ENGLISH-FON-UNIT-3-MEETING THE BASIC NEEDS OF PATIENT-PART 2(HYGIENIC NEEDS)-UPLOAD
Hygienic needs:

- Hygiene:

- Hygiene is keeping the body neat and clean, which prevents the body from infection and maintaining proper hygiene leads to a feeling of well-being.
- Personal and Environmental Hygiene:

- Practice of proper personal hygiene is an essential part of our daily life. Good personal hygiene is important for both health and social reasons.
- Hygiene is generally a set of practices that are associated with the preservation of health and healthy living. The focus is mainly on personal hygiene, which includes cleanliness of hair, body, hands, fingers, feet and clothing, and menstrual hygiene.
- Improvement in personal knowledge, skills and practices can modify individual behaviour towards healthy practices, which generally focus on hygiene promotion. Safe hygiene practices involve a broad range of healthy behaviours such as washing hands before eating, washing hands properly after cleaning a child’s bottom, and properly disposing of feces. Such information on hygiene should be shared with the community so that the public can understand hygiene and its associated health risks and change their behavior to properly use better hygiene practices.
- Although hygiene and infection are vital factors of environmental health, it is also good to be aware of the link between emerging issues like global warming and medical conditions, for example, many health problems are related to our environment and lifestyle. A sedentary lifestyle makes a person prone to obesity, cardiovascular disease. Our environment is everything that surrounds us. It includes all the external influences and conditions that can affect our health, life and growth. These influences are constantly changing and their impact on our health is not easily seen.
- Meaning of personal hygiene:

- Personal hygiene involves maintaining the cleanliness of a person’s body and clothing to maintain overall health and well-being. Personal hygiene can be described as the principle of maintaining the cleanliness and grooming of the external body.
- Meaning of Environmental hygiene:
- Environmental hygiene is a group of activities aimed at protecting people from dangerous conditions arising from unsanitary conditions in shelters, air supplies, or bodily nourishment centers.
- These conditions involve unsanitary water supplies, waste disposal systems, food sources, and temporary or permanent housing structures.
Environmental Hygiene in Health Care:

- Complete environmental hygiene is important to prevent the transmission of infectious diseases in healthcare settings. Environmental hygiene involves the effective cleaning of surfaces using appropriate products, proper decontamination of medical equipment and devices used in patient-care procedures, safe and appropriate handling of sharps, blood and body fluid spills, and waste and linen.
- Environmental Surface Cleaning:
- Environmental cleaning reduces the number of infectious agents on surfaces and also the risk of cross-infection. Minimized. Cleaning is a procedure that seeks to physically remove foreign materials (for example, dust, soil, blood, secretions, excretions, and microorganisms) from a surface or object through the use of water, detergents, and mechanical action (friction).
- Cleaning Standards, Decontamination of Medical Equipment and Devices :

- Used patient care equipment should be handled in a manner that prevents exposure to skin and mucous membranes, contamination of clothing, and transfer of microorganisms to other patients and the environment. Do.
- Shared patient equipment such as infusion pumps, oximeters, BP cuffs, commodes must be cleaned and decontaminated before use on another patient. The method used should be consistent with CDC guidelines.
- Spills should be removed immediately or as soon as possible, and the area should be cleaned and disinfected, depending on the setting and volume of the spill. Small spills can be easily managed by applying sodium hypochlorite solution (1%) to the patient care area and covering the spill with a paper towel for 10 minutes. Immediately wipe the area with a paper towel and then clean the area with detergent and water. Large spills (greater than 10 cm) containing blood or body fluids should be contained and, in addition to cleaning as above, a chlorine-based disinfectant should be used.
- Personal protective equipment, including gloves at a minimum, must be worn when cleaning up spills of blood and body substances.
Safe Handling of Sharps:

It is important that all staff are aware of the inherent risks of injury associated with the use of sharp materials such as needles, scalpels and lancets.
Safe Handling of Waste :
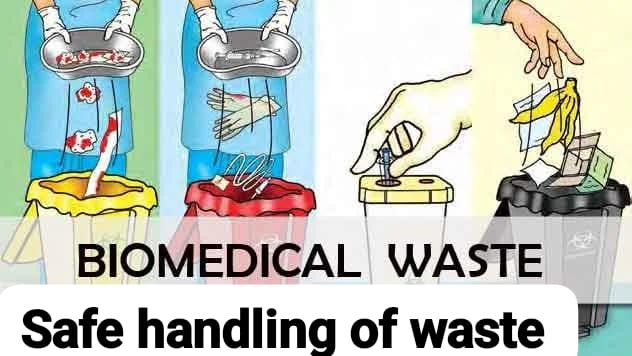
- It is important that all staff members working with waste adopt such procedures. Which reduces the risk to themselves and their environment. Dressings and bandages, materials that are only stained or have minimal contact with body substances, disposable nappies, incontinence pads or sanitary napkins are not considered medical waste and can be disposed of as general waste.
- Appropriate personal protective equipment (PPE) must be worn when handling all waste, with appropriate care taken to protect against exposure to blood and body fluids and injury.
- Provide training to health care workers regarding correct procedures for handling waste.
Safe Handling of Laundry and Linen :
All used linen should be handled properly to prevent the spread of microorganisms into the environment and to avoid contact with staff members’ clothing
The following principles should be applied to linen used by the patient:
- All used linen is considered contaminated and therefore minimal handling is recommended. is.
- Applicable PPE (Personal Protective Equipment) must be worn when handling soiled linen to prevent skin and mucous membranes from coming into contact with blood and body fluids.
- Dispose of all linen at the point of care in an appropriate linen container.
- Linen that is heavily contaminated with blood or body fluids that may leak should be disposed of in a leak-proof bag and secured before transport.
- Proper hand hygiene should be maintained after handling all used linen.
Role of nurses in maintaining personal and environmental hygiene:
- Properly follow hand washing practices.
- Treat every person as infectious and follow standard precautions.
- Wear PPE (Personal Protective Equipment Kit). They should know the steps of donning and removing PPE.
- Provide clean and neat linen for use in the unit and by the patient.
- Train all staff on bio-medical waste management.
- Provide health education to patients and the public on disease prevention and health promotion.
Hygiene :

Personal hygiene is necessary to maintain a person’s comfort and well-being. Various personal and socio-cultural factors Influences the client’s hygiene practices. The nurse determines the client’s ability to perform self-care and provides hygienic care according to the client’s needs and preferences. When providing hygiene, the nurse should maintain the client’s independence as much as possible, maintain privacy, provide respect, and promote the client’s physical comfort.
Factors influencing in Hygiene practices:
- 1) Personal preference:
- Each person has their own preferences and desires for when to bathe, shave, and do hair care, etc. Similarly, each person chooses different products according to personal preferences, needs, and financial resources. The nurse helps the client to individualize care.
- 2) Social Practices:
- Social groups influence hygiene practices and preferences. During childhood, hygiene practices are influenced by family customs, and as children enter their adolescence, hygiene practices may be influenced by the behavior of their peer group. During the adult years, work groups and friendships shape people’s expectations, and hygiene practices may change among older adults due to living conditions and available resources.
- 3) Socioeconomic status:
- The type and extent of hygiene practices are influenced by the person’s economic resources. The nurse determines which products/supplies the client can afford.
- 4) Health Belief and Motivation:
- Knowledge about the importance of hygiene for well-being influences hygiene practices. Knowledge alone is not enough. The client must be motivated to maintain self-care.
- 5) Cultural Beliefs:
- The client’s cultural beliefs and personal values influence hygiene care.
- 6) Physical condition:
- Some physical limitations or disabilities may reduce the physical energy to perform hygienic care, which may affect hygienic practices. For example, a client with traction or an intravenous line may require assistance in maintaining hygiene.
Role of nurse in providing safe, clean & hygienic environment:
- A nurse is a person who is responsible for the health of a patient in a hospital. A nurse in a hospital provides curative services to the patient and also provides preventive services to prevent the patient from developing other complications.
- The environment plays a very important role in promoting the health of the patient. Providing a promotive environment to improve the health condition of the patient is an important role of the nurse. The nurse helps the patient to create a therapeutic environment through the following measures:
- 1) Unit Cleaning:
- Unit cleaning is the main important factor. It will be done by carbolization with antiseptic solution (Sevlon or Lysol). All items that come in contact with the patient, such as lockers, cardiac tables, beds, I/V stands, etc., should be properly disinfected.
- 2) Physical Setup:
- The physical setup of the unit should be proper. There should be enough space between the beds to avoid injuries due to crowding. There should be a chair or table with each bed. Extra items should be removed from the unit.
- 3) Noise free environment:
- To reduce noise in the ward, restrict the entry of more relatives in the ward because more relatives in the hospital can increase the noise and the chances of cross infection are also high. Therefore, relatives must be allowed as per the hospital policy.
- 4) Aseptic technique:
- If an infected patient is present in the ward, then aseptic technique should be used. Then it is the responsibility of the nurse to shift the infected patient to the isolated unit and treat him by maintaining proper aseptic technique. Then after the infected patient is discharged, the ward should be cleaned by the sweeper with antiseptic solution.
- 5) Fumigation:
- It is the duty of the nurse to carry out fumigation in each unit after some specific time so that the infection can be removed from the environment. The nurse should supervise the employees of class IV during their work.
CARE OF EYES:
CARE OF EYES:
- Eye care is a procedure in which the eye is cleaned or irrigated and the prescribed ocular preparation is instilled and assessed. Hygienic care of the eye prevents infection and helps maintain the function of the eye. Hygienic care of the eye is always done as part of the general bathing procedure.
- Purpose:
- To relieve pain and discomfort.
- To prevent or treat infection.
- To maintain cleanliness of the eye.
- To maintain normal function of the eye.
- To prevent obstruction.
- To prevent and treat ice injury.
- To detect disease in early stages.
- To detect drug induced toxicity in early stages.
- To prevent corneal damage in sedated and unconscious patients.
- General Instructions:
- Unconscious patients are at risk of ice injury, so it is important to swab the ice daily with a wet cotton swab.
- Ice cleaning should always be done from the inner canthus to the outer canthus.
- Use normal saline to remove crusts.
- During bath time, clean both eyes with a separate washcloth portion.
- When performing a sterile procedure, clean both eyes with a separate cotton swab and swab each eye with a single swab and do not touch the inner side of the swab.
- Equipment:
- Machines and towels,
- Cotton balls,
- Thumb forceps,
- Bowel,
- Kidney tray,
- Clean face towels,
- Sterile 0.9% sodium chloride.
- Preliminary Assessment:
- Check:
- Check the patient’s diagnosis.
- Check the doctor’s order for any specific instructions.
- Assess the patient’s general condition.
- Assess the patient’s self-care ability.
- Assess whether all articles are available in the unit.
- Preparation of Patient and Unit:
- Explain the procedure to the patient.
- Explain how the patient can help you.
- Adjust the bed properly for the nurse to work comfortably.
- Arrange the articles conveniently on the bedside table.
- Remove all pillows, leaving one pillow under the patient’s head to keep it flat.
- Protect the pillow and bed with a mackintosh and towel under the head.
- Procedure:
- Explain the procedure to the patient.
- Tilt the patient’s head backward and support it well.
- Wash hands thoroughly using bacteriocidal soap.
- Ensure that adequate light source is available.
- Pour sterile normal saline into a bowl and wet a cotton swab.
- Always clean the infected or uninflamed eye first.
- Stand in front of the patient.
- Take two cotton balls dipped in sterile 0.9% normal saline and squeeze them well.
- Start cleaning from the inner canthus to the outer canthus of the eye in one straight stroke.
- Do not apply pressure to the eyeball.
- Use a new swab each time, and use separate swabs for both eyes. Repeat the procedure until all discharge is removed.
- Once both eyelids are completely clean and dry, provide the patient with a comfortable position.
- Properly dispose of waste as per hospital policy.
- Wash hands.
- Record the procedure in the nurse’s record sheet.
- Aftercare of the patient and articles:
- Instill any medication ordered.
- Remove towel and mackintosh from under the patient’s head.
- Adjust the position of the patient’s bed.
- Properly bedding the bed. Provide a comfortable position for the patient.
- Take all articles to the utility room. Clean them. Boil bowls. Send towels to the laundry.
- Keep articles in proper place.
- Do proper hand washing.
- Record the procedure with date and time.
- Record observations made on the nurses’ record.
CARE OF NOSE :
- The nose is an external midline projection from the face.
The purpose of the nose is to warm, clean, and humidify the air breathed by a person.
In addition, it helps the person smell and taste.
The nose is divided into two passageways by a partition called the septum. The openings to these passageways are the nostrils. Bony projections, called turbinates, protrude into each breathing passageway.
They help increase the area of the inner surface of the nose. - Purpose:
- To prevent the growth of bacteria.
- To clean the patient’s nose.
- To relieve pain and discomfort.
- To prevent or treat infection.
- To maintain the cleanliness of the nose.
- To maintain the normal function of the nose.
- To prevent obstruction.
- To prevent and treat injury to the nose.
- To detect disease in its early stages.
- To prevent and treat injury to the nose.
- To prevent damage to the nose.
- Equipment:
- Cotton,
- Saline or water,
- Towel.
- Preliminary Assessment:
- Check:
- Check the patient’s diagnosis.
- Check the doctor’s order for any specific instructions.
- Assess the patient’s general condition.
- Assess the patient’s self-care ability.
- Assess whether all articles are available in the unit.
- Preparation of Patient and Unit:
- Explain the procedure to the patient.
- Explain how the patient can help you.
- Adjust the bed properly for the nurse’s comfortable working.
- Arrange the articles conveniently on the bedside table.
- If conditions permit, remove all pillows, leaving one pillow under the patient’s head to keep it flat.
- Protect the pillow and bed with a mackintosh and towel under the head.
- Procedure:
- Explain the procedure to the patient.
- Tilt the patient’s head back and support it well.
- Wash hands thoroughly using a bacteriocidal soap.
- Ensure that adequate light source is available.
- Remove nasal secretions properly using cotton balls and water.
- Use new cotton balls while removing secretions. Repeat the procedure until the secretion is completely removed.
- Do not apply pressure to the nose.
- Use a new swab each time, repeat the procedure until all secretions are removed.
- Provide the patient with a comfortable position when the nose is completely clean and dry.
- Dispose of waste properly as per hospital policy.
- Wash hands.
- Replace equipment.
- Record procedures in nurse’s record sheet.
- Aftercare of the patient and articles:
- Remove towels and mackintosh from under the patient’s head.
- Adjust the position of the patient’s bed.
- Properly bedding the bed and provide a comfortable position for the patient.
- Take all articles to the utility room. Clean them. Boil bowls. Send towels to the laundry.
- Keep articles in proper place.
- Perform proper hand washing.
- Record procedures with date and time.
- Properly record observations made on the nurse’s record.
CARE OF EARS:

- Normal ears require minimal hygiene. Patients with excessive cerumen (ear wax) and dependent patients and those with hearing aids may require the assistance of a nurse.
- Purpose:
- To maintain the proper function of the hearing aid for those with hearing aids.
- To use the correct technique to clean the patient’s ears properly.
- To ensure that the patient follows preventive guidelines for hearing loss.
- Patients with hearing loss cannot communicate effectively.
- Equipment:
- Cotton ball,
- Warm liquid paraffin or vegetable oil,
- Patient hearing aids,
- Sponge, water, towel,
- Dump cloth
- Preparation of patient:
- Instruct the patient to properly clean the external ear, avoiding the use of sharp objects such as cotton-tipped applicators and hairpins, which can cause deep cerumen or trauma to the ear canal.
- Instruct the patient to avoid inserting pointed objects into the ear canal.
- Advise the patient to have regular hearing checks in patients over 65 years of age.
- Advise family members of patients with hearing loss to avoid shouting and speak in a low tone instead.
- Procedure:
- Confirm the patient’s identity by asking for his/her identity and date of birth.
- Explain the procedure to the patient, including risks and benefits, and obtain valid consent.
- Before performing a careful evaluation of the ear, listen to the patient, assess symptoms, and take the patient’s history.
- Assess the patient’s record to ensure that the patient has no known allergies.
- Do not use pins or slides to clean the ear. Use only clean buds to clean the ear.
- When the ear is completely clean and dry, provide the patient with a comfortable position.
- Properly dispose of waste as per hospital policy.
- Wash hands.
- Replace equipment.
- Record the procedure in the nurse’s record sheet.
- Aftercare of the patient and articles:
- Remove towels and mackintosh from under the patient’s head.
- Adjust the position of the patient’s bed.
- Properly bed the bed and provide the patient with a comfortable position.
- Take all articles to the utility room. Clean them. Boil bowls. Send towels to the laundry.
- Keep articles in proper place.
- Proper hand washing.
- Recording procedures with date and time.
- Proper recording of observations made on nurses’ records.
CARE OF FEET AND NAILS:

- Definition:
- Foot and nail care refers to the cleaning of a person’s feet and nails to prevent infection. Feet and nails require special attention to prevent infection, odor (bad smell), and tissue injury, especially in diabetic patients. Problems are usually caused by abuse or poor care of feet and nails, such as improper trimming, continuous exposure to harsh chemicals, wearing poorly fitted shoes, and any infection.
- Physical Assessment of Feet:
- Complete examination of the patient’s feet, including the skin surface, number, size, and shape of the toes.
- Proper inspection of the feet for tenderness, dryness, inflammation, and cracking.
- Carefully check the area between the toes to assess for any fungal infection.
- Proper assessment of the patient’s gait. Painful foot disorders can cause limping or an unnatural gait. Normally, the toes are straight and flat. The foot should be in straight alignment with the ankle and tibia.
- Patients with peripheral vascular disease, such as diabetes, should be assessed for adequate circulation to the peripheral area. Palpation of the dorsalis pedis and posterior tibial pulses can assess whether adequate blood flow is reaching the peripheral area. In the heel, changes in skin color, texture, and temperature indicate whether the patient needs special foot care.
- Diabetic patients should be assessed for neuropathy (degeneration of peripheral nerves). It is characterized by loss of sensation and is assessed by checking sensation to touch (pinprick and temperature).
- Normal healthy nails are transparent, smooth, and convex, with a nail bed angle of approximately 160 degrees. Nails are surrounded by a cuticle that slowly grows over the nails and should be pushed back regularly.
- The skin around the nail beds and cuticles should be smooth and free of inflammation.
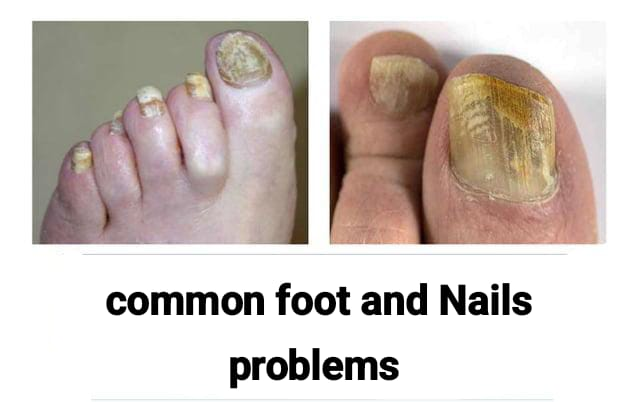
- Diseases cause changes in the shape and curvature of nails. Inflammatory lesions of the nail beds can result in thickened, horny nails that may separate from the nail bed.
Common foot and nails problem :
- Patients at risk for foot or nail problems are:
- Older adults,
- Patients with diabetes,
- Patients with heart failure and renal disease,
- Patients who have had a cerebrovascular accident (CVA) attack.
- Types of foot and nail problems are:
- 1) Callus:

- It is a thickening of the epidermis and consists of a mass of horny, keratotic cells. Calluses are usually flat, painless, and found on the surface of the foot or the palm of the hand. Usually, it is caused by local friction or pressure.
- Implication:
- Can cause discomfort when wearing tight shoes.
- Nursing Intervention:
- People should use gloves when handling tools or objects that may cause friction.
- Advise people to wear comfortable shoes.
- To soften the cell layer, soak the callus in warm water and Epsom salt. Once it has softened, a pumice stone should be used to remove the callus.
- Using creams or lotions can reduce the formation.
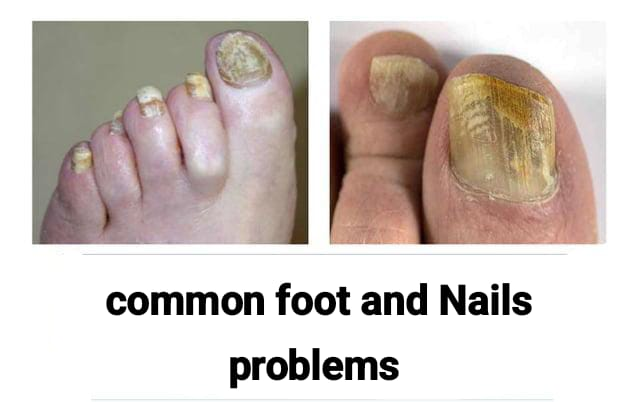
- 2) Corns:
- Corns, also called keratosis, are usually caused by friction and pressure from shoes. They are mainly found on the bony prominences on the toes. Corns are usually cone-shaped, round, and raised.
- Implication:
- The conical shape puts pressure on the underlying dermis, making it thin and tender. The pain is aggravated by wearing tight shoes. If the corn grows, the person may suffer from gait alteration due to pain.
- Nursing Intervention:
- Surgical removal is usually necessary, depending on the size of the corn and the severity of the pain.
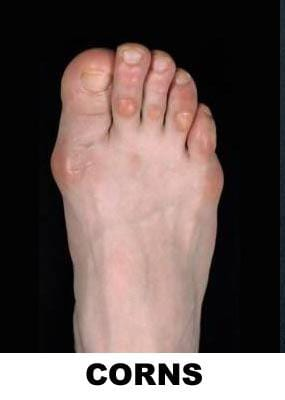
- 3) Plantar warts:
- Fungal lesions appear on the soles of the feet and are caused by the papillomavirus.
- Implication:
- Vats are usually contagious, painful, and cause difficulty walking.
- Nursing Intervention:
- Application of salicylic acid.
- Electro desiccation (electric Burning with sparks).
- Freezing with solid carbon dioxide.
- 4) Athlete’s Foot (Tinea pedis):
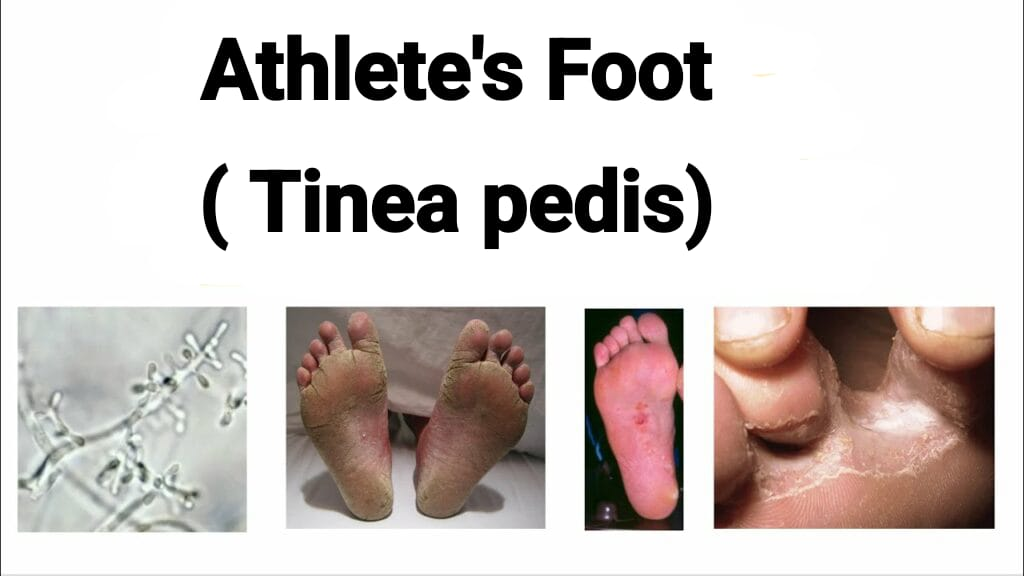
- It is a fungal infection of the foot. In this condition, the skin between the toes and on the soles of the feet becomes scaly and cracked. Small blisters containing fluid may form. This problem is usually seen in people whose feet sweat a lot when they are confined to tight-fitting shoes.
- Implications:
- Athlete’s foot can spread to other parts of the body, especially the hands. It is contagious and frequently recurs.
- Nursing Intervention:
- Keep the feet well ventilated.
- Keep the feet properly dry.
- Bathing and applying powder can cause infection. It can be prevented.
- If necessary, use antifungal foot powder.
- Wearing clean socks and stockings can reduce its incidence.
5) In-grown nails:

- Toenails or fingernails grow inward into the soft tissues around the nails. In-grown nails are usually the result of improper nail trimming.
- Implication:
- Localized pain may occur due to pressure on the toe.
- Nursing Intervention:
- Repeated hot shocks (immersing) in antiseptic solutions and removing parts of the nail that have grown into the skin may help. Proper nail trimming technique should be followed.
- 6) Paronychia:
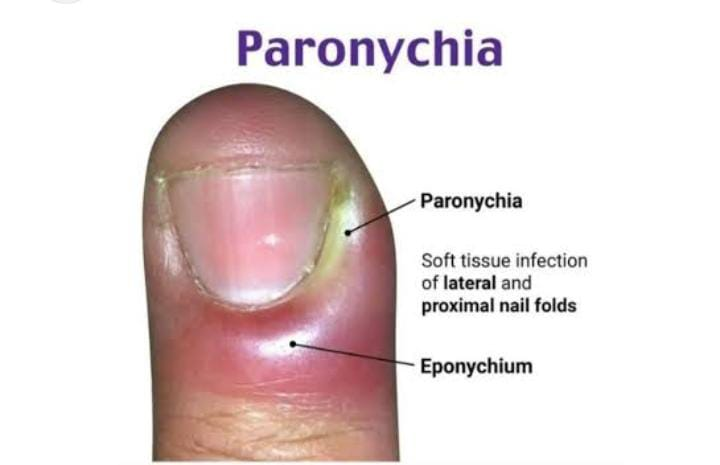
- Inflammation of the tissues around the nails can occur after hangnails (hangnails are a sign that the skin around the fingernails lacks oil) or other injuries. It occurs in people who frequently immerse their hands in water or wash their hands frequently and is also common in diabetic patients.
- Implication:
- The area may be infected.
- Nursing Intervention Intervention):
- Treatment includes hot compresses or soaks and topical use of antibiotic ointments.
- Paronychia can usually be prevented by maintaining regular hygienic care of the hands.
- 7) Foot Odours:
- Foot odors are usually caused by excessive perspiration which promotes the growth of microorganisms.
- Implications:
- Discomfort and bad smell.
- Frequent washing of feet.
- Use of foot deodorants and powders.
- Wearing clean lightweight footwear.
Procedure of foot care:
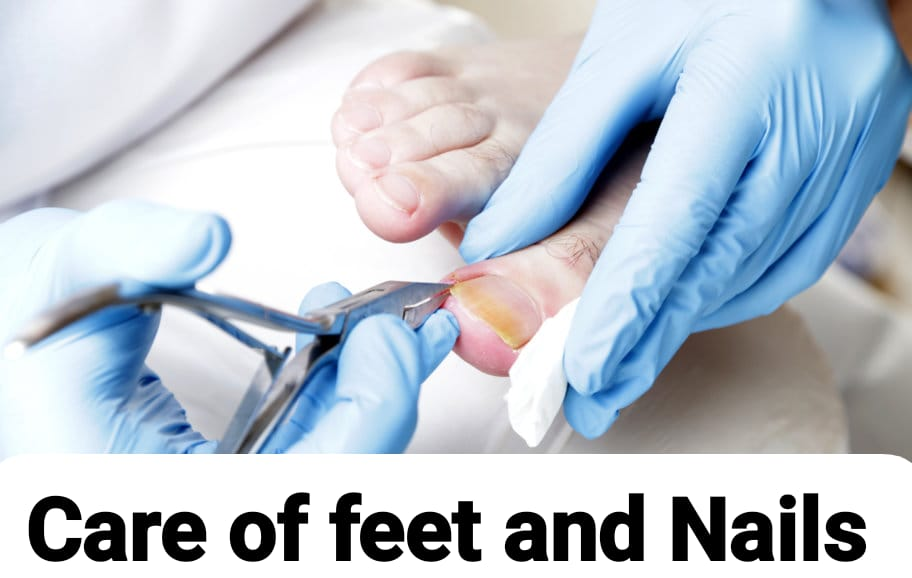
- Definition (Definition) :
- Foot and nail care refers to cleaning a person’s feet and nails to prevent infection. Feet and nails require special attention to prevent infection, odor (bad smell) and tissue injury, especially in diabetic patients. Problems are usually caused by poor care of feet and nails such as improper trimming, continuous exposure to harsh chemicals, wearing poorly fitted shoes and any infection.
- Purpose of Foot Care:
- The purpose of foot care is to promote optimal foot health, Prevent complications and promote overall well-being.
- 1) Prevent infection:
- Regular foot care helps detect signs of infection early (such as cuts, blisters, and fungal infections).
- 2) Promote circulation circulation):
- Proper foot care can improve blood flow to the foot and maintain circulation in patients with circulatory problems and diabetes.
- 3) Reduce Pain and Discomfort:
- Proper foot care can relieve pressure points, calluses, and conditions that create discomfort.
- 4) Prevent Ulcers and Injuries:
- Regular inspection and care helps in early detection of wounds and ulcerations. Which is usually important in diabetic patients.
- 5) Enhance Mobility:
- Healthy feet contribute to improving mobility which is important for independence in daily living activities.
- 6) Maintain hygiene:
- Proper foot washing and nail trimming maintain hygiene and reduce the risk of infection.
- Indications of Foot Care:
- Diabetic patients,
- Peripheral vascular disease,
- Neuropathy,
- Elderly patients,
- Patients with infections and wounds,
- Patients with calluses and corns,
- Patients with deformities,
- Swelling and heel,
- Poor foot hygiene,
- Patients with limited mobility.
- Articles:
- A tray containing:
- Sponge cloth -1: To clean the callused area of the foot.
- Macintosh with towel: To protect bed linen and garments.
- Hand towel or bath towel-1: To dry the skin.
- Vaseline or cream: To apply on the skin to prevent dryness.
- Big basin with warm water: To dip the patient’s feet.
- Nail cutter or nail file: To trim or cut the nails.
- Kidney tray and paper bag: To receive the waste.
- Set of new linen: To change if the linen gets soiled.
- Pair of gloves: To prevent cross infection while cleaning the feet.
- Procedure:
- Proper hand washing with soap and water.
- Arrange all the articles properly at the patient site.
- If possible, provide the patient with a sitting position on a chair.
- Fill a basin and bowl with warm water (water temperature: 43 – 44°C/ 100- 101°F).
- Place a towel with a Macintosh on the patient’s lap.
- Then place the bowl of water on the patient’s lap.
- Place the basin on a paper lining on the floor. Ask the patient to dip his/her fingers in the bowl of water and immerse his/her feet in the basin filled with warm water for 10-20 minutes.
- Remove the basin and bowl and allow the fingers to dry thoroughly.
- Cut the fingernails straight with a nail cutter and shape the nails with a file.
- Wear gloves and clean the callused area of the patient’s feet with a sponge cloth. Dry the feet and trim the toenails.
- Apply Vaseline/cream to the feet and hands.
- Inspect the nails and surrounding skin after soaking and trimming the nails.
- Record the procedure and observations. Report any breaks in the skin.
- After care:
- Wash all articles properly.
- Dry them properly and replace them in their place.
- Wash the hands properly.
- Provide the patient with a comfortable position.
- Special Care for Patients with Diabetes or Peripheral Vascular Disease:
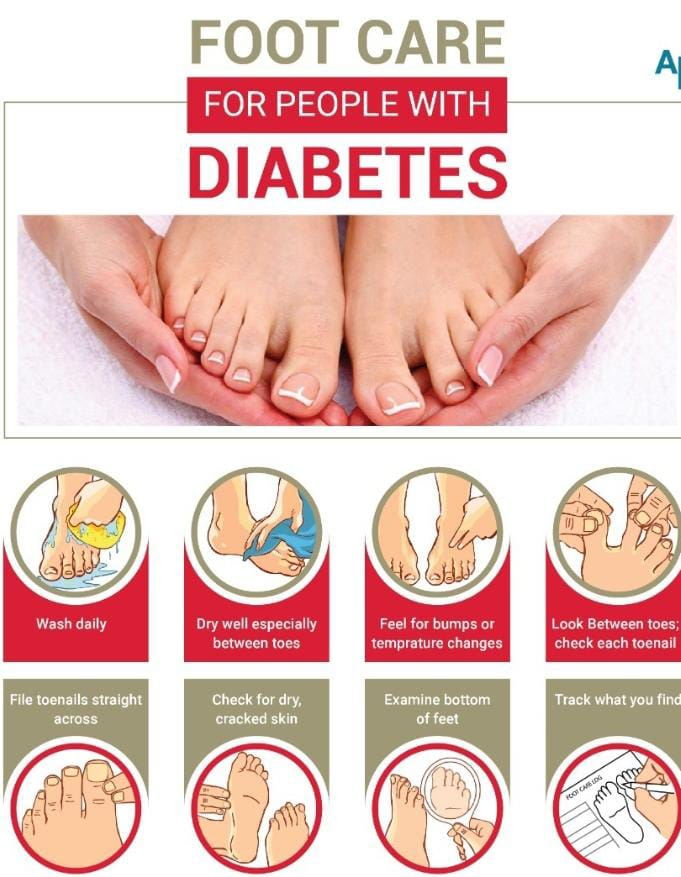
- What to do to care for the feet and nails of a diabetic patient:
- Patients with diabetes and peripheral vascular disease are at particularly high risk of foot and nail problems because they have poor peripheral blood supply to the feet. This reduces sensation in the feet. Trauma to the feet of diabetic patients can go unnoticed with breaks in the skin, and infection can easily develop due to poor circulation.
- Notice and feel your feet daily for blisters, open sores, cuts, changes in color, or ingrown toenails.
- Wash your feet daily with soap and lukewarm water. Be sure to wash between your toes.
- Keep your feet dry, especially between your toes. Use powder if necessary.
- Cut your toenails straight across. Keep your skin soft.
- Apply moisturizing lotion to the top and bottom of your feet. Do not apply between your toes.
- Change to clean shoes daily that fit well and do not have holes or tarnish.
- Examine your shoes daily to assess if there are any irritating objects in your shoes.
- Wear comfortable shoes that fit properly.
- Get your feet checked regularly by a doctor.
- What not to do to care for the feet and nails of a diabetic patient:
- Do not let feet become dry and cracked.
- Do not wear tight socks or knee-high socks.
- Use hot water to wash feet No.
- Do not use corn medicines or blades.
- Do not wear torn or tight shoes.
- Do not use a heater or hot water bottle to warm the feet. It can be harmful.
- Important Guidelines for Daily Foot Care :

