ENGLISH-27/02/2020 CHILD HEALTH NURSING (Done- UPLOAD)PAPER NO-9
27/02/2020 CHILD HEALTH NURSING-PAPER SOLUTION NO.9
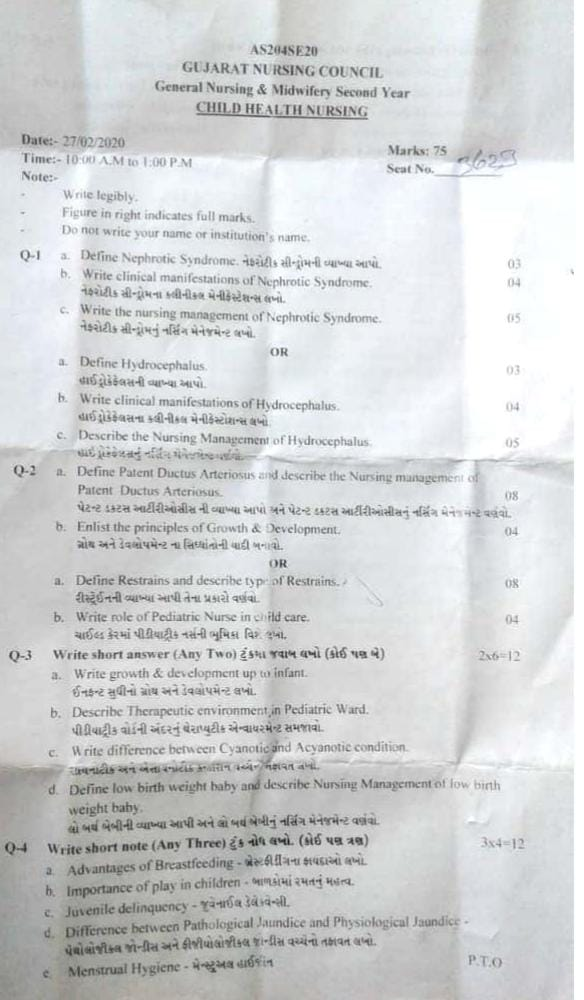
Q-1 a. Define Nephrotic Syndrome.03
This is a disease of the urinary system. Which commonly causes hospitalization in children.
This syndrome has signs and symptoms of more than one condition. Nephrotic syndrome is mainly characterized by severe edema (swelling), hypoalbuminemia, albuminuria, and hyperlipidemia, i.e. hypercholesterolemia.
Nephrotic syndrome is a kidney disorder. In which glomerular permeability increases, which filters proteins present in blood plasma. Due to which the amount of protein increases in the urine and the amount of protein in the blood decreases.
Due to the decrease in the amount of protein in the blood, the fluid in the blood is transferred from the capillaries to the surrounding tissues and cells. Due to which edema i.e. swelling is seen.
Thus, nephrotic syndrome is a very complex and common pediatric problem in children.
b. Write clinical manifestations of Nephrotic Syndrome.
In nephrotic syndrome, this condition progresses slowly or sometimes it is seen in an acute condition. Signs and symptoms are seen according to the severity of the condition.
Swelling is seen around the eyes of the child, i.e. peri-orbital puffiness is seen.
A large increase in weight is seen in the child’s weight in a short period of time.
Edema is seen in all parts of the body, including the legs, scrotum, and hands. This generalized edema is known as anasarca.
When this swollen area is pressed, a pit forms in it, i.e. pitting edema is seen. Due to this swelling, striae are also seen in the skin due to stretching. Due to skin damage, there is also a chance of local infection.
Protein is excreted in the urine, which is called proteinuria, and the amount of protein in the blood decreases, which is called hypoalbuminemia.
In addition, diarrhea, vomiting, and anorexia are seen in the child.
Urine output is less than normal.
The child shows symptoms of anemia.
Liver enlargement and increased blood pressure are also seen.
Problems such as ascites, pleural effusion, respiratory infection, etc. are seen due to hypoalbuminemia.
In some cases, muscle wasting is also seen.
The condition of malnutrition and failure to thrive of the child is also seen.
c. Write the nursing management of Nephrotic Syndrome.Write the nursing management of Nephrotic Syndrome.05
- In the management of nephrotic syndrome, the child has to be given special bed rest and a high protein diet.
He is given minimum fluid intake and a special record of input and output is maintained. - Special care should be taken during the hospitalization of the child. He and his parents should be informed about the disease condition and all its aspects so that his anxiety can be reduced and his cooperation can also be obtained.
Regular monitoring of the child’s vital signs is necessary. - Prescribed by the doctor Administer the prescribed medicine on time and maintain its recording.
Pay special attention to the nutritional needs of the child and keep a record of all the diet and fluids given to him. - Provide the child with supplementary vitamins and minerals in his food.
Perform all procedures on the child with aseptic technique and take into account the issues of infection prevention in his care.
Special care should be taken of the child’s skin and prevent skin breakdown and also prevent bed sores by changing alternative positions. - The child’s general condition should be assessed daily, including his weight, vital signs, Alert level etc. If any abnormality is found in this, immediate intervention should be taken.
- The child’s hygiene should be taken care of and his fingernails should be kept short so that he can be prevented from injuries.
- Keeping in mind the child’s play and recreational activities, his mind should be diverted by doing activities that can be done on different beds.
OR
a. Define Hydrocephalus. Define Hydrocephalus.03
Hydrocephalus is an abnormality of the nervous system of a child. In which there is an abnormal collection of fluid in the ventricles inside the child’s brain.
This fluid is cerebrospinal fluid, the reason for which is its absorption is not normal and its production is more than normal.
Thus, due to the imbalance of cerebrospinal fluid, its accumulation in the ventricles of the brain is known as hydrocephalus. Hydrocephalus is also caused by obstruction in the pathway of CSF.
Due to this condition, enlargement of the ventricles of the brain and the head is seen. Due to which the circumference of the head increases and the head appears larger than normal.
b. Write clinical manifestations of Hydrocephalus.
HydroCyclocephalusNa Congenital and acquired.
The symptoms of hydrocephalus depend on its type and severity of the disease.
The common clinical manifestations seen in this condition are as follows.
In it, the enlargement of the head is excessive. Due to this, the frontals are bulging (upward). The cranial sutures remain open, which also have difficulty in closing. Their closure is delayed.
Venes appear on the scalp and the head part appears shiny due to the filling of the fluid.
