ENGLISH-GNM-S.Y-PAEDIA-GNC PAPER SOLUTION -31/03/2022 (DONE)-UPLAOD NO.12
Paper Solution (31/03/2022):
Q-1
A. Define “Tetralogy of Fallot” Define ‘Tetralogy of Fallot’.03
Tetralogy of Fallot is a congenital heart defect. In which four heart defects are found together in a child.
1) Ventricular septal defect,
2) Pulmonary stenosis,
3) Overriding aorta,
4) Right ventricular hypertrophy.
••>
1) Ventricular septal defect:
In ventricular septal defect, there is an abnormal opening in the septum separating the right and left ventricles.
2) Pulmonary stenosis:
In pulmonary stenosis, the pulmonary artery (the blood vessel that carries deoxygenated blood from the right ventricle to the lungs) narrows, which obstructs the blood flow from the right ventricle.
3) Overriding aorta aorta):
Overriding of aorta is a condition in which normally the aorta (the main blood vessel that carries oxygenated blood from the heart to the body) originates from the left ventricle of the heart, but in overriding of aorta, the aorta originates directly above the ventricular septal defect on the left ventricle.
4) Right ventricular hypertrophy:
When the pulmonary artery (A blood vessel that carries deoxygenated blood from the right ventricle and delivers blood to the lungs for oxygenation) narrows and stenosis, requiring the right ventricle of the heart to do extra work (pumping) to pump blood from the right ventricle to the lungs. This extra pumping causes the muscles of the right ventricle of the heart to thicken, which is called hypertrophy.
B. Write clinical manifestations of “Tetralogy of Fallot” 04
- Cyanosis,
- Bluish discoloration of lips, skin, and nails,
- Shortness of breath,
- Clubing,
- Fatigue,
- Poor growth ,
- Breathing difficulty,
- Abnormal murmur sound,
- Irritability,
- Dyspnea,
- Episodes of cyanotic spells (tat spells) including cyanosis, hypoxia in the child after feeding and any painful procedure Breathing difficulties,
- Polycythemia,
- The child’s skin becomes cool and clammy.
C. Write difference between acyanotic & cyanotic heart disease. Write the difference between acyanotic and cyanotic heart disease. 05
Difference between Cyanotic and Acyanotic Condition
Introduction :
Congenital Heart Defects are mainly of two types: Cyanotic Condition and Acyanotic Condition. Both the conditions differ according to the level of blood flow and oxygenation in the cardiac field of the patient. The main difference depends on the amount of oxygen in the patient’s blood and the resulting blue color (cyanosis) seen on the skin.
Cyanotic Condition:
Cyanotic condition is a condition in which deoxygenated blood mixes with pure blood inside the patient’s heart and oxygen-depleted blood reaches various parts of the body. This causes a bluish tinge to the patient’s lips, nails, and skin, which is called cyanosis.
In this condition, Right to Left Shunt is usually seen, in which deoxygenated blood from the right side of the heart goes directly to the left side and is pumped through the body.
For example:
Tetralogy of Fallot, Transposition of Great Arteries, Tricuspid Atresia, Total Anomalous Pulmonary Venous Return, etc.
Symptoms:
- Skin, lips, and nails appear blue (cyanosis)
- Oxygen saturation is less than 85%
- Patient tires easily
- Respiratory rate increases
- Growth delay is observed
Acyanotic Condition:
In an acyanotic condition, the patient has abnormal blood flow to the heart but there is no direct effect on the oxygenation of the blood. That is, only oxygenated blood flows in the patient’s body and cyanosis is not observed.
In this condition, a Left to Right Shunt is usually seen, in which oxygenated blood from the left side turns to the right side and returns to the pulmonary circulation.
For example:
Atrial Septal Defect, Ventricular Septal Defect, Patent Ductus Arteriosus, Atrioventricular Canal Defect, etc.
Features:
- No blue discoloration of the skin is visible
- Oxygen saturation is normal (≥ 95%)
- The patient has little respiratory distress
- Symptoms of pulmonary congestion and heart failure are present
- Sometimes a rasp and a throat murmur are heard
The main difference between Cyanotic and Acyanotic Cardiac Conditions is that in Cyanotic, the patient’s body has oxygen-depleted blood circulating in it, causing cyanosis, while in Acyanotic, there is a silent disorder within the heart despite the presence of oxygenated blood. Both types of conditions can be serious for pediatric patients and require immediate medical and surgical intervention. As a nurse, it is a very important responsibility to understand this difference and provide proper monitoring and care to the patient.
D. Describe nursing management of “Tetralogy of Fallot” .08
The nursing management of tetralogy of Fallot is as follows.
- This is a condition of cyanotic heart disease, and special care is needed when cyanosis is seen in a child.
