ENGLISH-22/02/2018 (GNM : 2nd year Child health nursing)(Done)PAPER NO-1O
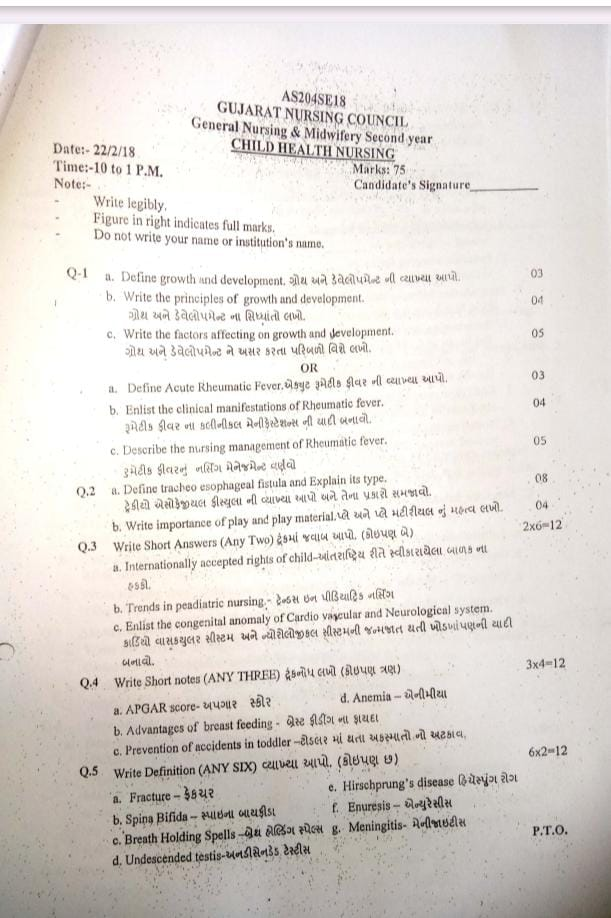
2nd year Child health nursing 22/02/2018 PAPER SOLUTION NO.10
Q-1
a. Define growth and development. Define growth and development.03
Growth
Growth is a physical maturation process in which the number and size of body tissues increase and the size or number of body organs increase. The increase in growth is due to cell division and the increase in the components inside the cells, which leads to the growth of the body. The changes in the body due to growth are measured in inches/centimeters and pounds/kilograms. Growth is progressive and measurable in which Height and weight increase. With good nutrition, proper growth is seen according to age, so eating good food leads to good growth.
OR
Growth is physical maturation in which the size and shape of various organs of the body increase. Which is seen due to the multiplication of cells and increase in intracellular substance. The change in growth can be measured in centimeters and kilograms.
Development : Development:
Development is the process by which the body matures functionally and physiologically. Development involves an increase in skills and capacity to function. Psychological, emotional and social changes occur. Development is difficult to measure, but it can be measured.
b. Write the principles of growth and development. Write the principles of growth and development.04
- Growth and development are closely related to each other. In a child, growth and development occur in parallel and continuum.
- We use the words growth and development interchangeably. But the two words are not the same. They have different meanings. Both cannot be used interchangeably, we use both the terms together for the sake of simplicity.
- It is very important to understand the characteristics and principles of growth and development in children, which are given below.
- Growth and development is a continuous process. It is unique for every child. Along with this, it also follows the pattern of individual differences.
- The pattern of growth and development in each child is seen according to his stage. It can be predicted. The stages are similar for all children, but the time to achieve those stages may vary. E.g. Every child learns to sit, learns to speak, but the time to achieve this function is different for all children.
- Growth is seen in the size and shape of each organ and in its coordination.
- Growth and development are seen according to these principles: Cephalo-caudal i.e. from head to tail and Proximo-distal i.e. from the midline and center to the periphery.
- Growth and development are seen according to these principles: Simple to Complex. In which initially mass movement and activity are seen in simple patterns. Over time, it is seen in specific actions and responses i.e. complex tasks.
- Development is mainly seen due to stimulation. In this, as the child is given stimulation, his development is seen better.
- Growth and development are interdependent on many factors such as hereditary and environmental.
- The influence of society is particularly visible on the growth and development of a child. Development is also based on cultural aspects.
- In growth and development, physical, mental, social, emotional activities are found in a positive correlation and all those factors are connected to each other.
- Growth and development is sometimes fast, sometimes slow and sometimes stable.
c. Write the factors affecting on growth and development. Write about the factors affecting growth and development.05
Factors affecting growth and development
Some factors that promote or inhibit the process of growth. There are two factors. Environmental factors
Hereditary factors
(1) Hereditary factors
- Genetic factors are important factors that affect the growth and development of a child. They affect height, body structure, skin color, eyes, and hair.
