ENGLISH-MSN : 2 (PAPER SOLUTION) (30/07/2024)-UPLOAD no.8
PAPER SOLUTION NO.8-GNC-30-07-2024
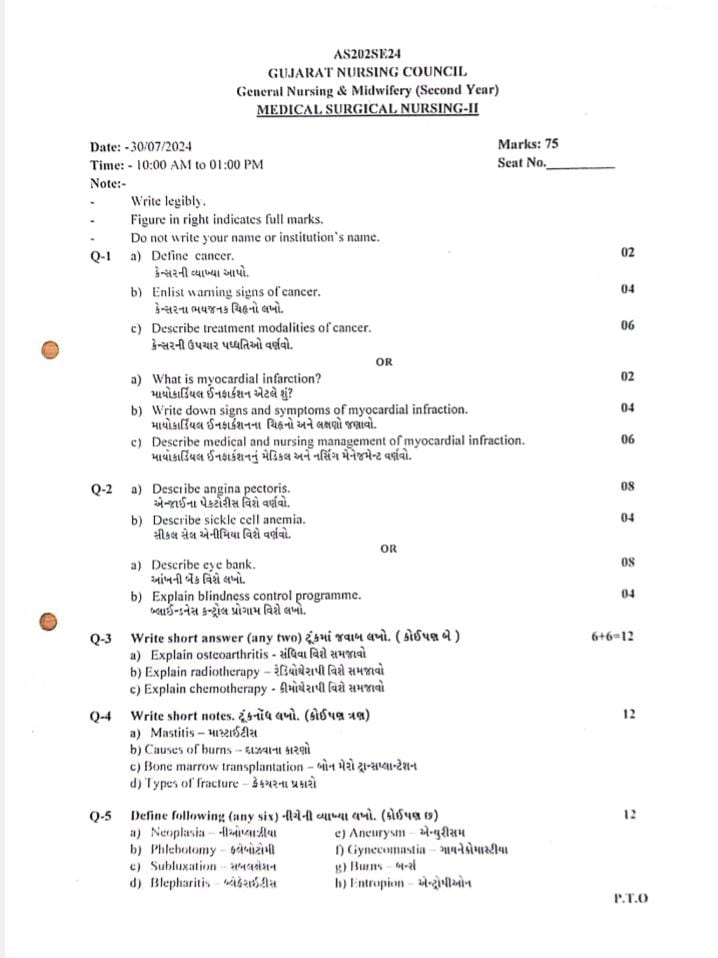
Q-1 a) Define cancer.(02)
Cancer is a group of diseases in which cells grow uncontrollably and can invade nearby tissues and spread throughout the body. Cancer is a disease in which cells grow uncontrollably and multiply, can invade nearby organs and spread throughout the body. Cancer cells spread through the blood and lymphatic system in the body. Cancer is not a single disease but a group of about 100 types of cancer. Cancer is named after the part of the body, organ or tissue where it starts.
For example:
- if cancer starts from colon it’s called colon cancer
- if cancer starts from basal cell of skin its called as a basal cell carcinoma.
b) Enlist warning signs of cancer. (04)
Warning sign of cancer:
CAUTION
1) C:= change in bowel and bladder habit
2) A:=A sore that does not cure
3) U:=Unusual bleeding and discharge
4) T:=Thickening of lump in breast or any other parts
5) l:=Indigestion and difficulty in swallowing
6) O:=Obvious change in mole
7) N:=Naging cough and soreness
Change in bowel and bladder habit
Description( Description ):= In a normal person, the habit of bowel is one to two times.
It changes to 3 to five times.
Bladder:= A normal person passes out the bladder five to six times a day. It increases to 10 to 20 times.
1) Urine and stool change in consistency, size and frequency. Blood is present in urine and stool.
A sore that does not cure.
Description ( Description ):=
1):= In this, the sore keeps getting bigger.
2):= It is very painful.
3):= Blood comes out of it.
In this, wherever the sore falls or ulcer occurs in the body, it never heals, instead of healing, it increases and increases excessively.
Unusual bleeding and discharge.
Description ( Description )
1) :=Blood comes from urine and stool.
2) :=Blood comes from any part of the body such as 1)nipple, 2)penis.
Bleeding or discharge comes from any part of the body, this is a sign of a type of cancer.
Thickening of lump and mass in breast or any other parts of the body.
Description ( Description ):= If there is a lump and mass, then it never heals.
It gets bigger and bigger in its place.
And that lump and mass also causes more pain and becomes like a lump.
Indigestion and difficulty in swallowing.
Description ( Description ):= In this, whatever is eaten is not digested and it becomes difficult to swallow food.
As a warning to a person who has cancer, regurgitation of food occurs.
Obvious change in mole.
Description (description ):= If there is any mass and lump, its size changes.
The lump and mass become larger in the place where it decreases.
- Necrosis, nagging cough and hoarseness.
Whenever coughing and nagging occurs, a hoarse sound is felt. - There is a change in the voice.
- The voice becomes thick.
- Blood comes out in the phlegm.
- All these signs are warning signs of cancer.
c) Describe treatment modalities of cancer.(06)
The various treatment modalities for cancer are given below:
Treatment Modalities for Cancer:
Surgery:
- Procedure: Removal of a cancerous tumor through surgery.
- Purpose: To stop the spread of cancer by removing the tumor completely or partially.
Radiation Therapy:
- Procedure: To destroy cancer cells using high-energy rays.
- Purpose: To reduce the size of the tumor and destroy cancer cells.
Chemotherapy:
- Procedure: To stop or destroy cancer cells from growing through medicine.
- Purpose: To stop the spread of cancer cells and destroy them.
Hormone Therapy:
- Procedure: To block hormones necessary for the growth of cancer.
- Purpose: To control the growth of hormone-sensitive tumors.
Immunotherapy:
- Procedure: To strengthen the body’s immune system or increase its ability to fight cancer.
- Purpose: To stimulate the immune system to recognize and destroy cancer cells.
Targeted Therapy:
- Procedure: To destroy cancer cells by targeting specific genes or proteins.
- Purpose: To target specific tumor markers or genes, so that healthy cells are less damaged.
Stem Cell Transplant:
- Procedure: Replacing the patient’s own stem cells with new ones.
- Purpose: To restore damaged cells that have been destroyed by chemotherapy or radiation.
Phototherapy:
- Procedure: To destroy tumors using a special type of light.
- Purpose: To effectively destroy tumor cells with light.
Laser Therapy:
- Procedure: To destroy cancer tumors using laser beams.
- Purpose: To target and destroy specific tumors.
Clinical Trials:
- Procedure: To participate in testing new treatments and medicines.
- Purpose: Practical training for new and unproven treatments.
These different approaches to cancer treatment are chosen based on the severity, type, and physical condition of the patient.
OR
a) What is myocardial infarction? (02)
This is a type of medical emergency. In which the condition in which the myocardium of the heart is permanently damaged due to blockage in the coronary artery that supplies blood to the heart, due to lack of blood supply, is called myocardial infarction.
The cause of blockage in the artery is the condition of thrombus formation and atherosclerosis. Due to which the myocardium does not get oxygenated blood supply and its muscle tissue gets necrosis.
