Anal Sphincter: This is involuntary and automatically contracts to prevent premature release of feces.
- External Anal Sphincter: This is voluntary and allows control over the release of feces during defecation.
3. Layers of the Large Intestinal Wall 🧱
The wall of the large intestine is made up of the same four basic layers as the rest of the gastrointestinal tract:
- Mucosa (Innermost Layer):
- Structure: The mucosa is lined with simple columnar epithelial cells that secrete mucus to lubricate the passage of feces and protect the lining from mechanical stress.
- Goblet Cells: These specialized cells secrete mucus that lubricates and protects the intestine from digestive enzymes and friction from the waste material.
- Submucosa:
- Structure: This layer contains blood vessels and lymphatic vessels that help absorb water and nutrients.
- Function: It provides structural support and supplies blood and nutrients to the tissue of the large intestine.
- Muscularis Externa:
- Structure: The muscularis externa consists of two layers of smooth muscle:
- Circular Muscle Layer: This helps in constricting the lumen of the colon.
- Longitudinal Muscle Layer: The teniae coli are three bands of longitudinal muscle that run along the length of the large intestine and help contract the intestine to move fecal matter.
- Structure: The muscularis externa consists of two layers of smooth muscle:
- Serosa (Outer Layer):
- Structure: This is the outermost layer of the large intestine, part of the peritoneum. It helps reduce friction and protects the intestines.
4. Functions of the Large Intestine ⚙️
The large intestine has several essential functions, primarily related to the absorption of water, electrolytes, and formation of feces:
- Water Absorption: The large intestine absorbs most of the water that remains after digestion in the small intestine, turning the liquid chyme into more solid stool.
- Electrolyte Absorption: It absorbs important electrolytes, such as sodium and potassium, to maintain fluid balance and prevent dehydration.
- Fermentation of Undigested Food: The large intestine houses a large number of bacteria that help ferment certain undigested carbohydrates, producing gases and some vitamins (like vitamin K and biotin).
- Storage and Elimination: The large intestine stores fecal material until it is ready to be excreted. The rectum signals the brain when it is full, prompting the urge to defecate.
- Bacterial Flora: The large intestine is home to trillions of bacteria, known as the gut microbiota, which assist in the fermentation of undigested carbohydrates, production of certain vitamins, and protection against harmful microorganisms.
5. Common Disorders of the Large Intestine ⚠️
- Irritable Bowel Syndrome (IBS): A functional gastrointestinal disorder characterized by abdominal pain, bloating, and changes in bowel habits (diarrhea, constipation, or both).
- Diverticulitis: Inflammation or infection of small pouches (diverticula) that can form in the walls of the large intestine, often leading to pain, fever, and changes in bowel movements.
- Colorectal Cancer: Cancer that affects the colon or rectum, typically starting as benign growths (polyps) that can become malignant over time.
- Ulcerative Colitis: A type of inflammatory bowel disease (IBD) that causes long-term inflammation and sores in the colon and rectum.
- Crohn’s Disease: Another form of IBD, it can affect any part of the digestive tract, but it most commonly affects the ileum and the ascending colon.
The large intestine plays a critical role in absorbing water and electrolytes, forming feces, and maintaining fluid balance. It also hosts a complex microbiome that aids in fermentation and nutrient production. Through its various sections—cecum, colon, rectum, and anus—the large intestine ensures that waste is processed and expelled efficiently, contributing to the body’s overall health.
8. Accessory Organs 🔧
- Liver: Produces bile.
- Gallbladder: Stores bile produced by the liver and releases it into the small intestine to aid in fat digestion.
- Pancreas: Releases digestive enzymes into the small intestine.
The alimentary canal is a perfectly designed system that takes in food, processes it, absorbs nutrients, and expels waste. From the mouth to the anus, every part plays a vital role in ensuring the body gets the nutrients it needs to function!
Accessory Organs of Digestion 🛠️
These organs aid in the digestive process, even though food doesn’t pass through them directly. Instead, they release important substances that assist in the breakdown of food and absorption of nutrients. Here’s an engaging look at them:
1. Liver 🍏
- Purpose: The body’s chemical processing plant!
- Key Features:
- Bile Production: The liver produces bile, which is essential for breaking down fats into smaller droplets (emulsification) to make them easier to digest.
- Detoxification: It filters out toxins, drugs, and other harmful substances from the blood.
