ENGLISH-MENTAL HEALTH NURSING (SECOND YEAR)PAPER SOLUTION : PAPER SOLUTION NO.12 (30/03/2022)
PAPER SOLUTION NO.12 (30/03/2022)
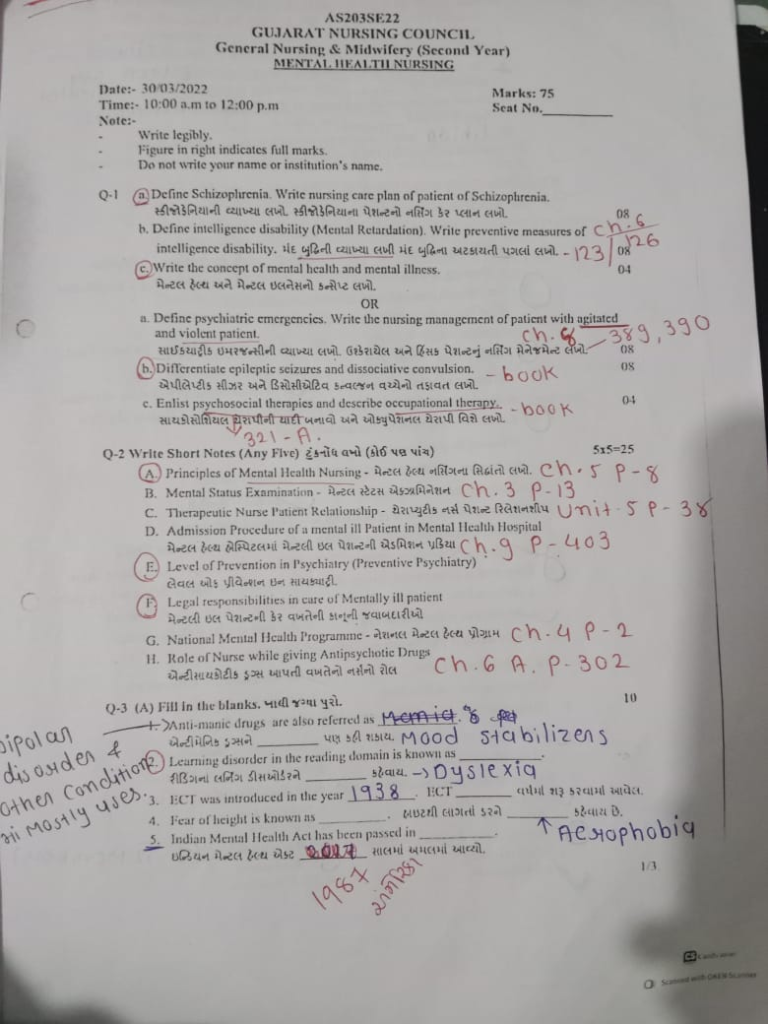
Q- 1
a.Define Schizophrenia. Write nursing care plan of patient of Schizophrenia. Write the definition of schizophrenia. Write a nursing care plan for a patient with schizophrenia.08
The term “schizophrenia” was coined by Eugen Bleuler in 1908.
The name derives from the Greek words “schizo-schizo” (split) and “phren-phren” (mind), meaning that fragmented thinking is commonly seen in this disorder.
Schizophrenia is a psychotic condition that is characterized by a disruption of the brain’s It affects normal functioning, which includes disturbances in a person’s thinking, emotion, and behavior functions. A person with schizophrenia experiences changes in behavior, perception, and thinking that can disconnect them from reality. When a person loses touch with reality, they experience psychosis.
Impaired Insight is a common feature of schizophrenia. The person who coined the term Schizophrenia is Eugen Bleuler.
OR
In 1908, psychiatrist Eugen Bleuler coined the term schizophrenia, which is derived from the Greek words skhizo (split) and phren (mind). Thus, schizophrenia is a psychotic condition in which
” Thinking, emotions, mood, and volition (Willpower) disturbances that usually lead to social withdrawal are called schizophrenia “which lasts more than a month
Schizophrenia is a very serious condition in which a person feels alienated from reality and has difficulty in thinking, acting and expressing his emotions.
Nursing care plan of patient of Schizophrenia (Nursing care plan of patient of Schizophrenia):
1.Nursing Diagnosis:
Disturbed Thought Process related to altered perception (hallucination or delusion)Thought disorder in which the patient is unable to connect with reality
Short-Term Goals:
The patient can recognize false thoughts that are driving their behavior.
The patient can remain calm during hallucinations.
Long-Term Goals:
The patient can differentiate between hallucinations and delusions.
Patient can learn reality testing.
Nursing Interventions:
- Talk to the patient calmly, directly, and clearly
- Ask about hallucinations: “Are you seeing or hearing something?”
- Gently remind for reality testing: “I know you’re feeling that way, but I’m not feeling anything like that.”
- Convince the patient not to act on the wrong idea.
- A safe space for the patient Prepare the environment: Remove excessive noise, darkness, and frightening objects. Encourage regular medication (antipsychotic) intake and monitor for effects. Nursing Diagnosis: Impaired Social Interaction related to poor reality contact and withdrawal (patient avoids contact with others and remains socially withdrawn). Short-Term Goals: Patient nurse or Have a small talk with the counselor
- Initially, one-to-one interaction begins Do.
- Gently motivate the patient for daily greetings, eye contact.
- Slowly expose to group therapy.
- Encourage positive social behavior (Positive reinforcement)
- Monitor regularly for withdrawal symptoms.
- Provide step-by-step instructions for hygiene.
- Keep items such as a mirror, toothbrush, and clean clothes available.
- If the patient does not do so, give a verbal reminder.
- Keep a daily checklist for self-care.
- Provide positive encouragement for independent care.
Be ready to move into a social environment
Long-Term Goals:
Participate in patient group activities
Be active in social settings
Nursing Interventions:
3.Nursing Diagnosis:
Self-Care Deficit (hygiene and grooming) related to apathy and cognitive impairment (Patient fails to care for themselves).
Short-Term Goals:
Patient performs activities such as bathing, changing clothes
Long-Term Goals:
Patient performs activities of daily living (ADLs) independently
Nursing Interventions:
4.Nursing Diagnosis:
Risk for Violence – Self or Others related to paranoid delusion or auditory hallucination (Patient may harm self or others)
Short-Term Goals:
Patient does not engage in any harmful behavior
Inform staff immediately if frightened.
Long-Term Goals:
Patient can control anger and distressing thoughts
Nursing Interventions:
- Continuously monitor for aggressive tendencies (restlessness, pacing, shouting).