When the child’s head is percussioned, a cracked pot type resonance is seen. This sign is also known as McVens sign.
The child’s eyes are tilted downward. A large part of the sclera is visible above the cornea. This type of eye is known as sunset eye.
In this condition, intracranial pressure increases. Due to which nausea, vomiting, restlessness, irritability and high pitched cry are seen.
The child also experiences an increase in temperature and blood pressure.
Increased muscle spasticity, ataxia, papilloedema, urinary incontinence and a gradual decrease in mental activity are also seen.
The above clinical manifestations are seen in hydrocephalus. The increase or decrease in symptoms depends on the severity of the disease condition. If the disease condition is more severe, then neurological disturbances are more likely to be seen.
c. Describe the Nursing Management of Hydrocephalus. Write the nursing management of hydrocephalus.05
Continuous monitoring of the intracranial pressure of a child with the condition of hydrocephalus should be done. If any signs or symptoms of ICP increase are seen, then treatment should be started immediately.
Head circumference should be monitored regularly.
The child’s behavior and his cry pattern should be specially monitored. His restlessness level or irritability level should be checked specifically.
The child’s head and body should be supported during the child’s movement so that no damage or injury occurs.
While sleeping, the child’s head should be supported by a sponge so that injury to the head can be prevented and a comfortable position can be maintained and the pressure on the head can be minimized.
If the child has undergone surgery, it is necessary to take care of the shunt area and take steps to prevent infection there.
The position of the shunt and its working condition should be continuously monitored.
The child’s vital signs should be continuously observed.
The child should be given IV fluid as well as nasogastric fluid Maintain and monitor the input and output chart.
Plans should be made to ensure that the child’s nutritional needs are met.
Maintaining the child’s skin integrity is particularly important. Keep changing the position as per the child’s need so that bed sores can be prevented.
Exercises can also be prescribed to the child as per the need.
The anxiety level of the child can be reduced by informing the parents about every procedure and information.
While performing every procedure with the child, aseptic technique can be maintained and infection can be prevented.
Maintain special monitoring of the child’s general condition and also convince the child’s parents for routine care and regular monitoring. If any symptoms of abnormality are seen, immediately contact the hospital or doctor.
Q-2 a. Define Patent Ductus Arteriosus and describe the Nursing management of Patent Ductus Arteriosus. 08
Patent Ductus Arteriosus is a congenital heart defect. This condition occurs when blood vessels called ductus arteriosus connect the pulmonary artery and aorta in the fetal circulation during intrauterine life. But after the birth of the newborn, it normally closes in the first week of life. However, if the condition of Ductus Arteriosus remains patent or open even after birth, that is, if it fails to close, then the condition is called Patent Ductus Arteriosus. This condition of Patent Ductus Arteriosus is usually seen more in premature babies whose weight is less than 1.5 kilograms.
Nursing management of Patent Ductus Arteriosus.Nursing management of Patent Ductus Arteriosus:
- Properly monitor the child.
- Properly assess the child’s vital signs.
- Properly assess the child’s cardiac function.
- Properly assess the child’s symptoms such as breathing difficulty, sweating, and fatigue.
- Inform the child’s parents about the child’s condition, its causes, its symptoms and signs, its treatment, and life expectancy. Provide complete education about style modification.
Preoperative Nursing Management:
- Provide proper position to the child. Provide oxygen to the child.
- Provide proper psychological support to the child.
- Monitor the child’s blood oxygen level regularly.
- Provide proper protection to the child to prevent infection and trauma.
- Provide complete education to the child’s parents and caregivers about the child’s condition, its causes, symptoms and signs.
- Provide care to the child by maintaining proper aseptic technique. Provide intravenous fluids to maintain the child’s nutritional status.
Properly clothe the child to prevent hypothermia. - Properly provide antibiotic medicine to prevent infection.
Post-operative Nursing Management:
- Properly close monitoring of the child.
- Continuously monitor the child’s vital signs.
- Continuously monitor the child’s intake output chart. Provide adequate intravenous fluids to maintain the child’s nutritional status.
- Provide adequate respiratory support to the child.
- Properly administer oxygen to the child.
- Properly suction to keep the child’s airway clear.
- Continuously maintain the child’s body temperature and avoid exposing the child to the external environment.
- The child Provide a nutritious diet.
- Maintain proper hygienic conditions to prevent the child from infection.
- Provide dressings by maintaining proper aseptic technique on the operative site.
- Monitor the child’s daily weight.
- Continuously monitor the child for any complications.
- Provide education to the parents to provide adequate care to the child.
- Provide complete education to the parents about the child’s condition. Provide proper psychological support to reduce the anxiety of the child and his family members.
- Advise the parents of the child to provide the prescribed medication to the child.
- Properly advise the parents of the child to provide the prescribed medication to the child.
- Provide proper Provide psychological support.
- Advise the child’s parents to follow up regularly.
b. Enlist the principles of Growth & Development. Enlist the principles of Growth & Development. 04
- Growth and development are closely related to each other. In a child, growth and development occur in parallel and continuum.
- We use the words growth and development interchangeably. But the two words are not the same. They have different meanings. Both cannot be used interchangeably, we use both the terms together for the sake of simplicity.
- It is very important to understand the characteristics and principles of growth and development in children, which are given below.
- Growth and development is a continuous process. It is unique for every child. Along with this, it also follows the pattern of individual differences.
- The pattern of growth and development in each child is seen according to his stage. It can be predicted. The stages are similar for all children, but the time to achieve those stages may vary. E.g. Every child learns to sit, learns to speak, but the time to achieve this function is different for all children.
- Growth is seen in the size and shape of each organ and in its coordination.
- Growth and development are seen according to these principles: Cephalo-caudal i.e. from head to tail and Proximo-distal i.e. from the midline and center to the periphery.
- Growth and development are seen according to these principles: Simple to Complex. In which initially mass movement and activity are seen in simple patterns. Over time, it is seen in specific actions and responses i.e. complex tasks.
- Development is mainly seen due to stimulation. In this, as the child is given stimulation, his development is seen better.
- Growth and development are interdependent on many factors such as hereditary and environmental.
- The influence of society is particularly visible on the growth and development of a child. Development is also based on a cultural aspect.
- In growth and development, physical, mental, social, emotional activity is seen in a positive correlation and all those factors are connected to each other.
- Growth and development is also seen at times fast, at times slow and at times stable.