This condition is also known as heart attack. It is also an important cause of mortality.
b) Write down signs and symptoms of myocardial infraction. (04)
- In this condition, ischemic pain is mainly seen due to insufficient oxygenated blood supply to the myocardium.
- It is characterized by retrosternal chest pain or chest heaviness in the middle of the chest.
- This pain is very severe and may radiate to the left side of the jaw and arm.
- Nausea and vomiting are also seen in this condition.
- Due to stimulation of the sympathetic nervous system, profuse sweating (diaphoresis) is also seen and the skin is cold and clammy.
- Hypotension and tachycardia are also seen due to decreased cardiac output.
- The person may experience shock and may also experience difficulty breathing or shortness of breath.
- Anxiety, palpitations and headaches are also seen in the person.
Cardiac arrhythmia is also seen in this condition. - This is a very serious medical emergency condition. If not treated on time, the person may die.
c) Describe medical and nursing management of myocardial infraction. (06)
- This is an emergency medical condition. In which immediate management is done.
- To reduce the oxygen demand of the myocardium, give the person rest and start oxygen therapy.
- Give emotional support to the person and try to reduce anxiety.
- By giving nitroglycerides medicines, the patient feels relief in pain.
- Morphine is also given for pain management.
- The general condition of the person as well as his cardiac function should be monitored regularly and should be observed for complications.
- The hemodynamic status of the patient should be monitored and his urine output should also be monitored.
- In emergency conditions, thrombolytic therapy, blood thinner medicines should be given as per the doctor’s order.
- The patient’s level of consciousness should be monitored, his nutritional status should be monitored and the general condition should be observed.
- Stool softeners and sedative medicines are also given to the patient as per the need and doctor’s order.
- Health education should be given to the patient regarding his lifestyle modification, diet, exercise, non-pharmacological management.
- Advise the patient to minimize his risk factors.
Take medicine on time and also explain about follow-up care. - In severe cases, surgical or invasive procedures are also performed. Explain about all the care and precautions of this procedure.
Q-2
a) Describe angina pectoris. (08)
Introduction:
Angina pectoris is also known as ‘ischemic chest pain’. Angina pectoris is the medical term used for ‘chest pain’ and ‘discomfort’ caused by coronary heart disease. Angina is not a disease but a symptom of coronary artery disease. Due to plaque deposits in the coronary arteries, it becomes narrowed, due to which not enough blood and oxygen reaches the heart muscles and due to which chest pain is seen.
Types of angina pectoris:
✓ Stable (classic) angina: In stable angina, chest pain is seen when exertion, exercise or any stressful activity is done. This pain can be relieved by rest and medication.
✓ Unstable Angina: Unstable angina is the least common and most severe type. In which chest pain is seen during rest or minimal exertion. Hence, it cannot be relieved by rest and medication. This is an impending sign for a heart attack.
✓ Variant Angina: Variant angina, also known as ‘Prinzmetal’ and ‘vasospastic angina’, in which chest pain is seen due to spasm in the coronary arteries. This pain is seen during periods of rest and this pain is seen during midnight and early morning hours.
✓ Refractory Angina: Refractory angina is a severe and persistent form of angina in which chest pain persists despite medication, lifestyle changes, angioplasty, and bypass surgery. Treatment options include enhanced external counterpulsation (EECP), spinal cord stimulation, and heart transplantation.
✓ Silent Angina: In silent ischemia, the patient does not feel pain, meaning there are subjective data omissions. But it can be determined with the help of ECG, exercise stress test, and Holter monitoring.
Causes of angina pectoris:
- Deposition of plaque in coronary artery
- Coronary artery spasm
- Arterial embolism
- Narrowing of heart valve (aortic stenosis)
- Hypertrophic cardiomyopathy
- Severe anemia
Signs and symptoms seen in angina pectoris
- Chest pain
- This pain is felt as pressure, tightness, squeezing, heaviness, burning.
- This pain is seen radiating to the neck, jaw, shoulder, arm and back.
- Discomfort
- Shortness of breath
- Fatigue
- Weakness
- Sweating
- Nausea
- Vomiting
Diagnostic evaluation of angina pectoris
- History collection
- Physical examination
- Electrocardiogram (ECG/EKG)
- Echocardiogram
- Coronary angiography
- Exercise stress test
- Blood test – cholesterol level, troponin, creatine kinase (CK-MB), myoglobin
Medical management of angina pectoris:
Oxygen therapy: Administer oxygen through a nasal cannula or mask. So that the heart muscles get oxygen.
Vasodilator: Use nitroglycerin as a vasodilator drug. It dilates blood vessels to improve blood flow. (Angina can be relieved by nitroglycerin, so nitroglycerin is the drug of choice)
Antiplatelets: Antiplatelet drugs thin the blood and prevent blood clots. For example, aspirin.
Beta blocker: Provide beta blockers to reduce the heart’s workload. It slows the heart rate and decreases blood pressure. For example, propranolol, atenolol
Calcium channel blocker: Calcium channel blocker blocks the entry of calcium into the heart muscle, causing the muscle to relax and helping the arteries to widen and lower blood pressure. For example, amlodipine, nifedipine
ACE inhibitor: ACE inhibitor prevents the conversion of angiotensin I to angiotensin II and promotes diuresis, vasodilation, and reduces the workload of the heart. For example, enalapril, captopril
Statin: Statin decreases cholesterol levels and reduces the risk of plaque buildup in the arteries. For example, atorvastatin.
surgical management of angina pectoris:
✓ Coronary artery bypass grafting (CABG)
In CABG, a new route is created for a narrow or blocked coronary artery or it is bypassed. In which healthy blood vessels are harvested from any part of the body such as the chest, leg, arm and these harvested blood vessels are attached to the coronary artery and the blocked part is bypassed and normal blood flow is restored. CABG is mainly preferred in multiple coronary artery blockage conditions. Apart from this, CABG is done when medication and angioplasty fail.
✓ Percutaneous transluminal coronary angioplasty (PTCA)
PTCA is a minimally invasive surgical procedure which is used to open narrow and blocked coronary arteries. In which a balloon attached to a catheter is inserted into the narrowed artery and then the balloon is inflated so that the artery widens and the plaque flattens against the artery wall, thereby improving coronary blood flow.
✓ Atherectomy is a surgical procedure used to remove plaque deposited in an artery. In this procedure, a small cutting device, blade, laser or drill is attached to a catheter and inserted into the artery and with its help, the plaque is cut and the plaque is removed, thereby increasing coronary blood flow. Methods like directional, rotational, laser are used in atherectomy.
✓ Coronary stent A coronary stent is a small mesh-like tube or artificial support device made of metal or polymer. The stent is inserted into a narrowed or blocked coronary artery with a balloon catheter and placed in the correct position. The balloon is then inflated and the stent is expanded. Once the stent is expanded, the balloon is deflated and removed, and the stent is permanently placed to keep the coronary artery open.
