—ENGLISH-ANATOMY UNIT : 10 REPRODUCTIVE SYSTEM (PART : 1) FEMALE
REPRODUCTIVE SYSTEM (Reproductive System):
INTRODUCTION (Introduction):
- An ability that allows an individual to An individual can produce or give birth to its offspring. This process is called reproduction.
- Due to reproduction, the species maintains its existence.
- Almost all the systems of the body are started at the time of birth, but the reproductive system is such a system, which starts (active) at the time of puberty.
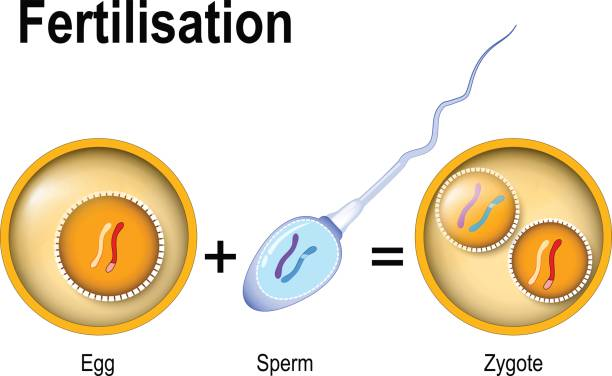
- There are certain types of germ cells inside the human being. They are called gametes.
The primary (main) sex organ of the female is the ovary and the MALE has the testes. - The ovary produces female eggs and the testes produce male sperm.
All other reproductive organs work as accessory organs or supportive organs.
When male and female gametes fuse, they form a zygote, which later develops into a fetus.
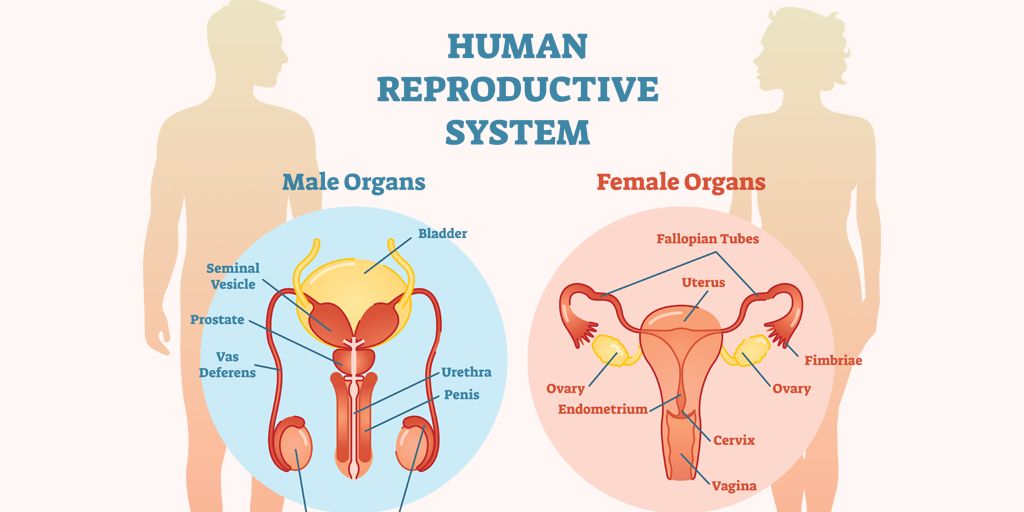
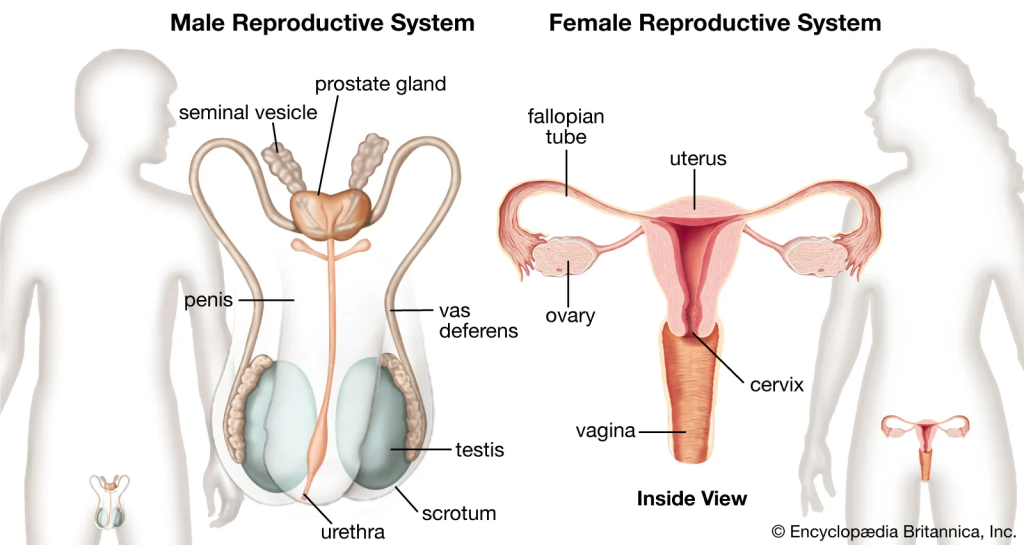
Human reproductive system is as follows :-
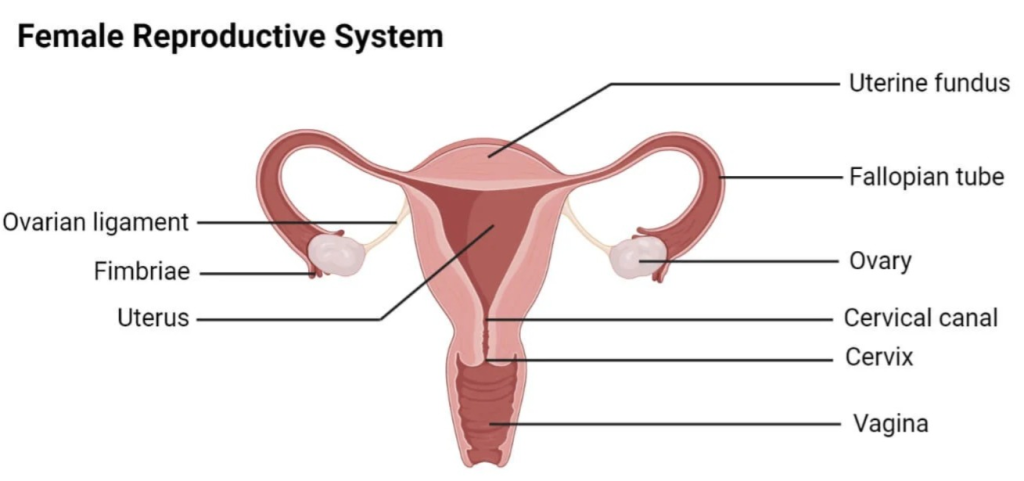
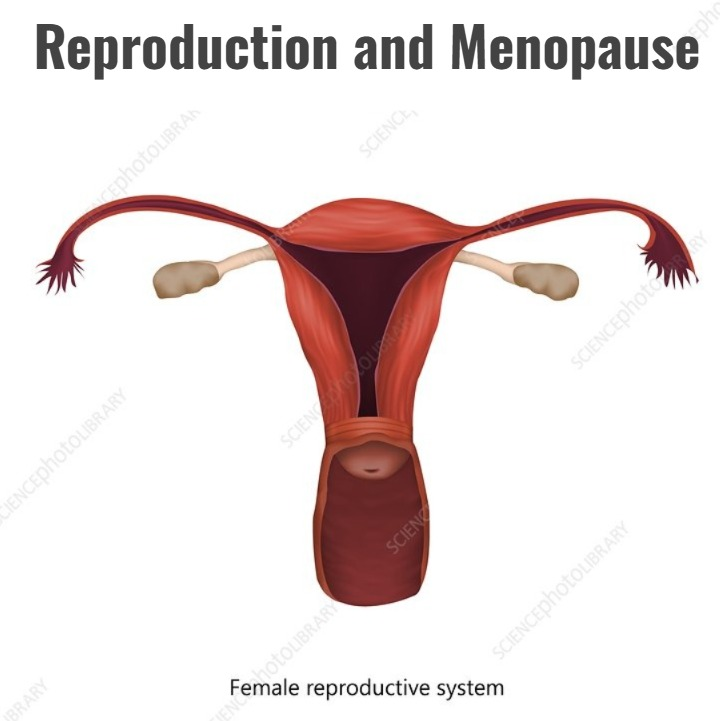
1) FEMALE REPRODUCTIVE SYSTEM (Female Reproductive System)
2) MALE REPRODUCTIVE SYSTEM (Male Reproductive System)
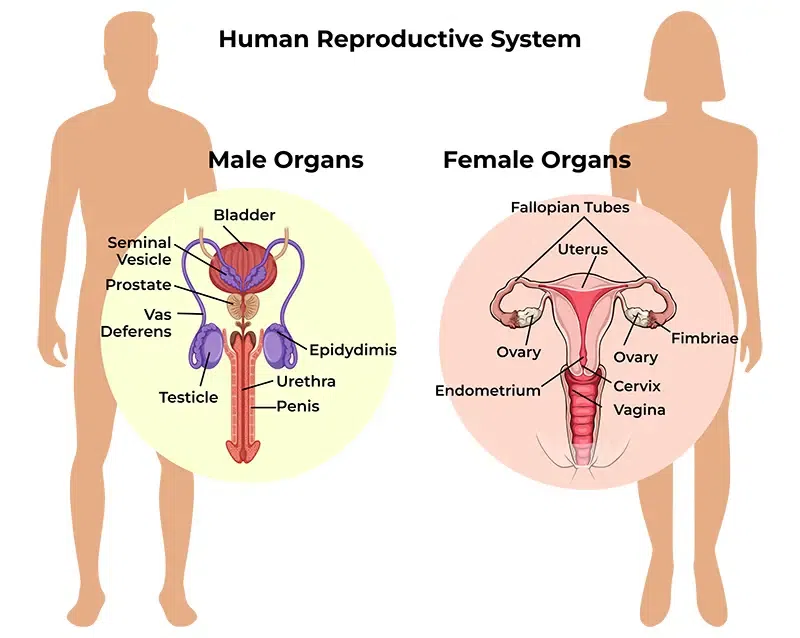
1) FEMALE REPRODUCTIVE SYSTEM (Female Reproductive System):
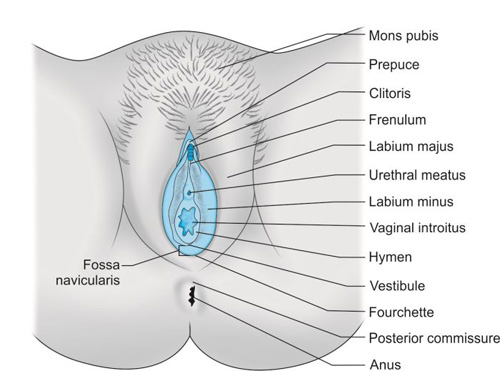
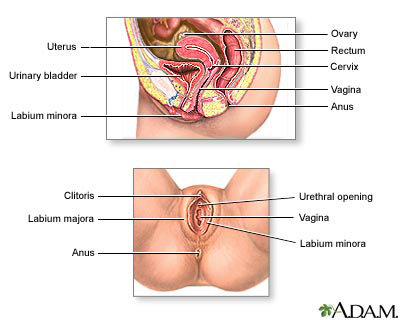
A. External genitalia of female / VULVA / PUEDENDAM
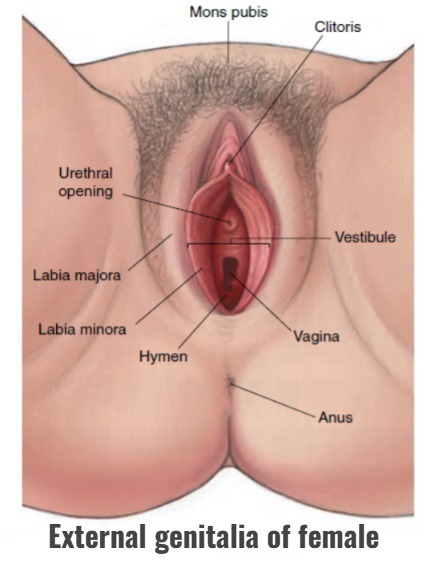
- Mons pubis
- Labia majora
- Labia minora (Labia minorora)
- Clitoris
- Perineum
- Vestibule
- Mammary gland
MONS PUBIS:
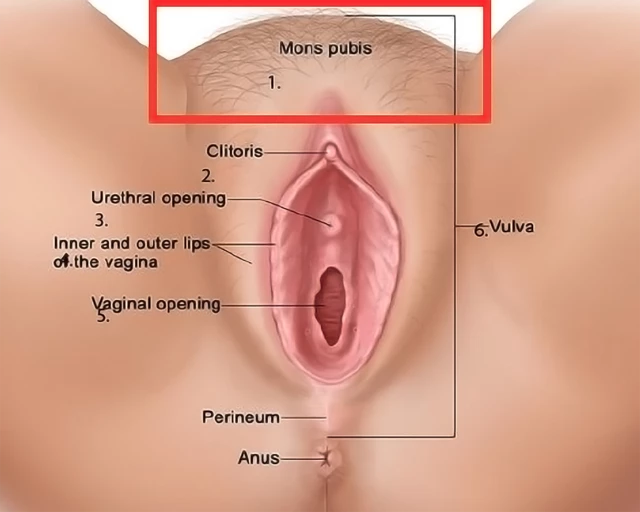
- The mons pubis is a cushion-like structure made of fat and skin that lies in front of the symphysis pubis.
- During puberty it becomes covered with hair and forms a horizontal margin.
