ENGLISH-FON-GNM-UNI-2-RECORDING AND REPORTING (UPLOAD-UNIT-2-PART-4)-UPLOAD

Record

- A record is a written and legal documentation that provides information about the care provided by a nurse to a patient.
- A record is a clinical, scientific, administrative, and legal document that provides information about the care provided by a nurse to an individual, family, or community.
- A record is found in written form while a report is found in both oral and written forms.
Write purpose of record
- To communicate clearly and effectively with other healthcare professionals
- To record diagnoses
- To plan any type of care or program
- For legal documentation or legal accountability
- For historical records
- For decision analysis
- To help in research and to improve nursing care
Write down different methods of record charting

Narrative charting
- This is a traditional method of recording nursing care. In which the patient’s condition, symptoms, and treatment are documented in chronological order, i.e., in paragraph form. This method is not used today because it is time-consuming and difficult to retrieve.
Problem oriented charting
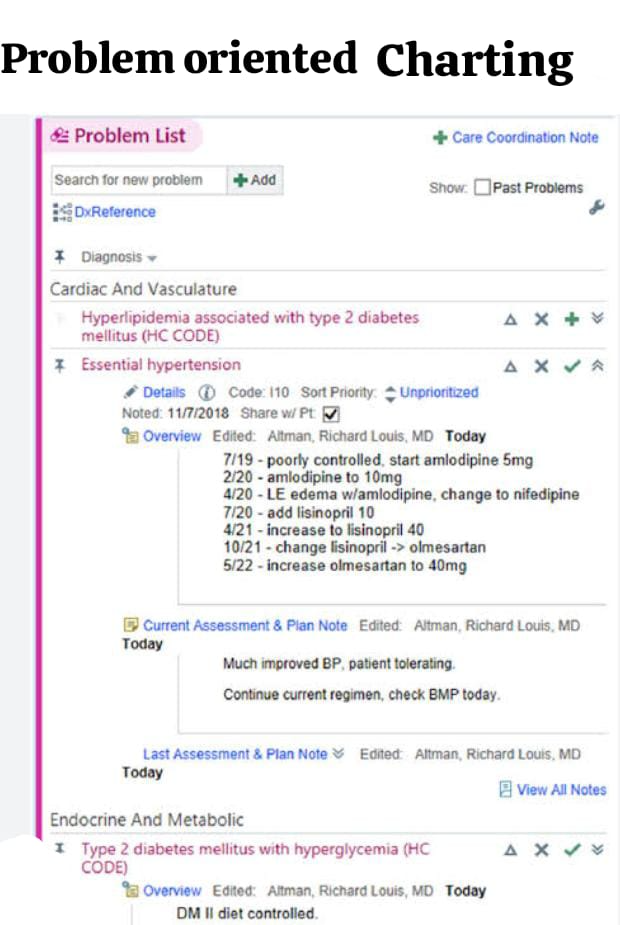
- Problem-oriented charting is done keeping in mind the patient’s problem, in which each member of the health team makes a list of the patient’s problems.
Source oriented charting
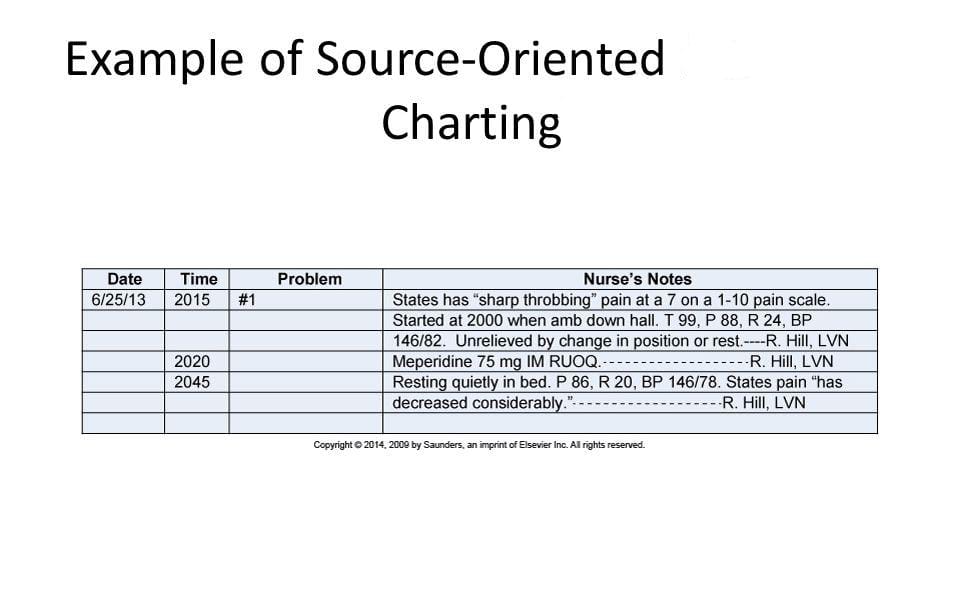
- In source-oriented charting, documented information is organized based on the source. In source-oriented charting, each member of the health care team (such as physicians, nurses, physical therapists) records separately. This provides fragmented documentation.
Focus charting (Data – Action – Response)
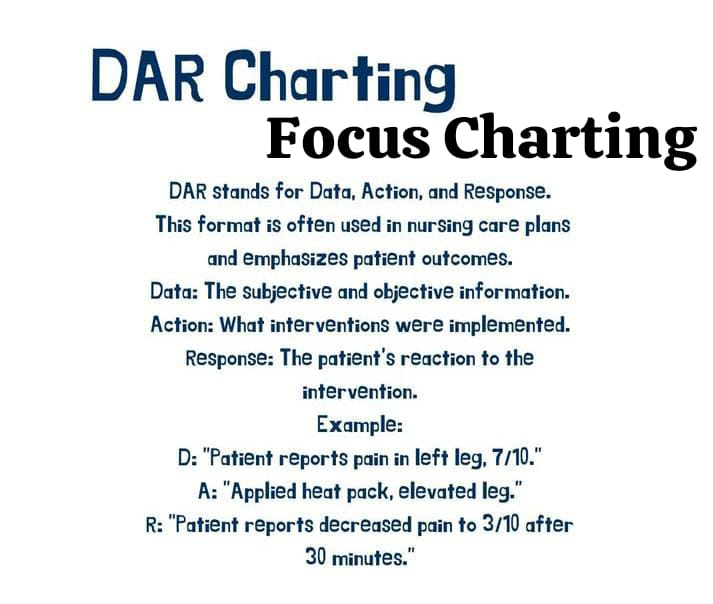