- Which depends on the genes of the parents. If the height of the parents is high, then the height of their child will also be high, if the parents are highly intelligent, then their child will also be highly intelligent, like some factors that affect the child.
- Some genetic diseases that affect the growth and development of the child such as thalassemia, hemophilia.
- So the child also has a chromosomal abnormality along with that disease in which Down is seen.
- In addition to this, gender also affects the growth and development of the child. If a male baby is heavier and longer than a female baby, girls mature earlier than boys. But the height and weight are less in comparison to boys.
- In race and nationality, different races also grow and develop at different times, and their physical characteristics differ depending on the national group.
(2)Environmental Factors
Prenatal Factors
Intra-uterine environment affects the growth and development of the fetus
Maternal Malnutrition
If the mother does not take a proper diet during pregnancy and develops anemia If present, intrauterine growth retardation, low birth weight, preterm baby and disturbances in growth and development occur in later life.
Maternal Infection
Some intrauterine infections such as HIV, hepatitis are transmitted to the fetus through the placenta and affect its growth and development. Due to which congenital anomalies and congenital infections are seen.
Maternal Substance Abuse
Some teratogenic drugs, when taken during pregnancy, can cause congenital malformations, and smoking, tobacco, and alcohol also affect growth and development.
Maternal Illness
Conditions like hypertension, anemia, heart disease, hypothyroidism, diabetes, chronic renal failure, hyper pyrexia etc. which affect the growth of the fetus. If iodine deficiency is found in the mother, then the baby may suffer from mental retardation.
Miscellaneous
Prenatal conditions that affect the growth of the fetus. Which affects the growth and development of the fetus such as uterine malformation, malposition of the fetus, bicornuate uterus, oligohydroamnios, polyhydramnios etc.
Postnatal Environmental Factors:
Growth Pattern
Growth pattern is according to the size of the baby at birth. If the baby has a low birth weight, complications may occur later.
Nutrition
Nutrition is very important for the growth and development of the child. It should be quality and quantitative nutrition. It should contain protein, carbohydrates, vitamins, fats and minerals in sufficient quantities which help in the growth and development of the child. If the child is well nourished then physical and mental growth is seen well.
Childhood Illness
Heart disease, kidney, liver malignancy, digestive disorders, metabolic disorders, etc. affect the growth and development of the child.
Physical Environment
Environmental conditions such as housing, its living conditions, environmental sanitation, ventilation, fresh air, hygiene, safe water supply, affect growth and development.
Psychological Environment
A good psychological environment such as a healthy family, a good parent-child relationship, and healthy interactions with other family members helps in emotional, social, and intellectual development. If a child does not get proper love, affection, and security, he or she becomes emotionally disturbed.
Cultural Influence
Culture affects growth and development. According to culture, its food habits, its beliefs, its living standard, education level, etc. affect growth and development.
Socioeconomic Status
Due to poor socio-economic status, a child cannot grow and develop properly and cannot get a proper nutritional diet.
Climate and Season.
Climate and season affect growth. Weight gain occurs in summer. Height increases in spring season compared to rainy season.
Play and Exercise
Play and exercise increase physiological activity and muscular development, as well as physiological, social, moral, intellectual development, and physical exercise improves health.
Intelligence
Which affects mental and social development. If a child has high intelligence, he will be able to adapt to the environment. If there is low intelligence, then it will not be able to be exhausted.
Hormonal Influence
Hormones greatly affect the growth and development of the child. Due to imbalance in them, problems are seen in growth and development.
OR
a. Define Acute Rheumatic Fever.03
Rheumatic fever is an autoimmune collagen disease that is usually caused by a hypersensitivity reaction to group A, B-hemolytic streptococcal (GABHs) infection.
Rheumatic fever is characterized by inflammatory lesions of connective tissue and endothelial tissue. It commonly affects the heart, joints, blood vessels, and other connective tissues, mainly affecting the cardiac valves (mainly the mitral valve). This disease is usually seen mainly in children between the ages of 5 and 15 years.
Rheumatic fever is usually caused by genetic conditions, environmental factors, unhygienic living conditions,
Poor dietary intake.
b. Enlist the clinical manifestations of Rheumatic fever04
- Fever,
- Joint pain,
- Cardiac symptoms such as,
- Carditis,
- Heart murmur,
- Chest pain.
