ENGLISH-FUNDA UNIT-2 (part-1) (UPLOAD)
AS PER INC SYLLABUS (FULL COURSE)
UNIT-2-Nursing care of the patient
a) Patient Environment in the hospital:
Patients unit
b) Therapeutic environment
- Physical factors – lighting temperature,
ventilation, humidity, noise, pestilence. - Safety needs, prevention of
environmental hazard - Psychosocial and aesthetic factors.
c) Patient’s Adjustment to the Hospital.
- Understanding the patient as a
person, socio-economic, and cultural
background, health status etc. - Effect of hospitalization on patient and
family. - Admission, transfer, discharge
procedures
d) Basic Nursing Skills-
- Communication
- Nursing interview
- Recording and reporting
e) Nursing Process
- Meaning and importance
- Assessment, Nursing diagnosis
Planning, Implementation and
Evaluation - Nursing care plan
nursing care of the patient

- Key terms :-
- (1) LAMA:- Leave against medical advice (Leave without medical advice).
- (2) Fire drills:- An emergency procedure used in the event of a fire is called a fire drill.
- (3) Confronting:- To confront a person with a difficult situation means to meet or deal with it.
- (4) Insight:- Insight is the capacity of someone to understand a person or something deeply and accurately.
- (5) Palliative care:- Palliative care is provided to terminally ill patients and their families by organized health services.
- (6)ECG:- Electrocardiogram
- (7) Admission:- Entry of the patient into the hospital
- (8) Unit:- The space in which the client stays in the hospital is called a unit.
- (9) Discharge:- Exit of the patient from the hospital.
- a) Patient Environment in the hospital Patients unit:

- ∆ Patient environment in the hospital Patient’s near-by space:
- Importance:-
- If the environment means or the surrounding of the patient is safe and comfortable, then his chances of improving his health can increase.
- If the surrounding of the patient is safe and comfortable, then the chances of depression can also decrease.
- Special considerations come within a safe and secure healing environment that promotes mobility means or movement and socialization that creates a home-like environment. An environment that relaxes the mind body and soul also provides the patient with a very quick recovery.
- Patient Environment in Hospital – Patient Unit:

- Definition:
- A Patient Unit is an area in a hospital where arrangements are made for the comfortable and safe care of a patient. It includes the patient’s bed, furniture, medical equipment and all necessary facilities, which make treatment and rehabilitation accessible.
- Components of Patient Unit:
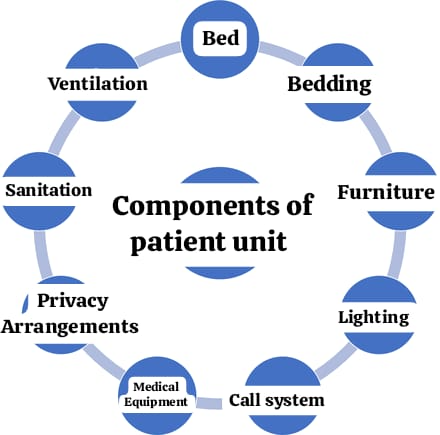
- 1.Bed and Bedding:
- Comfortable and adjustable hospital bed for the patient.
- Clean linen and mattress for the patient.
- Bed side rails for the patient’s safety.
- 2.Furniture:
- Bedside table: To keep necessary items close to the patient.
- Over-bed table: For eating or personal use by the patient.
- Chairs for visitors: Seating arrangements for the patient’s relatives.
- 3.Lighting:
- Lamp or reading light for lighting.
- Arrangement of natural light to make the patient feel comfortable.
- Call System:
- Nurse call bell: Patient can call the nurse for necessary help.
- 5.Medical Equipment:
- IV Stand: For fluids or medications.
- Oxygen Support System: For patients with breathing difficulties.
- Monitoring device: For the patient’s vital signs.
- 6.Privacy Arrangements:
- Curtain arrangement for the patient that maintains privacy during checkup or treatment.
- 7.Sanitation:
- Grab bars and non-slip flooring for the patient in the nearby washroom.
- Cleaning arrangement to keep dustbins and bathrooms clean.
- 8.Ventilation:
- Proper air flow in the patient’s room for fresh air.
- A/C or heater for comfortable thermal comfort of the patient.
- Importance of a Well-Designed Patient Unit:

- 1.Patient Comfort:
- A light and comfortable environment provides less anxiety and stress for the patient.
- 2.Faster Recovery:
- A comfortable and well-designed unit helps in the recovery process.
- 3.Infection Control:
- Maintaining cleanliness and design reduces the risk of infection.
- 4.Safety:
- The use of bed side rails, non-slip floors, and call systems is essential to increase patient safety.
- 5.Effective Communication:
- Provides rapid communication and collaboration between the patient and the nurse or doctor.
- Types of Patient Units:
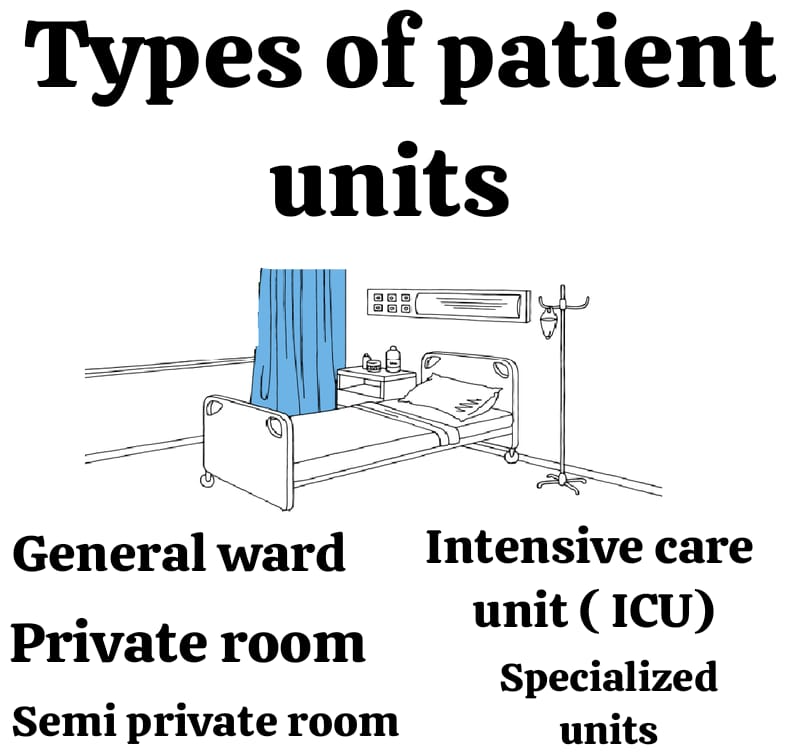
- 1,General Ward :
- Sharing space where many patients are together.
- Low cost and accessible health services.
- 2.Private Room :

- Special rooms for individual patients.
- Provides greater comfort and privacy.
- 3.Semi-Private Room :

- Two or three patients share.
- More comfortable than a general ward.
- 4.Intensive Care Unit (ICU):

- Equipped for critically ill patients, full of machines and monitoring systems.
- 5. Specialized Units :

- Specially designed for maternity wards, pediatric units, or orthopedic care.
Role of Nurses in Patient Unit Maintenance :

- 1.Cleanliness and Hygiene:
- Keeping the patient unit clean and odorless.
- 2.Monitoring:
- Using medical equipment to check the patient’s vital signs.
- 3.Patient Comfort:
- Responsible for the patient’s medication, food and comfort.
- 4.Education:
- Teaching the patient and his family about the call button and safety processes.
- 5.Safety:
- Eliminating hazardous components and maintaining a safe environment for the patient.
- b) Therapeutic Environment:-

- Therapeutic environment is a physical, social, and psychological safe space that is created specifically for the patient to recover quickly. Therapeutic environment is considered a physical space that helps the individual overcome work and medical issues.
- ∆ Hospital Physical and Environmental Plane:
- There should be a place with low population.
- The hospital site should be elevated.
- There should be independent access with a street.
- The following things should be kept away:- Dust, smoke, bad odor, noise, and traffic.
- There should be sufficient light.
- Ventilation should be done naturally.
- There should be a water facility for drinking water.
- There should be a good drainage system.
- Care should be taken to prevent pets and other insects from entering.
- ∆ Important points for hospital construction

