ENGLISH-FON-GNM UNIT-4- PART-2 PHYSIOLOGICAL ASSESSMENT-UPLOAD
Vital sign (vital sign)

• A vital sign is a type of indicator that provides information about the physiological status of the body and also indicates the body’s response to the physical environment and psychological stressors.
• Vital signs mainly include 4 parameters: TPR BP ( Temperature , Pulse, Respiration rate , Blood pressure )
1 Temperature
2 Pulse
3 Respiration rate (Respiration rate)
4 Blood pressure
• Nowadays Pain is known as the fifth vital sign.
• Vital sign is also known as Cardinal sign.
• Vital sign It is an important parameter that describes the physiological status of the body.
• Vital signs are key measurements of the basic functions of the body.
• Any changes or abnormalities in the vital organs of the body are reflected by vital signs.
• Vital signs are a part of physical assessment. The nurse who measures.
Write down purpose of assessment of vital sign (रित्र डॉन प्रप्स ओसेम्टल सेन्ट)
• To monitor overall health.
• To determine the health status of the client.
• To determine early signs of medical conditions.
• To check the client’s response to treatment.
• To identify life-threatening conditions (shock, cardiac arrest)
• To establish baseline measurements.
1) Temperature

• Body temperature is the balance between heat production and heat loss.
• Heat production is known as thermogenesis.
• While heat loss is known as thermolysis.
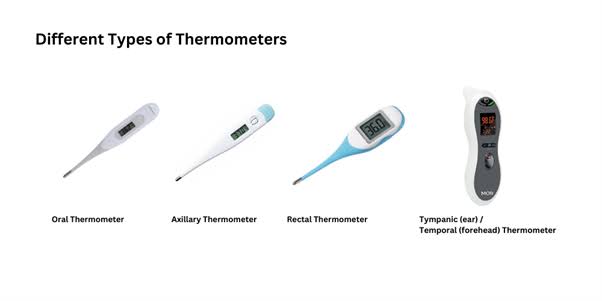
• Thermometers are used to measure temperature. They come in different types.

Write down types of body temperature Temperature)
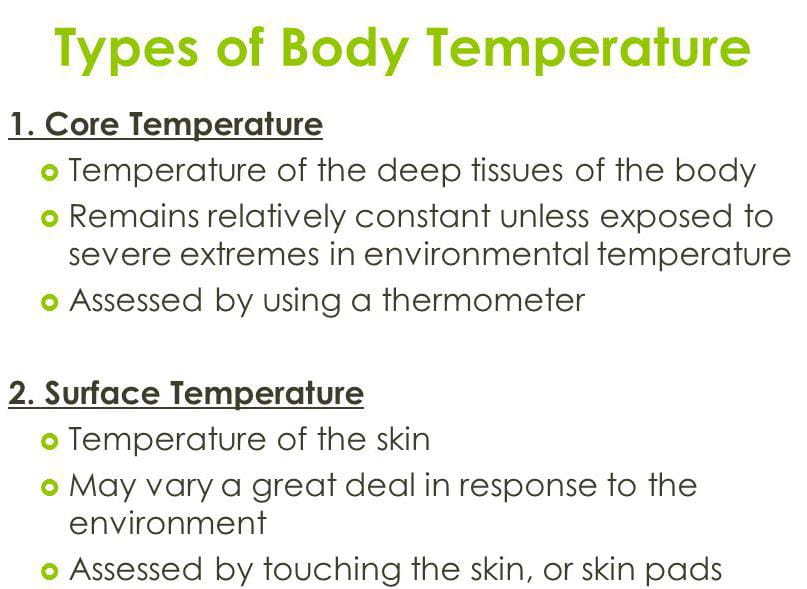
There are mainly two types of body temperature:
1) Surface body temperature
2) Core body temperature
1) Surface body temperature

• Surface body temperature measures the temperature of the body’s surface, i.e. skin, subcutaneous tissue, and fat.
• Such as the temperature of the axilla or forehead.
• Surface body temperature is less reliable because it is affected by the surrounding environment.
2) Core body temperature
• Core body temperature measures the temperature of the body’s deep tissues.
• Temperatures taken from the rectum, oral cavity, tympanic membrane, etc.
• This temperature is the most important and most reliable.
Write down factor affecting temperature
• Age
Age is an important factor affecting body temperature. Since the thermoregulation center in a newborn baby is immature, its body temperature fluctuates rapidly. Similarly, the thermoregulation center is found to be ineffective in old age people and subcutaneous fat loss is seen in old age people. In addition, due to decreased activity and decreased metabolic rate, body temperature is sensitive to extreme temperatures. Exercise Exercise increases muscle activity, which leads to the utilization or breakdown of carbohydrates and fats, which increases metabolism and also increases heat production. Which causes an increase in body temperature.
• Environment
Body temperature is affected by the environment. Especially in young children and the old age, body temperature is affected by the environment because thermoregulation control is not effective. Therefore, body temperature decreases in cold weather while body temperature increases in hot weather.
• Hormonal level
Body temperature also fluctuates due to hormones. Due to the decrease in the level of the hormone progesterone, there is a decrease in body temperature, while due to the increase in the level of progesterone, there is an increase in body temperature. Therefore, due to the increase in the level of progesterone during the menstrual cycle, body temperature increases. Therefore, the temperature fluctuates more in females than males.
• Stress
Physical or emotional stress activates the sympathetic nervous system, which causes changes in hormonal and neural stimulation. These physiological changes increase the metabolic rate, which in turn increases heat production and increases body temperature.
• Circadian rhythm
Body temperature changes by 0.5-1°C throughout the day. Body temperature is lowest around 4 am while body temperature is highest between 6 pm and midnight.