OR
a. Define Restrains and describe type of Restrains. Define Restrains and describe type of Restrains.08
- Restrains are a type of protective device. Which limits the movement and freedom of an individual, i.e. restraint is used to mobilize any body part, i.e. to restrict the movement of any body part.
- Physical restraint is mainly used in health care settings. In which the movement or mobility of a body part is restricted using a physical device or technique.
- Restraints are used in health care, psychiatric, and correctional settings.
purpose of restraints
- To prevent a patient from falling down For
- To provide safety to the child
- To protect the client from injury
- To maintain the child in the prescribed position.
- To limit the child’s movement during the procedure
- To provide constant immobilization
indication of restraint
- Agitation or aggression
- Seizure or tremor
- Medical procedure
- Alter mental state
- Suicidal behavior
contraindication of restraint
- Osteoporosis
- Respiratory disease
- Cardiovascular Diseases
- Pregnancy
- Childbirth
- Mental conditions (PTSD, anxiety)
types of physical restraints ( Types of Physical Restraints)
1) Mummy restraints
2) Elbow & knee restraints
3) Extremity restraints
4) Abdominal restraints
5) Jacket restraints
6) Mitten or finger restraints
7) Crib net restraints
8) Safety belt
Mummy restraints :
- Mommy restraints are a type of physical restraint used on infants and small children.
- Mommy restraints are primarily used to perform head and neck examinations, treatments, and procedures. To perform procedures such as eye irrigation, gastric lavage.
- In addition, mother restraints are used to restrict limb movement and immobilize the limb.
Purpose:
- To immobilize the infant’s arms and legs.
- Child’s To examine the head and neck.
- To perform the procedure
- To puncture the jugular vein
- To pass a Rileus tube
Elbow restraints:
- An elbow restraint is a type of physical restraint.
- An elbow restraint is primarily used to hold the elbow in an extended position. So that it cannot reach the face.
- Elbow restraints are used to prevent and control flexion of the elbow.
- Elbow restraints are used in infants receiving scalp vein infusions and in infants who have undergone cleft lip repair surgery.
- Elbow restraints are made of a double piece of cloth or other strong material.
Purpose (Purpose) :
- When surgery has been performed on the head or face
- When eczema or other skin disorders are present on the head or face
- When a scalp vein needle has been placed
Extremity restraint (Extremity Restraint)
- Extremity restraints are used to limit the movement of the extremities (legs and arms).
- Extremity restraints include wrist restraints, ankle restraints, and elbow restraints.
- These restraints are used during medical procedures, aggressive behavior, and post-operative care.
Purpose :
- Prevent Harm to Self and Others
- Ensure Safety
- During Medical Procedures
Abdominal Restraint
- Abdominal restraints are used to limit the movement of the torso or abdomen.
- Abdominal binders, abdominal straps, and torso restraints are used as abdominal restraints.
- Abdominal restraints are used during post-operative care, medical procedures, and trauma care.
Purpose (Purpose) :
- Prevent abdominal movement
- Stabilize abdomen
- Prevent further injury
Body jacket
- A body jacket is also known as a waist restraint.
- A body jacket is wrapped around the torso and minimizes movement of the arms, chest, and abdomen.
- This restraint is attached to the bed.
Purpose:
- Prevent Self Harm
- Ensure Safety
- Reduce Agitation
- During Medical Procedures
Mitt Restraint
- A hand restraint is also known as a finger restraint.
- A hand restraint is a type of restraint used to limit the movement of the hand.
- A hand restraint prevents the use of the hand.
- Therefore, this restraint is used in children and psychiatric conditions. So that the patient can be prevented from removing dressings, tubes, cannulas.
Purporse (Purpose) :
- Prevent removal of medical devices
- Prevent self-injury
- Protect the environment
Saftey belt (safety belt)
- A safety belt is also known as a restraint belt.
- A safety belt restraint is made of an electrically non-conductive material.
- A safety belt is mainly used to prevent the patient from stretching and falling down from the operating table.
- A safety belt also prevents the patient from leaving the bed.
Crib net restraint
- Crib net restraint is also called bed net.
- This restraint prevents infants and young children from getting out of beds and cribs.
- This restraint is made of mesh and net It is easy to install and adjusts to any bed or crib.
Purpose
- Prevent falldown
- Ensure safety
- Reduce risk of injury
hazards and risk of restraints
- Tissue damage
- Development of pressure sore
- Sore and gangrene
- Injury to brachial Plexus
- Damage and Injury to the Other Part of Body
- Ischemia and Nerve Damage
- Loss of Muscle Tone
- Foot Drop and Wrist Drop
- Reduce Body Mass
- Constipation
- Psychological hazards (frustration, loss of dignity, depression)
nursing responsibility during use of restraints
- Assess the client’s behavior and assess their need for restraints.
- Check the doctor’s order for restraints.
- Obtain consultation from the client’s family members and friends as per hospital policy.
- Provide complete information about the client’s family members and friends about the need for restraints, their type and their procedure.
- Follow the institute’s policy and guidelines for restraints.
- Use adequate assistant staff while applying restraints.
- Use the least restrictive, reasonable and appropriate restraints.
- Ensure that the patient can move freely.
- Take special care to ensure that the restraints do not cause circulatory arrest.
- Do not use restraints in place of IV sites.
- Pad the bony prominence area before applying restraints.
- Maintain patient’s safety, comfort, privacy, and dignity during restraints.
- Be aware of any wrinkles in the restraints.
- The patient can be easily, closely, and regularly monitored Keep it in such a place.
- Visit the restrained patient every 30 to 60 minutes and review him regularly.
- Avoid using restraints until both are in place and use other practices, interventions, and alternate techniques instead.
- When removing restraints, remove only one restraint at a time.
- Document the restraints used.
b. Write role of Pediatric Nurse in child care. Write about the role of a pediatric nurse in child care.04
- With the changes in the field of medicine and technological advancements, the role of a pediatric nurse has also undergone many changes to meet the new demands in child health care.
- The role of a pediatric nurse has become specialized in every aspect of care. Whether the child is healthy or sick, all care is provided by nurses through a comprehensive approach at every stage.
The role of a nurse changes in different institutions, but their basic responsibilities and roles are the same everywhere.
A pediatric nurse has specialized training in pediatrics. Their detailed roles are classified as follows.
CARE GIVER.
A pediatric nurse provides preventive, promotive, curative and rehabilitative care to the child in every setting. This care is planned based on the needs of the child. It includes all the needs related to therapeutic needs, comfort, safety and personal hygiene.
HEALTH EDUCATOR.