- Fox charting is a method of identifying and organizing narrative charting. It involves data, action, and response. Fox charting involves collecting data, taking a specific action on it, and observing the patient’s response to that action. Fox charting also includes concerns related to the client’s problem as well as the results of diagnostic tests.
PIE charting
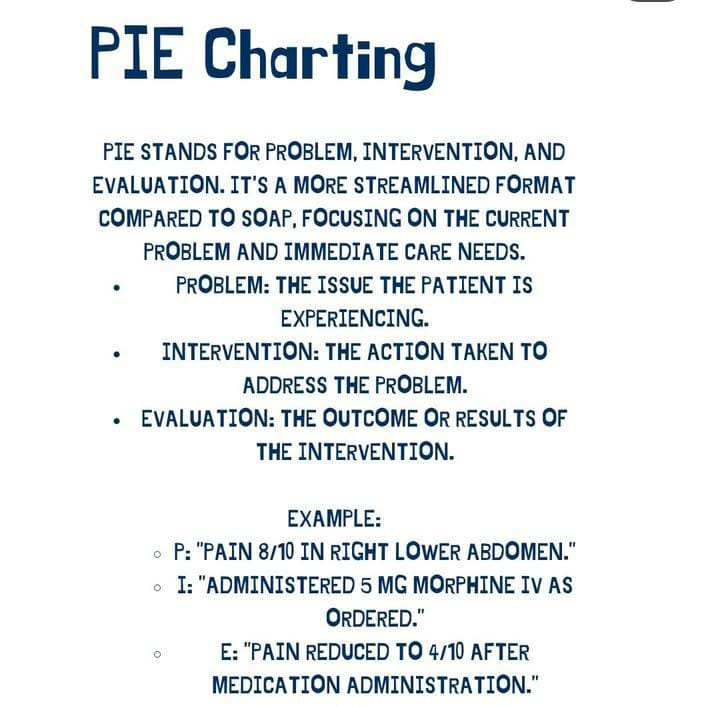
- PIE charting is a nursing origination that includes problem-intervention-evaluation. In this charting, a specific intervention is taken on the problem by identifying it and then its evaluation is done. In this charting, the flow sheet and nurse progress notes are assessed with the nursing plan. After assessment, the client’s problem is considered and related specific intervention is done and its evaluation is done.
SOAP charting
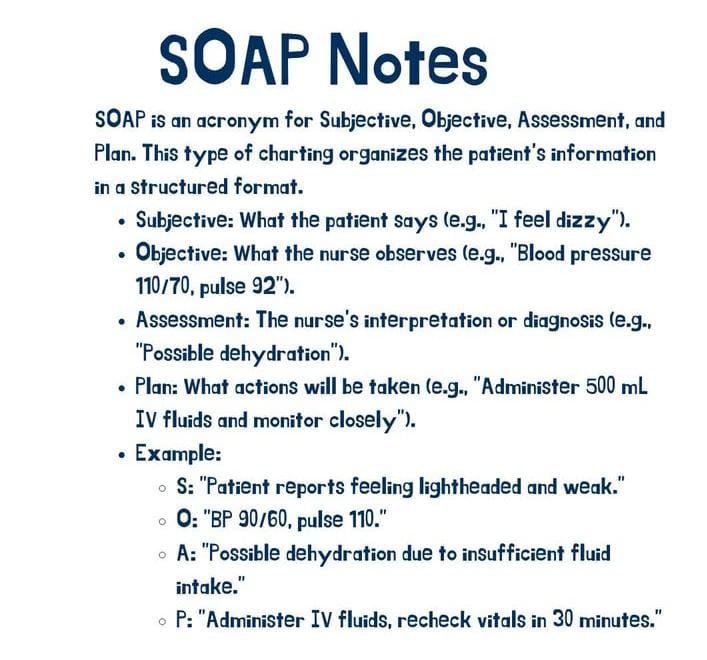
- SOAP charting is a format developed according to the medical model, which includes Subjective, Objective, Assessment, and Plan.
Write down types of records
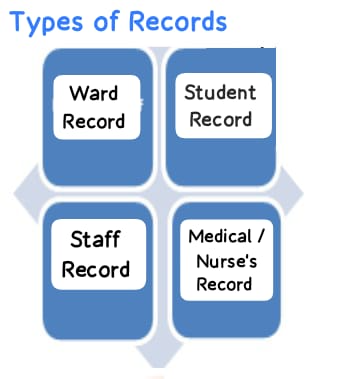
Ward record
- Patient Clinical Record
- Admission record
- Discharge record
- Death register
- Call book
- Indent book
- Instruction book
- Complaint book
- Attendance record
- Round register
- Treatment record
- Drug Maintenance Register
- Stock and Issue Register
- Visitor record
- Movement register
- Over book
Student record
- Application Form
- Admission register Register
- Class Attendance Record
- Leave Register
- Clinical and Field Experience Register
- Mark List Register
- Internal Assessment Register
- Extracurricular Activities Register
- Practical Record Register
- Cumulative Health Record
Staff record
- Application record
- Health record
- Leave record
- Progress report
- Record of Educational Qualifications, Previous Experience
Medical / nurse’s record
- Nurses Report Book
- Nurses’ Progress Note
- Nurses Assessment Sheet
- Standardized Care Plan
- Shift Record
- Treatment Chart
Write Principles of Record

