ENGLISH-FON:UNIT-6 -THERAPEUTIC NURSING CARE-PART-1(CARE OF PATIENTS WITH RESPIRATORY PROBLEMS/DYSPNEA)-UPLOAD
Therapeutic Nursing Care:

Part : 1 Care of the patient with Respiratory problem/ Dyspnea (Care of the patient with Respiratory problem/ Dyspnea).

Key terms :
Define/Explain Dyspnea/Shortness of breath

Dyspnea is a condition of difficulty in breathing or discomfort, in which a person experiences shortness of breath, rapid breathing, tightness in the chest, or increased effort to breathe. This condition can be caused by many problems such as the lungs, heart, circulatory system, anemia, or anxiety. Evaluation of dyspnea depends on the severity of symptoms and the underlying cause, so that appropriate treatment can be given.
Define sinusitis

Infection and inflammation of the sinuses is known as sinusitis. Sinuses are air-filled cavities located in the face and skull.
Explain / Define adenoiditis

Adenoids (which are small masses of tissue located behind the nasal cavity, near the throat). Their infection or inflammation is called adenoiditis. Adenoids are part of the immune system and help trap bacteria and viruses that enter the body through the nose. Adenoiditis in children is usually caused by bacterial and viral infections. It is characterized by abnormal growth of lymph nodes and their growth occurs in the nasopharynx. Tonsils and adenoids are lymphoid structures and are mainly located in the oropharynx and nasopharynx. They are at their full size in childhood and become smaller as we move into adulthood.
Explain /Define Laryngitis (डीफिन लारिंगीतिस )

Infection and inflammation of the larynx (voice box) is known as Laryngitis. The larynx is situated in the upper part of the respiratory tract, and its infection and inflammation is called laryngitis. It also causes hoarseness of voice and speech problems.
Explain/ Define pharyngitis

Infection and inflammation of the pharynx is known as pharyngitis. Also known as ‘sore throat’. Pharyngitis is an infection and inflammation of the pharynx, which is located at the bottom of the mouth. This is caused by certain types of viruses and bacteria that enter the pharynx due to a cold, flu or sinus infection and cause the condition of pharyngitis.
Explain/Define Tonsillitis (Define Tonsillitis)

Infection and inflammation of the tonsils is known as Tonsillitis. Which is seen due to bacterial and viral infections. (Tonsils are Small mass of tissue located on the side of the throat that filters and kills foreign bodies that enter through the nose and mouth.
Explain/Define Allergic Rhinitis

Allergic rhinitis is the inflammation of the nasal mucosa caused by an allergen substance, which is called Allergic Rhinitis. Inflammation of the mucous membrane in the nasal cavity due to an allergen substance is called Allergic Rhinitis. Allergic rhinitis is called Type 1 Hypersensitivity reaction.
Explain/ Define deviated nasal septum

The septum between the nostrils, which is normally thin and straight, deviates and protrudes from the midline, causing nasal obstruction and breathing difficulty. The nasal septum, which is normally thin and straight and is located between the two nostrils, deviates from its place and bends inward or to one side in the nostril, and is called a deviated nasal septum. Deviated nasal septum is a common physical disorder in which the nasal septum of the nose is displaced. The septum mainly separates the right and left nasal cavities and is located in the middle and divides the nose equally into two parts. Deviated nasal septum causes nasal obstruction and this can be more common in infections or allergic reactions. When obstruction occurs, breathing through the nose becomes difficult. This is mainly seen in children and is mainly congenital and can also be seen due to any injury.
Explain/Define Common cold

Common cold is an acute viral contagious infection that creates inflammation in the mucous membrane of the nose. It occurs in the upper respiratory tract and is caused by rhinovirus, picovirus or coronavirus etc. Common cold is an average one A mild cold lasts for two to three (2 to 3) days. Severe cold lasts for two weeks.
Transmission of infection: Common cold is spread by direct hand-to-hand contact with infected secretions or from a contaminated surface. For example, if a person with common cold touches their nose and then touches something else, the common cold virus may be on that surface. Now, if someone else touches that surface, they are at risk of getting common cold. In addition, the common cold virus can survive on surfaces such as pens, books, telephones, computer keyboards, and coffee cups for a few hours.
Explain / Define epistaxis

Epistaxis means nose bleed or nasal hemorrhage Bleeding from the nostrils or nasal cavity due to rupture of vessels in any area of the mucous membrane in the nose is known as epistaxis. Epistaxis is also called nose bleed. This is a condition in which active bleeding occurs from the nostrils, nasal cavity or nasopharynx. This occurs when the blood vessels inside the nose are damaged or injured. Bleeding from the front or back of the nose is called nose bleed or epistaxis.
Explain/ Define peritonsillar absess

A peritonsillar abscess is a complication of tonsillitis in which pus collects around the tonsils. That is, pus collects in the peritonsillar space. Thus, the collection of pus around the peritonsillar space is called a peritonsillar abscess.
Explain /Define bronchitis

Inflammation of the bronchi and bronchioles tubes is known as bronchitis. Bronchitis is also known as ‘blue blotter’.Bronchitis is an infection and inflammation of the bronchi of the lower respiratory tract. In bronchitis, the condition of breathing difficulties arises due to the production of mucus in the bronchi due to infection.
Explain/ Define bronchiectasis

Bronchiectasis is a chronic respiratory condition characterized by abnormal and irreversible dilation, inflammation, and thickening of the bronchi and bronchioles. As a result, mucus accumulates in it and the mucus is not cleared properly from the airways, leading to recurrent respiratory infections.
Explain /Define pulmonary tuberculosis

Pulmonary tuberculosis is a serious infection caused by the bacterium Mycobacterium tuberculosis that mainly affects the lungs but can also spread to other areas of the body. Pulmonary tuberculosis is spread through the air, that is, by coming into contact with an infected person coughing or sneezing.
Explain /Define lung abscess

In lung abscess, a pus-filled cavity is found in the lung parenchyma and inflammation and necrosis are seen in the surrounding tissue.
Explain /Define pleural effusion

Abnormal fluid collection in the pleural cavity is known as pleural effusion.
Explain/ Define pulmonary edema

Pulmonary edema is a condition in which there is an accumulation of fluid or fluid buildup around the lungs and this fluid collects in the air sacs (alveoli) causing breathing difficulties, coughing, wheezing, and feeding difficulties.
Explain /Define Empyema

Empyema is a condition in which there is an accumulation of pus in the space between the lungs and the inner surface of the chest wall (the pleural space). Abnormal collection of pus found in the pleural cavity is known as Empyema. Empyema is also known as ‘Pyothorax’ and ‘Purulent Pleuritis’. Empyema is mainly seen as a complication of pneumonia and lung abscess.
Explain/ define Emphysema

Emphysema is a Greek word meaning ‘inflation’ . Emphysema is a chronic lung disease. In which there is over-distension and over-inflation of the air sacs (alveoli) of the terminal bronchioles in the lungs and the air sacs are gradually damaged, due to which shortness of breath is seen. Emphysema is also known as ‘Pink puffer’ .
Due to some reason, hyperinflation is seen in the alveoli.
Due to which destruction is seen in the wall of the alveoli capillary. Due to this, the elasticity of the alveoli is lost, in addition to this, the gas exchange capacity of the alveoli is lost. Air is trapped in the alveoli. The condition of emphysema is seen.
Explain /Define pulmonary embolisms (Define Pulmonary Embolism)

Pulmonary embolism is the obstruction and blockage of one or more pulmonary arteries due to thrombus formation (blood clot). This thrombus originates from the vascular system or right heart and travels to the pulmonary artery.
Explain/ define pneumothorax

Pneumothorax is a medical condition in which there is a leakage of air or gas into the pleural cavity, causing the lungs to collapse. Pneumothorax is a condition in which air leaks into the space between the lungs and the chest wall, causing the lungs to collapse. It can be caused by injury, lung disease, or congenital abnormalities. Symptoms include chest pain, difficulty breathing, and sometimes a bluish discoloration of the skin due to oxygen deficiency.
Explain /Define Pneumonia
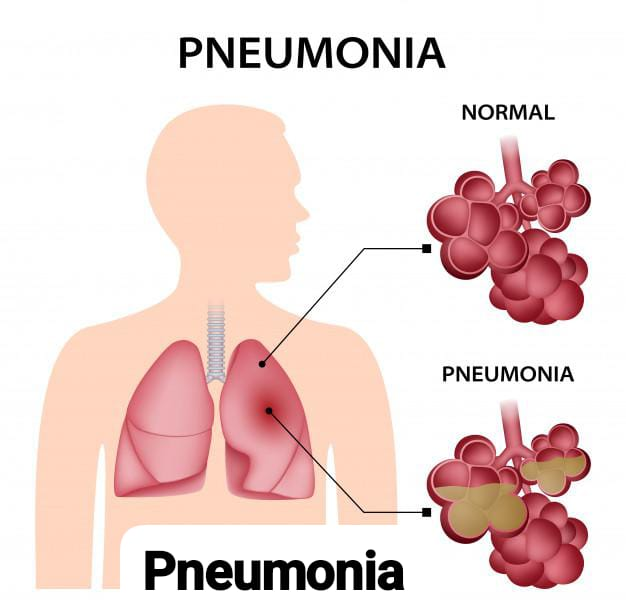
Pneumonia is the infection and inflammation of the lung parenchyma (alveoli) which is caused by bacterial, viral or fungal infections. In which the air sacs fill with fluid or pus and become solid. The alveoli normally work to exchange gases, but in the condition of pneumonia, due to infection and inflammation and accumulation of pus, gas exchange is interfered with.
Explain / Define Bronchial asthma

Bronchial asthma is a chronic inflammatory respiratory disorder. In which the airway becomes hyperresponsive to certain stimuli, due to which the airway becomes inflamed and narrowed, and due to mucus production, the airway constricts and obstruction is seen in it. Asthma is reversible. Due to certain etiological factors, the airway becomes hyperresponsive. Due to this, inflammation is seen in the airway. Due to which hypersecretion of mucus, contraction of airway muscles and swelling in bronchial membranes are seen, due to which airway narrowing occurs. Due to this, cough, chest tightness, shortness of breath and wheezing sound are seen.
Explain / Define cystic fibrosis

Cystic fibrosis is a hereditary and is a genetic disorder that commonly affects the lungs in which mutations in the cystic fibrosis conductance regulator (CFTR) cause excessively thick, tenacious mucus and abnormal secretion of sweat and saliva in the lungs.
Explain/Define Asphyxia:

It is a state of suffocation.
Explain/Define Chest Trauma:

He suffered chest injury.
Explain/Define Hypoxia:

Having inadequate oxygen in the tissues.
Explain/Define Pulse Oxymetry:

Pulse oximetry is a non-invasive method for estimating arterial oxygen.
Explain/Define Postural Drainage:

Postural drainage is a technique for draining secretions from different segments of the lungs by gravity using different body positions.
Explain/Define Thoracotomy:

An opening is made in the thorax.
Explain/Define Cyanosis:

Cyanosis is a bluish discoloration of the skin, especially of the lips, earlobes, etc.
Explain/Define Inhalation:

Inhalation involves the taking in of air or vapors into the lungs. is.
Breathing and Coughing Exercise:

Deep breathing and cuffing exercises are recommended after surgery. These exercises help improve breathing, which in turn helps clear secretions from the lungs and reduce the risk of pneumonia.

