ENGLISH-FON-UNIT-3-MEETING THE BASIC NEEDS OF PATIENT -PART-4-(NUTRITIONAL NEED)-UPLOAD
NUTRITIONAL NEEDS:

- Key terms:
- Nutrition: Nutrition is the sum total of all interactions between an organism and the food it consumes.
- Therapeutic Diet: A therapeutic diet is planned to prevent a patient from developing nutrient-related further complications.
- Renal diet: Renal diet is a therapeutic diet planned for patients suffering from renal disorders.
- Cardiac diet: Cardiac diet is a therapeutic diet planned for patients suffering from cardiac disorders. Which also includes restrictions of salt and fatty acids.
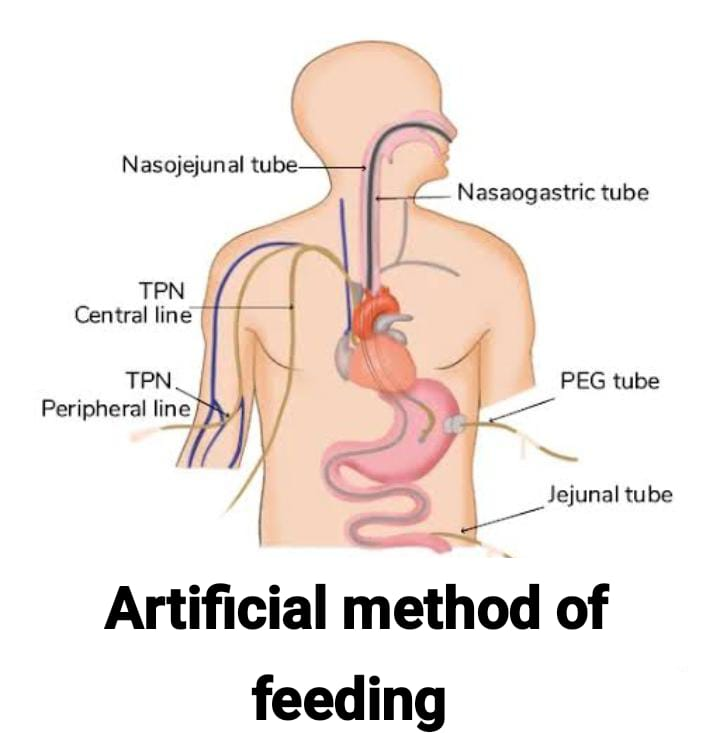
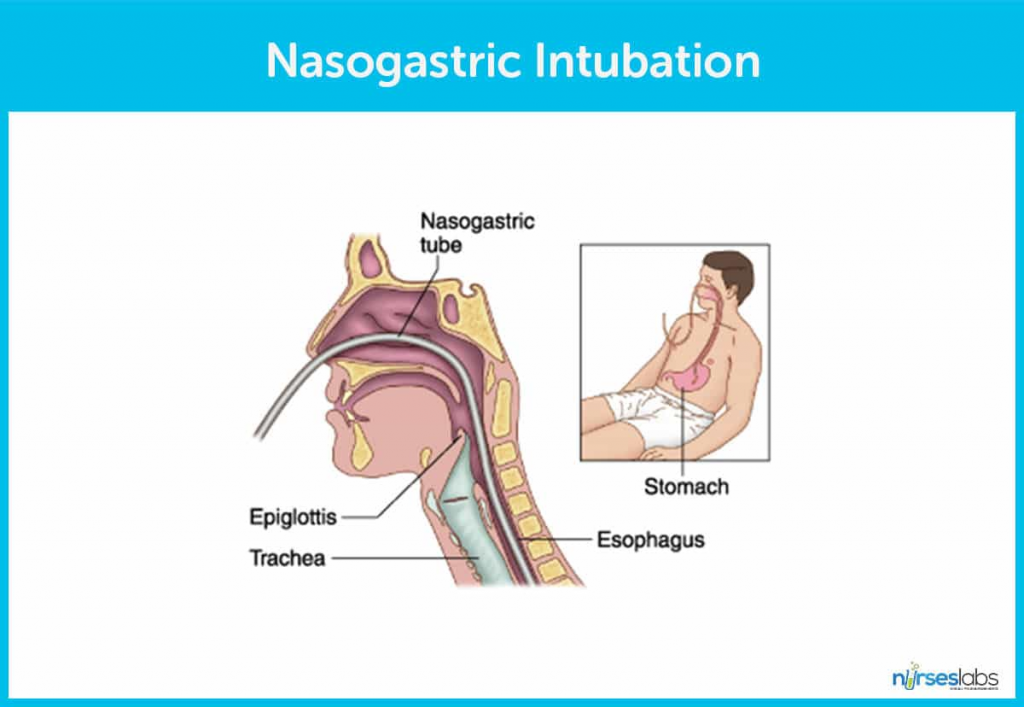
- Nasogastric intubation: In this, a tube is inserted into the esophagus and stomach through the nose.
- Nasogastric Feeding: Nasogastric feeding is an artificial method of giving fluids and nutrients through a tube that is inserted through the nose, mouth, or nasopharynx. Passed through the esophagus and stomach.
- Gastrostomy: It is an opening made in the stomach.
- Gastrostomy feeding: It is a method of feeding a patient through a gastrostomy tube.
- Parenteral Parenteral Feeding/Nutrition: Parenteral feeding refers to the administration of therapeutic agents, including food, outside the alimentary tract. In other words, it is the forcing of fluid into cavities, blood vessels, or body tissues through a hollow tube or needle. Parenteral nutrition involves the infusing or indwelling of glucose, amino acids, lipids, minerals, electrolytes, trace elements, and vitamins through a peripheral or central venous catheter. The administration of a combination of all nutrients through an intravenous route is collectively known as total parenteral nutrition (TPN).
- Gastric Irrigation: Gastric irrigation or stomach wash means irrigating or washing out the stomach with a solution. Gastric irrigation is most frequently used in emergency treatment during times of gastric dilatation and poisoning.
Nutrition
- Maintenance of good nutrition means adequate food intake.
Sufficient quantity and good quality food, which provides all the nutrients required for the growth, maintenance and physical activity of the body. - Introduction:
- Maslow’s Hierarchy of Needs categorizes the human need for food and nutrition as one of the basic needs of every living being. To maintain a normal healthy life, every person should maintain nutritional status. When a person does not take care of his nutrition, he is prone to getting diseases. A person needs to have strength to fight against diseases. To a large extent, the strength of a person to fight against infections is generated by taking proper diet. For example, a person who does not eat a nutritious diet is more likely to get infections like tuberculosis. A person’s ability to work is fulfilled when he has adequate energy to complete the work. But when a person becomes ill, his nutritional needs are affected. Loss of appetite and loss of taste due to illness or medication can be the reasons.
- As a person loses interest in taking food according to his body requirements, the person feels tired and his efficiency in completing tasks decreases. Damaged tissues need to be replaced and this can usually be done only by eating an adequate amount of nutritious food.
- Importance of Nutrition:
- Nutrition is very important for survival, its function starts from birth and continues till death.
- Nutrition is very important for growth and development.
- Nutrition is the primary need of every individual.
- According to Maslow’s Hierarchy of Needs, the basic need of every human being is nutrition.
- Nutrition is also very essential for tissue repair and healing.
- Nutrition is considered as a symbol of hospitality and social status.
- It also has ritualistic importance.
- Nutrition fulfills not only the nutritional needs of a person but also the social and related needs. For example, many function parties (formal/informal) are organized according to meal times.
- Growth, development, activity, maintenance of health, recovery from illness and injury and ability to reproduce are all functions that require adequate nutritional intake. These nutritional requirements vary throughout the life span. This is usually due to changes in the body of a person such as body size, different types of activities that are done by the person and due to health and illness.
- Carbohydrates, fats and proteins are essential nutrients and are considered as macronutrients. Vitamins and minerals are micronutrients and are required in small amounts to regulate body functions. The energy required by a person is provided by carbohydrates, proteins and fats. Body functions are regulated by vitamins, minerals and water.
- Basal metabolic rate (BMR) is the energy required to perform the involuntary activities of the body at rest. In other words, the energy required to maintain the metabolic activities of the cells. In this involuntary activity, maintenance of body temperature and muscle tone, production of body secretions, maintenance of respiratory and cardiac functions and prolonging sleep are all involved and as the age of a person increases, BMR (basal metabolic rate) also decreases with all these factors.
- The standard weight for a female of 5 feet height is 45-46 kg. + 2.5 kg for every additional inch above 5 feet. But for a male it is 48-49 kg, + 2.7 kg for every additional inch above 5 feet.
- Body Mass Index (BMI) is the ratio of weight and height.
- BMI = Body weight in kilograms (Kg) and height in meters := Weight in kilograms/ [Height in meters]2.
- BMI = Body weight in pounds and height in inches = 703 x Body weight in pounds/ [Height in inches]².
- Low height of a person indicates poor nutritional status and health problems.
- Excess weight indicates obesity and its associated health problems.
- Calorie requirement of each person is different according to the age, height, weight, and work done by the person.
Principles of Nutrition:
- Body cells have a requirement of adequate nutrients if food intake is not adequate then physiological functioning can be impaired.
- Important nutrients for the maintenance of health include carbohydrates, proteins, fats, vitamins and minerals. Water is important for maintaining the balance of body fluids.
- Every human’s nutrient requirement differs from person to person and body to body. It depends on the person’s growth, age, activity level, climate, emotional status and pregnancy.
- Hunger, thirst, and safety are nature’s first defense against malnutrition.
- Psychological and cultural factors also influence food selection and patterns of behavior associated with food.
Factors Affecting Nutritional Needs :

- Food habits differ from person to person. Different factors are responsible for this food variation.

- Developmental Stage Stages):
- As a person grows, nutritional requirements change from birth. By the age of one year, an infant’s birth weight has tripled. Breastfeeding is the exclusive source of nutrition for the first six months of life, followed by continued breastfeeding with the introduction of appropriate complementary foods. During the toddler and preschool stages of development, their appetite is significantly lower compared to other stages. When they enter school, their energy requirements increase. They may need foods that have high nutritional value. During the adolescent period, a child undergoes rapid physical, emotional, social and sexual maturation. During this period, children become more conscious about their weight and may start skipping meals. Some children may develop eating disorders such as anorexia nervosa. When a person is an adult, rapid growth does not occur. Then the person becomes more aware of preventive measures such as exercise and there is more concentration on reducing BMR.
- Pregnancy and lactation are periods in which there is a need for more nutrition and during that time, the nutritional needs of a woman increase. Calorie requirement increases during the second and third trimester. The nutritional need of the lactating mother also increases. Breast milk contains nutrients according to the mother’s intake.
- Older adults have a reduced BMR and physical activity. Energy utilization is also reduced. They have trouble in taste discrimination. Thirst is reduced. The total calorie requirement of the body is also reduced, but the energy requirements of nutrients like protein, calcium and vitamin B are reduced.
- Culture:
- According to culture, food habits develop to a large extent. Different combinations of food and the way of food preparation depend on the culture. At the same time, the availability of food and income also influences income habits.
Factores Affecting Nutrition:

Development (Developmental):

- Individual nutritional needs increase during rapid periods of growth, for example in infancy and adolescence, while adults and older generations require fewer calories and dietary changes. Mothers need additional calorie requirements during pregnancy and lactation.
- Gender:
- Men and women have different nutritional requirements due to body composition and reproductive function.
- Age:
- Throughout life, there are changes in activity levels, metabolism, and body composition, which lead to changes in nutritional requirements. For example: Infants and older people consume semi-solid foods. Toddlers prefer hand foods. Adolescents prefer fast food and snacks.
- Ethnicity and Culture:
- Ethnicity and culture determine food preferences. For example, in Indian scenarios, traditional people advise pregnant women to avoid eating papaya and watermelon.
- Personal Preferences:
- People’s likes and dislikes towards food also affect nutrition. A person’s interest, food habits, fasting habits, physical consciousness, beauty consciousness, self-esteem, all these factors affect food preferences.
- Religious practices:
- Some religious groups avoid consuming certain foods. Religious practices affect food intake. For example, some religions allow only vegetables to be consumed and avoid animal intake.
- Lifestyle:
- Certain types of lifestyle are linked to food-related behavior. Living standard, peer group, gender, occupation, and interests greatly influence food selection.
- Economic status:
- Not all people have the financial resources to do extensive food preparation and storage facilities. What to eat, how much to eat, and how often to eat are affected by a person’s economic condition. For example: Eating three meals a day is the desire of a poor person.
- Medications and therapy:
- Drugs alter appetite, disturb taste perception, and interfere with the absorption and excretion of nutrients.
- Biological Factors:
- Biological factors such as illness, chemotherapy, drug intake influence appetite.
- Availability of food:
- The availability of food also affects nutrition. For example, South Indians prefer fish, rice, etc., while North Indians prefer chapatis and vegetables. And also, it is eaten more frequently during the availability of seasonal food.
- Political system:
- Political system also increases the amount of nutrients, such as a food item being stored in the store due to political influence but not supplied to the public, also affects nutritional status.
- Psychological Factors:
- a) Level of Stress, Emotions:
- When there is happiness, appetite increases and when there is stress, appetite is minimized which affects the nutrition of the body.
- b) Fasting habits:
- Girls prefer to fast on some special days. Which affects their nutrition.
- c) Beliefs about the effect of food on health also affect food preference:
- As per research studies, people do not prefer to consume desi ghee etc. as fat intake leads to the development of heart problems.
- Advertisement:
- Advertising and media influence people’s food choices and eating patterns. And it has a greater influence especially on children.
- Alcohol Consumption:
- Nutritional deficiency occurs due to excessive alcohol intake because excessive alcohol intake depresses appetite. Drinking alcohol can cause weight gain through the addition of calories and due to alcohol’s effects on fat metabolism. Excessive consumption contributes to nutritional deficiencies.
- Environmental factors:
- Temperature greatly influences food preferences. As there is a high energy requirement during the cold season, due to which people prefer to consume dry fruits.
- Health :
- A person’s health status is greatly affected by their eating habits and nutritional status. As the ability to ingest food depends on the condition of the person’s mouth, oral structures and ability to swallow. Impairment in any of these components can interfere with eating patterns.
Terminologies associated with food intake:
- Anorexia: Loss of appetite.
- Dysphagia: Difficulty swallowing.
- Dyspepsia: Feeling of fullness due to indigestion.
- Nausea: Feeling of vomiting.
- Belching: Noisily expelling gas from the mouth.
- Regurgitation: Backflow of partially digested food from the stomach into the mouth Vomiting: The throwing out of stomach contents through the mouth. Reduced food intake can occur due to the following reasons: /wp:paragraph –>
- Vomiting: The throwing out of stomach contents through the mouth.
- Food intake can be reduced due to the following reasons:
- Anorexia, which can be caused by systemic or local diseases.
- Pain due to any disorder.
- Psychological issues such as fear, anxiety or depression.
- Social factors such as loneliness.
- Changes in the ability to smell and taste.
- Difficulty in chewing.
- Chronic gastrointestinal problems.
- After-effects of drug therapy.
- Inadequate food availability due to various reasons.
- Increased food intake can occur due to the following reasons:
- Bad eating habits.
- Anxiety.
- Certain medications such as corticosteroids and antidepressants.
- Diabetes mellitus.
- Hyperthyroidism.
- Hypoglycemia etc.
Assessment of nutritional status:

- The person’s needs Assessing nutritional status is necessary to identify, plan according to need, implement the plan, and evaluate outcomes. When a person is sick, his needs also change and then he may need a ‘therapeutic diet’ according to his physical condition.