- Provide patient with a calm and neutral environment.
- Maintain staff readiness – code for emergency.
- Inform the doctor to administer a tranquilizer or sedative.
- Support the patient and show love and acceptance.
Schizophrenia is one of the most challenging diseases in the field of mental health.
As nurses, our main goal is to:
- Keep the patient safe.
- Support medication and treatment.
- Try to shift the focus away from hallucinations and delusions and towards reality.
- Encourage the patient to resume their social and personal lives.
b. Define intelligence disability (Mental Retardation).Write preventive measures of intelligence disability, Write preventive measures of intelligence disability.08
Mental Retardation (Mental Retardation) :
- Mental retardation is also called “intellectual disabilities”.
- Mental retardation is a developmental condition in which a child’s cognitive and problem-solving skills are impaired. Also known as ‘cognitive developmental delay’.
- In which there are limitations in the child’s intellectual function and adaptive behavior.
- Mental retardation is a condition in which a child has difficulties in learning, thinking, problem solving, reasoning and understanding concepts compared to other children.
- These limitations can range from mild to profound.
Prevention is better than cure. This means that we should take steps to prevent a condition before it occurs.
There are three types of prevention of mental retardation:
1) Primary prevention
2) Secondary prevention
3) Tertiary prevention
1) Primary prevention:
- Primary prevention involves preventing the causes and factors that lead to mental retardation.
- Providing good antenatal, intranatal and postnatal care to the mother.
- Providing universal immunization to the child. Such as providing BCG vaccine, polio vaccine, DPT vaccine and MMR vaccine.
- Immunizing the mother and child against rubella so that mental retardation can be prevented.
- Giving folic acid medicine to the mother during the antenatal period in the first trimester. So that neural tube defects in the child can be prevented.
- Ask the mother to avoid toxic substances, alcohol, nicotine and cocaine during pregnancy.
-Prohibit the mother from coming into contact with radiation. - Provide nutritional supplementation during pregnancy.
- Use iodized salt so that diseases caused by iodine deficiency can be prevented.
- Genetic counseling of parents at risk To do.
- To eliminate the misconception in the community and provide health education to the people.
- To improve the socio-economic condition of the people.
- Avoid pregnancy before 21 years and after 35 years so that complications can be prevented.
- Keep the period between two pregnancies to be at least three years.
- In the mother’s Prevent Rh isoimmunization.
- Screening pregnant women for diseases like syphilis and rubella.
- Examining the fetus through immunostaining, fetoscopy, biopsy and ultrasound.
- Treating childhood diseases like diarrhea, brain infection and protein energy malnutrition.
- Providing a proper environment for the mental development of the child.
- Long-term exposure to lead affects brain development, so reduce pollution.
- Provide health education to the community about the causes and prevention of mental retardation.
2) Secondary prevention:
- Identify preventable diseases like measles, rubella early And to treat them properly.
- Identify conditions like hydrocephalus, galactosemia and provide treatment for them.
- Treat emotional and behavioral problems.
3) Tertiary prevention : (Tertiary prevention)
- Physical and To solve psychological problems.
- Hospitalizing severely mentally retarded patients and providing special care.
- Providing education and training to mentally retarded children so that they can be prevented from becoming mentally handicapped.
- Sending such children to special institutions where they are given education, training and work according to their capacity.
C.Write the concept of mental health and mental illness. Write the concept of mental health and mental illness.04
Mental health :- Mental health is a state of well-being in which each individual realizes his or her own abilities, can cope with the normal stresses of life, can work productively and fruitfully, and is able to make a contribution to his or her community.
Mental illness :- Mental illness means a mental health condition that affects a person’s mood, thinking, and behavior. Such as schizophrenia, depression, eating disorders.
Meaning of Mental Health (Concept of Mental Health):
Mental Health is an important part of human life, which directly affects a person’s thoughts, emotions, behavior and social relationships.
Mental health is a state in which a person can recognize themselves, handle their stress, produce results at work and make a positive contribution to society.
Key Key Features of Mental Health:
- Self-extensions (self-acceptance)
- Self-confidence and autonomy
- Ability to cope with stress
- Positive thoughts and feelings
- Healthy internal and social relationships
Meaning of Mental Illness (Concept of Mental Illness):
Mental Illness is a disorder in a person’s thinking, feelings, mood and behavior due to which the person cannot maintain his daily activities and relationships.
These diseases are medically recognized and can be controlled or treated through pharmacotherapy and psychotherapy.
Key Characteristics of Mental Illness:
- Incoherent thoughts and behavior
- Decreased functional ability in daily life.
- Behavioral instability and anxiety
- Delusions and hallucinations
- Decreased self-confidence and withdrawal.
OR
a. Define psychiatric emergencies. Write the nursing management of patient with agitated and violent patient. Write the definition of psychiatric emergencies. Write the management of agitated and violent patients.08
In a psychiatric emergency, there is a disturbance in the behavior, affect and thought of the person, which requires immediate treatment. For this, the following things are necessary,
A. The patient considers it necessary for his discomfort
B. According to the patient’s signs, family friends or authority consider it necessary
C. Due to the prognosis, doctors and nurses consider it necessary that if left untreated, it can be fatal.
Definition:
A psychiatric emergency is a sudden onset and abnormal disorder or socially inappropriate behavior due to an emotional or physiological situation.
Example.. suicidal episodes, acute psychotic reaction, acute alcoholism or acute anxiety.
Major emergencies:
• Suicidal patient
• Agitation and violent patient
Minor emergencies:
• Grief Reaction
• Rape
• Disaster
• Panic Attack
Medical emergencies seen in psychiatry:
• Delirium due to life-threatening conditions
• Neuroleptic malignant syndrome
• Serotonin syndrome
• Psychiatric medication overdose.
• Overdose or withdrawal of narcotics.
Nursing management of patient with agitated and violent patient (Nursing management of agitated and violent patient):
- This patient is disturbed, unmanageable and psychotic
- They are irrational, uncooperative, delusional, paranoid, aggressive and have hallucinations
- Treatment
- Inj.chlorpromazine 100mg IM ( for sedation) or inj. Diazepam 10-20 mg IV slowly
- Use a calm, quite, firm and unhurried approach
- In some psychotic conditions, ECT may be given when violence is seen
- Nursing care,
- Maintain a non-threatening approach, do not challenge the patient, speak in a low voice
- Isolate if necessary, minimum Keep in a room with furniture
- Minimize visitors
- Provide high calorie diet finger food
- Don’t s,
- Do not keep any weapon that can cause injury near the patient. Do not sit too close to the patient. Do not allow a relative or friend who provokes the patient to enter his room. Do not argue with the patient.
b. Differentiate epileptic seizures and dissociative convulsions. Write the difference between epileptic seizure and dissociative convulsion.08
Difference between epileptic seizure and dissociative convulsion:
1.Definition:
Epileptic seizure:
Epileptic seizure is a neurological condition caused by sudden and unstable changes in the electrical activity of the brain. It occurs as a result of dysfunctional signaling of neurons.