LABIA MAJORA (Labia Majora):
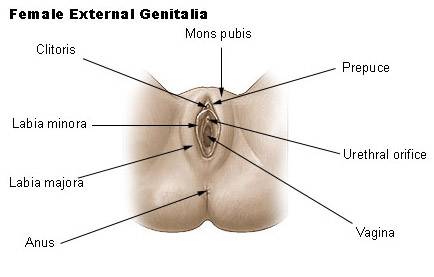
- There are two thick folds on the front side. Which form the brim of the vulva. (The vulva is the external reproductive organ, also called the vulva).
- Labia Majora is made up of skin, fat, areolar tissue, and smooth muscle. On the surface of which hairs are located. On its inner side are the sebaceous glands.
The round ligament ends at the labia majora. - The labia majora meet anteriorly at the mons pubis and posteriorly at the skin of the perineum. Just as the male has the scrotum, the female has the labia majora.
LABIA MINORA:
- The labia minora are two small skin folds (which do not contain fat or hair but do contain many sebaceous glands) located inside the labia majora.
- Its upper part meets the clitoris and forms the prepuce (the cover of the clitoris in females, just like the foreskin on the penis in males), and its lower part forms the floor (frenulum) of the clitoris.
CLITORIS (Clitoris):
- It is cylindrical in shape and triangular in shape. It is made up of erectile tissue (stimulating tissue).
- Just as a male has a penis, a female has a clitoris.
It contains sensory nerve endings. It acts as an aphrodisiac during sexual intercourse.
PERINEUM (Perineum):
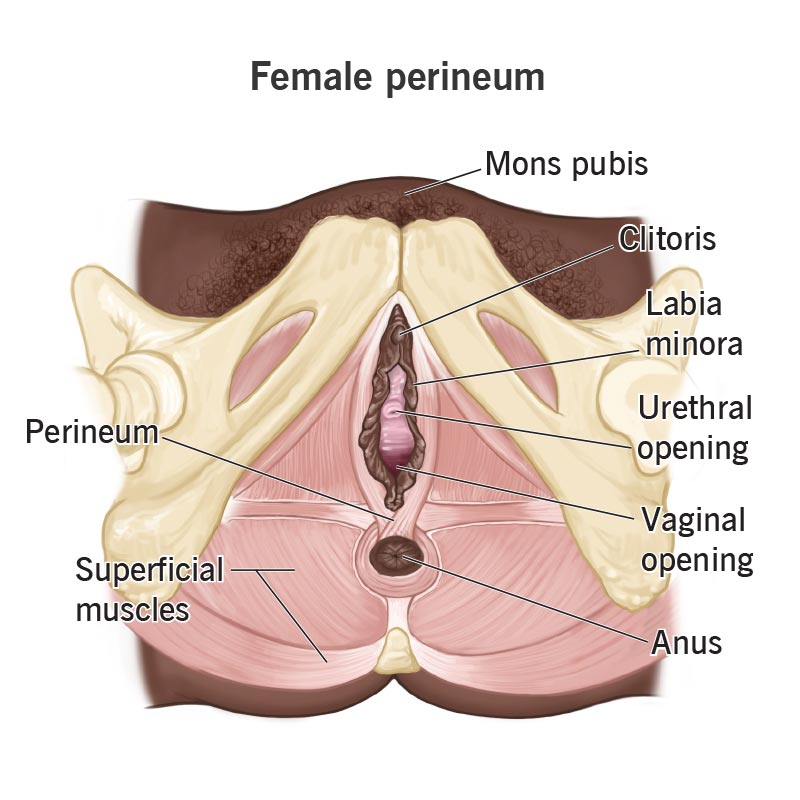
- This is an area that extends from the base of the labia majora to the anal canal. It is roughly triangular in shape.
- It is made up of connective tissue, fat, and muscle. It provides attachment to the muscles of the pelvic floor.
VESTIBULE:
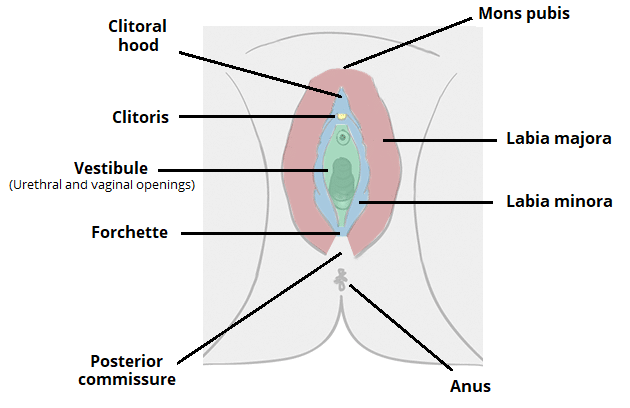
- Vestibular glands (Bartholin glands) are 2 and are located on both sides of the vaginal opening. They are about the size of a pea. They have ducts that open into the vagina and secrete mucous. This keeps the vulva moist and the vaginal cavity wet.