- A) Anthropometric Collect anthropometric measurements.
- B) Determine biochemical data.
- C) Inspect for clinical signs of nutritional status.
- class=”has-inline-color”>D)Dietary History.
- A) Collect anthropometric measurements:
- Anthropometric measurements include measuring height, weight, skin folds, arm circumference, and waist circumference. It helps in assessing the client’s calorie-energy expenditure balance.
- BMI= Weight in kg/(Height in meters)²
- B) Determine biochemical data:
- Hemoglobin level, hematocrit.
- Serum albumin Level, Transferrin.
- Total Leukocyte Count.
- Creatinine Clearance.
- Blood Urea Nitrogen Level.
- Blood Glucose Level.
- Cholesterol, Lipid Profile.
- C) Inspect for Clinical signs of nutritional status:
- Such as weakness, fatigue, pale color, loss of appetite, assessment of body system.
- D) Dietary History:
- Asking the client about his/her food preferences, restrictions, daily food intake, liking , Ask about food habits, daily food intake, intake of vitamin supplements in detail.
Ask about dietary problems: such as chewing, swallowing, health history, financial status, family type, etc.
Diet in Health and Illness:

- Diet plays an important role in illness. Diet may have to be modified depending on the patient’s disease condition, severity of the disease, nutritional status of the patient and the metabolic changes involved. Therefore, some changes need to be made in the diet used for feeding normal, healthy individuals so that it can be made suitable to meet the modified nutritional needs when the person is suffering from any illness. In some illnesses, dietary modifications involve few changes, but in others, some alterations and adjustments have to be made.
A therapeutic diet is planned to maintain and restore good nutrition. - In most cases, a therapeutic diet is used to supplement a patient’s medical or surgical treatment, while in some cases, such as diabetes mellitus, a therapeutic diet, rather than medical therapy, is the most important aspect of a patient’s treatment.
- In some disease conditions, the body cannot produce enough Nutrients are not available in sufficient amounts or are not able to utilize the available nutrients due to faulty digestion, absorption, or transportation of food elements, thus affecting the nutritional homeostasis of the sick person. The diet needs to be suitably modified.
- Modified / Therapeutic Diet:
- A modified/therapeutic diet is concerned with the use of food as an agent for effective recovery from illness, not only in the care of the sick but also in the prevention of disease and maintenance of health.
General objectives of therapeutic diet:
- To maintain good nutritional status of the patient.
- To address nutritional deficiencies due to disease.
- To provide rest to the body or specific organs affected by the disease.
- To adjust food intake to the body’s ability to metabolize nutrients during the disease.
- To bring about changes in body weight whenever necessary For.
Special diets:

- Hospitals usually make modifications to the daily diet which can be classified as general, light, soft, liquid or clear liquid. General diets are comparable to normal, adequate, daily diets. Light and bland diets are similar but do not include spicy foods and high roughage. Soft diets are made up of foods that have a fine texture and low cellulose content and may exclude meat. Full liquid diets include all liquid foods including gelatin and ice cream, while clear liquid diets include soups, tea, coffee, clear soups, stained fruit juices and gelatin. There are many other special diets for specific purposes or conditions. A normal well balanced diet is vegetarian or non-vegetarian which is taken by a healthy adult. But when a person is sick then such a diet is not suitable for him. When a person is sick then the content, preparation and calorie of his food is adjusted to the patient’s needs to provide digestible and suitable food to the patient.

- Hospitals usually make modifications to the daily diet which can be classified as general, light, soft, liquid or clear liquid. General diets are comparable to normal, adequate, daily diets. Light and bland diets are similar but do not include spicy foods and high roughage. Soft diets are made up of foods that have a fine texture and low cellulose content and may exclude meat. Full liquid diets include all liquid foods including gelatin and ice cream, while clear liquid diets include soups, tea, coffee, clear soups, stained fruit juices and gelatin. There are many other special diets for specific purposes or conditions. A normal well-balanced diet is a vegetarian or non-vegetarian diet that is followed by a healthy adult. But when a person is sick, such a diet is not suitable for them. When a person is sick, the content, preparation and calorie content of his food are adjusted to the patient’s needs to provide digestible and suitable food to the patient.

- In this diet, Solid diet, soft diet and liquid diet are involved.
- Solid diet:
- This involves a normal, well-balanced diet that does not require any changes. Solid diet is served to patients who can tolerate it.
- Soft Diet:
- Soft diet group is easy to chew and easily digestible. Very ill, elderly, patients recovering from surgery and patients who have dental problems and/or have had dental surgery are given soft diet. Some of the food preparations include khichdi, dalia, kanji, lentils which are cooked soft, custard, porridge and boiled/mashed potatoes.
- A soft diet is often a bland diet. It does not contain chillies, spices and other irritating substances. It avoids foods that are high in fibre. Fried food is also not given. Baking, boiling, steaming and grilling can be used. Strong coffee, tea, alcohol and meat extracts should be avoided. If the patient is suitable, curd and milk can be given in plenty.
- Liquid diet:
- A patient who cannot tolerate a normal diet and a soft diet is given a clear liquid diet and a full liquid diet.
- Clear liquid diet:
- This group of liquids has a residue. This includes light black tea, weak black coffee, clear soups, clear juices, and other beverages. The food value of these items is almost nil. Generally, this is used for short periods.
- Full liquid diet:
- This type of liquid diet is provided when the patient is unable to swallow, and he/she needs to receive nourishment for a considerable period. Patients on tube feeding require a completely liquid diet.
- Soups are various food items that are boiled and mixed with lentils, vegetables or rice to make a thick solution. High protein, calcium, vitamins and minerals are provided through a liquid diet. When a patient is on a tube feeding or jejunostomy feed, a liquid diet is given to him, but it is modified accordingly. Low carbohydrate, low protein and low fat foods can be prepared according to the therapeutic needs of the patient.
Therapeutic diet:
A therapeutic diet is planned to prevent a patient from developing nutrient-related further complications. Therapeutic needs vary from patient to patient. Based on physiological and pathological changes, the requirement of diet needs to be changed.
- Therapeutic diet such as,
- High calorie diet: In malnutrition.
- Low calorie diet: In obesity.
- High protein diet: For the treatment of diseases like kwashiorkor.
- Low protein diet: In nephrotic syndrome.
- Fat free diet: To reduce stimulation of the gallbladder in chronic colitis.
- Low salt or salt free diet: In cases of high blood pressure, kidney disease and liver disease.
- Sippy Diet: For peptic ulcers.
- High Fiber Diet: To prevent constipation, treat constipation, and treat irritable bowel syndrome
- Low Fiber Diet: To reduce bowel irritation and ulcerative colitis.
- Renal Diet : In cases of nephrotic syndrome or chronic renal disease.
MEETING THE NUTRITIONAL NEEDS:

- Nutrition is concerned with the process by which we take in materials/nutrients from the environment and use them to maintain and promote body functions. Eating, digestion (mechanical and chemical), absorption and utilization of nutrients, all these are involved in nutrition.
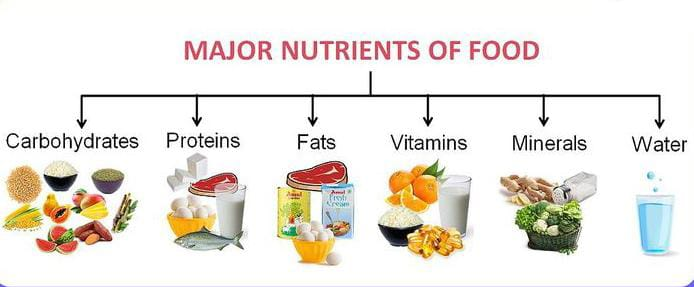
Nutrients such as:
- Water,
Carbohydrates,
Protien,
Fats,
Minerals,
Vitamins, etc. - Water:
- Water accounts for 50% to 60% of an adult’s total body weight. Two-thirds of the body’s water is inside the cells (intracellular fluid) and the rest is present as extracellular fluid. As a person ages, the total body water and extracellular fluid decrease. Water is more essential than food because it acts as a solvent and many solutes dissolve in it. It helps in digestion, absorption, circulation and excretion. It also helps in regulating body temperature. An adult needs to consume 2.2 L to 3 L of water/day.
- Carbohydrates:
- Proteins and fats are the basic sources of energy. Carbohydrates are starches and sugars. These are organic compounds that contain carbon, hydrogen and oxygen. Carbohydrates are classified according to the structure of the molecules within them. They are simple – monosaccharides and disaccharides or complex – polysaccharides. Carbohydrates are converted into glucose for transportation through the blood. Insulin and glucagon are hormones that maintain serum glucose levels.
- Protein:
- Proteins consist of 22 basic building blocks of amino acids. They are a major component of all living cells. It is essential for the repair of body tissues, the formation of enzymes, muscles, skin, blood and bone matrix. Proteins are grouped into complete and incomplete proteins. This classification is based on the amino acid composition. Complete proteins contain all the essential amino acids that support growth and development. Incomplete proteins are deficient in one or more essential amino acids. Animal proteins such as eggs, dairy products and meat are complete proteins. Grains, legumes and vegetables are incomplete proteins. Pancreatic enzymes in the small intestine break down dietary proteins into amino acid particles.
- Fats:
- Lipids are insoluble in water; thus, insoluble in blood. In the diet, lipids are considered triglycerides.
- Vitamins:
- Minerals and water are known as regulatory nutrients. Because these nutrients are essential for the metabolism of energy nutrients. Vitamin C and the B complex are water-soluble vitamins. The B complex includes thiamine (B1), riboflavin (B2), niacin (B3), biotin (B7), folate (B9), and cobalamin (B12). These vitamins are absorbed directly into the bloodstream.
- Fat soluble:
- Fat soluble vitamins include vitamins A, D, E, and K. These vitamins are absorbed across the lumen of the intestine and transported in the lymphatic circulation. Excess fat-soluble vitamins are stored in the liver. Very high levels of vitamins A and D can be toxic because they are stored in the body and are not excreted in excess amounts.
- Minerals:
- These are inorganic elements present in body fluids and tissues of our body. Minerals can be lost through excessive cooking or soaking. Calcium, phosphorus, sulfur, sodium chloride, potassium, and magnesium are called macrominerals because our body requires more than 100mg/day. Zinc, manganese, chromium, copper, selenium, fluoride, and iodine are known as microminerals and the body requires less than 100 mg/day.
Factores for assessing the patients Nutritional status:

- Appearance:
- The first step in the assessment is to closely observe the person’s nutritional status and general appearance. Is the weight/height ratio appropriate, reflecting the number of calories the person needs? Is the skin color clear and the skin texture smooth? Many nutritional deficiencies are first apparent in changes to the skin and mucus membranes. Is the hair thick and shiny? Are the lips and gums intact, or are they red, pale, or swollen?
- Dietary History:
- The patient’s dietary history includes information about typical meal patterns, types of foods commonly eaten, likes and dislikes, and allergies, if any.
- Current Needs:
- Nutrition assessment also includes considering current needs. Is the person growing? Are there any special needs created by tissue repair and healing? Is the person underweight?
- Ability to eat:
- Various factors such as muscle strength, hand coordination, or discomfort in the mouth can affect eating ability. Some common problems faced by hospitalized people are immobilization that does not allow for easy eating or swallowing, restraint or immobilization of the dominant hand, and conditions such as extreme fatigue or weakness.
- Level of knowledge:
- Does the patient know what a good diet is? If a special diet is prescribed, does the patient understand the diet and its purpose? This information is essential to effectively plan an intervention.
- Current intake:
- It is important to gather information about what the patient currently eats and drinks, including the calorie content, eating patterns, and food preferences. It may be important to measure all fluids ingested so that the measured outputs can be compared.
Therapeutic diet planning and serving:
Diet plan for patient suffering from fever:

Objectives of this diet plan:
- To maintain adequate nutrition.
To get relief from symptoms.
To maintain electrolyte balance.
To avoid intestinal irritation. - Fever is a condition in which the body temperature is elevated above normal levels. It can be acute or chronic.
- Diet planning for such patients should include increasing energy intake (10-20%), protein intake (1/ 1/2 to 2 times) from egg/milk intake, carbohydrate intake, emulsified fat intake, mineral and vitamin intake and fluid intake (beverages, soup, juice, plain water).
- Modified diet includes the following foods such as, plenty of fluids, milk and milk products, low fiber diet, high biological value protein (eggs, milk, fish, meat), Gelatin based desserts (honey, jam).
- Food to be Avoided:
- High fiber foods, raw vegetables and fruits (except papaya, banana), fried fatty foods, spices and condiments.
Therapeutic diet for cardiac patient:
- Cardiovascular disease is a disease of the heart and blood vessels. Cardiovascular diseases include diseases such as hypertension, angina pectoris, ischemic heart disease and myocardial infarction.
- Food Recommended for Cardiac Patient:
Food low in cholesterol and saturated fat.
- Skimmed milk, skimmed milk Cheese made from milk.
- Grains and legumes.
- Whole grains.
- All vegetables and fruits.
- High fiber and soluble fiber such as oatmeal, millets, pectin, gums, etc.
- Lean meat, egg whites, and fish.
- Vegetable oil, sugar and jaggery.
- Food to be Avoided:
- •Cholesterol rich food,
•Whole milk, butter, cream, cheese (processed).
•Indian sweet meals like, •Puddings, bakery products.
•Organ meats (liver).
- Egg yolk, fish.
- Nuts, oilseeds, pickles.
- Margarine, vegetable, fried food.
- Alcohol.
- Regular low cholesterol and low fat and high fiber diet fiber diet:
- Energy: 1600 k cal.
Fat: 40g.
Protein: 65g.
Therapeutic diet for cronic Renal failure:
- Chronic renal failure is also known as chronic kidney disease (CKD). In chronic kidney failure, the function of the kidneys slowly and progressively deteriorates, leading to electrolyte imbalance and fluid imbalance. In chronic renal failure, renal excretory and regulatory functions are slowly, insidiously, and irreversibly impaired. The final stage of chronic kidney disease is called end-stage renal disease (ESRD). Chronic kidney disease is a condition in which the kidneys gradually fail to filter waste products and fluids from the body, resulting in the accumulation of toxic substances in the body. This condition is mainly caused by various reasons such as diabetes, hypertension, glomerulonephritis, polycystic kidney disease, etc. Diseases etc.
- Food tips in chronic renal failure:
- In chronic renal failure, the diet should be low in protein based on the urea content in the blood.
- For its proper utilization, the prescribed quantity of low protein should be of essentially good quality. Milk and its products or eggs should be a part of the planned diet.
- Cereals, pulses, peas, beans should be taken only in the prescribed amount.
- Fats and carbohydrates can compensate for the low protein diet to meet the calorie requirement.
- Thus, ghee, oil, sugar, potatoes and other starchy foods can be used to increase the palatability (palatability) of the diet.
- Cakes, biscuits and bakery products, jams, squash and sherbet can be used except where salt is restricted.
- Use fruits and fruit juices to supply vitamins and minerals.
- Lime, mango, plum, orange, cucumber, tomato, pomegranate can be taken except where potassium is restricted.
- Use spices and condiments in small quantities.
- Low protein diet and low sodium diet for chronic renal failure:
- Protein:
- Sedentary worker : 20 gm
Moderate worker : 30 gm
Heavy worker : 40 gm. - Calories :
- Sedentary worker : 2040
Moderate worker : 2197
Heavy worker :2363 - Sodium :
- Sedentary worker : 180 mg
Moderate worker : 215 mg
Heavy worker : 255 mg - Potassium:
- Sedentary worker : 1226 mg
Moderate worker : 1382 mg
Heavy worker : 1982 mg. - Phosphorus:
- Sedentary worker: 441 mg
Moderate worker: 586 mg
Heavy worker: 717 mg. - Food to be avoided:
- Extra milk and milk products.
- Meat, poultry and fish.
- Dry fruits, i.e. almonds, peanuts, cashews and walnuts.
- Extra pulses, cereals, legumes, peas, beans.
- Cakes, biscuits and bakery products, jams, (if sodium restricted).
- Camppa, cola, squash and sherbet, (if (if sodium restricted).
- Fruits and fruit juices such as lemon, lime, mango, plum, orange, grapefruit, tomato, pomegranate (if potassium restricted).
- Green leafy vegetables (if potassium restricted).
Therapeutic diet plan for gout patient:

- Gout is an abnormality of purine metabolism in which abnormally high levels of uric acid accumulate in the blood. The normal blood level of uric acid is 2-4 mg/100 ml. When this increases, uric acid salts form crystals and are deposited in the joints and surrounding tissues. This disease usually occurs after the age of 35 and mainly affects males. It is characterized by sudden and acute onset and localized arthritic pain that usually begins in the big toe and continues down the leg.
- Free foods:
- These are foods in which the amount of purine is negligible and can be used daily considering the total calorie requirement.
- •Wheat, rice, Semolina, maida, maize,
•Washed pulses except lentils.
•All fruits.
•Milk and milk products.
•Nuts and oil seeds.
•All vegetables except eggs, spinach, mushrooms, asparagus.
•Tea and coffee, aerated beverages.
•Pickles and condiments. - Food to eat occasionally:
- The following foods have a moderate purine content and During the remission period, Victoza can be taken once:
- •Fish, poultry, shellfish.
•Mushrooms, asparagus, spinach, and dried peas and lentils. - Food to avoid:
- The following foods are very high in purines and should be avoided completely:
- Red meat, organ meats Meat like kidney, brain, heart, meat extract.
Mussels, partridge, sardines, herring, anchovies and mackerel.
Yeast (baker and brewer)
Whole pulses like rajmah, channe and rongi.
Therapeutic diet for obese patient.

- Obesity is a medical condition in which there is excessive accumulation of fat in the subcutaneous tissue and other parts of the body of a person. Body Mass Index (BMI) is a useful screening parameter to measure the obesity of a person.
- BMI ( Body Mass Index) = Weight in kg/( Height in meter)2
- In BMI,
Underweight: < 18.5 kg/ m2, Normal weight: 18.5-24.9 kg/ m2, Overweight: 25.0-29.9 kg/ m2, Obese: > 30 kg/ m2. - Energy: A reduction of 1000 kcal per day is required to lose approximately 1 kg of weight per week. A reduction of 500 kcal per day will result in a weight loss of about 1/2 kg per week.
- Proteins and fats: Slightly more than normal protein and 20% of total energy should be provided by fat. Unsaturated fats should be avoided. Fried food should be restricted.
- The following foods should be restricted or avoided:
- High-fat foods such as butter, processed cheese, chocolate, cream, ice cream, fatty meat, fried foods such as samosas, parathas, puris, potato chips, nuts, pastries, etc.
- Bread, cakes, High carbohydrate foods like cookies, dried fruits, potatoes, sweet potatoes, honey, jams and rich puddings.
- Carbonated and malted beverages, alcoholic drinks and sweetened fruit juices.
Foods recommended for weight loss:
- Low calorie, High fiber, high protein diet.
- Low fat, low sugar and refined carbohydrates.
- Use lean meat.
- Take three meals a day.
- Vegetable soup, salad, plain lassi and lemon water are advised.
- All grains, pulses, beans, eggs and poultry and milk are recommended. Is.
- A salad of carrots, radishes, cabbage, tomatoes, cucumbers, pickles and onions should be taken in sufficient quantity.
Therapeutic diet for Diabetic patient:
- Diabetes is a chronic metabolic disorder in which the metabolism of carbohydrates, proteins and lipids is impaired. Diabetes is a group of metabolic disorders in which a person’s blood has high sugar levels. This is mainly due to an impairment in the secretion of insulin hormone and the action of insulin hormone in the body. High blood sugar levels are seen in the body.
- Diabetes mellitus “ 3 P ” syndrome is mainly seen.
- 1)P: Polyuria (frequent urination),
- 2)P: Polydipsia (increased thirst),
- 3)P: Polyphagia (increased hunger).
- Dietary management in diabetic patient :
- A therapeutic diet plays an important role in the treatment of diabetes. The diet can be used alone or in combination with insulin injections or oral hypoglycemic drugs.
- A person’s diet plan depends on their height, weight, age, sex, physical activity, and the nature of their diabetes. The following are the essential considerations:
- 1) Determining energy requirements.
2) Distribution of energy in terms of carbohydrates, fat and protein
3) Determining carbohydrate, fiber and preparation time.
4) Distribution of carbohydrates.
5) Stages of diabetes with reference to the absence or presence of any complications. - Diet and feeding patterns:
- In diabetics, the amount and timing of food intake, particularly carbohydrates, should be controlled to prevent fluctuations in blood glucose levels beyond the normal range. Intake of refined sugar should be reduced as it causes a sharp rise in blood sugar levels after intake. The patient should avoid fasting and binge eating. Adjustments should be made for exercise and eating properly and not overeating due to hunger.
- Food not allowed:
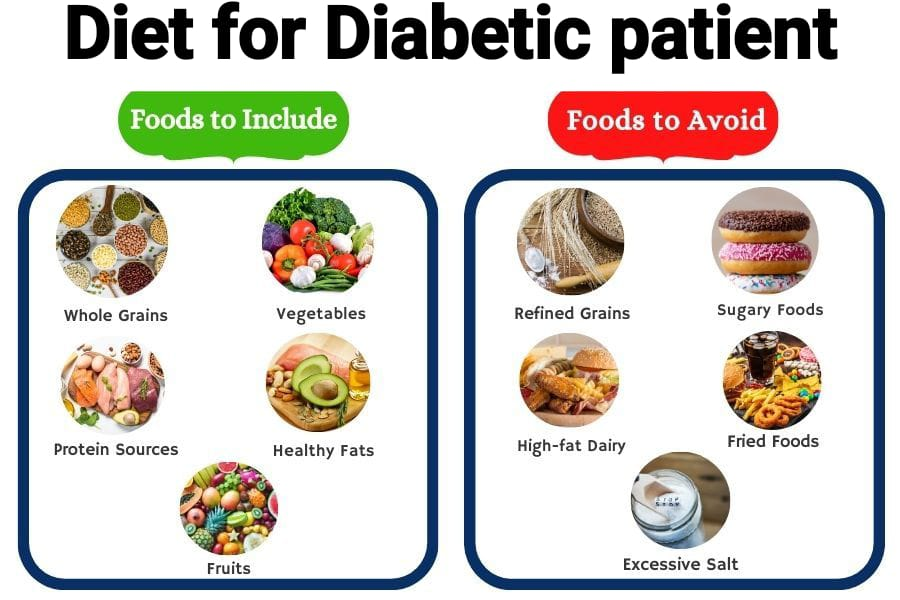
- Glucose, sugar, honey, all tweets, chocolate and candies.
- Food to be Avoided or restricted:
- Potatoes, jam, arvi, sweet potato, mango, grapes, banana, alcoholic beverages, fried foods, paranthas, puris, pakodas, dal moth, methi, deep fried vegetables, Dry fruits, saturated oils, cakes and pastries.
- Foods to be used freely:
- Green leafy vegetables, tomatoes, cucumbers, radishes, lemons, clear soups, black coffee and unsweetened tea, buttermilk, sour chutneys, pickles without oil, etc.
Diet during Radiation Therapy therapy):
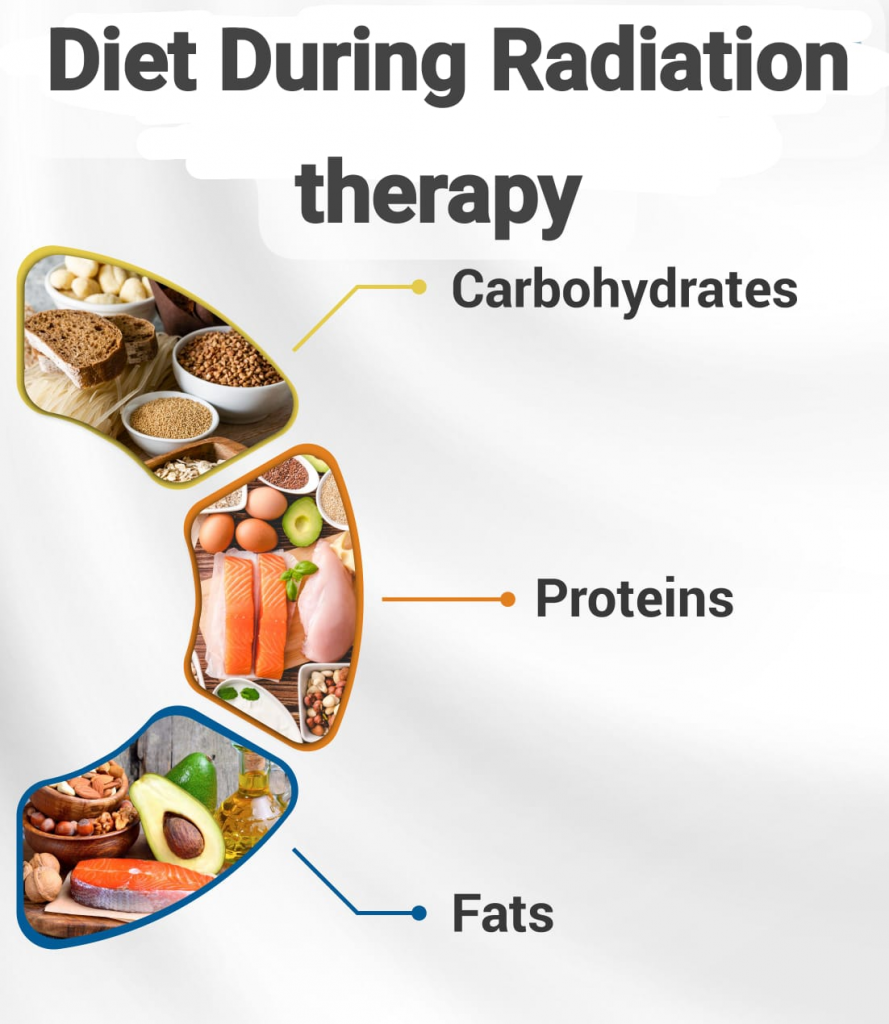
- Ionizing radiation is used in radiation therapy. Abnormal cellular growth is prevented by using this radiation. This radiation therapy is Damages and necrotizes cancerous cells.
- Purpose:
- 1.Primary: Primary purpose is only for the treatment of cancer and its cure.
- 2.Adjuvant: Adjuvant is used only in pre-operative and post-operative conditions and is used with chemotherapy.
- 3.Palliative: Any of these It is used in emergency conditions such as superior vena cava compression and spinal cord compression.
- 4. Prophylactic purpose: This radiation therapy is given only in the suspected area.
- Providing proper nutrition daily is an important treatment for patients who are on radiation therapy. To maintain good health, it is necessary for patients with radiation therapy to eat good food daily. If the patient is taking poor nutritious food then his condition may get aggravated but if he is taking nutritious diet in proper amount then he gets early recovery and relief from pain.
- The daily diet should include food items from each of the following groups:
- Milk and milk products: Milk, curd, fresh paneer, lassi etc.
- Grains: Wheat flour, Daliya Suji, Bread, Noodles, Macaroni etc.
- Pulses and Beans: All types of lentils, Rajma, Raungi, White gram, Soybean and their products.
- Fats and Oils: Butter, Cream, Ghee, Refined Oil, etc.
- Fruits: All seasonal fresh fruits, fruit juices and all dry fruits.
- Vegetables: All fresh and green leafy vegetables.
- Meat and poultry: Mutton, chicken, fish and eggs.
- A variety of foods are needed to maintain healthy tissues and rebuild damaged tissues both during and after treatment.
- Some common reactions and discomforts of radiation therapy after treatment Following are some common reactions to radiation therapy and relevant suggestions to reduce discomfort after treatment:
- 1) Dryness of mouth: Drink 8-10 glasses of fluid throughout the day.
- 2) Pain in mouth and throat: Avoid hot, spicy and irritating foods.
- Avoid alcohol and smoking.
- Avoid very hot and cold foods. Let hot foods cool to medium temperature.
- Rinse your mouth daily with a mouthwash made with 1/4 teaspoon of salt and 1/4 teaspoon of baking soda in a glass of water.
- Modify the consistency of the diet according to individual needs. Blend all foods in a high-speed mixer to a liquid or semi-solid consistency for easy swallowing.
- Start with milk/soup to avoid mouth irritation.
- 3) Loss of taste and smell: To improve taste and flavor, use various types of taste and smell agents, e.g. Herbs like coriander, mint, lemon, cardamom, Chinese lentil, cloves, essences like cayenne, vanilla, rose, etc. Syrups, milk shakes, fruit shakes and chocolates etc. enhance the taste.
- 4) Depressed Appetite::Eat whenever you like and however you like, but don’t skip meals.
- Food should be taken in small quantities but at frequent intervals.
- 5) Nausea: Carbonated Avoid beverages, cold jelly, and ice cream.
- 6) Loss Motion/Indigestion: Take liquids at frequent intervals, and then gradually ingest semi-solid and then solid food.
- Have a choice:
- The consistency of the patient’s food includes the following foods (food of a consistency vice patient includes the following foods):
- a) Liquid: Water, tea, coffee, lemon water, carbonated water, lassi, sherbet, squash, fruit juice, soup, buttermilk water.
- b) Semi Liquid: Milk, egg yolk, milk powder, honey, Horlicks, Proteinex, Spit, Complan, Feradol, Milk fruit shake, cornflakes.
- C) Semi-solids: Wheat, lentils, semolina, halwa, khichri, custard, kheer, rice flour, egg pudding, cooked lentils, mashed potatoes and stews of vegetables, butter, fruits.
Therapeutic diet in liver disease Diseases):
- The liver is the largest organ in the body, accounting for 2.5 to 3% of body weight. It is a multifunctional organ that plays an important role in the metabolism of fats, carbohydrates, and proteins. Most of the end products of food digestion are transported directly to the liver, stored there, and sent to other parts of the body when needed. Toxic substances are detoxified here. Thus, the liver has an important impact on the nutritional status of a person, and diseases of this organ significantly affect health. Although liver disease can have a number of causes such as infections, toxins, metabolic or nutritional factors, carcinoma, etc., the pathological changes seen are similar basic changes including atrophy (degeneration of hepatic cells), fatty infiltration (deposition of fat droplets in hepatic cells), fibrosis (end result if liver is damaged), necrosis (death of hepatic cells). A common symptom in all liver diseases is jaundice. It is the result of increased bilirubin levels in the blood and gives a yellow color to the skin and sclera of the eyes. Urine appears dark yellow or brown due to the presence of bilirubin. Normal serum bilirubin level is 0.1 to 0.8 mg/ 100 ml.
Dietary Management:
Objectives:
- To relieve symptoms.
- To regenerate liver tissues.
- To prevent further damage to the liver.
- Energy: Due to anorexia, initially only 1500 to 2000 Kcal is acceptable. Gradually increase energy intake by 20 to 30% more than normal intake.
- Proteins: Increase protein intake to overcome negative nitrogen balance, which can promote regeneration of liver cells and prevent fatty infiltration of the liver. The amount of protein needs to be adjusted according to the extent of liver damage. On the other hand, in acute cases, protein intake may also have to be decreased.
- Carbohydrates: A high carbohydrate diet is recommended. A daily intake of 300-400 g of simple carbohydrates such as glucose, sugar, honey, sugarcane juice, fruits and fruit juices, grains and root vegetables is recommended.
- Fats: The digestion and absorption of fats are affected by liver disorders because bile secretion is impaired. Tolerance to fats varies from person to person. Therefore, in mild to moderate cases, 40 to 50 gm of total fat can be provided per day. In severe cases, total fat may be restricted to 20-30 g/day due to liver damage. The quality of fat needs to be modified. Emulsified fats such as milk and eggs should be given as they do not require bile for their emulsification.
- Vitamins and minerals: All minerals, especially calcium and iron, should be provided in adequate amounts in the diet. Due to reduced fat intake, fat soluble vitamins such as vitamins A and D are deficient. Supplements of vitamins A, K, C and B group need to be given.
- Feeding pattern: The food served should be well cooked, attractive and appetizing as anorexia is a problem. The consistency of the diet and the frequency of feeding need to be modified. Patients with mild hepatitis can eat a diet of normal consistency while in cases of acute hepatitis, a liquid or soft diet is recommended. In very severe cases, tube feeding may be required.
- Food to be included: Sugar, glucose, honey, pulses, milk and milk products, eggs, fruits and vegetables.
- Food to be avoided or restricted: Fried and fatty foods, fats, oils, nuts, oil seeds, strongly flavored vegetables and meats and alcohol The intake of is also restricted.
Therapeutic diet in gastrointestinal disorders:

- The gastrointestinal tract is involved in the digestion, absorption and utilization of food. Digestive system disorders are organic and functional in nature. Depending on the nature of the disease, there may be disturbances in the size, enzyme production, release and transport mechanisms. These abnormalities interfere with the efficiency and completeness of digestion and absorption. Common disorders include diarrhea, constipation, peptic ulcers, malabsorption syndrome, dysphagia, anorexia nervosa, nausea, and vomiting.
Diarrhea (Diarreoea):
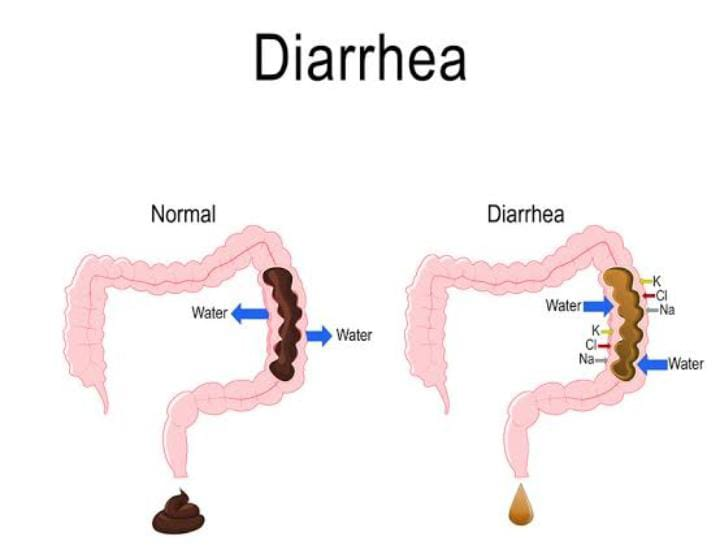
- Definition:
- Diarrhea is a condition in which liquid, loose and watery stools are passed more than three times a day (in 24 hours). And the frequency of these loose, watery stools is also high. Due to diarrhea, excessive amounts of fluid and electrolytes are lost from the body, due to which the condition of dehydration arises. Diarrhea is one of the top three causes of mortality in developing countries.
- Types of Diarrhea:
- There are four main types of diarrhea.
- 1) Acute Diarrhea
2) Chronic Diarrhea
3) Persistent Diarrhea
4) Dysentery - 1) Acute Diarrhea:
- Acute diarrhea is a condition in which the onset of diarrhea is sudden and of short duration, lasting less than two weeks. Acute diarrhea is mainly caused by any infection.
- 2) Chronic Diarrhea:
- Chronic diarrhea is a condition in which loose watery stools persist for more than 3 weeks, it is called chronic diarrhea. Chronic diarrhea is caused by any organic disease.
- 3) Persistent Diarrhea
- Persistent diarrhea is a condition in which attacks of acute diarrhea occur for more than two weeks and that diarrhea is caused by an infection.
- 4) Dysentery (Dysentery)
- Dysentery is a condition in which blood, mucus and pus are present in the stool and is accompanied by abdominal colic, fever, and tenesmus (this is a condition in which there is a need to pass stool even though the bowel is already empty.).
- Causes of Diarrhea:
- Unhygienic conditions Due to.
Infection. - Viral infection:
- Rota virus,
- Enterovirus,
- Adeno virus,
- Measles virus Due to.
- Due to the influenza virus.
- Bacterial infection :
- E coli,
- Caused by Shigella bacteria,
- Caused by Salmonella bacteria.
- Caused by Staphylococcus bacteria.
- Caused by Vibrio cholerae.
- Parasitic infection:
- Entamoeba histolytica,
- Giardia lamblia,
- Cryptosporidium,
- P. falciparum, P. vivax, P. ovale and P. malariae.
- Fungi infection:
- Caused by Candida albicans,
- Infectious condition:
- Upper respiratory infection,
- Otitis media,
- Tonsillitis,
- Pneumonia,
- Urinary tract infection.
- Dietetic or nutritional factors:
- Overfeeding,
- Starvation,
- Food allergy and food poisoning.
- Other predisposing conditions
- Such as,
- Age,
- Season,
- Artificial feeding,
- Signs and symptoms of Diarrhea:
- Frequent passing of loose watery stools.
- Dehydration,
- Abdominal pain.
- Low grade fever.
- Loss of appetite.
- Abdominal distension.
- Behavioral changes such as
- irritability,
- restlessness,
- weakness,
- fatigue,
- inability to sleep properly,
- Physical changes such as
- weight loss,
- poor skin turgor,
- dry mucous membranes.
- Dry lips,
- pallor,
- shrinking of the eyelids,
- depressed fontanelles,
- Changes in vital signs such as
- low blood pressure,
- tachycardia,
- rapid respiration,
- cold limbs,
- decreased urinary output,
- loss of consciousness,
- Medical management of diarrhea:
- Provide rehydration therapy to the patient.
- Provide oral rehydration solution (ORS) to maintain the hydration status of the patient.
- Oral rehydration therapy is considered an effective treatment for mild to moderate dehydration.
- Provide intravenous fluid therapy to the patient
- If the patient has a condition of dehydration and ORS therapy is not properly effective, provide intravenous fluid therapy to the patient.
- Provide proper feeding to the child along with intravenous therapy to prevent malnutrition.
- Provide easily digestible food to the child who can take food through the mouth.
- Ex:= Toast, rice, blanched food.
- Maintain adequate fluid and electrolyte levels of the patient.
- If the patient has diarrheal disease due to any bacterial infection, provide antibiotic medicine.
- Provide antidiarrheal medicine to the child, such as,
Loperamide, Bismuth Subsalysilate. - Maintain proper fluid and electrolyte levels of the patient.
- Provide oral rehydration solution (ORS) to maintain the hydration status of the patient.
- Provide intravenous (IV) fluid therapy if the patient is severely dehydrated.
- Provide proper nutritional support to the patient.
- Treatment and Dietary Management in Acute Diarrhea:

- Acute diarrhea is of short duration. Due to which there is excessive loss of water and electrolytes. If it is not controlled, it can be fatal. Timely steps should be taken to rehydrate the patient by providing oral rehydration therapy which is a simple, inexpensive and effective treatment. It can be prepared at home and ORS packets are also available in the market as per the following standard WHO/UNICEF formula.
- Oral Rehydration Solution (ORS):
- Sodium chloride : 3.5 g,
Sodium bicarbonate : 2.5 g,
Potassium chloride : 1.5 g,
Glucose : 20 g. - Dissolve in 1 liter of clean drinking water.
ORT should be started as soon as the child passes a loose stool. - ORS should be given to the child as often as possible, the general rule is one glass after each stool.
- If the child is breast-feeding, it should be continued along with ORT. Other fluids such as coconut water, barley water, weak tea, buttermilk water, albumin water, buttermilk, cereal water and bean water should also be given.
- Chronic Diarrhea:
- Dietary management:
- The main objective of the watery management of chronic diarrhea is to replace water and electrolytes and to eliminate extra Providing nutrients.
- Energy requirements increase by 10-20% to compensate for lost weight and weakness. Fiber intake and fat intake should be restricted. More carbohydrates are needed to meet the high energy requirements. Mineral and vitamin supplements should be added to the daily diet.
- Foods to be Allowed:
- Washed pulses, refined cereals, well-cooked vegetables, bananas, papaya, milk products, chicken and fish.
- Foods to be Restricted :
- Whole Cereals, Pulses, Raw Vegetables and Fruits, Fried Foods, Nuts, Milk and Milk Based Beverages.
- Constipation
- Constipation is a condition in which feces (stool) are retained in the colon for a longer period than its normal emptying length. Constipation is characterized by irregular, infrequent, or difficult stool passage. Usually, the residue of food eaten one morning reaches the large bowel the next morning. Defecation usually occurs within 12-72 hours after eating. Constipation is a condition in which bowel movements are infrequent, difficulty in emptying the bowel occurs, difficulty in passing stool arises, or incomplete bowel evacuation/emptying occurs. The condition of constipation is mainly caused by the hardening of the stool, inadequate intake of fiber food and low water intake.
- Constipation is of two types: atonic and spastic:
- Loss of muscle tone in the colon or rectum can cause difficulty in evacuating stool and result in atonic constipation. This type of constipation is commonly seen in the elderly, pregnant women, and sedentary workers. This type is often called “Lasy bowel syndrome”.
- Spastic constipation is caused by increased muscle tone that narrows the lumen. Common causes of constipation include poor dietary habits such as irregular meals, inadequate fluid intake, emotional disturbances, and hemorrhoids.
- Treatment:
- The aim of treatment should be:
- Develop regular bowel habits.
- Follow a regular meal pattern.
•Consume a high-fiber diet.
•Increase exercise and activity.
- Dietary Management (Dietary management) :
- A normal diet with modifications in fiber and fluid intake is recommended.
- High-fiber foods such as whole grain cereals, whole pulses, green leafy vegetables and high-fiber fruits should be eaten in large amounts. Prunes and prune juice are beneficial. They stimulate intestinal motility.
- Patients are also advised to drink plenty of fluids. 8-10 glasses of fluids are advised a day. Constipation can also be relieved by drinking a glass of warm water, lemon juice, early in the morning. In cases of chronic constipation, inert laxatives like isabgol can be helpful. The use of mineral oils like liquid paraffin and castor oil should be discouraged as they seriously interfere with the absorption of fat soluble vitamins, vitamins A and K.
- Foods Recommended: Consume at least 1.5 liters of fluids, whole grain cereals, millets and oats, pulses with husks (legumes with husks), fibrous fruits and vegetables, milk, buttermilk, soups, green salads, peeled fruits and vegetables.
- Foods to be Avoided (Food to be avoided) : Refined cereals, pulses, castor oil and liquid paraffin etc.
- Peptic ulcer diet :

