Anatomy -Unit-2-The Respiratory system
🌬️ The Respiratory System: Breathing Life into the Body 🌬️
The respiratory system is responsible for taking in oxygen and expelling carbon dioxide from the body. It plays a vital role in gas exchange and homeostasis, ensuring that cells receive the oxygen they need to produce energy and that carbon dioxide, a waste product, is removed efficiently.
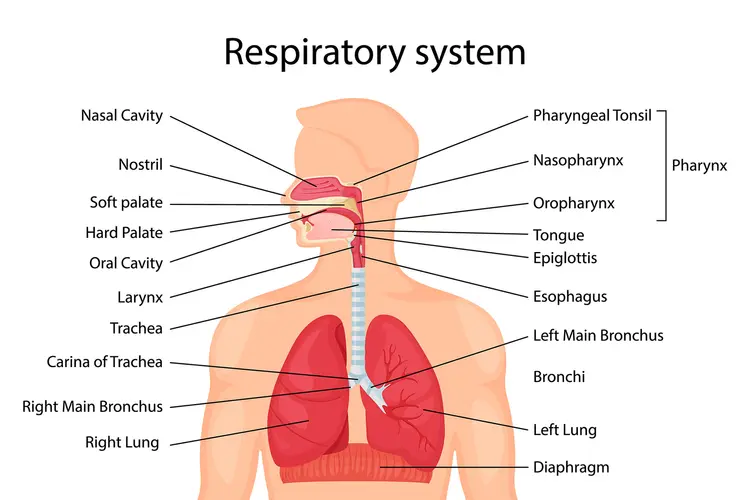
1. Anatomical Overview of the Torso (The Body’s Breathing Zone)
The torso (or trunk) contains the vital organs for respiration, including the lungs, trachea, bronchi, and diaphragm. The torso is the central body region that houses the organs responsible for the mechanics of breathing.
- Thoracic Cavity: This cavity is enclosed by the rib cage, sternum (breastbone), and vertebrae (spine). It houses the lungs, heart, esophagus, and trachea (windpipe).
- Pleural Membranes: The lungs are surrounded by double-layered membranes called the pleura:
- Visceral Pleura: The inner layer that is directly attached to the surface of the lungs.
- Parietal Pleura: The outer layer that lines the chest wall and diaphragm.
- Diaphragm: This is a large, dome-shaped muscle that separates the thoracic cavity from the abdominal cavity. It plays a crucial role in breathing by contracting and relaxing to allow air in and out of the lungs.
2. Structure of the Organs of Respiration
The organs of respiration can be grouped into the upper respiratory system and the lower respiratory system. Let’s take a detailed look at each organ involved in respiration.
Upper Respiratory Tract 🫁
- Nose and Nasal Cavity:
- Structure: The nose is made up of cartilage and bone, with nostrils (external openings). The nasal cavity is divided by the nasal septum and lined with mucus membranes.
- Function: The nose warms, moistens, and filters air as it is inhaled. It also helps trap dust, microbes, and other particles in mucus, which is moved by cilia (tiny hair-like structures).
- Pharynx (Throat):
- Structure: The pharynx is a muscular tube that extends from the nasal cavity to the larynx. It is divided into three parts: the nasopharynx, oropharynx, and laryngopharynx.
- Function: The pharynx serves as a passage for air, food, and liquids. It also plays a role in voice resonance.
- Larynx (Voice Box):
- Structure: The larynx is located at the top of the trachea and contains the vocal cords. It is composed of cartilage (including the thyroid cartilage, also known as the Adam’s apple) and is lined with mucous membranes.
- Function: The larynx is responsible for voice production, protecting the trachea, and directing air to the lower respiratory tract. The vocal cords vibrate when air passes through, producing sound.
Lower Respiratory Tract 🌬️
- Trachea (Windpipe):
- Structure: The trachea is a tube-like structure made of C-shaped cartilage rings that prevent it from collapsing. It is lined with ciliated epithelial cells and mucous membranes.
