ENGLISH-18/02/2019(MSN:1)(Done-upload)-PAPER SOLUTION NO.10
18-02-2019-PAPER SOLUTION NO.10

Q-1 a. Write definition of Hernia. 03
Hernia is a condition in which a body organ or the muscular wall of the organ protrudes from its normal cavity.
The abdominal cavity has a muscular wall that plays an important role in supporting the abdominal organs.
When this muscular wall is bulging at some point, the abdominal organ protrudes from that bulging area into another cavity.
Hernia means that any organ protrudes from its normal cavity into another cavity, it is called a hernia.
Hernia := hernia may be defined as a protrusion of the organ from its normal body cavity to the other body cavity.
b. Explain types of Hernia. 04
There are three types of hernias.
1)Reducibal hernia,
2)Irreducible hernia,
3)Strangulated hernia
1)Reducibal hernia,
=> A reducible hernia can be placed back in its normal place.
=> A reducible hernia can be returned to its normal place if the protruding organ is pushed back.
=> People with this type of hernia wear a special type of hernia belt so that the protruding organ remains in its normal place.
2) Irreducible hernia,
=> Irreducible hernia is a type of hernia in which the organ that has protruded cannot be placed back in its normal place.
=> This is mainly due to the fact that the organ is blocked by other intestines at the place where it has protruded.
=> Surgery is mainly required to treat an irreducible hernia.
3) Strangulated hernia
=> In a strangulated hernia, the organ that has protruded is mainly twisted in the intestines and the blood supply there is impaired.
=> This impaired blood supply leads to the formation of ischemia, necrosis and gangrene.
=> Immediate surgery is required in strangulated hernia.
Classification of the hernia. (Classification of hernia):
There are a total of ten classifications of hernia.
1)Inguinal hernia,
2)Femoral hernia,
3)umbelical hernia,
4)Incisional hernia,
5)Hiatal hernia,
6)Epigastric hernia,
7)Obturator hernia,
8)Spigelial hernia,
9)Ventral hernia,
10)Herniation of intervertebral disc
1)Inguinal hernia,
=> Inguinal hernia occurs mainly in the groin region (the area between the abdomen and thigh).
=> Inguinal hernia is mainly when the intestine protrudes from the week point of the inguinal canal and forms a triangle shape in the abdominal muscles near the groin region.
Mainly
•>Obesity,
•> Pregnancy,
•> Heavy lifting,
•> Straining during stool pass.
2) Femoral hernia,
=> Inguinal hernia is mainly found in the area between the abdomen and thigh.
=> Femoral hernia is mainly a bulge-like structure that appears in the upper part of the thigh.
=> Femoral hernia occurs in the lower part of the inguinal ligament.
=>Femoral hernia is mainly seen in women, pregnant women and obese people.
3)Umbelical hernia,
=> Umbilical hernia is mainly seen when the abdominal wall around the umbilical cord is weakened.
=> Umbilical hernia mainly protrudes from the umbilical cord and the area nearer to the umbilical cord.
=> Umbilical hernia is mainly seen in newborns, children and adults.
4)Incisional hernia,
=> Incisional hernia is mainly seen when the intestine protrudes from the surgical area after previous abdominal surgery, which is called Incisional hernia.
=>This hernia is mainly seen in elderly or over weight people.
5) Hiatal hernia,
=>Hiatal hernia is mainly an abdominal organ that protrudes from the abdominal cavity through the diaphragm muscles into the chest cavity.
=> Due to this, symptoms like heart burn and stomach acid are seen.
6) Epigastric hernia,
=> Epigastric hernia is mainly seen when the upper middle abdomen muscles are weak and the abdominal organ protrudes.
=> Epigastric hernia is mainly seen in men and is more common in women.
=> This is mainly seen in people between the ages of 20 and 50.
7) Obturator hernia,
=> Obturator hernia is mainly a protrusion of an abdominal organ through a gap in the front part of the pelvis and the bone.
8) Spigelial hernia,
=> In Spigelian hernia, the abdominal organ protrudes mainly through the spigelian fascia.
9) Ventral hernia
=> Ventral hernia is mainly a protrusion of an abdominal organ through a gap in the abdominal wall due to scar tissue developing in the abdominal wall, causing the abdominal wall to become weak and the abdominal organ to protrude through it.
10) Herniation of intervertebral disc
=> It is called a hernia due to increased pressure in the intervertebral disc.
=> Intervertebral disc herniation is mainly seen when lifting any heavy object.
c. Write first 24 Hours Nursing Management for Patient with Hernioplasty. 05
Management of the patient after hernioplasty
Advise the patient to avoid heavy objects, weight lifting.
Advise the patient to wear a supporting belt.
Monitor the patient regularly.
Provide proton pump inhibitor medicine to the patient.
Advise the patient to eat fruits and high fiber fruits.
Advise the patient to do nasogastric suctioning.
Provide analgesic medicine to relieve the patient’s pain.
Provide antibiotic medicine to the patient.
Properly assess the patient’s health.
Assess the type of hernia the patient has.
Assess the patient for any signs and symptoms of hernia.
Provide complete information about the surgical procedure to the patient.
Prepare the patient properly for surgery.
Provide analgesic medicine to relieve the patient’s pain.
Advise the patient to do daily routine activities in small amounts and frequent amounts.
Monitor the patient for redness, itching, infection in the surgical incision.
Conduct proper wound assessment of the patient.
Provide the patient with a high-fiber diet, high fluids, and stool softeners.
Assess the patient for any complications.
Provide proper psychological support to the patient.
Advise the patient to follow up regularly.
Properly dress the patient’s surgical area.
Provide a calm and comfortable environment for the patient.
Properly provide intravenous fluids to the patient.
Properly provide mind diversional therapy to the patient.
Advise the patient to engage in small amounts of physical activity.
Advise the patient to engage in small amounts of daily routine activity.
OR
a. Write definition of Pneumonia. 03
Pneumonia is an infection and inflammation of the lung parenchyma (alveoli) caused by bacterial, viral or fungal infection. In this, the air sacs fill with fluid or pus and become solid. The alveoli normally function to exchange gases, but in the condition of pneumonia, due to infection and inflammation and accumulation of pus, gas exchange is interfered with.
b. Explain types of Pneumonia. 04
On the basis of etiological factors
Bacterial pneumonia:
Pneumonia caused by bacterial infection is known as bacterial pneumonia. Streptococcus pneumoniae, Mycoplasma pneumoniae and Haemophilus influenzae bacteria cause pneumonia.
Viral pneumonia:
Pneumonia caused by viral infection is known as viral pneumonia. Viruses such as influenza, coronavirus, adenovirus and respiratory syncytial virus are responsible for causing pneumonia.
Fungal pneumonia:
Pneumonia caused by fungal infection is known as fungal pneumonia.