The pediatric nurse provides incidental and planned health teaching to the child’s parents and family members on all matters related to child care. So that the child can be given proper care.
ADVOCATIVE ROLE.
The pediatric nurse strives to ensure that the child receives quality care by using the scientific principles of child health care. Works to provide maximum benefit to the child from his/her care.
MANAGER.
To fully fulfill every care of the child, the nurse works as the manager of the pediatric care unit and helps in organizing each of his/her care properly.
TEAM LEADER.
The pediatric nurse works as a team leader in her/his unit and leads everyone to provide better care by maintaining proper communication between each staff and subordinates. Distributes responsibility among everyone.
NURSE AS A RECREATIONIST.
Plans different types of recreational activities for the child to modify his stress during his hospital adjustment procedure and hospitalization and helps in modifying the child’s behavior.
NURSE AS A COUNSELOR.
Provides counseling and guidance to the child to make decisions during critical care decisions and any problem-solving approach to the parents.
SOCIAL WORKER.
She works with special welfare agencies and provides necessary social support for the social problems and adjustment of children and their family members.
NURSE AS A RESEARCHER.
The nurse conducts different types of research during her clinical practice in the pediatric unit and tries to bring new concepts. She finds new ways to deal with health problems. Nursing plays a role as a continuous research to provide better health care facilities.
Q-3 Write short answer (Any Two) (4) 2×6=12
a. Write growth & development up to infant. Write the growth and development up to the infant.
Definition:
Growth means the formal changes in the size, weight and dimensions of the body and Development means the continuous and gradual process of development of the patient’s functioning, intelligence, senses and behavior. Both are important for physical and mental health after birth.
1) Neonatal period – 28 days after birth
Physical Growth:
- Average weight: 2.5 to 3.5 kg
- Length: About 50 cm
- Head circumference: ~35 cm
- Chest circumference: ~33 cm
- Daily weight loss (up to 10%), which then returns in 10 to 14 days.
Physiological Development:
- Respiratory rate: 40-60/min
- Heart rate: 120-160/min
- Body temperature may be irregular.
- Respiration is irregular and mainly chest-breathing.
Reflexes (Reflexes):
- Moro reflex
- Rooting reflex
- Grasp reflex
- Sucking reflex
This reflex indicates the completion of the patient’s nervous system.
2) Infant period – 1 month to 1 year
Weight and Length:
- The birth weight doubles by 5 months.
- The weight triples by 1 year of age (~9-10 kg).
- Length reaches ~75 cm by 1 year of age.
Changes in head and chest circumference:
- anterior fontanelle closes at 12-18 months Is
Motor Development:
- Holds head up at 3 months
- Sits with support at 5-6 months
- Starts to crawl at 7-8 months
- Tries to stand at 9-10 months Is
- Walks at 12 months
Teething:
- First tooth appears around 6 months – lower central incisors
- 6 to 8 teeth appear within 1 year
Sensory and Cognitive Development:
- Identifies sounds, pays attention to objects that appear
- Distinguishes between mother and stranger at 6 months
- Says one word at 9-10 months (mama, dada)
- Eating separately Recognizes, tries to eat with a spoon
Social and Emotional Development:
- Smiles and responds with vocalizations
- Personal connections develop
- Separation anxiety develops
- Parents are important for psychological security
Growth and development from infancy to adulthood play a fundamental role in the overall health of the patient. This includes all areas of physical, intellectual, emotional and social development. As a pediatric nurse, understanding each step and identifying abnormalities is essential
b. Describe Therapeutic environment, in Pediatric Ward. Explain the therapeutic environment within a pediatric ward.
Meaning and Importance:
A therapeutic environment is an environment that positively influences the physical, mental, and emotional health of a pediatric patient. It is the primary responsibility of the nursing team to create a safe and comfortable environment for the child in the stressful environment of the hospital. A therapeutic environment provides a gentle foundation for children’s developmental milestones, recovery, and emotional well-being.
1) Physical Safety and Hygiene:
Aseptic technique is essential for infection control in the pediatric ward. Hand hygiene, sterile equipment, and regular disinfection are essential to protect all patients from cross-infection. Floors should be non-slippery and sharp objects should be kept out of reach of children.
2) Pleasant and Stimulating Environment:
Colorful walls, cartoon images, child-sized furniture, and interactive toys in the ward provide relaxation to the patient. This environment reduces hospital anxiety in the child and promotes his development. The lighting should be soft so that a sense of natural peace is felt.
3) Parental Presence:
Parental involvement is a form of psychological reassurance for the child. Allowing the child to stay with the parents helps in increasing security and trust for the child. The presence of parents can help the child accept treatment more easily.
4) Compassionate Nursing Staff:
The empathetic and child-centered behavior of the nursing staff is a fundamental element of a therapeutic environment for the patient. It is necessary to communicate at the patient’s level, check up through play, and act sympathetically.
5) Play Therapy and Educational Activities:
Play therapy reduces the patient’s feelings of tension, fear, and isolation. Cardboard games, puzzles, rangoli, stories, and educational toys keep them engaged. These activities are very useful for cognitive development as well as emotional expression.
6) Noise and Light Control:
A noise-free environment should be maintained as per the wishes of the pediatric patient. Low lights, soft sounds, and adequate rest time should be provided. Unannounced noise disrupts the child’s physical recovery.
7) Privacy and Individualized Care:
Maintaining privacy for each patient is an integral part of the therapeutic environment. Physical, psychological and social support should be provided according to the needs of the individual patient. Bed arrangement should also be based on personal space.
8) Supportive Services:
Multidisciplinary services such as child psychologist, dietitian, counselor, and physiotherapist in the ward enhance the quality of the therapeutic environment. Emotional, educational, and physical support are essential for children.
9) Parental Education
Providing health education to parents, such as about the patient’s condition, medications, home care, and immunizations, so that they can cooperate in the treatment. This relationship builds trust between the nurse and the patient family.
Conclusion:
A therapeutic environment for pediatric patients is essential not only for physical but also for emotional health. A well-organized, loving and child-friendly environment is extremely important for recovery, development and self-confidence in children. Every nurse should adopt a sensitive and responsible approach to create this environment.
c. Write difference between Cyanotic and Acyanotic condition.Write difference between Cyanotic and Acyanotic condition
Difference between Cyanotic and Acyanotic Condition
introduction :
Congenital Heart Defects are mainly of two types: Cyanotic Condition and Acyanotic Condition. Both conditions differ according to the level of blood flow and oxygenation in the cardiac field of the patient. The main difference depends on the amount of oxygen in the patient’s blood and the resulting blue color (cyanosis) seen on the skin.