- Function: The trachea transports air to the bronchi and lungs. The cilia in the trachea help move mucus up to the throat to be expelled or swallowed.
- Bronchi:
- Structure: The trachea divides into two primary bronchi (right and left), each leading into one lung. These primary bronchi further branch into secondary and tertiary bronchi, and finally into smaller bronchioles.
- Function: The bronchi conduct air into the lungs and divide into smaller bronchioles. The smooth muscles in the walls of the bronchi help regulate airflow.
- Lungs:
- Structure: The lungs are paired organs located in the thoracic cavity. The right lung has three lobes, while the left lung has two lobes to accommodate the heart. The lungs are covered by a pleura (two-layered membrane).
- Function: The lungs are the primary organs for gas exchange. Oxygen from the air is absorbed into the bloodstream, and carbon dioxide is expelled from the bloodstream into the airways to be exhaled.
Alveoli 🫁
- Structure: The alveoli are tiny air sacs at the end of the bronchioles. They are surrounded by a network of capillaries (tiny blood vessels). Each alveolus is made up of epithelial cells and has a thin membrane for easy gas exchange.
- Function: The alveoli are the sites where oxygen from the air diffuses into the bloodstream, and carbon dioxide diffuses out of the blood into the alveolar space, to be exhaled.
3. Mechanism of Breathing (Pulmonary Ventilation)
Breathing is the movement of air into and out of the lungs and is controlled by the diaphragm and intercostal muscles (muscles between the ribs).
- Inhalation: When the diaphragm contracts, it moves downward, increasing the volume of the thoracic cavity. This creates a negative pressure that draws air into the lungs.
- Exhalation: When the diaphragm relaxes, it moves upward, and the intercostal muscles help push air out of the lungs, decreasing the volume of the thoracic cavity.
4. Gas Exchange (External Respiration)
The primary function of the respiratory system is the exchange of oxygen and carbon dioxide. This occurs in the alveoli:
- Oxygen diffuses from the alveoli into the capillaries, where it binds to hemoglobin in red blood cells and is transported to body tissues.
- Carbon dioxide diffuses from the capillaries into the alveoli to be expelled from the body during exhalation.
5. Summary of the Respiratory Organs
| Organ | Structure | Function |
|---|---|---|
| Nose/Nasal Cavity | Cartilage, bone, mucous membranes | Warms, moistens, and filters air |
| Pharynx | Muscular tube | Passage for air, food, and liquids; voice resonance |
| Larynx | Cartilage, vocal cords | Voice production, protects trachea |
| Trachea | C-shaped cartilage, ciliated epithelium | Transports air to lungs |
| Bronchi | Cartilage, smooth muscle | Conduct air to lungs |
| Lungs | Lobed, surrounded by pleura | Gas exchange: oxygen in, carbon dioxide out |
| Alveoli | Air sacs, surrounded by capillaries | Site of gas exchange (oxygen and carbon dioxide) |
| Diaphragm | Dome-shaped muscle | Assists in inhalation and exhalation by altering thoracic volume |
Fun Fact:
Each alveolus is surrounded by around 300 million alveoli in each lung! This large surface area facilitates efficient gas exchange between the lungs and blood.
Muscles of Respiration: The Engine Behind Breathing 🌬️
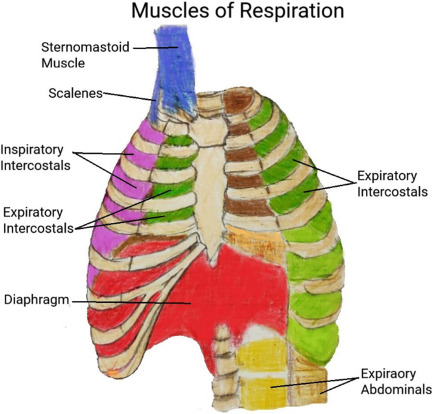
Breathing is a mechanical process that involves inhalation (taking air into the lungs) and exhalation (expelling air from the lungs). This process relies on the muscles of respiration, which work together to alter the volume of the thoracic cavity (chest cavity), creating pressure changes that facilitate airflow into and out of the lungs.