If the patient has had minor surgery, provide instructions to do breathing and cuffing exercises every hour for the first two to three days after surgery, and if the patient has had major surgery, provide instructions to do these exercises until the pain at the incision site is reduced. These exercises are usually most effective in a sitting position.
Provide instructions to move the patient and change position every two hours. This position change helps the breathing and cuffing exercises work better.
Deep breathing exercises:

- Perform this exercise every hour while the patient is awake.
- Breathe deeply and slowly through the nose, expanding the lower ribcage and allowing the abdomen to move forward.
- Hold for a count of 3 to 5.
- Breathe slowly and completely through the pursed lips. Do not forcefully exhale.
- Rest and repeat 10 times every hour, if the patient feels dizzy or lightheaded, give rest.
Breathing Techniques:
1) Deep breathing:

- Sit or stand in a comfortable position with your elbows slightly back, this position allows the chest to expand further.
- Take a deep breath and hold it as long as you can.
- Let the air out and then cough forcefully.
- These steps should be repeated 10 times every hour.
2) Diaphragmatic breathing:

- Relax your shoulders and sit back or lie down.
- One hand on your belly and one on your chest Hold.
- Breathe through your nose for 2 seconds, feel the air moving into your abdomen and your stomach expanding. The stomach should move more than the chest.
- Pressing on the abdomen, exhale through pursed lips for 2 seconds.
- Repeat.
3) Pursed lip breathing:

Inhale slowly through the nostrils.
Purse your lips, as if you are blowing on something.
Exhale as slowly as possible through pursed lips. It should take at least twice as long as it took to inhale.
Repeat.
Coughing Exercises:

- It is best to perform cuffing exercises when the patient is fresh and comfortable.
- Instruct the patient to lie on his/her back and, if the surgeon permits, to bend his/her knees and rest his/her feet on the bed.
- Support the incision firmly with the patient’s hands. A small pillow can be used for support.
- Encourage the patient to take a deep breath and cough firmly. If the patient coughs up some mucus, clear it into a tissue. Repeat the cough until there is no more mucus. If the patient has a lot of mucus, give them rest between exercises so that they do not get tired.
Coughing Techniques:

Different techniques of coughing include cascade cough, huff cough, quad coughing and controlled coughing.
1) Cascade Cough:

Ask the patient to take a slow, deep breath and hold it for 2 seconds, while the expiratory muscles contract. Ask the patient to perform a series of coughs while opening the mouth and exhaling, which causes coughing (coughing) in the lower volume of the lungs. This helps in airway clearance and maintains a patent airway in patients with large amounts of sputum.
2) Huff Cough:

In this, the patient opens the glottis by saying the word “huff” while exhaling. The huff cough stimulates the natural cough reflex. This method is useful for clearing the central airway. Patients who practice this regularly inhale more air and may progress to Cascade Cough.
3) Quad Cough:

This is used for patients who lack control of their abdominal muscles, such as those with spinal cord injuries. The patient or nurse, using their hands, pushes the abdominal muscles inward and upward toward the diaphragm while the patient inhales with maximum expiratory effort, causing coughing (coughing).
4) Controlled Coughing:

Ask the patient to take two slow, deep breaths, in through the nose and out through the mouth. Ask them to take a third deep breath and hold their breath for a count of 3. Ask them to cough fully for two or three consecutive coughs without breathing between coughs. Ask the patient to expel all the air from their lungs. The patient should be given proper precautions for coughing and not just clearing the throat. Instruct the patient to cough 2 or 3 times every 3 hours during walking time.
The effectiveness of cough is determined by the amount of sputum in the expectorated sputum and the patient’s swallowed sputum report.
Oxygen cylinder with flow meter and humidifier):

Oxygen cylinders are a crucial component in medical settings. Oxygen cylinders are used to provide supplemental oxygen to patients who are unable to breathe properly, have breathing difficulties, and require higher levels of oxygen. Oxygen cylinders can store oxygen under high pressure. This allows medical professionals to provide oxygen therapy to patients with breathing difficulties, such as those with chronic obstructive pulmonary disease (COPD), pneumonia, asthma, or patients recovering from surgery. Oxygen cylinders are available in a variety of sizes and shapes, ranging from small portable cylinders to large stationary cylinders. Portable cylinders are typically used for ambulatory patient transport, while stationary cylinders are typically used in hospitals, clinics, or long-term care settings.
Cylinders are typically made of aluminum or steel to withstand high pressure. They are filled with compressed oxygen gas, which is purified to medical-grade standards to ensure its safety for patient use. The flow of oxygen from the cylinder is controlled using a flowmeter or regulator. This equipment controls the flow of oxygen to the patient, which is used by the healthcare person to adjust the flow as per the patient’s requirement. Oxygen cylinders should be properly cared for due to the high pressure of the gas contained in them. They should be stored in well-ventilated areas away from heat sources and flammable materials. In addition, healthcare personnel need proper training in oxygen therapy and its safe handling. Regular observation of the oxygen level in the cylinders should be done to ensure that sufficient oxygen is available for patient care. Empty cylinders should be changed immediately to avoid interruption in oxygen supply.
Uses:

There are many important uses of oxygen cylinders in medical settings:
1) Oxygen therapy:
The primary use of oxygen cylinders is to provide supplemental oxygen to patients with respiratory conditions. This involves individuals who have difficulty breathing due to conditions such as pneumonia, asthma, chronic obstructive pulmonary disease (COPD), or respiratory failure. Oxygen therapy helps improve blood oxygenation, providing relief from symptoms such as shortness of breath and fatigue.
2) Emergency Situation:
Oxygen cylinders are essential during emergency situations such as cardiac arrest, trauma or respiratory distress. They provide a readily available source of oxygen to stabilize the patient until more comprehensive treatment can be given.
3)Surgical procedure:
Oxygen cylinders are used in the operating room to provide oxygen to patients undergoing surgery under general anesthesia. Oxygen is essential to maintain adequate tissue oxygenation during surgical procedures and for postoperative recovery.
4) Transportation:
The use of portable oxygen cylinders is commonly used during patient transportation, within healthcare facilities, and during ambulance or air ambulance transfers. They ensure that patients can receive continuous oxygen therapy during the transfer, especially those who rely on supplemental oxygen for their daily activities.
5) Home care:
Oxygen cylinders are provided for use in a home healthcare setting for patients who require long-term oxygen therapy. These cylinders provide a convenient and reliable source of supplementary oxygen for individuals with chronic breathing conditions. Overall, oxygen cylinders play an important role in providing adequate oxygen to patients and in obtaining the oxygen they need to support breathing in various medical settings.
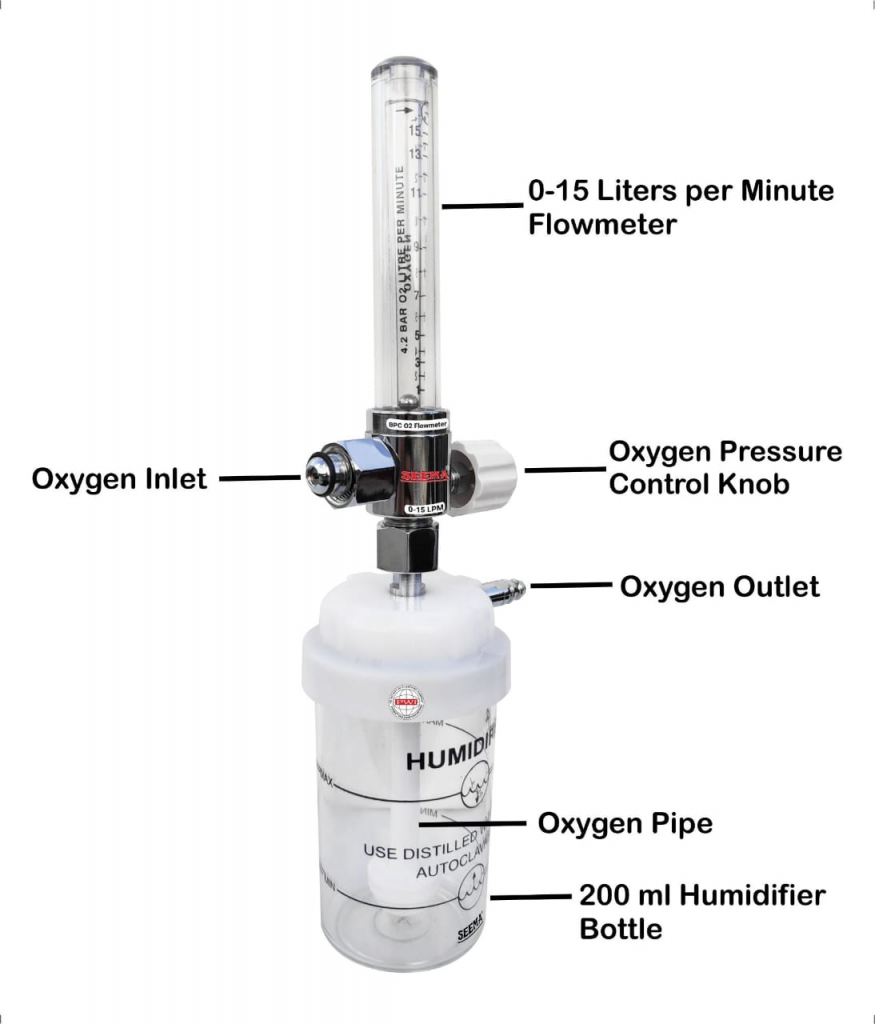
Parts of oxygen cylinder:
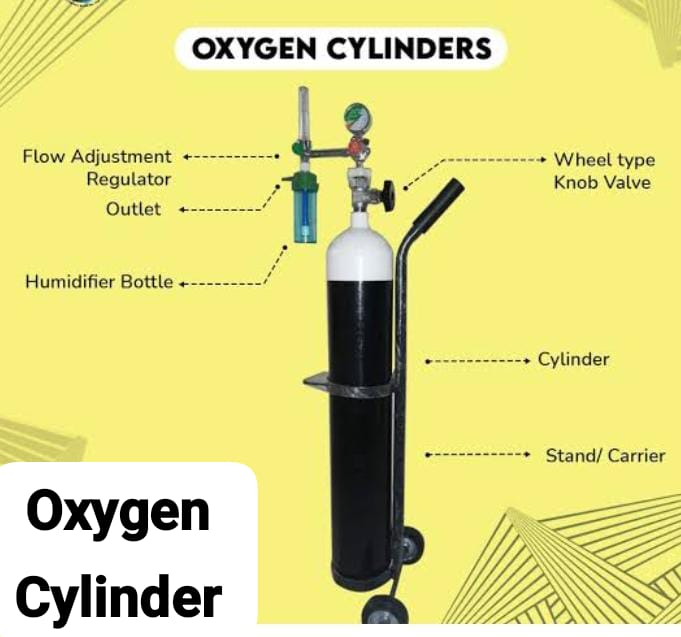
1)Cylinder,
2)Valve,
3)Regulator,
4)Flow meter,
5)Humidifier
1) Cylinder:
The main part of the oxygen cylinder is usually made of aluminum or steel and is made to withstand high pressure. It contains compressed medical-grade oxygen gas.
2) Valve:
The valve is located at the top of the cylinder and controls the flow of oxygen from the cylinder. It can be opened or closed to start or stop the flow of oxygen.
3) Regulator:

The regulator connects to a valve and controls the rate at which oxygen flows from the cylinder. It usually has a gauge that shows the pressure of the oxygen inside the cylinder and a knob or dial to adjust the flow rate. Flow is measured in liters per minute (LPM) and can be adjusted to meet the patient’s oxygen needs.
4) Flow meter:
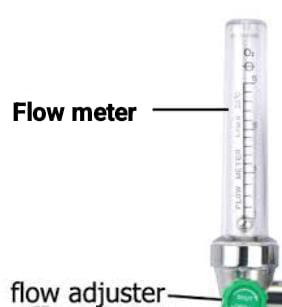
A flow meter is a device that connects to a regulator and measures the rate of flow of oxygen in liters per minute. It usually consists of a tube with a ball or float that increases or decreases depending on the flow rate. The flow meter provides a visual indication of the flow of oxygen, which allows the healthcare provider to adjust it as needed to provide adequate oxygen therapy.
5)Humidifier:

A humidifier is also attached to the oxygen cylinder. Humidifiers add moisture to the oxygen flow to prevent dryness and irritation of the respiratory tract, especially during prolonged oxygen therapy.
Types of Oxygen Cylinder
In medical settings, several types of oxygen cylinders are available, each designed for a specific purpose and patient’s needs.
1. Portable Oxygen Cylinder:

These cylinders are small and lightweight, due to which their transportation is easy. They are typically used for ambulatory patients or during transfers in healthcare facilities. A portable cylinder allows the patient to maintain mobility while taking oxygen therapy.
2. Stationary Oxygen Cylinder:
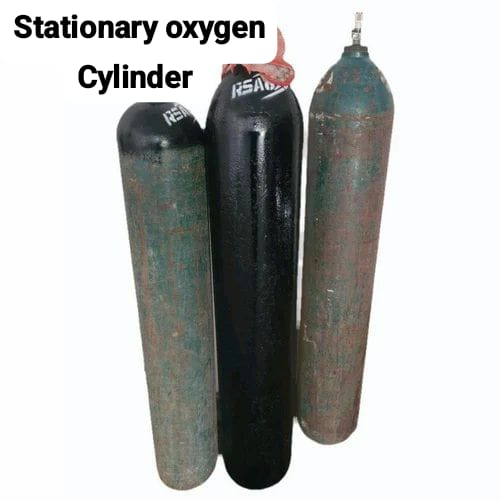
Stationary oxygen cylinders, also known as bulk oxygen cylinders, are large cylinders that are stable and are typically used in hospitals, clinics, or long-term care facilities. They hold a large volume of oxygen and are connected to oxygen delivery systems to provide continuous oxygen therapy to multiple patients.
3. Liquid Oxygen System:

Liquid oxygen systems store oxygen in liquid form at very low temperatures. These systems are often used in home healthcare settings for patients who require long-term oxygen therapy. Liquid oxygen systems offer higher oxygen volumes and require less frequent refilling than compressed gas cylinders.
4. Emergency oxygen cylinder