2. INTERNAL REPRODUCTIVE ORGANS (Internal Reproductive Organs):
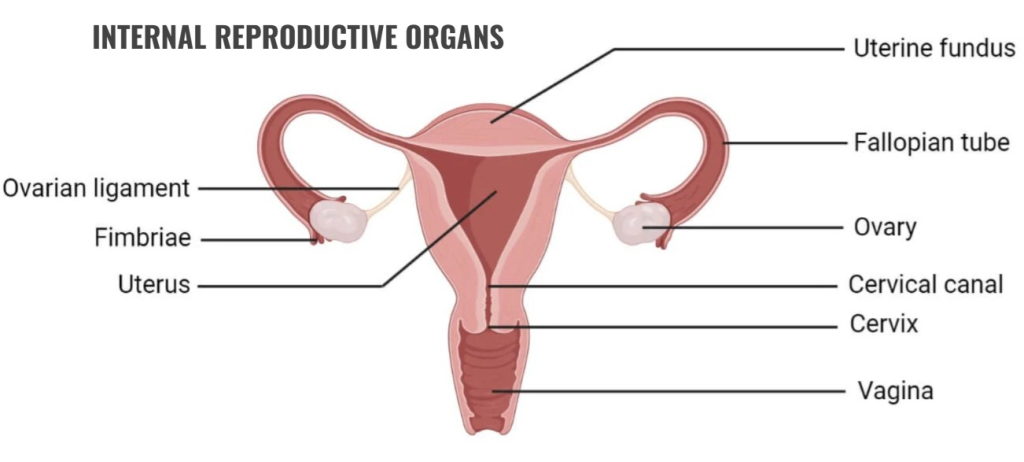
These organs reside within the pelvic cavity. They include the following organs.
Internal reproductive organs are as follows.
- Vagina
- Uterus
- Uterine tube or Fallopian tube or Salpinges
- Ovaries.
VAGINA:
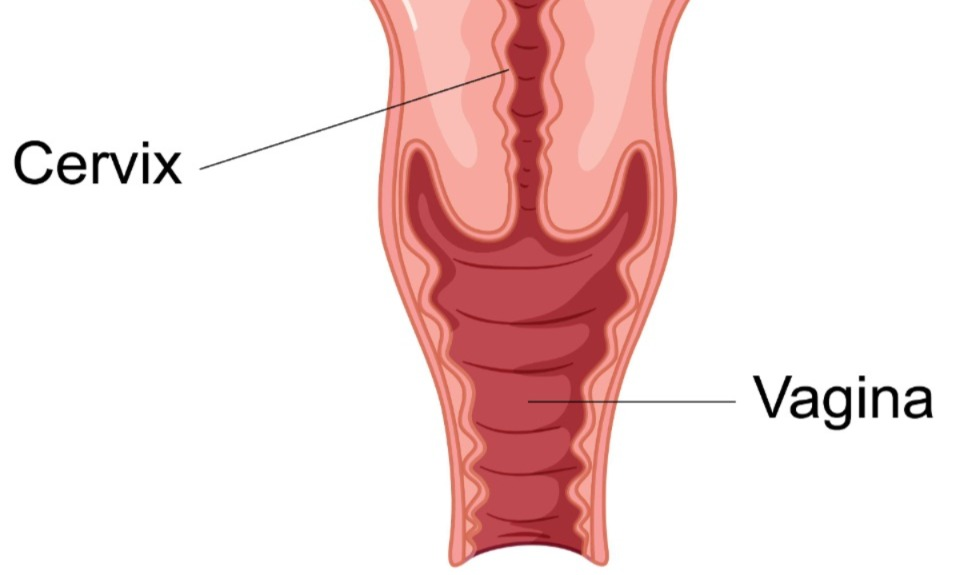
- The vagina is a fibromuscular tube. Its lining is made up of stratified squamous epithelium cells. It is the structure that connects the internal and external reproductive organs.
- It is located in front of the urinary bladder and behind the rectum. Its front wall is 7.5 cm and the back wall is 9 cm.
Structure of Vagina
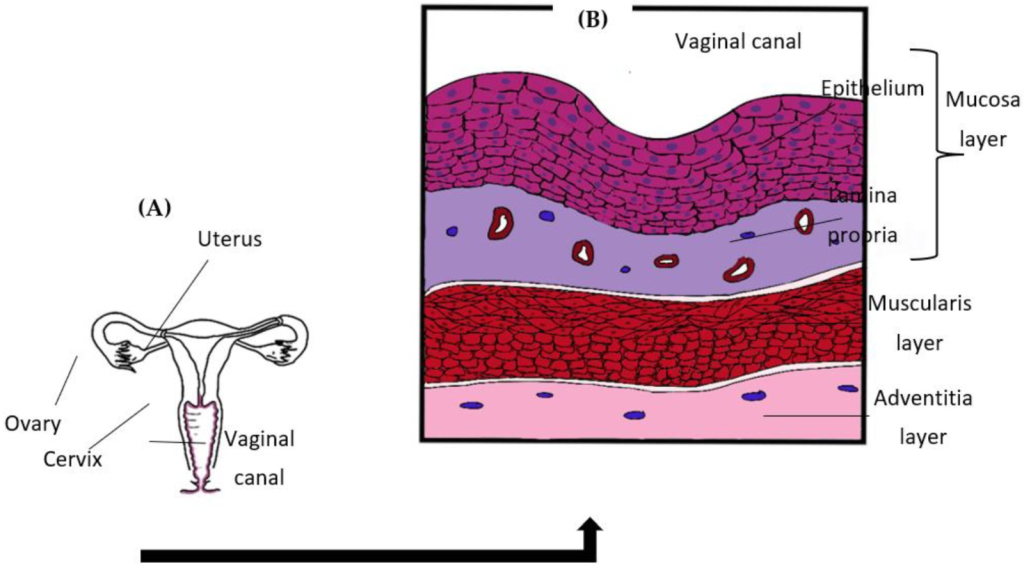
Vajayana has three layers
1.Outer Layer (Outer Layer)
2.Middle Layer (Middle Layer)
3.Inner Layer (Inner Layer)
1.Outer Layer :- The outer layer is made up of areolar tissue
2.Middle Layer (Middle Layer) :- The middle layer is made up of smooth muscles.
3.Inner Layer :- It is made up of stratified squamous epithelium tissue. Which forms rugae (rugae – like projections).
It does not contain any secretions. It remains moist due to cervical secretions.
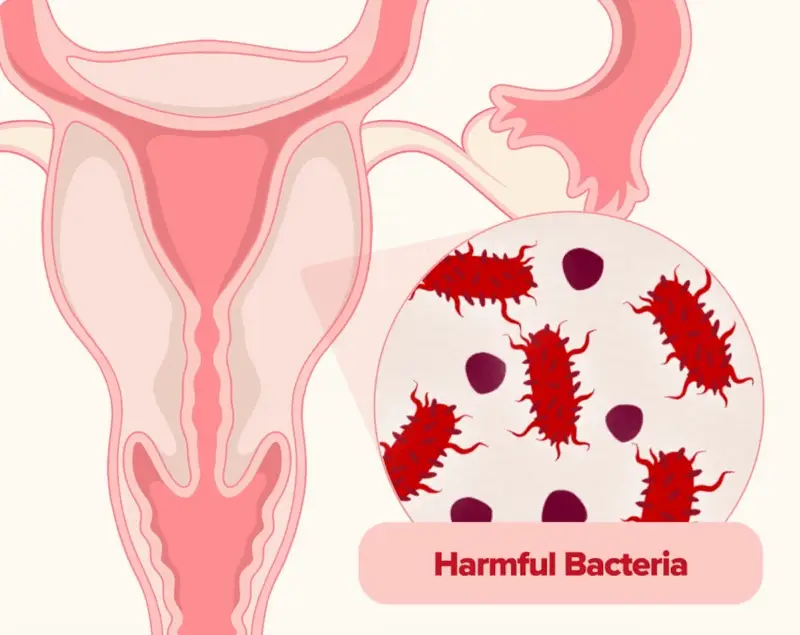
Between puberty and menopause, bacteria called lactobacillus acidophilus make the pH of the vagina acidic. Which is 4.9 to 3.5. Due to the acidic pH, infecting microorganisms do not enter the vagina.
Blood Supply :
By the uterine artery and vaginal artery which are branches of the internal iliac artery.
The venous plexus is located in the wall of the muscles and drains into the internal iliac vein.