On the basis of anatomical structure:
Pneumonia is classified as follows on the basis of anatomical structure:
Lobar pneumonia:
In lobar pneumonia, infection is seen in one or more lobes of the lungs.
Broncho pneumonia:
In broncho pneumonia, infection is seen in the bronchi in addition to many lobes.
Interstitial pneumonia:
In interstitial pneumonia, the interstitial tissue and alveolar septa are infected.
On the basis of broad classification:
Community acquired pneumonia:
Pneumonia that occurs in the community is called community acquired pneumonia.
Hospital Acquired Pneumonia:
Pneumonia that occurs after 48 hours of hospitalization is called hospital acquired pneumonia.
Ventilator Associated Pneumonia:
Pneumonia that occurs due to endotracheal intubation or mechanical ventilation is called ventilator associated pneumonia.
Aspiration Pneumonia:
Pneumonia that occurs due to aspiration of endogenous or exogenous substances is called aspiration pneumonia.
c. Write the Nursing Management for Pneumonia. 05
Nursing management of pneumonia:
Ineffective breathing pattern related to impaired exhalation and anxiety:-
Assess the patient’s respiration rate
Assess breathing pattern
Place the patient in the Fowler’s position
Give the patient oxygen
Check ABGs and oxygen levels to determine the effectiveness of treatment
- Ineffective airway clearance related to increased production of secretions:-
Assess the patient’s mucus production
Check the color and consistency of sputum
Help the client cough up sputum effectively
Encourage oral fluids to thin secretions
Increase room humidity
Give the patient steam inhalation
Give the patient a nebulizer
Do chest physiotherapy
Repeat oral every 2 hours Care
- Activity intolerance related to inadequate oxygenation and dyspnea:
Check the level of dyspnea
Give the patient oxygen
Reduce or stop activity if there are changes in respiration
Active exercise after respiration therapy
- Anxiety related to acute breathing difficulties and fear of suffocation:-
Stay with the patient when the patient has breathing difficulties
Maintain a calm environment
Teach the patient breathing retention and relaxation techniques
Clear all the doubts of the patient
Give the patient diversional therapy
- Disturbed sleep pattern related to dyspnea and external stimuli:-
Assess the patient’s sleep pattern
Ask not to use sleeping pills
The patient should be given a ventilated room
If necessary, the patient Give oxygen
- Administering Medications and Pharmacological Support
7.Initiating Measures for Infection Control & Management
8.Managing Acute Pain & Discomfort
9.Maintaining Normal Body Thermoregulation
- Promoting Optimal Nutrition & Fluid Balance
- Promote client education.
Q-2 a. List out the types of Anaesthesia and explain in details about care of Boyel’s Apparatus. 08
There are three types of anesthesia.
1) Local anesthesia:-
This affects a limited area of the body (local part). It usually affects only the part of the body on which surgery is to be performed, which part needs to be numbed.
The following chemicals are used in local anesthesia.
Xylocaine hydrochloride
Lignocaine hydrochloride
Amethocaine hydrochloride
Procaine hydrochloride
2) Spinal anesthesia:-
There are two types of this-
1) Epidural anesthesia:-
When anesthesia is injected into the epidural part of the spinal cord, it is called epidural anesthesia.
2) Spinal Anesthesia:-
When anesthesia is injected into the subarachnoid space of the spinal cord, it is called spinal anesthesia.
3) General Anesthesia:-
When the sensation is to be lost in the entire body, the person is rendered unconscious. This is called general anesthesia. General anesthesia can be given in the following ways-
Through Intravenous
Through Inhalation
Care of Boyel’s Apparatus:
Boyle’s apparatus is a modern anesthesia machine that delivers a fixed mixture of anesthetic gases and liquid drugs such as oxygen and nitrous oxide to the patient.
Daily maintenance and checking are essential for the proper functioning of this machine.
The outside of the machine should be cleaned daily with disinfectant to prevent the spread of pathogens during anesthesia.
The flowmeter and vaporizer should be checked daily for any gas leakage or defects.
The oxygen cylinder connected to the machine should be checked for sufficient gas and its pressure gauge should be in good condition.
It is necessary to check regularly whether the tubing and connections are installed correctly.
The anesthetic vaporizer should be calibrated periodically and the medication should be checked for correct filling.
A logbook should be kept of the daily use, servicing and defects of the machine.
The Boyles apparatus should be serviced annually by a qualified biomedical engineer.
Emergency oxygen supply should be available.
The machine should always be kept in a dry, clean, dust-free environment and the area should be free from any flammable materials to ensure patient safety and long-term operation of the machine.
b. Explain about special consideration in care of elderly. 04
1) Promotion of Self Respect and Dignity:-
Some institutes or groups usually have some restrictions on personal choice and independence.
The feelings and emotions of the elderly should be respected.
While the staff makes positive efforts to develop good relationships with the patients and gain their personal respect and friendship.
By developing good relationships, the group can be controlled and difficult situations can also be made easier.
2) Promotion of Comfort:
Relaxation is necessary for physical and mental comfort. There are many factors that contribute to the comfort of the elderly such as skin care, care of bone structure, maintenance of temperature and fluid balance.
3) Safety:-
Provide unpolished floors, good lighting, proper bed height, proper walking aids
4) Daily Living Activities:-
Encourage the patient to do as much daily activity as possible so that complications like dehydration, thrombosis, pressure sores, contractures, etc. can be avoided.
5) Promotion of independence:-
Encourage the patient to take self-care as much as possible and ask him to make his own decisions.
6) Encourage mobility and movement
7) Ask him to take necessary medicines and provide sufficient knowledge about those medicines such as side effects of the medicine, its use.
8) If the patient is in pain, do rehabilitation according to his condition.
Additional Information:-
Skin care:-
Use mild soap
Bath once or twice a week
Hair care and brushing every day
Use moisturizers
Keep nails short
Use sunscreen, hat, long-sleeved clothing
Stay away from things like hot water bottles.
Pay attention to footwear so that sores do not occur
Avoid sun stroke
Supporting Changes in Bones and Joints:-
Do light exercise
Avoid falling
Take precautions
Give a balanced diet that includes calcium and vitamin D supplements
Monitor and treat patient for pain
Give the patient more time because it may take more time to work.
Supporting Changes in Vision:-
Proper lighting should be provided to the patient
If necessary, the patient should be helped in choosing clothes
Natural tear products should be used.
The patient should be approached directly.
Supporting Changes to Hearing:-
While talking, the extra noise should be reduced.
Put yourself in the patient’s place so that the patient’s needs can be understood
Before speaking, make sure that the person’s attention is on you or not.
Get checked by a doctor and if necessary, get wax (mel) removed
Arrange a hearing assessment and if necessary, provide a hearing aid.