- Skin rashes,
- Subcutaneous nodules,
- Chorea (involuntary, rapid movement),
- Fatigue,
- Abdominal pain,
- Headache,
- Tachycardia,
- Malaise,
- Sweating,
- Skin rash,
- Epistaxis,
- Anemia,
- Weight loss,
- Weakness,
- Shortness of breath,
- Swelling of lymph nodes,
- Abdominal pain.
c. Describe the nursing management of Rheumatic fever. Describe the nursing management of rheumatic fever05
- Provide continuous bedrest to the child.
- Continuously monitor the child’s body temperature.
- Provide adequate nutritious and bland diet to the child.
- Get adequate information from the child’s parents.
- Get all the laboratory tests done on the child.
- Get information about the child’s sleep pattern.
- Give the child complete bed rest.
- Check the child’s vital signs such as temperature, pulse, respiration, blood pressure, etc.
- Check the child’s heart sound.
- Give the child the prescribed medicine.
- Listen to the child’s breathing rate and see if there are any abnormalities.
- Change the child’s position every two hours.
- Tell the child to do deep breathing exercises every 1 to 2 hours.
- Feed the child in small amounts and frequently.
- Give oxygen to the child if he/she needs it.
- Check the child’s intake output.
- Check the child’s daily weight.
- Give supplements if necessary.
- Monitor the child to see if there are any complications.
- Give the child food with less salt, less oil and less calories.
- Tell the child not to add salt to the food.
- Tell the child to do their daily routine activities in small amounts.
- Provide psychological support to the child.
- Ask the child to express his feelings.
- Ask the child to do Mind Diversification Therapy.
- Explain all the procedures for the disease and its treatment to the child and his family members.
- Providing proper knowledge about the child’s diet and follow-up.
Q.2
a. Define tracheoesophageal fistula and explain its type. Define tracheoesophageal fistula and explain its types.08
Tracheoesophageal fistula is an abnormal communication between the esophagus (the tube that is responsible for passing food from the mouth to the stomach) and the trachea (the tube that carries air to the lungs and works to take air from the lungs).
Tracheoesophageal fistula is a congenital anomaly in which the esophagus There is an abnormal communication/connection between the trachea and the larynx. This type of congenital disorder is usually seen in premature children, low birth weight children, and children whose mothers have polyhydramnios. Children with this condition of tracheoesophageal fistula also have congenital heart disease and gastrointestinal (GI) anomalies.
Five types of tracheoesophageal fistula.
Type A: Without Fistula:
In this type, there is no communication between the esophagus and the trachea, there is a blind pouch and the upper segment of the esophagus ( Proximal) is a blind pouch and its lower segment (distal) is also a blind pouch.
Type B : Tracheoesophageal fistula (upper segment):
In this type, the upper segment (proximal) of the esophagus forms a fistula (abnormal communication) with the trachea while the lower segment (distal) of the esophagus is a blind pouch.
Type C : Tracheoesophageal Tracheoesophageal fistula (lower segment):
In this type, the upper segment (proximal) of the esophagus is a blind pouch while the lower part (distal) of the esophagus forms a fistula with the trachea.
Type D: Tracheoesophageal fistula (upper segment and lower segment communication):
In this type, the upper and lower parts of the esophagus are abnormally connected to the trachea. Communicates.
Type E : H Type( H Type):
This type does not have a blind pouch of the esophagus but it forms an abnormal communication with the trachea, forming an H-shaped tracheoesophageal fistula.
b. Write importance of play and play material. Write the importance of play and play material.04
Importance of play and play material:
Introduction:
Play is a natural and essential activity in a child’s life. It is not limited to entertainment alone, but it acts as a medically proven tool for the overall development of the child. Play and appropriate play materials are essential for a child’s neurological, cognitive, emotional, and social development. Various types of play activities strengthen the synaptic connections in the patient’s brain, which helps in increasing his learning potential.
1. Neurological and Cognitive Development:
During play, the child’s brain is engaged in a variety of new cognitive activities, due to which the activity in the cerebral cortex and hippocampus of the brain increases. Play materials such as puzzles, cubes, and board games increase cognitive skills such as attention, memory, and problem-solving ability.
2.Fine and gross motor development:
When a child does physical activities, his motor development occurs. Play materials such as balls, skipping ropes, or climbing frames strengthen gross muscles. While blocks, craft tools, etc. develop fine motor skills. These activities develop the musculoskeletal system.
3. Emotional and behavioral regulation:
Play provides a platform for the patient to understand and express their emotions. Therapeutic play helps reduce negative emotional states such as anxiety, fear, and stress in patients. Medical play is especially useful for patients who require surgical or long-term treatment.
4. Social and Communication Skills:
Group play or cooperative play develops social skills such as sharing, turn taking, and leadership in patients. In the preschool age group, children can understand the perspective of others through role play, which provides the basis for developing empathy and interpersonal relationships.
