ENGLISH-CHN-1-UNIT-3-Health Assessment
CHN-1-UNIT-3-Health Assessment:
Health Assessment
a) Characteristics of a healthy
individual
b) Health assessment of infant,
preschool, school going, adolescent,
adult, antenatal woman, postnatal
woman, and elderly.
CHN-1-UNIT-3-Health Assessment:

Introduction :

Good health is essential to leading a successful life. Health for All is a worldwide social goal to be achieved. The spread of health education and awareness for all has brought about positive changes in the overall attitude of individuals, governments and social organizations towards health. Targets have been set for people to achieve optimal health. Health assessment is one of the most important components in the nursing process. Health assessment is valuable for assessing the health status of individuals, families and communities. Further planning can be implemented and evaluated on the basis of health assessment. Nurses are expected to have in-depth knowledge of assessment skills. Health assessment is a regular and continuous process. In any setting of a health unit that focuses on health and wellness, nurses are responsible for providing primary health care. Therefore, health assessment skills have become more important than health assessment.
Advantages:

- Health assessment provides knowledge of the health status of individuals, families, and communities.
- Health assessment helps identify health problems in a community and provides information to prepare a plan.
- Health assessment provides an opportunity to directly interact with people of different age groups in the community.
- Helps to develop good relationships in the community.
- Health assessment helps in early diagnosis of diseases and disorders.
- Helps in identifying health problems in the community.
- Provides information to prepare a plan.
- Also helpful in providing education in the community and providing protection against diseases. है.
Characteristics of a healthy individual:

Characteristics of a healthy individual:
Health:

- Health is a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity. Therefore, health does not mean being free from illness but achieving the best state of health that enables a person to lead a productive life and that can be useful not only for oneself but also for others, therefore staying healthy by using all modern facilities is our birth right.”
- There is no system that can describe the universally acceptable characteristics of a healthy person because those characteristics are also influenced by the aging process, life events and personal values. Health and disease are subjective states, which are difficult to measure. Therefore, the evaluation of symptoms of a healthy individual should be done according to the level of health, disease and functions. Here are the characteristics of a healthy person… 1. Physical characteristics 2. Social characteristics Characteristics)
Here are the characteristics of a healthy person which are as follows…
1. Physical characteristics
2. Social characteristics
3. Spiritual & cultural characteristics
4. Mental characteristics (mental characteristics)
Physical characteristics :

Physical characteristics of a healthy individual ):

- Physical health is the foundation for a person’s overall health. When a person is healthy, every organ and system in their body functions properly. The physical characteristics of a healthy individual help in identifying them medically. Physical characteristics are related to the structure and function of the body and can be measured through a head-to-toe assessment. Such characteristics are easier to understand on a head-to-toe basis. The physical characteristics of a healthy person are shown below.
- A healthy person appears to be pleasant, cheerful, has a normal height and weight, is intelligent, has a smiling face, is friendly in nature, is well dressed and has good posture.
- A healthy individual is also well oriented to time, place and person. Responds to questions immediately. Maintains eye-to-eye contact. And are fully conscious and have good judgment capabilities.
- The speech of a healthy individual is clear and appropriate, uses correct words, has a good grasp on sentences and wording.
1.Maintained Head and Brain Function:
- A healthy person’s brain is active. He does not have neurological problems like dizziness, memory loss, or anxiety. Eyes are bright and vision is clear. Oxygen and blood supply to the brain is adequate. The ears are of normal size and symmetry and there is no discharge from the ears. Hearing is normal. The nose is of the same color as the face, no lesions or nodules are seen, and no discharge is seen. The nasal septum is in the midline and olfactory function is normal.
- Head: The head of a healthy person is symmetrically rounded and has a full range of motion. The skull is firm and symmetrical and free from inflammation, cysts, lesions, and tenderness.
2.Oral Health and Dental Hygiene:

- Lips are symmetrical, smooth, moist and free of nodules and ligatures. Buccal mucosa is pink, moist and free of discolorations. No ulcers are seen.
- Teeth are 28 to 32 and are white, in good condition and strong. Dental caries is not seen. Gums are pink, clean and free of erythema, cyanosis, bleeding and swelling and inflammation. Halitosis (bad smell) is not present in the mouth. Tongue is clean and does not show any signs of infection or fungal growth.
3.Normal Skin and Hair Condition:

- Skin is moisturized, elastic and of equal tone. There is no itching, rash or dryness. Hair is shiny, strong and falls out less. Hair is clean, well oiled, well combed (well combed), without dandruff and the skull is smooth.
4.Cardiac and Respiratory Function:
- Pulse Rate: 60–100 bpm
- Respiratory Function: 12–20 breaths/minute
- Blood Pressure: 120/80 mmHg
- No dyspnea, tachycardia or There should be no symptoms of Bradycardia.
5.Normal Body Temperature:

- A body temperature of 98.6°F (37°C) is considered ideal. Extreme temperature changes: Fever, Hypothermia: indicate health disturbances.
6. Healthy Neck, Shoulders and Posture:
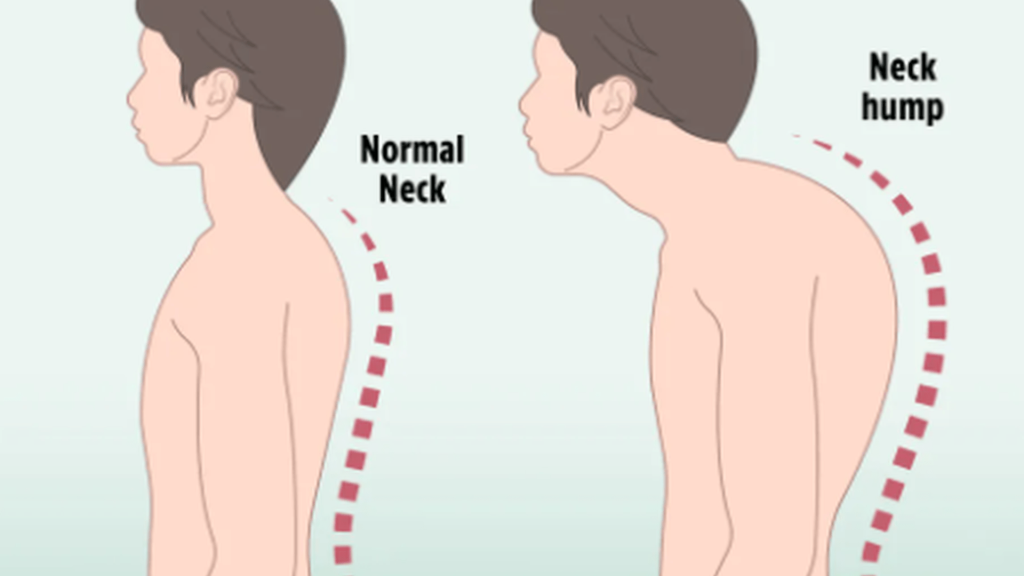
- Body posture is straight and balanced. There is no pain or stiffness in the neck and shoulders. Posture is a highlight of healthy coordination of the nervous system and muscles.
7. Body Mass Index (BMI):
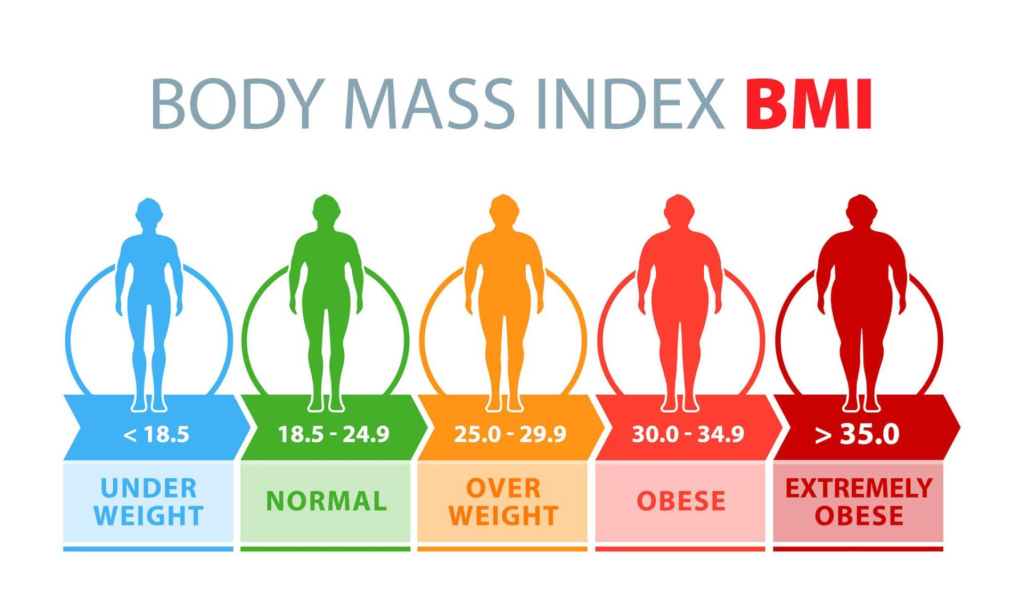
- Ideal BMI Range: 18.5 – 24.9 This range indicates that a person is neither underweight nor overweight nor obese. This person’s nutrition and metabolism are in balance.
8. Hand Muscle Strength and Grip:

- Active hand grip and steady hand movements indicate healthy neuromuscular function. The person does not feel tired while writing, holding, or lifting.
9. Energy Level and Physical Activity:

- A healthy person can easily perform any daily activity: such as walking, standing, working. There should be no complaints like continuous tiredness, lethargy or fatigue.
10. Healthy Digestive Function and Appetite:

- The person feels regular hunger and food is digested properly. There are no gastric issues like acidity, bloating or constipation. Liver, pancreas, and intestines work well.
11. Urinary and Excretory Function:
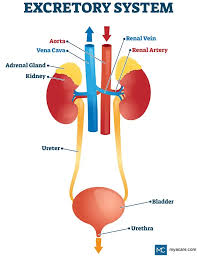
- Urinary excretion is regular and easy. The color of the urine is pale yellow and there is no burning or odd odor. Bowel Movements are regular.
12. Sleep Pattern and Quality:

- A healthy person gets 7-8 hours of uninterrupted sleep every day. After sleeping, one feels refreshed and mentally clear. No disturbances such as Insomnia, Hypersomnia, or Sleep Apnea.
13. Muscle Tone and Strength:

- The muscles of the body are fit and proper. The person can easily perform activities like stretching, lifting or walking. There will be no symptoms like sarcopenia.
14. Leg Function and Structure:
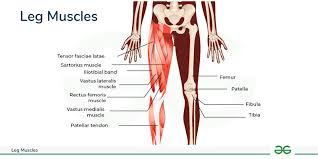
- The legs are strong, balanced and pain-free. A healthy gait – that is, the way you walk – is stable. There is no pain, swelling or muscle pressure in the joints.
The physical characteristics of a healthy individual are extremely important for their overall health status. When each organ of the body functions properly, the person remains active and healthy in every aspect of life. Everything from his behavior to his body language shows a healthy baseline. Such physical health helps a person live a long, energetic and high-quality life.
Social Characteristics:

Social Characteristics of Healthy Individual:

Social Health is an important organ of entire health. According to the World Health Organization (WHO), health is not just the absence of disease in the body, but also a complete well-being in mental, physical and social terms. That is, a person is considered healthy only when he can properly fit into his society, interact and maintain healthy relationships.
The social characteristics of a healthy individual are detailed below:
1.Effective Communication Ability:
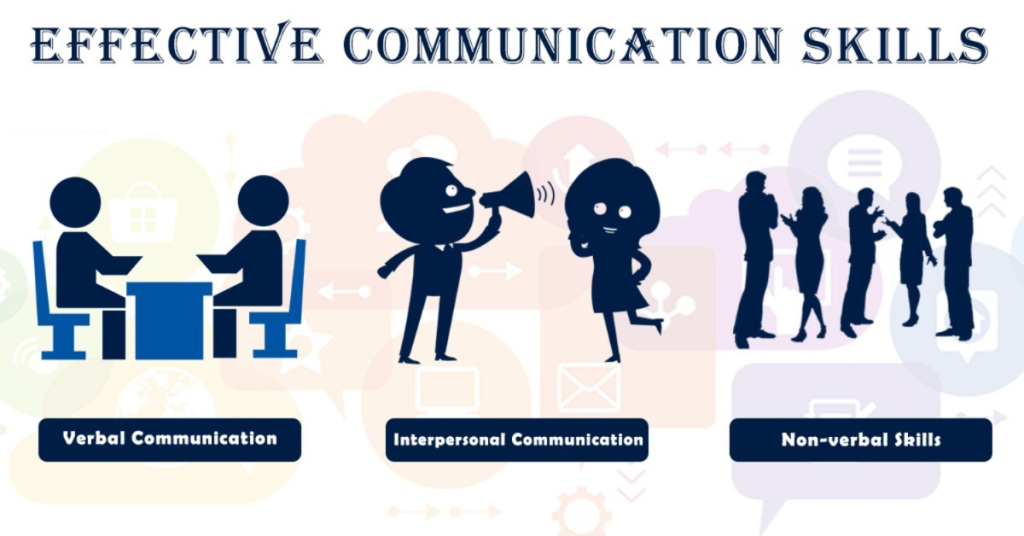
- Effective communication is essential for a healthy person to be socially active. He or she can talk to others openly and clearly. The understanding of words, body language, and expression is also appropriate. This ability increases social engagement and confidence.
2. Empathy and Sensitivity:

- A healthy person can understand the feelings and situations of other people. Being empathetic, they do not impose their views but respond accurately and sympathetically. This feature is essential for both mental and social health.
3. Social Adaptability:
- A healthy person can adapt to all kinds of social situations. He can easily build relationships with people from different backgrounds. Adaptability is a sign of strong emotional intelligence. Social change follows the socialization process and social control.
4. Maintaining Healthy Relationships:

- A healthy person maintains cooperative and healthy relationships with his family, friends, colleagues, society and community etc. It has trust, belief and mutual respect. Adopts a positive approach to avoid quarrels or disputes.
5. Conflict Resolution Skills:

- A healthy person can communicate calmly even in negative situations. Maintains logical and emotional balance to resolve conflicts. Adopts an assertive approach, not aggressive or passive.
6.Teamwork and Cooperation:

- A healthy person can work well in a team. He is cooperative and also respects the ideas of other people. Through this, group efficiency increases. Participation in teamwork demonstrates healthy social behavior.
7. Social Responsibility:

- A healthy individual is aware of his/her social, environmental and moral responsibilities. He/she participates in cleanliness, green initiatives, service activities. Instead of being passive, actively contribute to society.
8. Staying Away from Loneliness or Isolation:
- A healthy person stays socially connected. It avoids loneliness or social isolation, as these two things can lead to depression, stress and poor social health.
9. Social Engagement and Participation:

- A healthy person enthusiastically participates in various social activities: such as family gatherings, festivals, community service, etc. These activities provide him with social support, self-worth and mental well-being.
10. Respectful Behaviour and Tolerance:

- A healthy person is tolerant of other people’s opinions, cultures, religions, and lifestyles. It respects diversity and avoids any kind of discrimination or disrespect.
11. Leadership and Initiative Level:

- A healthy person can step forward and take initiative when needed. He can show his leadership in the group and motivate others.
12.Self-Image and Social Satisfaction:

- A healthy person is satisfied with their identity, their role, and their social status. He does not have a feeling of insecurity or comparison, due to which he can create healthy social interactions.
13.Moral and Ethical Values:
- A socially healthy person has strong moral values, which are seen in their behavior and relationships. He believes in living a responsible life and stays away from unemployment, gambling, lying, etc.
14.Stress Management in Social Context:

- A healthy person can handle social pressure or stress in a positive way. He gives a mature response and can control his emotions, which does not spoil social relationships.
The social characteristics of a healthy individual reflect the quality of his understanding, feelings, behavior and relationships with others. These characteristics are not limited to social health, but can also be linked to physical, mental and emotional health. A healthy social life provides a person with joy, support and self-satisfaction – which ultimately enhances the quality of life.
Spiritual and Cultural Characteristics:
Spiritual and Cultural Characteristics of Healthy Individual:
- A healthy individual is not just healthy in body or mind – spiritual and cultural health are also important parts of that person’s health. The World Health Organization (WHO) defines health as a holistic state, in which there must be a balance between the body, mind, society and spirit.
- Spiritual and cultural health is manifested in a person’s life values, beliefs, customs, religious practices and interaction with society.
- Spiritual and cultural characteristics play an important role in health. One believes in one’s own religion but also respects the religions and beliefs of others.
1.Self-awareness and Inner Peace:
- A healthy person knows their spirit and inner-self. They have confidence within themselves and a clear purpose in life. Spiritual health gives a person emotional stability. Easily manages hormonal balance and neurological functions.
2. Faith and Understanding of Religion:
- A healthy person knows their own religious beliefs, but they also respect the religious sentiments of others. This faith gives a person resilience, hope, and clarity of thoughts, especially during life stress.
3. Moral and Ethical Values:
- Ethical judgment is strong in a spiritually healthy individual. He always makes decisions based on human values - such as honesty, compassion and justice. His behavior also has a positive effect on personal and professional relationships.
4. Spiritual Stress Management:
- A healthy person manages stress naturally through meditation, prayer, yoga, etc. These practices have a positive effect on the limbic system of the brain and reduce cortisol levels – called the stress hormone.
5. Compassion and Spirit of Service:

- A healthy spiritual person is always helpful to others. He has a sense of empathy and selfless service within him. This positive energy also improves mental health in society.
6. Clarity of Life’s Meaning and Purpose:

- A spiritually healthy person lives a “Purpose-Driven Life”. His life is not just for a job or material gain, but for inner growth and contribution to society. This outlook on life keeps a person away from depression and anxiety.
7. Cultural Awareness and Integrity:

- A healthy person respects his/her own culture, language, festivals and traditions. He/she has tolerance and adaptability towards other cultures. Such behavior becomes very necessary in a virtual multicultural society.
8. Spiritual Community Participation:

- A healthy spiritual person participates in religious or spiritual events. By attending Bhajans, Kirtans, Satsangs or religious gatherings, they experience community connection and mental well-being. This way he gets a social support system.
9. Cultural Tolerance and Inclusive Approach:

- A healthy person is tolerant of other religions and cultural beliefs. They do not discriminate based on race, religion, or gender. Such an inclusive approach is mandatory for social peace and coexistence.
10. Spiritual Leadership and Guidance:
- A healthy spiritual individual guides others through their behavior, thinking, and lifestyle. Their life example is helpful to others – especially in tough times.
Spiritual and cultural characteristics are a reflection of the inner state, behavior, and societal contributions of a healthy individual. Such a person not only lives a peaceful life, but also makes others happy and positive.
Spiritual health promotes self-confidence, stress resistance, and the importance of life, while cultural health keeps a person connected to their roots and helps increase sociability.
Mental Characteristics:

Mental Characteristics of Healthy Individual:
- Not only physical health, but mental health is also equally important for a healthy life. According to the World Health Organization (WHO), mental health is a state in which a person realizes his or her own potential, can cope with the stresses of life, can work productively and is able to make a contribution to society.
- Healthy mental characteristics are those characteristics that show how a person’s mind works, and how he or she thinks, feels and relates to himself or herself and others.
1. Emotional Stability:
- A healthy person has control over emotions. He knows how to express emotions like anger, sadness, joy, fear in a healthy way. He does not overreact, nor does he remain passive, he responds accurately.
- Emotional stability indicates healthy communication between the limbic system and the prefrontal cortex of the brain.
2. Adaptability & Coping Skills:

- A healthy individual can cope properly with psychological stress. He can keep his mind stable in conditions like life changes – job, relationships or damage.
- This person has healthy coping mechanisms, such as mindfulness, reasoning, journaling, guided breathing, etc.
3.Self-confidence and self-esteem:
- A person with a healthy mind recognizes his own worth and believes in his capacity. He expresses himself positively and is not afraid to make decisions.
- A healthy self-image is the basis for a person’s personal and professional growth.
4. Realistic Thinking & Insight:
- A healthy mental person has a realistic and neutral view of life situations.
He thinks based on facts and logic and does not get caught up in illusions or myths. - This quality is linked to a person’s Executive Functioning ability, which is managed by the Prefrontal Cortex.
5. Decision-Making Ability:
- A healthy person can make the right and timely decisions even in conditions where there is pressure. It analyzes relevant facts and considers possible outcomes.
- Good decision making shows a clear mind and strong cognitive functions.
6. Social Interaction & Communication Skills:

- A mentally healthy person builds cooperative and positive relationships with others. He can clearly express himself and is willing to listen to others.
- Effective verbal and non-verbal communication is essential for mental health.
7. Memory & Cognitive Ability:
- A person with a healthy mind has good memory, attention, learning and reasoning powers. It has the ability to adopt new ideas and stay focused.
- Cognitive functions are governed by the Frontal Lobe, Hippocampus, and Cerebral Cortex.
8. Mood stability and absence of mood disorders (Stable Mood and Absence of Mood Disorders):
- Mood stability is an important mental characteristic. A healthy person has very few mood ups and downs and stays away from sharp emotions like mood or depression.
- Stable mood means no mood disorders like depression, bipolar disorder, etc.
9.Impulse Control:
- A mentally healthy person can control their desires and immediate reactions. He will not immediately overreact to any situation.
- In this way, a person can channel his negative energy into a positive channel.
10. Sense of Humor and Creativity:
- A healthy brain can maintain laughter and creativity even in conditions of depression. It allows for new ways of thinking and can also take life lightly.
- A healthy sporty approach is important for a person’s overall well-being.
11. Learning Ability & Open-mindedness:
- A healthy person is constantly ready to learn and is open to new things. He also knows how to take criticism and grows from it.
- These traits show mental flexibility.
12.Self-control & Delayed Gratification:

- A healthy person can wait patiently for a desired result and forgo immediate gratification.
- This trait indicates the strong functioning of the person’s Executive Control System.
13.Mental Resilience:
- A healthy mind is capable of recovering even after problems. It moves forward with courage after tough situations.
- Resilience is a major positive indicator of mental health.
Healthy mental characteristics indicate the maturity, stability, and level of a person’s mind. Such 0 characteristics make a person positive, stable and capable not only in today’s time, but in every stage of life.
Other mental characteristics:
- A mentally healthy person is well adjusted to himself and to society.
- A mentally healthy person is aware of his limits, he knows his strengths and weaknesses.
- He maintains balance in all aspects of life, work and behavior. He is responsible for his actions.
- They have the ability to bear the strain and stress of life and have the ability to adjust according to the situation.
- They are free from mental conflicts and tension.
- A mentally healthy person is satisfied with his job and occupation.
- They do not live in fantasy but in the reality of the world.
- They have good social relations with the people of the society. Maintains relationships.
- A mentally healthy person can solve all the tasks that come in life in a natural and mature manner without any problems.
- A mentally healthy person has self-confidence, self-identity and a strong sense of self-esteem.
- He can think for himself and has the ability to make his own decisions.
- Has the ability to provide and receive love Has a variety of interests and lives a well-balanced life between work, rest and recreation. Has the ability to solve the demands of life. and the ability to solve problems.
- A mentally healthy person behaves in a responsible manner and can clearly express his feelings and thoughts.
- A mentally healthy person can adjust to new situations with minimal discomfort.

Health Assessment :

- Health assessment is essential for decision-making, planning, implementation and evaluation of health and community services. Health assessment is a regular and continuous process. Health assessment is an important tool for assessing the health status of individuals, communities and nations. Many aspects are included in the health assessment.
Advantages:

- Health assessment provides knowledge of the health status of individuals, families, and communities.
- Health assessment helps identify health problems in a community and provides information to prepare a plan.
- Health assessment provides an opportunity to interact directly with people of different age groups in the community. is.
- Helps to develop good relations in the community.
- Health assessment helps in early diagnosis of diseases and disorders.
- Helps in identifying health problems of the community.
- Provides information for preparing a plan.
- It is also helpful in providing education in the community and providing protection against diseases.
Components of health assessment:
A health assessment typically involves two components.
1) History Tacking
2) Physical Examination
1) History Tacking :

- Patient’s faith and fear, attitude towards health, pre-treatment History taking is essential for getting a prescription and treatment. History taking is a tool for collecting information about a person, their family, socioeconomic background and nutrition, previous diseases, accidents and present illnesses etc.
- History taking is a tool for collecting information about a person, their family, socioeconomic background, nutrition status, previous medical and surgical history and present complaints. History taking is helpful in obtaining information about a person’s previous health status and present problems. Collecting history can help gain patient confidence and establish rapport.
Importance of history taking in health assessment ( Importance of history taking in health association ):
- History taking plays a vital role in health assessment in any age group, hence it is desirable that the community health nurse should be aware of the different aspects of history collection.
Classification of Histories:
(I) Complete history:
- This type of history is taken at the time of the first meeting, in which the nurse and the patient assess the health problems and take steps to solve them. is.
(ii) Inventory history:
- Here the complete history is collected over more than one session or meeting.
(iii) Problem Focused history :
- This type of history is helpful for immediate assessment and immediate action.
(iv) Interim history:
- This type of history is useful for obtaining information about problems and needs that have arisen since the last meeting. It is actually a need based history.
Responsibilities of Community health nurse in History tacking:

- Introduce yourself to the person.
- Address the patient respectfully.
- Keep the patient in a comfortable condition.
- Sit close to the patient when talking to them. (Furniture should not become a barrier between the nurse and the patient).
- Try to listen more, give minimum directions.
- Solve and formulate present problems.
- Collect information about personal, family, previous treatment, emotional aspects and social background.
- Do not ignore any experience of the patient.
- Remember that someone’s life may be contrary to your beliefs.
- Concentrate on the patient’s main complaint (there may be more than one).
- Be mindful of the patient’s confidentiality, secrecy, and privacy.
- Do not hesitate to ask essential questions (asking questions to know the history is not a sin or a crime, always remember this concept).
- Do not criticize any habit or attitude of the patient (being a judge is not part of collecting history).
- Use language that the patient can understand.
- Be tolerant while collecting history from the patient. (Do not show haste/impatience/intolerance).
Component of history/ Structure of history:
- Personal and Social History
- Family History
- Past Medical History ( Past medical history )
- Present illness ( Present illness )
- Chief Complaint ( Chief Complaint )
Component of history / Structure of history ( Component of history / Structure of history ) :
Personal and Social History:
- It includes…
- Name ( Name )
- Sex ( Sex )
- Age ( Age )
- Address and Phone no. ( Address and Phone no. )
- Education ( Education )
- Occupation: Type of work, Duration of Employment and hours of work
- Monthly income
- Religion
- Habits: Rest, sleep, recreation etc. ( Rest , Sleep and Recreation etc)
- Nutritional Status ( Nutritional Status )
- Marital Status ( Marrital Status )
- Number of Family Members ( Number of Family Members )
- History of taking drugs, alcohol or Smoking etc… urinary and bowel Activity, Sexual Activity ( History of tacking drugs, alcohol or Smoking etc… urinary and bowel Activity, Sexual Activity ).
Family history:

- Type of family
- Number of members in the family
- Any significant illness in the family
- Health history of the family members
- Family income
Past medical history:

- Any illness in the Childhood
- Immunization
- H/O Allergy
- Medical illness in the past
- Serious Accident and Injury
Surgical History :

- Any Operation, Hospitalization if any, History of Blood Transfusion
Present illness:
Onset of Disease (Onset of Disease), its Duration ( it’s Duration ), Symptoms and location (Symptoms and location ), Precipitating Factors Associated Symptoms (Precipitating Factors Associated Symptoms ), Treatment tacken (Treatment tacken ), Current medication and its prescription (Current medication and it’s preparation ), Side effects of medication if any (Side effects of medication if any)
Chief Complaint (Chief Complaint ) :

Present Complaint, Onset, Duration Medication
Physical Examination:
- Physical examination involves (1) inspection (2) palpation (3) auscultation (4) percussion (5) observation of general appearance.
- It is essential to obtain the patient’s cooperation for physical examination.
- In the case of a child, the mother should be assured before collecting facts. Physical examination for health assessment should include the following points:
- Measuring weight and height
- Taking temperature, pulse, respiration, blood pressure and pulse oximetry.
- Examining physical and mental development.
- Assessment of the individual’s appearance, general figure, shape, color.
- Head to toe examination.
- Physical examination and history collection, both of these activities can be done at the same time.
General Survey:

General survey includes the client’s general appearance, age, sex, gait, body movement, body type, personal hygiene, speech, dressing mood and manner.
Vital Sign: In this, temperature, pulse, respiration and blood pressure are checked.
Height and weight: In this, height and weight are recorded.
Physical Examination: A physical examination of all structures, organs and body systems is done.
Preparation For Physical Examination:
- Prepare all required equipment such as blood pressure instrument, stethoscope, tongue depressor, clinical thermometer, knee hammer, needle and pin, salt, sugar, hot and cold water, etc…
- Prepare the examination table with clean top and bottom sheets.
- Provide a screen to the examination table to provide privacy.
- Your Provide an introduction to the client.
- Provide the patient with a comfortable environment free from distractions and disturbances.
- Properly lit for observation.
- Explain the purpose of the physical examination to the client.
- Provide education to the client to empty the bladder before starting the physical examination.
- Properly warm the hands before starting the physical examination.
- Properly record the client’s height and weight.
- Properly and comfortably lay the client down on the examination table.
- Properly record the client’s temperature, pulse, respiration, and blood pressure.
- Cover the patient with a top sheet and Expose only the part to be examined.
- Maintain the patient’s dignity and privacy.
- Avoid unnecessary touching and handling.
- Be polite and gentle when performing a physical examination.
- Carefully examine sensitive areas such as the breasts and genital area.
Techniques of Physical Examination:
Physical Assessment Four basic techniques are used.
Physical examination is a detailed inspection or detailed study of the physical and psychological condition of the patient.
1.Inspection
2.Palpation
3.Percussion
4.Auscultation (Auscultation)
1.Inspection:

- In this method, the general condition of the patient is known from the observation of his body, meaning that in this, the general appearance of the patient is seen, what is the color of the patient’s skin, whether there is any rash on the skin or not, or if there is a deformity anywhere in the body, it is examined, the patient’s diet history is taken, during the inspection, the doctor listens to all the complaints of the patient and a history is written accordingly. Thus, through the inspection, the patient’s history of illness, current complaints and body functions can be known.
2. Palpation:

- That is, to examine by putting your hands on the body, the act of examining the body parts by feeling them. Fingers are used for palpation, which helps to know the size and position of the organ. In addition, this exam is done when there is any tumor in the neck or tenderness is felt in the armpit or groin.
3. Percussion:

- Percussion involves placing fingers on the patient’s body parts and tapping on them. Through tapping, the sound of the internal organs is observed by listening to it, which gives an idea of the condition of the internal organs. Whether the patient’s bladder is full or empty can be known through percussion. In addition, examination can be done on the chest, abdominal and back parts through percussion.
4. Auscultation:

In this, the patient’s body is examined with a stethoscope or fetoscope. The sound inside the body is heard. This method is used to listen to the sound of the chest, listen to the heart rate, and take blood pressure.
Special Equipment: Certain types of examinations are performed using special equipment, for example, otoscope, ophthalmoscope, speculum scope, X-ray sonography, etc.
Sequence ( Sequence ):
General Overview ( General overview ) :

These include general appearance, build, gait, coordination, balance, mental status, height, weight, cognition, vital signs, temperature, pulse, respiration, and Blood pressure is recorded.
Skin ( Skin ): The visible surface of the skin is inspected and palpated.
The nails and hair are inspected.
If there are any lesions, they are evaluated.
Head ( Head ): It involves inspection and palpation of the cranium, eyes, ears, nose, sinuses, mouth and throat.
Neck (Neck): It involves inspection and palpation of the thyroid gland, lymph nodes, carotid pulses and jugular veins.
Back (Back): It involves the symmetry of the back, spinal alignment, scoliosis, lordosis, costovertebral angle, Tenderness, mobility of the spine are inspected and palpated.
Anterior trunk: Inspect the breast and palpate for any lumps and nodules.
Auscultate breath sounds, heart sounds, apical pulse, and palpate carotid pulse, brachial pulse.
Abdomen: Check the color, counter and diaphragmatic movement in the abdomen. Inspect.
The abdomen is palpated to assess for any tenderness, lumps, and the liver, spleen, inguinal nodes, and femoral pulse are also palpated.
Musculoskeletal system: It includes gait, posture, weight bearing, and extremities in the ankles. It includes upper and lower extremities inspected and palpated. Muscle tone, wasting of muscles, symmetry, range of motion of the lower extremities and edema are checked. The popliteal, dorsalis pedis and posterior popliteal arteries are palpated.
Neurological System:
Reflexes such as biceps, triceps, brachioradialis, patellar, Achilles and calf and plantar reflexes are tested.
Balance and fine motor movement are tested.
Cranial nerves and sensory perception are tested.
It assesses color, warmth, strength, range of motion, gait, and gross motor movement.
Genitourinary System:
Any changes to the external genitalia Discharge, growth and any abnormalities are examined.
If necessary, rectal examination, vaginal examination and prostate examination are performed.
Health Assessment of Infant:

Children who are below one year of age are called infants. The infant’s health history and important information is collected from the mother. In the absence of the mother, all this information is collected from the infant’s care taker. The following points are described in the health assessment of the infant.

Personal data ( Personal data ) :
- It assesses the child’s name, age and parents’ name, address and telephone number.
Past health history:
- It assesses the child’s general health and strength.
- The mother’s health is assessed before and during pregnancy.
- The mother’s age is assessed.
- The mother’s use of prescribed or non-prescribed drugs during pregnancy is assessed. Smoking, illegal drugs, alcohol, etc. are assessed. It assesses whether the pregnancy is planned, normal, or high risk.
- It assesses whether there are any complications during the pregnancy.
- It assesses whether there are any illnesses.
- It assesses whether there is exposure to toxins, chemicals, radiation, and other hazards.
- The gestational period at the time of delivery, the place of birth is hospital delivery and home delivery.
- Type of delivery: Spontaneous vaginal delivery or operative delivery such as forceps or cesarean section.
- Apgar score
- Birthweight, length, head and chest circumference of the baby, to see if there are any complications.
Neonatal history:
- Condition of the baby at the time of birth.
- If oxygen, ventilator and incubator care are provided. Gestational Age, assess for congenital abnormalities.
- Problem: Feeding, respiratory distress and jaundice.
- Age at the time of discharge from the hospital.
- No weight at the time of discharge from the hospital.
- First month of life: Family adaptation
Feeding History:
- Breastfeeding, Duration, Supplement Started, Type, Amount, Weight Gain, Age Started Solid Food, Start, Food No Type, Infant Response to the Food, Parent Response to Their Infant, Weaning, Food Preference, Current Feeding, Type, Schedule.
Developmental History:
- Height and weight at different ages, head, rolled, back to stomach and back, sitting with support and without support, walking with support and without support, speaking words.
- Eruption of first tooth.
Health Assessment of pre – school child:

- Pre-school going age is the age between 1 and 4 years. This period is a period of intense growth and development. During this period, children (Children) are more likely to suffer from malnutrition, infection, diarrhea and dehydration.
- Immunization is almost complete during this period.
The discussion of health assessment of a pre-school going child is done under the following steps:
1. Past medical history of the child
2. Personal and family history of the child
3. Child’s Growth and development related various health check up.
4. Child’s immunization status.
5. Child’s nutritional level and his eating habits (dietary pattern)
6. Present condition of child’s health and his major health problems.
7. Child’s head to toe physical examination and review of his body system.
1) Personal data ( Personal data ):
- Name ( Name ),
- Sex and age,
- Whether the child is studying in a crèche or a sports school, the name, address and telephone number of the parents.
- How long is the stay in the crèche/play school? (What is the duration of stay at Crech / Play way school).
- Weather the child like to attend Play way school or not.
2) Past medical history:
- Child’s general health and strength.
- Any history of communicable disease or accident and hospitalization for any reason.
- If the child has been hospitalized, what was the reason and duration of hospitalization and treatment?
- Assess the child’s reaction to the illness and hospitalization.
- Type of family
- Number of members in the family
- Any significant illness in the family
- Socioeconomic Status of the Family
- Number of children in the family ( Number of Children in the Family )
3) Family history:
4) Immunization history:
- It can be recorded from the child’s immunization card. Whether the child has been immunized against all vaccine-preventable diseases.
5) Nutritional / Dietic history:
- At what age does a child start eating normal food?
- At what interval and what foods are given to the child. Does this food fulfill the nutritional requirements of the child?
- What type of food is prepared for the child?
- Ability to self-feed.
- History of any type of food allergy.
- Weight gain.
6) Developmental history:
- History of weight and height at different ages, head, chest and mid-arm circumference at different ages.
- At what age does the child start walking, speak one word, speak two word sentences, use the toilet?
- Dresses himself, gets dressed with help, starts running, climbs stairs, engages in solitary play Stayed, walked, descended stairs with alternate feet, followed commands.
- Recognize color and slip patterns.
- Habit – Nail biting, thumb sucking
7) Present Condition of Health and Major Health Problems:
- Child’s General Appearance
- Level of Nutrition
- Child’s Complaint
- The time of onset of the parent’s complaint about the child’s health is noted.
8) Physical Examination (Physical Examination):
General appearance, weight, height, temperament, as well as level of intelligence are noted, recording of vital signs.
Whether the child is oriented to time, place and person or not, and whether he gives immediate answers to questions.
Speech, mental status and gait, coordination and balance are noted.
Head and scalp are noted for dandruff Come.
Note pediculosis, color and texture of hair.
Eyes: Any infection, discharge, and eyesite.
Nose: Rhinitis or deviated nasal septum.
Mouth: Note tongue and buccal mucosa.
Teeth: Any Also assess for carries and malocclusion.
Throat: Inspect for adenoids and enlarged tonsils.
Ear: Assess for any discharge present.
Neck: Palpate lymph nodes and assess for any abnormalities.
Back: Note symmetry, spinal alignment To do.
Anterior trunk: Note rickets, heart sounds, lung sounds, and assess for enlarged abdomen and any abnormalities.
Musculoskeletal System: Inspect gait and posture, knock knee, and evidence of rickets, note bowel and bladder habits, make provisional diagnosis based on history and physical examination to plan care.
Health Assessment of School Going Child:
Health assessment of school going children is a part of school health services. Apart from community health nurses, teachers and physicians are also involved as they are members of the school health team. The components of the health evaluation of a school going child are:
1) Periodic Check up of children:
Health check up at the time of admission.
Health check up of children every year and more frequent health check up.
Health check-up of children every four years.
Health check-up during school life.
Periodic check-up can be done before the completion of 4 years or even more often. The check-up at the time of admission to school includes measuring height and weight, dental check-up, eye check-up, speech and hearing check-up, detection of worms in the stomach, finding blood and urine and finding out whether the child is suffering from any hitherto unknown disease or disorder.
2) Nutritional Assessment:
- This includes food assessment, food the child receives at home and supplementary meals provided at school.
- This, in turn, gives an idea of the child’s height, weight, appearance, build and nutritional status.
- The food the child receives at home and the supplementary meals at school meet the child’s calorie and nutrient requirements for proper growth and development. If the food provided to the child at home is not sufficient and there is a deficiency of essential nutrition, then the parents are given education to improve the child’s diet at home.
3) Daily Examination:
- Daily examination of the child is conducted by the teacher. For this reason, it is essential that teachers are trained in diagnosing illnesses and providing routine treatment.
- It is important to keep an eye out for colds, coughs, head aches, skin diseases and other infections during daily examinations.
4) Personal and Family History of Children:
- History can be collected through parent-teacher or parent-community health nurse meetings held periodically at the time of admission to school or after, which is desirable for health assessment.
5) Past medical history:
- The child’s past medical history can be obtained from the child or parents.
- Thus, teachers, parents, community health nurses and doctors etc. have a joint responsibility for the health assessment of school going children. Here, it is necessary to clarify that a comprehensive record of all the facts and information collected from the health assessment should be documented in the child’s health card.
Health Assessment of Adolescent:

Adolescent is a young person (he or she) who is in the process of becoming an adult from a child. Children in the age group of 13 to 18 years are called adolescent children. By the age of 18, complete physical development and stability are achieved. According to WHO, the adolescent period from the age of 10-19 years is divided into three stages. Complete physical check-up and history play an important role in the health assessment of an adult person. By this age, complete physical development and stability are achieved.
1.Early Adolescent 10-13 Years
2.Middle Adolescent 14-16 Years
3.Late Adolescent 17-20 Years
Personal Biodata ( Personal Biodata ):
- Name ( Name )
- Age ( Age )
- Sex ( Sex )
- Parents name, address and telephone number ( Parents name, address and telephone number )
- Educational Qualification ( Educational Qualification )
- Hobbies and interests
- Whether the adolescent adult is independent or not, dependent on parents for financial support.
- If independent, employment type and income
- History of taking drugs, tobacco and alcohol etc
- Nutritional Pattern: Appetite, Type of food preferred, fluid intake, interval between meals, quantity of essential nutrients and calorie requirements, exercise and recreation, bowel and bladder habits.
Past medical history:
- History of any medical and surgical disorder.
- Operation,
- Hospitalization,
- Duration of treatment,
Family history:
Type of Family:
- Number of members in the family and their educational qualifications,
- Whether there is any consanguinity in the family.
- Employment status of the family, family income, relationship of parents with each other.
- Adequacy of food, clothing, and transportation, relationship of siblings with each other,
- Sibling Illness
Immunization history:
- Recording the date, time, complete and incomplete of immunization from the health card or immunization card.
Sexual Development:
- Breast development and age of menarche in girls,
- Pubic hair growth and voice changing in boys,
- Social relations with same and opposite gender, curiosity about gender,
- Parents’ Response and Child’s Introduction to Sexuality and Dating.
Social History:
- Sleep Patterns,
- Problems,
- Terrors,
- Speech Clear,
- Stuttering,
- Delight,
- Stress and its Level.
Discipline Used ):
- Type,
- Frequency,
- Effectiveness,
- Attitude,
- Parents’ response to temper tantrums.
- School ( School ): School, Grade, Attendance, Failure, Performance level, problems.
- Social Behaviour: Peers, parents, teachers, type of peer group, level of independence and spiritual practices.
Present Illness:
- In the peer group, they easily fall prey to the habit of alcohol, drugs and smoking which may result in social problems, their personal health Problems and family problems arise.
- They want self-respect and identity in friends and society. They try their best to fulfill the desire for appreciation. If they fail to achieve, they may feel inadequate and lose mental balance, which may result in depression.
- Depression: It can be caused by fatigue, boredom, restlessness, failure to achieve one’s goals, difficulty in concentration. Such conditions require professional help. These health problems are specific to the period of adolescence, which are taken seriously. Professional help, guidance and counseling are required along with the involvement of parents.
Self Esteem Related Problems:
Health Assessment of Adult :