Axillary temperature

• This is a method of surface body temperature.
• This is the safest and most non-invasive method.
• The axillary site is the most common site for children.
• Normal temperature: 97.6°F (36.5°C)
• Axillary temperature is 1°F lower than oral temperature. When it is 2°F lower than the rectal temperature.
Indication
• Convulsion
• Mentally ill patient
• Unconscious
• Cough
• This route is preferred when oral temperature is contraindicated.
Contraindication
• Mastectomy (operative side avoided)
• Extreme perspiration
Advantages (Advantages)
• Less discomfort
• Less chance of cross infection
• Do not affect hot or cold drinks
Disadvantages (Disadvantages)
• Give False Reading
• Chances of being affected by external environment
• Give False Reading Due to Perspiration
Procedure (Procedure)
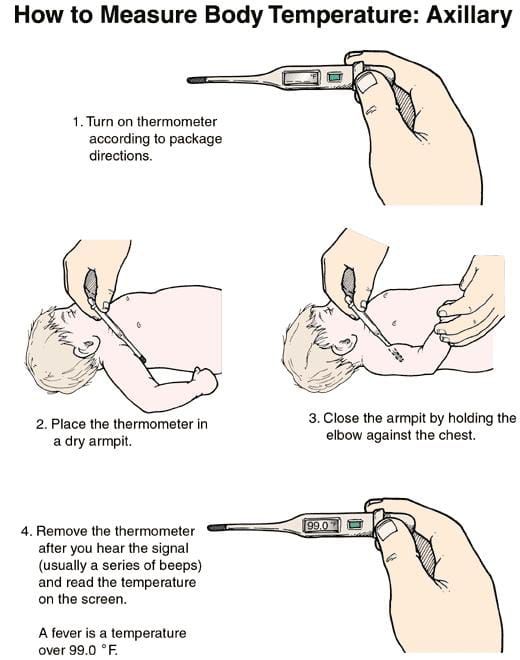
Identify the patient.
- Explain the procedure.
- Arrange the necessary articles at the patient’s bedside.
- Wash hands.
- Provide a comfortable position to the patient.
- Check whether the patient’s axilla is dry or not.
- If the axilla is moist, dry it with a dry cloth or napkin.
- Hold the thermometer with the thumb and forefinger and shake it. So that the mercury comes to its normal level. (Bring it down to 35°C)
- Then place the thermometer in the axilla in the vertical direction.
- Keep the arm down and keep it tightly against the body and keep the forearm in a resting position on the chest. So that it can be prevented from coming into contact with the external environment.
- Place the thermometer there for 3-5 min.
- Remove the thermometer and wipe it gently with a stem to bulb swab in a twisting motion.
- Then hold the thermometer at eye level and check the reading.
- Finally, clean the thermometer stem to bulb with a soapy swab and then clean it with a wet swab.
- Provide a comfortable position to the patient.
- Replace articles.
- Wash hands.
- Record the temperature.
Oral temperature

- Oral temperature is taken near the blood vessels under the tongue.
- This is the most common, convenient and comfortable method.
- Normal temperature: 98.6°F (37°C)
- Oral temperature is checked 15-20 minutes after eating a hot or cold food. So that an accurate temperature measurement can be made.
Advantages
- No need for privacy
- Give reliable and accurate readings (due to the good blood supply under the tongue and the bulb not coming in contact with the external environment, it gives accurate readings)
- The thermometer can be easily held under the tongue.
Disadvantages
- The chances of the thermometer breaking down due to biting increase.
- If the disinfectant is not removed perfectly, it will give a bad test.
- If the thermometer is not disinfected perfectly, it can cause cross-infection.
- If the thermometer is not placed properly and comes into contact with the environment, it can give false readings.
Contraindication
- Oral surgery
- Mouth breather
- Dyspnea
- Frequent cough
- Convulsions, seizures
- Unconscious patient
- Mentally retarded
- Children <6 years
- Nausea, vomiting
Procedure
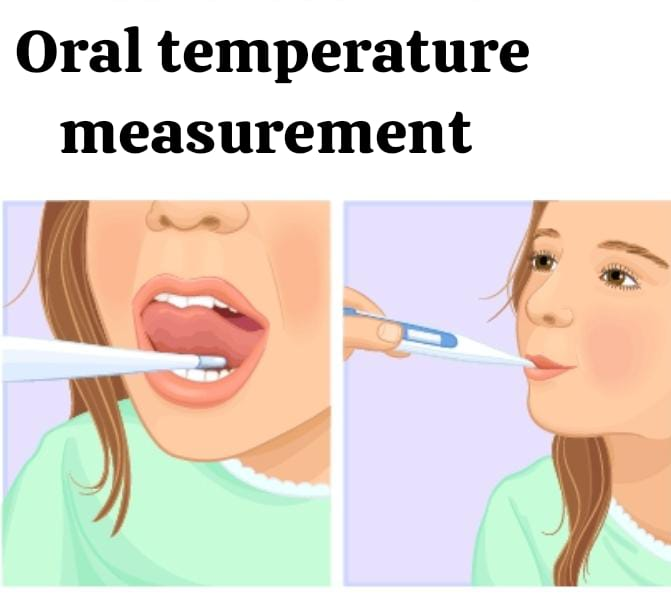
- Identify the patient.
- Explain the procedure.
- Arrange the necessary articles at the patient’s bedside.
- Wash hands.
- Provide the patient with a comfortable position.
- Ask the patient to open his mouth.
- Hold and shake the thermometer with the thumb and forefinger. So that the mercury comes to its normal level. (bring it down to 35°C)
- Then place the bulb of the thermometer under the patient’s tongue.
- Ask the patient to close the lips but not to close the teeth.
