ENGLISH-MENTAL HEALTH NURSING (GNM 2ND YEAR) 03/07/2023 PAPER SOLUTION (Done)-UPLOAD-8
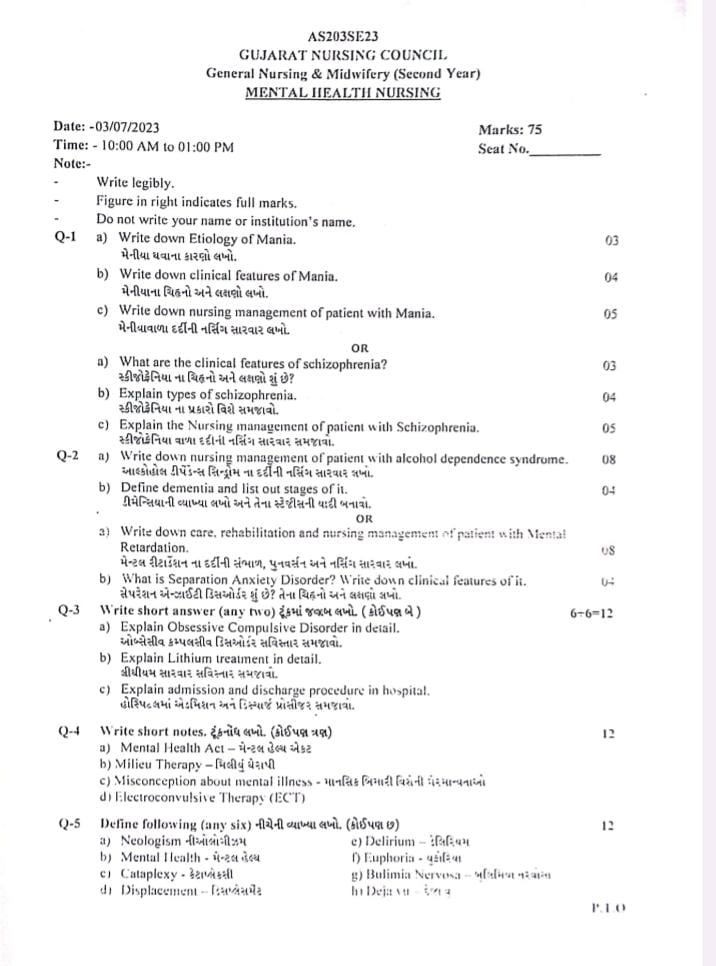
MENTAL HEALTH NURSING (GNM 2ND YEAR) 03/07/2023 PAPER SOLUTION NO.8
Q-1
a) Write down Etiology of Mania. Write the causes of mania.03
A. Genetics:
- Family History:
- If a family member has mania, other members are at higher risk of developing the condition.
- Twins Studies:
- Identical Twins Twins) are more likely to develop mania than Fraternal Twins.
B. Brain Chemistry:
- Imbalance of neurotransmitters like Dopamine and Norepinephrine can cause mania.
C. Substance Abuse:
- Drugs and Alcohol Overuse can cause a Manic Episode.
D. Stressful Life Events:
- Traumatic Experiences or Life Stress can cause Manic Episodes.
E. Medication:
- Side effects of medications such as Antidepressants, Stimulants, and Steroids can cause mania.
F. Sleep Disturbance:
- Changes in sleep patterns are a major risk factor for Mania.
G. Medical Conditions:
- Thyroid Disorder and Neurological Conditions are associated with symptoms of mania.
H. Brain Lesion:
- Right Fronto-Temporal or Left Parieto-Occipital Lesion is associated with mania.
I. Psychological Factors:
- Personality Traits and Coping Mechanisms are also responsible for causing mania.
b) Write down clinical features of Mania. Write the signs and symptoms of mania.04
1. Euphoria:
- Symptoms:
- Mild elevation in mood is seen.
- The person feels Emotional and Physical Wellbeing.
2. Elation:
- Symptoms:
- Moderate Mood Elevation occurs.
- The person experiences enjoyment and excitement.
3. Exaltation:
- Symptoms:
- Severe Mood Elevation occurs.
- Grandiosity Delusion occurs, in which the person considers himself grandiose and unique.
4. Ecstasy:
- Symptoms:
- Extreme Severe Elevation of Mood.
- The person experiences Extreme Joy, which is usually seen in Delirious Mania.
1. Psychomotor Activity:
- Increased Psychomotor Activity:
- The person becomes more active and hyper-agitated.
2. Speech and Thought Disturbances:
- Flight of Ideas:
- The person jumps from one thing to another, without a logical connection.
- Pressure of Speech:
- The person speaks more loudly and continuously, making it difficult to stop.
- Delusion of Grandiosity:
- The person begins to think of himself as Great or special.
- Delusion of Persecution:
- False belief that others will harm him (Harmful Intentions by Others).
- Distractibility:
- Lack of proper attention, easily distracted by surrounding objects.
- Poverty of Thought:
- Reduced Thought Variety, and thoughts pass through the brain very slowly (Slow Thinking).
Other Features of Mania
Behavioral Features:
- Impulsive Behavior: The person behaves in an unplanned and risky way.
- Action-Oriented Wishes: Doing everything right away Desire to Act Quickly.
- Positive Self-Image: The person sees themselves as Great or Superior.
- Tendency to Blame Others: Blame Others for their mistakes.
Cognitive Features:
- Exhibit Poor Judgment: Inability to Make Rational Decisions.
- Denial of Problems: Refuse to Acknowledge Problems.
- Poor Judgment (Poor Judgment): The habit of taking poor and risky decisions.
Physical and Social Features:
- Loudness: The way of speaking becomes more Loud and Intense.
- Hyperactivity: There is Excessive Activity both physically and mentally.
Productivity:
- Greater and more productive behavior (Increased Productivity), although it may not be appropriate.
Infatigability:
- Not feeling tired (Inability to Feel Tired).
Biological Features:
- Increased Libido (Increased Libido):
- Increased Sexual Desires.
Insomnia:
- Difficulty Sleeping or not sleeping at all.
c) Write down nursing management of patient with Mania. Write the nursing management of a patient with mania.05
Describe the nursing management of mania.
- Therapeutic nursing needs
- Administering medications prescribed by a psychiatrist
- Always remember the 5 rights before giving medicine
- After giving medicine, observe and record its side effects or any changes in the patient
- If the patient is on lithium carbonate therapy, check the lithium level
- If the patient is going to be given ECT, explain it and let him talk about his illness
- Advise him to take less salt since he is on lithium medicine
2. Physical Needs
- Encourage the patient to reduce physical activity and sleep
- To divert the patient’s energy and focus, activities such as knitting, making balls of socks, etc. should be done
- Encourage him to play games like carom, badminton, tennis, etc.