5.Supporting Changes in Smell and Taste:-
Attractive meals should be prepared in which food with good smell should be prepared.
Spoiled food should not be given to eat
6.Supporting Changes in the Cardiovascular System:-
People get tired more easily due to cardiovascular changes, so they should be given more rest.
According to healthcare professionals, regular blood pressure monitoring should be done
If the person is unable to move on his own, he should be made to change positions frequently
Ask him to drink enough fluids and seek immediate medical help if the patient is dehydrated.
7.Supporting Changes in the Respiratory System:-
Short-term activities should be planned
More time is needed for rest.
If the person is unable to move on their own, they should be changed frequently
If the person is coughing continuously during or after meals, then ask them to consult a doctor
Keep the body alignment and position proper
Stay away from polluted air
Give oxygen therapy if necessary
8.Digestive Care:-
Maintain oral hygiene
Take appropriate treatment if there is tooth damage
Provide a comfortable environment for eating
Feed high fiber, high protein food with different tastes and textures.
Advise to drink more fluids
Give calcium and vitamin D supplements to prevent osteoporosis
9.Supporting Changes in Elimination:-
Maintain daily activities
Plan for the bathroom when going out
Reduce caffeine intake
Increase fiber intake
Do light exercise
Provide emotional support.
Everything should be given as needed.
- Urinary Care:-
Increase fluid intake
Drink less fluid before bedtime
Wear clothes that can be easily removed
Use absorbent pads
- Elderly care at home:-
If there is a wound, take care of it and get it dressed regularly
Monitor vital signs and give medicine on time.
Manage any pain or discomfort the patient may experience
Help with daily hygiene needs.
OR
a. Prepare the Nursing Care Plan for Diabetic patient. 08
1️⃣ Assessment :
Patient complains of polyuria (frequent urination), polydipsia (excessive thirst), fatigue, blurred vision.
Blood glucose levels elevated (FBS > 126 mg/dL).
Dietary history shows high carbohydrate intake.
May show signs of delayed wound healing or tingling in feet (neuropathy).
2️⃣ Nursing Diagnosis :
Imbalanced nutrition: More than body requirements r/t excessive intake of carbohydrates.
Risk for unstable blood glucose levels r/t inadequate insulin administration.
Deficient knowledge regarding disease condition and self-care.
(Lack of knowledge about the disease and ignorance about self-care)
Risk for infection r/t delayed wound healing and reduced immunity.
3️⃣ Goals / Objectives:
Patient will maintain blood glucose within normal range (70–110 mg/dL).
Patient will verbalize understanding of diabetic diet and self-monitoring.
Wounds (if present) will show signs of healing without infection.
Patient will demonstrate insulin administration technique correctly.
4️⃣ Planning:
Plan individualized meal chart with balanced carbs and fiber.
Schedule regular blood glucose monitoring.
Plan teaching sessions on insulin use and foot care.
Provide wound care and monitor for signs of infection.
5️⃣ Interventions:
Monitor blood glucose levels before meals and at bedtime.
Educate patient on diabetic foot care, proper footwear, daily foot checks.
Administer insulin as prescribed and observe for hypoglycemia symptoms.
Provide diabetic-friendly diet with guidance from dietician.
Encourage fluid intake and promote exercise (e.g., walking).
Maintain hygiene and check any wound for delayed healing.
6️⃣ Rationale:
Monitoring glucose prevents hypo-/hyperglycemia.
Education increases compliance and reduces complications.
Proper insulin use ensures control of sugar levels.
Balanced diet aids in long-term disease control.
Early identification of infection improves outcomes.
7️⃣ Evaluation:
Patient’s blood glucose maintained within target range.
Patient verbalizes understanding of disease and self-care steps.
No signs of wound infection or new complications.
Improved nutritional habits observed.
8️⃣ Health Education:
Teach patient the importance of adherence to insulin therapy.
Educate about symptoms of hypoglycemia & hyperglycemia.
Reinforce the need for routine check-ups (HbA1c every 3 months).
Emphasize diabetic foot care and eye check-ups.
Avoid smoking and alcohol.
Special Notes:
Maintain patient’s psychological support.
Encourage self-monitoring using glucometer.
Refer to diabetic educator or counselor if no
b. Explain about stages of illness, 04
Stages of illness:
These indicate the process of development of a disease. These stages are helpful in helping people focus on their health-related goals and also give healthcare professionals clues as to when their treatment should be increased or changed. They are divided into five main stages:
- Incubation Period:
In this stage, pathogens such as bacteria, viruses, fungi, etc., enter the body but it takes time for their full effects to be seen.
This is the period before symptoms appear.
For example, when a person is suffering from heart disease, it may take a short time to see the proper symptoms such as swelling or pain.
Symptoms: No symptoms are seen in this stage.
- Prodromal Period:
In this stage, the initial symptoms of the disease begin to appear, but they are not very clear.
Symptoms can usually be in the form of malaise, fatigue, body aches and fever.
In this stage, the person is preparing for the complete development of the disease.
Symptoms: Minor discomfort, dyspepsia, nausea and other common symptoms.
- Illness Period:
In this stage, the disease occurs with its complete symptoms.
Specific effects begin to appear on the body, and the symptoms of the disease develop rapidly.
In this stage, the patient feels the most distressed and unwell, and their symptoms can become more pronounced and dangerous.
For example, the high symptoms of flu include chills, fever, and sore throat.
Symptoms: Fever, Nasal Congestion, Chest Pain, Cough.
- Convalescence Period:
In this stage, the patient is at rest and the body begins to recover.
The symptoms of the disease begin to subside, and the body is gaining strength for the whole world.
In this stage, the patient often relies on treatment and rest.
Symptoms: Fatigue decreases, the body starts functioning better, and strength returns.
- Recovery Period:
In this stage, the patient is almost recovered and it may not take much time for all their symptoms to go away.
The patient can return to a healthy state and perform normal activities.
But, sometimes, the patient may experience relapse, as the disease spreads.
Symptoms: Recovery in health and physical strength.
Conclusion:
These stages of illness are a very important part of explaining the development of any disease. These stages may be different for each person.
Q-3 Write Short Answers (Any Two)2×6-12
a. Explain about Altered Immune Response.
Altered Immune Response
Definition:
An altered immune response is a condition in which the normal response of a patient’s immune system is decomposed, causing it to be hypoactive, hyperactive, or misdirected. As a result, the patient may develop pathological conditions such as infection, autoimmune disorders, allergic reactions, or immunodeficiency.