✓ Transmyocardial laser revascularization (TMR)
Transmyocardial laser revascularization is a surgical procedure used to relieve severe angina caused by advanced coronary artery disease. In this procedure, a special CO2 laser is used to create small channels in the heart muscle, which increases blood flow to the heart. This method is not used today.
b) Describe sickle cell anemia. (04)
sickle cell anemia
- Sickle cell anemia is also known as ‘sickle cell disease’.
- Sickle cell anemia is an inherited blood disorder in which red blood cells are sickle shaped, meaning they are sickle or crescent shaped.
- These sickle-shaped red blood cells stick to the blood vessels and block the blood vessels.
- In sickle cell anemia, abnormal hemoglobin production is seen. Which is known as hemoglobin S.
- This hemoglobin sticks to each other after delivering oxygen to the body tissues and forms clumps.
- Due to this clumping, the red blood cells become stiff and their shape looks like a sickle and these sickle-shaped red blood cells stick to the blood vessels and block the blood vessels.
causes of sickle cell anemia
- Sickle cell anemia is an inherited disorder. Hence, when one copy of the sickle cell gene is inherited from both the parents, i.e., a total of two, then the condition of sickle cell anemia is seen.
- If a person has only one copy of the sickle cell gene, then he does not have the condition of sickle cell anemia. But such people pass the sickle cell gene to their children.
- Thus, for sickle cell anemia to occur, one copy of the sickle cell gene must be inherited from both parents.
- If both parents have one normal gene and one abnormal gene, then their children have a 25% chance of inheriting both normal genes, a 50% chance of inheriting one normal and one abnormal gene, and a 25% chance of inheriting both abnormal genes.
sign and symptoms of sickle cell anemia
Chronic anemia: Sickle-shaped red blood cells break down rapidly, leading to a condition called anemia. This can cause fatigue and weakness.
Episodes of pain: Recurrent episodes of pain are known as ‘sickle cell crises’. Sickle red blood cells cause blockage in blood flow, causing severe pain. These crises are mainly seen in the chest, abdomen and joints.
Swelling of hands and feet (dactylitis): Painful swelling of the hands and feet is seen. This is the first sign seen in infants and young children.
Delayed growth and development: Growth and development delays are seen in children with sickle cell anemia.
Jaundice: Due to increased breakdown of red blood cells, the level of bilirubin in the body increases, due to which the skin, sclera, and mucous membranes appear yellow.
Vision problems: Blood vessels in the eye are damaged, due to which vision issues are seen.
Acute Chest Syndrome: Acute chest syndrome is seen in the condition of sickle cell anemia. In which conditions like chest pain, breathing difficulty, fever, visible lung infiltrate are seen.
Stroke: Stroke condition is seen due to blood flow blockage in the brain.
Priapism: Painful prolonged erection is seen.
Leg ulcer: Chronic, non-healing sore is seen on the leg.
Organ damage: Due to repeated blood flow blockage, organ damage like spleen, liver, kidney and heart occurs.
diagnostic evaluation of sickle cell anemia
- History Collection
- Physical Examination
- Complete Blood Count
- Peripheral Blood Smear
- Hemoglobin Electrophoresis
- Reticulocytes
- Bilirubin Level
- Serum Iron Level
- Genetic Testing
Management of Sickle Cell Anemia
Hydroxyurea: Hydroxyurea stimulates the production of fetal hemoglobin and helps reduce the frequency of pain episodes and acute chest syndrome.
Pain Management: Use nonsteroidal anti-inflammatory drugs and opioid drugs to control pain episodes.
Blood Transfusion: Blood transfusion is done in conditions with severe anemia, acute chest syndrome, and stroke.
Bone marrow transplantation: Bone marrow transplantation is performed to potentially cure sickle cell anemia. In which the faulty bone marrow is replaced with bone marrow from a healthy donor.
Antibiotics: Penicillin is given prophylactically to prevent infection in children with sickle cell anemia. Because such children are prone to infections caused by the bacteria Streptococcus pneumoniae.
OR
a) Describe eye bank. (08)
An eye bank is a medical organization where the cornea is removed from the eye of a person immediately after death and stored, and then transplanted into people with corneal defects.
Objectives:
- To collect eyes from donors after death.
- To determine the suitability by examining the quality of the cornea.
- To preserve the donated eyes in a suitable medium.
- To make corneas available to needy patients.
- To create awareness among the people about eye donation.
- To train medical personnel in eye removal and preservation.
Functions of Eye Bank:
- To examine the donated eyes.
- To preserve the cornea.
- To conduct lab tests of the cornea.
- To match the tissue with the recipient.
- To provide information through public awareness programs.
Main Functions:
- Collect donated eyes within 6-8 hours.
- Examine cornea and perform laboratory tests (for HIV, Hepatitis etc.).
- Preserve cornea in MK medium, Cornisol etc.
- Maintain proper documentation and donor register.
- Send cornea to eligible patients and licensed doctors.
- Conduct awareness programs in schools, colleges and communities.
- Preservation Methods of Cornea:
- MK Medium 3–4 days
- Cornisol / Optisol-GS 10–14 days
- Glycerin method: Long term preservation (for research)
Eligibility for Donation:
- A person of any age and gender can donate.
- Eye removal is necessary within 6 hours after death.
- Donors with diseases like cancer, HIV, hepatitis are considered unsuitable.
Role of Nurse:
- To convince the patient’s family for eye donation.
- To support the medical team in eye removal.
- To assist in eye removal by maintaining aseptic technique.
- To help maintain necessary documents and records.
- To participate in awareness programs about donation.
Importance:
- People with corneal blindness regain their sight.
- Helps in reducing blindness in developing countries like India.
- Promotes humanitarian values.
- Useful in the field of medical research and education.
b) Explain blindness control programme. (04)
- India is the first country in the world to launch a National Level Blindness Control Programme.
- The National Programme for Control of Blindness was launched in the year 1976. It is a 100% centrally sponsored programme.
- The Trachoma Control Programme was started in the year 1963 and was merged with the NPCB Programme in the year 1976.
- Causes of blindness are as follows: Cataract (62%), Refractive error (20%), Glaucoma (6%), Posterior segment disorder (5%), Posterior capsular opacification (1%), Corneal blindness (1%), Surgical complications (1%) and Other causes (4%)
Goal: To reduce the prevalence of blindness from 1.4% to 0.3% by the year 2020.
Objective:
- To reduce the prevalence of blindness and vision impairment. To reduce the backlog of blindness through identification and treatment of blindness.
- To develop comprehensive eye care facilities in all districts.
- To develop human resources for providing eye care services.
- To increase awareness in the community for eye care.
- To improve the quality of delivery services.
- To secure the participation of voluntary organizations and private practitioners for eye care.
- To expand research for the prevention of blindness and visual impairment.
Activities under NPCB program
- Cataract Operation
- Involvement of NGOs
- IEC Activity
- Management Information System
School Eye Screening Program
- Collection and Utilization of Donated Eyes
- Control of Vitamin A Deficiency
- Monitoring and Evaluation by Survey
- Strategies of NPCB program
- Promoting free cataract surgery through NGOs and private sector
- Making the program comprehensive by including other eye diseases besides cataract. Such as glaucoma, retinopathy
- Screening people above 50 years of age for cataract.