5.Health care and therapeutic value:
Play is a therapy for patients admitted to the hospital. During pain, play helps in the release of endorphins from the patient’s brain, which are called natural painkillers. In the case of children, child life specialists use play to reduce negative reactions during medical interventions. Play is also useful in managing the trauma response of the patient.
Play and play materials are the basis for the multi-dimensional growth of the child. They are useful from medical, psychological and social angles. Every patient needs to get the space of play and play materials according to the age. It is not only for entertainment, but also works as a therapeutic tool that gives long-term effect in the life of the child.
Q.3 Write Short Answers (Any Two) Give a short answer. (Any two) 2X6=12
a. Internationally accepted rights of child-
The rights of children were declared by the United Nations on 20 November 1959. They were made with the aim of fulfilling the special needs of the child.
These rights are as follows.
- No right to free education.
- No right to name and nationality.
- Right to special care if the child is handicapped. Right to affection, love and good understanding.
- Right to adequate quality nutrition. The right to receive first aid or relief in times of any calamity or distress.
- The right to receive good medical care. The right to play well and to have recreational facilities.
- The right to develop one’s abilities and become a useful member of society. The right to be brought up in a peaceful and fraternal environment.
- All the above rights are also the right of children to exercise all rights equally without discrimination of religion, caste, creed, sex, color, etc.
b. Trends in pediatric nursing
- In the past, adults and children were given the same treatment. But currently, due to the high mortality and morbidity seen in the pediatric age group, more importance has been given to children and child care.
- In addition, due to the development in the medical and surgical branches, the focus is on the special area of child health.
The following trends and practices are being seen in child health care in pediatrics. - Currently, pediatric care is provided by pediatricians and trained registered nurses.
A scientific treatment approach is maintained in care from infancy to adolescence period. is. - Special vaccines are administered for the prevention of diseases.
Regular assessment of the child’s growth and development is done. - Instead of curative care, emphasis is placed on preventive services and health promotion.
Advancement of technology and science is seen in the medical field. So that high quality care can be provided. - Evidence-based practice is seen in the care of children.
More emphasis is placed on institutional care instead of home care for any kind of care for children. This institute i.e. hospital which has been developed with changes that are liked by children through modernization. - Family-centered care is provided in every care of the child under the supervision of health care members with the support of parents and family members. Even during illness, the child is not separated from his parents and family members.
- Rooming in, that is, keeping the child with his mother as much as possible and keeping the mother with him in every care, is implemented.
- During the hospitalization of children, their visiting hours have been increased and flexible hours have been kept.
- There is a support group for parents, which helps in reducing the anxiety of the parents. And the play and recreational needs of children are taken into consideration.
- In the care of children, sub-specialties of pediatric services such as neurology, cardiology, nephrology, etc. have developed.
- Cost containment means providing the best care at low cost and preventing duplication of nursing care.
- Preventive care involves such efforts that the health of the child can be improved at low cost and the care can be protected against diseases.
- Continuity of care is provided in continuity of care. If a child is hospitalized due to an acute disease without any interference, then after giving treatment in the hospital for a few days, the further treatment is given to the child outdoors. Thus, continuity of drug is maintained.
- Color coded management with Green classification = Child does not need medicine but needs advanced home care. Pink classification = Child needs to be provided care like a patient. Yellow classification = Child needs specific treatment at home.
c. Enlist the congenital anomaly of Cardio vascular and Neurological system. List the congenital anomalies of the cardiovascular system and the neurological system.
Congenital Anomalies of the Cardiovascular System
(Congenital Anomalies of the Cardiovascular System)
- Atrial Septal Defect (ASD) – Atrial Septal Defect
- Ventricular Septal Defect (VSD)
- Patent Ductus Arteriosus (PDA)
- Tetralogy of Fallot (TOF)
- Transposition of the Great Arteries (TGA)
- Transposition of the Great Arteries (TGA)
- Tricuspid Atresia
- Pulmonary Stenosis
- Aortic Stenosis
- Coarctation of Aorta
- Total Anomalous Pulmonary Venous Connection (TAPVC) Connection
- Truncus Arteriosus
- Pulmonary Atresia
- Hypoplastic Left Heart Syndrome
- Ebstein’s Anomaly
- Double Outlet Right Ventricle (DORV) – Double Outlet Right Ventricle
- Single Ventricle Defect – Single Ventricle Defect
Congenital Anomalies of the Neurological System
(Congenital Anomalies of the Neurological System)
- Anencephaly
- Spina Bifida
- Meningocele
- Myelomeningocele
- Hydrocephalus
- Microcephaly
- Lissencephaly
- Dandy-Walker Syndrome
- Chiari Malformation
- Cerebral Palsy
- Encephalocele
- Holoprosencephaly
- Tuberous Sclerosis
- Sturge-Weber Syndrome
- Congenital Muscular Dystrophy
- Neural Tube Defects (NTDs)
- Craniosynostosis
Q.4 Write short notes (ANY THREE) 3X4=12
a. APGAR score-
The Apgar scoring was developed in 1952 by obstetric anesthesiologist Virginia Apgar and has become the standard method for evaluating newborns. Apgar is an instant, quick, and complete assessment of the health of a newborn or neonate or it is a practical method for evaluating a neonate or newborn. The APGAR score is the most important part of immediate newborn care.