- Nutrient Storage: Stores vitamins and minerals like iron and vitamin A.
- Metabolism: It regulates blood sugar levels and stores glucose in the form of glycogen.
2. Gallbladder 🏖️
- Purpose: The liver’s storage unit for bile!
- Key Features:
- Bile Storage: The gallbladder stores bile produced by the liver until it’s needed for digestion.
- Bile Release: When food enters the small intestine, especially fatty foods, the gallbladder releases bile into the duodenum to aid in fat digestion.
Anatomy of the Gallbladder 🏖️
The gallbladder is a small, pear-shaped organ that plays an essential role in the digestion of fats by storing and concentrating bile produced by the liver. Let’s explore its detailed anatomy and its functions in the digestive system.
1. Location and Structure 📍
- Position: The gallbladder is located under the right lobe of the liver, on the right side of the abdomen, just beneath the diaphragm.
- Size: It is approximately 7-10 cm (3-4 inches) long and 4 cm (1.5 inches) wide in adults.
- Shape: The gallbladder is pear-shaped, with a broader, fundus (bulging part) and a narrow, cervix that connects to the bile ducts.
- Sections: The gallbladder has three main parts:
- Fundus: The rounded, wide end of the gallbladder that is directed toward the anterior abdominal wall.
- Body: The main portion that stores bile.
- Neck: The narrow, tapered portion that leads to the cystic duct, which connects to the common bile duct.
2. Function of the Gallbladder ⚙️
The primary role of the gallbladder is to store and concentrate bile produced by the liver, releasing it into the duodenum (the first part of the small intestine) to aid in the digestion of fats. Here’s a more detailed look at its functions:
- Bile Storage: The liver produces bile continuously, but the gallbladder stores it between meals. The gallbladder can store about 30-50 milliliters of bile.
- Bile Concentration: The gallbladder concentrates bile by absorbing water and electrolytes, making it more potent and efficient in breaking down fats.
- Bile Release: When fatty food enters the duodenum, the gallbladder contracts and releases bile into the common bile duct, which carries it to the duodenum. This release is regulated by the hormone cholecystokinin (CCK), which is secreted when food (especially fats) is present in the stomach and small intestine.
3. Gallbladder and Bile Flow 🧃
The bile produced by the liver travels through the hepatic ducts to the common hepatic duct. The bile then flows into the gallbladder through the cystic duct for storage and concentration. When food is consumed, the following steps occur:
- Storage and Concentration: The bile is stored in the gallbladder, where water and salts are absorbed, making the bile more concentrated.
- Release of Bile: After a meal, especially a fatty meal, cholecystokinin (CCK) triggers the gallbladder to contract. The sphincter of Oddi relaxes, allowing bile to flow from the gallbladder through the cystic duct into the common bile duct and finally into the duodenum to help digest fats.
4. Bile Pathway 🚶♂️
The bile produced in the liver flows along a series of ducts:
- Hepatic Ducts: Bile flows from the liver through the right and left hepatic ducts.
- Common Hepatic Duct: The right and left hepatic ducts merge to form the common hepatic duct, which carries bile to the gallbladder or directly to the duodenum.
- Cystic Duct: This duct connects the gallbladder to the common hepatic duct. Bile flows from the liver to the gallbladder via the cystic duct for storage and concentration. When needed, bile flows back from the gallbladder into the common bile duct.
- Common Bile Duct: The common bile duct carries bile from the liver and gallbladder to the duodenum. This duct also receives digestive enzymes from the pancreas via the pancreatic duct.
5. Sphincter of Oddi 🔒
- Function: The sphincter of Oddi is a muscular valve located at the junction of the common bile duct and the duodenum. It controls the flow of bile and pancreatic juices into the duodenum.
- Regulation: The sphincter of Oddi opens in response to the hormone cholecystokinin (CCK), which is released when food (especially fat) enters the stomach and small intestine. This allows bile to flow into the duodenum, aiding in fat digestion.
6. Gallbladder and Digestion 🍽️
The gallbladder plays an essential role in fat digestion by storing bile and releasing it when necessary:
- Bile Composition: Bile contains bile salts, bilirubin, cholesterol, and phospholipids. Bile salts emulsify fats, breaking them down into smaller droplets, which makes it easier for digestive enzymes to further break down fats into fatty acids and glycerol for absorption.