Dissociative Convulsion [also known as Functional Seizure or Pseudoseizure]:
This is a Non-Epileptic Attack resulting from psychogenic stress or internal mental conflict. There are convulsions without any Electrical Disturbance in the brain.
2.Cause
Epileptic Seizure:
Electrical Abnormality of the Brain
Brain Injury, Infection, Tumor, Genetic Factors
Dissociative Convulsions:
- Severe Emotional Trauma
- Psychiatric Illnesses
- Conversion Disorder
- History of Abuse or Stress
3.Electroencephalography (EEG -Electroencephalograph)
Epileptic Seizure:
Epileptic Activity is seen on EEG.
Dissociative Convulsion:
EEG is normal, no Electrical Abnormality is seen.
4.Clinical Presentation:
Epileptic Caesar:
- Abrupt Onset
- Tonic-Clonic Movements
- Tongue Bite, Urinary Incontinence
- Postictal Confusion
Dissociative Convulsions:
Psychotherapy, Cognitive Behavioral Therapy
Psychiatric Medication if necessary
Epileptic seizures are neurological disorders caused by electrical abnormalities in the brain, while dissociative seizures are a response to mental conflict that occurs without physiological activity in the brain. Accurate clinical observations and appropriate investigations are necessary for the diagnosis and treatment of both.
c. Enlist psychosocial therapies and describe occupational therapy. Enlist psychosocial therapies and describe occupational therapy. 04
Psychosocial therapy is a treatment method that affects the psychological and social life of the patient, and helps to improve his mental health.
The following are the main psychosocial therapies:
- Individual Psychotherapy
- Behavior Therapy
- Cognitive Behavior Therapy (CBT)
- Family Therapy
- Group Therapy
- Motivational Enhancement Therapy
- Occupational Therapy
- Social Skill Training
- Milieu Therapy
- Play Therapy – especially for children
- Music Therapy
- Art Therapy
Occupational Therapy:
- The primary goal of occupational therapy is to enable people to participate in their life activities. Occupational therapy helps people regain their independence in living activities.
- Some of the methods used for mental rehabilitation include housing placement (e.g., halfway homes, supervised housing), vocational training (shelter workshops, vocational guidance).
- In mental health, occupational therapy aims to help people with mental and to help cope with the challenges of daily life imposed by emotional illnesses.
- Occupational therapists identify problem areas and plan activities accordingly.
Problem areas in mental patients-
- Motor (e.g. psychomotor activity).
- Sensory (e.g. Hallucinations, Delusions)
- Cognitive (e.g. Decision Making, Problem Solving)
- Interpersonal (e.g. Self-Concept, Emotions)
- Interpersonal (e.g. Socialization, Communication)
- Self-Care (e.g. Basic and Instrumental Activities of Daily Living)
- Productivity (e.g. work, job)
- Leisure (e.g. interests, enjoyable activities)
- Occupational therapy approaches
. Break down and complete learning activities to achieve new teaching ways of approaching tasks - Teach adaptive activities
- Role of nurse…
The nurse should work for the good health and well-being of family groups and communities - The nurse should conduct an occupational assessment of the client
- Encourage the client to be involved in occupational therapy Should
- Therapists should help within the therapy
Q-2 Write Short Notes (Any Five) 5×5 = 25
A. Principles of Mental Health Nursing – Write the principles of Mental Health Nursing.
1.Patient is Accepted Exactly as He is (Patient is accepted exactly as he is)
Acceptance means being free from any kind of prejudice or judgment. Acceptance expresses feelings of love and care. Acceptance does not mean complete permission, but rather the setting of positive behaviors to respect him as an individual human being.
A. Being Non-judgmental and Non-punitive
The patient’s behavior is not judged as right or wrong, good or bad. The patient is not punished for his unwanted behavior. Punishment such as directly chaining, retraining, or keeping him in a separate room and indirectly ignoring his presence or deliberately ignoring or avoiding him. A nurse who shows acceptance does not reject a patient even when they behave contrary to her expectations.
B. Being Sincerely Interested in the Patient.
- Being genuinely interested in another person means taking into account the other person’s interests
- studying the patient’s behavior patterns
- allowing him to make his own choices and decisions as much as possible
- being aware of his likes and dislikes.
- being honest with him.
- Take time to listen to what he or she has to say.
- Avoid sensitive topics and issues.
- Recognize and reflect on the feelings the patient may express – when the patient
C. Recognize and Reflect on Feelings which Patient may Express
When the patient talks, it is not important to note the content, but to recognize and reflect on the feelings behind the conversation.
D . Talking with Purpose
The nurse’s conversation with the patient should revolve around his needs, desires, and interests. When problems are not clear, indirect approaches such as reflection, open ended questions, focus on the issue, and presenting reality are more effective.
E.Listening
Listening is an active process. The nurse must take the time and energy to listen to what the patient is saying. She must be an empathetic listener and show genuine interest.
F. Allowing patient to express strongly held feeling (Permitting patient to express strongly held feeling)
The expression of strong emotions is very explosive. It is better to allow the patient to express their strong feelings without rejection or punishment. 2. Use Self-understanding as therapeutic tools The psychiatric nurse must have a realistic self-understanding and be able to recognize their own feelings and responses. Consistency is used to contribute to patients security. This means The staff should take steps to ensure the safety of the patient during the ward routine.
4. Reassurance should be given in a Subtle and Acceptable Manner-(अश्वसन देखाना)
Reassurance builds the patient’s confidence. The nurse needs to explain and analyze the patient’s situation to provide reassurance.
5.Patient’s Behaviour is Changed through Emotional Experience and not by Rational Interpretation Use Self understanding as therapeutic tools
Advising patients to rationalize is not effective in changing their behavior. Role-play and social drama etc. can help change their behavior.
6. Unnecessary Increase in Patient’s Anxiety should be Avoided (Unnecessary Increase in Patient’s Anxiety should be Avoided)
To avoid unnecessary anxiety in the patient, the following things should be taken care of
- The nurse should not show her anxiety.