NERVE SUPPLY:
There are parasympathetic nerves, sympathetic nerves and somatic nerve supply
FUNCTIONS:
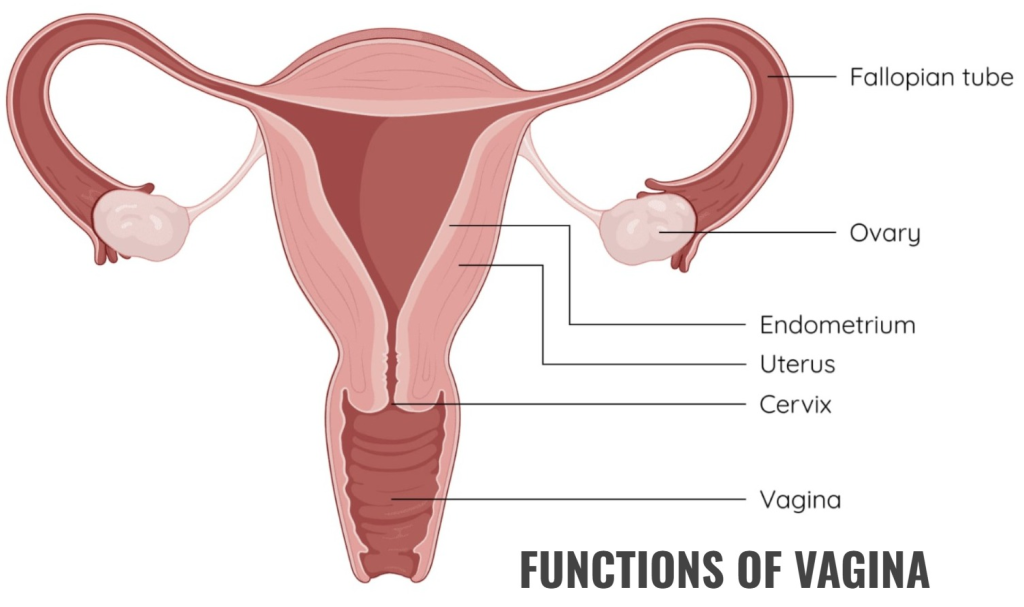
- The vagina allows the entry of the penis during intercourse.
- It holds the sperm until it moves to enter the uterus.
- It is an elastic structural part that helps the baby to come out during birth.
- The sensory nerve endings in the vagina provide the feeling of sexual pleasure.
- It acts as the outer opening of the urinary tract.
- Women experience monthly menstrual bleeding, in which blood from the uterus comes out through the vagina.
- The acidic pH of the vaginal cavity inhibits the growth of microorganisms.
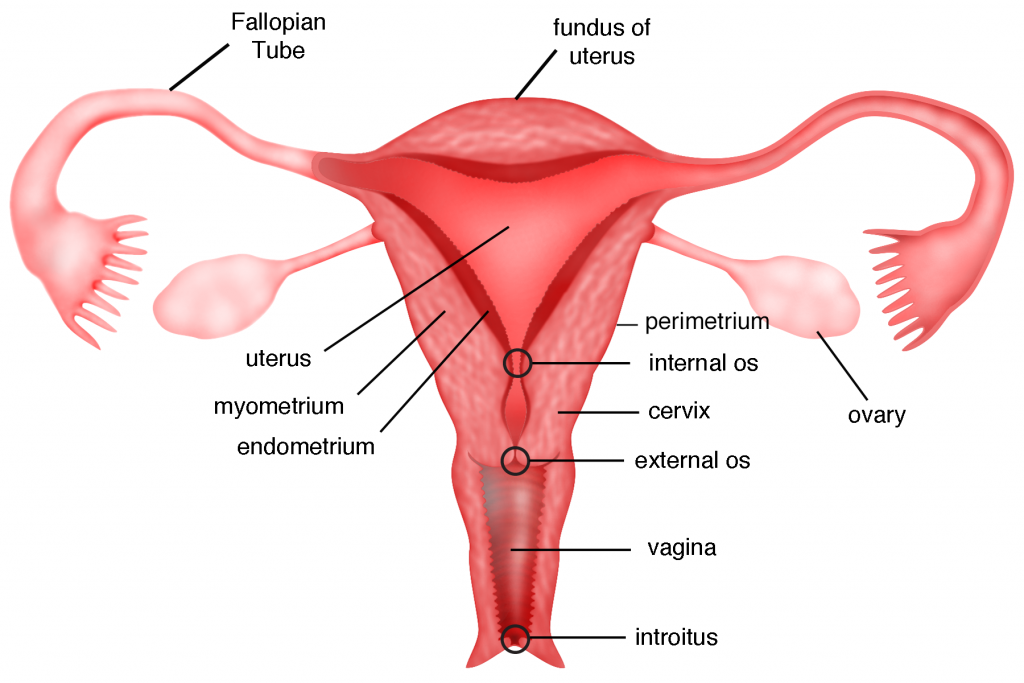
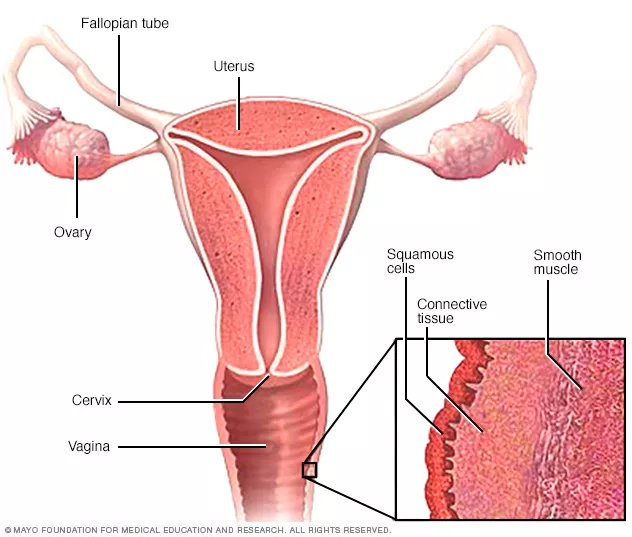
UTERUS (ऎट्रुस):
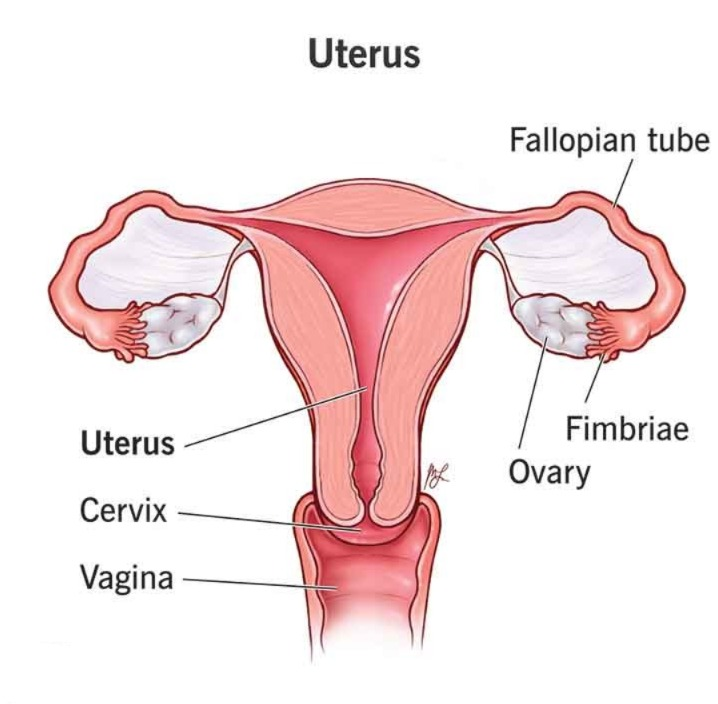
- The uterus is a hollow and muscular inverted pear-shaped organ. It is an organ located within the pelvic cavity. Which is located between the urinary bladder and the rectum.
- In most women, the uterus is bent forward (anteflexion) and forward (anteversion) and is at a right angle (90°- right angle) to the vagina.
- Its anterior wall is attached to the bladder and forms the vesicouterine pouch. The pouch of peritoneum that forms between the bladder and the uterus is called the vesicouterine pouch.
- When the body is in an upright position, the uterus The length is 3 inches, the width is 2 inches, and the thickness is 1 inch. Its weight is 30 to 40 grams.