Major Types of Altered Immune Responses:
1️⃣ Hypersensitivity Reaction
A response in which the immune system responds more than normal. There are four types:
Type I (Immediate/Anaphylactic reaction):
The moment the allergen enters the patient’s body, histamine and immune chemicals are released. Example: Asthma, Anaphylaxis, Allergic rhinitis
Type II (Cytotoxic reaction):
Antibodies directly damage the patient’s cells. Example: Hemolytic anemia, Blood transfusion mismatch
Type III (Immune complex reaction):
Antigen-antibody complex forms and causes tissue damage. Example: Systemic lupus erythematosus (SLE), Rheumatoid arthritis
Type IV (Delayed hypersensitivity):
This type is mediated by T-lymphocytes and appears slowly. Example: Tuberculin test (Mantoux), Contact dermatitis
2️⃣ Immunodeficiency
The immune system is weak or does not respond at all. Two types:
Primary Immunodeficiency:
Present from birth. Example: Severe Combined Immunodeficiency (SCID)
Secondary Immunodeficiency:
Acquired by the patient, such as HIV/AIDS. Example: Acquired Immunodeficiency Syndrome (AIDS)
3️⃣ Autoimmune Disorders
The immune system attacks its own body cells as a foreign body. Example:
Type 1 Diabetes Mellitus
Hashimoto’s thyroiditis
Multiple sclerosis
Myasthenia gravis
4️⃣ Transplant Rejection
The patient’s immune cells respond to the donated organ and reject it. Example: Kidney graft rejection, Liver transplant rejection
Mechanism:
Altered Immune Response occurs through abnormal activation of the patient’s B-lymphocytes, T-lymphocytes, macrophages, cytokines and complement system.
As a result, inflammation, cell lysis, tissue destruction or microbial invasion occurs in the patient’s body.
Diagnostic Tests:
CBC with Differential count
Immunoglobulin levels (IgG, IgA, IgM)
ANA test
ELISA (for HIV)
Skin allergy test
Lymphocyte proliferation assay
CRP, ESR
Treatment:
Hypersensitivity Antihistamines, Corticosteroids, Epinephrine
Autoimmune Disorder Immunosuppressants (e.g., Methotrexate), Monoclonal antibodies
Immunodeficiency IVIG (Intravenous Immunoglobulin), Antiretroviral therapy
Transplant Rejection Cyclosporine, Tacrolimus, Steroids
Nursing Care:
Take precautions to protect the patient from infection
Monitor the patient’s vital signs
Observe for side effects during immunotherapy
Educate the patient on personal hygiene
Counsel the patient on booster doses or recovery
Summary: Altered Immune response is a disruption in the functioning of a patient’s immune system, which can often lead to life-threatening conditions. Its timely diagnosis, treatment, and nursing management are essential for the patient’s survival.
b. Define Hypovolemia and write Nursing Care of Hypovolemia.
Hypovolemia:
Hypovolemia is a clinical condition in which the volume of blood or fluid in the patient’s body is reduced. This condition is characterized by a decrease in intravascular volume, which can lead to decreased organ perfusion and more severe conditions such as shock. The main causes of hypovolemia include excessive bleeding, dehydration, persistent vomiting, diarrhea, severe burns, and polyuria. The main clinical symptoms in the patient include tachycardia, hypotension, cold clammy skin, rapid breathing, oliguria and altered mental status. If not treated promptly, this condition can become life-threatening.
Nursing Care of Hypovolemia:
1.Monitoring of Vital Signs:
The patient’s vital signs such as blood pressure, pulse rate, respiratory rate and temperature must be monitored regularly so that positive or negative changes in the patient’s condition can be identified in a timely manner.
2.Fluid Replacement Therapy:
The first aim should be to replace the lost volume by providing intravenous fluids to the patient. The nurse should carefully monitor the type, rate, and response to fluids.
3.Intake and Output Monitoring:
Accurate documentation and monitoring of the patient’s fluid intake and urine output are very important. Symptoms such as oliguria or anuria indicate the severity of hypovolemia.
4.Assessment of Mental Status:
Regular assessment of the patient’s mental status is necessary because decreased blood supply to the brain can cause altered sensorium or confusion.
5.Skin and Peripheral Circulation Observation:
Peripheral perfusion is assessed by skin color, temperature, and capillary refill time, which can indicate the condition of hypovolemia.
6.Oxygen Administration:
If the patient shows symptoms of hypoxia, oxygen therapy should be administered.
7.Emotional Support and Communication:
It is also the nurse’s responsibility to explain the condition to the patient and his family, reassure them, and provide emotional support to the patient.
Hypovolemia is a condition that requires serious and immediate attention, and timely recognition and appropriate nursing intervention are essential for its effective management.
c. Write about role of Circulatory Nurse In Operation Theatre.
Introduction:
Circulatory Nurse is a nurse in the nursing team of Operation Theatre (OT) who is responsible for all the orderliness, cooperation and safety of OT, staying outside the sterile field. She functions as a non-sterile team member and controls life-saving or surgical instruments.
Major Responsibilities of Circulatory Nurse in Operation Theatre:
- Participate in pre-operative preparation:
Check the cleanliness and sanitization of OT.
Keep necessary instruments and suture materials available.
Ensure the functionality of OT table, suction, cautery, monitors etc.
Open sterile packs and give them to scrub nurse
Check consent form and match patient identity
It is necessary to complete all preparations as per pre-operative safety checklist.
- Patient Transfer and Positioning:
Assist in transferring patient from stretcher to OT table.
Position patient as directed by surgeon and anesthetist (e.g., lithotomy, prone, supine)
Fix safety belts
Proper positioning prevents nerve injury and pressure ulcers.
- Provide Non-Sterile Support during surgery:
Open OT doors, maintain records, and bring supplies
Specimens (biopsy, tissue) are labeled and sent to lab.
Deliver blood products, medications, implants to surgeon
Documentation (instrument count, time of incision, closure, sponge count)
Circulatory nurse acts as a link between sterile team and outer OT area.
4.Communication Link:
Talk to external OT team, like laboratory, blood bank, CSSD, pharmacy
Pass-on for critical call/notification surgeon
Co-ordinate with patient’s relatives for updates (if allowed)
Nurse ensures smooth intra-operative communication.
5.Help in Emergency Management:
Keep crash cart/nebulizer/oxygen cylinder ready
Bring immediate equipment in case of anaphylactic reaction or cardiac arrest
Help in providing additional instrument/equipment
Quick response saves life during OT emergencies.
6.Post-operative Documentation & Clean-up:
Confirm final sponge/needle/instrument count
Maintain specimen dispatch records
Send OT instruments to CSSD for disinfection
Discard used linen/waste as per biomedical waste management
Disinfect and re-stock OT for next case
Post-op record keeping ensures legal and procedural safety.
Qualities Required:
Alertness & quick response
Effective communication
Infection control knowledge
Accurate documentation skill
Team coordination & empathy
Conclusion:
The Circulatory Nurse works as the “invisible backbone” in the silent and sensitive environment of the OT. She/he is responsible for communication, management, and coordination between the patient, OT team, and other departments throughout the surgical procedure, outside the sterile field.
d. Define Epilepsy and write Nursing Care of Epilepsy.