- A hypoxic spell is an episode in which cyanosis develops due to the child not getting enough oxygenated blood. During this time, it is very important to give the baby oxygen therapy, especially the chest position, to remove the oxygen supplement spell. Give the child IV fluid.
- Collect a complete history from the child’s mother and father and decide on a care plan accordingly.
Take anthropometric measurements of the child periodically so that growth failure can be identified in the child. - Keep checking the child’s vital signs at regular intervals so that the child’s condition and oxygen level can be maintained.
- The child’s feeding behavior, his nutritional needs, his intake and output chart, all these things need to be specially monitored and recorded.
- Keep investigating the child’s lab reports from time to time so that information can be obtained about the child’s clinical condition.
- The child’s respiratory system and heart sound should be assessed. So that the problem can be identified early.
- It is necessary to explain the child’s condition and prognosis to his mother and father.
- The child should be prohibited from doing outdoor games and excessive activities and his attention should be diverted to indoor games and games that reduce physical stress.
- The child and his parents will develop fear and anxiety, so psychological counseling is necessary for everyone.
- Chronic Due to the problem, there is a possibility that the child may get repeated infections, so it is especially important to take preventive care of the child.
OR
A. Define “Nephrotic Syndrome” OR “Write the definition of Nephrotic Syndrome.03
Nephrotic syndrome is a combination of two words.
- Nephron Meaning the basic structure of the kidney.
- Syndrome Meaning a group of symptoms.
Nephrotic syndrome in children is a kidney disorder in which Due to damage to the glomeruli, which are the filtering units of the kidneys, or due to an increase in the permeability of the glomeruli, protein is excreted from the body through urine, in which mainly albumin is excreted from the body.
Due to the excretion of protein from the body through this urine, the amount of protein in the blood decreases, which causes swelling in the feet, particularly around the ankles, and in the abdomen, causing a condition called edema. Due to which the lipid and cholesterol levels in the blood also increase.
Nephrotic symptoms are a collection of symptoms that are mainly seen due to damage to the glomeruli in the kidneys.
Nephrotic syndrome mainly has four symptoms.
1) High levels of protein in the urine are excreted from the body (proteinuria).
2) Decreased amount of protein in the blood. (Hypoalbuminemia).
3) Increase in the amount of lipids in the blood (Hyperlipidemia).
4) Swelling in the body part (in the heel).
These four main symptoms are seen in nephrotic syndrome.
Nephrotic syndrome affects people of any age. It is mainly seen in children between the ages of 1 and 7 years.
B. Write causes of Nephrotic Syndrome. Write the causes of nephrotic syndrome.04
- Due to glomerular disease,
- Due to hereditary conditions,
- Certain types of diseases such as cardiovascular disorders, damage to small blood vessels of the kidneys,
- Certain types of disease conditions are more common in children, mainly
- Due to abnormal kidney function,
- Due to diabetic kidney disease,
- Due to certain types of infections,
- Due to medication,
- Focal segmental glomerulosclerosis (FSGS),
- Scattered scarring of Glomeruli,
- Membranous nephropathy,
- Due to heart failure, due to certain diseases such as hepatitis B, hepatitis C, malaria etc.
C. Enlist signs & symptoms of Nephrotic Syndrome. Write the signs and symptoms of nephrotic syndrome.05
- Swelling.
- Weight gain in a child.
- Swelling is mainly seen in the lining of the eye socket and around the eye (in the periorbital area).
- Swelling is mainly seen in the feet and ankles due to prolonged sitting or standing.
- Face puffiness.
- Proteinuria.
- Hypoalbuminemia.
- Hypercholesterolemia.
- Diarrhea.
- Vomiting.
- Liver enlargement.
- Increase in blood pressure.
- Anemia.
- Infection of the respiratory tract, peritoneum, and skin.
- Pale skin.
- Skeletal muscles Wasting.
- Swelling is often seen in the wall body, which is called Anasarka.
- Ascites,
- Pitting edema,
- Oliguria (decreased urine output).
- Weight gain.
- Hematuria (blood in urine.)
- Respiratory distress.
- Increased blood pressure.
- Kidney failure.
- Increase in cholesterol levels in the body.
- Feeling tired.
- Getting an infection immediately.
- Not feeling hungry.
- Feeling tired.
D. Describe nursing management of “Nephrotic Syndrome” Write the nursing management of “Nephrotic Syndrome”.08
- Properly assess the child.
- Monitor the child’s vital signs.
- Monitor the child’s fluid balance.
- Monitor the child’s weight regularly.
- Monitor the child’s intake output chart.
- If the child has a condition of edema, elevate the extremities.
- If the child has a condition of edema, administer diuretic medicine and monitor fluid levels.