Cyanotic Condition:
Cyanotic condition is a condition in which deoxygenated blood mixes with pure blood inside the patient’s heart and oxygen-depleted blood reaches various parts of the body. This causes a bluish tinge to the patient’s lips, nails, and skin, which is called cyanosis.
In this condition, Right to Left Shunt is usually seen, in which deoxygenated blood from the right side of the heart goes directly to the left side and is pumped through the body.
For example:
Tetralogy of Fallot, Transposition of Great Arteries, Tricuspid Atresia, Total Anomalous Pulmonary Venous Return, etc.
Symptoms:
- Skin, lips, and nails appear blue (cyanosis)
- Oxygen saturation is less than 85%
- Patient tires easily
- Respiratory rate increases
- Growth delay is observed
Acyanotic Condition:
In an acyanotic condition, the patient has abnormal blood flow to the heart but there is no direct effect on the oxygenation of the blood. That is, only oxygenated blood flows in the patient’s body and cyanosis is not observed.
In this condition, a Left to Right Shunt is usually seen, in which oxygenated blood from the left side turns to the right side and returns to the pulmonary circulation.
For example:
Atrial Septal Defect, Ventricular Septal Defect, Patent Ductus Arteriosus, Atrioventricular Canal Defect, etc.
Symptoms:
- No blue discoloration of the skin
- Oxygen saturation is normal (≥ 95%)
- Patient has mild respiratory distress
- Symptoms of pulmonary congestion and heart failure are seen
- Sometimes a gurgling sound and a throat murmur are heard
The main difference between Cyanotic and Acyanotic Cardiac Conditions is that in Cyanotic, the patient’s body is deficient in oxygenated blood, causing cyanosis, while in Acyanotic, there is a silent disturbance within the heart despite oxygenated blood. Both types of conditions can be serious for pediatric patients and require immediate medical and surgical intervention. As a nurse, it is a very important responsibility to understand this difference and provide proper observation and care to the patient.
d. Define low birth weight baby and describe Nursing Management of low birth weight baby. Define low birth weight baby and describe nursing management of low birth weight baby.
Low birth weight means that the weight of the child at the time of birth is less than 2500 gm, this condition is called low birth-weight baby (LBW).
In which, very low birth weight baby means that the weight of the child is 1500 grams or less, it is known as very low birth weight baby.
While, extreme low birth weight baby means that the birth weight of the infant is less than 1000 grams, this condition is called extreme low birth weight baby.
Nursing Management:
Give vaccines according to the immunization schedule.
Thermal protection:
Keep the baby in an incubator or radiant warmer.
Adopt Kangaroo Mother Care to avoid hypothermia.
Nutritional support:
Encourage breastfeeding.
If the baby cannot breastfeed, then nasogastric feeding should be done.
Weight should be checked regularly.
Infection Prevention:
Adopt sterile technique.
Frequent handwashing.
Respiratory Management:
Apnea monitoring should be performed.
Give oxygen therapy if necessary.
CPAP or mechanical ventilation if necessary.
Skin Care:
As the skin is delicate, take regular skin care.
Hypothermia and dehydration Prevent.
Parental Education:
Training parents for home care.
Q-4 Write short note (Any Three)3x 4 = 12
a. Advantages of Breastfeeding.
- Breastfeeding develops a psychological bond between mother and baby.
- Human milk is available to the baby at the body temperature required.
- Milk is fresh, sterile and free from contamination and goes directly into the baby’s mouth.
- Human milk is ideal when it is readily available.
- Breast milk is a safe and protective food,
it is the perfect food for infants. - It meets the total nutrient requirements of the baby for the first six months.
- It is very important for the baby’s brain growth because breast milk contains a high amount of lactose and galactose.
- Breast milk contains vitamins, minerals, electrolytes and water which help in the maturation of the infant’s intestinal system. It is very important for.
- Breast milk provides such a facility that the absorption of calcium increases so that the growth of the baby’s bones improves.
- Breast milk is easily digested.
- Breast milk contains all the necessary nutrients that the baby needs.
- Breast milk protects the baby from infection and deficiency.
Breast milk is already prepared .
Breastfeeding is a method of family planning, breastfeeding is a natural contraception that has a major impact on the population of developing countries. - It prevents children from diarrhea and also has a laxative action.
- Breastfeeding does not have any dangerous allergic effects.
- Breastfeeding can save time, money and energy.
- Breastfeeding is good for the mother and Helps in building a healthy relationship with the child.
- The chances of conception are reduced during lactation.
- Best feeding helps in involution of the uterus (i.e. bringing the uterus to a pre-pregnant state).
- Breastfeeding reduces the chances of sunburn, gastrointestinal infections and ectopic eczema,
and also reduces the chances of scurvy and rickets. - Breastfeeding reduces the chances of breast cancer.
- Breast milk contains IgA and IgM macrophages, lymphocytes, lysosomes, etc., due to which diarrhea and acute respiratory infections can be prevented in babies.
And it prevents malaria and viral and bacterial infections. - Breast milk protects against conversion, hypocalcemia, tetanus, deficiency of vitamin E and zinc.
- Exclusive breastfeeding can prevent malnutrition in children.
- Breastfeeding increases the intelligence of the child, and the child feels secure (due to the infant-mother bond)
- The chances of illness in the child are reduced.
- Breastfeeding reduces the chances of postpartum hemorrhage (in which there is excessive bleeding from the genital tract after delivery).
- The chances of ovarian cancer are also reduced.
- It helps in reducing the excess fat stored in the mother during pregnancy.
b. Importance of play in children – Importance of play in children.
Introduction:
Play is not just a way to pass the time for children, but it is a natural therapeutic medium for physical, mental, social and emotional growth. Different types of games, depending on the developmental stage of the child, help in developing physical health, brain stimulation, communication skills and cognitive functions. Play is extremely important for medical, psychological and neurological health.
Main Advantages of Play in Children:
Physical Development:
During play, a child’s gross motor skills such as running, jumping, climbing, etc. become stronger. The musculoskeletal system is strengthened and coordination and balance are developed.
Sensory Development:
Various games simulate the patient’s human senses such as visual, auditory, tactile, etc., due to which perception and sensory integration improve.
Cognitive Development:
During play, the patient develops observation, memory, focus, problem-solving and decision-making skills. Creative thinking and imagination also become more active.