- Ask him to take a short nap during the afternoon and get 6 to 7 hours of sleep during the night To encourage sleep
3. Safety and Security
- Take care that the patient does not get injured, if there is any wound or cut, dress it
- Keep the surrounding environment quiet so that he does not get any other stimulation
- Control the patient’s behavior so that he does not hurt anyone else, restrict him for certain activities
4. Nutritional Needs
- Manic patients are not calm, so give them “finger food”
- Tell the patient to drink more fluids while on lithium therapy
- Give the patient a high calorie, high protein diet
- The patient does not feel hungry, so he does not eat enough food, so weigh him regularly and maintain an intake output chart To do
5. Improve judgment and concentration
- The patient should be given a task every day and check how he completes it
- Correct the behavior with other patients. Be a little friendly with the patient and ignore the unwanted behavior
- Let the patient read a little or encourage him to watch a T.V. movie
- Start with small tasks
6. Improve communication
- Talk to the patient simply and briefly and do not argue with him/her in any way
- Give praise for positive changes in patient communication
- Talk to the patient with a smile but never make fun of the patient
- Check his/her social interaction from the first day itself
- Good and real nurse To maintain a therapeutic relationship
- Encourage and provide opportunities for them to talk to other people
- Try to help the patient nurture his hobbies
7. Recreation Need
- First let the patient play alone and then encourage two or three to play together
- It is better if the game is short and simple
- The patient can also be given recreation by playing games like Sudoku, Ludo, Snakes and Ladders etc.
8. Spiritual Needs
- Encourage the patient about his religious beliefs
- Encourage him to talk to the priest or other religious leaders in whom he believes who come to the hospital
- Allow him to pray alone or in a group
- Celebrate festivals according to his religion such as Diwali, Holi, Ramadan, Eid, Christmas, etc.
OR
a) What are the clinical features of schizophrenia? What are the signs and symptoms of schizophrenia? 03
Usually, the personality and behavior of a patient with schizophrenia are seen to be different at different times. Often the symptoms are very rapid and severe. Schizophrenia can be classified into the following categories according to its symptoms.
Positive symptoms:
Symptoms that are only seen in patients with schizophrenia, which are also known as psychotics
Delusions: – In which a person feels that someone is oppressing him, someone is conspiring against him, other people are talking about him, such delusions are seen
Hallucinations: – False hallucinations
Aggression: – Lack of control over emotions
Agitation :-In which nervousness is seen
Suspiciousness :- Being suspicious
Hostility :-Contradictory behavior
Excitement:- Appearing unnecessarily excited
Grandiosity:- Feeling of grandeur in which he feels like he is the Prime Minister
Conceptual Organization :- Unable to organize his concepts.
Negative Symptoms:
- Emotional thought that is not consistent with the event and mood
- Withdrawal from family, friends and social activities
- Lack of motivation leads to a lack of joy and interest in life and a lack of hygiene and grooming
- Lack of performance in daily life tasks
- Moodiness
- Catatonia
Schizophrenia Symptoms Bluner’s 4 “A’s”
1. Associative disturbance or looseness
This is a thought disorder. Such a person cannot think logically.
2. Affect disturbance In this, there is disturbance in the patient’s mood, i.e. the patient’s mood is flat or blunt.
3. Ambivalence
Showing contradictory feelings and desires towards the same person, thing or situation.
4. Autistic Thinking
This is a thought disorder in which the person is lost in lucid dreams and is unaware of their surroundings.
First Rank Symptoms
- Audible thoughts
- No one else has control over their body
- Thought withdrawal
- Thought withdrawal
- Thought Insertion
- Thought Diffusion
- Delusional Perception
Second Rank Symptoms
- Perplexity-Confusion
- Delusional Perception
- Depressive or euphoric mood
- Dryness in emotions
In addition
Disturbances in attention
Cannot maintain attention for a long time
Insight
Inside is affected
Disorders of activity
Negativity and Automatism
Study type speech and activity
Impulsivity
b) Explain types of schizophrenia. Explain the types of schizophrenia.04
Types of schizophrenia
F 20-0 paranoid schizophrenia
F 20-1 hebephrenic schizophrenia
F 20-2 catatonic schizophrenia
F 20-3 undifferentiated schizophrenia
F 20-4 post – schizophrenic disorder
F 20-5 residual schizophrenia
F 20-6 simple schizophrenia
F 20-8 other schizophrenia
F 20-9 schizophrenia unspecified
Paranoid Schizophrenia
This is the most common type. People with this type of schizophrenia They have delusions that they are being punished by others. Their thinking, speech, and emotions, however, remain completely normal. Their onset is gradual. In some cases, it is acute. Good prognosis. Persecution and grandeur disorders are seen.
•Hebiphrenic Or Disorganized Schizophrenia
People with this type of schizophrenia are often confused and incoherent, and they have jumbled speech. The worst prognosis. Their external behavior is emotionless or inappropriate, stupid or childlike. They cannot perform their daily activities properly. Hallucinations are also seen. The worst prognosis is seen after Hebephrenic schizophrenia.
Catatonic Schizophrenia
Onset is acute and sudden. The most striking physical symptoms of this type are physical. People with catatonic schizophrenia are usually immobile and unresponsive to the world around them. They often become very rigid and rigid, staying in one place and not moving. Their behavior is bizarre. They may repeat words spoken by another person. People with catatonic schizophrenia are at risk of malnutrition and self-injury. They have the best prognosis. ECT and IV LORAZEPAM are their best treatments.
Undifferentiated Schizophrenia
This subtype is diagnosed when a person’s symptoms do not clearly represent one of the other three subtypes.
Post Schizophrenic Depression
A depressive episode arising as a result of schizophrenic illness where some low-level schizophrenic symptoms may also be present.
Residual Schizophrenia
This Type I schizophrenia is chronic. Hallucinations, delusions and other symptoms may also be present but are significantly less common than when schizophrenia is diagnosed. Symptoms include eccentric behaviour, emotional blunting, excessive and illogical thinking.
Simple Schizophrenia
Insidious and progressive prominent negative symptoms are seen.