- Both the wall and the floor should be shock absorbent, non-porous, attractive, and fire resistant, durable, and easy to clean. The floor should not be too slippery, otherwise the chances of accidents may increase. There should be no cracks in the walls and floor of the hospital, otherwise insects will start living in them.
- The floor area of the hospital should be of exact size, it should accommodate proper and sufficient patient beds and the space should not be increased or decreased.
- The number of windows and doors should be sufficient. To make the patient feel good, the windows should open outwards so that the patient gets proper amount of ventilation.
- Fumigation is a process which is done to make the entire room free from harmful microorganisms. The construction of the room should be done in such a way that the patient does not have any problem during fumigation.
- The toilet is kept away from the general ward and it should be cleaned twice a day to avoid bad odor and a clean toilet keeps many diseases away and the toilet should be made in a place where direct sunlight can fall on it.
- The main interest of the hospital should be a reception counter so that the coming patients can get help.
- If there is a kitchen and dining area in the hospital, then they are kept away from everyone, which if we understand the reason, helps in keeping the food safe and protected from infection.
- Isolation ward arrangements should be made in the hospital so that if any other patient has a disease that can spread, they can get treatment in a separate place so that the chances of other patients and health care providers getting this disease can be reduced.
- Aseptic technique should be used from the time the patient arrives in the hospital until he leaves so that the safety of the patient and the health care provider himself can be maintained, in which masks, gloves, and PPE kits should be used.
- Arrangements for storing and disposing of biomedical waste should be completed inside the hospital.
- If any kind of emergency situation occurs inside the hospital such as fire, then it is mandatory to have at least one emergency exit inside the hospital.
- The electricity system inside the hospital should be complete and a generator should also be included in it. The hospital staircase should not be circular, instead it should be straight, but if the hospital staircase is more slippery, it can also put the patient in trouble and the chances of accidents increase.
- Inside the hospital, the patient’s needs like hot and cold water should be available, the patient’s bed should have side railings, parking should be separate and some distance should be kept so that there is no more noise. The condition of the toilet inside the hospital should be working.
- “Patient safety”

- S = Sense the Error
- A = Act to Prevent
- F = Follow Safety Guidelines
- E = Inquiry
- T = Take Appropriate Remedial Measures
- Y = Your Responsibility
Therapeutic Environment – Physical Factors: Lighting

- Introduction:
- A therapeutic environment is a healthcare setting that works to create conditions conducive to the healing, comfort and well-being of the patient.
- This environment makes the patient’s recovery faster and more stable. The role of lighting as a major physical factor is extremely important.
- Proper lighting not only increases visibility for medical procedures but also has a positive effect on the patient’s mood, sleep cycle and the overall recovery process.
- Importance of Lighting in a Therapeutic Environment:
- 1.Enhances Healing:
- Natural light improves the patient’s mood and reduces depression.
- UV light is beneficial for producing vitamin D.
- 2.Promotes Safety:
- Proper lighting helps patients avoid falls or accidents.
- Makes accurate treatment and monitoring easier for nurses and doctors.
- 3.Supports Circadian Rhythm:
- Lighting balances the patient’s sleep-wake cycle, which is essential for recovery.
- 4.Enhances Mood and Comfort:
- Dim lighting provides comfort at night.
- Contrast lighting is important for the mental comfort of the patient.
- Types of Lighting in a Therapeutic Environment:
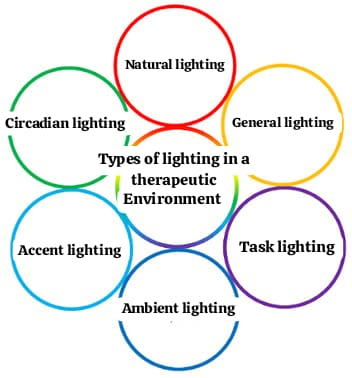
- 1.Natural Lighting :

- It is beneficial for the patient to be in contact with nature during the day.
- Can be placed in rooms near windows or balconies.
- Example: Sunlight.
- 2. General Lighting :

- Sufficient light for a healthy room environment.
- Example: LED lights or tubelights.
- 3.Task Lighting :

- Focused light for a specific task.
- Example: Reading lamp or overhead light over a patient’s bed.
- 4. Ambient Lighting :

- Soft lighting to create a peaceful atmosphere.
- This reduces patient tension in healthcare settings.
- 5.Accent Lighting :

- To highlight art or attractive points in a room.
- Useful for redecorating rooms.
- 6.Circadian Lighting :

- Designed for the patient’s sleep-wake cycle.
- Brighter during the day and softer light at night.
Impact of Lighting on Patient Recovery :

- 1.Physical Healing:
- Natural light strengthens the patient’s immune system.
- Good lighting helps in precision in the surgical area.
- 2.Mental Well-being:
- Dim lighting reduces tension and depression.
- Bright light keeps the mood energetic.
- 3.Sleep Improvement:
- Proper lighting balances the patient’s circadian rhythm.
- Lower light at night helps the patient sleep.
- Safety:
- Clear lighting helps the patient stay safe during movement.
- A night lamp is useful for the patient at night.
- Lighting Design Considerations for a Therapeutic Environment:

- 1.Adjustability:
- The ability to adjust brightness and color according to the patient’s comfort.
- 2.Glare Reduction:
- Excessive brightness causes discomfort to the patient.
- 3.Energy Efficiency:
- Energy-saving systems such as LED lighting.
- 4.Placement:
- Proper placement of lamps, floor lights, and reading lights near the bed.
- Role of Nurses in Managing Lighting:

- 1.Monitoring Patient Needs:
- Allowing sufficient time for the patient to obtain healthy lighting.
- Adjusting Lighting:
- Adjusting lighting levels for patient privacy and comfort.
- 3.Educating Patients:
- Using soft lighting at night and assisting with sleep.
- Ensuring Safety:
- Lighting design eliminates risk factors for the patient.
- Therapeutic Environment – Physical Factors: Temperature