These cylinders are specifically designed for use during emergencies, such as cardiac arrest, trauma, or breathing difficulties. They usually have a quick-release valve or regulator to facilitate oxygen therapy in critical situations.
5. Aviation oxygen cylinder
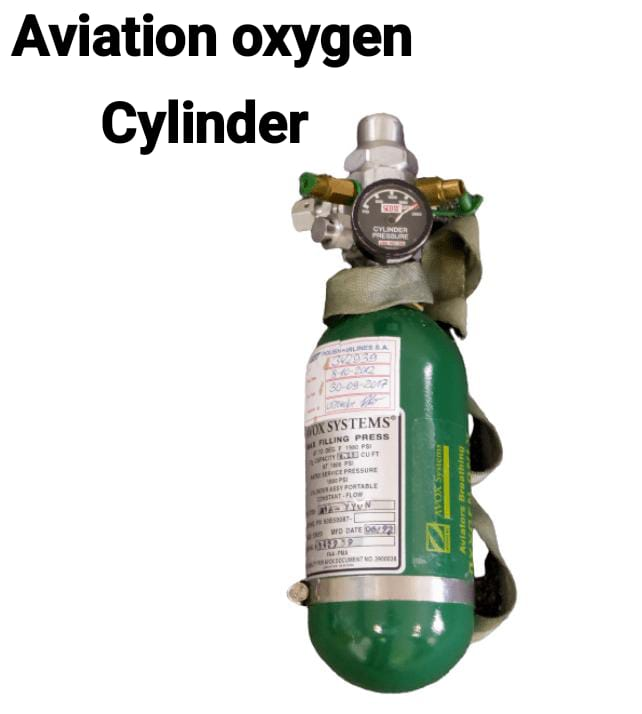
These cylinders are designed for use in aircraft to provide sufficient oxygen to passengers at high altitudes where oxygen levels are low. Aviation oxygen systems are used to maintain safe oxygen levels during air travel, especially for people with breathing conditions.
Cylinder according to colour code:
In medical settings, oxygen cylinders are often distinguished by colour-coding, which helps healthcare personnel quickly identify the cylinders.
1.Green:

Green cylinders usually contain oxygen. They are used for medical oxygen therapy and are the most common type of oxygen cylinder in healthcare settings. Green color is known as the universal color for oxygen.
2.Blue:

Blue cylinders usually contain nitrous oxide, commonly known as
“laughing gas”. Nitrous oxide is used for analgesia and anesthesia during medical procedures and is often mixed with oxygen for safe administration.
3. Gray or Silver:

Gray or silver cylinders often contain carbon dioxide (CO2) or other specialty gases used in medical applications, such as carbon dioxide for insufflation during endoscopic procedures and for cryotherapy.
4. White:

White cylinders are usually used for non-medical gases, such as nitrogen or compressed air, which can be used for various purposes in medical equipment, such as powering medical equipment and pneumatic tools.
Humidifier (Humidifier):
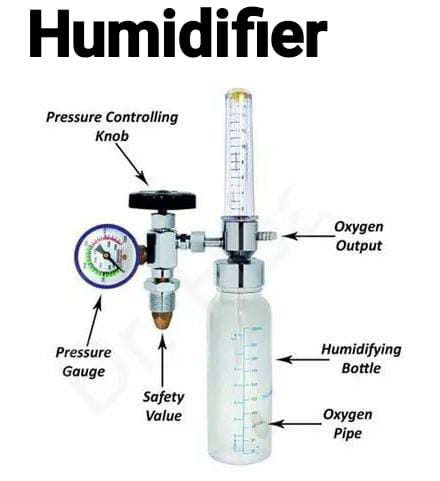
A humidifier in an oxygen cylinder is a device that adds moisture to the flow of oxygen to prevent dryness in the airways. It helps keep the respiratory tract moist and can be especially useful for people using oxygen therapy for long periods of time. Typically, a humidifier is a container filled with sterile water through which oxygen is passed, drawing moisture out before it is inhaled. This helps prevent burning sensation and discomfort in the nose, throat and lungs.
Purpose:

- The purpose of a humidifier for oxygen cylinders is to add moisture to the oxygen given to the patient, especially during oxygen therapy.
- When oxygen is delivered through a nasal cannula or mask, it can sometimes produce dryness and burning sensations in the respiratory tract. Humidifiers help relieve this discomfort by moistening the oxygen and ensuring that the airways remain moist and preventing burning, dryness, and damage to the mucous membranes. Reduces Risk.
- Humidifiers are especially important for people who need long-term oxygen therapy, as they help improve comfort during treatment.
Parts of Humidifier:
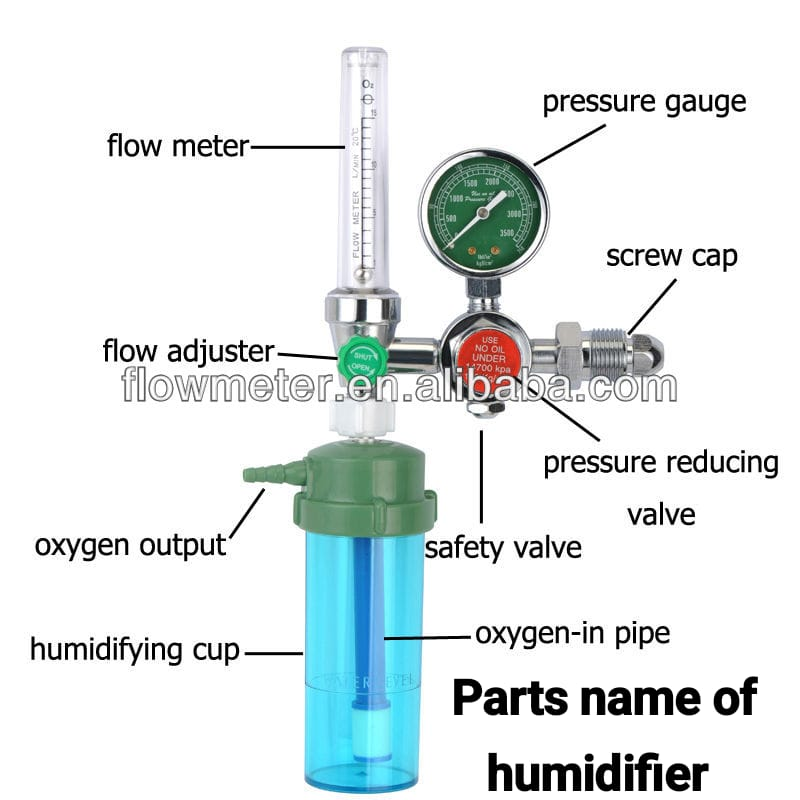
The parts of a humidifier in an oxygen cylinder usually include the following:
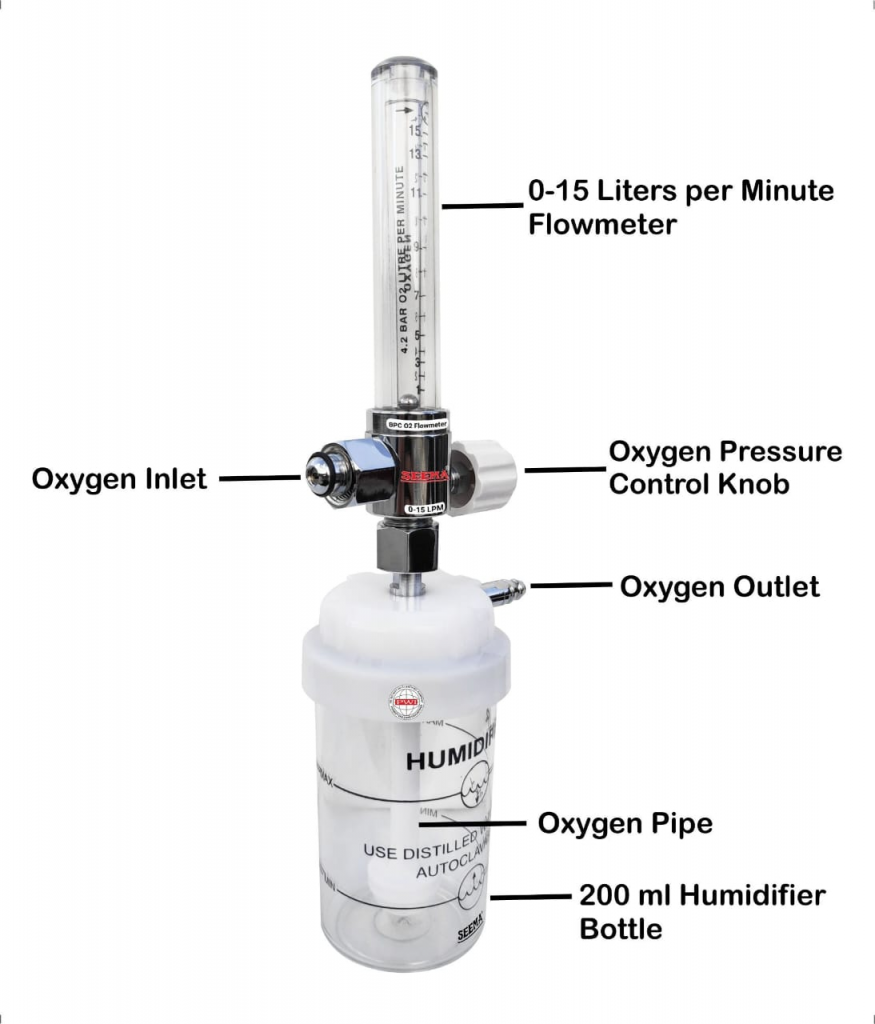
1) Reservoir or water chamber:
This is the main container where sterile water is stored. Oxygen passes through this chamber, and the oxygen is moisturized as it flows.
2) Inlet and outlet ports:
These are the openings where oxygen enters and exits the humidifier. The inlet port connects to an oxygen source, such as an oxygen cylinder or concentrator, while the outlet port provides humidified oxygen to the patient.
3) Baffle or Diffuser:
This component helps distribute the oxygen evenly throughout the water chamber.
4) Adjustment Dial or Control or Control):
Many humidifiers have an adjustment dial or control that allows users to regulate the amount of moisture added to the oxygen flow based on the patient’s needs and environmental conditions.
5) Safety Features
Many modern humidifiers have safety features such as pressure release valves and alarms.
Use:
Oxygen contained in cylinder The use of a humidifier involves the following:
1. Moisturizing the Airway:
Oxygen therapy sometimes produces dryness and a burning sensation in the respiratory tract. Humidifiers add moisture to the oxygen, ensuring that the airways remain moist and reducing the risk of discomfort and damage to the mucus membranes.
2. Eliminating Dryness:
By moisturizing the oxygen, humidifiers help eliminate dryness in the nose, throat, and lungs, making breathing more comfortable for people undergoing oxygen therapy.
3.Improving Comfort:
Humidified oxygen is more comfortable to breathe, especially for patients on long-term oxygen therapy who require continuous oxygen support for long periods of time.
4. Reducing Irritation:
Dry air can produce a burning sensation in the airways, which can cause coughing, sore throat, and other discomfort. Humidifiers help reduce the burning sensation by maintaining the moisture level in the oxygen flow.
5.Enhancing therapy adherence:
Comfortable oxygen therapy is crucial for the patient. By ensuring that the oxygen has sufficient moisture, a humidifier increases the comfort of the patient. Thus, a humidifier helps prevent dryness by properly moisturizing the air.
After use:

1. Disconnect from oxygen source:
Before cleaning, make sure that the humidifier is disconnected from the oxygen cylinder and concentrator to avoid accidental flow of oxygen.
2. Empty the water chamber:
Carefully empty the remaining water from the humidifier’s water chamber.
3. Disassemble the parts:
Separate the reservoir, water chamber, inlet and outlet ports, wick or wick pad (if applicable), and any other removable parts.
4. Use mild soap and Cleaning with Water:
Wash all removable parts thoroughly using a solution of mild soap and warm water. Use a brush or sponge to remove any residue or deposits. Pay attention to any cracks or areas where bacteria or mold can accumulate.
5. Rinse thoroughly:
After cleaning, wash all surfaces with clean water to remove any soap residue.
6. Disinfect:
To disinfect a humidifier, a mixture of one part white vinegar and three parts water can be used. Fill the water chamber with the vinegar solution and let it soak for at least 30 minutes. After that, rinse thoroughly with clean water.
7. Dry Completely:
Allow all parts to air dry properly before reassembling the humidifier.
Ensuring that there is no moisture, as moisture can promote bacterial growth.
8. Reassemble and reconnect To do:
Once dry, reassemble the humidifier. Ensure that all the pins are properly connected. And do regular maintenance and checking of humidifier.
Oxygen Cannula/ Nasal Cannula:
Introduction:
An oxygen cannula is a medical device used to provide oxygen supplements to a patient. This oxygen cannula is also known as a nasal cannula. This nasal cannula was introduced in 1960 by American physician and pulmonologist Dr. Alvan L. Barach. This nasal cannula is mainly used when the patient needs a low flow rate and medium concentration of oxygen. In it, the flow rate of oxygen is 1-6 liters/minute. And the concentration of oxygen is 24 – 44%. This nasal cannula is usually made of medical grade silicone.
Parts of Oxygen Cannula:
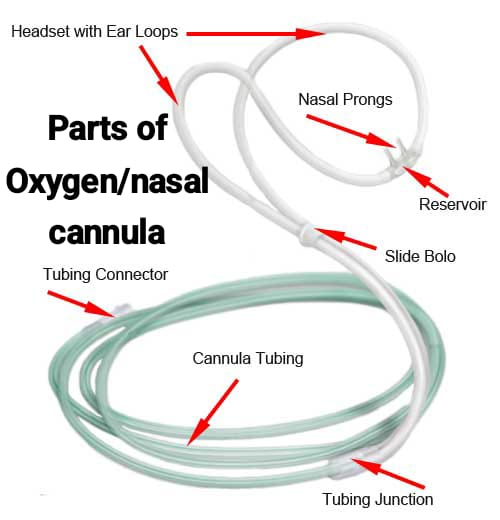
1) Nasal prongs,
2) Reservoir,
3) Ear loops,
4) Regulating Ring,
5) Oxygen tubing,
6) Connector
1) Nasal prongs:
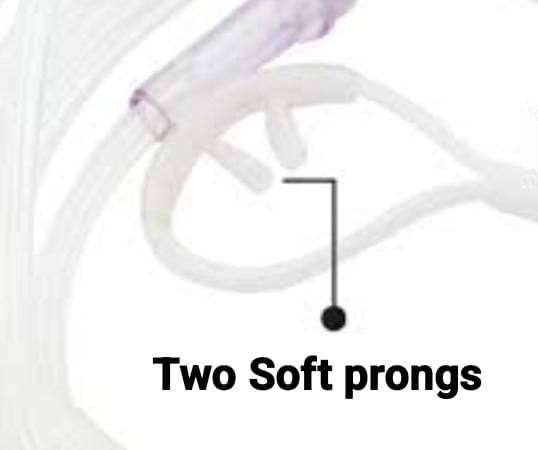
Nasal prongs are two small covered tips that are fitted into the nostrils to provide oxygen.
2) Reservoir:
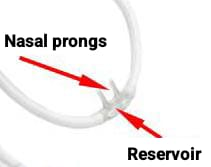
The reservoir is the part that connects the nasal prongs to the ear loop. Works.
3) Ear loops:
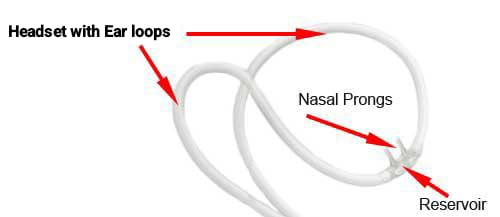
The ear loop is the part through which the cannula is secured in place, which is placed over the ear.
4) Regulating Ring:

This regulating ring is used to properly adjust and fix the ear loop on the head.
5) Oxygen Tubing:
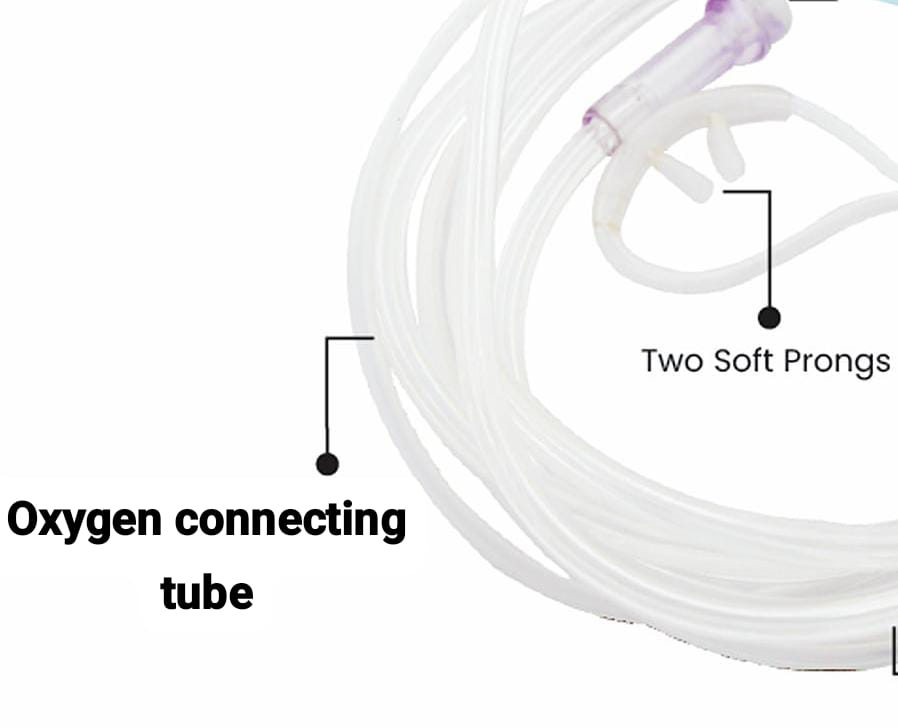
Oxygen tubing works to deliver oxygen to the nasal prongs properly.
6) Connector:
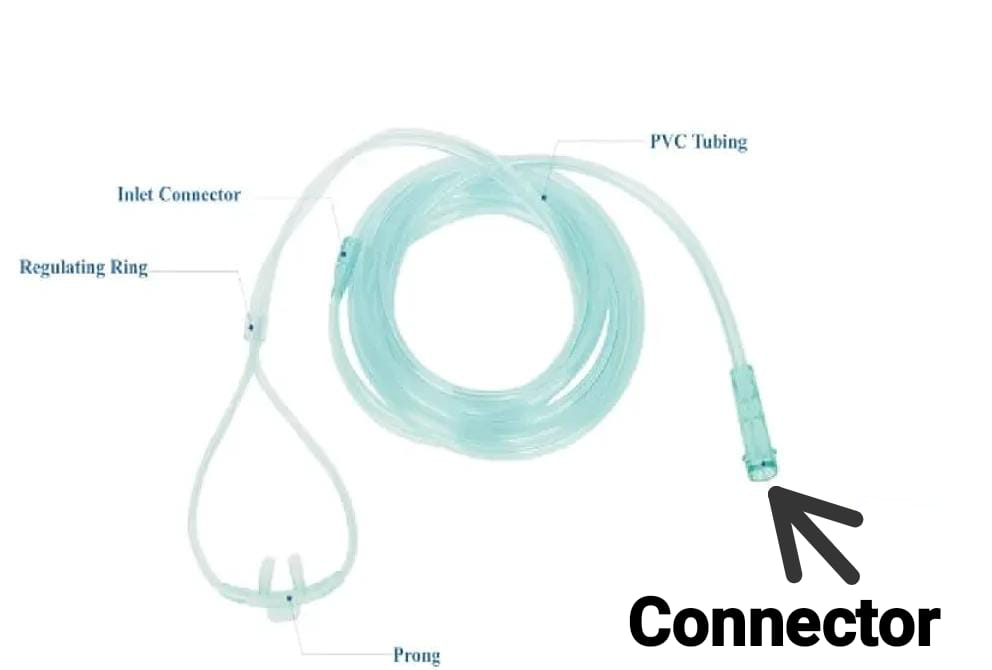
This connector is connected to an oxygen source.
Uses:
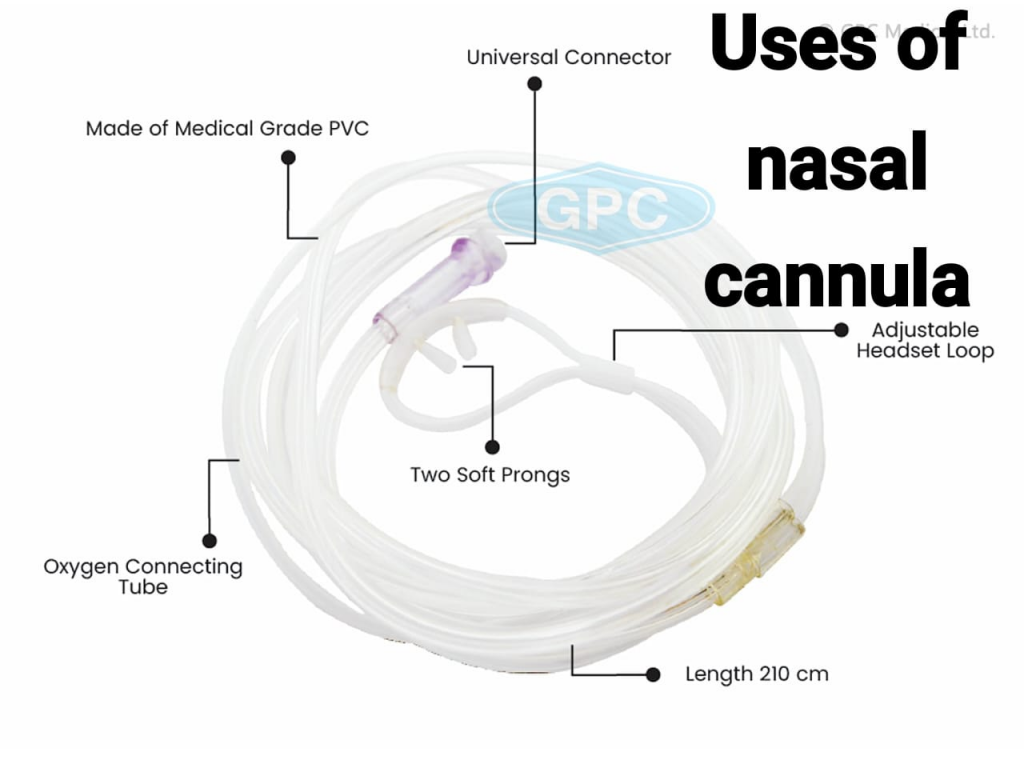
This nasal cannula is a disposable device made of silicone that has two prongs through which oxygen can be provided to the patient.
1) Oxygen therapy:
It is used to provide proper oxygen to patients who have chronic obstructive pulmonary disease (COPD) conditions.
2) Supplemental Oxygen:
A nasal cannula is used to provide supplemental oxygen to patients who are in recovery from surgery and illness.
Advantage:
- It enables the client to communicate and eat with oxygen therapy.
- This nasal cannula can be easily used at home.
- It is safe and simple to use.
- It delivers low concentrations of oxygen is.
Disadvantage:
- This nasal cannula cannot be used in conditions of nasal obstruction.
- The nasal cannula can dry out the mucous membrane, so a flow rate of more than 4 ml / min is required to humidify.
- The prongs of the nasal cannula can easily come out of the nostril.
- Causes skin irritation or skin breakdown on the ear or nostril.
- It cannot be used for mouth breathers.
Size of Different Nasal Cannula Prongs prongs):
1) Small size cannula:

The diameter of its prongs is available in 1.4 mm to 1.8 mm. It is commonly used in infants.
2) Medium Size Cannula:

The diameter of its prongs is available in 2.0 mm to 2.5 mm. It is commonly used in pediatrics.
3) Large Size Cannula:

The diameter of its prongs is available in 2.8 mm to 3.5 mm. Its use is usually done in adults.
After care:
Cannula is usually single use i.e. disposable which is properly discarded in a yellow bio hazard bin after being used once.
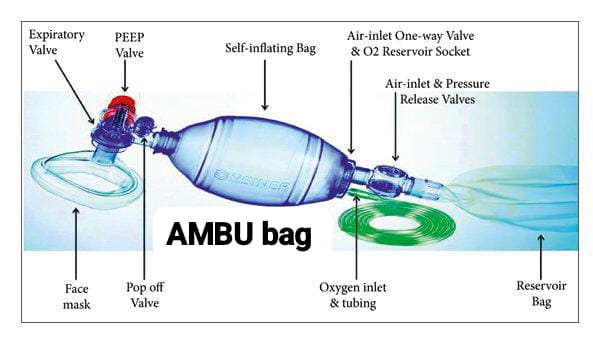
AMBU Bag:
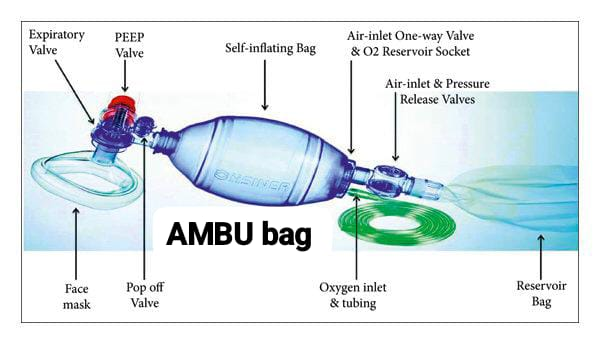
Introduction:
AMBU Bag‘s full name is Artificial Manual Breathing Unit (Artificial manual breathing unit) . AMBU Bag is also known as Bag Valve Mask (BVM). This AMBU Bag is used to provide positive pressure ventilation when there is insufficient and ineffective breathing. The main bag part of this AMBU Bag is made of silicone material. It is made of silicone so that it is self-inflating, that is, after pressing the bag and releasing it, the bag returns to its normal place.
Other names of the AMBU Bag:
1) Manual Resuscitator,
2) Self-inflating,
3) Bag-mask ventilation
Parts of AMBU bag:
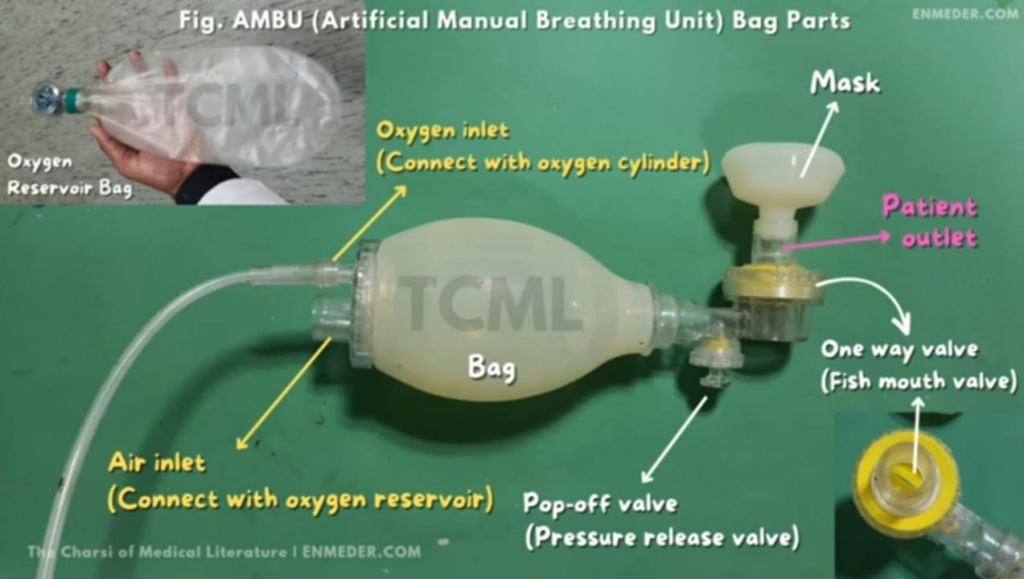
1) Inlet,
2) Main Body: It has an inlet valve.
3) Patient Outlet: It has 1) Pop of valve 2) Fish mouth valve and 3) Expiratory valve. Thus,
Ambu bag mainly has four valves:
1) Inlet valve,
2) Pop of valve,
3) Fish mouth valve,
4) Expiratory valve (Expiratory valve).
1) Inlet: There are usually two openings in the inlet part of the AMBU bag.
A) Large opening,
B) Small opening.
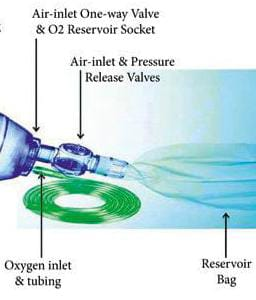
A) Large opening:
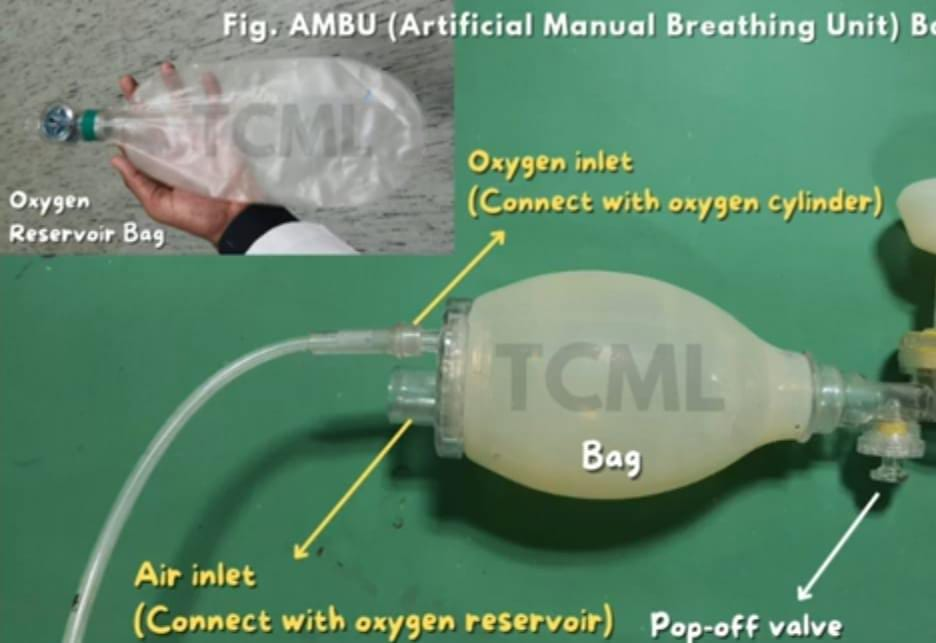
The reservoir bag is attached to this large opening.
B) Small opening:
The small opening is connected to the oxygen supply.
2) Main body/Self-inflating bag( Main body/ (Self inflating bag) ):

This is the main bag of AMBU bag The part is made of a flexible component, i.e. silicone, which is usually used to provide air and oxygen to the patient, and its function is to pass oxygen and air in a single direction. This bag is a self inflating bag, meaning that after pressing the bag, the bag returns to its normal place when released.
3) Patient outlet:
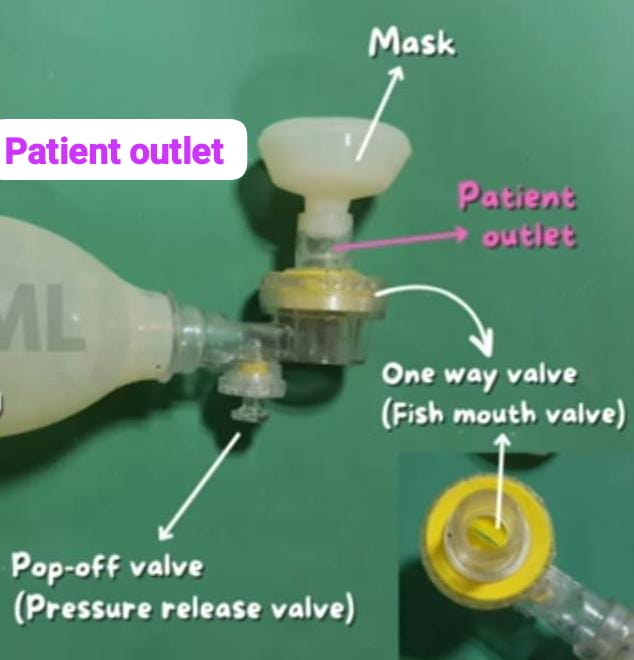
This part of the AMBU bag is placed at the patient site and attached to the patient outlet. It has 1) Pop of valve 2) Fish mouth valve and 3) Expiratory valve.
1) Pop of valve:

When oxygen is provided through the AMBU bag, the extra oxygen is removed through this Pop-of valve which is provided for the safety of the patient because when excess oxygen is released into the patient’s body through the AMBU bag, the extra oxygen is released through this Pop-of valve and the lungs are starved. Damage can be prevented.
2)Fish mouth valve:
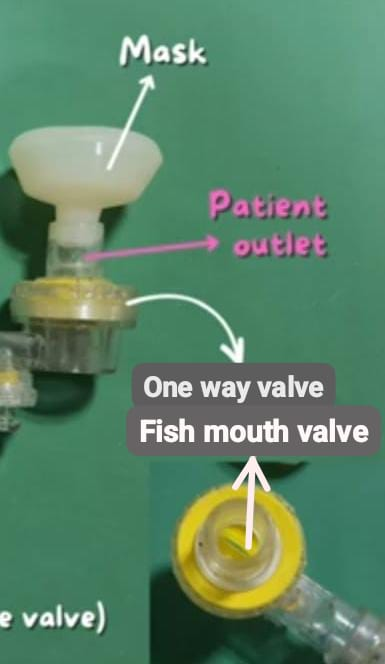
When the bag of the AMBU bag is pressed by hand, oxygen is released in one direction i.e. the fish mouth valve opens and when the patient exhales, this fish mouth valve closes due to which the air exhaled by the patient does not enter the Ambubag.
3) Expiratory valve:
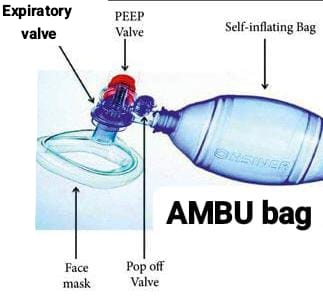
The air exhaled by the patient is released through the expiratory valve.
Uses of AMBU bag:
- The AMBU bag is used to provide ventilation to patients who are unable to breathe or have inadequate breathing patterns.
- The AMBU bag is used to improve breathing in patients who are unable to breathe effectively and on their own due to medical conditions such as chronic obstructive pulmonary disease (COPD).
- The AMBU bag is also used to maintain ventilation during the induction, maintenance, and recovery phases of anesthesia.
- The AMBU bag is used to maintain positive pressure ventilation in emergency situations to keep the airway properly patent.
- The AMBU bag is used to support initial ventilation in patients with breathing compromise or difficulty and in emergency medical situations such as trauma.
- The AMBU bag is also used to provide ventilation support in patients who have been intubated but require manual ventilation.
- The AMBU bag is used during emergency situations where a child is in respiratory distress or has the possibility of respiratory arrest.
Size of AMBU bag:
AMBU bags are available in different sizes such as:
1) Small Size(Small Size),
2) Medium size(Medium size),
3) Large Size(Large Size)
1) Small Size:

This AMBU bag is available in 250 ml size. It is commonly used in neonates.
2) Medium Size:

This AMBU bag is available in a size of 500 ml. It is commonly used in pediatrics.
3) Large Size:

This AMBU bag is available in 1000 ml size. It is commonly used in adults.
Mask Size of AMBU bag:
AMBU bags are commonly used in the following standard mask sizes, measured in cm (diameter):

1) Neonates: Size 0 (about 4 cm)
2)Infant: Size 1 (about 5 cm )
3) Children: Size 2 (approximately 7 cm)
4) Adult: Size 3 or 4 (approximately 9 cm or 11 cm).
These different sizes are designed to fit the patient properly and provide effective ventilation.
After care:

After using the AMBU bag, all its parts should be properly separated and then its parts should be After separating, clean it properly in running water and then dip the AMBU bag properly in Cidex (glutaraldehyde) solution so that it can be properly sterilized and then the AMBU bag can be reused.
AMBU bag cannot be autoclaved because it is made of silicone and there are chances of damage.
Oxygen inhalation:

Oxygen inhalation is used to treat patients with respiratory dysfunctions. ‘Anoxaemia (Extremely low or absence of oxygen in the blood)’ or ‘Hypoxaemia (Low level of oxygen in the blood). The normal amount of oxygen in arterial blood should be in the range of 80 to 100 mm Hg. If it falls below 60 mm of Hg, irreversible physiologic effects can occur.
Cerebral cells receive 20 percent of the body’s oxygen supply and if their O₂ supply is cut off, it takes only a few minutes (5 to Can only live for 7 minutes. Oxygen administration treats the effects of oxygen deficiency but does not correct its cause.
Indications of Oxygen Therapy:
1) Cynosis :
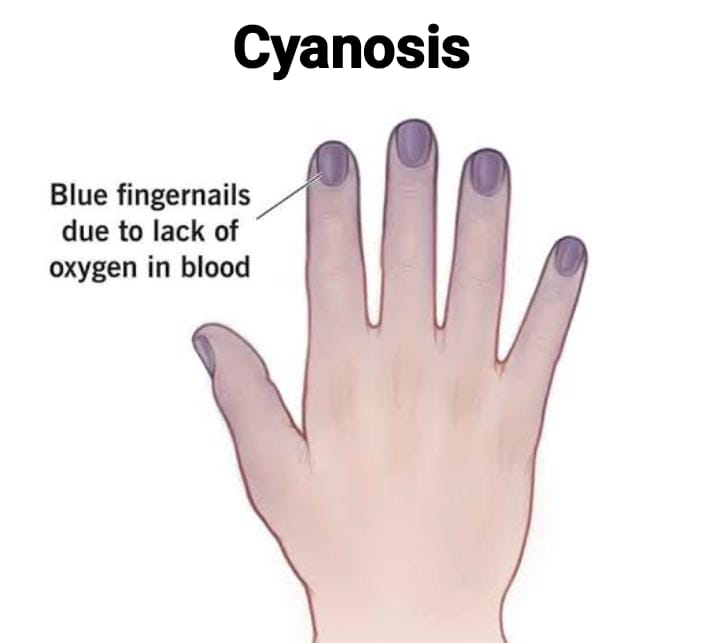
Bluish coloration of the skin, nail beds and mucous membranes occurs due to decreased blood supply, resulting in a decrease in the amount of oxygen in the hemoglobin of the blood.
2)Breathlessness:
Breathlessness can be caused by asthma, emphysema, pulmonary embolism, coronary thrombosis and other cardiac insufficiency.
3) Anemia (Anaemia):