Pfropf Schizophrenia
There are types associated with mental retardation. They are called grafted schizophrenia.
c) Explain the Nursing management of patient with Schizophrenia. Explain the nursing management of a patient with schizophrenia.05
1.TherapeuticNursing Management
- Giving the medicines prescribed by the psychiatrist
- Always remember the 5 rights before giving the medicine
- After giving the medicine, observe its side effects or any changes in the patient and record them To do
- If the patient is to be given ECT, explain it and let him talk about his illness
2. Psychosocial Nursing Management
- Sit close to the patient
- Talk to the patient in a comfortable environment with a reliable communication so that his anxiety is removed
- Encourage the patient to talk about his problem
- Never criticize him while he is talking or being talked to
- Encourage the patient to talk
- Talk to the patient in a simple language that he can understand
- Listen calmly when the patient talks about his delusions and observe how it is reflected in his behavior
- Never validate his delusions but provide him with a safe environment
- Never talk about the patient’s hallucinations, talk about everything else
- Never ignore the patient, sometimes take a little time to talk to him Take a pose and use interview techniques like pinpointing, clarifying, reflecting, summarizing etc. during the conversation.
- Increase self-concept To increase the patient’s self-concept, he should be assigned some tasks like calling everyone for day activities, asking them to check whether everyone has eaten or not, asking them to clean up etc.
- Improve attention and judgment The nurse should play games like carrom, chess, ludo etc. with the patient. Small problems should be asked to solve them. The patient’s attention should be kept on the task.
- Improving family support A relative of the patient should always be with the patient who can help with his problem. The patient’s daily activities such as personal hygiene, diet, etc. can be of help.
3. Physical Needs Nursing Management
a) Provide protection :-
- Do not keep any sharp or injurious objects like knife, blade, rod, glass objects etc. near the patient until they are ready
- If the patient is quarreling with others and hitting each other, then he can be punished like not allowing him to participate in sports etc.
b) Help maintain personal hygiene
- Encourage the patient to brush
- Ensure the patient to empty his/her bowels and bladder completely as the patient can fill them
c) Help with sleeping
- Encourage the patient to go to bed early at night. I should switch off the light. Also, put a floor lamp on the bedside.
- If a patient is disturbing another patient, you should be separated.
- Give the patient a glass of warm milk to drink.
- Make the patient active during the day.
- Forbid the patient from taking naps in the afternoon.
d ) Nutritional Needs
- The next day, a balanced diet should be planned for the patient
- The patient should be served food that he likes and in his own container and he should eat it himself
- If the patient is skeptical about eating, first get his relative to test the food Should
- The patient should get food according to his needs
4. Recreational Needs Nursing Management
- The patient should be asked about his hobbies so that he can be given the recreational he likes
- The patient should be given a game like carrom board or ludo to play
- To use up energy, a game like badminton can also be given to the patient
- Initially, the patient No competitive games should be given or done
- If someone wins a competition, he should be congratulated
5. Spiritual Needs Nursing Management
The patient should be encouraged to pray every day and separate arrangements should be made for him and all the upcoming festivals should be celebrated in a proper manner but no one can ever be forced to celebrate other religions or festivals
Q-2
a) Write down nursing management of patient with alcohol dependence syndrome. Write the nursing management of a patient with alcohol dependence syndrome.08
COMMON NURSING DIAGNOSIS OF ALCOHOL DEPENDENCE SYNDROME
Increased anxiety
Altered sleep pattern
Impaired social interaction
Altered nutrition less than body Requirement
Disturbed self-esteem
Manipulative behavior
Ineffective individual coping
Risk for harming self and others
Impaired social interaction
decrease coping Abilities
1. Increased Anxiety
Objectives: To help reduce the patient’s anxiety level.
Nursing Intervention
Assess the anxiety level.
Assist the patient with his/her Problems should be accepted.
Establish a trustworthy relationship with the family and client.
The patient should be helped to cope with his symptoms.
Do not fight him by thinking that he is a drug addict.
Encourage the patient to express his feelings and emotions.
To support the patient Family members should be encouraged.
Anti-anxiety medication should be given as prescribed.
2. Altered sleep patterns
Objectives: To help the patient improve his/her sleep pattern.
Nursing Intervention
- The client’s sleep pattern should be assessed.
- The patient should be motivated to get 6-8 hours of sleep during the night.
- Provide the client with a safe and calm environment.
- Encourage relatives to stay close to the patient.
- Provide the patient with a glass of warm milk before sleep.
- Provide the patient with back massage and support.
- Ask the client to take a warm bath before sleep.
- Ask the patient to read books of his/her choice.
- Ask him/her to do some relaxation exercises.
- Play some music to have a smooth effect on the client’s mind.
- Motivate the client to attend spiritual prayer.
- Give sedative medicine as per the prescription.
- Impaired Communication
Objectives: The patient’s communication should improve and interact with people.
Nursing Intervention
- Assess the patient’s level of communication and social interaction.
- Maintain a friendly approach with the patient and communicate appropriately with the patient.
- Encourage them to participate in group therapy to promote their communication.
- Spend time with the patient and communicate with them in a language that is simple and understandable to the patient.
- Give them opportunities for social interaction and provide a friendly environment.
- The client should be motivated to engage in social interaction.
- Reduces self-esteem and self-concept
Objectives: – The patient’s self-concept should be improved.
Nursing intervention
- Give a brief explanation for the activity and help the patient identify his positive points.
- Increase his sense of self by giving attention, motivate the patient for such activities that he can do with confidence.
- Anchor the client for positive physical habits.
- Teach the patient exercises to increase self-esteem.
- Do not put the patient in a difficult decision-making condition and the relatives should also support the patient.
- The therapeutic relationship should provide opportunities for the expression of feelings and emotions.
- Administer medications as prescribed and monitor potential side effects of medications.
Rehabilitation of alcohol dependence syndrome
- While the person is recovering from alcohol dependence, social support is usually required to function and lead a normal life.
- Available as inpatient units, comprehensive outpatients, day care centers, and drug de-addiction centers.
- Help them to quit the drug they are dependent on.
- Occupational and social rehabilitation, teaching relaxation techniques, religious therapy
- Motivate them to be helpful and respected.
- Motivate them to participate in self-help groups.
- Help them to lead a productive and respectful life.
b) Define dementia and list out stages of it. Write the definition of dementia and list out its stages.04
Dementia is a serious cognitive disorder in which a person’s memory, thinking ability and behavior problems are seen. It starts slowly and gets worse over time. In Dementia, a person cannot remember anything and has problems in their daily activities. Dementia is most common in old age people. Dementia is chronic and usually irreversible
STAGES OF DEMENTIA
*Stage-1 (Early Stage)
*Stage-2 (Middle Stage)
*Stage-3 (Final Stage)
*Stage-1(Early Stage)
-Forgetfulness.
-Lose interest in the environment.
-Cannot do their work well.
*Stage-2 (Middle Stage)
-Progressive memory loss.
-Feel confused in answering questions.
-Does not follow any instructions.
-Irritable and anxious.
-Social isolation.
-Rejects personal hygiene.
*Stage-3 (Final Stage)
-Weight loss (does not eat proper food).