- Fat Digestion: Once bile is released into the duodenum, it aids in the digestion and absorption of dietary fats and fat-soluble vitamins (A, D, E, and K).
- Absorption: After fats are emulsified, the smaller fat particles are absorbed through the intestinal walls into the bloodstream.
7. Disorders of the Gallbladder ⚠️
Several common disorders can affect the gallbladder, leading to symptoms ranging from mild discomfort to severe conditions:
- Gallstones: Cholesterol or pigment stones can form in the gallbladder when there is an imbalance in the components of bile, such as excessive cholesterol or insufficient bile salts. Gallstones can obstruct the flow of bile, leading to pain and potentially gallbladder inflammation (cholecystitis).
- Cholecystitis: Inflammation of the gallbladder, often caused by gallstones blocking the cystic duct. This can lead to pain, fever, and nausea.
- Gallbladder Cancer: A rare but serious form of cancer that can develop in the gallbladder, often associated with long-standing gallstones or chronic inflammation.
- Biliary Dyskinesia: A condition where the gallbladder does not empty properly, causing pain and digestive problems.
- Acute and Chronic Cholecystitis: A condition in which the gallbladder becomes inflamed, usually due to gallstones or infection.
8. Gallbladder Removal (Cholecystectomy) 💉
- Procedure: Cholecystectomy is the surgical removal of the gallbladder, usually performed when a person has symptomatic gallstones or cholecystitis. This is a common procedure that can be done through laparoscopy (minimally invasive surgery) or open surgery.
- Post-Surgery: After gallbladder removal, bile flows directly from the liver into the small intestine, although it is less concentrated. Most people can live without their gallbladder, but they may experience changes in digestion, especially after consuming fatty meals.
The gallbladder is a small, pear-shaped organ that plays a crucial role in digestion by storing and concentrating bile produced by the liver. When fat enters the small intestine, the gallbladder releases bile to help break down fats for absorption. It is connected to the liver and duodenum through a series of ducts, and its function is regulated by hormones like cholecystokinin (CCK). Disorders like gallstones and cholecystitis can impair the gallbladder’s function, leading to pain and other digestive issues.
3. Pancreas 🍯
- Purpose: The multi-tasker of digestion!
- Key Features:
- Digestive Enzymes: The pancreas produces amylase (for carbs), lipase (for fats), and proteases (for proteins) to break down food in the small intestine.
- Insulin & Glucagon: It also produces the hormones insulin and glucagon, which regulate blood sugar levels in the body, ensuring the proper storage and use of glucose.
4. Salivary Glands 💦
- Purpose: The body’s first line of digestion!
- Key Features:
- Saliva Production: The salivary glands produce saliva, which moistens food for easier swallowing and starts the breakdown of starches with the enzyme amylase.
- Lubrication: Saliva also lubricates food, making it easier to form a bolus (a soft mass of chewed food) for swallowing.
- Antibacterial Action: It contains lysozyme, an enzyme that helps fight off bacteria in the mouth.
Anatomy of the Salivary Glands 💦
The salivary glands are a group of exocrine glands located in the mouth and are responsible for producing saliva, which is essential for the initial stages of digestion. Saliva helps moisten food, begins the breakdown of carbohydrates, and protects the oral cavity from infections. Let’s dive into the detailed anatomy and functions of the salivary glands.
1. Types of Salivary Glands 🧠
There are three major pairs of salivary glands, each responsible for producing and secreting saliva. These glands are classified into major and minor glands:
Major Salivary Glands 🍽️
The major salivary glands are large and responsible for most of the saliva production. They consist of the following:
- Parotid Glands:
- Location: The parotid glands are the largest of the salivary glands and are located just in front of the ears, beneath and in front of the ear lobes, extending down to the angle of the jaw.
- Structure: The parotid glands are serous glands, meaning they primarily secrete serous fluid, which is watery and contains amylase (an enzyme that starts the breakdown of starches).
- Duct: The saliva produced by the parotid glands drains through the Stensen’s duct, which opens into the buccal cavity (the inner part of the cheek), opposite the upper second molar.
- Submandibular Glands:
- Location: The submandibular glands are located beneath the mandible (lower jaw), near the angle of the jaw.
- Structure: The submandibular glands are mixed glands. They produce both serous fluid (containing amylase) and mucous fluid (which lubricates food for easier swallowing).
