ENGLISH-FON-GNM UNIT-4 PART-1 PHYSICAL ASSESSMENT-UPLOAD
Physical assessment
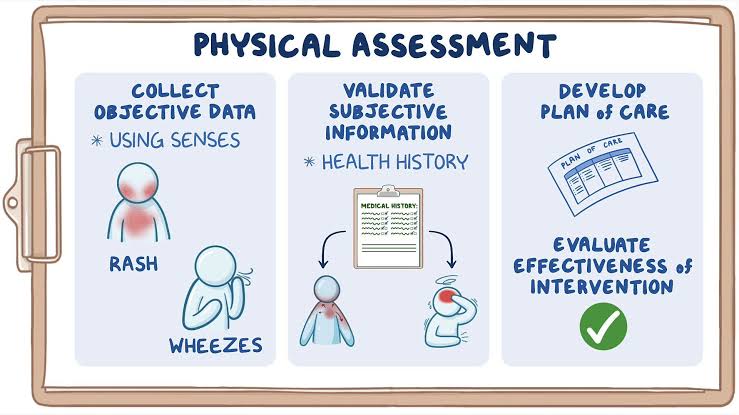
• Physical assessment is a systematic process in which objective information is collected by directly observing the patient or through examination techniques.
• Physical assessment is a systematic process used by health care professionals to evaluate the body and its function.
• In which data is collected about the physical condition of the patient using inspection, palpation, percussion and auscultation methods.
Write down purpose of physical assessment
• To establish a baseline.
• To collect physical and mental data of the patient.
• To collect data systematically.
• To identify current health problems.
• To detect diseases in their early stages.
• To identify the cause of the disease.
• To monitor changes in the patient’s health status.
• To develop a care plan.
• To contribute to medical research.
Health history

• Health history means systematic collection of subjective data
• Health history collects the patient’s health-related subjective data. This data is followed in chronological order.
Write down purpose of health history

• To collect subjective data from the patient
• To understand the patient’s current and past medical issues
• To develop a nursing diagnosis
• To establish a baseline
• To improve communication
Write down components or format of health history

1) Biographical Data
2) Chief Complain
3) History of Present Illness
4) Past health history
5) Family history
6) Environmental history
7) Current health information
8) Psychosocial History
9) Review of System
→
1) Biographic data
• First of all, the biographical data of the patient is collected.
• In which the basic personal information of the patient is collected.
• This data is collected during the initial assessment. In which the following information is collected:
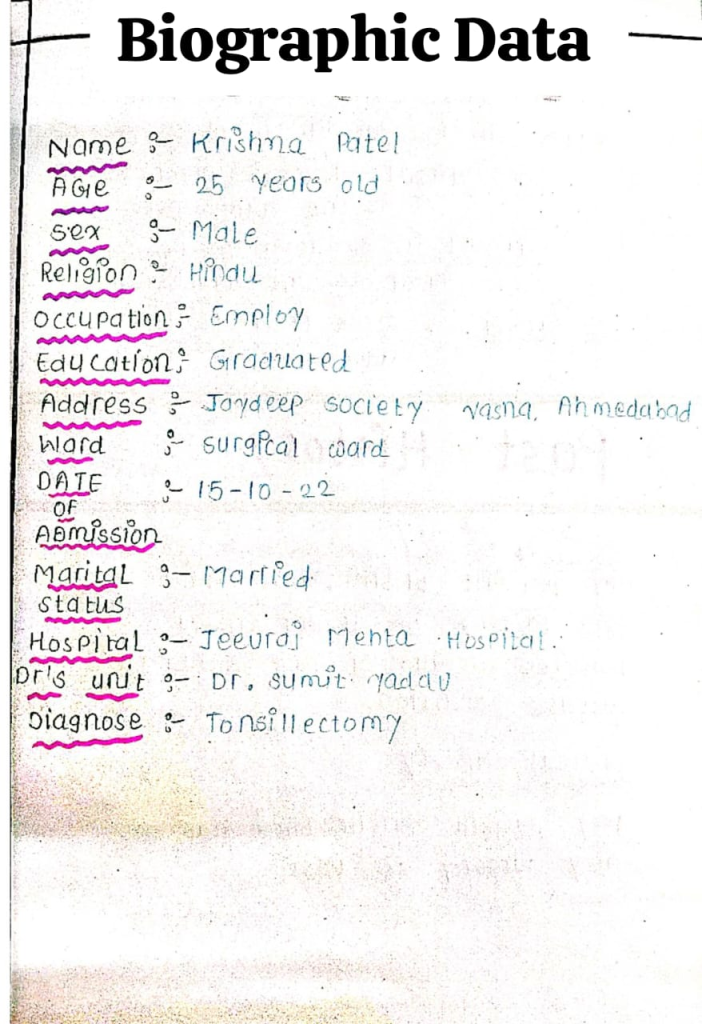
Name
Age
Gender
IPD number
Education
Occupation
Marital status
Religion
Address
Ward
Date of admission
Diagnosis
Doctor name
2) Chief complaint