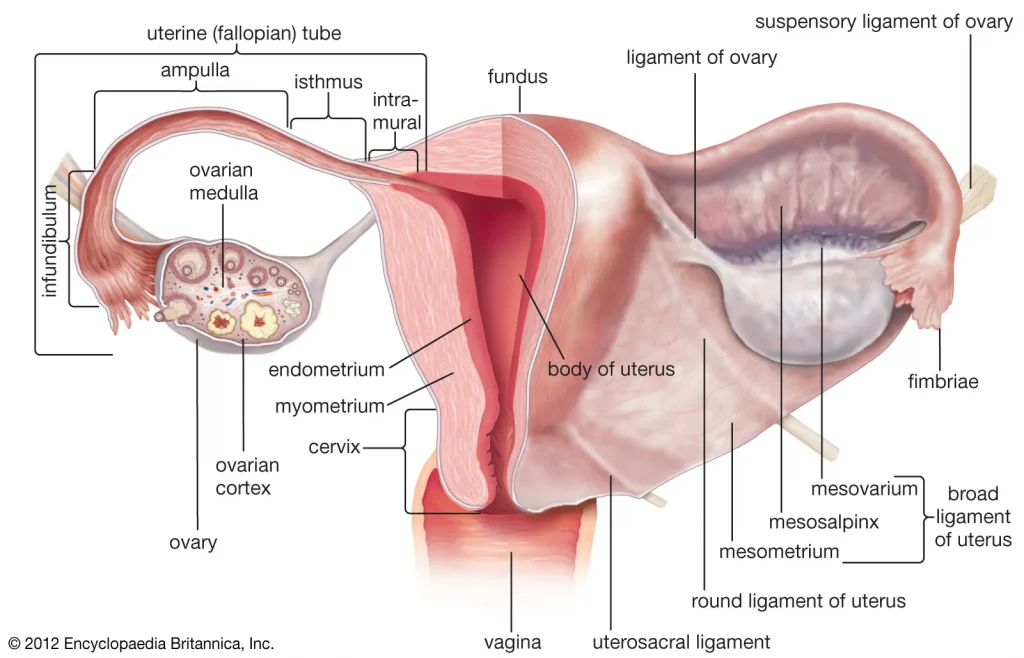
The parts of the uterus are as follows:
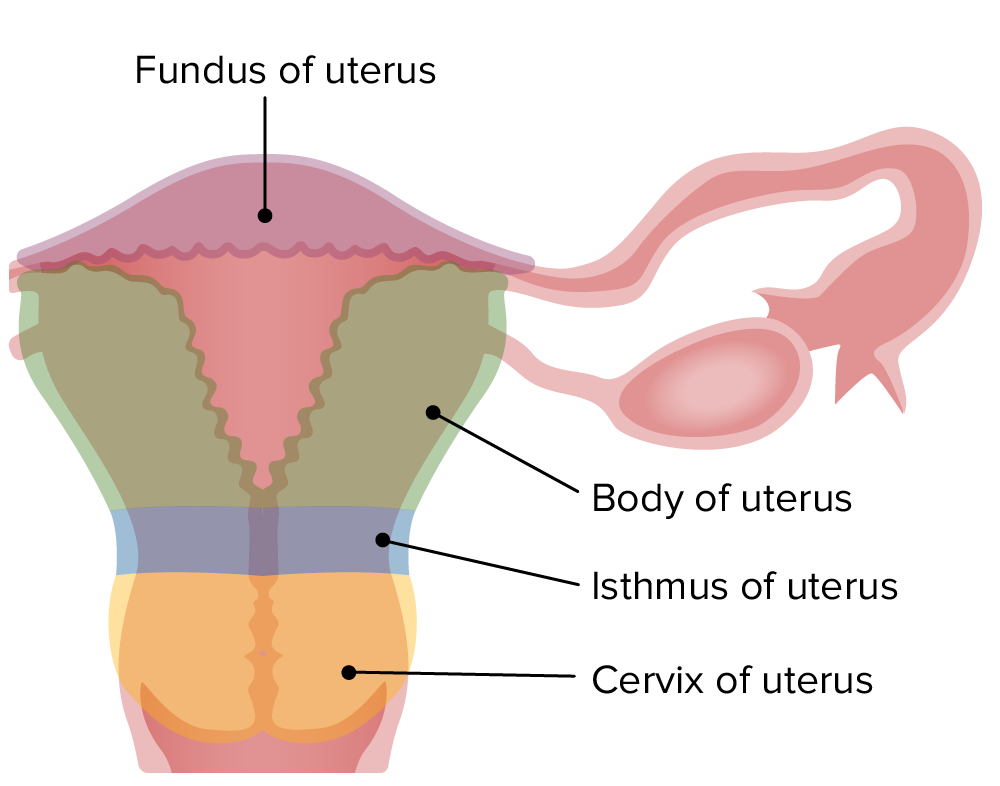
- Fundus:- It is dome-shaped. The fallopian tube opens from its upper part.
- Body:- The body is the main part. The uterus becomes narrower as it goes down. It forms the internal os (mouth). Which continues forward to form the cervix.
- Cervix:- It is called the neck of the uterus. It opens or protrudes into the anterior part of the vagina. Its opening is called external os.
STRUCTURE:
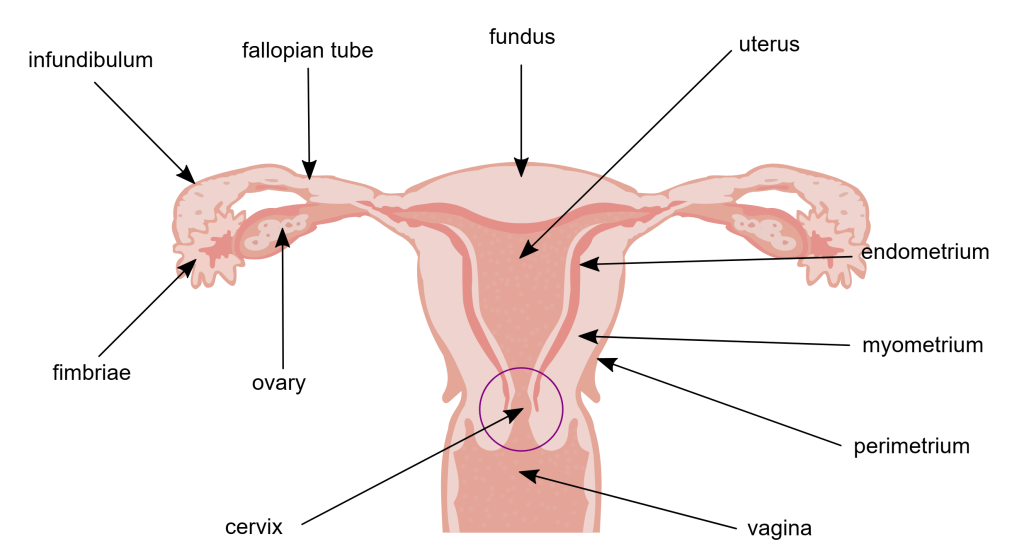
The uterus has 3 layers:
Perimetrium
Myometrium
Endometrium
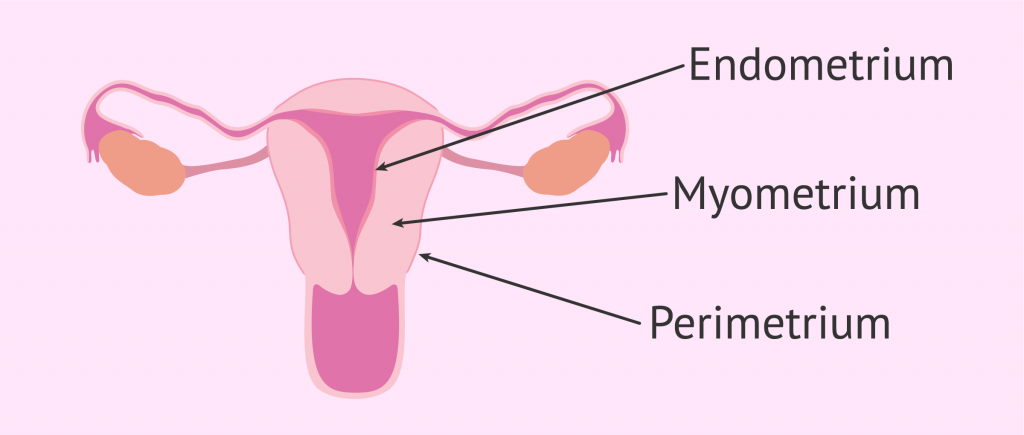
Perimetrium:
- This is a layer of peritoneum. It is spread around the uterus. There is a fold of peritoneum on the fundus and body on the front and the urinary bladder on the top.
- The pouch of peritoneum formed between the uterus and bladder on the front is called the vesico-uterine pouch while on the back the peritoneum extends from the fundus to the cervix. The pouch formed between the rectum and uterus on the back is called the pouch of Douglas or rectouterine pouch.
- Laterally (on the side) it is double folded. The layer of peritoneum forms the broad ligament and the round ligament on the side, which join the uterus to the pelvis.
MYOMETRIUM (myometrium):
- This is the thickest layer of the uterus. It contains a mass of smooth muscle and is accompanied by areolar tissue, blood vessels and nerves.
ENDOMETRIUM (Endometrium):
It is made up of columnar epithelium tissue and is lined by tubular cell glands that secrete mucus.
It has two layers in total.
- Functional layer (functional layer)
- Basal layer
1.Functional layer
- It is the upper layer. It is rich in blood vessels for the first 15 days or half of the cycle and if the ovum (egg) is not fertilized then this layer is shed (shed) and menstruation begins.
- If fertilized then it remains for 9 months (pregnancy) and then sheds and during 9 months it is called decidua.
2.Basal layer
This is the layer that lies in front of the myometrium. It is not shed during the menstrual cycle. This is the layer from which the new and fresh layer is formed.
The 2/3rd layer of the endometrium is made up of mucus membrane and the lower part is made up of stratified squamous epithelium up to the vagina.