- Continuously maintain the child’s nutritional status.
- Advise the child to avoid protein and salt.
- Provide proper medication to the child.
- Provide complete information to the child’s parents about his disease condition, its causes, its symptoms and signs and diagnostic evaluation.
- Advise the child’s parents to maintain personal hygiene to prevent infection.
- Provide emotional support to the child’s parents.
- Maintain proper interpersonal relationship (IPR) with the child’s parents.
- Provide complete education to the child and his family members.
- Clear all doubts of the child and his family members.
- Encourage the child to participate in different play activities.
- Frequently monitor the child’s vital signs To do.
- Provide the child with the medication prescribed properly.
- Continuously monitor the amount of fluid the child is taking or the amount of intravenous fluid the child is being given.
- Provide the child with a nutritious diet.
- Advise the child to take small frequent feedings.
- Provide education to the parents to provide the child with a sodium restricted diet.
- Provide the child with proper supplementary vitamins and iron.
- Advise or follow up regularly with the child’s parents.
Q-2 Write Short Notes. (Any five) (5*5=25)
1.Role of a paediatric health nurse. Role of a paediatric health nurse
In the present times, as the demand for medical surgical and sub-specialties is increasing and new challenges are arising in child health care, the role and responsibility of a paediatric nurse also becomes very challenging. In the present time, it is very important to keep in mind the specific role and responsibility of the nurse to provide special care according to the needs of the child through the use of specialist pediatric nurses and specialized technology.
As a pediatric nurse, it is necessary to work on both aspects of care and cure together. In which care is a continuous process, which is very useful at all times when the child is sick or healthy.
Cure can generally be used in the diagnosis and treatment of the child when he is sick.
As a pediatric nurse, he has to provide care and counseling to the child and his parents in different places like hospital, home, clinic or community. Therefore, the role and responsibilities of a pediatric nurse are highly specialized, as follows.
Caregiver.
When a child is sick and admitted to the hospital, the primary role of a nurse is to provide care to the child. The nurse should act as the primary care giver in every aspect of the child’s care such as treatment, feeding, hygiene, safety, etc.
Child Care Advocate.
Advocacy is a basic requirement for comprehensive family-centered care of the child or family.
In which the nurse acts as an advocate for the child to receive the best possible treatment from the unit and to receive good quality health services based on scientific principles. For this, the nurse works to ensure that the child gets maximum benefit.
Team leader.
The nurse works well with her team members and takes the leadership herself, maintains good communication between everyone and participates in the care of the child. As a team leader, she keeps everyone together and distributes equal responsibility among everyone. She also gives everyone equal opportunities and is always ready to solve any problem.
Educator and Managerial Role.
The nurse provides education to the child and his parents on every aspect during the treatment of the child. They participate in the care of the child by providing health education on issues such as nutrition, immunization, medication, personal hygiene, etc.
In addition, the nurse manages every activity in the pediatric ward and hospital and maintains coordination and management between all.
Counselor.
A nurse works with children as a good counselor. The nurse helps the child and his parents to make the right decisions and provides counseling for critical condition decisions.
Recreationist.
The nurse provides different types of activities to the child during his hospitalization. Which activities reduce the child’s anxiety and help him to divert his mind and adjust to the hospitalized environment.
Researcher.
In today’s modern times, many changes are coming in the health care facility. In which as a pediatric nurse, he participates in many research projects. Research provides new concepts for better treatment plans and health care facilities for children. Many technological advancements can also be implemented in health care through research.
2.Difference between Kwashiorkor & Marasmus – Difference between Kwashiorkor and Marasmus
(This question should be written on both sides like the difference, here for the sake of simplicity it is given in both lines which should be taken into consideration. And in each line, information about Kwashiorkor is given first and then about Marasmus is given.)
- Kwasiorkor is mainly caused by protein deficiency while marasmus is caused by both protein and calorie deficiency.
- Kwasiorkor is usually seen in children between six months and three years of age… Marasmus is usually seen in children under one year of age.
- Kwasiorkor does not show any loss of subcutaneous fat. Marasmus shows loss of subcutaneous fat.
- Kwasiorkor Swelling is seen in the body.. In marasmus, swelling is not seen in the body..
- In kwashiorkor, the part of the child’s ribs is not seen very prominent.. In marasmus, the part of the ribs is seen prominent..
- In kwashiorkor, the child is seen lethargic… In marasmus, the child is seen alert and irritable..
- In kwashiorkor, muscle wasting is not seen in the child or it is seen normal… In this, severe wasting is seen in the child’s muscles..
- In this case, the child’s appetite is seen to be low… In this case, the child’s appetite is high and the child eats well as soon as he is fed.