Social Development:
Interpersonal skills such as cooperation, harmony, sharing and fair play develop in the patient through group play. Social role playing helps the patient to understand social structures.
Emotional Development:
Play helps the patient to express their emotions, release frustrations, and reduce stress. This increases emotional resilience and self-esteem.
Language Development:
During play, patients learn new words, practice verbal communication, and develop language fluency.
Personality Development:
Play helps patients develop self-expression and leadership skills. Personal skills like leadership, confidence and adjustment ability develop.
Health Maintenance:
Physical activity provides protection against non-communicable diseases like obesity and diabetes in patients. Play also boosts cardiovascular health.
Behavioral Modulation:
Play develops discipline, rule-following, and frustration tolerance in the patient, which is also helpful in later life.
Therapeutic Value:
Other patients such as autism, ADHD (Attention Deficit Hyperactivity Disorder), and developmental Play acts as an effective therapy for patients with developmental delays.
Play is not just entertainment for a child, but also a source of all-round development. Play Therapy in Pediatric Nursing is an indispensable component for the positive health of the patient. Through play, the child becomes physically, mentally and emotionally well-equipped and his life can become healthier and happier.
c. Juvenile delinquency – Juvenile delinquency.
Juvenile delinquency is one of the most common problems of society. ‘Juvenile’ means childhood and ‘delinquency’ means antisocial behavior or criminal behavior
Juvenile delinquency is a type of criminal act that is usually committed by children and teenagers who are under the age of 18. Juvenile delinquency is illegal or antisocial repetitive behavior by a child that is usually committed by an individual under the age of 18. This juvenile delinquency can range from relatively minor crimes such as vandalism, shoplifting to more serious crimes including assault, drug crimes, and property crimes. This juvenile delinquency behavior involves lying, stealing, stealing from home, running away from school, running away from home, disobeying anyone, fighting, looting, sexual assault, etc.
Etiology/cause of the Juvenile Deliquency:
- Due to family dynamics such as That,
- Hereditary,
- Due to chromosomal defects
- Due to parental conflict,
- Due to death,
- Abuse,
- Due to neglect of the child,
- Due to low parental supervision,
- Poor parent-child relationship,
- Peer group influence
- Due to factors such as,
- Peer pressure,
- Due to the influence of delinquent peer groups Due to,
- Socioeconomic factors such as,
- Low socio-economic conditions,
- Low income,
- Poverty,
- Unemployment,
- Inadequate Due to housing conditions,
- Due to lack of education,
- Due to community environment such as,
- Due to availability of drugs,
- Due to criminal neighborhoods,
- Due to unsatisfactory conditions in schools and colleges such as,
- Recreational facilities are inadequate,
- Teacher student relationship is improper,
- Academic failure,
- Substance abuse such as,
- Alcohol,
- Drug abuse Due to,
Clinical manifestation/ sign and symptoms of the Juvenile Deliquency (Juvenile Delicacy Symptoms and Signs)
1) Behavioral problems are seen
such as,
theft,
vandalism,
alcohol abuse,
assault and assault,
bullying,
damage,
2) School Difficulties
Academic Struggle,
Poor School Performance,
Running away from school,
Being indisciplined in school,
Conflict between teacher and friends.
3) Peer Relationship
Peer Rejection,
Social Isolation,
Difficulty in Forming Relationships with Peer Group,
4) Family Conflict
Parent-Child Relationship Impaired,
Less Parental Supervision Getting,
Less parental support,
5) Emotional disturbances
Depression,
Anxiety,
Anger,
Impulsive behavior,
6) Substance abuse
Using alcohol,
Using drugs,
7) Legal issues
Involving in criminal activities.
Diagnostic evaluation of the Juvenile Deliquency:
Legal history,
Family assessment,
Social and environmental factors assessment,
Psychological assessment,
Substance abuse assessment,
Educational assessment,
Management of the Juvenile Deliquency:
- Provide proper education to the child to prevent delinquency.
- Take early intervention against the child to prevent him from doing any illegal activity.
- Provide proper cognitive behavioral therapy to the child.
- Give advice to the child’s family members or provide proper love and affection to the child.
- The child’s school and college The atmosphere of the school should be familiar so that the child can be prevented from doing illegal activities.
- Advise the child’s teachers to work properly with their students and provide a comfortable environment.
- Advise the child to provide a healthy family environment.
- Advise the child’s parents and caregivers to provide the child with proper love and affection from the family.
- Advise the parents to fulfill the basic needs of the child.
- Provide proper educational opportunities to the child.
- Advise the child to do proper exercise, sports, and recreational activities.
- Provide proper counseling and guidance to the child.
- Provide proper work and comfortable living conditions for the child. Provide environment.
- Provide proper psychological support to the child.
- Provide complete education to the child about social and anti-social behavior and legal and illegal behavior.
d. Difference between Pathological Jaundice and Physiological Jaundice-Write the difference between Pathological Jaundice and Physiological Jaundice.
Introduction:
Jaundice is a condition caused by an increase in the level of bilirubin in the patient’s blood, in which the skin and sclera appear yellow. Jaundice is especially common in newborn patients. It
There are two types — Physiological Jaundice and Pathological Jaundice. The differences between the two are very important for the diagnosis and treatment of the patient.
1.Definition:
Physiological Jaundice:
This is a common type of newborn jaundice, which is caused by incomplete development of the liver. It is not associated with any underlying disease and is usually not dangerous.
Pathological Jaundice:
This is a type of jaundice that appears in newborns within the first 24 hours of birth and is indicative of a more severe pathological condition. This can be harmful to the patient and requires immediate treatment.
2. Onset Time:
Physiological Jaundice:
Usually occurs between 24 and 72 hours after birth.
Pathological Jaundice:
Appears within the first 24 hours of birth.
3. Bilirubin Level:
Physiological Jaundice:
Bilirubin levels are usually ≤ 12 mg/dl.
Pathological Jaundice:
Bilirubin levels can be ≥ 15 mg/dl or increase rapidly ≥ 0.5 mg/dl per hour.
4. Causes:
Physiological Jaundice:
Liver immaturity, excessive red blood cell hemolysis, slow bilirubin metabolism.
Pathological Jaundice:
Rh incompatibility, ABO incompatibility, Neonatal sepsis, Hemolytic anemia, G6PD deficiency, Congenital infections.
5.Symptoms:
Physiological Jaundice:
Mild skin pigmentation, patient is generally healthy.