The APGAR score is,
1) Immediately after birth,
2) 1 minute after birth
3) 5 minutes after birth. The Apgar scoring performed at one minute provides information about the baby’s physical health and helps the physician assess and decide whether immediate or future medical treatment will be needed.
While, the 5-minute Apgar score, if performed, provides information about the baby’s response to pre-resuscitation measures.
In the APGAR score,
A:= Appearance
(Skin Color),
P:=Pulse (Heart Rate),
G:=Grimes (Reflux Irritability),
A:=Activity
(Muscle Tone),
R:=Respiration (Respiratory Efforts)
are assessed.
Five Criteria of the Apgar Score:
1) (A: Appearance) Skin Color:
Score 0: Complete Body blue or pale.
Score 01: Body pink and extremities blue.
Score 02: Body and extremities pink, no cyanosis seen.
2) P: Pulse rate:
Score 0: Sebaceous.
Score 01: Less than 100 pulses per minute.
Score 02: More than 100 pulses per minute.
3) G: Grimace (reflex irritability)
Score 0 : No response to stimulation.
Score 01 : Grimaces on suction or aggressive stimulation.
Score 01 : Crying on stimulation.
4) A : Activity:
Score 0 : None.
Score 01 : Some flexion.
Score 02 : Flexed arms and legs that resist extension.
5) R : Respiratory effects:
Score 0 : Absent,
Score 01: Weak irregular and gasping,
Score 02: Strong and lusty.
The total score of the APGAR score is 0-10.
•> APGAR score at 1 minute after birth:
If the Apgar score is between 7-10, it is considered normal, meaning no depression, in which the baby is provided with normal post-delivery routine care.
If the APGAR score is between 4-6, it indicates mild depression, in which the child requires assistance for breathing.
If the APGAR score is between 0-3, it indicates severe depression, in which the child requires resuscitation.
•> APGAR score at 5 minutes after birth:
If the APGAR score is between 7-10, it is considered normal,
but if the Apgar score is below 7, then the baby needs to be monitored for another half hour.
d. Anemia –
Anemia is the most common blood disorder seen in infants and children. It is usually found in areas with poor socioeconomic conditions. Anemia is a condition in which the circulating red blood cells and hemoglobin levels are lower than their normal levels (reduced number). Due to this, the oxygen carrying capacity of the red blood cells decreases. It is usually seen due to various reasons such as nutritional deficiency (iron, vitamin B12, or folate), chronic disease, genetic condition, and blood loss.
Different blood levels according to age
Children 6 months to 6 years:= 11gm/ dl.
Children 6 years to 14 years:= 12 gm/ dl.
Above 14 years in male:=13 gm/ dl.
Female:= 12 gm/ dl.
If the hemoglobin level in a child is between 10 gm/ dl – 11 gm/ dl, it is called mild anemia.
If the hemoglobin level in a child is 7 If it is between gm/dl – 10 gm/dl, it is called moderate anemia.
If the hemoglobin level in the child is less than 7 gm/dl, it is called severe anemia.
Etiology/ cause of the Anemia:
- Due to nutritional deficiency.
- Chronic diseases Due to.
- Due to genetic factors.
- Due to blood loss.
- Due to infection.
- Due to bone marrow disorders.
- Due to vitamin deficiency.
- Impaired production of red blood cells Due to.
- Due to excessive amount of blood loss.
- Due to decreased production of red blood cells.
Clinical manifestation/ sign and symptoms of the Anemia:
- Fatigue,
- Weakness,
- Paleness of the skin, conjunctiva and mucous membranes,
- Shortness of breath,
- Dizziness,
- Headache,
- Rapid and irregular heartbeat,
- Cold hands and feet.
- Brittle nails.
- Poor concentration.
- Cognitive difficulties.
- Growth and development delays.
- Loss of appetite.
- Dizziness.
- Tachypnea.
- Tachycardia.
- Palpitation.
- Diarrhea and vomiting.