- Wash and soak your feet daily using lukewarm water. Dry your feet thoroughly. Also, dry between your toes thoroughly.
- Do not cut corns or calluses or use commercial removers. Consult a physician.
- If your feet sweat a lot, apply a bland foot powder. Wear shoes with porous uppers.
- If you notice dryness on the sides of your feet or between your toes, apply lanolin, baby oil, or corn oil and rub it gently into the skin.
- File your toenails straight across and square. Do not use scissors or nail cutters.
- Do not use any preparations for the treatment of athlete’s foot or toenails without medical advice. Consult a physician or podiatrist.
- Avoid the use of elastic stockings, knee-high hosiery. Do not cross your legs as this impairs blood flow in the lower extremities.
- Inspect your feet daily, including the top and sole of your feet, the area between your heels and toes.
- Wear clean socks and stockings daily. Socks should be free of holes that can cause pressure.
- Do not walk barefoot.
- Wear properly fitting shoes. The soles of your shoes should be flexible and not slippery.
- Do daily exercises to improve blood circulation in the lower extremities. Walk slowly, elevate, rotate, flex and extend the legs at the ankles. Hang the legs over the sides of the bed for one minute and then extend both legs. Hold them parallel to the bed for one minute while in supine line down and finally rest them.
- Avoid applying hot water bottles or heating pads to the legs. Use warm shocks and extra covering.
- Wash minor cuts immediately and allow them to dry thoroughly. Only mild antiseptics should be applied to the skin. Avoid application of mercurochrome or iodine.
- Contact a physician for treatment of cuts and lacerations and get their consent.
Care of mouth/oral cavity:
- Care of mouth is the procedure of providing assistance to the weak or debilitated people by mechanically cleaning the teeth and rinsing the mouth.
- The mouth is the portal of entry for both the respiratory tract and the ingested food. The process of chewing is the first step in the digestion of food. A clean mouth gives the face more attractiveness than any other feature. The health of the lips, teeth, gums and other oral structures is of great importance to the individual. Good oral hygiene requires preventive and therapeutic measures. The mouth also becomes an ideal incubator for the growth of germs; Its proper care prevents oral diseases and damage to teeth. Brushing and flossing are essential for proper cleaning. Oral care must be provided daily.
- Indications:
- Mouth breathers,
- Patient who has oral thrush,
- Oral surgery patient (sterile special mouth care),
- Patient who is on oxygen inhalations,
- Children under 3 years of age,
- Patient who is unable to maintain adequate oral hygiene.
- Purpose of Oral Hygiene:
- To maintain a healthy state and hygiene of the mouth, teeth, gums, and lips.
- To clean food particles, plaque, and bacteria from the teeth and mouth.
- To stimulate appetite.
- To provide a sense of well-being.
- To massage the gums.
- To relieve discomfort caused by unpleasant odors and tastes.
- To prevent gum infection and inflammation.
- To alleviate discomfort caused by unpleasant odors and tastes.
- To stimulate appetite to enhance well-being and comfort.
- To prevent soreness, caries, and infection in oral tissues.
- To prevent dryness in mucous membranes.
- In a conscious patient:
- Articles:
- A clean tray containing:
- A small Macintosh with face towel: To protect bed and garments.
- Tumbler/feeding cup with plain water: To rinse and clean the mouth.
- Soft bristled toothbrush.
- Toothpaste/tooth powder/available dentifrices.
- Mouthwash solution:
- Sodium chloride,
- Thymol,
- Potassium permanganate diluted solution 1:1000,
- Listerine/Chlorhexidine.
- Cotton applicators/cotton balls.
- Emollients: Glycerin Liquid Paraffin, Vaseline, Coconut Oil.
- K – Basin, Emesis Basin – 2.
Kidney Tray.
Paper Bag.
Clean Gloves. - Preparation of Patient:
- Check the condition of the oral cavity.
- Check the patient’s ability for self-care.
- Check the patient’s general condition.
- Assess the frequency of mouth care as needed by the patient.
- Keep in mind specific precautions for patient movement and positioning.
- Procedure:
- Assess the patient’s condition, the condition of their mouth, and their level of consciousness.
- Inspect the patient’s lips, teeth, buccal mucosa, gums, palate, and tongue.
- Explain the procedure to the patient and encourage their active involvement.
- Provide a screen.
- Assess the patient’s condition, the condition of their mouth, and their level of consciousness.
- Inspect the patient’s lips, teeth, buccal mucosa, gums, palate, and tongue.
- Explain the procedure to the patient and encourage their active involvement.
- Provide a screen.
- Bring the patient to the side of the bed and close to the nurse.
- Wash hands and wear gloves.
- Provide a high Fowler or semi-Fowler position as tolerated by the client.
- Place the patient on a small Macintosh with a face towel on the chest.
- Place a kidney basin near the patient’s chin.
- Apply toothpaste to the brush.
- Holding the brush over a basin, pour a small amount of water onto the toothpaste.
- Instruct the patient to hold the toothbrush bristles at a 45-degree angle to the gum line. Brush the inside and outside surfaces of the upper and lower teeth, from the gum line to the crown of each tooth.
- Clean the biting surfaces back and forth, first the distal side and then the proximal side, and clean the upper jaw first and then the lower jaw.
- Have the patient hold the brush at the same angle (45°) to the tongue and brush lightly horizontally across the tongue, taking care not to trigger the gag reflex.
- Have the patient rinse the mouth thoroughly by taking water in their mouth and spitting into a kidney tray.
- Allow the patient to rinse their mouth with mouthwash as desired.
- Assist in wiping the mouth with a face towel.
- Apply emollient to the lips.
- Aftercare:
- Assist in providing the patient with a comfortable position.
- Discard waste.
- Clean used articles and replace equipment in the right place.
- Wash hands properly.
- Properly document the time of the procedure, the solution used, and the condition of the patient’s face.
Oral care of unconscious patient:
- Oral care of unconscious patient is the procedure of providing oral care to unconscious people by mechanically cleaning the teeth and cleaning the mouth. Good oral hygiene is essential for preventive and therapeutic measures. The mouth also becomes an ideal incubator for the growth of germs; its proper care prevents oral diseases and damage to the teeth. Brushing and flossing are essential for proper cleaning. Oral care in unconscious patients should be provided daily and at intervals of every 1-2 hours.