- Screening children for refractive error and providing them with free eye glasses.
- Cover underserved areas.
- Build capacity among eye care providers.
- Conduct activities through IEC to create awareness about eye care in the community.
- Strengthen the district hospital by upgrading its infrastructure, contractual staff and funds.
- Establish vision centers in all PHC centers.
- Create multipurpose district mobile ophthalmic units to improve coverage.
Components of NPCB program:
- Eye Care Service
- Preventive Measures
- Infrastructure Development
- Human Resources Development
- Supply of Essential Drugs and Equipment
- Data Collection and Monitoring
- Partnership and Collaboration
Q-3 Write short answer(Any two) 6+6 = 12
a) Explain osteoarthritis
Osteoarthritis
Osteoarthritis is a chronic, degenerative and slowly progressive disorder that causes deterioration of articular cartilage. Osteoarthritis mainly affects the hip bone and knee bone. Osteoarthritis is also called degenerative joint disease. It is a slow, progressive, non-inflammatory disorder that mainly affects mobile joints and particularly articulation joints.
Osteoarthritis is caused by the breakdown of the cartilage around the joint.
Types of Osteoarthritis:
1) Primary Osteoarthritis:
Primary Osteoarthritis is seen in elderly people and mainly in women.
Osteoarthritis is seen due to trauma, hereditary, obesity, age etc.
2) Secondary Osteoarthritis:
Secondary osteoarthritis is seen at any age. It is mainly seen due to any previous injury, repeated strain or sprain, joint dislocation, fracture, inflammation, congenital dislocation of hip, Disorder of nervous system, Use of corticosteroids etc.
Etiology:
- More common in women due to older age,
- Genetic factors,
- Excessive weight,
- Obesity,
- Septic arthritis,
- Trauma,
- Strenuous and repetitive exercise,
- Joint injury,
- Decreased estrogen levels.
- Caused by increased parathyroid hormone.
- Caused by metabolic diseases such as diabetes, gout, and other hormonal disorders.
Clinical manifestation/ sign and symptoms:
- Joint pain,
- Joint stiffness,
- Pain increases with activity and decreases with rest.
- Joint stiffness in the morning.
- Paresthesia (tingling and numbness sensation),
- Swelling,
- Muscle weakness,
- Bony deformity,
- Joint swelling (warmth, effusion, synovial thickening).
- Joint tenderness and soreness.
- Back pain.
- Reduced joint flexibility.
- Reduced range of motion in the affected joint.
- Cracking (a sound caused by friction between two bones).
- Swelling in the bone.
- Grating sensation.
Diagnostic evaluation:
- History taking and physical examination
- X-ray,
- CT scan,
- MRI,
- Blood test,
- Analysis of synovial fluid,
- Erythrocyte sedimentation rate ( ESR Test),
- Radionuclide imaging.
Management of Osteoarthritis:
- If the patient is in pain, provide analgesic medicine.
- Ex: acetaminophen
- Provide medicine to relieve inflammation and pain.
- Ex: = NSAID ( Non steroidal anti inflammatory drug),
- Ibruprofen,
- Naproxen.
- Tramadol.
- Cox 2 inhibitor drug.etc.
- To reduce stress on the joints, reduce proper weight.
- To do proper exercise, exercise causes joint movement and muscle strengthening of the muscles that are around the joints.
- Simple exercises like swimming and walking, i.e. doing them on a flat surface, are less stressful on the joints.
- To tell the patient to take proper nutrition, get proper sleep and reduce stress, due to which well-being improves.
- To tell the obese patient to reduce weight.
- Due to weight loss, stress on the knee joint, hip joint and spine is reduced and due to this, pain is also relieved.
- When the patient’s pain level increases excessively, it is also necessary to manage the patient surgically.
- Use supportive devices such as splints, shoes, due to which the pain level decreases.
- Use supportive assistive devices, due to which the pressure on the joint is reduced and it is mainly used to stabilize the ligament and reduce the pain level.
- Glucosamine and chondroitin: This is mainly used to reduce pain in a person who has a condition of osteoarthritis.
Provide hot and cold applications to the patient.
- Providing hot therapy reduces joint stiffness and it should be provided mainly two to three times throughout the day.
- Cold therapy is mainly used to reduce swelling and cold applications should not be applied for more than 20 minutes.
Surgical management of Osteoarthritis:
1)Osteotomy:
In osteotomy, the bone is cut from above and below and the weight is reduced, which reduces the pain level.
2) Joint fusion:
In joint fusion, the damaged joint is removed and the two bones are fused and this is mainly done in places where joint replacement is not effective.
3)Arthroscopy:
In arthroscopy, the damaged cartilage is cleaned and the tissues are repaired.
4)Joint replacement:
In joint replacement, the surgeon removes the damaged joint surface and replaces it with a plastic or metal device called a prosthesis.
Nursing management:
- Assess the patient’s pain level.
- Measure the location and intensity of the patient’s pain using a pain scale.
- Provide the patient with hot or cold applications.
- Instruct the patient to change positions frequently and to assume a comfortable position.
- Instruct the patient to take complete rest.
- Instruct the patient to take the prescribed analgesic medicine.
- Provide the patient with a comfortable mattress, pillow, and proper rest.
- Instruct the patient to maintain good body mechanics while walking, sitting, moving, or lifting anything.
- Ask the patient to use devices such as splints, braces, traction, etc. properly.
- Ask the patient to adopt stress management techniques.
- Provide education to the patient to reduce activities that increase the pain level.
- Provide education to the patient to maintain correct posture and body mechanics.
- Ask the patient to roll a towel and then rest it at neck level.
- Ask the patient to reduce weight.
- Advise the patient to do range of motion exercises.
- Provide education to the patient to get adequate rest, sleep, and nutrition.
- Check the patient for inflammation at the joint site.
- Assess the patient’s range of motion of the affected joint.
- Ask the patient to do range of motion exercises.
- Provide the patient with a safe environment, for example, raise the chair, use high grip and tub and toilet, the use of mobility aids/wheelchair rescue.
- Provide assistance to the patient in active and passive exercises.
- Ask the patient to do early ambulation by use of assisting device like crutches, walker and canes.
- Provide education to the patient to do exercises.
- Ask the patient to use assistive devices.
- Ask the patient to maintain a comfortable position.
- Ask the patient to maintain proper posture.
- Ask the patient to lose weight if he is obese.
- Ask the patient to take the prescribed medicine.
- Advise the patient to make lifestyle modifications.
b) Explain radiotherapy
Introduction:
Ionizing radiation is used in radiation therapy. Ionizing radiation is used to destroy the genetic material of abnormal cancerous cells. This radiation is used to prevent abnormal cellular growth. This radiation therapy damages cancerous cells and causes them to necrosis.
Radiation therapy is used to stop cell growth. It is also a type of cancer treatment that uses high doses of radiation to kill cancer cells and shrink tumors.
Purpose:
1Primary: Primary purpose is only for the treatment and cure of cancer.
- Adjuvant: This is used only in pre-operative and post-operative conditions and is used with chemotherapy.