- Cardiac enlargement with murmur sound.
- Jaundice in some cases, Petechiae and ecchymosis may also be present.
- Hepatomegaly may occur.
Diagnostic evaluation of the Anemia:
- History taking and physical examination,
- Complete blood count test.
- Peripheral blood smear.
- Additional blood tests.
- Bone marrow aspiration and biopsy.
- Imaging tests.
- X-ray.
- CT scan.
- M .R .I.
- Genetic Testing.
- Stool Examination
Management of the Anemia:
- Assess the cause of anemia in the child.
- If the child’s anemia condition is due to nutritional deficiency, provide the child with adequate nutritional supplements such as iron, vitamin B12 and folate.
- Provide the child with a properly iron-rich nutritious diet.
- Provide the child with adequate nutritional supplements according to the nutritional deficiency. Provide supplementary diet.
- If the child’s anemia condition is due to any infection or chronic disease, then treat the child for that condition immediately.
- If the child has a severe anemia condition, then do proper blood transfusion.
- Monitor the child regularly.
- If the child’s anemia condition is due to excessive blood loss, then stop it and start intravenous infusion. Start immediately.
- Provide complete education to the child and his/her family members about the child’s condition, its causes, its symptoms and signs, and its treatment.
- Do all the laboratory investigations of the child.
- Do regular screening of the child to prevent the child from the condition of anemia.
b. Advantages of breast feeding
- Breastfeeding develops a psychological bond between mother and baby.
- Human milk is available to the baby at the body temperature required.
- Milk is fresh, sterile and free from contamination and goes directly into the baby’s mouth.
- Human milk is ideal when it is readily available.
- Breast milk is a safe and protective food, the perfect food for infants.
- It meets the total nutrient requirements of the baby for the first six months.
- It is very important for the baby’s brain growth because breast milk contains a high amount of lactose and galactose.
- Breast milk contains vitamins, minerals, electrolytes and water which are very important for the maturation of the infant’s intestinal system. It is necessary.
- Breast milk provides such a facility that the absorption of calcium increases so that the growth of the baby’s bones improves.
- Breast milk is easily digested.
- Breast milk contains all the necessary nutrients that the baby needs.
- Breast milk protects the baby from infection and deficiency.
Breast milk is already prepared.
Breast Feeding is a method of family planning, breastfeeding is a natural contraception that has a major impact on the population in developing countries. - It prevents children from diarrhea and also has a laxative action.
- Breastfeeding does not have any dangerous allergic effects.
- Breastfeeding can save time, money and energy.
- Breastfeeding is good for the health of mother and child. Helps in building relationships.
- The chances of conception are reduced during lactation.
- Best feeding helps in involution of the uterus (i.e. bringing the uterus to a pre-pregnant state).
- Breastfeeding reduces the chances of sunburn, gastrointestinal infections and ectopic eczema,
and also reduces the chances of scurvy and rickets. - Breastfeeding reduces the chances of breast cancer.
- Breast milk contains IgA and IgM macrophages, lymphocytes, lysosomes, etc., due to which diarrhea and acute respiratory infections can be prevented in babies.
And it prevents malaria and viral and bacterial infections. - Breast milk protects against conversion, hypocalcemia, tetanus, deficiency of vitamin E and zinc.
- Exclusive breastfeeding can prevent malnutrition in children.
- Breastfeeding increases the intelligence of the child, and the child feels secure (due to the infant-mother bond)
- The chances of illness in the child are reduced.
- Breastfeeding reduces the chances of postpartum hemorrhage (in which there is excessive bleeding from the genital tract after delivery).
- The chances of ovarian cancer are also reduced.
- It helps in reducing the excess fat stored in the mother during pregnancy.
c. Prevention of accidents in toddler – Prevention of accidents in toddlers.
Prevention of Accidents in Toddler
(Prevention of Accidents in Toddler)
Toddler stage is that stage of life where a child’s motor skills develop rapidly and his interaction with the surrounding environment also increases. In this stage, the patient is very restless and curious but does not understand the dangers. As a result, such patients are more likely to suffer from various types of accidents such as falls, burns, poisoning, drowning, electrical injuries, and trauma.
To prevent such accidents in toddlers, the following steps should be carefully adopted:
1. Continuous observation and supervision:
Never leave a toddler patient alone at any time. Visual observation by an adult is essential during every activity.
2. Removing household hazards:
Keep sharp corners of furniture, glassware, sharp objects, poisonous substances, medications, etc. out of toddler’s reach.
3. Electrical Safety:
Install safety covers on power sockets. Loose wiring, unprotected electrical equipment, charging points, etc. should not be around toddlers.