Epilepsy:
If the patient has repeated episodes of seizures, then that condition is converted into epilepsy. Epilepsy is a mental abnormality in which the electrical impulses of the neurons in the brain of a person are greatly disturbed, due to which abnormal electrical activity is seen in the neurons and the condition of epilepsy occurs, due to which jerking moments arise in the body.
Nursing management of epilepsy:
Maintain a properly safe environment to prevent the patient from injury.
Keep the side rails up to prevent the patient from injury.
Do not put any kind of object in the patient’s mouth.
If the patient is wearing anything around the neck, loosen it.
Do not restrain the patient to prevent injury.
Provide a small pillow under the patient’s head.
If the patient is vomiting, take proper care to prevent aspiration.
Keep suction readily available.
Keep the patient’s airway patent so that he can breathe properly.
Advise the patient to take proper bed rest.
Advise the patient to take a special ketogenic diet, which mainly keeps the amount of carbohydrates low and provides high amounts of fiber, minerals, and protein.
Provide the patient with intravenous fluids.
Provide oxygen therapy to the patient.
Provide proper work and comfortable environment to the patient.
Advise the patient to take medication properly.
Q-4 Write Short notes (Any Three) 3×4-12
a. Suture Material
Definition:
Suture material is a surgical thread that is used to close a patient’s wound or incision. Its main purpose is to connect the tissues of the body and keep them in place until the natural healing process.
Need for Sutures:
For hemostasis
For tissue approximation
To prevent infection
To heal the wound quickly and properly
To maintain the stability of an organ or bone
Main Types of Suture Material:
- According to Absorbability
A. Absorbable Sutures:
This material is absorbed by the body itself within a few days after it is inserted into the body.
Use: Internal organs, gastrointestinal tract, gynecological surgeries
Examples:
Plain Catgut (from animal intestine)
Chromic Catgut (treated for time-delay)
Polyglactin 910 (Vicryl)
Polyglycolic acid (Dexon)
Polydioxanone (PDS)
Absorption Time:
Vicryl: ~60-90 days
Catgut: ~7-10 days
PDS: ~120-180 days
B. Non-Absorbable Sutures:
This material is not absorbed by the body and often has to be surgically removed.
Use: Skin, cardiovascular, neurological, and orthopedic surgeries
Examples:
Silk
Nylon (Ethilon)
Polypropylene (Prolene)
Polyester (Ethibond)
Stainless Steel wire
2.According to Structure:
A. Monofilament Sutures:
Made of a single fiber → Less abrasion → Less risk of infection
Example: Nylon, Prolene, PDS
B. Multifilament Sutures:
Woven with many fibers → Stronger → More knot security
Example: Silk, Vicryl, Polyester
3.According to Origin
A. Natural Sutures:
Obtained from natural sources
Example: Catgut (sheep intestine), Silk (silkworm)
B. Synthetic Sutures:
Man-made polymer-based materials
Example: Vicryl, Nylon, PDS, Prolene
4.According to Usage Site As per):
Site Preferred Sutures
Skin Nylon, Prolene
Internal Organs Vicryl, PDS
Cardiovascular Prolene
Orthopedic Stainless steel wire
Neurosurgery Silk, Prolene
Suture Sizes:
Larger number → thinner thread
0 to 7 = thick sutures (for orthopedic or fascia)
4-0 to 10-0 = finer sutures (for blood vessels, nerves, eyes)
Example:
6-0 Nylon → Used for facial/cosmetic suturing
0 Vicryl → For muscle closure
Suture Needles (Types of Suture Needles):
Cutting Needle – Hard tissue (Skin)
Reverse Cutting – Plastic surgery
Tapered Needle – Soft tissue (intestine, bladder)
Blunt Needle – Friable tissues (liver)
Role of Nurse with Suture Materials:
Maintain sterile field
Choosing the right type – Absorbable vs. Non-absorbable
Checking suture expiry date & labeling
Preparing instruments and sutures in OT set-up
Assisting/handling sutures as per doctor’s orders
Assessing sutures for post-op wound inspection
Following aseptic technique for suture removal
Documentation – Suture type, size, site, date of removal
Suture materials are a basic surgical tool for patient safe wound care. Their proper selection, use and management are a skill
b. Haemodialysis
Definition:-
Hemodialysis is a method of removing excess waste (metabolic waste products) from the body in cases of renal failure, in which excess waste is removed from the blood. After removing harmful substances, the purified blood is returned to the patient’s body.
Purpose :-
To remove excess waste from the patient’s body.
To make the body’s buffer system positive
To remove excess fluid from the body
To reduce water retention
To maintain the level of electrolytes in the body
To prevent other complications
Indications:-
Acute renal failure
Chronic renal failure
Uremia
Renal encephalopathy
Severe edema
Metabolic acidosis
Procedure :-
In hemodialysis, there is a machine (dialyzer) for purifying the blood. In which impure arterial blood is taken from the patient’s body and sent to it. The useless waste in the blood is filtered and then becomes pure blood, which is injected into the patient through a vein.
In hemodialysis, a fistula (connection between an artery and a vein) is made. From where impure blood is removed and pure blood is introduced.
This fistula can be made on wrist, arm and neck.
Complication:-
Dehydration
Hypovolemia
Hypotension
Hypovolemic shock
Septicemia
Death
Care during hemodialysis:-
Check the patient’s weight and record it.
Written consent is obtained from the patient for dialysis.
Explain the dialysis procedure to reduce their anxiety
Provide the patient with a comfortable position
Ask the patient to stop antihypertensive and vasodilator medications before dialysis, if any, as dialysis can cause hypotension
Check and monitor vital signs
If there is any problem during dialysis, the patient should be asked about it and if necessary, the doctor should be informed immediately.
Check the patient’s fistula site regularly because due to the use of heparin during the procedure, the clotting process slows down and the possibility of bleeding increases.
All emergency medications should be kept ready with the patient
The patient should be given the necessary medications.
After the completion of hemodialysis, the patient’s weight should be checked again
The patient should be given the necessary medications after hemodialysis.
c. Graft versus host disease.
This is a systemic disorder in which the graft immune cells recognize the host as a foreign substance and then attack the recipient body cells. Graft means donation and host means the tissue of the recipient. In this, the reaction towards the graft that is placed is seen from the host body, which can be immediate and rejection can also be seen in the later stage. The signs of this rejection are seen like antigen antibody reaction.
The full form of GVHD IS GRAFT VERSUS HOST DISEASE.
Graft versus host disease occurs when an immunodeficient patient transfers or transplants with immunocompetent cells. Graft versus host disease is seen. Graft versus host disease occurs when the human leukocyte antigen (HLA) of the donor and recipient do not match.
