ENGLISH-COMMUNITY HEALTH NURSING – 2 (GNM THIRD YEAR) PAPER SOLUTION : 08/07/2025 (DONE)-PAPER SOLUTION NO.11
PAPER SOLUTION NO.11 – 08/07/2025

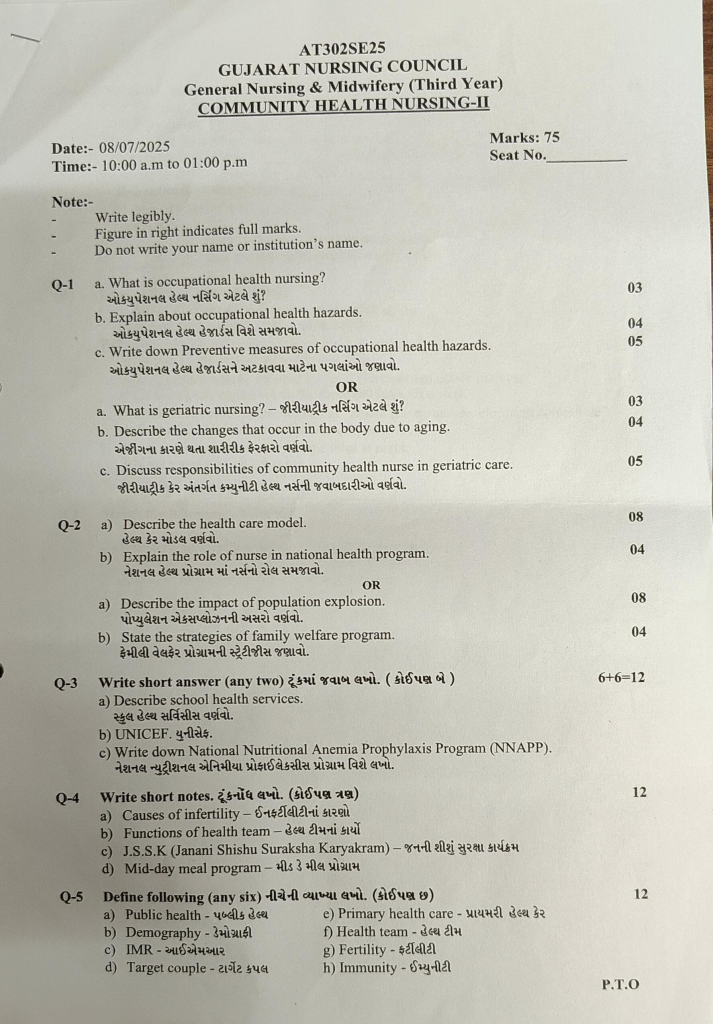
Q-1 a. What is occupational health nursing? What is Occupational Health Nursing? 03
Definition:
Occupational Health Nursing is a specialized branch of nursing that is responsible for maintaining and improving the physical, mental, and social health of workers in the workplace. An Occupational Health Nurse is a licensed Registered Nurse (RN) who has specialized training in the prevention, treatment, and rehabilitation of health hazards, occupational diseases, and injuries.
Aim:
To ensure a safe, healthy, and productive work environment for workers.
Main Functions:
- Health Assessment
- First Aid
- Disease Prevention
- Health Education
- Policy Development
- Return-to-Work Management
- Safety construction as per OSHA (Occupational Safety and Health Administration).
b. Explain about occupational health hazards. Explain about occupational health hazards.04
Occupational Hazards:
Occupational hazards involve a wide range of risks that workers may experience depending on their specific job role and environment.
Occupational hazards are potential risks or dangers that health care workers are exposed to in their workplace environment.
These hazards arise from various aspects of the workplace, such as,
physical conditions,
chemical materials,
biological agents,
psychological factors, and
mechanical hazards, etc. These factors pose a risk to the health, safety, and well-being of workers and can lead to injuries, illnesses, or even death if proper precautions and safety measures are not taken.
Occupational hazards that workers may be exposed to include:
- 1) Physical hazards,
- 2) Chemical hazards,
- 3) Biological hazards,
- 4) Mechanical hazards,
- 5) Psychological hazards.
1) Physical hazards:
- Physical hazards are caused by exposure to heat and cold. Workers are exposed to direct exposure to high temperatures of the sun such as farmers, builders, laborers etc.
- There are also high temperatures inside the valley such as the Kotar Gold Valley in Mysore, some industries will have local ‘hot spots’ such as ovens and furnaces that radiate heat such as bakeries, metal works, asbestos factory engine rooms etc.
- The effects of high temperatures include extreme heat, heat allergies, heat exhaustion, and muscle cramps.
- Many workers are exposed to low temperatures such as in ice factories, high altitudes, cold storage, cold laboratories, etc. These workers may develop chills (pain, itching, and swelling in the hands and feet due to poor blood supply due to excessive exposure to cold), erythrocyanosis, and respiratory difficulties.
- High Humidity:
- In industries such as textile, paper, and ice factories, high humidity increases the effects of heat and cold along with exposure to extreme temperatures.
- Noise:
- Loud noise is produced in steel, oil, textile, and automobile factories. Loud noise is harmful to health. Its effects depend on the intensity and duration of exposure to loud noise. Loud noise can cause fatigue, nervousness, irritation and partial or complete hearing loss.
- Light:
- Workers may come into contact with poor or glaring and bright light. Poor light causes strain and pain in the eyes, eye strain, headaches. Blurring and bright light causes discomfort, blurring of vision, irritation and visual fatigue.
- Vibration:
- Vibration occurs while working on machines like grinding, cutting, drilling boring machines etc. Vibration can cause fatigue, nervousness and local effects such as hand and joint injuries etc.
- Radiations:
- Exposing yourself to radiation from X-rays and radioactive isotopes can cause skin and blood cancer, which can result in genetic changes, malformations, sterility etc. People working in radiology departments, watch factories, ammunition factories come into contact with ionizing radiation. Ultraviolet (UV) radiations such as during welding cause conjunctivitis and keratitis. Ultraviolet radiation can cause sunburn. Roadbuilders, sailors, shepherds and farmers can be affected by ultraviolet radiation.
2) Chemical Hazards: Factories use some or the other chemicals. Chemicals work in 3 ways.
- 1) Local Action: Some chemicals can cause conditions like dermatitis and eczema.
- 2) Inhalation: Inhalation of gases and vapors can cause respiratory diseases.
- 3) Ingestion
- Mercury, lead, arsenic, zinc, chromium and cadmium, phosphorus etc. cause various diseases.
- Types of which are hazardous
- Gas like carbon monoxide, ozone, carbon dioxide, hydrogen and cyanide etc.
- Fumes and vapors from various types of acids, vapors of mercurial etc.
- Mists Mist from the electroplating industry.
- Dust: Small particles formed by crushing and grinding rocks, ores, metals, wood, etc.
- Chemical agents that are harmful to the skin, respiratory system, and gastrointestinal system.
- Skin problems include dermatitis, eczema, urticaria, ulcers, and cancer.
- Respiratory problems include various types of pneumoconiosis. Silicosis due to quartz dust,
Anthracosis due to coal dust,
Byssinosis due to cotton dust,
Asbestosis due to asbestos dust,
Respiratory distress due to carbon monoxide, hydrogen sulfide and hydrogen
Cyanide Chlorine, ozone, nitrogen oxide, sulfur dioxide can cause throat irritation. Lung cancer can be caused by asbestos, beryllium, coal tar, mineral oil.
3) Biological Hazards:
- Biological hazards are caused by infectious and parasitic agents such as viruses, rickettsia, bacteria. This can also lead to hookworm infestation in farmers. Leptospirosis can occur in workers working in mines.
- Tanning factories, veterinary hospitals and dispensaries, zoos, circuses, agricultural workers, butcher shops, etc. can cause various zoonotic diseases such as brucellosis, mycotic infections, parasitic infections and anthrax.
- Health workers working in hospitals/dispensaries may come into contact with patients infected with diseases such as tuberculosis, hepatitis, HIV and serum hepatitis etc.
4) Mechanical Hazards:
- Unprotected machines and their protruding and moving parts and machines with low safety can cause various accidents and injuries, which can lead to partial and permanent disability.
5) Psychological Hazards:
- Different types of work adjustment problems such as lack of proper job satisfaction,
- Insecurity, frustration and environmental tension prevent a person from adjusting properly. Due to these conditions, physical health problems such as increased blood pressure, indigestion, insomnia,
- loss of appetite and conditions like heartburn can occur.