- Palliative: This is used when there is any emergency condition. Such as, superior vena cava compression and spinal cord compression etc.
4) Prophylactic purpose: This radiation therapy is given only in the suspected area.
Action of Radiation therapy:
1) Normal cell: Radiation therapy affects normal cells but normal cells have the capacity to grow back. Therefore, normal cells do not suffer from problems due to radiation therapy.
2) Abnormal cell: X-rays and gamma rays destroy the genes of cancerous cells and prevent them from growing.
(Types of Radiation Therapy)types of Radiation Therapy:
1)external beam radiation therapy (tele therapy)(External beam radiation therapy- Tele therapy)
2)Internal radiotherapy (brachytherapy) (Internal radio therapy- Brachy therapy)
▲ 1)external beam radiation therapy ( (External beam radiation therapy-tele therapy-Tele therapy):=
In this therapy, radiation is applied to the cancerous cells using a machine using X-rays (x-rays) and gamma rays (γ -Rays).
The main advantage of this is that this therapy affects the maximum depth of the cell and does not affect the surface area, so this radiation therapy is very beneficial.
External beam radiation therapy is used for skin lymphoma, breast, colorectal, It is used to treat various types of cancer including skin lymphoma, breast, colorectal, esophageal, and head, neck, lung, brain tumor, and prostate cancers.
▲ 2) Internal Beam Radiation Therapy – (Internal Beam Radiation Therapy: brachytherapy)
In this therapy, a radioisotope is implanted directly inside the cell. So that the abnormal cell is destroyed. Brachytherapy is a type of internal radiation that is used for the treatment of head and neck, breast, cervix, prostate and eye cancer. In this, seeds, ribbons and capsules are used.
There are mainly two types of it which are as follows.
► A) Shield:-In this type, the radiation is implanted through a needle tube and applicator.
► B) Unshield:- In this type, the radiation is implanted through a tablet or injection. Thus, there are two types of radiation therapy.
Safety Standard of Radiation Therapy:
Distance: When providing radiation therapy, the health care personnel should stay away from the patient’s bed. It is not necessary to stand near the patient’s bed continuously while providing radiation therapy.
Time:
When providing radiation therapy to the patient, the patient can work next to the patient for a maximum of 30 minutes.
Shield: When providing radiation therapy, health care personnel should use a protective shield and cover all parts of the body.
When providing radiation therapy, health care personnel should use a dosimeter that determines the dose of radiation. A separate private room should be kept for health care personnel. In which they can wear personal protective equipment.
Children and pregnant women should be kept away from the area when providing radiation therapy.
☆ Side effects of radiation therapy:-
- Vomiting,
- Nausea,
- Diarrhea,
- dysphagia (difficulty in swallowing),
- Fatigue,
- weakness,
- xerostomia (dryness of mouth),
- stometitis (inflammation of mucous membrane of mouth),
- loss of appetite
- increased risk of infection
- alopecia (hair loss)
- body ache,
- leukopenia
- impaired skin integrity,
- anemia,etc.
☆ Nursing management of radiation therapy :-
- Inform the patient that the skin area should be covered.
- Explain the procedure to the patient
- Tell the patient about the equipment needed for the procedure and the duration of the procedure.
- Tell the patient and their relatives that when radiation therapy is being given, all persons other than the patient should stay away from the area.
- Tell the patient that young children and pregnant women should stay away from the area where the radiation is being given.
- Educate the patient to eat small meals and give the patient antidiarrheal medicine.
- Insert the patient’s urinary catheter so that the bladder can be emptied properly.
- Inform the patient not to use any type of oil or emollient.
- Tell the patient not to go out in the sun.
- Maintain proper oral hygiene.
- Communicate with the patient and his/her relatives or by telephone.
- If the patient has oral cancer, do not brush too vigorously, but maintain oral hygiene by taking it easy.
- Maintain the patient’s hydration status.
- Maintain the patient’s nutritional status.
- Tell the patient to keep the cancerous area covered as much as possible.
- Answer all the questions of the patient and his/her relatives correctly.
- Tell the patient to be careful not to injure any part of the body as much as possible.
- Tell the patient that hair loss on the head is common while undergoing radiation therapy, so the hair grows back, so there is no need for the patient to be discouraged.
- Provide psychological support to the patient.
- Tell the patient to do his daily routine activities in small amounts.
- Provide the patient with different types of recreation therapy and mind diversion therapy.
- Maintain good communication habits with the patient.
- Thus, do this type of nursing management while giving radiation therapy.
c) Explain chemotherapy –
- Chemotherapy is a therapy to kill abnormal cancer cells in a cancer tumor in the body. Chemotherapy is a treatment to destroy cancer cells with chemical agents.
- This chemical agent is a treatment to prevent the reproduction and cellular function of abnormal cancer cells by disturbing them and preventing them from multiplying and spreading from one place to another.
- This therapy is sometimes used along with radiation therapy.
- This therapy is specifically given to reduce the size of the tumor before surgery.
- This therapy first affects the cancer cells that have spread throughout the system in every part of the body and finally acts to reduce its size in the main place where the cancer is located.
- The chemical agents given in this therapy are very important in destroying specific malignant cancer cells and using this agent in combination with other agents gives very effective results.
Detailed information about chemotherapy (Chemotherapy in Detail):
How chemotherapy works (How Chemotherapy Works):
Chemotherapy treatment is given in the body through injection or oral medicine. This treatment spreads throughout the body through the blood circulation and destroys fast-growing cancer cells. Chemotherapy effectively reduces the size of the cancer tumor and destroys cells that have spread to other parts.
Different types of chemotherapy (Types of Chemotherapy):
1.Adjuvant Therapy:
- It is given after surgery to remove the main tumor, so that the remaining cancer cells are destroyed.
2.Neoadjuvant Therapy:
- It is given before surgery, so that the size of the tumor is reduced and it becomes easier to remove it.
3.Metastatic Therapy:
- This method is used when the cancer has spread, which destroys the tumor and prevents its spread.
Chemotherapy Treatment (Chemotherapy Drugs): Several types of treatment are used for chemotherapy. Some of the common treatments include cyclophosphamide, methotrexate, doxorubicin, and paclitaxel. Treatment is given alone or as a combination therapy.
Side Effects of Chemotherapy: Chemotherapy treatment is very powerful and it destroys rapidly growing cells. This can cause some side effects, such as:
- Myelo suppression: Most chemotherapy drugs suppress the bone marrow, which reduces the production of blood cells.
- Fatigue: The cause of this is unknown, but anemia, weight loss, and sleep patterns are seen due to disturbed sleep patterns.
- Nausea and vomiting: These are the most common side effects
- Mouth infection occurs due to cytotoxic drugs, which is called stomatitis.
- Cardio toxicity
- Alopecia, which means hair loss. Changes in taste and smell are seen.
- Leukemia
- Skin changes: In which hyperpigmentation, infection, disheveled nail coloration, ulcers, and photosensitivity are seen.
- Pulmonary toxicity
- Diarrhea and constipation, loss of appetite.
- Renal toxicity: In which nephrotoxicity and renal failure are seen.
- Neuro toxicity: In which CNS damage and peripheral nerve damage are seen.