GRAFT VERSUS HOST DISEASE occurs after:
1)blood transfusion,
2)liver, kidney and bone marrow transplantation,
3)after fetal thymus transplantation,
GRAFT VERSUS HOST DISEASE occurs within 100 days of transplantation.
It mainly affects the
Skin,
Liver,
and the Gastrointestinal Track.
sign and symptoms/clinical manifestation of GRAFT VERSUS HOST DISEASE.
macula popular rashes on the skin,palms,hands and soles of feet.
These rashes spread throughout the entire body.
Abdominal pain,
nausea,
vomiting,
diarrhea,
malabsorption,
mild jaundice and elevated liver enzymes,
bacterial and fungal infections,
if symptoms are limited to the gastrointestinal tract and skin, then the prognosis is good, but if multisystem involvement is present, the prognosis is not very good.
treatment of GVHD:
Provide corticosteroid medicine to the patient.
Provide immunosuppressant agents (methotrexate, Cyclosporine) to the patient.
Proper assessment should be done when blood transfusion is required.
Assess the patient for any adverse reactions.
Assess the patient for skin redness, erythema, swelling.
Provide immunosuppressive therapy to the patient.
If the patient has any other signs and symptoms, inform the doctor immediately.
d. Nursing Process-
Nursing process was introduced by HALL in 1955. This is a systemic decision making process. In which the problem is solved through the steps of assessment, nursing diagnosis, planning implementation, evaluation. This is a continuous process. The health status and health problem of the patient are assessed from time to time. And the nursing care is modified based on the feedback or evaluation received from it. Thus, the nursing process is a continuous cycle. The steps shown above are interrelated and interdependent.
Nursing process is a systemic process of providing nursing care to the patient, the steps of which are as follows.
1.Nursing Assessment:-
Definition:-
Assessment means collecting clinical information and interpreting it.
In this, information about the patient’s wellness, functional ability, physical status, strength, actual and potential health problems is collected.
Purpose of assessment:-
To obtain information about the patient’s health
To know the patient’s normal function
To arrange the information obtained
To investigate the nursing problem
To create a nursing diagnosis frame
To identify the health problem
To identify the client’s strength
To identify the need for health teaching
Type of Assessment:-
Initial assessment:-
This assessment is done at the time of admission. Date:- Nursing admission
B.Problem focused assessment:-
Early assessment is done to identify the specific problem.
Dental:- Fluid intake and urine output are checked every hour to assess the problem of urination.
C. Emergency Assessment:-
Rapid assessment is done to identify the physiological crisis of the patient such as life threatening problem.
Dental:- Assessment of client’s airway,
Breathing status and circulation after cardiac arrest.
D.Time lapsed assessment:-
In this, data is compared with the initial assessment. In this, reassessment is done. In this, the current condition of the client is compared with the baseline data taken earlier.
Component of assessment:-
Collecting data
Organizing data
Validating data
Recording data
1.Collecting data:-
The process of obtaining information about the health status of the client is called data collection. It includes nursing health history, physical assessment,
physical examination, laboratory results and diagnostic tests.
The data includes past history as well as present complaints.
While collecting data, the following points should be kept in mind.
- Data collection should be systematic and continuous so that errors in the data can be prevented.
- The data should not be based on actual or potential health problems.
- Data should be descriptive, clear, concise, complete
Type of Data :-
There are two types of data.
Subjective data
Objective data
Subjective data:-
This is known as symptoms or covert data.
Subjective data is given by the patient himself.
In this data, the patient himself describes his previous experience, as well as feelings, emotions in his own words.
Objective data :-
This is known as sign or overt data.
Objective data is taken by the health team such as observation, physical examination, diagnostic test is measured.
Source of data :-
Primary sources:-
In this, data is obtained directly from the patient, in which physical examination and interview are used.
Secondary sources:-
In this, data is obtained from the patient’s relatives, medical records, charts and other members of the health team.
Method of Data Collection:-
- Observation:-
In this, information is obtained by observing the patient.
- Interview:-
Interview is a planned and purposeful communication with the patient to obtain information. In which information is collected to identify the client’s problem, to teach the patient, and to provide counseling.
- Examination:-
Systematic data is collected to identify health problems. Which includes physical examination techniques, interpretation of laboratory results, and measurement.
Cephalo caudal approach :– Head to Toe examination
Body system approach:- Examination of body system
Review of system approach:– Examination of particular area
Organizing Data :-
The nurse organizes the data collected from the patient in a proper manner.
3.validating data:-
Validation means in simple words, cross checking the information obtained. Whether the information obtained is factual or true or not is confirmed.
- Recording data :-
Recording of the document is important. The record should be accessible, understandable and complete, legible.
Recording should be done systematically.
2.Nursing Diagnosis:-
Nursing diagnosis is the second step of the nursing process. Which follows the nursing assessment.
In this phase, the collected data is analyzed to identify the problem and make a nursing diagnosis, based on which nursing care is provided.
The North American Nursing Diagnosis Association (NANDA 1992) defines Nursing Diagnosis as:
The North American Nursing Diagnosis Association (NANDA 1992) defines nursing diagnosis as follows:
“A clinical judgment of an actual or potential health problem of an individual, family, or community. A nursing diagnosis provides information for the selection of nursing interventions to achieve that outcome.”
A nursing diagnosis is written in a written format and is called a “PES”.
P=Problem statement/diagnostic label/definition
E=Etiology/related factors/causes
S=Defining
characteristics/signs and symptoms
PURPOSES OF NURSING DIAGNOSIS:-
A. To analyze the data collected.
B. To determine the client’s normal functional level statement.
C. To identify the client’s strengths and weaknesses.
D. To make diagnostic weaknesses.
CHARACTERISTICS OF NURSING DIAGNOSIS:-
- It clearly and concisely states the health problem
- It is based on existing evidence about the client
- It is potentially useful for providing nursing therapy (care).
- It is a basis for planning nursing care and also for providing nursing care.
TYPES OF NURSING DIAGNOSIS :-
- Actual Nursing Diagnosis:-
The problem that is found during the nursing assessment (Problem + Etiology + Signs/Symptoms) is called Actual Nursing Diagnosis. And this is based on the current signs and symptoms of the patient
Drugs :-
-Imbalanced Nutrition: Less than body.
- secretions Acute Pain (Chest) related to coughs secondary to pneumonia
-Activity Intolerance related to general weakness.
- High Risk Diagnosis :- This is also called potential problem. There are no signs or symptoms in this. This is a clinical judgment. But in this, the problem is not present but the risk factor is present.
Eg:-
1) Risk for impaired skin integrity Related to surgery. In this, the patient is at risk of bed sores due to prolonged bed rest and changing positions.