4. Safety on Staircases and High Places:
Install childproof gates on staircases and have fall protection on all high places.
5. Prevention from hot things:
Take special care to ensure that stoves, hot water, heaters or hot food do not come into contact with toddlers.
6. Prevent Poisoning:
Store toxic substances such as cleaning agents, insecticides, bathroom products, etc. in childproof boxes.
7. Prevent Drowning:
Do not leave toddlers alone in tubs, buckets, pots, etc. filled with water. Maintain strong supervision near water bodies.
8. Prevent Aspiration:
Do not give toys, beads, nuts, etc. with small parts to toddlers. Toys should be age-appropriate.
9. Fire Safety:
There should be a smoke detector in the home. Parents or caregivers should be trained in CPR (Cardiopulmonary Resuscitation) so that the patient can respond immediately in an emergency situation.
10. Safety during sleeptime:
Install a roll-over guard at the corner of the crib or bed. The sleeping area on the cot should be flat and free of obstructions.
11. Safety during driving:
It is not safe to carry a toddler patient in a car without a child seat or on the lap. Proper restraint is necessary for vehicle safety.
12. Play Area should be safe:
The play area should be non-slippery and there should be no electrical or mechanical hazards.
Conclusion:
Accidents in toddlers affect their development and can cause physical and mental trauma. To prevent such accidents, active observation by parents and caregivers, safety precautions in the home, and being alert for toddler patients are very important. Better treatment than disease is advanced protection, and this position is supported for the safety of toddlers.
Q.5 Write Definition (ANY SIX) Give the definition. (Any six) 6X2=12
a. Fracture-
Fracture is a breakdown in the continuity of a bone.
A fracture is a break in the structure of a bone. A fracture involves the bone, its tissues, bone marrow, and periosteum.
A fracture of a bone can be either partial or complete.
e. Hirschsprung’s disease
Hirschsprung Disease is a congenital neurogenic disease of the intestine, in which ganglion cells (nerve cells) are not present in a certain part of the large intestine, due to which that part cannot perform peristaltic movement and stool does not move forward, resulting in obstruction. This disease mainly affects the rectum and sigmoid colon and presents in newborns with symptoms such as delayed passage of meconium, abdominal distension, and constipation. Diagnosis is by rectal biopsy, manometry, and barium enema, and treatment involves surgical removal of the affected intestine.
f. Enuresis – Enuresis
Enuresis is a common pediatric problem in which a child experiences frequent involuntary urination while sleeping. The condition of frequent involuntary urination while sleeping, when voluntary urine control should normally be achieved, is called enuresis. And this condition is seen in a child even after 5 years. Enuresis (bedwetting) is also called nighttime incontinence.
b. Spina Bifida – Spina Bifida
Spina bifida is a congenital neural tube defect. The neural tube is responsible for forming and closing the spinal cord and brain during early embryonic development. When the spinal cord forms, it does not close completely, leaving a gap between the vertebrae. This incomplete spinal cord closure results in various malformations of the spinal cord and spinal column.
When the vertebral column fails to close and a space is left between them, tissue is exposed from this bony space and a sac-like structure protrudes outward. Spina bifida is called.
c. Breath Holding Spells
Breath holding spells are a common situational disorder.
Breath holding spells are also called “infantile syncope”.
Breath holding spells are involuntary reflexive episodes and psychosomatic disorders that are mainly seen in young children, i.e. children between six months and six years of age. In a breath holding spell, when a child cries, his breathing is held involuntarily for a short time. Breathing is temporarily held and due to this, the child loses consciousness. This breath holding spell is seen during anger, festration.
During a breath holding spell, the child loses consciousness, cyanosis is seen and twitching and tonic-clonic movements are also seen in the child. The child becomes limp, lifeless and very pale. And the heart rate slows down and laryngeal spasms are seen and this type of attack lasts for one to two minutes.
g Meningitis- Meningitis
Meninges: Meninges are the protective membranes of the brain and spinal cord that cover the brain and spinal cord. These meninges have three other layers.
1) Duratea
(outermost layer),
2) Arachnoid mater
(intermediate layer),
3) Pia mater
(innermost layer)
Thus, there are three layers of meninges that cover and protect the brain and spinal cord.
Meningitis: When there is infection and inflammation in the meninges layer surrounding the brain and spinal cord, the condition is called meningitis. This infection can be caused by bacteria, viruses, and microorganisms.
d. Undescended testis
Undescended testis, also known as “cryptorchidism”, is a condition in which one or both testicles fail to move down from the abdomen into the scrotum before they are born. This condition can affect the development and function of the testicles. This condition is more commonly seen in premature infants. Normally, the testes are present in the abdominal area of the fetus until 7 months of intrauterine life and these testes descend into the scrotum between 8 and 9 months of intrauterine life. When due to some type of factor, these testes do not descend into the scrotum and the testes remain present in the abdominal area of the newborn, this condition is called undescended testes.