- Showing attention to the patient’s shortcomings.
- Making the patient face repeated failures.
- Making demands on the patient that he/she is clearly unable to meet.
7. Objective Observation of Patient to Understand his Behavior
So that what the patient wants to be said can be assessed. The nurse should not mix her own feelings, judgments and opinions.
8. Maintain Realistic Nurse-Patient Relationship
A realistic or professional relationship focuses on the individual’s personal and emotional needs, not on the needs of the patient and the nurse.
9. Avoid Physical and Verbal Force as Much as Possible (Do not use any kind of physical or mental force)
The nurse should not give any kind of punishment if the patient is suffering from psychological trauma. In addition, the nurse can prevent unpredictable behavior by studying the patient’s behavior. The nurse should perform the procedure quickly and should not show the patient that she is uncomfortable. If the patient is restrained, explain the reason. When there is a positive change in the patient’s behavior, allow the patient to interact with others.
10. Nursing Care is Centered on the Patient as a Person and not on the Control of Symptoms
There is a reason behind the behavior seen in a person. The nurse should have an understanding of why the symptoms of this behavior occur. Many times, the patient shows symptoms of different behaviors in the same situation. Therefore, nursing care should be done by keeping the patient in mind and not by keeping his symptoms in mind
11. All Explanations of Procedures and other Routines are Given According to the Patient’s Level of Understanding (Explaining the routine and other routines to the patient according to his understanding)
Routines and procedures should be explained according to the understanding and needs of the psychiatric patient so that his anxiety is removed to a large extent and every person has the right to know the procedures being performed on him, that is, he is mentally ill, so it should not be necessary to explain this to him.
12. Many Procedures are Modified but Basic Principles Remain Unaltered-(Many procedures will be modified but these basic principles will remain the same)
Many procedures will be modified according to the needs of the patient, the method will change but these basic principles will remain the same, which mainly involves taking care of the patient, including his safety, security, therapeutic relationship, procedures, etc……
B. Mental Status Examination – Mental Status Examination.
MSE is a standard structure or a whole process with the help of which a psychiatric patient’s A systematic assessment can be done, in which the patient’s behavior, concentration, thought process, attention, and emotional function are examined, from which the patient’s mentality is concluded, which is called MSE.
DEFINITION :- Mental status examination means the evaluation of a person’s intellectual, cognitive ability, mood, and thought process.
Before MSE, it is necessary to assess vital signs.
(Blood pressure, heart rate, respiratory rate, temperature)
• Topics are assessed in MSE :-
- 1) GENERAL APPEARANCE AND BEHAVIOR
- 2) SPEECH/TALKING PATTERN
- 3) MOOD/AFFECT
- 4) THOUGHT
- 5) PERCEPTION
- 6) COGNITIVE FUNCTION
- 7) MEMORY
- 8) INTELLIGENCE
- 9) INSIGHT
- 10) JUDGMENT
- 11) ATTENTION
1) GENERAL APPEARANCE AND BEHAVIOR :- (General Appearance and Behavior)
Appearance:- How a person looks…. old, young,…etc…
Conscious:- Is the person alert, drowsy, stupor, or comatose….
Hygiene:-
- How does he keep his rice…..
- Does he keep it properly or not…..
Sleep (sleep) :-
- Does he sleep properly or not…
- How much time does he sleep…
Posture :-
- During the examination, to see what the person’s posture is like
- In which, he talks openly or not….
- Does he answer the question asked or not….
- Does he sit with his head down or does he talk while looking in front of him…
Eye to eye contact :-Does he talk while looking into the eyes, how long and when does he look away…
Gait (way of walking):-When the patient comes, how does he walk? Does he come confidently or does he come as if he is scared…
Facial expressions ( facial expressions):- What kind of facial expressions do they give…
Eating pattern :-Does he eat properly or not and if he eats too much No….
2) SPEECH/TALKING PATTERN :-(Speech/Talking Pattern )
- Does the person start speaking very quickly or does he speak slowly…
- Does he respond out of fear or not…
- Does he respond by shouting loudly…
- Question Answers true or false….
- Repeats one thing after another…..(clang association)
- Mumbles…..(mumbring)
- Turns things around instead of directly..
- (Circumstantial)
- (tangential – Tangential – Correct answer is not Hayse)
3) MOOD/AFFECT :-
What is the mood….
- Sad, anxious, depressed, angry, euphoric, fear, restlessness, irritable
- The mood keeps changing….!! How many times does it change..
- According to the response, is there a mood or not…
4) THOUGHT :- (Thought – Thought)
- What are the thoughts of a person….
- positive (positive) / negetive (negative)
- Thoughts are fast and change frequently….
- Flights of ideas :-
- Thoughts come continuously but their direction keeps changing…….
- Unclear Thoughts
Neologism (Neologism) :- Pronounce new words that have no meaning j
5) PERCEPTION :- (Perception) :-
Hallucination (Hallucination) :-
- There is no external object/sound/smell/touch, yet it seems to be there
- Auditory, visual, olfactory, gustatory, tectile
Illusion :-
- False perception of external stimuli
- Deja vu:- Feeling of having seen something in a previous life but never having met it in real life…..
- Jamais Vu:- Forgetting even family members with whom one lives…..
6) COGNITIVE FUNCTION:-
(Cognitive function) :-
- To know whether a person is conscious or not….
- Gives us replay slowly (stupor)
- Behaves as if in a coma….
- How does it give information about old things…. Do you know the whole thing or do you remember a little bit? Is….
- Does it have a concept of time, place, person, etc.?
7) MEMORY :-
immediate (immediate ) memory :-
- To ask someone to repeat something….
remote (remote) memory :-
- Do you remember your marriage date, your age, when and where you got your job…
recent (recent) memory :-
- To know whether you remember recent events or not…
- What did you eat in the morning, when did you eat, when did you wake up…
8) INTELLIGENCE :-(Intelligence) :-
- Can you read or write…and how was your school performance…..
9) INSIGHT :-
- Is the person aware of his condition or not….
- What is the internal intelligence like….
- To know this, ask him questions about himself and based on his answers, decide whether insight is present or not….
10) JUDGMENT :-
- The information about this is based on the knowledge, education level of the person…
- Every person’s judgment is different…
11) ATTENTION / CONCENTRATION :- (Attention / Concentration) :-
- Ask the person to subtract 7 from 100 Next, keep asking…(100-7 = 93, 93-7 = 86……..)
- Or do a reverse count……(100,99,98,97…..)