2) High risk for infection related to hospitalization immuno suppressed medication.
In this, the patient is at risk of infection due to immunosuppressive medication.
- Wellness Diagnosis:-
This is a clinical judgment which is a process to change the specific level of wellness of the individual, family, community from an individual, family, community to a higher level of wellness. (Carpenito 1993)
Diagnosis: Birth of new born twins.
- Syndrome Diagnosis: This is a set of actual or high risk nursing diagnoses that are based on an event or situation.(Carpenito 1993)
Diagnosis:-a Rape,Trauma Syndrome
STATEMENT OF NURSING DIAGNOSIS:-
Nursing diagnosis provides guidance for planning to provide goal oriented nursing care.
A nursing diagnostic statement has three parts: problem, etiology & defining characteristics.
(1) Problem:
This describes the patient’s response for which nursing care is being provided. The nurse clearly and concisely states the problem that has occurred.
Definition:- Knowledge deficit, Acute, Chronic, Ineffective, Altered, Decreased etc.
2) Etiology:
Etiology is the component used to identify one or more health problems. Etiology provides guidance for planning nursing interventions. This helps the nurse to provide individualized care to the patient because both patients have the same problem but the causes are different.
Definition:- 1) Anxiety related to hospitalization
2) Anxiety related to diagnostic test
Problem:- Anxiety
Etiology:- hospitalization, Diagnostic test.
(3) Defining characteristics:
These are the signs and symptoms of the problem. Which help in making a nursing diagnosis. This includes subjective or objective data.
Definition:- 1. Fluid volume deficit related to decreased oral intake manifested by dry skin and mucous membranes.
- Risk for impaired skin integrity related to immobility manifested by redness on skin.
NANDA Diagnosis:–
NANDA diagnosis is a list of Diagnosis. (North American Nursing Association)
- Planning :-
Planning is an important step of the nursing process. It is a purposeful activity. Which includes critical thinking. What to do, when to do it, where to do it and who will do it can be decided and how to evaluate the results.
Definition:-
According to Cozier (1975) “Planning is a systematic phase of the nursing process that involves decision making and problem solving.
Purpose of planning:-
To guide activities for client care
To maintain continuity of care
To authorize specific activities
Type of planning:-
There are three types of planning
Initial planning:-
The planning that is done after the initial assessment is called initial planning. Planning should start early because of the tendency towards shorter hospital stays.
Ongoing planning:-
Ongoing planning is done by all the nurses who care for the client. This planning includes daily planning.
Discharge planning:-
This planning is a process of planning what will be required after the patient is discharged and is an important part of comprehensive care. This is included in every nursing care plan.
Phase of planning:-
Planning is a phase in which the nurse decides how to provide individual, goal-oriented nursing care.
There are 4 phases of planning.
Setting priorities
Setting goals
Determining nursing strategies
Developing a nursing care plan.
- Implementation:-
Simply put, implementation is the process of putting the plan into practice. It is the fourth step of the nursing process in which the nurse uses her knowledge and skills to provide nursing care.
PURPOSE OF IMPLEMENTATION:-
To provide technical nursing care
To provide therapeutic nursing care
To help the client achieve optimum level of health.
Performing Nursing Intervention:-
Nursing intervention is an activity that is performed by the nurse and includes preventing illness, improving and maintaining the health of the patient. Nursing interventions are as follows
To perform the patient’s activities themselves: – Bed bath, mouth care, vital check
To assist the patient in activities: – Range of motion exercises.
To supervise the activities that the patient performs himself.
- Evaluation:-
Evaluation is the fifth step of the nursing process. Which follows implementation.
In the evaluation phase, the nurse checks whether the nursing care plan has had an effect and whether the goals have been achieved.
Evaluation is a continuous process in which the nurse assesses and reassesses the program to determine whether the patient’s goals have been achieved.
Purpose of Evaluation:-
To obtain data on the nursing care provided and make a judgment about it
To check the patient’s behavioral response to the nursing intervention
To compare the patient’s current response with the previously determined criteria
To find out the shortcomings in the care plan
To check the quality of nursing care
Activity in Evaluation phase:-
To review the patient’s goals and criteria, outcomes
To obtain data
To obtain goals
To modify nursing care
To revise the patient’s goals and criteria to see the outcomes.
e. Role of Nurse in Cadaver Transplant
Introduction:
Cadaver Transplant is a process in which organs (such as kidneys, liver, heart) from a deceased person (Brain-dead donor) are used to transplant into a living patient. During this, the nurse plays an important and supportive role — for both the donor and the recipient.
Major Roles of Nurse in Cadaver Transplant:
- Assist in Donor Identification and Certification:
Assists in Neurological assessment required for identification of brain death
Performs continuous monitoring of the donor to maintain vital stability
Assists in Apnea test and documentation for brain death
Identification of the donor, proper documentation and structural process are essential.
2.Donor Management:
Maintain the donor’s vital signs (BP, HR, Temp)
Regularly check fluid balance, electrolytes, and oxygenation
Control ventilator support.
Maintain asepsis technique for infection prevention
It is necessary for the donor’s body to remain hemodynamically stable so that the organs remain alive.
3.Family Counseling and Psycho-social Support:
Explain the donor’s family about brain death
Provide complete information about organ donation
Provide psychological support to the bereaved family
With family psychological support, it becomes easier to get consent for organ donation.
4.Co-ordination with Transplant Team:
Coordinating between transplant coordinator, surgeon, anesthetist and OT staff
Helping in completing documentation and consent forms
Being prepared for logistic transfer from OT to ICU
Active and prompt communication determines the success of the transplant.
5.Preparations of the Recipient:
Assessing the recipient’s pre-transplant investigations and lab values
Noting NPO status, medications and pre-operative checklist
Providing emotional support and counseling to reduce anxiety
It is very important that the recipient is mentally and physically prepared for the transplant.
6.Intra-operative Assistance:
Support in OT by maintaining sterile technique
Keep instruments, fluids, graft preservation solutions, etc. ready
Assess recipient when transferring to ICU after OT
Nursing support is important for surgical team to maintain sterile field and for graft stability.
7.Post-operative Care:
Assess recipient’s vital signs, urine output, graft functioning
Monitor immunosuppressive therapy.
Insist on strict aseptic precautions for infection prevention.
Provide psychological counseling and post-discharge education.
The post-transplant phase is the most sensitive and requires skilled care to prevent graft rejection.
(Summary):
Cadaver organ transplant is a life-saving procedure in which the nurse acts as a technical, emotional, and ethical care provider for both donor and recipient.
The nurse’s role encompasses many areas, including assessment, management, coordination, documentation, psychological support, and post-transplant care.