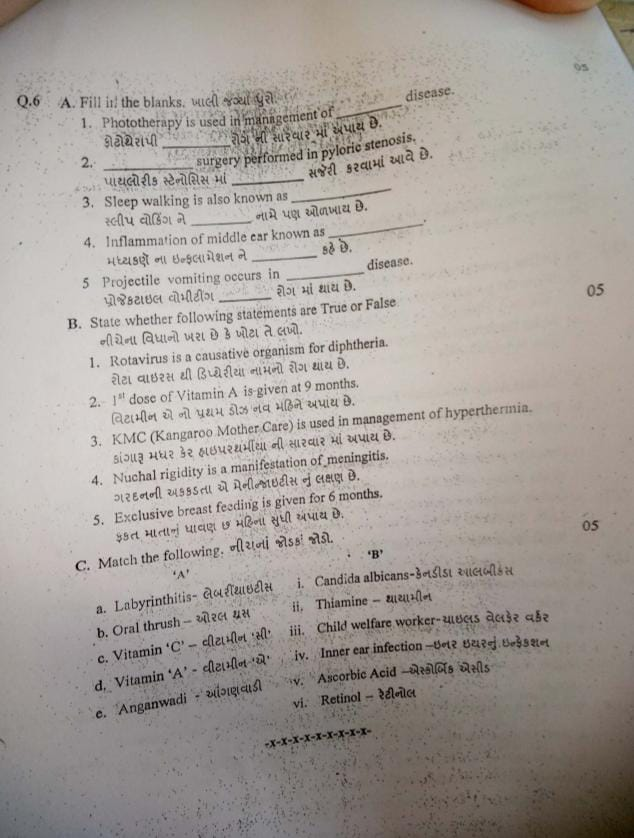
Q.6 A. Fill in the blanks, 05
1.Phototherapy is used in management of ………………. Phototherapy ……………………………..is used in the treatment of diseases.
✅ Neonatal Jaundice.
Phototherapy is used in the treatment of neonate jaundice .
2………………..surgery performed in pyloric stenosis. In pathological stenosis………………. surgery is performed.
✅ Pyloromyotomy
In pathological stenosis, pyloromyotomy surgery is performed.
3. Inflammation of middle ear known as……………. Inflammation of the middle ear is called ……………..
✅Otitis media. Inflammation of the middle ear is called otitis media . Inflammation of the middle ear is called otitis media .
4. Sleep walking is also known as…………….. Sleep walking is also known as………………….
✅Somnambulism.
Sleep walking is also known as Somnambulism .
5 Projectile vomiting occurs in ………………. disease. Projectile vomiting occurs in ………………….disease.
✅Pyloric stenosis disease.
Projectile vomiting Pyloric stenosis disease.
B. State whether the following statements are True or False. 05
- Rotavirus is a causative organism for diphtheria. Rotavirus causes a disease called diphtheria: ❌
✅ Correct: Rotavirus is a causative organism for diarrhea.
🔁 Rotavirus causes diarrhea. The cause of diphtheria is — Corynebacterium diphtheriae. - 1 dose of Vitamin A is given at 9 months. First dose of Vitamin A is given at 9 months. ✅ 1 dose of Vitamin A is given at 9 months.👍 First dose of Vitamin A is given at 9 months.
- KMC (Kangaroo Mother Care) is used in management of hyperthermia. : ❌
✅ Correct: KMC is used in management of hypothermia (low body temperature).
🔁 Nuchal rigidity is a manifestation of meningitis.✅ Nuchal rigidity is a manifestation of meningitis.👍 Neck stiffness is also a symptom of meningitis. - Exclusive breast feeding is given for 6 months. Exclusive breast feeding is given for 6 months.✅ Exclusive breast feeding is given for 6 months.👍 Exclusive breast feeding is given for 6 months.
C. Match the following. Match the pairs of ‘Nira’. A 05
‘A’ ‘B’
a. Labyrinthitis- Labyrinthitis i. Candida albicans-Candida albicans
b. Oral thrush-Oral thrush ii. Thiamine
c. Vitamin ‘C’ – Vitamin C iii. Child welfare worker
d. Vitamin ‘A’ – Vitamin A iv. Inner ear infection-Infection of the inner ear
e. Anganwadi v, Ascorbic Acid
vi. Retinol– Retinol
✅ Matching Order(Answer):
a → iv
b → i
c → v
d → vi
e → iii