- You can ask about month, week, days…..
C. Therapeutic Nurse Patient Relationship – Therapeutic Nurse Patient Relationship.
Definition:
A therapeutic nurse-patient relationship is a professional relationship between a nurse and a patient, the purpose of which is to improve the mental, physical and social health of the patient. It is extremely important to maintain trust, empathy, respect and professional boundaries in this relationship.
Objectives:
- To provide mental support to the patient.
- To effectively address the patient’s fears, doubts, pain, etc.
- To increase self-confidence and self-defense in the patient.
- Involving the patient in treatment.
- Supporting patient behavior improvement.
Key Components:
- Trust: Creating an environment where the patient trusts the nurse.
- Empathy: To understand the patient’s situation emotionally.
- Respect: Respect the patient’s human rights and personality.
- Genuineness: The nurse’s behavior should be honest and open.
- Professional Boundaries: Keep the relationship within professional limitations.
Therapeutic NursePatient Phases of Therapeutic Relationship:
1. Pre-interaction phase
It starts when the nurse is assigned a patient. This is the phase before interacting with him. During this phase, the nurse has some fear and anxiety. She sets her objectives. To overcome her anxiety, she takes the help of the clinical supervisor because she also has many misconceptions or beliefs about the patient, whether the patient will accept her or not, whether she will behave violently, for which she often talks to the nurse of the next shift or makes guesses from the records.
2. Orientation phase
This phase begins when the nurse interacts with the patient, where the nurse introduces herself and the patient is also unaware of it. In this phase, both get to know each other, accept each other, and a contract is made with each other regarding treatment. This time, while communicating with the patient, show trust in your behavior towards him. Tell the patient about the confidentiality of the information received. The orientation phase is complete when both the nurse and the patient accept each other as unique human beings.
3. Working phase
This phase is a phase for the problem solving process for the nurse and the patient, in which the nurse works to complete the goals set in the orientation phase and works for the patient’s recovery. In this, the nurse overcomes her anxiety and reduces her fear. During this time, the patient is encouraged for socialization, motivated for communication, helped in finding solutions, etc.
4. Termination phase
This is the final phase of the therapeutic relationship between the nurse and the patient. This phase is also called the resolution phase or the end phase. The main purpose of the termination phase is to end the therapeutic relationship between the nurse and the patient. The termination phase begins when the patient signs the contract of the orientation phase. The patient is discharged. The patient goes on parole and does not return. Due to moving to another place as per the clinical rotation. Due to improvement in the patient. Due to no longer needing a one-to-one relationship. The nurse terminates the relationship even though the patient is in the hospital. The patient is discharged from the hospital and ends the therapeutic relationship. The termination phase occurs for various reasons. It is important to inform the patient about the termination and they have the right to know. The patient should be allowed to express their thoughts and feelings.
Role of Nurse:
- Empathetic treatment of the patient.
- Active listening.
- Support for the patient’s emotional ups and downs.
- Guidance for behavior modification.
- Responding patiently and handling anger or frustration.
D. Admission Procedure of a Mental Ill Patient in Mental Health Hospital – Admission Procedure of a Mental Ill Patient in Mental Health Hospital.
Admission to a Psychiatric Hospital
- 1. Admission on a voluntary basis
- 2. Admission in special circumstances
- 3. Reception orders
1. Admission on voluntary basis
Admission as a voluntary patient
Request for admission by guardian
Regulations with respect to voluntary patients:
On receipt of the request, the Medical Officer-in-Charge shall examine within a period of 24 hours and if satisfied, he may accept such application as a voluntary patient.
Every voluntary patient admitted shall be bound to abide by the rules framed by the Medical Officer.
Admission on voluntary basis
Request by the Principal for admission as a voluntary patient
Request by the Guardian for admission to the ward.
2. Admission in special circumstances:
Any mentally ill person who does not or cannot express his wish for admission may be admitted and kept as a patient in a mental hospital on an application made on his behalf by a relative or friend of the mentally ill person if the Medical Officer-in-Charge is satisfied that it is necessary to do so in the interests of the mentally ill person
3. Reception Orders
Application for Reception Orders:
• An application for a reception order may be made by
– The Medical Officer in Charge
– The spouse or other relative of the mentally ill person
-Where the Medical Officer in Charge is satisfied that:
-The treatment in the mental hospital is necessary to continue for more than six months
It is in the interests of the health and safety of the mentally ill person or for the protection of others The application is to be made to the Magistrate within the local limits of the jurisdiction of the Psychiatrist Hospital.
Every application shall be as follows:
Duly signed and verified
Must be accompanied by two medical certificates
Two medical practitioners, one of whom shall be in the service of the Government
E) Level of Prevention in Psychiatry (Preventive Psychiatry) – Levels of Prevention in Psychiatry.
Levels of Prevention in Psychiatry
(Preventive Psychiatry)
Five main levels (levels) have been identified for the prevention of psychiatric diseases. Each level is helpful in keeping the mental health of the patient safe by intervening at a different stage of the disease development.
1. Primordial Prevention
Definition:
This level is the earliest of all levels. The risk factors for the disease have not yet arisen, and the aim is to prevent these risk factors from arising. At this level, social, economic, and cultural determinants are addressed so that mental health conditions do not arise.
Example:
- Proper psychosocial development in childhood
- Policies to reduce poverty
- For a healthy lifestyle Awareness
- Safe and positive environment for children
2.Primary Prevention
Definition:
This stage is when no psychiatric disease has started yet. The main aim is to prevent the disease from starting. This includes efforts to reduce risk factors and increase protective factors.
Example:
- Life skills education
- Mental health awareness programs
- Substance abuse prevention Prevention)
- School Mental Health Programs
3.Secondary Prevention (Secondary Prevention)
Definition:
In this stage, symptoms of the disease have already started, but they have not yet taken a serious form. The aim is to identify the disease early (early diagnosis) and start treatment immediately (early treatment) so that the development of the disease can be stopped.
Example:
- Screening programs
- Suicide risk identification and intervention
- Initiation of therapy for early symptoms
4. Tertiary Prevention Prevention)
Definition:
At this stage, the disease has become established. The aim is to prevent relapse in the patient, control residual symptoms, and help the patient return to a normal life through rehabilitation.
Example:
- Rehabilitation centers
- Support groups Groups)
- Chronic Medication and Monitoring
- Family Support and Community Support
5. Quaternary Prevention
Definition:
This stage is a very important requirement of modern times. Its purpose is to protect patients from overmedicalization and unnecessary medical interventions.