- Thus, it is important to take measures to prevent such hazards from occurring in workers by early and proper identification.
c. Write down Preventive measures of occupational health hazards. 05
- Steps to Prevent Occupational Hazards: Here is a structured approach to prevent occupational health risks:
- 1) Identify hazards: Conduct regular workplace inspections and risk assessments to identify potential hazards such as chemical exposure, ergonomic stressors, noise levels and psychosocial factors such as workplace stress or bullying.
- 2) Assess Risk: Evaluate the likelihood and severity of harm caused by identified risks. Prioritize risks based on their potential impact on worker health and safety.
- 3) Implement Controls:
- Engineering Controls: Modify the workplace or equipment to eliminate or reduce hazards at source.
- For example, installing ventilation systems to control airborne contaminants or redesigning workstations to improve ergonomics.
- Administrative Controls: Establish procedures and policies that reduce exposure to hazards. This includes rotating tasks to reduce repetitive strain, reducing hazards, providing scheduled breaks to reduce fatigue, and providing training on safe work practices.
- Personal Protective Equipment (PPE):
- Provide appropriate PPE such as gloves, helmets, respirators, and ear protection.
- Ensure that PPE is properly selected, fitted, and used in accordance with manufacturer’s instructions and training.
- 4) Providing Training and Information: Provide education to workers about potential workplace hazards, safe work practices, emergency procedures, and the proper use of PPE.
- Training should be comprehensive, ongoing, and accessible to all employers, including new hires and contractors.
- 5) Monitor and Review: Regularly monitor workplace conditions and health surveillance data to evaluate the effectiveness of control measures.
- Periodically review risk assessments and update procedures as necessary to address new hazards or changes in work processes.
- 6) Encourage Reporting and Participation: Establish a culture where workers feel empowered to report hazards, oversights, and health concerns without fear of retaliation.
Encourage active participation in safety committees, programs to identify hazards, and safety improvement initiatives. - 7) Promote Health and Wellbeing:
- Support worker health and well-being through initiatives such as wellness programs, ergonomic assessments, mental health support, and access to healthcare services.
- Assess factors outside of work that may affect worker health, such as stress management programs.
- 8) Compliance and Continuous Improvement:
- Adhering to occupational health and safety regulations, standards and industry best practices, regularly reviewing policies and procedures to collect new knowledge, technological advancements and lessons learned from incidents or near misses.
- By systematically following these steps, organizations can effectively prevent occupational health hazards, protect the health and safety of workers and create a culture of safety in the workplace.
OR
a. What is geriatric nursing?- What is geriatric nursing? 03
- Geriatric Nursing is a special branch of nursing that provides health care for the physical, mental, social and emotional health needs of elderly persons. The main objective is to maintain the age-related diseases, chronic illnesses, and the dynamics of daily life and quality of life seen in elderly persons. Geriatric nursing is a branch of nursing that provides nursing care in a professional and kind manner to maintain the health of elderly persons and improve their functional ability and quality of life.
b. Describe the changes that occur in the body due to aging. Describe the physical changes caused by aging.04
- The human body gradually experiences changes at the physical, biological and metabolic levels in various systems as it ages. These changes affect the functional ability and sensitivity of the body.
- (Integumentary System Changes):
- Skin thinning: The amount of collagen and elastin decreases, causing the skin to lose elasticity.
- Dry Skin: The sebaceous glands reduce their production of oil.
- Wrinkles: Caused by exposure to UV radiation and slow cellular regeneration.
- (Musculoskeletal System Changes):
- Sarcopenia: Decreased muscle thickness and energy.
- Osteoporosis: Decreased calcium in the bones makes the bones fragile.
- Joint Stiffness: Arthritis occurs due to wear and tear of cartilage.
3.(Cardiovascular System):
- Atherosclerosis: Plaque buildup in blood vessels causes the vessels to constrict.
- Reduced Cardiac Output: The heart’s pumping ability decreases.
- The heart’s vessels become hard.
4.(Respiratory System):
- Reduced Pulmonary Function: The elasticity of the alveoli decreases.
- Respiratory Muscle Weakness: Oxygen levels decrease.
5.(Digestive System):
- Reduced Gastric Acid Production: Digestion slows down.
- Constipation: Intestinal movement (peristalsis) decreases.
6.Urinary System:
- Reduced Renal Function: Glomerular filtration rate (GFR) decreases.
- Bladder Capacity Reduction: Frequent urination.
- Nervous System:
- Neuronal Loss: Neurons in the brain are lost, which affects memory.
- Slowed Reflexes: The ability to respond quickly is reduced.
- Hormonal Changes:
- Menopause & Andropause: Estrogen in females and testosterone in males decrease.
- Slowed Metabolism: The conversion of nutrients into energy slows down.
9.(Vision and Hearing):
- Presbyopia: The elasticity of the lens of the eye decreases.
- Presbycusis: Hearing loss due to age, especially at high frequencies.
10.(Immune System):
- Immunosenescence: The number and functional ability of immune cells decreases, which increases the risk of infection.
- Aging is a natural process that gradually affects every system of the body. However, these changes can be slowed and controlled by adopting a proper diet, regular exercise, adequate sleep and a stress-free lifestyle.
c. Discuss responsibilities of community health nurse in geriatric care. Discuss the responsibilities of community health nurse in geriatric care.05
Responsibilities of Community Health Nurse in Geriatric Care:
Geriatric Care is a service for patients who are geriatric persons — people of advanced age, especially those with chronic diseases, mental health, and social support needs. The part of geriatric care is very important for a Community Health Nurse, and it includes the following responsibilities:
- Conducting Health Assessment:
A Community Health Nurse conducts a complete physical, mental and functional health assessment to determine the health status of a geriatric person.
This includes evaluation of vital signs, ADLs (Activities of Daily Living) and IADLs (Instrumental Activities of Daily Living).
- Chronic Disease Management:
Geriatric persons usually have long-term diseases like Diabetes Mellitus, Hypertension, Arthritis, etc. The nurse is responsible for their regular monitoring, medication adherence and lifestyle management.
- Medication Management:
Geriatric persons often engage in polypharmacy – i.e. taking multiple medications at the same time. The nurse monitors the correct dosage, timing and drug interactions of medications and ensures their proper use.
- Fall Prevention and Safety Evaluation:
Geriatric persons are at increased risk of falls. The nurse evaluates safety hazards in the home and surrounding environment and provides education to reduce them.
- Pain Management:
Nurses measure pain levels using pain assessment tools and suggest appropriate interventions – such as pharmacological and non-pharmacological methods.
- Cognitive and Mental Health Support:
Mental health issues such as dementia, depression, and Alzheimer’s disease are common in geriatric persons. Community health nurses try to improve their mental health through regular observation and monitoring.
- Health Education and Counseling:
Geriatric persons and their caregivers are provided with information and education about healthy lifestyles, nutrition, medication regimens, and disease prevention.
- Social Support and Referral Services:
When geriatric persons need additional help or special facilities, nurses refer them to home health agencies, old age homes, or medical specialists.
- End-of-Life Care:
When a geriatric person is living with a terminal illness, community health nurses provide support for palliative care and hospice services.
- Family and Caregiver Support:
Nurses provide training and necessary help to family members and caregivers for memory care, handling aggression, and respite care.
Thus, community health nurses play an important role in the overall development of physical, mental, and social health for geriatric persons. Their service proves to be a milestone in improving the quality of life of geriatric persons.
Q-2
a) Describe the health care model. Describe the health care model.08
A health care model is a scientific and systematic standard that serves as a guideline for how health care is delivered. This model helps in providing health services at various levels – such as disease prevention, diagnosis, treatment, rehabilitation, and maintaining quality of life. Choosing the right health care model is especially important for geriatric persons, as they have special needs for physical, mental, and social support.
Below is a detailed description of the various health care models:
- Biomedical Model:
The biomedical model defines health only as body-related disease or illness. The main goal of this model is to find the causes of illness and to carry out its scientific diagnosis and treatment. This model focuses on the physiological elements of the geriatric person, and ignores the psychological or social aspects.
- Biopsychosocial Model:
The biopsychosocial model takes a holistic view, taking into account three main elements:
- Biological
- Psychological
- Social
According to this model, a person’s health is not only based on the state of their body, but also on their mental Condition, emotional state and social conditions are also important.