- Duct: The saliva from the submandibular glands drains into the mouth via the Wharton’s duct, which opens under the tongue at the sublingual caruncle.
- Sublingual Glands:
- Location: The sublingual glands are located beneath the tongue, in the floor of the mouth.
- Structure: These are the smallest of the major salivary glands and are primarily mucous glands. They produce a thick, mucus-like secretion that helps lubricate food.
- Ducts: The sublingual glands have multiple small ducts (called Rivinus ducts), which open along the sublingual fold under the tongue. One main duct (the Bartholin’s duct) also drains into the submandibular duct.
Minor Salivary Glands 🦷
- The minor salivary glands are smaller glands scattered throughout the mucous membranes of the oral cavity, including the lips, cheeks, hard palate, soft palate, and floor of the mouth. These glands produce mucous saliva that helps in lubrication and protection.
- These glands do not have large ducts like the major glands. Instead, they secrete saliva directly into the oral cavity through smaller duct openings.
2. Structure of the Salivary Glands 🧬
Salivary glands are composed of clusters of acinar cells (the basic functional unit) and ductal systems that transport saliva to the oral cavity:
- Acini (Plural of Acinus):
- Acini are clusters of secretory cells that produce the saliva. These cells are classified into two types:
- Serous cells: These cells produce a watery secretion that contains enzymes like amylase (which starts the breakdown of starch) and lysozyme (which has antibacterial properties).
- Mucous cells: These cells secrete mucus, which helps lubricate food and protect the mouth’s mucous membranes.
- Acini are clusters of secretory cells that produce the saliva. These cells are classified into two types:
- Duct System:
- The acini drain their secretion into a system of ducts that transport saliva to the oral cavity.
- The ducts are lined with epithelial cells that can modify the composition of saliva. For example, they can adjust the electrolyte concentration, such as increasing sodium and chloride and decreasing bicarbonate and potassium.
3. Functions of the Salivary Glands 🏃♂️
The main functions of the salivary glands include the production of saliva, which plays several critical roles in digestion and oral health:
- Moistening and Lubricating Food: Saliva moistens food, making it easier to chew and swallow. It also helps form a bolus (a soft mass of chewed food) that is easier to move down the esophagus.
- Initiating Digestion: The amylase enzyme in saliva begins the breakdown of carbohydrates (specifically starches) into smaller sugars like maltose. This is the first step in carbohydrate digestion.
- Antibacterial Action: Saliva contains lysozyme, an enzyme that helps kill harmful bacteria and prevent infections in the oral cavity. It also contains IgA (Immunoglobulin A), an antibody that helps protect against oral pathogens.
- Maintaining Oral Health: Saliva helps neutralize acids in the mouth, protecting teeth from decay. It also helps remineralize enamel by providing calcium and phosphate ions.
- Tasting: Saliva helps dissolve food particles so that they can interact with the taste buds on the tongue, allowing for the sensation of taste.
- Cleansing the Mouth: Saliva helps rinse away food particles and debris from the mouth, maintaining cleanliness and hygiene.
- Buffering: Saliva contains bicarbonates, which act as a buffer to maintain the pH of the oral cavity and prevent the mouth from becoming too acidic.
4. Regulation of Saliva Production 🧠
The production of saliva is regulated by the autonomic nervous system, and it can be stimulated by several factors:
- Parasympathetic Stimulation: This is the main driver of saliva production. When you think about, smell, or even taste food, the parasympathetic nervous system activates and increases saliva flow to prepare the mouth for digestion.
- Sympathetic Stimulation: In contrast, the sympathetic nervous system (activated during stress or fight-or-flight situations) reduces the volume of saliva production but increases the viscosity (thickness) of the saliva. This is why your mouth may feel dry during anxiety or stress.
- Hormonal Regulation: Certain hormones, such as aldosterone, can influence the amount of salt and water in saliva. Some medications may also affect saliva production.
5. Disorders of the Salivary Glands ⚠️
Several common conditions can affect the function and health of the salivary glands:
- Xerostomia (Dry Mouth): A condition in which there is reduced saliva production, often caused by medication, dehydration, or autoimmune diseases like Sjogren’s syndrome. It can lead to difficulty swallowing, bad breath, and increased risk of dental cavities.
- Sialolithiasis (Salivary Stones): The formation of stones in the ducts of the salivary glands, most commonly in the submandibular gland. These stones can block the flow of saliva, causing pain and swelling.