- Definition:
- A Therapeutic Environment is a healthcare environment that is comfortable and conducive to treatment for the patient. Physical factors such as temperature, lighting, noise control, and ventilation play an important role in this.
- Importance of Temperature in a Therapeutic Environment:
- 1.Patient Comfort:
- A suitable temperature provides physical and mental comfort to the patient.
- Extreme heat or cold can increase stress and anxiety.
- 2.Faster Recovery:
- Ideal temperatures alleviate symptoms of illness and speed up recovery.
- 3.Infection Control:
- A proper balance of temperature reduces the spread of infection, especially in sensitive areas such as the ICU.
- 4.Physiological Stability:
- Maintaining a patient’s body temperature at a normal level is important for fever management.
- Ideal Temperature Range for Patient Care:
- 1.General Patient Rooms:
- 22°C to 24°C (72°F to 75°F): A comfortable environment for the patient.
- 2.Neonatal Units:
- 24°C to 26°C (75°F to 79°F): A warm environment for the newborn.
- 3.Intensive Care Units (ICU):
- 21°C to 23°C (70°F to 73°F): Temperature control reduces infection.
- 4.Operation Theatres:
- 20°C to 22°C (68°F to 72°F): Minimum temperature required to maintain sterility.
- Factors Influencing Temperature in the Patient Environment:
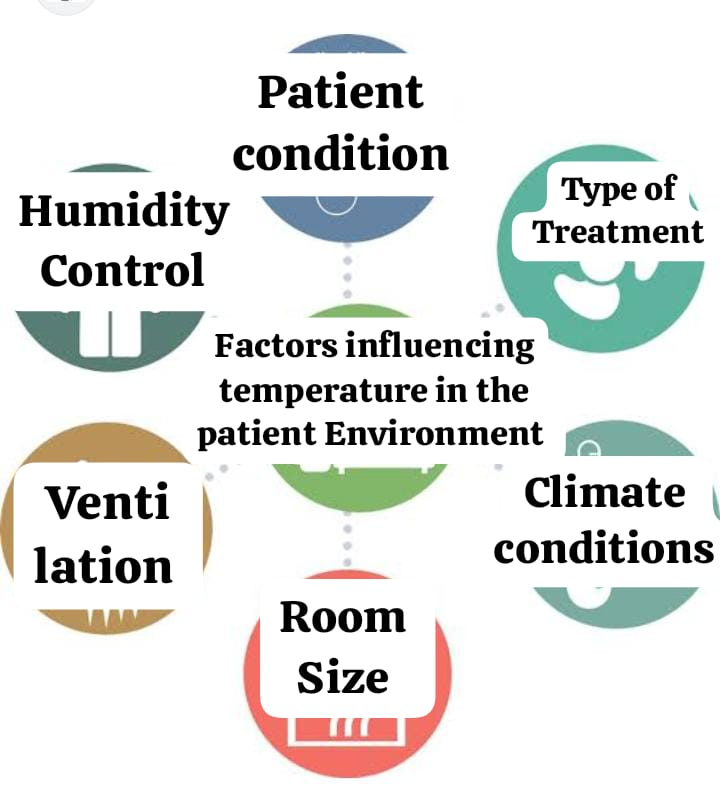
- 1.Patient’s Condition:
- A patient with fever or hypothermia may need to maintain a higher or lower temperature.
- Type of Treatment:
- Lower temperatures are required for sterile procedures in theatres.
- Climatic Conditions:
- Adjust the temperature according to the climate of the hospital location.
- Room Size and Ventilation:
- Larger rooms require more ventilation to maintain a constant temperature.
- 5.Humidity Control:
- A humidity level of 30% to 50% makes the temperature comfortable.
- Challenges in Maintaining Therapeutic Temperature:
- Climate Extremes:
- It is difficult to maintain an ideal temperature in areas with hot or cold climates.
- 2.Power Supply:
- Frequent power outages can cause temperature levels in the room to fluctuate.
- Individual Patient Needs:
- The temperature needs of each patient may be different.
- 4.Ventilation Systems:
- Old or malfunctioning ACs and heaters.
- Steps to Maintain Ideal Temperature:
- 1.Use of HVAC Systems:
- Balancing the temperature through heating, ventilation, and air conditioning systems.
- 2.Regular Monitoring:
- Use of a thermometer to monitor the temperature in the patient’s room.
- 3.Patient Feedback:
- Get feedback from the patient on whether the environment is comfortable or not.
- 4.Proper Insulation:
- Reducing heat loss through insulation on hospital walls and ceilings.
- 5.Zoning Techniques:
- Maintaining different temperature ranges in different departments.
- Role of Nurses in Temperature Maintenance:

1.Observation:
- Monitoring the patient for signs of cooling or heating.
- Adjustment:
- Using bedsheets, blankets, or heating devices as needed.
- Communication:
- Contacting for immediate observation if there is a problem with the patient’s temperature for comfort.
4.Emergency Action:
- If the patient is severely cold or hot, notify staff for immediate help.
- Temperature is an important factor in the patient’s comfort and recovery. An ideal therapeutic environment can be maintained with effective supervision by healthcare professionals and appropriate technical support. This allows the patient to be comfortable, safe, and receive rapid treatment.
- Therapeutic Environment – Physical Factors: Ventilation
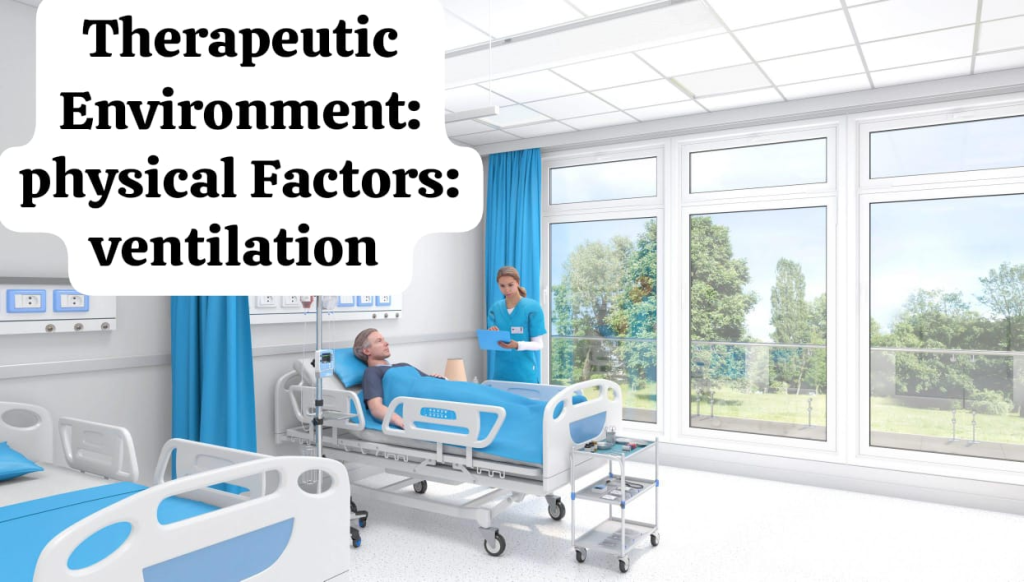
- Definition:
- Ventilation is the process of maintaining fresh air and clean air circulation in a healthcare environment. It is important for removing pollutants, odors, and infectious agents from the air. Proper ventilation is essential for patient comfort, safety, and recovery.
- Importance of Ventilation in Therapeutic Environment:
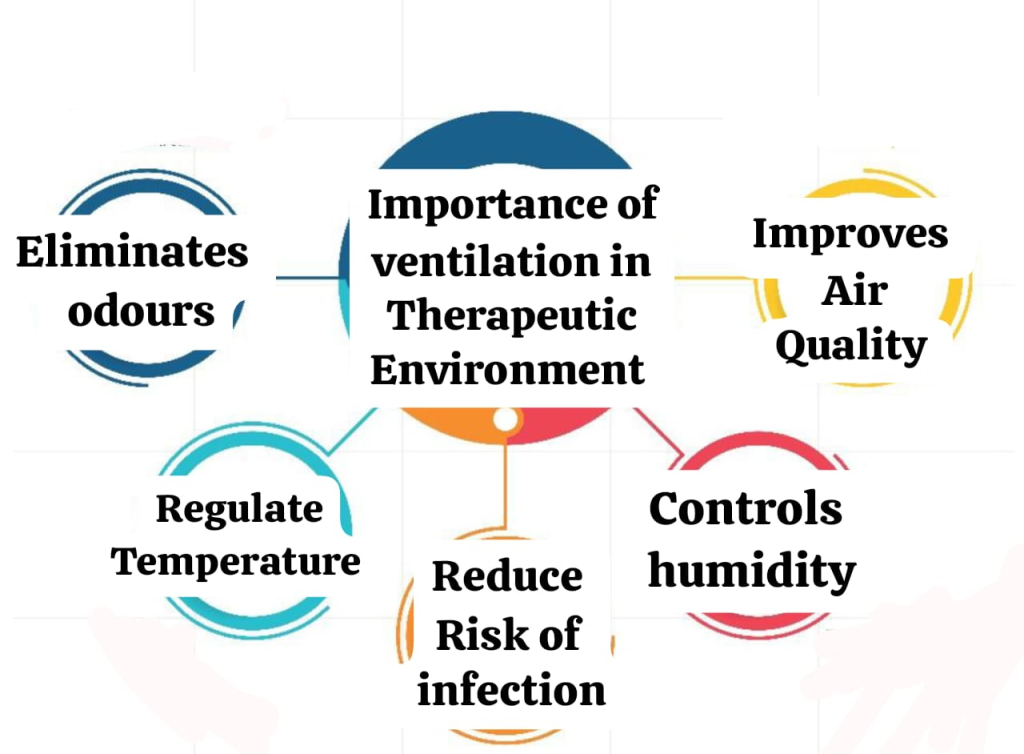
- 1.Improves Air Quality:
- Provides fresh air by removing pollutants and infectious dust.
- Especially needed in areas like laboratories and ICUs.
- 2.Controls Humidity:
- Maintains ideal humidity levels (30-50%) to help with patient comfort and infection control.
- 3.Reduces Risk of Infection:
- Helps remove infectious microbes from the air and maintain a safe environment.
- 4.Regulates Temperature:
- Fresh air flow keeps temperatures cool.
- 5.Eliminates Odors:
- Removes odors and chemicals from operating theaters and patient rooms.
- Types of Ventilation:

- 1.Natural Ventilation:
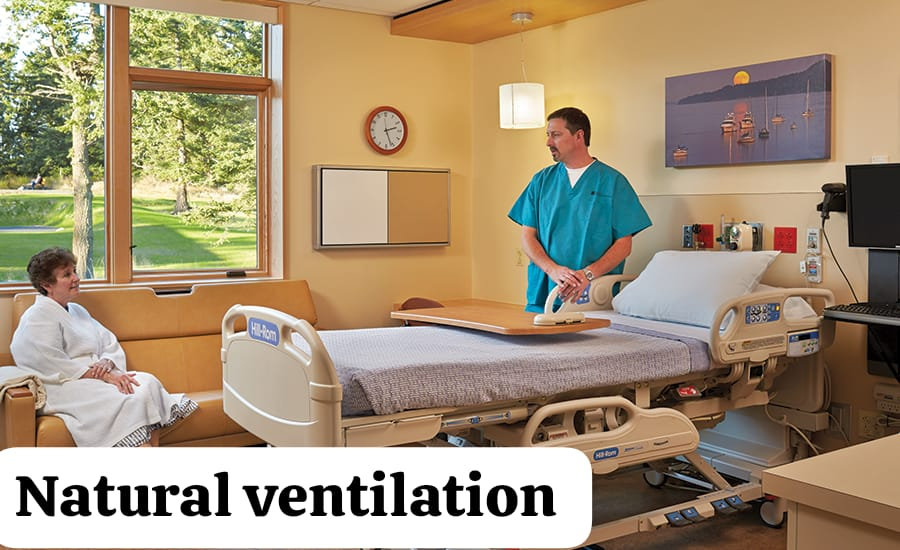
- Fresh air through windows and doors.
- Commonly used in patient rooms.
- 2.Mechanical Ventilation:
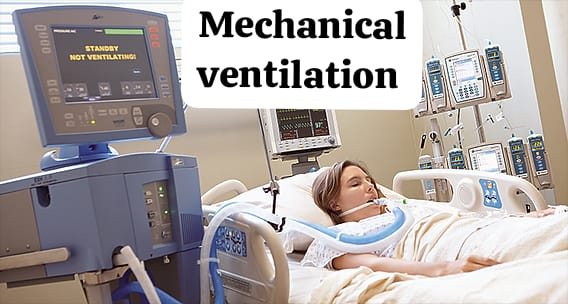
- Use of HVAC (Heating, Ventilation, and Air Conditioning) system.
- Essential in operation theatres and ICUs.
- 3.Hybrid Ventilation:
- Ventilation with natural and machine assistance.
- 4.Exhaust Ventilation:

- A special air exchange system to remove contamination and odors.
- Ventilation Standards for Healthcare Settings :
- 1.Air Changes Per Hour (ACH):
- 12 ACH is required in ICU and Operation Theatre.
- 6 ACH is sufficient for General Ward.
- 2.Pressure Control:
- Positive pressure in Operation Theatre prevents infection.
- Negative pressure in Isolation Room prevents the spread of infection.
- 3.Filtration System:
- HEPA filters are useful for removing microbes from the air.
- Factors Influencing Ventilation:
- 1.Room Design:
- Room layout and window and door position.
- 2.Climate Conditions:
- Different techniques have to be adopted for ventilation in cold or hot regions.
- 3.Patient Density:
- As the number of patients increases, more ventilation is required.
- 4.Type of Healthcare Facility:
- More controlled ventilation is required in ICUs and operating theaters.
- Challenges in Maintaining Ventilation:
- 1.Power Failures:
- Ventilation can be disrupted by relying on machines.
- 2.Filter Maintenance:
- HEPA filters and air ducts need to be cleaned regularly.
- 3.Humidity Issues:
- High humidity levels can be attractive to mold and fungus.
- 4.Cost of Advanced Systems:
- High-end ventilation systems can be expensive.
- Steps to Ensure Proper Ventilation:
- 1.Installation of HVAC Systems:
- Healthcare requires access to fresh air and filtered air.
- 2.Regular Maintenance:
- Cleaning filters and ducts.
- 3.Use of Exhaust Fans:
- To remove air from a contaminated or smelly room.
- 4.Proper Room Design:
- Windows and doors should be designed in appropriate locations.
- 5.Monitor Air Quality:
- Track carbon dioxide and oxygen levels with an air quality monitoring device.
- Role of Nurses in Ventilation Maintenance:
- 1.Observation:
- Observe the patient for shortness of breath or discomfort.
- 2.Reporting:
- Immediately report any HVAC system or ventilation malfunctions.
- 3.Education:
- Instruct patients and staff to maintain ventilation in the room.
- 4.Emergency Preparedness:
- Provide oxygen support as needed to the patient.
- Ventilation is a cornerstone of patient comfort and recovery. It is critical for infection prevention, fresh air, and temperature regulation. Proper maintenance, system upgrades, and a comfortable environment for the patient ensure optimal outcomes for the medical professional in a therapeutic environment.
- Therapeutic Environment – Physical Factors: Humidity

- Definition:
- Humidity is the amount of moisture in the air, which is important for patient comfort, infection prevention, and recovery. It is important to maintain ideal humidity levels (30% to 50%) in healthcare settings to keep the air clean and provide a comfortable environment for the patient.
- Importance of Humidity in a Therapeutic Environment:

- 1.Maintains Airway Moisture:
- Low humidity can dry out the airways, which can make breathing more difficult.
- High humidity reduces the accumulation of mucus in the airways.
- 2.Prevents Dehydration:
- A proper humidity level keeps the body’s water levels balanced.
- 3.Reduces Risk of Infections:
- Low humidity promotes the growth of viruses and bacteria.
- At ideal humidity levels, it is easier to control infectious microbes in the air.
- 4.Promotes Skin Integrity:
- Low humidity can cause the skin to become dry and dull.
- 5.Improves Comfort:
- Provides ease of breathing and comfort for the patient.
- Ideal Humidity Levels in Healthcare Settings:
- 1.General Patient Rooms:
- 30% to 50%: Comfortable and reduces the risk of infection.
- 2.Operation Theatres:
- 20% to 60%: To maintain sterility.
- 3.ICU and Neonatal Units:
- 40% to 60%: Humidity levels support the immune system of hypersensitive patients.
- Effects of Improper Humidity Levels:
- 1.Low Humidity (too dry air):
- Respiratory tract irritation and difficulty breathing.
- Skin problems such as dryness and irritation.
- Increased risk of bacterial and viral infections.
- 2.High Humidity:
- An ideal environment for the growth of fungi and mold.
- Respiratory diseases such as asthma and allergies increase.
- Lack of comfort in patients.
- Factors Influencing Humidity in Hospitals:
- 1.Climate:
- Humidity levels are higher than normal in hot and humid regions.
- The air remains dry in cold regions.
- 2.Ventilation Systems:
- HVAC systems help in controlling humidity levels.
- 3.Room Usage:
- Humidity levels are strictly controlled in operation theatres and isolation rooms.
- 4.Patient Condition:
- Humidity is more effective for patients with respiratory diseases.
- Managing Humidity Levels in Healthcare Settings:
- Use of Humidifiers and Dehumidifiers:
- Use appropriate devices to increase or decrease humidity in the air.
- Regular Maintenance of HVAC Systems:
- Keep filters clean and inspect equipment.
- Monitoring Devices:
- Use hygrometers to track humidity levels with great accuracy.
- Ventilation Adjustments:
- Maintain proper airflow in areas such as the operating theater and ICU.
- Patient Feedback:
- Make any changes based on the patient’s comfort level.
- Challenges in Humidity Control:
- 1.Climate Variability:
- It is difficult to control high humidity levels in hot climates.
- 2.Equipment Costs:
- Humidifier and dehumidifier systems are expensive.
- 3.Power Supply Issues:
- The system may not function properly due to a faulty power supply.
- 4.Maintenance Requirements:
- Equipment requires regular maintenance.
- Role of Nurses in Humidity Management:
- 1.Observation:
- Observing the effect of humidity on the patient’s respiratory or skin conditions.
- 2.Reporting Issues:
- Reporting immediately any malfunctions in the HVAC system or humidity equipment.
- 3.Patient Comfort:
- Try to improve humidity levels to make the patient comfortable.
- 4.Emergency Adjustments:
- Urgent use of a humidifier or dehumidifier.
- Humidity is an important factor in patient comfort, infection control, and health promotion in healthcare settings. Modern equipment and systematic monitoring are essential to maintaining appropriate humidity levels. Through the efforts of nurses and healthcare professionals, a comfortable and recovery-supportive environment can be created for the patient.
- Therapeutic Environment – Physical Factors: Noise
- Definition:
- Noise is unwanted or inaudible sound that disrupts a patient’s comfort, psychological state, and recovery. It is important to control noise levels in healthcare settings because it can affect the physical, mental, and psychological health of patients.
- Sources of Noise in Healthcare Settings:
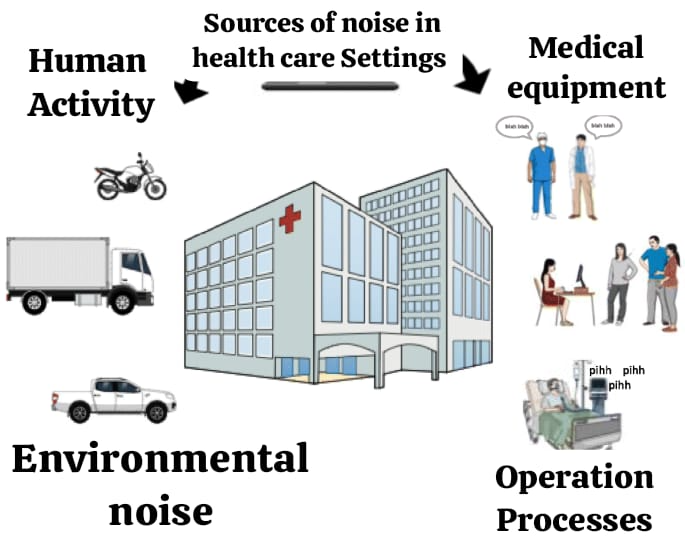
- 1.Medical Equipment:
- The sound of monitors, alarms, and ventilators.
- Emergency equipment, such as defibrillators and oxygen machines.
- 2.Human Activity:
- Communication or discussion between staff and patients.
- The sound of family members and visitors.
- 3.Environmental Noise:
- External noise such as traffic or construction work.
- The sound of an HVAC system or fan in a healthcare setting.
- 4.Operational Processes:
- The friction of moving beds or the rattling of beds.
- The sound of doors opening and closing during ward operations.
- Impact of Noise in a Therapeutic Environment:
- 1.On Patients :
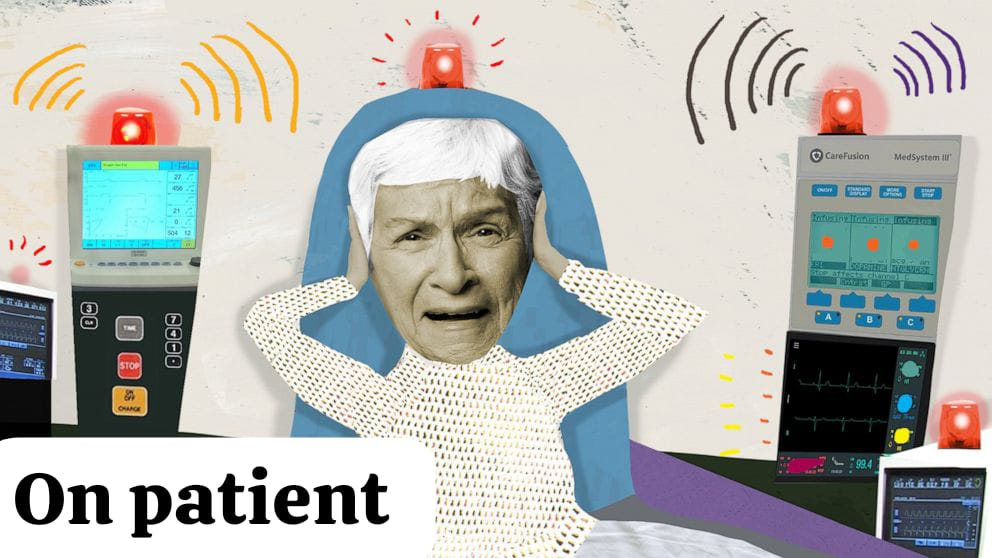
- Disturbed Sleep: Noise disrupts sleep quality and recovery.
- Increased Stress: Noise increases stress levels, which increases heart rate and blood pressure.
- Delayed Recovery: Noise slows down patient recovery, especially in ICU patients.
- 2.On Healthcare Providers :
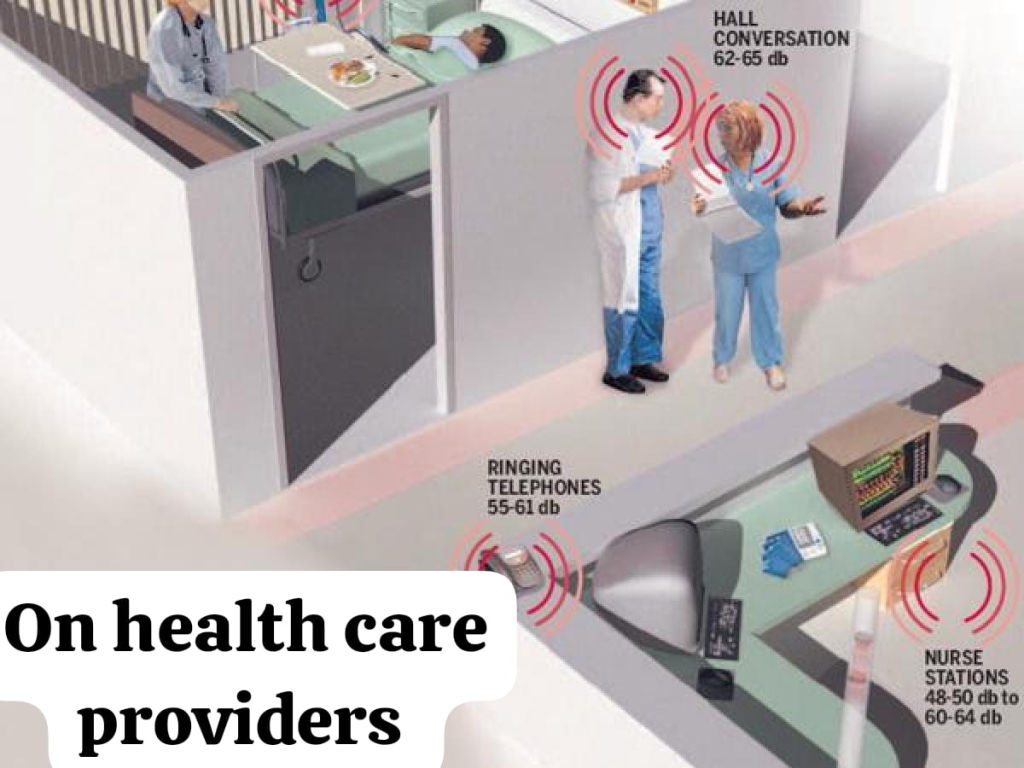
- Reduced Concentration: Noise can be a barrier to staff focusing on work.
- Communication Errors: Loud noise can cause communication difficulties between staff and doctors.
- 3.On Visitors and Family :