Example:
- Prevent unnecessary medication
- Prevent “labeling” of mental illness
- Proper medical education and limited, professional treatment (rational treatment – Rational Treatment)
Preventive Psychiatry – Preventive psychiatry is an important way to protect patients from psychiatric diseases and help them have a better quality of life. Each Prevention Level – Prevention Level plays its own specific role. If implemented systematically from Primordial Prevention to Quaternary Prevention, we can reduce the burden of psychiatric diseases.
F) Legal responsibilities in care of Mentally ill patient – Legal responsibilities in care of Mentally ill patient.
Legal responsibilities in care of Mentally ill patient
1. Informed Consent:
- It is mandatory to obtain informed consent from a mentally ill patient or his/her legal guardian before providing treatment.
- It is essential to provide information about the treatment, its risks, benefits, options and the patient’s rights. If the patient is not capable of giving consent, a Legal Guardian or court order is required.
2. Confidentiality:
- It is not legally permissible to share a mental health patient’s information, such as diagnosis, treatment, case details, etc., with others.
- This information can only be disclosed with the patient’s permission or by court order. Policies like HIPAA (Health Insurance Portability and Accountability Act) also protect it.
3. Negligence and Standard of Care:
- It is necessary for health workers to take full care to avoid negligence in caring for patients.
- Failure to provide proper care, medication, or supervision can be a legal offense.
4. Restraint and Seclusion:
- When a mentally ill patient becomes violent Physical restraint or seclusion may be given but legal rules must be followed.
- It is necessary to document how, for how long and for what reason the patient was restrained.
5.Legal Guardianship:
- When a patient is unable to make any kind of decision, a person is made a legal guardian by a court order.
- That person can then make all the decisions for the patient – regarding treatment, hospitalization, etc.
6. Forced Treatment:
- When the patient’s health or the life of another is in danger, the patient can be given compulsory treatment by a court order.
- That is, treatment is applicable even against the will, but it must have a legal basis.
7.Authorized Mental Health Institutions:
- Only established and registered mental health care centers should be used to admit mentally ill patients.
- Where accredited services are available and are legally operated.
8.Reporting of Abuse (Reporting of Abuse):
- If any kind of abuse is done to the patient (such as physical, mental or sexual abuse), then it is mandatory to immediately report it to the Authority.
9. Mental Health Care Act (Mental Healthcare Act : 2017, India)
- Under this act, the patient is guaranteed human rights, sexual dignity, confidentiality, and appropriate treatment The right to receive is given.
- According to this act, any person who is admitted or given medicine against his will should be legally regularized.
Legal responsibility is very sensitive while taking care of a mentally ill patient. It is necessary to keep the patient’s rights, confidentiality and safety in mind at every step. If the rules are not followed legally, then one may have to face legal action at the individual or institutional level.
G. National Mental Health Programme – National Mental Health Programme.
The National Mental Health Programme was launched by the Government of India in 1982. Maharashtra was the first state to implement the National Mental Health Programme. Mental illness is a burden on the community and the National Mental Health Program was created to alleviate the burden and strengthen the infrastructure.
Aims :
- Prevent and treat mental and neurological disorders and their associated disabilities.
- Use mental health technology to improve general health services To do.
- Using the principles of mental health for national development. So that the quality of life can be improved.
Objectives (Objective)
To ensure the availability and accessibility of minimum mental health care, especially for vulnerable groups and the underprivileged in the near future. – To use mental health knowledge for social development and for general health care. – Increase community participation and self-help efforts in providing mental health services.
Strategies
Integrate mental health with primary health. – Provide tertiary care institutions for the treatment of mental disorders. – Implement District Mental Health Program in all districts.
- Remove the stigma attached to mentally ill patients and protect their rights.
- Provide facilities of psychiatric units and psychiatric hospitals at grass root level.
Specific approaches
- Diffusion of Mental Health Skills to Peripheral Areas
- To spread mental health skills to the peripheral areas.
- To start mental health care from the grass root level.
- Instead of focusing on mental health care in urban areas, focus on rural and peripheral areas. (Peripheral areas such as sub-centers, primary health centers )
Component of NMHP (Component of NMHP)
- Village & sub enter level :
(Village and Sub Center Level) To identify psychiatric disorders at the village and subcenter level and refer them to the PHC or District Hospital. - Primary health center :
(Primary Health Center) To identify and treat minor psychiatric disorders at the PHC level and refer them to the District Hospital if necessary. - District hospital :
(District Hospital) There is a psychiatrist in the district hospital who diagnoses various mental disorders and provides treatment for them. - Teaching unit :
(Teaching unit) In the teaching unit, people are explained about mental health and how to maintain mental health. - Rehabilitation :
(Rehabilitation) To create rehabilitation centers and provide special rehabilitation services there. - Prevention :
(Prevention) To prevent alcohol and substance abuse related problems. - Mental health training :
(Mental Health Training) To organize a training program where health care personnel are provided training on mental health.
H. Role of Nurse while giving Antipsychotic Drugs. Role of Nurse while Administering Antipsychotic Drugs.
Role of Nurse while Administering Antipsychotic Drugs:
1. Pre-medication Assessment of the Patient:
The nurse should assess the patient’s complete mental status, vital signs, allergy history, medication history, and current physical condition. It is especially necessary to check the patient’s temperature, blood pressure, pulse rate and respiratory rate.
2. Proper Drug Identification and Preparation:
Properly identify antipsychotic drugs such as Haloperidol, Risperidone, Olanzapine etc., prepare the correct dosage as per the doctor’s order and administer.
3. Check Dose and Route Route):
Ensure the correct dose of the drug and the route of administration such as oral, intramuscular or intravenous. Follow the Three-check system and Five Rights – Right Patient, Right Drug, Right Dose, Right Time, Right Route.
4. Observation for Adverse Effects during Administration:
Continuous observation for common side effects of antipsychotic drugs such as Extrapyramidal Symptoms, Sedation, Orthostatic Hypotension, Waning of Consciousness, Dry Mouth, Weight Gain etc. To do.
5.Monitoring for Therapeutic Effect:
The nurse should monitor the effectiveness of the medication. For example, to check whether the patient’s condition has improved, such as whether there is a decrease in hallucinations, delusions, aggressive behavior, etc.
6. Patient and Family Education:
The nurse should inform the patient and his family about the proper use of medications, regularity, side effects, and what to avoid while taking the medication. Explaining not to stop the medication.
7.Ensure Compliance:
The nurse should follow-up and conduct motivational interviews to ensure that the patient is taking the medicine regularly.