- Chief complaint is a type of brief statement that shows the primary reason for the patient to be hospitalized.
- Which the patient describes in his own words. This chief complaint is arranged according to chronological order.
- In which after writing the name of the patient, he comes to the civil hospital and his chief complaint is written as follows.
For example,
Rameshbhai came to civil hospital, Rajkot on with the chief complaints of :
Fever × 3 days
Headache × 3 days
Cough × 5 days
Weakness × 10 days
3) History of present illness
- In present illness, the patient’s chief complaint is collected in some depth. In which relevant and essential data are collected on the chief complaint.
- In which information about factors like onset, duration, frequency, location, quality, quantity, alleviating factors, aggressive factors etc. is collected.
4) Past health history

- In past health history, information about the patient’s previous health condition, surgery is collected.
- So that it can be correlated with the present history. Past health history includes the following aspects:
- Medical conditions
- Surgery
- Allergy
- Childhood illness
- Immunization
- Hospitalization
- Trauma-injury-accident
- Medication
- Obstetric and gynecological history (for female)
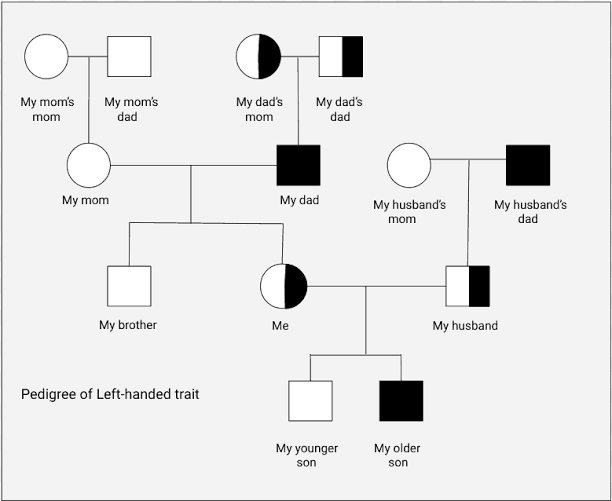
5) Family history

- Family history collects information about the patient’s family members.
- In which information like family type, number of family members, income, hereditary illness etc. is collected.
- Because some conditions are seen due to genetics or environmental factors. Such as diabetes, hypertension, thalassemia, cancer etc.
- In family history, a family tree is drawn in which all the family members of the patient’s house are mentioned and a family table is also drawn.
6) Environmental and occupational history (Environmental and Occupational History)

- In environmental history, information about the environment, hygiene, hazards around the patient is collected.
- In occupational history, information about where the patient works, job time, working environment, presence hazard, pollutants, safety measures etc. is collected.
7) Current health information (Current Health Information)