Pathological Jaundice:
Symptoms such as continuous redness, inability to eat, increased sleepiness, stupor and sometimes seizures.
6. Complications:
Physiological Jaundice:
Complications are not usually seen, the risk of Kernicterus is very low.
Pathological Jaundice:
Serious complications such as Kernicterus, Brain damage, Hearing loss, Developmental delay are possible.
7. Treatment:
Physiological Jaundice: Observation, increase breastfeeding. No special intervention is required.
Pathological Jaundice:
Immediate phototherapy, exchange transfusion, intensive medical care are required.
8. Duration:
Physiological Jaundice:
Recovers on its own in approximately 5 to 7 days.
Pathological Jaundice:
Can persist for a longer period and the patient’s condition may worsen if proper treatment is not given.
9. Difference in Clinical Management:
Conclusion:
Physiological Jaundice is a common, self-limiting and less complicated condition, while Pathological Jaundice is a severe and high-risk condition that requires timely recognition and immediate medical intervention. As a nursing professional, it is very important to closely monitor the patient, record symptoms, and provide appropriate management in collaboration with the doctor.
e) Menstrual Hygiene –
Menstrual hygiene :
1) Menstrual hygiene is the type of hygiene that a girl needs to maintain when she gets her menstrual period every month after 12 to 16 years.
2) When a girl goes to school, she needs to have complete information about her menstrual cycle.
3) Sanitary pads should be used when periods start.
4) Sanitary pads should be changed every six to seven hours.
5) When periods start, one should take a bath once or twice a day.
6) Take adequate rest during periods
7) Drink plenty of water during periods.
8) Eat foods rich in iron and vitamin C.
9) Wash hands properly before and after using sanitary pads.
10) Change sanitary pads frequently.
11) Wrap the used pads in cloth or paper and throw them in the dustbin.
12) Wash hands properly after using the pads.
13) It is very important to maintain hygiene during periods.
14) Take a bath once or twice a day during periods and wear clean clothes.
15) Wash private parts properly with water after using the toilet and urinating.
16) Always use cotton undergarments.
17) Do not use wet undergarments.
18) When using a sanitary pad, it should be properly covered and thrown in a dust bin.
19) If you are not using a sanitary pad and are using a household cloth, then change it frequently.
20) Clean the cloth with soap and water.
21) Then dry it in sunlight.
22) Only then use that cloth.
23) When sitting down to eat, clean your hands with soap and water.
Accordingly, proper hygiene should be maintained during your period.
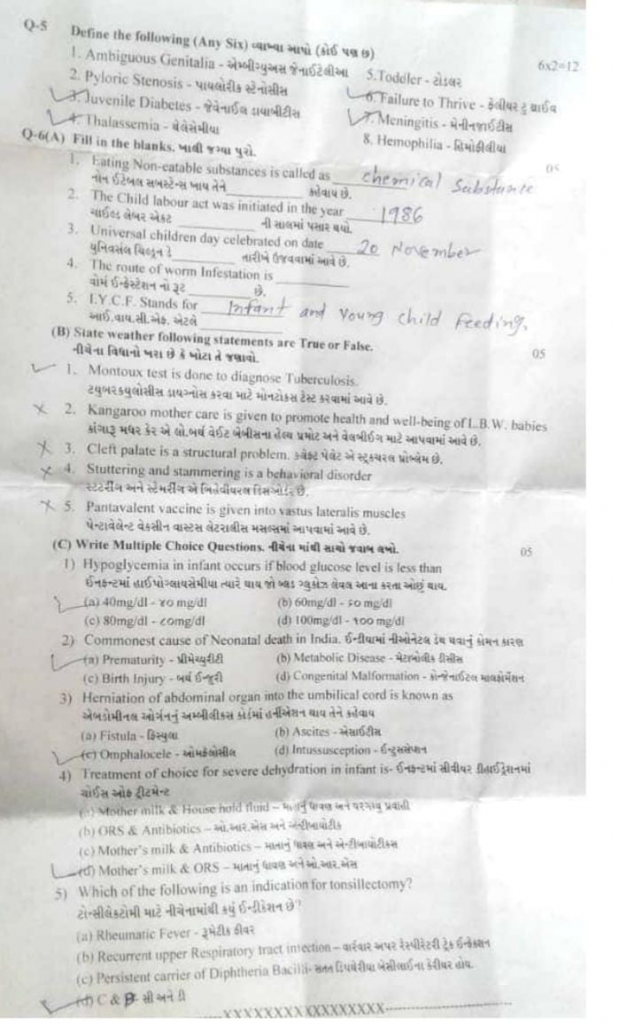
Q-5 Define the following (Any Six) Give a description (any six):
1. Ambiguous Genitalia
Ambiguous genitalia is also known as intersexuality disorder and disorder of sexual development (DSD). This is a condition in which the genital area of a child does not clearly appear to be male or female at birth. This involves different types of anatomical variations, including the involvement of the genital area in which the child is born. At times, there may be both male and female characteristics or it is usually not possible to differentiate between male and female with certainty.
2.Pyloric Stenosis – Pyloric Stenosis
Pyloric: The pyloric part of the stomach.
Stenosis: Narrowing of the body part.
The pyloric part of the stomach becomes narrow due to thickening of the muscle fibers.
Pyloric Stenosis is a condition where the muscle in the pyloric sphincter area in the stomach becomes hypertrophied, due to which that area narrows and creates an obstacle for food to pass from the stomach into the esophagus.
3.Juvenile Diabetes- Juvenile Diabetes
Juvenile diabetes is a chronic metabolic disorder in which carbohydrate, protein and lipid metabolism are impaired.
Diabetes is a group of metabolic disorders in which high blood sugar levels are seen in a child’s blood. This is mainly due to an impairment in insulin secretion and insulin action in the body.
The ”3 P” syndrome is mainly seen in diabetes mellitus.
1)P:= Polyuria (Frequent urination:= Frequent passing of urine),
2)P:= Polydipsia (Increased thirst:= Feeling very thirsty),
3)P:=Polyphagia (increased hunger := feeling very hungry).
Juvenile diabetes mellitus is usually a hereditary disorder
This is a type of diabetes mellitus in which the pancreatic beta cells in the body, which are responsible for producing insulin, are destroyed due to any autoimmune disease, resulting in a total deficiency of insulin.
In this, due to the total deficiency of insulin, insulin is taken through injection.
This type of diabetes is mainly seen before the age of 30.