- “peptic ulcer” is a word made up of two words.
- 1)peptic,
2)ulcer - 1)peptic: Peptic comes from the Latin word “pepticus” .
- 2)ulcer: Ulcer comes from the Latin word “ulcus “ .
- Ulcus meaning a sore or a wound:
- A peptic ulcer is an erosion or excavation (hollow area) in the mucosal lining of the stomach and the first part of the small intestine (duodenum) The ulcer that forms is called a peptic or duodenal ulcer.
- Peptic ulcer is a sore or open sore that develops in the mucosal lining of the stomach and the first part of the small intestine, the duodenum. It is mainly caused by excessive secretion of acidic contents in the stomach. It is called peptic and duodenal ulcer. Hereditary, irregular food habits, mental stress and strain, excessive consumption of strong tea, coffee, spices, alcohol are predisposing factors for peptic ulcer. Anxiety, worry, stress, drugs such as analgesics cause hypersecretion of acid. The most common symptom of peptic ulcer is upper central abdominal pain. In peptic ulcer, there is a burning and pressing pain when the stomach is empty and, if there is a gastric ulcer, it may occur after meals. This can be accompanied by heartburn, vomiting, and weight loss. Bleeding may occur in some patients and may appear as black stools (melena) or vomiting of blood.
- If the peptic ulcer is in the stomach, it is called a gastric ulcer.
- If the peptic ulcer is in the first part of the small intestine (duodenum), it is called a duodenal ulcer.
- If the peptic ulcer is in the just upper part of the stomach, i.e. in the esophagus, it is called an esophageal ulcer. Comes.
- Types of peptic ulcer:
- There are two types of peptic ulcer.
- 1) Acute peptic ulcer,
2) Chronic Peptic ulcer (Chronic peptic ulcer) - 1)Acute peptic ulcer,
- Acute peptic ulcer is mainly superficial in which erosion of the superficial mucosal layer occurs. Acute peptic ulcer heals within a short time but if left untreated, bleeding and perforation can occur.
- 2) Chronic peptic ulcer
- Chronic peptic ulcer has a deep, sharp edge and a clean base. Chronic peptic ulcer also involves the mucosa and submucosa. If this ulcer penetrates the stomach, it also affects the organ (pancreas) near the stomach.
- Diet and feeding pattern:
- The approach to dietary management of peptic ulcers has changed considerably in recent times. The so-called bland diets used in the past for the treatment of peptic ulcers have proven ineffective. A diet that restricts foods that are mechanically, chemically, and thermally irritating to the gastrointestinal tract.
- Mechanically irritating: Mechanically irritating foods are those that increase peristaltic action due to their core, fibrous nature, e.g. whole grain cereals, skins, and fibers of fruits and vegetables.
- Chemically irritating: Chemically irritating foods stimulate gastric juices and are responsible for causing discomfort and pain. These foods include spices, condiments, meat extractives, fried foods, and stimulating beverages such as alcohol, tea, coffee, cola, and carbonated drinks. Thermal irritation is caused by very hot and cold foods. Therefore, changes in the bland diet are based on neutralizing gastric acid and decreasing bulk, which involves the following steps:
- Frequent feeding: Frequent feeding is necessary to continuously dilute and neutralize stomach contents.
- The quality of food: Stomach overfilling and distension arise To avoid this, the amount of food eaten should be small.
- Easily Digestible Fats: Easily digestible fats like whole milk fat, egg yolk, cream and butter are used in moderate amounts because they reduce the emptying time of the stomach and reduce motility.
- Try to avoid caffeine: Caffeine Try to avoid beverages such as coffee, cola, tea and alcohol.
- Avoid cigarette smoking.
- Avoid excessive spices and meat extracts.
- Avoid frequent use of drugs that damage the stomach lining, such as aspirin.
- Ulcers are known as a disease of the stomach, stomach, and intestines. Cold milk is a good buffer for ulcers.
- Boiling, baking, stewing and poaching are the preferred methods of cooking.
Food to be avoided:
- All whole grain cereals,
- All stimulating beverages,
- Wall pulses,
- Raw fruits,
- Spices, condiments and fried foods.
Care of the patient with dysphagia:
- Dysphagia means difficulty in swallowing This condition differs from patient to patient. Because some patients may have difficulty in swallowing some food. But some patients find it impossible to swallow. Some may choke while coughing or eating or drinking. While giving food to such patients, the nurse needs to understand the patient’s condition and rest for at least half an hour before taking food. After resting, the person’s swallowing difficulty reduces and he becomes able to swallow food. After resting, they should be seated upright in a chair. If the patient is on bed rest, raise the head end to a 90-degree angle as per the patient’s tolerance. Then provide liquids as per the patient’s preference. Avoid distractions while the patient is feeding as the focus is mainly on swallowing. Sudden coughing, choking, cyanosis, changes in voice, hoarseness, clearing the throat after eating and regurgitation are some of the signs of aspiration. It is advised to reduce the use of sedatives or hypnotics as these agents may interfere with swallowing.
- Causes of dysphagia:
- Aging,
- Muscular dystrophy,
- Myasthenia Gravis,
- Stroke,
- Cerebral Palsy,
- Multiple Sclerosis,
- Connective Tissue Disorder,
- Vagotomy,
- Guillain Barre Syndrome,
- Muscular Dystrophy,
- Parkinson’s Disease,
- Diabetic Neuropathy,
- Candidiasis,
- Head and Neck Cancer,
- Mediastinal Mass,
- Cervical spondylosis,
- Peptic ulcers, etc.
Care of the patient with Anorexia nervosa:
- Anorexia nervosa is a serious and potentially life-threatening eating disorder and self-starvation, in which the person has a fear of gaining weight and disturbing body image. Therefore, the person restricts food intake to lose body weight, thereby losing weight. Boys and girls self-restrict their diet to achieve slimness and weight loss. Anorexia is a syndrome in which three essential criteria are found
such as,
1) Self-induced starvation. - 2) Fear of becoming fat and excessive desire to become thin.
- 3) Medical signs and symptoms due to starvation.
- Types of Anorexia:
- There are two types of anorexia, namely
- 1) Restrictor type,
2) Bulimic (Binging (uncontrolled episodes of eating) and Purging (self-induced vomiting)) type. - 1) Restrictor type:
- In this type, the person restricts food, meaning that food Eating is avoided.
- 2) Bulimic (Binging and Purging) Type:
- (Binging (uncontrolled episodes of eating) and Purging (self-induced vomiting)) Type. In bulimia, the person eats uncontrollably and then self-induced vomiting due to fear of becoming excessively fat.
- Anorexia nervosa is an eating disorder. In this disorder, the person is obsessed with what he eats and his weight. Therefore, he places restrictions on his food intake and refuses to eat at times. But some diseases can also lead to anorexia [loss of appetite]. When the patient has loss of appetite, he should be encouraged to eat frequently and given light meals. It is good to advise family members to eat with the patient. Bringing them to the dining table is an encouraging and stimulating act for the patient to eat. The patient should be encouraged to keep a food diary which he can refer to whenever he wants. Maintain oral hygiene. Blood values or other investigations should be done to identify any underlying disorders.
- Management of Anorexia Nervosa:
- Provide proper comprehensive care to the patient.
- Provide proper medical treatment to the patient.
- If the patient has a condition of electrolyte imbalance or dehydration, advise him to take adequate fluid intake.
- Advise the patient to take a properly nutritious diet.
- Provide proper psychotherapy to the patient.
- Provide education to the patient’s family members to provide proper care to the patient.
- Provide proper interpersonal therapy to the patient.
- Conduct regular physical examinations of the patient, including daily weight monitoring of the patient.
- Conduct proper laboratory investigations of the patient.
- Provide proper psychotherapy and proper medication to the patient.
- Advise the patient on proper behavioral modification and nutritional rehabilitation.
- Advise the patient to feed in small and frequent amounts.
- Provide the patient with proper work and a comfortable environment.
Care of the patient with nausea and vomiting:
- Nausea is the sensation of vomiting. Vomiting is the expulsion of stomach contents through the mouth. Vomiting, also known as emesis, is the forceful expulsion of stomach contents through the mouth and sometimes through the nose. Vomiting is a reflux process that is stimulated by the vomiting center in the medulla oblongata. During vomiting, the duodenum contracts, causing the duodenal contents to enter the stomach. After this, the stomach and abdominal muscles contract, and the stomach contents are forcefully expelled through the mouth and sometimes through the nose. Although vomiting requires little attention, if there is frequent and persistent vomiting, it is considered a serious condition and requires proper evaluation. If there is persistent vomiting, there is a chance of dehydration, electrolyte imbalance, and aspiration of vomiting. Aspiration of vomiting can lead to conditions such as asphyxia (suffocation), pneumonia (infection and inflammation of the lung parenchyma), and atelectasis (collapse of a lung or part of a lung). Other symptoms of vomiting include excessive salivation, tachycardia, tachypnea, sweating, dilated pupils, and pallor. Symptoms like are also seen.
- The patient should be asked to brush twice a day and maintain oral hygiene. The underlying cause needs to be treated. Home remedies like ginger water can be tried and fatty foods can be avoided. If the patient is bedridden, then the patient should be provided with a side lying position to prevent aspiration of vomit.
- Causes of vomiting:
- The causes of vomiting are divided into non-organic and organic causes.
- Non-organic causes
- 1) In neonate:
- Due to swallowing of amniotic fluid and blood.
- Due to faulty feeding technique.
- Due to side effects of drugs.
- 2) In infants:
- Due to gastroesophageal reflux.
- Due to overfeeding.
- Due to anatomical obstruction.
- Due to systemic infection.
- Due to gastroenteritis.
- Due to excessive crying.
- Due to faulty feeding habits.
- 3) In childhood:
- Due to excessive overfeeding.
- Due to gastritis.
- Due to any type of behavioral disorder.
- Due to gastroesophageal reflux.
- Due to medication.
- Due to systemic infection.
- Due to sinusitis.
- Due to otitis media.
- Organic cause
- 1) Infections
- Due to viral hepatitis.
- Tonsillitis.
- Due to acute respiratory infection.
- Intrauterine infection
- Meningitis.
- Due to otitis media.
- Due to pancreatitis.
- 2) Mechanical condition.
- Due to congenital anomalies.
- Due to tracheoesophageal fistula (TEF).
- Due to pyloric stenosis.
- Esophageal atresia.
- Due to intestinal obstruction.
- Due to hiatus hernia.
- 3) Neurological cause
- Due to abnormality of the central nervous system.
- Due to birth asphyxia.
- Due to birth defect.
- Due to intracranial hemorrhage.
- Due to increased intracranial pressure.
- Due to subdural hematoma.
- 4) Metabolic cause
- Diabetes mellitus. Due to uremia.
- Due to galactosemia.
- Due to hypoglycemia.
- Due to inborn error of metabolism.
- 5) Toxic agent
- Due to food poisoning.
- Due to drug poisoning.
- Due to allergic food intake
- Due to psychiatric condition.
- Medical management of vomiting:
- Proper assessment of the patient.