- In current health information, the patient’s current lifestyle is known.
- In which information is collected about allergies, any habits like tobacco, smoking, alcohol, caffeine etc., medication, exercise, sleep pattern, dietary pattern etc.
8) Psychosocial history
- In psychosocial history, information is collected about the psychological and social life of the patient.
- In which information is collected about the patient’s family relationship, personal relationship, social relationship, working relationship, coping strategy, mental status, emotional status, personality, lifestyle, job, married life etc.
9) Review of system
In a review of system, system wise data of the patient is collected, which includes all the systems of the body so that the real problem can be identified.
In a review of systems, data is collected from the patient’s system, which includes all the body’s systems, so that the real problem can be identified.
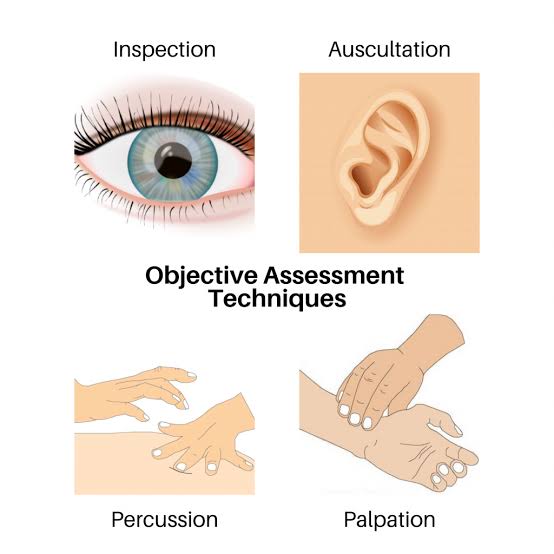
Write down techniques of physical examination (Write down technique of physical examination)
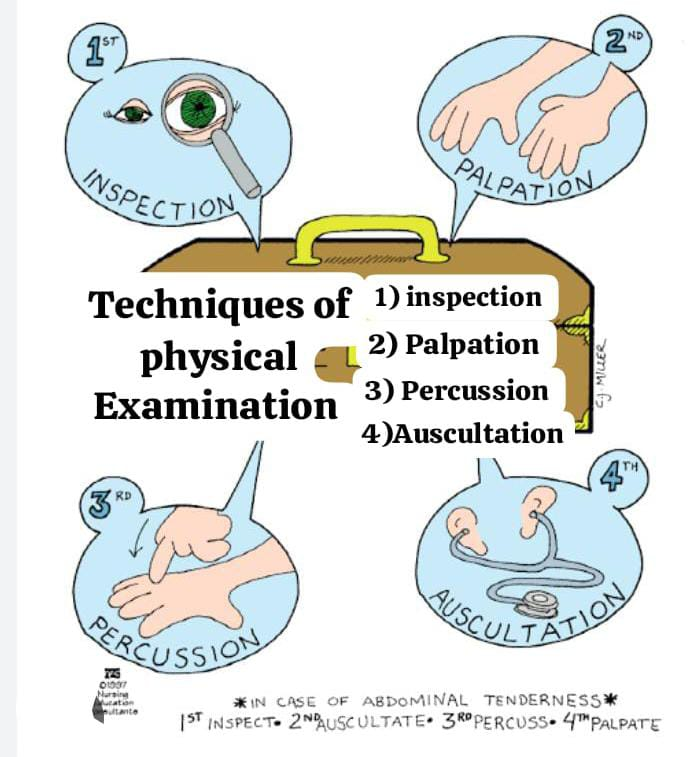
There are mainly four techniques used for physical examination
1) Inspection
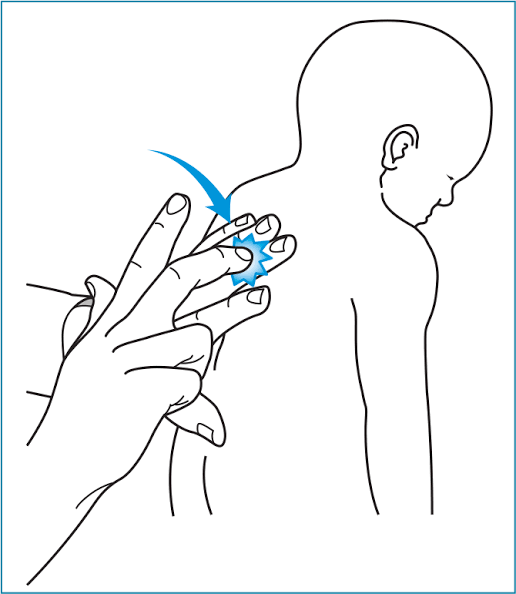
2) Palpation
3) Percussion (Percussion)
4) Auscultation
1) Inspection
• Inspection means to observe, to observe.
• That is, in inspection, observation of every area of the body is done.
• In inspection, a visual examination of the body is done. That is, normal and abnormal are found using vision.
• Inspection involves careful observation of the body’s general appearance, color, size, shape, stature, gait, posture, and symmetry, etc.
• In which the following observations are made:
• Overall appearance (color, size, shape, stature, gait, posture and symmetry)
• State of consciousness
• Grooming and personal hygiene
• Body size or body build
• Expression
General instructions
• There should be adequate light in the room while performing the inspection.
• Compare one side of the body with the other side of the body in the same way.
• Use additional light and various scopes when inspecting other organs of the body, such as body cavities.
• Inspect each area of the body for color, size, shape, symmetry, position, and abnormalities.
2) Palpation