1. Primary Muscles of Respiration
The primary muscles of respiration are responsible for the mechanics of breathing. These muscles are mainly involved in inhalation and exhalation, although some also play a role in both processes.
1.1. Diaphragm 🫁
- Structure:
The diaphragm is a dome-shaped muscle located at the base of the thoracic cavity, separating the chest from the abdominal cavity. - Function:
- The diaphragm is the most important muscle for breathing. It plays a critical role in inhalation and exhalation.
- Inhalation: When the diaphragm contracts, it flattens and moves downward, increasing the volume of the thoracic cavity. This reduces pressure within the lungs, causing air to flow in.
- Exhalation: When the diaphragm relaxes, it moves upward, reducing the space in the thoracic cavity and pushing air out of the lungs.
- Contribution to Breathing: The diaphragm is responsible for about 75% of the effort during normal, quiet breathing (called tidal breathing).
1.2. External Intercostal Muscles 💪
- Structure:
The external intercostal muscles are located between the ribs. These muscles run diagonally from the bottom of one rib to the top of the next. - Function:
- Inhalation: The external intercostal muscles contract, causing the ribs to elevate and expand outward. This action increases the volume of the thoracic cavity, allowing air to enter the lungs.
- Contribution to Breathing: The external intercostal muscles contribute to about 25% of the effort during normal breathing, especially in forced inhalation (deep breathing).
2. Accessory Muscles of Respiration
The accessory muscles are used during forceful inhalation or exhalation (such as during exercise, coughing, or respiratory distress). These muscles become active when the body needs extra help to expand or contract the thoracic cavity.
2.1. Accessory Muscles for Inhalation
- Sternocleidomastoid (SCM):
- Structure: Located in the neck, running from the sternum and clavicle to the mastoid process of the skull.
- Function: When contracted, the SCM elevates the sternum and increases the volume of the thoracic cavity, aiding in deep inhalation.
- Scalenes:
- Structure: A group of three muscles (anterior, middle, and posterior) located in the neck.
- Function: The scalenes elevate the first two ribs, further expanding the thoracic cavity during deep breathing.
- Pectoralis Minor:
- Structure: A small muscle located in the upper chest.
- Function: During deep inhalation, it helps elevate the ribs and expand the chest.
2.2. Accessory Muscles for Exhalation
- Abdominal Muscles:
- Structure: Includes the rectus abdominis, obliques, and transversus abdominis.
- Function: These muscles contract to increase abdominal pressure and push the diaphragm upwards, aiding in forceful exhalation.
- Internal Intercostal Muscles:
- Structure: Located beneath the external intercostals, they run in the opposite direction.
- Function: The internal intercostals help lower the ribs and decrease the thoracic cavity volume during forced exhalation.
3. Mechanism of Breathing: Contribution of Muscles
The process of breathing involves inhalation and exhalation, which are controlled by the diaphragm and intercostal muscles, with accessory muscles becoming involved during more forceful breathing.
3.1. Inhalation Process
- Diaphragm contracts and moves downward.
- External intercostal muscles contract, lifting the ribs upward and outward.
- Accessory muscles (SCM, scalenes, pectoralis minor) may also assist to increase the volume of the thoracic cavity.
The combined contraction of these muscles increases the volume of the chest cavity, lowering the air pressure inside the lungs compared to the outside, allowing air to flow in.
3.2. Exhalation Process
- Diaphragm relaxes and moves upward, reducing the thoracic cavity’s volume.
- Internal intercostal muscles and abdominal muscles contract to force the ribs down and push the diaphragm further upward, respectively.
- In forced exhalation, the abdominal muscles play a significant role in pushing air out rapidly.