- If the patient’s vomiting condition is due to a non-organic cause, provide sips of water appropriately.
- Properly assess the patient’s hydration status.
- Properly maintain the patient’s hydration status.
- Properly assess the patient’s electrolyte balance.
- Continuously observe the patient.
- Continuously assess the consistency, frequency, and duration of the patient’s vomiting.
- Properly assess the patient’s hydration status.
- Properly assess the patient’s vital signs.
- Provide intravenous fluids to maintain the patient’s hydration status and prevent electrolyte imbalance.
- Provide the patient with prescribed antiemetic medication.
- Properly investigate the patient’s blood.
- Provide the patient with small amounts of easily digestible bland food if the vomiting subsides.
- Properly tilt the patient’s head to one side to prevent aspiration of vomit.
- Provide proper comfort measures to the patient.
- Advise the patient to maintain proper hygienic conditions.
- Involve family members in the patient’s care and provide proper emotional support to the parents.
- Collaborate with other health care personnel for proper care of the patient.
- Provide education to the patient to take medication properly.
- Advise the patient to have regular follow-up.
Artificial method of feeding (Artificial method of feeding)
Nasogastric intubation:
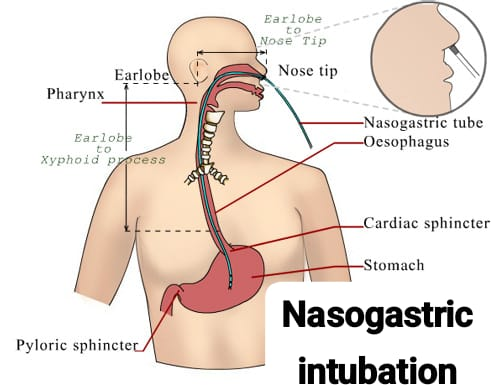
Definition (Definition) :
Nasogastric intubation is a procedure to insert a tube through the nose into the esophagus and stomach.
Indications of nasogastric intubation:
- When the patient is unable to ingest, chew, and swallow food When.
- If there is a fracture of the (jaw).
- When the patient refuses food.
- When the patient is too weak to swallow food.
- When the patient is unable to retain food.
- If the mouth, throat, and esophagus have undergone surgery. When.
- When there is paralysis in the face and throat.
Contraindications of nasogastric intubation:
- Gastric surgery,
- Esophageal Surgery,
- Polyps in the nose,
- Deviated nasal septum,
- Ulcers,
- Tracheoesophageal fistula.
General Instructions (General instructions):
- If the patient has dentures, they should be removed to prevent dislodging and blocking the respiratory tract.
- A rubber tube can be placed in a bowl of ice to cool and stiffen it.
- Lubricate the tube with a suitable lubricant: preferably soluble jelly.
- When removing the tube, pinch the tube and pull it out gently and quickly so that fluid does not trickle down the pharynx.
- Do not use force when introducing the tube. Due to this, it damages the mucous membrane and there are chances of injury.
- Watch for complications like nausea, vomiting, distension, diarrhea, aspiration, pneumonia.
- Procedure:
- Preparation of the Patient (Preparation of the patient):
- Identify the patient’s name, bed number, etc.
- Check the doctor’s order to see if there are any specific precautions for the patient’s movement and positioning.
- Check the patient’s level of consciousness.
- Check the patient’s ability to move.
- Explain the procedure properly to the patient to gain the patient’s confidence.
- Provide the patient with proper privacy through a screen.
- Provide the patient with proper mouthwash to clean the mouth.
- Clean the patient’s nostrils properly.
- Preparation of the Articles:
- A tray containing:
- A small Macintosh with a towel: To protect the bed, linen.
- A bowl of cold water containing the Rhyles tube: To make the tube hard for easy insertion.
- A cotton-tipped applicator: To clean the nostril.
- A water-soluble jelly-like lubricant: To lubricate the Rhyles tube to prevent friction between the mucous membrane and the tube.
- Adhesive plaster and scissors: To fix the tube in position.
- A bowl of water, stethoscope: To test the location of the tube.
- Saline or soda bicarbonate solution: To clean the nostril.
- A kidney tray and paper bag: To collect the waste.
- Steps of Procedure:
- Wash hands with soap and water: To prevent cross-infection.
- Spread a mackintosh and towel: To protect bed linen.
- Clean nostrils with a cotton-tipped applicator soaked in saline: To clean nostrils.
- Take a Rhylus tube and measure the distance from the bridge of the nose to the earlobe, then from the earlobe to the tip of the xiphoid process of the sternum to insert the tube and mark it with adhesive: To determine the approximate length of the tube to reach the stomach.
- Lubricate the tube with water-soluble jelly for about 6-8 inches: Lubricating the tube reduces friction between the tube and the mucous membrane.
- Hold the coiled tube in the right hand to introduce the tube: The nasal septum deviates to the right side.
- Tilt the patient’s head back before inserting the tube into the nostril and pass the tube slowly into the posterior nasopharynx: Following the natural contours of the body facilitates passage of the tube.
- The patient may gag reflex when the tube reaches the pharynx, let him relax for a few moments: The gag reflex is triggered by the presence of the tube. Helps prevent aspiration.
- Hold the patient’s head in a partially flexed position: The flexed head position makes swallowing easier and less likely to enter the trachea.
- Continue advancing the tube until it reaches the previously made mark: The mark on the tube indicates that the tube has reached the stomach.
- Aspirate gastric contents with a syringe: Fluid cannot be aspirated freely from the lungs. The glands of the mucus membrane lining the esophagus and stomach produce mucus and gastric juice.
- Place the end of the tube in a bowl of water and note the rhythm of the escaping bubbles: If the tube is in the trachea, the bubbles will be in sync with the expiration of the breath. Normal respiration occurs in the lungs, resulting in air being expelled with expiration.
- Ask the patient to speak: If the patient is unable to speak, the tube will be in the trachea.
- The conformation of the tube’s place can be confirmed using a stethoscope: When air is flushed, a flushing sound will be heard over the stomach.
- Take 5-10 ml of air and push it into the distal end of the tube: The air pushed in with force produces a hushing sound.
Nasogastric feeding:
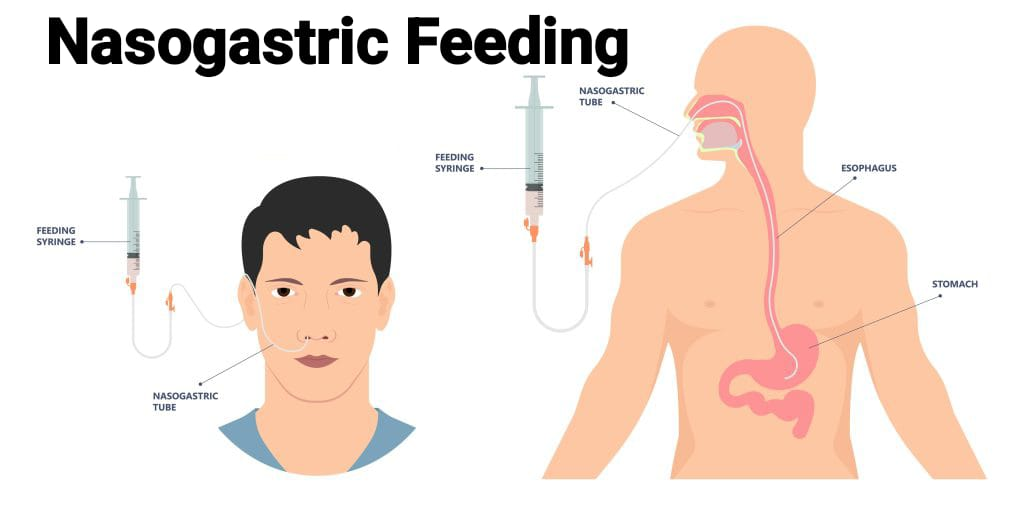
- Nasogastric feeding is an artificial method of delivering fluids and nutrients through an artificial tube that passes through the nose, mouth, or nasopharynx into the esophagus and stomach.
- Method of Administration:
- 1) Continuous Feeding Method:
- This method is used for critically ill patients. Continuous drip-feeding helps in minimizing nausea, cramping, and diarrhea. The infusion pump uses gravity flow of fluid at a rate of 500 ml/hr.
- 2) Intermittent Feeding Method:
- In intermittent feeding method, feeding is provided periodically. 400 ml is given every time for a duration of 30 minutes and four to five times a day through drip method.
- 3) Bolus Feeding Method:
- Slowly pour the prescribed amount of fluid (250-400ml) into the barrel of a syringe or funnel attached to the end of the tube. Fluid flows into the stomach by gravity.
- Indications of Nasogastric feeding:
- Tube feeding is indicated when the patient is unable to ingest, chew or swallow food but is still able to digest and absorb nutrients. E.g. in cases of unconscious and semiconscious patients.
- When the patient is too weak to swallow food or when conditions make it difficult for him to take large amounts of food orally. E.g. conditions like acute and chronic infections, severe burns, malnutrition and prematurity etc.
- When the patient is unable to retain food. E.g. vomiting, anorexia nervosa etc.
- When the condition of the mouth and esophagus makes swallowing difficult or impossible.
- For patients who refuse to take food. For example, patients with depression.
- Contraindication:
- Gastric surgery,
- Tructoesophageal fistula,
- Paralytic ileus,
- Acute abdominal pain.
- General instructions:
- Feedings can be given at intervals of 2, 3 or 4 hours and the amount should not exceed 150 to 300 ml per feed. The total amount in 24 hours varies between 2000 and 3000 ml. If the drip method is used, the flow rate should not exceed 10 to 60 ml per minute. This causes distension, nausea, regurgitation and excessive peristalsis which are associated with excessive and rapid administration.
- Gastric or nasogastric feeding should be given by the doctor’s order.
- If the patient is conscious, provide reassurance to the patient to gain his confidence and cooperation.
- Wash hands properly before providing nasogastric tube feeding.
- Record the patient’s intake-output accurately.
- Assess the patient for complications such as nausea, vomiting, distention, diarrhea, aspiration, pneumonia, asphyxia, fever, water and electrolyte imbalance. Water and electrolyte imbalance may be reflected by changes in skin, vital signs, intake and output, level of consciousness, body weight, moisture of mucous membranes and serum analysis.
- Articles :
- A tray containing:
- Feeding cup with water: For rinsing the mouth before and after feeding.
- Kidney tray.
- Towel: To protect garments and linen.
- Paper bag: To collect waste.
- A clean 50 cc syringe or funnel in the tray: To provide nasogastric feeds.
- A glass of feed in a bowl of warm water: To provide feed at body temperature.
- Ounce glass: To measure fluid intake.
- 5 CC clean syringe: To aspirate before providing nasogastric feeding.
- Procedure:
- After inserting the nasogastric tube into the gastric cavity, aspiration is performed. If the output is less than the input, nasogastric feeding is given as per the doctor’s order.
- If the residual content is within the normal limit and the placement of the tube is confirmed, return the gastric content to the stomach using gravity using a 5 CC syringe. Spread a towel over the patient’s neck: Prevents fluid electrolyte imbalance by returning gastric contents to the stomach.
- If tube placement in the stomach is confirmed, pinch the feeding tube and attach the barrel of the feeding syringe distension to the tube: Pinching the feeding tube prevents air from entering the stomach and prevents stomach distension.
- Raise the barrel of a feeding syringe full of water above the patient’s head level and allow the fluid to enter by gravity: The water cleans the tube and the rate of flow is regulated by raising or lowering the syringe.
- Pour the feed into the syringe barrel and let it flow by gravity. Continue pouring feed/formula into the barrel when it is three-quarters empty. Pinch the tube whenever necessary to stop pouring: To prevent air from entering the tube.
- When the feeding is complete, flush the tube with 30 ml of plain water: This will prevent clogging of the feeding tube.
- When the tube is clear, properly close the end of the feeding tube: To prevent leakage and air from entering the patient’s stomach.
- Wash all equipment properly with warm water and dry it properly and then replace it every 24 hours as per the hospital policy: To prevent bacterial concentration.
- Nasogastric feeding is given in the semi-Fowler position, then the head of the bed is kept at 30-60° for at least 30 minutes: This can prevent regurgitation.
- Proper hand washing: To reduce the risk of transmission of microorganisms.
- Properly document the amount and type of feeding, amount of water, and tolerance of the feed.
- Properly monitor the patient’s breath sounds, bowel sounds, gastric distension, diarrhea, system and therapeutic effect of feeding, and intake output: Evaluates the effect of aspiration on the gastrointestinal system and the therapeutic effect of feeding.
- Properly monitor the patient’s breath sounds, bowel sounds, gastric distension, diarrhea, intake output of the system and the therapeutic effect of feeding: Evaluates the effect of aspiration on the gastrointestinal system and the therapeutic effect of feeding.