• In the palpation method, every area and organ of the body is palpated.
• In this method, tactile sensation i.e. touch is used. That is, the body part is palpated using the hand and fingers.
• In which the texture, size, shape, consistency and location of the body and organs are known using the fingertips and palm.
• In addition, body temperature, pulse, turgor, texture, moisture, tenderness, thickness and distension are also checked with the help of palpation.
• Palpation is mainly done in two ways. Gentle Palpation and Deep Palpation
• In gentle palpation, 1cm deep is pressed. Gentle palpation is used to determine the characteristics of the skin and superficial tissues, as well as to check the pulse and assess tenderness.
• In deep palpation, 4-5 cm deep is pressed. Which is used to assess deep organs such as the liver
General instructions
• Before palpation, i.e. before touching the patient, explain the entire procedure to him and take his permission.
• Nails should be neatly trimmed and short.
• Gently rub the hand before palpating the patient.
• Always perform gentle palpation first, followed by deep palpation.
• Use both hands to assess the size and shape of the organ. Entrap the organ between both hands.
• Use the dorsal surface to check temperature.
• Use the ulnar surface to check vibration.
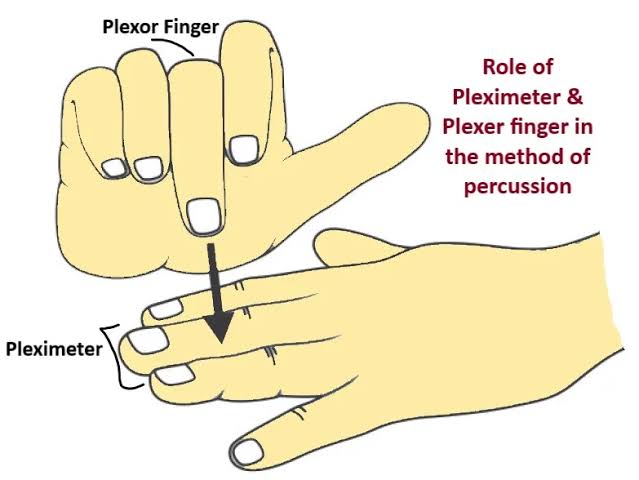
3) Percussion