- Ask the thermometer to hold there for 2-3 min.
- Remove the thermometer and wipe it gently with a stem to bulb swab in a twisting motion.
- Then hold the thermometer at eye level and check the reading.
- Finally, clean the thermometer from stem to bulb with a soapy swab and then clean it with a wet swab.
- Provide the patient with a comfortable position.
- Replace the articles.
- Wash hands.
- Recording temperature.
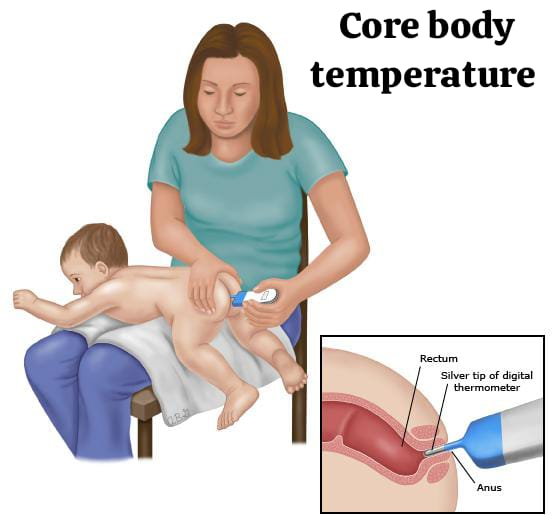
Rectal temperature

• Rectal site is a method of measuring core body temperature.
Rectal temperature is the most reliable and most accurate method.
- Normal temperature: 99.6° F (37.5° C)
- Rectal temperature is 1° F higher than oral temperature and 2° F higher than axillary temperature.
- This method is mainly used in children younger than 6 years.
Indication :
- Oral or Nasal Surgery
- Respiratory Obstruction (Mouth Breather)
- Mouth Disorder
- Unconscious, Mentally Retarded Patient
- Convulsion Patient
- Young, Restless and Irritable Children
Contraindication :
- Anal or Rectal Surgery (Anal Fissure, Hemorrhoid)
- Diarrhea
- Constipation
- Quadriplegic Patient
- Cardiac Patient (Vagus Nerve Stimulation May Cause Bradycardia and Syncope Hence Rectal Temperature is Not Taken in Cardiac Patient)
Advantages
- Most Reliable and Accurate Method
- Note Affected by external environment
Disadvantages
- Need privacy
- Need to lubricate the bulb
- Contaminated to the face
Procedure

- Identify the patient.
- Explain the procedure.
- Arrange the necessary articles at the patient’s bedside.
- Wash hands.
- Provide privacy.
- Provide the patient with a lateral or prone position.
- Shake the thermometer before inserting it so that the reading can be brought to the normal value.
- Lubricate the bulb part of the thermometer and the part up to one inch above it with a water-soluble jelly. (So that the mucous membrane of the anus can be protected from friction and trauma)
- Insert the rectal thermometer in the posterior and downward direction.
- Insert the thermometer up to 1-1.5 inches in adults and up to 0.5-1 inch in infants.
- During this, ask the patient to exhale and inhale deeply.
- Do not use any force to insert the thermometer.
- Hold the thermometer there for two minutes.
- Then remove the thermometer gently and wipe it gently with the help of a stem to bulb swab. So that the secretions present in it can be removed.
- Then keep the thermometer at eye level and check the reading.
- Finally, clean the thermometer from stem to bulb with a soapy swab and then clean it with a wet swab.
- Provide a comfortable position to the patient.
- Replace the article.
- Wash hands.
- Record the temperature.
Tympanic membrane temperature

- Tympanic temperature is an example of core body temperature.
- This route provides results within 2-3 sec, so this method is the fastest method of temperature measurement.
- Therefore, this method is used to measure temperature in pediatric, intensive care units.
- Normal Temperature: 99.6°F
Indication
- In ICU Setting
- In Emergency Condition
Contraindication
- Perforated Ear Drum
- Ear Infection
- Ear Surgery
Procedure
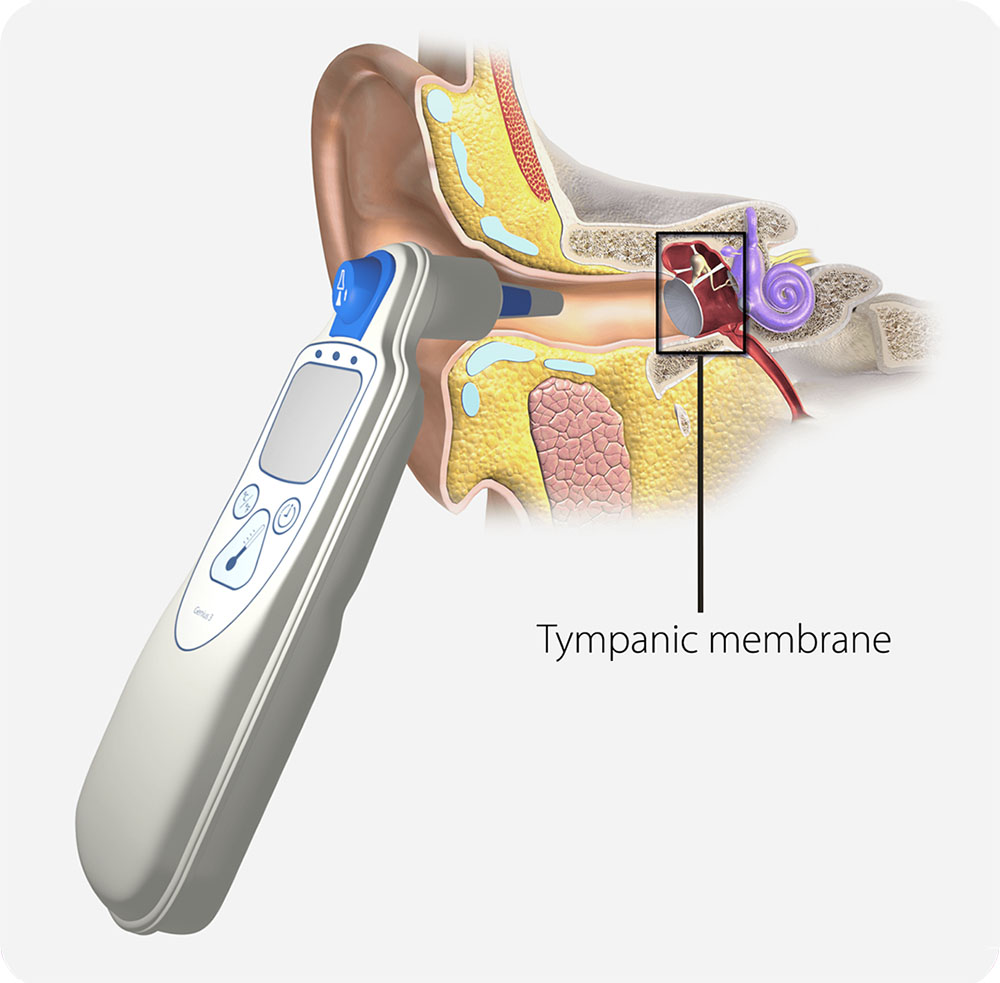
- Identify the patient.