- Indications:
- Mouth breathers,
- Patients who are on oral hygiene,
- Oral surgery patients (sterile special mouth care),
- Patients who are on oxygen inhalations,
- Children under 3 years of age,
- Patients who are unable to maintain adequate oral hygiene.
- Purpose of Oral Hygiene:
- To maintain a healthy state of the mouth.
- To maintain a healthy state and hygiene of the mouth, teeth, gums, and lips.
- To clean food particles, plaque, and bacteria from the teeth and mouth.
- To stimulate appetite.
- To provide a sense of well-being.
- To massage the gums.
- To relieve discomfort caused by unpleasant odors and tastes.
- To prevent gum infection and inflammation.
- To alleviate discomfort caused by unpleasant odors and tastes.
- To stimulate appetite to enhance well-being and comfort.
- To prevent soreness, caries, and infection in oral tissues.
- To prevent dryness in mucous membranes.
- Solution Commonly Used:
- Potassium Permanganate (KMNO4): 1: 5000- 1: 6000.
- Hydrogen Peroxide (H2 O2 ) : 1: 8.
- Sodium Chloride (Nacl): 1 tsf to an eyeful of water.
- Lemon Juice (C6 H8 O7): 2 tablespoons to a cup of water.
- In an unconscious patient:
- Articles:
- A clean tray containing:
- A pair of gloves: To prevent cross infection.
- Small Macintosh with face towel: To protect bed and garments.
- A bowl containing solution: This acts as an oxidizing agent.
- A bowl with plain water to wet the gauze piece.
- A tray with forceps – 1 to hold the gauze piece.
- A gauze piece in a container to clean the mouth.
- Mouth gag – 1 to keep the mouth open when the patient is helpless.
- Tongue depressor – 1 to press the tongue.
- Cotton applicators/cotton balls to apply emollient.
- Emollient: Glycerin Liquid Paraffin, Vaseline, Coconut Oil to lubricate the muscle membrane.
- K – Basin,
Emesis Basin – 2.
Kidney tray.
Paper bag. - A bowl of water to receive dentures if the patient has them.
- Preparation of Patient:
- Check the condition of the oral cavity.
- Check the patient’s ability for self-care.
- Check the patient’s general condition.
- Assess the frequency of mouth care as needed by the patient.
- Keep in mind specific precautions for patient movement and positioning.
- Properly follow the doctor’s instructions.
- Properly arrange articles.
- Provide privacy to the patient.
- Assess the patient’s condition, the condition of their mouth, and their level of consciousness.
- Inspect the patient’s lips, teeth, buccal mucosa, gums, palate, and tongue.
- Provide patient screens and provide them with privacy.
- Check the condition of the oral cavity.
- Check the patient’s ability for self-care.
- Check the patient’s general condition.
- Assess the frequency of mouth care as needed by the patient.
- Keep in mind specific precautions for patient movement and positioning.
- Follow the doctor’s instructions properly.
- Arrange articles properly.
- Provide privacy to the patient.
- Assess the patient’s condition, the condition of their mouth, and their level of consciousness.
- Inspect the patient’s lips, teeth, buccal mucosa, gums, palate, and tongue.
- Provide privacy by providing the patient with a screen.
- Wash hands with soap and water and wear gloves.
- Prepare antiseptic solution for mouthwash.
- Place patient under head with small Macintosh and face towel.
- Place kidney tray near patient’s cheek.
- Do not pour water into patient’s mouth while patient is unconscious.
- Place a well-protected gag in patient’s mouth and wrap a piece of gauze around forceps, completely covering tips.
- Moisten gauze and dip it in cleaning agent, gently swab each tooth, taking care to clean sides of teeth.
- Use mouth gag to clean inside and chewing surfaces of teeth.
- Keeping the mouth gag in position, clean the tongue using arterial forceps covered with a piece of gauze.
- Apply emollient to keep the lips and tongue soft.
- Aftercare:
- Remove the kidney tray, Macintosh and towel.
- Provide the patient with a comfortable position.
- Discard the waste.
- Clean the used articles and replace the equipment in the right place.
- Tidy the unit.
- Wash hands properly with soap and water.
- Properly document the time of the procedure, the solution used and the condition of the patient’s face.
Bed bath:
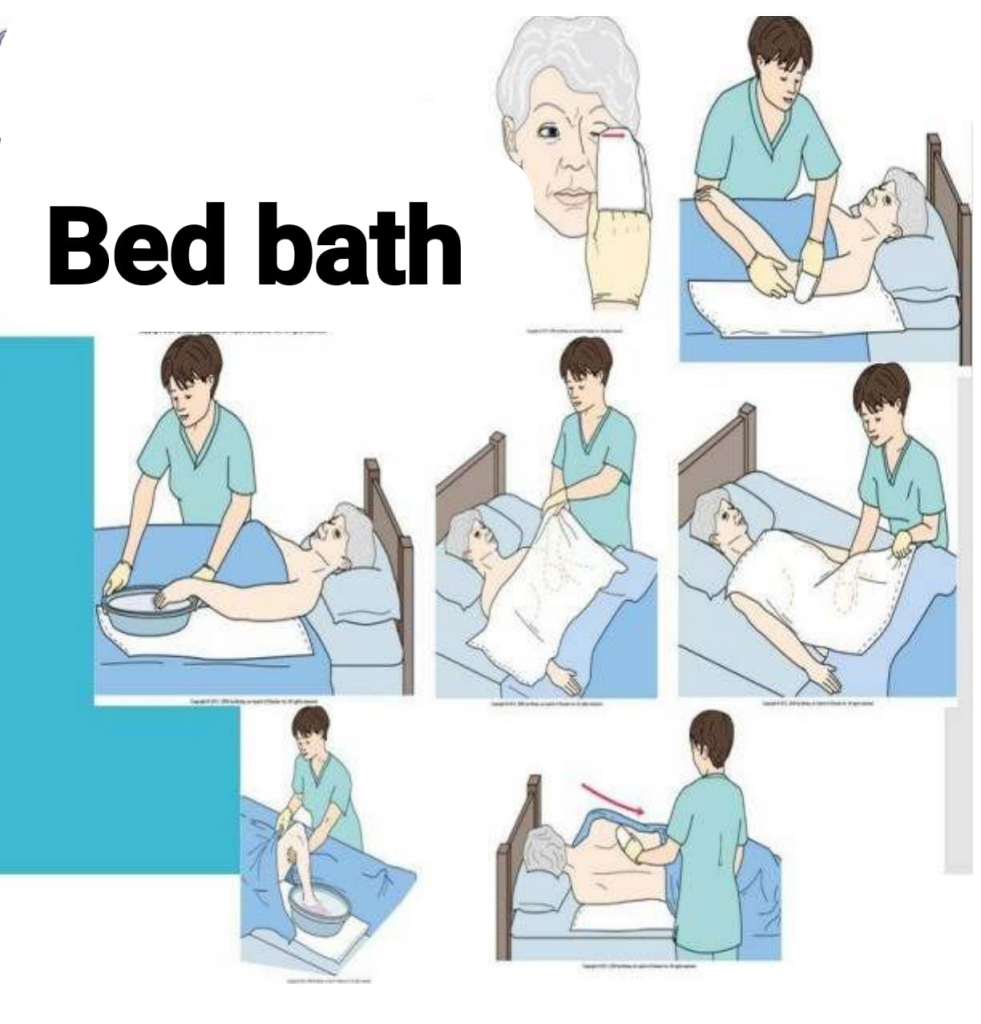
- Bed bath is a procedure of cleaning the entire body of a dependent patient or a patient who is dependent on bed and is not capable of physically or mentally performing and maintaining self-care. Bed bath is given to a patient who is confined to bed and is not capable of physically or mentally performing self-care. The skin is a sensory and excretory organ. It is very sensitive. Therefore, it is necessary to bathe the patient and free the skin from the accumulation of dirt, microorganisms and also prevent the skin from bed sores.
- Purpose:
- To clean the body.
- To stimulate circulation.
- To produce feelings of well-being.
- To prevent bed rest.
- To improve self-esteem.
- To promote relaxation and comfort.
- To provide active and passive exercise.
- To relieve fatigue and induce sleep.
- To increase elimination through skin shedding.
- To improve nurse-patient relationships.
- General instructions:
- Maintain patient privacy by using screens or curtains.
- The patient’s unit should be comfortably warm and free of drafts.
- Bed bath should not be provided immediately after meals to the patient as it affects the normal process of digestion.
- Unnecessary exercise of the patient should be avoided.
- Avoid overexposure of the patient.
- Pay special attention to pressure points and skin creases and folds.
- Use proper body mechanics during the procedure.
- Clean from the cleanest to the least clean area.
- The temperature of the water should generally be kept according to the comfort of the patient, with the water temperature for adults being 110°F to 115°F (43 – 45°C) and for children 100°F to 105°F.
- Prevent bed sheets from getting wet.
- First clean the site away from the patient’s extremities.
- Articles needed for Bed Bath:
- Trolley for placing articles.
- Draw sheet with Macintosh: To prevent soiling of the patient’s clothes and bed sheets.
- Bath Basin – 1: To take water for bed bath.
- Sponge cloth – 2: One sponge cloth to apply soap and the other to clean the skin.
- Small bowl (bowl) – 1: To keep the sponge cloth used for applying soap.
- Soap with soap dish: To clean the skin.
- Bath towel – 1: To dry the skin.
- Face towel-1: To dry the patient’s face.
- Bath blanket/sheet – 1: To cover the patient.
- Body powder or oil: To treat pressure points and avoid dryness.
- Nail cutter or scissors: To trim the nails.
- Comb and oil: To comb the hair properly.
- A kidney tray and paper bag: To collect waste.
- Jugs-2: To collect hot and cold water.
- Bucket – 1: To discard waste paper.
- Set of patient’s clothes: To change clothes.
- Screen/curtain: To provide privacy.
- A laundry bag: To discard soiled linen.
- Bath thermometer: To check the temperature of the water.
- Preparation of the patient:
- Properly prepare the patient and the environment.
- Properly assess the patient’s tolerance level, level of activity, cognitive level, and musculoskeletal function.
- Explain the procedure to the patient and their relatives so that they can be encouraged to participate.
- Adjust the bed to the proper position so that proper body mechanics can be maintained.
- Bring the patient to the edge of the bed and bring him close to the nurse.
- Provide privacy to the patient with a screen or curtain.
- If the patient’s condition is proper, remove the backrest and place a pillow under the patient’s head.
- Ensure that windows and doors are properly closed and the room is free from drafts.
- If the patient requires it, provide him with a bedpan or urinal.
- Remove the patient’s top linen and clothes.
- Provide the patient with a bath blanket/seat in place of the top linen.
- Procedure:
- Wash hands properly with soap and water.
- Wear clean gloves.
- Arrange all the articles on the patient’s side in a way that they can be easily reached.
- Then mix hot and cold water in a basin. And measure the temperature by placing the elbow in the water or by placing the dorsum surface of the hand for tolerance. (However, checking the water with a thermometer is more preferable).
- Place a bath towel on the patient’s chest under the chin.
- Wash and dry the forehead, cheeks, nose, neck, and ears. Observe for any abnormalities.
- Ask if the patient wants to use soap on the face.
- Dry the patient’s face with a face towel.
- Place the bath towel lengthwise under the most distal arm. Wrap the right arm in a sponge towel. Wash the patient’s hands with soap and water by raising the arm and supporting the patient’s wrist and elbow with long, firm strokes from distal to proximal.
- Raise and support the hand above the head while washing the axilla thoroughly.
- Rinse and dry the arm and axilla properly, applying talcum powder if necessary.
- Fold a bath towel in half and place a basin on the towel. Immerse the patient’s hand in the water. Wash and dry thoroughly, paying special attention to the skin between the fingers and nails.
- Repeat the same for the other hand.
- Cover the patient’s chest with a bath towel and fold the bath blanket up to the level of the umbilicus.
- With one hand, remove the edge of the towel from the chest. Clean the chest using long, firm strokes with a light hand.
- Take special care to wash the skin folds under the breasts in female patients. Keep the chest covered between wash and rinse periods.
- Allow to dry properly.
- Fold the bath blanket back over the pubic region, leaving the towel over the chest. Clean the abdomen, paying special attention to the umbilicus and abdominal folds.
- Keep the abdomen properly covered while washing and rinsing.
- Allow to dry properly.
- Remove the towel and replace the bath blanket, completely covering the patient.
- Change the water.
- Discard the wastewater in a bucket.
- Turn the patient into a prone or side lying position. Place a towel lengthwise on the patient’s side.
- Drape the bath blanket over the patient’s shoulders and thighs.
- Wash, rinse and dry the back from the neck to the buttocks. After the back is dry, rub the back completely with coconut oil using a quick circular motion, using a longitudinal, circular motion.
- Pay special attention to all pressure points.
- Dress the patient in upper garments and cover the patient with the bath blanket.
- Fold the bath blanket towards the midline and bring out the farthest leg.
- Flex the knee. Place the bath towel lengthwise under the leg.
- Change the water as required.
- Place the basin on a towel and place the feet in the basin.
- Use long, firm strokes to wash from the ankles to the knees and from the knees to the feet and dry thoroughly.
- Finally, clean the feet in water, paying special attention to the toes and nails.
- Exposing only the genital area, clean the perineum thoroughly and dry it. Pay special attention to the skinfolds. If the patient is able to do this, he can do it himself.
- Have the patient wear lower garments. Remove the bath blanket. Cover the patient with top linen.
- After care of the patient:
- Cut fingernails and toenails.
- Apply oil if necessary and comb hair.
- Offer hot drinks as per permission.
- Change bed linen if necessary.
- Position patient for comfort and proper alignment.
- Take this opportunity to educate patient about hygiene during bathing.
- Then, educate their relatives about the importance of maintaining personal hygiene.
- Wash hands properly.
- Record all observations made during bathing along with the procedure performed in the nurse’s record sheet.
- After care of the articles:
- Take all articles to the utility room and clean them with soap and water. Dry them and replace them in their respective places.
- Disinfect the linen and other articles if the patient is suffering from an infectious disease.
- THERAPEUTIC BATH :
- Therapeutic bath is administered to treat a disease condition and reduce symptoms.
- Chlorhexidine gluconate (CHG : Chlorhexidine gluconate) : It is used to decrease the colonization of microorganisms and prevent VAP (Ventilator Associated Pneumonia) and other Helps reduce HAIs (Hospital Acquired Infections).
- Sitz bath: Potassium permanganate is used here. It is used to decrease pain and inflammation after perineal surgery or hemorrhoids.
- Hot water bath: It is used to relieve spasms and muscular tension.
- Warm water with salt: It is used to provide a relaxing and soothing (comfortable) effect to the muscles.
- Cool water bath: To reduce fever and muscle tension.
- Oatmeal bath: Used to reduce skin irritation, soften and lubricate dry skin.
- Corn starch bath: Skin Used to reduce irritation.
Care of hair:

- A person’s appearance and feelings of well-being generally depend on the look of their hair. Normally, the hair and skin on the scalp are neither dry nor oily. Healthy hair on a healthy scalp constantly falls out and new hair grows in its place. A person’s general health affects hair growth. However, physical changes, emotional and physical stress, aging, infections, and certain diseases or drugs can affect the characteristics of the hair. Hair loss (alopecia) can be caused by improper hair care practices.
- Purpose:
- To maintain clean and healthy hair.
- To provide feelings of well-being.
- To prevent hair loss and promote hair growth.
- To prevent accumulation of dust, dandruff and oil.
- To stimulate blood circulation.
- To observe the scalp.
- To prevent and treat pediculosis (lice).
- To prevent itching and infection.
- Measures for hair care:
- Brushing and Combing:
- Hair needs to be brushed daily to keep the hair clean and to distribute the oil evenly along the hair shaft. Patients who are capable of self-care should be encouraged to maintain daily hair care. Patients who are unable to do self-care should be assisted by a nurse.
- Long hair requires some extra care. When the patient is confined to bed even for a short period. When the scalp is lacerated or cut, blood and topical medications can also cause tangling. Frequent brushing and combing helps to keep long hair neatly groomed. Braids can help to prevent frequent tangling, but braids should not be too tight.
- Articles:
- Bath towels – 2: One to protect the shoulders and garments and the other to protect the bedclothes.
- Clean comb: To comb the patient’s hair.
- Kidney tray with carbolic lotion 1:20 or Dettol 1:40: To disinfect the comb.
- Oil in a container: To remove tangles and nourish the hair.
- Paper bag: To collect lost hair.
- An apron: To protect the nurses’ uniform.
- Preparation of the patient:
- Provide proper explanation to the patient.
- If possible, make the patient sit on a chair/stool or provide the patient with a Fowler position on the bed.
- Place a towel on the patient’s shoulders.
- Place one towel on the bed linen and pillows; and place another on the patient’s shoulders to protect the bottom sheet and the patient’s clothes.
- Steps of procedure:

- To properly brush/comb, divide the hair into two sections. Then divide each section into two more sections. Dividing the hair into smaller sections allows for easier brushing.
- Brushing/combing is done from the scalp to the ends of the hair.
- If tangles are present, the nurse may use her fingers to separate small locks of hair by holding them firmly close to the scalp and combing the loose ends of the locks. This prevents painful pulling of the scalp during combing.
- Applying oil or moisturizing the hair with water, alcohol, or lotion often frees the hair for easier combing.
- If the tangles are out of control, the tangles can be cut only with the patient’s written consent.
- To comb curly hair, start at the neckline and gradually lift and fluff the hair outwards until it reaches the forehead.
- The nurse combs one side of the head at a time and then repeats on the other side.
- After combing the hair thoroughly, braid the hair two on each side of the head behind the ears to make the patient more comfortable.
- Discard loose hair in a paper bag and if there are any, wash it with lotion.
- After care of the patient and articles:
- Remove the towel and kidney tray.
- Provide the patient with a comfortable position.
- Replace articles properly.
- Wash hands properly.
- Document scalp and hair condition with date and time on the nursing record sheet.
Hair wash:
Shampooing (Head Bath):