-Cannot communicate.
-Cannot recognize family.
-Loses ability to walk and sit.
-Death can also occur.
OR
a) Write down care, rehabilitation and nursing management of patients with mental retardation. Write the care, rehabilitation and nursing management of a mental retardation patient.08
Care
1. Secure and Stable Environment :
It is necessary to provide a secure and stable environment to a patient with mental retardation. Constantly changing environment can make them nervous, so a safe environment should be provided by maintaining a routine.
2. Basic Needs:
Help the patient maintain hygiene, nutrition and sleep pattern.
3. Communication:
Communicate with the patient clearly, simply and patiently. If the patient is verbal, then encourage them, if non-verbal, explain the conversation through sound, pictures or gestures.
4. Parental Involvement:
Train parents and caregivers about the patient’s daily behavior, needs and techniques.
Rehabilitation:
1. Behavior Therapy Therapy):
Behavior therapy is given to the patient to develop appropriate behavior and reduce undesirable behavior.
2.Speech Therapy:
Language stimulation and speech skills are helpful for patients with language development delays.
3.Occupational Therapy:
Daily Making the patient independent in activities of life — such as dressing, eating, buttoning, etc.
4. Vocational Training:
Training for small trades according to the patient’s ability — such as paper bag making, packing, nursery gardening.
5. Social Skill Training:
Social behavior such as saying “Namaste”, standing in line, and increasing contact with other people are trained.
Nursing Management:
1.Assessment:
▪︎ Assess the patient’s cognitive level, verbal ability, motor skill, social response.
▪︎ Monitor comorbidity such as epilepsy or autism.
1.Assessment:
▪︎ Assess the patient’s cognitive level, verbal ability, motor skill, and social response.
▪︎ Check for comorbidities such as epilepsy or autism.
2.Nursing Diagnosis:
▪︎ Impaired verbal communication related to delayed mental development.
▪︎ Self-care deficit related to impaired intellectual functioning.
▪︎ Risk for injury related to poor judgment and unsafe behavior.
▪︎ Social isolation related to limited interaction skills.
3.Planning and Implementation:
▪︎ Create an Individualized Care Plan for each patient.
▪︎ Encourage their progress through positive reinforcement.
▪︎ Provide home care training for parents.
▪︎ Monitor changes in the patient’s mood and behavior.
4.Health Education:
▪︎ Educate parents and caregivers about Mental Retardation.
▪︎ Inform about rehabilitation, therapy, and school facilities.
▪︎ Provide a planned guide for the patient’s future.
5.Documentation:
▪︎ Daily observation, Keep proper records of behavioral changes, progress, compliance, etc.
b) What is Separation Anxiety Disorder? Write down clinical features of it. What is Separation Anxiety Disorder? Write its signs and symptoms.04
Definition:
Separation Anxiety Disorder is a type of anxiety disorder in which the patient (mostly seen in children) experiences unbearable fear, worry or distress when separated from their parents, caregivers or a loved one.
This condition is said to occur when this fear is above the normal developmental level and Affects the patient’s social, academic, or behavioral functioning.
This disorder most often begins in childhood, but can also be seen in adolescence or adulthood.
Clinical Features:
1. Excessive distress:
The patient experiences excessive distress when being away from an attachment figure — such as crying, shaking, screaming, arguing about why they shouldn’t go.
2. Fear of harm:
The patient has a genuine fear that an accident, illness, or death will happen to their parents or a close person.
3. Somatic symptoms due to separation:
Such as stomachache, headache, vomiting, dizziness, etc. — especially when going to school, hostel or a new place.
4. School avoidance or clinging behavior:
Not going to school becomes a normal daily behavior. The patient constantly wants to be close to the parents, and refuses to be alone.
5. Nightmares and sleep disturbance:
Dreams in which the patient loses his family — causing fear in sleep, waking up from sleep unconscious.
6. Regression:
Thumb sucking, demanding to sleep with parents — which indicate behavior at a later stage of mental development for the age.
7. Excessive worry:
The patient is constantly worried that he will be forgotten, lost, kidnapped, etc.
Q-3 Write short answer (any two) Write a short answer. (Any two) 6-6=12
a) Explain Obsessive Compulsive Disorder in detail. Explain Obsessive Compulsive Disorder in detail.
Obsessive-Compulsive Disorder (OCD):
This is a Common, Chronic and long-lasting Disorder, in which the person has Uncontrollable Thoughts (Obsession) and Behaviors (Compulsions), which he feels Urge (desire) to Repeat is.
- Obsession: Repeated Thoughts
- Compulsion: Repetitive Behaviors
Obsession and Compulsion are Observable.
Obsession:
There is a repetition of unwanted thoughts, even though the person does not want them to be, and all this happens in the conscious state. This causes Anxiety and Fear.
Example:
- A person has frequent Thoughts of Germs or Contamination.
Compulsion:
Without Desire, the continuous Repetition of Actions without purpose which cannot be Controlled.
Example:
- Frequent Hand Washing.
- Checking (Check) (Do) Whether the door is Locked or not.
CAUSES OF OCD-(Causes of OCD)
Biological Factor:
- If Parents (Parents) or Siblings (Brothers and Sisters) If you have OCD, the Possibility of it increases.
- Identical Twins have a higher Chance of OCD than Dizygotic Twins.
Brain Chemistry:
- Imbalance of the Serotonin Neurotransmitter causes changes in Mood.
Environmental Factor:
- Traumatic Events, Abuse and Stress OCD Symptoms are seen due to.
Cognitive Factor:
- Certain Thought Patterns and Beliefs, such as Excessive Need for Control, can lead to OCD.
Neurological Factor:
- Brain Structure (Brain Structure) Abnormalities in structure and Function can cause OCD.
Infection:
- Streptococcal Infection can cause OCD.
CLINICAL MANIFESTATION OF OCD-(Clinical manifestation of OCD)
Obsession:
- Fear of Contamination
- Doubting
- Need for Order
- Aggressive Thoughts
Compulsion:
- Washing/Cleaning
- Checking (e.g., Locks, Door)
- Activity Repetition (e.g., Counting)
- Touching (e.g., repeatedly Touching Walls)
- Alprazolam : 0.5-1 mg/day
- Clonazepam : 0.25-0.5 mg/day
- Clomipramine
- Fluoxetine
- Fluvoxamine
- Used for Severe Anxiety and Tics Disorder When there is a History of Hyperactivity Disorder.
- Haloperidol
- Risperidone
TREATMENT MODALITIES-
Pharmacological Treatment
Benzodiazepines :
Antidepressants :
Antipsychotics:
ECT (Electro-Convulsive Therapy):
- OCD Severe Depression
Self-Help Group:
- Maintain a Healthy Lifestyle.