- In this case, the child’s face is seen to be moon-shaped… In this case, the child’s face is seen to be monkey-shaped.
- In this case, the child’s hair changes are seen to be gray or red in color… In this case, the child’s hair changes are not seen much.
- In this condition, when the child is given adequate amount of protein, the child’s condition often improves… In this, the child’s condition improves quickly by providing the child with an adequate amount of protein as well as carbohydrates and fats.
3.Megacolon – Megacolon
Megacolon is a type of congenital anomaly of the gastrointestinal system. It is also known as Hirschsprung’s disease. Hirschsprung’s disease is also called “megacolon” and “congenital aganglionic megacolon”. Hirschsprung’s disease is usually caused by the congenital absence of parasympathetic ganglionic nerve cells in both the mucosal and submucosal layers of the distal colon and rectum, resulting in extreme dilatation of the colon. Hirschsprung’s disease is of variable length and sometimes involves the colon wall. This disease mainly involves the rectosigmoid colon.
Etiology/cause of the Megacolon:
- Due to ganglionic nerve damage in a part of the colon.
- Due to chronic constipation.
- Due to narrowing of the rectum.
- Due to the absence of parasympathetic ganglionic nerve cells in the rectum and colon.
Clinical manifestation/ Sign and symptoms of the Megacolon ( Signs and symptoms of Megacolon):
- Delayed passage of meconium (stool).
- Vomiting (with bile or fecal matter).
- Diarrhea.
- Dehydration.
- Failure to thrive.
- Abdominal distension.
- Chronic constipation.
- Anorexia.
- Visible peristalsis on the abdominal wall.
- Superficial veins visible.
- Abdominal discomfort and irritability.
- Child passes ribbon-like, fluid-like stool.
- Gross malnutrition and failure to grow.
- Malnutrition.
- Anemia.
Diagnostic evaluation of the Megacolon:
- History tacking and physical examination.
- Rectal examination.
- Barium enema.
- Rectal biopsy.
- Barium enema.
- Anorectal manometry.
- Genetic testing.
Management of the Megacolon:
- Megacolon Management involves surgical removal of the aganglionic, non-functioning, and dilated segments of the colon followed by end-to-end anastomosis to maintain the function of the internal sphincter of the rectum and the continuity of the rectum.
Initially, after the diagnosis is confirmed, a colostomy or ileostomy is performed to divert fecal materials. - Swenson’s operation
Swenson’s operation is a surgical technique named after the American surgeon Orver Swenson. In this procedure, the affected part of the colon or the part in which ganglionic cells are absent is removed. The healthy portion of the colon is then reconnected to the anus. This procedure bypasses the affected area, allowing normal stool flow. - Abdominoperitoneal pull through
Abdominoperitoneal pull through is also called the “Soave” and “Duhamel procedure”. This is another surgical procedure used to treat Hirschsprung’s disease. In this procedure, the affected portion of the colon is removed and then the healthy portion of the colon is anastomosised with the anus, making the colon patent. - The optimal age for this operation is six to eight months after the temporary conformal. Then it is done after the age of 12 to 15 months of the child when the child’s weight is 7 to 9 kg.
- In older children whose symptoms are not severe, management in this condition should include repeated enemas with isotonic saline and stool softeners.
- Properly provide intravenous fluids to the child.
- Aspiration of the child through a nasogastric tube.
- Properly providing antibiotic medication to the child.
Nursing management of the Hirschsprungs Disease. (Nursing Management of Hirschsprung’s Disease)
Preoperative Nursing Care
- Provide the child with proper antibiotic medicine.
- Provide the child with rectal wash with less than 300 ml of normal saline.
- Note the frequency and type of the child’s stool.
- Avoiding temperature from the child’s rectal area can prevent injury.
- Maintaining the child’s nutritional level.
Post-operative nursing care
- Properly assess the child’s vital signs.
- Provide general post-operative care to the child.
- Advise the child to maintain proper aseptic technique at the surgical site.
- Dress the child with proper aseptic technique.
- Properly Advise on careful handwashing.
- Properly assess the child’s surgical site.
- Regularly check colostomy function.
- Properly assess the child for any other complications.
- Provide proper skincare to the child.
- As per the prescription Change the dressing regularly.
- Advise the child to properly apply zinc paste to the surgical site.
- Advise the child to maintain proper hygiene and cleanliness at the surgical site.
- Regularly assess the function of the colostomy.
- Provide the child with prescribed medications regularly.
- Advise the child to follow up regularly.
4.Factors affecting on growth & development – Factors affecting on growth & development
Growth
Growth is the physical maturation in which the size and shape of the various organs of the body increase. Which is seen due to the multiplication of cells and increase in intracellular substance. The change in growth can be measured in centimeters and kilograms.