3. Holistic Model:
The holistic model considers a complete health approach.
According to this model, a person’s healthy life is not only about being disease-free, but also includes physical, mental, emotional, social and spiritual elements.
Nursing care, diet therapy, meditation, physiotherapy etc. are also part of this model.
4. Primary Health Care Model Model):
The primary health care model is the basic foundation of healthcare.
Its four main principles are:
- Equity
- Accessibility
- Participatory Approach
- Comprehensive Care
This model is especially useful for providing health care at the community level for individuals. Its aim is to make healthcare accessible to everyone.
5.Patient-Centered Care Model:
The patient-centered care model is a method of healthcare in which the needs, preferences and values of the individual are kept at the center. It includes the following elements:
- Informed Decision Making
- Empathic Communication
- Caregiver Support
- Personalized Care Plan
6. Continuity of Care Model:
Continuity of Care Model means that healthcare should be continuous and connected: especially for geriatric persons. In this model, healthcare services are provided through cooperation between different agencies and phases, such as:
- Hospital Care
- Home Care Services (Home Care Services)
- Follow-Up Visits
- Palliative Care
Each health care model has its own characteristics and uses. Choosing the right model for a person is very important to maintain their health and improve their quality of life. A combined approach can also be more effective at times, in which elements of the above-involved models are combined and applied as needed.
b) Explain the role of nurse in national health program. Explain the role of nurse in national health program.04
Role of Nurse in National Health Program:
Nurse is the basic base of the Health Care System. The role of nurses is very important in the successful implementation of various National Health Programs of the Government of India such as TB Control, Immunization, Maternal and Child Health Care, NCDs, Family Planning and Disease Surveillance.
They continuously provide public health services in health centers, sub-centers, ANM sub-centers, school health programs, camp-based services etc.
- Assistance in Primary Health Care:
- Nurses identify common diseases in local people at an early stage such as:
- Diarrhea
- Malaria
- Respiratory Infections
- Scabies
- Tuberculosis
- They provide primary treatment:
- Wound Management
- Oral Rehydration Therapy (ORT)
- Temperature and blood pressure checks
- Refer patients with severe conditions to the next center.
- Participation in Immunization Programs:
- Under Universal Immunization Program (UIP): Giving vaccines like BCG, OPV, Pentavalent, Measles, Rotavirus.
- Giving TT and Td vaccines to pregnant women.
- Nurse follows Cold Chain Management:
- Ice Line Refrigerator (ILR)
- Deep Freezer
- Checks Vaccine Vial Monitor (VVM).
- Maternal and Child Health Services:
- Services provided by nurses:
- Antenatal Care (ANC)
- Postnatal Care (PNC) – Guidance and services for Institutional Delivery.
- Distribution of Iron-Folic Acid Tablets, Calcium Tablets.
- Nutrition education for undernourished or underweight mothers.
- Measuring the weight of the baby, updating the development chart, doing Growth Monitoring.
- Family Planning Services and Counseling:
- The nurse uses and distributes various contraceptive methods:
- Condom
- Oral Contraceptive Pills (OCPs)
- Intrauterine Contraceptive Device (IUCD – Copper-T)
- Emergency Contraception
- Counseling and educating the couple on the right choice.
- Identifies and refers for sterilization camps.
- Disease Surveillance and Reporting:
- Nurses report on Notifiable Diseases such as:
- TB
- Malaria
- Dengue
- Cholera
- Diphtheria
- COVID-19.
- They collect data for IDSP (Integrated Disease Surveillance Program).
- Provide daily, weekly and monthly reports to the Health Department.
- Health Education and Awareness:
- Nurses in School Health Program, Village Panchayat Meeting, ANM/VHSNC Meeting etc.:
- Spread awareness on TB, HIV/AIDS, Malaria, Malnutrition, Drug Detoxification etc.
- Use IEC/BCC material (Information, Education and Communication / Behavior Change Communication).
- Participation in NHM and Non-Communicable Disease Programs:
- Nurses serve in pilot and Health and Wellness Centres under NHM (National Health Mission).
- For screening programmes:
- Blood Glucose Test
- Blood Pressure Check
- Pap Smear,
- Mammography Referral
- Form filling, data analysis, and patient follow-up in Cancer Registry (NCRP – National Cancer Registry Program).
- Data Management and Documentation:
- Nurses maintain folders for each patient:
- ANC/PNC Record
- Immunization Register
- OPD/IPD Forms
- Govt. Portals like HMIS (Health Management Information System), RCH Portal (Reproductive & Child Health Portal) are entered.
- In addition, they also learn to use new technologies like Mission Indradhanush and eVIN.
- A nurse is not just a treatment provider, but a health educator, who has rendered excellent services to reach crores of people in rural and urban areas with the health benefits of the government. The contribution of nurses is invaluable for the successful implementation of every National Health Program.
- Their work is a pillar for Health Equity, Disease Prevention, and long-term health policy.
OR
a) Describe the impact of population explosion. Describe the impact of population explosion.08
1.Burden on Healthcare Infrastructure:
Overpopulation puts excessive pressure on healthcare facilities. Overcrowding occurs in hospitals and clinics due to more patients. Long queues in outpatient departments, delayed diagnosis and inadequate treatment increase.
- Increase in Communicable and Vector-Borne Diseases:
Where the population is high, sanitation and hygiene are poor. As a result, patients are more likely to contract diseases like Tuberculosis, Dengue, Malaria and Cholera.
3.Nutritional Deficiencies and Malnutrition:
Population growth puts pressure on the Food Supply. As a result, there is a shortage of Essential Nutrients. Protein Energy Malnutrition and Micronutrient Deficiencies are seen especially in Children and Pregnant Patients.
4.Inadequate Maternal and Neonatal Care:
Due to more patients, there is less availability of Gynecological Services. As a result, Prenatal Care, Institutional Deliveries and Neonatal Intensive Care are affected.
5.Mental Health Disorders:
Social Stressors, Unemployment and Resource Scarcity that come with overpopulation increase the risk of Anxiety, Depression and Substance Use Disorders in patients.
6.Low Doctor-to-Patient Ratio:
As the number of patients increases, Doctor Availability decreases. India’s Doctor-Patient Ratio is much lower than the World Health Organization’s criteria. Due to which Personalized Care cannot be provided.
7.Environmental Health Hazards:
Population growth increases Pollution Levels. Due to Air Pollution, Chronic Obstructive Pulmonary Disease, Bronchial Asthma and Allergies increase in patients.
8.Increased Infant and Maternal Mortality:
Where health centers are overloaded, Essential Obstetric Services are not available in sufficient quantity. Due to which Maternal Mortality Rate and Infant Mortality Rate increase.
- Urban Slum Expansion and Poor Living Conditions:
Overpopulation in big cities promotes Slum Development. In such places, there is less effectiveness in Clean Water, Sewage Management and Disease Control.
- Strain on Public Health Budget:
The increasing population puts pressure on the Budget Allocation on the government’s health programs. This means that Preventive Healthcare, Immunization and Rehabilitation Services for patients also decrease.
All the effects of overpopulation have negative effects on individual, social and national health levels. In such a situation, there is a need to make strong efforts towards Health Policy Reform, Efficient Resource Management and Population Stabilization Strategies. Only then can our country achieve a Sustainable Health System.
b) State the strategies of family welfare program. State the strategies of family welfare program.04
Family Welfare:
India is the first country in the world that has implemented the Family Welfare Program on a national basis through the government. Family Welfare is also known as the Family Planning Program. This family planning program was included as an official program since 1952.
Definition:
Family planning means planning a family size that is affordable by the parents and is for the health and welfare of the family. Family planning is a method that helps an individual or couple achieve the following objectives:
1) Avoiding unwanted births.
2) Achieving wanted births.
3) Spacing pregnancies.
4) Using appropriate methods of contraception.
Objectives of Family Welfare Program:
The National Family Welfare Program in India is a comprehensive initiative aimed at improving the health and well-being of the family.
The Family Welfare Program is designed to achieve various objectives to improve family life and societal health.
Here are the objectives of the Family Welfare Program.
Objectives of Family Welfare:
Improving the overall health and well-being of the family is a broad spectrum goal of Family Welfare among the objectives of Family Welfare.