- Testicular and ovarian function is altered.
- Weakness, fatigue, and weight loss occur.
Nursing Care of Patient During Chemotherapy:
- Nursing management of the patient during chemotherapy should be done very carefully. Which includes the following points.
- Before starting chemotherapy, it is necessary to completely review any patient. In which the description of the drug, what type of drug it is, what agent it is, what is its dosage, what is its route of administration, all this information needs to be reviewed.
- It is necessary to identify the patient who is to be given chemotherapy.
- Assessing the patient and checking his blood reports to monitor whether he has any kind of problem is very important before starting chemotherapy.
- It is especially important to review the patient’s anxiety level and psychological status. Explain all the processes to him so that his anxiety can be removed.
- After starting chemotherapy, the patient will see some side effects, which should be explained and prepared in advance.
- Chemotherapy agents are given in very specific doses and after taking all precautions.
It is necessary to take great care while preparing medicine and medicine for chemotherapy patients. - Any disposable items left after giving the dose of medicine or unused drug should be properly discarded.
- If any medicine is spilled while giving chemotherapy to the patient, it is necessary to manage the spill properly.
- It is necessary to take steps to protect the patient and the staff, for this, precautions should be taken to ensure that the medicine does not spill and does not fall on the skin.
- While preparing this chemotherapeutic agent for the patient, the staff should take complete precautions. Special care should be taken to ensure that the medicine does not come into contact with the staff through inhalation.
- After giving chemotherapy to a patient, all the details should be recorded and reported systematically. Such as the name of the chemical agent, dose, route, time, premedication, postmedication, if there is any complaint, it is necessary to document everything properly.
Post-Chemotherapy Care:
In post-chemotherapy care, it is necessary to follow the doctor’s instructions and recommendations. Improve lifestyle by maintaining methods for disease remission, exercise, and mental dignity.
Chemotherapy is a very effective and necessary treatment, which can improve the lives of cancer patients.
Q-4 Write short notes. (12)
a) Mastitis
Mastitis is an infection and inflammation of the breast tissue. It is a condition that causes pain, swelling, redness in the breast.
There are 2 types of mastitis.
1.Puerperal
2.Non-puerperal
1.Puerperal mastitis:
This occurs due to blockage or excessive milk production after pregnancy, lactation and delivery.
2.Non-puerperal
This does not occur due to pregnancy or lactation. This causes lesions on the breast.
Etiology:
Bacteria: streptococcus staphylococcus
Milk stasis- Milk collection occurs in the breast due to lack of lactation.
This is more common in the puerperal (post-delivery) period (6 weeks after delivery).
Hormonal changes: estrogen
- Progesterone
- Dead cell buildup in the milk duct
- HIV
- Diabetes
- Wearing tight-fitting clothes
- Maternal stress
- Trauma to the breast due to an accident
Clinical manifestations:
- Breast discharge
- Swelling
- Lump
- Pain
- High grade fever
- Lesion on breast
- Skin redness
- Inflammation on breast
- Tender or warm breast
- Body ache
- Malaise
- Fatigue
- Breast engorgement
- Chills
- Rigor
Management:
1.medical management
- surgical management
- nursing management
1.medical management:
Analgesic medicine:
This medicine is given for breast pain.
Eg.ibrupofen
This medicine is safe during breast feeding.
This medicine does not harm the baby either.
Antibiotic medicine:
This medicine is given to reduce the infection in the breast.
Eg.cephalexin
Erthromycine
Antipyretic medicine:
This medicine is given to cure the fever caused by the infection.
2.surgical management:
- If an abscess is found in the breast, drainage is done.
- In this, local anesthesia is given, after which the abscess accumulated in the breast is drained with needle aspiration.
- If the abscess is deep, general anesthesia is given in the operation room and a small incision is made and drained.
- And finally the abscess is treated with antibiotics.
Nursing management:
- Encourage the mother to breastfeed
- Ask the mother to breastfeed even if the affected breast is painful.
- Frequent breastfeeding can prevent engorgement in the breast and prevent the milk duct from becoming blocked.
- Apply left compression on the breast before and after breastfeeding to relieve pain.
- If left compression does not work, apply an ice pack to the breast only after breastfeeding to provide comfort and release.
- Do not use an ice pack before breastfeeding as it reduces the flow of milk.
- Encourage the mother to take pain killer medicine to reduce pain
- Instruct the patient to drink 10 glasses of water a day and eat a well-balanced diet
- Breastfeeding mothers should consume 500 extra calories a day.
- Dehydration and poor nutrition reduce milk supply, so instruct the patient to drink more water and eat a good diet
- If there is discharge from the nipple, wash the nipple gently and let it dry. Then wear clothes.
- If there is excessive discharge, ask her to use a disposable breast pad.
- This disposable breast pad absorbs the discharge.
- Ask the patient to keep cabbage leaves on the breast. As cabbage leaves help in reducing infection, change them when the cabbage leaves become dirty
- Ask the patient to massage the breast.
- Ask the patient to wear a supportive cloth (bra).
- PREVENTION:
- Breastfeed equally on both breasts.
- Empty both breasts completely while breastfeeding to prevent engorgement and blockage of the duct.
- Use good breastfeeding technique while breastfeeding to prevent soreness.
- Drink plenty of fluids to reduce dehydration.
- Rest.
- Apply gentle compression on the breast before breastfeeding.
- Maintain hygiene.
- Hand washing
- Clean the nipple
- Clean the breast
- Keep baby clean
b) Causes of burns
Thermal burns:
Thermal burns are the most common type of burn. Thermal burns are caused by contact with fire, flame, hot liquids, hot objects, and steam. The severity of thermal burns depends on the temperature of the object and the duration of exposure. Examples include residential fires and automobile accidents.
Chemical burns:
Chemical burns are caused by contact with household or industrial chemicals such as strong acids, alkalis, and organic compounds. Examples include sulfuric acid, phosphoric acid, sodium, and calcium hypochlorite. The severity of chemical burns depends on the concentration, volume, and duration of exposure of the chemical.
Electrical burns:
Electrical burns are caused by electrical energy or electrical shock. The severity of electrical burns depends on the intensity of the current and the duration of exposure. For example, electrical burns are caused by the shock of coming into contact with faulty electrical wiring. Electrical burns are difficult to diagnose because they do not show any symptoms on the skin but do show internal damage.
Radiation burns:
Radiation burns are caused by exposure to radioactive sources such as UV light, X-rays, and gamma rays. For example, nuclear bomb explosions. The severity of radiation burns depends on the strength, duration, distance, and surface area of the radiation.
Inhalation burns:
Inhalation burns are caused by exposure to asphyxiants, smoke, etc., such as carbon monoxide poisoning.
c) Bone marrow transplantation
Bone Marrow Transplantation
Introduction:
Bone Marrow Transplantation is a special medical procedure in which healthy hematopoietic stem cells are transplanted into the patient’s body, so that new and healthy blood cells can be made in the patient’s bone marrow. This therapy is especially used for hematological disorders such as leukemia, lymphoma, aplastic anemia and some metabolic or immune deficiency diseases.