Development
Development is the process in which the body matures functionally and physiologically. In development, there is an increase in the capacity to perform skills and functions. In which psychological, emotional and social changes take place. It is difficult to measure development but it can be measured.
Factors affecting growth and development:
Some factors that promote or inhibit the process of growth. There are two factors. Environmental Factors
Hereditary Factors
Hereditary Factors
- Genetic Factors are important factors that affect a child’s growth and development. They affect height, body structure, skin color, eyes, and hair.
- Which depends on the genes of the parents. If the height of the parents is high, then the height of their child will also be high, if the parents are highly intelligent, then their child will also become highly intelligent, like some factors that affect the child.
- Some genetic diseases that affect the growth and development of the child such as thalassemia, hemophilia.
- So the child also has a chromosomal abnormality along with that disease, in which Down is seen.
- In addition to this, gender also affects the growth and development of the child. While male babies are heavier and longer than female babies, girls mature earlier than boys. But their height and weight are less compared to boys.
- In race and nationality, different races also grow and develop at different times and their physical characteristics differ from national group to national group.
Environmental Factors:
Prenatal Factors
Intra-uterine environment affects fetal growth and development
Maternal malnutrition
If the mother does not take a proper diet during pregnancy and is anemic, then intra-uterine growth retardation, low birth weight, preterm baby and disturbances in growth and development occur in later life.
Maternal Infection
Some intrauterine infections such as HIV, hepatitis are transmitted to the fetus through the placenta and affect its growth and development. Due to which congenital anomalies and congenital infections are seen.
Maternal Substance Abuse
Some teratogenic drugs, when taken during pregnancy, can cause congenital malformations, and smoking, tobacco, and alcohol also affect growth and development.
Maternal Illness
Conditions like hypertension, anemia, heart disease, hypothyroidism, diabetes, chronic renal failure, hyper pyrexia etc. which affect the growth of the fetus. If iodine deficiency is found in the mother, then the baby may suffer from mental retardation.
Miscellaneous
Prenatal conditions that affect the growth of the fetus. Which affect the growth and development of the fetus, such as uterine malformation, malposition of the fetus, bicornuate uterus, oligohydroamnios, polyhydramnios, etc.
Postnatal Environmental Factors:
Growth Pattern
Growth pattern is according to the size of the baby at birth. If the baby has a low birth weight, complications may occur later.
Nutrition
Nutrition is very important for the growth and development of the child. It should be quality and quantitative nutrition. It should contain protein, carbohydrates, vitamins, fats and minerals in sufficient quantities which help in the growth and development of the child. If the child is well nourished then physical and mental growth is seen to be good.
Childhood Illness
Heart disease, kidney, liver malignancy, digestive disorders, metabolic disorders like those affect the growth and development of the child.
Physical Environment:
Environmental conditions like housing, its living conditions, environmental sanitation, ventilation, fresh air, hygiene, safe water supply are essential for growth and Development
affects.
Psychological Environment:
A good psychological environment such as a healthy family, a good relationship between the child and the parents, and healthy interactions with other family members help in emotional, social, and intellectual development. If a child does not get the proper love, affection, and security, he or she may become emotionally disturbed.
Cultural Influence
Culture affects growth and development. According to the culture, its food habits, its beliefs, its living standard, education level, etc. affect growth and development.
Socioeconomic Status
Due to poor socio-economic status, the child cannot grow and develop properly and cannot get a proper nutritional diet.
Climate and Season.
Climate and season affect growth. Weight gain occurs in summer. Height increases in spring season compared to rainy season.
Play and Exercise
Play and exercise increase physiological activity and muscular development, as well as physiological, social, moral, intellectual development and health improves due to physical exercise.
Intelligence
Which affects mental and social development. If the child has high intelligence, he will be able to adapt to the environment. If he has low intelligence, he will not be able to adapt.
Hormonal Influence
Hormones greatly affect the growth and development of the child. Due to imbalance in them, problems are seen in growth and development.
5.Juvenile delinquency – Juvenile Delinquency
Juvenile delinquency is one of the most common problems of society. ‘Juvenile’ means childhood and ‘delinquency’ means antisocial behavior or criminal behavior
Juvenile delinquency is a type of criminal act that is usually committed by children and teenagers who are below 18 years of age. Juvenile delinquency is illegal or antisocial repetitive behavior by a child, usually committed by individuals under the age of 18. This juvenile delinquency can range from relatively minor crimes such as vandalism, shoplifting to more serious crimes including assault, drug offenses, and property crimes. This juvenile delinquency behavior involves lying, stealing, stealing from home, running away from school, running away from home, disobeying someone, fighting, looting, sexual assault, etc.