The following steps in the health assessment of an adult Following is the Personal Biodata: Name, Sex, Age, Address and Phone Number. number),
Religion, Nationality, Educational Qualification, types and working hours, Monthly income, Marital status, Age of Spouse, Education and occupation of Spouse, Number of Children and their age.
History of present illness illness):
Chief Complaint,
Onset and its Duration
Location of Symptoms
Treatment tacken and its response
Treatment tacken and its response
Current medication
Past health history:
Childhood illness, date and type of medication or surgical disease, accident, operation, its duration and response to treatment.
Immunization History
Drug, food and any other allergy history.
Family health history:
Type of Family:
Number of members in the family, their educational level, Employment status of family members, family income and any significant illness in the family.
Personal Habits and Living Patterns:
Rest and sleep, how many hours of rest are given, type of sleep sound and disturbed.
Employment ( Employment ) :
Duration, type, working hours and working environment.
Stress ( Stress) :
At home In the family, at the workplace and with relatives and friends.
Exercise:
Nutritional Status:
- Type of food, vegetarian or non-vegetarian, interval between meals.
- Any changes in appetite, special diet for any reason, bowel and bladder habits.
Psychosocial history:
- Client’s relationships with family members, friends, neighbors, coworkers, spouse, religious groups, social and civic organizations in the community.
- Satisfaction with employment, occupation, and household responsibilities.
Physical Examination:
General Overview:
- General Appearance: Healthy or chic looking, nourishment, body type normal, well built, height, weight, personality, gait, balance, speech, mental status, vital signs, temperature, pulse, respiration and blood pressure are recorded.
Examination of Skin:
- Color, rash, dryness, presence of lesions.
- Head: In this, the cranium is inspected and palpated. The scalp and its texture, color, dandruff, pediculosis, etc. are inspected and palpated.
- Eyes: Vision with or without glasses, discharge, infection and any other abnormalities.
- Ears: Discharge capacity is assessed. Nose, mouth, throat and preauricular and postauricular and occipital nodes are palpated.
- Neck: Inspect and palpate.
Thyroid gland:
- Lymph nodes and carotid pulsation and jugular vein are felt and range of motion is checked. is noted.
- It notes symmetry and spinal alignment and assesses scoliosis, lordosis, and mobility.
- In this, the breast is inspected, the chest is watched for expansion, breath sound, heart sound, apical pulse, auscultation is done.
- The axillary gland is palpated.
- The abdomen is assessed for any scar present, then the liver, spleen, inguinal nodes and femoral pulse are palpated. The abdominal cavity is assessed for fluid and bowel sounds are auscultated.
Back:
Anterior trunk ( Anterior trunk ):
Abdomen (Abdomen):
Musculoskeletal System:
- It involves examination of the upper and lower extremities. And the range of motion of the joint is noted and whether any swelling or tenderness is present is also noted.
Neurological System:
- It tests tenderness, color, warmth, strength, range of motion, gait, gross motor movement, reflexes, balance, fine motor movement, cranial nerves, sensory perception.
Genitourinary System:
- The external genitalia are inspected for any discharge or infection.
- A rectal examination is performed if necessary.
- The prostate is examined if necessary. Examination is done.
- If female, vaginal examination and Pap smear test are done.
- A care plan for adults is made based on the history and physical examination.
Health Assessment of Antenatal Women:
- Antenatal health assessment of a woman starts from the time of confirmation of pregnancy.
- Most common antenatal health assessment Objective is the physical and psychological response of a pregnant woman to pregnancy.
Components of Antenatal Assessment:
- Taking Medical History
- Physical Examination
- Laboratory Examination
- Monitoring Growth and Development of Embryo
- Detecting Risk of Pregnancy
1.Tacking Medical History:
Collecting medical history is an important method for data collection.
Attention is provided to the following sections in the antenatal assessment.
( i ) History Regarding Menstrual Cycle
( i ) History Regarding Menstrual Cycle
Regularity of Menstrual Cycle , Flow , Amount and Interval
Complications Regarding Menstrual Cycle
(ii) Obstetrical History
Previous Pregnancy
Date
Experience at the time of Delivery and in the post Delivery period
Age, sex, and birth weight of child born prior to existing pregnancy.
Health condition of former child at present.
Present pregnancy:
Signs and symptoms of planned, unplanned, unwanted pregnancy
Personal and family history:
Social history,
Educational standard of woman and her husband,
Marital and Sexual history,
Occupational standard of the woman and her husband,
Exercise, rest, sleep, food, recreation and elimination related history.
2.Physical Examination:
General Examination
Measuring height and weight
Temperature, Measuring pulse, respiration and blood pressure.
Gynecological Examination:
Breast Examination
Examination of abdomen and palpation
Vaginal Examination if necessary.
3.Laboratory Examination:
According to the physical condition of the pregnant woman, laboratory examinations are performed such as,
Hemoglobin testing,
Blood group and Rh factor,
WBC count and DLC count,
Urine examination (for glucose and albumin) and microscopic Examination, Pap smear test Blood serum examination Stool test Chest X-ray if necessary Ultrasonography
4. Monitoring Growth and Development of fetus:
To check the growth and development of the embryo/fetus in the womb, the pregnant woman should undergo the following You should call the clinic regularly.
Once a month, until the 30th week of pregnancy.
From the 30th to the 36th week, every 15 days.
Then until the pain starts, once every 7 days.
5. Detecting the high risk pregnancy (Detecting the high risk Pregnancy):
- High-risk pregnancies can be assessed based on the following factors:
- Age of the pregnant woman is less than 15 years or more than 30 years.
- Multipara pregnant woman.
- Anemia.
- Malpresentation.
- More than one baby in the womb.
- Preeclampsia and eclampsia.
- Antepartum hemorrhage (APH).
- Early stillbirth, death of baby in the womb, instrumental delivery, cesarean section.
- Longer period of gestation (more than 2 weeks or due date of delivery).
- Hydroamnios.
- Pregnant women who are suffering from heart disease, kidney disease, diabetes, TB etc.
- Pregnant women whose height is less than 140 cms.
Health Assessment of Post Natal Women:
The postnatal period is the period of 6 weeks after the delivery of the baby. During this period, the organs return to their pre-pregnancy stage.
AIMS:
- To provide care to the mother and child and to help the mother achieve optimum health as early as possible.
- To protect the mother and child from complications in the postnatal period.
- To avoid breast engorgement and protect the baby from physiological jaundice and dehydration Assisting mothers to initiate early breastfeeding.
- Providing mothers with personal hygiene, perineum care, breast care and nutritionally related health education.
- Teaching mothers about postnatal exercise.
- Providing family planning services.
- Teaching newborn babies to care.
- During the postnatal health assessment, the health of the mother is assessed along with the health of the baby.
- Main Components of Postnatal Health Assessment:
- Physical Examination
- Laboratory Examination
- To find out Psychological response
Physical Examination:
Objectives of postnatal physical examination:
- To collect data regarding involution of the uterus.
- To assess the needs of the lactating mother For.
- To provide health education.
Physical Examination include:
- General Observation
- Note the mother’s general appearance, posture, and facial expression.
- Recording of vital signs:
- Severing occurs immediately after delivery. Due to this, lots of heat is lost from the mother’s body and the temperature initially falls down. Therefore, provide warmth in this phase.
- The pulse rate also falls down. Therefore, check the blood pressure and if it is low, raise the foot end of the bed. Perform a quick examination to obtain evidence of excessive blood loss. Also take measures of resuscitation in between.
Abdominal Examination:
- After delivery, the uterus becomes hard and contracted. After delivery, the size of the uterus is about 2.5 cm above the umbilicus and then gradually decreases, in which the size of the uterus decreases by 1. 25 to 2.5 cm. If the uterus feels soft, it means that some membranes or pieces of placenta are left inside the uterus. Then, the uterus should be massaged to contract it and, if necessary, removed, and a vaginal examination should be done.
Bladder Examination:
- Watch the abdomen to assess whether the bladder is distended. After the placenta is removed, antidiuretic hormone is released into the blood. This starts diuresis and the bladder feels full. Many times the mother does not feel the urge to pass urine. This can be due to minor injuries or due to bruises to the urethral muscles during delivery of the baby, which causes temporary paralysis of the muscles. Therefore, the mother is encouraged to pass urine. If the mother is unable to pass urine, catheterization is performed. The mother is able to pass urine on her own after a few hours. If the mother is unable to pass urine on her own, encourage the mother to pass urine. A full bladder can result in poor uterine contractions and bleeding from the vagina through open uterine sinuses.
Breast Examination:
- The mother may be exhausted after delivery. Her breasts may become heavy due to lactation. Cleaning the breasts and helping the mother feed the baby. Many times, the nipple cracks, which are painful for the mother, so the mother has problems in feeding the baby best. This crack is treated by applying antiseptic cream to the nipple, but then the nipple is cleaned before feeding the baby. After feeding the baby, the excess milk is expressed and removed, due to which the condition of breast engorgement can be avoided.
Examination of the uterus:
- The uterus is checked for its consistency. The fundal height of the uterus is checked every day to assess the condition of its involution. The size of the uterus decreases by 2.5 cm every day and from the 13th day onwards it is not palpable above the symphysis pubis.
- Examination of Perineum and Vagina: The perineum and vagina are inspected for tar, laceration and episiotomy wound. Decidua forms a layer inside the uterus in 1-2 days. In which the outer layer secretes lochia. It is red for 2-3 days first. Then it changes to pink for 4 to 7 days. And then there is creamy white lochia. The color, quality and smell of lochia are noted. During the postnatal period, the uterus, cervix, vagina and perineum return to their normal tone.
Pelvic Examination:
- Pelvic examination is done after 6 weeks of the baby’s birth, due to which the involution of the pelvic organs can be noted.
Laboratory Examination:
- Blood hemoglobin level is assessed on the third day after delivery and then the puerperium At the end of the period, blood hemoglobin is assessed, urine test is done for routine examination and if necessary, ultrasonography is also done.
Examination of psychological responses:
- Developmental approach
- Acceptance of the Baby
- Caring for a newborn baby
- Providing feeding to the baby.
- Relief from the discomfort of pregnancy, labor pain and delivery.
- Regarding physical and mental strength.
- Establishing a family relationship with the baby.
Dependent Phase:
- For a few days after pregnancy, a woman needs help to take care of the child and also in her own care. How long she remains dependent on others depends on her mental status, will power and physical stamina. Emotional ups and downs can be seen during this period.
Bonding with infants:
- The mother provides love to the baby by holding her baby close to her body. The father and other family members also assist in the care of the baby and get satisfaction by touching and holding the baby.
Adverse Responses:
- If there is an unwanted pregnancy and the child is born due to some compulsion, then the mother shows rejection towards her child. This situation should be handled by providing proper counseling to the mother and all the family members should provide proper counseling to the mother and help her accept her baby.
Health Education:
- When assessing or caring for a postnatal woman, health education should be provided to her on proper rest, sleep, nutrition, personal hygiene, baby care, cord care, eye care, skin care and adequate feeding of the baby.
Postnatal visit ):
- The community health nurse makes multiple visits depending on the type of delivery and the delivery, but in the case of a normal delivery, a minimum of four visits are made.
- The first visit is made within 24 hours of delivery and discharge from the hospital.
- The second visit is made on the third day of delivery when the mother has chances of breast engorgement and this visit is done to assess physiological jaundice in the newborn.
- The third visit is done on the fifth day of delivery and the fourth visit is done after 7 to 10 days, after which the visits are increased according to the requirement. The woman then attends the postnatal clinic with the baby after 6 weeks.
Breast self examination:

INTRODUCTION ( Introduction ):
Breast self examination is done to see if there is any kind of abnormal mass like lump and nodule in the breast.
PURPOSES ( Purpose ):
1) Any To see if there is any kind of abnormality.
2) To detect breast cancer early.
3) To see if there is any kind of abnormality in the breast.
Time (time):
1) Breast self-examination is usually done once a year in normal women.
2) If there is breast cancer, it is done twice a year.
3) It is done once a month during menopause.
4) It is done once a month during the reproductive age.
There are a total of 5 steps for breast self-examination:
1)step:1
Stand in front of the mirror. Then look at the breast to see if there is any abnormality in it such as redness, discharge, abnormal size, inverted nipple, swelling, dimpling, bulging. Thus, see if there is any abnormality in the breast.
Step : 2
In this step, keep your hands behind your head, then bend your head forward with your hands and Look in the mirror to see if the size of the breast is symmetrical.
Step : 3
In this step, place your hands on your waist and then lean forward and see if there is any lump in the breast, its size, symmetry and shape.
Step : 4
- In this step, stand in front of a mirror.
- Then raise your left hand.
- Then palpate the left breast with the first three fingers of your right hand. First of all, palpate in a circular motion.
- Palp it from the outside to the inside.
- Then quiz the nipple.
- See if there is any discharge in it.
- Now palpate the right breast in the same way.
- This step will help you to know if there is any lump in the breast.
Step : 5
- Then squeeze the nipple to see if there is any discharge.
- Thus, through breast self examination, it is known from this step whether there is any abnormality in the breast and if breast cancer is going to occur, it is known at an early stage.
Health Assessment of the Aged Person:

History taking and complete physical check-up are major components in the health assessment of an elderly person. However, attention should be paid to the following factors:
Old age people are prone to more than one health problem. Loneliness, lack of productivity and neglect increase the problem.
Symptoms of disease in old age people cannot be pronounced well.
In most cases, pain complaints may be unbelievable, because their attitude towards the feeling of pain may change.
Old age people may choose to live with the disease, because they believe that there is no cure for it now or they may think that others will ignore them if they complain.
The behavior of family and society towards the elderly person plays an important role in their health assessment.
The behavior of family and society towards the elderly person is their Health assessment plays an important role.
Assessment of Disabilities:
Old people may suffer from physical, mental, social and sexual disabilities or impairments. They may experience problems in moving, sitting and standing, climbing stairs, opening jars or boxes, grasping small objects, reaching for objects above their head level, and maintaining balance, etc.
Similarly, problems may arise for them in cooking, housework, shopping, taking medicine, managing money, and performing daily living activities (going to the toilet, bathing, changing clothes, eating, etc.). This ends the freedom and self-reliance of the old person. They become dependent on others or have to use some assistive devices to help them. Therefore, the elderly need more social protection and support.
Past medical history:
Past medical history is assessed by:
General health and strength,
Youth and childhood diseases (measles, diphtheria, polio, T.B. Jaundice, high blood pressure, diabetes, heart disease etc.)
Surgery and serious accidents
Allergies, emotional level.
Previous treatment.
Personal and Family History:
Here, attention is paid to place of birth, domestic environment, marriage, divorce, socio-economic group, education, cultural background, family condition, interests and various aspects of general life.
To know about any hereditary disease, it is necessary to know the family history. Similarly, it is important to know about sexual behavior, professional conduct, travel, religious beliefs, and financial limitations.
Review of System:
- Although a head-to-toe physical examination is necessary for a correct assessment, it is not necessary to review all systems every time. Through a physical examination, health can be evaluated by examining all the important organs and systems of the body. It should be remembered here that old age is called the home of diseases, so the results of this test help in determining many diseases or health problems.
Present Illness:
- Its assessment may vary from person to person, and there may be one or more reasons for it.
Chief Complain:
- When evaluating the health of the elderly, their chief complaint should be asked so that priority can be determined in the implementation of care. At the end of the health evaluation, the community health nurse should question herself, if any information is missing, then she should ask and get it, and try to collect related information and facts accordingly.