BLOOD SUPPLY:
Arterial supply: – Blood reaches the uterus through the uterine artery and is a branch of the internal iliac artery.
Venous drainage: – Veins are similar to arteries but blood drains into the iliac vein.
Nerve Supply:
Parasympathetic nerve supply comes from the sacrum and sympathetic nerve supply comes from the lumbar region.
Supporting Structure:
The uterus is supported by surrounding organs. Which are in the pelvic cavity and there are ligaments. Which support the uterus. Like :-
- broad ligaments
- round ligaments
- Uterosacral ligaments
- Transverse cervical ligaments
- Pubocervical fascia
The above structures help the uterus maintain its shape and provide structural support.
FUNCTIONS OF UTERUS:
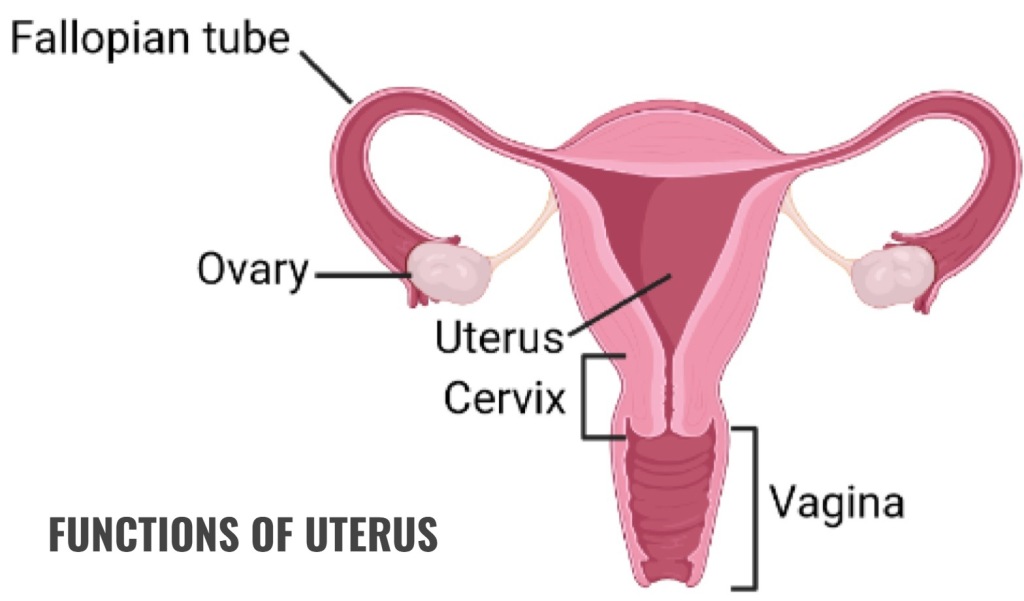
- The uterus helps in the fertilization of the ovum and sperm.
- After fertilization, it helps the zygote to implant in the inner wall of the uterus and maintains the pregnancy.
- During pregnancy, as the content inside the uterus increases, the size of the uterus also increases so that the pregnancy can continue.
- The uterus during pregnancy It functions to provide nutrition to the fetus in the mother.
- It helps the baby to come out during delivery by causing the muscles of the uterus to contract.
- The endometrium, the inner wall of the uterus, breaks down during the menstrual cycle. This cycle continues every 26 to 30 days, and the chance of infection is reduced due to the influx of wbc.
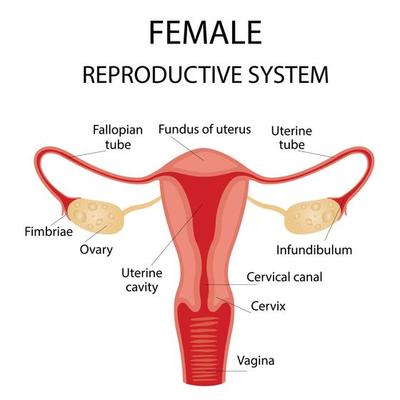
FALLOPIAN TUBE/ SALPHINGES / MULERIAN DUCT / UTERINE TUBE (Fallopian Tube, Salphinges, Mullerian Duct, Uterine Tube):
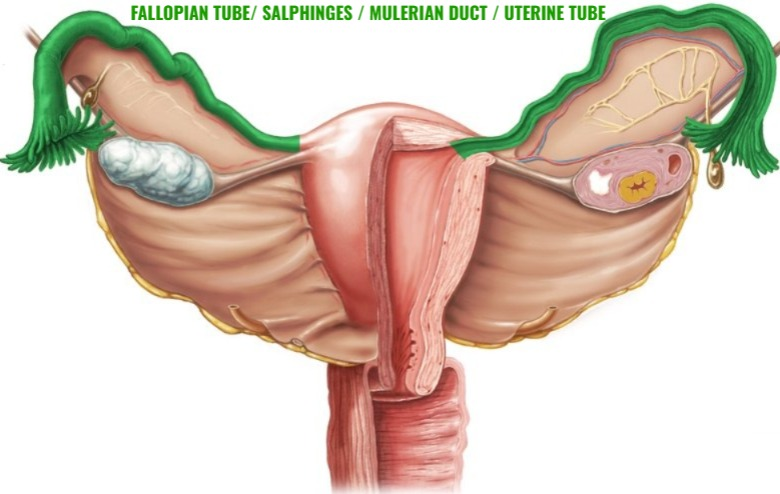
They are 2 in number. They are attached to the fundus and body and there is one on both sides of the fundus. They are 10cm long.
Its main parts are as follows.
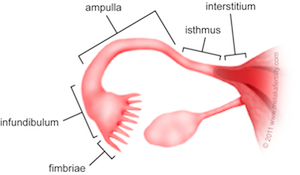
- Interstitial:- This part is attached to the uterus. It is the part of the uterus that begins after the fundus.
- Isthmus:- This is narrow and is approximately 2.5 cm long.
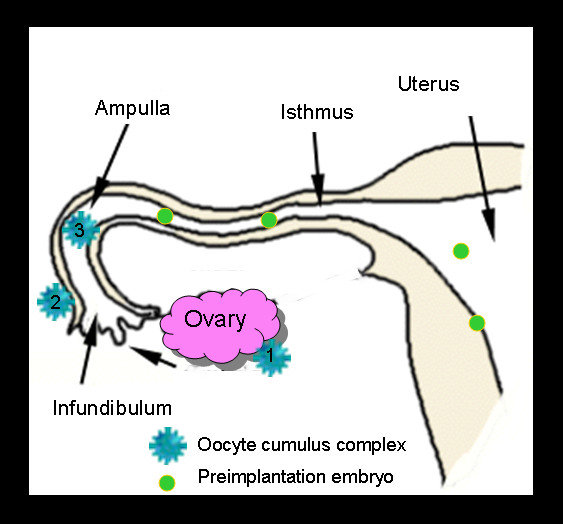
- Ampulla:- The ampulla is the widest part of the tube. Here the ovum and sperm are fertilized.
- Infundibulum:- This is the last part of the fallopian tube and is shaped like a funnel.
At the end of this, finger-like projections are formed. These are called fimbriae. The fimbriae receive the egg cells. It has three layers
- Outer Layer (Outer Layer) which is made of peritoneum.
- Middle Layer (Middle Layer) which is made of muscles.
- Inner Layer (Inner Layer) which is made of mucus membrane and ciliated epithelium tissue.
Functions of FALLOPIAN TUBE:
- It causes the egg (ovum) to undergo peristalsis and reach the ampulla.
- The mucus secreted by it provides an ideal environment for the ova and sperm.
- The egg and sperm fertilize here and form a zygote.
- The fertilized zygote travels to the uterus.
Ovaries:
- The ovary is a female gonad. It is located on either side of the uterus in the ovarian fossa. It is located behind the broad ligament.
- It is 2 in number (pair of ovaries). It is homologous to the testis.
- It is attached to the pelvic wall by ovarian wall ligaments.
Location:
It is a structure surrounding the ovarian fossa (a fossa is a pit-like structure that contains an organ) in which it is located behind the ureters (back of the urinary tract), the obliterated umbilical The artery (which is an artery that disappears shortly after birth) is supported by
obturated intercostal muscles, vessels, and nerves in front and below.
Shape and Size:
The ovary is oval in shape. It is 3 cm long, 1.5 cm wide and 1 cm thick.
Surface And colour :
In young adults, the ovary is pink in color and smooth. In older women, it is rough, irregular, and gray in color because they have ovulated frequently.
Attachment:
Both ovaries are attached to the uterus at the top by the ovarian ligament and at the back by the broad ligament. It is called the mesovarium, blood vessels and nerves pass through the mesovarium.
Blood Supply:
It is supplied by the ovarian artery and is a branch of the abdominal aorta.
The vein is called the pampiniform plexus. It emerges from the ovary itself.
The right vein drains into the inferior vena cava and the left vein drains into the left renal vein.
Nerve Supply:
Sympathetic fibers that emerge from the T10 and T11 spinal ligaments.
Parasympathetic nerves emerge from the vagus nerve.