- Explain the procedure.
- Arrange necessary articles at the patient’s bedside.
- Wash hands.
- Hold the thermometer in the dominant hand.
- Use the patient’s ear on the same side as the hand holding the thermometer, i.e. if the thermometer is in the right hand, use the patient’s right ear.
- Now grasp the patient’s external ear from the midpoint with the non-dominant hand and pull the external ear up and back.
- If it is a child, then pull the external ear down and back.
- Now slowly insert the thermometer probe in a back-forth motion. Insert it until it reaches the seal of the ear canal.
- After keeping the probe in the correct position, activate the button there.
- After the temperature is measured, a sound or flash light is seen from it.
- From this, remove the thermometer slowly.
- Read the temperature.
- Provide a comfortable position for the patient.
- Then discard the probe cover.
- Replace the articles.
- Wash hands.
- Recording temperature.
2) Pulse


• Pulse is the rhythmic pulsation of an artery that occurs in response to the cardiac cycle.
• Pulse is the rhythmic dilation of an artery that occurs due to the opening and closing of the aortic valve.
• Pulse is also known as heart rate.
• Pulse rate is a number that denotes the number of times the heart contracts in one minute.
• The pulse is heard or felt where the artery crosses the bony surface area.
• The normal pulse rate in an adult is 60-100/min, meaning that an average pulse of 72/min is seen in a normal adult.
• Infants have a pulse rate of 120-140/min, while children have a pulse rate of approximately 100/min.
• Pulse is mainly assessed using palpation and auscultation methods.
• In which gentle pressure is applied to the pulse site with the help of 3 middle fingertips (index, middle and ring finger) and the pulse is palpated.
• Pulse is not palpated with the thumb because the thumb has its own sensation.
• Pulses located in the periphery of the body are known as peripheral pulse. Such as the arteries in the foot, neck
• The pulse near the apex of the heart is called the apical pulse.
Write down characteristics of pulse
1) Rate
2) Rhythm
3) Volume (Volume)
4) Elasticity
5) Eqality
1) Rate
Rate is a type of number that denotes the number of times the heart contracts in one minute. In adults, the normal pulse rate is 60-100 bpm, with an average of 72 bpm.
2) Rhythm
Rhythm is the regular pattern of the pulse for a specific time frame, i.e. the regularity of the heart rate.
3) Volume
Volume refers to the fullness of the artery or the force of blood during each beat (contraction). That is, the amount of blood ejected by the heart against the artery wall during each beat is known as volume. The amount of blood ejected by the left ventricle during each contraction is known as stroke volume. Which is normally about 70 ml.
4) Elasticity
The ability of the arterial wall to expand and contract is known as elasticity. Normally, the artery is smooth, soft and straight. But with increasing age, there is a decrease in elasticity.
5) Eqality
Eqality means equality. That is, the pulse felt in both the upper limb and the lower limb. In some cases, the pulse is not felt in the affected extremity, such as thrombus formation.
Write down most common pulse site
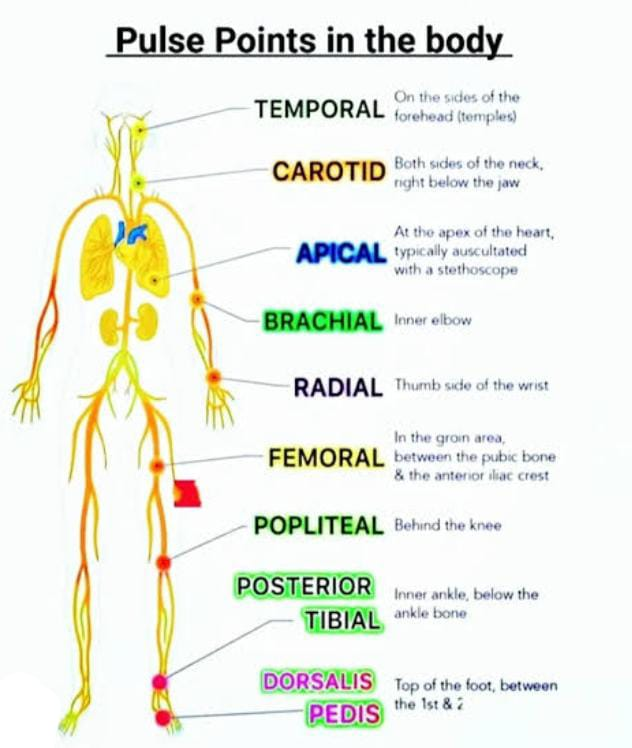
Carotid
The carotid pulse is located on the side of the neck, below the ear tube, in the middle of the angle formed by the trachea and sternocleidomastoid muscles. It can be easily accessed. This pulse is assessed for only 5-10 seconds and both carotid pulses are not assessed simultaneously because palpating both carotid pulses simultaneously interrupts blood flow to the brain.