- Increased Anxiety: A stressful environment does not allow family members to feel comfortable.
- Acceptable Noise Levels in Healthcare:
- Daytime: 35 dB (decibels).
- Nighttime: 30 dB (decibels).
- Operation Theatres and ICU: 20-25 dB.
- Sources of Excessive Noise:
- 1.Unnecessary Alarms:
- Frequent beeping of health monitors.
- 2.Crowded Areas:
- Waiting areas and hospital courtyards.
- 3.Construction and Maintenance:
- Noise from machinery and tools.
- Strategies to Manage Noise in Healthcare Settings:
- 1.Environmental Modifications:
- Use of soundproof doors and windows.
- Install noise reduction materials such as carpets and wall panels.
- 2.Alarm Management:
- Prioritize important medical alarms and reduce unnecessary alarms.
- 3.Staff Training:
- Encourage nurses and healthcare professionals to maintain a peaceful environment.
- 4.Patient and Family Education:
- Give patients and visitors guidance on reducing noise.
- 5.Use of White Noise Machines:
- It creates a comfortable environment for the patient and masks the noise.
- 6.HVAC System Maintenance:
- Regular maintenance of fans and air conditioners reduces noise.
- Challenges in Noise Control:
- 1.High Patient Turnover:
- Noise increases with more patients and visitors.
- 2.Unavoidable Environmental Noise:
- Noise from outside traffic or nearby construction.
- 3.Equipment Dependency:
- It is difficult to reduce noise because medical equipment is indispensable.
- Role of Nurses in Noise Reduction:
- 1.Monitoring:
- Monitoring the noise level in the patient room.
- 2.Reporting:
- Reporting unnecessary noise from staff or machines.
- 3.Patient Comfort:
- Ensuring that the noise level is comfortable for the patient.
- 4.Educating Visitors:
- Politely asking visitors to reduce noise.
- Noise is an important factor in healthcare settings that affects patient comfort and recovery. Therefore, noise control can improve patient comfort and staff efficiency. Appropriate management and use of technology can help reduce noise levels, which is a key goal of a therapeutic environment.
- Pestilence
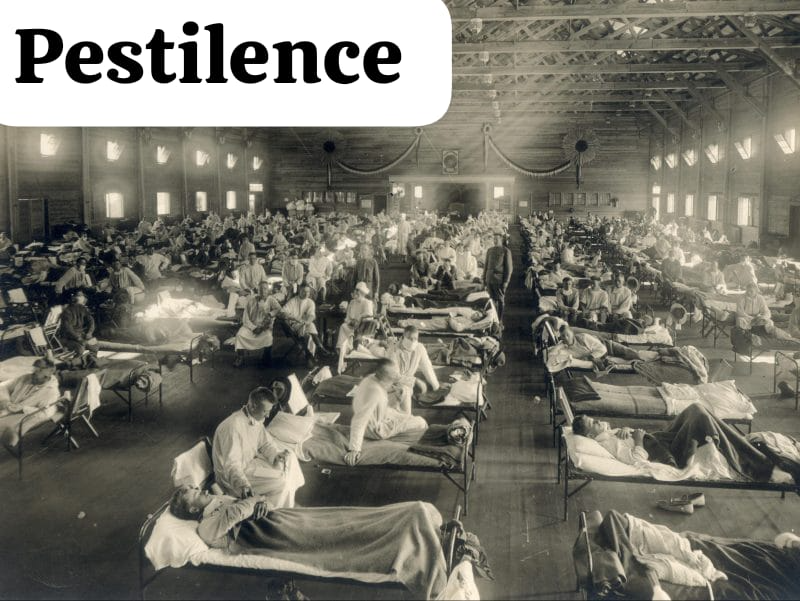
- Definition:
- Pestilence is a serious and fatal infectious disease that spreads rapidly and causes large-scale mortality. Pestilence is usually used to refer to epidemics that cause significant global or regional mortality, such as plague and cholera.
- Characteristics of Pestilence:
- High Mortality Rate:
- Pestilence has a serious impact on health systems and the way of life of people.
- Rapid Spread:
- Widespread spread by human contact, waterborne transmission, or airborne pathogens.
- Global or Regional Impact:
- Pestilence usually affects the lives of a large number of people, leading to the declaration of an epidemic.
- Caused by Pathogens:
- Bacteria, viruses, or parasites are the main causes of pestilence.
- Causes of Pestilence:
- Infectious Agents:
- Bacteria: Plague, tuberculosis.
- Virus: Covid-19, Ebola.
- Parasites: Malaria.
- Poor Sanitation:
- Dirty water or unclean food is a major factor in the spread of pestilence.
- Overcrowding:
- Overcrowding in urban areas encourages pestilence to spread rapidly.
- Globalization:
- Travel and trade allow pestilence to spread from one country to another.
- Weak Immune Systems:
- Children, the elderly, or immunocompromised individuals are at greater risk for pestilence, for example.
- Examples of Pestilence in History:
- The Black Death (1347-1351):
- A plague in Europe that killed over 25 million people.
- Spanish Flu (1918-1919):
- A global pandemic that killed an estimated 50 million people.
- Cholera Outbreaks:
- A major outbreak in the Indian subcontinent in the 19th and 20th centuries.
- COVID-19 Pandemic (2019-2023):
- A coronavirus pandemic that has had a severe impact on global health, economic conditions, and society.
- Impact of Pestilence:
- Health Impact:
- High mortality and strain on health services.
- Mental health stress and fear.
- Economic Impact:
- Business closure and economic downturn.
- Increased costs for health systems.
- Social Impact:
- Spread of infection in crowded areas.
- Delays in communication due to quarantine and isolation.
- Global Impact:
- Restrictions on international trade and travel.
- Preventive Measures for Pestilence:
- Vaccination Programs:
- To increase immunity.
- Example: COVID-19, malaria.
- Improved Sanitation:
- Proper hygiene standards for clean water and food.
- Quarantine and Isolation:
- Infected people are isolated to prevent the spread of infection.
- Awareness Campaigns:
- Informing people about precautions, such as wearing masks and washing hands.
- International Collaboration:
- WHO and other organizations cooperate to prevent pestilence.
- Role of Healthcare Professionals:
- Monitoring and Surveillance:
- Tracking and detecting early signs of pestilence.
- Public Education:
- Public awareness and education about infection prevention measures.
- Treatment and Management:
- Proper treatment of infected patients.
- Collaboration:
- Working with health systems, governments, and international organizations.
- Pestilence is a major challenge for humanity, affecting health, economic, and social systems. Its prevention requires extensive education, proper health infrastructure, and global cooperation. Historical examples of pestilence prove that prevention and vigilance are the best protection against pestilence.
- ∆ Safety measures inside the hospital:
- Never lower the railing of the hospital bed and ask the nurse to use the bed controls so that there is no mistake and do not use the bedside table for support on the bed – keep the glass in the drawer
- If any relatives of the patient smoke, then forbid them.
- Wash hands, do not allow people who are already ill to visit, ask for the vaccine.
- Help clean your environment, prevent falls.
- Safety Needs for Admitted Patients

- Definition:
- Safety requirements are measures to provide physical, psychological, and social safety for patients in the hospital setting. A comfortable and safe environment for hospitalized patients is essential for proper treatment and rapid recovery. This includes everything from infection control to proper medication use and providing security for daily operations.
- Key safety areas for hospitalized patients:

- Physical Safety:
- Fall Prevention:
- Prevent the patient from falling by installing bed side rails.
- Use of non-slip flooring.
- Provide a walker or wheelchair to help the patient walk.
- Safe Movement of the patient:
- Help the patient avoid injury from hospital machines or equipment.
- Transfer of the patient should be done only with the help of nursing staff.
- Bed Position:
- Use an adjustable bed to keep the patient in a comfortable position.
- Safe Use of Objects:
- Keep equipment like heaters, oxygen cylinders in the hospital safely.
- Infection Control:
- Hand Hygiene:
- Ensure that nurses, doctors, and patients use hand sanitizer or soap.
- Use of PPE Kit:
- Provide staff with quality PPE kits for infectious patients.
- Isolation Protocols:
- Keep patients at risk of infection in separate rooms.
- Maintaining Cleanliness:
- Clean bedsheets, linens, and medical equipment daily.
- Medication Safety:
- Rights of Medication:
- Give medication only after checking the patient for the right medication, dose, time, route, and dosage.
- Checking for Allergies:
- Get prior information about the patient’s drug allergies.
- Proper Storage:
- Storing medicines safely, especially those that require refrigeration.
- Prevent Medication Errors:
- Errors can be avoided through a double check system.
- Psychological Safety:
- Stress Reduction:
- Encouraging the patient to stay with a family member for peace of mind.
- Respect and Privacy:
- Maintaining confidentiality during patient information and treatment.
- Positive Communication:
- Communicating with the patient in a polite and understanding manner, so that he feels safe.
- Psychological Support:
- Providing emotional support to the patient through counseling.
- Environmental Safety:
- Electrical Safety:
- Regularly checking whether medical equipment is working properly.
- Lighting and Temperature:
- Ensure comfortable lighting and airflow for the patient.
- Non-Slip Flooring:
- Special flooring to prevent slippery flooring.
- Noise Reduction:
- Maintain a peaceful environment for the patient.
- Emergency Preparedness:
- Provide CPR machines:
- Keep CPR machines ready for immediate assistance in case of sudden cardiac arrest.
- Fire Safety:
- Keep fire extinguishers and fire protection procedures active.
- Accident Preparedness:
- Ensure the presence of first aid kits and nursing staff.
- Role of Nurses in Patient Safety for admitted patients:

- Observation and Monitoring:
- Regularly monitor the patient’s vital signs and health.
- Contact the doctor immediately if the patient shows any urgent signs.
- Education and Awareness:
- Inform the patient about the proper use of medication and treatment.
- Guide the patient and family on hygiene and infection prevention.
- Communication:
- Continuous and clear communication with the patient and family.
- Sharing medication information and the patient’s condition among members of the healthcare team.
- Maintenance:
- Maintain the functionality of medical equipment and the cleanliness of the patient’s room.
- Safety requirements are a fundamental part of creating a comfortable and treatment-supportive environment for the patient. The primary responsibility of nurses and healthcare teams is to systematically provide physical, psychological, and environmental protection for hospitalized patients. Appropriate policies, precautions, and communication can help patients experience a more comfortable and safe experience.
- Prevention of Environmental Hazards in Hospital
- Definition:
- Environmental Hazards are hazards in the hospital environment that can have a harmful effect on patients, staff, and visitors. These hazards can be caused by factors such as infection, chemical hazards, physical hazards, or noise and pollution. Preventing environmental hazards is essential for health care and patient safety.
- Types of Environmental Hazards in Hospitals:
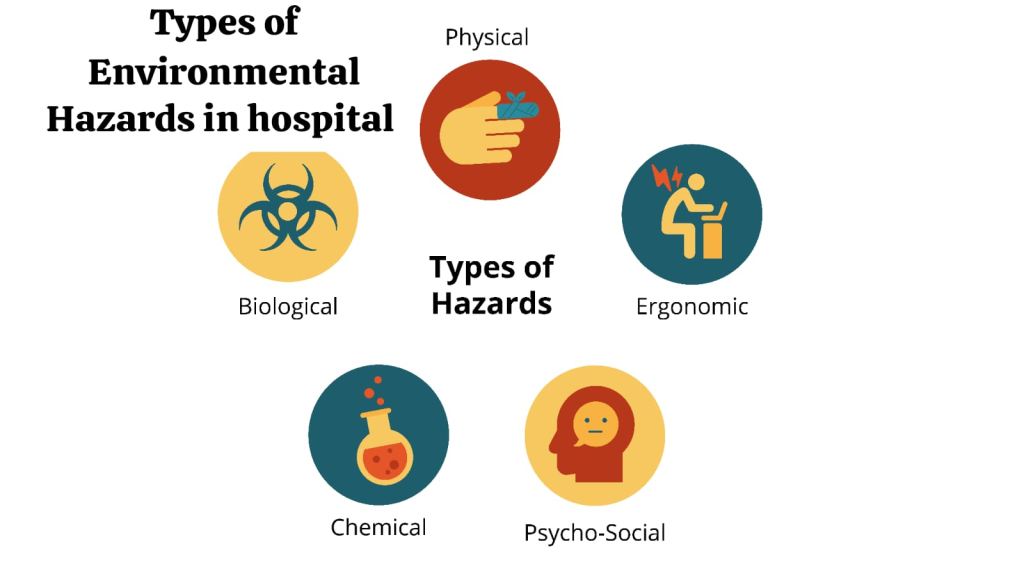
- 1.Biological Hazards:
- Infectious Agents such as bacteria, viruses, fungi.
- Bloodborne Pathogens such as HIV, Hepatitis-B.
- 2.Chemical Hazards:
- Dangerous drugs or chemicals, such as cytostatic drugs, disinfectants.
- Gas leakage, such as oxygen or anesthetic gas.
- 3.Physical Hazards:
- Falls due to lack of non-slip floors.
- Improperly serviced electrical equipment.
- 4.Ergonomic Hazards:
- Heavy equipment or patient handling for nursing staff.
- 5.Environmental Pollution:
- Contaminated water, sewage, and waste dumping.
- Noise pollution increases stress in the hospital environment.
- Strategies for Preventing Environmental Hazards:

- Biological Hazard Prevention:
- Infection Control Practices:
- Use PPE kit (gloves, mask) and maintain hand hygiene.
- Isolation of patients wherever necessary.
- Sterilization:
- Regular sterilization of medical equipment.
- Vaccination:
- Required vaccinations for healthcare staff and patients.
- Chemical Hazard Prevention:
- Proper Storage:
- Storage of chemicals and solvents properly.
- Spill Management:
- Keep a spill kit available for chemical or blood leakage.
- Waste Disposal:
- Dispose of biomedical waste in accordance with government regulations.
- Physical Hazard Prevention:
- Floor Safety:
- Using non-slip materials and maintaining cleanliness.
- Electrical Safety:
- Regular maintenance and inspection of medical equipment.
- Equipment Handling:
- Training in the use of machinery and operating equipment.
- Ergonomic Hazard Prevention:
- Proper Lifting Techniques:
- Training nursing staff in proper manual handling for patient transfers.
- Use of Assistive Devices:
- Using wheelchairs, lifts, and trolleys.
- Environmental Pollution Prevention:
- Water Management:
- Provision of clean drinking water.
- Waste Segregation:
- Separation of bio-medical and general waste.
- Noise Control:
- Controlling the noise level of medical equipment and maintaining a peaceful environment.
- Role of Nurses in Preventing Environmental Hazards:
- 1.Observation and Monitoring:
- Proper observation of risk factors for patients and staff.
- 2.Education and Training:
- Educating patients, staff and visitors about infection and risk prevention.
- 3.Waste Management:
- Following the rules for proper disposal and disposal of biomedical waste.
- 4.Emergency Preparedness:
- Knowing and implementing immediate protocols for situations such as infection, leakage or fire. Environmental hazards in hospitals can have a serious impact on health.
- These hazards can be prevented through infection control, safe waste management, prevention of chemical hazards, and successful training. With the proper efforts of nursing staff and healthcare professionals, it is possible to create a safe and comfortable environment, which is comfortable and healthy for patients and staff.
- ∆ Psychosocial factors:-
- Assessment to get the basic needs of the patient, which includes emotional and mental well-being, is called psychosocial needs.
- If we understand, we know that mental health is related to physical health, which means that if there is any impact on mental health, it can also affect the person’s body physically. Psychosocial factors such as stress, depression, hopelessness, all these can cause heart disease.
- The patient should feel safe and secure overall. Each person’s primary desire is to be recognized as a unique person so that the patient can feel at ease in their relationships with the staff and with other patients and families.
- Patient adjustment in the hospital
- Introduction
- A health care facility is an institution where health-related care is provided. The patient receives a lot of personal attention in the care they receive. As soon as they get admitted to the hospital, the patient has to face the hospital staff, doctors, nurses. The hospital environment is different from the home environment for them. Their daily routine changes and due to the change in the environment, they also feel anxiety. All this can change the patient emotionally, mentally and physically and for the patient, their income and socioeconomic status and culture can affect their health status.
- Factors affecting patient adjustment in hospital:-
- -Age
- -Gender
- -Literacy level
- -Language
- -Work
- -Residence
- -Income and status in society
- -Belief
- -Nationality
- ∆ Patient’s reaction to hospitalization:
- Fear
- Loneliness
- Anxiety
- Loss of identity
- ∆ Patient’s Emotional reaction to hospitalization:
- The patient feels depressed.
- The patient feels irritable.
- The patient also feels angry.
- The patient feels dependent on others
- The patient feels denied
∆The nurse’s role in adjusting the patient:- - Welcome the patient.
- The nurse should show empathy to the patient.
- Always respect the patient.
- Do not treat any patient differently from anyone else.
- Always address the patient with the titles of Mr. and Mrs.
- Do not try to impress the patient.
- Listen to the patient.
- Talk to the patient and ask him questions.
- Help the patient and his family adjust.
- Provide orientation to the patient and his family.
- Respect the patient’s privacy.
- Explaining any procedure to be performed with the patient.
- ∆ Causes of fear and anxiety.
- The patient isolates himself from his entire family.
- He feels afraid of seeing his illness progressing.
- The patient walks in pain.
- The patient fears for his family that he may fall ill.
- The patient feels fear and anxiety due to his economic problems.
- ∆ Advantages of Hospitalization:-
- Diseases can be prevented due to hospitalization.
- Health is promoted due to hospitalization.
- Hospitalization helps in curing diseases.
- Understanding the patient personally