- Provide instructions to the patient to notify the nurse if the patient experiences a sensation of fullness, nausea, and vomiting: which indicates feeding intolerance.
આફ્ટર કેર ઓફ ધ પેશન્ટ એન્ડ આર્ટીકલ્સ (After care of the patient and articles) :
- પેશન્ટને માઉથવોશ ઓફર કરવું પેશન્ટ નું ફેસ અને હેન્ડ ક્લીન કરવા અને તેને ડ્રાય કરવા.
- પેશન્ટના નેક ની અરાઉન્ડમાં રહેલા ટોવેલ ને રીમુવ કરવો.
- પેશન્ટને બેડ પર કમ્ફર્ટેબલ પોઝિશન પ્રોવાઇડ કરવી.
- જો અન્કંશીયસ અથવા સિરિયસલી ઇલ પેશન્ટ હોય અને જો પેશન્ટના માઉથ માં સિક્રીસન એ કલેક્ટ થયેલું હોય તો સક્ષન એપ્લાય કરવું.
- બધા જ આર્ટીકલ ને યુટીલીટી રૂમમાં લઇ જવા વેસ્ટ ને પ્રોપર્લી ડિસ્કાર્ડ કરવા અને આર્ટીકલ્સ ને શોપ અને વાર્મ વોટર દ્વારા ક્લીન કરવા ત્યારબાદ પ્રોપર્લી ડ્રાય કરવા અને તેને તેની પ્રોપર પ્લેસ પર રિપ્લેસ કરવા.
- પ્રોપર્લી હેન્ડ વોશિંગ કરવા.
- પેશન્ટ ને ફીડિન્ગ પ્રોવાઇડ કરેલું હોય તેનું પ્રોપર્લી રેકોર્ડિંગ અને રિપોર્ટિંગ કરવું.
- જ્યારે ટ્યુબ ફીડિંગ સ્ટોપ કરવાનું હોય ત્યારે ડોક્ટર્સ ઓર્ડર મુજબ ટ્યુબ ને રિમૂવ કરવી.
Gastrostomy Feeding:
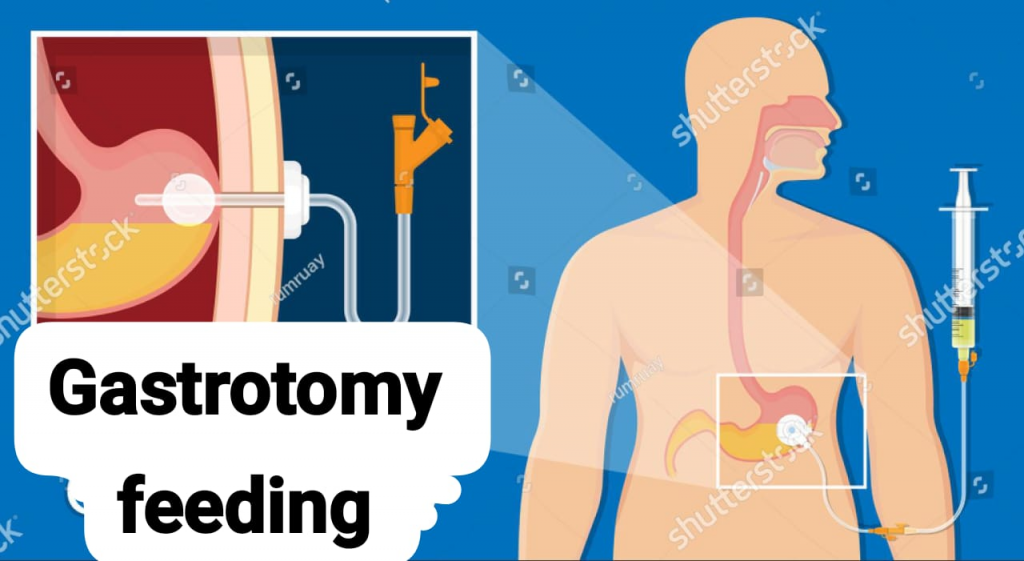
- An artificial, surgically created opening connecting the inside of the stomach to the abdominal wall through which a tube is placed. In a gastrostomy, a portion of the stomach is brought up to the abdominal wall and an opening is made through the abdominal wall. A tube is inserted through which feedings can be given. It is essential that the feeding should be as per the doctor’s orders.
- Method of gastrostomy feeding:
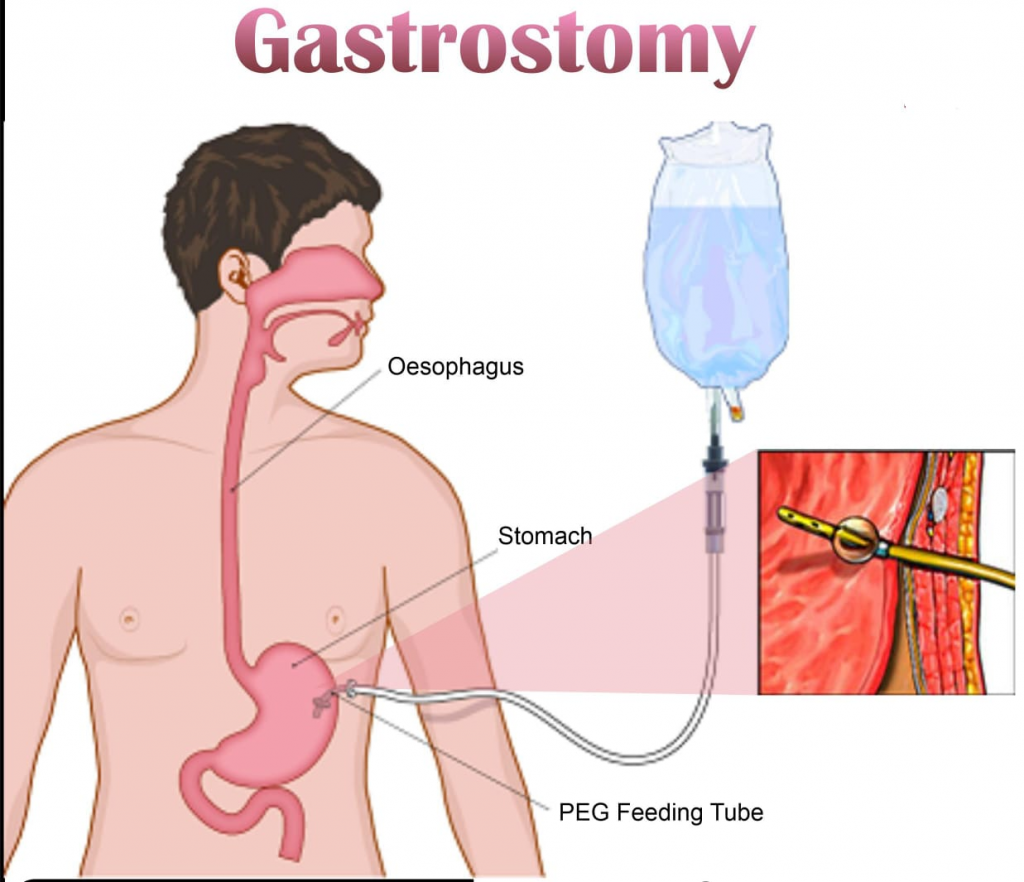
- Syringe Feeding: In this method, a 50 CC syringe is used to give the feed as per the physician’s order.
- Indications of gastrostomy feeding:
- Patients with impaired swallowing.
- The patient’s level of consciousness is decreased.
- Tumors or fistulas in the upper alimentary tract.
- In cases after operations on the alimentary tract, when the normal route makes it impossible for food to reach the stomach.
- A try containing:
- Feeding with water.
- Kidney tray.
- 50 CC and 5 CC clean syringes.
- One ounce glass.
- Procedure:
- Properly assess the client for gastrostomy feeding needs: Identifies clients who require gastrostomy feeding.
- Auscultate bowel sounds before feeding and consult a physician if bowel sounds are absent: Absent bowel sounds indicate decreased or absent peristalsis movement, which increases the risk of aspiration and abdominal distension.
- Obtain patient baseline weight and laboratory values: Provides objective data to measure the effectiveness of feeding.
- Verify physician’s order for feeding formula, rate, route, and frequency: Gastrostomy feeding must be ordered by a physician.
- Properly assess for any breakdown, irritation, or drainage at the gastrostomy site: Infection, pressure from the gastrostomy tube, or gastric secretions can cause skin breakdown.
- Properly explain the procedure to the client: If the patient is properly informed, greater patient cooperation can be obtained and the procedure can be performed easily.
- Proper hand washing: To reduce the transmission of microorganisms.
- Preparing a feeding container to administer formula continuously
- a) Tube feeding should be at room temperature: Cold formula can cause gastric cramping and distension because it is not warmed by the mouth.
(b) Attach tubing to the container as needed or prepare a ready-to-hang container.
(c) Stir the formula well. Fill the container and tubing with formula. - Elevate the head of the patient’s bed at 30 to 45°: Elevating the client’s head helps prevent the chance of aspiration.
- Apply gloves and verify tube placement.
- Attach a syringe and aspirate gastric contents/secretions, observe their appearance, and check pH: Fluid from a gastric tube in a client who has fasted for at least 4 hours usually has a pH range of 1 to 4, especially when the client is not receiving gastric acid. Continuous administration of tube feedings may elevate pH. Gastric residuals determine gastric emptying, delaying gastric emptying. Delayed gastric emptying is indicated by 100 ml because more is left in the client’s stomach from the previous feeding.
- Use of water via feeding tube as ordered with or between feedings: Provides the client with a source of water to maintain fluid and electrolyte balance.
- Flush the tube with 30 ml of water every four to six hours before and after administering medication through the tube: Maintains patency of the tube and provides the client with some free water. Small gastrostomy tubes are prone to clogging and are difficult to replace.
- Close the proximal end of the gastrostomy tube with a cap or clamp when tube feedings are not being administered: Properly closing the tube prevents excess air from entering the gastrostomy tract and prevents leakage of gastric contents.
- Properly rinse the container and tube with warm water after providing all intermittent feedings: Rinsing the container and tube with warm water clears old tube feedings and prevents bacterial growth.
- The gastrostomy exit site is usually left open to the air. However, if a dressing is required due to drainage, change the dressing daily or as needed and notify the physician of the drainage. Inspect the exit site at each shift: Gastric drainage leakage can cause irritation and excoriation. The skin around the feeding tube should be cleaned daily with warm water and mild soap; a small piece of gauze dressing may be applied to the incision.
- Proper disposal of supplies and hand washing: Reduce transmission of microorganisms.
- Evaluate the client’s tolerance to tube feeding. Evaluate the amount of aspirate every 8-12 hours: Evaluation of tolerance to tube feeding is done by checking.
- Monitor the client’s fingerstick blood glucose level every 6 hours until the maximum rate of administration is reached and maintained for 24 hours: Alerts the nurse to the client’s glucose and fluid intake volume tolerance.
- Monitor the patient’s intake-output every 8 hours: Intake output is an indication of fluid balance.
- Weigh the client daily until the maximum rate of administration is reached and maintained for 24 hours. Then weigh the client 3 times a week: Weight gain is an indicator of impaired nutritional status. However, a sudden gain of more than 2 lb in 24 hours suggests fluid retention.
- Monitor the patient’s laboratory values for return to normal: Improving laboratory values indicate a return to normal nutritional status.
- Assess stoma for skin integrity: Gastric secretions can cause injury or necrosis at the stoma site.
- Properly record and report the procedure.
- Complications of Gasterostomy feeding:
- The skin surrounding the gastrostomy site may break down.
- When gastric emptying is delayed and formula is administered rapidly, the client may aspirate the formula and vomiting may occur.
- The client may develop diarrhea: Diarrhea indicates intolerance.
- Nurses Responsibility during gasterostomy feeding:
- Properly care for the skin around the patient’s gastrostomy site and keep it properly clean and dry.
- To protect the skin from irritation from hydrochloric acid Applying a waterproof ointment such as zinc oxide around the tube can be helpful.
- Keep changing the patient’s position. Provide the patient with a side-lying position in the main preferable position to prevent aspiration of contents.
- Suction the patient’s airway to keep it clear but do not suction while providing feeding.
- Assess the patient for any complications such as loose stools, wound infection, etc.
- Report any abnormalities to the physician.
- Properly record and report the amount, type, and client response to feeding.
- Maintain proper intake-output charting of the patient.
Parenteral feeding/Nutrition:
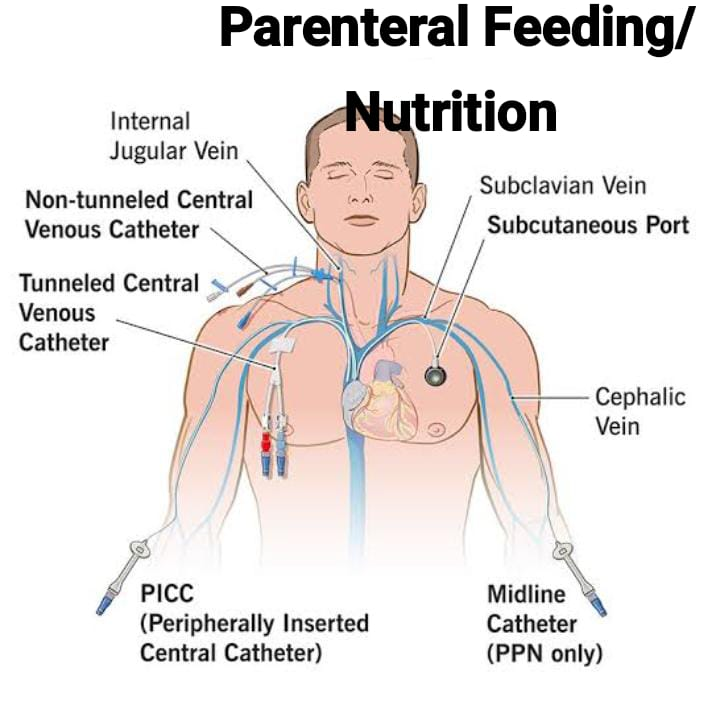
- Parenteral feeding is the provision of therapeutic agents and also involves food, which is provided from outside the alimentary tract. In other words, it forces fluid into cavities, blood vessels, or body tissues through a hollow tube or needle. Parenteral nutrition (PN), a solution containing glucose, amino acids, lipids, minerals, electrolytes, trace elements, and vitamins, is infused through a peripheral or central venous catheter. The solution is a combination of all nutrients given collectively through an intravenous route, which is called “total parenteral nutrition”.
- Indication of parenteral feeding:
- When the client is unable to eat or drink for an extended period of time.
- When the client is unable to absorb nutrients and fluids provided through the gastrointestinal tract.
- Unconscious patients who are unable to absorb gastrointestinal nutrients.
- Initiation of parenteral nutrition:
- A central venous catheter (CVC) is placed in the jugular vein as a subclavian vein for parenteral nutrition therapy. The nurse assists in this procedure to insert the central venous catheter. Specially trained nurses insert peripherally inserted central catheters (PICCs). Chest x-ray films are used to confirm the location of the central venous catheter. The client may have a long-term central venous access device, such as a tunneled catheter or implanted port. Before starting the infusion, verify the physician’s orders. An infusion pump is always used. It is recommended to start the infusion at 40 to 60 mL/hr. The rate is gradually increased until the client’s nutritional needs are completely met.
- Care of a client receiving parenteral nutrition:
- Nursing care of a client receiving PN is based on four major nursing goals:
- 1) Prevent infection.
- 2) Maintain the parenteral nutrition system.
- 3) Prevent metabolic, electrolyte, or fluid balance complications.
- 4) Assess the client’s readiness for parenteral nutrition (PN).
- Primary methods of preventing infection include asepsis during insertion and care of central venous catheters, use of in-line filters, and maintaining secure, uncontaminated tubing connections. (Parenteral Nutrition) PN solutions should not exceed their 24-hour infusion limit.
- Regularly monitor laboratory measurements of clients receiving parenteral nutrition.
- Continuously test the client’s blood glucose level and urine glucose level when parenteral nutrition is initiated to assess the client’s metabolic tolerance.
- Be alert when there are changes in vital signs and fluid balance and abnormal laboratory results as they indicate infection, hyperglycemia and electrolyte imbalance.
- Report any unusual symptoms to the physician.
- If body temperature is increased, increased temperature is an early sign of infection so report to the physician.
- Complications of the catheter insertion:
- Arterial puncture,
- Air embolism,
- Catheter embolism,
- Pneumothorax.
- Complications of total parenteral nutrition:
- Fluid and electrolyte imbalance or circulatory overload.
- Infiltration.
- Embolism and thrombus.
- Phlebitis.
- Hyperglycemia.
Total Parenteral Nutrition (TPN):
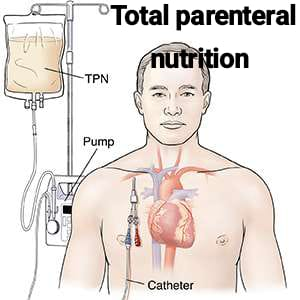
- Total Parenteral Nutrition is a parenteral Also known as nutrition, it involves the administration of nutrients such as amino acids, lipids, dextrose, vitamins, minerals and water through the bloodstream, through a venous access device.
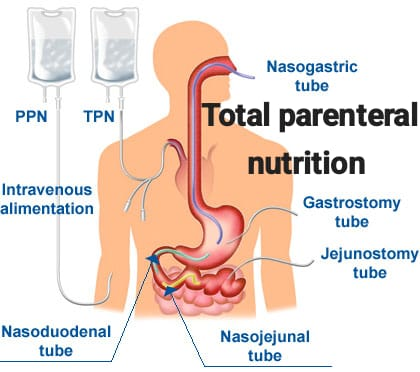
Purpose:
- To replace acute nutritional deficiencies.
- To restore the fluid lost from the body.
- To fulfill the patient’s basic requirement of calories, water, minerals and vitamins.
- When the patient To supply nourishment and fluid to the body when oral intake is contraindicated.
- To promote the client’s fluid, electrolyte, and acid-base balance.
Indications:
- In patients with a paralyzed or non-functional GI tract or conditions requiring bowel rest, Such as small bowel obstruction, intestinal obstruction, ulcerative colitis, pancreatitis, inflammatory bowel disease etc.