The objectives of family welfare are as follows:
1) Promoting Reproductive Health:
To maintain the reproductive health of the family by ensuring that they have access to reproductive health related services, including,
Family planning, maternal and child health care, and prevention and management of reproductive tract infections. Their involvement is ensured.
2) Reducing Maternal Mortality Rate:
Maternal death and complications can be reduced by providing skilled care to the mother during pregnancy, during childbirth, and during the postpartum period.
3) Reduce Infant and Child Mortality:
Proper nutrition, immunization and provision of proper health care services to infants and children can reduce the morbidity and mortality rate in children.
4) Promoting Family Planning:
Encouraging individuals or couples to space their pregnancies and use contraceptive methods to plan pregnancies as per their choice.
5) Ensuring Safe Motherhood:
Promoting safe childbirth practices, prenatal care and postnatal care to improve maternal health outcomes.
6) Improving Nutrition and Hygiene:
Assessing malnutrition and promoting hygienic practices to improve the overall health and well-being of families.
7) Preventing and Management of Communicable Diseases:
Identifying and treating infections that affect reproductive health, such as sexually transmitted and other communicable diseases.
8) Social Support:
Social support includes providing a social support system to families and particularly vulnerable populations, such as single-parent households, low-income families, and families with disabilities and chronic illnesses. This support involves financial assistance, counseling services, and community-based support.
9) Promotion of Small Family Sizes:
Encouraging families to voluntarily choose small family sizes to improve maternal and child health outcomes and overall family well-being.
10) Promotion of Spacing Methods:
Advising the use of contraceptives to space pregnancies. This can promote healthier outcomes for the mother and her child.
11) Ensuring Access to Contraceptives:
Ensure that adequate contraceptives reach all eligible couples to properly adopt family planning.
12) Prevention of Unwanted Births:
Provide information and services to prevent unintended pregnancies, which can lead to better maternal health and improvements in socio-economic outcomes for families.
13) Promotion of Planned Pregnancy:
Encourage couples to plan and prepare for pregnancy in order to promote the health of both the mother and the child.
14) Promotion of Birth Spacing:
Advise families to maintain adequate space between pregnancies to maintain the overall well-being of the mother and child and reduce complications due to close pregnancies.
15) Age-appropriate Childbearing:
Advise families to plan for age-appropriate pregnancies to reduce complications due to early or late pregnancies.
These objectives collectively aim to empower individuals and families to make informed choices about their reproductive health and family planning, thereby improving overall health outcomes and enhancing the quality of life for families.
Role of Nurse in Family Welfare Program:
The role of a nurse in a family welfare program is diverse and multifaceted. Nurses play different roles in different settings of family welfare services. It usually depends on their post and their capacity to perform the work.
The role of Community Health Nurse (CHN) in Family Welfare Services is important to promote reproductive health, family planning and overall well-being in the community. Here are the main aspects of their role:
1) Survey work:
The nurse collects demographic facts through a survey.
She makes a list of the house numbers and their locations in the community.
The nurse collects information about pregnant mothers, eligible couples,
contraceptive users, children and children below school going age through a survey. Then she classifies the couples into high, medium and low priority.
To collect feedback on how many couples use contraceptives and how many people do not use them to form a further action plan.
2) Health Education:
To provide education about health and family planning to individuals, families and communities.
To make people aware about available family planning services.
To provide education and detailed information to couples about different types of contraceptives so that they can adopt them as per their choice.
To provide education to mothers to breastfeed their children for at least one year as it works as a natural contraceptive.
To provide education on immunization, nutrition, first aid and personal and environmental hygiene in the community.
3) Coordinator and Provider of Family Welfare Services:
To supply various types of contraceptives available to eligible couples.
To arrange family planning clinics and camps to create awareness about the needs and available services among the people.
To follow the rules and regulations of the State Government and the State and to provide direct services within legal and professional limits.
It coordinates the services of Gynecologists and other Family Welfare Services personnel.
5) Motivation Function:
Motivates eligible couples to adopt small family norms by using contraceptives.
Works to explain the need and importance of family planning.
To identify women who need medical termination of pregnancy and refer them to the doctor early.
To establish depots for adequate contraceptive supply and distribution in each village so that adequate supply of contraceptives can be ensured.
6) Administrative Role:
To determine the date and location of family planning clinics and arrange equipment, supplies and other resources in the clinics.
To supervise and guide multipurpose health workers in the clinics and distribute contraceptives and insert and remove IUD.
To provide assistance to the medical officer in conducting the clinics.
To organize family planning camps and assist doctors in male-female and female sterilization operations.
To maintain aseptic technique during operations.
Provide follow-up services to couples who have accepted the family planning method.
Plan and evaluate the education program.
7) Consultant:
As a coordinator in family welfare services and as a direct care provider, it is important to consult with them before starting any type of health care program in the community.
8) Counselor:
The nurse counsels eligible couples and target couples on different contraceptive methods and provides them with the opportunity to choose the best suitable method for spacing.
9) Supervisory Role:
As a supervisor, the nurse working in the family welfare department encourages her staff to actively participate in the family welfare program.
As a supervisor, the nurse organizes in-service education programs for health workers, professionals, and nursing personnel.
10) Domiciliary Services:
Home visits are an important part of the family program. These services are provided by multipurpose health workers and health assistants.
Among the services,
Providing education and motivation to eligible couples.
Provide advice for follow-up if using IUD and pills and provide education for follow-up in cases of vasectomy, tubectomy, medical termination of pregnancy (MTP).
Provide domiciliary care for antenatal, postnatal, newborn and toddler.
Provide referral services if any have post-operative complications.
11) Record Maintenance:
The nurse is responsible for maintaining all records in the family planning program such as,
Eligible couple records,
Target couple records,
Intrauterine devices records,
Sterilization operation records,
Clinic and camp records,
Health education activity records,
Training records,
Medical records etc.
The nurse is responsible for preparing monthly reports and submitting them to the authorities.
12) Role in Research:
The community health nurse is a primary member of the multidisciplinary research team. The nurse has to cooperate and participate in the research activities of the family welfare services.
13) Evaluation Role:
The nurse evaluates the work performed in the family welfare program and prepares its reports. On the basis of this evaluation, any further changes are made in the implementation of the program and the desirable targets are achieved.
14) Collaborator:
Community health nurses work in collaboration with health teachers and non-governmental organizations in the community to improve health care services.
Nurses work collaboratively with doctors, dispensers, vaccinators, trained birth attendants, and lady health visitors to provide family welfare services in the community.
Community health nurses play a crucial role in empowering individuals and families to make informed decisions about their reproductive health, supporting healthy pregnancy and childbirth, and contributing to the overall well-being of the community through effective family welfare programs.
Q-3 Write short answer (any two) Write short answer. (any two) 6+6-12
a) Describe school health services. Describe School Health Services.
School Health (Definition) :
School Health is a process of school that contributes to the maintenance and improvement of the health of students and school staff, including health services, healthy living and health education.
School Health Services: School health services are the provision of need-based comprehensive health services to school children or pupils, teachers and other persons so that their health is maintained. can be promoted and diseases can be prevented and controlled and their health can be maintained.
Objectives of School Health Program: School health program has multiple objectives, which aim to promote and maintain the health and well-being of students, thereby improving their overall education experience and outcomes.
The objectives for school health program are as follows:
1) Promotion of Health Education:
- To provide education to students on health related topics such as nutrition, physical activity, hygiene, mental health, substance abuse prevention and sexual health.
- Improves the education and awareness of students.
2) Prevention and Control of Disease:
- Measures are taken to prevent and control communicable diseases in children (ex: vaccination, hygiene practices).
- Screening of children for common health issues such as vision, hearing etc. and early management of any disease can be done.
3) Promotion of Mental Health:
- Child To create awareness about mental health and remove social stigma.
- If a child has stress, anxiety and any other mental problem, provide proper support to the child and take proper measures for its treatment.
4) Promotion of Healthy Behavior: Advise the child to do proper physical activities such as playing games, exercising, going to play outdoor games, etc. And educate the child for healthy eating habits such as giving advice on adequate nutritious diet intake.
5) Environmental Health and Safety:
- To ensure that the school environment is safe and clean, including,
- Clean drinking water, sanitation facilities,
- Safe playgrounds etc. Involvement of and provide education to the student for accident prevention and safety measures.