What is bone marrow?:
Bone marrow is the soft, spongy tissue that is found inside our long bones and from which blood cells – such as red blood cells, white blood cells and platelets – are made.
Types of Bone Marrow Transplantation:
1.Autologous Transplantation:
The patient’s own healthy stem cells are taken beforehand and then injected back into the patient’s body after chemotherapy or radiation therapy.
- Allogeneic Transplantation:
Stem cells from another person – usually a relative or a perfectly matched donor – are transferred to the patient.
- Syngeneic Transplantation:
A transplant of stem cells from an identical twin who has the same genes.
Procedure:
The patient is first given high-dose chemotherapy or radiation therapy to kill damaged or cancerous cells.
Healthy stem cells are then transferred intravenously into the patient’s body – much like a blood transfusion.
The stem cells then travel to the bone marrow and begin making new blood cells. This process is called engraftment.
Complications and Risks:
Graft-versus-host disease (GVHD): A risk seen especially in allogeneic transplantation, in which the donor’s immune cells attack the patient’s body as if it were a foreign body.
Infection, bleeding, organ damage, and immune dysfunction are also possible.
Likelihood of Success:
Success depends on many factors such as the patient’s age, the type and stage of the disease, and the patient’s general health before the transplant. If the transplant is done at the right time and with the right donor, sometimes the patient can be perfectly healthy.
Bone Marrow Transplantation is a life-saving and life-changing therapy that is especially given in severe hematological diseases. For its success, proper diagnosis, timely treatment and continuous monitoring are very important.
Nursing management :
Prepare the patient physically and psychologically.
Explain the procedure to the patient and his family members.
Tell the patient and his family members about its risks, benefits and return consent.
Keep the patient isolated.
Restrict entry to visitors.
See if the patient has any side effects of chemotherapy and radiotherapy during this time.
See the patient’s intravascular output.
Check the patient’s vital signs.
Administer i.v. fluid to the patient.
Maintain strict aseptic technique.
To administer prescribed medicine blood components.
To provide psychological support to the patient.
To tell the patient and his family members about coping abilities.
To dress the central line properly after bone marrow transplantation.
To see if there is any kind of infection after bone marrow transplantation.
To tell the patient and his family members about regular follow-up.
complications :
-> Hematopoietic : Infection, nosocomial infection, Anemia.
->Gastrointestinal Tract : Nausea, Vomiting, Diarrhea.
-> Renal and Genitourinary: Renal failure, Hemorrhagic Cystitis,
–> Hepatic: Hepatomegaly, Bilirubinemia, Coagulopathy disorder.
-> Pulmonary : Bacterial Pneumonia, Fungal infection, TB toxoplasmosis, Pulmonary, fibrosis.
d) Types of fracture
1) complete
2) Incomplete
3) communicated fracture
4) open fracture
5) closed fracture
According to anatomical placement of fragments
1) Avulsion
2) Compression
3) Depressed
4) Compound
5) Epiphysial
6) Green steak
7) Impacted
8) Oblique
9) Transverse
10) Pathological
11) simple
12) Spiral
13) Stress
☆ 1) Complete: In a complete fracture, the bone is The entire continuity breaks and the bone divides into two parts, and the bone breaks into two parts from the middle, which is called a complete fracture.
☆2) Incomplete fracture: In this, the bone does not break down completely, it breaks in the cross section, so it breaks only in some parts, it does not divide into two parts completely, which is called an incomplete fracture.
☆ 3) Communicated fracture: In this, the bone breaks into small parts and remains spread in the same place. Small parts of the bone break but remain in the same place, which is called a communicated fracture.
☆ 4) Open fracture: In this, the bone breaks down in such a way that the skin is also involved. The bone also breaks down the skin and damages the mucous membrane.
There are three grades of open fractures.
- 1) Grade 1
- 2) Grade 2
- 3) Grade 3
☆-> Grade 1: In this, the wound is clean and the fracture is smaller than one centimeter.
☆-> Grade 2: In this, the wound is large and the soft tissue is not damaged to a large extent.
☆-> Grade 3: In this, the wound is very contaminated and the soft tissue is also injured.
☆5) Closed fracture: In this, the bone breaks but the skin remains intact. The bone breaks inside the skin.
According to anatomical placement or fragments:
1) Avulsion fracture: In this, there are tendons and ligaments around the bone. Due to the stretching of these tendons and ligaments, the bone also comes outwards, so a small part of the bone breaks.
2) Compression fracture: In which the bone is compressed and the bone breaks down, it is called a compression fracture.
3) Compound fracture: In the fracture, there is also involvement of the skin and mucous membrane along with the bone.
4) Depressed fracture: This is mostly seen in the skull bone, in which the bone is pushed inwards.
5) Epiphysial fracture: In this, the epiphysial, that is, the last part of the bone breaks down.
6) Green steak fracture: In this, the bone breaks from one side and the bone bends on the other side.
7) Oblique fracture: In this, the ball breaks down horizontally.
8) Transverse fracture: In this, the bone breaks down transversely.
9) Impacted fracture: In this, the bone fragment enters another bone.
10)Pathological: In this, the bone breaks down from the diseased side, which is called a bone tumor.
11)Simple fracture: In this, the bone breaks down and it is only in its area, the skin does not break down
12)Spiral: In this, the bone breaks down from the middle part, which is called a spiral fracture.
13)Stress: In this, stress is repeatedly applied to the bone and the bone and muscles do not recover and if the bone breaks down, it is called a stress fracture.
14) Impacted: When one bone pushes heavily on another bone, it is called an impacted fracture.
Q-5 Define following (any six) – (12)
a)Neoplasia
Neoplasia is a pathological process in which cells of the body begin to divide irregularly and uncontrollably, ignoring their normal growth process. This division results in the formation of new and abnormal masses of tissue called neoplasms.
Neoplasms or tumors can be of two types: Benign – which are usually harmless and do not spread to other organs, and Malignant – which can become cancerous and can spread to surrounding tissues and distant organs through metastasis. Neoplasia is caused by genetic or epigenetic changes in the control mechanisms of normal cells. This process is especially important in oncology – the study of cancer.
b) Phlebotomy
Phlebotomy is a medical procedure in which an opening is made in a vein. In which a needle is inserted into the vein and blood is removed.
This procedure is mainly done for diagnostic purposes, treatment (therapeutic purposes), blood donation, or blood collection.
- It is also called venipuncture in another language.
- In this, blood is removed using a needle.
- This procedure is used to diagnose and treat many medical conditions.
There are two types: vein puncture and capillary puncture
c) Subluxation
Subluxation is a medical condition in which the connection between a joint or bone is not completely severed, but the bone is slightly displaced from its normal anatomical position, which is called Partial Dislocation. Subluxation usually occurs due to accidents, ligament sprains, muscular weakness, neurological conditions, or congenital defects. In this condition, the patient may experience symptoms such as pain, swelling, restricted movement, and muscle spasm in the joint. Subluxation can occur in any joint such as the shoulder joint, knee joint, elbow joint, or vertebral column. Medical imaging techniques such as X-ray, MRI, or CT scan are used to diagnose this condition. Timely and proper management of subluxation is necessary because if it is not treated properly, problems such as chronic pain, joint instability, or degenerative changes can arise.