8. Documentation:
It is necessary to document each administered medication, time, dose, route, and any observations.
9. Immediate Response to Critical Reactions:
Antipsychotic Arrange immediate medical attention for severe drug reactions such as Neuroleptic Malignant Syndrome, Akathisia, Dystonia.
10. Interprofessional Communication:
Communicate with physicians and the mental health team regarding medication side effects, therapeutic response, and any other problems.
All these measures are important for the nurse to ensure the successful and safe administration of antipsychotic therapy. Shows responsibility.
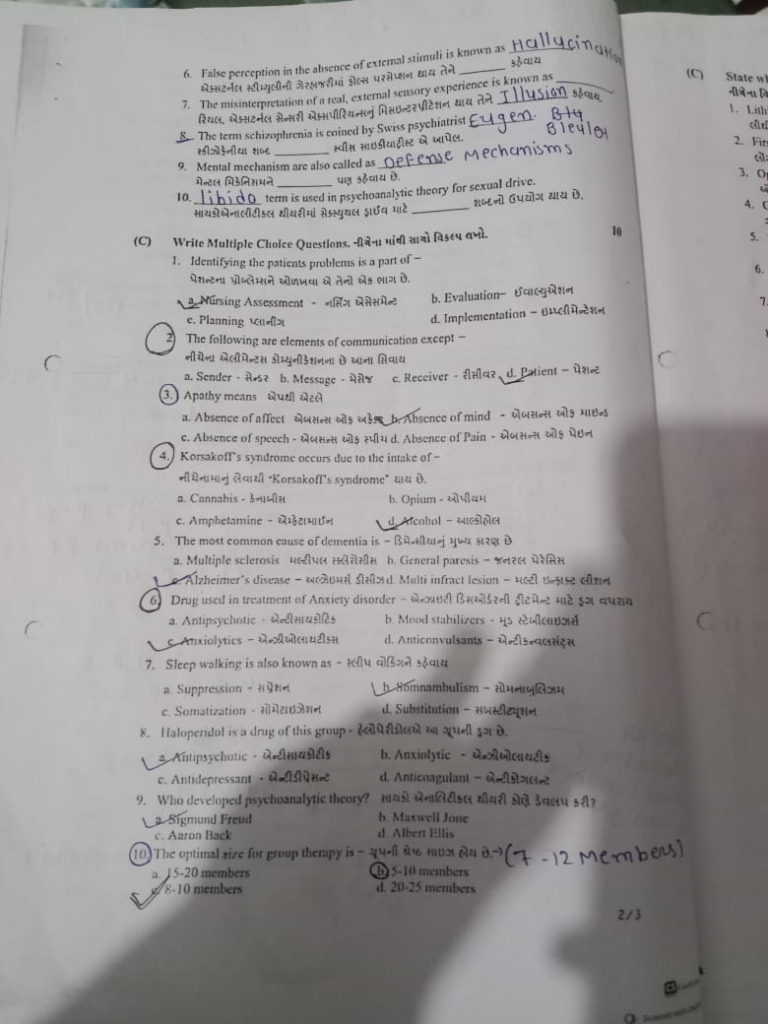
Q-3 (A) Fill in the blanks, fill in the blanks. ( 10 )
1)Anti-manic drugs are also referred to as….. Anti-manic drugs are also referred to as….. ✅ Mood stabilizers🔹 Anti-manic drugs are also called mood stabilizers.
2) Learning Disorder in which Reading domain is known as….. Reading learning disorder is…. called. ✅ Dyslexia🔹 The learning disorder of reading is called dyslexia.
3) ECT was introduced in the year …. ECT was started in the year ….. ✅ 1938
🔹 ECT 1938 was started in the year .
4) Fear of height is known as …. Fear of height …. It is called. ✅ Acrophobia
🔹 The fear of heights is called Acrophobia.
5) Indian Mental Health Act has been passed in …. Indian Mental Health Act …. It came into effect in 1987.
6) False perception in the absence of external stimuli is known as …. False perception occurs in the absence of external stimuli. It is called.✅ Hallucination
🔹 False perception in the absence of external stimuli is called Hallucination .
7) the misinterpretation of a real external sensory experience is known as ….
Real external sensory experience is known as …. Called. ✅ Illusion🔹 The misinterpretation of real external sensory experience is called Illusion.
8) the term schizophrenia is coined by Swiss psychiatrist …. The word schizophrenia …. The word schizophrenia was coined by a Swiss psychiatrist. ✅ Eugen Bleuler🔹 The word schizophrenia was coined by a Swiss psychiatrist named Eugen Bleuler.
9) mental mechanism are also called as …. Mental mechanism is also called as ….✅ Defense mechanisms🔹 Mental mechanism is also called as Defense mechanism .
10)…. Term is used in psychoanalytic theory for sexual drive. In psychoanalytic theory for sexual drive …. The word is used.✅ Libido🔹 In psychoanalytic theory, the word libido is used for sexual drive.
( B ) Write Multiple choice questions. Write the correct option from the following. 10
1) identifying the patients problems is a part of …. Identifying the patient’s problem is part of it.
✅ a. Nursing assessment
b. Evaluation
C. Planning
d. Implementation (Implementation)
Rationale: In the nursing process, identifying patient problems occurs during the assessment phase.
2 ) The following are elements of communication except …. Following are elements of communication except….
a. Sender ( Sender )
b. Message c. Receiver ( receiver )
✅ d. Patient (Patient)
Rationale: The basic elements of communication are sender, message, receiver, and feedback. Patient is not a universal communication element unless in a specific context.
3 ) Apathy means…. From the app means….
✅ a. Absence of affect (Absence of affect)
b. Absence of Mind (Absence of Mind)
c.Absence of Speech (Absence of Speech)
d.Absence of Pain (Absence of Pain)
Rationale: Apathy is defined as lack of emotion or interest-a reduced emotional response.
4 ) Korsakoff’s Syndrome Occurs due to the intake of …. The following causes ‘Korsakoff Syndrome’.
a.Cannabis
b.Opium
c.Amphetamine
✅ d. Alcohol
Rationale: It is a chronic memory disorder caused by severe deficiency of thiamine (Vitamin B1), most often due to alcohol misuse.
5) The most common cause of dementia is …. The main cause of dementia is.
a.Multiple Sclerosis (Multiple Sclerosis)
b.General paresis (General Paresis)
✅ c. Alzheimer’s Disease (Alzheimers Disease)
d. Multi infract lesion (multi infract lesion)
Rationale: Alzheimer’s is the most common type of dementia, especially in elderly individuals.