Etiology/cause of the Juvenile Deliquency:
- Due to family dynamics such as,
- Hereditary,
- Due to chromosomal defects
- Due to parental conflict,
- Due to death,
- Abuse,
- Due to neglect of the child,
- Due to low parental supervision,
- Due to poor parent-child relationship,
- Due to peer group influence
- Such as,
- Due to influence of delinquent peer group,
- Due to socio-economic factors such as,
- Due to low socio-economic condition,
- Due to low income,
- Due to poverty,
- Due to unemployment,
- Due to inadequate housing conditions,
- Due to lack of education,
- Due to community environment such as,
- Due to availability of drugs,
- Criminal neighborhood Due to,
- Unsatisfactory conditions in schools and colleges such as,
- Inadequate recreational facilities,
- Improper teacher student relationship,
- Academic failure,
- Substance abuse such as,
- Due to alcohol,
- Due to taking drugs
Clinical manifestation/ sign and symptoms of the Juvenile Deliquency:
1) Behavioral problems such as,
Theft,
Vandalism,
Alcohol abuse,
Mass killing and assault,
Hooliganism,
Damage To do
2) School Difficulties
Academic Struggle,
Poor Performance in School,
Running Away from School,
Being Indisciplined in School,
Conflicts Between Teacher and Friends.
3) Peer Relationships
Peer Rejection,
Social Isolation,
Difficulty Forming Relationships with Peer Groups,
4) Family Conflict
Parent Child Relationship impairment,
Less parental supervision,
Less parental support,
5) Emotional disturbances
Depression,
Anxiety,
Anger,
Impulsive behavior,
6) Substance abuse
Alcohol use,
Drug use,
7) Legal issues
Involvement in Criminal Activities.
Diagnostic Evaluation of the Juvenile Delinquency:
- Legal History,
- Family Assessment,
- Social and Environmental Factors Assessment,
- Psychological Assessment,
- Substance Abuse Assessment,
- Educational Assessment.
Management of the Juvenile Deliquency:
- Proper Education to Prevent Child from Delinquency Provide.
- To take early intervention against the child to prevent him from doing any illegal activity.
- To provide proper cognitive behavioral therapy to the child.
- To give advice to the child’s family members or to provide proper love and affection to the child.
- The atmosphere of the child’s school and college should be familiar so as to prevent the child from doing illegal activities. Can be done.
- Advise the child’s teachers to work properly with their students and provide a comfortable environment.
- Advise the child to provide a healthy family environment.
- Advise the child’s parents and caregivers to provide the child with proper love and affection from the family.
- Advise the child’s parents to fulfill the child’s basic needs Provide.
- Provide proper educational opportunities to the child.
- Advise the child to do proper exercise, sports, and recreational activities.
- Provide proper counseling and guidance to the child.
- Provide proper work and a comfortable environment to the child.
- Provide proper psychological support to the child.
- Provide complete education to the child about social and anti-social behavior and legal and illegal behavior.
6.Enuresis – Enuresis
Enuresis is a common pediatric problem in which the child experiences frequent involuntary urination while sleeping. When The condition of frequent involuntary urination during sleep, when voluntary urine control should normally be achieved, is called enuresis. And this condition is seen in a child even after 5 years.
Enuresis (bedwetting) is also called nighttime incontinence.
Etiology/ cause of the Enuresis:
- Because the bladder is small,
- Because of hormonal imbalance,
- Because of urinary tract infection,
- Because of diabetes,
- Because of chronic constipation,
- In the urinary tract Due to structural problems,
- Due to delayed bladder maturation,
- Due to genetic predisposition,
- Due to impaired production of antidiuretic hormone (ADH),
- Due to overactive bladder muscles,
- Due to psychological factors,
- Due to family conflict,
- Due to property adjustment.
- Due to very strict parents.
- Due to neuromuscular bladder function alteration,
- Due to neurological deficit,
- Genitourinary Due to urinary infection,
- Due to anatomical defect,
- Because of toilet training being improper,
- Because of parent child relationship being impeded,
- Because of child being mentally disturbed
types of the Enuresis:
There are a total of two types of enuresis.
1) Primary Enuresis
2) Secondary Enuresis
1) Primary Enuresis
When a child has never achieved normal bladder control due to any organic cause and develops a condition of bedwetting, it is called primary enuresis.
In primary and persistent enuresis, when the neurological maturation of the child’s urinary bladder control is delayed, it is called primary enuresis.
2) Secondary enuresis
Secondary enuresis is when a child has been bedwetting for a few months. Bladder control has been achieved but when the child’s bladder control is impaired again due to any stressful environment such as illness, hospitalization, family conflict, separation of parents and night time bed wetting, it is called secondary enuresis.