Exhalation occurs when the volume of the thoracic cavity decreases, increasing the pressure in the lungs and pushing air out.
4. Summary of Muscles of Respiration and Their Contribution
| Muscle Group | Function | Contribution to Breathing |
|---|---|---|
| Diaphragm | Main muscle for inhalation and exhalation | 75% of the effort in normal breathing |
| External Intercostals | Elevate the ribs for inhalation | 25% of the effort in normal breathing |
| Accessory Muscles | Assist with deep breathing or forced breathing | Used during intense activity or distress |
| Abdominal Muscles | Aid in forceful exhalation | Active in forced exhalation |
| Internal Intercostals | Depress the ribs for forced exhalation | Active in forced exhalation |
Fun Fact:
The diaphragm is often called the “breathing muscle” because it plays the most significant role in normal, quiet breathing. During deep or forceful breathing, muscles like the abdominals and intercostals take over.
The muscles of respiration work in harmony to ensure proper airflow into and out of the lungs. Inhalation is mainly powered by the diaphragm and external intercostals, while exhalation is a passive process, except during forced breathing, when additional muscles help with the expulsion of air.
Application and Implications of the Respiratory System in Nursing 🩺
The respiratory system is vital to overall health, and understanding how it functions is essential for nurses to provide effective care. Nursing care related to the respiratory system involves monitoring and managing respiratory health, from preventing infections to assisting patients with chronic respiratory conditions.
1. Monitoring Respiratory Function

Nurses are often the first line of defense in detecting and responding to changes in a patient’s respiratory function.
- Assessment Techniques:
- Vital Signs: Nurses regularly monitor respiratory rate, oxygen saturation (SpO2), and lung sounds (using a stethoscope to listen for abnormalities such as wheezing, crackles, or absent breath sounds).
- Auscultation: Listening to lung sounds for abnormalities such as crackles (indicative of fluid), wheezing (narrowed airways), or stridor (obstruction in the upper airway).
- Pulse Oximetry: This non-invasive tool provides real-time data on blood oxygen levels, a critical measure of respiratory function.
- Assessment of Breathing Patterns:
- Normal Breathing: 12-20 breaths per minute (adults).
- Abnormal Breathing Patterns: Conditions such as dyspnea (difficulty breathing), tachypnea (rapid breathing), or bradypnea (slow breathing) require prompt evaluation and intervention.
Application:
- Monitoring respiratory status allows nurses to detect early signs of respiratory distress (e.g., increased work of breathing or low oxygen saturation) and provide early intervention (e.g., administering oxygen, adjusting patient positioning, or performing chest physiotherapy).
2. Managing Respiratory Disorders

Nurses play a key role in managing patients with a variety of respiratory disorders, such as asthma, chronic obstructive pulmonary disease (COPD), pneumonia, and pulmonary edema.
Asthma and COPD:
- Medications: Nurses are responsible for administering medications such as bronchodilators, corticosteroids, and leukotriene inhibitors to manage symptoms.
- Patient Education: Nurses educate patients on how to use inhalers properly, the importance of adherence to medication regimens, and recognizing early signs of exacerbations.
Pneumonia:
- Antibiotics: Nurses assist in administering antibiotics or antivirals and monitor the patient for signs of improvement or adverse reactions.
- Oxygen Therapy: In cases of hypoxia, nurses monitor oxygen levels and ensure correct oxygen delivery through nasal cannulas, face masks, or non-invasive ventilation.
Pulmonary Edema:
- Fluid Management: Nurses closely monitor fluid balance and manage diuretics to reduce fluid accumulation in the lungs.
- Positioning: Proper positioning of patients, such as elevating the head of the bed, helps improve oxygenation and relieve dyspnea.
Application:
Nurses provide ongoing monitoring, medication management, and patient education to reduce the frequency of flare-ups, improve quality of life, and avoid hospital readmissions for respiratory conditions.