Temporal
The temporal pulse is located on the lateral side of the eye and above the zygomatic bone.
Brachial
The brachial pulse is located in the antecubital fossa. Which is used to check the pulse during cardiac arrest in infants. Brachial pulse is used to measure BP.
Radial
The radial pulse is located on the inner side of the wrist and under the thumb in the radial bone. The radial pulse is the most common site for pulse assessment. This pulse is used for BP assessment.
Apical
The apical pulse is located on the left side of the chest, towards the left mid-clavicular line, in the 5th intercostal space. It is located below the left nipple. It is auscultated with the help of a stethoscope.
Femoral
The femoral pulse is located below the inguinal fold between the anterior iliac spine and the symphysis pubis. It is used to check the pulse during cardiac arrest.
Popliteal
Popliteal pulse is located in the popliteal fossa. It is located on the side of the medial tendon behind the knee. It is used to check the circulation of the lower extremities. Popliteal pulse is used to check the blood pressure of the lower limb.
Posterior tibial
The posterior tibial artery is located on the inside of the ankle and behind the medial malleolus.
Pedal or dorsalis pedis
The dorsalis pedis is located slightly lateral to the tendon of the big toe on the top of the foot. Which is used to check peripheral circulation, especially foot circulation.
Alterations in pulse
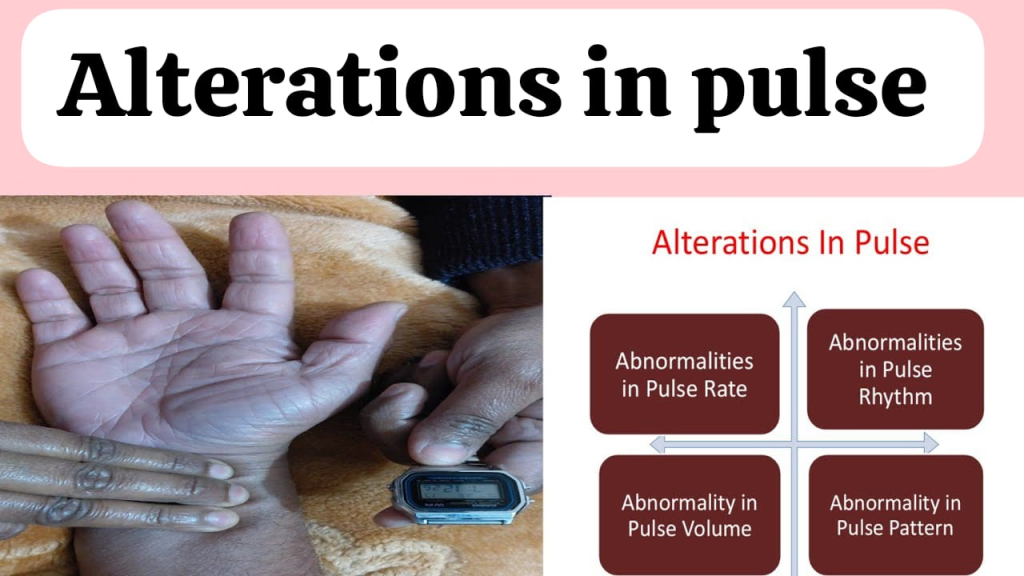
Tachycardia
An increase in pulse rate is known as tachycardia. In which the pulse rate exceeds 100 bpm.
Bradycardia (Bradycardia)
A decrease in pulse rate is known as bradycardia in which the pulse rate falls below 60 bpm.
Pulse deficit (Pulse deficit)
Due to improper contraction, the peripheral pulse is not palpated, which is known as pulse deficit.To detect pulse deficit, the radial pulse and apical pulse are palpated and compared. In which the apical pulse is palpated while the radial pulse is not.