4.Thalassemia – Thalassemia
Thalassemia is a group of hereditary hemolytic anemias. It is an autosomal recessive genetic disorder in which there is a reduction in the synthesis of hemoglobin/inadequate amount of production.
Thalassemia is a genetic blood disorder in which the body does not produce enough hemoglobin (a protein in red blood cells that carries oxygen into the body). In this, red blood cells are destroyed in large amounts, due to which the condition of anemia arises.
5.Toddler – Toddler
Toddler (Toddler) is a pediatric There is a developmental stage, which is usually used for children aged 1 year to 3 years. This stage is extremely important for the physical, mental, linguistic and social development of the child.
Toddler patients have the ability to learn rapidly and develop new skills such as walking, talking, exploring.
This stage sees significant growth and developmental milestones.
Main features of the toddler period:
- Walking begins
- Language development begins
- Attempt for independence
- “Me” sense and demand for independence increases
- Key stage of emotional and social development
6.Failure to Thrive – Failure to Thrive
Failure to thrive is especially seen in infants and young children. In which the expected growth of the child is not seen.
Failure to thrive is a problem especially seen in children from poor socio-economic groups. This terminology was mentioned in 1915, after which it was also known as emotional deprivation.
Failure to thrive is a chronic and progressive disorder of infants and children. In which the child does not gain the expected weight for his age and his weight is lost. His weight is found to be less than normal for his age.
Failure to thrive does not cause any significant problems in the length or height of the child or in all aspects of his development. The main characteristic is that their weight is not normal for their age.
There are many psychological and physiological reasons for failure to thrive, as well as some external and internal factors.
7 Meningitis – Meningitis
Meninges: The meninges are the protective membranes that cover the brain and spinal cord. There are three other layers in these meninges. 1) Duramater
(outermost layer) 2) Arachnoid mater (intermediate layer) 3) Pia mater (innermost layer)So, these are the three layers of the meninges that cover and protect the brain and spinal cord.
Meningitis: When there is infection and inflammation in the meninges layer surrounding the brain and spinal cord, the condition is called meningitis. This infection can be caused by bacteria, viruses, and microorganisms.
8.Hemophilia – Hemophilia
Hemophilia is an inherited bleeding disorder that is usually caused by a deficiency of plasma coagulation factors (factors 8, 9, and 11). It is usually found in high amounts in males. In which excessive bleeding occurs and blood clotting is poor.
Classification of the Hemophillia
There are a total of 3 classifications of hemophilia.
1) Hemophilia A,
2) Hemophilia B,
3) Hemophilia C.
1) Hemophilia A
Hemophilia A is caused by a deficiency of factor VII(8). is.
2) Hemophilia B,
Hemophilia B is usually caused by a deficiency of factor IX(9).
3) Hemophilia C.
Hemophilia C is caused by a deficiency of factor Xi(11).
Q-6(A) Fill in the blanks :05
1.Eating Non-catable substances is called as……… Eating Non-catable substances is called as……… : Answer: Pica
2.The Child labour act was initiated in the year…….. 1986
3. Universal children day celebrated on date……… Universal Children’s Day…….was celebrated as Answer: 20th November
4. The route of worm infestation is…….worm infestation no route……… Answer: Feco-oral route
5. I. Y.C.F. Stands for……. I.Y.C.F. That is…….. Infant and Young child feeding.
(B) State weather following statements are True or False. State whether the following statements are true or false.
1.Montoux test is done to diagnose Tuberculosis. ➡️ True
🟢 Montoux test is done to diagnose Tuberculosis. (True)
2.Kangaroo mother care is given to promote health and well-being of L.B. W. babies Kangaroo Mother Care is provided to promote the health and well-being of low birth weight babies: ➡️ True 🟢 Kangaroo Mother Care is provided to promote the health and well-being of low birth weight babies: (True)
3.Cleft palate is a structural problem.Cleft palate is a structural problem:➡️ True
🟢 Cleft palate is a structural problem (structural defect). (True)
4.Stuttering and stammering is a behavioral disorder Stuttering and stammering are behavioral disorders:➡️ False
🔴 Stuttering and stammering are disorders of language development, not behavioral disorders. (False)
5.Pantavalent vaccine is given into vastus lateralis muscles प्रतावलेंट वैक्सिन (true)
(C) Write Multiple Choice Questions.
1) Hypoglycemia in infant occurs if blood glucose level is less than….. Hypoglycemia in infant occurs if blood glucose level is less than…..
a) 40mg/dl
(c) 80mg/dl
(b) 60mg/dl
(d) 100mg/dl
✅ Correct Answer: (a) 40 mg/dl – 40 mg/dl
🟢 Infants are considered hypoglycemic when glucose < 40 mg/dl in the first few hours after birth.
2) Commonest cause of Neonatal death in India……Common cause of Neonatal death in India…..
(a) Prematurity
(b) Metabolic Disease
(c) Birth Injury
(d) Congenital Malformation
✅ Correct Answer: (a) Prematurity
🟢 Prematurity leads to organ immaturity, especially lungs, causing high neonatal mortality in India.
3) Herniation of abdominal organ into umbilical cord is known as ……. Abdominal organ into the umbilical cord is called herniation.
(a) Fistula
(b) Ascites – Ascites
(c) Omphalocele
(d) Intussusception -Intussusception
✅ Correct Answer: (c) Omphalocele – Omphalocele
🟢 Omphalocele is a congenital defect where intestines/organs protrude into the umbilical cord in a sac.
4) Treatment of choice for severe dehydration in infant is…….Infant ma seivyr dehidrashanma choisy af treitmant…..
(a)Mother milk & Household fluid – Mother milk and household milk
(b) ORS & Antibiotics – O. R. S. and antibiotics
(c) Mother’s milk & Antibiotics – Mother’s milk & ORS – Mother’s milk & ORS
(d) Mother’s milk & ORS
✅ Correct Answer: (b) ORS & Antibiotics – ORS & Antibiotics
🟢 ORS corrects fluid-electrolyte loss; antibiotics are given if infection is the cause of diarrhea.
5) Which of the following is an indication for tonsillectomy? Which of the following is an indication for tonsillectomy? :
(a) Rheumatic Fever
(b) Recurrent upper Respiratory tract invection
(c) Persistent carrier of Diphtheria Bacilli
(d) C & B
✅ Correct Answer: (d) C & B – Persistent diphtheria carrier & Recurrent URTI
🟢 Tonsillectomy is recommended in chronic/recurrent throat infections and persistent diphtheria carriers.