6) Counseling and Support Services: Provide appropriate counseling to the child who is going through personal and family issues. Provide support for the child’s social and emotional development through peer support groups and counseling sessions.
7) Cooperation and Partnership: Collaborate appropriately with families, community organizations, health care providers, and government agencies to effectively enhance health promotion efforts.
8) Other Objectives:
For positive health promotion of the child.
To detect any health related problem in the child early and provide immediate referral services to the child.
To assess and control communicable diseases in children.
To improve health awareness among children.
To provide a healthy environment for the child.
To inform the class teachers of the children about any problems seen in the children. To detect health problems like eye, skin, ear and dental problems early and provide proper hospital services to the child.
To reduce the morbidity rate in children. Accordingly, the objectives of the school health program have been formulated.
Common Health Problems in School Children: The various health problems seen in school going children generally vary depending on their age, religion and socioeconomic factors. Here is a list of health problems seen in school going children:
1) Respiratory infections: Including common cold, flu, tonsillitis, and bronchitis.
2) Gastrointestinal system: Including diarrhea, constipation, and abdominal pain.
3) Dental problems: Including cavities, tooth decay, and gingivitis.
4) Allergies: Allergic rhinitis (hay fever), food allergies, and skin allergies.
5) Injuries: Injuries due to falls, sports activities, or playground accidents.
6) Vision problems: Refractive errors such as nearsightedness or astigmatism.
7) Hearing problems: Hearing loss or ear infections.
8) Mental Health Issues: Anxiety Disorders, Depression, and Behavioral Changes.
9) Obesity and Overweight Due to excessive intake of fatty and spicy food and less physical activity.
10) Skin Conditions: Eczema, Dermatitis, and Fungal Infections Like Ringworm.
11) Nutritional Deficiencies: Iron Deficiency Anemia, Vitamin Deficiency.
12) Chronic Conditions: Asthma, Diabetes Epilepsy and Other Long Term Health Conditions.
13) Social and Emotional Issues: Bullying, Peer Pressure, Family and Academic Related Stress.
14) Infectious Diseases: Measles Chickenpox, and Other Communicable Diseases.
15) Sleep Disorders: Insomnia, sleep apnea, and inadequate amount of sleep due to various reasons.
16) Others: Tiredness, defective posture, headache, urinary infection, congenital health problems.
17) Anti-social problems: Stealing, lying, scheming, crookedness,
18) Habit Disorders: Thumb sucking, nail biting, bedwetting Waiting.
19) Personality Disorders: Jealousy, quick temper, timidity, shyness, daydreaming, fear and anxiety.
20) Psychosomatic Complaints: Tremors, headaches, asthma, depression, delusions, hallucinations.
21) Educational Difficulties: Lagging behind in studies, school phobia, school failure.
Collaboration between the child’s teachers, parents and health care personnel is essential for timely assessment of this common health problem seen in children and for its appropriate intervention, due to which the child’s condition can be treated timely and it can be prevented from becoming further complicated.
Aspects/Components of School Health Services:
- The school health program involves various components to promote and maintain the health and well-being of students. are.
- These services are necessary to ensure that students have access to healthcare resources and support in the school setting.
Here, the main aspects of school health services are given:
1) Health appraisal (assessment) of school children and school personnel.
2) Treatment and follow-up.
3) Prevention of communicable diseases.
4) Healthy school environment.
5) Nutritional Services.
6) First Aid and Emergency Care.
7) Mental Health.
8) Dental Health.
9) Eye Health.
10) Health Education.
11) Education of Handicapped Children.
12) Proper Maintenance and Use of School Health Records.
•>1) Health Appraisal (Assessment) of School Children and School Personnel:
In health appraisal (assessment), health assessment is performed not only of students but also of teachers and other school personnel.
Periodic health check-up of children, teachers and other school personnel.
When a child is admitted to school First medical examination and then medical examination every four years after admission and then examination at the time of leaving school.
In that examination,
Collect complete history of the child,
Do physical examination.
Do height, weight, teeth, speech, vision, hearing test of the child.
The child’s To conduct laboratory tests including blood, urine, and stool examination.
This responsibility is usually with primary health care which carries out services in rural areas and they are also responsible for providing treatment to children who are suffering from systemic infections, skin infections, or pediculosis.
To conduct daily check-ups of children by teachers in school health services and to train school teachers for the same and to refer the child immediately if he/she has any health related complications.
In which, the following changes are observed by the school teachers:
Dull face,
any abnormality,
coughing, sneezing, diarrhea.
Headache, fever, or chills,
redwatery eyes,
sleepiness,
pain in body,
scabies, pediculosis,
cold, nausea and vomiting are seen.
If any such symptoms are seen, the health care personnel should be informed by the jail teacher for immediate medical service.
2) Treatment and Follow-up:
- Advice should be given to the children regarding treatment and follow-up to cure any defect found in them.
- Inform the parents if any major illness is detected.
- Provide treatment and regular follow-up to the children by the school health nurse and provide proper care to the children. To do
Follow-up visits to maintain the child’s health.
3) Prevention of Communicable Diseases:
- Communicable diseases are controlled through timely immunization. Communicable diseases in children can be prevented through properly planned immunization for children.
- Properly immunize the child as per the National Immunization Schedule.
- Maintain proper records of immunization as part of the school health record and provide it to the child during school living time.
4) Healthy School Environment:
- School building and its environment play an important role in school health.
- School should be away from railway station, railway line, bus stand market and cinema.
- There should be one toilet facility for every 25 students which should be strengthened and arranged separately for boys and girls.
- School should have safe and separate drinking water, wash basin and school kitchen.
- The window size should be 25% of the floor area.
- The classrooms should be of white color.
- Proper lighting facility should be available.
- The school should have a separate water source.
- The school should have a separate room for the mid-day meal program (eating facility).
5) Nutritional Services:
- Diet is important for school children. It is important to provide nutritious food to a child who is physically and mentally weak.
- For proper development of the child, a nutritious diet should be taken, which should contain adequate amount of calories and protein.
Many children suffer from malnutrition, in which blindness and anemia are seen. - Malnutrition can be corrected through proper and adequate diet.
Provide a diet containing vitamin A (A) in nutrition.
To improve the health of children and prevent malnutrition A mid-day meal program is necessary to prevent it.
6) First Aid and Emergency Care:
- A first aid box should always be available in the school. So that accidents, abdominal pain, expected situations like spot accidents, epileptic convulsions and diarrhea can be handled.
- Teachers should be skilled in providing advice about first aid kits and drugs.
7) Mental Health:
- Excessive burden for studies and stress due to studies can lead to mental illness. There are many mental health problems such as juvenile delinquency, maladjustment, etc., which are common problems seen in children. For this, school children are helped by a vocational counselor or psychologist.
8) Dental Health: Children frequently suffer from dental diseases or defects and the treatment of such children and the teeth clinic are explained.
9) Eye Health:
- Schools are responsible for early detection of refractive error, treatment of squint, myopia eye infection etc.
- Children and Vitamin (A) administration.
- Providing basic eye health services in schools.
10) Health Education:
- Health education is very important for school children. Through it, awareness can be created by providing health matter related information. Motivation can be developed in children and health behavior can be changed.
Health education can change a child’s attitude towards health. - Health education is a key element of school health services.
- Health education can provide advice on personal hygiene, environmental health, nutrition, prevention and control of communicable diseases, first and emergency care, and home nursing. And parents can be given health education about reproductive health and psychological problems.
School teachers can motivate children to practice healthy habits through demonstrations, and provide proper education to children about maintaining high standards of cleanliness in schools, providing safe water supply, and having a good drainage system.
Health education should be need wise planned and organized, and the aim and objective should be achievable.
11) Education of Handicapped Children. Education of Handicapped Children The main aim of providing is that the child can live as normal a life as possible and remain independent.
12) Proper Maintenance and Use of School Health Records.
- Proper records should be maintained about the care provided to the child in the school.
- It records the child’s name, date of birth, names of his parents, etc.
- The child’s record also records the child’s past history, physical examination, and screening tests.
- Properly maintaining records can provide information about the child’s need for further treatment or any other health-related condition.
Role of the School Health Nurse in School Health Program:
1) General Physical Examination The School Health Nurse performs a general physical examination of the child. Conducts examination which involves head to toe examination.
2) Identify any abnormalities or defects: School health nurses identify possible abnormalities or defects early and treat them, and also provide advice for referral and follow-up where necessary.