Write down factor affecting pulse
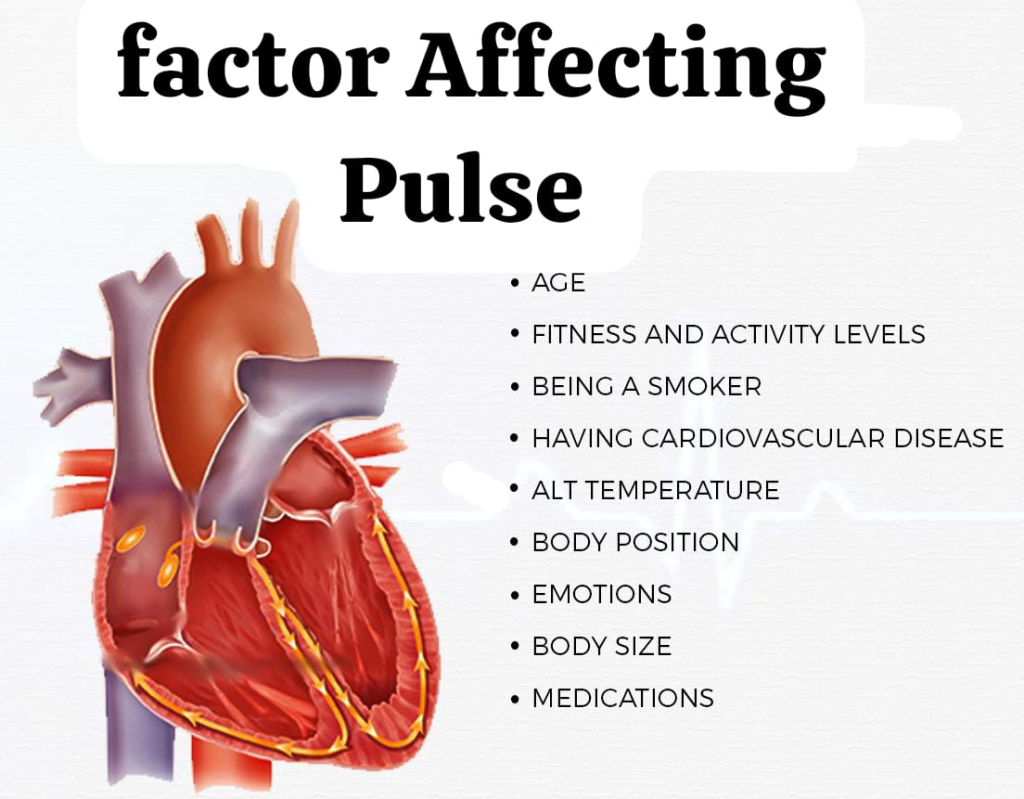
Age
With increasing age, there is a decrease in pulse rate, such as 130-140 bpm in newborns and a decrease with increasing age, and in adults it is 60-100 bpm. That is, the average is 80 bpm.
Sex (sex)
After puberty, the pulse is slightly higher in females than in males.
Exercise (Exercise)
Physical activity or exercise puts a load on the heart, which increases the pulse rate. But in laborers and athletic people, the pulse rate does not increase because the size and strength of the heart of these people increase, and a normal pulse rate is seen in these people.
Temprature
Due to an increase in body temperature, an increase in pulse rate is also seen, just as in fever, body temperature increases, due to which the pulse also increases.
Medication (Medication)
Medications like digoxin, atropine sulfate etc. increase the heart rate. While medicines like beta blockers and adrenaline cause a decrease in the heart rate.
Body position
The pulse rate increases slightly in the standing position.
Stress, anxiety
The pulse rate increases in conditions such as emotional stress and anxiety.
Relaxation & meditation (relaxation and meditation)
Relaxation techniques and meditation can cause a slight decrease in heart rate.
How to assess redial pulse (How to assess radial pulse)

• Wash hands.
• Explain the procedure to the patient.
• Provide the patient with a comfortable sitting or lying down position. Extend the wrist and keep the palm down.
• Then place the first, second and third fingers on the radial artery on the thumb side of the wrist.
• After placing these 3 middle fingers on the radial artery, apply gentle pressure on that place and feel the sensation there.
• If the sensation is felt (if the sensation is not felt, place the finger a little further back) count the pulse for 30 seconds with the help of a watch and multiply it by 2.
• Or count the pulse for one minute.
• Then provide the patient with a comfortable position.
• Record this palpated pulse. If any abnormality is found during palpation, note that too.
• Replace the article and wash your hands last.
3) Respiration (Respiration)
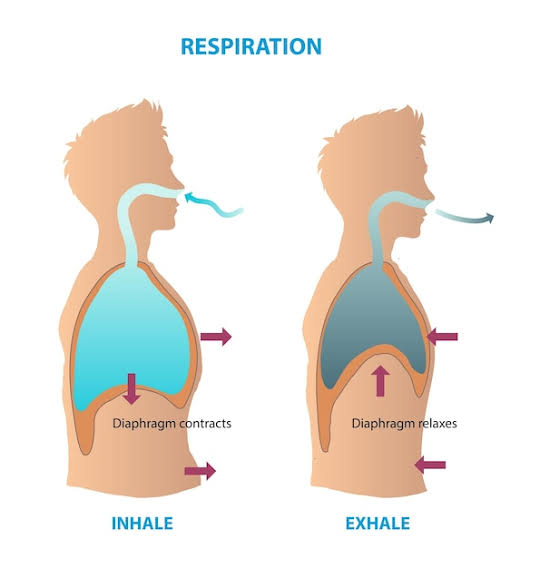
• Respiration is the act of breathing in which oxygen is inhaled and carbon dioxide is exhaled.
• Respiration rate is a number that denotes the number of breaths taken in one minute.
• Respiration is assessed by an inspection method.
• Normal respiration: 12-20 breath/min (in adult)
• Infant: 20-40 breath/min
• Preschool: 20-30 breath/min
• The respiratory regulation center is located in the medulla oblongata.
Write down factor affecting respiration rate
Age (Age)
With increasing age, there is a decrease in the respiration rate. For example, in a newborn, the respiration rate is 30-60 breaths/min, while in an adult it is 12-20 breaths/min.
Exercise (Exercise)
Due to exercise, the demand for O2 in the body increases, which is met by an increase in the respiration rate.
Emotional state
States like stress, anxiety, fear, excitement, etc. activate the sympathetic nervous system, which leads to an increase in respiration.
Medication
Medications such as sedatives, opioids, anesthesia, etc. reduce the respiratory rate.
Temprature
High body temperature as well as high environmental temperature cause an increase in respiration rate.
Altitude
In places with high altitudes, the oxygen level is low, due to which the body compensates by increasing respiration.
Trauma, injury
Due to trauma or injury, the brain stem is impaired and due to this, changes are seen in the respiration rate and rhythm.