3. Oxygen Therapy and Respiratory Support

Oxygen therapy is a common intervention in nursing care for patients with respiratory issues. Nurses must be proficient in administering oxygen and understanding its implications for different clinical conditions.
- Oxygen Delivery Devices:
- Nasal Cannula: Low to moderate flow oxygen (1-6 L/min).
- Face Mask: Higher flow oxygen, for short-term use in emergency situations or when nasal cannulas are insufficient.
- Non-invasive Ventilation (CPAP/BiPAP): For patients with acute respiratory distress or COPD.
- Mechanical Ventilation: For patients in critical conditions, requiring intubation and ventilation support.
Application:
- Nurses monitor oxygen saturation, watch for complications like oxygen toxicity, and ensure the safety of oxygen delivery, including checking for leaks or skin irritation from devices.
4. Postoperative Respiratory Care

After surgery, especially in patients who have undergone thoracic, abdominal, or general anesthesia, respiratory care is crucial.
- Prevention of Atelectasis (Lung Collapse):
- Nurses encourage deep breathing exercises, incentive spirometry, and early ambulation to prevent atelectasis and improve lung expansion.
- Pain Management:
Pain after surgery, especially abdominal or chest surgery, can prevent deep breathing. Nurses ensure that pain is well-managed to allow adequate breathing and coughing to clear secretions. - Monitoring for Complications:
Nurses are vigilant in monitoring for hypoxia, respiratory depression, and infection.
Application:
Postoperative care nurses actively help mobilize patients, encourage deep breaths, and assist with coughing and incentive spirometry to prevent lung complications after surgery.
5. End-of-Life Care and Palliative Respiratory Support

In end-of-life care or palliative care, nurses manage respiratory distress to provide comfort for terminally ill patients.
- Symptom Management:
- For patients experiencing dyspnea, nurses administer medications like morphine (to reduce breathing effort) or bronchodilators for comfort.
- Oxygen therapy is also provided to relieve air hunger.
- Positioning:
Proper positioning, such as elevating the head of the bed or positioning the patient on their side, can help ease the difficulty of breathing and improve comfort.
Application:
Nurses in palliative care focus on providing symptom relief, improving comfort, and offering emotional support to patients and their families.
6. Patient Education and Health Promotion

Nurses play an essential role in educating patients about respiratory health, prevention, and self-management.
- Smoking Cessation: Nurses educate patients about the detrimental effects of smoking on lung health and assist in providing smoking cessation programs or resources.
- Preventing Respiratory Infections: Nurses teach patients about proper hand hygiene, the importance of vaccinations (e.g., flu, pneumonia), and how to avoid exposure to respiratory pathogens.
- Asthma Management: Nurses help patients understand how to use inhalers properly, recognize triggers, and take preventive medications to control asthma symptoms.
- COPD Management: Nurses support self-management strategies like breathing exercises (e.g., pursed-lip breathing) and nutrition to maintain optimal lung function.
Application:
Nurses actively provide ongoing patient education to prevent respiratory issues, improve adherence to treatment, and manage chronic conditions.
7. Implications in Nursing Practice
- Critical Care: In the ICU or emergency room, nurses assess and manage severe respiratory conditions such as acute respiratory distress syndrome (ARDS), severe asthma attacks, and respiratory failure. This involves using advanced ventilators and continuous monitoring of blood gases.
- Chronic Disease Management: Nurses are instrumental in monitoring and providing care plans for patients with chronic respiratory diseases like COPD, asthma, and pulmonary fibrosis, helping to manage symptoms, reduce flare-ups, and improve quality of life.
- Emergency Response: Nurses in emergency settings must recognize respiratory distress early and provide immediate interventions (e.g., oxygen therapy, intubation, or CPR) to restore proper breathing.
The respiratory system plays a vital role in the homeostasis of the body. Nurses are integral in assessing, managing, and educating patients about respiratory health. From monitoring and supporting breathing to providing education, nurses contribute significantly to the prevention, treatment, and management of respiratory conditions across the lifespan.