- Various factors:
- Understanding the patient as a person is essential for the success of patient care and treatment. In this process, it is necessary to consider their health status along with their social, economic and cultural factors.
- Understanding the Patient as a Person
- Understanding the patient as a person is essential for humane treatment of the patient.
- Habits and Lifestyle: Understanding the patient’s daily life and habits can help in better planning their treatment.
- Identity and Aspirations: It is important to pay attention to the patient’s goals and hopes in life.
- Emotional Status: The state in which the patient is (such as stressed, anxious or calm), affects their treatment.
- Socio-Economic Background
- The patient’s social and economic factors play an important role in their health and treatment decisions.
- Family and Support System:
- Relying on family members and their support provides a strong foundation for the patient.
- Economic Status:
- Knowing the patient’s income, health insurance, and ability to pay for treatment, to create a fully appropriate and affordable treatment plan.
- Education Level:
- Understanding how the patient obtains and uses health-related information.
- Cultural Background
- The patient’s culture and traditions influence health and treatment decisions.
- Food and Dietary Habits:
- Recognizing any specific diet that is prescribed by that religion or culture.
- Health Beliefs:
- Understanding beliefs and assumptions about illness and treatment.
- Language and Communication:
- Communicating in a language that the patient feels comfortable speaking.
- Health Status
- The patient’s current and past health status is important in their treatment.
- Medical History:
- Details of previous illnesses or treatments.
- Present Complaints:
- Detailed information about the current illness and its symptoms.
- Mental and Physical Health:
- Make a complete diagnosis by considering both factors. By understanding the patient as a whole person, who has social, economic and cultural factors, more effective and personalized treatment can be provided. Such a holistic approach leads to rapid improvement in the patient’s health.
- Admission:

- Definition:
- To allow a patient to stay in a hospital for observation, investigation and treatment of the disease for which the patient is suffering.
- ∆ Type of admission
- Emergency admission:-
Emergency admission is done when the patient needs immediate treatment in an emergency situation for example heart attack, accident, labor pain, shock, hyperpyrexia in which the patient’s life is at risk, his admission is done in emergency. - Routine admission:-
Routine admission is done when the patient needs to be admitted to the hospital for investigation and treatment and surgery as per the planning. - ∆ Purpose of admission:
- To provide immediate care to the patient.
- To ensure the patient’s comfort and safety.
- To ensure that the hospital staff is ready for any emergency.
- To collect data from the patient.
- ∆ Procedure of admission:
- First of all, prepare the room, arrange all the items in one place and adjust the height of the bed.
- Introduce yourself to the patient, check the patient’s identification and greet the patient and his relatives.
- To check the patient’s vital signs and check the symptoms and if any specimen is to be collected for the lab, collect it.
- To provide privacy to the patient and if the patient needs an admission bath, then give it.
- To give information to the patient about the ward and tell the visiting hours.
- To answer any doubts of the patient and the patient’s relative.
- To maintain reports and records.
- ∆ Unit and its preparation:
- The place where the patient is kept during the hospital admission of the patient is called the unit.
- ∆ Some activities before admitting a patient
- Keep the patient ready and arrange the open bed.
- The patient should be able to access his bed easily. If necessary, increase or decrease the height of the patient’s bed.
- Assemble 21 and other supplies as needed such as bath basin, drinking glass, plate, thermometer, paper, lotion and hospital gown.
- Assemble special equipment if needed such as oxygen bottle, cardiac monitor, suction machine.
- ∆ Principle of admission:-
- Illness can be a romantic experience for the patient which can also stress physical and mental health.
- People have different types of habits and behaviors.
- Entering the hospital is a threat to one’s personal identity.
- A sudden change in the environment can produce fear and anxiety.
- Discharge:
- The nurse is responsible for the discharge of the patient. The planning and decision of discharge is not at the point, but from the start, when the patient enters the hospital, whether his condition has improved or not, the discharge decides whether the patient should be sent home or referred. The discharge will contain all the advice that will help the patient for full recovery.
- Types of Discharge: –
- Cure and Discharge: When the patient’s treatment is complete and the patient is discharged as per the doctor’s order.
- LAMA: – When the client wants to stop taking the treatment on his own and goes against the doctor’s medical advice and asks for discharge, it is called LAMA.
- Abscond:- When the patient leaves all the treatment incomplete and runs away without informing the hospital staff, it is called absconding.
- Transfer to another hospital When the patient is referred to another hospital so that he can get better or specialist service.
∆ Steps of Discharge:- - Take special care that the patient has the return consent for discharge and follow up.
- Inform the patient about all types of diet, medication and activity, exercise.
- Get him to sign the LAMA.
- Ask him to pack all the belongings in such a way that nothing is forgotten.
- Give a discharge slip with a follow up care.
- Complete the records and reports.
- Take care of the unit after discharge.
- Cure and Discharge: When the patient’s treatment is complete and the patient is discharged as per the doctor’s order.
- LAMA:-When the client wants to stop taking the treatment on his own will and goes against the doctor’s medical advice and asks for discharge, it is called LAMA.
- Abscond:-When the patient leaves all the treatment incomplete and runs away without informing the hospital staff, it is called abscond.
- Transfer to another hospital when the patient is referred to another hospital so that he can get better or specialist service.
∆ Steps of Discharge:- - Special care should be taken that the patient has a return consent for discharge and follow up.
- Inform the patient about all the types of diet, medication and activity, exercise.
- Getting the LAMA signed.
- Asking to pack all the belongings in such a way that nothing is forgotten.
- Giving a discharge slip with a follow up care.
- Completing records and reports.
- Post discharge care of the unit.
- ∆ Post Discharge unit care
- Cleaning the room before the admission of another patient.
- Prepare to send any articles used to the UTDT room and reuse them.
- Discard any items
- Send used linen to the laundry.
- If any patient had a communicable disease, get the room fumigated.
- ∆ Transfer procedure:
- (1) Transfer from one department to another
- The doctor in charge will write the order.
- The entire procedure should be done like the discharge procedure. Records and reports should be taken along with the nurse or doctor of the department where the patient is transferred and everything should be checked and admitted.
- The patient should be taken in a wheelchair or stretcher
- The entire procedure should be explained to the patient’s relatives
- (2) Transfer from one hospital to another
- Tell the patient’s relatives the purpose of the transfer.
- This procedure should also be done like the discharge procedure.
- All the information about the patient’s condition should be available to the doctor of the hospital where the patient is transferred.
Published
Categorized as GNM-FUNDAMENTAL-FULL COURSE, Uncategorised