Certein condition
In certain conditions such as anemia, sickle cell disease, respiratory conditions and heart conditions, O2 supply decreases, due to which an increase in respiration rate is seen.
Smoking
Long-term smoking damages the lungs, which causes changes in the respiration rate.
Procedure
• Identify the patient.
• Arrange the necessary articles at the patient’s bedside.
• Wash hands.
• After checking the pulse, the respiration rate is checked.
• Observe the chest movement without explaining the procedure to the patient.
• In an adult patient, place the patient’s arm on the chest and observe the movement of the chest up and down for one minute.
• While in an infant, observe the movement of the abdomen.
• Note the respiration rate, rhythm, and depth for one minute.
• Replace articles.
• Wash hands.
• To record respiration rate, rhythm and depth.

4) Blood pressure

• Blood pressure It is the 4th vital sign.
• The force or pressure exerted by the blood against the walls of the arteries is known as blood pressure.
• The force exerted by the blood against the walls of the blood vessels is known as blood pressure.
• There are two types of measurements in blood pressure:Systolic blood pressure and Diastolic blood pressure
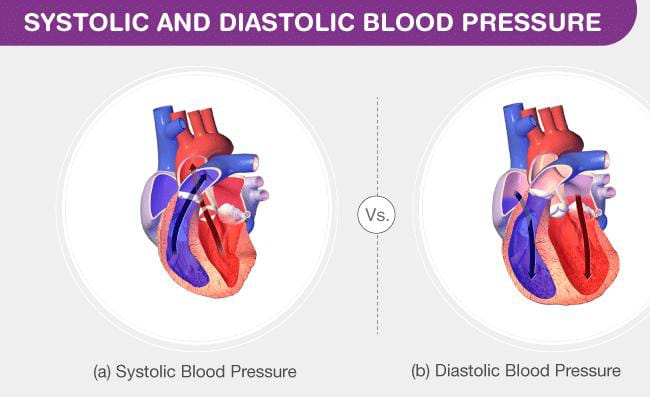
Systolic pressure:
Systole, i.e. the pressure exerted by blood on the artery wall during contraction, is known as systolic pressure.
Diastolic pressure:
The pressure on the artery wall due to blood flow during diastole is known as diastolic pressure, which is mainly found between 60-90 mmHg.
Pulse pressure:
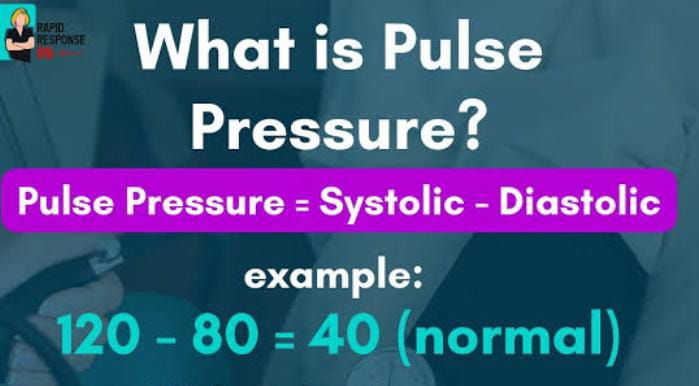
The difference between systolic and diastolic blood pressure is known as pulse pressure. It is usually 30-40 mmHg.
• Normal blood pressure is 120/80 mmHg.
• Blood pressure is measured in millimeters of mercury (mmHg).
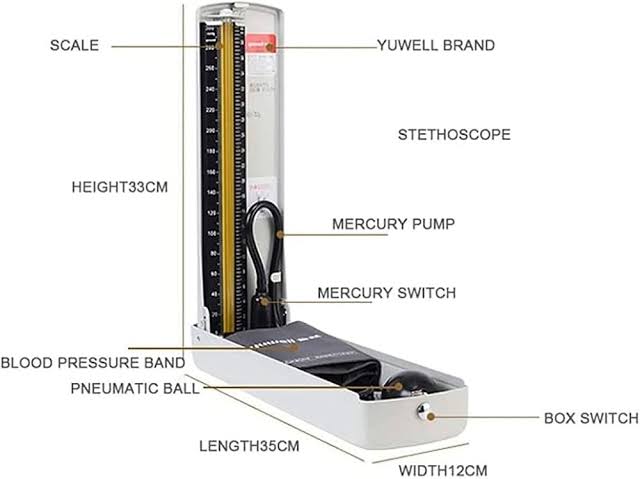
• A sphygmomanometer is used to measure blood pressure.