- Be Aware of
- Relaxation Techniques:
- Yoga (Yoga)
- Meditation (Meditation)
- Massage
Psychotherapy:
- Psychodynamic Psychotherapy
- Cognitive Behavioral Therapy (CBT – Cognitive Behavioral Therapy)
- Supportive Therapy
NURSING MANAGEMENT OF PATIENT WITH OCD-(Nursing Management of OCD Patients)
Common Nursing Diagnoses for OCD Patients:
- Severe Anxiety
- Impaired Communication
- Altered Coping Ability
- Impaired Judgment
- Disturbed Sleep Pattern
- Lower Self-Esteem
1. Severe Anxiety:
Objectives:
- Reduce Anxiety.
- Minimize Compulsive Behavior.
Nursing Interventions:
- Observe Anxiety Levels and Establish Relationship with Respect, Warmth, and Empathy.
- Provide a Clean and Comfortable Environment.
- Motivate the Patient to discuss their Anxiety .
- Identify Anxiety-Producing Situations and provide Psychological Support.
- Encourage the Patient to express their Feelings and work on alleviating their Fear.
- Discourage Compulsive Behaviors and administer Medications (Medication) as per Prescription .
2. Impaired Communication:
Objectives:
- Improve Communication.
- Enhance Social Interaction.
Nursing Interventions:
- Provide a Trusting Environment.
- Help develop an Effective Relationship with the Patient.
- Discover the Source of Anxiety and observe for other Symptoms like Rigidity (Rigidity) and Ambivalence (Ambivalence).
- Motivate the Patient (Patient) to engage in conversations with others.
- Communicate in a Simple and Concise manner, teaching Communication Skills .
3. Altered Coping Ability:
Objectives:
- Improve Coping Abilities.
- Help manage Obsessive-Compulsive Behaviors.
Nursing Interventions:
- Assess the Coping Abilities.
- Build a relationship with the Patient with Warmth and Respect.
- Fulfill the Dependency Needs of the Patient and provide Positive Reinforcement.
- Accept the Patient’s Compulsive Behaviors initially.
- Gradually set Limits on Ritualistic Behavior.
- Do not punish the Patient for their Symptoms.
- Observe how many times the Patient engages in Hand Washing within an hour.
- Teach new Adaptation Skills to deal with Ritualistic Behavior .
- Use Cognitive and Modeling Therapy
- Explain lithium treatment in detail.
Introduction:
Lithium is a mood stabilizer medication used to control manic and depressive episodes in mental disorders, especially bipolar disorder. It is also used in patients with acute mania, rapid emotional changes, and suicidal tendencies.
Mechanism of Action of Lithium
Lithium is a positive ion that enters cells in a similar way to sodium, and affects the flow of neurotransmitters. It specifically modulates the reuptake of serotonin and norepinephrine, which leads to mood stabilization.
It also inhibits the second messenger system and protein kinase within the cell, resulting in reduced mood swings in the patient.
Clinical Uses:
Bipolar Disorder – For both acute mania and maintenance therapy.
Recurrent Depression – Where other therapies have not been effective.
Schizoaffective Disorder – where there are mood swings with schizophrenia.
Suicidal Ideation – Effective in reducing suicide risk.
Aggression & Impulsivity – especially in patients with intellectual disability.
Therapeutic Range:
The therapeutic blood level for lithium is 0.6 to 1.2 mEq/L.
▪︎ < 0.6 mEq/L: Ineffective ▪︎ > 1.5 mEq/L: Toxic
Therefore, plasma level monitoring is essential.
Side Effects:
Gastrointestinal: Vomiting, Diarrhea
Neurological: Tremors, Lethargy, Panic
Endocrine: Hypothyroidism (Hypothyroidism)
Renal: Polyuria, nephrogenic diabetes insipidus
Cardiac: T-wave flattening on ECG
Lithium toxicity: If levels are high – ataxia, confusion, coma
Contraindications:
▪︎ Pregnancy – especially in the first trimester Teratogenic effect
▪︎ Kidney Disease
▪︎ Severe Dehydration
▪︎ Heart Block
Nursing Management:
Blood Level Monitoring:
▪︎ Lithium levels should be monitored for 5-7 days after initiation and regularly thereafter
▪︎ Monitor for lethargy, ataxia or confusion
Maintain hydration:
▪︎ The patient is advised to drink enough water to avoid dehydration. Thyroid and kidney function tests: Regular TFT (Thyroid Function Test) and RFT (Renal Function Test) should be performed. Watch for drug interactions: NSAIDs, ACE inhibitors, and diuretics may increase lithium levels. Patient education: Avoid excess salt while taking medications. Pregnancy or severe Inform the doctor immediately when you get sick. Do not stop medication suddenly. c) Explain admission and discharge procedure in hospital. Admission and discharge procedure in hospital. Admission Procedure. Admission Procedure. Admission is the process of admitting a patient to a hospital. This process can be of two types, Emergency or Routine, depending on the clinical condition of the patient.
(A) Preliminary Steps
Admission Desk: When the patient comes to the hospital, he first goes to the admission desk, where the patient’s basic information is taken such as name, age, gender, address, contact numbers, and emergency contact.
Admission Form: An admission form is filled by the patient or his family, in which the patient’s illness is (Illness), Past Medical History and other necessary details are written.
ID Verification: The patient’s identity document is verified such as Aadhar card, PAN card etc.
(B) Clinical Assessment
Physician Examination: The physician on duty conducts a physical examination of the patient and determines the need for admission.
Vital Sign Checking: Pulse, Blood pressure, temperature, respiratory rate are checked.
Admission Order: The physician orders admission and assigns the patient to a specific ward or unit.
(C) Ward Transfer:
The patient is taken to his ward on a stretcher or wheelchair.
The ward nurse receives the patient and conducts a nursing assessment.
The patient’s personal belongings are recorded.
The patient is allocated a bed and an admission nursing care plan is prepared.
Discharge Discharge Procedure
Discharge is the process in which a patient is discharged from the hospital after completing their treatment.
(A) Discharge Order
Treating Physician: After assessing the patient’s progress, if the patient is now stable, he gives an order for discharge.
Discharge Note: Prepared by the physician, which includes the diagnosis, treatment performed, Prescribed Medication, Follow-up instructions are given.
(B) Final Checking and Clearance
Billing Department: Prepares the final bill of all the charges of the patient such as room charge, medicine, diagnostic test etc.
Financial Clearance: The patient or his family has to pay the bill and get a receipt.
(C) Discharge Counseling
Nursing Staff: Provides health care instructions to the patient such as timing of home medications, diet, rest and home care instructions.