6 ) Drug used in treatment of Anxiety disorder…. Drug used for the treatment of anxiety disorders.
a.Antipsychotic (Antipsychotic)
b.Mood Stabilizer (Mood Stabilizers)
✅ c. Anxiolytics
d) Anticonvulsants
Rationale: Anxiolytics like benzodiazepines are used to relieve anxiety.
7) Sleep Walking is also known as…. Sleep walking is called ….
a.Suppression
✅ b. Somnambulism
c.Somatization
d.substitution
Rationale: Somnambulism refers to walking or performing complex behaviors while asleep.
8) Haloperidol is drug of this group…. Haloperidol is a drug of this group….
✅ a. Antipsychotic
b. Anxiolytics
C.Antidepressiin
d. Anticoagulant
Rationale: Haloperidol is a typical antipsychotic drug used to treat schizophrenia and psychotic disorders.
9) Who developed psychoanalytic theory…. Who developed the psychoanalytic theory ….
✅ a. Sigmund Freud
b. Maxwell Jones
c. Aaron Back
d Albert Allies
Rationale: Freud is the father of psychoanalysis.
a. 15 – 20 members ( 15 – 20 members) b. 5 – 10 members ( 5 – 10 members)
✅ c. 8 – 10 Members (8 – 10 members)
d. 20 – 25 Members (20-25 Members)
Rationale: Group therapy works best with 8 to 10 members, allowing participation and intimacy.
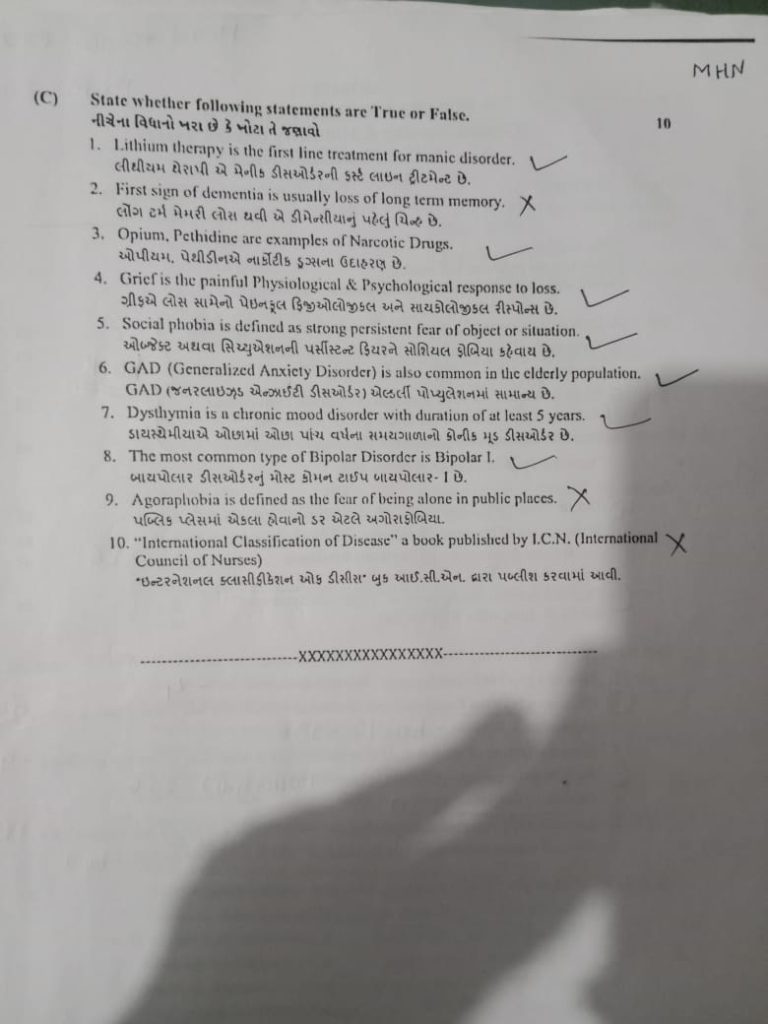
( c ) State whether following statements are true or false.
State whether the following statements are true or false. 10
1.Lithium therapy is the first line treatment for manic disorder ….
Lithium therapy is the first line treatment of manic disorder. ✅ True
Rationale: Lithium is considered a first-line mood stabilizer for acute manic episodes in Bipolar Disorder.
2. First sign of dementia is usually loss of long term memory…. Long-term memory loss is the first sign of dementia.❌ False
Rationale: Short-term memory loss is typically the first sign in dementia, not long-term memory.
3.Opium, pethidine Are Example of Narcotic drugs…. Opium, Pethidine are examples of narcotic drugs. ✅ True
Rationale: Both Opium and Pethidine are class=”has-inline-color”>narcotic analgesics used to relieve pain.
4.Grief is the painful physiological and psychological response to loss …. Grief is a painful physiological and psychological response to loss.✅ True
Rationale: Grief is an emotional and bodily reaction to loss, especially of loved ones.
5.Social phobia is defined as strong persistent fear of object or situation…. Persistent fear of an object or situation is called social phobia.❌ False
Rationale: Social phobia is the fear of being judged or embarrassed in social situations, not of objects or general situations.
6.GAD ( Generalized Anxiety Disorder ) is also common in Elderly Population …. GAD (Generalized Anxiety Disorder) is common in the elderly population. class=”has-inline-color”>prevalent among the elderly, often underdiagnosed due to overlapping symptoms with aging.
7) Dysthymia is a chronic mood disorder with duration of at least 5 years…. Dysthymia is a chronic mood disorder that lasts for at least five years.❌ False
Rationale:Dysthymia (Persistent Depressive Disorder) must last at least 2 years, not 5 years.
8) The most common type of Bipolar Disorder is Bipolar-1 …. The most common type of bipolar disorder is Bipolar-1. ✅ True
Rationale: Bipolar-I, which includes manic episodes, is more commonly diagnosed than Bipolar-II.
9) Agoraphobia is defined as the fear of being alone in public places…. Agoraphobia is the fear of being alone in public places.✅ True / खरो
Rationale: Agoraphobia is the fear of open/public spaces or being in a place where escape may be difficult.
10) “International Classification of Disease” a book published by I.C.N.( International Council of Nurses )….’ International Classification of Diseases ‘ Book I.C.N. Published by.❌ False
Rationale: ICD (International Classification of Diseases) is published by the WHO (World Health Organization), not ICN.