Histology Of Ovary (Histology (study of tissue is called histology) of ovary):
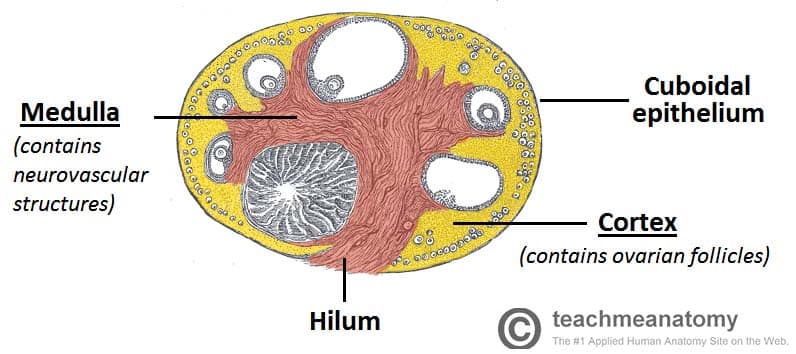
- The ovary is oval in shape.
It is lined with a single layer of cuboidal epithelium cells. It is called the germinal epithelium. - It contains dense tissue. It is called the tunica albinia and is located inside the germinal epithelium.
It has a total of 2 parts.
- Cortex:- It is made up of the stoma and follicles of the ovary.
- Medula:- It is made up of connective tissue and is connected by a network of blood vessels and is made up of elastic fibers.
Oogenesis:
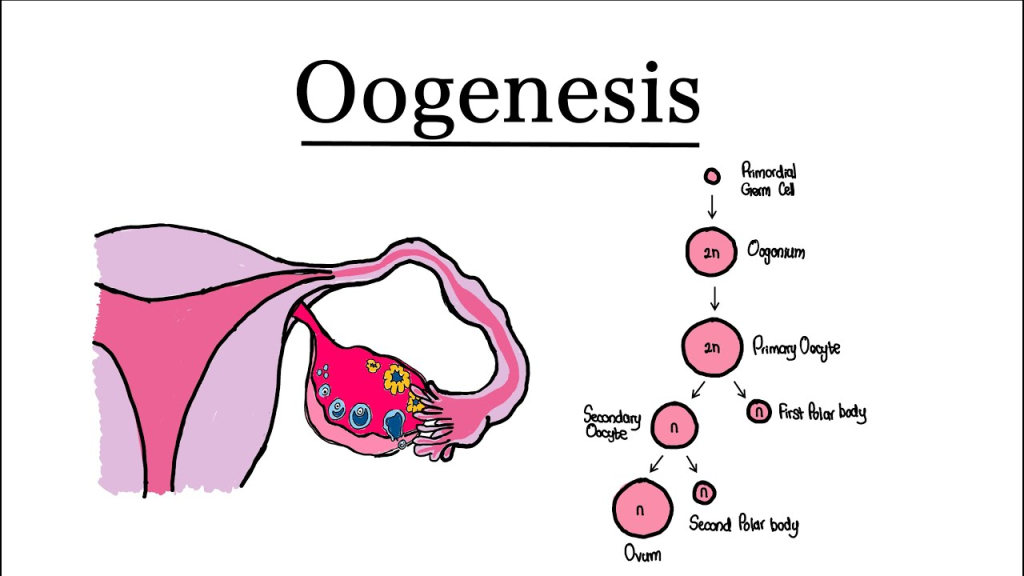
- This is a process of producing female gametes. The process of ova from primary germ cells is called oogenesis.
- By the 6th month of the intrauterine period, about 6 million oogonia are present. The oogonia undergo meiotic division and convert into primary oocytes and are arrested in prophase.
- The 1st meiotic division is arrested at puberty. When puberty begins, menstruation begins. The first menstrual cycle is called menarche.
- When the first menstrual cycle begins, ovulation occurs and the egg is released and ovulation occurs, the first egg is released.
- When ovulation occurs, follicles are formed before it. It happens with the help of FSH and then it is seen due to estrogen. Those follicles mature and become Graafian follicles.
- A mature ovum is formed from this Graafian follicle. The ovum is released on the 14th day of the menstrual cycle and if it is fertilized, it becomes a fetus and if it is not fertilized, menstruation occurs.
Menstruation Cycle:
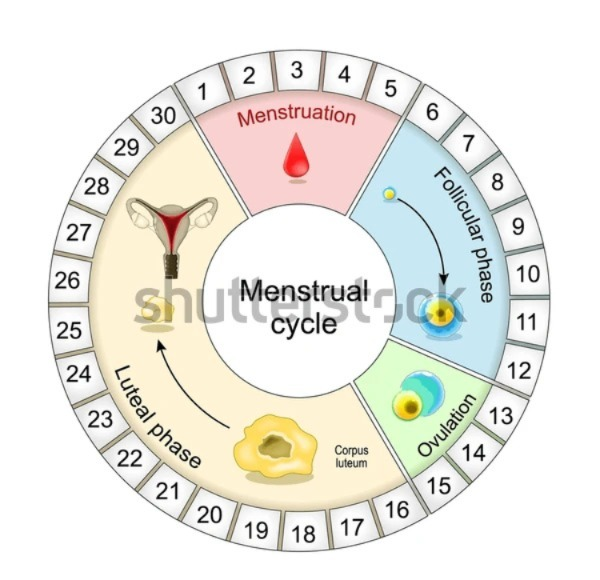
- The menstrual cycle occurs in females after puberty. In which changes are seen in the function of the ovaries and uterus.
- The menstrual cycle occurs every 26 to 30 days. This is due to changes in the blood hormone levels.
- The onset of the menstrual cycle is known as menarche.
- This cycle is seen continuously in females after puberty. Which temporarily stops during pregnancy and completely stops after the menopause period.
- The onset of menstruation is seen due to the degeneration of the corpus luteum layer in the uterus and bleeding comes out through the vaginal cavity.
- The following phases are seen in the menstrual cycle.
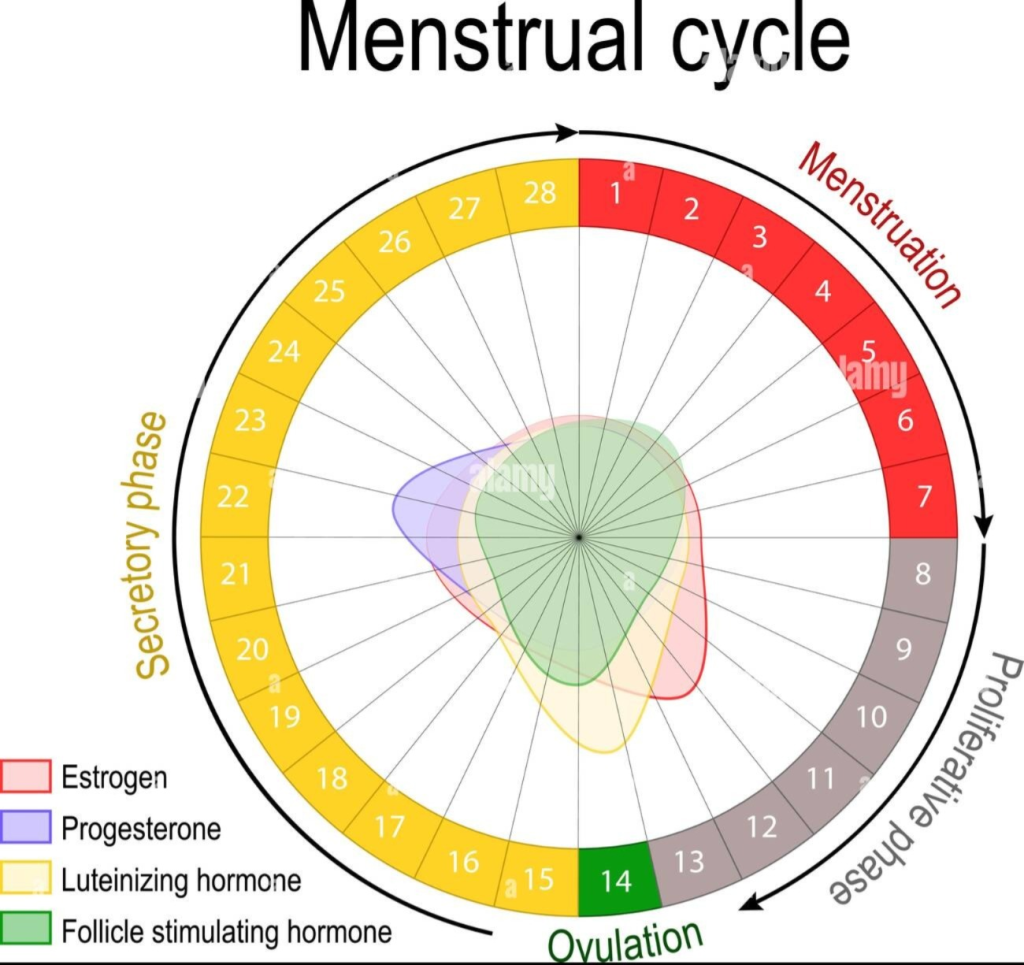
1. Menstrual Phase (Menstrual Phase):
- This phase occurs every 28 days and lasts for about four days. When the female releases an egg, the When fertilization does not occur, the levels of estrogen and progesterone, the hormones that support the wall of the uterus, decrease and the level of oxytocin hormone increases. Due to this, the stimulation of uterine contractions increases and the degeneration of the corpus luteum layer of the uterine wall begins and blood drains from the uterus through the vagina. This phase lasts for 1 to 4 days.