- The patient’s daily routine usually determines the frequency of shampooing. Patients who are bedridden, have excessive sweating, or have had any treatment that causes blood or solution to come out of the hair may need to be shampooed more frequently. The ability of the patient to follow instructions on how to shampoo and maintain a particular position without feeling discomfort is critical.
- Depends on the patient’s ability to maintain.
Patients who are allowed to sit in a chair can usually be shampooed in front of a sink. If the patient is unable to sit, place a small pillow or towel under the head and neck and allow the head to hang slightly over the edge of the bed. - Purpose:
- To maintain clean and healthy hair.
- To provide feelings of well-being.
- To prevent hair loss and promote hair growth.
- To prevent accumulation of dust, dandruff and oil.
- To stimulate blood circulation.
- To observe the scalp.
- To prevent and treat pediculosis (lice).
- To prevent itching and infection.
- Articles needed for shampooing:
- A pair of gloves: To reduce infection transmission.
- Bath towels 2: One to protect the hair and the other to dry the hair.
- Washcloth or face towel: To protect the ice.
- Bath blanket 1: To cover the patient.
- Macintosh: To make a trough and another to protect the pillow and bedclothes.
- Cotton balls and gauze pieces in a bowl: To plug the ears and cover the ice.
- Oil: To massage the hair.
- Shampoo or liquid shampoo: To clean the hair.
- Hair comb: To comb the hair.
- Kidney tray and paper bag: To collect the lost hair and used cotton plucks.
- Basin-1, Mug-1: To take water.
- Bucket-1: To collect dirty water.
- Jugs-2: One for hot water and one for cold water to maintain the temperature of the water.
- Preparation of the patient:
- Explain the procedure completely to the patient.
- Collect and arrange all the articles properly at the bedside.
- Provide privacy to the patient by using a screen.
- Close the windows and turn off the fan to prevent drafts.
- Cover the patient with a bath blanket and remove the top linen.
- Place a pillow under the shoulders to keep the patient in a horizontal position and to tilt the head.
- Cover the pillow with a mackintosh and a towel.
- Make a trough with the mackintosh and place it under the patient’s head, so that the water drains into the bucket.
- Plug the ears with cotton balls and cover the ear with a sponge cloth to reduce the chances of water getting into the ear and ear canal.
- Steps of procedure:
- Wash hands properly with soap and water.
- Comb the hair properly to remove any tangles and clean the hair properly.
- Cover the patient’s ear with a sponge cloth and provide the patient with a proper position to cover the ears with cotton balls.
- Keep the water temperature (43° to 44° C) between 110° F to 115° F. (The water temperature may vary depending on the patient’s tolerance.)
- Slowly pour water from the mug over the patient’s hair until the patient’s hair is completely wet.
- Then apply a small amount of shampoo.
- Work upwards with both hands. Start at the hairline and work towards the back of the neck. Lift the head slightly with one hand to wash the back of the head.
- Massage the scalp by applying pressure with the fingertips.
- Wash the hair properly with water and ensure that the shampoo is completely removed from the hair.
- Cover the head properly with a bath towel.
- Dry the face with a piece of cloth used to protect the ice. And dry the neck and shoulders properly as well.
- Use a second towel if necessary to dry the hair and scalp properly.
- Remove the comb and place it in a basin. Discard the cotton plug used in the ear in a paper bag.
- After care:
- Spread the hair on a towel placed on a pillow and allow it to dry.
- Provide the patient with a comfortable position.
- Change the linen properly if it is wet or soiled.
- Inspect the condition of the hair properly.
- Return all articles to their proper place after washing the hair.
- Wash hands properly.
- Record the procedure in the nurse’s record and also record any findings regarding the condition of the hair or scalp properly.
- Return to the bedside. When the hair is dry, comb the hair properly. Remove the towel spread on the pillow and provide the patient with a comfortable position.
Care of Genitalia
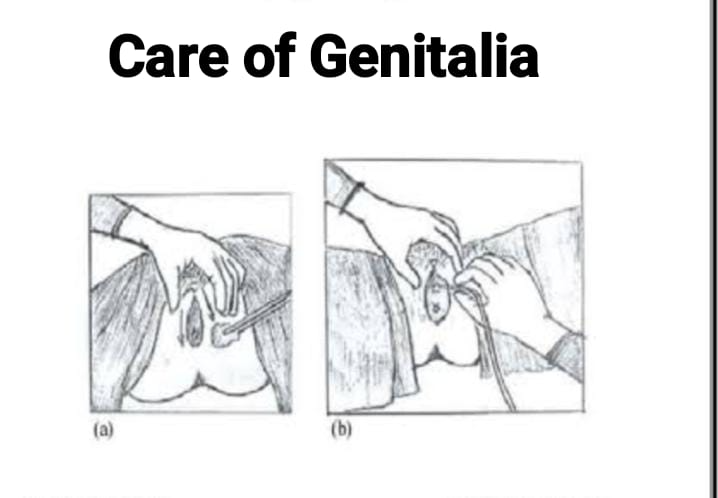
Perineal care / Meatal care:
- Introduction:
- Perineal care is also known as perineal-genital care. Perineal hygiene involves cleaning the external genitalia and perineum to prevent the growth of bacteria that increase rapidly in a warm, dark, and moist environment. Perineal care involves washing with soap and water, water only, or a commercially prepared perineal wash. It is performed as part of the patient’s bath or as a separate procedure. The perineal area is a conducive area for the growth of pathogenic organisms because it is a warm, moist area and is not a well-ventilated area. This area contains many orifices such as the urinary meatus, vaginal orifice and anus, through which pathogenic organisms can easily enter the body.
- Procedure of perineal care:
- Perineal care is the care of the perineum that involves cleaning the external genitalia and surrounding area using surgical aseptic technique or medical aseptic technique as needed. Maintaining proper cleanliness is essential to prevent bed sores and promote comfort.
- Principle:
- The most pertinent principle for perineal care is to clean the perineum from the cleanest to the least clean area.
- Purpose of perineal care:
- To promote cleanliness.
- To prevent infection.
- To remove irritating secretions.
- To promote healing.
- To provide comfort.
- Patients who require special attention to the perineal area:
- Patients who are unable to self-care.
- Patients who have an infection of the genito-urinary tract.
- Patients who have urinary and fecal incontinence.
- Patients who have excessive amounts of vaginal drainage and bleeding.
- Patients who have an indwelling catheter.
- Postpartum patients.
- Patients who have undergone surgery on the genito-urinary system.
- Patients who have had an injury, ulcer, or surgery in the perineal area.
- Preliminary assessment:
- Assess the condition of the patient’s perineal skin, itching, irritation, ulceration, and secretions.
- Assess perineal care needs and frequency.
- Perineal care should be performed using ‘aseptic’ or ‘clean’ techniques (remember that perineal care should be performed using aseptic technique when there is a wound).
- Assess for any lesions, orders, scars, inflammation, excoriations, and enlarged lymph nodes.
- Check physician orders for any specific instructions.
- Assess the patient’s self-care ability.
- Assess the patient’s mental ability to follow instructions.
- Check if the articles are available in the patient’s unit.
- Articles:
- Macintosh with towel: To protect the bed.
- Jug with warm antiseptic solution: To clean the perineum.
- A sterile tray containing:
A bowl of sterile wet cotton balls: To clean the perineum. - Sterile gauze piece: To dry the perineum.
- Artery forceps A pair of sterile gloves: To hold swabs for cleaning.
- Kidney tray/paper bag: To receive waste.
- A drape sheet: To drape the patient.
- Sterile pads and dressings: To keep the patient clean.
- Clean linen: To keep the patient clean.
- Soap and soap dish, towels: To wash hands.
- A bedpan: In case the patient needs to pass urine and stool.
- Preparation of the patient and the unit:
- Explain the procedure completely to the patient.
- Provide privacy to the patient with a screen and drape.
- Drape the patient for vaginal examination.
- Fold the top linen to the foot end of the bed.
- Remove all articles that may interfere with the procedure, such as air cushions or knee pillows.
- Provide an extra pillow to raise the patient’s head.
- Prepare the unit to avoid drafts.
- Adjust the bed to working height.
- When placing the bedpan, turn the draw sheet to the opposite side to avoid soiling or place a Macintosh under the buttocks on top of the draw sheet.
- Offer the bedpan, placing a clean bedpan on the bed on your working side. Ask the patient to flex their knees and lift their buttocks by pressing their feet against the mattress. Place the bedpan in position while sliding the left arm below the waist and gently lower the patient onto the bedpan, adjusting it so that it is comfortable for the patient.
- Untie the pads. Make observations for the color, odor, and amount of discharge. Discard the pad in a paper bag.
- Leave the patient alone for a while so that he can pass urine or stool if necessary (never leave the patient alone if he is very ill or weak and likely to faint).
- Obtain a toilet wash-down tray and arrange the article conveniently on the bedside table.
- Steps of procedure:
- Properly wash hands.
- Pour water on the perineum.
- Clean the perineum using a wet swab.
- Hold the swab with forceps and clean from top to bottom towards the anal canal.
- Use one swab for one swabbing.
- Clean the perineum from the midline outwards in the following order.
•Vulva,
•On both sides of labia majora,
•Inside labia majora on both sides.
•Outside labia majora on both sides. - Clean perineal region and anus thoroughly.
- Remove bedpan by supporting hip as before. Turn patient on one side and dry buttocks with dry rag.
- After care:
- Apply medicine and pad if necessary.
- Remove extra Macintosh if used.
- Change linen and straighten bed clothes if necessary. Arrange bed linen.
- Provide patient with comfortable position.
- Take bedpan to sanitary annex. Remove the cotton swab and empty the contents into the toilet.
- Properly clean all articles.
- Boil forceps.
- Properly replace articles.
- Remove screen and properly tidy unit.
- Properly wash hands with soap and water.
- Record procedure with date and time and observations.
Care of pressure points (back care)(Back care):