Clinical manifestation/sign and symptoms of the child with Enuresis. Symptoms and signs of a child with enuresis:
- Involuntary urination during sleep,
- Increased frequency of urination,
- Nocturnal enuresis,
- Psychological impact
- Self Low self-esteem, embarrassment,
- Social withdrawal,
- Frustration,
- Impairment of the child’s daily routine activities,
- Passing urine even during the day.
Diagnostic evaluation of the child with the Enuresis (Enuresis of the child with the Diagnostic Evaluation):
- History taking and physical examination,
- Detailed interview of the child and parents,
- Complete physical examination of the side,
- Lumbosacral spine X-ray,
- Intravenous Urogram,
- Urine analysis,
- Urine culture.
- Bladder function test.
- Uroflowmetry test.
medical management of the child with the Enuresis. (Medical Management of a Child with Enuresis):
The medical management of a child with enuresis depends on various factors such as the age of the child, the severity and frequency of bedwetting episodes, any medical and psychological factors, etc.
Fluid Restriction
Advise the child to have a reduced fluid intake in the evening and especially beverages such as cold drinks, tea, coffee, etc. should be consumed in reduced quantities in the evening. Advise the child’s parents to provide bladder control training to the child regularly.
Bladder Control
Advise parents to provide regular bladder control training to the child.
Provide proper medication to the child.
1) Desmopressin
Desmopressin is a synthetic form of antidiuretic hormone. This type of medication helps to reduce urine production at night.
2) Anticholinergic Medication
Anticholinergic medication helps to reduce the contraction of the bladder muscles.
Ex: Oxybutynin, Tolterodine.
3) Tricyclic Antidepressants
These types of medications are used to achieve bladder control and to treat depression. Helps to induce sleep. Ex: Amitriptyline, Nitroxazepine, Imipramine.
Nursing management of the child with the Enuresis:
- Properly assess the child.
- Properly assess the frequency, pattern, and severity of the child’s bedwetting.
- Provide complete education about enuresis to the child and his family members.
- Provide proper education to the child’s parents that the child should drink a limited amount of any fluid in the evening. To do.
- Provide proper emotional support to the child and his/her family members.
- Advise the child’s parents to take medication properly.
- Properly advise the child to completely empty the bladder before bedtime.
- Advise the child to properly set an enuresis alarm.
- Advise parents to provide proper bladder training to the child.
- Advise parents to use an electrical bell (buzzer) for the child.
- Provide emotional support and environmental modification to the child and his/her parents.
- Advise parents to provide positive reinforcement to the child.
- Provide proper work and a comfortable environment for the child.
7.Internationally accepted rights of children – Internationally accepted rights of children.
- The United Nations declared the rights of children on 20 November 1959. They were created with the aim of meeting the special needs of the child in mind.
These rights are as follows. - Right to free education.
- Right to name and nationality.
- Right to receive special care if the child is handicapped.
- Right to receive affection, love and good understanding.
- The right to adequate quality nutrition.
- The right to first aid or relief in times of distress.
- The right to good medical care.
- The right to play well and to have access to recreational facilities.
- The right to develop one’s abilities and become a useful member of society.
- The right to be brought up in a peaceful and fraternal environment.
All the above rights are also the right of children to exercise all rights equally without discrimination of religion, caste, creed, sex, color, etc.
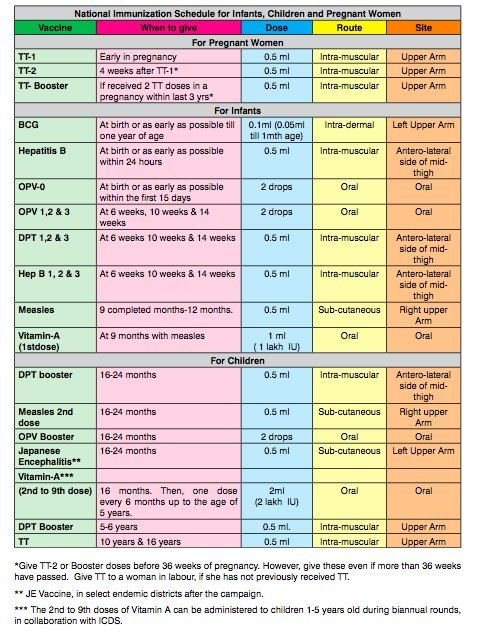
8.National immunization schedule for children – National immunization schedule for children
Q-3 (A) Multiple Choice Questions (MCQs) (10 Marks)