Anaemia can be caused by a deficiency in the quality or quantity of red blood cells.
3) High Altitudes
4) Disease related to the respiratory system.
5) Poisoning with chemicals that alter the tissues ability to utilize oxygen, such as cyanide poisoning to utilize oxygen Ex : Cyanide poisoning).
6) Shock and circulatory failure.
7) Haemorrhage and air hunger.
8) Asphyxia.
9) Patients under Anesthesia.
10) Patients who are Critically ill.
11) Psychologically induced Breathlessness
Methods of Oxygen Administration:
1) Nasal catheter
2) Nasal cannula/ nasal prongs
3) Simple face mask
4) Venturi mask
5) AMBU bag BAG)
6)Oxygen hood
7)Oxygen tent
8)Non-rebreather mask
9)Partially rebreather mask
10)Continuous Positive Airway pressure
11)Bilevel Positive Airway Pressure (BiPAP)
12)Mechanical ventilator
Equipment required for Oxygen Administration:
- Patient’s chart or Cardex
- Oxygen connecting tube
- Flow meter
- Humidifier bottle half filled with distilled water
- Oxygen source: Wall outlets or tray with oxygen cylinder (Oxygen source: Wall Outlets or Oxygen cylinder Tray with) :
- Nasal cannula of appropriate size or oxygen mask
- Nasal catheter Size-8-14 F (for nasal catheter insertion)
- Xylocaine Jelly 2% as lubricant (for nasal catheter insertion)
- Kidney tray
- Gauze pieces, Cotton swabs – bowl with sterile water
- “No smoking” sign board.
Nurse’s Responsibility for Administration of Oxygen Oxygen):
1) Check the patient’s name, bed number and other identification.
2) Diagnosis and check the need for O₂ therapy.
3) Check the doctor’s orders for initiation of therapy, dosage, etc.
4) Check the doctor’s orders for specific precautions regarding positioning and movement of the patient.
5) Assess the patient for any signs of clinical analysis, e.g. : Cyanosis.
6) Check the patient’s vital signs properly.
7)Check the results of arterial blood gas analysis.
8) Note any signs of pulmonary dysfunction.
9) Check the patient’s mental state and ability to follow instructions.
10) Check the available articles in the unit. Check the O₂ cylinder for its accessories and its working condition.
Procedure of Oxygen Administration:

1) Nasal catheter:
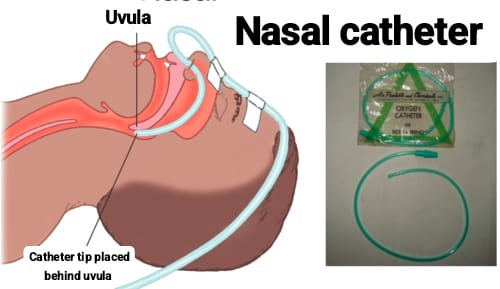
The nasal catheter reaches the uvula in the nostril and is held in place with adhesive tape. The catheter does not interfere with the patient’s freedom to eat, talk, and move around in bed. A flow of 1 to 4 liters of O₂ will be sufficient to maintain an oxygen concentration of 22 to 30%.
A nasal catheter is a soft tube with holes at short distances.
Procedure:
After lubricating the catheter well, an external nasal cannula is inserted into the patient’s nose. It should be inserted to a depth equal to the distance from the nares to the tragus of the ear. The tip should be above the uvula.
Limitations:
Low usage, gag reflex during insertion, nasal obstruction.
2) Nasal cannula/nasal prongs:
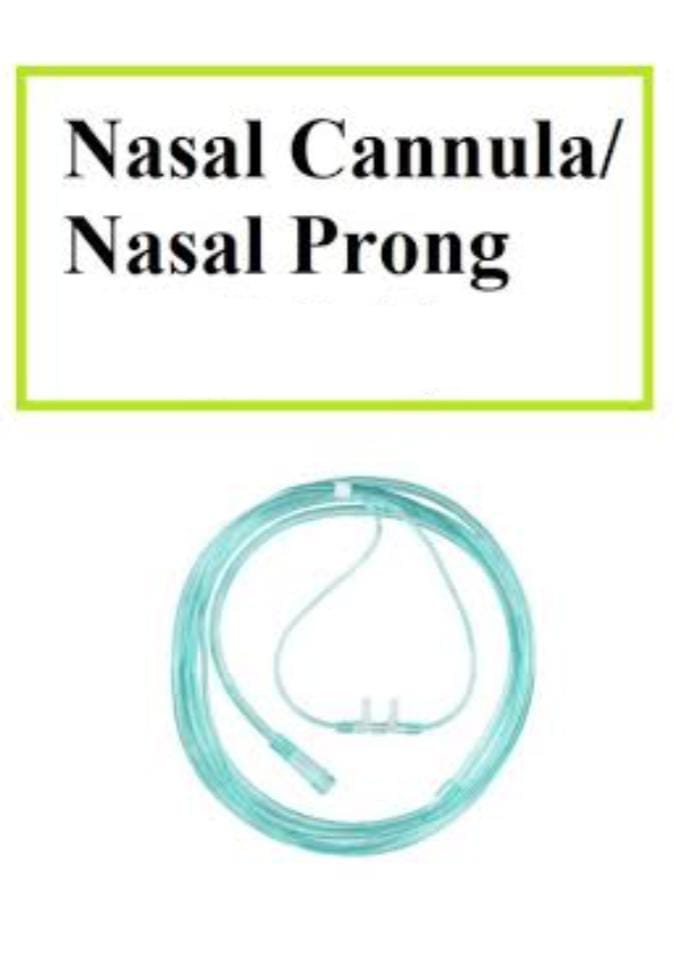
A nasal cannula consists of a small-bore tube connected to two short prongs that is inserted into the nares to provide oxygen to the patient directly from a flow meter or through humidified air.
It is used for short or long-term therapy (COPD patients) and is best used for stable patients who require low amounts of oxygen.
Procedure : Insertion of nasal Cannula:
Steps of Procedure:
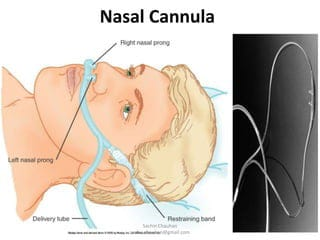
- Check the doctor’s order including date, time, flow rate: To avoid medication errors.
- Perform hand hygiene: To prevent the spread of infection.
- Explain the purpose and procedure to the patient and gather the equipment: Providing information can help gain the patient’s cooperation and reduce the patient’s anxiety level.
- Wall mount the flow meter Attach to outlet or oxygen cylinder. Fill humidifier approximately 1/2 with distilled water: Humidification prevents nasal mucosa from drying out.
- Attach cannula to adapter connecting tubing on humidifier: Flow testing is necessary before use to provide prescribed oxygen to patient.
- Check flow on hand by setting flowmeter to 2-3L/min: Proper position allows unobstructed flow of oxygen and makes patient breathing easier.
- Insert the nasal cannula into the patient’s nostrils, adjust the tubing behind the patient’s ears, and slide the plastic adapter under the patient’s chin until it is comfortable: Adjusting the tubing and maintaining proper position helps ensure uninterrupted oxygen flow.
- Document the following: date, time, method, flow rate, respiratory condition, and response to oxygen: Documentation maintains coordination of care.
Advantage:
Can provide 24% to 40% O₂ (oxygen) concentration. O₂ can be delivered at a rate of 1 to 6 liters per minute (L/min). It is convenient because the patient can talk and eat while receiving oxygen. Easy to use, low cost and disposable.
Limitations:
Can be easily dislodged, not as effective if the patient is a mouth breather, has blocked nostrils, deviated septum or polyps.
3) Simple face mask mask):

The O₂ mask covers the patient’s nose and mouth. The mask is beneficial for patients who are unable to breathe through their nose. A flow of 8 to 12 liters of O₂ will maintain an O2 concentration of 25 to 60%.
The mask fits over the patient’s mouth and nose and has an exhalation port (a hole in the side of the mask) through which the patient exhales CO, (carbon dioxide).
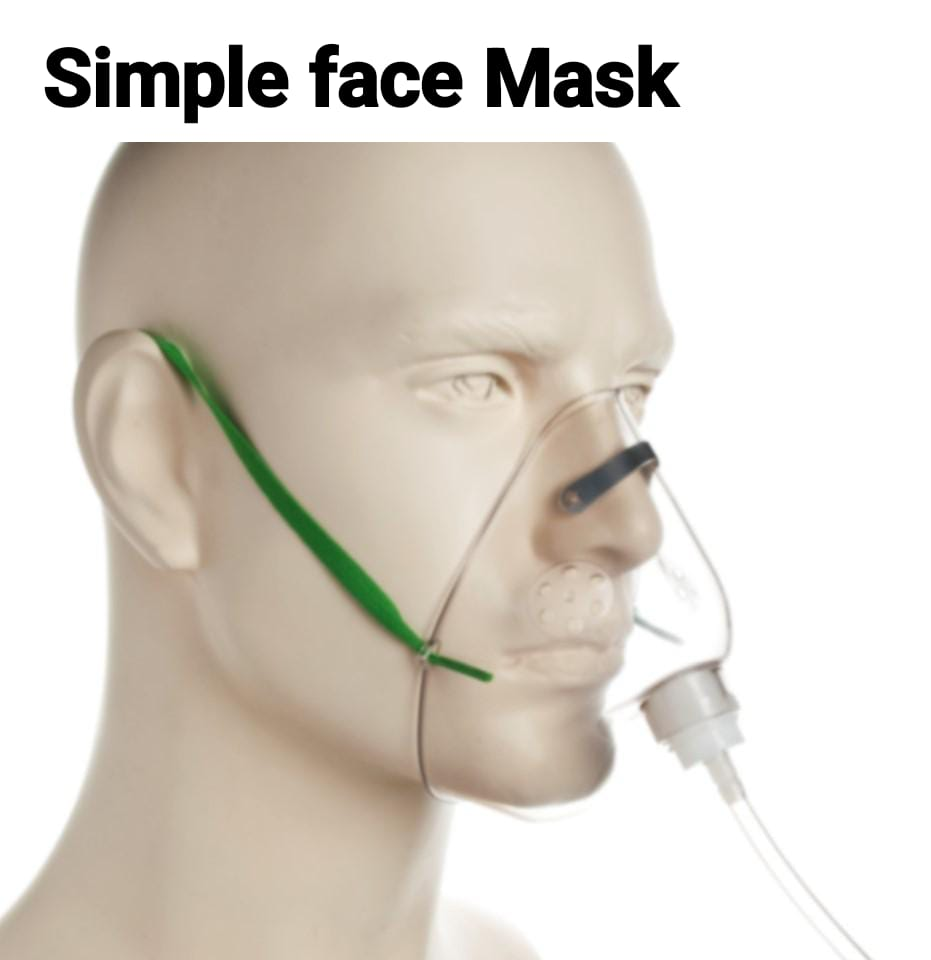
The mask is held in place by elastic at the back of the head, and it has a metal piece to fit over the nose to help the mask fit better for the patient. Humidified air may be attached if the concentration is drying out for the patient.
Advantages:
Can provide 40% to 60% oxygen concentration. Flow meter should be set to deliver oxygen at 5 to 10 L/min.
Disadvantages:
Eating with a mask is difficult. Masks can be confining for some patients, who may feel claustrophobic in the mask.
4) Venturi mask:

- High flow device.
- Allows precise measurement of delivered O2.
- Uses ports of different sizes to change the FiO2 fraction of inspired oxygen (24% to 50% concentration of O2 in the gas mixture).
- Useful in COPD patients where precise oxygen is delivered.
5) AMBU bag:
- AMBU : Artificial Manual Breathing Unit.
- Self-inflating bag.
- It has a gas inlet and valve.
- They have FiO2 > There is a probability of 90%.
6) Oxygen hood:
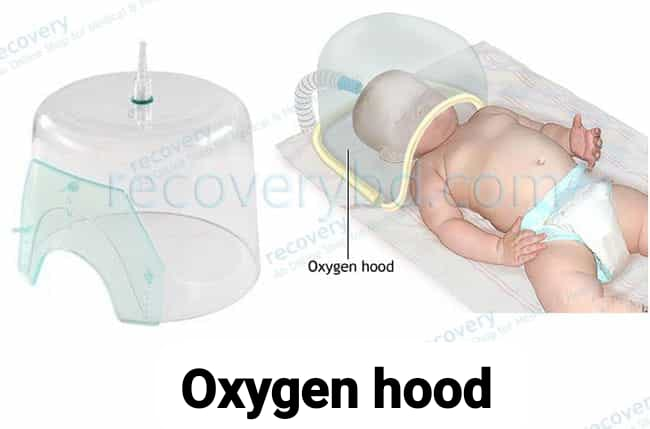
An oxygen hood is a plastic dome or box that contains warmed and humidified oxygen. Oxygen hoods are used for babies who can breathe on their own but still need supplemental oxygen.
7) Oxygen tent:
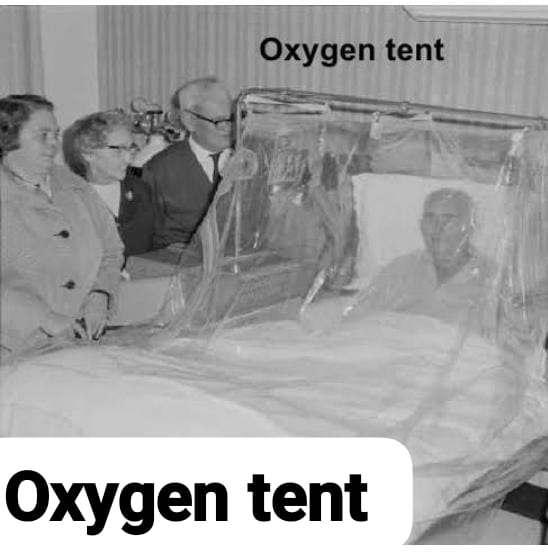
The patient’s bed includes a canopy (cover) that can fully or partially cover the patient and is connected to an oxygen supply. 10-12 liters of oxygen are required per minute.
Certain Advantages and Disadvantages of using Oxygen tent:
Advantage:
- It provides the patient with an environment with controlled O₂ concentration, temperature regulation and humidity control.
- It allows freedom of movement in the bed.
Disadvantages:
- Creates a feeling of isolation.
- It requires a high volume of oxygen (10-12 liters of oxygen per minute).
- It also increases the chances of fire.
- More time and effort are required to keep the tent clean and maintained.
8) Non-Rebreather Mask:
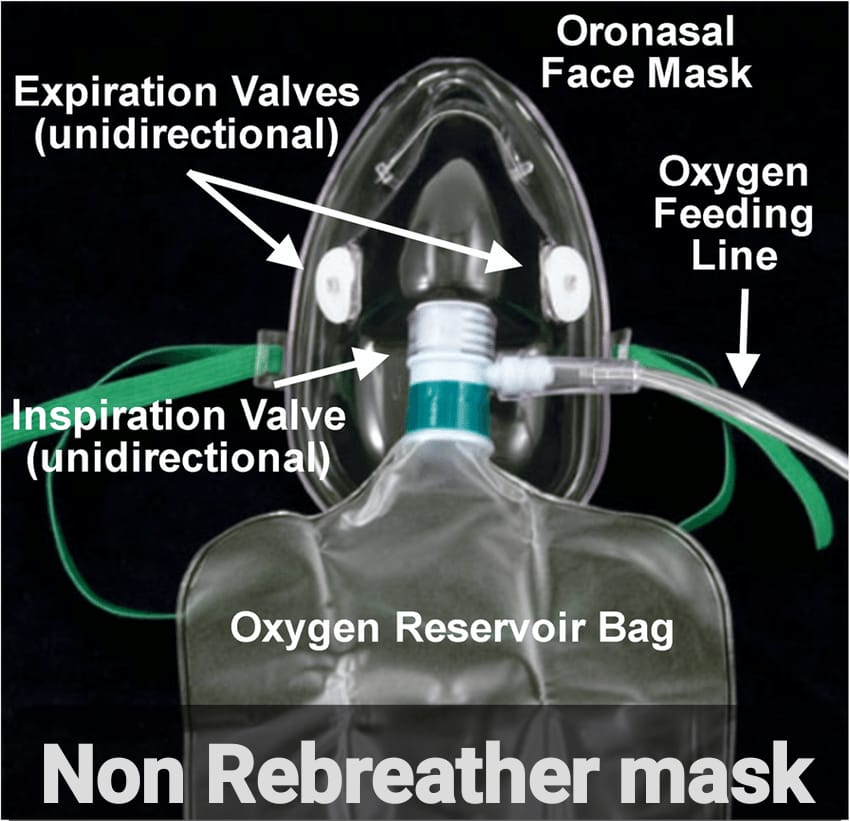
A non-rebreather mask is a mask connected to a reservoir bag that The meter is connected to tubing. It consists of a series of one-way valves between the mask and the bag and also on the cover of the exhalation port. The reservoir bag should never be completely deflated; if the bag deflates, there is a problem and immediate intervention is required. The one-way valve functions so that on inspiration, the patient breathes only into the reservoir bag; on exhalation, carbon dioxide is expelled through the exhalation port.
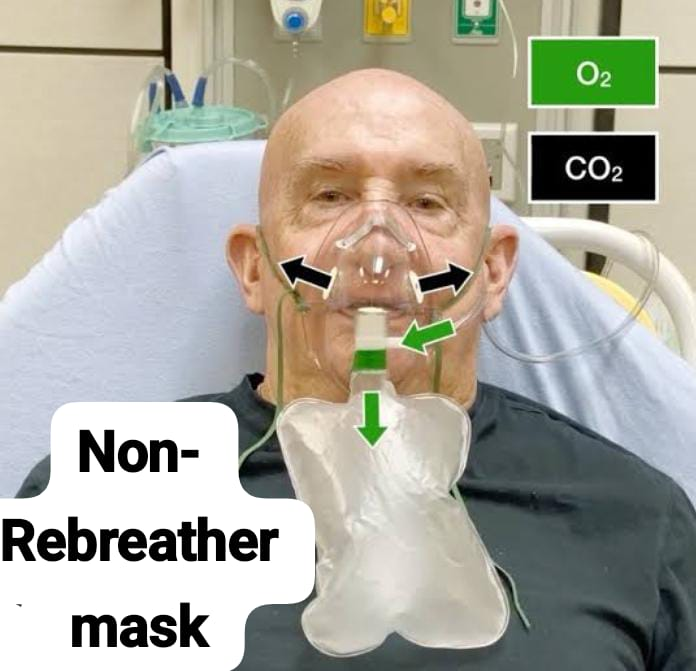
Non-Rebreather mask is used for patients who can breathe on their own but need a higher concentration of oxygen to maintain a satisfactory blood oxygenation level. is.
9) Partial Rebreather Mask:
A Partial Rebreather mask looks similar to a Non-Rebreather mask.
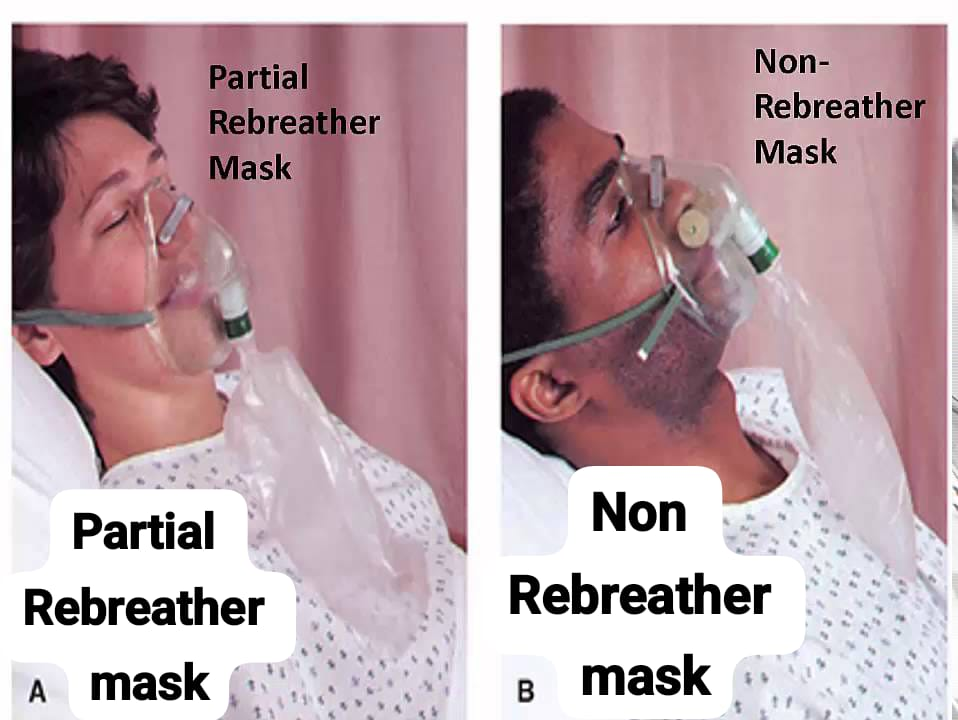
The difference between a Partial Rebreather mask and a Non-Rebreather mask is that the Partial Rebreather mask does not have a one-way valve, so the patient The patient’s exhaled air mixes with the inhaled air. Partial rebreather masks require 10-15 L/min of oxygen but deliver only 35-50% FiO2.
10) Continuous Positive Airway Pressure (CPAP):
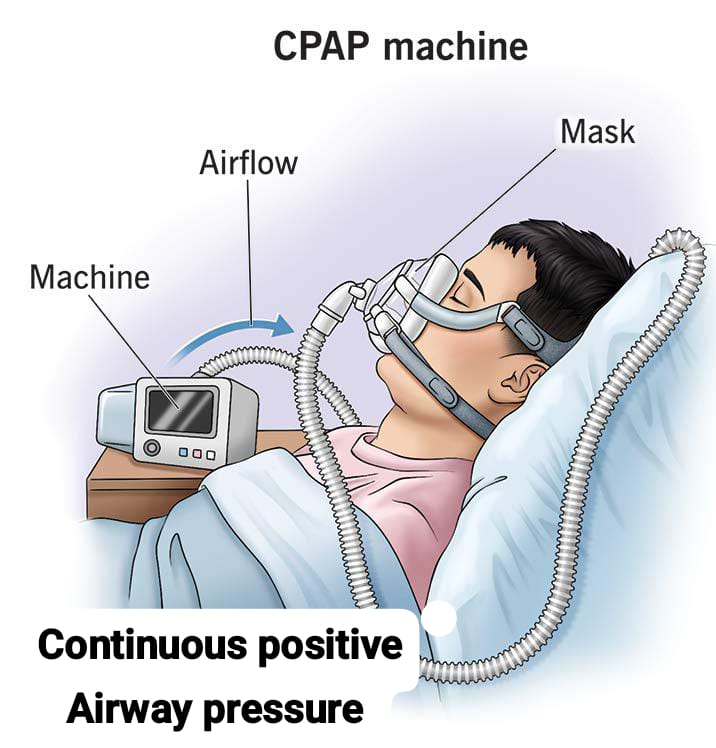
Continuous Positive Airway Pressure (CPAP) devices are used for people who are able to breathe on their own but need help keeping their airways unobstructed, such as those with Obstructed Sleep Apnea.
11) Bilevel Positive Airway Pressure (BiPAP):
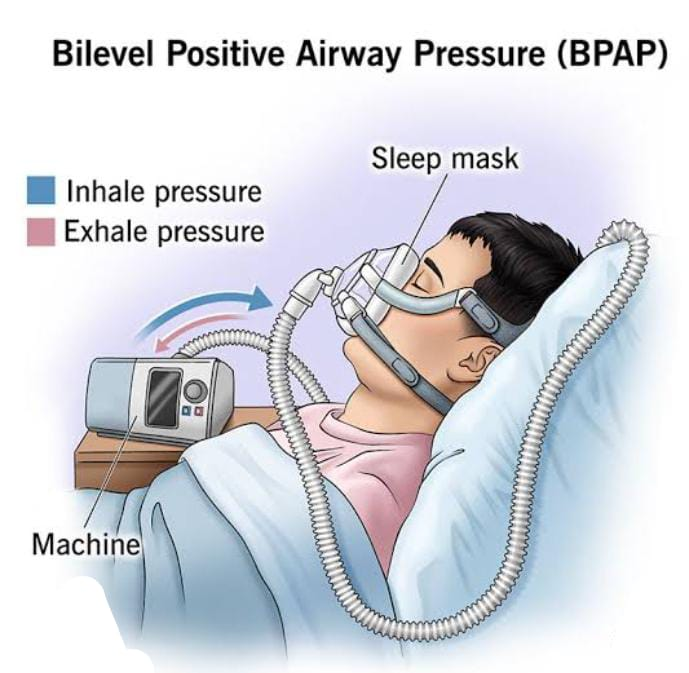
A BiPAP device is similar to a CPAP device in that it is used to prevent the airway from collapsing, but the BiPAP device has two pressure settings. One setting is used during inhalation and a lower pressure setting is used during exhalation. Patients using BiPAP devices in their home environment for obstructive sleep apnea often find these two pressures more tolerable because they do not have to exhale against the continuous pressure. In acute-care settings, BiPAP devices are also used as a noninvasive alternative to intubation and mechanical ventilation for patients in acute respiratory distress.
General instructions:
- The patient should be instructed to use lighting, matches, or Explain the dangers of smoking cigarettes, cigars, and pipes. Make sure the patient does not have any matches, cigarettes, or smoking materials on the bedside table.
- Ensure that a warning sign (Oxygen- No Smoking) is posted on the patient’s door and above the patient’s bed.
- Do not use oil on oxygen equipment. (Rationale: Oil can ignite if exposed to oxygen).
- With all oxygen delivery systems, oxygen is turned on before the mask is applied to the patient.
- Ensure that the tubing is always patent and that the equipment is functioning properly.
- Maintain a continuous oxygen concentration for the patient to breathe and monitor the equipment at regular intervals.
- Respiratory depression or Watch for distress.
- Encouraging or assisting the patient to move in bed. (Rational: To prevent hypostatic pneumonia or circulatory difficulties) Many patients are reluctant to move because they are afraid of oxygen apparatus.
- Provide frequent mouth care and ensure that the oxygen has adequate humidification.
After care of the patient and the articles:
- Stay with the patient.
- Keep the patient warm and comfortable.
- Observe the patient’s vital signs or symptoms and evaluate the patient’s progress.
- Observe the patient for any changes in symptoms after removing the O2 inhaler.
- Then record the date and time properly.
- Request for arterial blood gas analysis.
- Place all articles in the utility room.
- Clean the nasal catheter with cold water, then warm, soapy water and finally clean water. Boil it, store and send it for sterilization.
O2 inhalation Hazards of O2 inhalation:
1) Infection.
2) Combustion (fire) – O₂ supports combustion.
3) Drying of the mucus membranes of the respiratory tract.
4) O₂ Toxicity (O₂ toxicity).
5) Atelectasis.
6) Oxygen induced apnea.
7) Retrolental fibroplasia.
8) Asphyxia.
Inhalation:

Inhalation is defined as the taking of air or other vapors into the lungs through the mouth or nose. It is the breathing in of vapors containing medication. Medication can be added to the vaporizer as a liquid, then converted to vapor or prepared as a vapor.
It can be simple normal saline.
In case of Drugs:
Drugs can be administered by inhalation for systemic or local effects. Systemic effects occur immediately due to the large surface area of the lungs and the rich supply of blood vessels. Drugs used for local effects may be in the form of medicated steam and fumes, although fumes are rarely used.
Type of inhalation:
There are generally two types of inhalation:
1) Dry inhalation
2) Moist Inhalation
1) Dry inhalation:
Dry inhalation: Inhalation of fumes from volatile drugs is known as dry inhalation. Eg: Ether, Chloroform, Nitrous Oxide, Menthol, Eucalyptus, Spirit, Ammonia.
2) Moist Inhalation:
Inhalation of plain steam or drug-impregnated steam is known as moist inhalation. Moist steam inhalation is defined as the use of moist heat to relieve congestion in the lungs and helps in liquefying secretions, e.g. Steam, Tincture Benzoic.
Purpose:
- To relieve inflammation in acute colds and sinusitis.
- To relieve irritation by moistening in bronchitis and whooping cough.
- In the respiratory tract To provide antiseptic action.
- To provide warm and moist air after operations (Ex: tracheostomy).
- To soften thick and tenacious secretions.
- To relieve phlegm.
General instructions:
- The temperature of the water should be between 120 and 160 °F or 54.5 – 76.7 °C.
- The water in the inhaler should be below the spout to prevent scaling.
- The spout of the inhaler should be positioned so that the patient cannot touch it or bring their face too close to it.
- Keep the patient warm and dry before, during, and after inhalation. Avoid drafts.
- When using volatile drugs, keep the eyes closed to prevent irritation from the drug.
- Keep the patient under close observation throughout the procedure.
Preliminary Assessment:
- Check the doctor’s order for any specific instructions.
- Check the patient’s general condition and diagnosis.
- Check the self-care ability to follow instructions.
- Check the type, duration, and medication for inhalation.
- Keep articles available in the unit.
Preparation of patient and environment:
- Explain the procedure to the patient.
- Allow the patient to empty the bowel and bladder if necessary. Provide a bedpan or urinal to a bedridden patient.
- Provide the patient with a Fowler position using a backrest, cardiac table, and extra pillows.
- Close doors and windows to prevent drafts and turn off fans.
- Keep a sputum mug near the patient.
- Provide a face towel to remove sweat from the face during inhalation. To do.
- Before using the mouthpiece, boil it properly and let it cool.
- Arrange the articles properly on the bedside.
- If you want to use volatile drugs, then close the ice so that irritation caused by volatile drugs can be prevented because volatile drugs can irritate.
Equipments:

- A tray that contains:
- Nelson’s Inhaler,
- Large Bowl,
- Face Towel & Patient Towel – 1,
- Sheet,
- Goose Piece,
- Cotton Swab,
- Swab Stick,
- Kidney Tray & Paper bag.
Procedure:
- Proper hand washing.
Open the mouthpiece of the steam inhaler and cover it with sterile gauze and attach it to the inhaler. - Add medication if necessary or as directed by the physician.
- Close the inhaler through the mouthpiece and bring it to the patient’s bedside.
- Keep the spout away from the patient’s face and remove the cotton ball.
- Instruct the patient to take a deep breath through the mouth and exhale through the nose.
- Continue this procedure for 15 to 20 minutes.
- Keep the patient warm to prevent chilling.
- Provide chest physiotherapy to the patient and encourage the patient to cough up sputum.
After care:
- Remove the inhaler from the patient.
Use a face towel to wipe the perspiration from the patient’s face. - Remove the accessory and provide the patient with a comfortable position.
- Replace the articles after cleaning.
- Proper hand washing.
- Record the procedure in the nurse’s record sheet.
Suctioning:
Introduction:
Suctioning is used to clear the patient’s airway when the client is unable to clear secretions from the respiratory tract with cuffing. Primary suctioning techniques include Oropharyngeal, Nasopharyngeal Suctioning, Orotracheal and Nasotracheal Suctioning.
Definition:
( i ) Oropharyngeal Suctioning:
Oropharyngeal suctioning is the process of removing secretions from the oral cavity and pharynx. This process is performed when the client is able to cough effectively but cannot effectively clear the secretions through expectoration. Unable or swallowing phlegm.
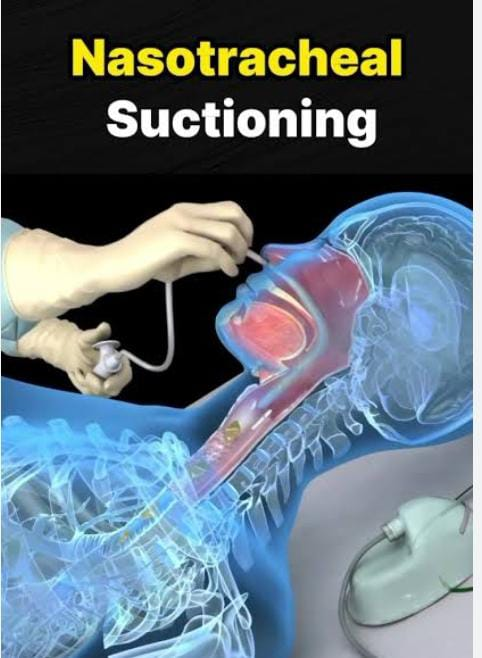
( ii ) Orotracheal and Nasotracheal Suctionning:
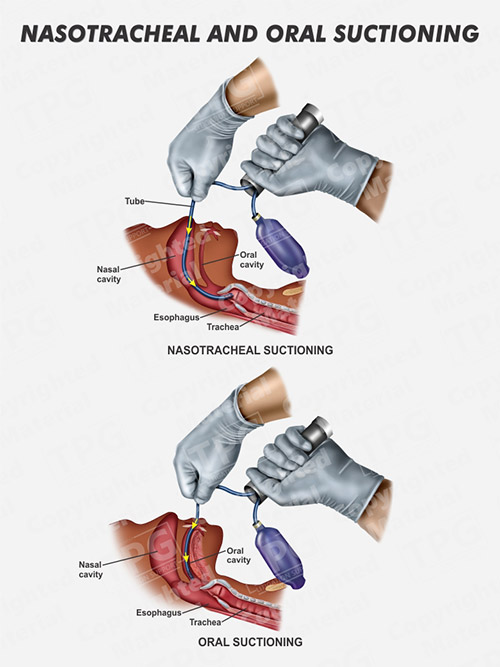
This is necessary when the client is unable to clear pulmonary secretions and does not have an artificial airway. Artificial airways include endotracheal, nasotracheal, or tracheostomy tubes.
Oral Airway:
The oral airway is the simplest type of artificial airway. It prevents tracheal obstructions caused by displacement of the tongue into the oropharynx in an unconscious client. Indications for an artificial airway include decreased level of consciousness, airway obstruction, mechanical ventilation, and removal of tracheal secretions.
It promotes orotracheal suctioning in an unconscious client. The suction catheter is passed through the center of the airway or from its side to gain access to the trachea.
Tracheal Airway:
Artificial tracheal airways include endotracheal, nasotracheal types. Due to which easy access can be obtained for deep tracheal suctioning. Removal of tracheal secretions should be done following aseptic technique. In asepsis, a freshly opened sterile catheter is handled with sterile gloves. Effective suctioning removes secretions from the right and left midsternal bronchi.
Purpose:
To remove secretions that obstruct the airway.
To facilitate ventilation.
To obtain secretions for diagnostic purposes.
To prevent infections if there is accumulation of secretions.
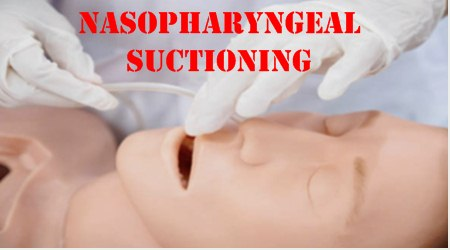
(iii) Oropharyngeal and Nasopharyngeal Suctioning:
Articles:
Appropriate size sterile suction catheter/smallest diameter (14- 18 Fr) that can effectively remove secretions.
Portable or wall suctioning with connecting tube or Y-connector.
Sterile water/normal saline in bowl.
Face mask.
Gloves.
Towel or waterproof pad.
Tongue depressor.
Nasal or oral airway.
Procedure:
Assess signs and symptoms that indicate the presence of upper airway secretions, such as gurgling respirations, restlessness, vomiting at the mouth, and drooling.
Explain the procedure to the client and their relatives.
Prepare and maintain necessary equipment and supplies.
Maintain patient privacy.
Provide the patient with a semi-recumbent position. Turn the head to one side. Provide the client with a semi-recumbent position and hyperextend the neck.
Provide the unconscious client with a side-lying position and face toward the nurse.
Place a towel on the pillow or under the chin.
Select the proper suction pressure for the suction unit. For a wall suction unit:
Adults 110-150 mm of Hg.
Children 95-110 mm of Hg.
Infants 50-95 mm of Hg.
Wash hands.
Wear gloves.
Using a gloved hand, attach the catheter to the connecting tubing of the suction machine, with the coiled catheter.
Measure the approximate distance between the client’s earlobe and the tip of the nose and place the forefinger at that point.
Moisten the distal 6-8 cm (3-4″) tip of the catheter with sterile solution.
A ) For nasopharyngeal suction, gently insert the catheter into the nostril. Guide the catheter medically along the floor of the nasal cavity.
b) For oropharyngeal suctioning, gently insert the catheter into one side of the mouth, and guide the catheter into the oropharynx. Do not apply suction during insertion.
When withdrawing, cover the suction part with the thumb, gently rotate it and withdraw it.
In the lungs, this procedure should not take more than 15 seconds.
Flush the catheter with sterile solutions and apply suction.
Nasopharynx and Oropharynx After suctioning, suck out secretions from the mouth or under the tongue.
After suctioning, wash hands properly and discard the used catheter.
Record the amount of secretions, consistency, color, order of secretions, and the client’s response to the procedure.
Note on orotracheal and nasotracheal suctioning:
Orotracheal or nasotracheal suctioning is required when the client is unable to cough and does not have an artificial airway.
The catheter is passed into the trachea through the mouth or nose.
This procedure is similar to nasopharyngeal suctioning.
This procedure is similar to nasopharyngeal suctioning. Same but the tip of the catheter is advanced into the client to suction the trachea.
The entire procedure from passing the catheter to removing it should not take more than 15 seconds because oxygen does not reach the lungs during suction.