- This menstrual flow contains endometrial glands, endometrial cells, blood and parts of the unfertilized ovum. Approximately 100 to 200 ml of blood is released during this phase. It comes out during 3 to 5 days, which is called the menstrual phase.
2. Proliferative Phase:
- The menstrual phase ends on the 5th day. Then, the proliferative phase begins from day 6 and lasts for 14 days.
- In this phase, follicle stimulating hormone stimulates the ovarian follicles and thus increases estrogen production. This estrogen stimulates the proliferation of the endometrium.
- The endometrium of the uterus begins to develop from the sixth day. Its cells multiply and due to which mucus secreting glands and blood capillaries increase. Thus, the endometrium of the uterus becomes bulky and vascular.
- At the end of this phase, the inner wall of the uterus is ready for the implantation of the fertilized egg. This phase ends with ovulation. At the end of this phase, there is a decrease in estrogen levels.
3. Secretory Phase:
- After the proliferation phase is complete, the secretory phase begins. The secretory phase starts from the 15th day of the menstrual cycle and lasts until the 28th day.
- Since the progesterone hormone is important in this phase, this phase is also called the progesterone phase.
- When a mature egg is released by the ovary due to ovulation, the amount of estrogen and progesterone hormones decreases, but the corpus luteum, the wall of the uterus, secretes progesterone and maintains pregnancy.
- Since this mature egg is not fertilized by the sperm, the corpus luteum It decreases progesterone and due to the decrease in progesterone hormone, the amount of oxytocin hormone increases and contractions begin in the muscles of the uterus.
- The next cycle begins at the end of this phase due to the corpus luteum not receiving the ovum and increased uterine contractions.
Reproduction and Menopause:
Reproduction:
Reproduction is the natural biological process of creating new generations in living organisms.
Reproductive System in Female:
The main organs of the Reproductive System in Female are as follows:
1.Ovaries:Produce eggs and hormones such as estrogen and progesterone.
2.Fallopian tubes:Carry eggs to the uterus. is.
3.Uterus: Here implantation occurs and the fetus develops.
4.Vagina: The external vagina is where the male’s sperm enters.
Reproductive Process:
- Every month, an egg is released from the ovaries – this is called ovulation.
- If that egg fertilizes with sperm, a zygote is formed.
- The zygote then implants in the uterus.
- This is where pregnancy begins.
- If fertilization does not occur, menstruation occurs. Is – The lining of the uterus is shed in the form of bleeding.
Hormonal Regulation:
Estrogen and Progesterone are the hormones responsible for the female menstrual cycle and pregnancy.
FSH (Follicle Stimulating Hormone) and LH (Luteinizing Hormone) are released from the pituitary gland and help in the growth and release of eggs.
Menopause: The final stage of the menstrual cycle
Menopause is the stage where The female’s menstrual cycle stops permanently and her reproductive ability ends.
Stages before Menopause:
Perimenopause: The years before menopause where hormonal changes begin.
Menopause: 12 The point in time when the menstrual cycle stops for months.
Postmenopause: The years after menopause where hormone levels remain stable but at low levels.
Common symptoms of menopause:
Hot flashes: A feeling of increased temperature in the palms, face, and chest.
Night sweats: Excessive sweating at night.
Mood swings: Sudden changes in mood.
Sleep disturbances: Sleep disturbances.
Vaginal dryness: Vaginal dryness.
Loss of libido: Loss of sexual desire. Decrease.
Osteoporosis: Decrease in bone density, increasing the risk of fractures.
Hormonal changes during menopause:
Estrogen levels drop significantly.
This increases the risk of problems like cardiovascular diseases and osteoporosis. is.
Structure and Function of the Breast:
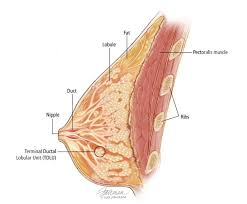
The physical structure and function of the breast are directly related to the physical development and motherhood of a female. The breast is mainly composed of mammary glands, which are responsible for milk production. Its structure and function are of particular importance in the nursing and medical fields.
Structure of the Breast:
The breast is a milk-producing organ located in the upper part of the female chest. The components inside the breast are as follows:
1.Mammary glands:
The main milk-producing glands.
These glands are divided into several lobes.
Each lobe has smaller lobules that contain alveoli.
2.Alveoli:
These are small round cells where milk is produced.
A hormone called prolactin is responsible for milk production.
3.Lactiferous ducts:
Milk from the alveoli travels through ducts.
These ducts travel in a single path to the nipple.
4.Lactiferous sinuses:
The enlarged part at the end of the ducts is where the milk stops first.
The milk is stored here for a short time before moving to the nipple.
5.Nipple:
The external part of the breast from which milk comes out.
The colored portion around each nipple is called the areola.
6.Areola:
It contains small glands called Montgomery’s glands, which keep the nipple moisturized.
7.Adipose tissue:
The fatty tissue surrounding the breast that cushions and supports it.
Function of the Breast:
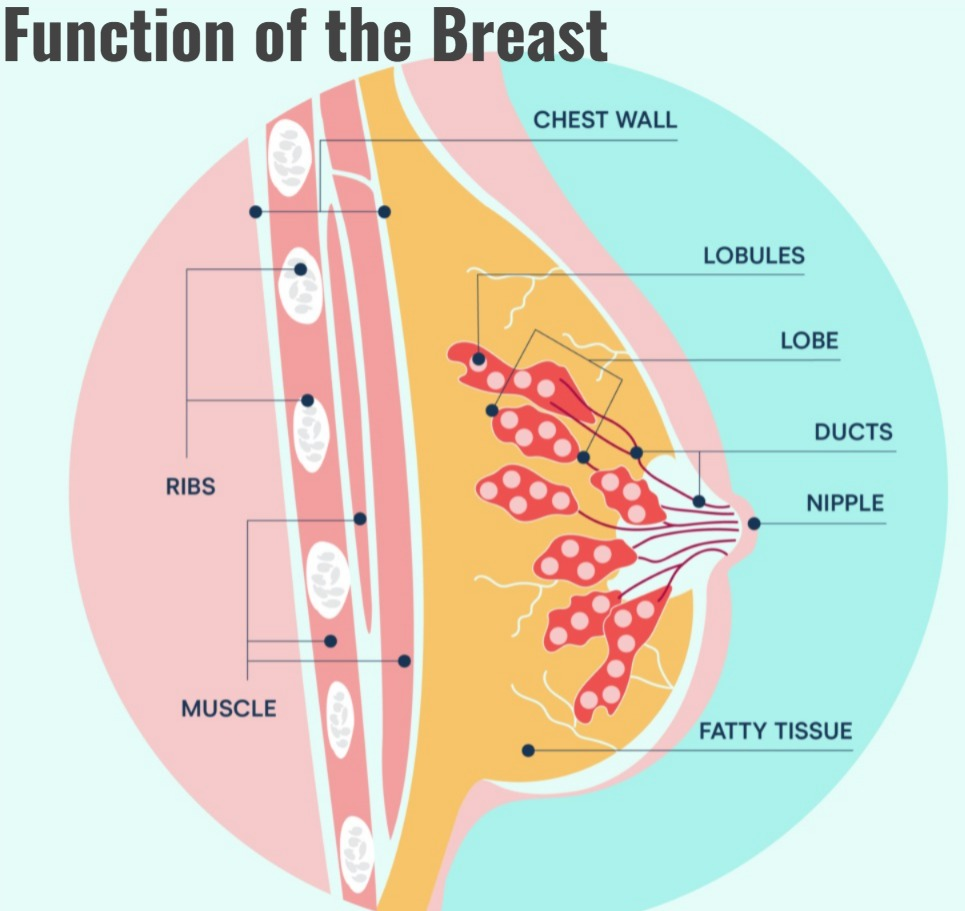
The main function of the breast is – lactation, i.e. the function of feeding milk to the baby. Its function is mainly under hormonal control.
Main functions:
1.Milk Production:
After the birth of the baby, the alveoli produce milk due to the prolactin hormone.
2.Milk Ejection:
When a baby drinks milk, the hormone oxytocin causes milk to come out – which is called the let-down reflex.
3.Nourishment to the Baby:
Milk contains antibodies, proteins, fats and lactose which are essential for the development of the baby.
4.Immunological Protection:
Breast milk contains antibodies like IgA which protect the baby from infection transmission.
5.Bonding between Mother and Child:
During breastfeeding, the hormone oxytocin creates an emotional bond between the mother and the baby.
Hormonal Control:
Hormonal Functions:
- Prolactin helps in the production of milk.
- Oxytocin helps in the ejection of milk.
- Estrogen Plays a role in breast development.
- Progesterone helps in the development of the gland.
Breast is an important organ of the female body, which is directly related to physical, hormonal and mental development. Its main function is milk production and nourishment.