- Definition:
- Back care is the procedure of cleaning and massaging the back for therapeutic and comfort measures of an individual.
- Purpose:
- To prevent bedsores on the back For.
- To stimulate circulation.
- To detect early signs of bedsores.
- To relieve pressure from pressure points and change the patient’s position.
- To keep the skin clean and dry.
- To refresh the patient and relieve fatigue.
- To enhance sleep.
- To improve the sense of well-being.
- Steps for back massage:
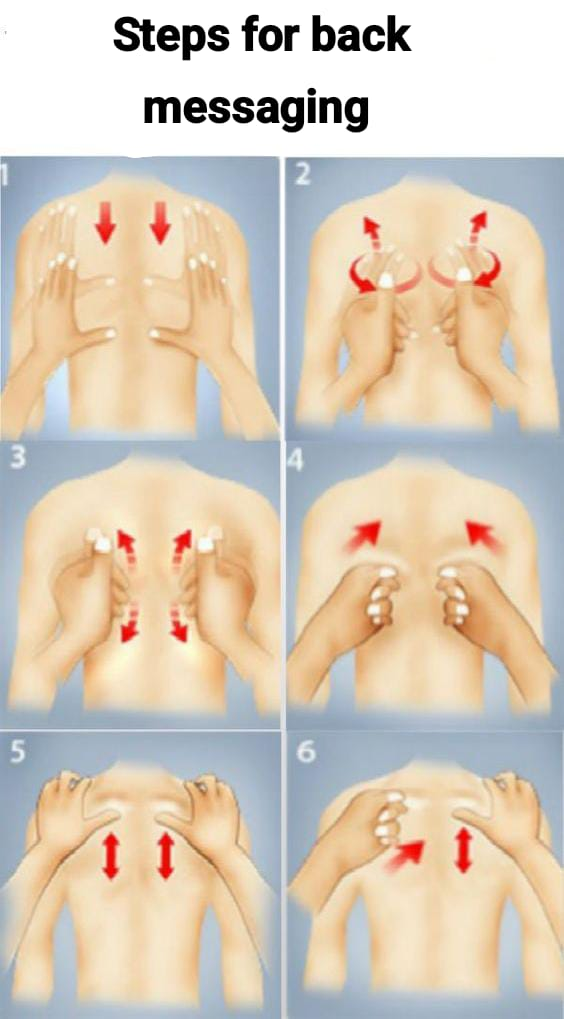
- 1. Effleurage
- 2.Petrissage
- 3.Hand over hand
- 4. Friction (Friction)
- 5.Brush stroke
- 6.Kneeding
- 7.Tapping
- 1.Effleurage:
- It is a smooth long-long stroke that moves the hand up and down the back. The hand is moved slightly down. The hand is moved firmly up the back. If slow light pressure is used, this rub has a relieving and sedative effect.
- 2. Petrissage:
- It involves massaging the back with both hands with short, quick strokes.
- 3. Hand over hand:
- In this, massage the back with short quick strokes with the alternate hand.
- 4. Friction:
- Massage the back with your thumb in a circular motion and an upward manner. Starting from the sacrum and moving outwards each time until the entire back is covered up to the shoulders.
- 5. Brush stroke:
- Lightly stroke the back with your finger tips to complete the massage.
- 6. Knead:
- To make light strokes on the back like kneading with both hands.
- 7. Tapping:
- To lightly tap the back with both hands.
- General instructions:
- Provide proper explanation to patients who are susceptible to pressure sores.
- Provide proper explanation to patients who are completely bedridden, such as paralyzed, unconscious, and bedridden, and their relatives.
- Back care should be followed by position changes.
- Early detection of pressure sores can be done by observing the skin of the patient’s back while providing back care to the patient.
- Comfort devices should be used after performing back care procedures.
- Articles:
- Screen: To provide privacy.
- Macintosh with cover: To protect bed linen.
- Fresh bed linen and patient’s clothes: To be changed if necessary.
- Tray Containing:
- Small basin: To receive water.
- Sponge cloth: To wash the back with soap and water.
- Soap with soap dish: To clean the skin.
- Spirit/Oil: To apply on the skin after drying the skin.
- Powder: To prevent friction.
- Towel: To dry the skin.
- Kidney dish: To receive waste.
- Preparation of the patient:
- Assess whether the patient needs back care.
- Explain the procedure properly to the patient.
- Assist the patient to move to the side of the bed and properly adjust the bed to a comfortable working height.
- Place the screen to provide privacy to the patient.
- Steps of procedure:
- Provide the client with a lateral or prone position.
- Expose the patient’s back, shoulders, upper arms and buttocks and properly cover the remaining body parts with a bath sheet.
- Properly wash hands with warm water.
- Wash the back thoroughly from the cervical spine to the coccyx with a mild soap, rinse thoroughly with soap and dry.
- Take spirit/oil on palm and massage it all over the back in circular motions until the spirit/oil evaporates and the skin is dry.
- Massaging the back:
- Take a small amount of oil/lotion on the palms of your hands and hold it for a minute.
- Using your palms, start at the sacral area using circular strokes.
- Move your hands to the center of the back and then up both scapulae.
- Massage the scapulae in circular motions.
- Move your hands down the sides of the back.
- Massage the area above the right and left iliac crests.
- Massage the back in a systematic pattern using a variety of strokes and appropriate pressure.
- Start with effluvium (light gliding strokes).
- Then gently massage the patient’s skin by alternating grasping and compression motions (patricesage). Complete the massage with extra long, stroking movements using the finger tips, which eventually become lighter in pressure again.
- Apply talcum powder to the back.
- Then remove the mackintosh and towel.
- Make the patient wear proper clothes.
- Turn the patient onto his back and provide a comfortable position.
- After care:
- Remove the screen.
- Wash the articles and place them in the utility room and replace them in their right place.
- Wash your hands properly.
- Properly record nursing interventions and client responses.
- Properly record any unusual findings.
DECUBITUS ULCERS OR BED SORES:
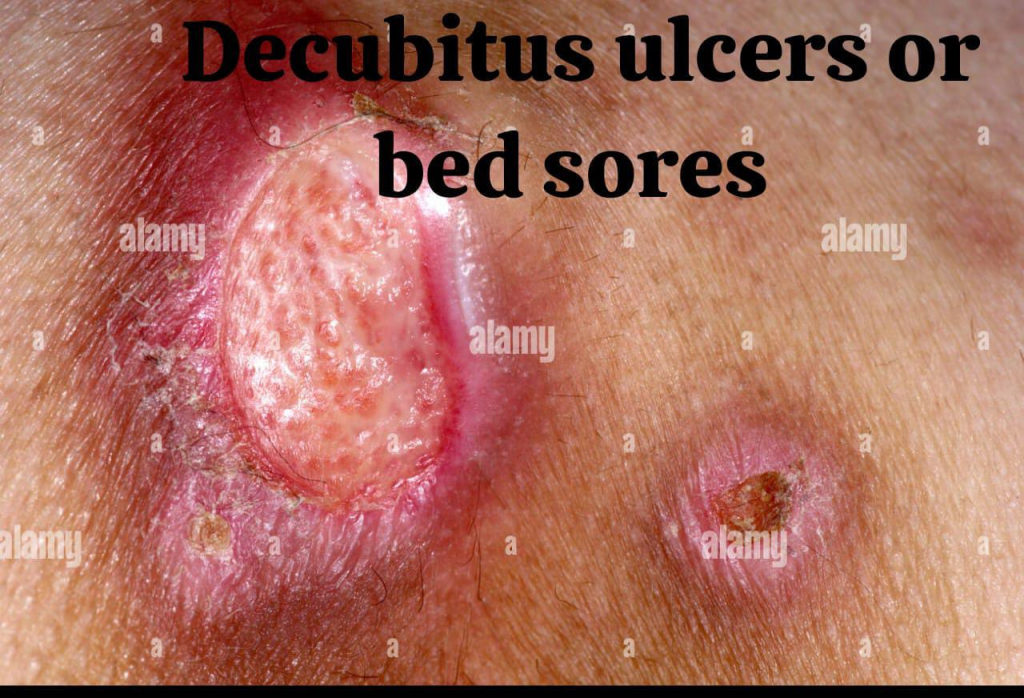
- Decubitus ulcers, also known as pressure sores or decubitus ulcers, are ulcerated or sore areas of tissue that develop due to prolonged pressure from lying down on a mattress or sitting in a chair, resulting in slow circulation and ultimately tissue death.
- Common sites:
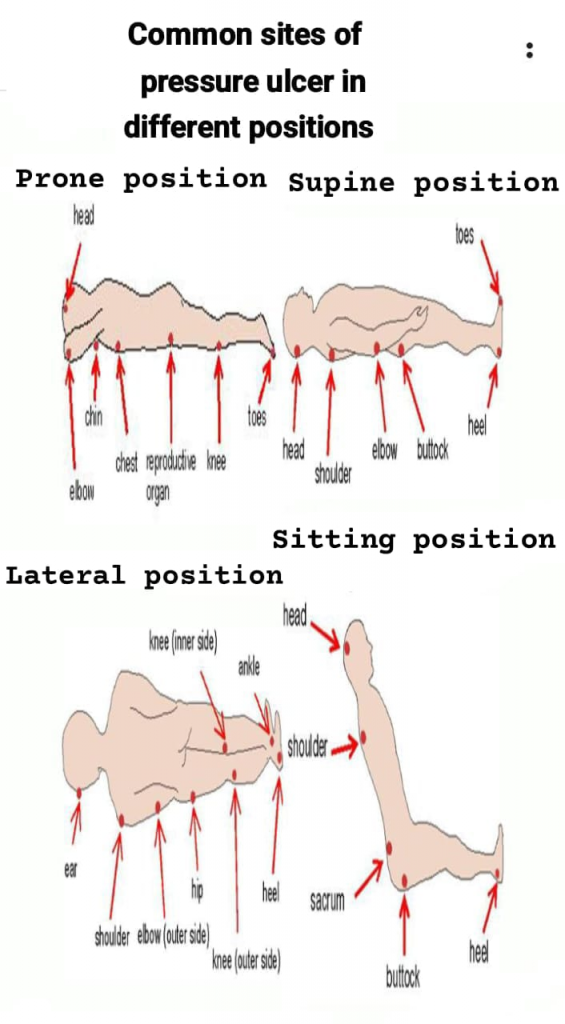
- Bed sores are usually found mainly in areas of bony prominences where there is not an adequate amount of blood supply and which usually depends on the position of the patient.
- In supine position:
- Head, back, part of the body, scapula, sacral area, elbow and heel are bony prominences.
- In side lying position:
- Ear, acromion process of shoulder, greater trochanter of hip, medial and lateral condyles and malleolus of ankle joint etc.
- In sitting position:
- Head, shoulder, sacrum, buttocks, heel
- In prone position:
- Ears, acromion process, breast, genital area, knee and toe.
- Causes of pressure sore:
- Pressure This is usually the primary cause of pressure sores. In a sick person, the area of tissue resting against the mattress is a sensitive area. Pressure in this area leads to circulatory failure in the weight-bearing area and reduced blood supply, resulting in tissue damage.
- Pressure increases in the affected areas in the following conditions.
- When there are any lumps or creases present in the bed.
- Due to incorrect positioning of the body.
- Due to not changing positions frequently.
- 1) Friction:
- Rough and hard surfaces can damage tissues. Due to contact with rough surfaces of the bed, wrinkles in the bedclothes, hard surfaces or presence of foreign bodies, friction can occur on the skin and ultimately cause tissue damage.
- 2) Moisture:
- Maceration of the skin can occur due to prolonged contact with moisture.
- 3) Presence of pathogenic organisms:
- When personal hygiene is not maintained properly, infection can settle down in the skin.
- Predisposing causes:
- Bed sores Stages,
- Impaired circulation,
- In the heel,
- Obesity.
- Prevention of pressure sores:
- To identify patients at risk of pressure sores.
- Perform daily skin examination of prone patients.
- Keep patient clean and dry.
- Change patient’s position every 2 hours.
- Use bed cradle to take off the weight of linen.
- Lubricate patient’s skin to prevent cracking.
- Protect patient’s skin from damage caused by body substances like urine, feces, sweat etc.
- Maintain proper fluid balance of patient and provide proper good diet.
- Massage pressure points properly to stimulate circulation.
- If the patient is provided with a bedpan, lift the patient properly when needed.
- Make the bed properly without wrinkles.
- Use an air mattress or water mattress to decrease pressure.
- Maintain the patient’s personal hygiene properly.
- Prevent friction on the patient’s body caused by any objects on the bed.
- Use comfort devices to take off weight on pressure points.
- Encourage the patient to move in bed.
- Signs and symptoms of pressure sore:
- Early symptoms of pressure sore include redness, tenderness, and discomfort. The area is cold to the touch and insensitive with local edema.
- Later, the area becomes blue or purple mottled. Due to continuous pressure, gangrene develops and the affected area closes.
- Stages of pressure ulcer:
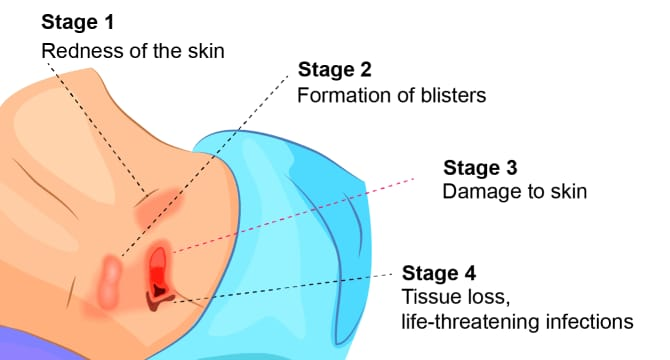
- Stage I : Redness of the skin that is neither relieved by massage nor by pressure caused by it.
- Stage: II : It involves superficial tissue damage and skin breakdown.
- Stage: III : Involving the skin Ulceration, which may or may not involve subcutaneous tissues, is the stage that produces serosanguinous drainage.
- Stage: IV: In this stage, ulceration is seen in deep structures along with invasion of deep tissues or structures such as fascia, connective tissue, muscles, and bone.
- Treatment:
- Once a decubitus ulcer develops, it is difficult to treat because it is susceptible to infection. Therefore, proper precautions should be taken to protect the wound from contamination.
- The following measures are taken by nurses:

- 1) If the patient shows any early signs and symptoms, report it to the physician immediately to prevent further damage.
- 2) Keep changing the patient’s position every 2 hours.
- 3) Use strict aseptic technique to prevent infection.
- 4) Use normal saline to clean the area.
- 5) Apply all possible measures to heal the wound.
- (i) Heat is applied for 10 minutes using a 150 volt bulb, which is kept 45 to 60 cm away from the wound.
- (ii) A few drops of insulin are applied to the wound and then it is cleaned and allowed to dry.
- (iii) Fill the ulcer cavity with granulated sugar.
- 6) Apply zinc oxide, which is a waterproof ointment, on the wound surface to prevent infection.
- 7) If slough is present, clean the area with hydrogen peroxide twice a day.
- 8) If the wound is infected, the physician must prescribe antibiotics to treat the infection.
- 8) It is necessary to provide the patient with comfort devices.
- 9) Mattresses (air, water) should be arranged on the bed.