Follow-up Appointment: Determines when the patient should visit the clinic again.
(D) Patient Release
After all procedures are completed The patient is discharged with dignity and instructed to take their relatives with them.
Conclusion:
The admission and discharge procedure in the hospital is done in a structured and systematic manner. The safe admission and discharge of the patient is the main responsibility of the healthcare team. It is essential to provide proper guidance to the patient or family at each step so that there are no problems during the treatment and the patient’s satisfaction level remains high.
Q-4 Write short notes. Write short notes. (Any three)12
a) Mental Health Act. Mental Health Act.
Mental Health Act 1987
History:
The Mental Health Act was drafted by Parliament in 1987
• Came into force in all states and union territories of India in April 1993
• Replaces the Indian Lunacy Act of 1912
• Which replaced the earlier Indian Lunatic Asylum Act of 1858
Definition
“An act to consolidate and amend the law relating to the treatment and care of mentally ill persons, and to make better provision in respect of their property and affairs and for matters connected with or incidental thereto”
The Mental Health Act is divided into 10 chapters and 98 sections.
Objectives:
1. To establish central and state authorities for licensing and supervision of psychiatric hospitals
2. To establish mental hospitals and nursing homes
3. To provide for the inspection of the workings of these hospitals
4. To provide for the custody of mentally ill persons who are incapable of caring for themselves and who are a danger to themselves and or others
5. To protect society from the dangerous manifestations of mental illness
6. To regulate the procedure of admission and discharge of mentally ill persons
7. To protect the rights of detained persons
8. To protect citizens from unnecessary detention
9. To provide for the maintenance of mentally ill persons
10. To provide legal aid at the expense of the state to indigent mentally ill criminals
11. Amendment of the Indian Lunacy Act to replace the objectionable terms
License
No person shall establish or maintain a psychiatric hospital or psychiatric nursing home unless he holds a valid license from the Central Government or a State Government
Application for License
A person who intends to establish or maintain a psychiatric hospital or psychiatric nursing home, unless he already holds a valid license Application to the licensing authority for grant of license.
Period and renewal of license
A license shall not be transferable or inheritable. Every license, unless earlier revoked, shall be valid for a period of five years from the date on which it is granted.
Admission and detention in a psychiatric hospital
1. Admission on voluntary basis
2.Admission in special circumstances
3. Reception orders
1. Admission on voluntary basis
Admission as a voluntary patient
Request for admission by guardian
Regulations in respect of voluntary patients:
On receipt of the request, the Medical The Officer-in-Charge shall examine within a period of 24 hours and if satisfied, he may accept such application as a voluntary patient.
Every voluntary patient admitted shall be bound to abide by the rules framed by the Medical Officer.
Admission on voluntary basis
Request by the Principal for admission as a voluntary patient
Request by the Guardian for admission to the ward
Regulations in respect of voluntary patients:
On receipt of the request, the Medical Officer-in-Charge shall examine within a period of 24 hours and if satisfied, he may accept such application as a voluntary patient.
Every voluntary patient admitted shall be bound to abide by the rules framed by the Medical Officer Admission in special circumstances:
Any mentally ill person who does not or cannot express his wish for admission may be admitted and kept as a patient in a mental hospital on application made on his behalf by a relative or friend of the mentally ill person if the Medical Officer-in-Charge is satisfied that it is necessary in the interests of the mentally ill person to do so
Reception Orders
➤Application for Reception Order:
• An application for a reception order may be made by
– the Medical Officer in Charge
– the spouse or other relative of the mentally ill person
> Where the Medical Officer in Charge is satisfied that:
. Treatment in a mental hospital is necessary for a period exceeding six months
It is in the interest of the health and safety of the mentally ill person or for the protection of others to apply to the Magistrate within the local limits of the jurisdiction of the psychiatric hospital.
➤ Every application shall be as follows:
Duly signed and verified
• Must be accompanied by two medical certificates
From two medical practitioners, one of whom shall be in the service of the Government
Oddish Charge:
Discharge by Medical Officer
■ Discharge on Application
Discharge on Request
Discharge of a person after inquiry has shown him to be of sound mind
Discharge by Medical Officer:
On the recommendation of two medical practitioners, one of whom shall preferably be a psychiatrist
The Medical Officer shall, by order in writing, direct the discharge of any person from a psychiatric hospital
Discharge on application, except for a voluntary patient
Any person detained in a psychiatric hospital under an order and in pursuance of an application
Discharge shall be granted on an application made on his behalf to the Medical Officer in Charge
No person shall be discharged if the Medical Officer in Charge certifies in writing that the person is dangerous and unfit to grow up.
Discharge on Request
Any person (not being a mentally ill prisoner) detained in pursuance of an order, who appears to have recovered from his mental illness, may apply to the Magistrate for discharge from a psychiatric hospital.
•The application made shall be supported by a certificate from the Medical Officer in Charge or a Psychiatrist
The Magistrate may, after making such inquiry as he thinks fit, order the person to be discharged or dismiss the application.
Discharge of the person found on inquiry to be of sound mind
If any person detained in a psychiatric hospital in pursuance of a reception order is subsequently found
on inquiry to be of sound mind or
capable of looking after himself and
managing his affairs
the Medical Officer-in-Charge shall discharge such person from such hospital or nursing home
Leave of Absence
Application for leave of absence may be made to the Medical Officer-in-Charge:-
by the mentally ill husband or wife
by the relative husband or wife of the mentally ill person or
by the person on whose application the mentally ill person was admitted
Every application shall be accompanied by a bond undertaking:-
to take proper care of the mentally ill person
to prevent the mentally ill person from harming himself or others, and
to return the mentally ill person to the mental hospital on the expiry of the leave
The Medical Officer-in-Charge may grant leave of absence for such period as he may deem necessary is
The total number of days shall not exceed sixty days
Subject to any general or special order of the State Government, any mentally ill person other than a voluntary patient
shall be removed from any mental hospital or mental nursing home to any other mental hospital or mental nursing home
within the State, or with the consent of the Government of that other State, to any other State
b) Milieu Therapy.
- Milieu is a French word in which Mi means middle and Lieu means environment. Thus milieu means environment.
- In psychiatry, Therapy involving the environment or milieu is called milieu therapy.
- Therapeutic milieu means providing the patient with a healthy environment that helps in the patient’s recovery. Most mental illness is caused by an unhealthy environment. Thus, a healthy therapeutic environment increases the social productivity of the patient.
- Miliue therapy includes a safe physical environment, all members of the treatment team, and other clients.
- The purpose of the therapeutic milieu is to promote the recovery of the client admitted to the hospital and prevent complications.
GOALS
- ~Change maladaptive behavior to adaptive behavior.