- Accurate:
Accuracy means precise. All records should be error-free. Use medical language and avoid spelling mistakes while writing records. Write full forms instead of short forms, such as Tetralogy of Fallot or Tracheoesophageal fistula instead of TOF.
- Completeness:
Complete sentences. Include all the necessary information for the record. Do not leave spaces between lines. Document any care omitted or refused by the patient.
- Organized:
While recording, write information like hospital name, patient name, registration number, gender, diagnosis etc. in chronological order.
- Compliance:
Compliance means to follow. To follow the rules, regulations and policies of the organization while recording.
- Confidentiality:
Confidentiality means to keep the patient’s personal information and data secret. Not to share it with anyone else.
- Accessible:
Keep the record easily accessible. So that it can be easily retrieved when needed.
- Security:
Store the record in a good place and keep it secure in a way that no unauthorized person can access it and cannot damage it.
- Relevance:
The record should be relevant to its purpose.
Report

- A report is a type of verbal or written communication.
- A report is a summary service of a nurse or any agency.
- A report is written daily, weekly, monthly or even yearly.
- A report should be accurate, appropriate, truthful, clear, brief, complete, legible and confidential.
- A report includes face to face meetings, telephone conversations, messengers, written messages, audiotape messages and computer messages.
Write down objective of reporting

- Provides an effective and essential tool for communication between the health team and its members.
- Saves time.
- Provides information on whether a particular procedure has been performed or not.
- Helps provide better care to the patient.
- Prevents duplication of work.
Write down importance of record and report
This is a type of legal documentation that makes it very useful in medicolegal cases.
- Accurate / legal documentation
Records and reports are reliable and accurate documentation for the conversation. Apart from this, records are very useful as legal documentation in medicolegal cases.
- Accountability
Records and reports promote accountability and transparency in the decision-making process.
- Communication
Records and reports provide facilities for clear and effective communication.
- Evaluation
Progress, outcomes, and performance can be evaluated with the help of records and reports.
- Research
Records are important for research.
- Vital statistics
Records are very important for vital statistics. With the help of records, current vital statistics can be known. Which is useful for comparing with other data.