3) Health Education:
- Children are advised by their parents and teachers to: Provide education such as maintain personal hygiene, prevention of communicable diseases, balanced diet, good nutrition.
- Provide proper health education in schools accordingly
4) First Aid Services: Provide emergency care and first aid services for injury or illness.
5) Periodic Visit: Periodic visit for medical checkup, follow-up and immunization program Take.
6) Immunization Record: Maintain proper records and provide immunization records to the child when he/she leaves school.
7) School Environment: Conduct proper examination of the school environment and identify hazards and report them to the authorities.
8) Maintain health records
Maintain a health record of each student, including his/her name, address, past health history, record of services provided and any investigation conducted, if any.
Thus, school health services are used to bring about improvement in the overall health condition of the child, and to identify any problems in the child early and take immediate measures.
b) UNICEF. UNICEF.
UNICEF (United Nations International Children’s Emergency Fund) is a global organization dedicated to advocating for and protecting the rights of children.
Founded in 1946, UNICEF works to improve the lives of children and their families in more than 190 countries and territories. It focuses on the most vulnerable and marginalized populations. Its efforts span a range of sectors, including health, education, nutrition, child protection and emergency relief.
Key Areas of UNICEF:
Health and Nutrition:
Ensure access to essential health care services and nutrition, including immunization, maternal and newborn care and treatment of malnutrition. Emphasize issues such as HIV/AIDS, water sanitation and hygiene.
Education:
Take measures to ensure that all children, especially girls and those in crisis-affected areas, have access to quality education. Support early childhood development and improve educational infrastructure and resources.
Child protection:
Provide protection to children from violence, exploitation and abuse. Address issues such as child labor, trafficking, and child marriage. Support legal and social systems to protect children’s rights.
Emergency Response:
Provide life-saving assistance during emergencies, including natural disasters, conflicts, and epidemics.
Ensure that children and families have access to shelter, food, clean water, medical care, and psychological support in all locations during emergencies.
Advocacy and Policy policy):
Advocate for policies and practices that promote children’s rights and well-being at the local, national and international levels. Partner with governments, NGOs and other stakeholders to influence policy changes and secure funding for child-focused programmes.
UNICEF’s Guiding Principles:
UNICEF’s work is guided by the principles of the Convention on the Rights of the Child (CRC). It outlines the fundamental rights of all children, including the rights to survival, development, protection and participation. The organization works on the belief that every child, regardless of their background and circumstances, should have a fair chance in life.
How UNICEF Operates Fundraising and Donations:
UNICEF is funded entirely by voluntary contributions from governments, private donors and fundraising initiatives.
Partnership:
To implement the program and reach children in need, the government collaborates with non-governmental organizations (NGOs), civil society, the private sector and the community.
Field Offices:
Operates field offices around the world to directly implement and monitor projects, ensuring that resources reach children and their families.
Key Programs and Initiatives:
Vaccine Alliance:
Works with partners to increase access to immunization in low-income countries.
UNICEF-School in a Box:
Provides portable learning supplies to children in emergency and conflict situations.
Impact:
UNICEF It has made significant progress in improving the lives of children globally.
It has contributed to reduced child mortality rates, increased school attendance, better nutrition and stronger child protection.
UNICEF continues to be a vital force in global efforts to create a world where every child is healthy, educated, protected and respected.
c) Write down National Nutritional Anemia Prophylaxis Program (NNAPP). Write about the National Nutritional Anemia Prophylaxis Program.
National Nutritional Anemia Prophylaxis (NNAPP) Program:
Introduction:
- NNAPP (National Nutritional Anemia Prophylaxis Program) was started in 1970, so that nutritional anemia could be prevented in pregnant women, lactating mothers, infants and children.
- Under this programme, pregnant women, lactating mothers and family planning beneficiaries are provided with iron and folic acid tablets.
- This programme has been initiated by the Maternal and Child Health (MCH) Department of the Ministry of Health and Family Welfare,
which is being implemented as part of the National Nutritional Anemia Prophylaxis (NNAP) Programme. - In which the target group has been expanded under the revised policy, which includes 6-12 months infants, school children and adolescents aged 11-18 years who Clinically diagnosed as anemic. They are included.
Specific Objectives:
- To assess the baseline condition of nutritional anemia in mothers and young children by estimating hemoglobin levels.
- Mothers and children with low Hb (hemoglobin) levels <10 g and <8 g Hb respectively should be treated with antianemia Provide treatment.
- Prophylaxis treatment to mothers with Hb level >10 gm and children with Hb level >8 gm.
- Continuously monitor the quality and distribution of tablets and consumption of supplements.
- Periodically assess the hemoglobin (HB) level of beneficiaries.
- Educate mothers through relevant nutritional education To encourage taking tablets. Activities:
This program involves the following activities:
- Promote regular consumption of iron rich food.
- Provide iron and folic acid supplements in the form of tablets to the target group.
- Identify cases of severe anemia and provide treatment for them.
- This program aims to improve dietary intake, promote consumption of iron and folate rich food and use of food items. Therefore, health and nutritional education is also involved.
Dose schedule:
- Child 6 month -5 year:= When the child is clinically anemic, 20 mg iron + 100 µg folic acid up to 100 days.
- School children 6-10 years :=30 mg iron + 250 mg folic acid for 100 days.
- Adolescent 11- 18 years :=100mg iron + 500 µg folic acid for 100 days.
- Pregnant mother:= 100mg iron + 500 µg folic acid for 100 days.
Nursing Mother and Family Planning Acceptors :=100mg iron + 500 µg folic Acid for 100 days.
Organization: This program is implemented by Primary Health Centers and their sub-centers. Multipurpose health workers and other paramedical staff at PHCs are responsible for the distribution of IFA (Iron and Folic Acid) tablets to the beneficiaries. ICDS (Integrated Child Development Services) scheme workers help in the implementation of the programme.
Q-4 Write short notes. Write short notes. (Any three) 12
a) Causes of infertility – Causes of infertility
There are three main causes of infertility.
A)Fault in female,
B)Fault in male,
C)Combined factor.
1)Fault in Female:
A) Ovarian Factor:
This is seen due to ovulatory dysfunction, mainly due to the following three reasons.
a) Anovulation/Oligoovulation:
Anovulation/Oligoovulation is usually seen due to disturbances in the hypothalamic-pituitary-ovarian axis.
Ovarian activity depends on gonadotrophins and normal secretion of gonadotrophins depends on GnRH (gonadotrophin releasing hormone) released from the hypothalamus. is.
(b) Luteinized Unruptured Follicle (LUF)
(Trapped Ovum):
This is due to inadequate growth and function of the corpus luteum.
( C) Trapped Ovum:
In this, the ovum is trapped inside the follicles, usually due to endometriosis or hyperprolactinemia.
2) Tubal Factors:
In this, infertility is usually due to tubopathy (tubal infection) due to which tubal functions are impaired.
Ex:= Defective ovum pickup and then infertility is seen.
3) Peritoneal factor:
One of the main factors of infertility is endometriosis.
4) Uterine factor:
There are some factors that stop the fertilized ovum from implanting in the endometrium.
These factors are like,
a) Endometriosis,
b) Fibroids Uterus,
c)Uterine hypoplasia,
d)Congenital malformation of the uterus.
5) Cervical factors:
These include second degree uterine prolapse,
retroverted uterus,
and changes in the composition of the cervical nucleus.
6) Vaginal factors:
These include vaginal atresia,
transverse vaginal septum,.
B) Fault in male:
1) Defective spermatogenesis Causes:
This causes infertility and is usually due to the following reasons:
Orchitis,
Undescended testicles,
Testicular toxins,
Primary testicular failure,
Genetic or chromosomal disorders such as 47,XXY,
Endocranial factors such as thyroid dysfunction.
2) Obstruction of the afferent duct system:
This is seen in two types.
1) Congenital:
Due to the absence of vas deferens.
2) Acquired:
This is usually due to some infection Due to,
Tuberculosis, Gonorrhea, and Surgical Trauma (During Herniorrhaphy).
3)Failure to Deposit Sperm in Vagina:
In this, sperm is deposited in the vagina due to failure.
The reasons for this are:
Impotence,
Ejaculatory Failure,
Hypospadiasis,
Bladder Neck Surgery.
4)Due to Errors in Seminal Fluid:
In this, due to immotile sperm,
sperm count is disturbed Due to,
Low fructose count.