OR
Subluxation is an abnormal condition of a joint in which a bone moves partially out of place, but does not completely separate. This condition is also called partial dislocation.
In simple terms, when one of the two bones in a joint moves slightly from its original position, but does not break, it is called subluxation.
d) Blepharitis
Blepharitis: Blepharitis is an inflammation of the eyelids, which also involves the eyelashes. When blepharitis occurs, the oil glands near the eyelids swell. Symptoms include dry eyes, burning, itching, and swelling of the eyelids.
E) Aneurysm
Aneurysm is a dilation and formation of a sac in the wall of an artery or vein where there is a weak point. And it is a bulging like formation in the wall of the vessels. This bulging also occurs in the aorta because there is a high amount of blood pressure there.
Classification: 1) Fusi form: In this type, the entire wall of the vessels forms a bulge.
2) Saccular: In this type, the wall of the vessels forms a sac like formation. In this, there is no involution of the entire wall.
3) Dissecting: In this, there are three walls of the vessels.
1) Tunica intima 2) Tunica media 3) Tunica albuginea . Dilation of one wall occurs.
4) According to cause:
1 ) true
In this, bulging formation occurs due to long-term disease in the artery such as
1) Hypertension
2) Arteriosclerosis.
2) false:
In this, bulging formation occurs when there is trauma to the wall of the artery. It is also called pseudo aneurysm.
f ) Gynecomastia
Gynecomastia is a medical condition in which there is enlargement of breast tissue in males. And there is enlargement of the male breast. Gynecomastia is usually seen due to hormonal imbalance i.e. imbalance of estrogen and testosterone hormones. In which the level of estrogen increases compared to testosterone. Gynecomastia is usually seen in higher amounts during infancy and puberty.
Pseudogynecomastia: Pseudogynecomastia is enlargement of the male breast but it is usually due to fat deposits.
Synonyms of pseudogynecomastia are also called adipomastia and lipomastia.
g) Burns
Burn injuries occur due to direct contact with thermal, chemical, electrical and radiation. Injuries to the skin and tissues caused by contact with hot liquids, hot objects, streams, fire, sun, electricity and chemicals are known as ‘burn injuries’. Burn injuries occur due to the transfer of heat energy to the body as a heat resource. This heat is transferred through conduction and radiation. Human skin can tolerate temperatures up to 42-44 c. But when exposed to temperatures higher than this temperature, tissue destruction occurs. Burn injuries are a major global public health problem and have a physical, psychological, and financial impact on people. Most burns occur accidentally. Burn injuries occur in people of all ages and all socioeconomic groups.
OR
Burns are injuries to the skin and/or internal parts of the body caused by contact with hot objects or chemicals.
h) Entropion
Entropion is an ophthalmological condition in which the eyelid, especially the lower eyelid, turns inward, causing the eyelashes and skin to rub against the transparent front surface of the eye, the cornea and conjunctiva, causing problems such as constant irritation, redness, watering, pain, and sometimes infection. This condition is usually caused by muscle weakness of the eyelid tissue in aging, skin laxity, trauma, or past genetic or surgical effects. If left untreated for a long time, it can cause serious consequences such as corneal ulcers or vision loss. Entropion is diagnosed through clinical assessment of the eyes and treatment involves relief with lubricant eye drops, taping, or surgery to improve the condition of the eyelid.
OR
Entropion is a condition in which the eyelid margin rolls inward.
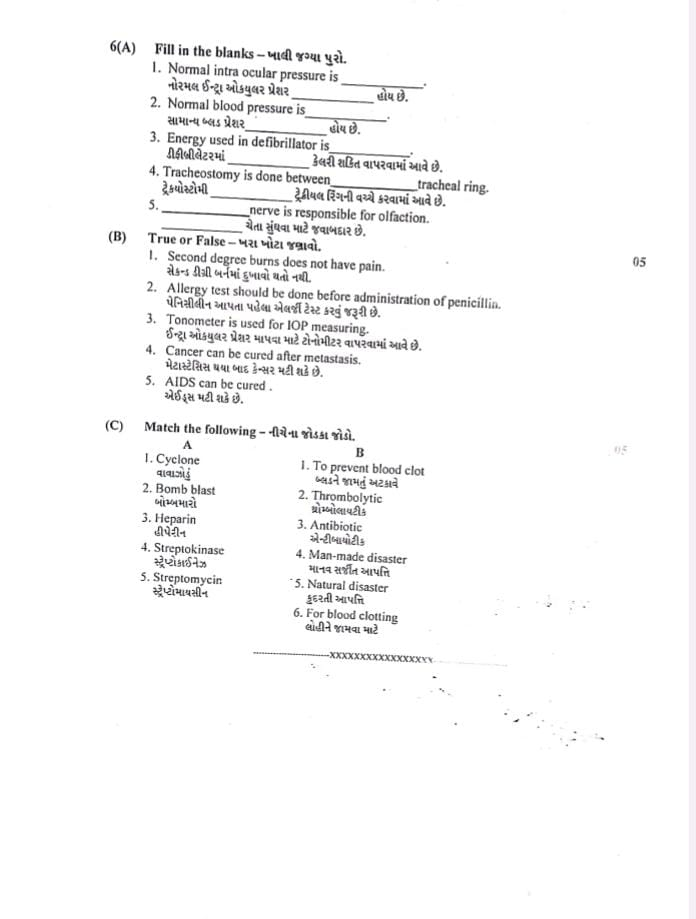
Q-6(A) Fill in the blanks(05)
1)Normal intra ocular pressure is___ .-10–21 mmHg
2) Normal blood pressure is____ .- 120/80 mmHg
3) Energy used in defibrillator is ____ . – 200–360 joules
4) Tracheostomy is done between _____ tracheal ring. – between 2nd and 3rd tracheal ring
5) ____ nerve is responsible for olfaction.– Olfactory nerve (Cranial Nerve I)
Q-6B)True or False (05)
1.Second degree burns does not have pain. – ❌ False – It is painful due to nerve exposure.
2.Allergy test should be done before administration of penicillia. -✅ True – Due to risk of anaphylaxis.
3.Tonometer is used for IOP measuring. – ✅ True – It measures intraocular pressure.
4.Cancer can be cured after metastasis. ❌ False – After metastasis, it is usually not curable.
5.AIDS can be cured. .-❌ False – AIDS has no cure, only management.
Q-6C) Match the following .(05)
A B
1.Cyclone 1.To prevent blood clot
2.Bomb blast2.Thrombolytic
3.Heparin3.Antibiotic
4.Streptokinase સ્ટ્રેપ્ટોકાઇનેઝ 4.Man-made disaster
5.Streptomycin 5.Natural disaster
6.For blood clotting
Answer
A (Terms) B (Matches)(Answer)
1.Cyclone 5.Natural disaster
2.Bomb blast 4.Man-made disaster
3.Heparin 1.To prevent blood clot
4.Streptokinase 2.Thrombolytic
5.Streptomycin 3.Antibiotic