1. Who is the father of pediatrics? Who is the father of pediatrics?
a. Abraham Maslow
b. Abraham Linkon
✅c. Abraham Jacob
d. George Hallet
2. Mother’s first breast milk is known as ? What is mother’s first breast milk called?
a. Fore milk
✅b. Colostrum
c. Hind milk
d. Transitional milk
3. It is example of cyanotic heart disease…
a. PDA
b. ASD
c. VSD
✅ d. Tetralogy of Fallot
4. Normal weight of new born in india is –
a. 2.4 Kg
b.3.9 Kg
✅ c. 2.8 Kg
d. 1.5 Kg
5. FIPV Vaccine given for protection against disease…FIPV Vaccine given for protection against disease.
a. TB
✅ b. Polio
c.Measles
d.Diarrhea
6. Rickets in Children occures due to Deficiency of…Rickets in Children occures due to Deficiency of…
a.Vita- A (Vitamin A)
✅ b. Vita – D (Vitamin D)
c.Vita – E (Vitamin E)
d.Vita – K (Vitamin K)
7.Anterior Fontanelle Closes at age of…Anterior Fontanelle Closes at age of…
✅ a. 18 Months
b.18 years
c.1.5Months
d.6 years
8. Eating of non-nutritive (Non – Edible)Substances is Known as…Eating non-nutritive substances.
a.Tics
b.Enuresis
✅ c. Pica
d.None of above
9. Wilm’s Tumors is Seen in…Wilm’s Tumors are seen in…
a.Brain (Brain)
b.lungs (Lungs)
c.Heart (Heart)
✅ d. Kidney (Kidney)
10. Canula size used in neonate…Canula size used in neonate.
a. 22
✅ b. 24
c. 20
d. 18
(B) Fill in the blanks, fill in the blanks. 10
1.Collection of C.S.F. in ventricles of brain is called …. The accumulation of C.S.F. in the ventricles of brain is called …. Koplik’s spot is a sign of …. disease.👉 Measles
3.Children’s day is celebrated on …. day in India. Children’s day is celebrated on …. day in India.👉 14th November
4.Commonly first teeth appear at …. age in child. Commonly first teeth appear at …. age in child. Comes in age.👉 6 Months
5.Head circumference & chest circumference are equal at …. The months are the same.👉: 6 Months to 12 Months
6.Commonly most vaccines are stored at temperature …. Most vaccines are usually …. Stored at 2°C to 8°C.
7.Full form of ICDS is…. The full name of ICDS is….👉 Integrated Child Development Services
8.Tetanus is caused due to …. Tetanus is a …. It is caused by the bacterium Clostridium tetani.
9.IMNCI Stands for…. The full name of IMNCI is…. 👉 Integrated Management of Neonatal and Childhood Illness
10.Down’s syndrome is caused due to trisomy (abnormality) …. of chromosome. Down syndrome…. is caused by a chromosome defect.👉 21
(C) state whether following statements are true or false. 10
1. BCG vaccine is given on right arm of baby… BCG vaccine is given on right arm of baby. ❌ False
BCG vaccine is administered in the left upper arm, not right.
BCG vaccine is given on right arm of baby.
2. Hemophilia is more common in male children…Hemophilia is more common in male children. ✅ True – True
Hemophilia is an X-linked recessive disorder, hence more common in males.
3. In epispadiyasis child can pass urine without any difficulty and abnormality. In epispadiyasis child can pass urine without any difficulty and abnormality. ❌ False
In epispadiasis, the urethral opening is abnormal, leading to urinary issues.
4.Baby should be breast feed after 48 hours of birth. ❌ False
Breastfeeding should begin within 1 hour of birth, not after 48 hours.
5. O.R.S. once prepared should be used in 24 hours…. It should be used within 24 hours of preparation. ✅ True
Prepared ORS should be used within 24 hours only.
6. Omicron Virus is Responsible for meningitis… Omicron virus is responsible for meningitis. ❌ False
Omicron is a variant of COVID-19 virus, not a cause of meningitis.
7. Rice watery stool is suggestive of dysentery… ❌ False
Rice watery stool is a sign of cholera, not dysentery.
8. Immediate health assessment of newborn child is done by APGAR Score… The APGAR score is used at birth to assess the health of the newborn. ✅ True
The APGAR Score is done at 1 and 5 minutes after birth to assess newborn’s health.
The health of the newborn is assessed by APGAR Score after birth.
9. Infant’ s eye and genitalia should not be covered while giving phototherapy. The infant’s eyes and genitalia should not be covered during phototherapy. ❌ False During phototherapy, infant’s eyes and genitalia must be covered to prevent damage. It is necessary to cover the eyes and genitalia during phototherapy.
10. Mid day meal program is also known as school lunch program… Mid day meal program is also known as school lunch program. ✅ True
Mid Day Meal Program is also referred to as the School Lunch Program.
Mid day meal program is also known as the school lunch program.