• Percussion i.e. tapping.
• In this method, the body surface is struck with the fingers using the hand and sound is produced and its quality is checked.
• This method is used to reflect the density of internal organs.
• In addition, the percussion method is used to detect the position, size, shape, air and fluid of the internal organs.
• In percussion, the pleximeter finger is tapped with the plexor finger and the quality of the sound produced is checked.
• Resonance sound is heard in the airy area. Just like resonance sound is heard in the lung area.
• A dull sound is heard in areas with fluid. For example, a dull sound is heard in the abdominal area.
4) Auscultation

• In this method, body sounds are listened to. Which is mostly handled using a stethoscope.
• In auscultation, internal sounds of the body are listened to using a stethoscope. Such as heart sound, breath sound
• The diaphragm of the stethoscope is used to listen to high pitch sounds. Such as heart sound, respiratory sound, bowel sound
• The bell of the stethoscope is used to listen to low pitch sounds. Such as a murmuring sound
Articles required during physical examination

• Stethoscope
• Thermometer
• Sphygmomanometer
• Laryngoscope
• Otoscope
• Ophthalmoscope
• Weight Machine
• Measuring tape
• Watch
• Pen light / Flashlight
• Tongue depressor
• Reflex hammer
• Tuning fork
• Gloves
• Hand sanitizer or soap
• Cotton swab
• Alcohol swab
• Specimen container
• Patient gown and drape sheet
• Pen
• Nursing record sheet
Head to toe assessment:
1) General Appearance
Level of consciousness (alert, drowsy, unconscious)
- Orientation (person, place, time)
- Posture
- Gait
- Nutritional status
- Hygiene and grooming
- Signs of distress or pain
2) Head and Scalp
Size and shape
Symmetry
Scalp lesions
- Tenderness
- Infestations
- Hair distribution and texture
3) Eyes
- Eyebrows and eyelashes (presence, distribution)
- Eyelids (swelling, ptosis, discharge)
- Conjunctiva and sclera (color, moisture)
- Pupils (size, shape, reaction to light and accommodation)
- Visual acuity (Snellen chart)
- Extraocular movements
4) Ears
- External ear (size, shape, discharge)
- Hearing (whisper test, Rinne and Weber if indicated)
- Internal ear (otoscope exam for tympanic membrane)
5) Nose and Sinuses
- External nose (symmetry, deformities)
- Nasal mucosa and septum (color, swelling, bleeding)
- Sinus tenderness
6) Mouth and Throat
- Lips (color, moisture, lesions)
- Teeth and gums (condition, bleeding, hygiene)
- Tongue (color, coating, movement)
- Tonsils and pharynx (inflammation, exudate)
7) Neck
- Symmetry
- Lymph nodes (size, tenderness)
- Thyroid gland (size, nodules)
- Trachea (midline or deviation)
- Jugular venous distension
8) Chest and Lungs
- Inspection (shape, symmetry, movement)
- Palpation (tenderness, chest expansion)
- Percussion (resonance, dullness)
- Auscultation (breath sounds, adventitious sounds)
9) Cardiovascular System
- Inspection (visible pulsations)
- Palpation (apical impulse)
- Auscultation (heart sounds, murmurs, rate, rhythm)
- Peripheral pulses (rate, rhythm, symmetry)
10) Abdomen
- Inspection (contour, scars, distension)
- Auscultation (bowel sounds, bruits)
- Percussion (tympany, dullness)
- Palpation (tenderness, masses, organomegaly)
11) Genitourinary (if indicated)
- External genitalia (lesions, discharge)
- Inguinal lymph nodes
- Urinary symptoms (frequency, pain, urgency)
12) Musculoskeletal
- Gait
- Posture
- Joint inspection (swelling, redness, deformities)
- Range of motion (active and passive)
- Muscle strength and tone
13) Neurological
- Mental status (alertness, memory, speech)
- Cranial nerves
- Motor function (strength, coordination)
- Sensory function (touch, pain, vibration)
- Reflexes (deep tendon, plantar)
14) Skin
- Color
- Texture
- Temperature
- Rashes
- Lesions
- Bruises
- Moisture
- Turgor