C)Combined factor:
In this, infertility is seen due to combined factors of both male and female.
b) Functions of health team – Functions of health team
Definition:
A Health Team is a coordinated team of various health professionals who coordinate workers like Doctor, Nurse, Pharmacist, Lab Technician, Multi Purpose Health Worker (MPHW), ASHA, ANM, Community Health Officer (CHO) etc.
All these members function in a collaborative, systematic and professional manner to maintain and improve the health level of the people. The main objective of the Health Team is to ensure Comprehensive, Curative, Preventive and Promotional Health Services.
Major Functions of Health Team:
1) Providing Primary Health Care:
- The first and main function of the Health Team is to provide Primary Health Services to the people.
- This includes Immunization, ANC/PNC Care, Minor Illnesses Management, First Aid, Nutrition Support, etc.
- Providing Accessible, Affordable and Acceptable Health Services to every person.
- Example: Routine immunization days, health screening for children, anemia treatment in adolescent girls.
2) Providing Health Education:
- Health Team works to increase Health Awareness among the people.
- It spreads awareness among the people on the subject of Sanitation, Safe Water, Personal Hygiene, Nutrition, Reproductive Health, Family Planning etc.
- Health Education is a powerful tool to change the Health Behavior of the people.
- Example: Providing education through PPT, dramas, conversations in Village Health and Nutrition Day (VHND).
3) Disease Prevention and Control:
- Health Team performs functions for early diagnosis and control of diseases.
- Precautions are taken for both Communicable Diseases (TB, Malaria, Dengue, Leprosy) and Non-Communicable Diseases (Diabetes, Hypertension).
- Activities like Surveillance, Screening, Isolation, Health Check-up, Mass Drug Administration are carried out.
- Example: Pulse Polio Campaign, TB DOTS therapy, Mass Deworming Program.
4) Providing Referral Services:
- When the patient needs more specialized treatment, the Health Team prepares a systematic route to send him to PHC → CHC → District Hospital.
- Referral Slip, Ambulance coordination and Feedback are included.
- Example: High-risk pregnancy detected at SC referred to FRU (First Referral Unit).
5) Maternal and Child Health Services:
- ANC for mothers, Tetanus toxoid injection, Iron-Folic Acid tablets, institutional delivery.
- EBF (Exclusive Breastfeeding), Growth Monitoring, Immunization Schedule for Infants.
- Health Team works through MCH card, Mother-child protection card.
- Example: Janani Shishu Suraksha Karyakram (JSSK), Janani Suraksha Yojana (JSY).
6) Documentation and Reporting:
- Maintaining accurate records of Health Services is the responsible work of Health Team.
- This includes OPD Records, Immunization Register, ANC/PNC Records, Death/Birth Registration and Monthly Reports.
- Example: Data entry on HMIS (Health Management Information System) Portal.
7) Organizing Health Camps and Weekly Programs:
- Health Team organizes Health Camps, School Screening, Eye Camps, Blood Donation Drives at Community level.
- Health Week (Nutrition Week, Breastfeeding Week) is celebrated for public awareness.
- Example: Anaemia Mukt Bharat Week, WASH (Water, Sanitation and Hygiene) Campaign.
8) Family Welfare and Contraceptive Services:
- IUCD insertion, Oral Pills distribution, condom distribution, NSV/LSV Referral
- Counseling and follow-up for eligible couples (15–45 yrs).
- Example: Mission Parivar Vikas, 360° family planning counseling.
9) Reaching Vulnerable and Remote Areas:
- Health Team takes services to difficult-to-reach tribal, remote, and urban slum areas.
- Outreach session, mobile health team, school health visits are conducted.
- Example: ASHA workers by foot visit tribal hamlets with vaccine carriers.
10) Teamwork and Coordination:
- For the success of the Health Team, each member must perform his/her work properly.
- Coordination is maintained through DRG Meeting, VHSNC Meetings, Monthly Microplanning Meetings.
- Example: Sharing the work of CHO with MPW, ASHA, ANM on different days.
- Health Team is an integrated functional method in which various experts from the health sector come together to ensure health services for everyone – from children to the elderly.
- This team provides a continuum of care from Primary to Tertiary level, in which Prevention, Promotion, Cure and Rehabilitation are all involved.
- Kind, professional and effective Health Team plays a major role in improving the overall health outcome of the people.
Health Team is an integrated functional method in which various experts from the health sector come together to ensure health services for everyone – from children to the elderly.
This team provides a continuum of care from Primary to Tertiary level, which involves Prevention, Promotion, Cure and Rehabilitation.
A kind, professional and effective Health Team plays a major role in improving the overall health outcome of the people.
C) J.S.S.K (Janani Shishu Suraksha Karyakram) – Janani Shishu Suraksha Karyakram
Definition:
Janani Shishu Suraksha Karyakram (J.S.S.K) is a national health initiative launched by the Ministry of Health and Family Welfare across India from June 1, 2011.
The objective of this program is to make all necessary health services Cashless and Free for Pregnant Mothers and Newborn Infants so that Any financial barrier to healthcare should be removed.
Main Objectives:
- To reduce the Mother Mortality Rate.
- To reduce the Infant Mortality Rate to zero.
- To ensure 100% Cashless institutional deliveries for Mothers and Infants To provide accessible and comprehensive care in Government hospitals.
- To provide accessible and comprehensive care in Government hospitals.
Key Free Services Provided under J.S.S.K:
A. Free services for Pregnant Mothers:
- Free Delivery Services – Both Normal and Caesarean.
- Free Drugs and Consumables – Medicines and supplies required during treatment.
- Free Diagnostics – Laboratory tests, ultrasonography, etc.
- Free Diet during Hospital Stay – Food in government hospital.
- Free Blood Transfusion – If required Free blood transfusion facility then.
- Free Transport Facility:
- Home → Health Facility
- Referral transport between facilities
- Hospital → Home
- Home → Health Facility
- Free Stay for 48 hours post-delivery in the hospital.
B. Free Services for Newborn Infants (up to 30 Days):
- Free treatment for sick newborn infants.
- Necessary medicines and lab tests free of charge.
- Free blood transfusion.
- Free transportation arrangements.
- Neonatal Intensive Care Unit where required (NICU) service.
C. Extended Benefits:
- Sick infants up to 1 year of age now also covered (Free treatment for sick infants up to 1 year of age).
- Free treatment for complications in post-natal period for mothers (Free treatment for complications in post-natal period for mothers)
Who is the beneficiary? (Beneficiaries):
- All Pregnant Women delivering in Government Health Institutions
- Mothers belonging to Scheduled Castes (SC) and Scheduled Tribes (ST) ( Mothers belonging to Scheduled Castes (SC) and Scheduled Tribes (ST)).
Role of Nurse:
- To provide understanding to mothers about JSSK scheme.
- To ensure all services before and after institutional delivery.
- To provide necessary assistance for Neonatal care for infants.
- To maintain medicines, tests and patient records.
- To provide education to mothers for follow-up visits for postnatal care.
- Providing health education to mothers and families about Government Health Schemes.
J.S.S.K is a human-centered health service that removes financial barriers to healthcare for mothers and infants. This scheme strengthens institutional deliveries, neonatal care, and postnatal maternal recovery. It is an important step towards Reducing Maternal and Infant Mortality.
d) Mid-day meal program – Mid-day meal program
The Mid-day Meal Program is also called the “School Lunch Program”. This program was introduced in 1961 in a throwout country. Its main objective is to attract more children to school, reduce school dropout and improve the nutritional status and literacy rate of children.
Beneficiaries:
Schoolgoing Child
Objective:
To enhance the child’s admission to school.
To improve the child’s attraction towards school.
To enhance the child’s attention in school.
To improve the child’s literacy rate.
To improve the child’s nutritional status.
To improve the child’s health status.
Principles of Mid-Day Meal Program:
The food provided in the Mid-Day Meal Program is a supplement and not a substitute for the home diet.
The diet provided in the Mid-Day Meal Program can meet 1/3 of the total energy requirement and half of the protein need.
The cost of the meal is reasonably low.
The meal is easy to prepare and does not involve any complicated cooking process.
It uses only locally available food, which reduces the cost of the meal.
The menu of the diet provided is continuously changed, which avoids monotony.
Aim of Mid-Day Meal Program:
1) To increase the child’s attention to school.