- Sialadenitis: Inflammation or infection of the salivary glands, often due to bacterial infection (like Staphylococcus aureus) or viral infection (such as mumps).
- Mumps: A viral infection that causes swelling of the parotid glands and can lead to pain and difficulty swallowing.
- Salivary Gland Cancer: Rare, but tumors can develop in the salivary glands, with parotid glands being the most commonly affected. Symptoms may include swelling or lumps in the mouth or jaw.
The salivary glands are essential for the initial stages of digestion, oral health, and overall well-being. They produce saliva, which not only helps moisten and lubricate food but also contains enzymes that begin carbohydrate digestion. The salivary glands also play a critical role in maintaining oral hygiene, protecting against infections, and buffering acids in the mouth. Disorders affecting the salivary glands can lead to discomfort, difficulty in eating, and increased risk of oral diseases.
The accessory organs of digestion play essential roles in helping the body break down and absorb nutrients. While they don’t come into direct contact with food, they produce and release substances (like enzymes and bile) that are vital for digestion, making them key players in the digestive process!
The Digestive System: Application and Implications in Nursing
The digestive system is essential for breaking down food, absorbing nutrients, and expelling waste, and understanding it is crucial for nurses in various healthcare settings. Nurses play an important role in managing patients with digestive disorders, promoting health, and providing patient education about nutrition, digestion, and prevention of gastrointestinal diseases. Below are key applications and implications of the digestive system in nursing practice:
1. Patient Assessment and History Taking 📝
Nurses are often the first healthcare professionals to assess patients for digestive problems. This includes collecting a thorough health history and performing physical examinations:
- Health History: Nurses should inquire about:
- Symptoms such as pain, bloating, nausea, vomiting, diarrhea, or constipation.
- Dietary habits, including food intolerance, food allergies, and nutritional deficiencies.
- History of gastrointestinal diseases, such as GERD, Crohn’s disease, ulcerative colitis, irritable bowel syndrome (IBS), and liver diseases.
- Medications that may affect the digestive system (e.g., antacids, antibiotics, NSAIDs).
- Physical Examination: Nurses should assess for signs of malnutrition, dehydration, abdominal distension, and tenderness upon palpation. Observation of stool characteristics can also help guide the assessment.
2. Nursing Care for Digestive Disorders 🏥
Nurses must provide care and support to patients with various digestive disorders, managing both acute and chronic conditions:
- Gastroesophageal Reflux Disease (GERD):
- Nursing Actions: Educate patients to avoid large meals, lying down immediately after eating, and foods that trigger reflux (e.g., spicy, acidic foods). Encourage weight loss and elevating the head of the bed.
- Implications: Monitoring for complications like esophagitis, Barrett’s esophagus, and esophageal cancer.
- Peptic Ulcers:
- Nursing Actions: Administer medications like proton pump inhibitors (PPIs) and antibiotics (for H. pylori infection). Ensure patients avoid irritating foods (e.g., caffeine, alcohol) and smoking.
- Implications: Regularly assess for signs of bleeding, such as vomiting blood or black, tarry stools.
- Irritable Bowel Syndrome (IBS):
- Nursing Actions: Help identify triggers (e.g., stress, certain foods) and encourage dietary changes like increasing fiber intake. Recommend probiotics and stress management techniques.
- Implications: Ongoing education to manage the chronic nature of the condition and prevent flare-ups.
- Inflammatory Bowel Disease (IBD) – Crohn’s and Ulcerative Colitis:
- Nursing Actions: Administer medications as prescribed, including anti-inflammatory drugs and immunosuppressants. Monitor for signs of complications like intestinal obstruction or malnutrition.
- Implications: Support during flare-ups, managing pain, and dehydration.
- Liver Diseases (e.g., Hepatitis, Cirrhosis, Fatty Liver Disease):
- Nursing Actions: Monitor liver function tests and bilirubin levels. Educate about the importance of avoiding alcohol and maintaining a balanced diet.
- Implications: Watch for signs of ascites, jaundice, and encephalopathy. Encourage adherence to medications like antiviral therapy and diuretics.
- Pancreatitis:
- Nursing Actions: Monitor vital signs, fluid status, and abdominal pain. Administer pain relief (e.g., opioids), and assist with nutrition management (initially through NPO status, then progressing to oral intake).