- ~Promote early recovery.
- ~Reduce length of hospital stay.
- ~Resocialize the client For.
- ~To promote self-confidence.
COMPONENTS
•Maintaining a Safe Environment
- ~Dispose of all needles safely and in a manner that does not come into contact with the client.
- ~Smoking should not be allowed and Restrict or monitor the use of matches and lighters.
- ~Keep sharp objects away from the patient.
- ~Identify potential objects e.g. Mop handles, hammer.
- ~Do not keep medication unlocked.
•The Trust Relationship
- ~Trust is the foundation of a therapeutic relationship, developing trust is the key to a therapeutic environment.
•Building Self Esteem
- ~Set and maintain limits.
- ~Accept the client as a person.
- ~Be decisive at all times.
- ~Provide the client with tasks, responsibilities, and activities at the beginning.
- ~Let the client make their own decisions based on their condition.
•Limit Setting
- ~State the expectation or limit clearly, directly, and simply, and as clearly as possible.
- ~The consequences of the client crossing the limit should also be clearly stated at the outset.
c) Misconception about mental illness. Misconceptions about mental illness.
Here are some common myths and misconceptions about mental retardation:
- Intellectual disability is similar to mental illness:
Intellectual disability is a developmental condition in which there is an alteration in intellectual function.
- People with intellectual disabilities cannot learn new skills.
People with intellectual disabilities can learn many new things and skills. Which requires different teaching methods and requires more effort to learn.
- Intellectual disability is more severe:
Intellectual disability is not always severe, it can be seen in mild to profound forms.
- Intellectual disability is caused by bad parenting It occurs due to:
Intellectual disability is not caused by bad parenting but by many other factors. Genetic factors, environmental factors, complications during pregnancy and birth
- People with intellectual disabilities are always seen as happy and friendly :
People with intellectual disabilities experience all kinds of emotions and personalities such as sadness, frustration, anger, joy
- Intellectual disability cannot be detected until the child is in school:
Intellectual disability can be detected during early childhood through developmental screening and assessment.
- People with intellectual disability cannot hold jobs:
Many people with intellectual disabilities are capable of doing work or jobs and they are able to do a variety of jobs.
- People with intellectual disabilities can be clearly identified by looking at them:
People with intellectual disabilities cannot be identified by looking at them. People with mild intellectual disabilities are difficult to identify. Identifying such people is a challenge.
d) Electroconvulsive Therapy (ECT)
Introduction:
Electroconvulsive Therapy (ECT) – Electroconvulsive therapy is a medical mental health treatment in which a controlled electrical current is passed through the patient’s brain to induce a therapeutic seizure. This therapy is mainly used for patients who have mental health conditions such as severe depression, bipolar disorder, schizophrenia, or catatonia and do not get relief from other treatments.
History and uses:
ECT was first developed in Europe in 1938. Before that, options for severe mental disorders were very ineffective. Today, ECT is given in a safer, controlled and modern way, using general anesthesia and muscle relaxants.
Procedure:
1. Pre-evaluation:
Before starting ECT, the patient’s medical history, physical examination, blood tests, ECG, (ECG), and often brain imaging tests (such as MRI) are taken.
2. Anesthesia and Muscle Relaxant:
The patient is placed under general anesthesia so that he does not feel any pain. Muscle relaxants are also given so that the muscular movements of the body are controlled during the seizure.
3. Placement of electrodes: Electrodes are placed on the scalp – either bilaterally or unilaterally.
4. Electrical stimulation: A controlled electrical current (such as 70-120 volts for 0.7 seconds) is given. As a result, the patient’s brain experiences a known and therapeutic seizure.
5. Post-procedure Monitoring: The patient is monitored in the recovery area after ECT, keeping in mind the condition. The patient wakes up in a very short time.
Frequency of Sessions:
A typical ECT consists of 6 to 12 sessions, which are given two or three times a week. In special cases, maintenance ECT may also be given, in which treatment is continued over the long term.
Indications:
- Treatment-resistant Depression
- Severe Suicidal Tendency
- Severe Catatonia
- Psychotic Depression
- Atypical Response to Therapy
Benefits:
- Rapid Treatment Outcome
- Immediate Effect in Severe Cases
- Improvement in the patient’s mood, expectations, and behavior
- Possibly less need for medical medications
Possible Side Effects:
- Temporary loss of orientation or disorientation
- Temporary memory loss, especially of recent events For
- Headache
- Vomiting or Nausea
- Fatigue
Rare Complications:
- Heart Rhythm Abnormalities (Cardiac Arrhythmia)
- Respiratory Depression
These complications are very rare and mainly occur in high risk patients.
Myths vs Reality:
- Many people believe that ECT is atrocious, but today’s method is very safe and medically approved.
- ECT causes permanent memory loss – this is also a misconception. Most patients are able to lead normal lives.
- Electroconvulsive Therapy (ECT) is a modern medical psychiatric intervention that often proves to be a turning point in the patient’s life.
Q-5 Define the following (any six) (Any six) 12
a) Neologism
Neologism is a newly coined word or phrase that has recently entered the language and was not previously in use. In medical and psychological terms, Neologism refers to the condition in which a person creates words that do not actually exist, but are meaningful to that person. This type of behavior is mainly seen in diseases such as Schizophrenia, Aphasia or Neurological Disorders. Neologism, apart from being a newly emerging part of the lexicon, can also be a pathological language feature that indicates trauma to the functioning of the language centers of the brain.
b) Mental Health Mental Health
Mental Health is a stable and positive mental state in which a person can manage the stresses of life to the best of their ability, work effectively, contribute to society, and maintain healthy relationships. Mental Health does not just mean the absence of mental illness, but also includes Emotional Well-being, Psychological Resilience and Cognitive Functioning. This includes illnesses such as Depression, Anxiety Disorders, Bipolar Disorder, PTSD and Schizophrenia. Mental Health is of central importance for Preventive Medicine and Public Health.
C) Cataplexy
Catalepsy is when a person remains in a constant position without any movement. It is seen in patients with schizophrenia.
d) Displacemem-Displacement
- Displacement means displacement
- In this defense mechanism, a person unconsciously transfers his emotional feelings to another person or object which is less dangerous.
- Example: A worker works in an office and his boss gets angry with him. This worker cannot tell the boss anything, so he goes home and gets angry with his family member, which is called displacement.
- A student A nurse gets scolded by her senior. The student nurse cannot get angry with her senior but she goes home and punishes her younger siblings and gets angry.
E) Delirium – Delirium
This is an acute common clinical syndrome, which is a reversible and organic condition, in which the person becomes confused and in which there is disorientation and disturbance in perception, and consciousness is impaired. The person cannot concentrate and in it acute Cognitive dysfunction is called delirium. Delirium is a syndrome, not a disease, and has many causes.