2) To reduce school dropout.
3) To improve the nutritional status and health status of the child.
4) To fulfill 1/3 of the child’s nutritional requirement.
5) To improve the child’s interest in school.
6) To reduce the child’s school dropout.
7) To attract more children to school.
Sample Menu for Mid-Day Meal Program
1) Cereals and Millets:= 75 gm/day/ child ,
2)Pulses:=30 gm/ day/ child,
3)Oil and fat:=8 gm/ day/ child,
4)Green leafy vegetables:=30 gm/ day/ child.
5)Non-green leafy vegetables:=30 gm/ day/ child.
Q-5 Define following (any six) Write the following definition. (Any six) 12
a) Public health – Public health
Public health is a collective approach in which the efforts of society, organizations and individuals to prevent diseases, enhance the quality of life and improve health are based on science and Systemic activity includes.
b) Demography – Demography
Demos means people
Graphine means the record.
Demography
The scientific study of human population and its elements i.e. size, composition and distribution is called demography. Demography is the scientific study of population.
Concept of Demography
Demography is a branch of science that studies human population, focusing on only three elements.
- 1) If there are any changes in the size of the population, i.e. the size increases or decreases.
- 2) The Structure (Basic of Age and Size).
- 3) Geographical distribution by state or region.
(c) IMR – IMR
IMR- I.M.R (Infant Mortality Rate)
Definition:
The number of children who die within the age of 1 year out of the total number of live births in a given population of one thousand in the same year is called Infant Mortality Rate (IMR).
Formula:
IMR (Infant Mortality Rate) =
Number of deaths of children under one year of age
——————- x 1000
Total number of live births in the year
d) Target couple – Target couple
Target couple means a couple who have 2 to 3 live children and need to be highly motivated about family planning. They are called target couples.
e) Primary health care – Primary health care
Primary health care is an essential (necessary) health care that is made universally accessible to everyone and acceptable to everyone through full participation in it and primary health care should be affordable to the community and the country.
f) Health team – Health team
A health team is a group of trained medical and non-medical personnel with different levels of knowledge, qualifications, abilities, personality and skills. A group of professionals who complement each other and who share a common goal of providing comprehensive health services to individuals, families and communities.
g) Fertility – Fertility
When there is the ability to conceive and bear children, it is called fertility. Fertility is the natural capacity to produce offspring.
h) Immunity – Immunity
Immunity is a type of resistance that is activated by the host’s body. When any foreign body (antigen) enters the host’s body, the antibody that fights against that antigen is called immunity. When any antigen (foreign body) enters the body, the body’s ability to fight against it is called immunity.
There are two main types of immunity:
- 1) Innate immunity
- 2) Acquired immunity
(1) Innate immunity-Innate immunity is the immunity that a person has by birth. This is a type of natural immunity.
(2) Acquired immunity-The immunity that the body gets during the life after birth is called acquired immunity.
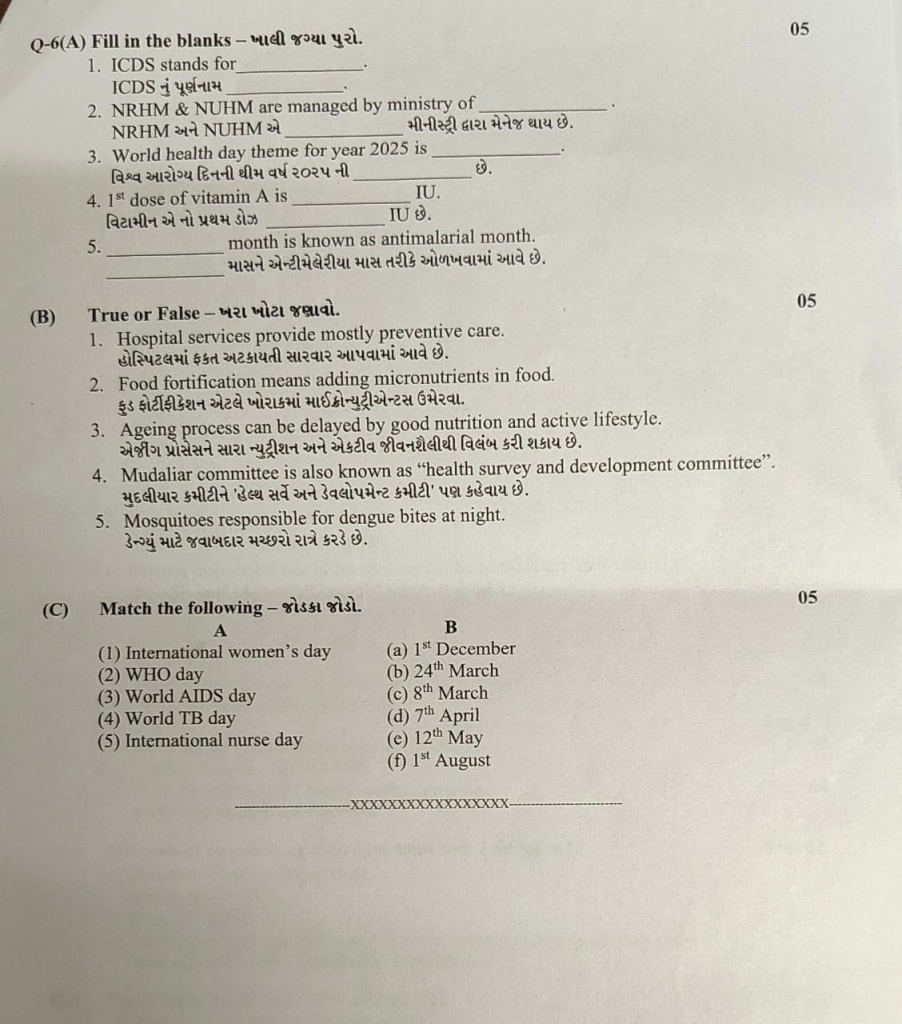
Q-6 (A) Fill in the blanks – Fill in the blanks.05
1.ICDS stands for……The full name of ICDS…… : Integrated Child Development Services
👉🏻 Full name of ICDS: Integrated Child Development Services
2.NRHM & NUHM are managed by ministry of……
NRHM and NUHM are managed by……Ministry of Health and Family Welfare 👉🏻 NRHM and NUHM are managed by Ministry of Health and Family Welfare.
3.World health day theme for year 2025 is……
The theme of World Health Day for the year 2025 is ……. is : “My health, my right”
👉🏻 Theme of World Health Day 2025: “My health, my right”
4.1 ^ (st) dose of vitamin A is IU…….
The first dose of vitamin A is……IU : 100,000 IU
👉🏻 The first dose of vitamin A is: 100,000 IU
👉🏻 The first dose of vitamin A is: 1,00,000 IU (for a child from 9 to 12 months)
5…….month is known as antimalarial month……. Month is known as antimalarial month: June👉🏻 June Month is known as antimalarial month.
B) True or False – Tell me the truth. 05
1.Hospital services provide mostly preventive care. Hospitals only provide preventive care : False ❌
(Hospitals mainly provide curative services, not preventive care.)
2.Food fortification means adding micronutrients in food. Food fortification means adding micronutrients to food: True ✅
3.Ageing process can be delayed by good nutrition and active lifestyle. The aging process can be delayed with good nutrition and an active lifestyle : True ✅
4.Mudaliar committee is also known as “health survey and development committee”.
Mudaliar committee is also known as ‘health survey and development committee’ : False ❌
5.Mosquitoes responsible for dengue bites at night.
Mosquitoes responsible for dengue bites at night : False ❌
(Aedes mosquito usually bites during daytime, especially early morning and late afternoon.)
(c) Match the following – Jodka Jodka. 05
A B
(1) International women’s day (a) 1 ^ (st) December
(2) WHO day (b) 24 ^ (th) March
(3) World AIDS day (c) 8 ^ (tn) March
(4) World TB day (d) 7 ^ (th) April
(5) International nurse day (e) 12 ^ (th) May
(f) 1 ^ (st) August
✅ Correct Match :
✅ (1 → c) 1 → (c) 8ᵗʰ March
✅ (2 → d) 2 → (d) 7ᵗʰ April
✅ (3 → a) 3 → (a) 1ˢᵗ December
✅ (4 → b) 4 → (b) 24ᵗʰ March
✅ (5 → e) 5 → (e) 12ᵗʰ May