- Implications: Be vigilant for complications like respiratory distress, infection, or shock.
3. Nutrition and Dietary Management 🍏
A vital role of nursing in the digestive system is promoting proper nutrition and managing special diets:
- Nutritional Assessment: Nurses assess the patient’s diet, identify deficiencies, and collaborate with a dietitian to develop an individualized plan to support digestion and absorption of nutrients.
- Enteral Nutrition: For patients unable to ingest food orally, nurses help with the management of enteral feeding tubes (e.g., nasogastric tubes or gastrostomy tubes) and ensure proper technique for feeding and hydration.
- Parenteral Nutrition: For critically ill patients who need intravenous (IV) nutrition, nurses must manage total parenteral nutrition (TPN) administration, monitoring for complications such as infection or electrolyte imbalances.
4. Pain Management and Comfort 💊
Many digestive disorders are accompanied by significant pain, which requires effective management:
- Pain Assessment: Nurses use tools like the visual analog scale or numeric pain scale to assess the severity of abdominal pain and ensure appropriate pain relief.
- Medication: Nurses may administer analgesics (e.g., acetaminophen, NSAIDs) or opioids (e.g., morphine) for pain management in severe cases. Careful attention to dosing is necessary, especially with opioids, to prevent side effects like constipation.
- Comfort Measures: In addition to medications, non-pharmacological methods such as positioning, warm compresses, and relaxation techniques can help alleviate discomfort.
5. Patient Education 📚
Education is a key responsibility of nursing in the context of the digestive system:
- Dietary Modifications: Nurses educate patients about appropriate diets based on their specific digestive conditions. This includes advising on low-fat, low-sodium, or high-fiber diets, and encouraging the elimination of trigger foods (e.g., spicy foods, caffeine, alcohol).
- Hydration: Emphasize the importance of maintaining adequate hydration, particularly for patients with diarrhea or vomiting, to prevent dehydration.
- Prevention of Complications: Nurses guide patients on preventing complications such as constipation, gastric reflux, or intestinal obstruction.
- Medication Compliance: Nurses ensure patients understand the importance of taking medications as prescribed, such as antacids, laxatives, or antibiotics for gastrointestinal infections.
- Screening and Early Detection: Educate on the importance of regular screenings, such as colonoscopy for colorectal cancer and liver function tests for hepatitis or cirrhosis.
6. Implications in Postoperative Care 🛏️
In patients who have undergone gastrointestinal surgery, nurses play a critical role in postoperative care:
- Monitoring for Complications: After surgeries like gastrectomy, bariatric surgery, or colorectal resection, nurses monitor for complications such as infection, wound healing, and bowel motility.
- Nutritional Support: Postoperative patients may need specific dietary adjustments or enteral/parenteral nutrition to support healing and prevent malnutrition.
- Pain Management: Postoperative pain is common, and effective pain management strategies (such as medication and comfort measures) are essential for patient recovery.
7. Psychological and Emotional Support 🧠
Digestive disorders, especially chronic conditions like Crohn’s disease, IBS, and liver disease, can have psychological and emotional impacts. Nurses must provide:
- Emotional Support: Acknowledge the impact of chronic gastrointestinal diseases on a patient’s mental health and well-being. Provide a compassionate ear and direct patients to support groups or counseling services if needed.
- Stress Management: Encourage relaxation techniques and stress management strategies to reduce the impact of stress on gastrointestinal symptoms, especially in conditions like IBS.
8. Special Considerations for Pediatric and Geriatric Patients 👶👴
- Pediatric Patients: Nurses must recognize that infants and children have different gastrointestinal needs. This includes managing gastroesophageal reflux (GER), colic, and diarrheal diseases, as well as ensuring proper growth and development through adequate nutrition.
- Geriatric Patients: Older adults are more susceptible to conditions like constipation, diverticulosis, and malabsorption syndromes. Nurses must assess for age-related changes in gastrointestinal function, such as slower gastric emptying and reduced enzyme activity.
The digestive system is essential for overall health and well-being, and nurses are key in managing and supporting patients with gastrointestinal conditions. Through patient assessment, care for digestive disorders, nutritional management, pain control, and patient education, nurses can greatly improve patient outcomes. Understanding the implications of the digestive system in nursing helps ensure a holistic approach to patient care, ultimately promoting health, recovery, and prevention of complications.