Alterations in blood pressure
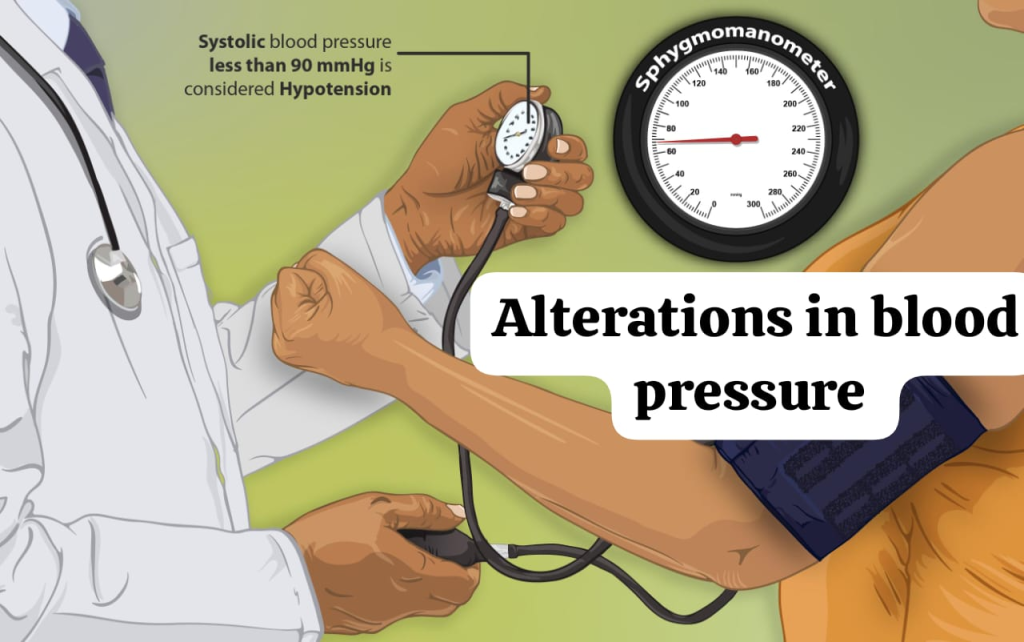
Hypertension (Hypertension) :
Hypertension means abnormally high blood pressure. When even after measuring blood pressure for 3 consecutive times, if systolic blood pressure is found to be more than 140 mmHg and diastolic blood pressure is found to be more than 90 mmHg, then it is known as hypertension.
Hypotension (hypotension):
Hypotension means a decrease in blood pressure. Hypotension is characterized by a systolic blood pressure of less than 90 mmHg and a diastolic blood pressure of less than 60 mmHg.
Orthostatic hypotension:
Orthostatic hypotension is also known as postural hypotension, in which a person experiences a significant drop in blood pressure when they get up from a lying or sitting position to an upright or standing position, which is known as orthostatic hypotension.
Write determinants of blood pressure
Blood pressure is determined by many factors, which are as follows.
• Cardiac output
• Peripheral vascular resistance
• Blood volume
• Elasticity of arteries
• Viscosity of blood
• Autonomic Nervous System Activity
• Hormonal Influence
• Gravity and body position
Write factors affecting blood pressure
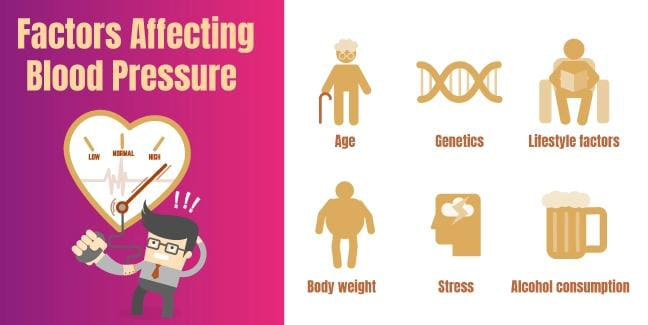
Age
As age increases, blood pressure also increases because blood vessels lose their elasticity and become stiff. Which causes an increase in blood pressure.
Genetics
People with a family history of high blood pressure are at increased risk of developing hypertension.
Gender
Blood pressure is higher in males than females after puberty, while blood pressure in females after menopause It is more common.
Weight
High blood pressure is more common in overweight and obese patients.
Ethnicity
High blood pressure is more common in African Americans than in European Americans.
Diet
High blood pressure can be seen in patients who consume high sodium diet, low potassium diet, fatty diet as well as alcohol, cocaine, caffeine.
Exercise / physical activity
Hypertension is more common in people with a sedentary lifestyle. The chances increase. People who are physically active have a reduced risk of developing hypertension.
Smoking
Chronic smoking causes damage to blood vessels and can lead to high blood pressure.
Emotional state
Chronic Stress, anxiety, fear etc. affect blood pressure.
Drug / medications
Medications like birth control pills, opioid analgesics, decongestants etc. affect blood pressure.
Temperature
Blood pressure varies with temperature. For example, people living in cold weather have slightly higher blood pressure, while people living in warm weather have slightly lower blood pressure.
Procedure

• Identify the patient.
• Arrange necessary articles at the patient’s bedside.
• Wash hands.
• Explain the procedure to the patient.
• Provide the patient with a sitting or supine position.
• If the patient has exercised, walked or smoked, then check his blood pressure after 30 minutes. Because due to this, an increase in blood pressure is observed.
• Check whether the mercury in the sphygmomanometer is at zero level or not. If it is not at zero level, then bring it to zero level and keep it at eye level.
• Keep in mind that the arm should be at heart level.
• Mostly use the left hand to measure BP.
• Attach the BP cuff 2.5 cm above the antecubital fossa and 2-3 fingers above the elbow.
• The BP cuff must be deflated.
• The BP cuff must be of the appropriate size. Because a cuff that is too wide can give false low readings, while a cuff that is too narrow can give false high readings.
• Palpate the brachial artery with the help of the finger tip.
• Then place the diaphragm part of the stethoscope on that place and hold it with the thumb and index finger and place the earpiece of the stethoscope in the ear.
• Then slowly inflate the cuff with the help of the other hand. During this time, the pulse becomes palpable and disappears.
• When the pulse reappears, quickly inflate the bulb to 30 mmHg.
• Then slowly deflate the bulb at a rate of 2-3 mmHg/sec.
• When the sound is heard / the pulse reappears, check the reading on the mercury scale and note it. This reading is known as the systolic blood pressure.
• Then deflate the continuous bulb slowly. Deflate slowly until the sound disappears.
• When the sound disappears, check the reading on the mercury scale. Which denotes the diastolic blood pressure.
• Deflate the cuff quickly after hearing the last sound evenly.
• Remove the cuff.
• If a false reading occurs, check the blood pressure again after five minutes.
• Provide the patient with a comfortable position.
• To replace articles.
• To wash hands.
• To record blood pressure.