Q-5 Write Definition (Any Six) 6×2-12
a. Kerning’s Sign
Kerning’s sign is a physical symptom of meningitis. In which the leg cannot be straightened when the hip is flexed 90 degrees, due to which severe stiffness is seen in the hamstring muscles. This is an important clinical feature for the condition of meningitis.
c. Halitosis
Halitosis is also called bad breath. In halitosis, an unpleasant odor is present when the breath is exhaled. Halitosis is mainly seen due to dental decay, poor dental care, any gum disease, and bacterial infection.
b. Hyperkalaemia
Hyperkalaemia is a condition in which the potassium level in the body or blood exceeds the normal potassium level.
Normal serum potassium level:
3.5 – 5.0 mEq/L .
Hyperkalaemia: Hyperkalaemia is when the potassium level is > 5.0 mEq/L or more. (In hyperkalaemia the potassium level is greater than 5.5meq/litre).
f. Haemorrhoids
Haemorrhoids are swollen blood vessels that are located in the anus and rectum. It can develop both internally and externally in the anus and rectum. Common symptoms include pain, itching, swelling, and bleeding. Hemorrhoids are caused by increased pressure on the lower anus due to chronic constipation or diarrhea, obesity, pregnancy, and heavy lifting.
c. Pleural Effusion
Pleural effusion is the accumulation of excess fluid between the layers of the pleura outside the lungs. The pleura is a thin layer that covers the inside of the lungs and chest cavity and helps to facilitate the movement of the lungs during breathing. When excess fluid accumulates in the pleural space, it can cause symptoms such as chest pain, shortness of breath, and cough.
g. Altered Sensorium
Altered Sensorium is a clinical condition in which a patient’s Consciousness, Cognition, and Awareness are altered. The patient may exhibit states such as Confusion, Disorientation, Delirium, Stupor, or Coma. Altered Sensorium is not a disease in itself but is a symptom of an underlying condition. This condition can arise due to Metabolic Disorders, Head Injury, Infections, Stroke, or Drug Toxicity. Its severity can range from mild to severe. Evaluation requires a history, clinical examination, laboratory tests, and imaging. If timely medical management is not done, the condition can become life-threatening.
h. Biopsy
A biopsy is a medical procedure in which a small sample of tissue is collected from the body for examination under a microscope.
A biopsy is done to diagnose diseases, usually to determine whether a tumor is benign or malignant (cancerous).
A biopsy can be done on any part of the body and is usually done using a needle, but sometimes a surgical procedure is required.
The collected tissue is examined by a pathologist, who provides a detailed report on the presence, type, and severity of any abnormalities found.
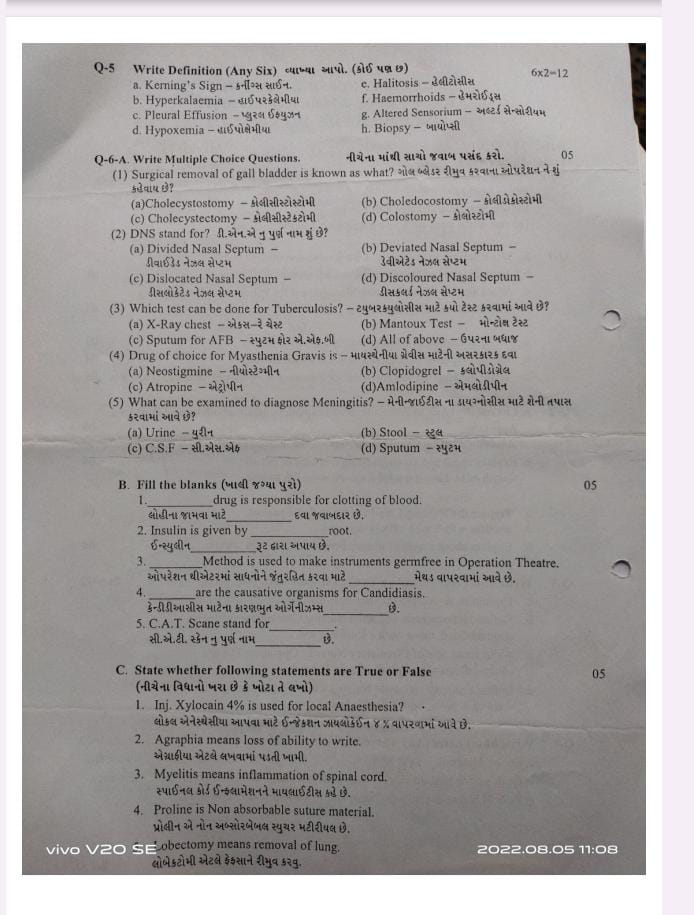
Q-6-A. Write Multiple Choice Questions. 05
(1) Surgical removal of gall bladder is known as what?
(a) Cholecystostomy
(b) Choledocostomy
✅ (c) Cholecystectomy
(d) Colostomy
📌 Correct Answer: (c)
📝 Rationale: Cholecystectomy = removal of gall bladder
(2) DNS stands for? What does DNS stand for?
(a) Divided Nasal Septum
✅ (b) Deviated Nasal Septum
(c) Dislocated Nasal Septum
(d) Discoloured Nasal Septum
📌 Correct Answer: (b)
📝 Rationale: DNS = Deviated Nasal Septum = Deviation of the nasal septum.
(3) Which test can be done for Tuberculosis?
(a) X-Ray chest
(b) Mantoux Test
(c) Sputum for AFB
✅ (d) All of the above
📌 Correct Answer: (d)
📝 Rationale: All tests are useful for diagnosing TB – chest X-ray, Mantoux, and AFB in sputum.
(4) Drug of choice for Myasthenia Gravis is:
✅ (a) Neostigmine
(b) Clopidogrel
(c) Atropine
(d) Amlodipine
📌 Correct Answer: (a)
📝 Rationale: Neostigmine is an anticholinesterase drug used in Myasthenia Gravis to improve muscle strength.
(5) What can be examined to diagnose Meningitis?
(a) Urine
(b) Stool
✅ (c) CSF
(d) Sputum
📌 Correct Answer: (c)
📝 Rationale: CSF examination helps detect infection in meningitis by lumbar puncture.
B. Fill the blanks 05
1……………………………drug is responsible for clotting of blood. Vitamin K
2.Insulin is given by …………….root. Subcutaneous
3…………………….Method is used to make instruments germfree in Operation Theatre. Autoclaving
4………………..are the causative organisms for Candidiasis. Fungi (Candida albicans)
5.C.A.T. Scane stand for………………… Computed Axial Tomography
C. State whether the following statements are True or False 05
1.Inj. Xylocain 4% is used for local Anaesthesia? ✔️
2.Agraphia means loss of ability to write. ✔️
3.Myelitis means inflammation of spinal cord. ✔️
4.Proline is Non absorbable suture material.✔️
5.Lobectomy means removal of lung. .❌