F) Euphoria – Euphoria
A mild elevation in mood is seen. And the person feels emotional and physical well-being. This is seen in mania.
g) Bulimia Nervousa – Bulimia Nervosa
Bulimia nervosa is characterized by repeated episodes of eating unusually large amounts of food and lack of control over eating. The person eats more and self-induces vomiting or misuses diuretic and laxative medications to prevent weight gain.
TYPES
(1) Purging type
The person eats more and self-induces vomiting.
(2)Non-purging type
The person eats more and immediately does exercise/yoga and fasting.
h) Dejavu – Deja Vu
In this, the person feels that he has seen this person, place or scene somewhere but does not know where and when. The real one experiences the situation for the first time which is called deja vu.
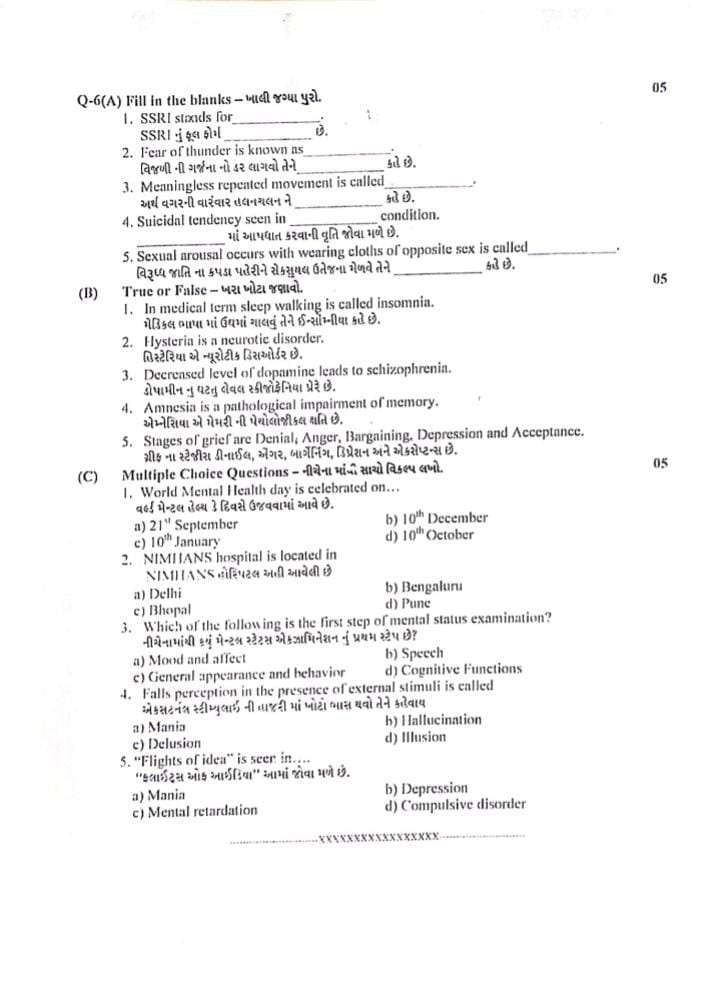
Q-6(A) Fill in the blanks – Fill in the blanks.
1) SSRI stands for……The full form of SSRI is……:✅ Selective Serotonin Reuptake Inhibitor
👉 The full form of SSRI is: Selective Serotonin Reuptake Inhibitor, which is a type of anti-depressant drug.
2) Fear of thunder is known as…… Fear of thunder is……:✅ Astraphobia
👉 Fear of thunder is called Astraphobia.
3) Meaningless repeated movement is called…… Meaningless repeated movement is called……:✅ Stereotypy
👉 Constant and unrestrained movement (such as waving hands, tapping) is called Stereotypy.
4) Suicidal tendency seen in…… condition…… A person who feels sexually aroused by wearing clothes of the opposite sex is called Transvestism.
B) True or False – Tell me the truth.
1.In medical term sleep walking is called insomnia. In medical terms, sleep walking is called insomnia: ❌ False
🔹 Sleep walking is medically called Somnambulism.
🔹 Insomnia means difficulty in falling or staying asleep.
2.Hysteria is a neurotic disorder. Hysteria is a neurotic disorder: ✅ True
🔹 Hysteria is classified under Neurotic Disorders, specifically as Conversion Disorder in modern psychiatry.
3. Decreased level of dopamine leads to schizophrenia. ❌ False
🔹 Increased dopamine activity (particularly in the mesolimbic pathway) is associated with positive symptoms of schizophrenia.
🔹 Dopamine deficiency is more commonly linked to Parkinson’s disease, not schizophrenia.
4. Amnesia is a pathological impairment of memory. Amnesia is a pathological loss of memory : ✅ True
🔹 Amnesia refers to pathological loss of memory, either temporary or permanent, due to brain injury or psychological causes.
5.Stages of grief are Denial, Anger, Bargaining. Depression and Acceptance. The stages of grief are Denial, Anger, Bargaining, Depression and Acceptance :✅ True
🔹 These are the Kubler-Ross Five Stages of Grief – a widely accepted psychological model of coping with loss.
C) Multiple Choice Questions. Write the correct option from the following.05
1.World Mental Health day is celebrated on… World Mental Health day is celebrated on…
a) 21 September
b) 10th December
c) 10th January
d) 10th October
Explanation: Every year on 10th October, World Mental Health Day is observed to raise awareness about mental health issues and mobilize efforts to support mental well-being globally.
2.NIMHANS hospital is located in…… NIMHANS hospital is located here.
a) Delhi
b) Bengaluru
c) Bhopal
d) Pune
Explanation: NIMHANS (National Institute of Mental Health and Neurosciences) is a premier mental health and neurosciences institute located in Bengaluru, Karnataka.
3.Which of the following is the first step of mental status examination? Which of the following is the first step in a mental status examination?
a) Mood and affect
b) Speech
c) General appearance and behavior
d) Cognitive Functions
Explanation: Mental Status Examination (MSE) begins with General appearance and behavior, as it gives the first observable insight into the patient’s mental and emotional state.
4.Falls perception in the presence of external stimuli is called……Falls perception in the presence of external stimuli is called
a) Mania
b) hallucinations
c) Delusion
d) Illusion
seeing a rope as a snake).
In contrast, Hallucination occurs without external stimulus.
5.”Flights of idea” is seer in….. “Flights of idea” is seen in.
a) Mania
b) Depression
c) Mental retardation
d) Compulsive disorder
Explanation: Flight of ideas is a symptom of Mania, where the person rapidly shifts from one idea to another with superficial connections — often seen in bipolar disorder during the manic phase.