- Patients who need to be on NPO for seven days or more.
- Critically ill patients.
- Patients with chronic or extreme malnutrition, chronic diarrhea or vomiting and requiring surgery or chemotherapy.
- Patients with hypermetabolic states, such as burns, sepsis, or trauma.
- Patients with severe eating disorders such as anorexia nervosa and bulimia nervosa.
Methods of parenteral nutrition:
- 1) Total Nutrient Admixture:
- Route: Central vein, usually enters the superior vena cava.
- Component and Indication:
- It is a formula that combines carbohydrates, in the form of a concentrated (20-70%) dextrose solution, proteins in the form of amino acids (3-15%), lipids in the form of emulsions (10-30%), including triglycerides.
- It is used for patients who require parenteral feeding for 7 days or more.
- 2) Peripheral Parenteral Nutrition:
- Route: Peripheral vein
- Component and Indication:
- The formula combines amino acids, vitamins, minerals and lipids in a low concentration dextrose solution.
- Indicated for patients requiring parenteral feeding for less than 7 days who do not already have enteral access.
- 3) Total Parenteral Nutrition :
- Route: Central vein/Peripheral vein
- Component and Indication :
- Combines dextrose, amino acids, vitamins and minerals. Lipids can also be mixed with the TPN solution if necessary. Fat emulsion (lipids)-10%, 20% or 30% emulsion composed of triglycerides, e.g. phospholipids, glycerol and water.
- Indicated for patients requiring complete parenteral administration (TPN).
- Preparations of Articles:
- A tray containing:
- Parenteral nutrition bag (mixture of lipids/nutrients): To administer nutrients to the patient.
- Volume control infusor: To regulate the flow of fluid.
- Administration tubing with Luer-lock connections: To administer fluid safely.
- Hypoallergenic tape: To secure dressing to site.
- Sterile dressing kit: For dressing catheter site.
- I/V stand: To hang feeds.
- Sterile gloves: Universal precautions.
- Preparation of the patient/unit:
- To identify patient by name and bed.
- Explain the procedure to the patient properly to gain the patient’s confidence and cooperation.
- Check the physician’s order for the type of fluid and the patient’s position and any specific pacifications.
- Properly collect all articles at the patient’s bedside.
- Assess the patient’s need for parenteral feeding and evaluate the patient’s nutritional status.
- Assess whether the patient has any allergies.
- Verify the physician’s order for formula, rate, route, and frequency.
- Assess baseline weight and laboratory values.
- Remove the nutrient admixture from the refrigerator at least 1 hour before administering the feeding to the patient.
- Hang on I/V stand (if refrigerated). Check date and patient name.
- Inspect fluid for cracking or creaming. Discard if present.
- Steps of procedure:
- Proper hand washing with soap and water: To reduce transmission of microorganisms.
- Using sterile technique, attach I.V. tubing (with filter) to nutrient admixture bag and remove air: Prevents air embolism.
- Close all clamps on new tubing and insert tubing into volume control infuser: To prevent free flow of parenteral nutrition fluid.
- If the venous access device (VAD) has a clamp at the proximal end, clamp the tubing: This prevents air embolus if the VAD is inserted into a central vein.
- If no clamp is available on the central (VAD), instruct the patient to perform the Valsalva maneuver while the new tube is attached: This creates positive pressure and prevents air from entering the tubing.
- Using sterile technique, connect the tubing to the hub of the VAD, ensuring that the connection is securely attached using a Luer-Lock connection: This prevents tubing disconnection.
- Open all clamps and regulate flow with a volume-controlled infusion: This maintains the appropriate administration rate.
- If dressing changes are indicated, use sterile technique to prevent site infection.
- Aftercare of the patient and articles:
- Assist the patient in providing a comfortable position: To help the patient feel well.
- Clean all articles with soap and water, place them back in their proper place, allow to dry, and replace. Dispose of disposable items according to protocols: To maintain cleanliness of equipment and control transmission of infection.
- Proper hand washing: To control transmission of infection.
- Recording the date, time, rate, amount and type of fluid, changes in tubing, patency of the tube and any unwanted effects: Documents the patient’s response to the therapy and identifies the presence of any adverse reactions.
- Points to remember:
- Properly check the label which indicates the nutrient content, all additives, mixing time and expiry date and time.
- Change the tubing every two to three (2-3) days to prevent the patient from being exposed to bacterial growth in the tubing.
- Confirm the position of the catheter tip and exclude traumatic pneumothorax, which is the most common complication related to catheter placement, before starting feeding. A chest radiograph should be obtained.
- The central catheter should be flushed daily with diluted heparin to avoid catheter thrombosis.
- With proper care, the central catheter can be maintained for several days or weeks to provide total parenteral nutrition (TPN).
- Nutritional monitoring: It is recommended that the following parameters be measured daily during TPN: body weight estimation; 12-hour intake-output chart; 8-hour urine-sugar no estimation; serum sodium, potassium, bicarbonate, calcium, and chloride; blood urea and serum creatinine levels. Liver function tests and serum protein should be measured twice daily.
- Check vital signs every four hours.
- Use aseptic technique when changing solutions, tubing, filters, or dressings.
- Check that all connections are securely taped and that catheters are clamped before opening the system.
Compare the patient’s daily weight with fluid intake and output.
- Gastric irrigation:
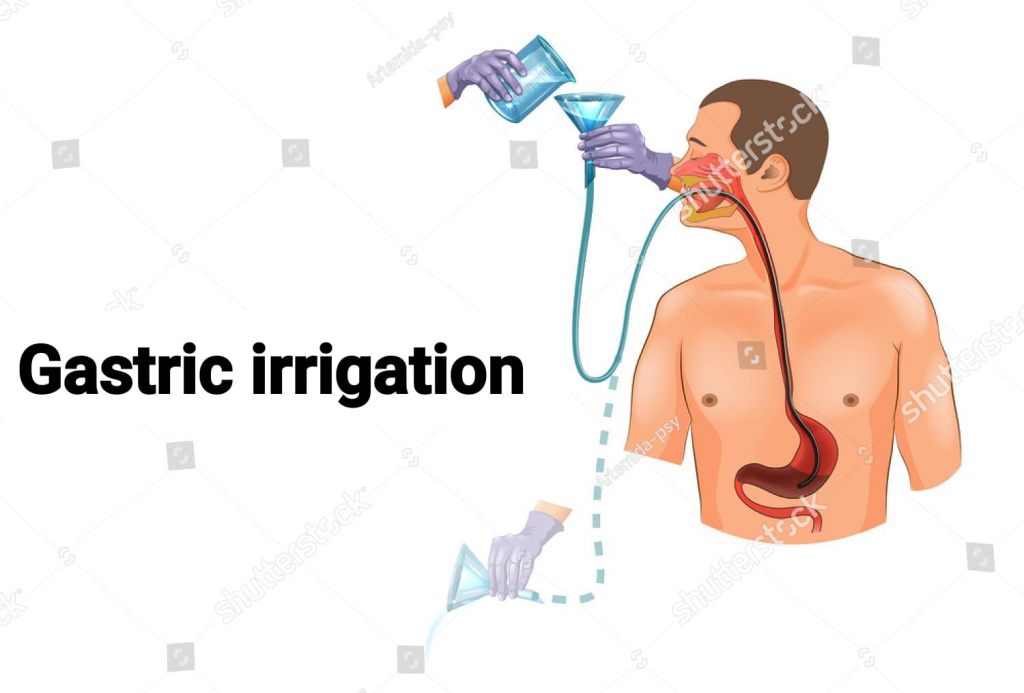
- Gastric irrigation or stomach wash means washing out or irrigating the stomach with a solution. This procedure is most frequently used to provide emergency treatment during emergency conditions such as gastric dilation and poisoning.
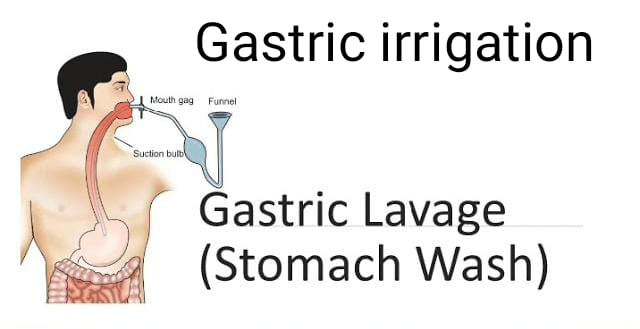
- Purpose :
- To remove poison from the stomach before it is absorbed into the gastrointestinal tract.
- To relieve nausea and vomiting when acute dilatation of the stomach is performed and in conditions of intestinal obstruction.
- To collect gastric contents for identification of poison.
- To obtain control of epithelial cells for bacteriological studies.
- To clean bleeding in gastric ulcers.
- To clean the stomach in preparation for surgery.
- Principle: It is based on Newton’s (III) third law i.e. for every action there is an equal and opposite reaction.
- Solution used:
- 1) Plain water,
2) Normal saline,
3) Sodium bicarbonate or basic acid solution in corrosive poisoning.
4) Specific antidotes if poison is identified. - a) Physical antidote: It mixes with the poison and dilutes the poison or prevents its absorption or causes membrane breakdown.
- b) Chemical antidote: It reacts with the poison and neutralizes it.
- C) Physiological antidote: This antidote has the opposite systemic effect. If the poison has a depressant action, the antidote has a stimulating effect on the body.
- Amount of fluid:
- Gastric irrigation is performed until the return flow is cleared. At least 500 ml of fluid should be introduced at a time to reach all parts of the mucous membrane of the stomach.
- Indications:
- Ingested poisons,
- In conditions where bleeding from gastric ulcers occurs,
- Corrosive poisoning,
- Kerosene and other hydrocarbons.
- General instructions:
- Explain the procedure properly to gain the confidence of the client and family.
- Remove dentures if present.
- If the operative client is unconscious, introduce a mouth gag to prevent the tube from biting.
- Lubricate the tube with a water-soluble jelly to facilitate insertion of the tube.
- Insert the tube slowly to prevent trauma.
- Be prepared to suction the airway immediately. If the client vomits during insertion, turn the patient into a three-quarter prone position immediately to prevent aspiration.
- Ensure proper placement of the tube.
- Avoid introducing air into the stomach.
- Continuously monitor the patient’s level of consciousness and vital signs during the procedure.
- The client may be interested in using a flavored mouthwash after the tube is removed.
- It is necessary to remove undigested food or to quickly remove poisonous substances. It will be necessary to introduce a gastric tube with a large lumen passing through the mouth into the stomach.
- Preparations of Articles:
- A tray containing
- Mackintosh and towel: To protect linen and garments from spoilage.
- A sterile Ewald tube 36-36 Fr: To be inserted into the mouth.
- Gasket piece: To wipe the mouth and lubricate the tube.
- Lidocaine jelly: For easy insertion.
- Adhesive strip: To secure the tube.
- Jug with solution for washing the stomach: To wash out the stomach contents.
- A funnel: To pour the solution.
- Ice water: To reduce blood flow from the ulcer for vasoconstriction.
- Sterile specimen bottle: To collect the specimen.
- Kidney tray and paper bag: To discard the waste.
- Thermometer (lotion): To check the temperature of the solution.
- Bucket: To collect the gastric drain.
- A stool: To conveniently hold the bucket.
- Procedure:
- Properly explain the procedure to the client: To gain patient confidence.
- Provide a screen to the client: To provide privacy.
- Bring all articles to the patient’s bedside: To save time.
- Place a bucket at the bedside: To receive return flow.
- Place a towel and a mackintosh on the patient’s chest: To prevent soiling of the bed and linen.
- Provide the client with a Fowler’s position with the head and neck well supported in the hypertonic position: For safe insertion.
- Wash hands properly with soap and water.
- Measure the tube as a gastric gauge.
- Lubricate the tube and place the tip of the tube far back in the mouth and ask the client to swallow. As he swallows, advance the tube gently and rapidly to the mark (18″fr).
- Aspirate stomach contents with a syringe and save them before introducing water or antidote: For lab analysis.
- Attach and hold the funnel directly below the stomach. Introduce the solution slowly, elevating the funnel so that the solution flows at the desired rate: For smooth flow of fluid into the stomach based on the principles of siphoning.
- Allow 300-350 ml of solution to enter the stomach: 300-350 ml of fluid covers all the curvatures of the stomach.
- Pinch the tube, invert the funnel over the bucket and allow the solution to return.
- The return flow is not clear Continue introduction and receiving of alternative fluids until then.
- Pinch the tube and place it in the kidney dish: To prevent air from entering the stomach and to prevent contamination.
- Record the time of lavage/irrigation, type of solution, amount used, characteristics of the returned solution i.e. color, content, consistency, order, quantity and condition of the patient: To maintain good communication within the team.
- Remove the mackintosh and towel and provide the client with a comfortable position: To prevent contamination and promote client comfort.
- Mouthwash may be used: For aesthetic sense.
- After care :
- Rinse mouth.
- Remove Macintosh and towel.
- Provide patient with comfortable position.
- Clean articles with soap and water, dry them properly and replace.
- Record time, date and amount of fluid used.
- Replace articles properly.